Disorders of Apocrine Glands Presenter Dr Thansiha Nargis

- Slides: 66
Disorders of Apocrine Glands Presenter: Dr. Thansiha Nargis Moderator: Dr. Spandana Hegde 26/8/2015
Content �Introduction �Anatomy �Composition �Disorders of apocrine glands • Bromhidrosis • Chromhidrosis • Fox–fordyce disease • Hidradenitis suppurativa
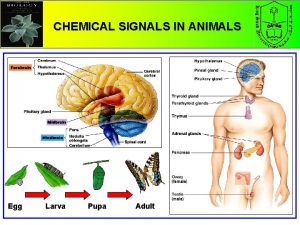
Introduction �Types of sweat glands �Eccrine �Apocrine �Eccrine- body to control its internal temperature in response to thermal stress �Apocrine : obscure but includes pheromone production
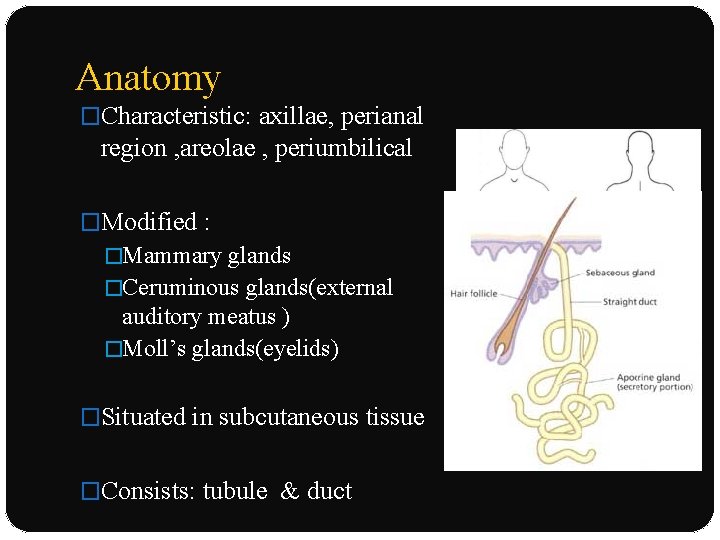
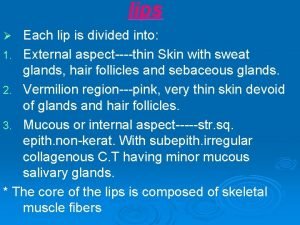
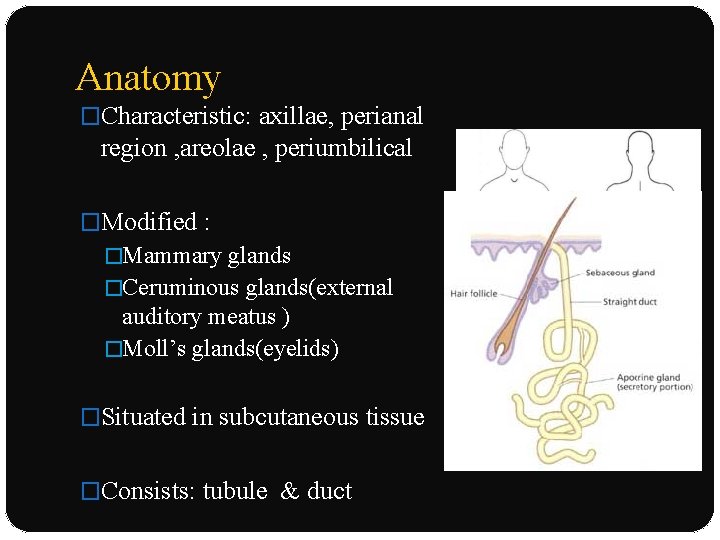
Anatomy �Characteristic: axillae, perianal region , areolae , periumbilical �Modified : �Mammary glands �Ceruminous glands(external auditory meatus ) �Moll’s glands(eyelids) �Situated in subcutaneous tissue �Consists: tubule & duct
Composition of secretion �Apocrine sweat : milky, viscid, without odor. � 3 precursors: fatty acids, sulfanyl alkanols , odiferous steroids �Corynebacterium striatum, convert it into odiferous substances
Disorders of Apocrine Gland
Bromhidrosis �Osmidrosis : body odour seen postpuberty �Bromhidrosis: eccrine or apocrine origin �Apocrine bromhidrosis : offensive or unpleasant body odor arising from apocrine gland secretions �Seen : axillae
Epidemiology �After puberty �No geographic predilection : summer months or warm climates - aggravate the disease �Poor personal hygiene
Etiology and Pathogenesis � Apocrine secretion -odourless : becomes odorous only after some hours 1. Odorous steroid secretion 2. Presence of axillary microflora 3. Eccrine sweat production
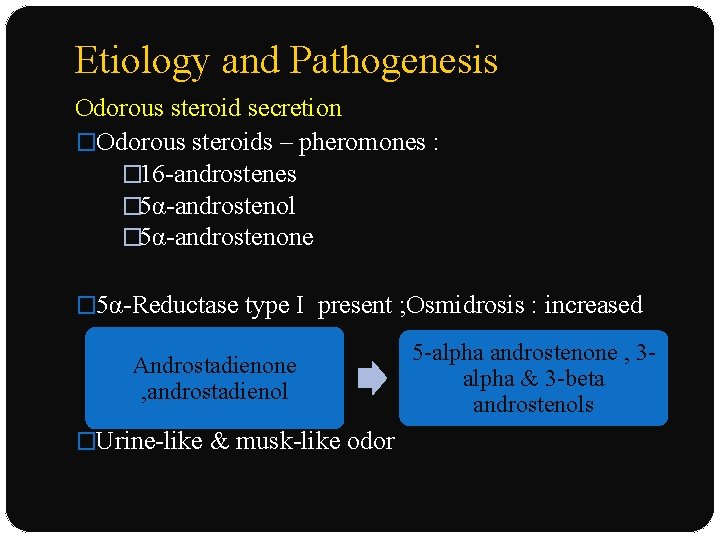
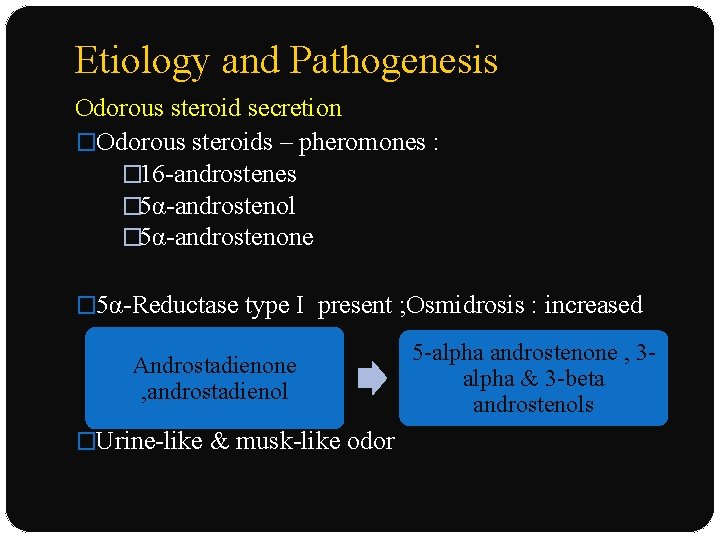
Etiology and Pathogenesis Odorous steroid secretion �Odorous steroids – pheromones : � 16 -androstenes � 5α-androstenol � 5α-androstenone � 5α-Reductase type I present ; Osmidrosis : increased Androstadienone , androstadienol �Urine-like & musk-like odor 5 -alpha androstenone , 3 alpha & 3 -beta androstenols
Etiology and Pathogenesis Presence of Axillary microflora �Hosts bacteria : aerobic Corynebacterium species : C. xerosis �Production: ammonia & short chain fatty acids: ε-3 - methyl-2 -hexenoic acid �Increased axillary p. H facilitate overgrowth of bacteria
Etiology and Pathogenesis Eccrine sweat production �Effect of hyperhidrosis on bromhidrosis is unclear �Eccrine bromhidrosis : action of bacteria on keratin : softened by eccrine secretions
