Colitis associated cancer risk and surveillance Risk and
- Slides: 34
Colitis associated cancer: risk and surveillance • Risk and risk factors of CRC in IBD • Molecular pathways of CRC in IBD • Surveillance colonoscopy • Chemoprevention
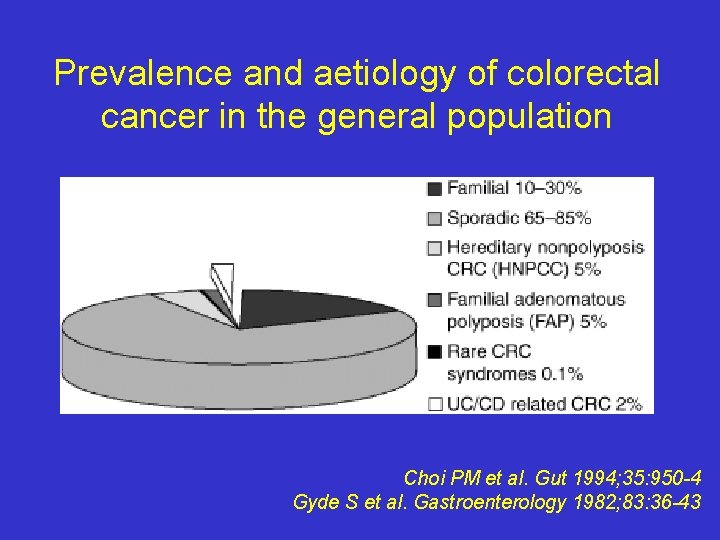
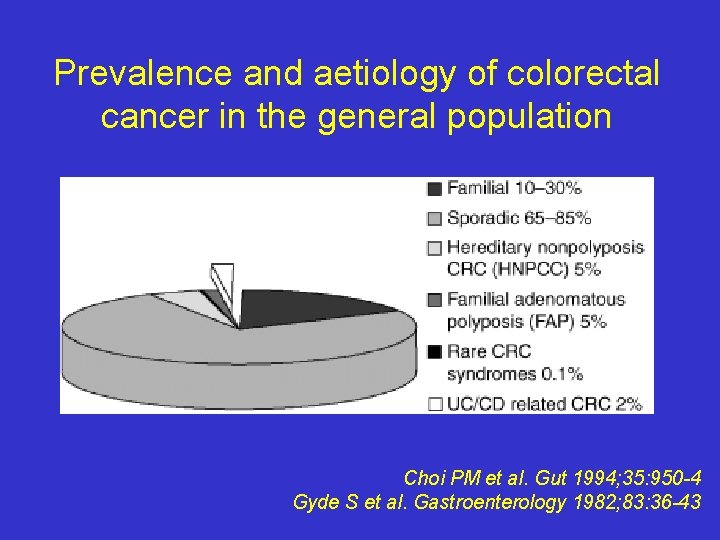
Prevalence and aetiology of colorectal cancer in the general population Choi PM et al. Gut 1994; 35: 950 -4 Gyde S et al. Gastroenterology 1982; 83: 36 -43
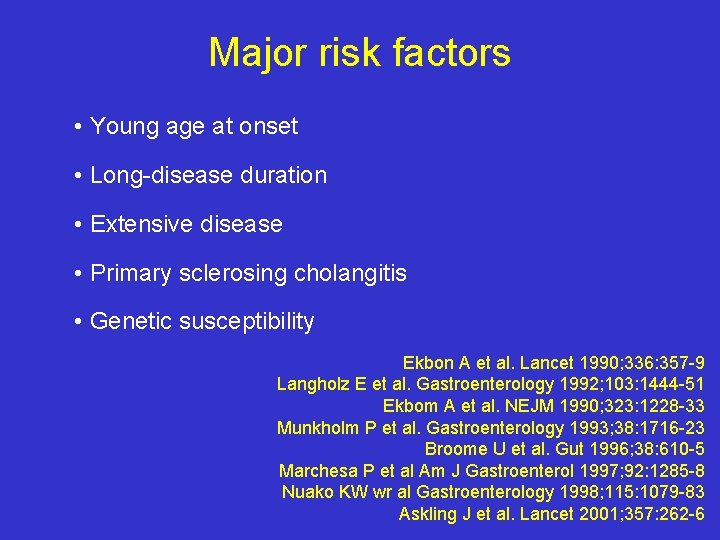
Major risk factors • Young age at onset • Long-disease duration • Extensive disease • Primary sclerosing cholangitis • Genetic susceptibility Ekbon A et al. Lancet 1990; 336: 357 -9 Langholz E et al. Gastroenterology 1992; 103: 1444 -51 Ekbom A et al. NEJM 1990; 323: 1228 -33 Munkholm P et al. Gastroenterology 1993; 38: 1716 -23 Broome U et al. Gut 1996; 38: 610 -5 Marchesa P et al Am J Gastroenterol 1997; 92: 1285 -8 Nuako KW wr al Gastroenterology 1998; 115: 1079 -83 Askling J et al. Lancet 2001; 357: 262 -6
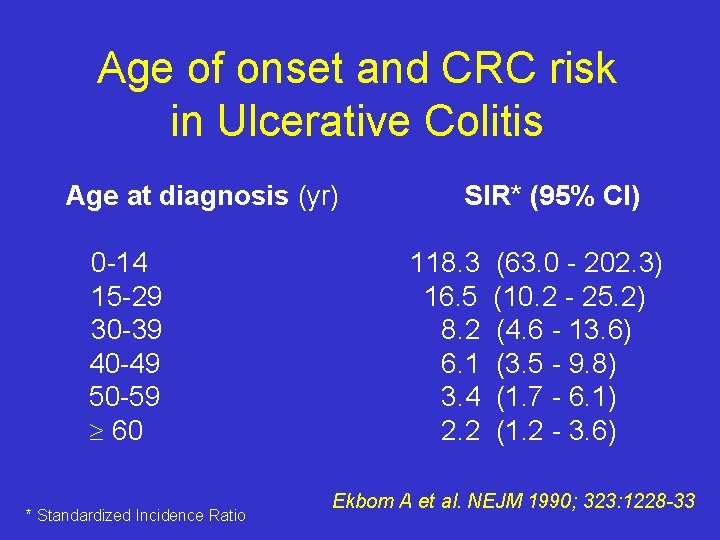
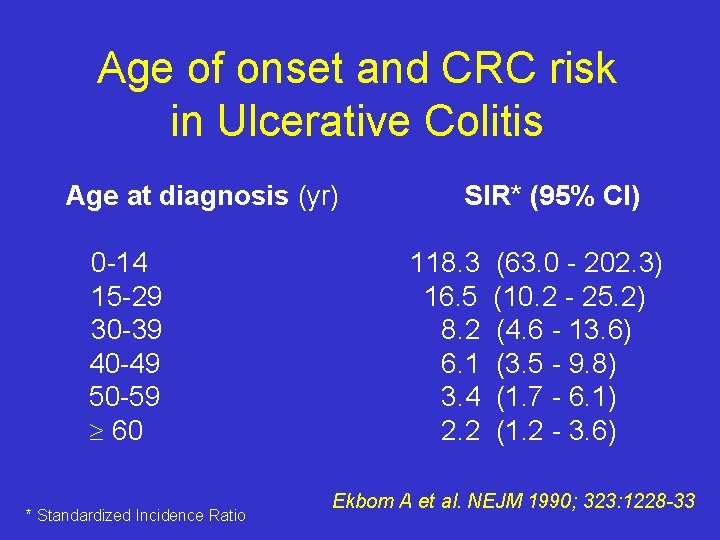
Age of onset and CRC risk in Ulcerative Colitis Age at diagnosis (yr) 0 -14 15 -29 30 -39 40 -49 50 -59 60 * Standardized Incidence Ratio SIR* (95% CI) 118. 3 16. 5 8. 2 6. 1 3. 4 2. 2 (63. 0 - 202. 3) (10. 2 - 25. 2) (4. 6 - 13. 6) (3. 5 - 9. 8) (1. 7 - 6. 1) (1. 2 - 3. 6) Ekbom A et al. NEJM 1990; 323: 1228 -33
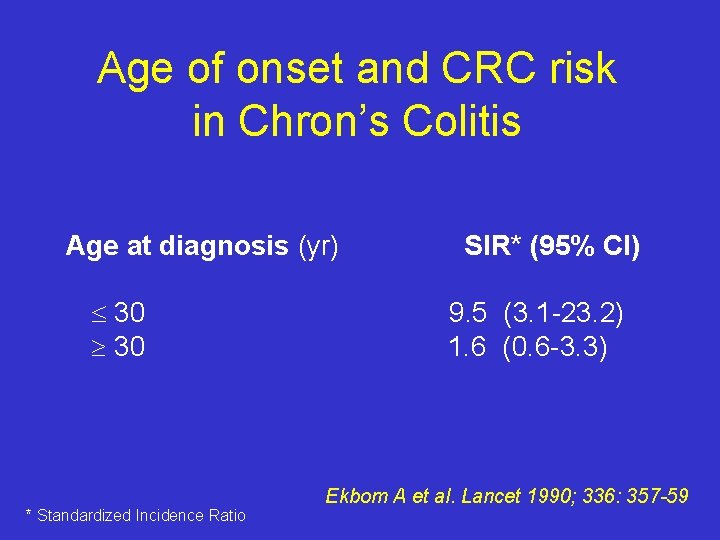
