Development of urology like clinical discipline Urinary tract



- Slides: 51
Development of urology like clinical discipline. Urinary tract infections Lecture № 1 Lecturer – Baralo Igor Vitalievich
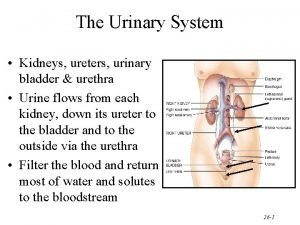
Subject urology Urology – this is a medical discipline, who teaches etiology, pathogeneses, diagnostics, treatment and prophylaxis of surgical disease of kidney, urinary tract, male genital organs, organs of retroperitoneal cavity and pelvic adipose cavity.
Surety, which makes urology a independent discipline: - specific methods for treatment of the patients - specific surgical and conservative treatment of the patients
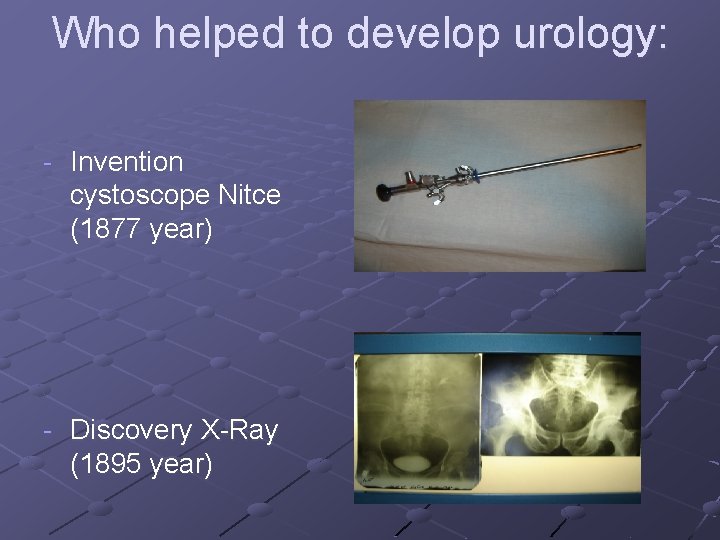
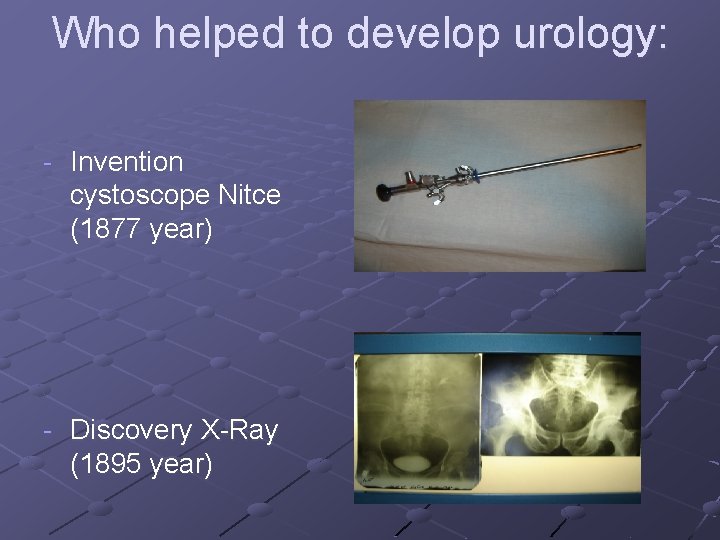
Who helped to develop urology: - Invention cystoscope Nitce (1877 year) - Discovery X-Ray (1895 year)
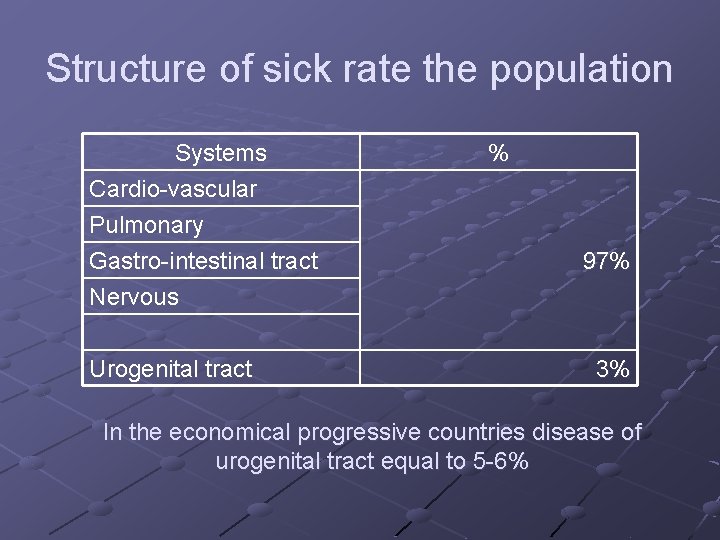
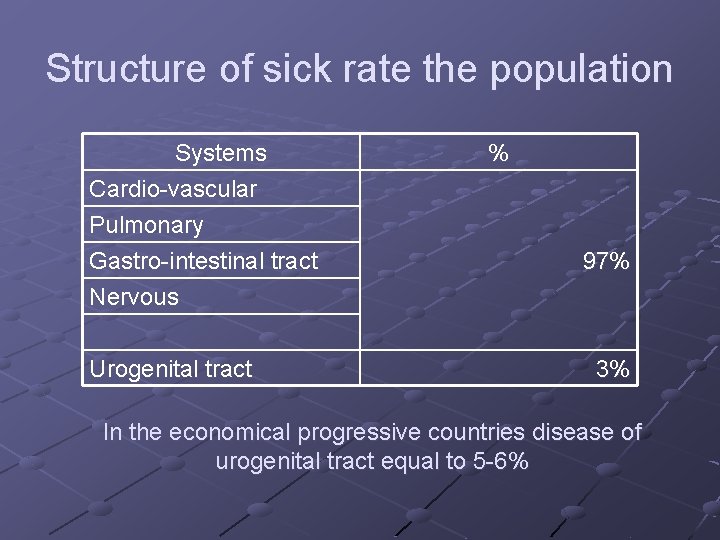
Structure of sick rate the population Systems Cardio-vascular Pulmonary Gastro-intestinal tract % 97% Nervous Urogenital tract 3% In the economical progressive countries disease of urogenital tract equal to 5 -6%
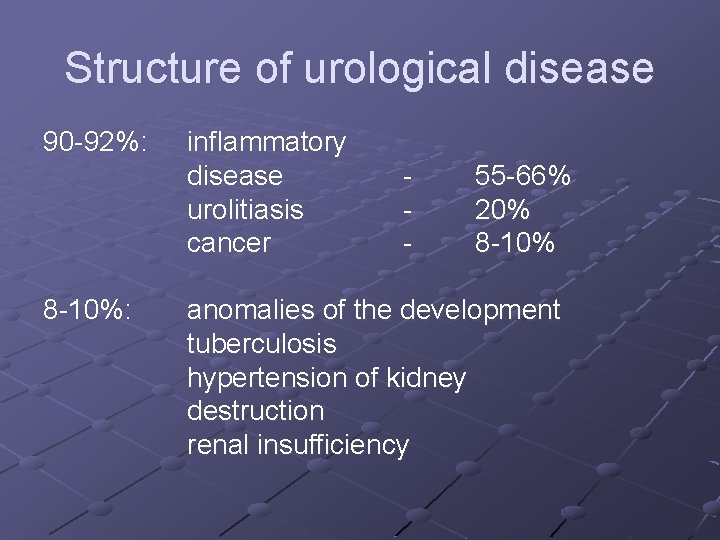
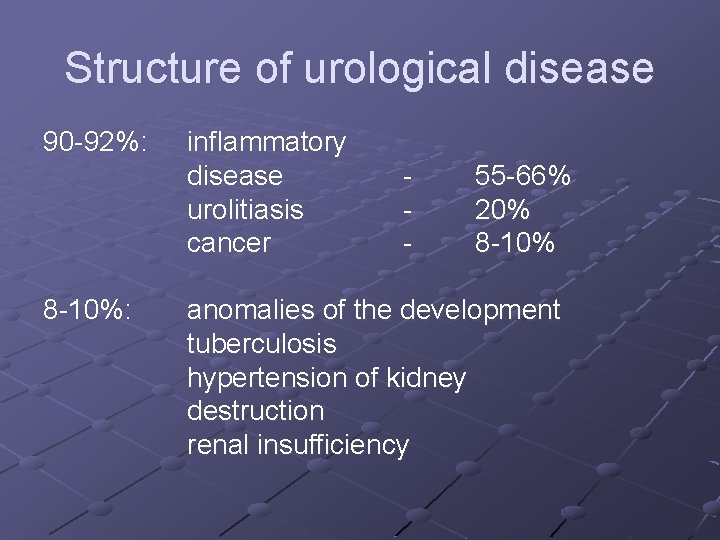
Structure of urological disease 90 -92%: 8 -10%: inflammatory disease urolitiasis cancer - 55 -66% 20% 8 -10% anomalies of the development tuberculosis hypertension of kidney destruction renal insufficiency
Unspecific inflammatory disease of urogenital tract – infection of urinary tract (UTI) Infection of urinary tract defined as the invasion of bacteria into the urethra, urinary bladder or kidney, which replies as the inflammatory action and causes clinical symptoms Urinary tract infection is one among the infection among the men
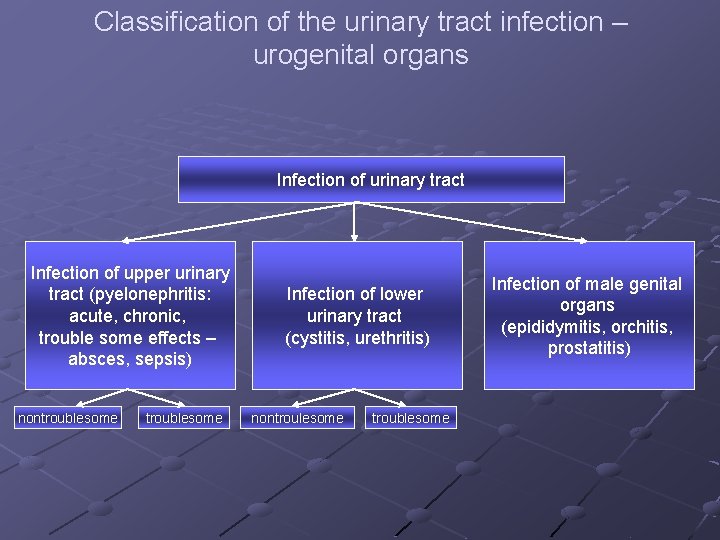
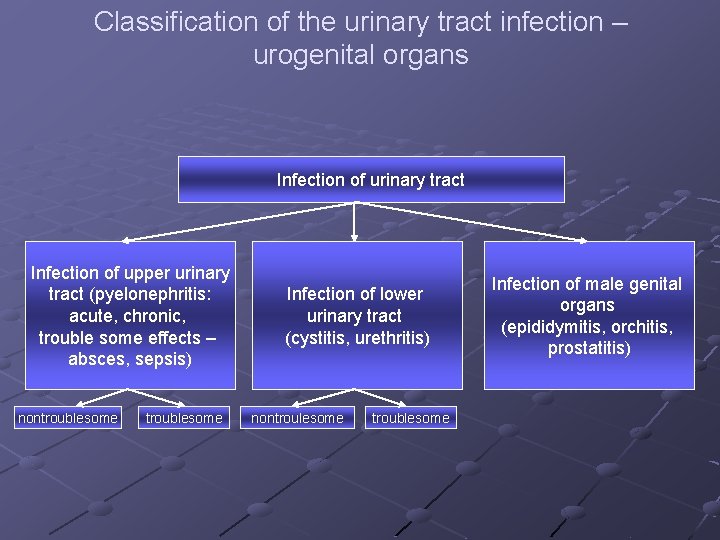
Classification of the urinary tract infection – urogenital organs Infection of urinary tract Infection of upper urinary tract (pyelonephritis: acute, chronic, trouble some effects – absces, sepsis) nontroublesome Infection of lower urinary tract (cystitis, urethritis) nontroulesome troublesome Infection of male genital organs (epididymitis, orchitis, prostatitis)

Pyelonephritis – it is Inflammatory unspecific process caused by the bacterial invasion in the parenchyma, calyxes and pelvic systems of the kidney and the most effected place in the intersticial tissue Pyelonephritis is present in 20 -30% of live people and on postmartum 8 -20% are found Thickly of situation the inflamatory process in urogenital system: Pyelonephritis 30% Cystitis 53% Other 17%
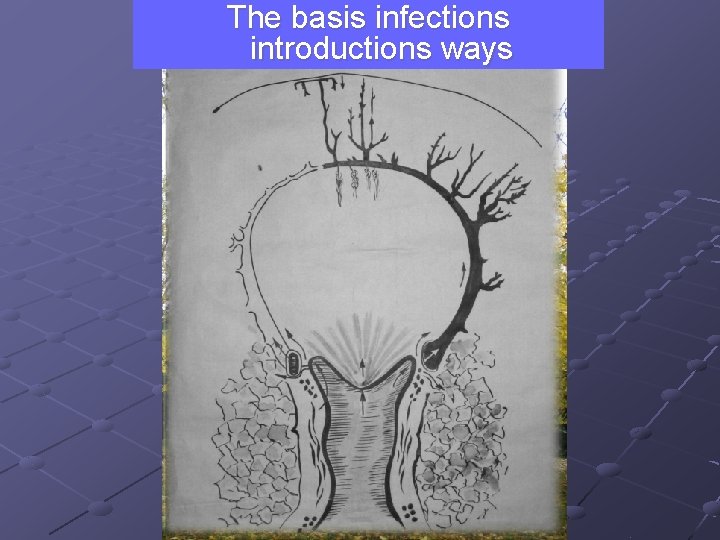
