DRUGS USED IN PEPTIC ULCER DISEASE Pathophysiology Most


- Slides: 45
DRUGS USED IN PEPTIC ULCER DISEASE
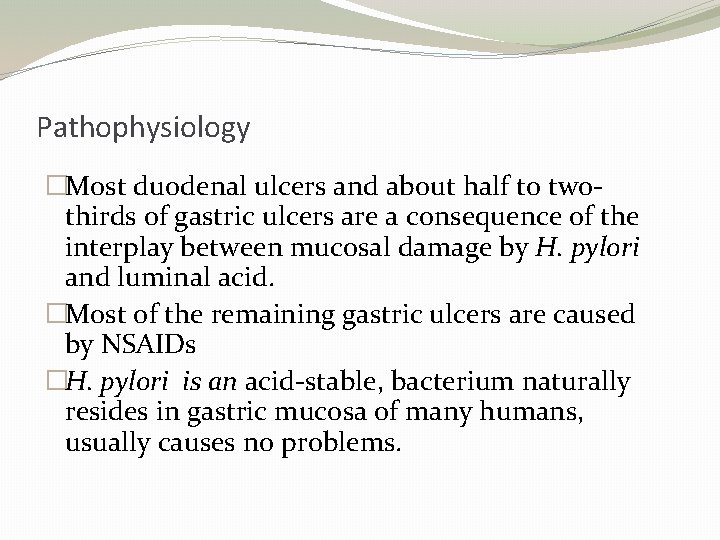
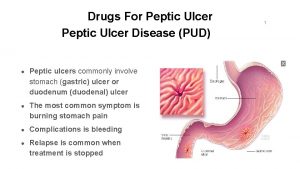
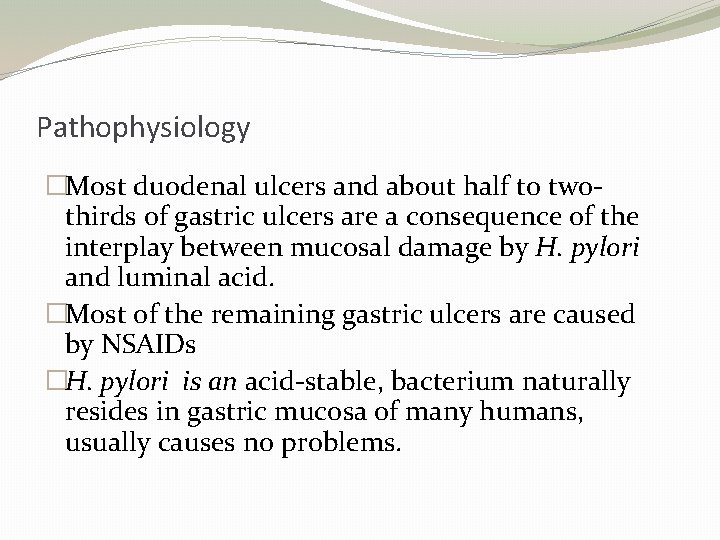
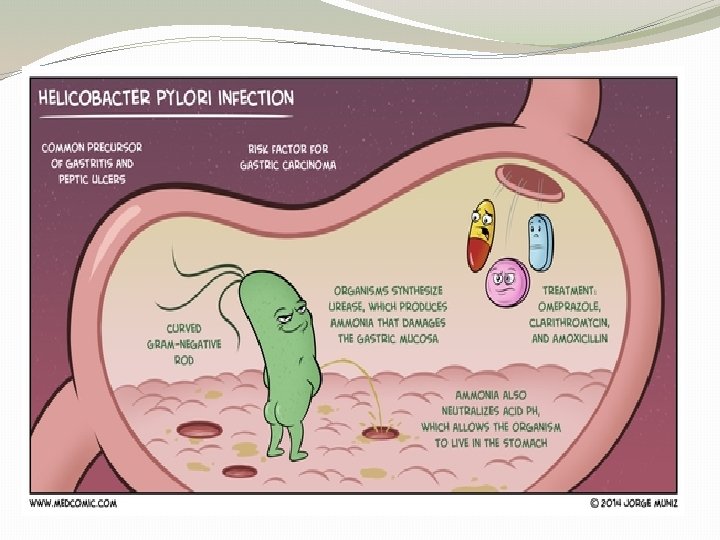
Pathophysiology �Most duodenal ulcers and about half to twothirds of gastric ulcers are a consequence of the interplay between mucosal damage by H. pylori and luminal acid. �Most of the remaining gastric ulcers are caused by NSAIDs �H. pylori is an acid-stable, bacterium naturally resides in gastric mucosa of many humans, usually causes no problems.
