Development of Urinary Male Genital System M Mansyur





- Slides: 43
Development of Urinary & Male Genital System M. Mansyur Romi
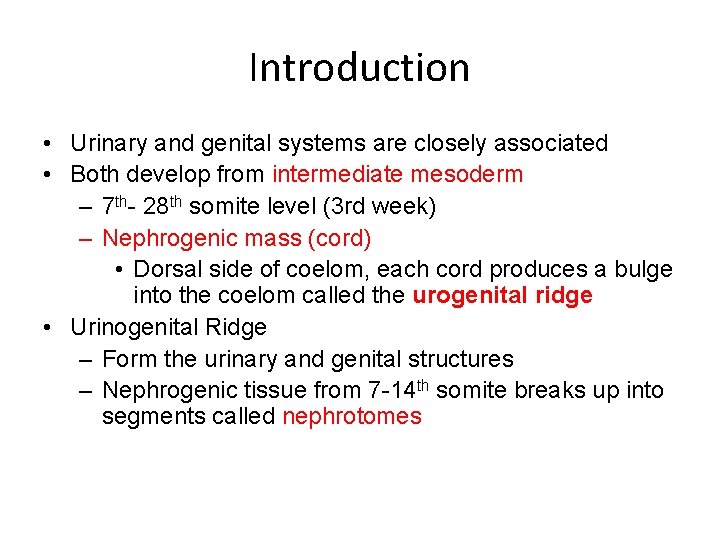
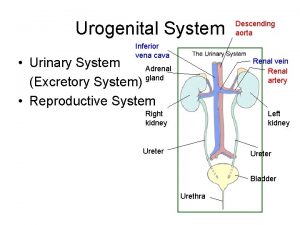
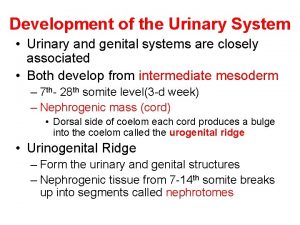
Introduction • Urinary and genital systems are closely associated • Both develop from intermediate mesoderm – 7 th- 28 th somite level (3 rd week) – Nephrogenic mass (cord) • Dorsal side of coelom, each cord produces a bulge into the coelom called the urogenital ridge • Urinogenital Ridge – Form the urinary and genital structures – Nephrogenic tissue from 7 -14 th somite breaks up into segments called nephrotomes
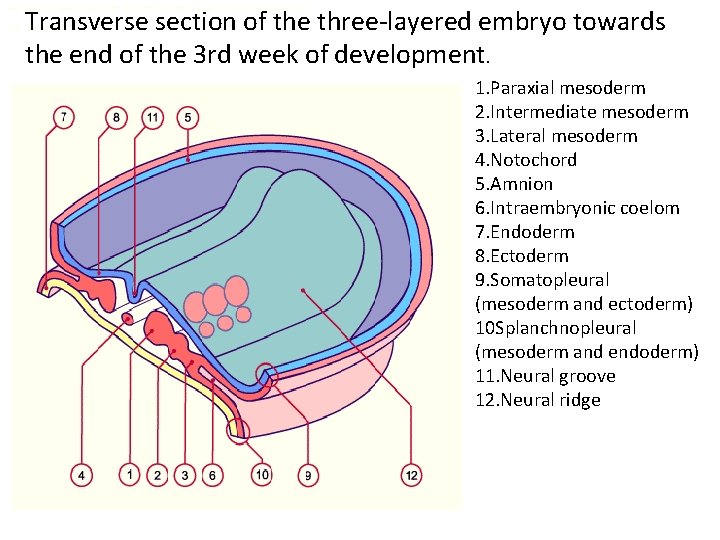
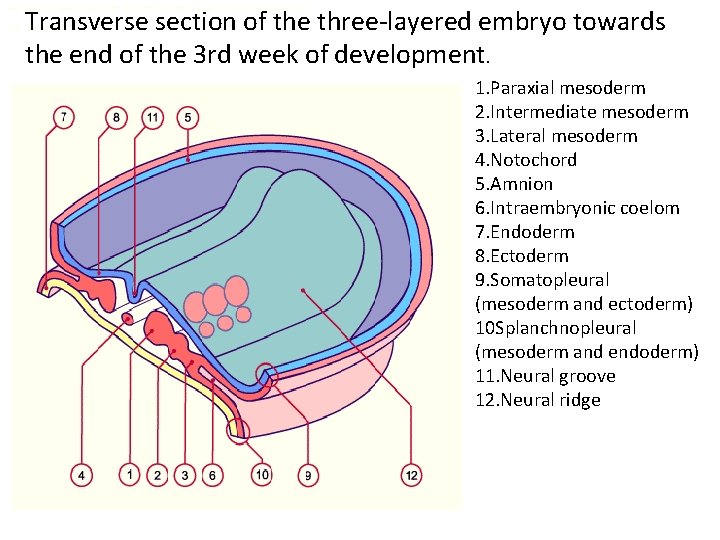
Transverse section and dorsal view of an embryo (trilaminar) Transverse section of the three-layered embryo towards the end of the 3 rd week of development. Fig. 1 - (ca. 21 days) 1. Paraxial mesoderm 2. Intermediate mesoderm 3. Lateral mesoderm 4. Notochord 5. Amnion 6. Intraembryonic coelom 7. Endoderm 8. Ectoderm 9. Somatopleural (mesoderm and ectoderm) 10 Splanchnopleural (mesoderm and endoderm) 11. Neural groove 12. Neural ridge
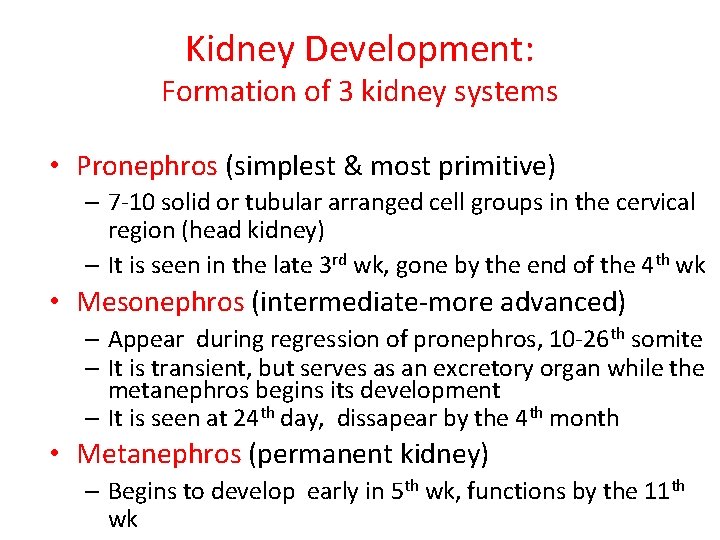
Kidney Development: Formation of 3 kidney systems • Pronephros (simplest & most primitive) – 7 -10 solid or tubular arranged cell groups in the cervical region (head kidney) – It is seen in the late 3 rd wk, gone by the end of the 4 th wk • Mesonephros (intermediate-more advanced) – Appear