CT Evaluation of Acute Enteritis and Colitis Is
- Slides: 40
CT Evaluation of Acute Enteritis and Colitis: Is It Infectious, Inflammatory, or Ischemic? Brandon C. Childers, MD 1 Sarah Wallace Cater, MD 1 Karen M. Horton, MD 1 Elliot K. Fishman, MD 1 Pamela T. Johnson, MD 1* 1 The Russell H. Morgan Department of Radiology and Radiological Science The Johns Hopkins Hospital, Baltimore, Maryland *Corresponding author: Pamela T. Johnson, MD 601 North Caroline Street, Room 4223 Baltimore, MD 21287 Email: pjohnso 5@jhmi. edu Office: (410) 955 -6785 Fax: (410) 955 -6786 RSNA 2014, Educational Exhibit ERE 121 14001401
Financial Disclosures The authors of this electronic publication have nothing to disclose.
Overview Enteritis and colitis are among the more common causes of abdominal pain. The causes are variable, as are the appropriate clinical management strategies. Although computed tomography (CT) is generally not indicated for first-line diagnosis of infectious or even inflammatory enterocolitis, many of these patients undergo CT evaluation during an acute abdomen workup. This exhibit reviews the CT findings of enteritis and colitis on the basis of cause. Infection—bacterial, viral, fungal, parasitic Inflammation—Crohn disease, ulcerative colitis Ischemia—arterial occlusion, venous occlusion, decreased flow Although there are many overlapping features of enterocolitis at CT, specific findings and patterns can offer important diagnostic clues to facilitate distinction. Although definitive diagnosis often relies on endoscopic biopsy result, stool culture result, or other clinical features, the radiologist can help guide the diagnosis. Emphasis is placed on geographic distribution, morphology of the wall and extraintestinal findings—often the key for distinguishing causes.
Key Concepts 1. Characteristic intestinal and extraintestinal CT findings are associated with each cause. 2. An optimized CT protocol is key to identify these features. 3. Infectious enterocolitis typically follows a geographic distribution depending on the organism responsible. 4. Ulcerative colitis and Crohn disease differ in distribution and in radiographic manifestations. 5. Ischemic enteritis and colitis have a highly variable appearance depending on the cause and chronicity of the bowel ischemia.
Learning Objectives 1. Be able to distinguish the various causes of enterocolitis by using key CT features. 2. Explain the importance of the general anatomic distribution of infectious enterocolitis. 3. Identify the key imaging features to differentiate ulcerative colitis from Crohn disease. 4. Recognize the range of appearances for ischemic enterocolitis and critical ancillary findings.
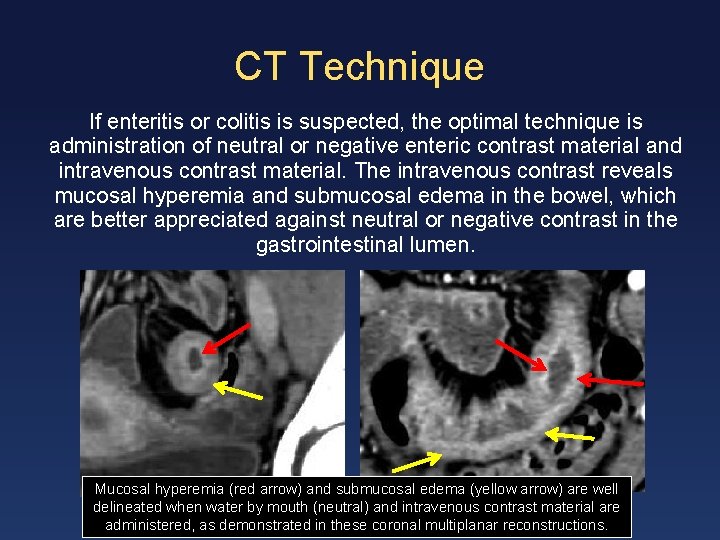
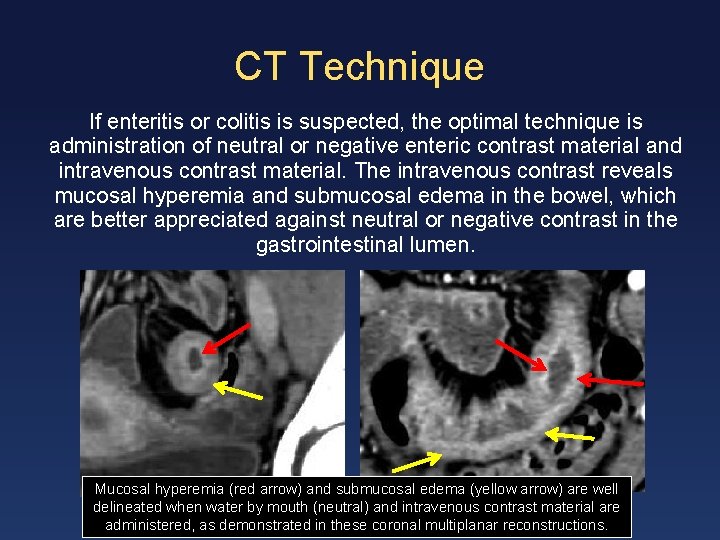
CT Technique If enteritis or colitis is suspected, the optimal technique is administration of neutral or negative enteric contrast material and intravenous contrast material. The intravenous contrast reveals mucosal hyperemia and submucosal edema in the bowel, which are better appreciated against neutral or negative contrast in the gastrointestinal lumen. Mucosal hyperemia (red arrow) and submucosal edema (yellow arrow) are well delineated when water by mouth (neutral) and intravenous contrast material are administered, as demonstrated in these coronal multiplanar reconstructions.