Clinical features HISTORY: �C/o an unpleasant body odor �Axillae : most common : genitals or plantar feet may also be affected �Axillary odor : rancid, acrid, musty, pungent, fecal �Sweat retention : axillary hair & clothing enhance odor
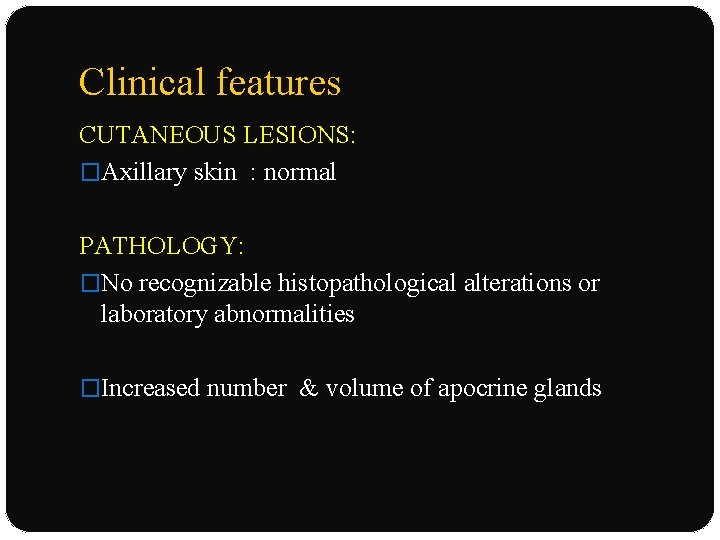
Clinical features CUTANEOUS LESIONS: �Axillary skin : normal PATHOLOGY: �No recognizable histopathological alterations or laboratory abnormalities �Increased number & volume of apocrine glands
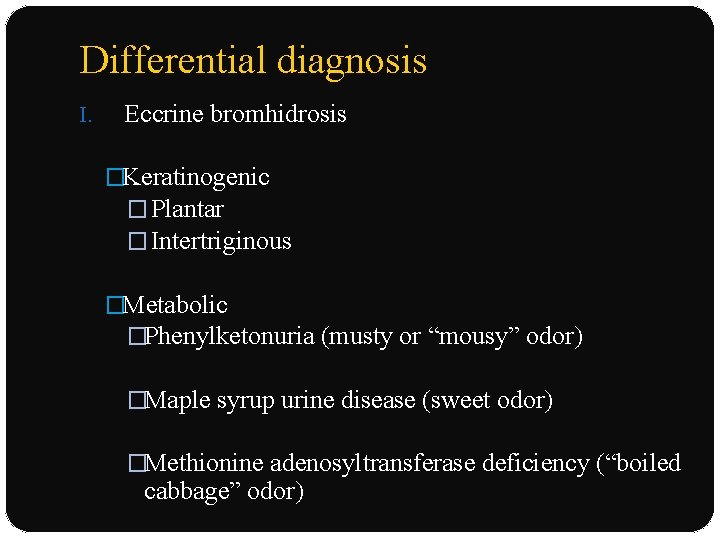
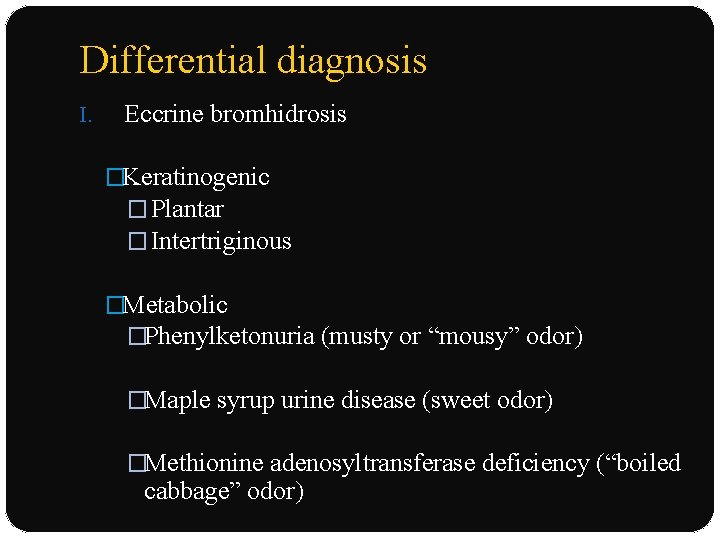
Differential diagnosis I. Eccrine bromhidrosis �Keratinogenic � Plantar � Intertriginous �Metabolic �Phenylketonuria (musty or “mousy” odor) �Maple syrup urine disease (sweet odor) �Methionine adenosyltransferase deficiency (“boiled cabbage” odor)
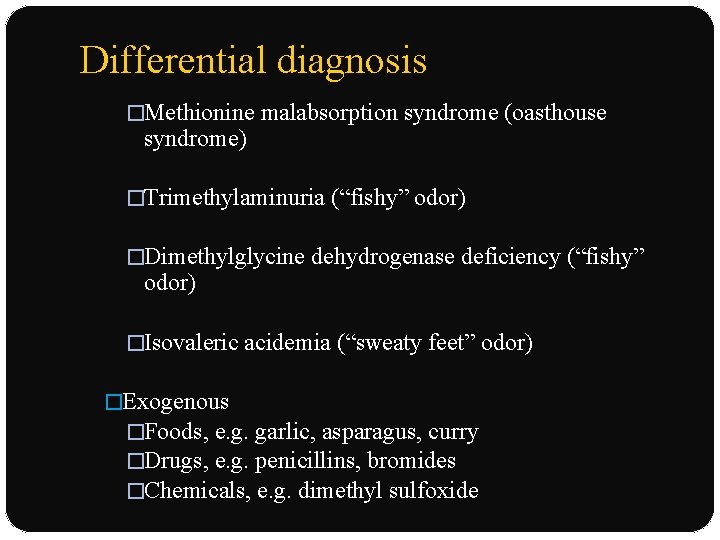
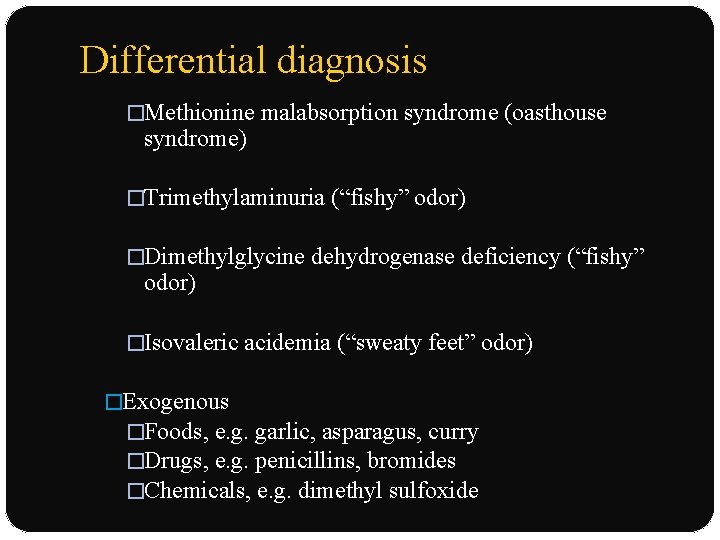
Differential diagnosis �Methionine malabsorption syndrome (oasthouse syndrome) �Trimethylaminuria (“fishy” odor) �Dimethylglycine dehydrogenase deficiency (“fishy” odor) �Isovaleric acidemia (“sweaty feet” odor) �Exogenous �Foods, e. g. garlic, asparagus, curry �Drugs, e. g. penicillins, bromides �Chemicals, e. g. dimethyl sulfoxide
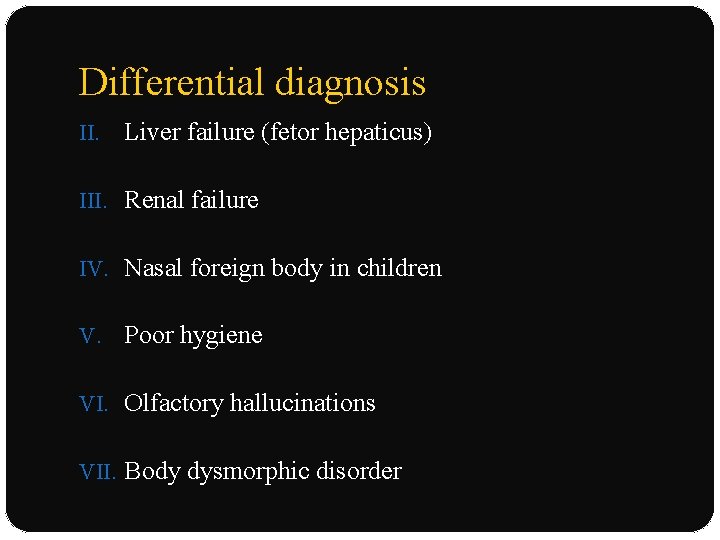
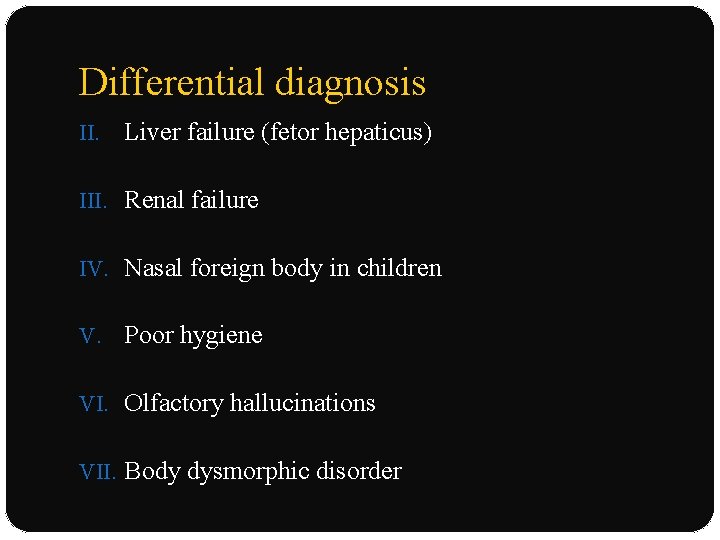
Differential diagnosis II. Liver failure (fetor hepaticus) III. Renal failure IV. Nasal foreign body in children V. Poor hygiene VI. Olfactory hallucinations VII. Body dysmorphic disorder
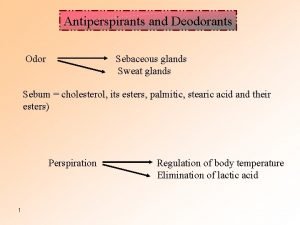
Treatment GENERAL MEASURES �Frequent washing �Use : deodorant or antiperspirant (aluminium chloride) or perfumes �Changing of soiled clothing �Remove axillary hair �Antibacterial soaps or topical antibacterial agents

Treatment NONSURGICAL THERAPY �Injection : botulinum toxin A �Frequency doubled, 1444 nm Q-switched Nd: YAG laser
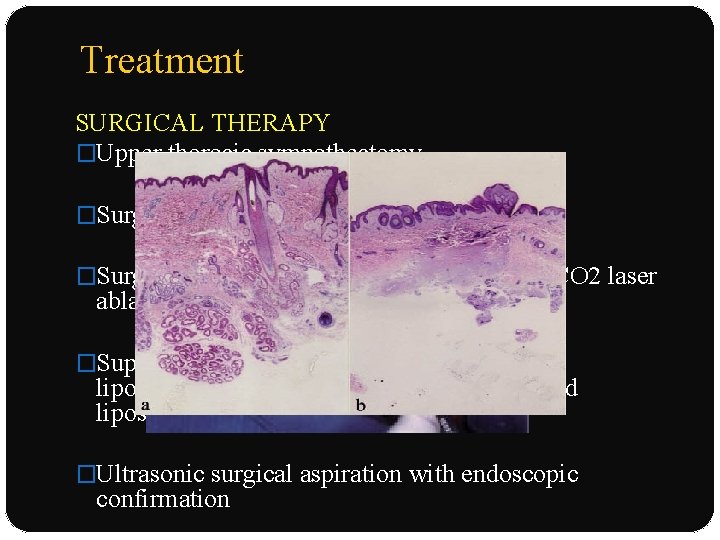
Treatment SURGICAL THERAPY �Upper thoracic sympathectomy �Surgical removal : apocrine glands �Surgical subcutaneous tissue removal with CO 2 laser ablation �Superficial liposuction, tumescent superficial liposuction with curettage, ultrasound-assisted liposuction �Ultrasonic surgical aspiration with endoscopic confirmation
Prognosis & clinical course �Chronic & nonremitting condition �Feel self-conscious & embarrassed �Develop impairment with psychosocial functioning
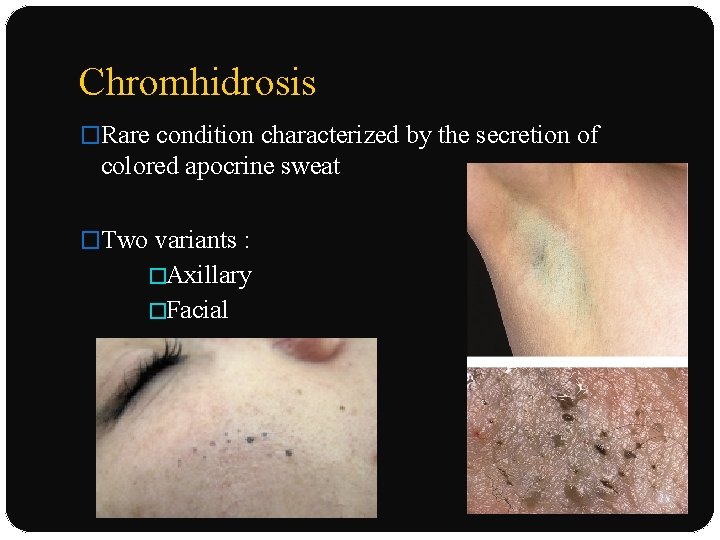
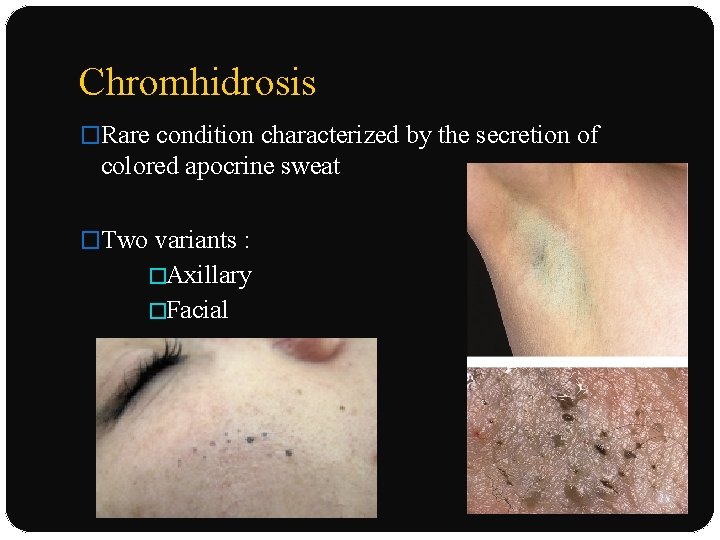