during regression of pronephros, 10 -26 th somite – It is transient, but serves as an excretory organ while the metanephros begins its development – It is seen at 24 th day, dissapear by the 4 th month • Metanephros (permanent kidney) – Begins to develop early in 5 th wk, functions by the 11 th wk
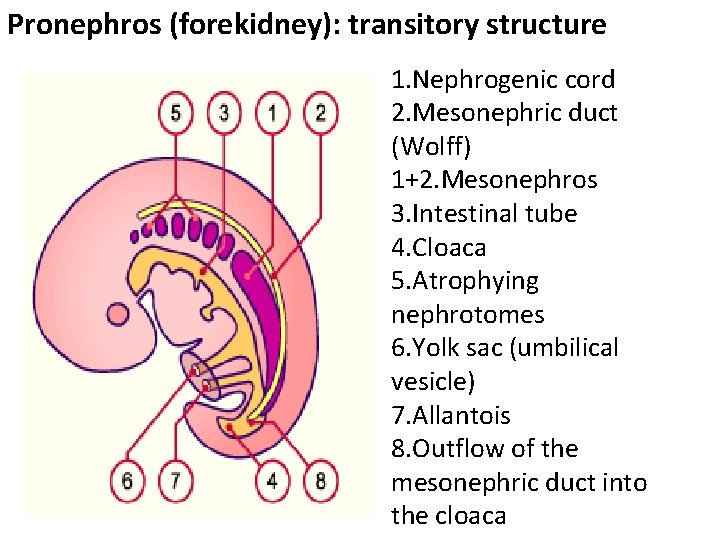
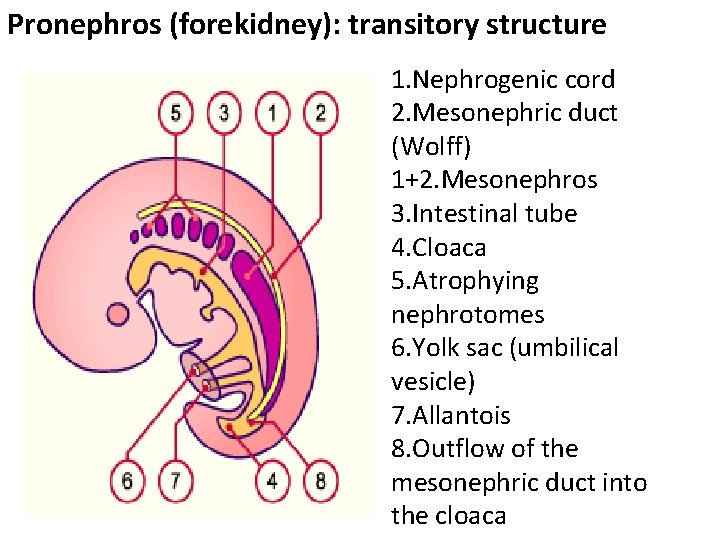
Pronephros (forekidney): transitory structure 1. Nephrogenic cord 2. Mesonephric duct (Wolff) 1+2. Mesonephros 3. Intestinal tube 4. Cloaca 5. Atrophying nephrotomes 6. Yolk sac (umbilical vesicle) 7. Allantois 8. Outflow of the mesonephric duct into the cloaca
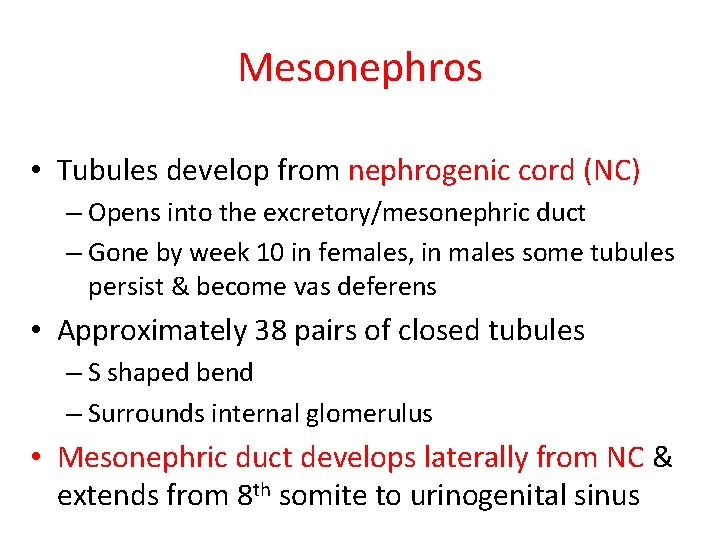
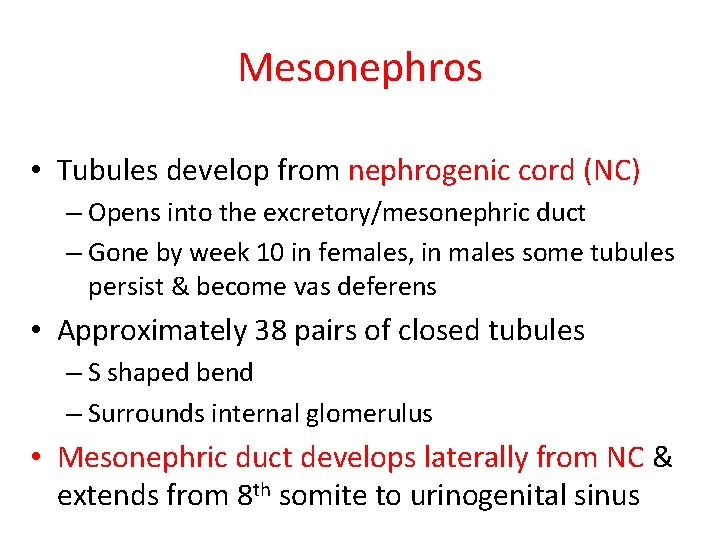
Mesonephros • Tubules develop from nephrogenic cord (NC) – Opens into the excretory/mesonephric duct – Gone by week 10 in females, in males some tubules persist & become vas deferens • Approximately 38 pairs of closed tubules – S shaped bend – Surrounds internal glomerulus • Mesonephric duct develops laterally from NC & extends from 8 th somite to urinogenital sinus
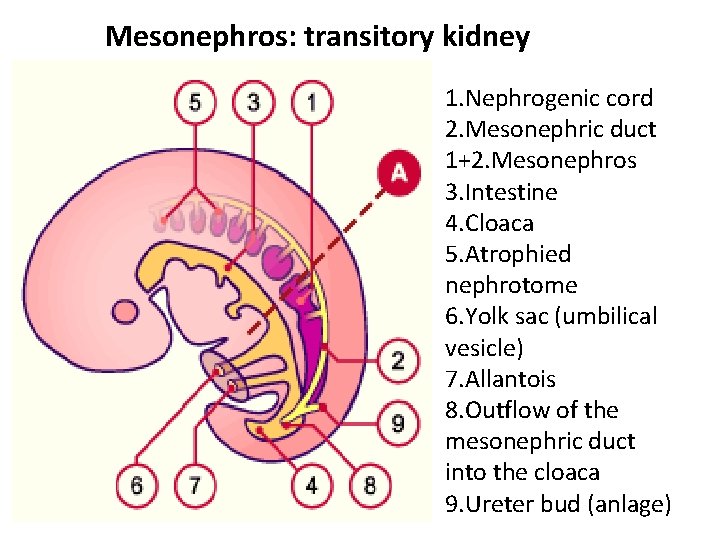
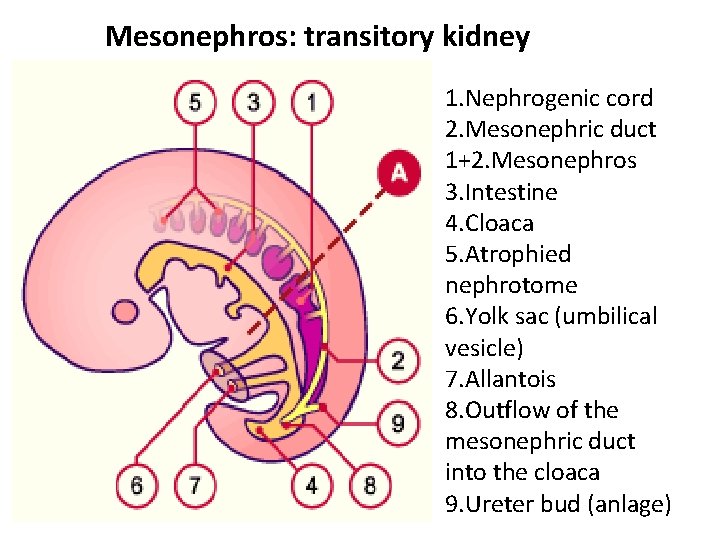
Mesonephros: transitory kidney 1. Nephrogenic cord 2. Mesonephric duct 1+2. Mesonephros 3. Intestine 4. Cloaca 5. Atrophied nephrotome 6. Yolk sac (umbilical vesicle) 7. Allantois 8. Outflow of the mesonephric duct into the cloaca 9. Ureter bud (anlage)
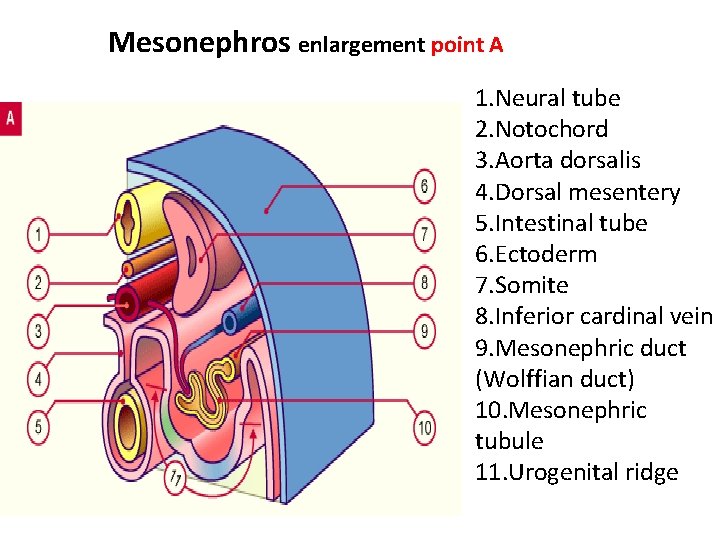
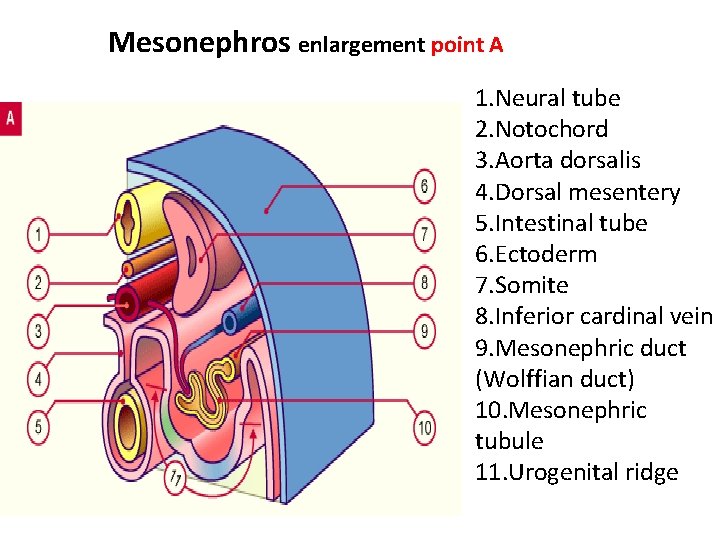
