DIAGNOSIS TREATMENT OF PARKINSONS DISEASE Sadhana Prasad Symposium











- Slides: 56
DIAGNOSIS & TREATMENT OF PARKINSON’S DISEASE Sadhana Prasad Symposium on Changes and Challenges in Geriatric Care
Disclosures • Work with various pharmaceutical companies intermittently • Honorarium will be donated

OBJECTIVES 1. Illustrate medications and conditions that may mimic PD 2. Describe the early symptoms of Parkinson’s Disease (PD) 3. Discuss initiating and stopping medications
Parkinson’s Disease Characterized by: (Slow, Stiff, Shaky) • Bradykinesia * • Rigidity * • Rest tremor--3 -6 Hz pill-rolling (absent 1/3) • Postural instability

Parkinson’s Disease (PD) • First description 1817 Parkinson, James An Essay on the Shaking Palsy, Sherwood, Neely, and Jones, London • Progressive neurodegenerative disease • Affects ages 40 onwards, mean age at diagnosis 70. 5 • Complex disorder with motor, non-motor, neuropsychiatric features
Disease vs Syndrome • Disease = a morbid process having characteristic symptoms; pathology, etiology, and prognosis may be known • Syndrome = a set of symptoms occurring together; different etiologies but similar presentation
Parkinson’s Syndromes Metabolic causes- • Hypothyroidism • Hypoparathyroidism • Alcohol withdrawl (pseudoparkinsonism) • Chronic liver failure • Wilson’s disease
P. Syndromes Medications**/chemicals— • neuroleptics (typicals more than the atypicals), • SSRI (selective serotonin reuptake inhibitors), • metoclopromide/maxeran, • Reserpine, • MPTP, • in Methcathinone (ephedrone) users – high plasma Manganese levels (NEJM Mar 6, 2008) • CO, cyanide, organic solvents, carbon disulfide
P. Syndromes Structural Causes— • Strokes • Tumors • Chronic subdurals • NPH (Normal Pressure Hydrocephalus)
P. Syndromes Lewy Body spectrum of Diseases (DLB=Dementia with LB)-----early onset visual (or other) hallucinations ---fluctuating cognitive abilities ---sleep disorders ---neuroleptic sensitivity, even to atypicals
P. Syndromes PSP (progressive supranuclear palsy)—or Steeles Richardson Olszewski Syndrome ---gaze abnormalities ---postural instability, early unexplained falls ---bulbar features—dysphonia, dysarthria, dysphagia ---rapidly progressive---median 6 yrs.
P. Syndromes CBD (cortico basal degeneration)-----Asymmetric parkinsonism ---postural instability ---ideomotor apraxia ---aphasia ---alien limb phenomenon ---impaired cortical sensations
P. Syndromes Multi System Atrophy-- (alpha-synuclein + glial cytoplasmic inclusions, autonomic dysfunction, pyramidal signs) • Shy Drager Syndrome, • Olivopontocerebellar atrophy, • Striatonigral degeneration
P. Syndromes Other Neurodegenerative Disorders— • Alzheimer’s Disease, later stages** • Huntington’s Disease (rigid form) • Frontotemporal Dementia with Parkinsonism, Chromosome-17 linked (FTDP-17) • Spinocerebellar ataxias
P. Syndromes Infections-- • encephalitis • HIV/AIDS • Neurosyphilis • Toxoplasmosis • CJD (Creuzfeld Jakob)--prion disease • Progressive multifocal leukoencephalopathy

P. Syndrome Essential Tremor-----action tremor (not rest tremor) ---more rapid (greater than 3 -6 Hz) ---usually hands, but can also affect legs, head/chin, voice, trunk ---can present with falls if legs and trunk involved
P. Disease ? ? DIAGNOSIS? ?