Factors, which are helping in the development of Pyelonephritis 1. The infections introductions ways (microorganisms don’t filtrate) а) ascending perineum is colonized E. coli women's urethra is shot б) haematogenic peritubular vessels blood flow is slow fagocytosis is low other vessels plasmacoagulated exciter local changes in parenchyma
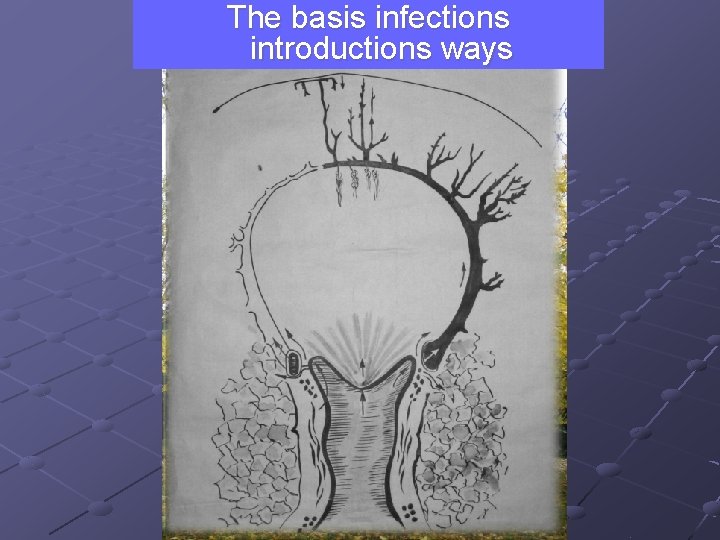
The basis infections introductions ways
Factors, which are helping in the development of Pyelonephritis 2. Kind and character of infections - virulent ( high bacteria's adhesive ability to urogenital and vaginal cells) no virulent plasmacoagulated (staphylococcus spp. ) no plasmacoagulated
Factors are helping in the progression of pyelonephritis 3. Local changes in the urogenital system - According to pathologic process а) failure of urodinamics anatomical (obstructional cause) -Urinary Stone Disease -tumour of urogenital system -congenital anomalia -acquisitional strictures of ureter -infravesical ostruction -pregnancy -prolapse of genital organs & urinary bladder among women functional -neurogenic problems (central genesis, detrusional sphincnteric dissenergy, chronic diabeters nephropathy– 70%) -urinary bladder-ureter reflux б) forein body in the urinary tract в) operative treatment in anamnesis - According to consnquences influences of pathological processes - reflux Formation of reservoir of retention urine Organal renal extracellular hypervolumeria Localization infection at kidney Destruction system chink-spase of the kidney -
Factors are promote of development the pyelonephritis 4. 4. Infringement of common resistance the organism 5. diabetes mellitus 6. 7. renal insufficiency immunosupresive conditions
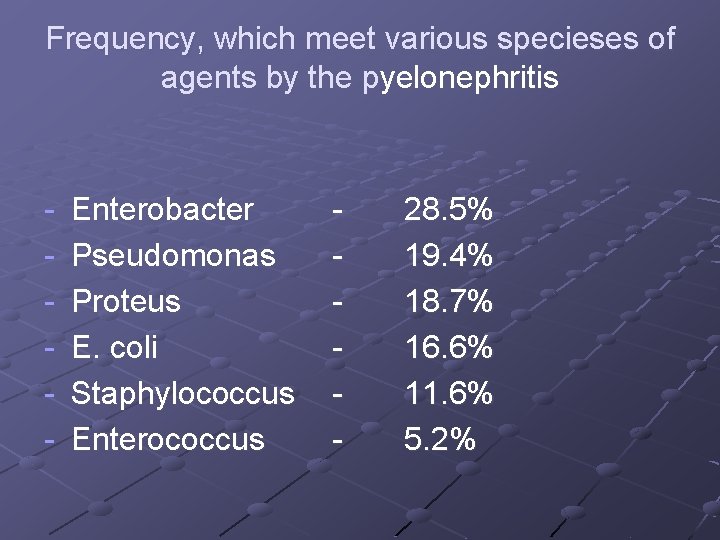
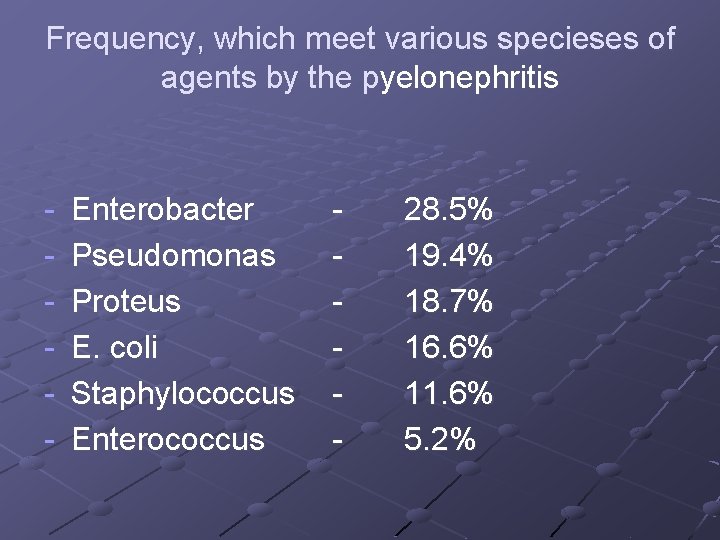
Frequency, which meet various specieses of agents by the pyelonephritis - Enterobacter Pseudomonas Proteus E. coli Staphylococcus Enterococcus - 28. 5% 19. 4% 18. 7% 16. 6% 11. 6% 5. 2%
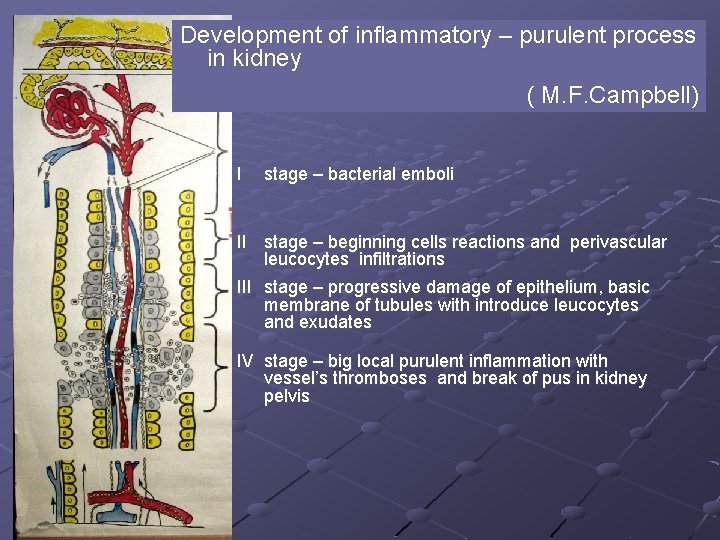
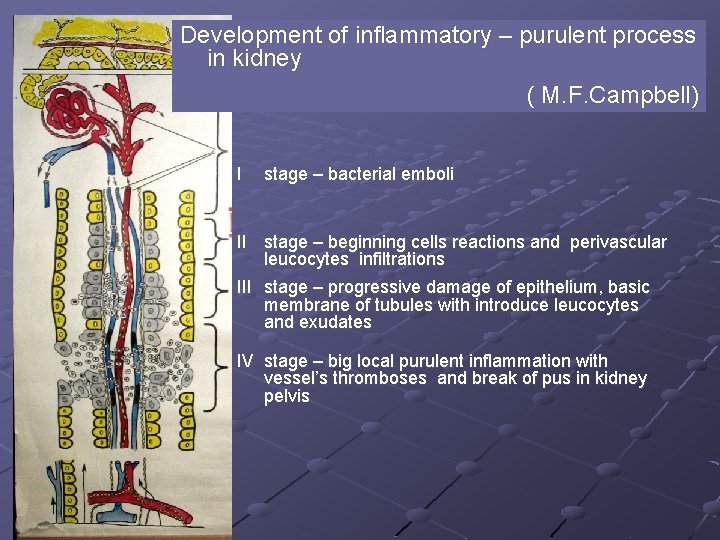
Development of inflammatory – purulent process in kidney ( M. F. Campbell) I stage – bacterial emboli II stage – beginning cells reactions and perivascular leucocytes infiltrations III stage – progressive damage of epithelium, basic membrane of tubules with introduce leucocytes and exudates IV stage – big local purulent inflammation with vessel’s thromboses and break of pus in kidney pelvis
Diagnostics of acute pyelonephritis (III stage) Clinic symptoms High temperature fever and down sweat artralgia and mialgia headache, nausea and vomitus arterial hypertension, bacterial shock Local symptoms Pain and muscular depend in back dysuria muddy urea polyuria, nocturia positive Pasternatsky symptom
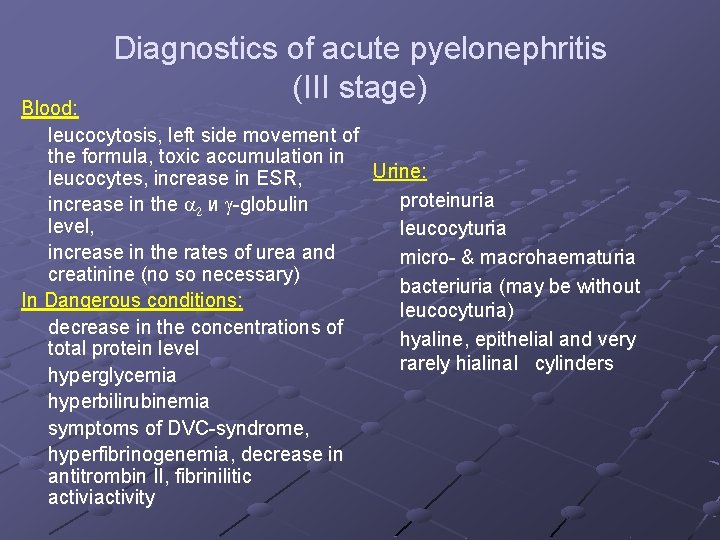
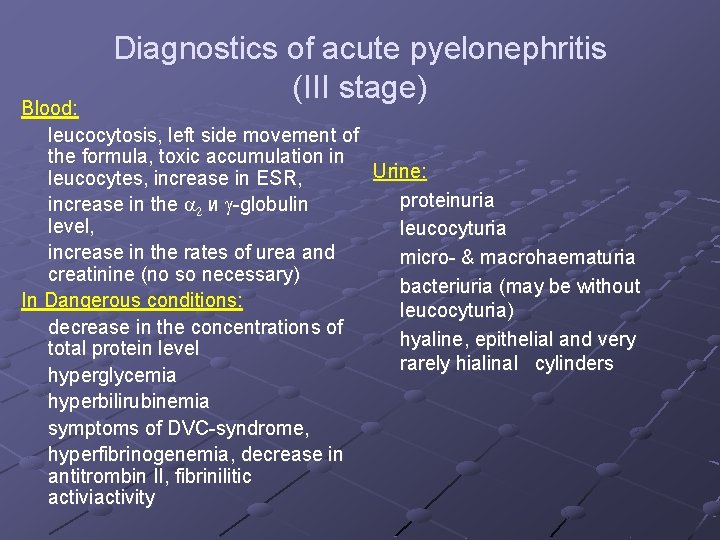