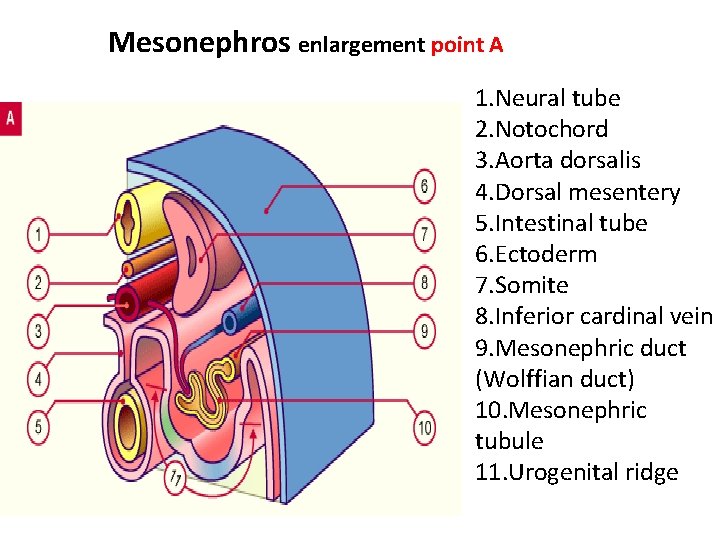
Mesonephros enlargement point A 1. Neural tube 2. Notochord 3. Aorta dorsalis 4. Dorsal mesentery 5. Intestinal tube 6. Ectoderm 7. Somite 8. Inferior cardinal vein 9. Mesonephric duct (Wolffian duct) 10. Mesonephric tubule 11. Urogenital ridge
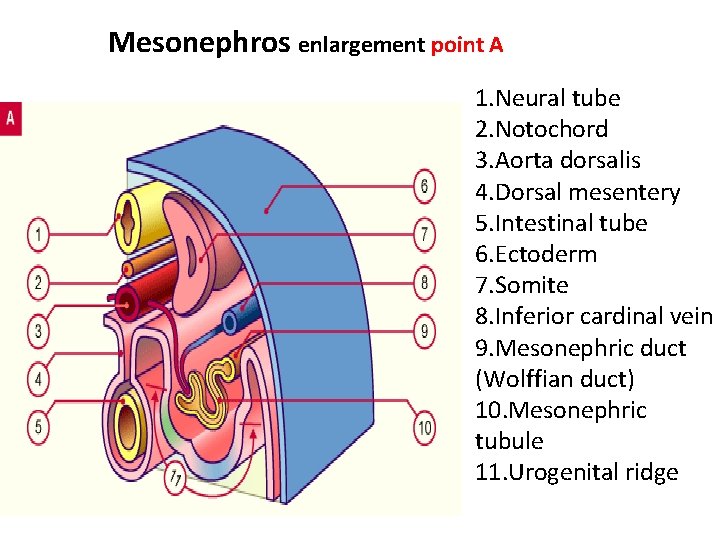
Mesonephros enlargement point A 1. Neural tube 2. Notochord 3. Aorta dorsalis 4. Dorsal mesentery 5. Intestinal tube 6. Ectoderm 7. Somite 8. Inferior cardinal vein 9. Mesonephric duct (Wolffian duct) 10. Mesonephric tubule 11. Urogenital ridge
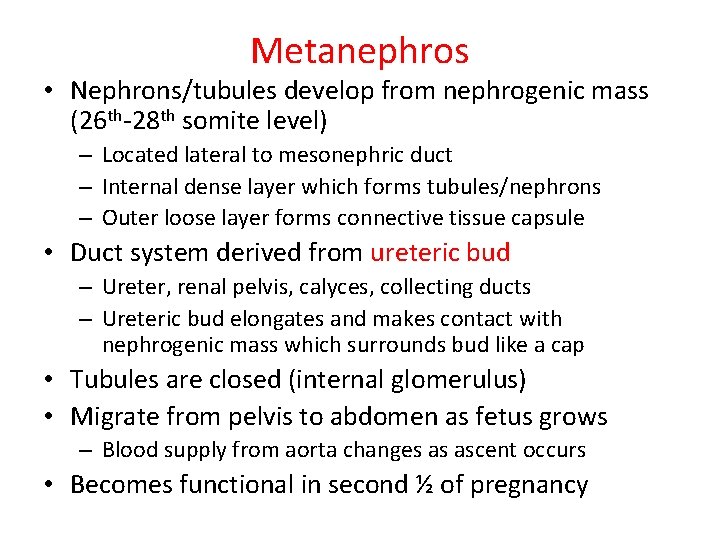
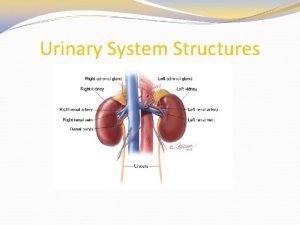
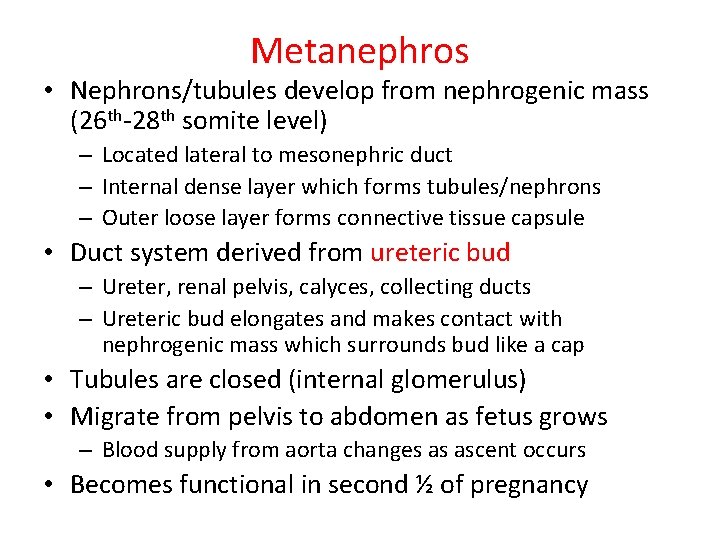
Metanephros • Nephrons/tubules develop from nephrogenic mass (26 th-28 th somite level) – Located lateral to mesonephric duct – Internal dense layer which forms tubules/nephrons – Outer loose layer forms connective tissue capsule • Duct system derived from ureteric bud – Ureter, renal pelvis, calyces, collecting ducts – Ureteric bud elongates and makes contact with nephrogenic mass which surrounds bud like a cap • Tubules are closed (internal glomerulus) • Migrate from pelvis to abdomen as fetus grows – Blood supply from aorta changes as ascent occurs • Becomes functional in second ½ of pregnancy
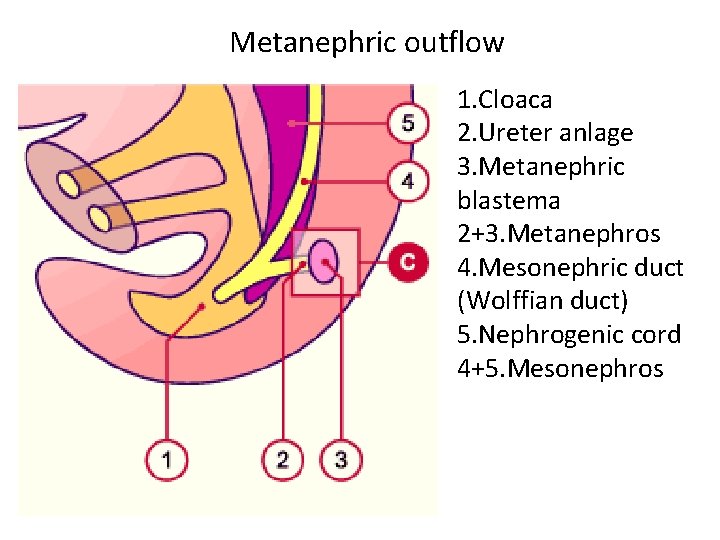
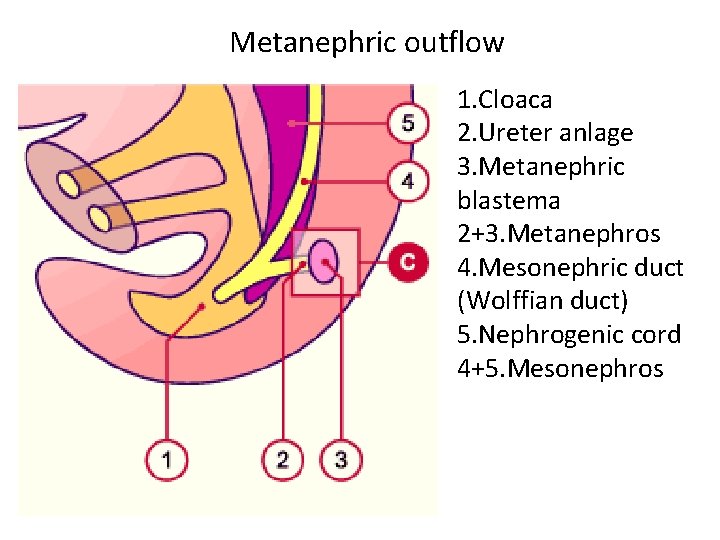
Metanephric outflow 1. Cloaca 2. Ureter anlage 3. Metanephric blastema 2+3. Metanephros 4. Mesonephric duct (Wolffian duct) 5. Nephrogenic cord 4+5. Mesonephros
