Skin Cancer Skin Cancer What is Cancer l















- Slides: 58

Skin Cancer
Skin Cancer
What is Cancer? l l Changes to the DNA of a cell (mutations) lead to cellular damage Mutations enable cancer cells to divide continuously, without the need for normal signals In some cancers the unchecked growth results in a mass, called a tumor Cancerous cells may invade other parts of the body interfering with normal body functions

What is Cancer? l l l Although cancer is often referred to as if it were a single disease, it is really a diverse group of diseases that affects many different organs and cell types The likelihood of developing any particular cancer depends on an individual’s genetics, environment, and lifestyle. The occurrence of some cancers may be prevented/reduced by wise lifestyle choices.
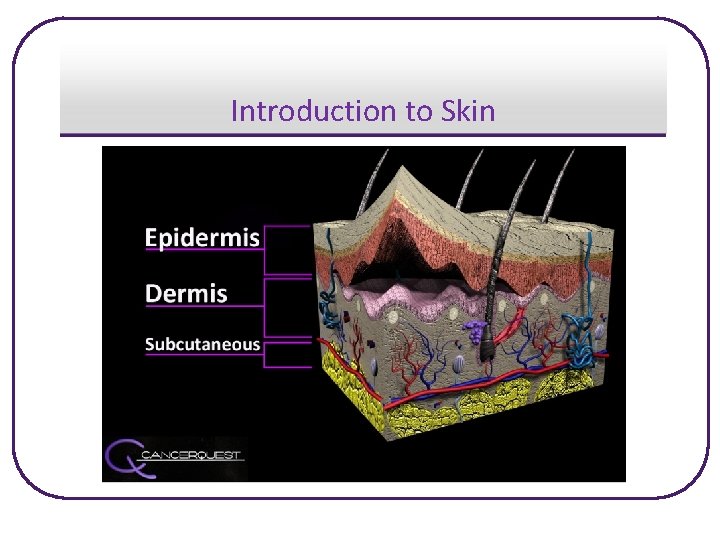
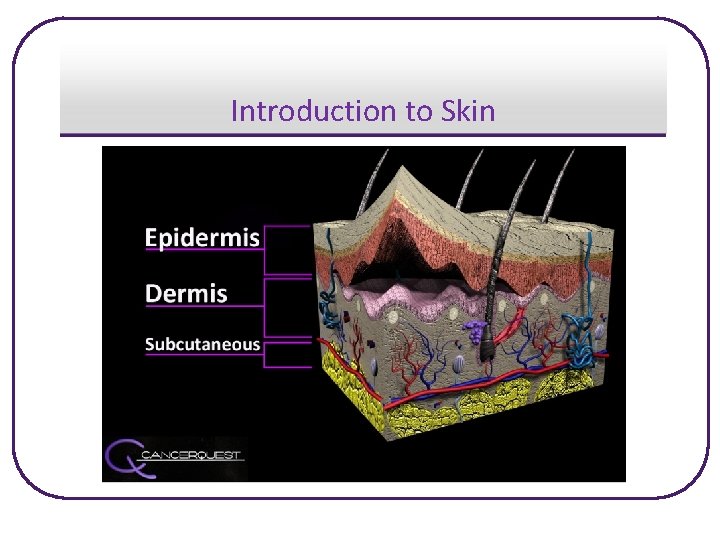
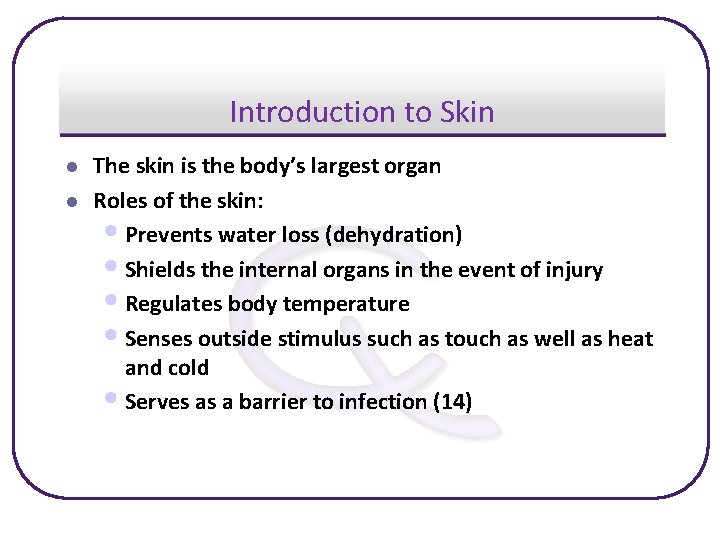
Introduction to Skin
Introduction to Skin l l The skin is the body’s largest organ Roles of the skin: • Prevents water loss (dehydration) • Shields the internal organs in the event of injury • Regulates body temperature • Senses outside stimulus such as touch as well as heat and cold • Serves as a barrier to infection (14)
Skin Cancer l Basics • An abnormal change in the skin resulting from uncontrolled • cellular growth There are three main types of skin cancer: » Basal Cell Carcinoma (BCC) » Squamous Cell Carcinoma (SCC) » Melanoma