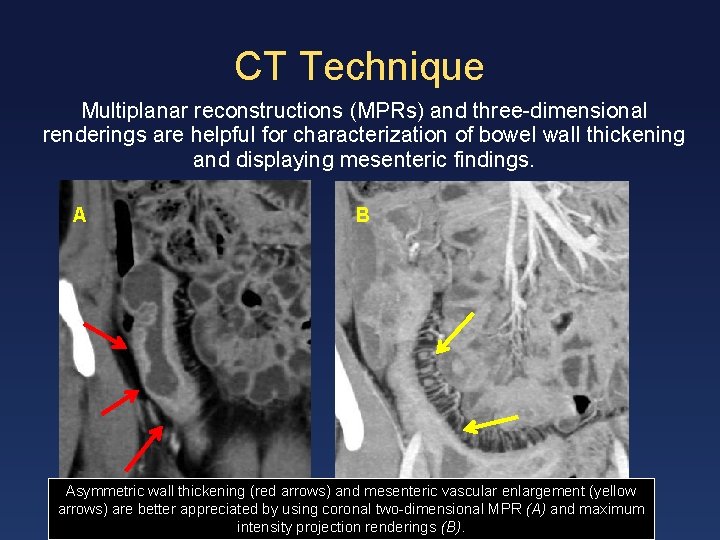
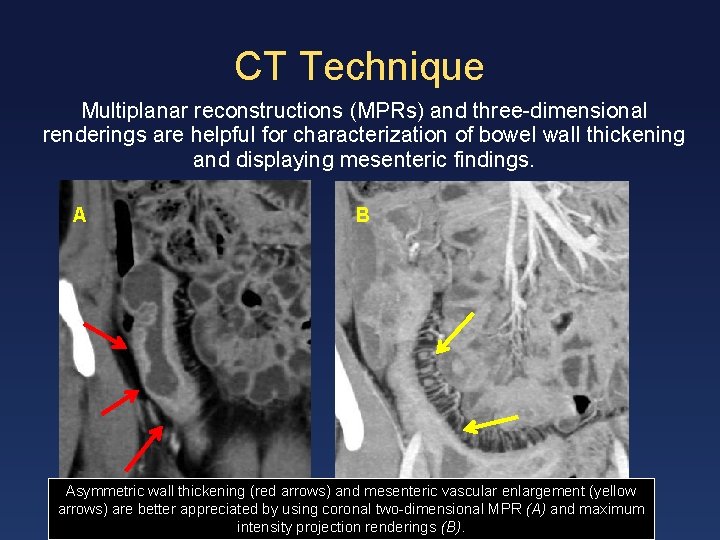
CT Technique Multiplanar reconstructions (MPRs) and three-dimensional renderings are helpful for characterization of bowel wall thickening and displaying mesenteric findings. A B Asymmetric wall thickening (red arrows) and mesenteric vascular enlargement (yellow arrows) are better appreciated by using coronal two-dimensional MPR (A) and maximum intensity projection renderings (B).
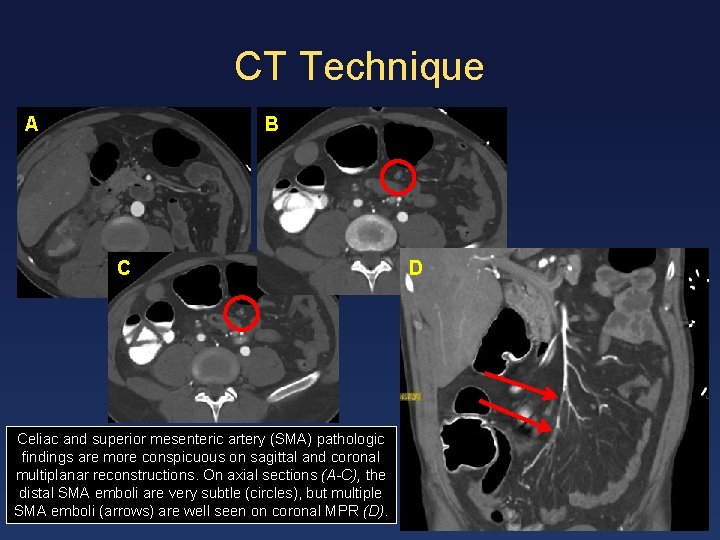
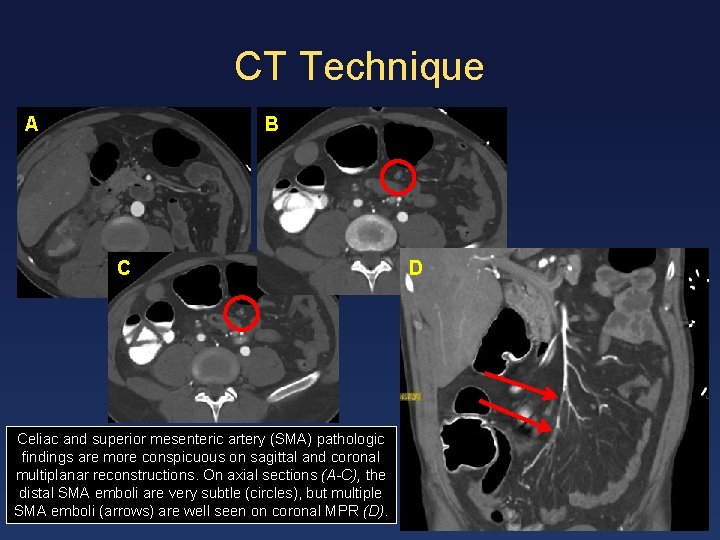
CT Technique A B C Celiac and superior mesenteric artery (SMA) pathologic findings are more conspicuous on sagittal and coronal multiplanar reconstructions. On axial sections (A-C), the distal SMA emboli are very subtle (circles), but multiple SMA emboli (arrows) are well seen on coronal MPR (D). D
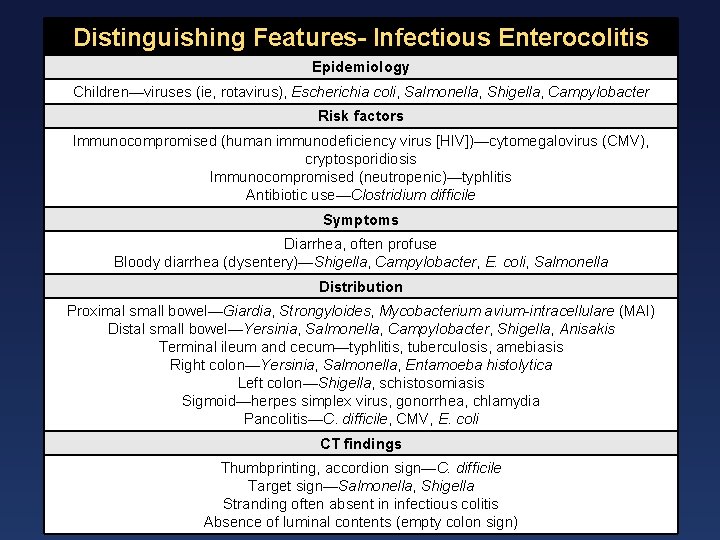
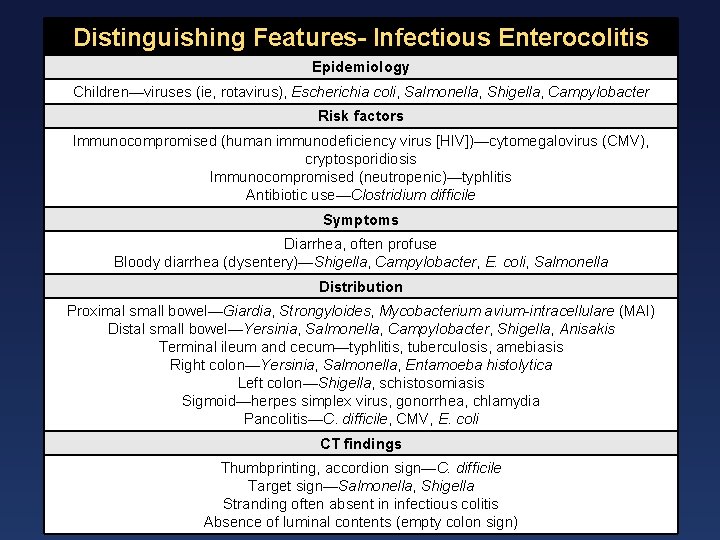
Distinguishing Features- Infectious Enterocolitis Epidemiology Children—viruses (ie, rotavirus), Escherichia coli, Salmonella, Shigella, Campylobacter Risk factors Immunocompromised (human immunodeficiency virus [HIV])—cytomegalovirus (CMV), cryptosporidiosis Immunocompromised (neutropenic)—typhlitis Antibiotic use—Clostridium difficile Symptoms Diarrhea, often profuse Bloody diarrhea (dysentery)—Shigella, Campylobacter, E. coli, Salmonella Distribution Proximal small bowel—Giardia, Strongyloides, Mycobacterium avium-intracellulare (MAI) Distal small bowel—Yersinia, Salmonella, Campylobacter, Shigella, Anisakis Terminal ileum and cecum—typhlitis, tuberculosis, amebiasis Right colon—Yersinia, Salmonella, Entamoeba histolytica Left colon—Shigella, schistosomiasis Sigmoid—herpes simplex virus, gonorrhea, chlamydia Pancolitis—C. difficile, CMV, E. coli CT findings Thumbprinting, accordion sign—C. difficile Target sign—Salmonella, Shigella Stranding often absent in infectious colitis Absence of luminal contents (empty colon sign)
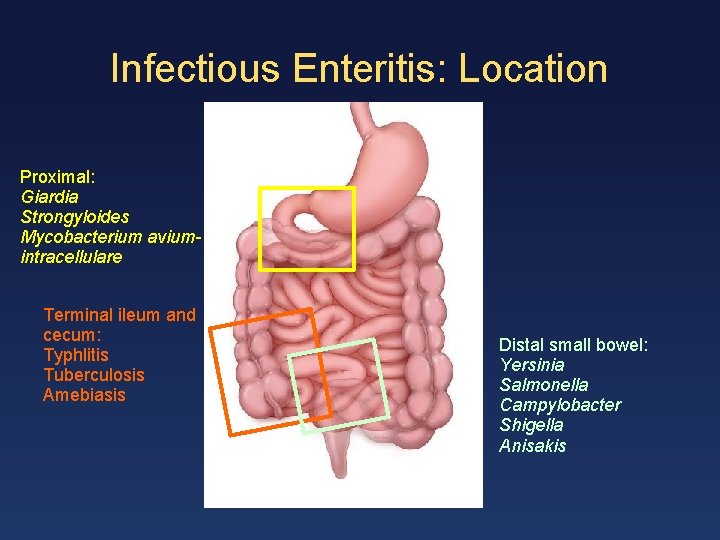
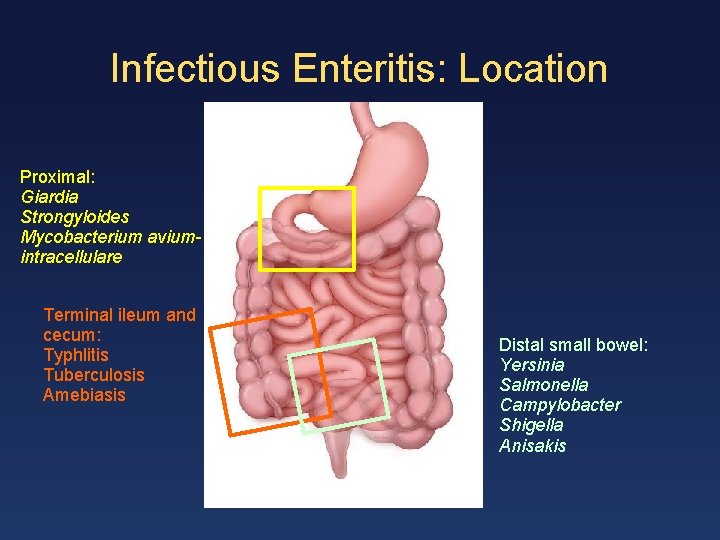
Infectious Enteritis: Location Proximal: Giardia Strongyloides Mycobacterium aviumintracellulare Terminal ileum and cecum: Typhlitis Tuberculosis Amebiasis Distal small bowel: Yersinia Salmonella Campylobacter Shigella Anisakis
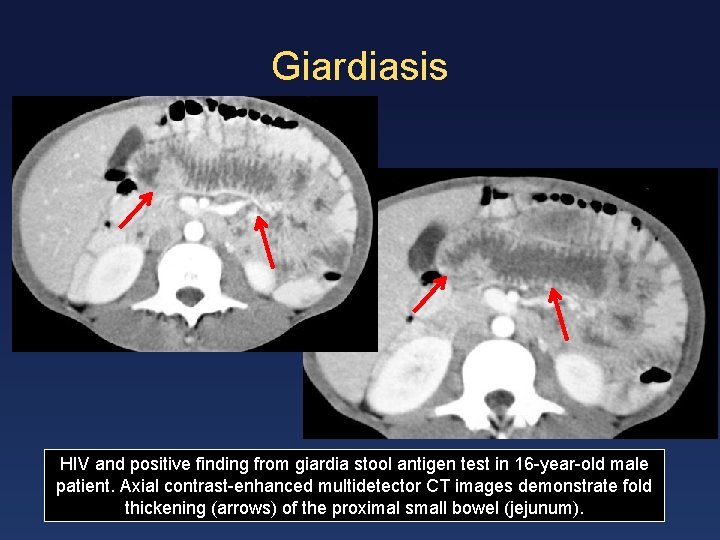
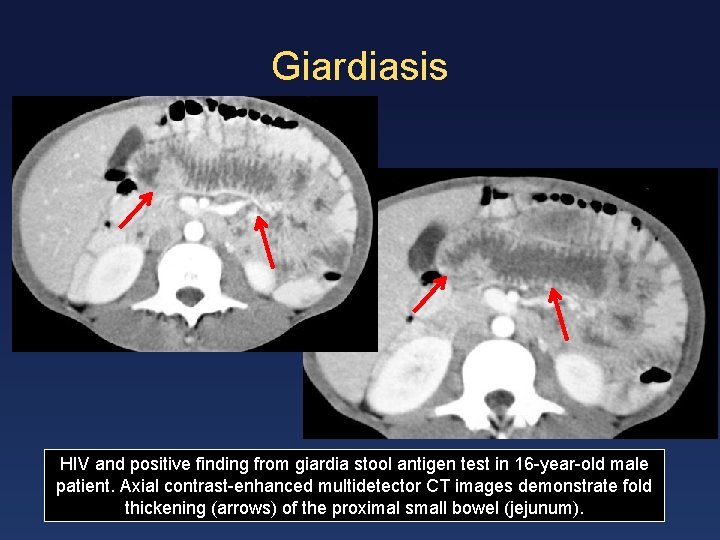
Giardiasis HIV and positive finding from giardia stool antigen test in 16 -year-old male patient. Axial contrast-enhanced multidetector CT images demonstrate fold thickening (arrows) of the proximal small bowel (jejunum).
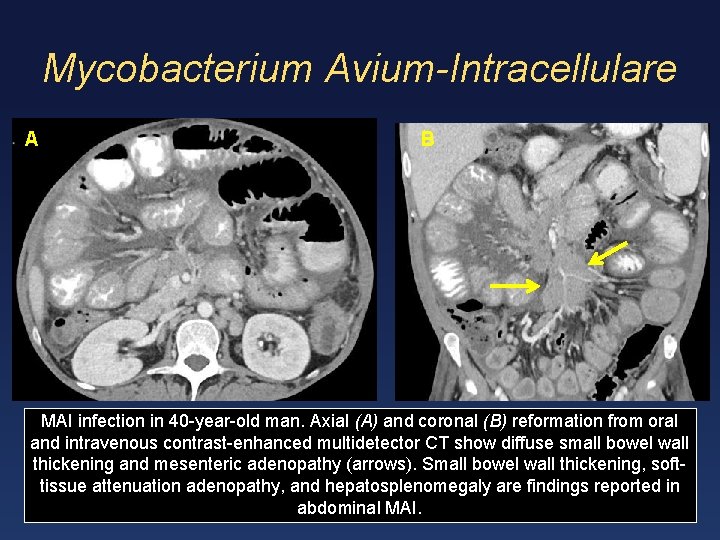
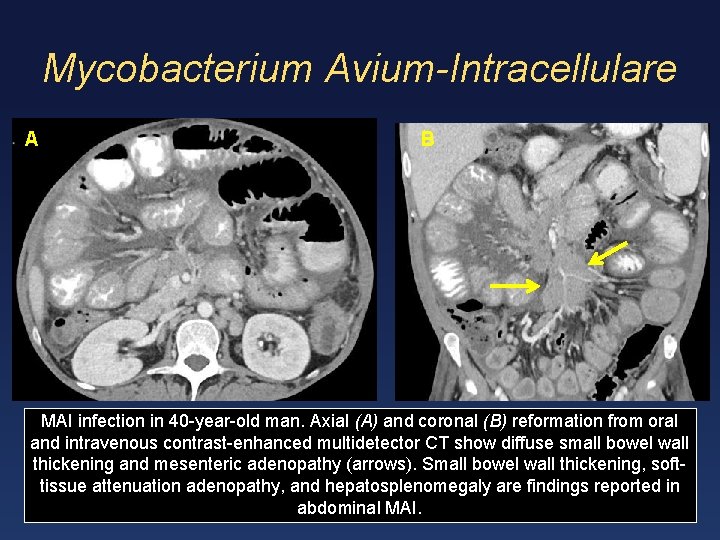
Mycobacterium Avium-Intracellulare A B MAI infection in 40 -year-old man. Axial (A) and coronal (B) reformation from oral and intravenous contrast-enhanced multidetector CT show diffuse small bowel wall thickening and mesenteric adenopathy (arrows). Small bowel wall thickening, softtissue attenuation adenopathy, and hepatosplenomegaly are findings reported in abdominal MAI.