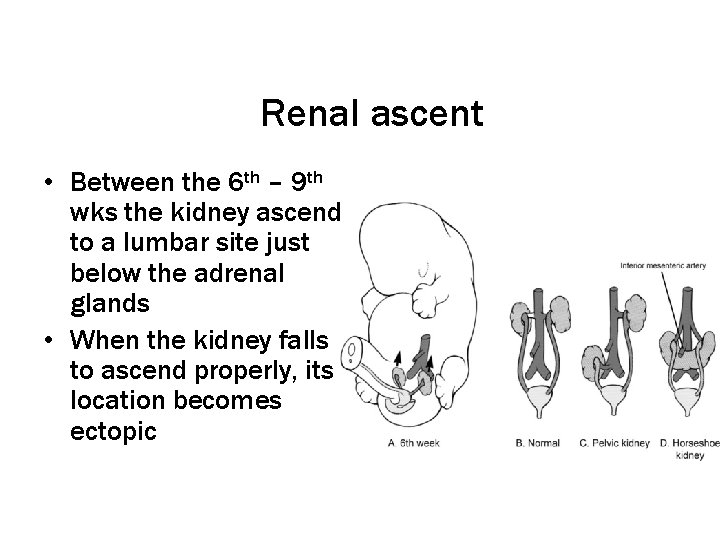
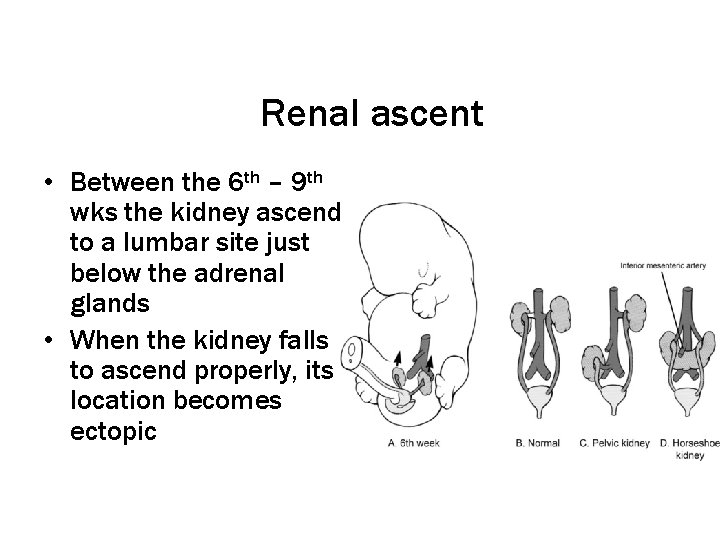
Renal ascent • Between the 6 th – 9 th wks the kidney ascend to a lumbar site just below the adrenal glands • When the kidney falls to ascend properly, its location becomes ectopic

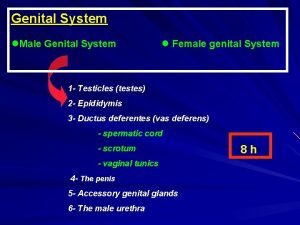
Male Genital Development • Development of gonads • Development of genital ducts • Development of external genital
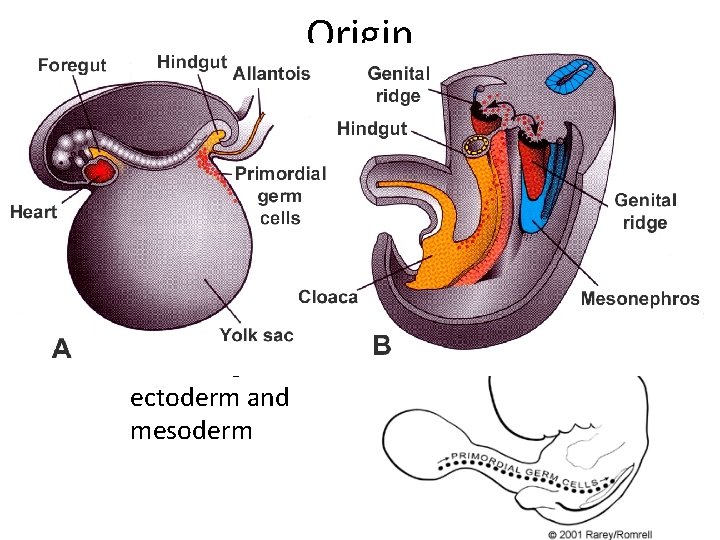
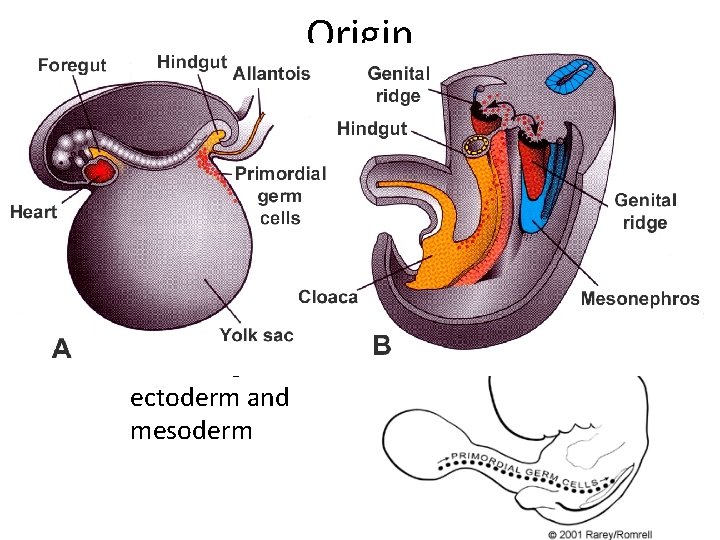
Origin • Gonads – intermedial mesoderm of mesonephros • Primordial germ cells – endoderm of yolk sac • External genitalia – ectoderm and mesoderm
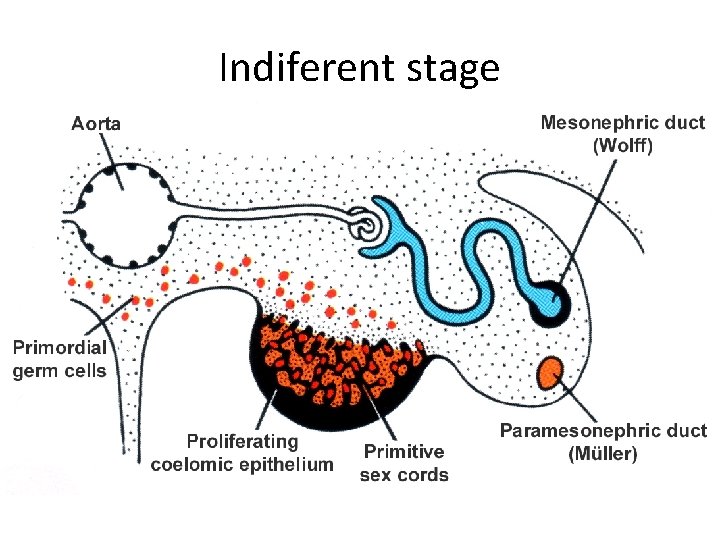
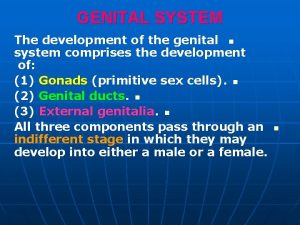
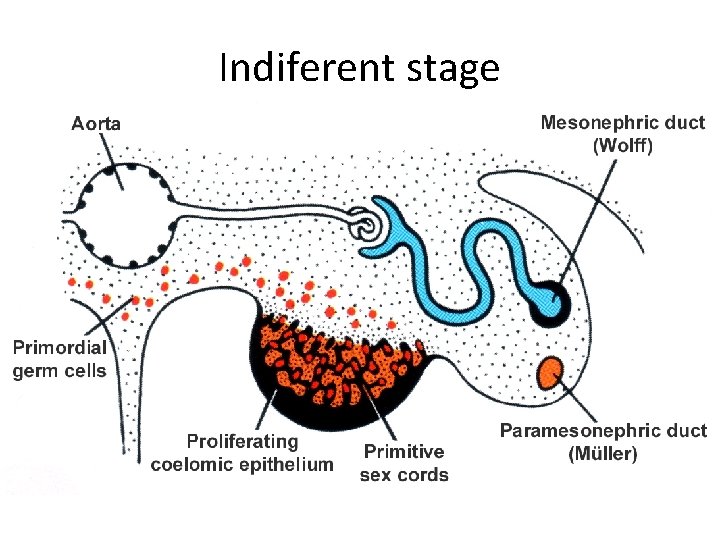
Indiferent stage • Both sexes has same first stage – coelomic epithelium • primary germ cords – primordial germ cells – mesonephric duct (Wollfian) and tubules – paramesonephric duct
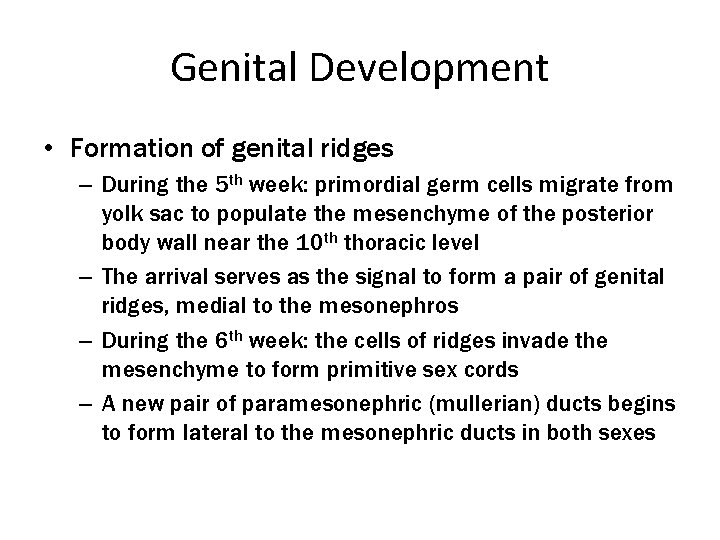
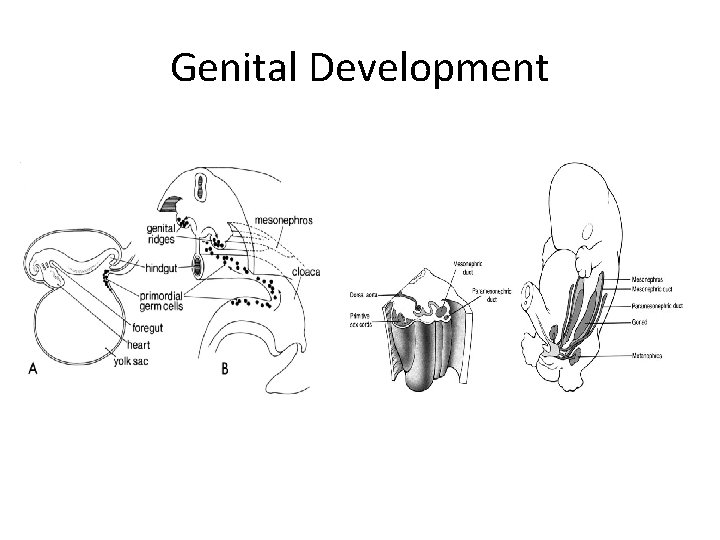
Genital Development • Formation of genital ridges – During the 5 th week: primordial germ cells migrate from yolk sac to populate the mesenchyme of the posterior body wall near the 10 th thoracic level – The arrival serves as the signal to form a pair of genital ridges, medial to the mesonephros – During the 6 th week: the cells of ridges invade the mesenchyme to form primitive sex cords – A new pair of paramesonephric (mullerian) ducts begins to form lateral to the mesonephric ducts in both sexes