Skin Cancer Statistics l Statistics (7) • According to the American Cancer Society skin cancer is the • • most common cancer in the United States, with over 1 million cases diagnosed per year. Over 10, 000 deaths estimated yearly in the U. S. Survival rates are very good when skin cancer is detected early » 5 year survival rates: Localized melanoma – 99% Regional melanoma – 65% Distant melanoma – 15%
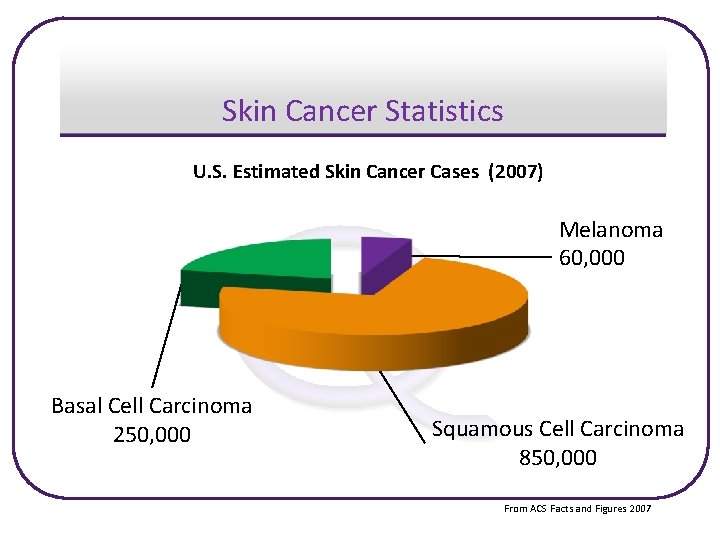
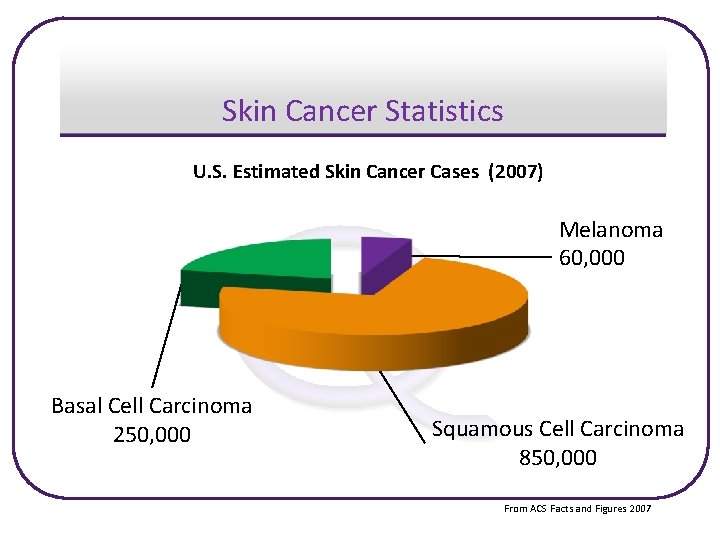
Skin Cancer Statistics U. S. Estimated Skin Cancer Cases (2007) Melanoma 60, 000 Basal Cell Carcinoma 250, 000 Squamous Cell Carcinoma 850, 000 From ACS Facts and Figures 2007
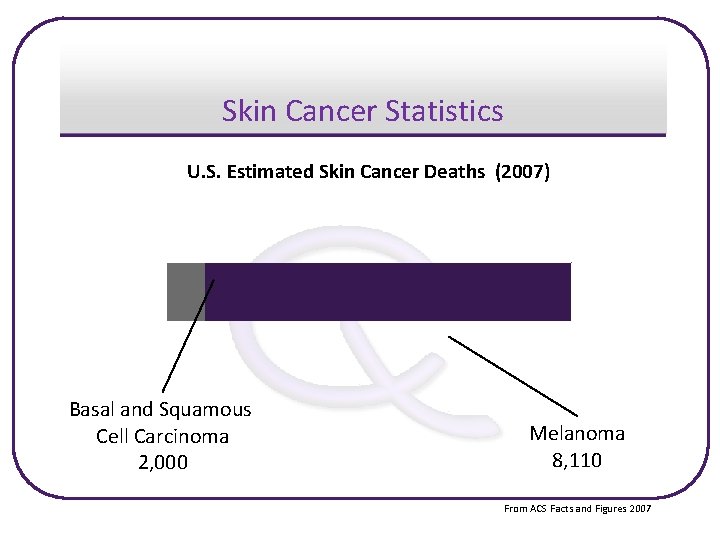
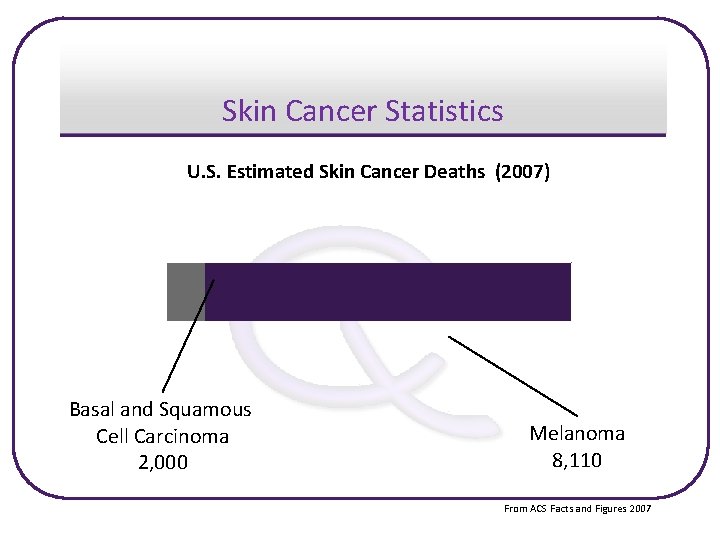
Skin Cancer Statistics U. S. Estimated Skin Cancer Deaths (2007) Basal and Squamous Cell Carcinoma 2, 000 Melanoma 8, 110 From ACS Facts and Figures 2007
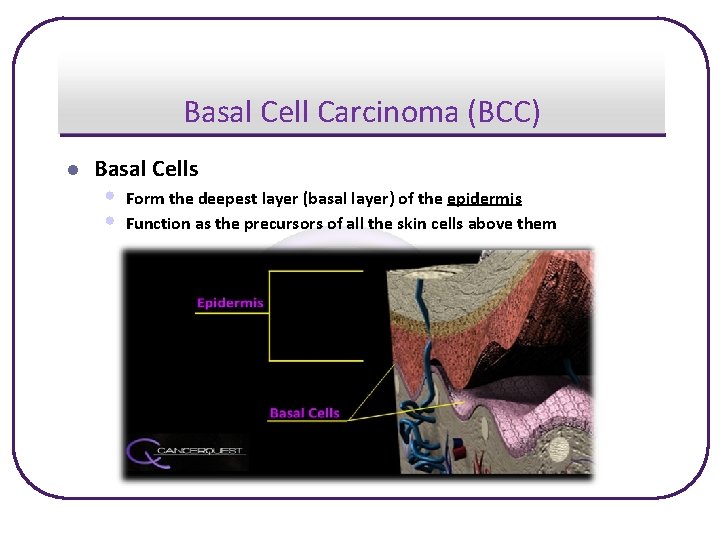
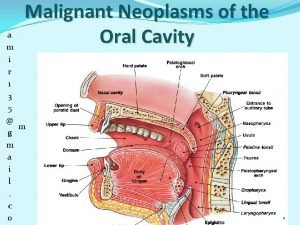
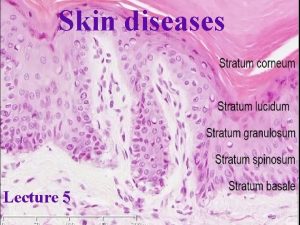
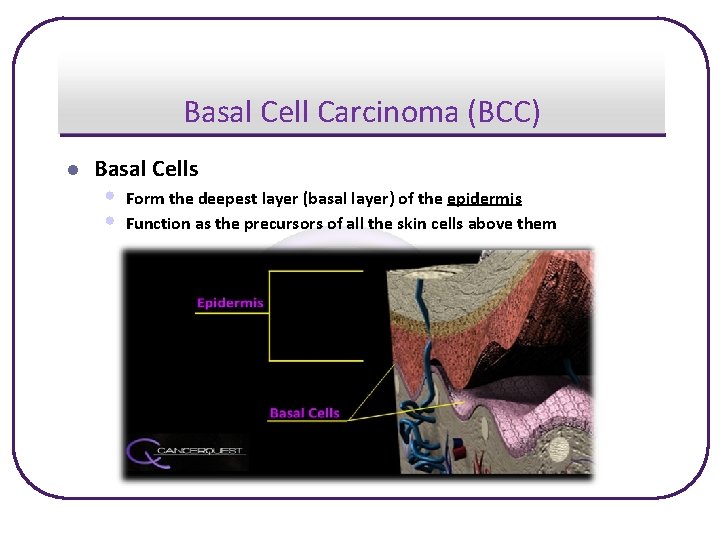
Basal Cell Carcinoma (BCC) l Basal Cells • • Form the deepest layer (basal layer) of the epidermis Function as the precursors of all the skin cells above them
Basal Cell Carcinoma (BCC) l About BCC • Least dangerous of the skin cancers, grows slowly, and rarely • • l spreads beyond original location Easily detected and treated Though seldom life-threatening, if untreated it can grow beneath the skin into underlying tissue and bone causing serious damage Statistics • Most common skin cancer • Estimated 800, 000 to 900, 000 people diagnosed yearly • One out of every three cancers diagnosed is BCC (7)
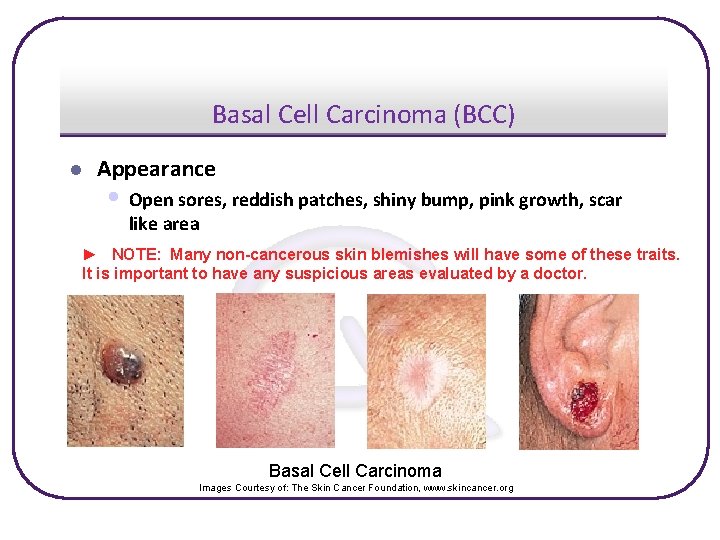
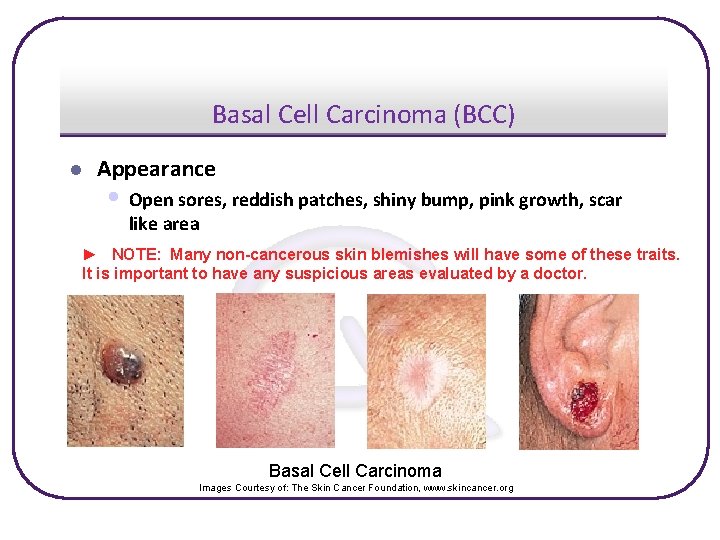
Basal Cell Carcinoma (BCC) l Appearance • Open sores, reddish patches, shiny bump, pink growth, scar like area ► NOTE: Many non-cancerous skin blemishes will have some of these traits. It is important to have any suspicious areas evaluated by a doctor. Basal Cell Carcinoma Images Courtesy of: The Skin Cancer Foundation, www. skincancer. org