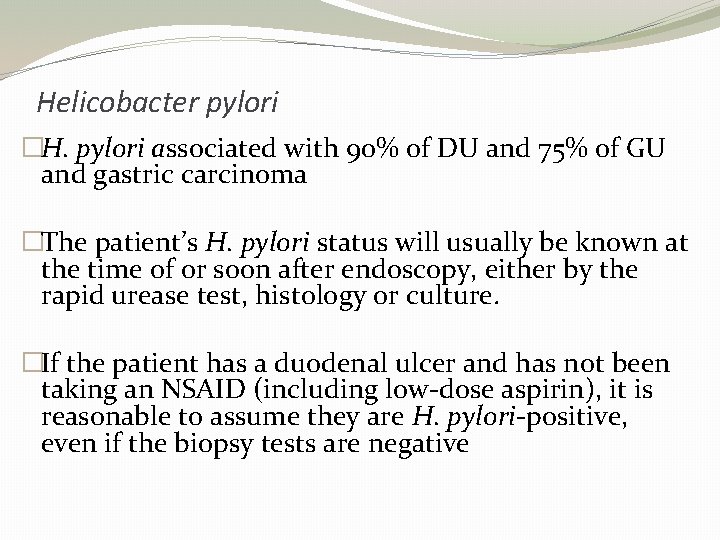
Helicobacter pylori �H. pylori associated with 90% of DU and 75% of GU and gastric carcinoma �The patient’s H. pylori status will usually be known at the time of or soon after endoscopy, either by the rapid urease test, histology or culture. �If the patient has a duodenal ulcer and has not been taking an NSAID (including low-dose aspirin), it is reasonable to assume they are H. pylori-positive, even if the biopsy tests are negative
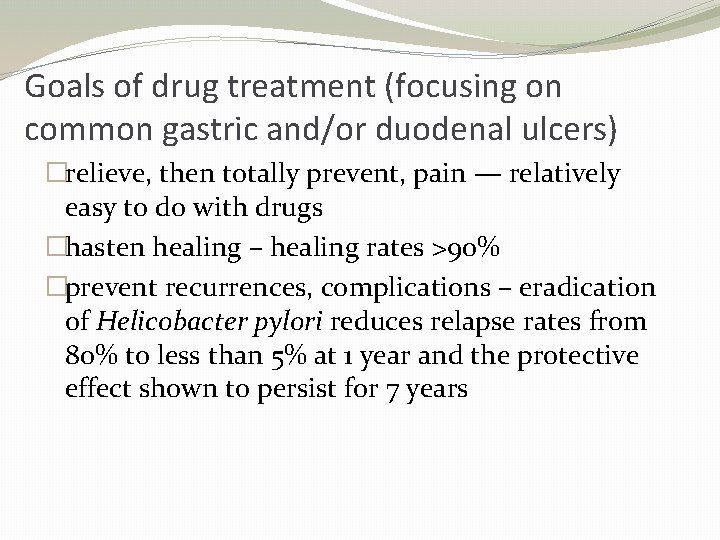
Goals of drug treatment (focusing on common gastric and/or duodenal ulcers) �relieve, then totally prevent, pain — relatively easy to do with drugs �hasten healing – healing rates >90% �prevent recurrences, complications – eradication of Helicobacter pylori reduces relapse rates from 80% to less than 5% at 1 year and the protective effect shown to persist for 7 years
Management of peptic ulcer �Previously, divided into 2 stages: �First, the healing of the acute ulcer; and �second, maintenance treatment to prevent recurrence. �Now not recommended for the great majority of patients with H. pylori-induced ulcers. �Eradication of the bacterium should be attempted at the same time as therapy is given to heal the ulcer.
