Chapter 6 Immediate Care of Acute Orthopedic Injuries
- Slides: 100
Chapter 6. Immediate Care of Acute Orthopedic Injuries Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
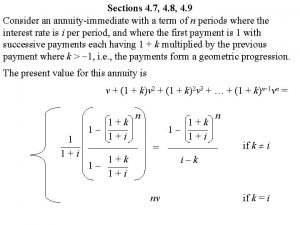
RICES • The prescription for immediate care • RICES – Rest – Ice – Compression – Elevation – Stabilization Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Immediate Care Myths • Acute care and immediate care the same. • Ice decreases swelling. • The goal of immediate care is to decrease inflammation. • The purpose of ice is to decrease hemorrhaging. • Inflammation and swelling are the same. • Ice should be applied for 20 min during immediate care. • All injuries should be treated for the same amount of time. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
What Is Immediate Care? • Care given immediately after an acute orthopedic injury • Subset of acute orthopedic injury care Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
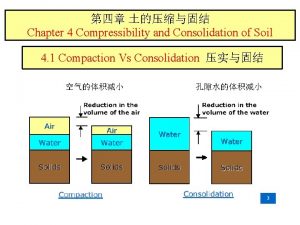
Acute Orthopedic Injury Care Typically three stages • Acute (0– 4 days) • Subacute (5– 14 days) • Postacute (>14 days) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Acute Orthopedic Injury Care (cont. ) Problems with the typical three stages • Range of acute care too wide – Treatment 10 min after injury is not the same as that needed 3 days after the injury. – Acute care, therefore, must be subdivided. • Injuries heal at different rates. – Type and severity of injury – Individual patient differences • Care dictated by patient progress, not by specific time frames Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Acute Orthopedic Injury Care (cont. ) New three stages • Acute (0– 4 days) – Emergency care (e. g. , CPR, if needed) – Immediate care (0– 12 h) – Transition care (12 h to 4 days) • Subacute (5– 14 days) • Postacute (>14 days) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Why RICES? • To limit (decrease): – Total injury – Swelling – Pain – Further injury – Muscle spasm – Inflammation? NO Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
RICES Theory • • • Rest Ice Compression Elevation Stabilization Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Rest: Why? Limits injury aggravation • Should be total during immediate care • Transition to “relative” rest • Different from, but related to, stabilization Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Ice/Cold: Why? • Most think it’s to control swelling. – Important but only part of immediate care • Limiting secondary injury and neural inhibition are more important than controlling swelling. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Ice/Cold: Why? (cont. ) • Two theories – Circulatory or decreased blood flow theory – Decreased secondary injury theory Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Decreased Blood Flow Theory • Older, traditional theory • Cold decreases blood flow. • Logic of theory – Cold causes vasoconstriction – Which decreases blood flow and therefore – Decreases hemorrhaging and therefore – Swelling is reduced • Flaw: Clotting occurs before tissue is cooled enough to substantially decrease blood flow. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Decreased Secondary Injury Theory • History • First proposed in 1976 – Refined in 1985 – Tweaked in 2002 • Flaw: – Cold application has little effect on hemorrhaging. • Limits amount of secondary injury and, therefore, edema. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
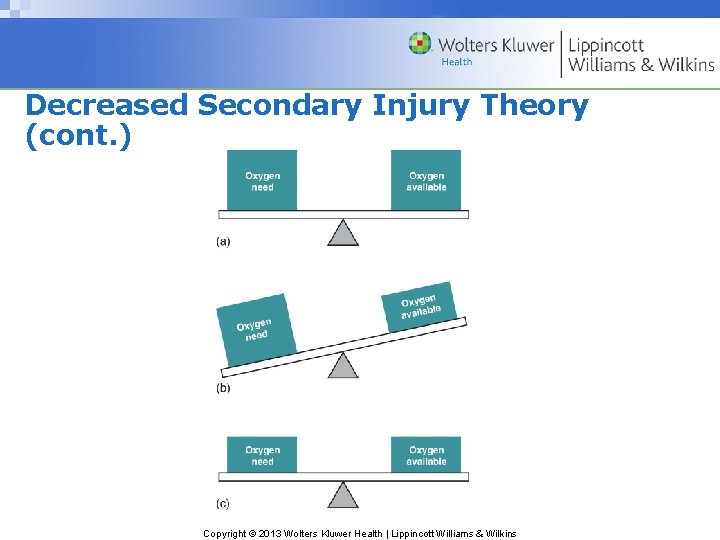
Decreased Secondary Injury Theory (cont. ) • Cold decreases cellular metabolism in viable cells, thus – Reduces oxygen demand (consumption) – Less secondary hypoxic injury – Less total injury – Less free protein generated by phagocytosis – Less edema Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