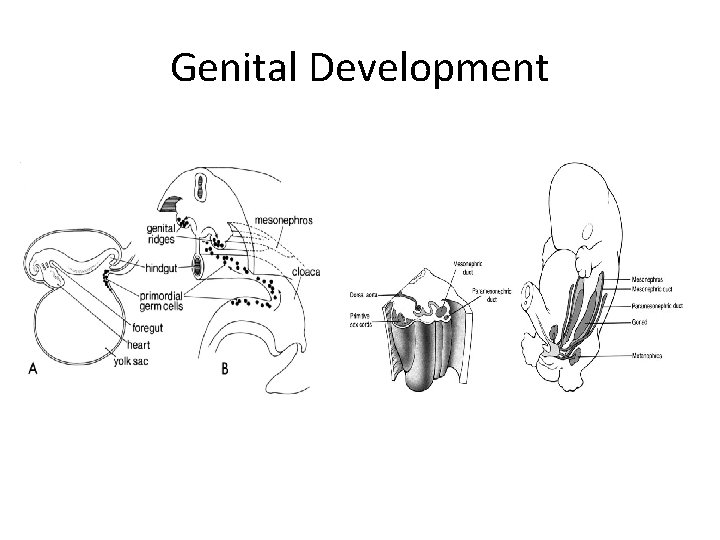
Genital Development
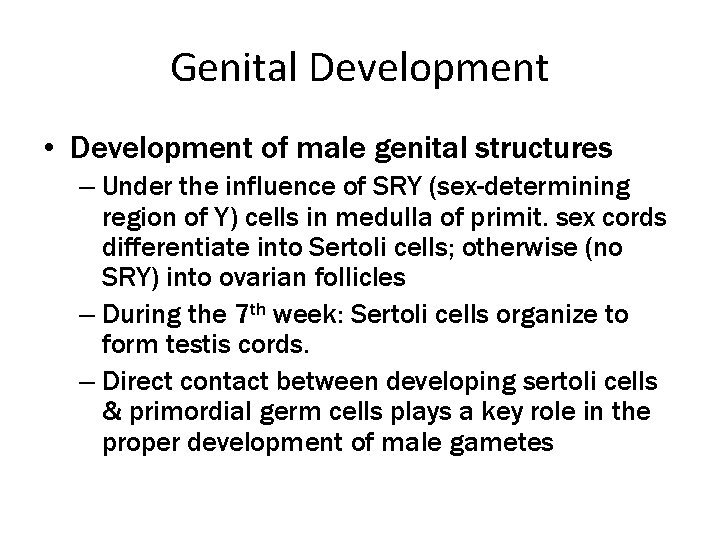
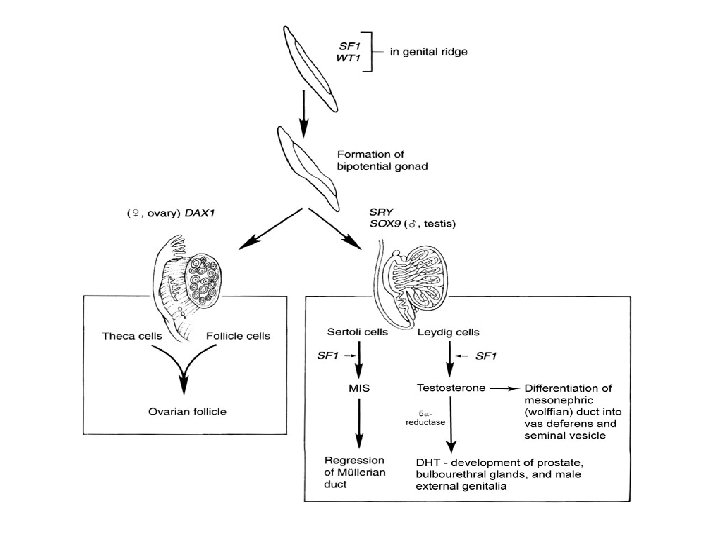
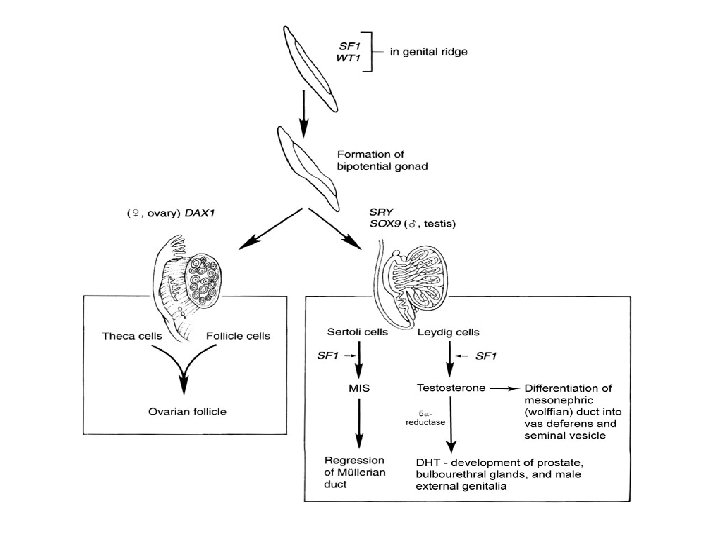
Genital Development • Development of male genital structures – Under the influence of SRY (sex-determining region of Y) cells in medulla of primit. sex cords differentiate into Sertoli cells; otherwise (no SRY) into ovarian follicles – During the 7 th week: Sertoli cells organize to form testis cords. – Direct contact between developing sertoli cells & primordial germ cells plays a key role in the proper development of male gametes
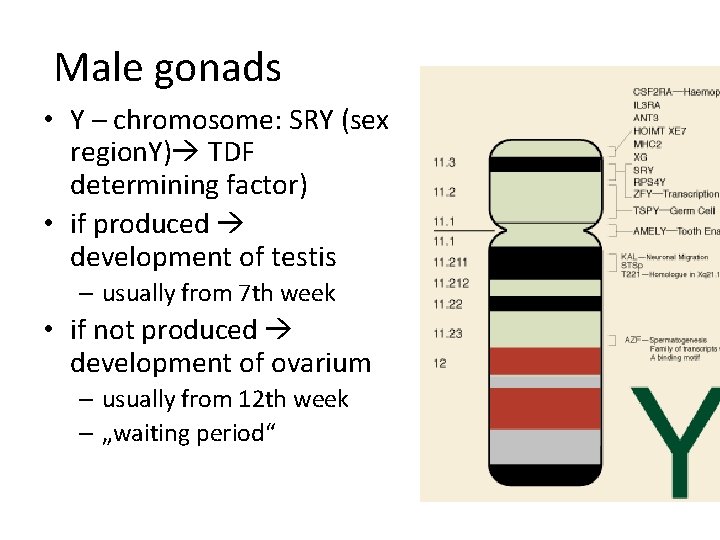
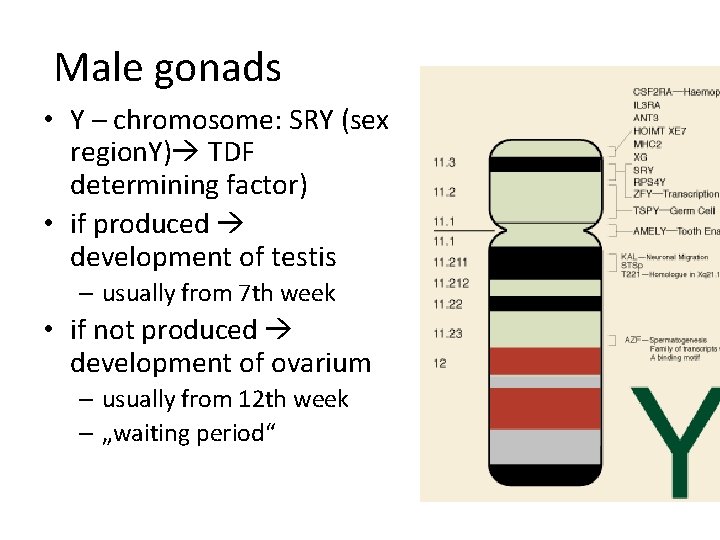
Male gonads • Y – chromosome: SRY (sex region. Y) TDF determining factor) • if produced development of testis – usually from 7 th week • if not produced development of ovarium – usually from 12 th week – „waiting period“ determining (testes
Genital Development
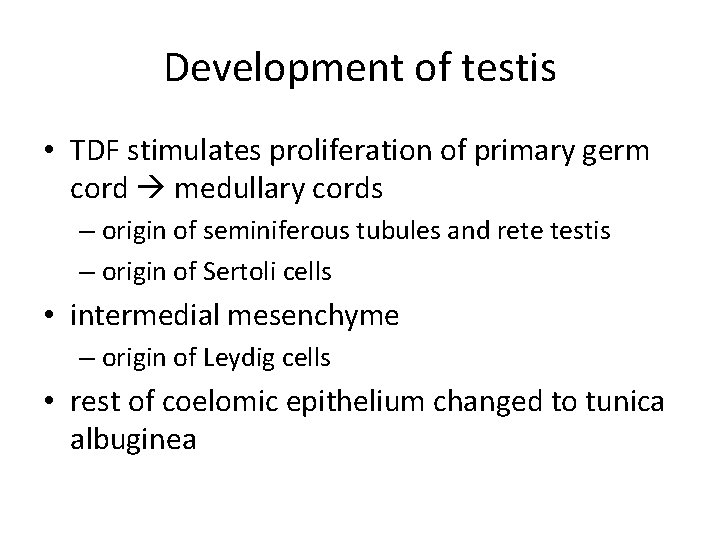
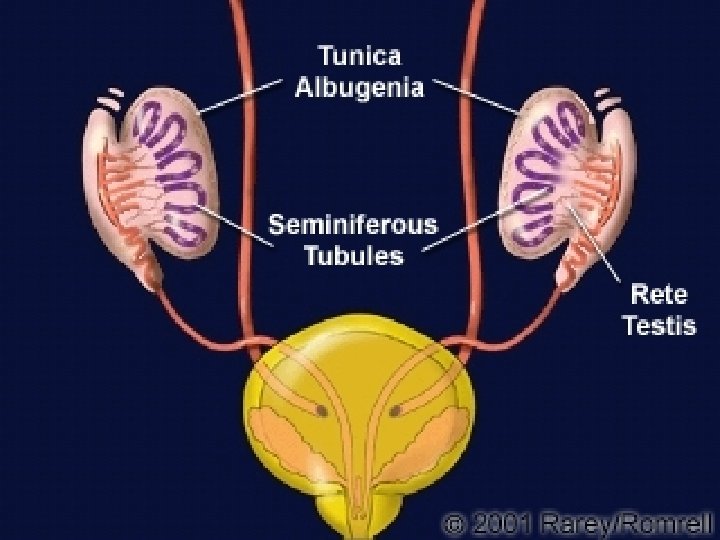
Development of testis • TDF stimulates proliferation of primary germ cord medullary cords – origin of seminiferous tubules and rete testis – origin of Sertoli cells • intermedial mesenchyme – origin of Leydig cells • rest of coelomic epithelium changed to tunica albuginea
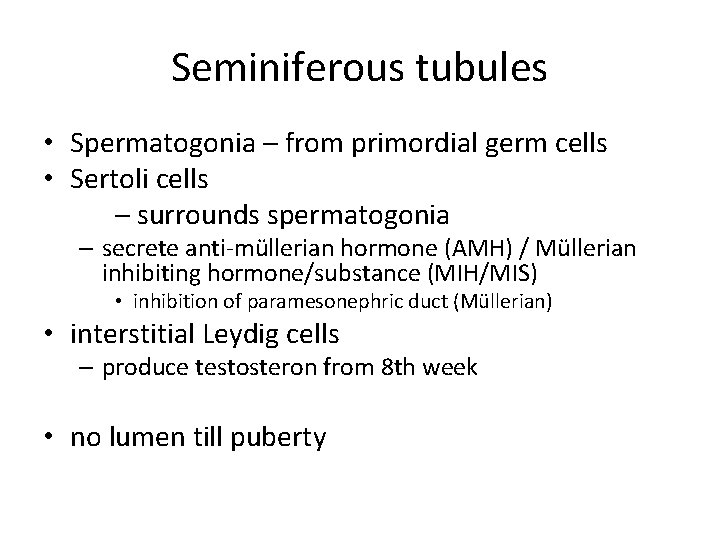