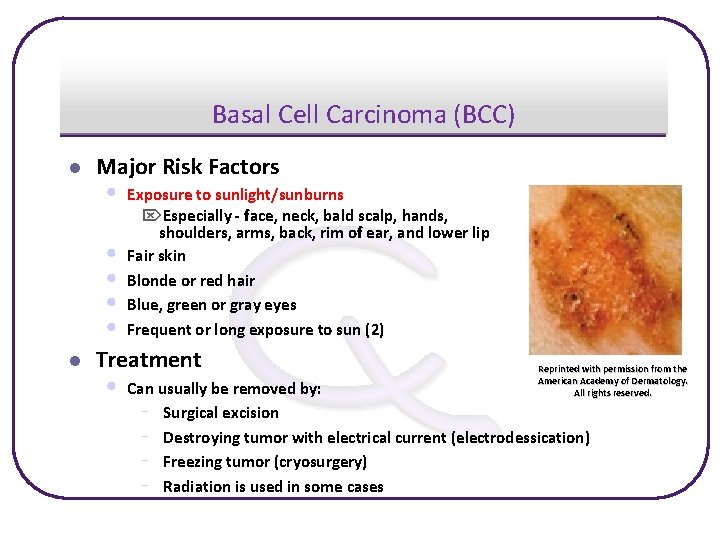
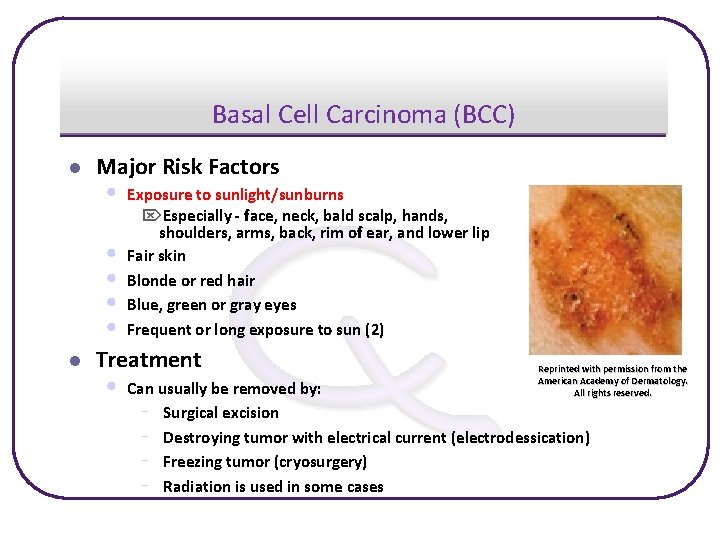
Basal Cell Carcinoma (BCC) l Major Risk Factors • • • l Exposure to sunlight/sunburns Especially - face, neck, bald scalp, hands, shoulders, arms, back, rim of ear, and lower lip Fair skin Blonde or red hair Blue, green or gray eyes Frequent or long exposure to sun (2) Treatment • Reprinted with permission from the American Academy of Dermatology. All rights reserved. Can usually be removed by: - Surgical excision - Destroying tumor with electrical current (electrodessication) - Freezing tumor (cryosurgery) - Radiation is used in some cases
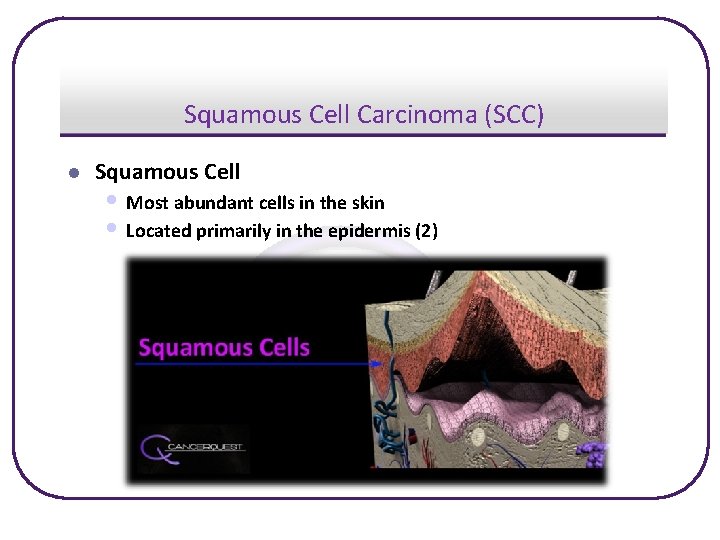
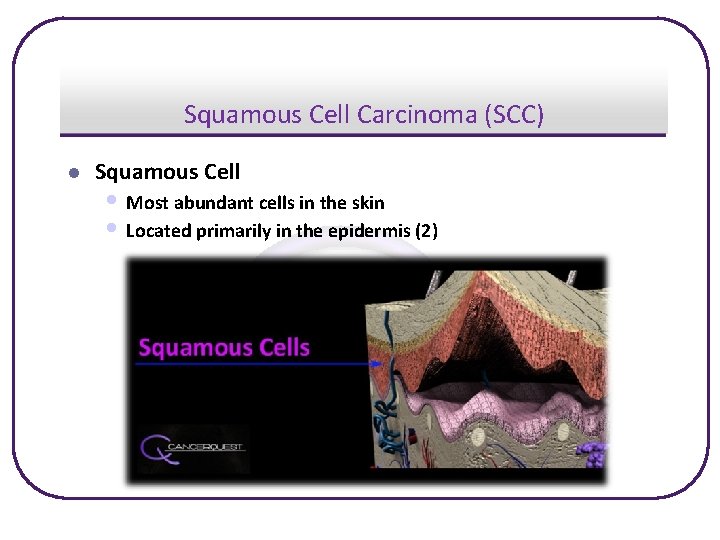
Squamous Cell Carcinoma (SCC) l Squamous Cell • Most abundant cells in the skin • Located primarily in the epidermis (2)
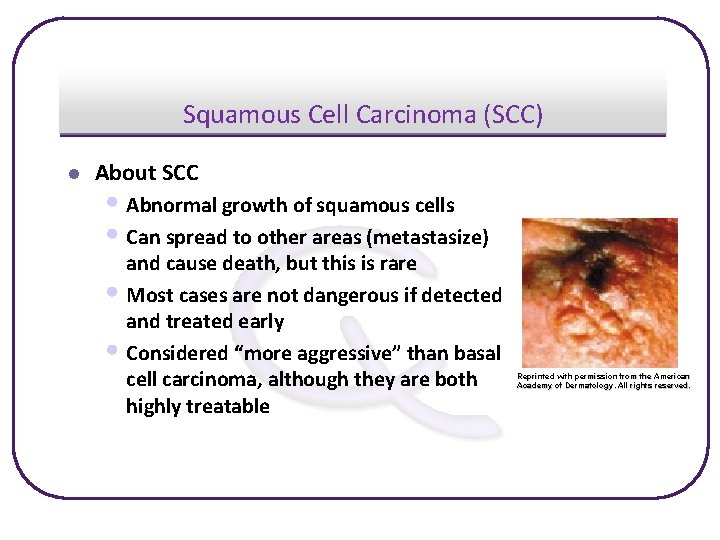
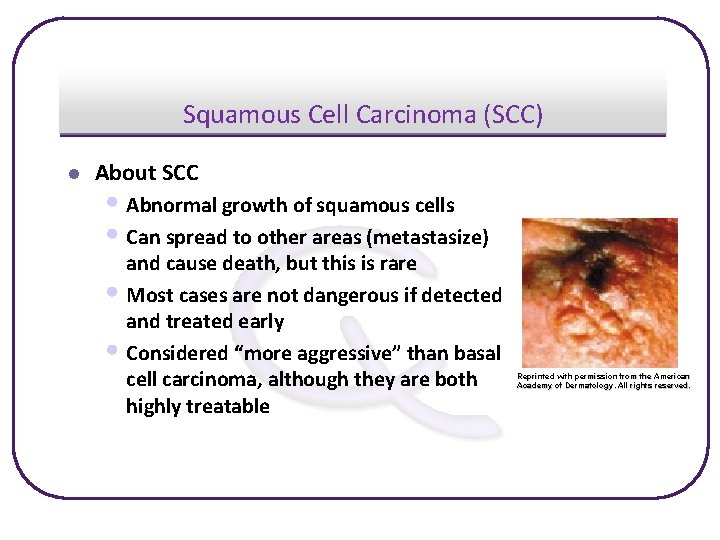
Squamous Cell Carcinoma (SCC) l About SCC • Abnormal growth of squamous cells • Can spread to other areas (metastasize) and cause death, but this is rare • Most cases are not dangerous if detected and treated early • Considered “more aggressive” than basal cell carcinoma, although they are both highly treatable Reprinted with permission from the American Academy of Dermatology. All rights reserved.
Squamous Cell Carcinoma (SCC) l Statistics for U. S. • Estimated 200, 000 to 300, 000 people diagnosed yearly • Second most common cancer diagnosed • 1, 000 – 2, 000 deaths yearly • Most cases are easily cured when caught early (7)
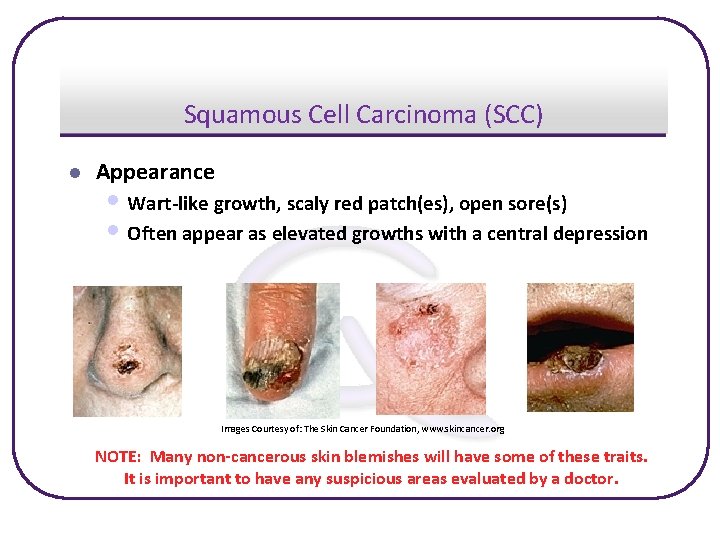
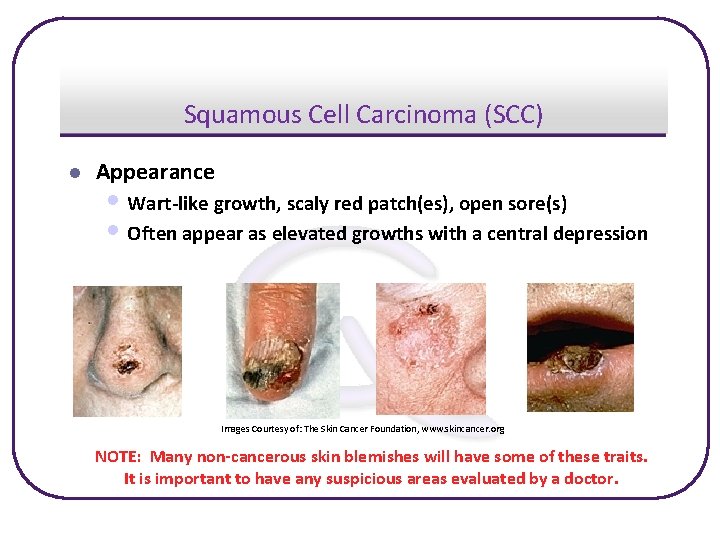
Squamous Cell Carcinoma (SCC) l Appearance • Wart-like growth, scaly red patch(es), open sore(s) • Often appear as elevated growths with a central depression Images Courtesy of: The Skin Cancer Foundation, www. skincancer. org NOTE: Many non-cancerous skin blemishes will have some of these traits. It is important to have any suspicious areas evaluated by a doctor.