Chromhidrosis �Rare condition characterized by the secretion of colored apocrine sweat �Two variants : �Axillary �Facial
Epidemiology �Onset at puberty, at the time of increased gland activity �Persists throughout life, improving in the aged �Axillary chromhidrosis : blacks �Facial chromhidrosis occurs exclusively in whites
Etiology and pathogenesis �Pigment : lipofuscins - golden-colored pigment - apocrine secretory cells �Lipofuscin granules : higher state of oxidation; produce darker colours �Imparts various colours : yellow, green, blue, or black �Nerve endings with receptors for substance P; potent vasodilator
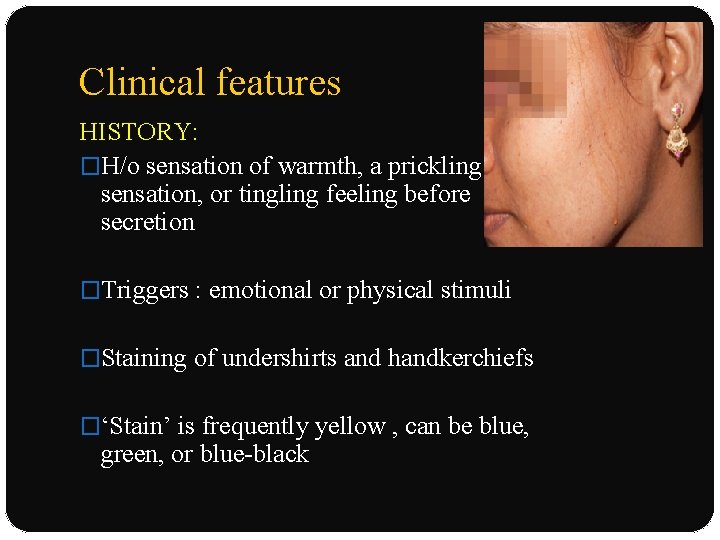
Clinical features HISTORY: �H/o sensation of warmth, a prickling sensation, or tingling feeling before secretion �Triggers : emotional or physical stimuli �Staining of undershirts and handkerchiefs �‘Stain’ is frequently yellow , can be blue, green, or blue-black
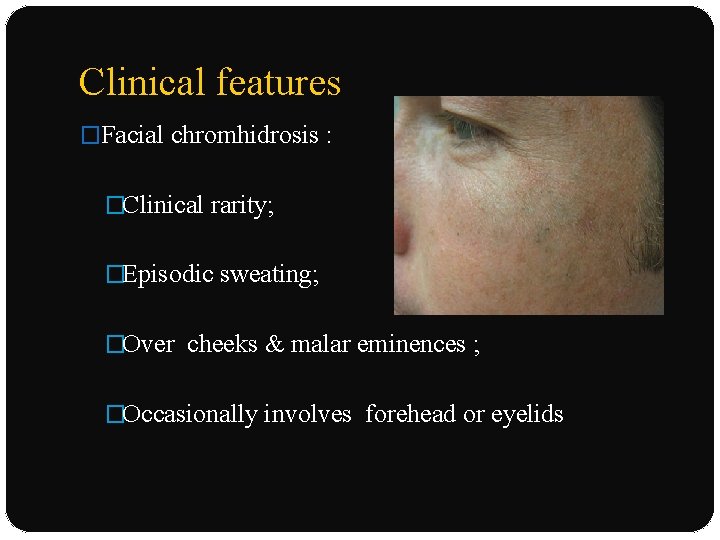
Clinical features �Facial chromhidrosis : �Clinical rarity; �Episodic sweating; �Over cheeks & malar eminences ; �Occasionally involves forehead or eyelids
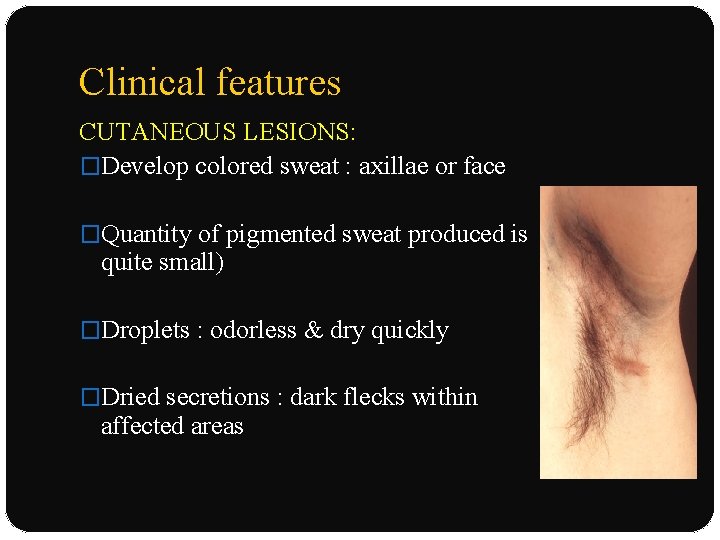
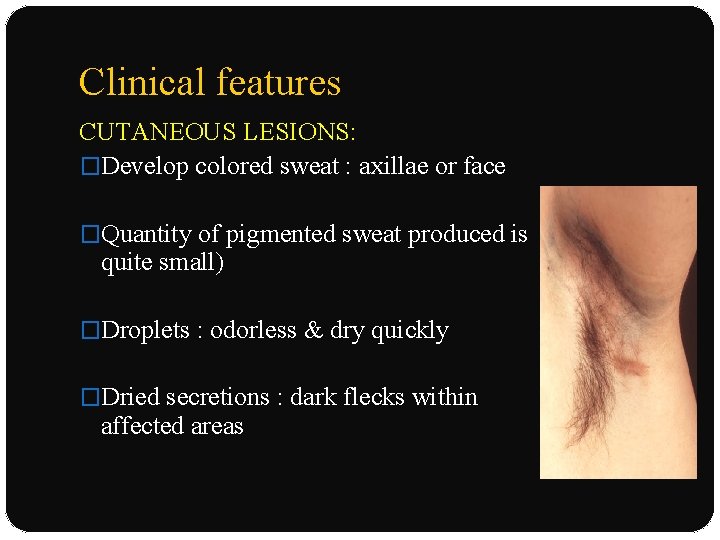
Clinical features CUTANEOUS LESIONS: �Develop colored sweat : axillae or face �Quantity of pigmented sweat produced is quite small) �Droplets : odorless & dry quickly �Dried secretions : dark flecks within affected areas
Special tests �Wood’s lamp examination �Yellow, blue, or green : yellow fluorescence �Black or brown: rarely autofluoresces �Stained clothing may fluoresce �Stimulated : injection of epinephrine or oxytocin
Laboratory tests: �Complete blood cell count : bleeding diathesis �Homogentisic levels in urine : alkaptonuria, �Bacterial & fungal cultures : pseudo-eccrine chromhidrosis
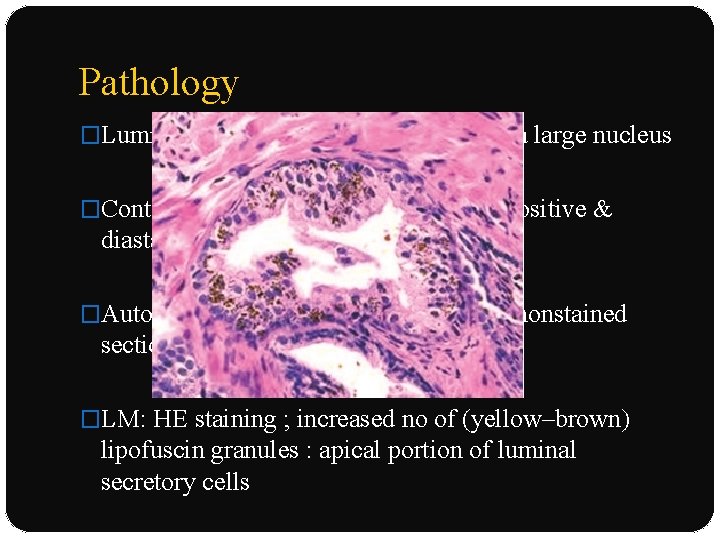
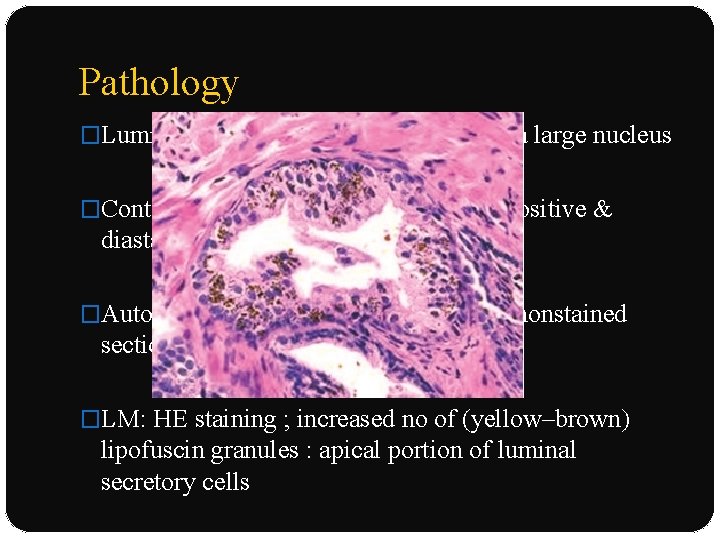
Pathology �Luminal cells : eosinophilic cytoplasm, a large nucleus �Contain lipofuscin, iron, lipid, or PAS positive & diastase-resistant granules �Autofluorescence : paraffin-embedded nonstained sections �LM: HE staining ; increased no of (yellow–brown) lipofuscin granules : apical portion of luminal secretory cells
Differential diagnosis 1. 2. 3. Eccrine chromhidrosis �Quinine ingestion Pseudo-eccrine chromhidrosis �Blue sweat with copper exposure �Extrinsic dyes, paints Alkaptonuria (ochronosis) 4. Hyperbilirubinemia 5. Hematohidrosis (bleeding diathesis) 6. Chromogenic bacteria ( Corynebacterium species), pseudomonas