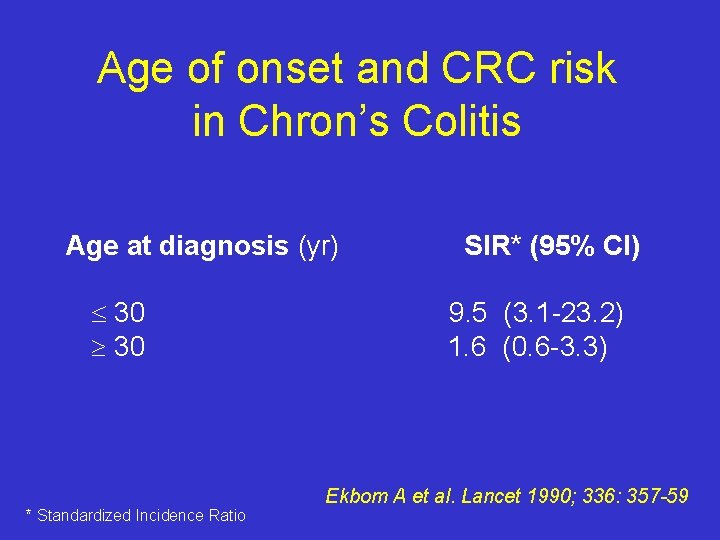
Age of onset and CRC risk in Chron’s Colitis Age at diagnosis (yr) 30 * Standardized Incidence Ratio SIR* (95% CI) 9. 5 (3. 1 -23. 2) 1. 6 (0. 6 -3. 3) Ekbom A et al. Lancet 1990; 336: 357 -59
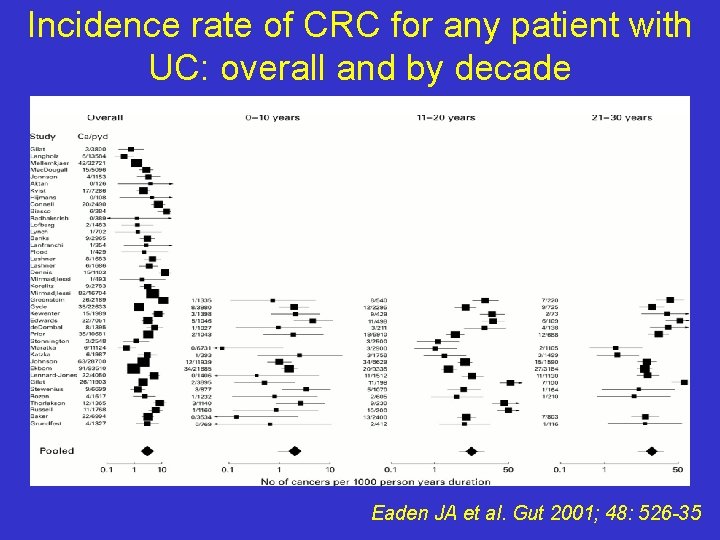
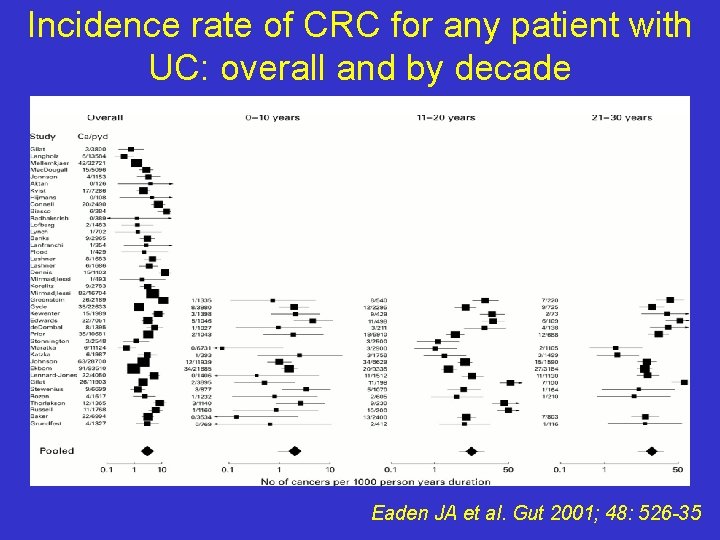
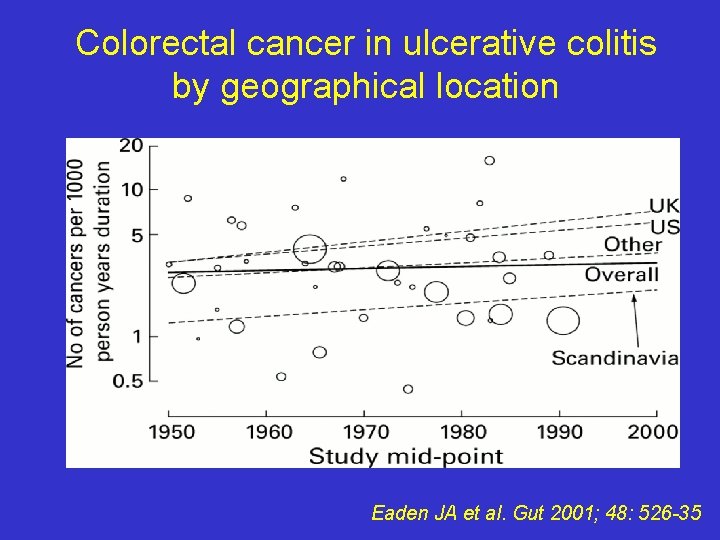
Incidence rate of CRC for any patient with UC: overall and by decade Eaden JA et al. Gut 2001; 48: 526 -35
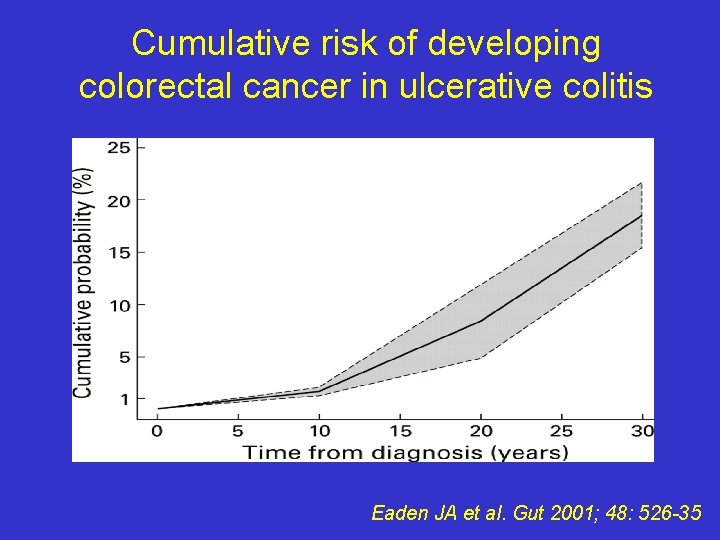
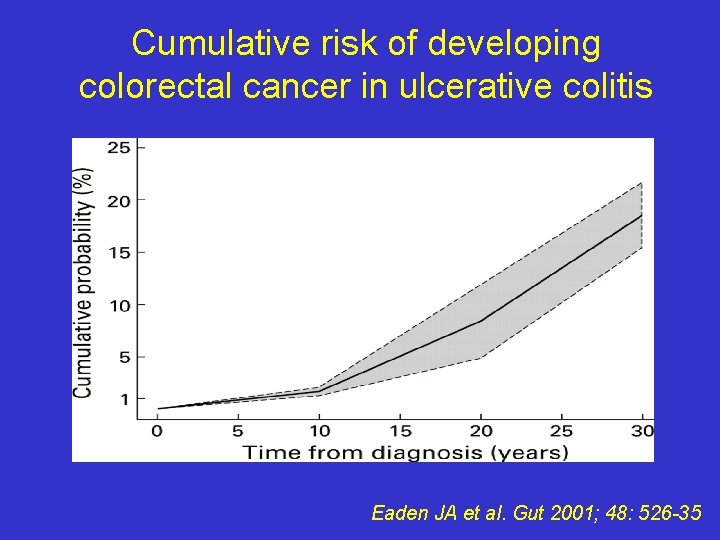
Cumulative risk of developing colorectal cancer in ulcerative colitis Eaden JA et al. Gut 2001; 48: 526 -35
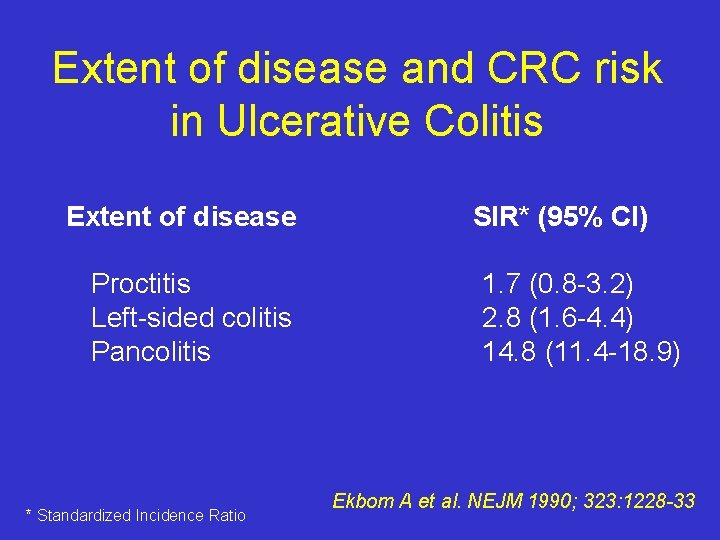
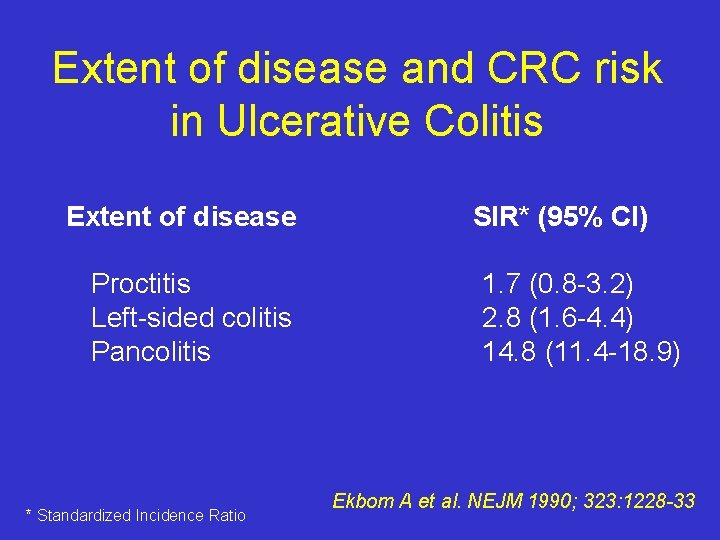
Extent of disease and CRC risk in Ulcerative Colitis Extent of disease Proctitis Left-sided colitis Pancolitis * Standardized Incidence Ratio SIR* (95% CI) 1. 7 (0. 8 -3. 2) 2. 8 (1. 6 -4. 4) 14. 8 (11. 4 -18. 9) Ekbom A et al. NEJM 1990; 323: 1228 -33
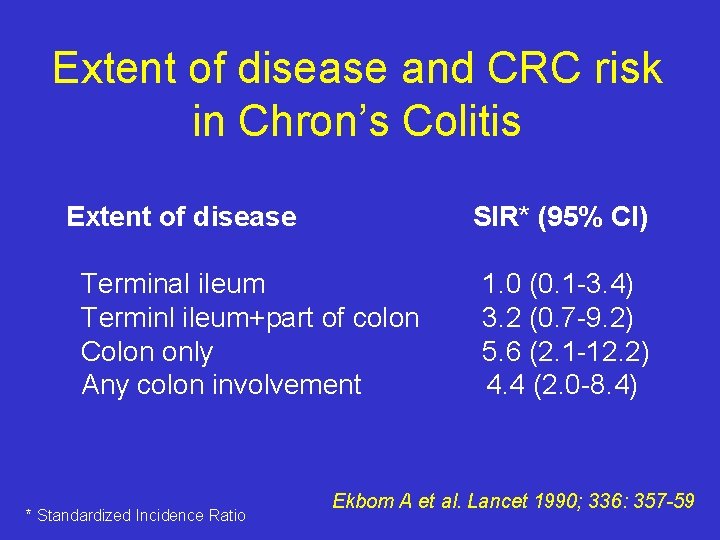
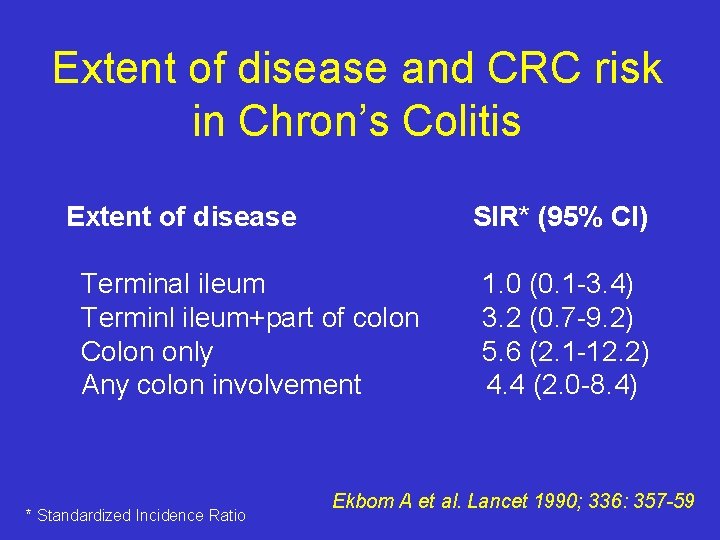
Extent of disease and CRC risk in Chron’s Colitis Extent of disease SIR* (95% CI) Terminal ileum Terminl ileum+part of colon Colon only Any colon involvement * Standardized Incidence Ratio 1. 0 (0. 1 -3. 4) 3. 2 (0. 7 -9. 2) 5. 6 (2. 1 -12. 2) 4. 4 (2. 0 -8. 4) Ekbom A et al. Lancet 1990; 336: 357 -59
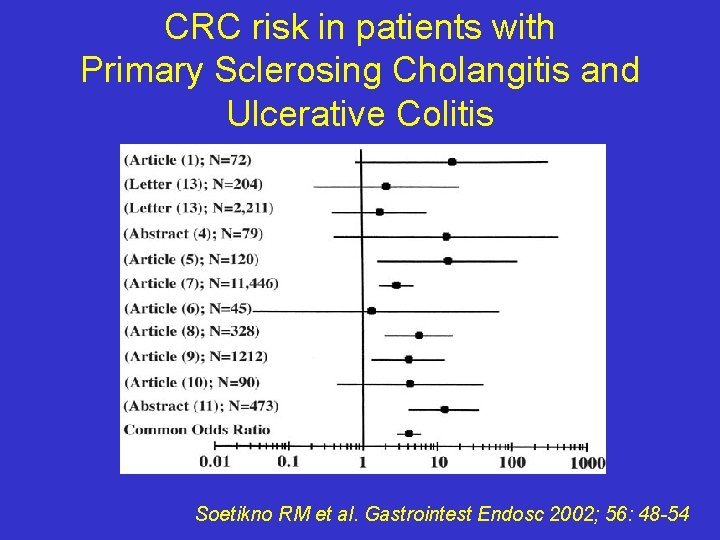