Squamous Cell Carcinoma (SCC) l Major Risk Factors • • • l Exposure to sunlight/sunburns Especially - face, neck, bald scalp, hands, shoulders, arms, back, rim of ear, and the lower lip Fair skin Blonde or red hair Blue, green or gray eyes Frequent or long exposure to sun (2) Treatment • Can usually be removed by: - Surgical excision - Destroying tumor with electrical current (electrodessication) - Freezing tumor (cryosurgery) - Radiation is used in some cases
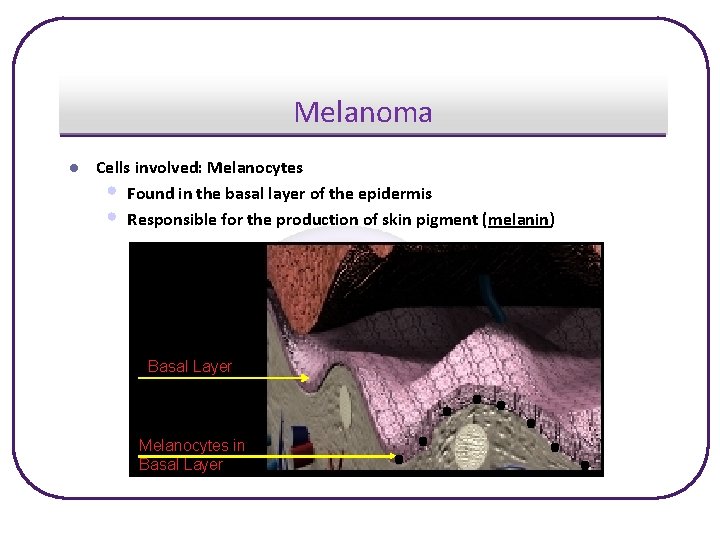
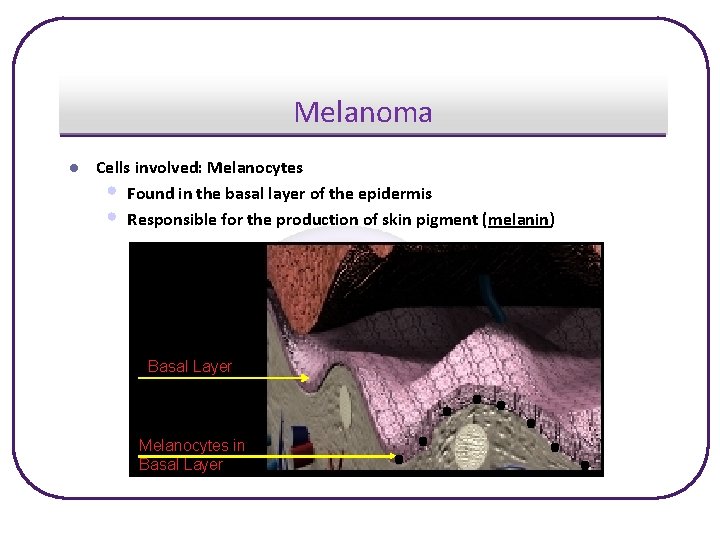
Melanoma l Cells involved: Melanocytes • Found in the basal layer of the epidermis • Responsible for the production of skin pigment (melanin) Basal Layer Melanocytes in Basal Layer
Melanoma l Statistics in the U. S. • Responsible for 75% of deaths due to skin cancer • Estimated over 60, 000 people diagnosed in 2007 • Highest death rate of all skin cancers • One American dies of melanoma almost every hour • Melanoma is the third most common cancer in • women aged 20 - 39 Estimated 8, 110 deaths in 2007 (7)
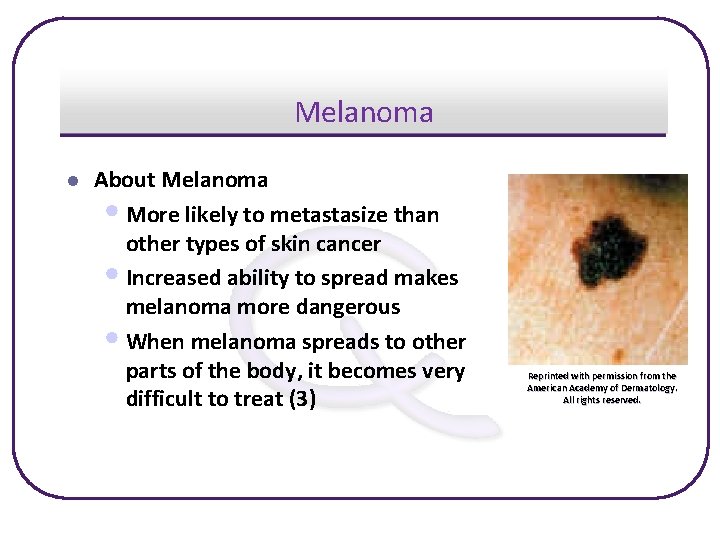
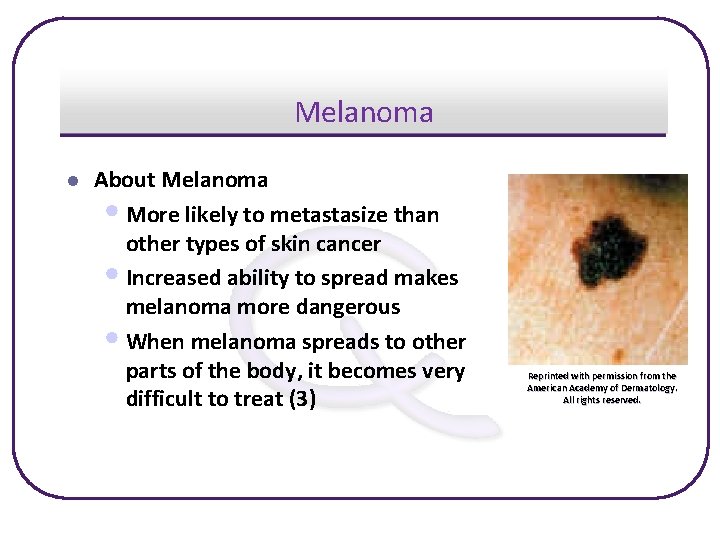
Melanoma l About Melanoma • More likely to metastasize than other types of skin cancer • Increased ability to spread makes melanoma more dangerous • When melanoma spreads to other parts of the body, it becomes very difficult to treat (3) Reprinted with permission from the American Academy of Dermatology. All rights reserved.
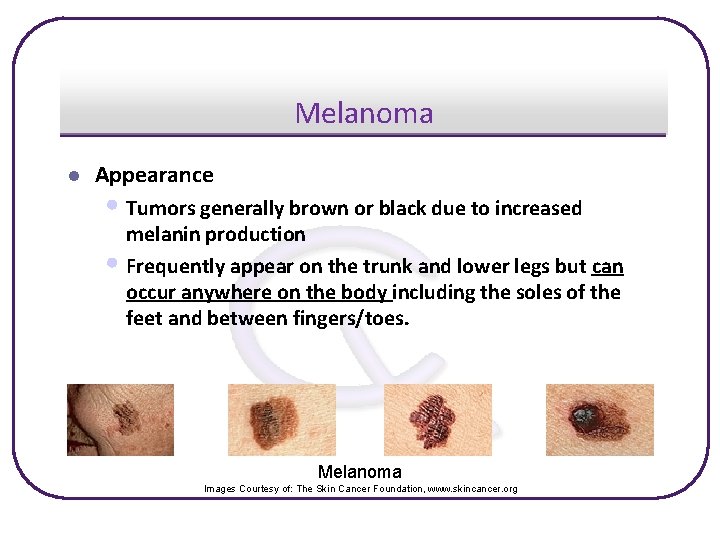
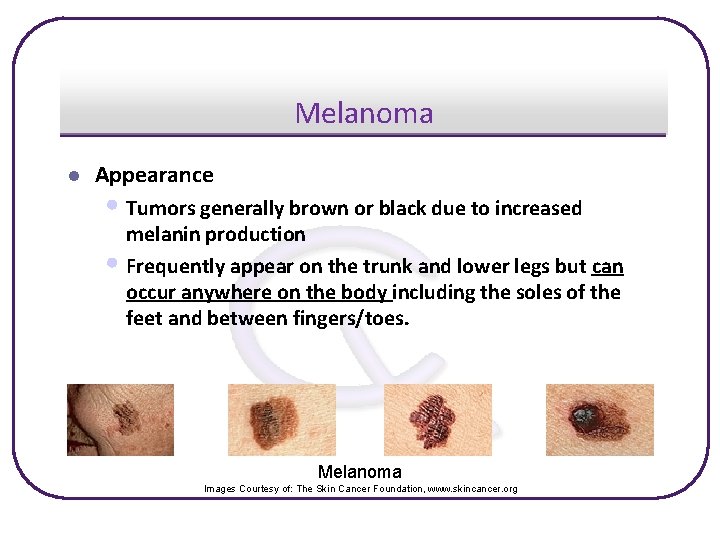
Melanoma l Appearance • Tumors generally brown or black due to increased melanin production • Frequently appear on the trunk and lower legs but can occur anywhere on the body including the soles of the feet and between fingers/toes. Melanoma Images Courtesy of: The Skin Cancer Foundation, www. skincancer. org
Melanoma l Treatment • Surgical removal of the primary tumor • Removal of surrounding tissue for staging purposes • Removal and examination of any additional suspicious growths • Chemotherapy and radiation may be used in advanced cases • Biological treatments including interleukin 2 (IL-2) • Investigational treatments