Seminiferous tubules • Spermatogonia – from primordial germ cells • Sertoli cells – surrounds spermatogonia – secrete anti-müllerian hormone (AMH) / Müllerian inhibiting hormone/substance (MIH/MIS) • inhibition of paramesonephric duct (Müllerian) • interstitial Leydig cells – produce testosteron from 8 th week • no lumen till puberty
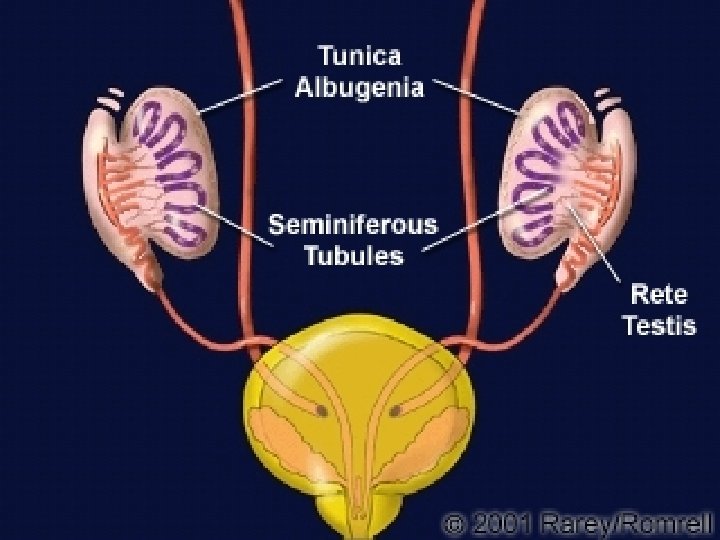
Genital ducts • Connected medullar cords – rete testis • Mesonephric tubules – Efferent ducts • Mesonephric duct (Wollfian) – Epididymal duct, ductus deferens, vesicular glands, ductus ejaculatorius – (ureter, pelvis, calices, collecting duct and tubules) • Paramesonephric duct (Müllerian) disappear
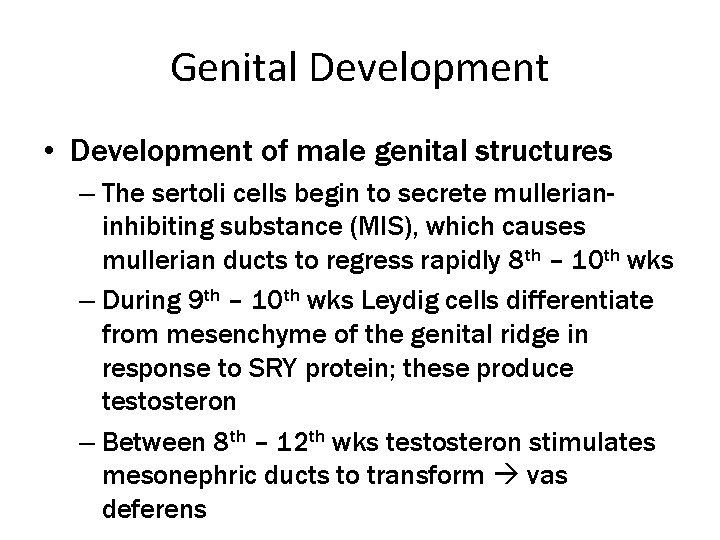
Genital Development • Development of male genital structures – The sertoli cells begin to secrete mullerianinhibiting substance (MIS), which causes mullerian ducts to regress rapidly 8 th – 10 th wks – During 9 th – 10 th wks Leydig cells differentiate from mesenchyme of the genital ridge in response to SRY protein; these produce testosteron – Between 8 th – 12 th wks testosteron stimulates mesonephric ducts to transform vas deferens

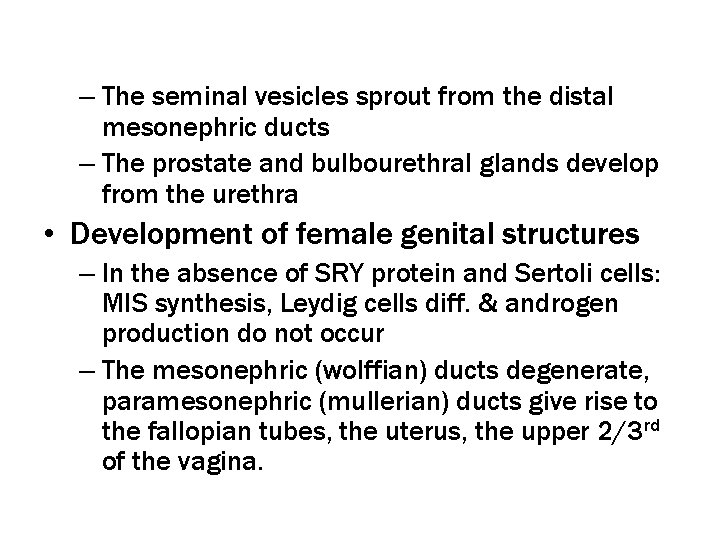
– The seminal vesicles sprout from the distal mesonephric ducts – The prostate and bulbourethral glands develop from the urethra • Development of female genital structures – In the absence of SRY protein and Sertoli cells: MIS synthesis, Leydig cells diff. & androgen production do not occur – The mesonephric (wolffian) ducts degenerate, paramesonephric (mullerian) ducts give rise to the fallopian tubes, the uterus, the upper 2/3 rd of the vagina.