Treatment �Manual expression : temporary improvement 48– 72 hrs �Botulinum toxin type A : facial chromhidrosis. �Capsaicin : topical cream : depletes & prevents reaccumulation of substance P- unmyelinated, slowconducting type C sensory fibers Prognosis & clinical course �Chronic disease ; improves in old age
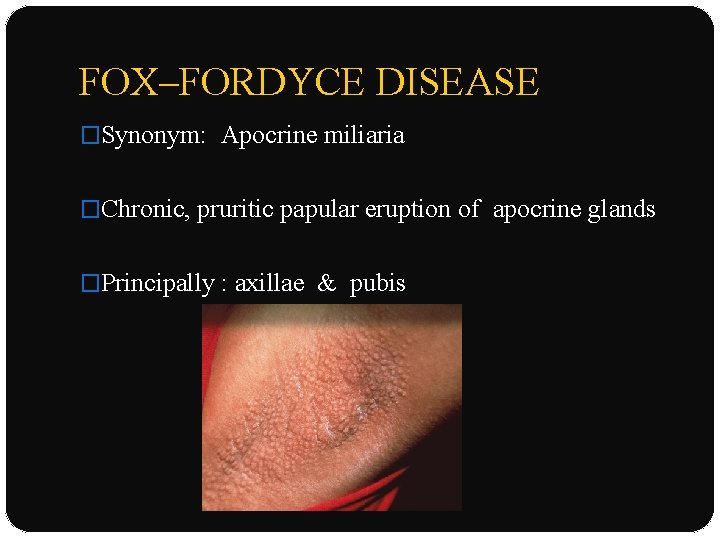
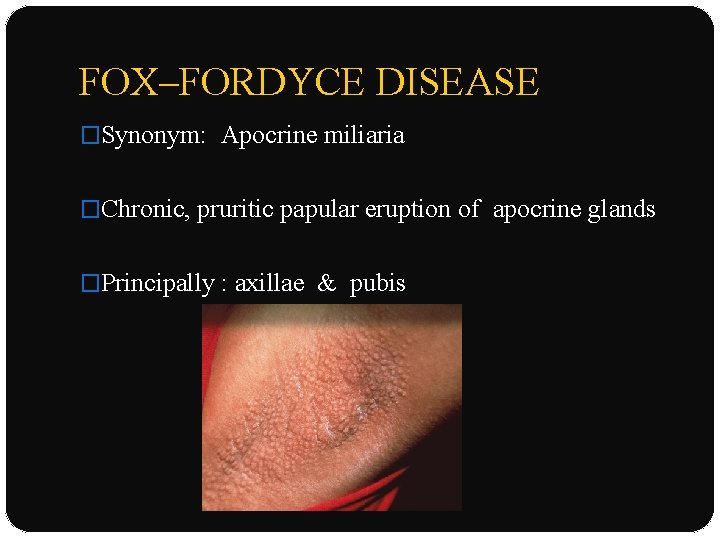
FOX–FORDYCE DISEASE �Synonym: Apocrine miliaria �Chronic, pruritic papular eruption of apocrine glands �Principally : axillae & pubis
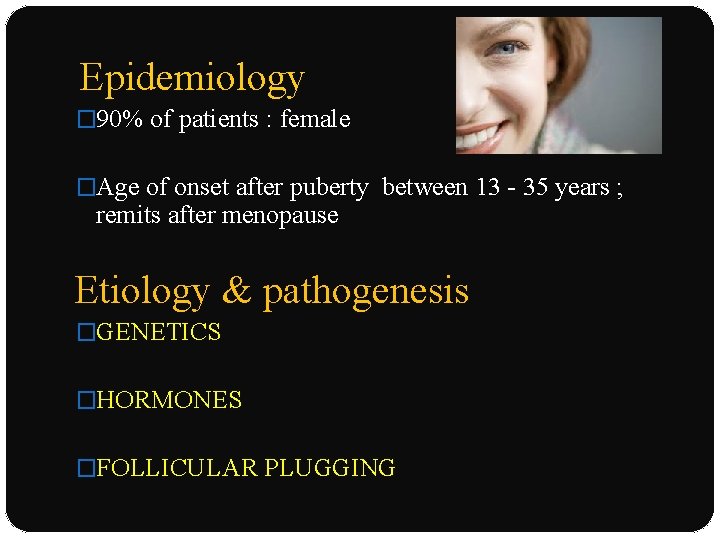
Epidemiology � 90% of patients : female �Age of onset after puberty between 13 - 35 years ; remits after menopause Etiology & pathogenesis �GENETICS �HORMONES �FOLLICULAR PLUGGING
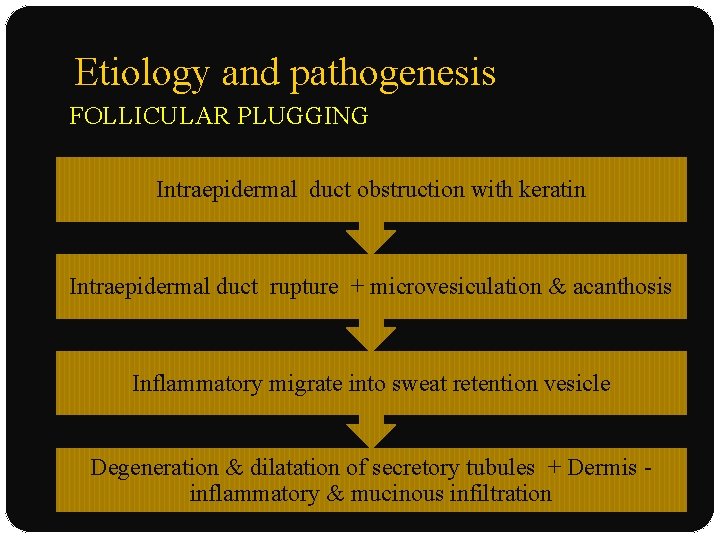
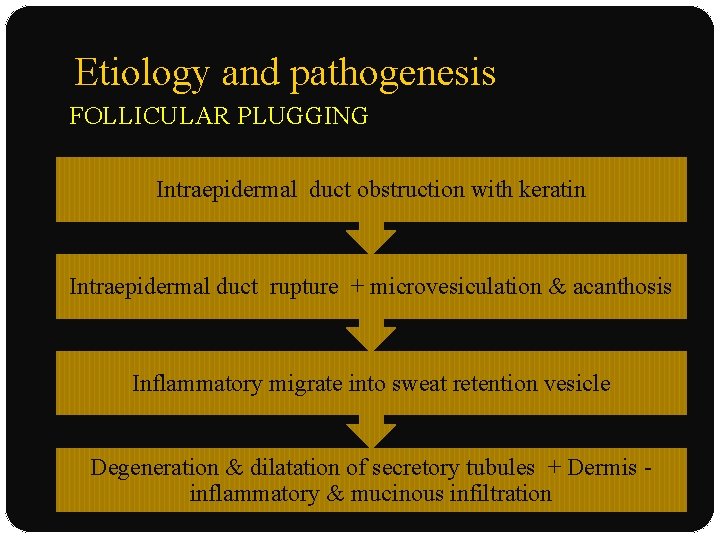
Etiology and pathogenesis FOLLICULAR PLUGGING Intraepidermal duct obstruction with keratin Intraepidermal duct rupture + microvesiculation & acanthosis Inflammatory migrate into sweat retention vesicle Degeneration & dilatation of secretory tubules + Dermis inflammatory & mucinous infiltration
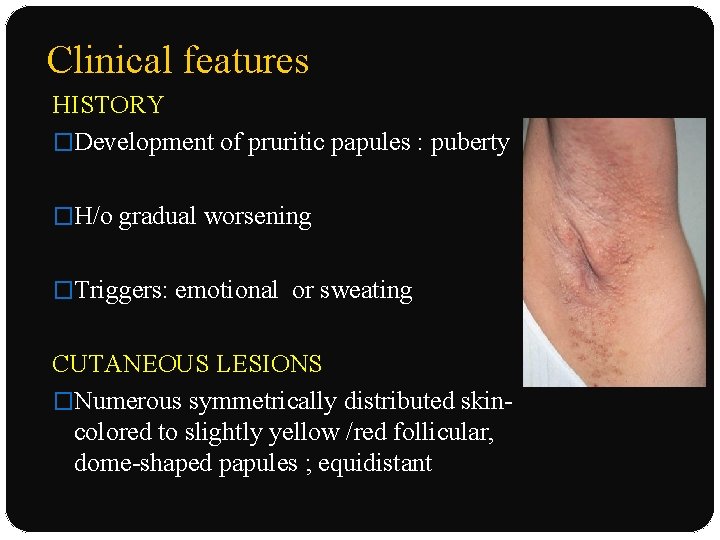
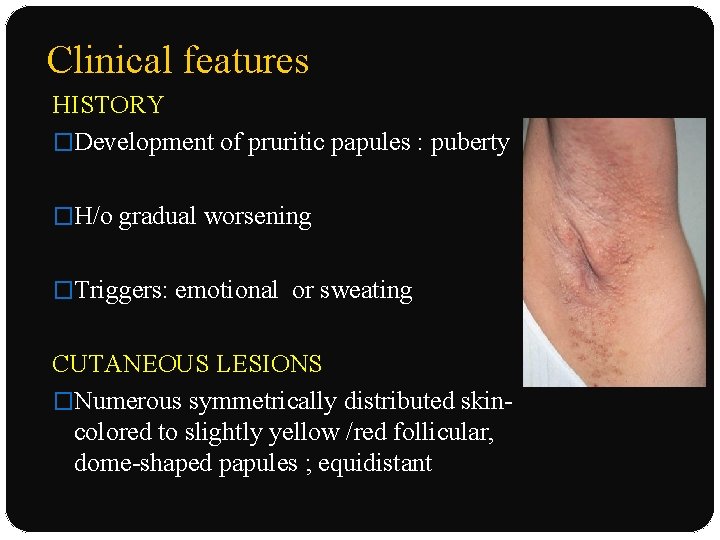
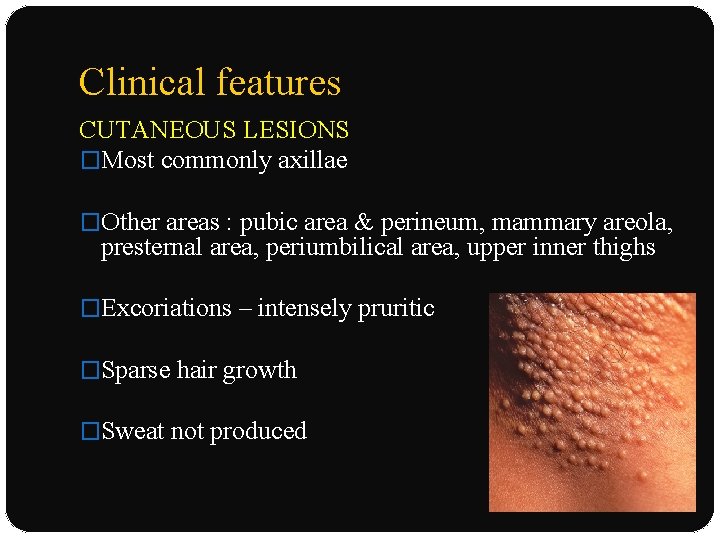
Clinical features HISTORY �Development of pruritic papules : puberty �H/o gradual worsening �Triggers: emotional or sweating CUTANEOUS LESIONS �Numerous symmetrically distributed skincolored to slightly yellow /red follicular, dome-shaped papules ; equidistant
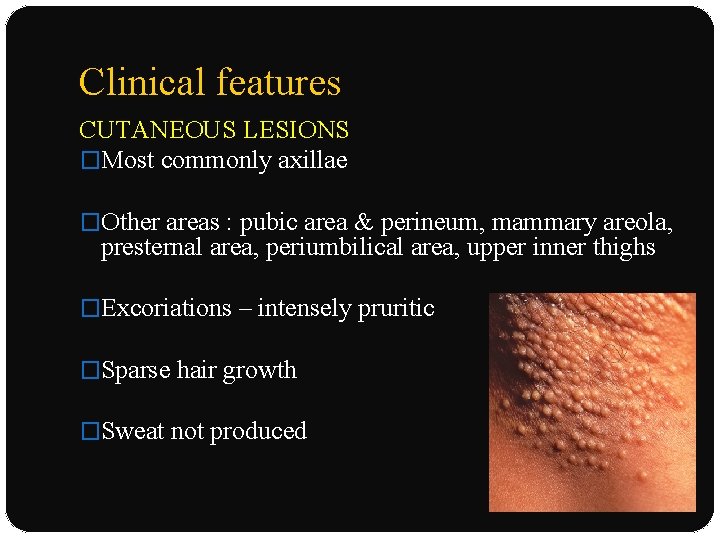
Clinical features CUTANEOUS LESIONS �Most commonly axillae �Other areas : pubic area & perineum, mammary areola, presternal area, periumbilical area, upper inner thighs �Excoriations – intensely pruritic �Sparse hair growth �Sweat not produced
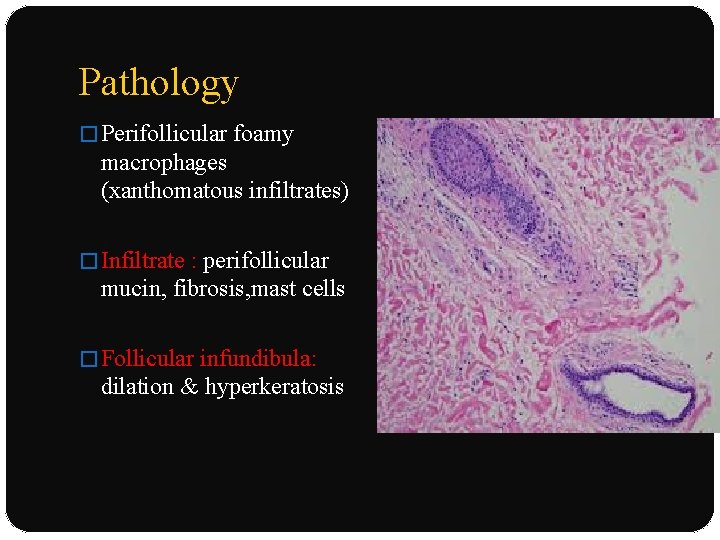
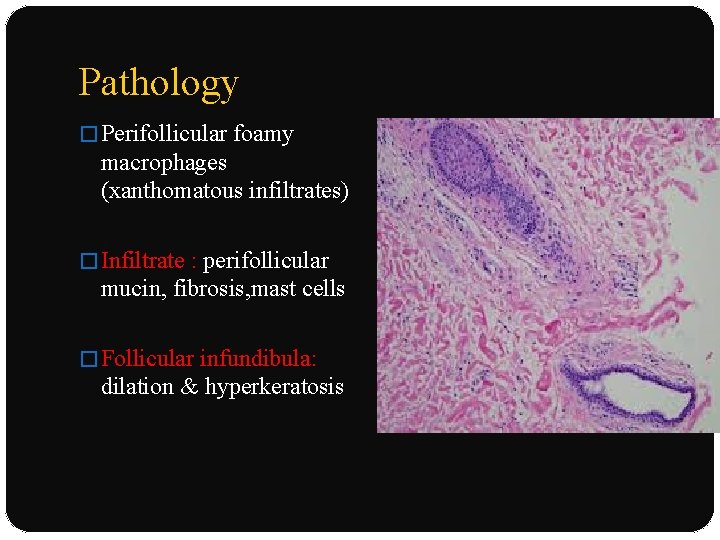
Pathology � Perifollicular foamy macrophages (xanthomatous infiltrates) � Infiltrate : perifollicular mucin, fibrosis, mast cells � Follicular infundibula: dilation & hyperkeratosis
Differential diagnosis �Lichen planus �Lichen nitidus �Folliculitis �Multiple syringomas
Treatment NONSURGICAL THERAPY: �Avoidance of excessive sweating or heat �Clindamycin with propylene glycol: eliminating symptoms and resolving papules �Topical tretinoin 0. 1% �Topical pimecrolimus ointment
Treatment �Systemic isotretinoin ; recurred within 3 months �Other reported: OCP, testosterone, topical or intralesional corticosteroids, ultraviolet light, X-ray SURGICAL THERAPY �Electrocoagulation �Surgical excision �Liposuction-assisted curettage