Eradication regimens �No need to continue antisecretory treatment if successfully treated with PPI and antibiotics, unless complicated by haemorrhage or perforation �The currently recommended eradication regimens include at least one agent that has ulcer-healing efficacy in its own right, eg proton pump inhibitor (PPI), histamine H 2 -receptor antagonist or bismuth plus two antibiotics: amoxicillin plus clarithromycin or metronidazole
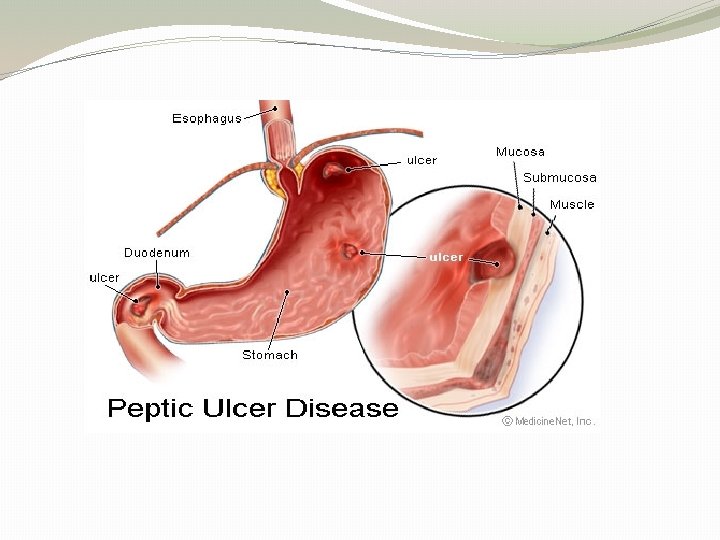
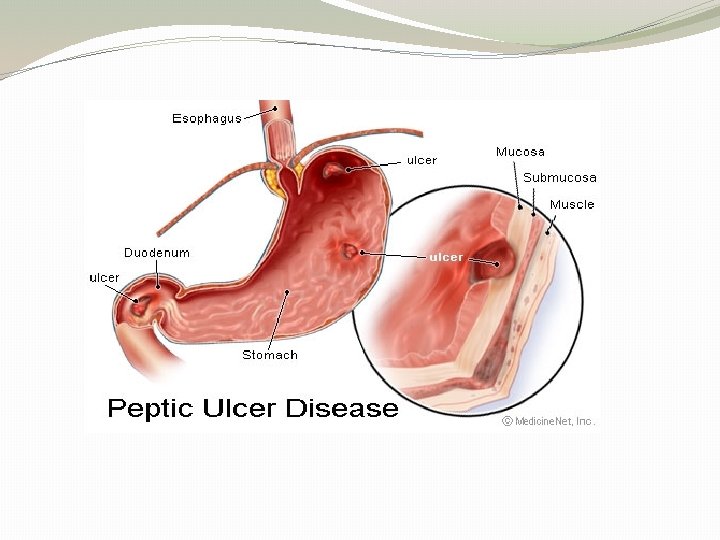
What is peptic ulcer disease (PUD)? �The term PUD generally refers to spectrum of disorders that includes Ø gastric ulcer (GU) Ø pyloric channel ulcer Ø duodenal ulcer (DU) Ø postoperative ulcers at or near the site of surgical anastomosis.
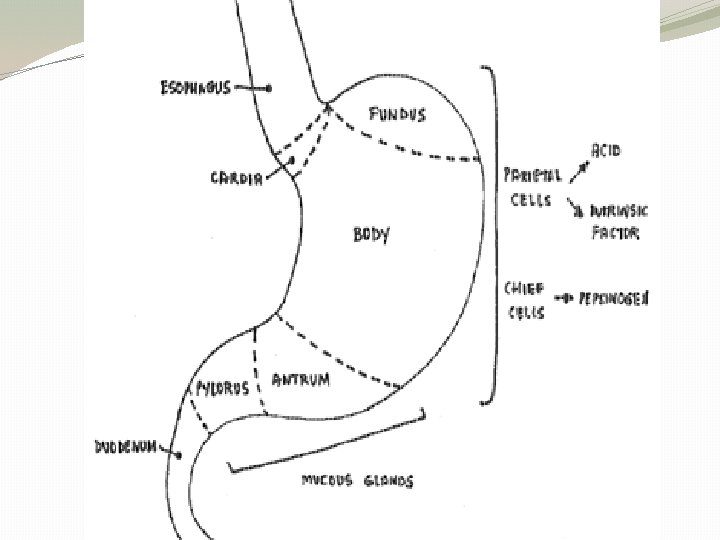
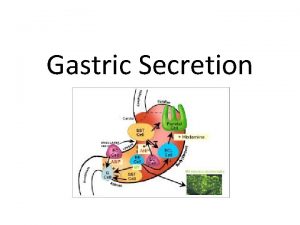
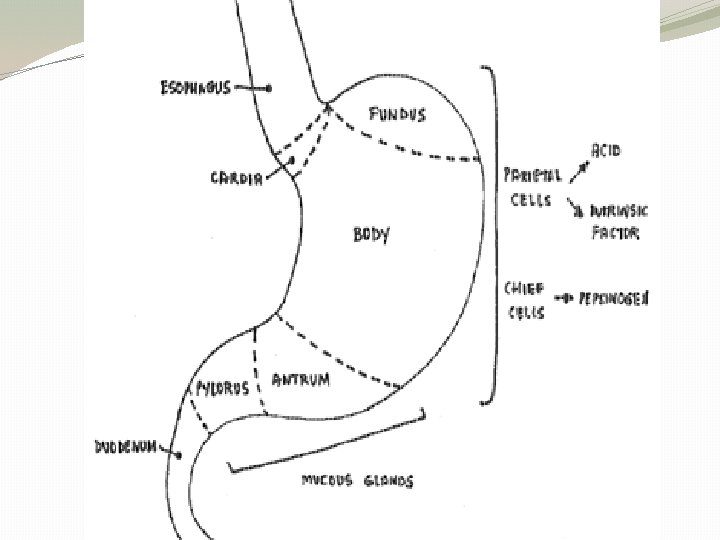
Regulation of gastric acid secretion �Terminal enzyme H+K+ATPase (protone pump)secretes H+ ions �Proton pump is activated by histamine, ACh & gastrin acting via receptors located in the basolateral membranes of parietal cells. �Histamine acting through H 2 receptors predominant role. �Gastrin and Ach act partly directly & partly indirectly by releasing histamine.
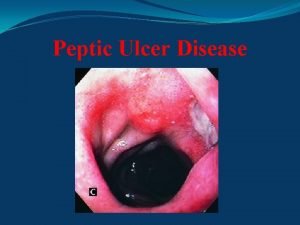
Peptic ulcer
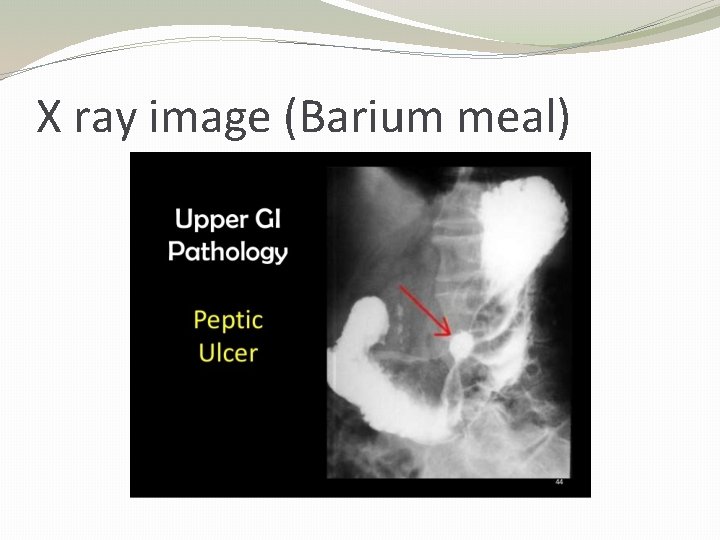
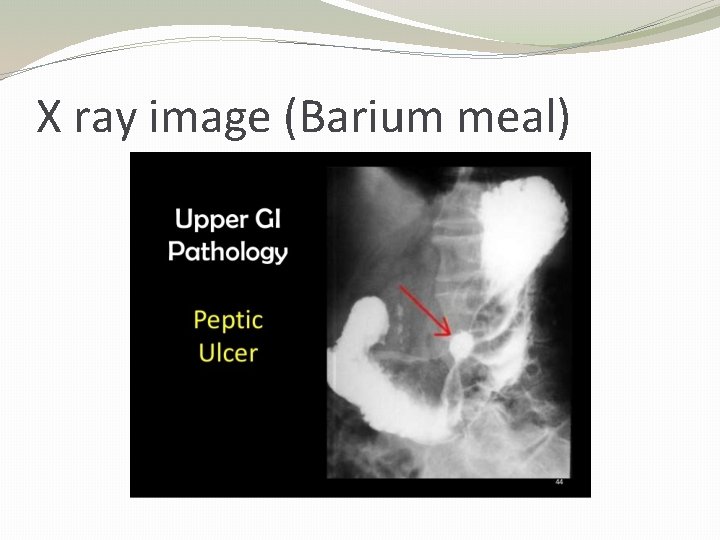
X ray image (Barium meal)
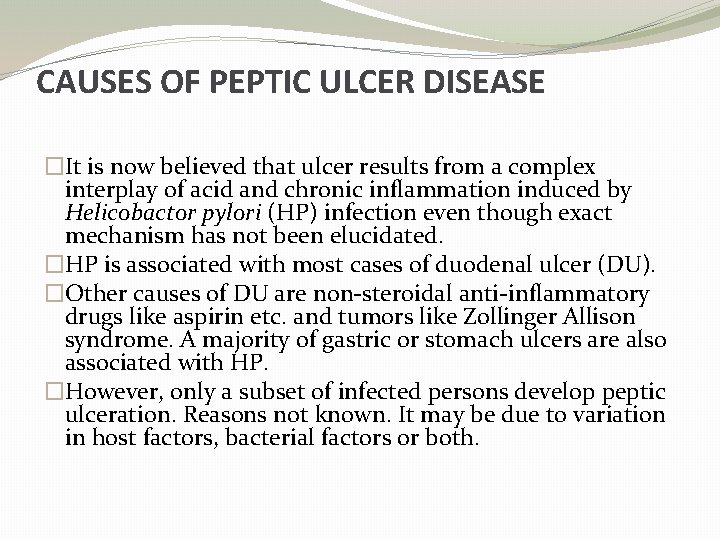