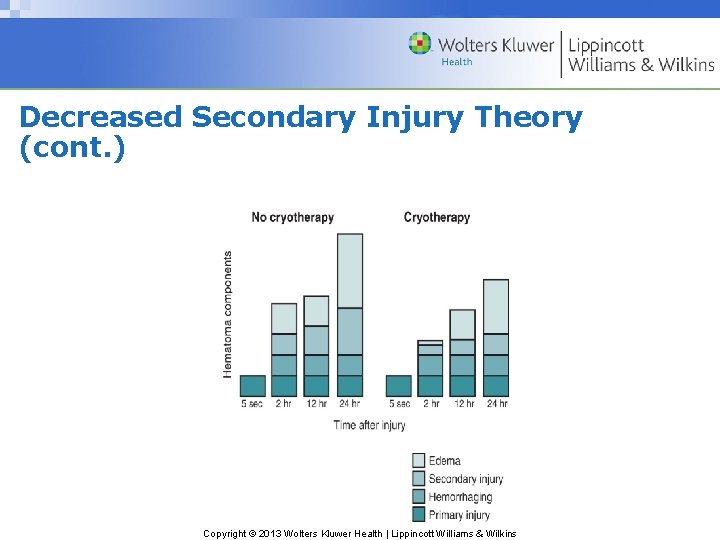
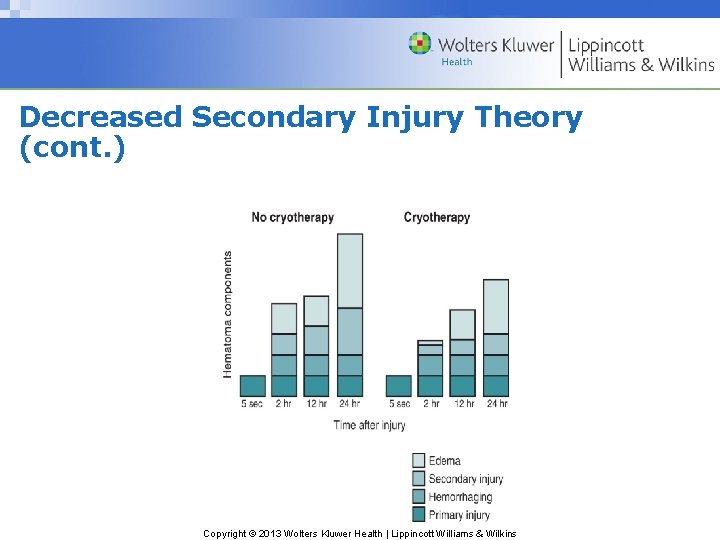
Decreased Secondary Injury Theory (cont. ) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
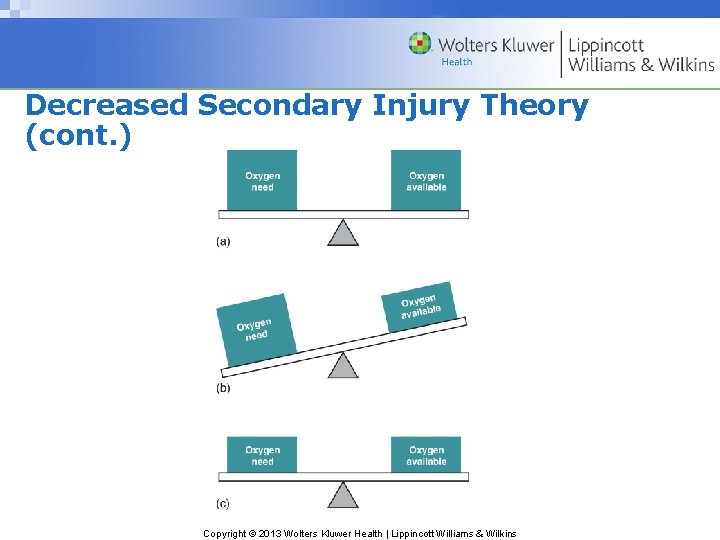
Decreased Secondary Injury Theory (cont. ) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
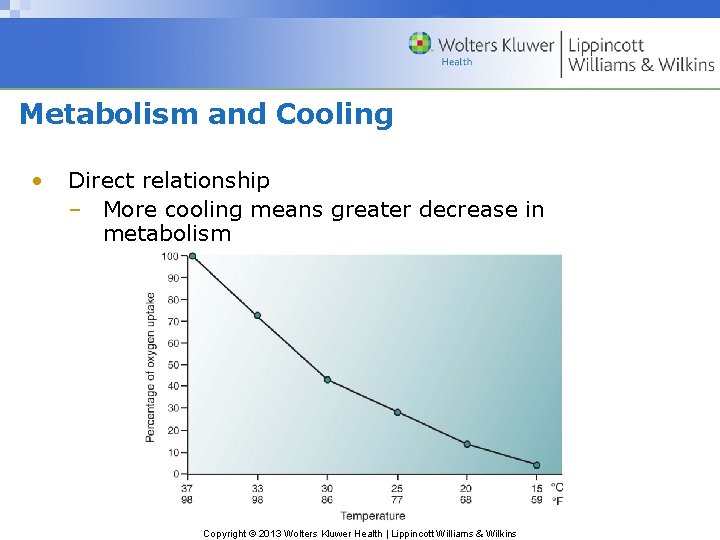
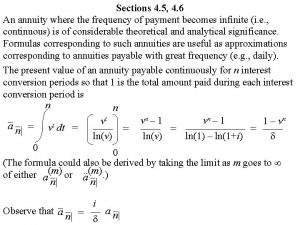
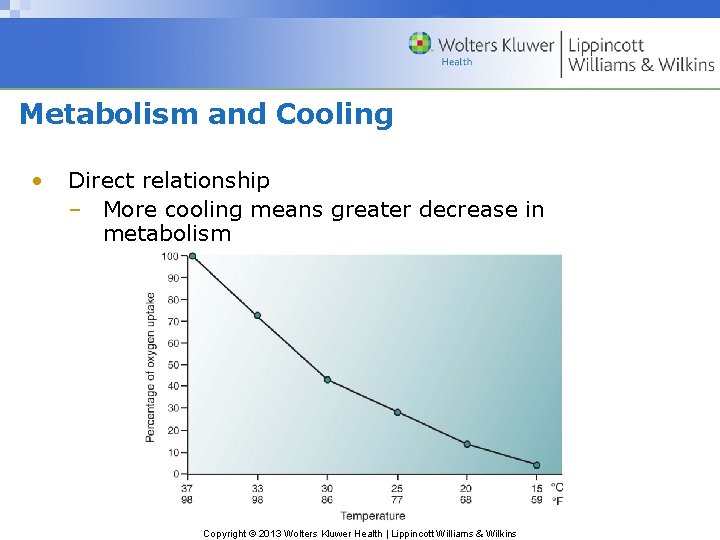
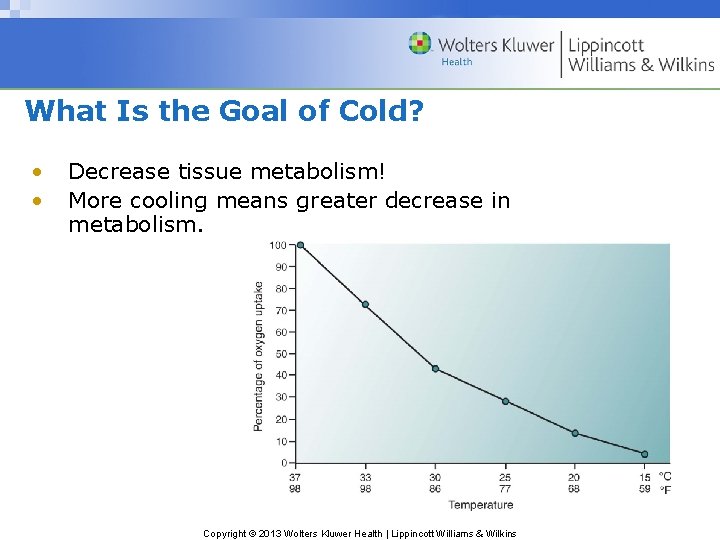
Metabolism and Cooling • Direct relationship – More cooling means greater decrease in metabolism Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Metabolism and Cooling (cont. ) • Heat increases metabolism. – Causes more secondary injury Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
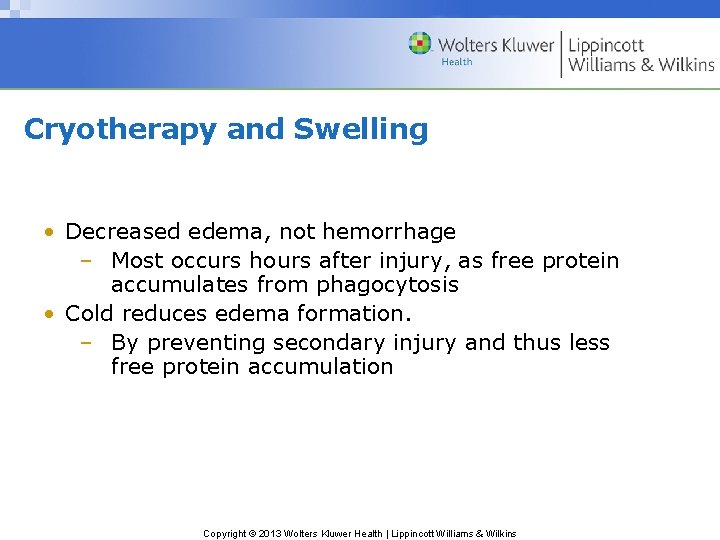
Cryotherapy and Swelling • Decreased edema, not hemorrhage – Most occurs hours after injury, as free protein accumulates from phagocytosis • Cold reduces edema formation. – By preventing secondary injury and thus less free protein accumulation Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Compression: Why? • Controls edema beyond normal volume (i. e. , after tissue spaces are filled) • Apply constantly until swelling is over. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
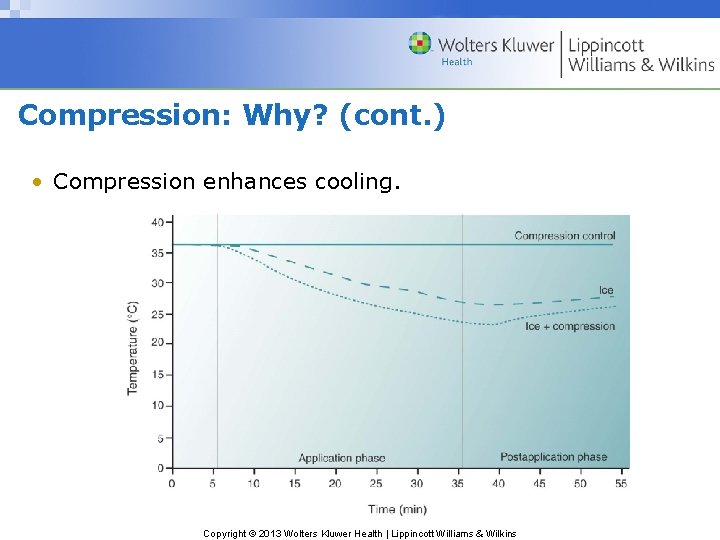
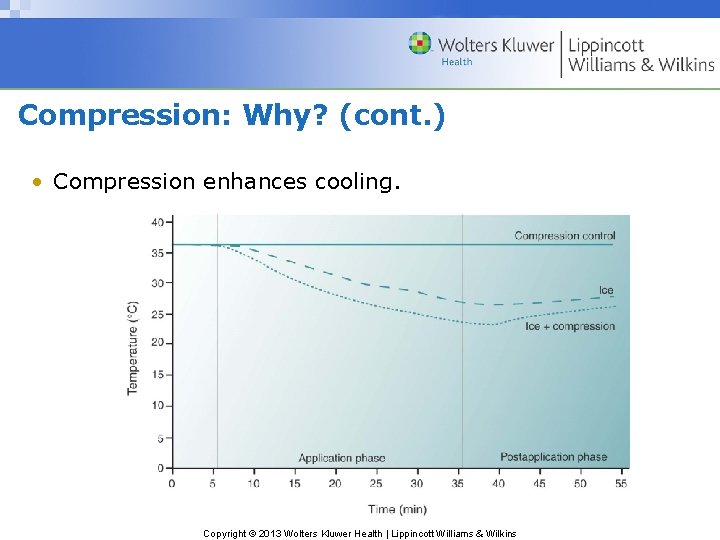
Compression: Why? (cont. ) • Compression enhances cooling. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
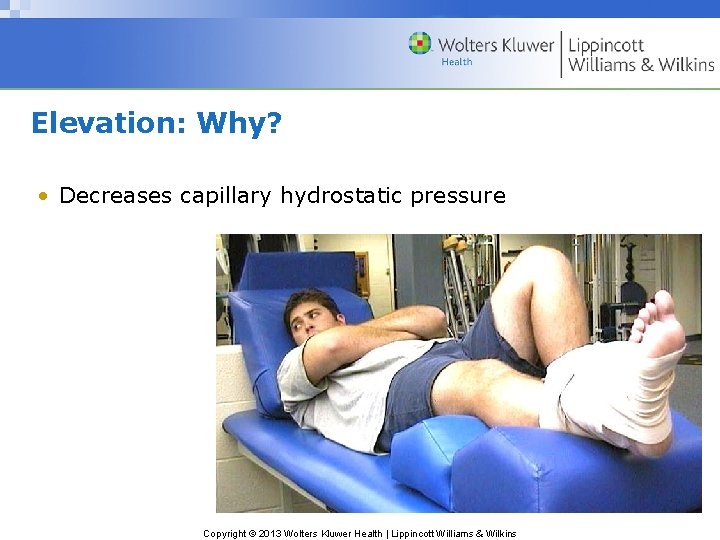
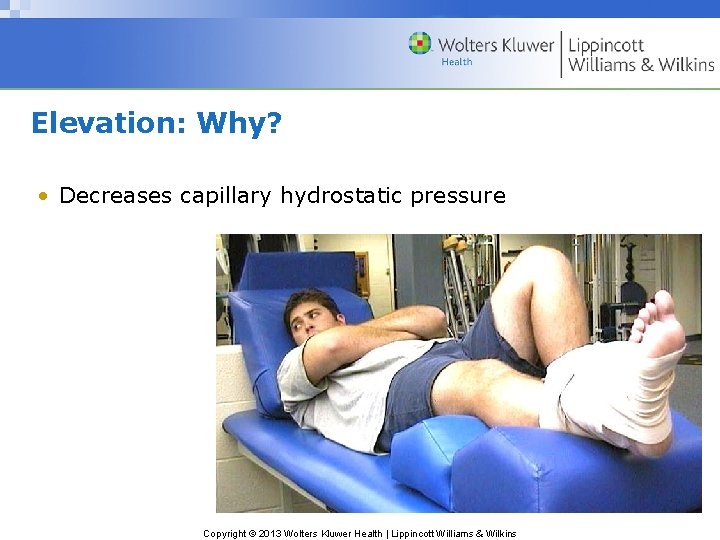
Elevation: Why? • Decreases capillary hydrostatic pressure Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Stabilization: Why? Controls neural inhibition • Process in which neural pathway is blocked so impulses cannot pass – Intended function does not occur. • Can be partial so function is diminished or total so function is abolished temporarily Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Stabilization: Why? (cont. ) Allows muscles to relax, thus • Decreases pain–spasm–pain cycle • Numerous braces and splints for stabilization Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
RICES Theory: Revisited • • • Rest Ice Compression Elevation Stabilization Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
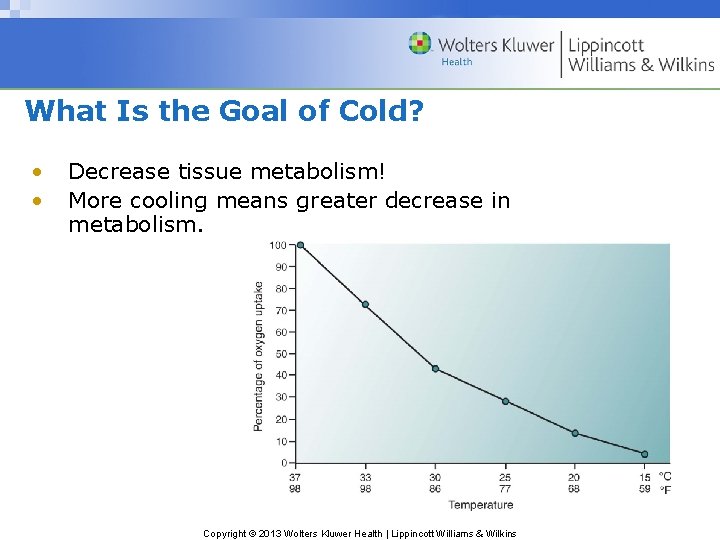
What Is the Goal of Cold? • • Decrease tissue metabolism! More cooling means greater decrease in metabolism. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
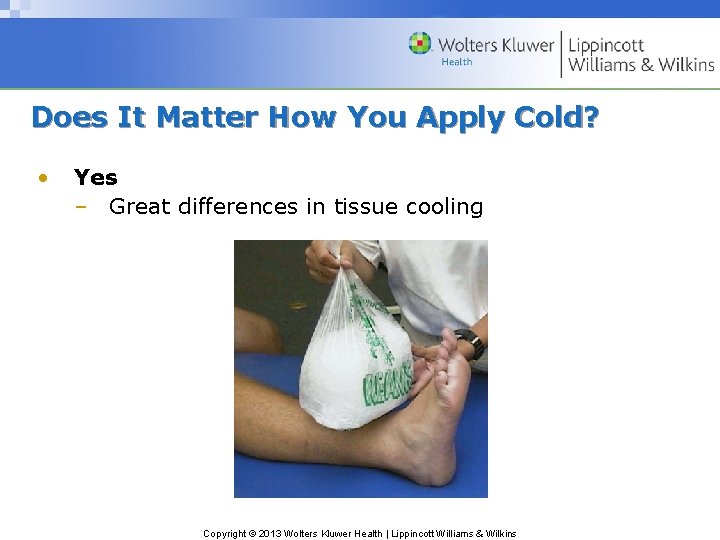
Does It Matter How You Apply Cold? • Yes – Great differences in tissue cooling Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Cryotherapy Physics and Physiology • Cold does not exist; it is not a physical substance. • Cold is absence of heat. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Physiology of Heat Transfer Conduction • Exchange of energy (heat) between two substances in contact with each other • Heat moves from body of higher energy to body of lower energy. • Causes warmer body to cool and cooler body to warm, until they reach equilibrium Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Rate of Conduction • • Temperature differential between body and modality Regeneration of body heat and modality cooling Heat storage capacity of cold modality Size of the cold modality Amount of tissue in contact with pack Length of application Individual variability Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Heat Storage Capacity • Specific heat • Latent heat of fusion Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
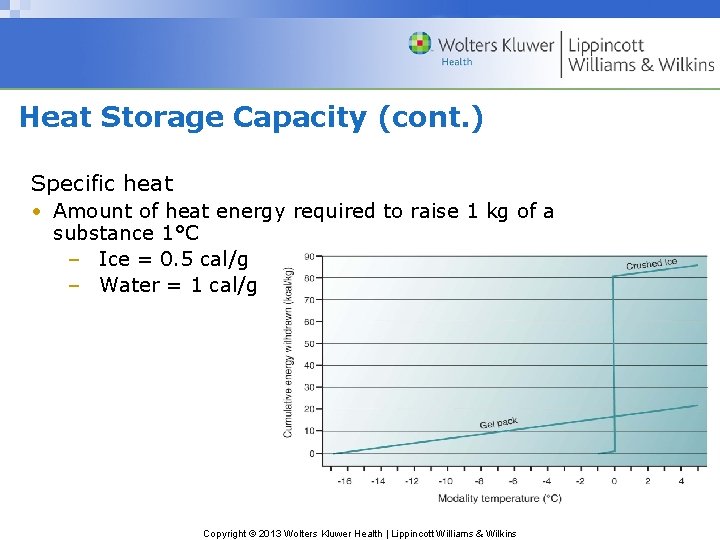
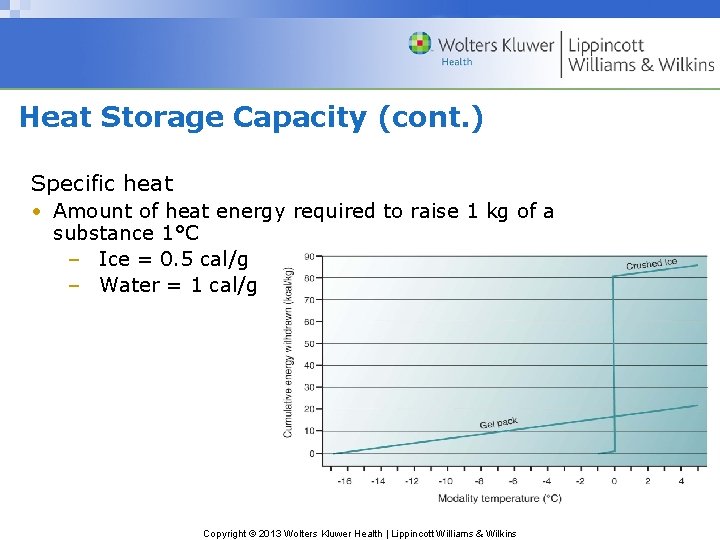