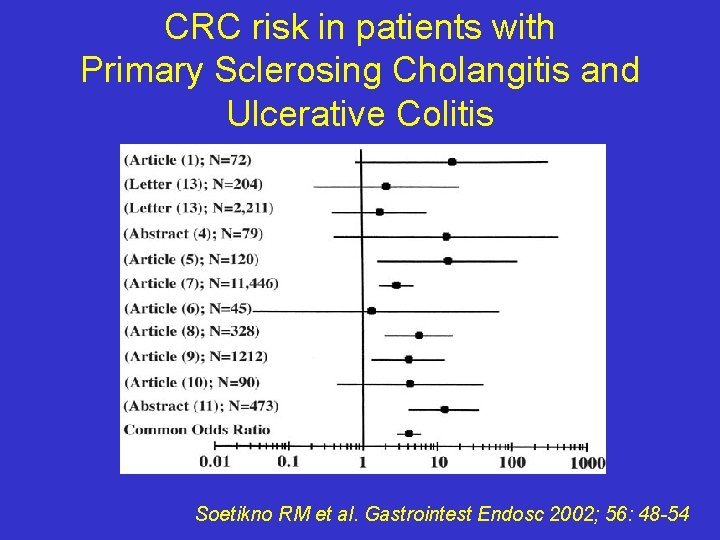
CRC risk in patients with Primary Sclerosing Cholangitis and Ulcerative Colitis Soetikno RM et al. Gastrointest Endosc 2002; 56: 48 -54
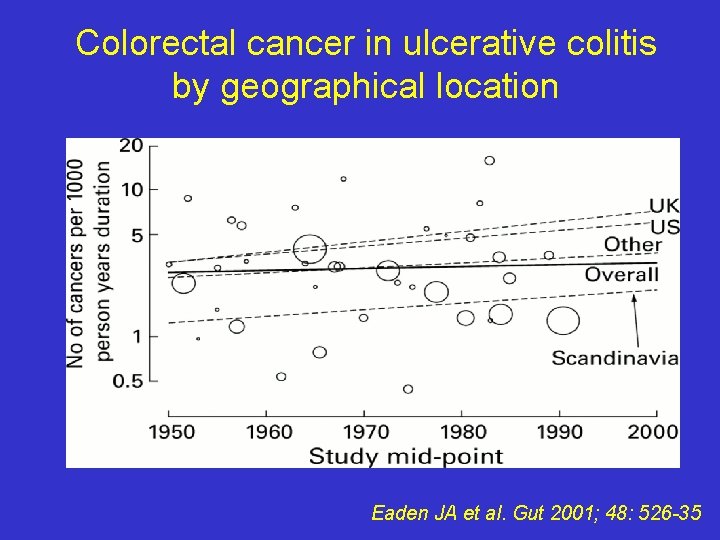
Colorectal cancer in ulcerative colitis by geographical location Eaden JA et al. Gut 2001; 48: 526 -35
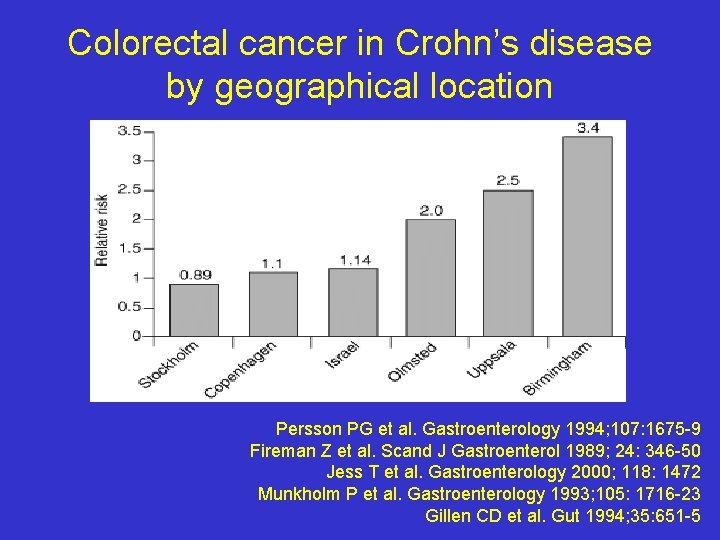
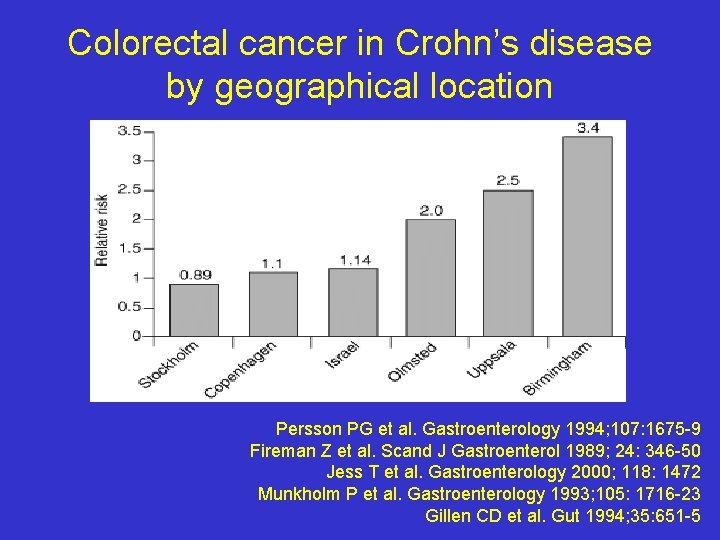
Colorectal cancer in Crohn’s disease by geographical location Persson PG et al. Gastroenterology 1994; 107: 1675 -9 Fireman Z et al. Scand J Gastroenterol 1989; 24: 346 -50 Jess T et al. Gastroenterology 2000; 118: 1472 Munkholm P et al. Gastroenterology 1993; 105: 1716 -23 Gillen CD et al. Gut 1994; 35: 651 -5
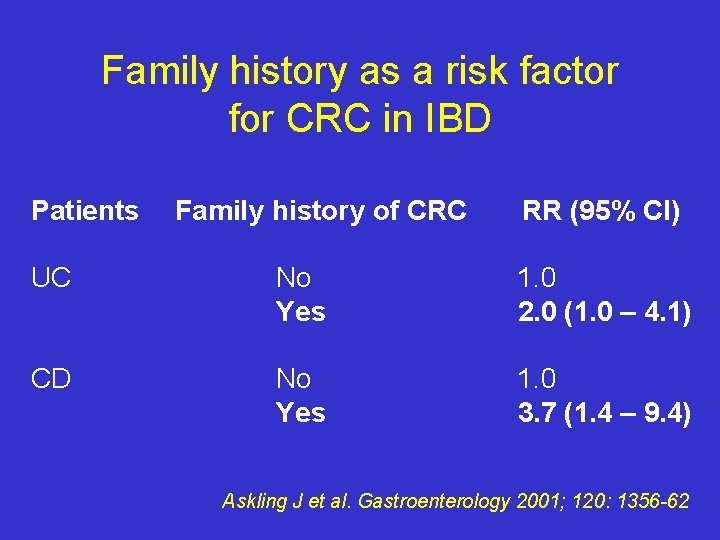
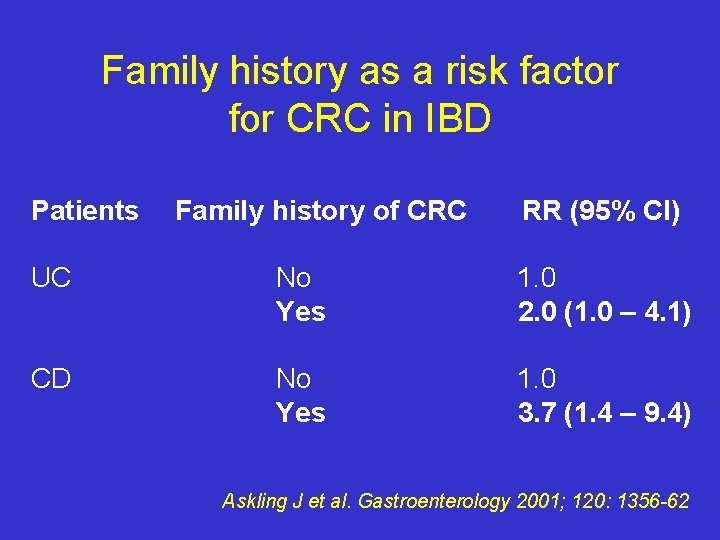
Family history as a risk factor for CRC in IBD Patients Family history of CRC RR (95% CI) UC No Yes 1. 0 2. 0 (1. 0 – 4. 1) CD No Yes 1. 0 3. 7 (1. 4 – 9. 4) Askling J et al. Gastroenterology 2001; 120: 1356 -62
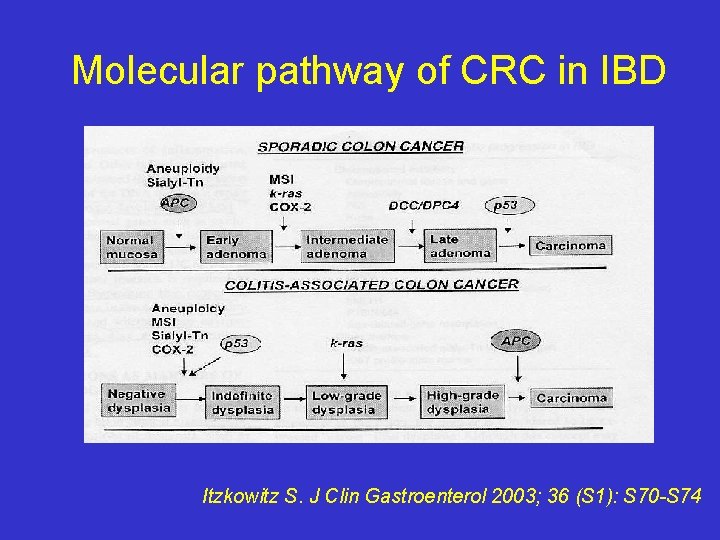
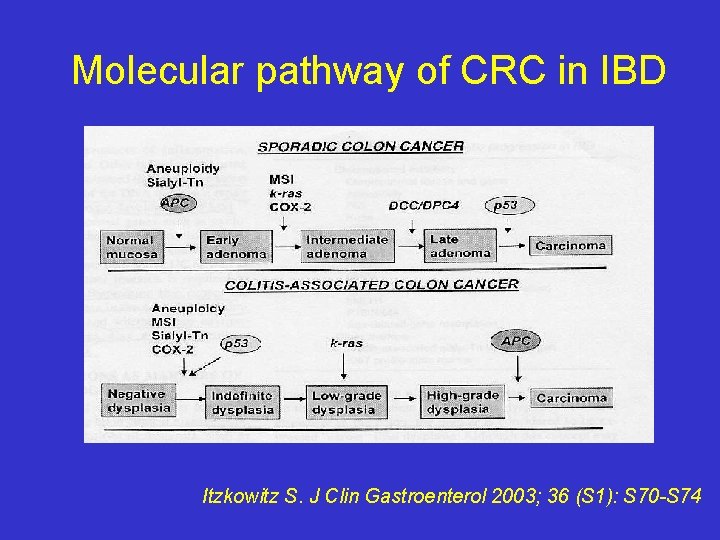
Molecular pathway of CRC in IBD Itzkowitz S. J Clin Gastroenterol 2003; 36 (S 1): S 70 -S 74
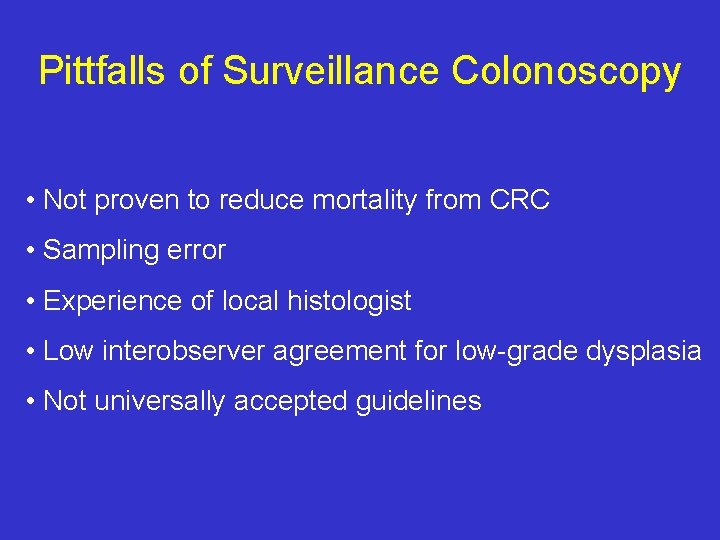
Pittfalls of Surveillance Colonoscopy • Not proven to reduce mortality from CRC • Sampling error • Experience of local histologist • Low interobserver agreement for low-grade dysplasia • Not universally accepted guidelines