Melanoma l Major Risk Factors l Other Risk Factors • Exposure to ultraviolet radiation » Sun » Tanning Lamps • No ethnic group is immune to skin cancer • Blonde or red hair – blue, green, or gray eyes • People with more moles are at a higher risk • Family and personal history of melanoma • Fair complexion Image courtesy of NASA

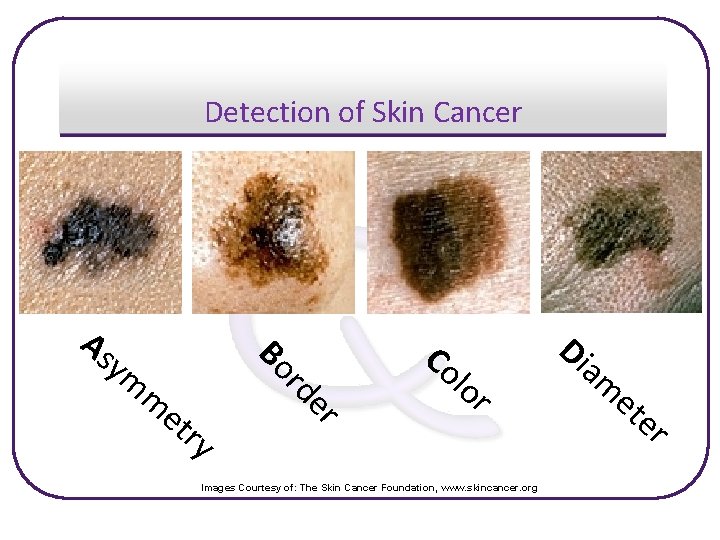
Detection of Skin Cancer l ABCDE’s of Skin Cancer (3) • These are the general characteristics used to identify skin growths of possible concern ü A – asymmetry – one half doesn’t look like the other ü B – border – irregular, ragged or blurred edges ü C – color – a mixture of colors or marks that change color ü D – diameter – a growth more than 6 millimeters across ü E – evolution – changes in shape, size or color » Note that not every skin cancer will have all of the following characteristics. Medical advice should be sought for any suspicious area or when an existing mark has a change in appearance
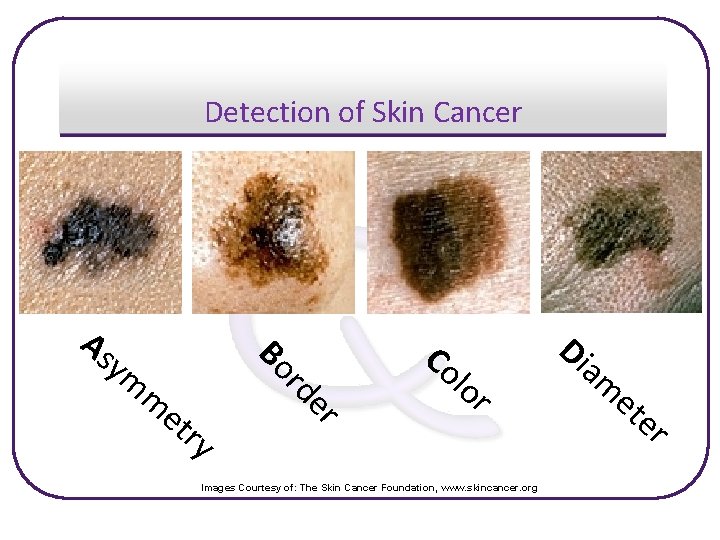
Detection of Skin Cancer er et ry rd m Bo As ym Co lo r Images Courtesy of: The Skin Cancer Foundation, www. skincancer. org Di am et er