Genital Development
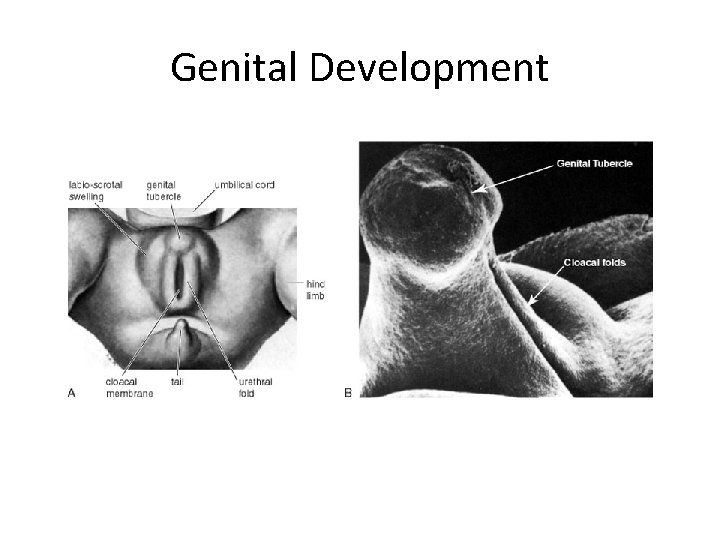
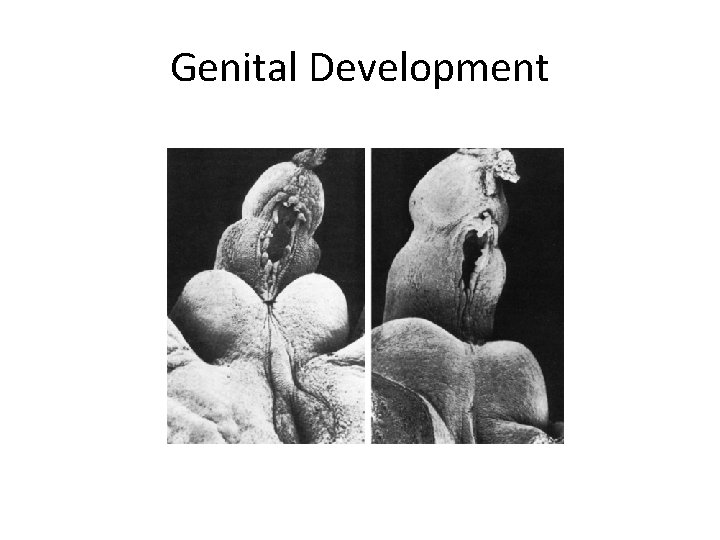
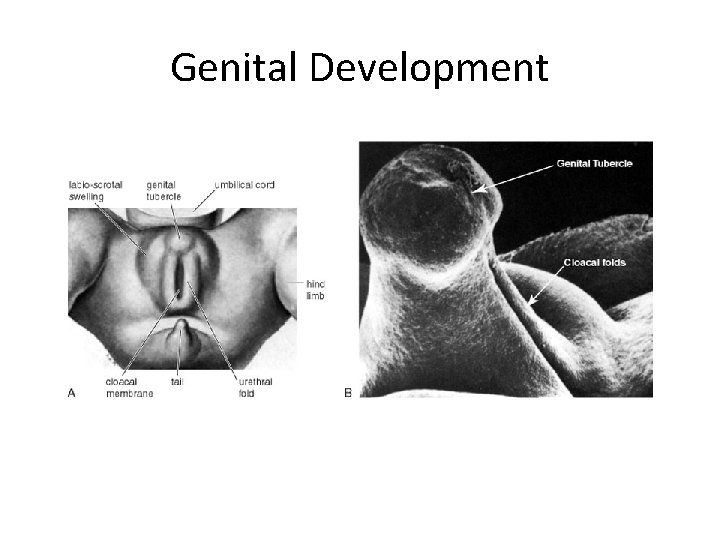
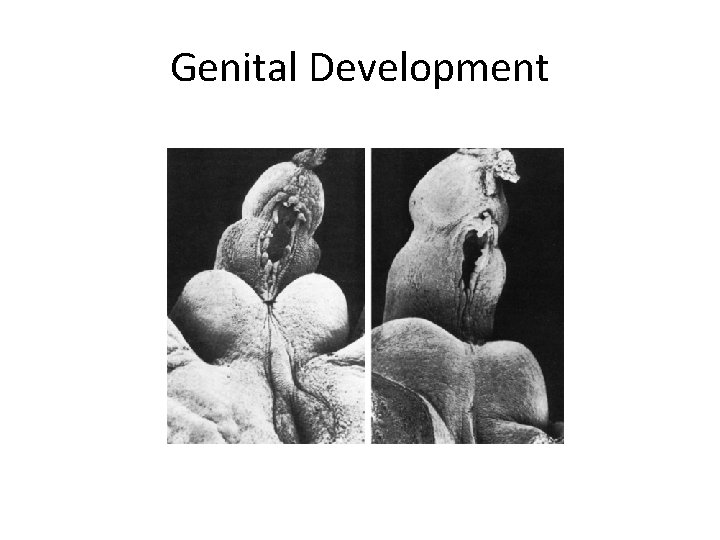
Genital Development • Development of external genitalia – The early development is similar in both sexes – In the 4 th mth, the effects of dihydrotestosteron (DHT) on the male external genital become readily apparent – In the absence of dihydrotestosteron female: the primitive perineum does not lengthen, and the labioscrotal and urethal folds do not fuse across the midline – The penile urethra is enclosed by the 14 th wk
Genital Development
External genitalia • indiferent stage • male genital • genital tubercle • urogenital folds • labioscrotal folds • penis • spongious urethra • scrotum

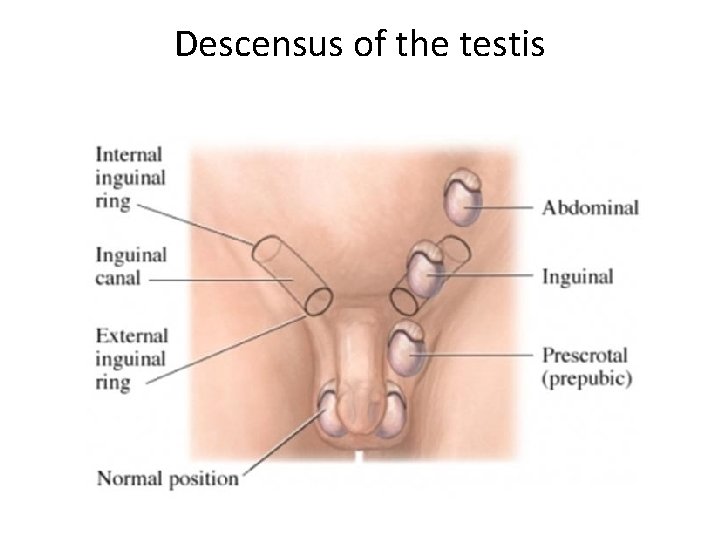
Gonadal descent – In both sexes the initial descent depends on a ligamentous cord: gubernaculum – Testes descend through inguinal canal down to the scrotum; ovaries remain within abdom. cvt – Testicles descend to internal inguinal ring by the 3 rd mth and complete their descent into the scrotum by the 7 th – 9 th mth
Descensus of the testis • from thoracolumbal area to scrotum – AMH, testicular growth, elongation of body – gubernaculum – connective cord between testis and scrotum • from 26 th week • mark of fetal maturity • cryptorchism vs. ectopic testis
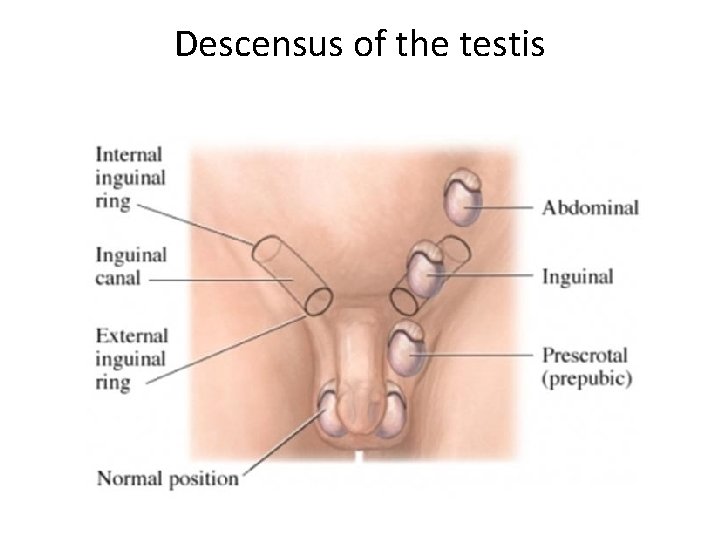
Descensus of the testis
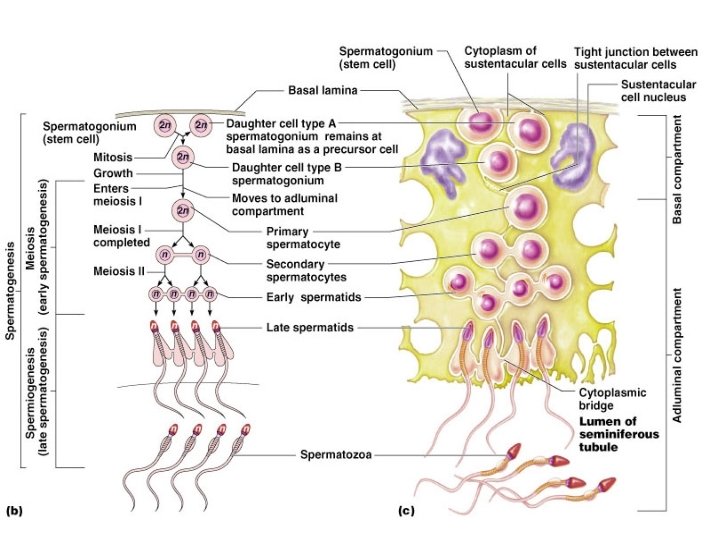
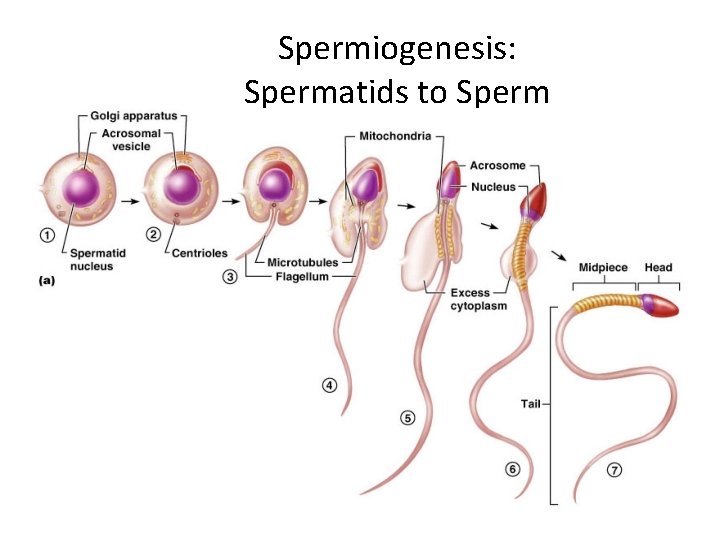
Spermatogenesis • Early in embryonic development, primordial germ cells enter the testes and differentiate into spermatogonia • Spermatogonia are diploid cells, each with 46 chromosomes (23 pairs) located around the periphery of the seminiferous tubules. • At puberty, hormones stimulate these cells to begin dividing by mitosis. Some remain at the periphery as spermatogonia. • Others become primary spermatocytes. Because they are produced by mitosis, primary spermatocytes are diploid and have 46 chromosomes.