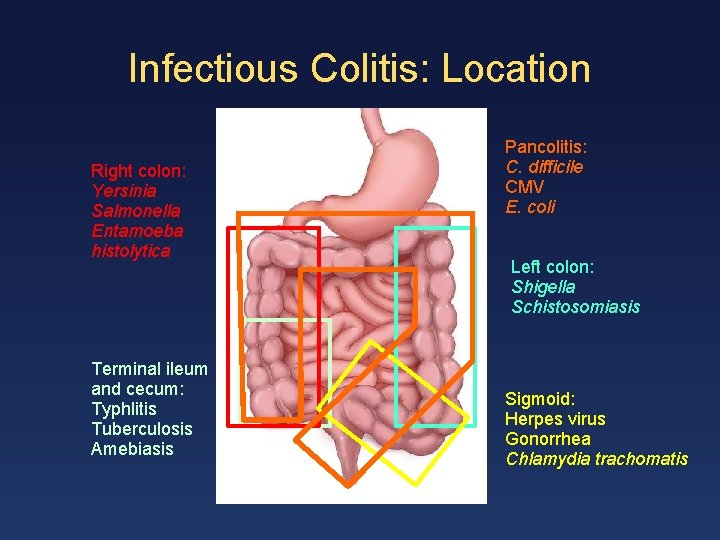
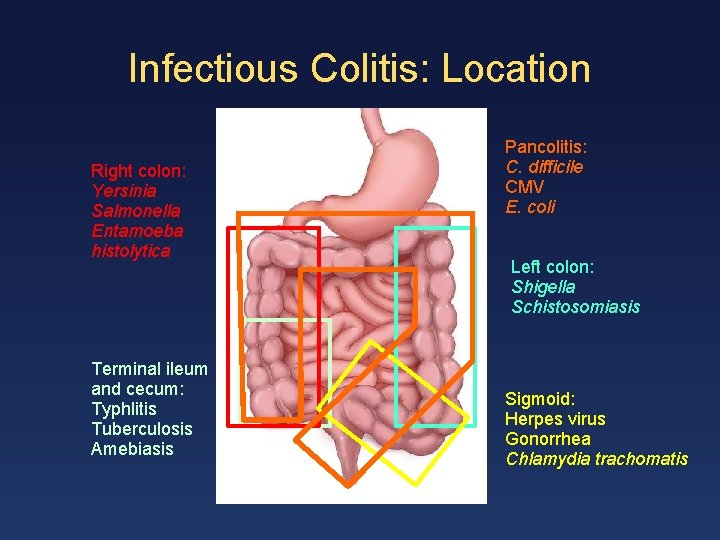
Infectious Colitis: Location Right colon: Yersinia Salmonella Entamoeba histolytica Terminal ileum and cecum: Typhlitis Tuberculosis Amebiasis Pancolitis: C. difficile CMV E. coli Left colon: Shigella Schistosomiasis Sigmoid: Herpes virus Gonorrhea Chlamydia trachomatis
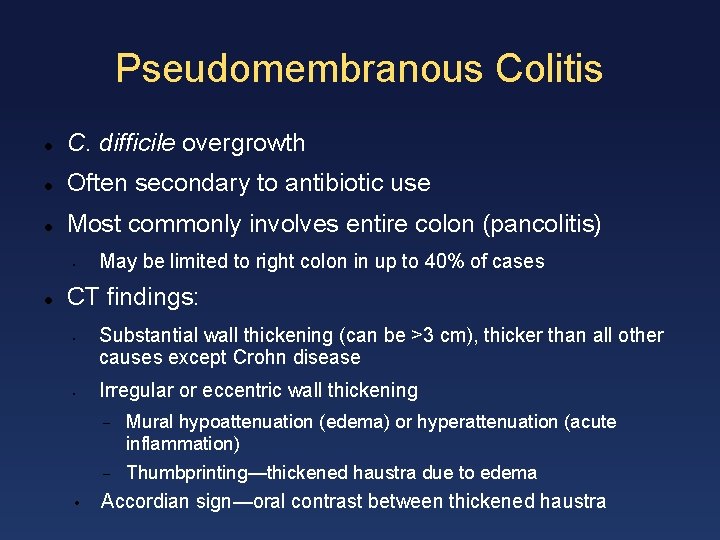
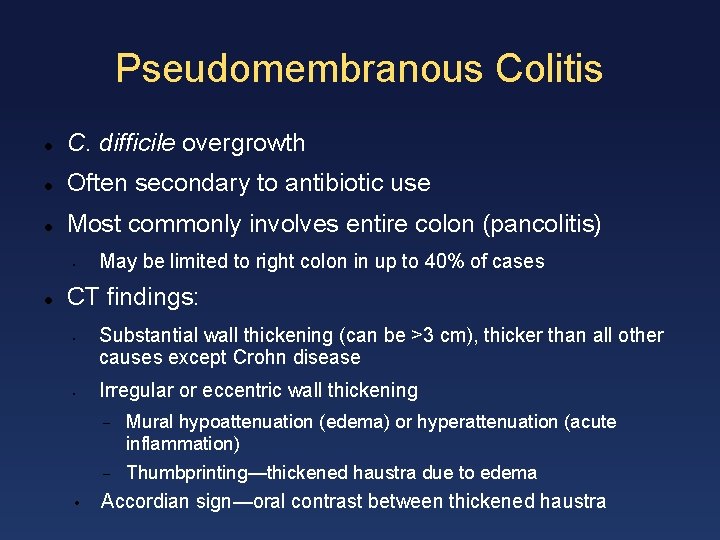
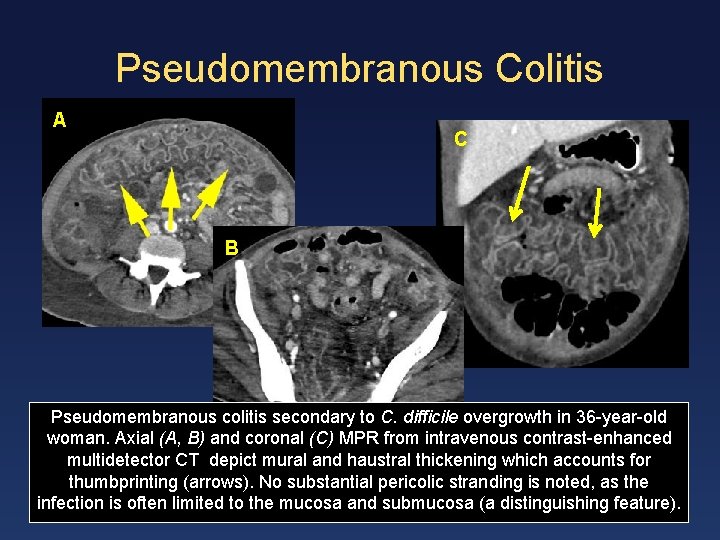
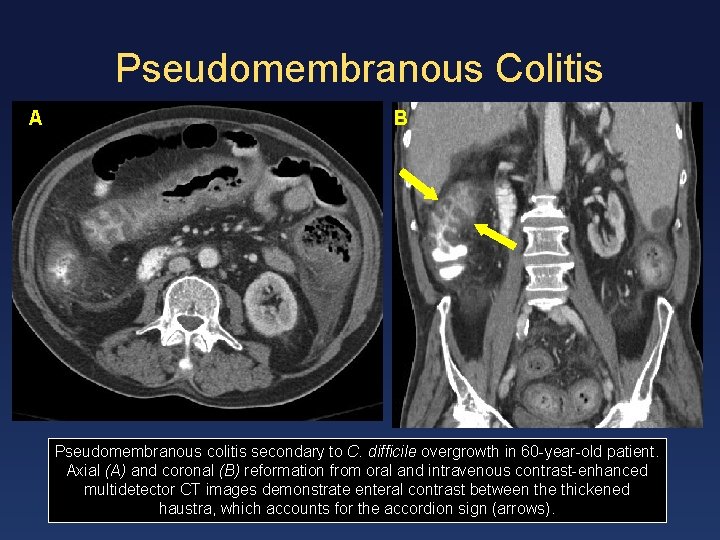
Pseudomembranous Colitis C. difficile overgrowth Often secondary to antibiotic use Most commonly involves entire colon (pancolitis) • May be limited to right colon in up to 40% of cases CT findings: • • • Substantial wall thickening (can be >3 cm), thicker than all other causes except Crohn disease Irregular or eccentric wall thickening Mural hypoattenuation (edema) or hyperattenuation (acute inflammation) Thumbprinting—thickened haustra due to edema Accordian sign—oral contrast between thickened haustra
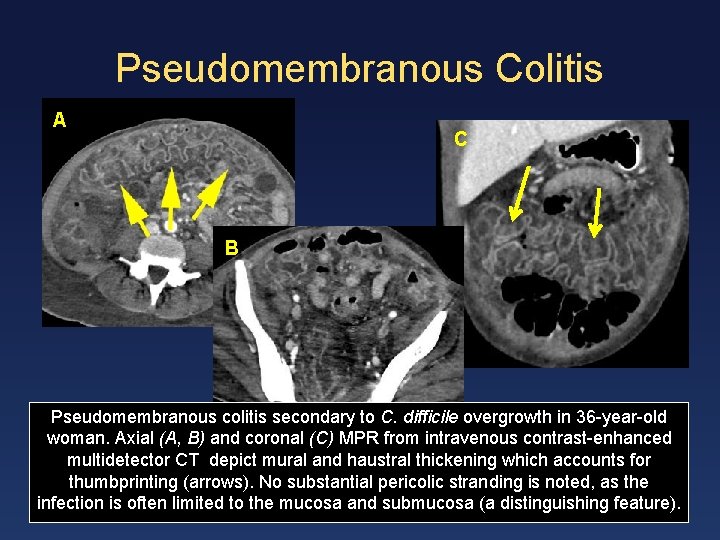
Pseudomembranous Colitis A C B Pseudomembranous colitis secondary to C. difficile overgrowth in 36 -year-old woman. Axial (A, B) and coronal (C) MPR from intravenous contrast-enhanced multidetector CT depict mural and haustral thickening which accounts for thumbprinting (arrows). No substantial pericolic stranding is noted, as the infection is often limited to the mucosa and submucosa (a distinguishing feature).
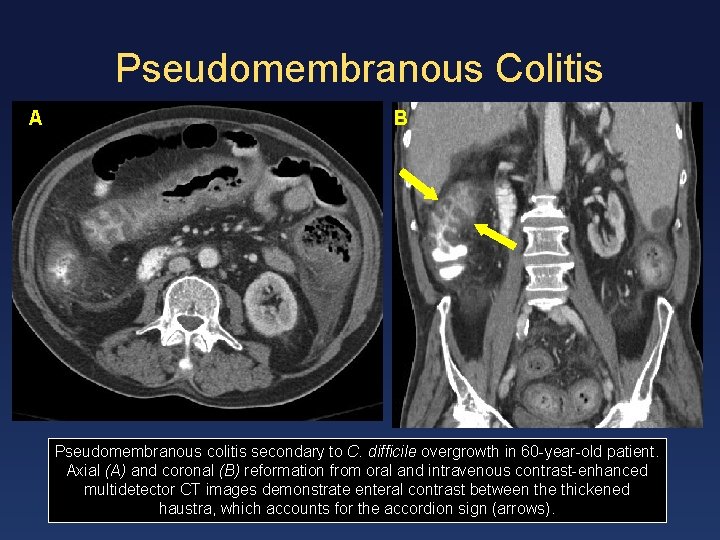
Pseudomembranous Colitis A B Pseudomembranous colitis secondary to C. difficile overgrowth in 60 -year-old patient. Axial (A) and coronal (B) reformation from oral and intravenous contrast-enhanced multidetector CT images demonstrate enteral contrast between the thickened haustra, which accounts for the accordion sign (arrows).