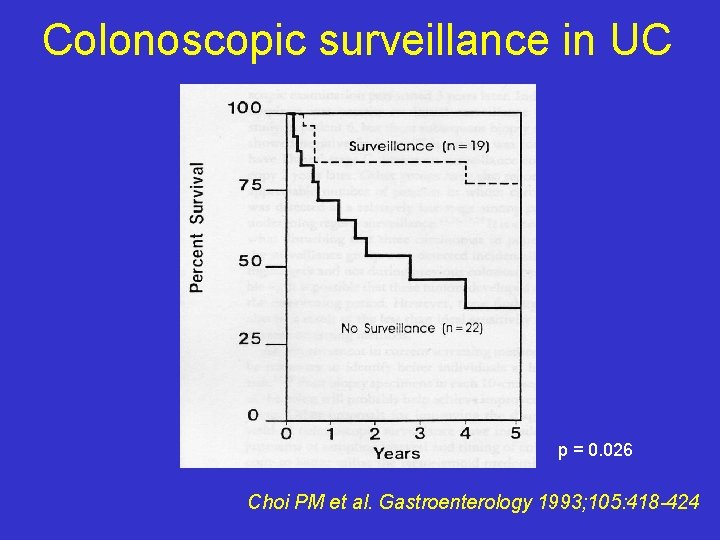
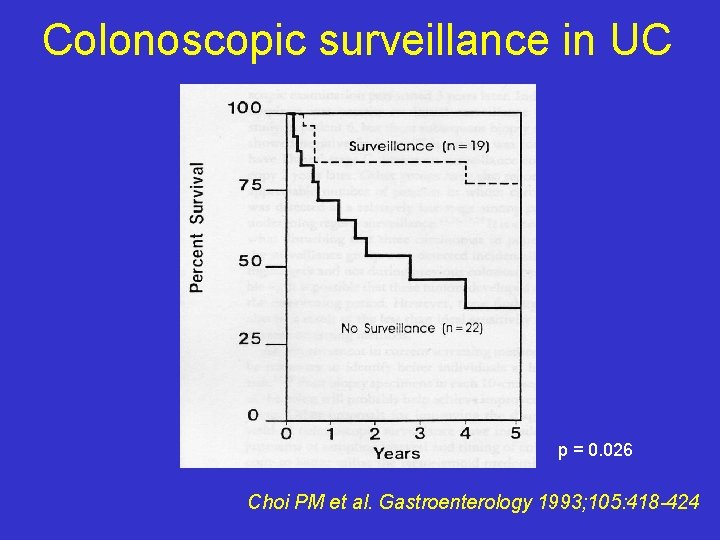
Colonoscopic surveillance in UC p = 0. 026 Choi PM et al. Gastroenterology 1993; 105: 418 -424
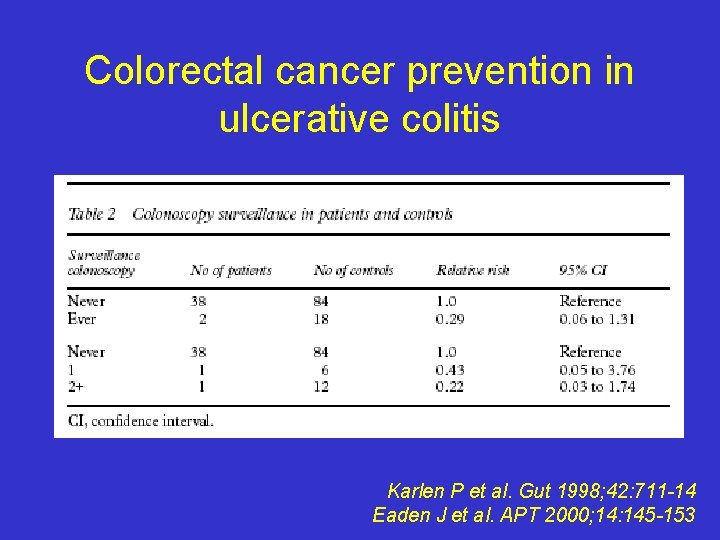
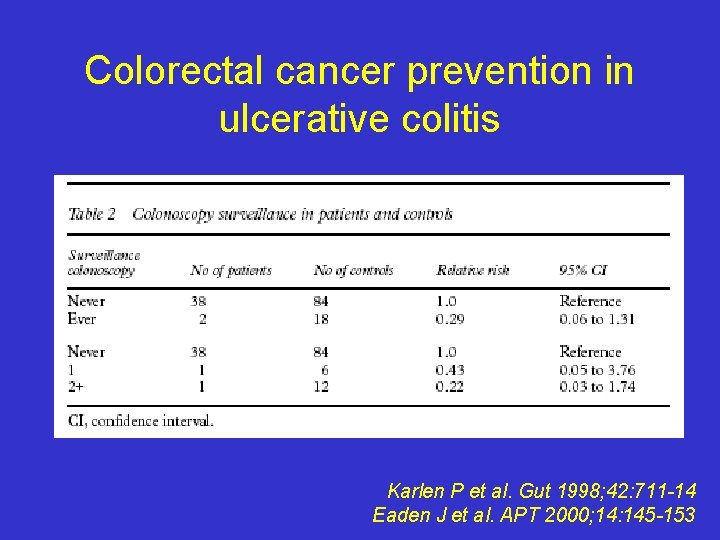
Colorectal cancer prevention in ulcerative colitis Karlen P et al. Gut 1998; 42: 711 -14 Eaden J et al. APT 2000; 14: 145 -153
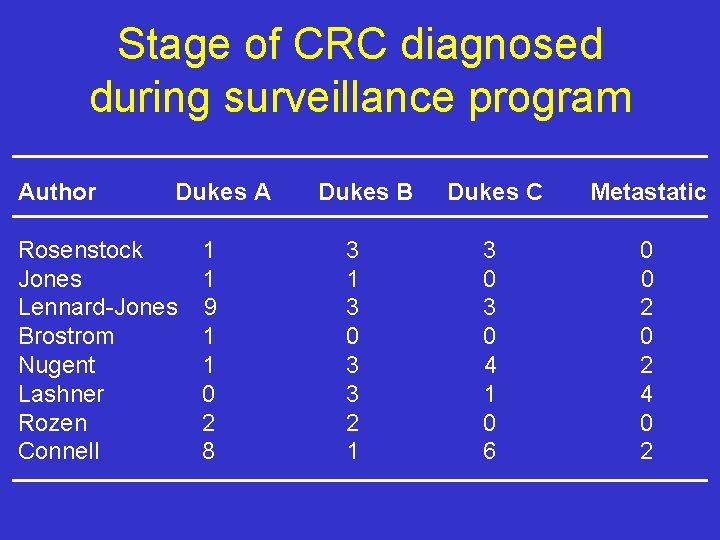
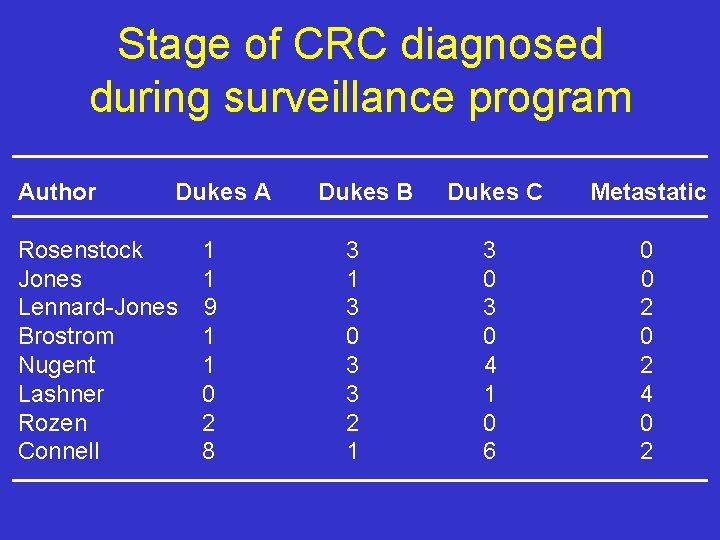
Stage of CRC diagnosed during surveillance program Author Dukes A Rosenstock Jones Lennard-Jones Brostrom Nugent Lashner Rozen Connell 1 1 9 1 1 0 2 8 Dukes B 3 1 3 0 3 3 2 1 Dukes C Metastatic 3 0 4 1 0 6 0 0 2 4 0 2
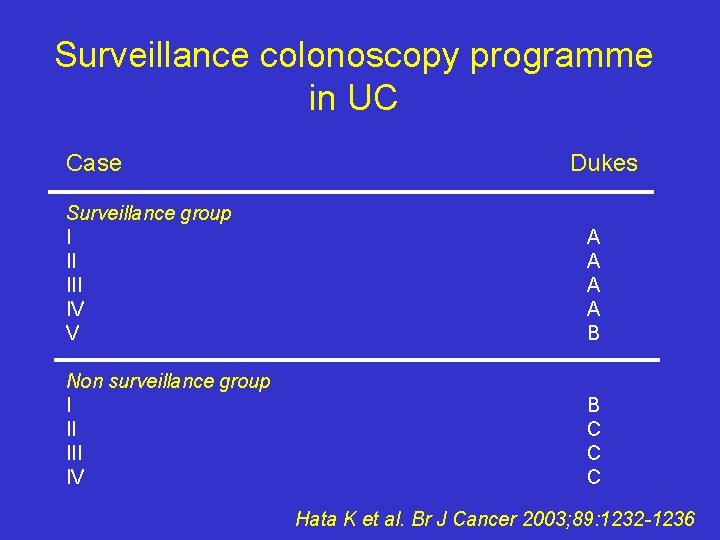
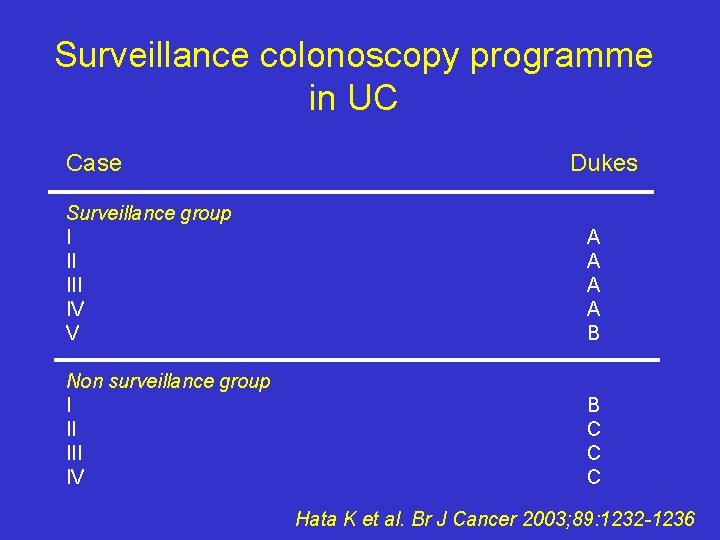
Surveillance colonoscopy programme in UC Case Dukes Surveillance group I II IV V A A B Non surveillance group I II IV B C C C Hata K et al. Br J Cancer 2003; 89: 1232 -1236
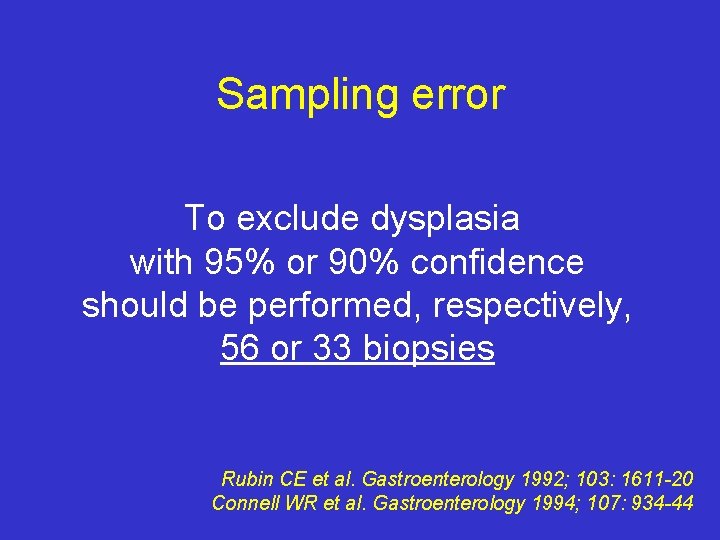
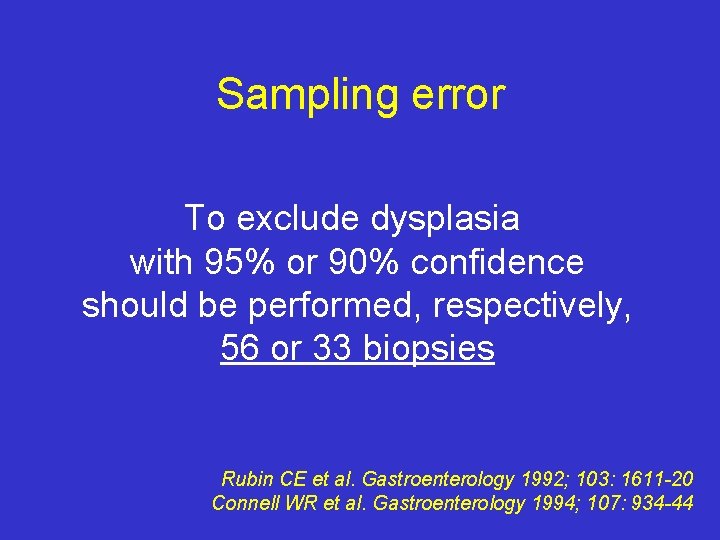
Sampling error To exclude dysplasia with 95% or 90% confidence should be performed, respectively, 56 or 33 biopsies Rubin CE et al. Gastroenterology 1992; 103: 1611 -20 Connell WR et al. Gastroenterology 1994; 107: 934 -44
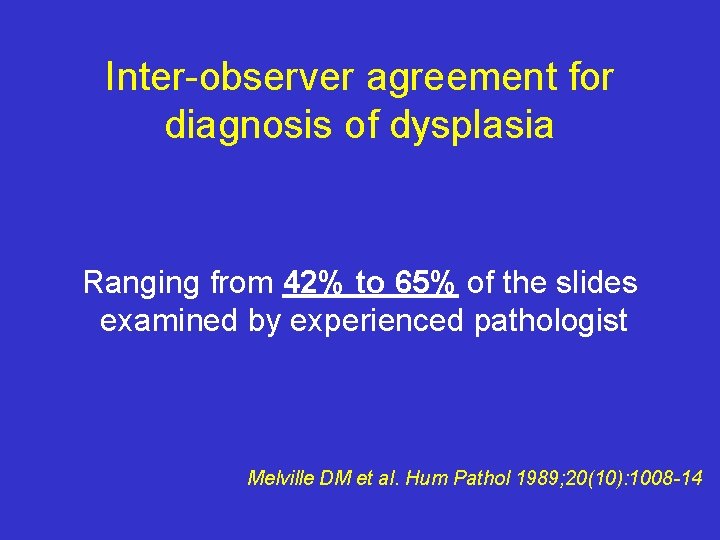
Inter-observer agreement for diagnosis of dysplasia Ranging from 42% to 65% of the slides examined by experienced pathologist Melville DM et al. Hum Pathol 1989; 20(10): 1008 -14