Heat Storage Capacity (cont. ) Specific heat • Amount of heat energy required to raise 1 kg of a substance 1°C – Ice = 0. 5 cal/g – Water = 1 cal/g Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Heat Storage Capacity (cont. ) • Latent heat of fusion – Amount of heat energy needed to convert a substance from a solid state to a liquid state without changing its temperature – Phase change – Ice to water = 80 cal/kg Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
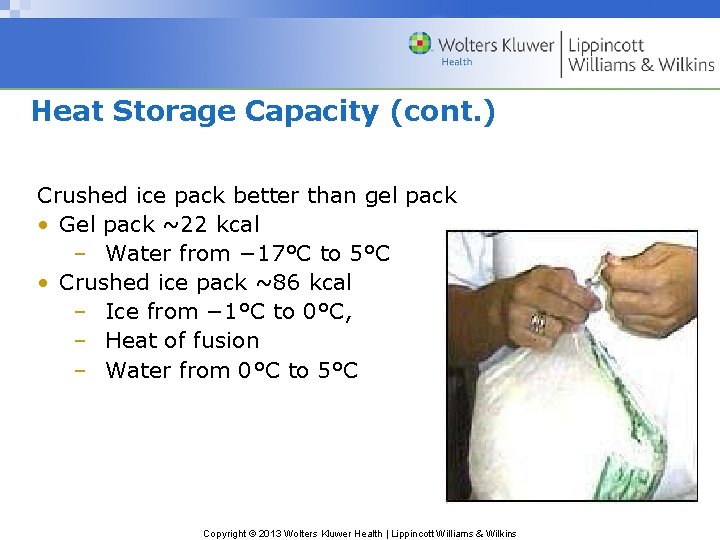
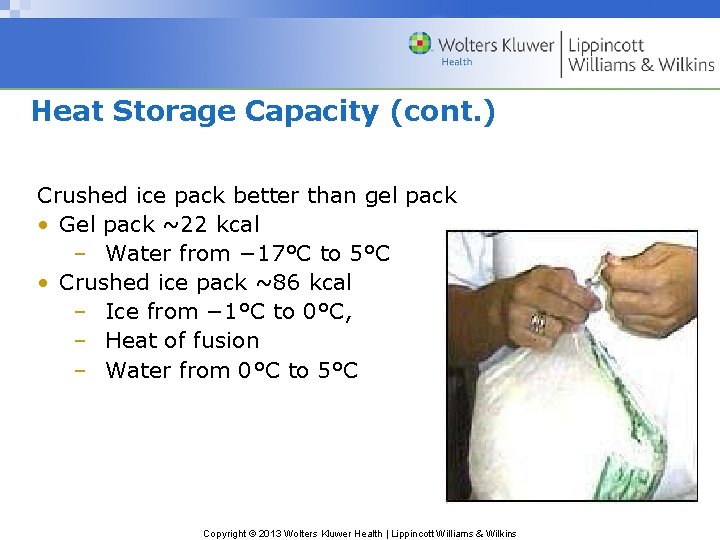
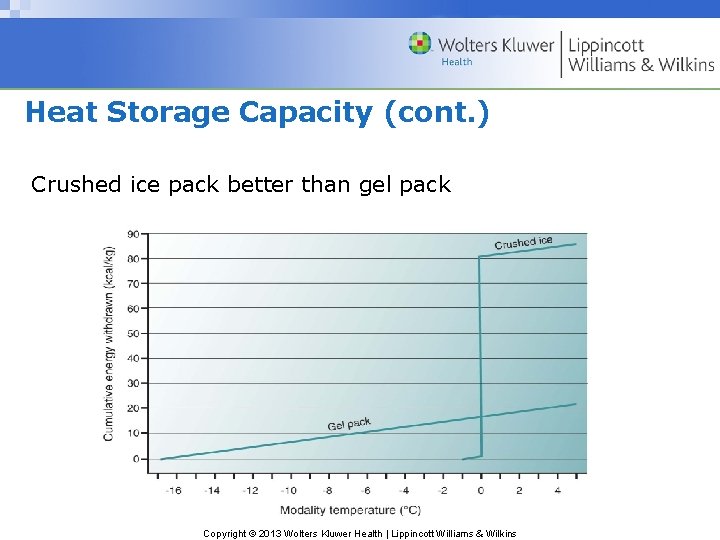
Heat Storage Capacity (cont. ) Crushed ice pack better than gel pack • Gel pack ~22 kcal – Water from − 17°C to 5°C • Crushed ice pack ~86 kcal – Ice from − 1°C to 0°C, – Heat of fusion – Water from 0°C to 5°C Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
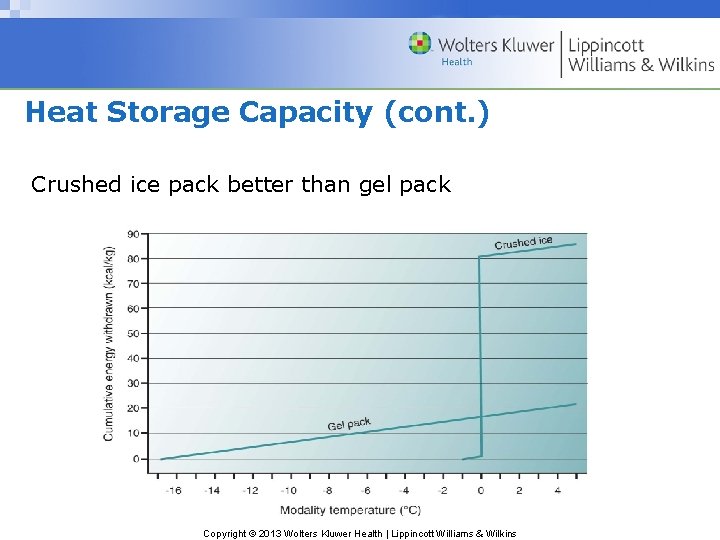
Heat Storage Capacity (cont. ) Crushed ice pack better than gel pack Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
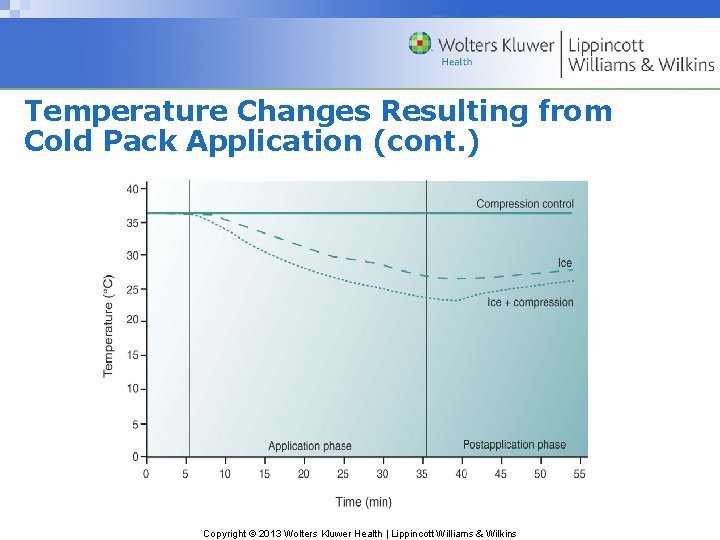
Temperature Changes Resulting from Cold Pack Application • Surface temperature – Repeated applications • Time ratio • Activity between applications (shower) – Compression wrap over cold pack Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
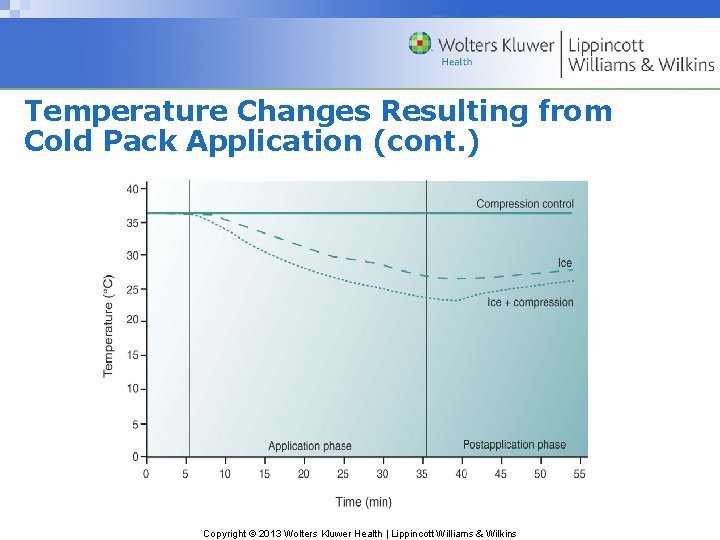
Temperature Changes Resulting from Cold Pack Application (cont. ) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
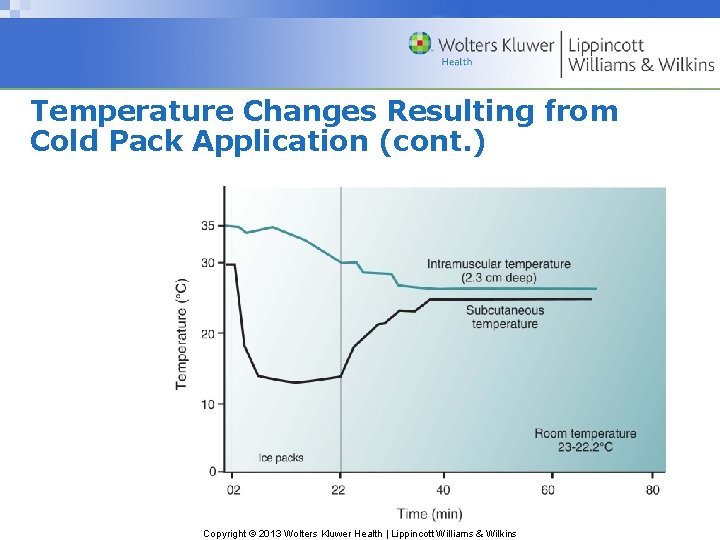
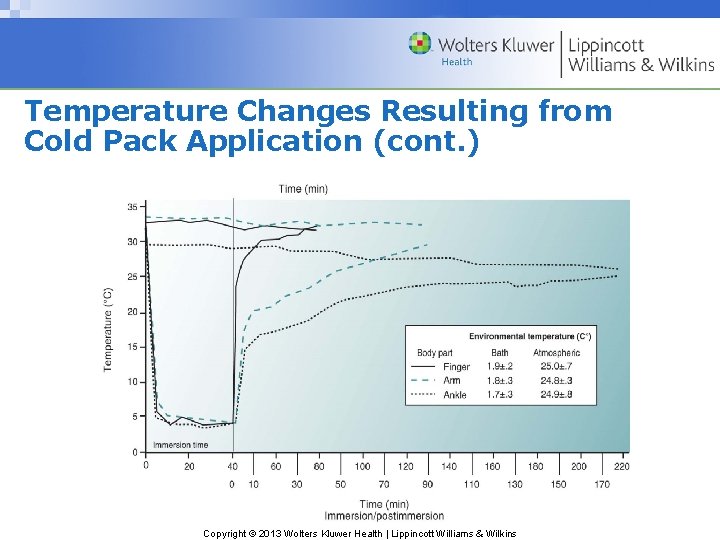
Temperature Changes Resulting from Cold Pack Application (cont. ) • Tissue temperature – Depends on depth and type of tissue – Delayed response – Continues to decrease after application Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
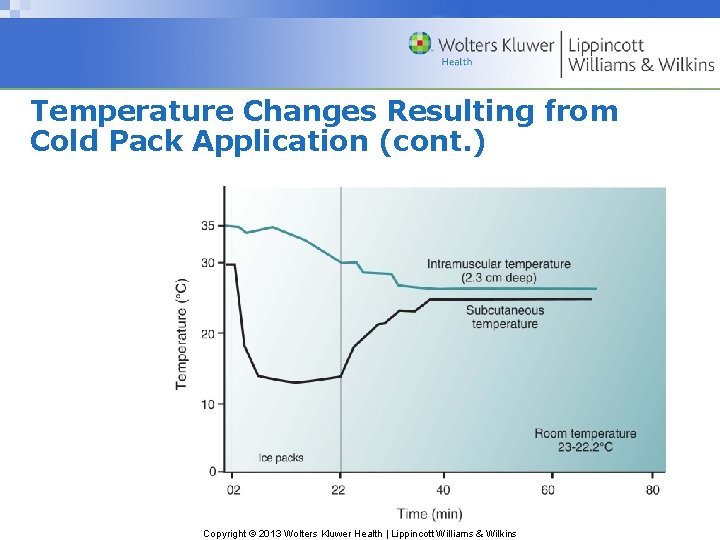
Temperature Changes Resulting from Cold Pack Application (cont. ) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Temperature Changes Resulting from Cold Pack Application (cont. ) • Tissue temperature – Amount of adipose tissue – Rewarming takes hours Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
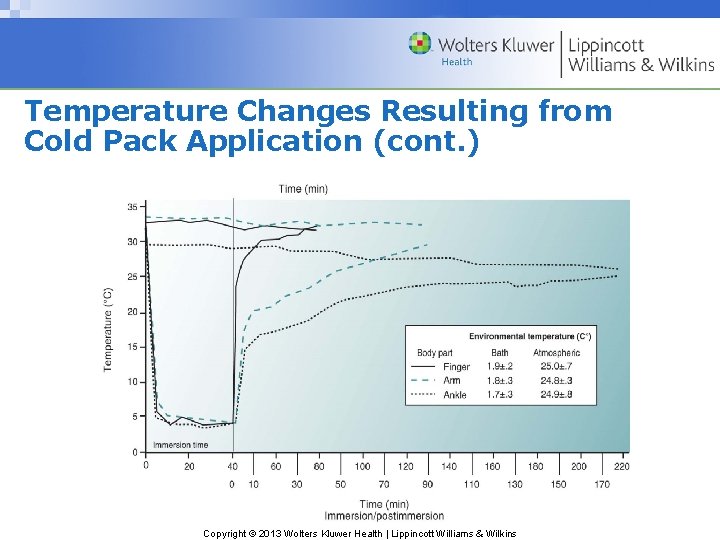
Temperature Changes Resulting from Cold Pack Application (cont. ) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Temperature Changes Resulting from Cold Pack Application (cont. ) • Articular temperature – Similar to tissue temperature – Delayed response – Continues to decrease after application – Amount of adipose tissue Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Temperature Changes Resulting from Cold Pack Application (cont. ) Rewarming after application • Depth of tissue • Amount of heat available to rewarm area: function of circulation and environmental temperature. • Activity level before cryotherapy and palmer • Amount of heat removed from body during application (i. e. , magnitude and duration of cold exposure) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
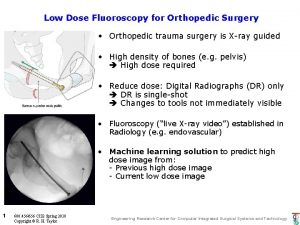
Cryotherapy: Application Principles • Tissue cooling depends on – Cold modality used – How modality is applied • Many protocols suggest – Length – Frequency – Duration Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors That Affect Tissue Cooling • Type of cold pack – Heat of fusion • Duration of application – Longer the application • More cooling • Slower rewarming • Size of cold pack – Larger cold pack, more cooling • Amount of tissue in contact with pack – More tissue contact, more cooling Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Factors That Affect Tissue Cooling (cont. ) • Depth of target tissue – Deeper target, less cooling • Type of cold pack • Method of application – On skin or over a towel or wrap – Compression over pack (per Merrick) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
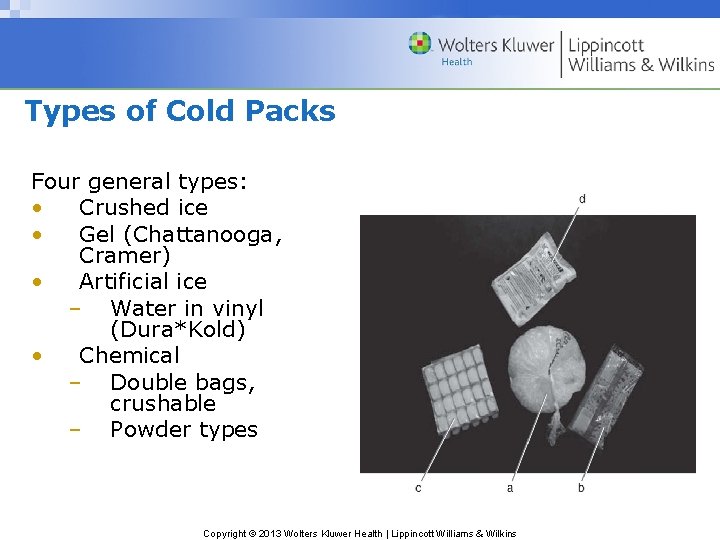