Typhlitis • Inflammation of predominantly the cecum and often terminal ileum in immunocompromised patients (most commonly neutropenia) • Often with associated infection—typically gram-positive gut flora (including C. difficile) • Medical emergency, with mortality rate as high as 50%, owing to high rates of necrosis, rupture, and peritonitis
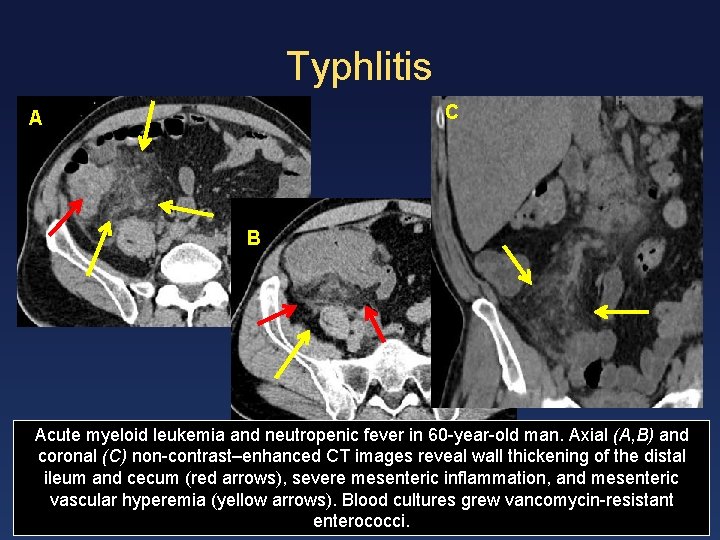
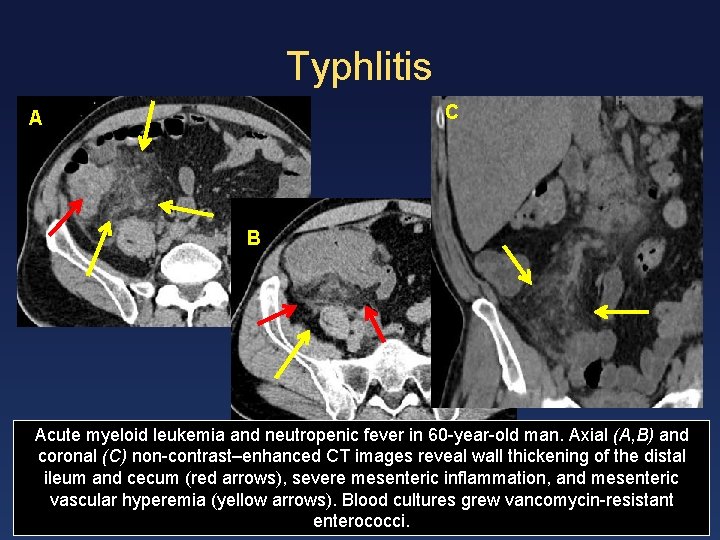
Typhlitis C A B Acute myeloid leukemia and neutropenic fever in 60 -year-old man. Axial (A, B) and coronal (C) non-contrast–enhanced CT images reveal wall thickening of the distal ileum and cecum (red arrows), severe mesenteric inflammation, and mesenteric vascular hyperemia (yellow arrows). Blood cultures grew vancomycin-resistant enterococci.
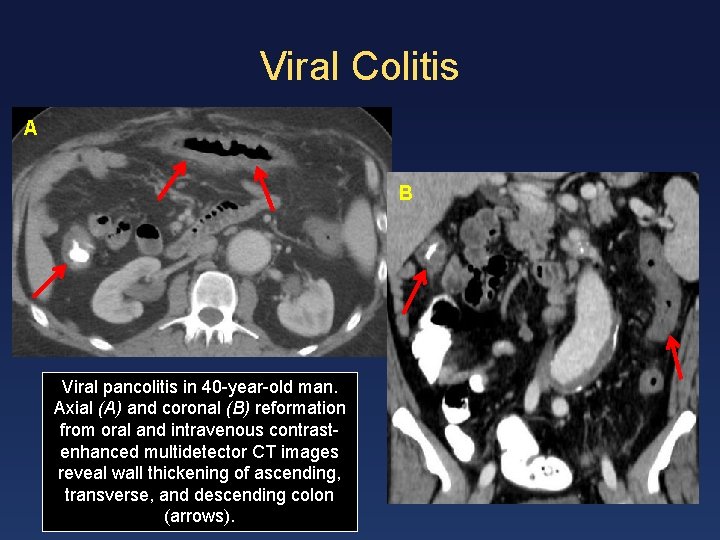
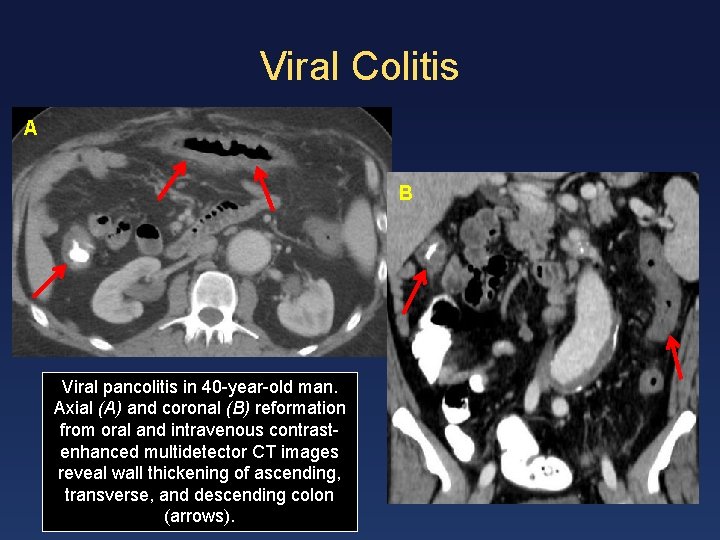
Viral Colitis A B Viral pancolitis in 40 -year-old man. Axial (A) and coronal (B) reformation from oral and intravenous contrastenhanced multidetector CT images reveal wall thickening of ascending, transverse, and descending colon (arrows).
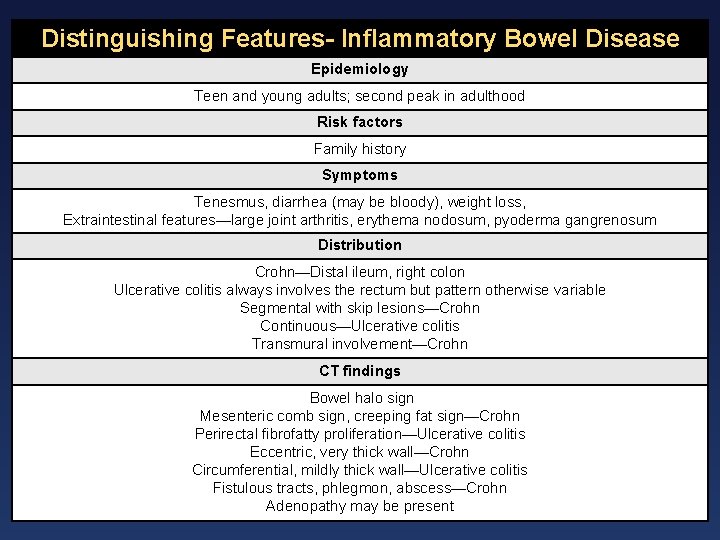
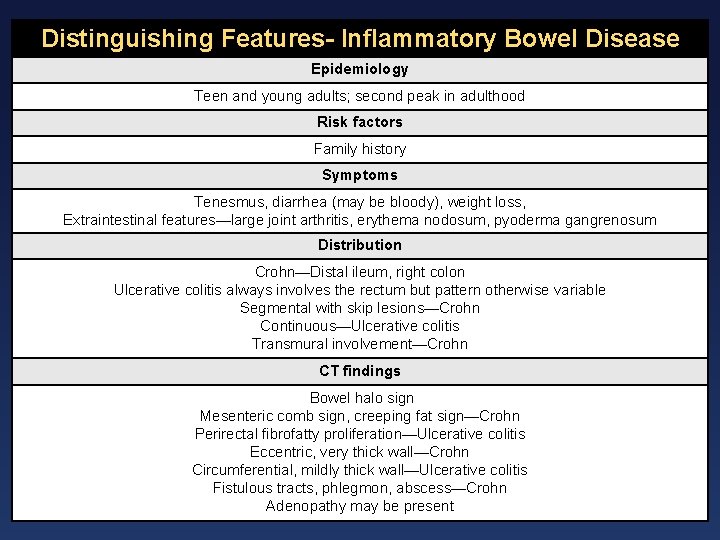
Distinguishing Features- Inflammatory Bowel Disease Epidemiology Teen and young adults; second peak in adulthood Risk factors Family history Symptoms Tenesmus, diarrhea (may be bloody), weight loss, Extraintestinal features—large joint arthritis, erythema nodosum, pyoderma gangrenosum Distribution Crohn—Distal ileum, right colon Ulcerative colitis always involves the rectum but pattern otherwise variable Segmental with skip lesions—Crohn Continuous—Ulcerative colitis Transmural involvement—Crohn CT findings Bowel halo sign Mesenteric comb sign, creeping fat sign—Crohn Perirectal fibrofatty proliferation—Ulcerative colitis Eccentric, very thick wall—Crohn Circumferential, mildly thick wall—Ulcerative colitis Fistulous tracts, phlegmon, abscess—Crohn Adenopathy may be present
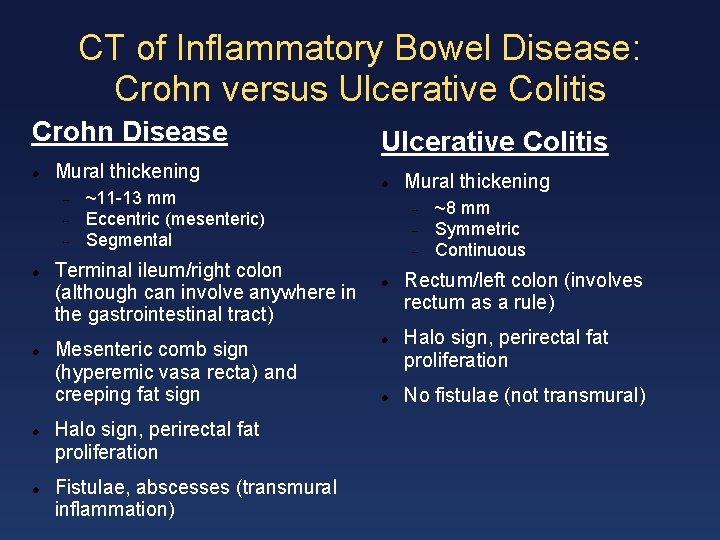
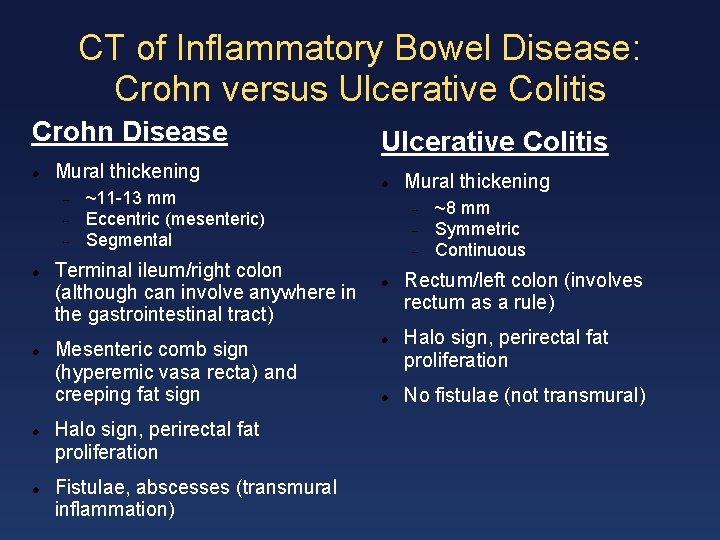
CT of Inflammatory Bowel Disease: Crohn versus Ulcerative Colitis Crohn Disease Mural thickening ~11 -13 mm Eccentric (mesenteric) Segmental Terminal ileum/right colon (although can involve anywhere in the gastrointestinal tract) Mesenteric comb sign (hyperemic vasa recta) and creeping fat sign Halo sign, perirectal fat proliferation Fistulae, abscesses (transmural inflammation) Ulcerative Colitis Mural thickening ~8 mm Symmetric Continuous Rectum/left colon (involves rectum as a rule) Halo sign, perirectal fat proliferation No fistulae (not transmural)
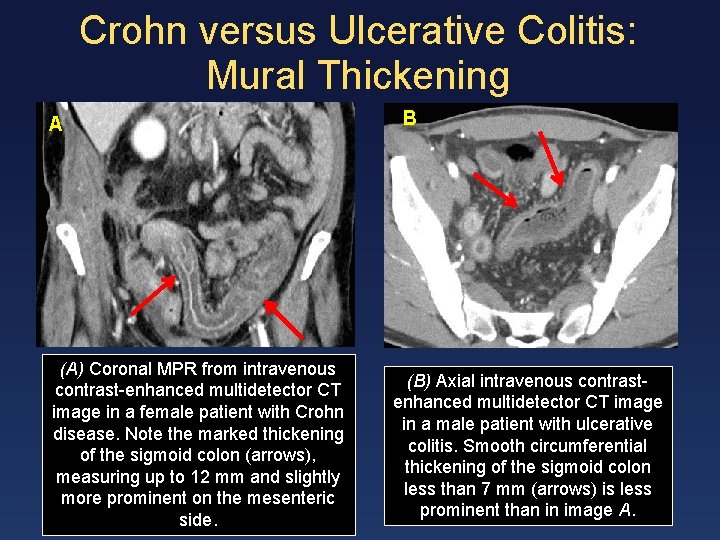
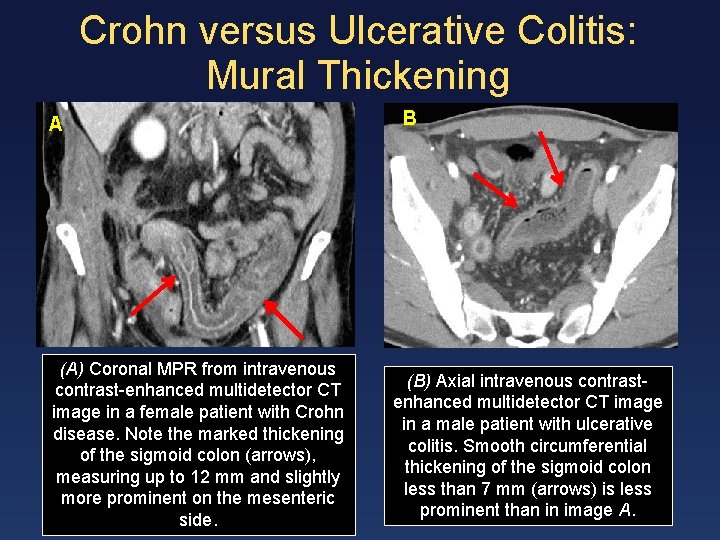
Crohn versus Ulcerative Colitis: Mural Thickening A (A) Coronal MPR from intravenous contrast-enhanced multidetector CT image in a female patient with Crohn disease. Note the marked thickening of the sigmoid colon (arrows), measuring up to 12 mm and slightly more prominent on the mesenteric side. B (B) Axial intravenous contrastenhanced multidetector CT image in a male patient with ulcerative colitis. Smooth circumferential thickening of the sigmoid colon less than 7 mm (arrows) is less prominent than in image A.