Diagnostics of acute pyelonephritis (III stage) Blood: leucocytosis, left side movement of the formula, toxic accumulation in Urine: leucocytes, increase in ESR, proteinuria increase in the a 2 и g-globulin level, leucocyturia increase in the rates of urea and micro- & macrohaematuria creatinine (no so necessary) bacteriuria (may be without In Dangerous conditions: leucocyturia) decrease in the concentrations of hyaline, epithelial and very total protein level rarely hialinal cylinders hyperglycemia hyperbilirubinemia symptoms of DVC-syndrome, hyperfibrinogenemia, decrease in antitrombin II, fibrinilitic activity
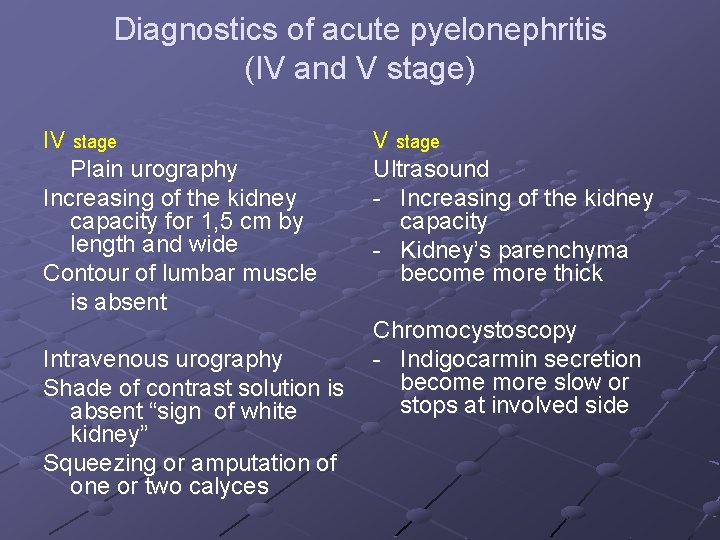
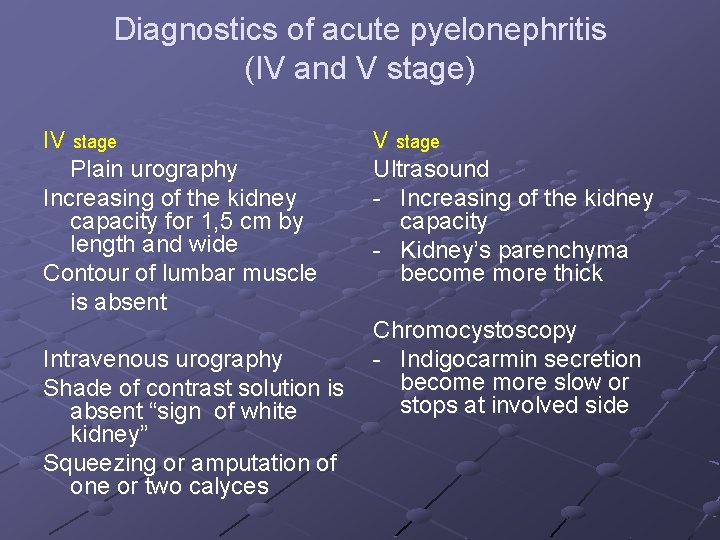
Diagnostics of acute pyelonephritis (IV and V stage) IV stage Plain urography Increasing of the kidney capacity for 1, 5 cm by length and wide Contour of lumbar muscle is absent Intravenous urography Shade of contrast solution is absent “sign of white kidney” Squeezing or amputation of one or two calyces V stage Ultrasound - Increasing of the kidney capacity - Kidney’s parenchyma become more thick Chromocystoscopy - Indigocarmin secretion become more slow or stops at involved side

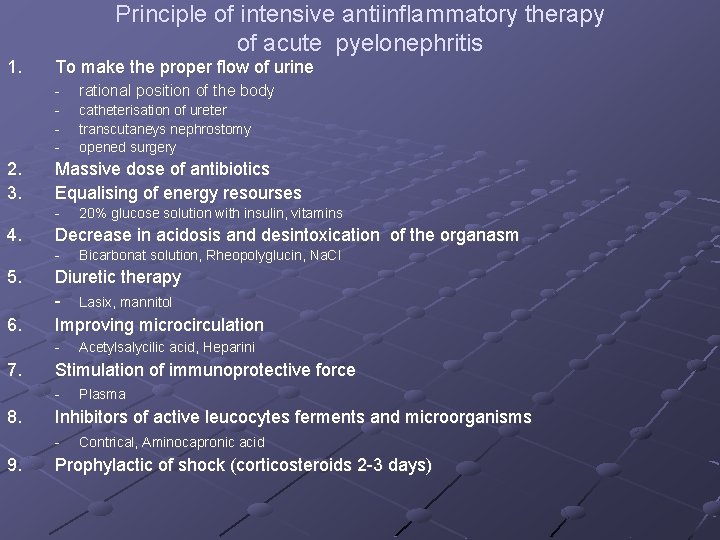
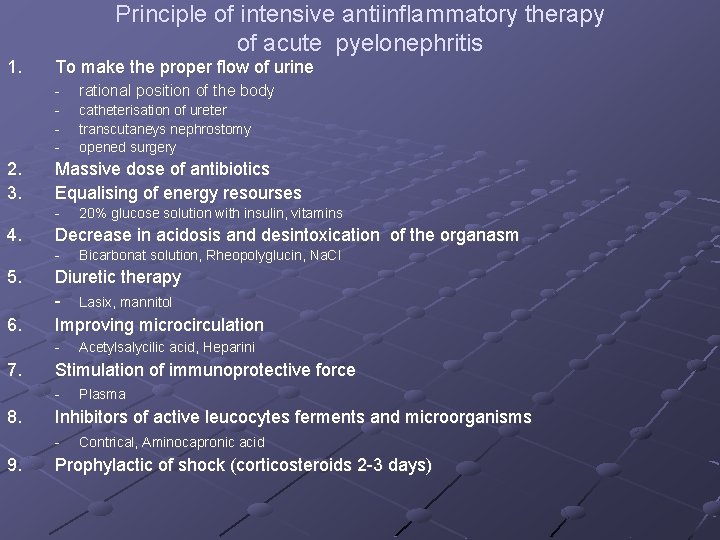
1. 2. 3. Principle of intensive antiinflammatory therapy of acute pyelonephritis To make the proper flow of urine - rational position of the body - catheterisation of ureter transcutaneys nephrostomy opened surgery Massive dose of antibiotics Equalising of energy resourses - 4. Decrease in acidosis and desintoxication of the organasm - 5. 6. Plasma Inhibitors of active leucocytes ferments and microorganisms - 9. Acetylsalycilic acid, Heparini Stimulation of immunoprotective force - 8. Bicarbonat solution, Rheopolyglucin, Na. Cl Diuretic therapy - Lasix, mannitol Improving microcirculation - 7. 20% glucose solution with insulin, vitamins Contrical, Aminocapronic acid Prophylactic of shock (corticosteroids 2 -3 days)
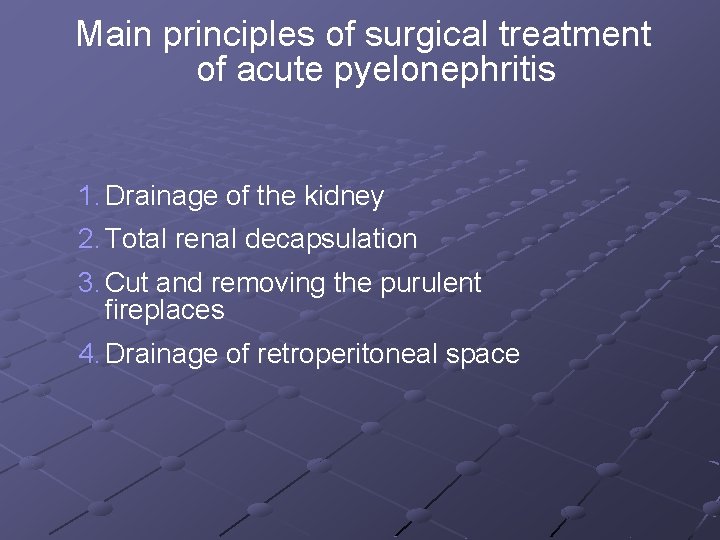
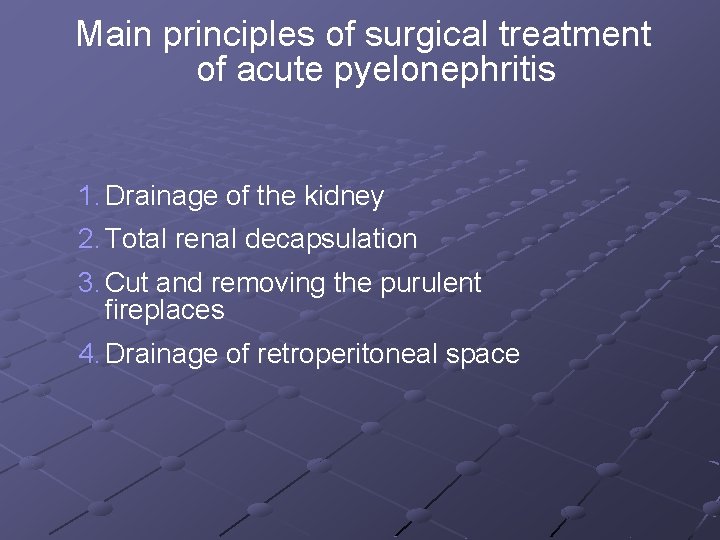
Main principles of surgical treatment of acute pyelonephritis 1. Drainage of the kidney 2. Total renal decapsulation 3. Cut and removing the purulent fireplaces 4. Drainage of retroperitoneal space
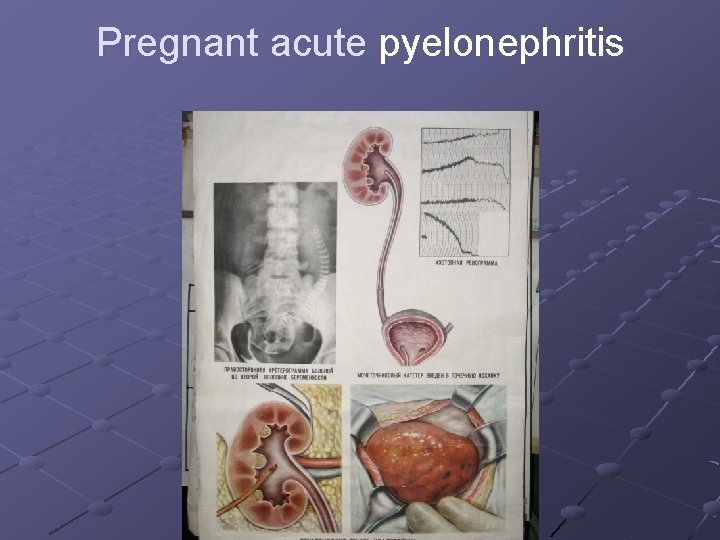
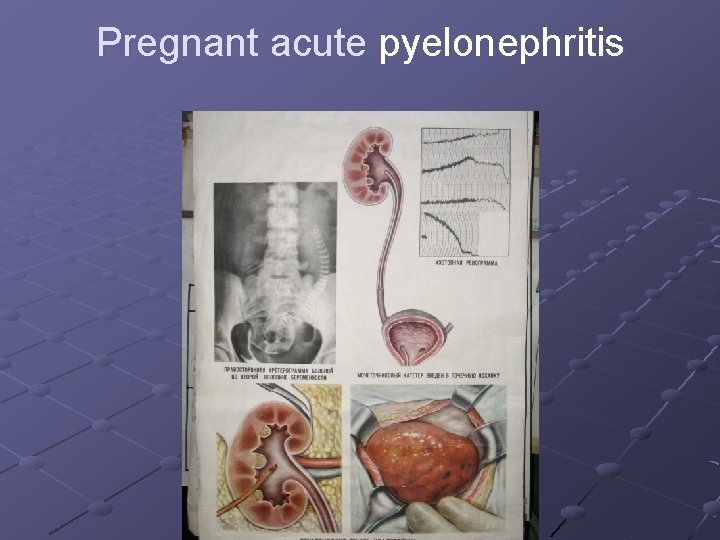
Pregnant acute pyelonephritis
Shock It is an extreme condition of the life, which is caused by the abundant stimulants and characterized by the progressive destruction (or) dysfunction life essential organs. First of all it affects hemodynamics and metabolism. Bacteriemic (septic or toxic-infectious shock) is one of the types of shock, it the main reason is infection and it causes paresis of peripheric vessels.
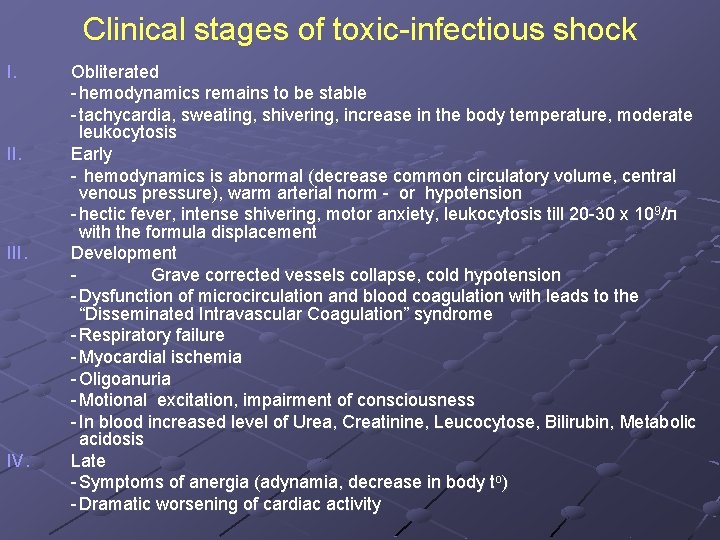