CAUSES OF PEPTIC ULCER DISEASE �It is now believed that ulcer results from a complex interplay of acid and chronic inflammation induced by Helicobactor pylori (HP) infection even though exact mechanism has not been elucidated. �HP is associated with most cases of duodenal ulcer (DU). �Other causes of DU are non-steroidal anti-inflammatory drugs like aspirin etc. and tumors like Zollinger Allison syndrome. A majority of gastric or stomach ulcers are also associated with HP. �However, only a subset of infected persons develop peptic ulceration. Reasons not known. It may be due to variation in host factors, bacterial factors or both.

Drugs to treat peptic ulcer �Antacids �Histamine H 2 -receptor antagonists �Proton pump inhibitors �Cytoprotective agents (eg bismuth, sucralfate) �Prostaglandin analogues (eg misoprostol) �Antibiotics for Helicobacter
Antacids �Neutralizes acid in gut lumen. �Many different antacid preparations �For symptomatic treatment of peptic ulcers mainly. �The most common preparations contain a mixture of aluminium hydroxide (digene) and magnesium hydroxide. ( milk of magnesia) � �Aluminium salts cause constipation while magnesium salts cause diarrhoea. Thus a combination of the two tends to have the least overall effect on gastrointestinal function.
�Some antacid preparations contain sodium, so care is required in patients with hypertension or cardiac, renal or liver disease, and in paediatric patients with diarrhoea or dehydration. �Sugar is present in some preparations, so care may be required in diabetic patients.
Histamine H 2 -receptor antagonists �Cimetidine, famotidine, and ranitidine �They are structurally related to histamine and are more potent at blocking histamine H 2 receptors, present principally in the gastric mucosa, than the more widespread histamine H 1 receptors.
Histamine H 2 -receptor antagonists �Well absorbed orally, although absorption is reduced by concurrent administration of antacids. �The plasma half-live is short but the duration of action allows for once- or twice-daily dosing. �Mainly excreted renally so dose reductions may be required in patients with significant renal impairment.
Histamine H 2 -receptor antagonists �In therapeutic doses, cimetidine inhibits liver oxidative enzymes (such as CYP 450) thus decreasing the metabolism of such drugs as warfarin, phenytoin, carbamazepine, prednisolone and theophylline. �Ranitidine & famotidine have much lower (and probably clinically insignificant) effects on liver metabolic activity when given in usual therapeutic doses.
Histamine H 2 -receptor antagonists �Adverse effects are uncommon with these agents but all of them can occasionally cause blood dyscrasias (presence of abnormal material in the blood, usually applied to diseases affecting blood cells or platelets. ) and skin rashes. �In therapeutic doses, cimetidine also causes gynaecomastia and can occasionally cause confusional states, particularly in the elderly and in patients with renal failure.