Know the Flow: Melanoma

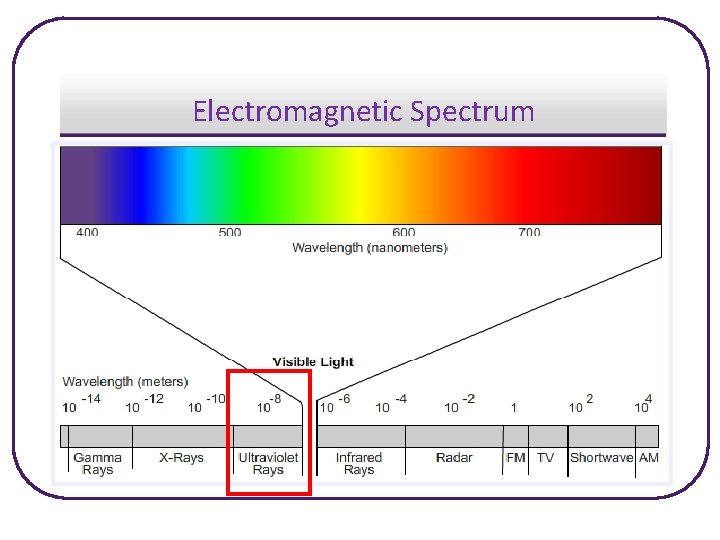
The Big Risk: Ultraviolet (UV) Radiation l Understanding UV Radiation • The nuclear reactions that fuel the sun and other stars release • • • an enormous amount of energy This energy is emitted as radiation of several kinds, including visible light and the heat that warms the earth UV light is a type of high energy (short wavelength) radiation that is produced by the sun There are three types of UV radiation: UVA, UVB, UVC UV RADIATION IS THE MAIN CAUSE OF SKIN CANCER
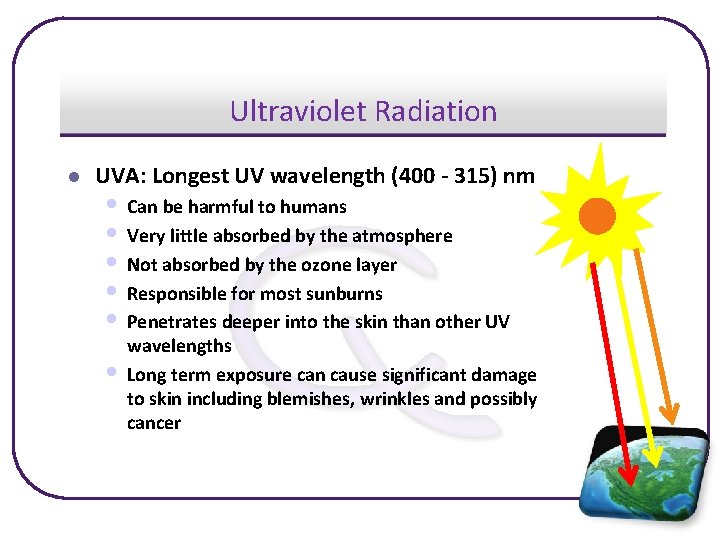
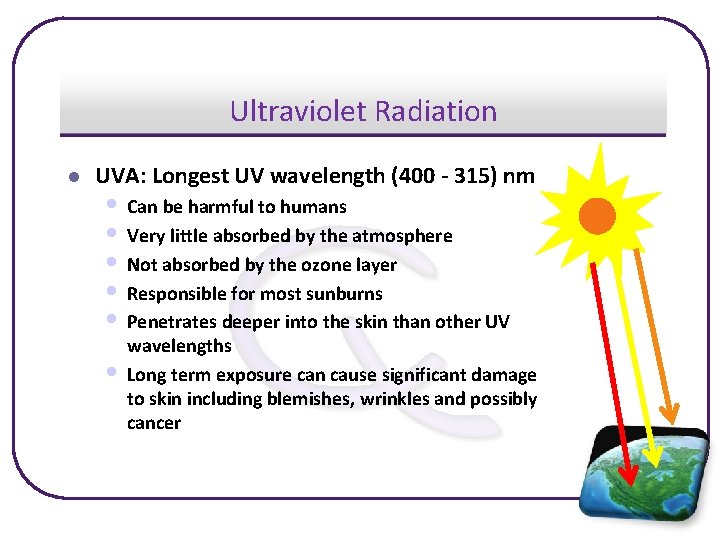
Ultraviolet Radiation l UVA: Longest UV wavelength (400 - 315) nm • Can be harmful to humans • Very little absorbed by the atmosphere • Not absorbed by the ozone layer • Responsible for most sunburns • Penetrates deeper into the skin than other UV • wavelengths Long term exposure can cause significant damage to skin including blemishes, wrinkles and possibly cancer
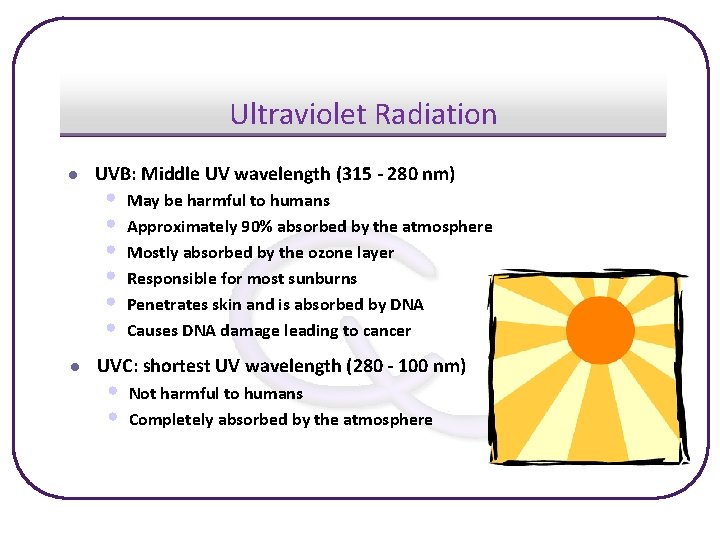
Ultraviolet Radiation l l UVB: Middle UV wavelength (315 - 280 nm) • • • May be harmful to humans Approximately 90% absorbed by the atmosphere Mostly absorbed by the ozone layer Responsible for most sunburns Penetrates skin and is absorbed by DNA Causes DNA damage leading to cancer UVC: shortest UV wavelength (280 - 100 nm) • • Not harmful to humans Completely absorbed by the atmosphere
Ultraviolet Radiation l Other bad things from UV radiation • • Immune System Suppression (17) • • Impairs the body’s ability to fight disease May activate viruses already in skin Can promote cancers and worsen infectious diseases caused by bacteria Research is ongoing to discover more Eye Disorders (20) • • • Cataracts Cancer of skin surrounding the eyes Burns caused by overexposure to UV light Macular degeneration: damage to the central part of the retina Pterygium: non-cancerous growth on the corner of the eye that can partially block vision
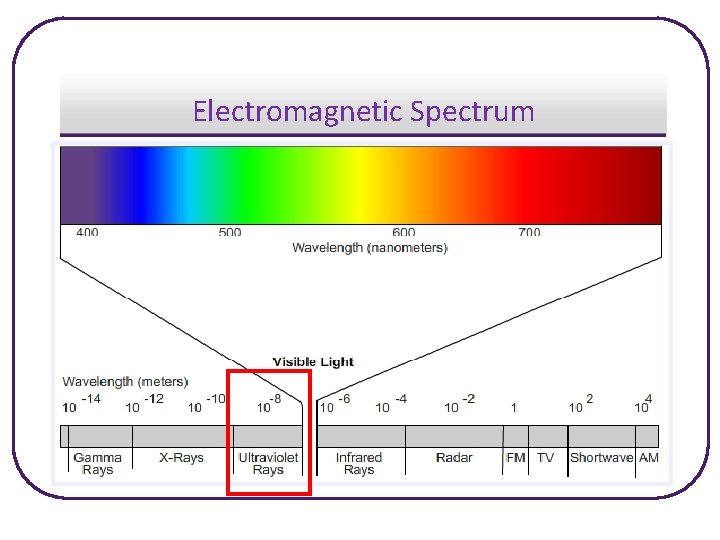
Electromagnetic Spectrum
Solar Radiation and the Earth’s Atmosphere
The Sun and You l Benefits of the SUN • The sun triggers Vitamin D synthesis, which is good for the body • Only SMALL amounts of sunlight are needed (10 -15 minutes; • NOT a suntan) Vitamin D is found in foods such as eggs, fish, and cheese Vitamin D