Types of Cold Packs Four general types: • Crushed ice • Gel (Chattanooga, Cramer) • Artificial ice – Water in vinyl (Dura*Kold) • Chemical – Double bags, crushable – Powder types Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Types of Cold Packs (cont. ) Crushed ice • Most effective because of heat of fusion • Excellent for on-the-field use because they don’t melt for hours stored if in insulated cooler • Should not be used if kept in a freezer (too cold) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Types of Cold Packs (cont. ) Gel • • pack Water, alcohol, and gel substance Cooled to ~1°F (− 17°C), so dangerous Not as effective as crushed ice packs (no heat of fusion) Even less effective if wrapped in towel Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
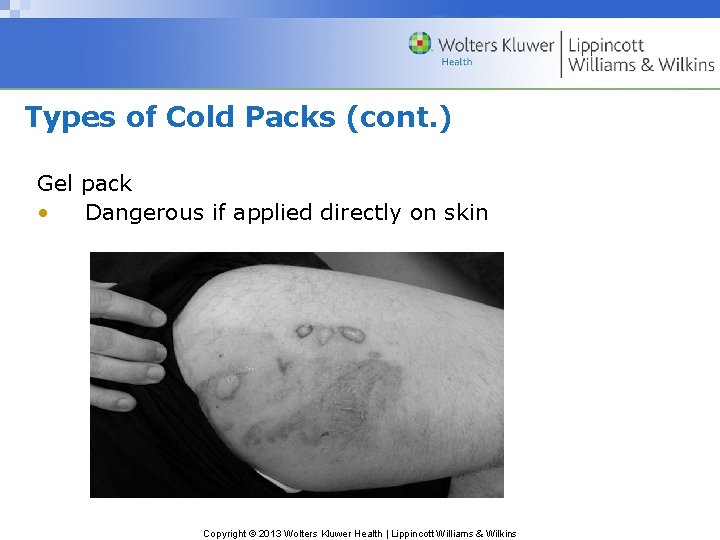
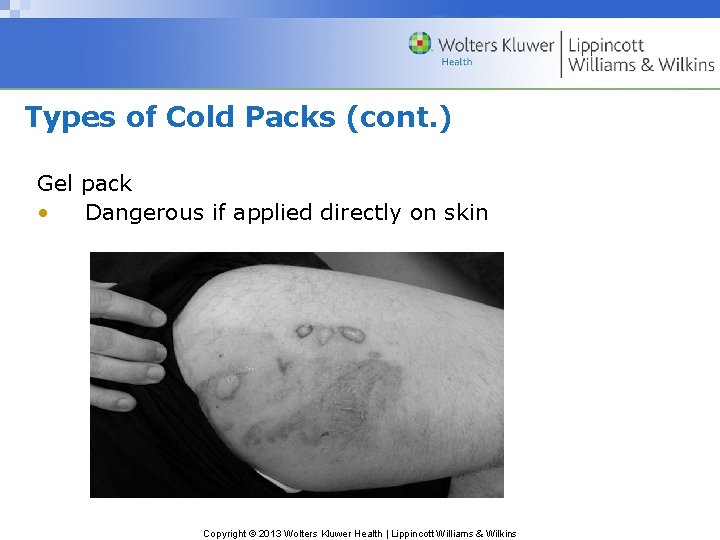
Types of Cold Packs (cont. ) Gel pack • Dangerous if applied directly on skin Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Types of Cold Packs (cont. ) Artificial ice • Water in vinyl pouches, surrounded by nylon cover (Dura*Kold) • Better than gel because of heat of fusion • Not as good crushed ice because of insulation from nylon cover • Good for home use Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Types of Cold Packs (cont. ) Chemical: double bags, crushable • • • Chemical reaction when inner bag is crushed and contents react with outer chemicals Least cooling Not recommended Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Types of Cold Packs (cont. ) Frozen Peas • • • Popular; cheap and convenient Effective – Better than nothing and gel packs – Worse than crushed ice packs or ice water immersion – Little phase change with peas Avoid if possible Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
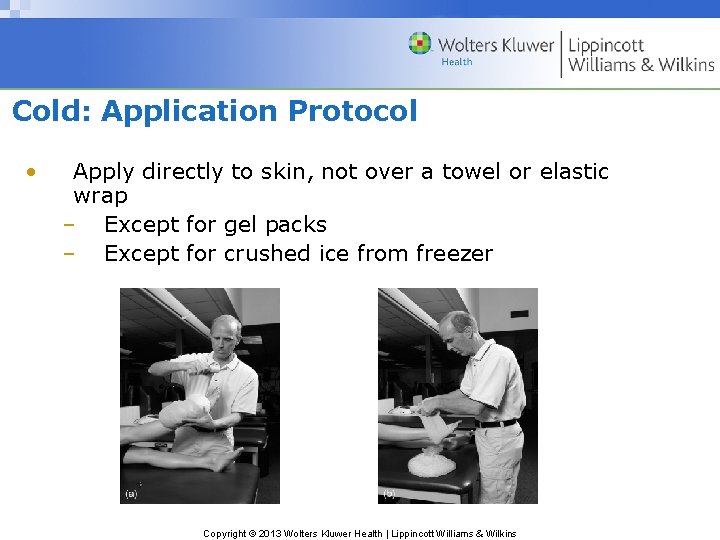
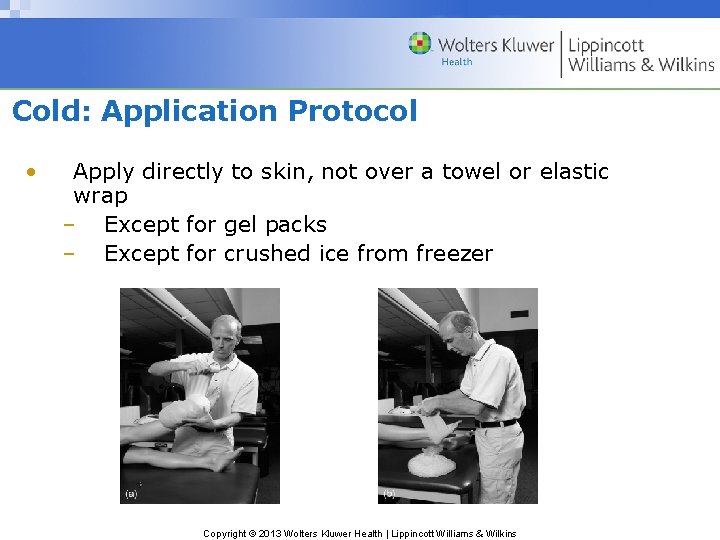
Cold: Application Protocol • Apply directly to skin, not over a towel or elastic wrap – Except for gel packs – Except for crushed ice from freezer Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
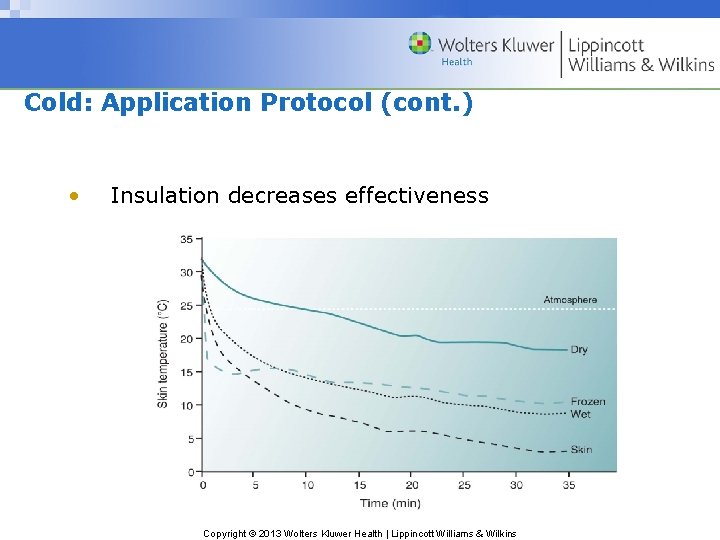
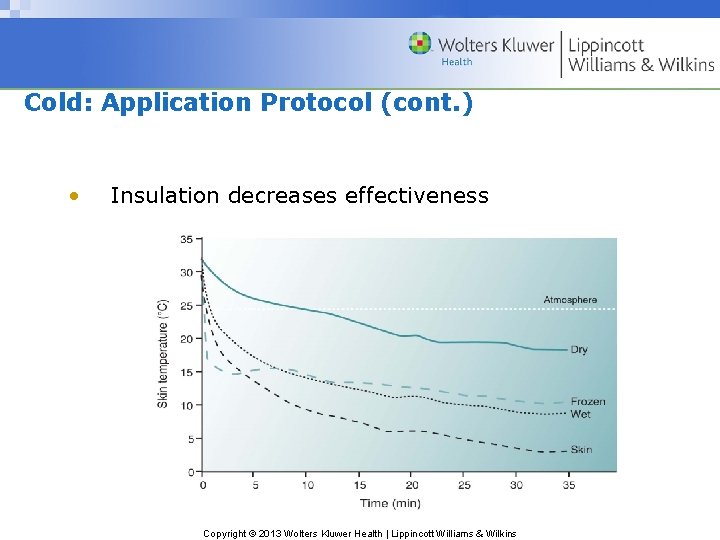
Cold: Application Protocol (cont. ) • Insulation decreases effectiveness Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
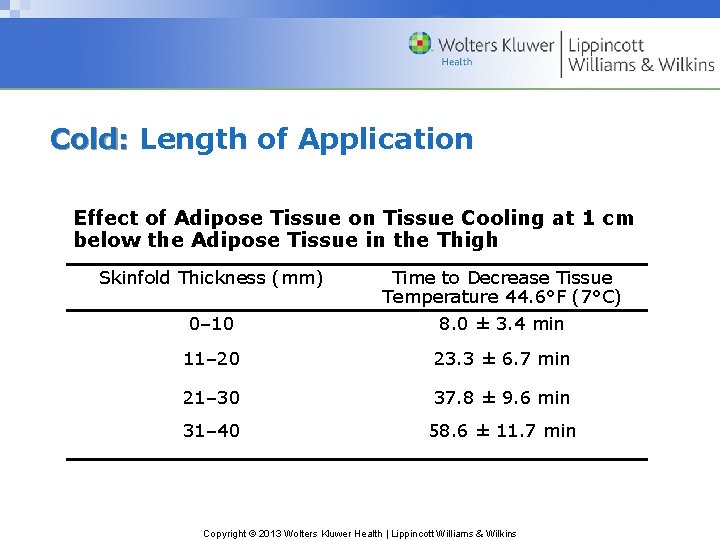
Cold: Length of Application • Intermittent, 30– 60 min every 2 h • Depth of target tissue • Adipose tissue— leave on longer Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
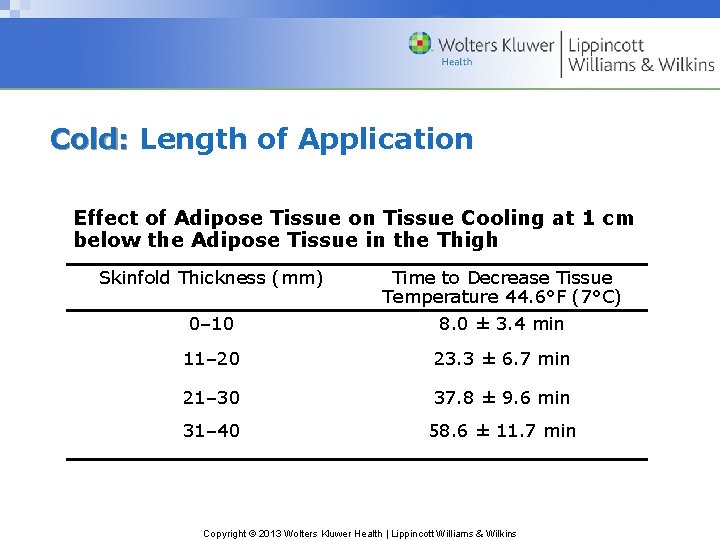
Cold: Length of Application Effect of Adipose Tissue on Tissue Cooling at 1 cm below the Adipose Tissue in the Thigh Skinfold Thickness (mm) 0– 10 Time to Decrease Tissue Temperature 44. 6°F (7°C) 8. 0 ± 3. 4 min 11– 20 23. 3 ± 6. 7 min 21– 30 37. 8 ± 9. 6 min 31– 40 58. 6 ± 11. 7 min Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Cold: Duration of Therapy • Severity of injury • Transition from RICES to cryotherapy techniques involving exercise Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Preventing vs. Removing Swelling • Preventing secondary injury versus removing free protein from extracellular spaces • Prevent: decrease metabolism – Cold effective • Remove: stimulate lymph flow – Cold is a waste of time. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
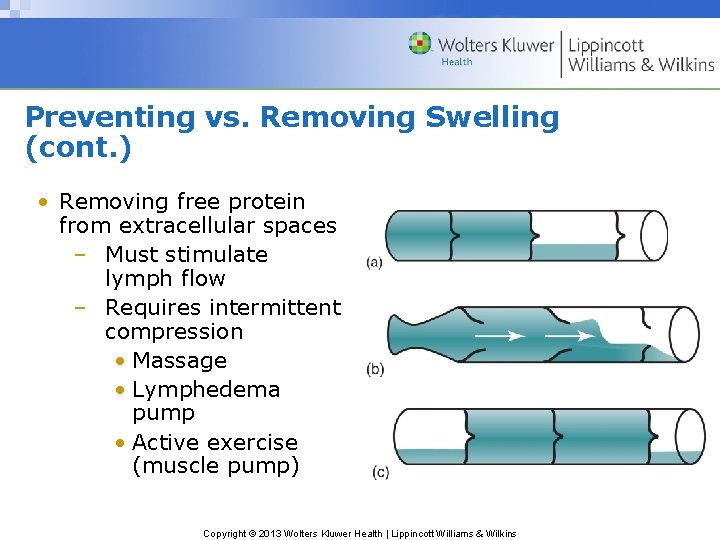
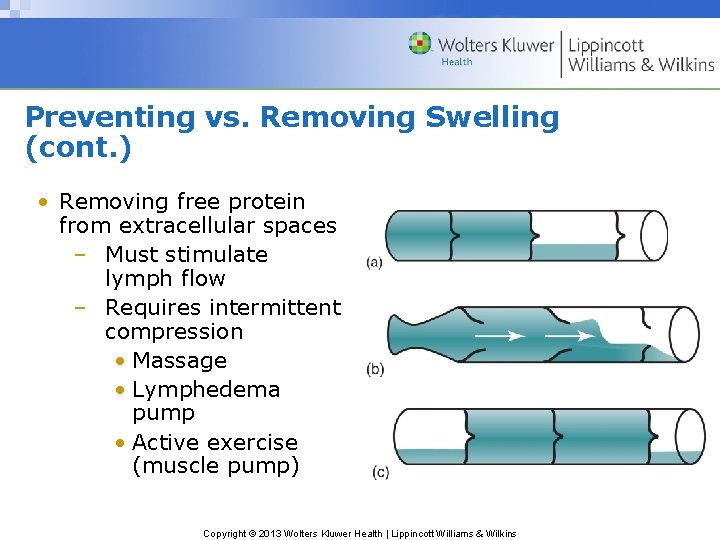
Preventing vs. Removing Swelling (cont. ) • Removing free protein from extracellular spaces – Must stimulate lymph flow – Requires intermittent compression • Massage • Lymphedema pump • Active exercise (muscle pump) Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
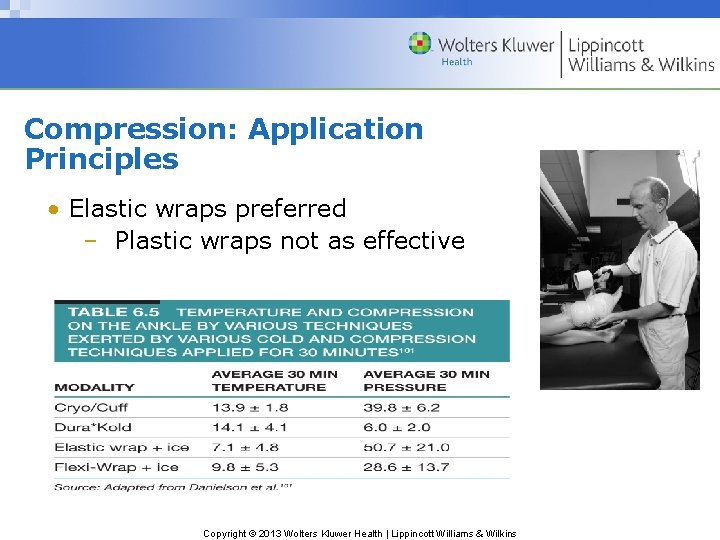
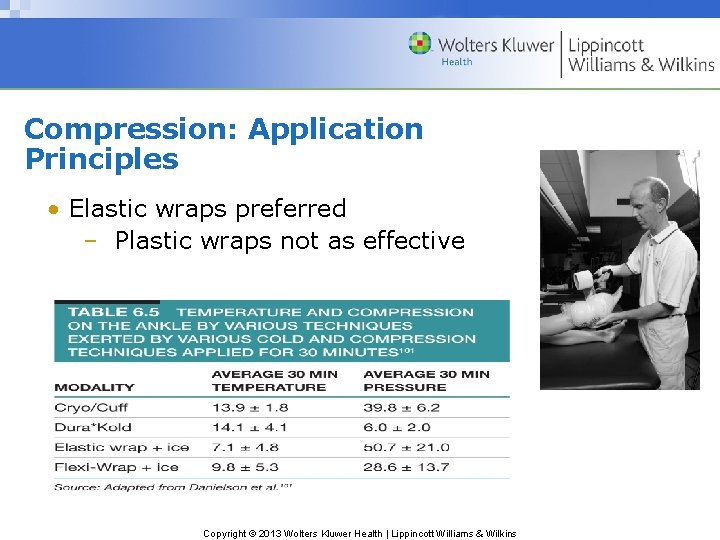