Proton pump inhibitors � These agents inhibit the enzyme hydrogen potassium adenosine triphosphatase, which is the final common pathway of acid secretion. � Thus suppress acid secretion irrespective of the stimulus to acid production. � Can abolish resting and stimulated acid secretion. � They have no significant direct effect on acetylcholine or histamine receptors. � Omeprazole, lansoprazole, pantoprazole, rabeprazole and esomeprazole
�Because they inhibit acid secretion regardless of the stimulus, suppression of acid production is more complete than with other agents such as the histamine H 2 -receptor antagonists. �Proton pump inhibitors (PPIs) have also been shown to heal ulcers more rapidly than other antiulcerants.
�Despite their short plasma half-lives—lansoprazole 1 to 2 hours, omeprazole 40 minutes, pantoprazole 1 hour, rabeprazole 0. 7 to 1. 5 hours and esomeprazole 2 hours—these drugs produce prolonged acid suppression for up to 24 hours.
�For peptic ulcer disease due to Helicobacter pylori, the PPIs are now commonly used in combination with antibiotics over a 1 - to 2 -week period. � Follow-up treatment for 4 to 8 weeks with either a histamine H 2 -receptor antagonist or a PPI may be indicated in some circumstances
�Lansoprazole and pantoprazole are well absorbed and exhibit high bioavailability. �Omeprazole has rather poor and variable bioavailability, which increases during treatment as gastric acid secretion is inhibited. �PPIs are extensively metabolised in the liver, and renal clearance of inactive metabolites is the major route of elimination. �Dose adjustment is not necessary either in patients with renal impairment or in those with mild to moderate hepatic impairment.
�Clarithromycin inhibits one major pathway of omeprazole metabolism—metabolism by cytochrome P 450 3 A 4 (CYP 3 A 4)—thus substantially increasing omeprazole plasma concentrations.
�Omeprazole has slight, but significant, inhibitory effects on hepatic oxidative enzymes, and it has been shown to significantly enhance the effects of phenytoin and warfarin, requiring increased monitoring of these drugs. �As yet, significant interactions with other drugs have not been identified. �Lansoprazole is a weak inducer of cytochrome P 450, but while there is a possibility of interactions with other drugs metabolised by this system, no clinical effects have been observed with diazepam, phenytoin or warfarin.
Cytoprotective agents Bismuth �It is not known exactly how bismuth subcitrate heals ulcers. �It is thought, however, to precipitate at the ulcer site under the influence of gastric acid, and bond with proteins to form an insoluble protective layer over the ulcer. �Systemic adverse effects are rare because systemic absorption of bismuth is minimal. �However, the drug is renally excreted and therefore should not be used in patients with renal failure, because the small amounts of bismuth absorbed may accumulate and are capable of producing neurotoxicity
�Adverse effects of bismuth include blackening of the faeces and occasional nausea and vomiting. A black coating of the tongue and dental plaque are also common. �Because gastric acid is required for bismuth to have its effect, the drug must be given 1 hour before meals. These factors may significantly influence compliance. �Concomitant administration of antacids or inhibitors of gastric acid secretion may also reduce bismuth’s efficacy. �Probably because bismuth has activity against H. pylori, recurrence of ulceration after a course of the drug is less frequent than after ulcer healing by other agents.
Sucralfate �Sucralfate is an aluminium salt of a sulfated disaccharide similar to sucrose. �It produces an adherent cytoprotective barrier over ulcers by complexing with proteins, pepsin and bile. �Its effect is entirely local on the peptic ulcer and only extremely small amounts of aluminium are absorbed systemically. �Because of its lack of systemic absorption, sucralfate causes very few systemic adverse effects, although constipation may sometimes occur.
Sucralfate �Even though systemic absorption is limited, longterm sucralfate therapy should not be used in patients with renal impairment because even the small amounts of aluminium absorbed may then accumulate and cause adverse effects �Sucralfate must be ingested at least 1 hour before meals because an acid environment is required for it to be effective. �Concomitant administration of antacids or inhibitors of gastric acid secretion reduce its efficacy.
Prostaglandin analogues Misoprostol � Misoprostol is a synthetic analogue of prostaglandin that both inhibits gastric acid secretion and produces mucosal cytoprotection. � Its cytoprotective effect is particularly evident against mucosal damage produced by nonsteroidal anti-inflammatory drugs, including aspirin. � Misoprostol is rapidly absorbed and has a short plasma half-life of approximately 30 minutes. It is metabolised to a variety of fatty acid products, most of which are excreted in the urine. � major adverse effects of misoprostol are diarrhoea, abdominal pain and loose stools. � may occasionally suffer menorrhagia or an accentuation of dysmenorrhoea. � Misoprostol is an abortifacient so it must not be used in pregnancy.