SA f NA o y rtes cou ge Ima Prevention American Cancer Society Recommendation “Slip! Slop! Slap! Wrap!” Slip on a shirt, Slop on 15 SPF (or higher) sunscreen, Slap on a hat, Wrap on sunglasses before any exposure to the sun. * From ACS Skin Cancer Fact Sheet 2006
Prevention l Limiting Exposure • The sun’s UV rays are the strongest between 10 a. m. and 4 p. m. , • • limit exposure to the sun during these hours if possible Exposure varies with times of the year and areas of the world Sunny seasons provide the most UV exposure
Prevention: Sunscreen l Reducing Risk While Being Exposed • • • SUNSCREEN! Your personal ozone layer! Blocks most UV radiation, although not all of it Different SPF numbers (Sun Protection Factors) SPF 15, 30, 45, etc. The higher SPF equals a longer period of protection Sunscreen wears off, so it must be reapplied every few hours…especially when sweating, swimming, or toweling off
Prevention l “Most people benefit from sunscreens with sun protection factor (SPF) numbers of 15 or more. The SPF number gives you some idea of how long you can stay in the sun without burning. For example, if you burn in 10 minutes without sunscreen and you apply a liberal dose with a SPF number of 15, you should be protected from sunburn for 150 minutes. Although sunscreens with identical SPF numbers give you equivalent sunburn protection from UVB rays, no sunscreen product screens out all UVA rays. Some may advertise UVA protection, but there is no system to rate UVA protection yet. ” (4)
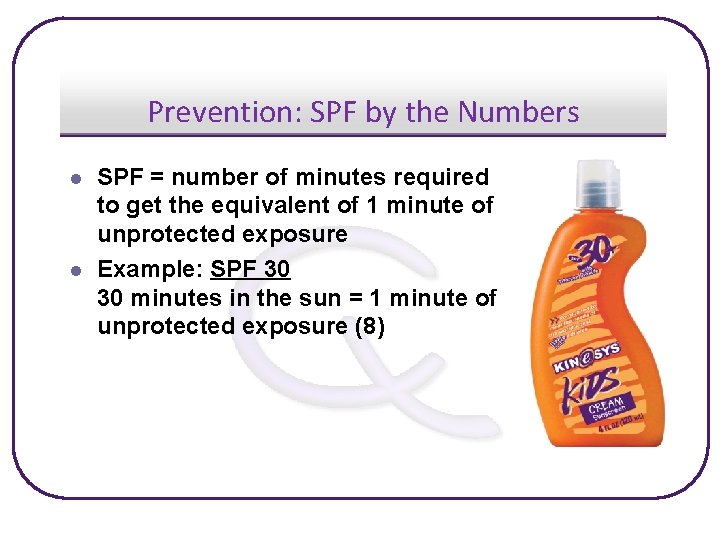
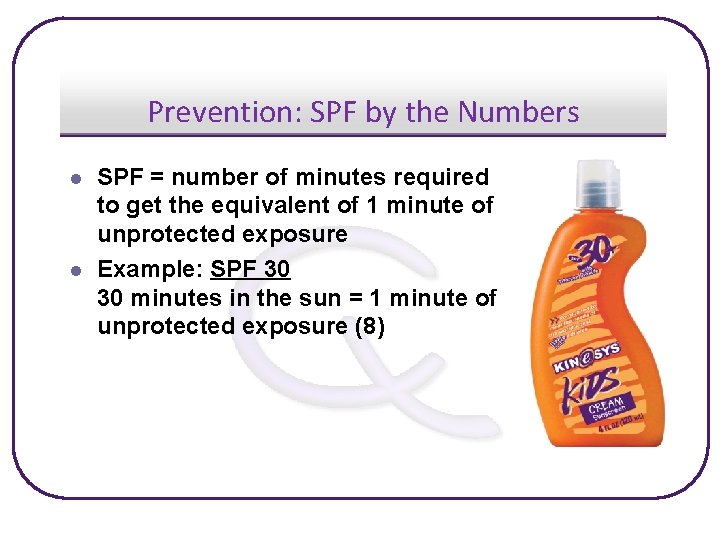
Prevention: SPF by the Numbers l l SPF = number of minutes required to get the equivalent of 1 minute of unprotected exposure Example: SPF 30 30 minutes in the sun = 1 minute of unprotected exposure (8)
Prevention l SUNSCREEN…USE IT! • “In 2003, only 14% of high school students reported routine sunscreen or sunblock use with an SPF of 15 or higher when outside for more than 1 hour on a sunny day, and this rate has remained unchanged since 1999. ” (18)

Sunscreen CAN Reduce Sun. BURN
Prevention l Protective Accessories (8) • Clothing » Provides UV radiation protection » Loose fitting, long-sleeved shirts and long pants made from tightly woven fabric offer the best protection » Typical lightweight t-shirts worn in the summer provide less protection than a sunscreen with an SPF of 15 or higher

Prevention l Protective Accessories (8) • Hats » Hats can help shield your skin from the sun’s UV rays » Wear hats with a brim that shades the face, ears, and the back of the neck • Umbrellas » Must be opaque, not transparent

Tanning l Dangers of Tanning (5) • Causes skin cancer! • Cosmetic issues • Leathery skin, wrinkled skin • Can suppress the immune system • Premature aging of the skin
Tanning Truths l Some Tanning Truths • “Tanning not only increases the risk for melanoma and squamous cell carcinoma, but accelerates skin aging” James M. Spencer, MD, director of dermatologic surgery at Mount Sinai Medical Center in New York City (12) • Five or more sunburns doubles your risk of developing skin cancer (13)
Tanning Myths l l Myth: Tanning is okay (5) Reality • NO! • • • Tanning provides excessive exposure to harmful UV radiation, which can cause skin cancer “A tan is actually the result of skin injury…[w]hen a person's skin darkens from a tan, it is an indication that damage has occurred to the skin and the skin is trying to protect itself by producing more pigment or melanin. ” James Spencer, MD, FAAD, professor of clinical dermatology at Mount Sinai School of Medicine (6) Using tanning oil will not prevent sun damage
Tanning Myths l l Myth: Tanning beds are safer than the sun Reality • NO! • Most tanning bed lamps emit both UVA and UVB rays • A study from Dartmouth in 2002 showed tanning bed users had 2. 5 times the risk of SCC and 1. 5 times the risk for BCC. (19) • “Indoor tanning…is a dangerous practice leading to a vast array of adverse effects” (10)

Artificial Tanning Salon Statistics (12) • $2 billion-a-year industry in the U. S. • Up to 28 million Americans tan indoors annually • There about 25, 000 tanning salons across the country • Adolescent females report the highest usage » About 36. 8% of the white female adolescents in the US report using a tanning bed at least once (11) Ohh yeah that looks healthy!
Artificial Tanning l Sunlamps and Tanning Beds • Emit both UVA and UVB rays • Can cause deep skin damge • Increases the risk for SCC and melanoma • May be linked to immune system • • • damage Can cause premature aging of the skin Currently 25 states have laws prohibiting the use of tanning beds by minors (9) NOT GOOD FOR YOUR SKIN!
UV Radiation Myths l l Myth: Clouds block UV radiation (16) Reality • • • Myth: Clothes block UV radiation (8) Reality • • Not really A thin layer of clouds can let up to 80% of UV rays through A thick layer of cloud cover can block most but not all UV rays Somewhat correct A white, dry cotton shirt provides less protection than sunscreen with an SPF of 15 Fabric that allows light through also allows UV ray’s through Wet clothing allows about 50% transmission of UV radiation
UV Radiation Myths l l Myth: Water doesn’t reflect UV radiation (8) Reality • • Yes it does! Sand concrete reflect 15% of UV radiation Water reflects less than 10% of UV radiation Snow reflects 80% of UV radiation
Cancer Myths l l Myth: Darker skinned people don’t get skin cancer Reality • False! • They are at risk for skin cancer and most frequently at risk • • for melanoma Frequent areas from cancer in darker skinned people are palms, soles, under nails, in the mouth, or on genitalia NO ONE is 100% risk free from skin cancer
Check Yourself Before You Wreck Yourself l Be in tune with your body • Pay attention to things inside and out • As always, if you are unsure about something seek • professional help A simple exam can be done to check for skin cancer » Check all areas of the skin » Focusing on the face, arms, neck and torso • Also, DON’T SMOKE it’s terrible for you!