Spermatogenesis • Each primary spermatocytes goes through the first meiotic division, meiosis I, to produce two secondary spermatocytes, each with 23 chromosomes (haploid). Just prior to this division, the genetic material is replicated. During meiosis I, one chromosome, goes to each secondary spermatocyte. • In the second meiotic division, meiosis II, each secondary spermatocyte divides to produce two spermatids. There is no replication of genetic material in this division, but a singlestranded chromatid goes to each cell. • As a result of the two meiotic divisions, each primary spermatocyte produces four spermatids, each spermatid has 23 chromosomes (haploid), one from each pair in the original primary spermatocyte.
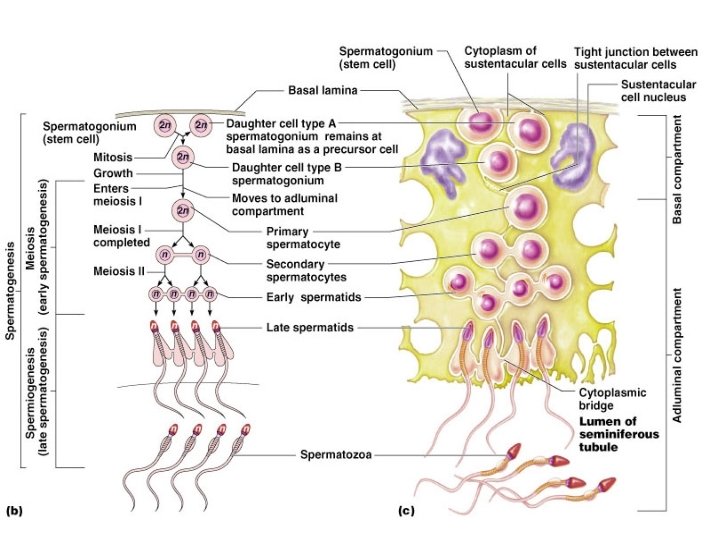
Spermatogenesis 38
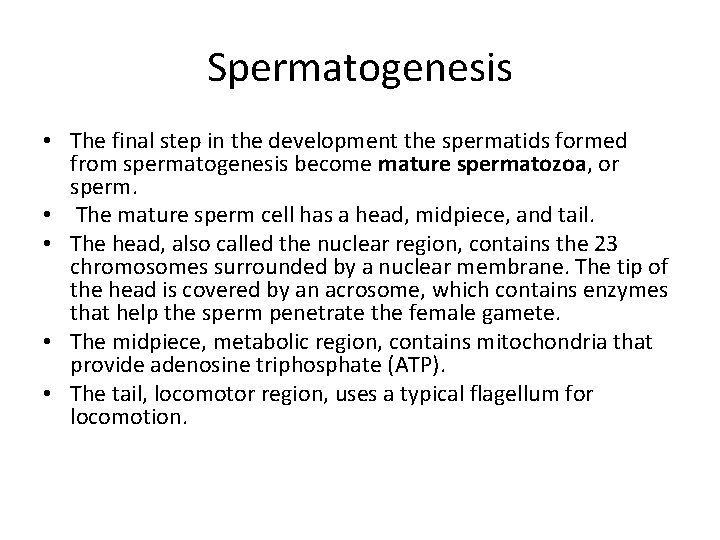
Spermatogenesis • The final step in the development the spermatids formed from spermatogenesis become mature spermatozoa, or sperm. • The mature sperm cell has a head, midpiece, and tail. • The head, also called the nuclear region, contains the 23 chromosomes surrounded by a nuclear membrane. The tip of the head is covered by an acrosome, which contains enzymes that help the sperm penetrate the female gamete. • The midpiece, metabolic region, contains mitochondria that provide adenosine triphosphate (ATP). • The tail, locomotor region, uses a typical flagellum for locomotion.


Spermatogenesis • The sperm are released into the lumen of the seminiferous tubule and leave the testes. They then enter the epididymis where they undergo their final maturation and become capable of fertilizing a female gamete. • Sperm production begins at puberty and continues throughout the life of a male. • The entire process, beginning with a primary spermatocyte, takes about 74 days. After ejaculation, the sperm can live for about 48 hours in the female reproductive tract.
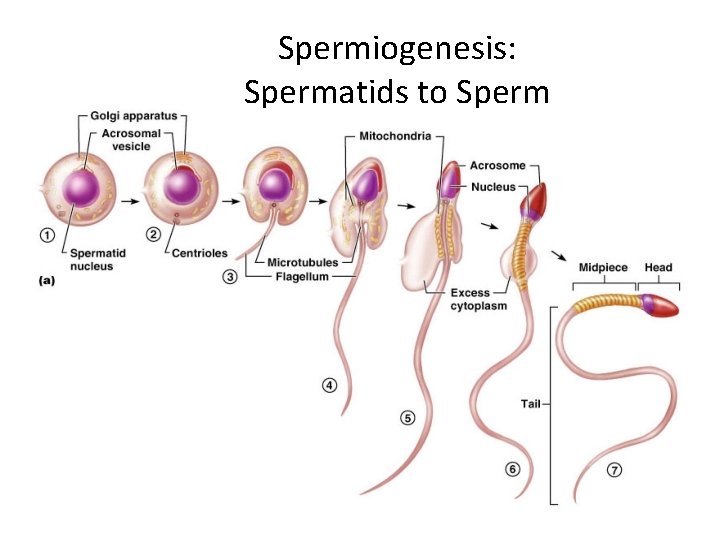
Spermiogenesis: Spermatids to Sperm 42
Pembuahan / fertilisasi / konsepsi
 Male genital variation
Male genital variation Reproductive system function
Reproductive system function Semen
Semen Prostate function
Prostate function Male genital tract
Male genital tract Lesson 14.2 male and female urinary structures
Lesson 14.2 male and female urinary structures Lymphatic system
Lymphatic system Male reproductive organs
Male reproductive organs Cloacal membrane
Cloacal membrane Urogenital sinus
Urogenital sinus Female reproductive system pictures real
Female reproductive system pictures real Urinary system introduction
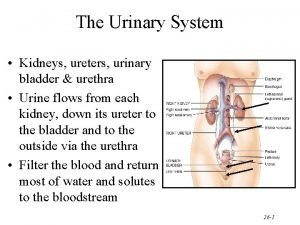
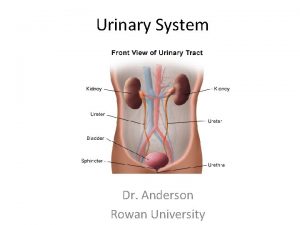
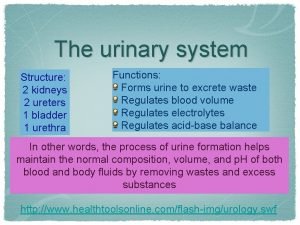
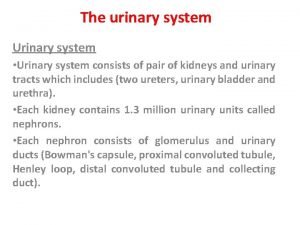
Urinary system introduction Kidneys location and structure figure 15-1
Kidneys location and structure figure 15-1 Pyelo medical terminology
Pyelo medical terminology Whats gametes
Whats gametes Male fetal pig reproductive system labeled
Male fetal pig reproductive system labeled Chapter 30 the urinary system workbook answers
Chapter 30 the urinary system workbook answers Chapter 15 the urinary system figure 15-3
Chapter 15 the urinary system figure 15-3 Chapter 20 urinary/excretory system
Chapter 20 urinary/excretory system Urinary system model
Urinary system model Urinary system model
Urinary system model Alimentary canal
Alimentary canal Urinary system powerpoint
Urinary system powerpoint Parietal layer of bowman's capsule
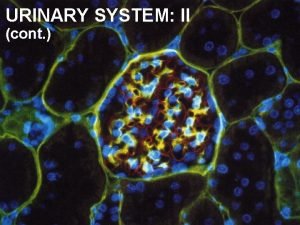
Parietal layer of bowman's capsule Antidiuretic hormone function
Antidiuretic hormone function Nephron urinary system
Nephron urinary system Figure 15-4 is a diagram of a nephron
Figure 15-4 is a diagram of a nephron Urinary system x ray labeled
Urinary system x ray labeled Defination of urinary system
Defination of urinary system Urinary system label
Urinary system label External anatomy of rat
External anatomy of rat Rat urinary system
Rat urinary system Vena cava function in excretory system
Vena cava function in excretory system Figure 15-3 the urinary system
Figure 15-3 the urinary system Macula densa
Macula densa Bowmans capsule
Bowmans capsule Urinary system
Urinary system Normal constituents of urine
Normal constituents of urine What is the name
What is the name Normal constituents of urine
Normal constituents of urine Urinary system
Urinary system Urinary system
Urinary system Cystolith medical term
Cystolith medical term Urine infection symptoms
Urine infection symptoms