Antibiotics for Helicobacter pylori � There has been a shift in the treatment of peptic ulcer disease following recognition of the central role of H. pylori in the pathogenesis of duodenal ulcer and, to a lesser but still important extent, gastric ulcer. � The current approach is to use antibiotics together with antisecretory agents to eradicate the organism, cure ulceration and minimise the risk of relapse, rather than use long-term antisecretory therapy. � Antibiotics currently used against H. pylori include amoxycillin, clarithromycin, metronidazole and tetracycline. These are used in combination with antisecretory drugs in three- and occasionally fourdrug regimens. � The choice of drugs used for these combinations will continue to change as resistance patterns evolve over time.
Eradication of H. pylori and ulcer healing First-line therapy Treatments to eradicate H. pylori are continually evolving. omeprazole 20 mg orally, twice daily for 7 days PLUS clarithromycin 500 mg orally, twice daily for 7 days PLUS amoxycillin 1 g orally, twice daily for 7 days.
For patients hypersensitive to penicillin, substitute amoxycillin with metronidazole. Use omeprazole 20 mg orally, twice daily for 7 days PLUS clarithromycin 500 mg orally, twice daily for 7 days PLUS metronidazole 400 mg orally, 3 times daily for 7 days.
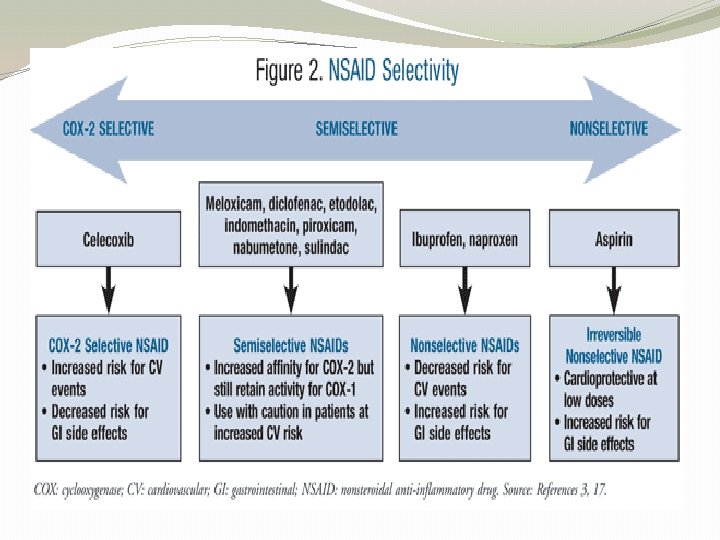
NSAID-induced ulcers Treatment �Most NSAID-induced ulcers (including those caused by lowdose aspirin) are gastric—they account for about 30% to 50% of all gastric ulcers. �Giving the NSAID as a suppository or with an enteric coating does not reduce the risk of gastric injury. �The treatment of choice is to stop the NSAID. �If the NSAID cannot be stopped, heal NSAID-induced gastric or duodenal ulcers with omeprazole 20 mg orally, daily each morning for 4 to 8 weeks.
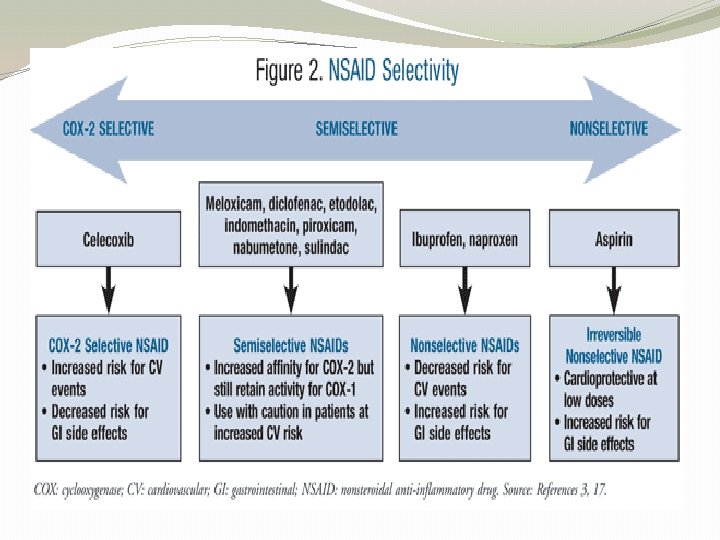
NSAID-induced ulcers Prophylaxis �The best prophylaxis is avoidance of unnecessary NSAID therapy, especially in noninflammatory arthritis where paracetamol is often sufficient. �If an NSAID is necessary, use the lowest dose possible. �There are differences in the ability of NSAIDs to cause gastric injury, � Eg : - there is higher risk of gastric ulceration with longer-acting NSAIDs such as piroxicam and ketoprofen and lower risk with shorter-acting NSAIDs such as ibuprofen and diclofenac. �The risk of ulceration is also reduced in patients taking highly selective COX-2 inhibitors.