Hidradenitis suppurativa �Synonyms: Acne inversa , Verneuil’s disease , Pyoderma fistulans significa �Distressingly chronic, disabling, suppurative, cicatricial follicular disease �Cutaneous disorder : targets apocrine gland-bearing skin sites : axillae & anogenital region
Epidemiology �Common in females �Female–male ratios ranging from 2: 1 to 5: 1 �Rarely develops before puberty or after menopause �Average of onset : 23 years
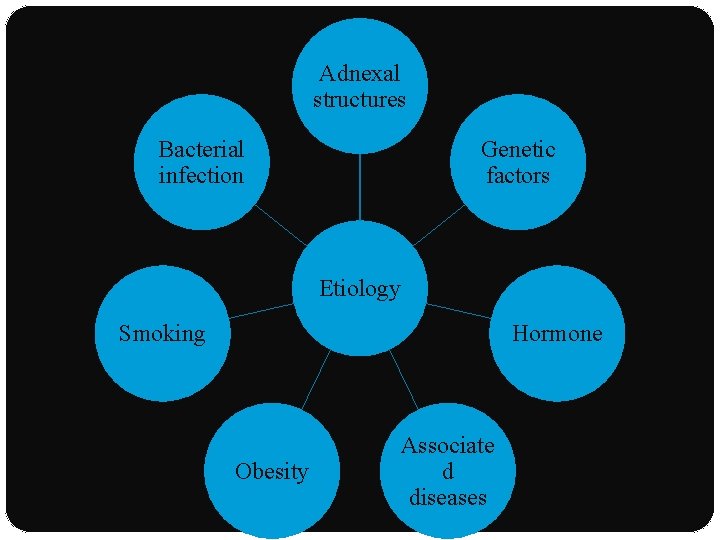
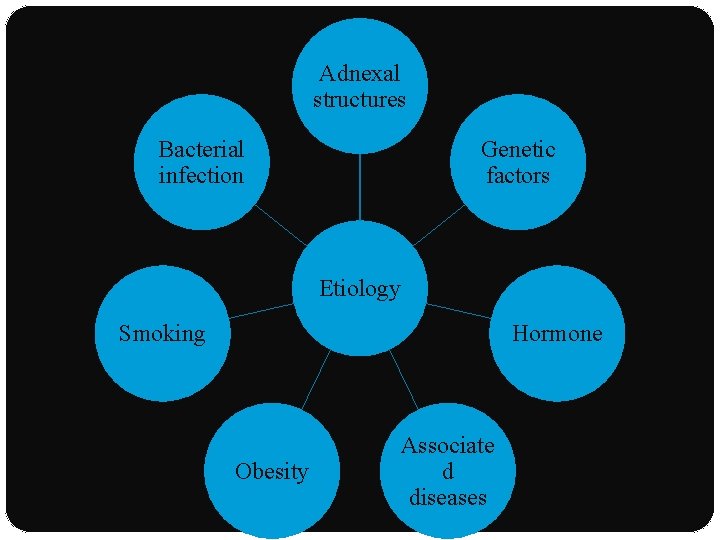
Adnexal structures Bacterial infection Genetic factors Etiology Smoking Hormone Obesity Associate d diseases
Etiology ADNEXAL STRUCTURES: �Primary disorder of apocrine glands : apocrinitis �Earlier : poral occlusion of the apocrine duct �Newer studies: gland inflammation & postulated that glands become secondarily affected
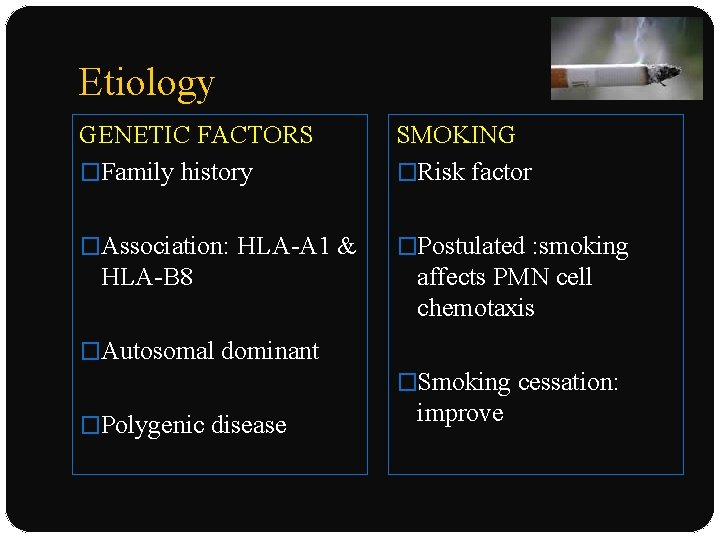
Etiology GENETIC FACTORS �Family history SMOKING �Risk factor �Association: HLA-A 1 & �Postulated : smoking HLA-B 8 affects PMN cell chemotaxis �Autosomal dominant �Smoking cessation: �Polygenic disease improve
Etiology HORMONES ANDROGENS �Develop at puberty or postpuberty : androgen influence �Disease flares: postpartum, association with OCP, premenstrual period �Antiandrogen therapy �No biochemical evidence of hyperandrogenism
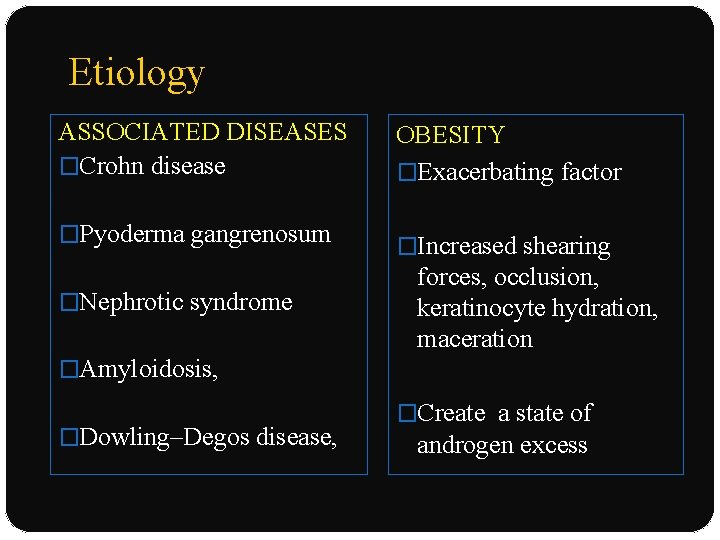
Etiology ASSOCIATED DISEASES �Crohn disease �Pyoderma gangrenosum �Nephrotic syndrome OBESITY �Exacerbating factor �Increased shearing forces, occlusion, keratinocyte hydration, maceration �Amyloidosis, �Dowling–Degos disease, �Create a state of androgen excess
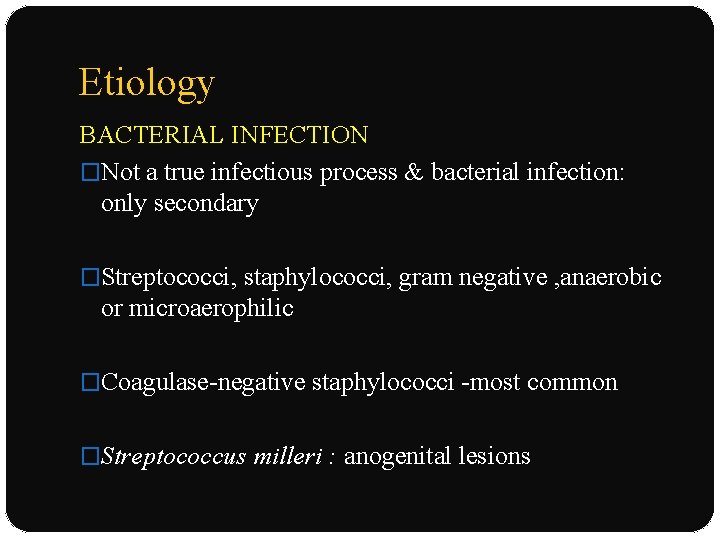
Etiology BACTERIAL INFECTION �Not a true infectious process & bacterial infection: only secondary �Streptococci, staphylococci, gram negative , anaerobic or microaerophilic �Coagulase-negative staphylococci -most common �Streptococcus milleri : anogenital lesions
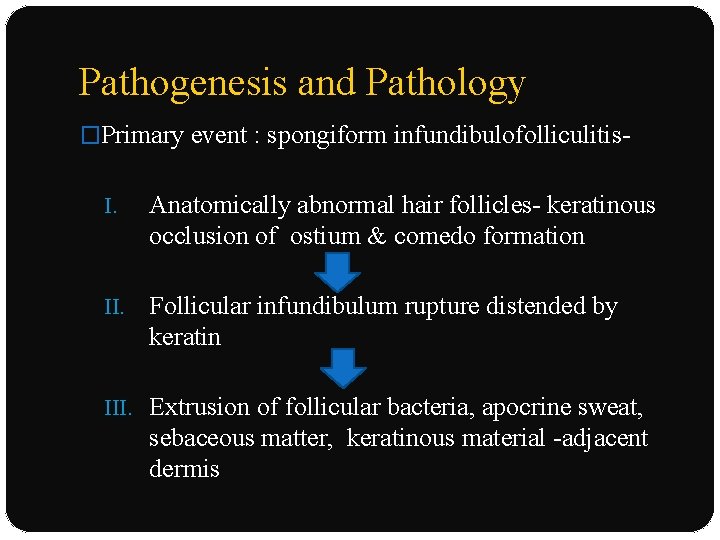
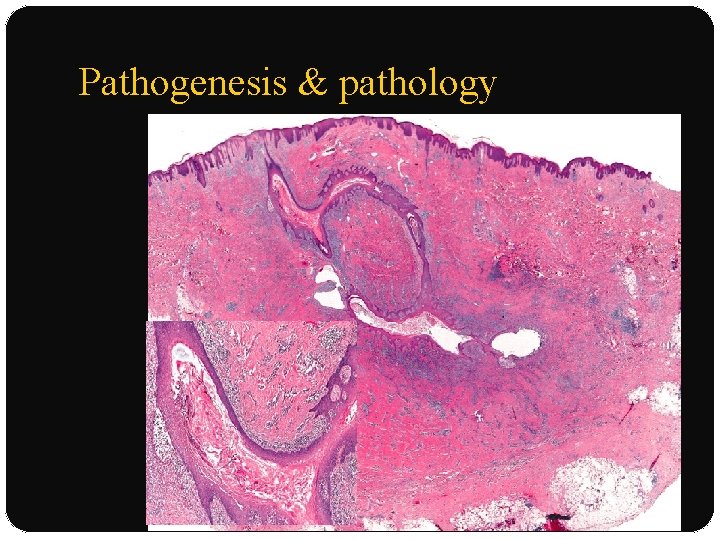
Pathogenesis and Pathology �Primary event : spongiform infundibulofolliculitis. I. Anatomically abnormal hair follicles- keratinous occlusion of ostium & comedo formation II. Follicular infundibulum rupture distended by keratin III. Extrusion of follicular bacteria, apocrine sweat, sebaceous matter, keratinous material -adjacent dermis
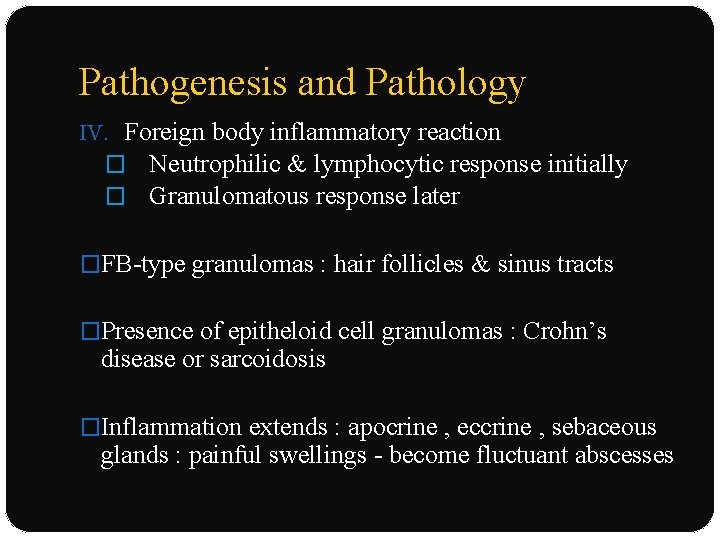