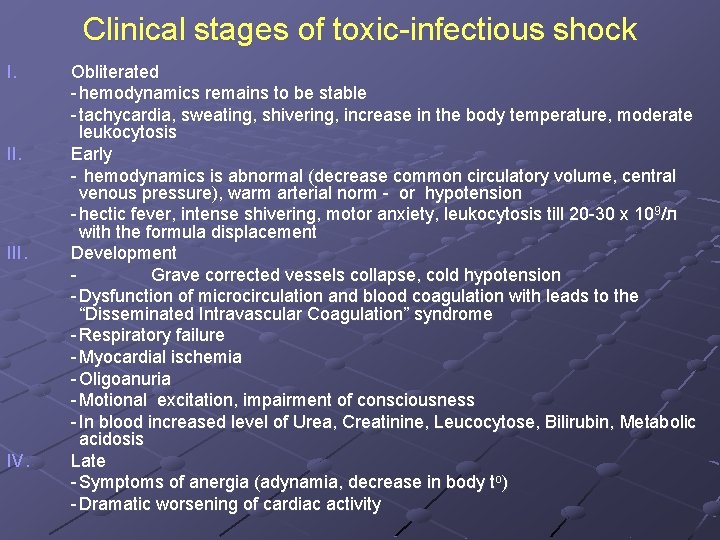
Clinical stages of toxic-infectious shock I. III. IV. Obliterated - hemodynamics remains to be stable - tachycardia, sweating, shivering, increase in the body temperature, moderate leukocytosis Early - hemodynamics is abnormal (decrease common circulatory volume, central venous pressure), warm arterial norm - or hypotension - hectic fever, intense shivering, motor anxiety, leukocytosis till 20 -30 х 109/л with the formula displacement Development Grave corrected vessels collapse, cold hypotension - Dysfunction of microcirculation and blood coagulation with leads to the “Disseminated Intravascular Coagulation” syndrome - Respiratory failure - Myocardial ischemia - Oligoanuria - Motional excitation, impairment of consciousness - In blood increased level of Urea, Creatinine, Leucocytose, Bilirubin, Metabolic acidosis Late - Symptoms of anergia (adynamia, decrease in body tо) - Dramatic worsening of cardiac activity
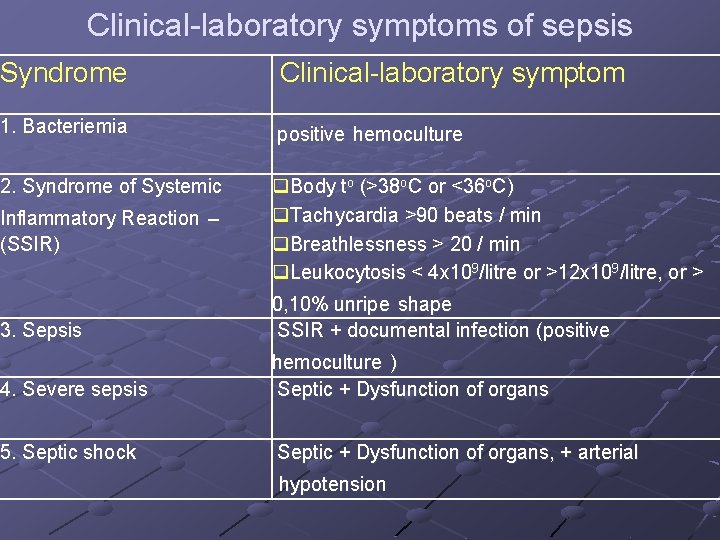
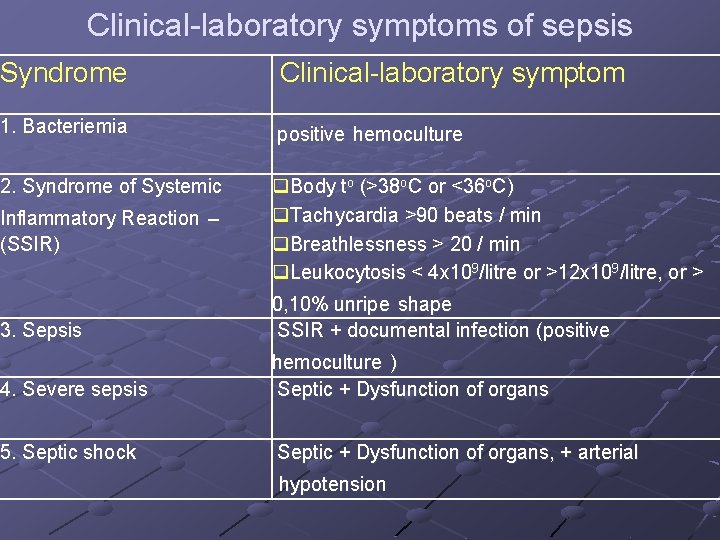
Clinical-laboratory symptoms of sepsis Syndrome Clinical-laboratory symptom 1. Bacteriemia positive hemoculture 2. Syndrome of Systemic q. Body tо (>38 о. С or <36 о. С) q. Tachycardia >90 beats / min q. Breathlessness > 20 / min q. Leukocytosis < 4 х109/litre or >12 х109/litre, or > Inflammatory Reaction – (SSIR) 3. Sepsis 0, 10% unripe shape SSIR + documental infection (positive 4. Severe sepsis hemoculture ) Septic + Dysfunction of organs 5. Septic shock Septic + Dysfunction of organs, + arterial hypotension
Forms of urosepsis I. II. IV. V. Bacteriemic shock - heaviness of clinical course wipe high-grade - the time of beginning early late Acute Lengthy acute Lengthy subacute Chronic
Principle of the treatment of bacteriemic shock 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. Vasopressor therapy (corticosteroids, adrenomimetics, dopamine) Plasma substitut therapy (polyglucin, helofusin) Recovery of the protein balance (albumin, plasma) Improvement of the blood microcirculation (rheopolyglucin, trental, heparin) Recovery of the water-electrolyte balance (0, 9% Na. Cl) Decrease of the acidosis (3% Na. HCO 3) Recovery of the urine passage from the kidney Antibacterial therapy Diuretic therapy Improvement of the nitrogen metabolism (testosterone propionate, retabolil) Desensitizing therapy Usage of the protease inhibitor (hordox, contrical) Immunotherapy (g - globulin, immune plasma, lysozyme, interferon, т activin, thymalin, methyluracil) Efferent methods of treatment (hemosorption, plasmapheresis, hemodialysis)