Compression: Application Principles • Elastic wraps preferred – Plastic wraps not as effective Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
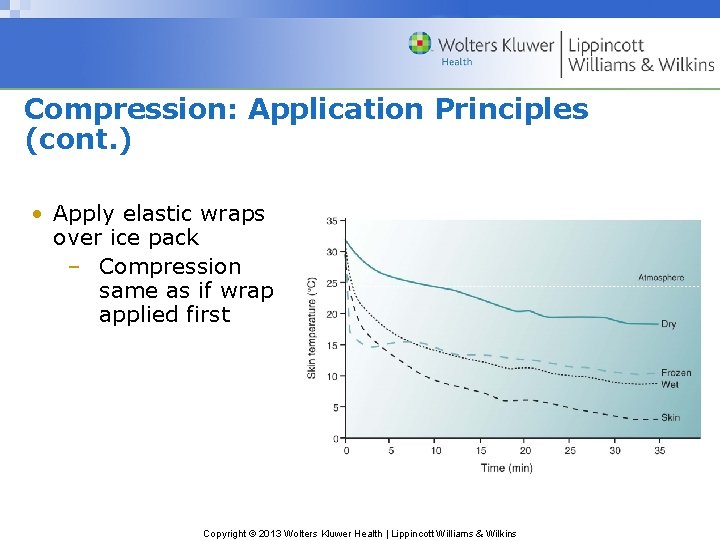
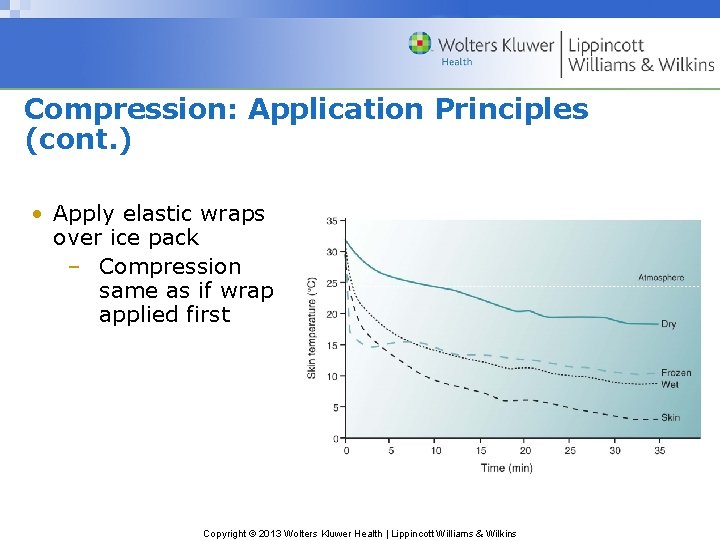
Compression: Application Principles (cont. ) • Apply elastic wraps over ice pack – Compression same as if wrap applied first Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Compression: Application Principles (cont. ) • Stretch elastic wraps ~75% as they are applied. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Cryotherapy: Contraindications and Precautions Cold is dangerous if • Too cold or too long • Under excessive compression • Patient suffers from some specific diseases, such as – Raynaud – Cold hypersensitivity – Cold urticaria Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Five-Step Application for Immediate Care • • • Foundation Preapplication tasks Application parameters Postapplication tasks Maintenance Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Step 1. Foundation • • Definition Effects Advantages Disadvantages Indications Contraindications Precautions Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Effects • Ice decreases metabolism in the injured tissue. – Decreases the need for oxygen – Decreases secondary hypoxic injury Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Effects (cont. ) Compression and elevation • Counteract edema and result in a decrease in swelling Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Effects (cont. ) Stabilization • Allows musculature around the injury to relax • Along with ice, limits pain–spasm–pain cycle Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Advantages • • Less total tissue damage means less healing needed. Decreased swelling means less pain. Decreased pain means less neural inhibition. Ice is relatively inexpensive. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Disadvantages • Effectiveness diminishes with time. • Full effects only if applied within 5– 10 min after injury Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Indications • Acute orthopedic or soft tissue injury Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Contraindications Do not use with a person who is • Hypersensitive to cold • Allergic to cold • Has circulatory abnormalities Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Precautions • • Ice packs not directly on skin continuously for >60 min Cold packs cooled to or less than − 17°C (0°F) should not be applied directly to the skin. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Step 2. Preapplication Tasks • • Selecting the proper modality Preparing the patient physically Preparing the equipment Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Selecting the Proper Modality • • Evaluate the injury or problem. Determine the treatment goals. Check for contraindications. Hypersensitive to cold? Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Preparing the Patient Physically • • • Remove overlying clothing. Remove braces and bandages, as necessary. Place patient in a comfortable position and so that the injured area is elevated. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Preparing the Patient Psychologically • • • Pain and frustration from the injury are usually the biggest problems. Reassure the athlete. Warn about precautions. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Preparing the Equipment • Prepare the ice pack – Crushed ice in a plastic bag • Big enough to extend 2– 3 in. beyond injury – Evacuate as much air as possible from the bag. – Tie a knot in bag. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Preparing the Equipment (cont. ) • • , Elastic wraps – Prefer 6 in. , never <4 in. – Double length or multiple for large areas Splint or sling Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Step 3. Application Parameters • Procedures – Ice bag – Elastic wrap – Stabilize – Elevate – Dosage – Duration – Frequency of application Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