Pathogenesis and Pathology IV. Foreign body inflammatory reaction � Neutrophilic & lymphocytic response initially � Granulomatous response later �FB-type granulomas : hair follicles & sinus tracts �Presence of epitheloid cell granulomas : Crohn’s disease or sarcoidosis �Inflammation extends : apocrine , eccrine , sebaceous glands : painful swellings - become fluctuant abscesses
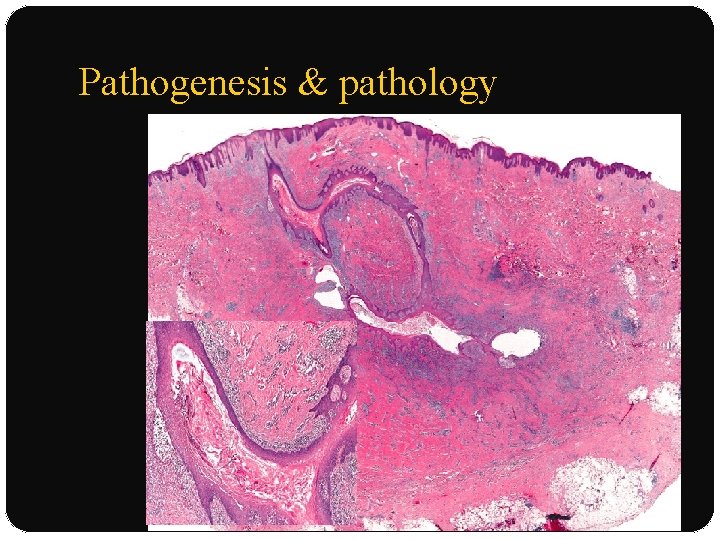
Pathogenesis & pathology
Clinical features � After puberty : both men & women � Sites : axillae submammary, inguinal, pubic, perineal, perianal � Female breast, neck, posterior aspect of the ears , adjacent scalp, back, buttocks � Extension to the scrotum or the labia � Anogenital involvement : frequent in males � Women : inguinal &mammary lesions
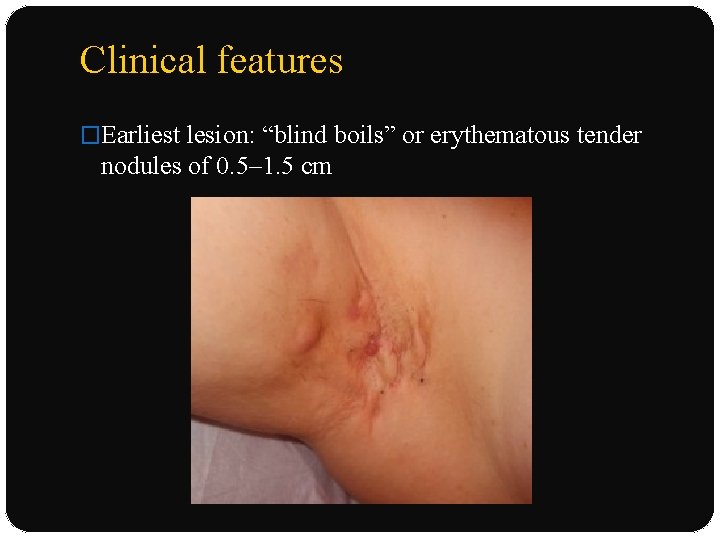
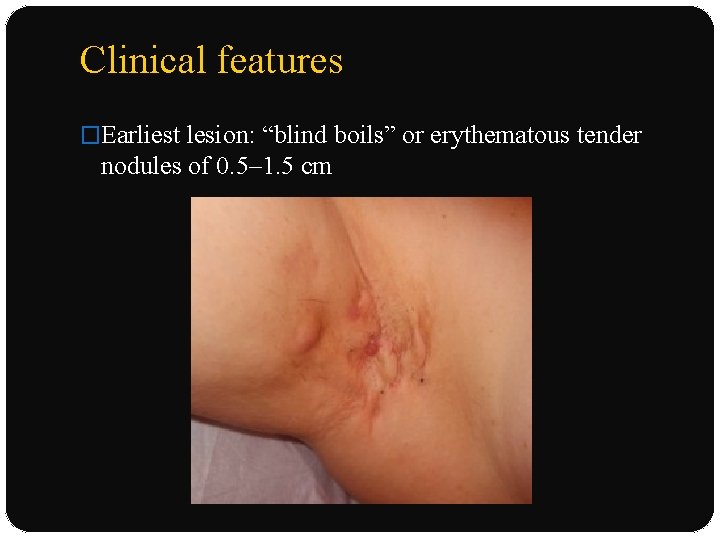
Clinical features �Earliest lesion: “blind boils” or erythematous tender nodules of 0. 5– 1. 5 cm
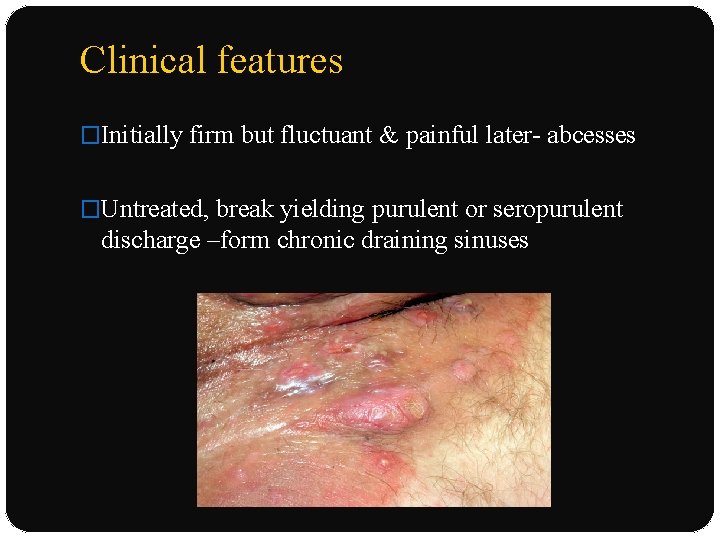
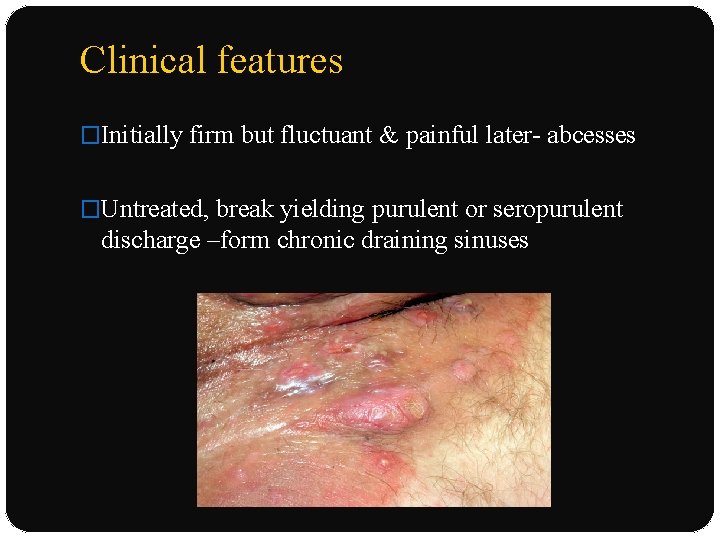
Clinical features �Initially firm but fluctuant & painful later- abcesses �Untreated, break yielding purulent or seropurulent discharge –form chronic draining sinuses
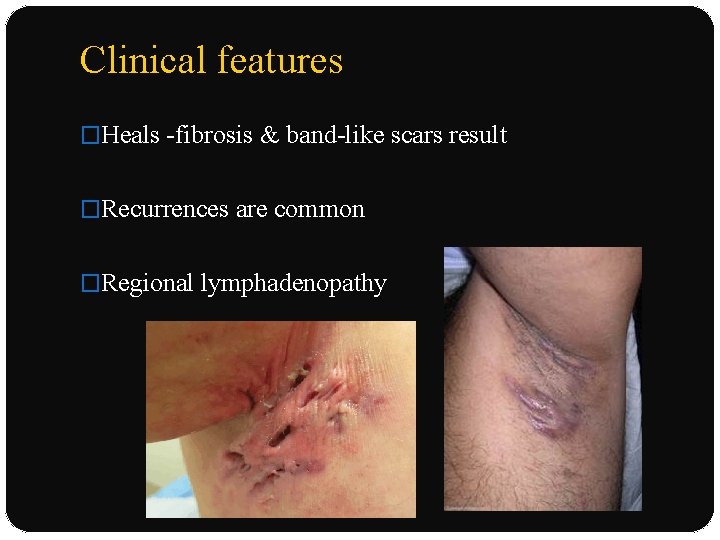
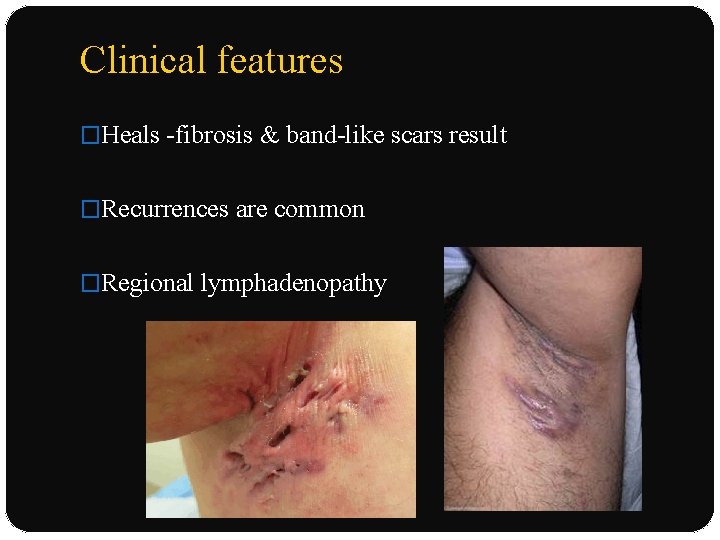
Clinical features �Heals -fibrosis & band-like scars result �Recurrences are common �Regional lymphadenopathy
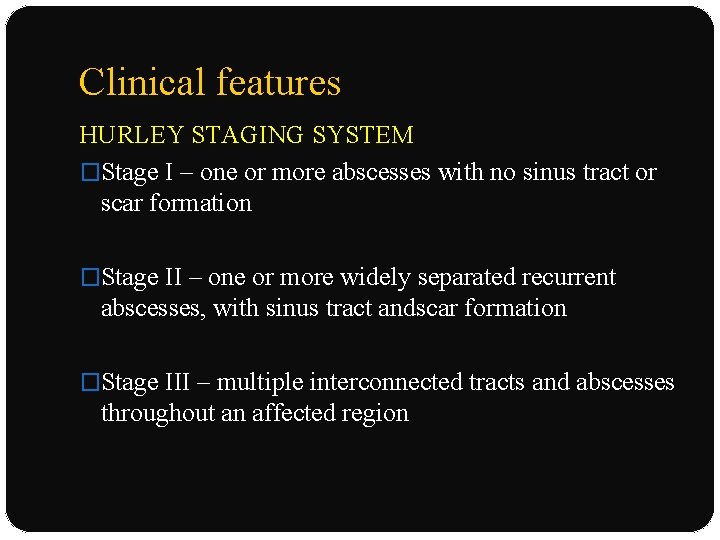
Clinical features HURLEY STAGING SYSTEM �Stage I – one or more abscesses with no sinus tract or scar formation �Stage II – one or more widely separated recurrent abscesses, with sinus tract andscar formation �Stage III – multiple interconnected tracts and abscesses throughout an affected region
Complications SYSTEMIC: �Local infection - septicemia �Lumbosacral epidural abscess LOCAL : �Scarring �Anal, urethral, or rectal strictures : chronic genitofemoral inflammation �Persistent penile, scrotal, or vulvar lymphedema �Squamous cell carcinoma
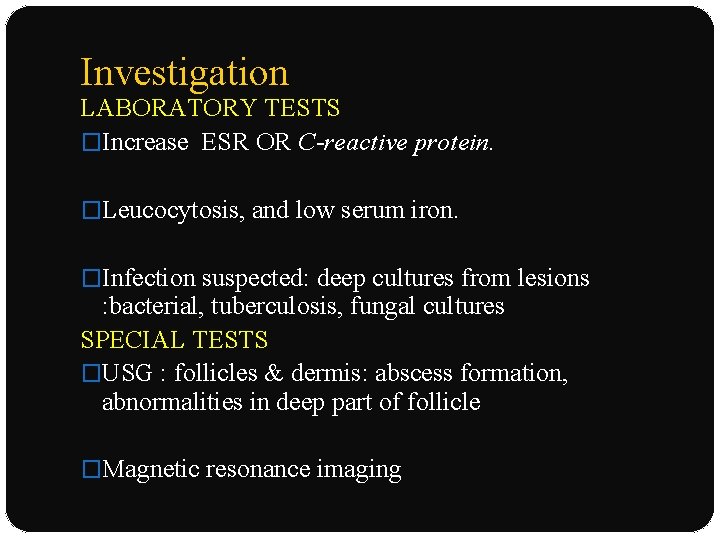
Investigation LABORATORY TESTS �Increase ESR OR C-reactive protein. �Leucocytosis, and low serum iron. �Infection suspected: deep cultures from lesions : bacterial, tuberculosis, fungal cultures SPECIAL TESTS �USG : follicles & dermis: abscess formation, abnormalities in deep part of follicle �Magnetic resonance imaging
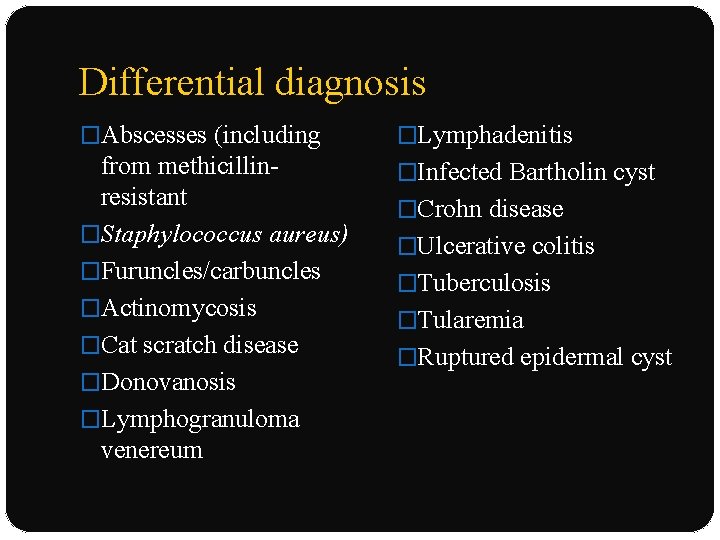
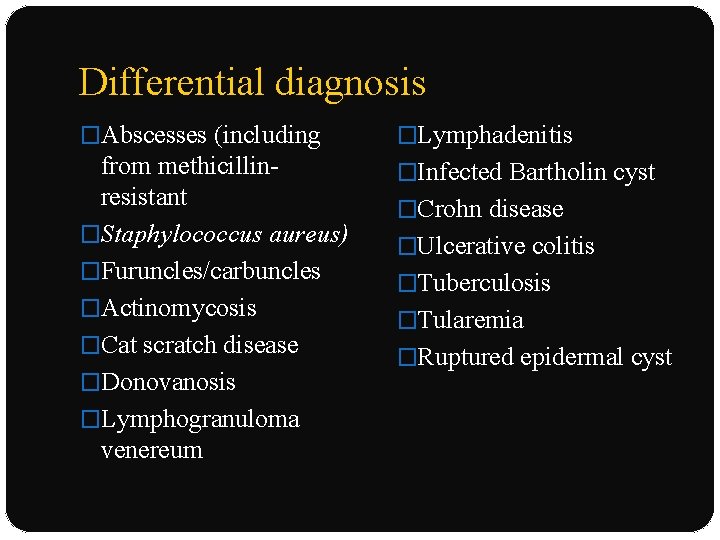