Diagnostic of chronic pyelonephritis In the exacerbation Symptoms are similar to acute pyelonephritis I and II phase - Common clinical symptoms occasionally «unfounded» increase the temperature profuse sweating, particularly in night change of the face colour (subicteritiousness, the skin colour - is earthy) xerodermia general weakness, fatigability, headache anorexia sickness, retching hypertension - Local symptoms pain, unpleasant sensation in regio lumbalis polyuria, nicturia disuria flakes, cloudy urine
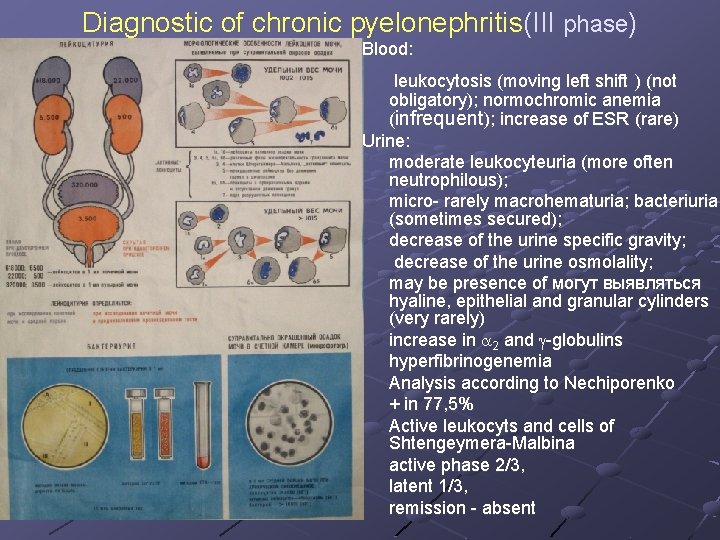
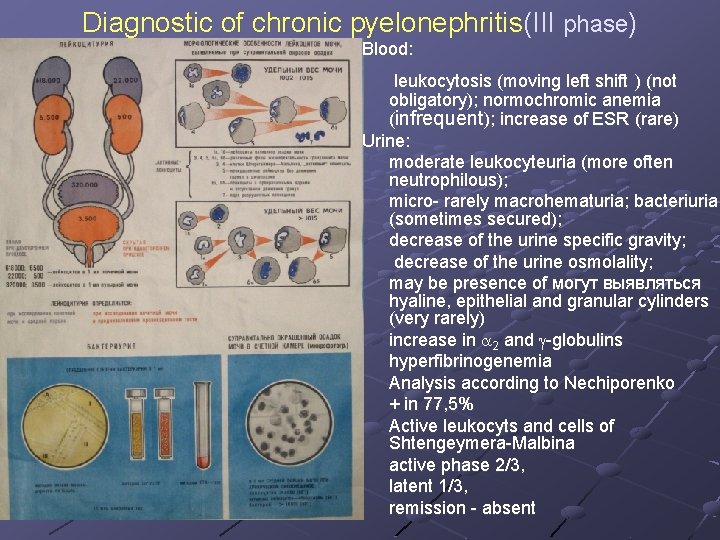
Diagnostic of chronic pyelonephritis(III phase) Blood: leukocytosis (moving left shift ) (not obligatory); normochromic anemia (infrequent); increase of ESR (rare) Urine: moderate leukocyteuria (more often neutrophilous); micro- rarely macrohematuria; bacteriuria (sometimes secured); decrease of the urine specific gravity; decrease of the urine osmolality; may be presence of могут выявляться hyaline, epithelial and granular cylinders (very rarely) increase in a 2 and g-globulins hyperfibrinogenemia Analysis according to Nechiporenko + in 77, 5% Active leukocyts and cells of Shtengeymera-Malbina active phase 2/3, latent 1/3, remission - absent
Diagnostic of chronic pyelonephritis(III phase) causes of the pyuria without the bacteriuria Atypical microorganisms Noninfectious diseases Micobacteria Stones Fungus Trauma Chlamydia trachomatis Tumor N. gonorrhoeae Glomerulonephritis Herpes simplex virus Vaginal contamination Cyclophosphamid
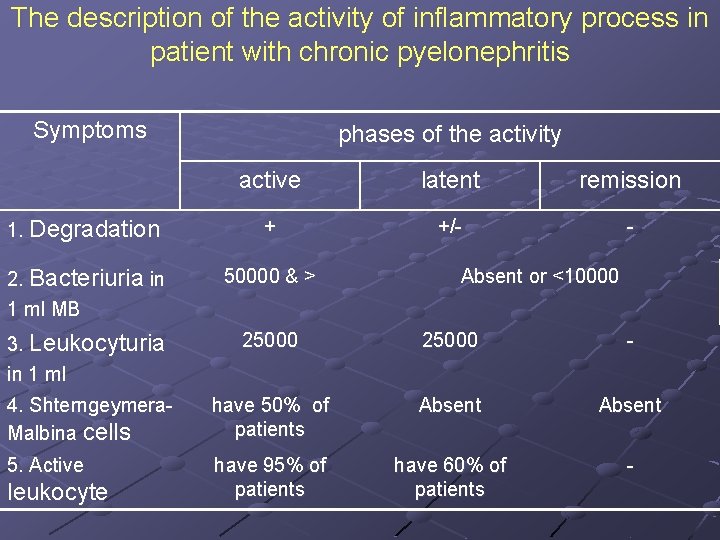
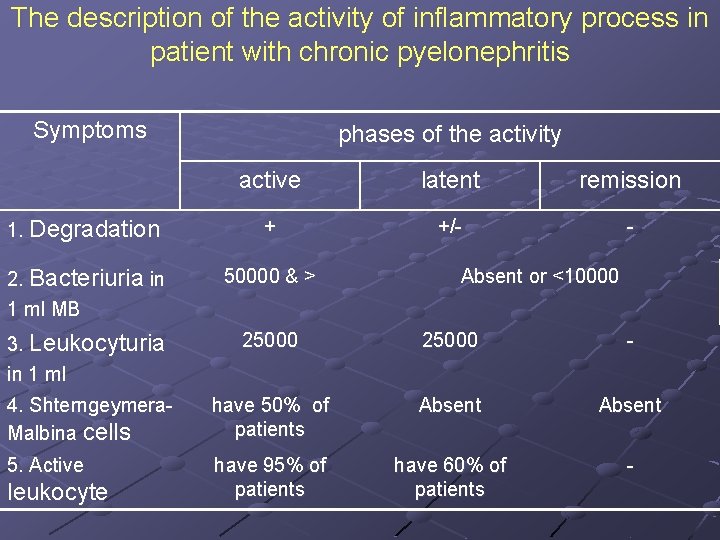
The description of the activity of inflammatory process in patient with chronic pyelonephritis Symptoms phases of the activity active latent remission 1. Degradation + +/- - 2. Bacteriuria in 1 ml МB 50000 & > 3. Leukocyturia in 1 ml 25000 - 4. Shterngeymera. Malbina cells have 50% of patients Absent 5. Active have 95% of patients have 60% of patients - leukocyte Absent or <10000
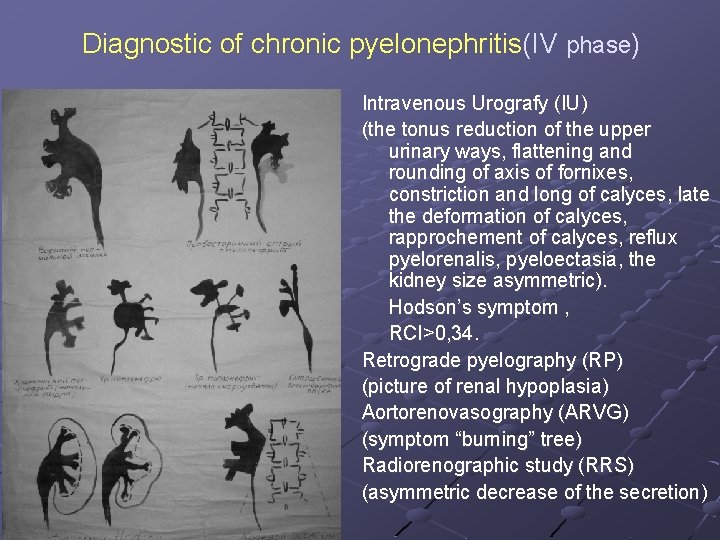
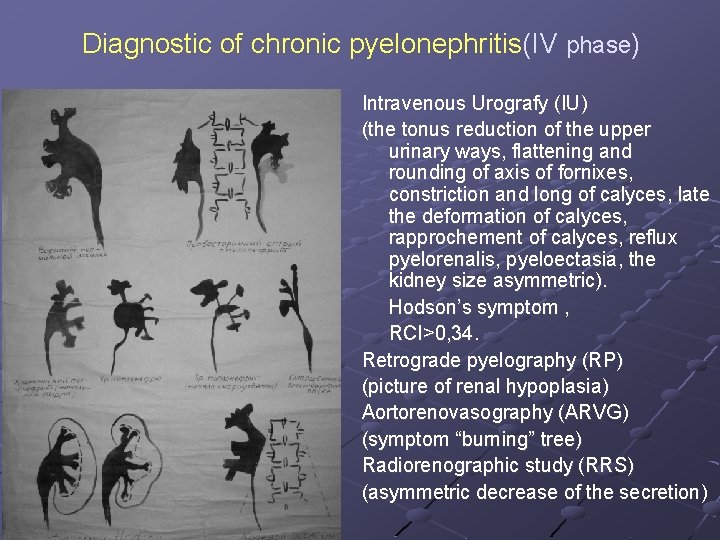
Diagnostic of chronic pyelonephritis(IV phase) Intravenous Urografy (IU) (the tonus reduction of the upper urinary ways, flattening and rounding of axis of fornixes, constriction and long of calyces, late the deformation of calyces, rapprochement of calyces, reflux pyelorenalis, pyeloectasia, the kidney size asymmetric). Hodson’s symptom , RCI>0, 34. Retrograde pyelography (RP) (picture of renal hypoplasia) Aortorenovasography (АRVG) (symptom “burning” tree) Radiorenographic study (RRS) (asymmetric decrease of the secretion)
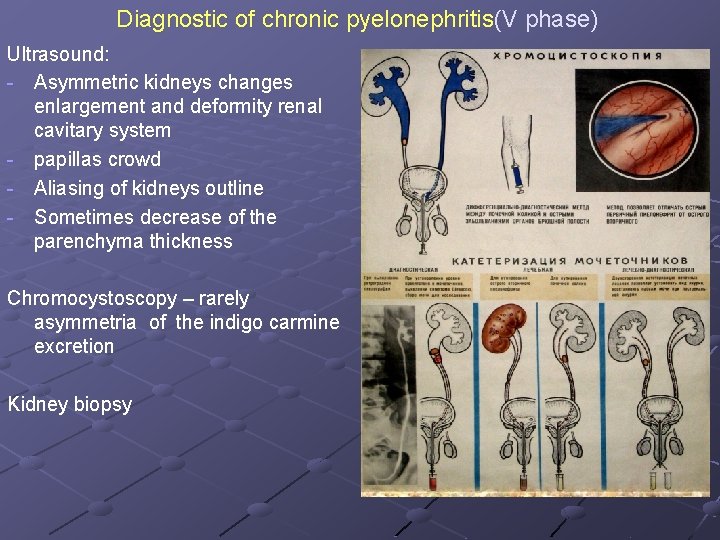
Diagnostic of chronic pyelonephritis(V phase) Ultrasound: - Asymmetric kidneys changes enlargement and deformity renal cavitary system - papillas crowd - Aliasing of kidneys outline - Sometimes decrease of the parenchyma thickness Chromocystoscopy – rarely asymmetria of the indigo carmine excretion Kidney biopsy