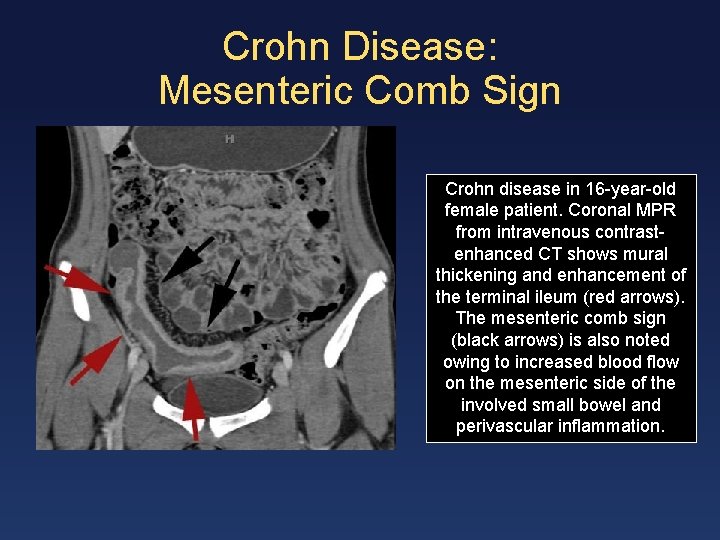
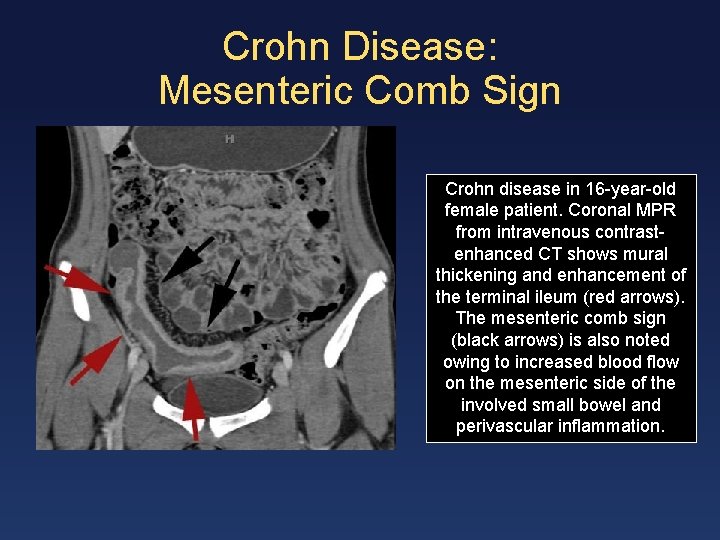
Crohn Disease: Mesenteric Comb Sign Crohn disease in 16 -year-old female patient. Coronal MPR from intravenous contrastenhanced CT shows mural thickening and enhancement of the terminal ileum (red arrows). The mesenteric comb sign (black arrows) is also noted owing to increased blood flow on the mesenteric side of the involved small bowel and perivascular inflammation.
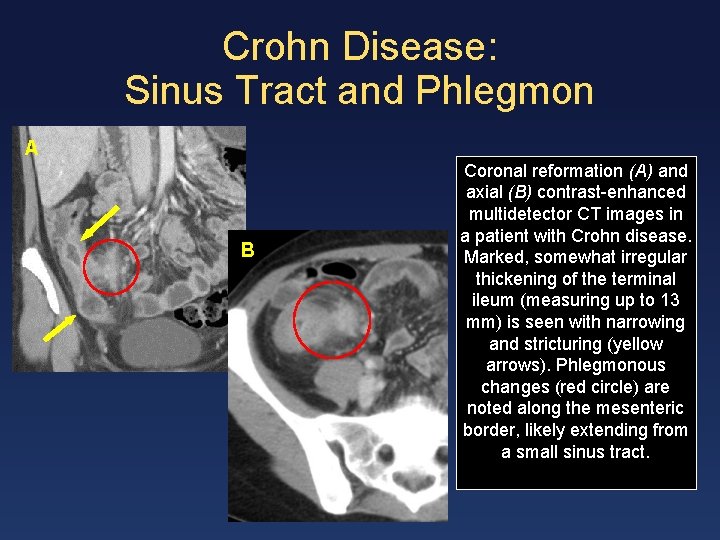
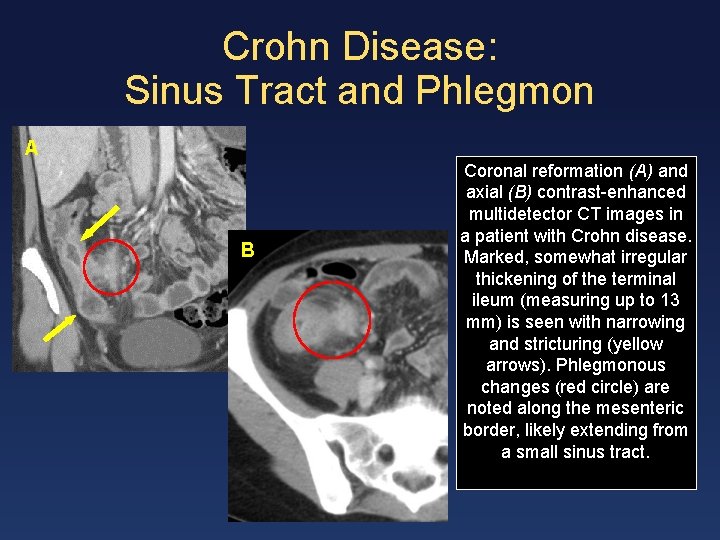
Crohn Disease: Sinus Tract and Phlegmon A B Coronal reformation (A) and axial (B) contrast-enhanced multidetector CT images in a patient with Crohn disease. Marked, somewhat irregular thickening of the terminal ileum (measuring up to 13 mm) is seen with narrowing and stricturing (yellow arrows). Phlegmonous changes (red circle) are noted along the mesenteric border, likely extending from a small sinus tract.
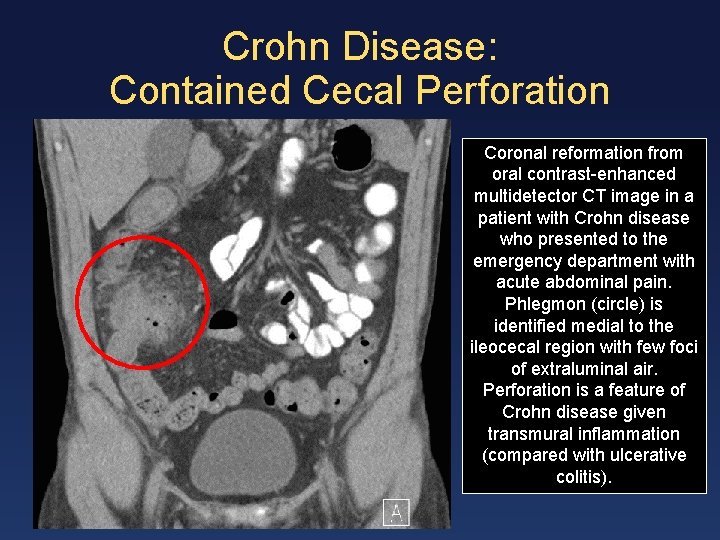
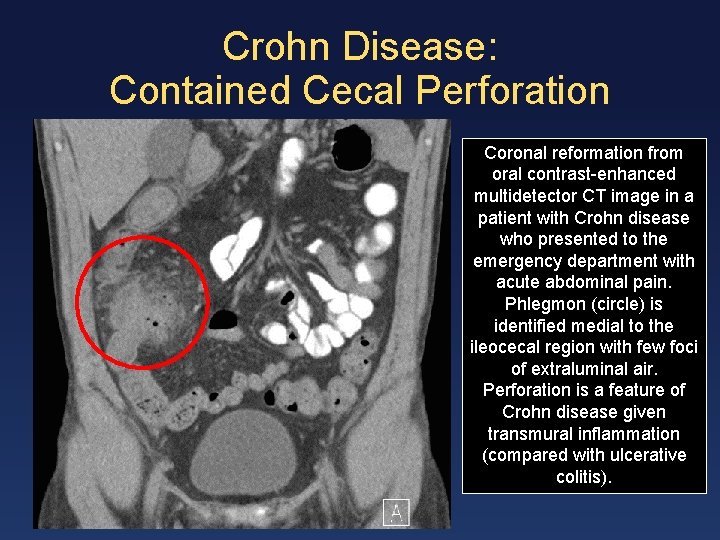
Crohn Disease: Contained Cecal Perforation Coronal reformation from oral contrast-enhanced multidetector CT image in a patient with Crohn disease who presented to the emergency department with acute abdominal pain. Phlegmon (circle) is identified medial to the ileocecal region with few foci of extraluminal air. Perforation is a feature of Crohn disease given transmural inflammation (compared with ulcerative colitis).
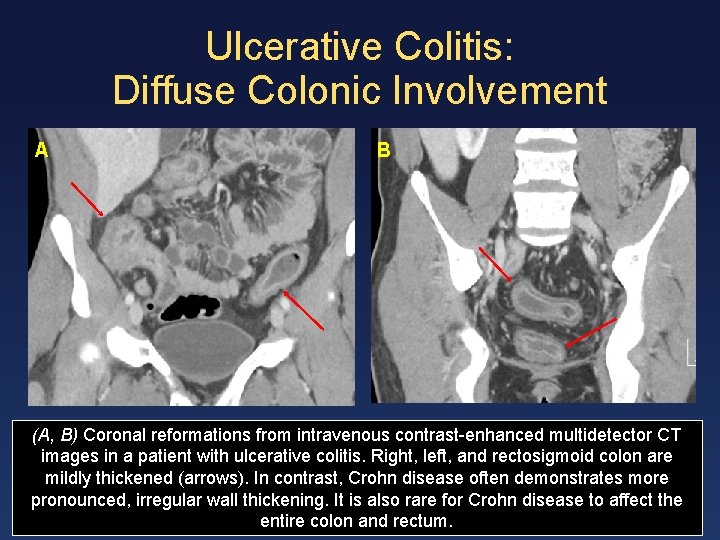
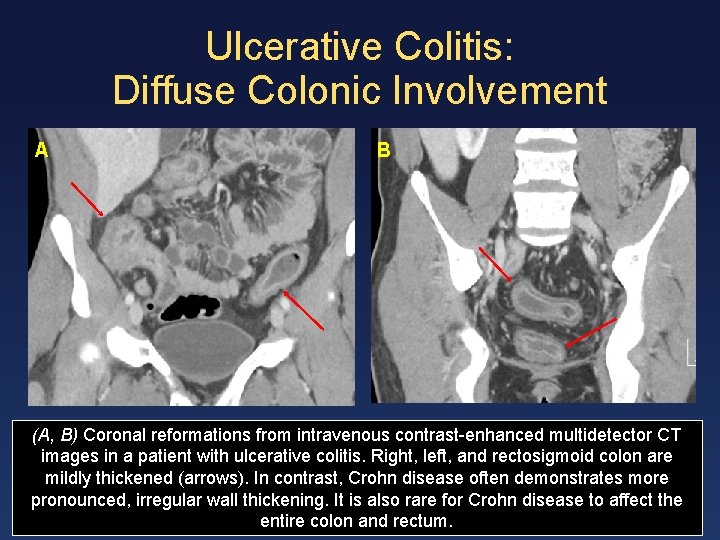
Ulcerative Colitis: Diffuse Colonic Involvement A B (A, B) Coronal reformations from intravenous contrast-enhanced multidetector CT images in a patient with ulcerative colitis. Right, left, and rectosigmoid colon are mildly thickened (arrows). In contrast, Crohn disease often demonstrates more pronounced, irregular wall thickening. It is also rare for Crohn disease to affect the entire colon and rectum.