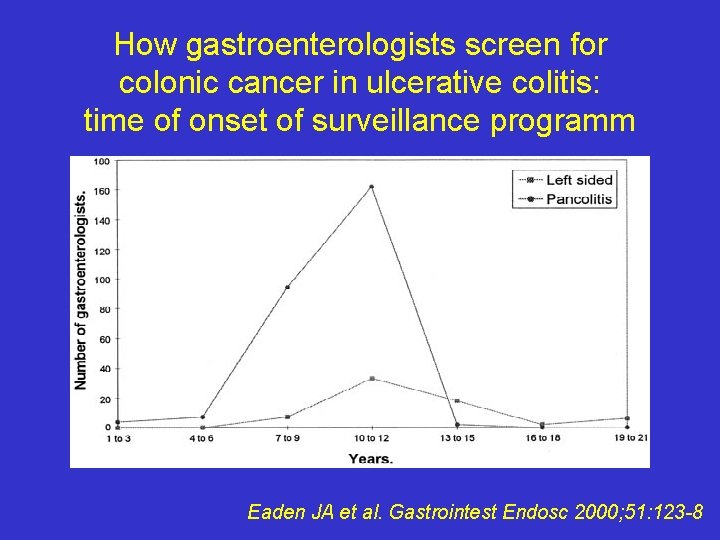
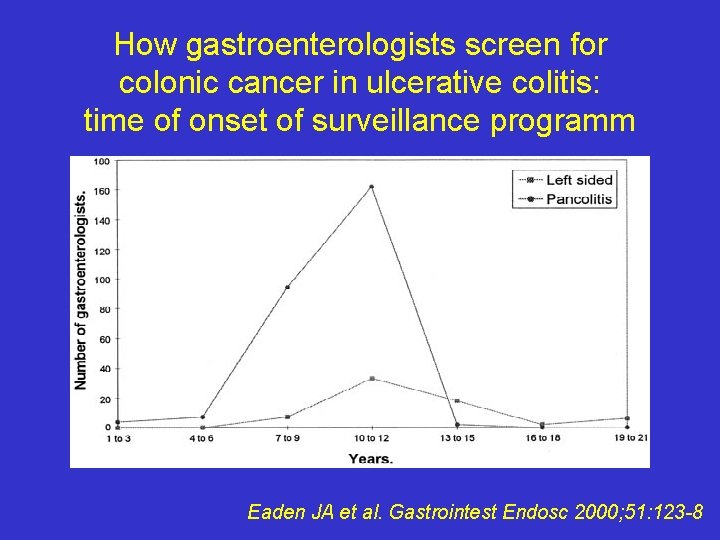
How gastroenterologists screen for colonic cancer in ulcerative colitis: time of onset of surveillance programm Eaden JA et al. Gastrointest Endosc 2000; 51: 123 -8
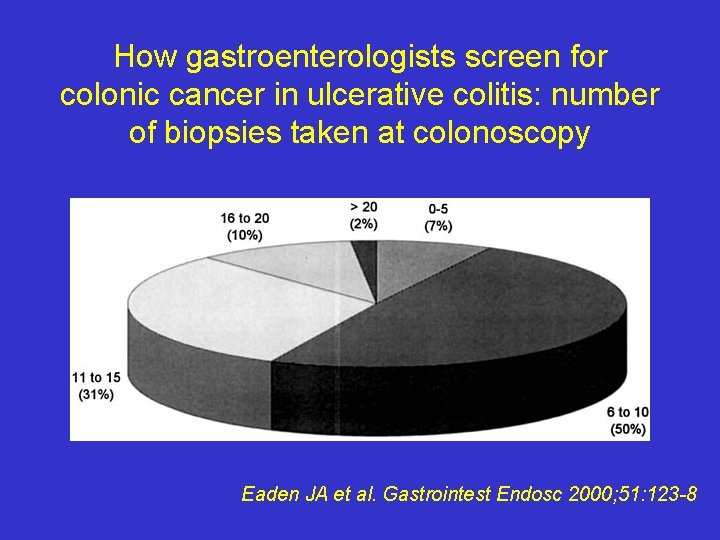
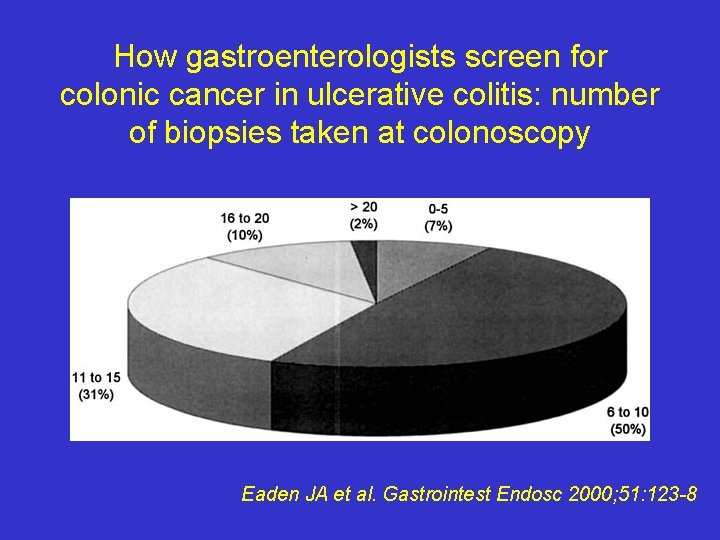
How gastroenterologists screen for colonic cancer in ulcerative colitis: number of biopsies taken at colonoscopy Eaden JA et al. Gastrointest Endosc 2000; 51: 123 -8
Guidelines for Colorectal Cancer Screening and Surveillance “Individuals with longstanding IBD (pancolitis for 8 or more years or, left-sided colitis for 15 or more years) may undergo colonoscopic surveillance with systematic biopsies every 1 -3 years… ALTHOUGH there is no direct evidence supporting this practice. ” Gastrointest Endosc 2000; 51(6): 777 -782
Clinical guidelines and rationale for CRC surveillance in patients with long-standing IBD • Surveillance every 1 -2 yrs after 8 yrs of disease in patients with pancolitis or after 15 yrs in those with left-sided colitis • Biopsy specimens should be taken every 10 cm in all 4 quadrants and that additional biopsies should be taken of strictures and mass lesions other than pseudopolyps. Polyps that appear potentially dysplastic can be removed by polypectomy with biopsy of adjacent flat mucosa to determine if dysplasia is present • No direct supporting evidence and no RCT of surveillance colonoscopy in patients with IBD Winawer S et al. Gastroenterology 2003; 124: 544 -560