Length of chronic pyelonephritis treatment - Not less 6 -8 monthes: first 2 -3 monthes right along next 3 -6 monthes interrupted courses - If pyelonephritis recurrence : interrupted courses since 1 -1, 5 years by 3 years
The peculiarity of complicated UTI (in contrast to simple, uncomplicated UTI) 1. Manifest multidrug resistance 2. Require more long courses of antibacterial treatment 3. Require more intensive urological investigation and treatment
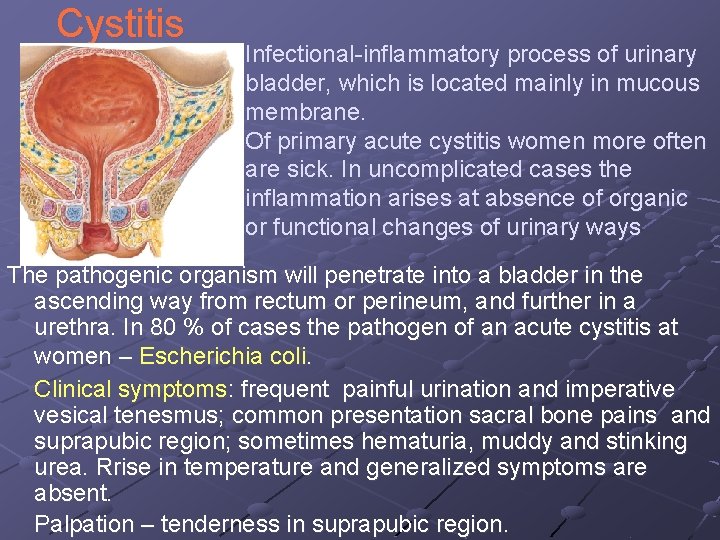
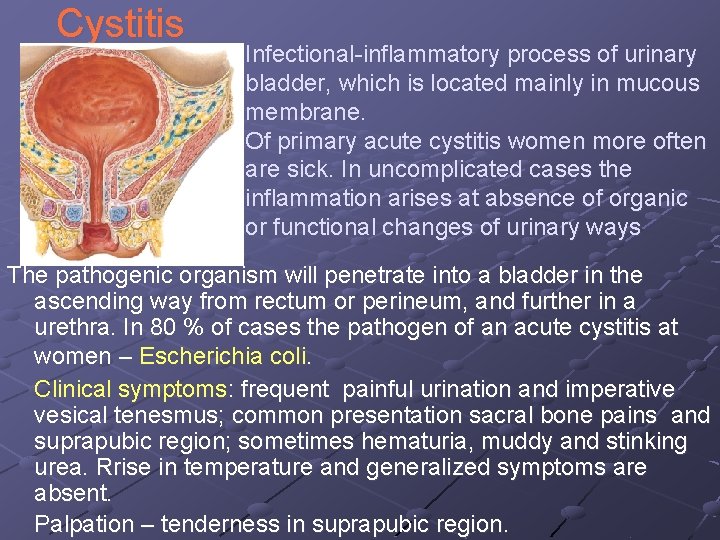
Cystitis Infectional-inflammatory process of urinary bladder, which is located mainly in mucous membrane. Of primary acute cystitis women more often are sick. In uncomplicated cases the inflammation arises at absence of organic or functional changes of urinary ways The pathogenic organism will penetrate into a bladder in the ascending way from rectum or perineum, and further in a urethra. In 80 % of cases the pathogen of an acute cystitis at women – Escherichia coli. Clinical symptoms: frequent painful urination and imperative vesical tenesmus; common presentation sacral bone pains and suprapubic region; sometimes hematuria, muddy and stinking urea. Rrise in temperature and generalized symptoms are absent. Palpation – tenderness in suprapubic region.
Cystitis Diagnostic – in urine analysis is revealed leucocyturia, bacteriuria and rarely hematuria. Urine for the bacteriological analysis take in sterile utensils from an average portion at urination after a careful toilet of an external aperture of urethra of cases the pathogen of acute cystitis, at women of a vulva and introduction in a vagina of a sterile tampon. Absence of growth of bacteria does not exclude a cystitis. Possible pathogenic organisms in that case clamydia, ureaplasmas, mycoplasmas. For exception of the complicated infection (a secondary cystitis) or a recurrent infection carry out the investigations directed to diagnostic its reasons (Ultrasound, Plane Urography, Intravenous Urography, Cystoscopy).
Cystitis Treatment starts with shot course (5 -7 day) antibacterial drugs wide spectrum movement, effective in relation to the majority of pathogenic microorganisms. Augmentin, trimetoprim with sulfamethoxazol, cifran, nitrofurantoin, roxytromycin. Besides ABD prescribe sparing diet, thermal procedure , analgetic, spasmolytics. In patient with bladder unstability – oxybutinin.

Prostatitis and chronic pelvic pain syndrome (CPPS) Bacterial prostatitis is a disease entity diagnosed clinically and by evidence of inflammation and infection localized to the prostate. According to the duration of symptoms, bacterial prostatitis is either acute or chronic, when symptoms persist for at least 3 months.