P. Dis -- Diagnosis • • A clinical diagnosis Cardinal features: Bradykinesia, rigidity Trial of sinemet (Levodopa/carbidopa) Confirmatory test: neuropathologic (autopsy)
P. Disease-Diagnosis • 1/3 will not respond to levodopa therapy • 1/5 with P. Syndrome will respond to levodopa ---Follow- up with time needed to clarify diagnosis
P. Disease---Diagnosis Minimum therapeutic dose: ---300 mg levodopa per day in divided doses ---can be lower in biologically old ---vast majority will need 400 -600 mg levodopa daily to achieve significant benefit
P. Disease- Diagnosis Consider alternative diagnosis if: • Early falls (postural instability) • Poor response to levodopa • Dysautonomia (urinary retention/atonic bladder, incontinence, orthostatic hypotension, impotence) • No rest tremor (in 1/3)
P. Disease-Diagnosis Alternative Diagnosis cont’d… • Cerebellar signs • Positive Babinski • Apraxia • Gaze abnormailities • Dementia concurrently with Parkinsonism • Strokes
P. Disease INVESTIGATIONS: • TSH • Calcium, albumin • CT head
OBJECTIVES 1. Illustrate medications and conditions that may mimic PD 2. Describe the early symptoms of Parkinson’s Disease (PD) 3. Discuss initiating and stopping medications

PD- CASE • Mr AB, married, active farmer, stressed care-giver • Drove his wife to the clinic, wife to see me re agitated dementia • One son also attended • Mr AB –stressed care-giver, on paxil (SSRI)
PD- case Mr. AB--- stressed caregiver • Slightly flexed posture • Slightly bradykinetic • Slightly diminished facial expression • No difficulty turning, getting in/out of armless chair
PD-case “I don’t have Parkinson’s Disease!!”
PD- case Mr. AB-- • 1 month later, referred re ? PD? ? • CT head, TSH, Ca normal • Slowing down x 1 yr, hypophonia, denied trouble turning in bed but took 5 tries in clinic, trouble getting out of soft chair, stopped taking baths x 3 years, mild rest tremor R hand, trouble doing up buttons and laces

IADL Instrumental Activities of Daily Living • • • S H A F T shopping housework accounting food preparation transportation