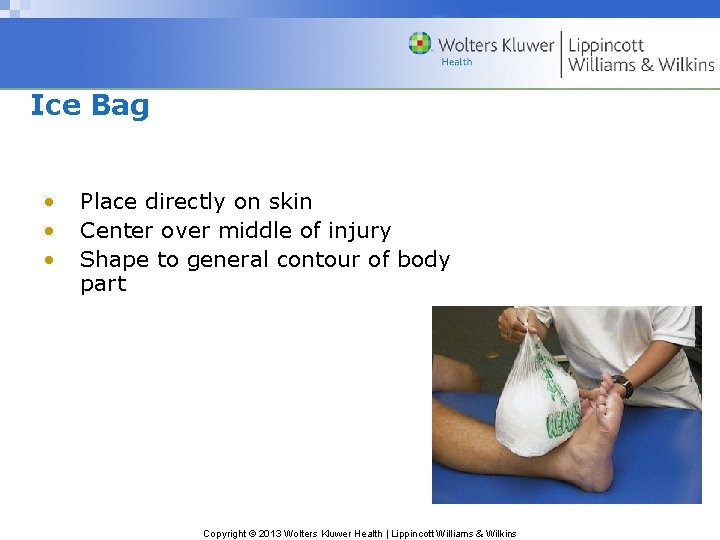
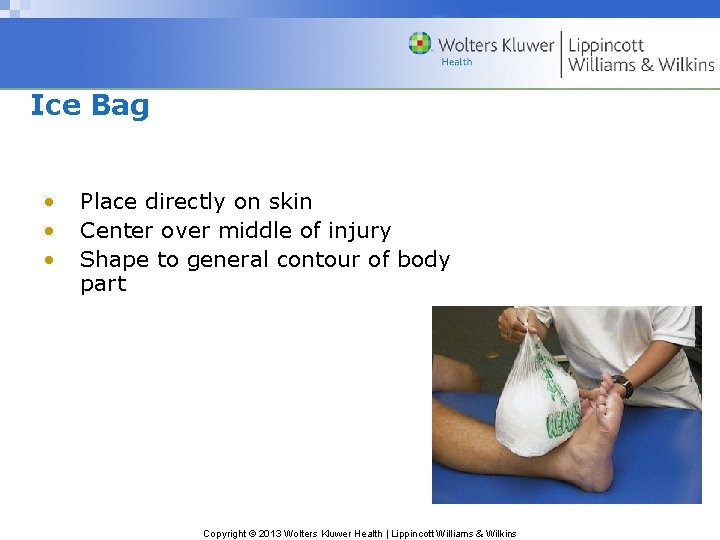
Ice Bag • • • Place directly on skin Center over middle of injury Shape to general contour of body part , Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Elastic Wrap • • • Apply snugly, but not too tightly (stretch to ~75% of length). Cover the entire area. Secure with clips, tape, or tuck. Wear constantly for 20– 24 h, except when changing ice bag. No Flexi-Wrap, no compression , Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
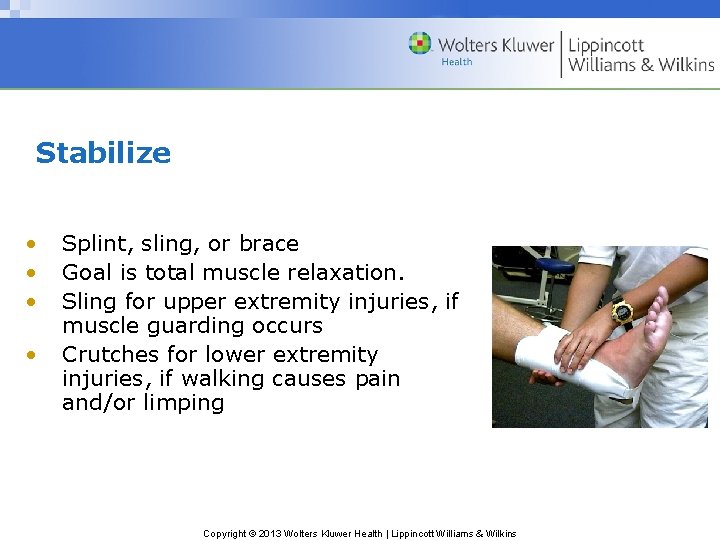
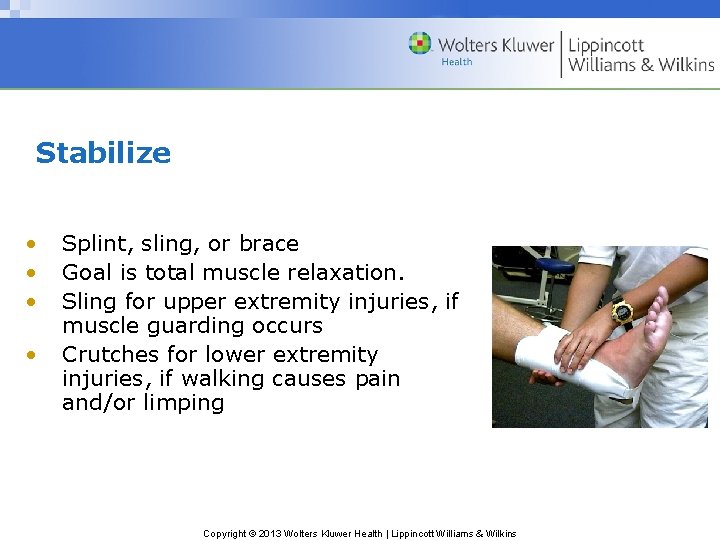
Stabilize • • Splint, sling, or brace Goal is total muscle relaxation. Sling for upper extremity injuries, if muscle guarding occurs Crutches for lower extremity injuries, if walking causes pain and/or limping Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Elevate • Six inches or so above heart , Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Dosage • • Ice pack extends 2– 3 in. beyond injury. Compression extends 2– 3 in. beyond ice pack. , Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Length of Application • • • , Ice bag, intermittently – 20– 60 min depends on injury and skinfold • 20 min, finger • 30 min ankle, arm • 45 min, thigh • +1 min per millimeter of skinfold Compression and elevation constantly Rest and stabilization until pain free Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Frequency of Application • • , Ice – 5– 10 min after injury – Second application 30– 60 min later, after shower and go home – Every 2 h thereafter (don’t stay up into night) Rest, compression, elevation, and stabilization constantly Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Step 4. Postapplication Tasks • • • Replace equipment/clean up area – Drain water and ice from ice pack (save the plastic bag for another use). – Return cold pack to refrigeration unit. Give patient written instructions – Time of next appointment – Rest injury – Time for reapplication of ice – Phone number for emergency Record treatment and unique patient response to treatment Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Step 5. Maintenance • • Keep ice machine in good repair. Replace elastic wraps as they deteriorate. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Crutch Use Who? • Any patient unable to walk without a limp Why? • Crutches facilitate proper gait by using arms to substitute for, or supplement, leg power. • Failure to use crutches may result in: – Delayed healing – Permanent abnormal gait Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Crutch Use (cont. ) Proper use requires • Proper fitting of crutches • Selecting the appropriate gait • Instructing patient to walk properly • Observing the patient practice the gait • Periodic reevaluating to make sure patient is using crutches properly Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
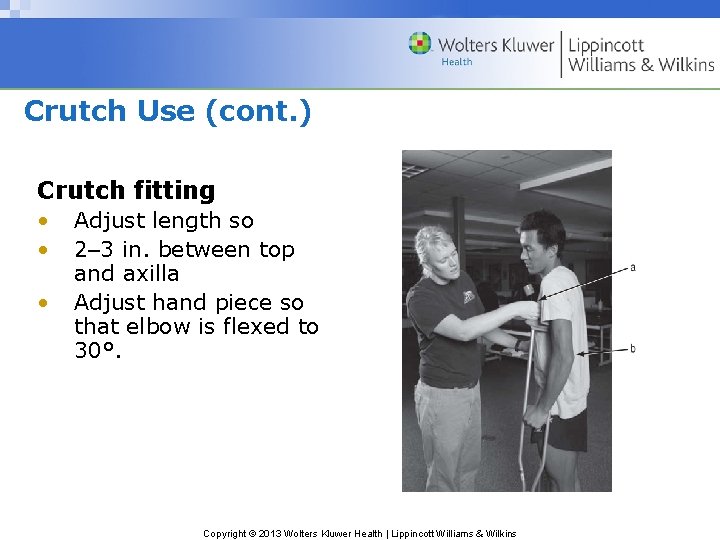
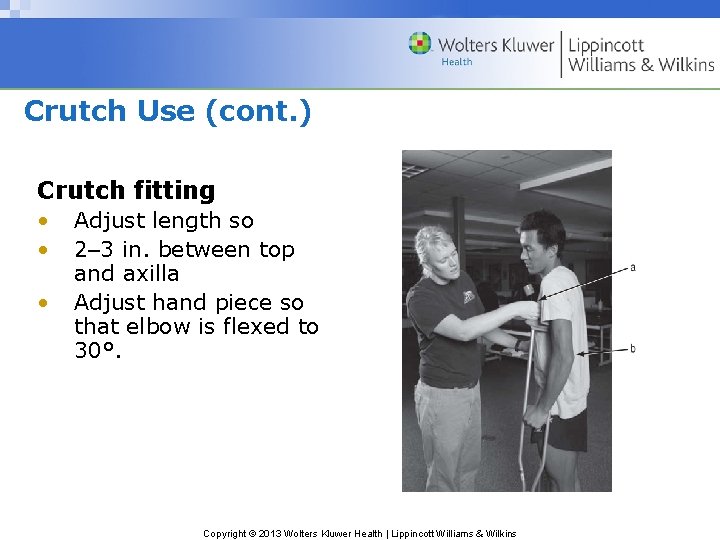
Crutch Use (cont. ) Crutch fitting • • • Adjust length so 2– 3 in. between top and axilla Adjust hand piece so that elbow is flexed to 30°. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
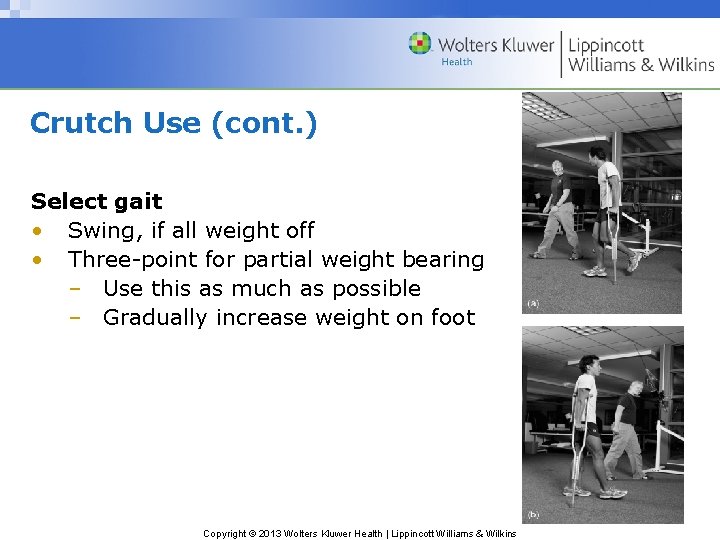
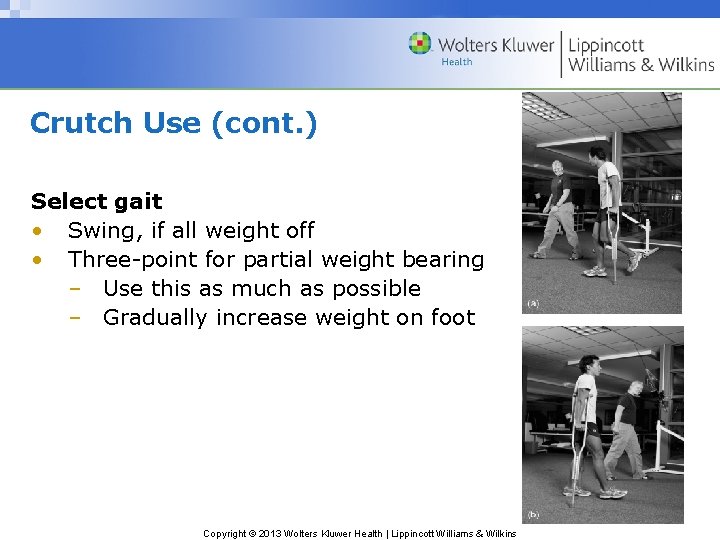