NSAID-induced ulcers �When nonselective NSAIDs are used, the risk of developing an NSAID ulcer (duodenal or gastric) can be reduced by 60% to 80% (depending on the agent) by taking concomitant omeprazole or double-dose famotidine. �Concomitant administration of synthetic prostaglandin misoprostol reduces the incidence of gastric and duodenal ulceration
�Standard doses of histamine H 2 -receptor antagonists have been shown to be an ineffective form of prophylaxis against the development of gastric ulcers, although ranitidine has been shown to prevent the less common problem of duodenal ulcers. �For cost-benefit reasons, prophylaxis is advised only for high-risk patients, �Eg Ø the elderly, those with a prior ulcer (especially those who have bled from an ulcer) Ø those with serious concomitant disease who would tolerate an ulcer bleed poorly Ø those taking high-dose NSAIDs, longer-acting NSAIDs and/or corticosteroids.

Questions ?
THANK YOU
 Morphology of peptic ulcer
Morphology of peptic ulcer Pud triple therapy
Pud triple therapy Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease Triple therapy for peptic ulcer disease
Triple therapy for peptic ulcer disease Patient counselling for peptic ulcer disease
Patient counselling for peptic ulcer disease Peptic ulcer disease
Peptic ulcer disease What is emetics
What is emetics Ajeerna symptoms
Ajeerna symptoms Vicaline pill application
Vicaline pill application Gastric ulcer vs duodenal ulcer
Gastric ulcer vs duodenal ulcer Stomach ulcer definition
Stomach ulcer definition Turburculousis
Turburculousis Proton pump inhibitor
Proton pump inhibitor Peptic ulcer diseas
Peptic ulcer diseas Acholorhydria
Acholorhydria Gastric ucler
Gastric ucler Tea pot deformity
Tea pot deformity Typhoid and tuberculous ulcer
Typhoid and tuberculous ulcer Ulcer niche and ulcer notch
Ulcer niche and ulcer notch Pathophysiology of hirschsprung disease
Pathophysiology of hirschsprung disease Mitral regurgitation symptoms
Mitral regurgitation symptoms Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Pathophysiology of ischemic heart disease
Pathophysiology of ischemic heart disease Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Nursing assessment for congestive heart failure
Nursing assessment for congestive heart failure Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Coronary artery disease pathophysiology
Coronary artery disease pathophysiology Disease modifying antirheumatic drugs
Disease modifying antirheumatic drugs Communicable disease and non communicable disease
Communicable disease and non communicable disease Composition of gastric acid
Composition of gastric acid Etanacept
Etanacept Seven tray in labour room
Seven tray in labour room Pregnancy medicine list pdf
Pregnancy medicine list pdf Pathophysiology of kidney stones
Pathophysiology of kidney stones Dumping syndrome pathophysiology
Dumping syndrome pathophysiology Petroleum gauze
Petroleum gauze Pathophysiology of tonsillitis
Pathophysiology of tonsillitis Hepatic encephalopathy pathophysiology
Hepatic encephalopathy pathophysiology Thyroglossal cyst pathophysiology
Thyroglossal cyst pathophysiology Thyroid storm รักษา
Thyroid storm รักษา Neonatal sepsis pathophysiology diagram
Neonatal sepsis pathophysiology diagram Pathophysiology signs and symptoms
Pathophysiology signs and symptoms Acholia causes
Acholia causes Chronic calculous cholecystitis
Chronic calculous cholecystitis Nursing interventions for thyroid storm
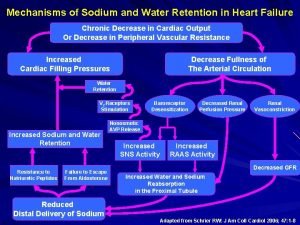
Nursing interventions for thyroid storm Pathophysiology of sodium and water retention
Pathophysiology of sodium and water retention