ADL Activities of Daily Living • • • D E A T H dressing eating ambulation toiletting hygiene
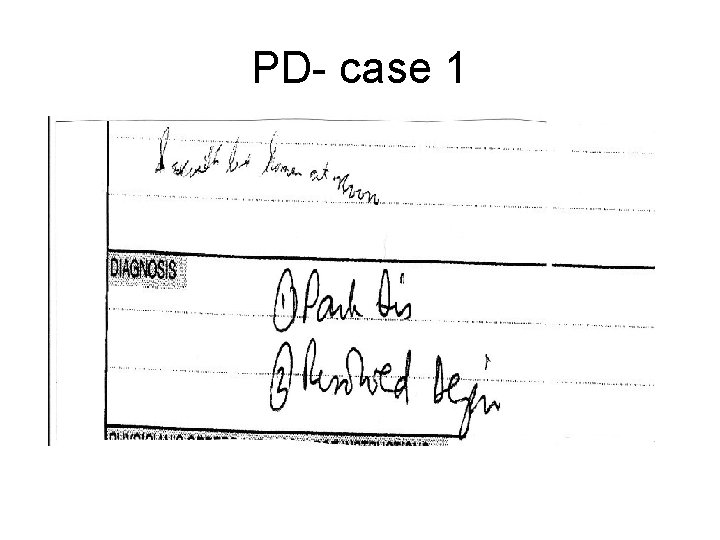
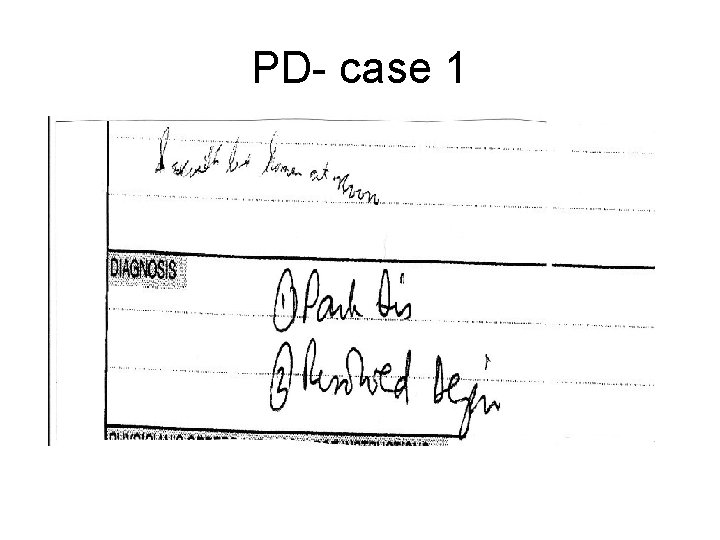
PD- case 1
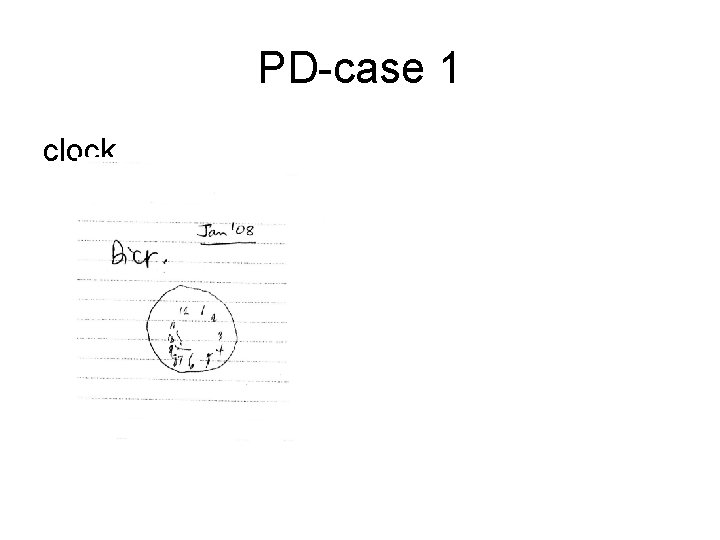
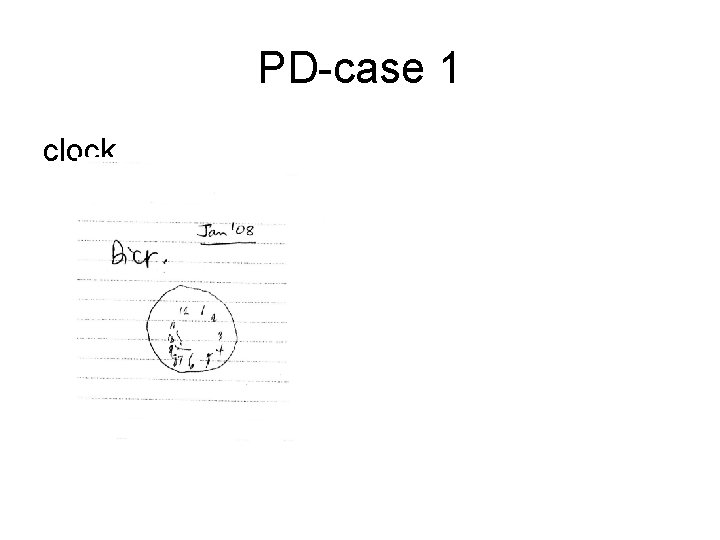
PD-case 1 clock
PD –Case 1 Diagnosis: Parkinson’s disease ---Hoehn & Yahr’s** stage 2

Hoehn and Yahr scale • 1. Unilateral involvement only, usually with minimal or no functional disability • 2. Bilateral or midline involvement without impairment of balance • 3. Bilateral disease; mild to moderate disability with impaired postural reflexes; physically independent • 4. Severely disabling disease; still able to walk or stand unassisted • 5. Confinement to bed or wheelchair unless aided Hoehn, MM, Yahr, MD. Parkinsonism: onset, progression and mortality. Neurology 1967; 17: 427.
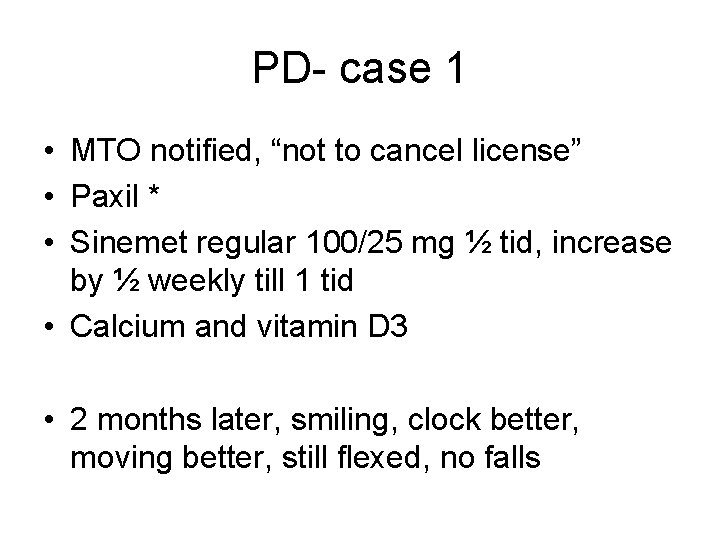
PD- case 1 • MTO notified, “not to cancel license” • Paxil * • Sinemet regular 100/25 mg ½ tid, increase by ½ weekly till 1 tid • Calcium and vitamin D 3 • 2 months later, smiling, clock better, moving better, still flexed, no falls