Differential diagnosis �Abscesses (including �Lymphadenitis from methicillinresistant �Staphylococcus aureus) �Furuncles/carbuncles �Actinomycosis �Cat scratch disease �Donovanosis �Lymphogranuloma venereum �Infected Bartholin cyst �Crohn disease �Ulcerative colitis �Tuberculosis �Tularemia �Ruptured epidermal cyst
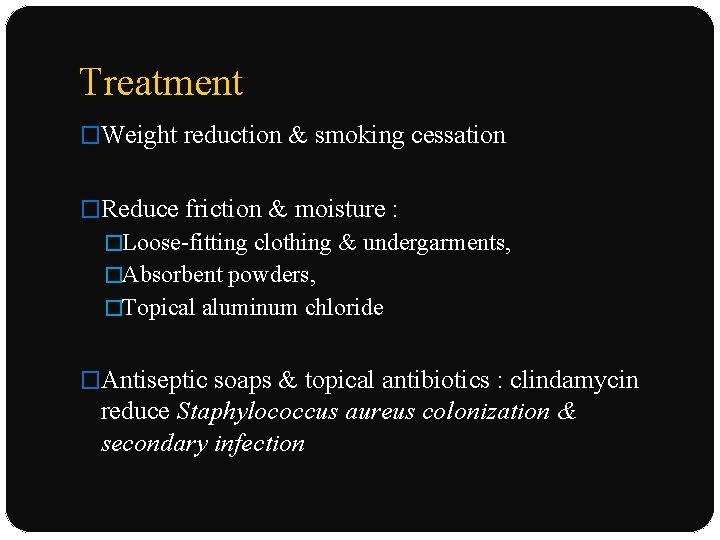
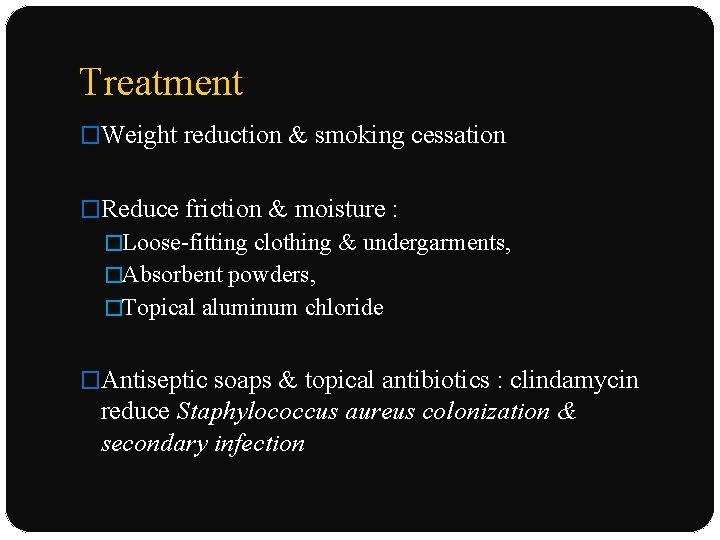
Treatment �Weight reduction & smoking cessation �Reduce friction & moisture : �Loose-fitting clothing & undergarments, �Absorbent powders, �Topical aluminum chloride �Antiseptic soaps & topical antibiotics : clindamycin reduce Staphylococcus aureus colonization & secondary infection
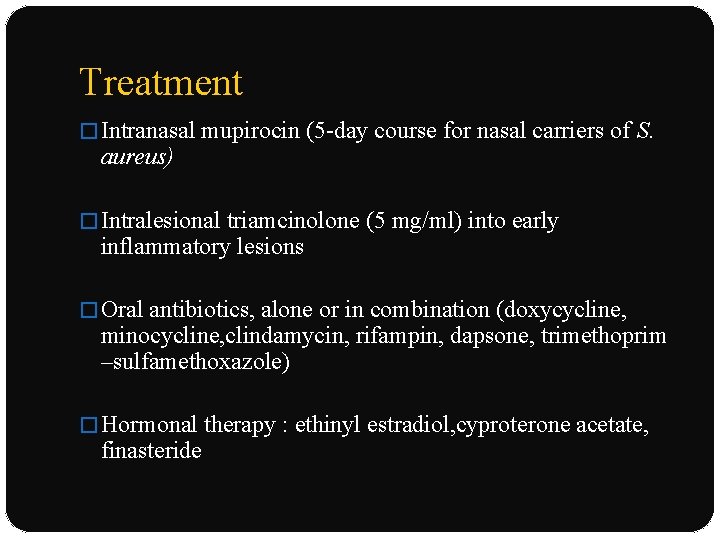
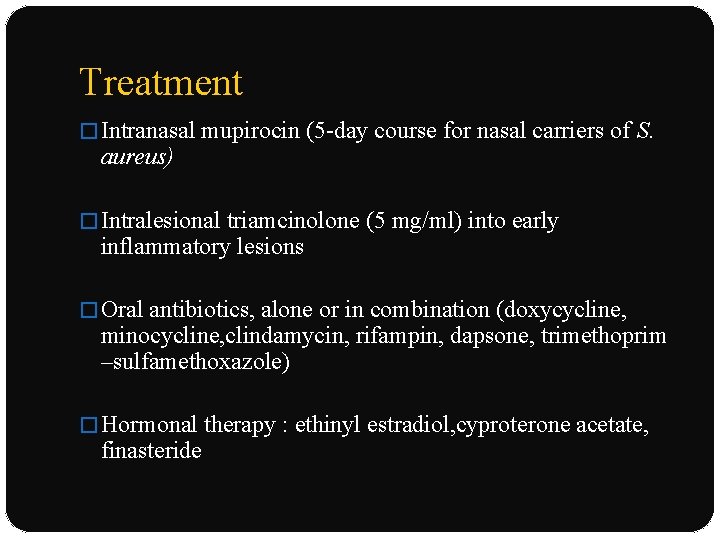
Treatment � Intranasal mupirocin (5 -day course for nasal carriers of S. aureus) � Intralesional triamcinolone (5 mg/ml) into early inflammatory lesions � Oral antibiotics, alone or in combination (doxycycline, minocycline, clindamycin, rifampin, dapsone, trimethoprim –sulfamethoxazole) � Hormonal therapy : ethinyl estradiol, cyproterone acetate, finasteride
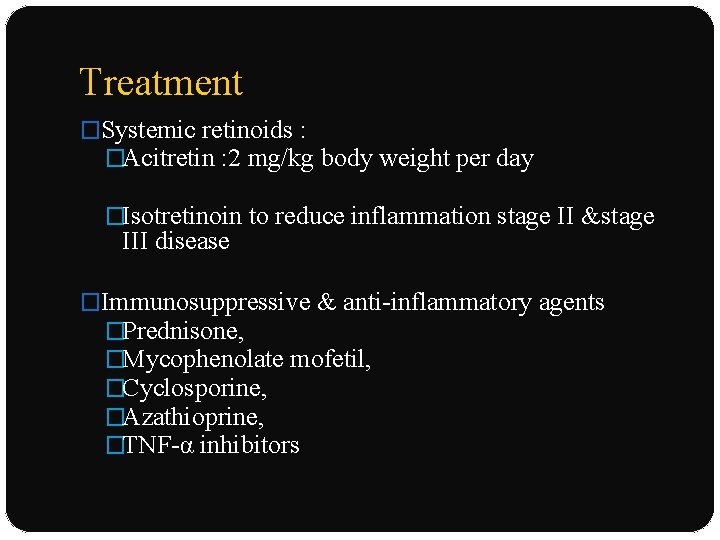
Treatment �Systemic retinoids : �Acitretin : 2 mg/kg body weight per day �Isotretinoin to reduce inflammation stage II &stage III disease �Immunosuppressive & anti-inflammatory agents �Prednisone, �Mycophenolate mofetil, �Cyclosporine, �Azathioprine, �TNF-α inhibitors
Treatment �Surgical excision, followed by primary closure or grafting �CO 2 laser stripping and second intention healing 55; Nd: YAG laser �Other : botulinum toxin A, photodynamic therapy
References �Bolognia text book of dermatology- 3 rd edition �Fitzpatrick textbook of general medicine – 8 th edition �Iadvl textbook of dermatology 3 rd edition �Rooks textbook of dermatology
Thank you
 Disease synonym
Disease synonym Epithelia
Epithelia Human scalp
Human scalp Cyclone nargis
Cyclone nargis Apocrine vs eccrine
Apocrine vs eccrine Phadebas paper
Phadebas paper Coiled gland
Coiled gland Cl channel
Cl channel Glands secrete what in reflex actions
Glands secrete what in reflex actions Poem about female reproductive system
Poem about female reproductive system Minor salivary glands
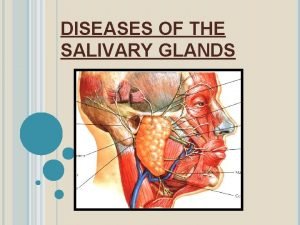
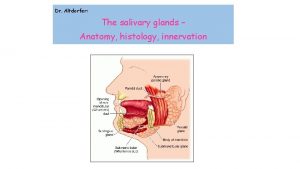
Minor salivary glands Enterochromaffin like cells
Enterochromaffin like cells Whats the difference between endocrine and exocrine glands
Whats the difference between endocrine and exocrine glands Male gonad
Male gonad Endocrine system function
Endocrine system function Male reproductive system front view
Male reproductive system front view Uterus perimetrium