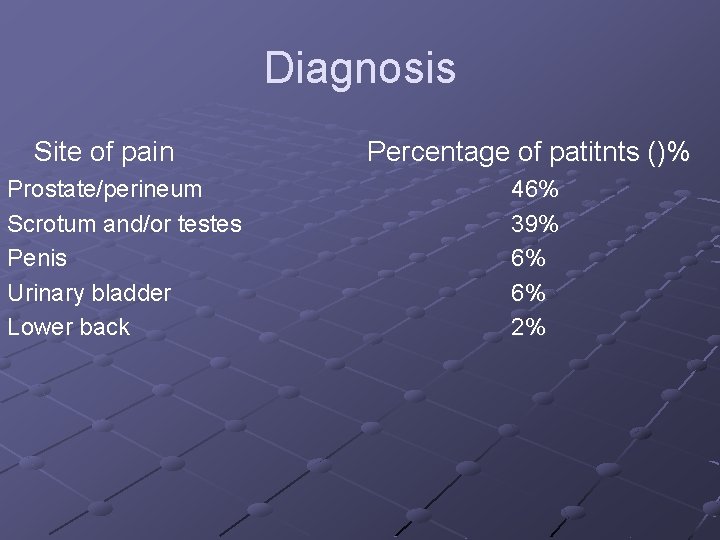
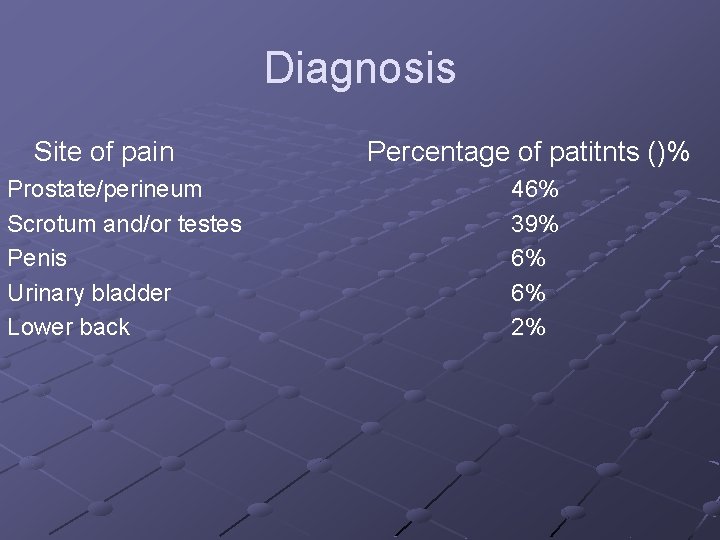
Diagnosis Site of pain Prostate/perineum Scrotum and/or testes Penis Urinary bladder Lower back Percentage of patitnts ()% 46% 39% 6% 6% 2%
Lower urinary tract symptoms in prostatititis and CPPS n n n Frequent need to urinate Difficulty urination, e. g. weak stream and straining Pain on urination, or that increases with urination
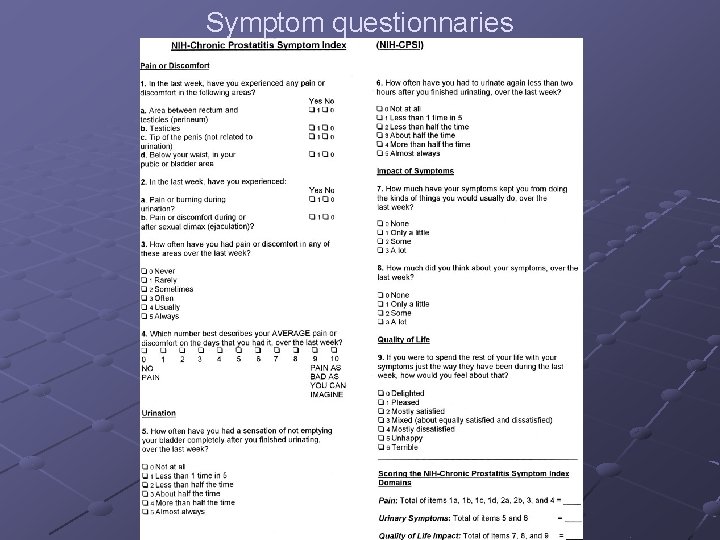
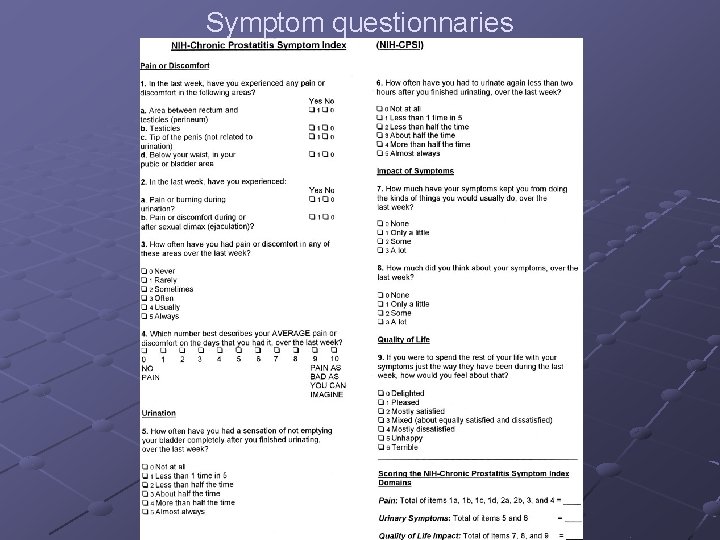
Symptom questionnaries
Clinical findins In acute prostatitis, the prostate may be swollen and tender on digital rectal examination (DRE). Prostatic massage is contraindicated. Otherwise, the prostate is usually normal on palpation.
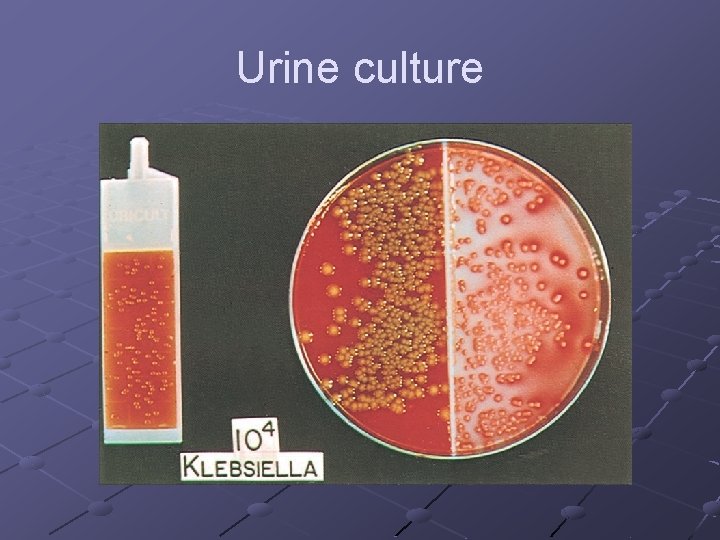
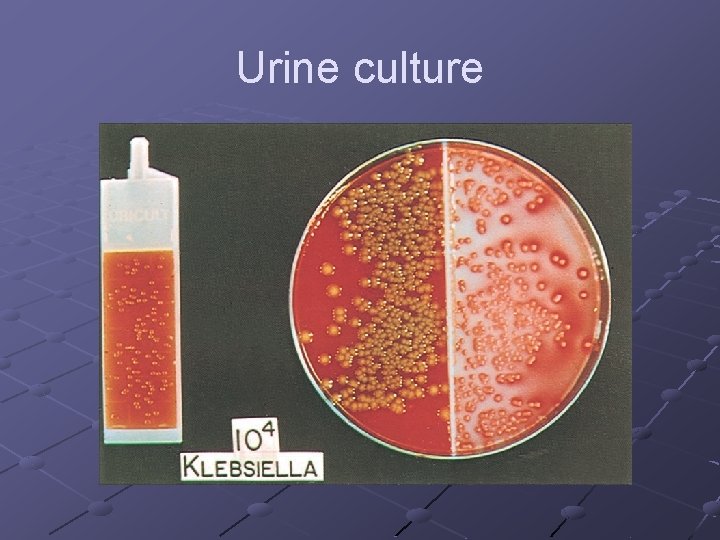
Urine culture
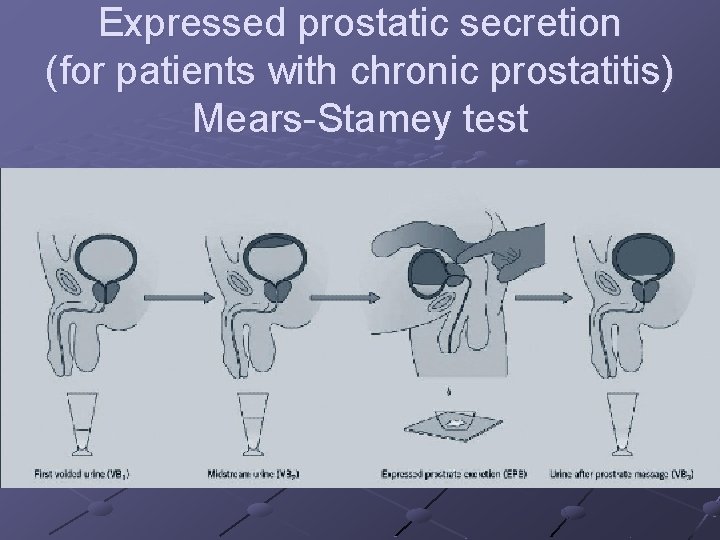
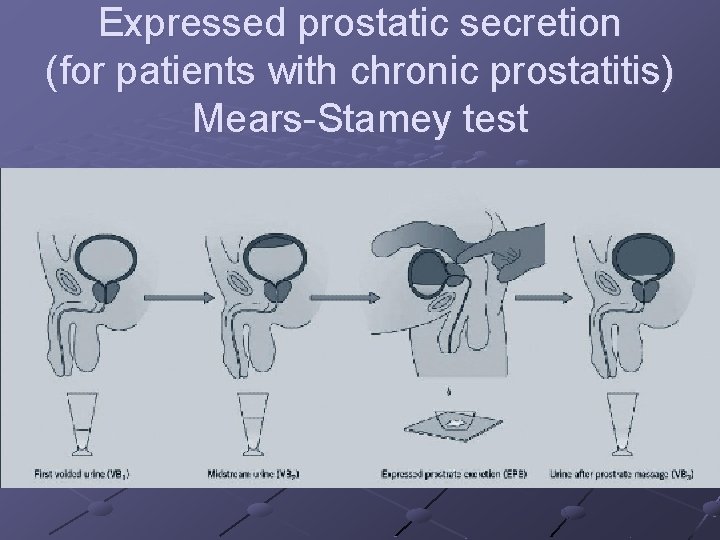
Expressed prostatic secretion (for patients with chronic prostatitis) Mears-Stamey test
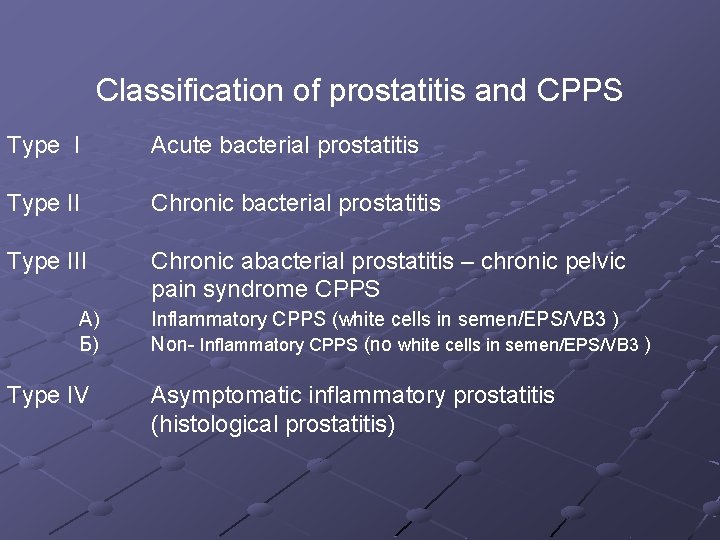
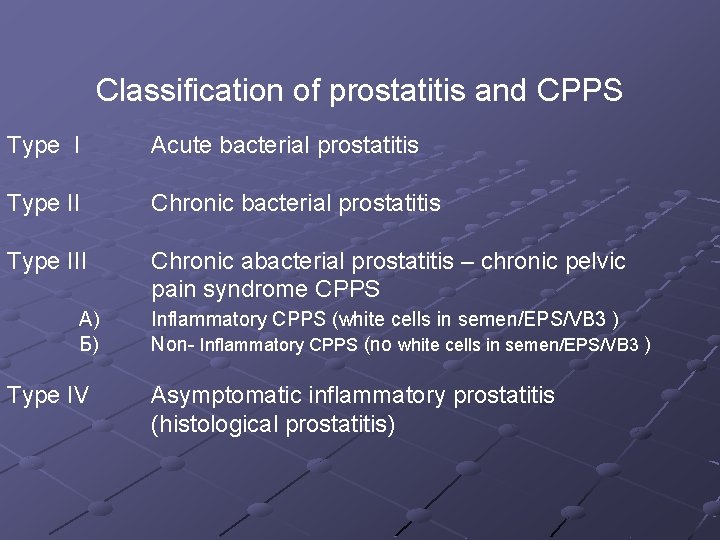
Classification of prostatitis and CPPS Type I Acute bacterial prostatitis Type II Chronic bacterial prostatitis Type III Chronic abacterial prostatitis – chronic pelvic pain syndrome CPPS А) Б) Type IV Inflammatory CPPS (white cells in semen/EPS/VB 3 ) Non- Inflammatory CPPS (no white cells in semen/EPS/VB 3 ) Asymptomatic inflammatory prostatitis (histological prostatitis)
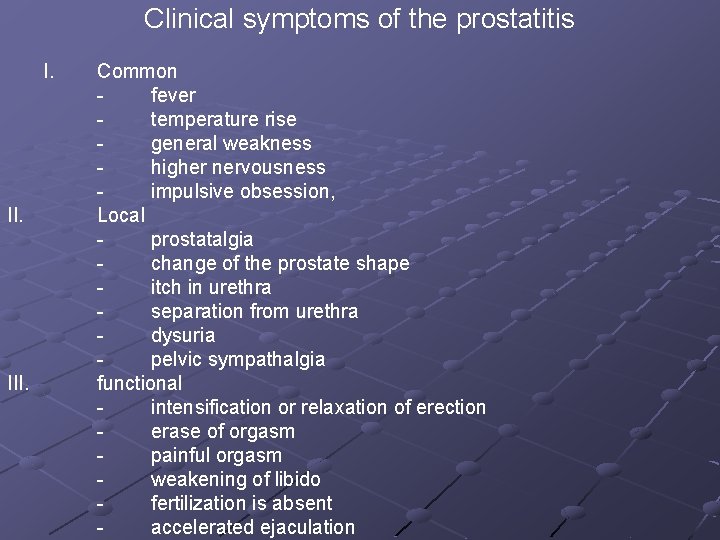
Clinical symptoms of the prostatitis I. III. Common fever temperature rise general weakness higher nervousness impulsive obsession, Local prostatalgia change of the prostate shape itch in urethra separation from urethra dysuria pelvic sympathalgia functional intensification or relaxation of erection erase of orgasm painful orgasm weakening of libido fertilization is absent accelerated ejaculation
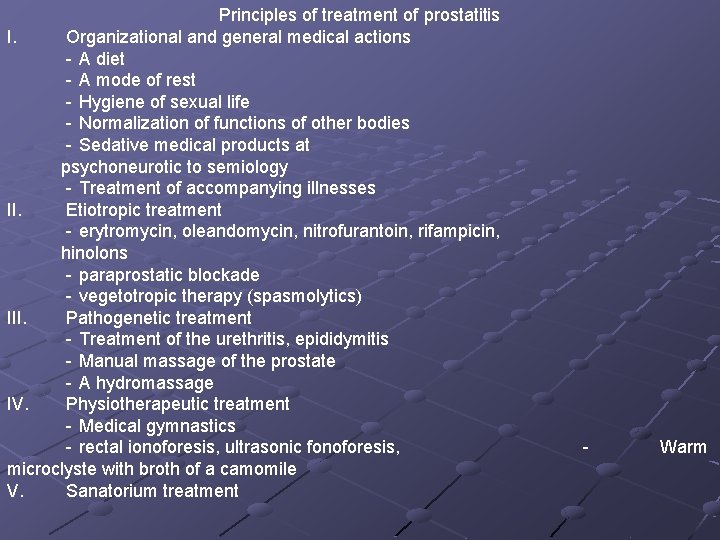
Principles of treatment of prostatitis I. Organizational and general medical actions - A diet - A mode of rest - Hygiene of sexual life - Normalization of functions of other bodies - Sedative medical products at psychoneurotic to semiology - Treatment of accompanying illnesses II. Etiotropic treatment - erytromycin, oleandomycin, nitrofurantoin, rifampicin, hinolons - paraprostatic blockade - vegetotropic therapy (spasmolytics) III. Pathogenetic treatment - Treatment of the urethritis, epididymitis - Manual massage of the prostate - A hydromassage IV. Physiotherapeutic treatment - Medical gymnastics - rectal ionoforesis, ultrasonic fonoforesis, microclyste with broth of a camomile V. Sanatorium treatment - Warm
 Complicated uti symptoms
Complicated uti symptoms Complicated urinary tract infection