PD-case 1 clock
PD—other issues • • • Depression Dementia Driving Falls Neuropsychiatric features “slowing down of thought processes” (the clock in Mr AB) • Constipation
PD-Treatment ? ?
OBJECTIVES 1. Illustrate medications and conditions that may mimic PD 2. Describe the early symptoms of Parkinson’s Disease (PD) 3. Discuss initiating and stopping medications
PD--Treatment • Geared towards mobility—levodopa, dopamine agonists, MAO B inhibitors • Rest tremor, cosmetic—anticholinergics (may worsen cognition) • Postural imbalance—no pharmacological treatment; exercise, gait aids, prevent fractures (Ca, Vit D 3, +/- bisphonates) • Dyskinesias-- ? amantadine (no clear evidence) Almeida, QJ, Recent Patents on CNS Drug Discovery, 2008: 3, 5 --54

PD--Which pharmaceutical? In Elderly- • Levodopa/ carbidopa (sinemet) – regular vs CR (controlled release) or Levodopa/ benserazide (prolopa) – regular vs HBS • COMT- inhibitor– entacapone (comtan)

PD- medications Levodopa • Well-established, for bradykinesia and rigidity • SE: nausea, orthostatic hypotension • Combined with peripheral decarboxylase inhibitor (carbidopa, benserazide) to prevent conversion to dopamine in the periphery before it crosses blood brain barrier
PD- medications Levodopa (l-dopa) -- l-dopa / carbidopa = sinemet reg. or CR -- l-dopa / benserazide = prolopa, medopar or medopar HBS • Competes with amino acids from protein for GI absorption • Regular-- before meals, quick in quick out, T 1/2 = 90 min • CR--- With meals, Controlled Release, slow in slow out, need 30% more to achieve same effect as reg. dose, erratic absorption in elderly
PD-medications L-dopa cont’d • SE- Nausea (Rx Domperidone) -Hallucinations (Rx lower dose, atypical n neuroleptics) -somnolence, confusion, agitation -motor fluctuations- after sev yrs of Rx
PD- medications L-dopa cont’d • Motor fluctuations (in 50%, after 5 -10 yrs) -wearing-off– Rx COMT – inhibitor*, ? CR -dyskinesias –(? ? Rx amantadine? ? ) -dystonias -variety of complex fluctuations in motor function
PD- medications L-dopa cont’d • Discontinuation— - gradually –over weeks, - to prevent malignant neuroleptic like syndrome or akinetic crisis
PD-medications L-dopa cont’d • Dopaminergic dysregulation syndrome (DDS)— tolerance to mood elevating effects - Compulsive use of dopaminergic drugs - Early onset males - Cyclical mood disorder - Impulse control disorder (hypersexuality, pathologic gambling) Giovannoni, G, Hedonistic homeostatic dysregulation…J. Neurol Neurosurg Psychiatry 2000; 68: 243
PD- medications COMT – inhibitor -Catechol-O-Methyl Transferase Inhibitor -((eg Tolcapone (Tasmar)---off market due to fulminant hepatitis causing 3 deaths)) -eg Entacapone (Comtan) -for wearing-off at end-of-dose of L-dopa -dose 200 mg-1600 mg, divided, daily, with L-dopa -SE-diarrhea in 5%, due to increased dopaminergic stimulation from L-dopa availability
PD-medications Dopamine Agonists: adjunct Rx to L-dopa. -Ergotamines—bromocriptine, ((pergolide)), ((cabergoline)) SE-same as L-dopa, uncommon Raynaud’s, erythromelalgia, retroperitoneal/pulmonary fibrosis -Non-Ergot—pramipexole, ropinirole, ((transdermal rotigotine)) SE—same as L-dopa, Sudden somnolence – caution with driving
PD-medications MAO-B inhibitors--adjunct Rx to L-dopa inhibitors-eg selegiline (eldepryl), rasagiline -somewhat helpful in young, early in disease -neuroprotective properties in animal models only Arch Neurology. 2002; 59: 1937