Uterus perimetrium Oxyntic glands
Oxyntic glands Endocrine glands secrete
Endocrine glands secrete Cladogram of earthworm trout lizard and human
Cladogram of earthworm trout lizard and human Where are the gastric glands located
Where are the gastric glands located Sialography
Sialography Specialised cell
Specialised cell Saliva formation
Saliva formation Classification of exocrine glands
Classification of exocrine glands Pineal and pancreas glands
Pineal and pancreas glands Holocrine secretion
Holocrine secretion Endocrine glands
Endocrine glands True capsule of thyroid gland
True capsule of thyroid gland Characteristics of epithelial tissue
Characteristics of epithelial tissue Difference between endocrine and exocrine glands
Difference between endocrine and exocrine glands Minor salivary glands
Minor salivary glands The only example of unicellular exocrine glands are
The only example of unicellular exocrine glands are Major endocrine glands male and female
Major endocrine glands male and female Httpv://www.youtube.com/watch?v=gvuiltwlel8
Httpv://www.youtube.com/watch?v=gvuiltwlel8 Hypothal
Hypothal Glands of the endocrine system
Glands of the endocrine system Popularly called lymph glands
Popularly called lymph glands Adrenal cushing
Adrenal cushing Adrenal glands
Adrenal glands Exocrine glands are ductless
Exocrine glands are ductless Salivary gland swelling
Salivary gland swelling Honey bee wax glands
Honey bee wax glands Gastric glands
Gastric glands Tissue
Tissue Minor salivary glands
Minor salivary glands Endocrine glands
Endocrine glands Multicellular exocrine glands can be classified
Multicellular exocrine glands can be classified Simple acinar gland histology
Simple acinar gland histology Layer of dermis
Layer of dermis Salivary gland parenchyma
Salivary gland parenchyma Cretinism
Cretinism Gonads
Gonads Type 2 pneumocytes surfactant
Type 2 pneumocytes surfactant Exocrine glands function
Exocrine glands function Parotid gland
Parotid gland What glands are flask shaped with short ducts
What glands are flask shaped with short ducts Chapter 16 matching questions 6-10
Chapter 16 matching questions 6-10 Parotid gland relations
Parotid gland relations Basal cell adenoma
Basal cell adenoma Male accessory glands
Male accessory glands Parathyroid gland image
Parathyroid gland image Thyroid class 11
Thyroid class 11 Sebum function
Sebum function Duct and gland difference
Duct and gland difference Spermatocytogenesis
Spermatocytogenesis Str papillare
Str papillare