Crutch Use (cont. ) Select gait • Swing, if all weight off • Three-point for partial weight bearing – Use this as much as possible – Gradually increase weight on foot Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Crutch Use (cont. ) Walking instructions • Proper gait • Amount of weight on foot • Up and down stairs – The phrase “the good go up to heaven, the bad down to hell” may help you remember which foot or leg goes first when walking up and down stairs. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Crutch Use (cont. ) Observe patient walking • Proper gait • Adjust if necessary Periodic reevaluation Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Medicated Ice Cups • For skin abrasions – Clean wound – Apply antiseptic – Cool tissue Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Medicated Ice Cups (cont. ) Materials • Four 2 -oz disposable cups • 1 oz of 2% lidocaine • 3 oz of 10% povidine-iodine • 3 oz of distilled or boiled water • Plastic stir sticks (handle) • Adhesive tape (to secure stir sticks in the center of cup) Mix together and pour into cups. Secure sticks in center of each cup with tape. Label and freeze overnight. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
Medicated Ice Cups (cont. ) Medicated ice massage • Seek physician advice and approval before using. • Hold by stir stick and roll the ice back and forth along lacerated skin ~10 min. • As ice melts, medicines flow into wound. • Debride the area (remove foreign materials). • Treat and protect the area as any open wound, emphasizing sterility. • Apply an ice pack for 20– 30 min each hour and compression constantly. Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins
 Immediate and temporary care given
Immediate and temporary care given Immediate newborn care steps
Immediate newborn care steps Five initial steps of newborn care
Five initial steps of newborn care Immediate objectives
Immediate objectives Primary secondary tertiary care nursing
Primary secondary tertiary care nursing Post-acute care collaboration
Post-acute care collaboration Acute care toolkit
Acute care toolkit Nursing care plan for acute pancreatitis
Nursing care plan for acute pancreatitis A short backboard or vest-style immobilization
A short backboard or vest-style immobilization Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries 17:6 providing first aid for burns
17:6 providing first aid for burns Injuries to muscles and bones chapter 15
Injuries to muscles and bones chapter 15 Chapter 14:1 using body mechanics
Chapter 14:1 using body mechanics Chapter 14 bleeding shock and soft tissue injuries
Chapter 14 bleeding shock and soft tissue injuries Chapter 13:2 preventing accidents and injuries
Chapter 13:2 preventing accidents and injuries Chapter 11 injuries to the shoulder region
Chapter 11 injuries to the shoulder region Chapter 11 assessment and evaluation of sports injuries
Chapter 11 assessment and evaluation of sports injuries Chapter 12 lesson 1 benefits of physical activity
Chapter 12 lesson 1 benefits of physical activity Chapter 4 preventing injuries through fitness
Chapter 4 preventing injuries through fitness Chapter 13 worksheet recognizing different sports injuries
Chapter 13 worksheet recognizing different sports injuries Chapter 4 basics of tissue injuries
Chapter 4 basics of tissue injuries Shoulder orthopedic tests
Shoulder orthopedic tests Lumbar orthopedic tests
Lumbar orthopedic tests Uva powerpoint template
Uva powerpoint template 2 minute orthopedic exam
2 minute orthopedic exam Search engine optimization for orthopedic practices
Search engine optimization for orthopedic practices Orthopedic history taking
Orthopedic history taking Schepelmann orthopedic test
Schepelmann orthopedic test Dr. craig shank orthopedic surgery
Dr. craig shank orthopedic surgery Icats nhs
Icats nhs Causes of orthopedic impairment
Causes of orthopedic impairment Orthopedic case presentation
Orthopedic case presentation Orthopedic case presentation
Orthopedic case presentation Idea orthopedic impairment
Idea orthopedic impairment Lokmanya orthopedic hospital pune
Lokmanya orthopedic hospital pune Pediatric orthopedics near tracy