PD-medications Anticholinergics—adjunct Rx to L-dopa, best Anticholinergics avoided in elderly -acetylcholine (ACh) and dopamine in balance in basal ganglia -decrease Ach to balance decrease in L-dopa -eg trihexyphenidyl (artane), benztropine (cogentin), orphenadrine, procyclidine (kemadrin) -SE-confusion, hallucinations, dry mouth, blurred vision, constipation, nausea, u. retention, glaucoma
PD-medications Amantadine-adjunct to L-dopa, best avoided in elderly -for dyskinesias -Antiviral agent—mechanism unknown -NMDA-receptor antagonist propertiesinterferes with excessive glutamate -SE-livedo reticularis, ankle edema, hallucinations
PD- Medications When do you stop the medications? --ALWAYS taper gradually over days to weeks to avoid NM-like syndrome --unable to take meds (dysphagia) --significant, intolerable SE impairing QOL --end-stage--- “infection comes as a friend”
OBJECTIVES 1. Illustrate medications and conditions that may mimic PD 2. Describe the early symptoms of Parkinson’s Disease (PD) 3. Discuss initiating and stopping medications
 Parkinsons disease hereditory
Parkinsons disease hereditory Tasha big feet
Tasha big feet Sadhana kanya vidyalaya hadapsar
Sadhana kanya vidyalaya hadapsar Parkinsons wiki
Parkinsons wiki Rayat shikshan sanstha sadhana vidyalaya hadapsar
Rayat shikshan sanstha sadhana vidyalaya hadapsar Rayat shikshan sanstha sadhana vidyalaya hadapsar
Rayat shikshan sanstha sadhana vidyalaya hadapsar Sadhana vidyalaya hadapsar pune 28
Sadhana vidyalaya hadapsar pune 28 Rectosigmoid junction
Rectosigmoid junction Shy drager syndrome
Shy drager syndrome Katharine hepburn parkinsons
Katharine hepburn parkinsons Types of nursing diagnosis
Types of nursing diagnosis Objectives of nursing process
Objectives of nursing process The nursing process
The nursing process Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Endodontic diagnosis and treatment planning
Endodontic diagnosis and treatment planning Oral diagnosis and treatment planning ppt
Oral diagnosis and treatment planning ppt Charting exercise chapter 28
Charting exercise chapter 28 Lateral throat form in prosthodontics
Lateral throat form in prosthodontics Behcet disease diagnosis
Behcet disease diagnosis Diagnosis of periodontal disease
Diagnosis of periodontal disease Nursing diagnosis for vision impairment
Nursing diagnosis for vision impairment Nursing diagnosis for meniere's disease
Nursing diagnosis for meniere's disease Nephrotic syndrome
Nephrotic syndrome Maple syrup urine disease treatment
Maple syrup urine disease treatment Modern treatment of heart disease
Modern treatment of heart disease Q
Q Disease control phase dental
Disease control phase dental Communicable disease and non communicable disease
Communicable disease and non communicable disease Bill prasad
Bill prasad Tk wright
Tk wright Drbavaharan13
Drbavaharan13 Rajesh prasad ias assam
Rajesh prasad ias assam Vanessa prasad permaul
Vanessa prasad permaul Prasad raghavendra
Prasad raghavendra Srinivas kantipudi
Srinivas kantipudi Amita prasad ias
Amita prasad ias Spread of chipko movement
Spread of chipko movement Ramananda prasad
Ramananda prasad Combination reaction example
Combination reaction example Ard prasad
Ard prasad Vanessa prasad permaul
Vanessa prasad permaul Lawrence prasad
Lawrence prasad Edamana prasad
Edamana prasad Annie prasad
Annie prasad Engage global solutions
Engage global solutions Astha prasad
Astha prasad What can we learn privately
What can we learn privately Sequence of making pochampally saree
Sequence of making pochampally saree Inbae lee
Inbae lee Rachit prasad
Rachit prasad Viji prasad
Viji prasad Prasad gourineni md
Prasad gourineni md Prasad calyam
Prasad calyam Prasad calyam
Prasad calyam Chandi prasad bhatt quotes
Chandi prasad bhatt quotes Dr vasudeva prasad atluri
Dr vasudeva prasad atluri