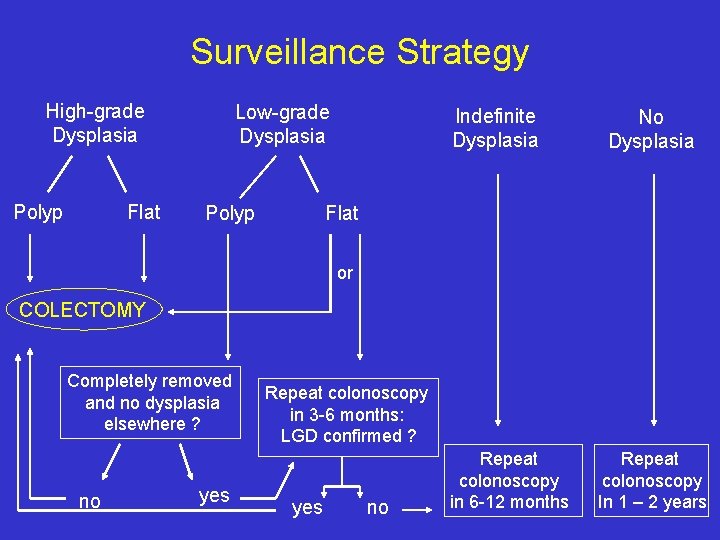
High-grade and Low-grade Dysplasia • Patients with high-grade dysplasia or multifocal low-grade dysplasia in flat mucosa – if confirmed by experienced pathologist – should be advised to undergo colectomy • Dysplasia-associated lesion or mass (DALMs) is a dysplastic mass lesion and is an indication for colectomy • Management of patients with unifocal low-grade dysplasia is still controversial and colectomy does not share the same consesus as high-grade or multifocal low-grade dysplasia Winawer S et al. Gastroenterology 2003; 124: 544 -560
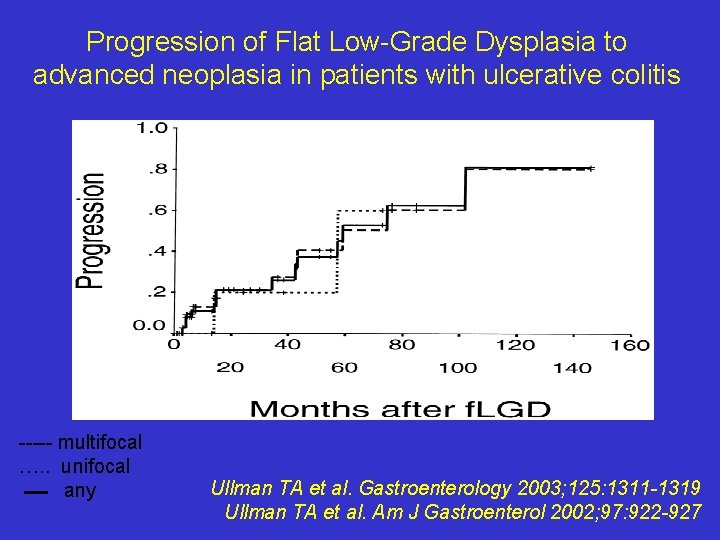
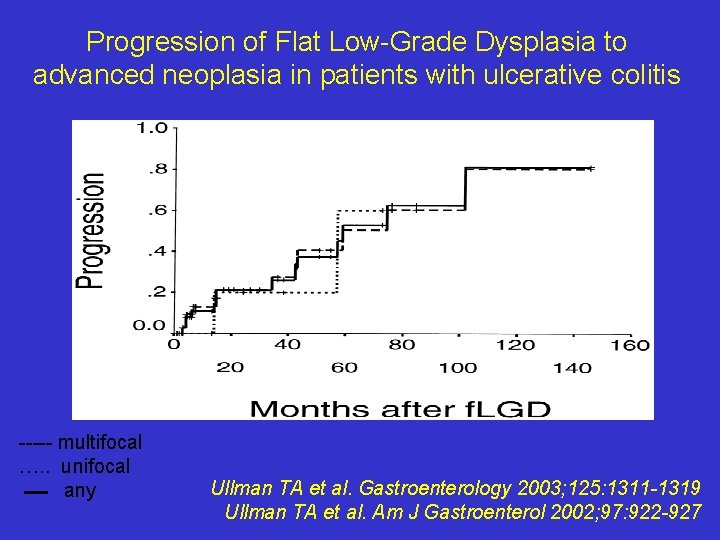
Progression of Flat Low-Grade Dysplasia to advanced neoplasia in patients with ulcerative colitis ----- multifocal …. . unifocal any Ullman TA et al. Gastroenterology 2003; 125: 1311 -1319 Ullman TA et al. Am J Gastroenterol 2002; 97: 922 -927
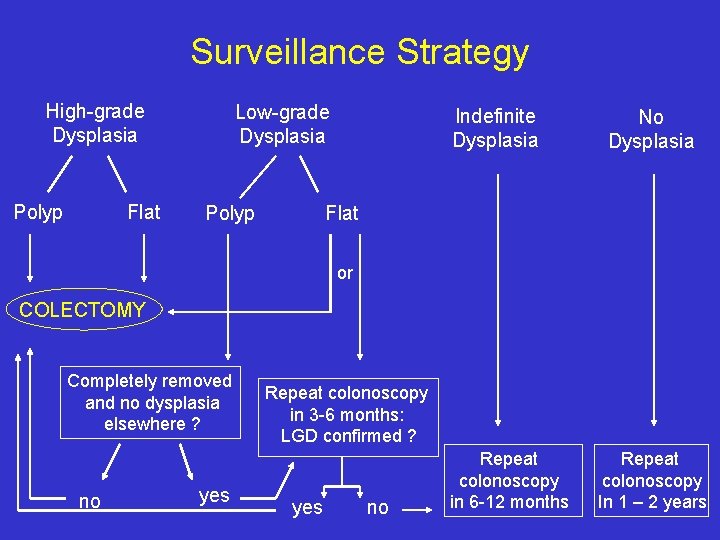
Surveillance Strategy High-grade Dysplasia Polyp Flat Low-grade Dysplasia Polyp Indefinite Dysplasia No Dysplasia Flat or COLECTOMY Completely removed and no dysplasia elsewhere ? no yes Repeat colonoscopy in 3 -6 months: LGD confirmed ? yes no Repeat colonoscopy in 6 -12 months Repeat colonoscopy In 1 – 2 years
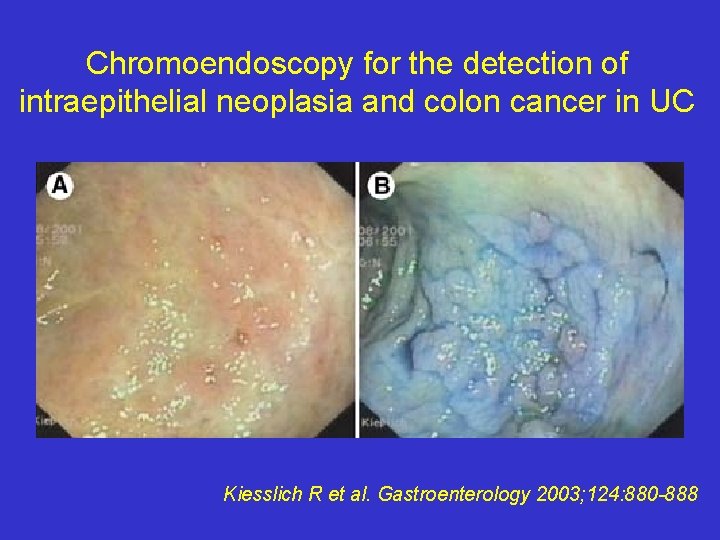
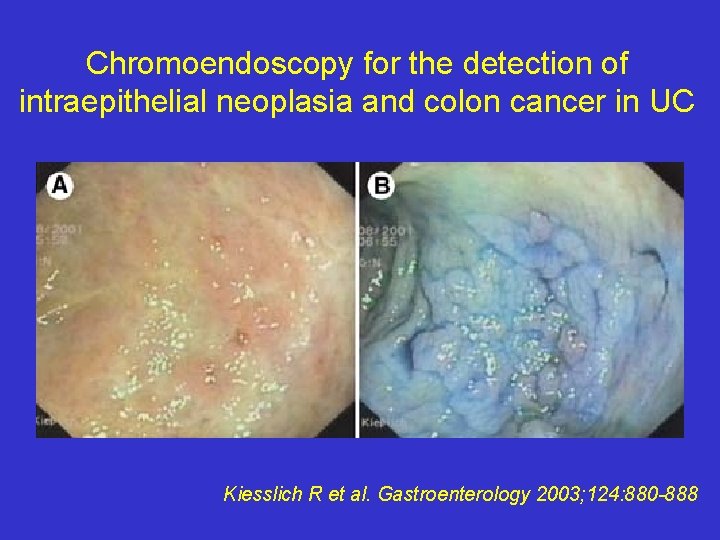