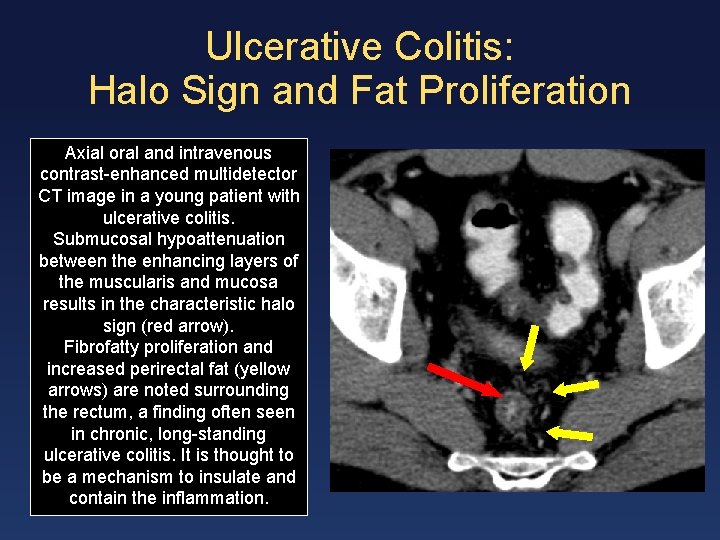
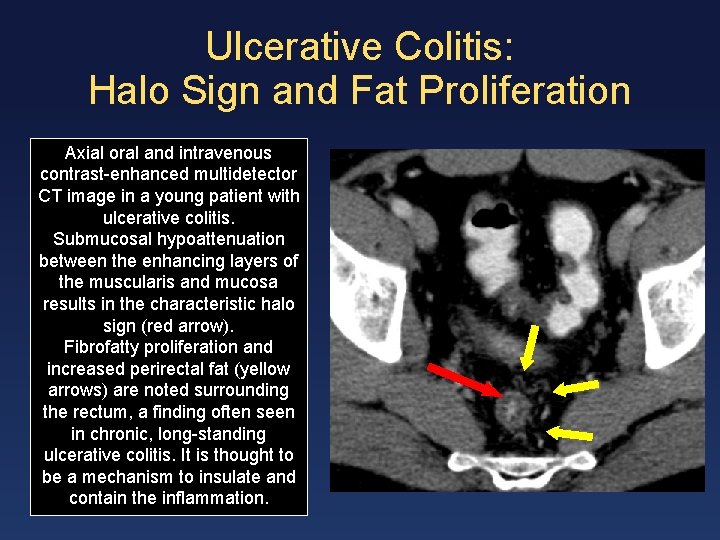
Ulcerative Colitis: Halo Sign and Fat Proliferation Axial oral and intravenous contrast-enhanced multidetector CT image in a young patient with ulcerative colitis. Submucosal hypoattenuation between the enhancing layers of the muscularis and mucosa results in the characteristic halo sign (red arrow). Fibrofatty proliferation and increased perirectal fat (yellow arrows) are noted surrounding the rectum, a finding often seen in chronic, long-standing ulcerative colitis. It is thought to be a mechanism to insulate and contain the inflammation.
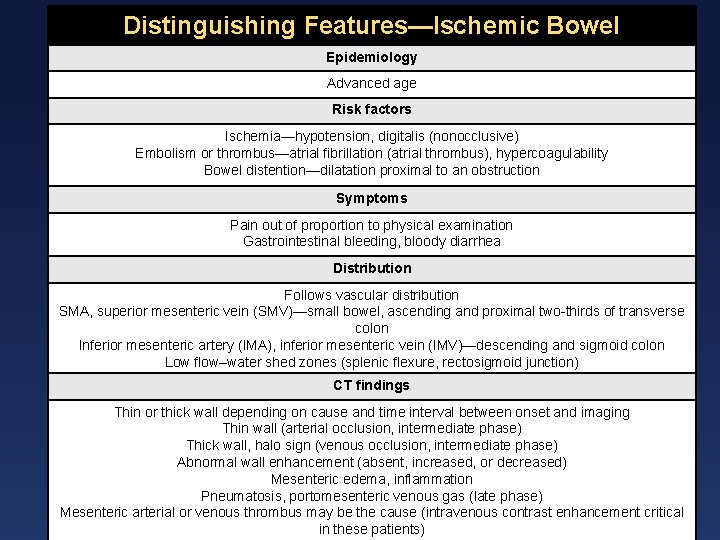
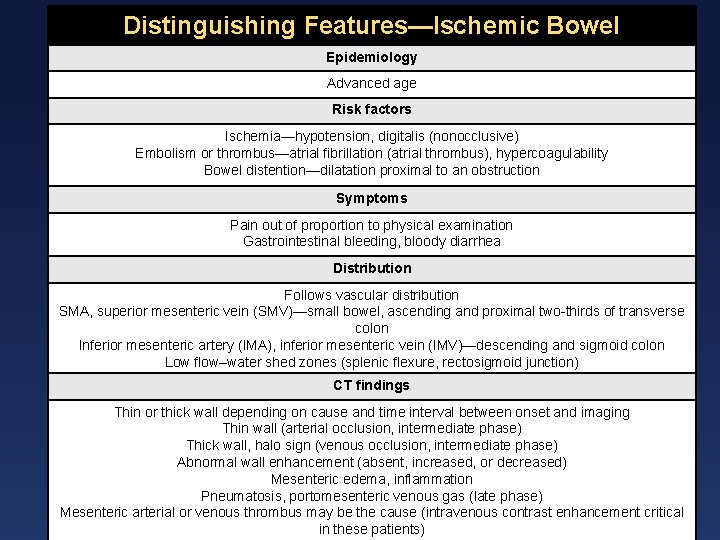
Distinguishing Features—Ischemic Bowel Epidemiology Advanced age Risk factors Ischemia—hypotension, digitalis (nonocclusive) Embolism or thrombus—atrial fibrillation (atrial thrombus), hypercoagulability Bowel distention—dilatation proximal to an obstruction Symptoms Pain out of proportion to physical examination Gastrointestinal bleeding, bloody diarrhea Distribution Follows vascular distribution SMA, superior mesenteric vein (SMV)—small bowel, ascending and proximal two-thirds of transverse colon Inferior mesenteric artery (IMA), inferior mesenteric vein (IMV)—descending and sigmoid colon Low flow–water shed zones (splenic flexure, rectosigmoid junction) CT findings Thin or thick wall depending on cause and time interval between onset and imaging Thin wall (arterial occlusion, intermediate phase) Thick wall, halo sign (venous occlusion, intermediate phase) Abnormal wall enhancement (absent, increased, or decreased) Mesenteric edema, inflammation Pneumatosis, portomesenteric venous gas (late phase) Mesenteric arterial or venous thrombus may be the cause (intravenous contrast enhancement critical in these patients)
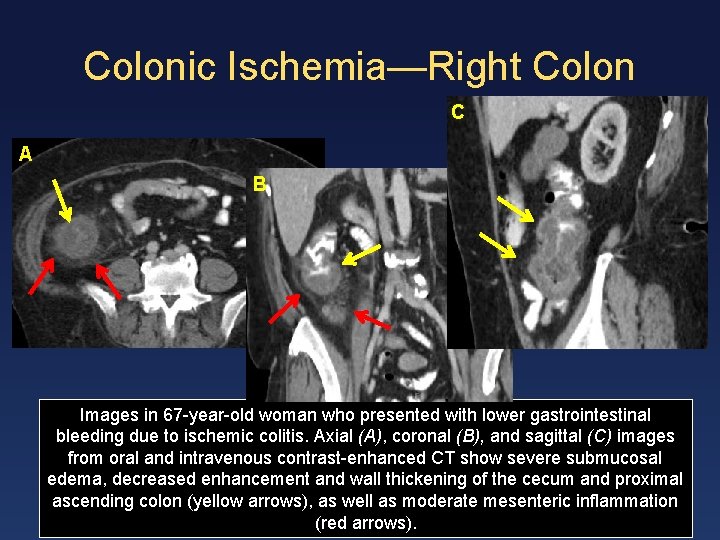
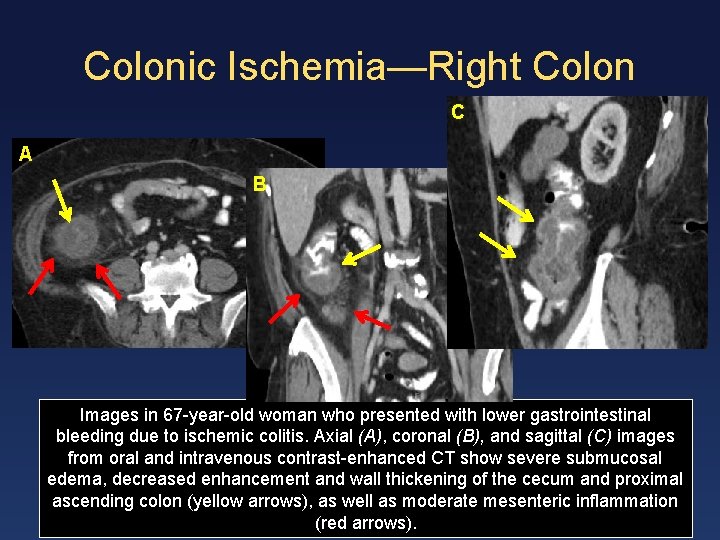
Colonic Ischemia—Right Colon C A B Images in 67 -year-old woman who presented with lower gastrointestinal bleeding due to ischemic colitis. Axial (A), coronal (B), and sagittal (C) images from oral and intravenous contrast-enhanced CT show severe submucosal edema, decreased enhancement and wall thickening of the cecum and proximal ascending colon (yellow arrows), as well as moderate mesenteric inflammation (red arrows).