Pediatric orthopedics near tracy Dr todd wilcox
Dr todd wilcox Chapter 10 - sentence check 2 answer key
Chapter 10 - sentence check 2 answer key Common chronic and acute conditions chapter 18
Common chronic and acute conditions chapter 18 Makalu gau frostbite
Makalu gau frostbite Unit 15:7 providing first aid for heat exposure
Unit 15:7 providing first aid for heat exposure Why does katniss detest haymitch?
Why does katniss detest haymitch? Sentinel injuries in infants are
Sentinel injuries in infants are Westfield sports injuries
Westfield sports injuries Yorkhill minor injuries
Yorkhill minor injuries Pack-strap carry first aid
Pack-strap carry first aid Kristen wilson injuries
Kristen wilson injuries Uc davis web scheduler
Uc davis web scheduler An epidemiologic survey of roller skating injuries
An epidemiologic survey of roller skating injuries Climatic injuries
Climatic injuries Climatic injuries
Climatic injuries Bo taoshi injuries
Bo taoshi injuries Miniscal cyst
Miniscal cyst Preventing hand injuries
Preventing hand injuries Examples of intentional injury
Examples of intentional injury Glycerin and gelatin fake skin
Glycerin and gelatin fake skin Intentional fallacy
Intentional fallacy Injuries first aid
Injuries first aid Pa wc bureau
Pa wc bureau Injuries first aid
Injuries first aid Characters of firearm injuries
Characters of firearm injuries Which osha document summarizes occupational injuries
Which osha document summarizes occupational injuries Sports injuries angus, on
Sports injuries angus, on Fundamentals of throwing a football
Fundamentals of throwing a football What does jem realize when he pounds the rail
What does jem realize when he pounds the rail Common track injuries
Common track injuries Hunger games chapter 20 questions and answers
Hunger games chapter 20 questions and answers How are sports injuries classified and managed
How are sports injuries classified and managed Chop saw injuries
Chop saw injuries Deadly dozen itls
Deadly dozen itls Carl clinton construction
Carl clinton construction Immediate family meaning
Immediate family meaning Brainpop world war 2
Brainpop world war 2 Immediate cause of ww1
Immediate cause of ww1 Graduated rhythm in design
Graduated rhythm in design Transfusion en urgence vitale immédiate
Transfusion en urgence vitale immédiate Addressing modes of 8086
Addressing modes of 8086 Causes and effects of the french revolution
Causes and effects of the french revolution Four phases of the french revolution
Four phases of the french revolution Syntax adalah
Syntax adalah What was an immediate cause of the 1789 french revolution
What was an immediate cause of the 1789 french revolution Perpetuity immediate formula
Perpetuity immediate formula Immediate annuity formula
Immediate annuity formula Immediate memory test
Immediate memory test Forward pass
Forward pass Immediate predecessor in project management
Immediate predecessor in project management Immediate phase
Immediate phase Immediate reinforcers
Immediate reinforcers Hlt addressing mode
Hlt addressing mode Immediate constituent analysis
Immediate constituent analysis Immediate family definition
Immediate family definition Immediate mode ui
Immediate mode ui Rice first aid
Rice first aid Direct experience
Direct experience This line represents calm, peace, and relaxation.
This line represents calm, peace, and relaxation. Ter thin client
Ter thin client Consolidation settlement formula
Consolidation settlement formula Perpetuity immediate formula
Perpetuity immediate formula Deferred update and immediate update
Deferred update and immediate update Declaration of the immediate causes
Declaration of the immediate causes What were the immediate effects of reconstruction
What were the immediate effects of reconstruction