Chromoendoscopy for the detection of intraepithelial neoplasia and colon cancer in UC Kiesslich R et al. Gastroenterology 2003; 124: 880 -888
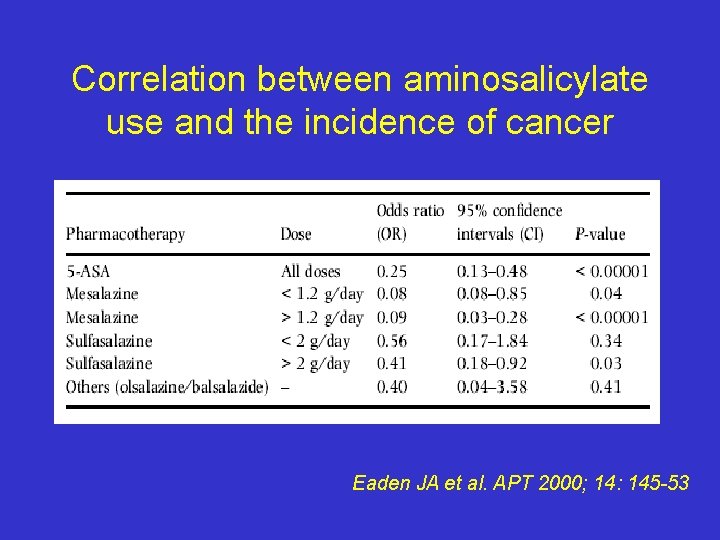
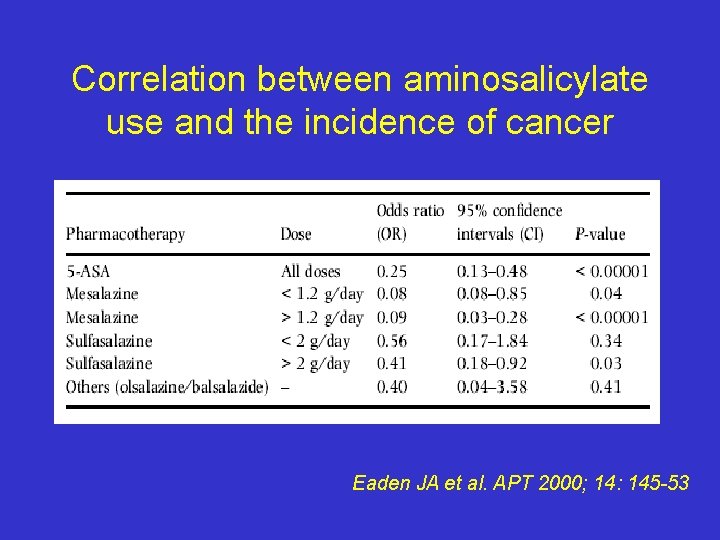
Correlation between aminosalicylate use and the incidence of cancer Eaden JA et al. APT 2000; 14: 145 -53
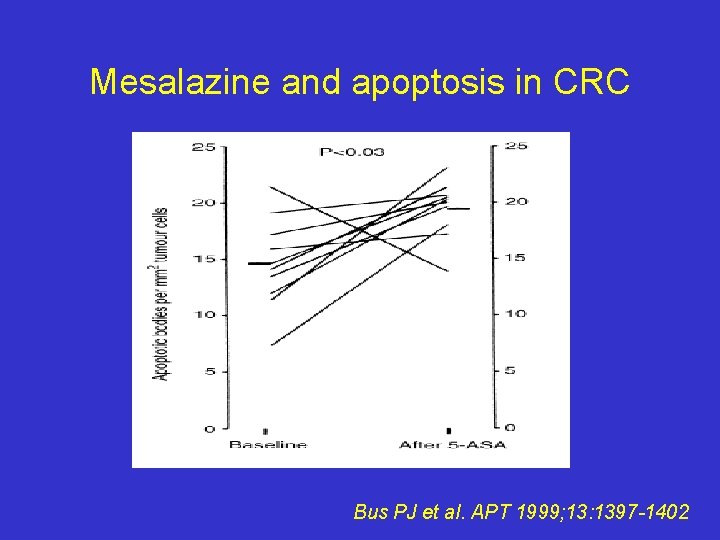
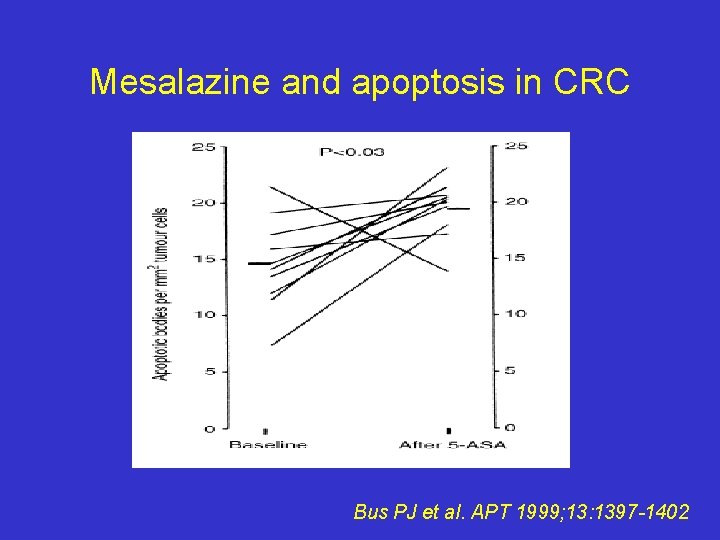
Mesalazine and apoptosis in CRC Bus PJ et al. APT 1999; 13: 1397 -1402
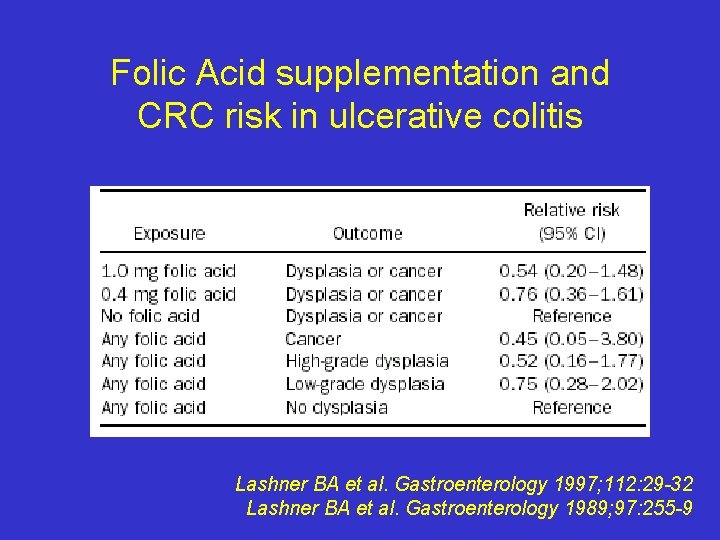
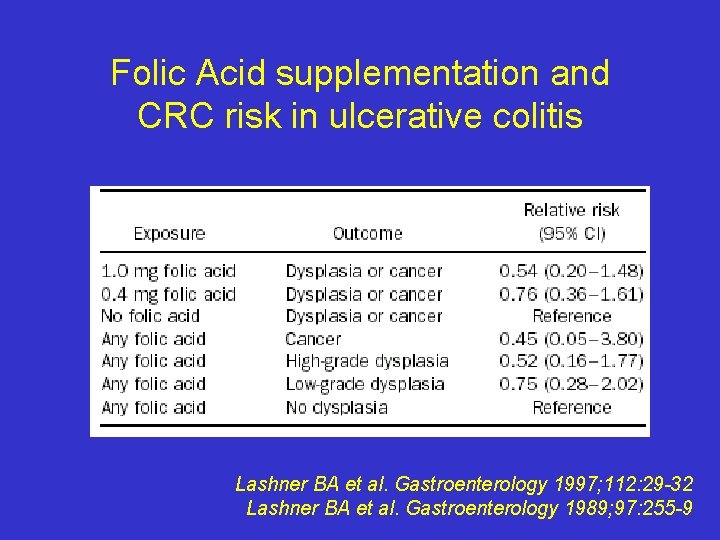
Folic Acid supplementation and CRC risk in ulcerative colitis Lashner BA et al. Gastroenterology 1997; 112: 29 -32 Lashner BA et al. Gastroenterology 1989; 97: 255 -9
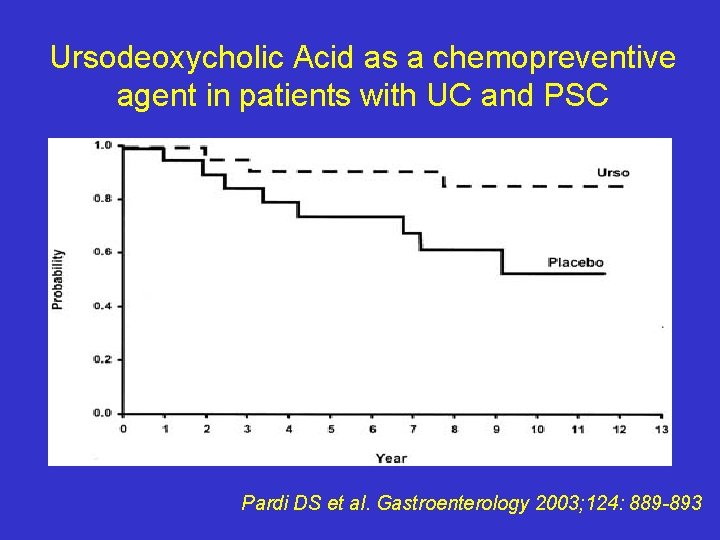
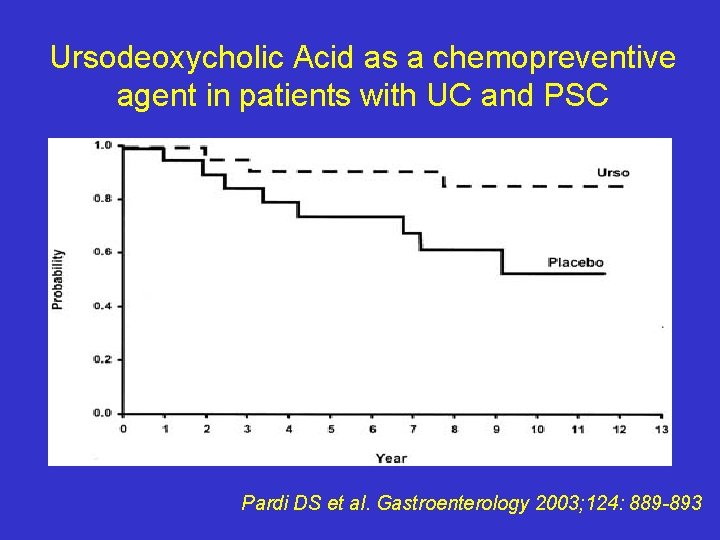
Ursodeoxycholic Acid as a chemopreventive agent in patients with UC and PSC Pardi DS et al. Gastroenterology 2003; 124: 889 -893
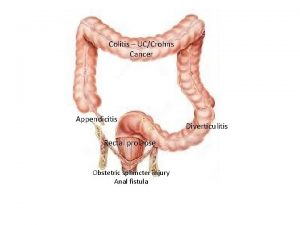
Conclusions • CRC is an important complication of long standing UC/CD colitis • Surveillance colonoscopy probably beneficial, even though not fully evidence-based • Aminosalicylates, ursodiol, folate supplemantation may contribute to a reduction of CRC incidence or mortality
 Ddsep 8
Ddsep 8 Ulcerative colitis crohn's disease
Ulcerative colitis crohn's disease Lymfocytær colitis
Lymfocytær colitis Ulcerative colitis treatment
Ulcerative colitis treatment Vsiblin
Vsiblin Hemicolitis