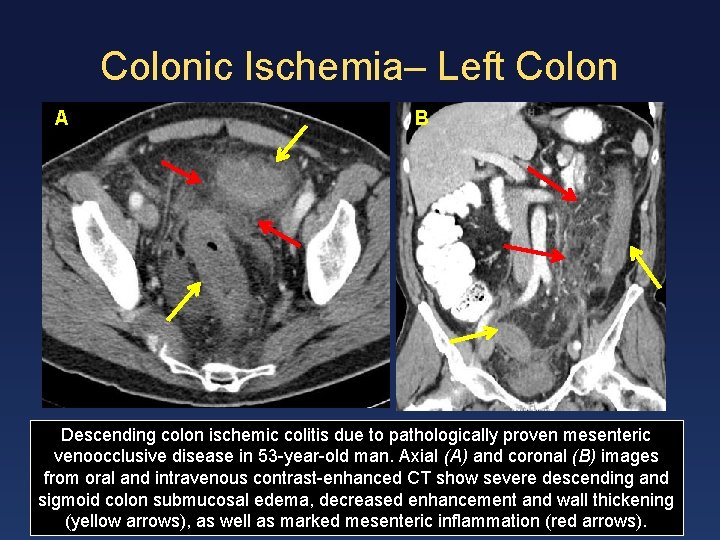
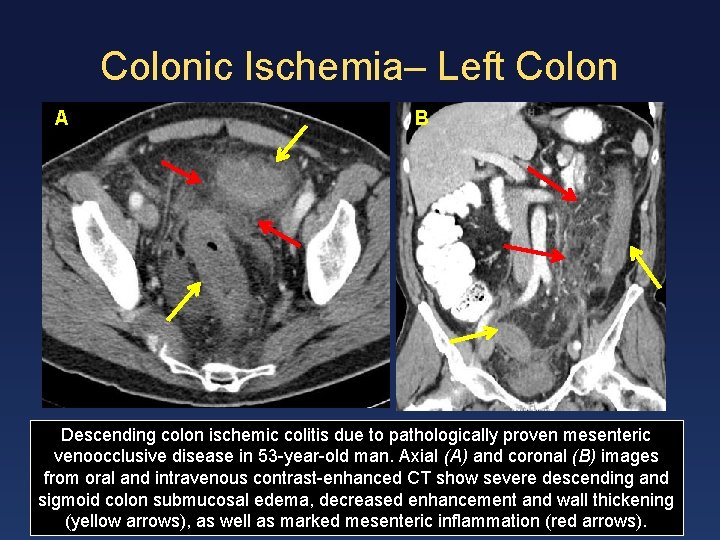
Colonic Ischemia– Left Colon AA B Descending colon ischemic colitis due to pathologically proven mesenteric venoocclusive disease in 53 -year-old man. Axial (A) and coronal (B) images from oral and intravenous contrast-enhanced CT show severe descending and sigmoid colon submucosal edema, decreased enhancement and wall thickening (yellow arrows), as well as marked mesenteric inflammation (red arrows).
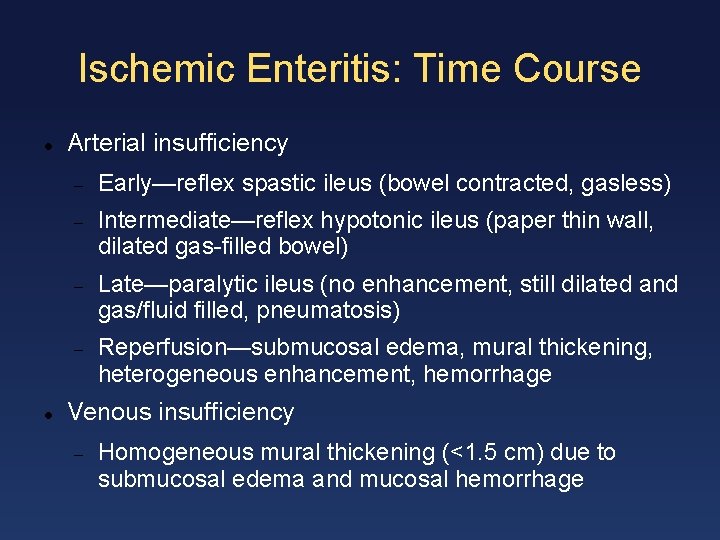
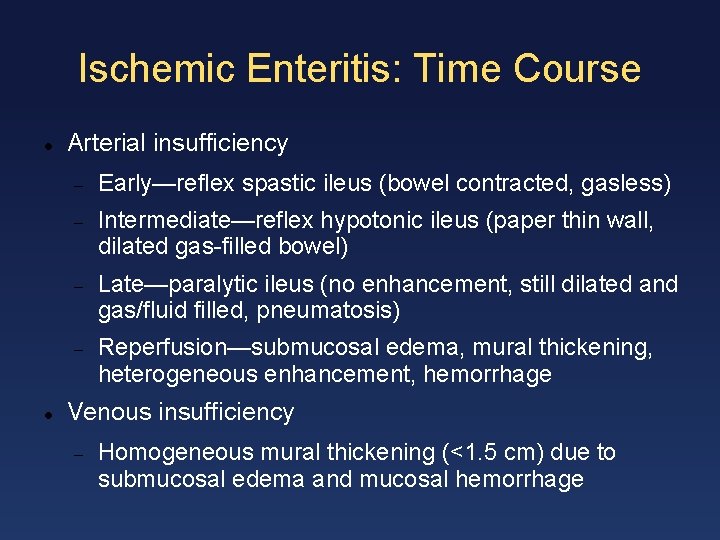
Ischemic Enteritis: Time Course Arterial insufficiency Early—reflex spastic ileus (bowel contracted, gasless) Intermediate—reflex hypotonic ileus (paper thin wall, dilated gas-filled bowel) Late—paralytic ileus (no enhancement, still dilated and gas/fluid filled, pneumatosis) Reperfusion—submucosal edema, mural thickening, heterogeneous enhancement, hemorrhage Venous insufficiency Homogeneous mural thickening (<1. 5 cm) due to submucosal edema and mucosal hemorrhage
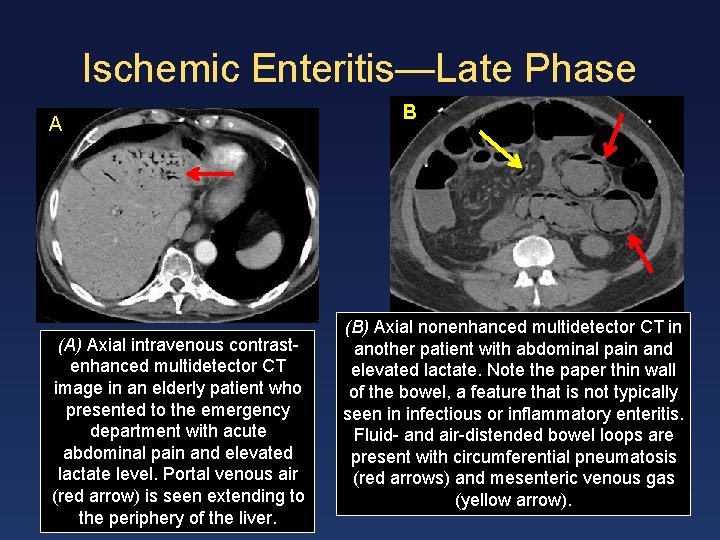
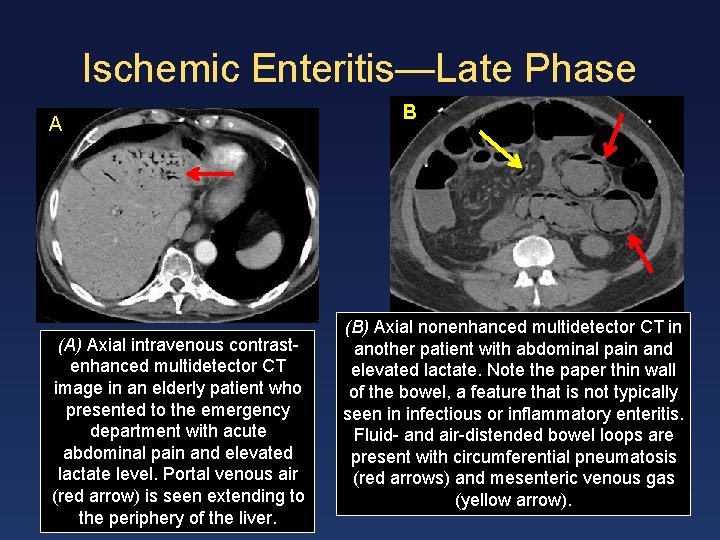
Ischemic Enteritis—Late Phase A (A) Axial intravenous contrastenhanced multidetector CT image in an elderly patient who presented to the emergency department with acute abdominal pain and elevated lactate level. Portal venous air (red arrow) is seen extending to the periphery of the liver. B (B) Axial nonenhanced multidetector CT in another patient with abdominal pain and elevated lactate. Note the paper thin wall of the bowel, a feature that is not typically seen in infectious or inflammatory enteritis. Fluid- and air-distended bowel loops are present with circumferential pneumatosis (red arrows) and mesenteric venous gas (yellow arrow).
Ischemic Bowel: Extraintestinal Findings Arterial compromise Venous insufficiency Thrombus in SMV, IMV, or branches Engorgement of mesenteric veins with collateral vessels Nonocclusive Small caliber SMA and branches Reperfusion injury Emboli or thrombi in SMA, IMA, or branches Mesenteric fat stranding—often pronounced and localized Late phase Portomesenteric venous gas
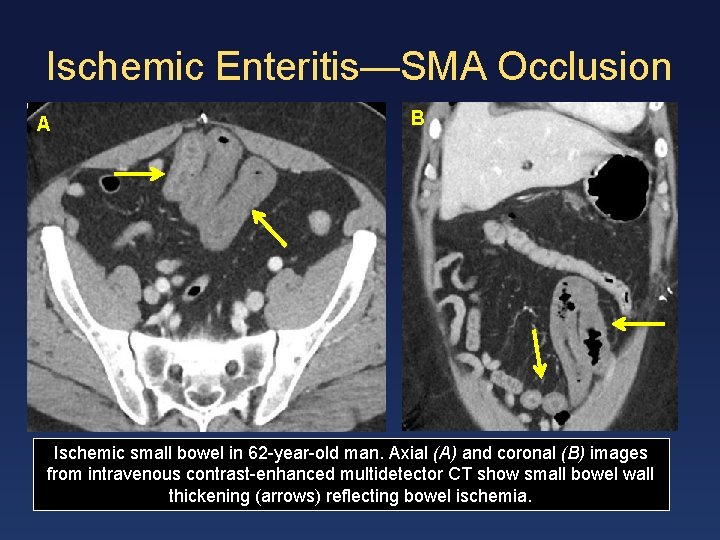
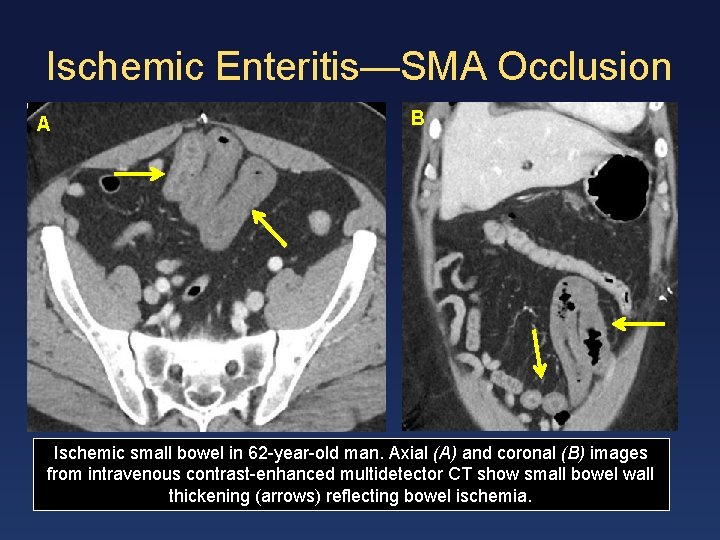
Ischemic Enteritis—SMA Occlusion A B Ischemic small bowel in 62 -year-old man. Axial (A) and coronal (B) images from intravenous contrast-enhanced multidetector CT show small bowel wall thickening (arrows) reflecting bowel ischemia.