References 1. Basal Cell Carcinoma. The Skin Cancer Foundation. 2006. http: //www. skincancer. org/basal/index. php (accessed 6/12/06) 2. Squamous Cell Carcinoma. The Skin Cancer Foundation. 2006 http: //www. skincancer. org/squamous/index. php (accessed 6/12/06) 3. American Cancer Society. Learn About Skin Cancer – Melanoma. 2007. http: //www. cancer. org/docroot/lrn_0. asp 4. Sunscreens and Sun-Protective Clothing. Federal Trade Commission. May 2001. www. ftc. gov/bcp/conline/pubs/health/sun. htm (accessed 7/3/2006) 5. The Darker Side of Tanning. American Academy of Dermatology http: //www. fda. gov/cdrh/consumer/tanning. html, (accessed 6/29/2006) 6. Innovative Public Service Advertisement Campaign Sends Strong Message To Teens About Dangers Of Indoor Tanning American Academy of Dermatology. October 19 2006. http: //www. medicalnewstoday. com/medicalnews. php? newsid=54504 (accessed 11/13/2006) 7. American Cancer Society Cancer Facts and Figures, 2007. American Cancer Society Publication. Atlanta, GA. 2007.

References 8. American Cancer Society. Skin Cancer Prevention and Early Detection. http: //www. cancer. org/docroot/PED/content/ped_7_1_Skin_Cancer_Detection_What_You_Can_Do. as p (accessed 11/13/06). 9. Tanning Restrictions for Minors A State-by-State Comparison. March 2007. http: //www. ncsl. org/programs/health/tanningrestrictions. htm 10. Jody A. Levine MD, Michael Sorace MD, James Spencer MD and Daniel M. Siegel MD. The indoor UV tanning industry: A review of skin cancer risk, health benefit claims, and regulation. Journal of the American Academy of Dermatology. Volume 53, Issue 6, December 2005, Pages 1038 -1044. 11. Catherine A. Demko, Ph. D; Elaine A. Borawski, Ph. D; Sara M. Debanne, Ph. D; Kevin D. Cooper, MD; Kurt C. Stange, MD, Ph. D. Use of Indoor Tanning Facilities by White Adolescents in the United States. Arch Pediatric Adolescent Medicine. 2003; 157: 854 -860. 12. The Skin Cancer Foundation. The Case Against Indoor Tanning. 2007. http: //www. skincancer. org/artificial/index. php

References 13. Pfahlberg A, Kolmel KF, Gefeller O. Adult vs childhood susceptibility to melanoma: Is there a difference? Arch Dermatol, Sep 2002; 138: 1234 – 1235. 14. Vander's Human Physiology: The Mechanisms of Body Function, 10/e. Eric P. Widmaier, Hershel Raff, Kevin T. Strang. 2006. Mc. Graw-Hill Inc: New York, New York. 15. Ries LAG, Harkins D, et al. SEER Cancer Statistics Review, 1975 -2003, National Cancer Institute. Bethesda, MD. http: //seer. cancer. gov/csr/1975_2003/, based on November 2005 SEER data submission, posted to the SEER web site, 2006. 16. Carolyn Strange. Thwarting Skin Cancer with Sun Sense. FDA Consumer Magazine (July-August 1995) http: //www. fda. gov/fdac/features/695_skincanc. html (accessed 7/5/07) 17. Stephen E. Ulrich. Mechanisms underlying UV-induced immune suppression. Mutation Research (571) 185 -205. 2005 18. Sherry Everett Jones, Mona Saraiya. Sunscreen Use Among US High School Students, 1999 -2003 Journal of School Health, April 2006, Vol. 76, 4, 150 -153.
References 19. Margaret R. Karagas; Virginia A. Stannard; et al. Use of Tanning Devices and Risk of Basal Cell and Squamous Cell Skin Cancers Journal of the National Cancer Institute; Feb 6, 2002; 94, 3; Research Library pg. 224 20. World Health Organization. Global disease burden from solar ultraviolet radiation. http: //www. who. int/mediacentre/factsheets/fs 305/en/index. html
 Skin cancer abcde
Skin cancer abcde Integumentary system psoriasis
Integumentary system psoriasis Melanoma examination
Melanoma examination Thin skin vs thick skin
Thin skin vs thick skin Milady chapter 23 pdf
Milady chapter 23 pdf Skin information
Skin information Breakthrough cancer pain
Breakthrough cancer pain Definition of cancer according to who
Definition of cancer according to who Cancer du cavum
Cancer du cavum Biology of cancer
Biology of cancer Breast cancer jeopardy questions
Breast cancer jeopardy questions Cancer du col
Cancer du col Cancer du col
Cancer du col International society of nurses in cancer care
International society of nurses in cancer care Endometrial cancer
Endometrial cancer National breast and cervical cancer early detection program
National breast and cervical cancer early detection program Single cancer pathway
Single cancer pathway Lab diagnosis of cancer
Lab diagnosis of cancer Luminal a breast cancer
Luminal a breast cancer Stage 2b pancreatic cancer
Stage 2b pancreatic cancer Lic cancer cover plan 905
Lic cancer cover plan 905 Missouri cancer registry
Missouri cancer registry Amsterdam criteria
Amsterdam criteria Hpv cervical cancer
Hpv cervical cancer Cancer osseo
Cancer osseo Shaukat khanum pharmacy
Shaukat khanum pharmacy Steve curtis cancer
Steve curtis cancer Lymph diagram
Lymph diagram High sierra ahec
High sierra ahec Cancer personnalité
Cancer personnalité Syntactic sugar causes cancer of the semicolon
Syntactic sugar causes cancer of the semicolon Cancer de colon
Cancer de colon Nursing care plan of cancer patients ppt
Nursing care plan of cancer patients ppt Thyroid pathology
Thyroid pathology Thyroid cancer: a case-based approach
Thyroid cancer: a case-based approach Hpv cervical cancer
Hpv cervical cancer Klotho cancer
Klotho cancer Cancer progression
Cancer progression Tumor suppressor genes
Tumor suppressor genes Care plan of breast cancer
Care plan of breast cancer Prostate cancer tnm classification
Prostate cancer tnm classification Reproducibility project cancer biology
Reproducibility project cancer biology Femarelle meaning
Femarelle meaning Uretäroskopisk stenextraktion
Uretäroskopisk stenextraktion The poem reveals three phases of life
The poem reveals three phases of life Conclusion of breast self examination
Conclusion of breast self examination Stomach cancer symptons
Stomach cancer symptons Ajcc staging breast
Ajcc staging breast Heliobactor
Heliobactor Hospital max peralta extensiones
Hospital max peralta extensiones Pes statement for cancer
Pes statement for cancer Cistoadenoma papilar
Cistoadenoma papilar Microanatomy
Microanatomy Self breast exam
Self breast exam Loss of heterozygosity
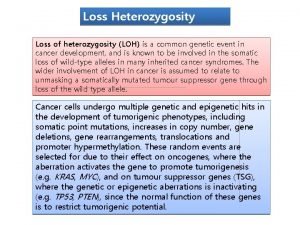
Loss of heterozygosity Breast cancer risk
Breast cancer risk Lcif childhood cancer
Lcif childhood cancer Biology of cancer
Biology of cancer Floor of mouth cancer
Floor of mouth cancer