Hemicolitis Bilharzial colitis
Bilharzial colitis Inflammatory bowel disease
Inflammatory bowel disease Oligoartriitti
Oligoartriitti Andrew grossman md
Andrew grossman md Ulcerative colitis
Ulcerative colitis Appendcolith
Appendcolith Mayo 1 ulcerative colitis
Mayo 1 ulcerative colitis Ulcerative colitis hla
Ulcerative colitis hla Seesile
Seesile Colitis diet
Colitis diet Filgotinib ulcerative colitis
Filgotinib ulcerative colitis Ilness script
Ilness script Brfss texas
Brfss texas Risk factors of head and neck cancer
Risk factors of head and neck cancer Personal care products and cancer risk
Personal care products and cancer risk Market risk credit risk operational risk
Market risk credit risk operational risk Risk factors of cancer
Risk factors of cancer Tyrer-cuzick score chart
Tyrer-cuzick score chart Breast cancer risk
Breast cancer risk Lifetime risk of lung cancer
Lifetime risk of lung cancer Continuous analysis and surveillance system
Continuous analysis and surveillance system Reconnaissance and surveillance leaders course
Reconnaissance and surveillance leaders course Types of undercover assignment
Types of undercover assignment Regulatory agencies
Regulatory agencies Who rsv surveillance
Who rsv surveillance Surveillance post opératoire
Surveillance post opératoire Types of surveillance
Types of surveillance Fixateur externe risque
Fixateur externe risque Primary surveillance radar (psr)
Primary surveillance radar (psr)