Complicated urinary tract infection Histological structure of kidney
Histological structure of kidney Urethra
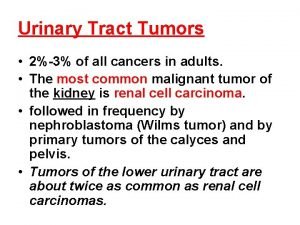
Urethra Tumor in the urinary tract
Tumor in the urinary tract Urinary tract infection in pregnancy ppt
Urinary tract infection in pregnancy ppt Urised otc
Urised otc Bladder infection symptoms
Bladder infection symptoms Pyramidal vs extrapyramidal tract
Pyramidal vs extrapyramidal tract Olivospinal tract vs tectospinal tract
Olivospinal tract vs tectospinal tract Development of urinary bladder
Development of urinary bladder Bladder mesoderm
Bladder mesoderm Dr donaldson urology
Dr donaldson urology Urology near oakley
Urology near oakley Urology match
Urology match Urology match
Urology match Rpug in urology
Rpug in urology Children urology
Children urology Dr hassan urology
Dr hassan urology Urology
Urology Vaginal agensis
Vaginal agensis Refhelp
Refhelp Pediatric urology salary
Pediatric urology salary Urology coding cheat sheet
Urology coding cheat sheet Ubc urology
Ubc urology Srmc urology
Srmc urology What are the objectives of clinical pharmacy
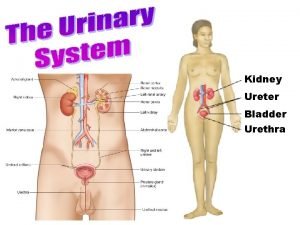
What are the objectives of clinical pharmacy Introduction of urinary system
Introduction of urinary system Urinary bladder apex and base
Urinary bladder apex and base Superior surface of urinary bladder
Superior surface of urinary bladder Surface of urinary bladder
Surface of urinary bladder Figure 15-3 is a diagram of the nephron
Figure 15-3 is a diagram of the nephron Superior surface of urinary bladder
Superior surface of urinary bladder Py/o medical term
Py/o medical term Urinary system facts
Urinary system facts Cvc care bundle checklist
Cvc care bundle checklist Mammary papilla pig
Mammary papilla pig Chapter 30 the urinary system workbook answers
Chapter 30 the urinary system workbook answers Chapter 22 urinary elimination
Chapter 22 urinary elimination Kidney pyramid labeled
Kidney pyramid labeled Lesson 14.2 male and female urinary structures
Lesson 14.2 male and female urinary structures Order of urine flow through kidney
Order of urine flow through kidney Nephron urinary system
Nephron urinary system Spermatic cord
Spermatic cord Negative leukocyte esterase
Negative leukocyte esterase Chapter 25 urinary catheters
Chapter 25 urinary catheters Chapter 24 urinary elimination
Chapter 24 urinary elimination Chapter 22 urinary elimination
Chapter 22 urinary elimination Chapter 20 urinary/excretory system
Chapter 20 urinary/excretory system _____ is difficulty in starting a urinary stream.
_____ is difficulty in starting a urinary stream. Urinary system model
Urinary system model Urinary system fun fact
Urinary system fun fact