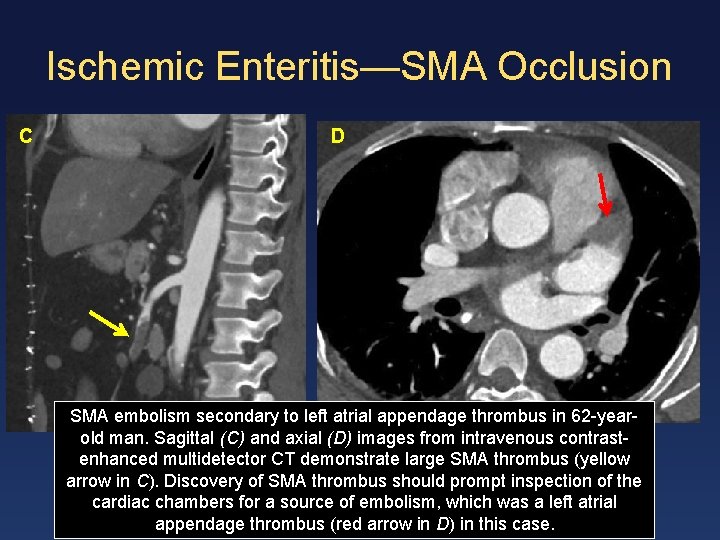
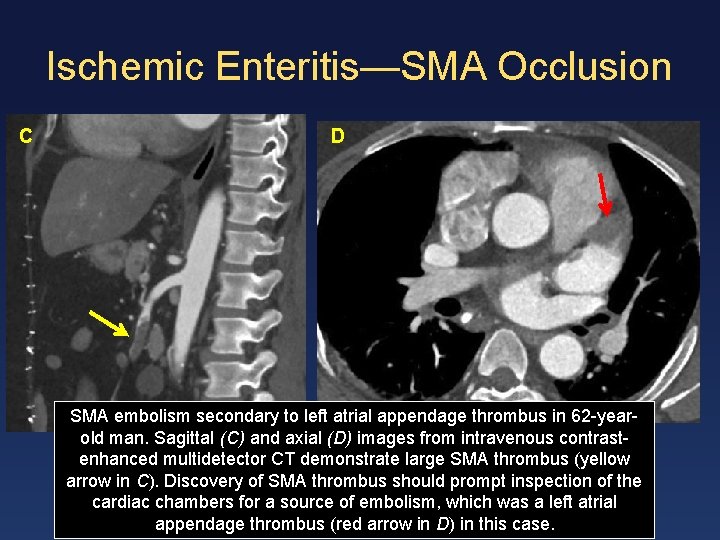
Ischemic Enteritis—SMA Occlusion C D SMA embolism secondary to left atrial appendage thrombus in 62 -yearold man. Sagittal (C) and axial (D) images from intravenous contrastenhanced multidetector CT demonstrate large SMA thrombus (yellow arrow in C). Discovery of SMA thrombus should prompt inspection of the cardiac chambers for a source of embolism, which was a left atrial appendage thrombus (red arrow in D) in this case.
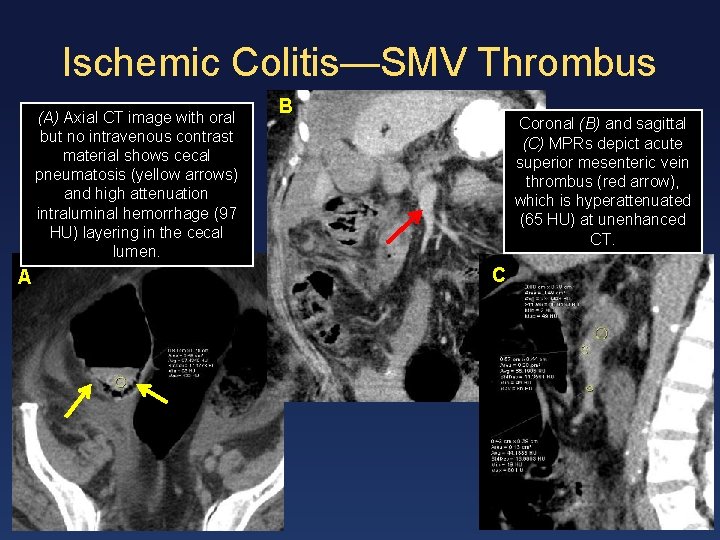
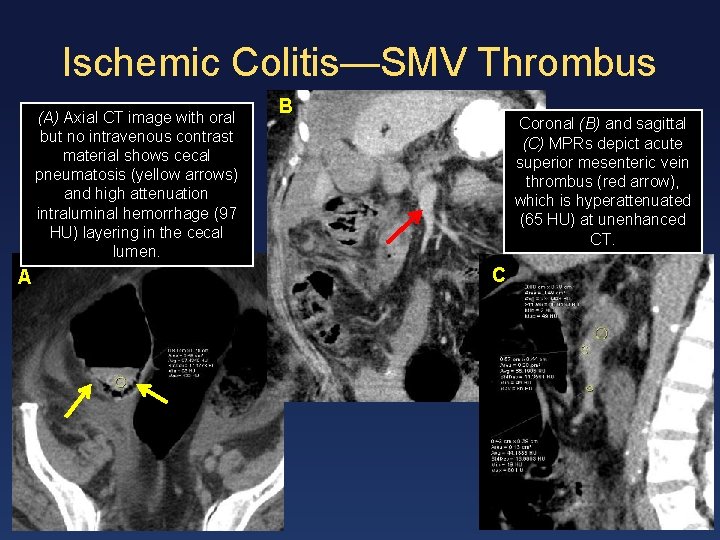
Ischemic Colitis—SMV Thrombus (A) Axial CT image with oral but no intravenous contrast material shows cecal pneumatosis (yellow arrows) and high attenuation intraluminal hemorrhage (97 HU) layering in the cecal lumen. A B Coronal (B) and sagittal (C) MPRs depict acute superior mesenteric vein thrombus (red arrow), which is hyperattenuated (65 HU) at unenhanced CT. C
Conclusions Enteritis and colitis are extremely common causes of abdominal pain. Enterocolitis is usually due to one of three causes: infection, inflammatory bowel disease, or ischemia. CT technique with intravenous contrast material and neutral or negative oral contrast material is essential to evaluate the bowel, mesentery, and vasculature in these patients and demonstrate characteristic findings. By focusing on distribution patterns and gastrointestinal and extraintestinal manifestations, the radiologist can determine the cause in many cases, facilitating proper and timely treatment.
Acknowledgment We thank Hannah Ahn for creating the graphic art in slides 10 and 13.
Suggested Readings Ambrosini R, Barchiesi A, Di Mizio V, et al. Inflammatory chronic disease of the colon: how to image. Eur J Radiol 2007; 61: 442 -448. Barral M, Boudiaf M, Dohan A, et al. MDCT of acute colitis in adults: an update in current imaging features. Diagn Interv Imaging 2015; 96: 133 -149. Balthazar EJ, Yen BC, Gordon RB. Ischemic colitis: CT evaluation of 54 cases. Radiology 1999; 211: 381 -388. Bruining DH, Loftus EV, Jr. Crohn's disease clinical issues and treatment: what the radiologist needs to know and what the gastroenterologist wants to know. Abdom Imaging 2009; 34: 297302. Cao J, Liu WJ, Xu XY, Zou XP. Endoscopic findings and clinicopathologic characteristics of colonic schistosomiasis: a report of 46 cases. World J Gastroenterol 2010; 16: 723 -727. Cevallos AM, Katelaris PH, Farthing MJ. Pathogenesis of giardiasis. Gastroenterology 1993; 105: 306 -307. Cruz C, Abujudeh HH, Nazarian RM, Thrall JH. Ischemic colitis: spectrum of CT findings, sites of involvement and severity. Emerg Radiol 2015; 22(4): 357 -365. Fishman EK, Kavuru M, Jones B, et al. Pseudomembranous colitis: CT evaluation of 26 cases. Radiology 1991; 180: 57 -60. Fishman EK, Wolf EJ, Jones B, Bayless TM, Siegelman SS. CT evaluation of Crohn's disease: effect on patient management. AJR Am J Roentgenol 1987; 148: 537 -540. Frager DH, Frager JD, Wolf EL, et al. Cytomegalovirus colitis in acquired immune deficiency syndrome: radiologic spectrum. Gastrointest Radiol 1986; 11: 241 -246. Hoeffel C, Crema MD, Belkacem A, et al. Multi-detector row CT: spectrum of diseases involving the ileocecal area. Radio. Graphics 2006; 26: 1373 -1390. Horton KM, Corl FM, Fishman EK. CT evaluation of the colon: inflammatory disease. Radio. Graphics 2000; 20: 399 -418. Iacobellis F, Berritto D, Fleischmann D, et al. CT findings in acute, subacute, and chronic ischemic colitis: suggestions for diagnosis. Biomed Res Int. doi: 10. 1155/2014/895248. Published August 27, 2014. Koh DM, Burn PR, Mathews G, Nelson M, Healy JC. Abdominal computed tomographic findings of Mycobacterium tuberculosis and Mycobacterium avium intracellulare infection in HIV seropositive patients. Can Assoc Radiol J 2003; 54: 45 -50. Madureira AJ. The comb sign. Radiology 2004; 230: 783 -784. Merine DS, Fishman EK, Jones B, Nussbaum AR, Simmons T. Right lower quadrant pain in the immunocompromised patient: CT findings in 10 cases. AJR Am J Roentgenol 1987; 149: 1177 -1179 Moscandrew ME, Loftus EV, Jr. Diagnostic advances in inflammatory bowel disease (imaging and laboratory). Curr Gastroenterol Rep 2009; 11: 488 -495. Navaneethan U, Giannella RA. Infectious colitis. Curr Opin Gastroenterol. 2011; 27: 66 -71. Pantongrag-Brown L, Krebs TL, Daly BD, Wong-You-Cheong JJ, Beiser C, Krause B, Brown AE. Frequency of abdominal CT findings in AIDS patients with M. avium complex bacteraemia. Clin Radiol 1998; 53: 816 -819.
Suggested Readings Philpotts LE, Heiken JP, Westcott MA, Gore RM. Colitis: use of CT findings in differential diagnosis. Radiology 1994; 190: 445 -449. Plastaras L, Vuitton L, Badet N, Koch S, Di Martino V, Delabrousse E. Acute colitis: differential diagnosis using multidetector CT. Clin Radiol 2015; 70: 262 -269. Re gent D, Croise -Laurent V, Mathias J, Fairise A , Ropion-Michaux H , Proust C. Acute gastritis and enteritis. In: Taourel P, ed. CT of the Acute Abdomen. Berlin Heidelberg, Germany: Springer-Verlag, 2011: 239 -271. Ribeiro MB, Greenstein AJ, Yamazaki Y, Aufses AH, Jr. Intra-abdominal abscess in regional enteritis. Ann Surg 1991; 213: 32 -36. Romano S, Lassandro F, Scaglione M, Romano L, Rotondo A, Grassi R. Ischemia and infarction of the small bowel and colon: spectrum of imaging findings. Abdom Imaging 2006; 31: 277 -292. Romano S, Romano L. Ischemia (acute mesenteric ischemia and ischemic colitis). In: Taourel P, ed. CT of the Acute Abdomen. Berlin Heidelberg, Germany: Springer-Verlag, 2011; 183 -197. Romano S, Russo A, Daniele S, Tortora G, Maisto F, Romano L. Acute inflammatory bowel disease of the small intestine in adult: MDCT findings and criteria for differential diagnosis. Eur J Radiol 2009; 69: 381 -387. Scaglione M, Di Mizio V, Pinto A, Antonietta Mazzei M, Romano L, Grassi R. Gastrointestinal tract. In: Scaglione M, Linsenmaier U, Schueller G, eds. Emergency Radiology of the Abdomen. Berlin Heidelberg, Germany: Springer-Verlag, 2012; 133 -163. Segatto E, Mortele KJ, Ji H, Wiesner W, Ros PR. Acute small bowel ischemia: CT imaging findings. Semin Ultrasound CT MR 2003; 24: 364 -376. Sharif S, Hyser M. Ischemic proctitis: case series and literature review. Am Surg 2006; 72: 1241 -1247. Sherman SC, Weber JM. The CT diagnosis of Ascariasis. J Emerg Med 2005; 28: 471 -472. Soyer P, Boudiaf M, Guerrache Y, Hoeffel C, Dray X, Taourel P. Nonischemic colitis. In: Taourel P, ed. CT of the Acute Abdomen. Berlin Heidelberg, Germany: Springer-Verlag, 2011: 221 -237. Taourel P, Aufort S, Merigeaud S, Doyon FC, Hoquet MD, Delabrousse E. Imaging of ischemic colitis. Radiol Clin North Am 2008; 46: 909 -924. Thoeni RF, Cello JP. CT imaging of colitis. Radiology 2006; 240: 623 -638. Vilela EG, Torres HO, Martins FP, Ferrari Mde L, Andrade MM, Cunha AS. Evaluation of inflammatory activity in Crohn's disease and ulcerative colitis. World J Gastroenterol 2012; 18: 872 -881. Wee B, Poels JA, Mc. Cafferty IJ, Taniere P, Olliff J. A description of CT features of Clostridium difficile infection of the small bowel in four patients and a review of literature. Br J Radiol 2009; 82: 890 -895. Wiesner W, Khurana B, Ji H, Ros PR. CT of acute bowel ischemia. Radiology 2003; 226: 635 -650.