Orthopedic limitations and Hand Injuries Ch 41 and











- Slides: 42
Orthopedic limitations and Hand Injuries Ch 41 and 42 in Trombly OT 460 A
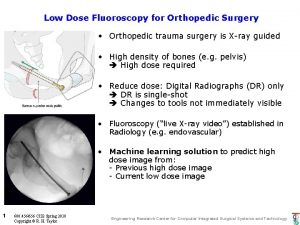
Orthopedic Conditions Caused by injuries, diseases and deformities of joints and related structures Caused by trauma, cumulative trauma, or congenital anomaly Rising incidence related to many competitive and recreational sports as well as increase in the elderly population and a concurrent home injuries and falls Prevention= jt protection, positioning Remediation= ROM, strength, nerve re-education 11/30/09 OT 460 A 2
Evaluation in OT Assessment of roles Controlled ROM w/in precautions Non-resistive activities for 1 st 4 -6 wks. Orthopedic protocol for specific condition/ specific physician ID tasks that client is having difficulty with Measure ROM early, strength later Note skin color, sensation, pain level, edema 11/30/09 OT 460 A 3
Intervention for fractures Medical Treatment Mobilization vs. Resting Splint, Cast, Brace, ORIF vs. External Fixator Early mobility when possible PROM, AAROM, AROM Splinting Scar tissue and wound management Connective tissue work Passive stretch, dynamic splinting, myofascial release 11/30/09 OT 460 A 4
Shoulder Fx Isometric exercises while immobilized moving toward isotonic ex Pain control Wall climbing Codmans exercises Scapular mobilization Jt. Replacements- AAROM daily, skateboard, Pulley 11/30/09 OT 460 A 5

Elbow Fx Complication: Volkmann’s ischemia Pale, bluish skin Absence of radial pulse Decreased hand sensation Splinting 90 -100 degrees of flexion Full ROM not always achieved 11/30/09 OT 460 A 6
Forearm fractures Radius or ulna short cast AROM as soon as possible per MD protocol Manage edema, pain, nerve damage 11/30/09 OT 460 A 7
Hip fractures Common in Older adults ORIF (femur fx) vs. THR Wt. Bearing status NWB, TTWB, PWB, 50% WB, FWB Precautions: No extremes in flexion, adduction, IR/ER Sleep w/abduction wedge Use LH equip for reaching, dressing, bathing 11/30/09 OT 460 A 8

Low Back Pain Acute pain- proportional to physical findings Chronic pain- lasts for months/ years Results in personality changes Disproportionate to physical problem Goal to get people back to function, manage pain, reduce illness behavior, reduce disuse 11/30/09 OT 460 A 9
Intervention for LBP Positioning Adaptive equipment Reconditioning Strengthening Environmental modification Body mechanics 11/30/09 OT 460 A 10
Body mechanics Neutral pelvis, prop foot Bend at the knees to lift, do half-kneel, squat or golfer’s lift Avoid twisting, excessive bending or reaching Sit to work if possible Balance load 11/30/09 OT 460 A 11

Hand Impairments Ch 42 in Trombly

Hand Therapy Originated during WWII Is done by OT/PT, nurses, orthopedics, Workman’s comp and voc specialists, PA CHT-Certified Hand Therapist- Must have 5 years working with hands. Sit for national exam by ASHT Though tx could focus on specific anatomic structures, the function is what’s important 11/30/09 OT 460 A 13
Psychosocial factors Adaptive responses Emotional factors Support systems Motivation Type of injury (e. g. traumatic vs. repetitive) 11/30/09 OT 460 A 14
Hand Therapy Concepts Tissue healing Antideformity positioning Attend to Pain PROM can be injurious Judicious use of heat & cold Isolated exercise vs. purposeful activity vs. therapeutic occupation 11/30/09 OT 460 A 15
Tissue Healing Sequence: Inflammation, fibroplasia, maturation and remodeling Vasoconstriction to vasodilation WBC’s promote phagocytes removing dead tissue or foreign body 11/30/09 OT 460 A 16
Interventions during tissue healing phases Inflammation phase: rest is advised, edema management, pain control and positioning Fibroplasia phase- starts at 4 days to 6 weeks. Formation of scar tissue. Begin AROM, Splint Maturation phase-may last for years. Gentle resistive activity, avoid inflammation, dynamic or static splinting, scar tissue management 11/30/09 OT 460 A 17

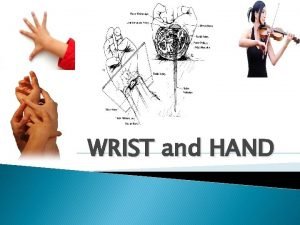
Antideformity Positioning Position to avoid: Wrist flexed, MP jts stiffen in hyperextension and DIP’s flexed, adducted thumb Called the Intrinsic Plus position Wrist in neutral or extension MP’s in Flexion IP’s in Extension Allows collateral ligaments at the MP joints and the volar plate at the IP joints to maintain their lengths Flexor and extensor tendon repair not conducive to these positions 11/30/09 OT 460 A 18
Attend to Pain Myth of No-Pain, No Gain Pain induced by therapy can cause CRPS or Complex regional pain syndrome Watch for pt’s body language, face, Use visual and verbal analog scales Change treatment to a “hand’s off approach” 11/30/09 OT 460 A 19

PROM Can be injurious to delicate tissues in the hand Can incite inflammation and trigger CRPS Gentle and Pain-Free Low load-long duration splinting may be more effective than PROM Can cause inflammation if PROM is done after heat application 11/30/09 OT 460 A 20

Judicious use of heat Do not use on inflamed or edematous extremities May degrade collagen and contribute to microscopic tears Heat can have a rebound effect, with stiffening following its use Use aerobic exercise to warm up tissue Elevate the extremity in conjunction with heat Monitor frequently for signs of inflammation 11/30/09 OT 460 A 21
Exercise vs. Occupation Isolate for discrete components that are involved Integrate pt directed goals into hand therapy Encourage use of UE in ADL’s Purposeful activity- not only exercise, produces coordinated movement patterns in multiple planes, leads to better movement quality Occupational as means-get benefit of improved quality of movement & return to occupation 11/30/09 OT 460 A 22
Evaluation in Hand Therapy History Injury, work and leisure interests, roles, Physician recommendations and precautions Pain Acute vs. chronic Intensity Type of pain Myofascial/ Trigger points vs. joint Analogs, draw on a body 11/30/09 OT 460 A 23
Evaluation (continued) Physical Exam Observe, Cervical screening, posture, guarding, atrophy, edema Wounds Universal precautions Stage, type, (red, yellow, black) Red-revascularizing Yellow-exuidate- needs cleansing and debreidment Black-necrotic- needs debriedment 11/30/09 OT 460 A 24
Evaluation (continued) Types of Debridement Chemical (e. g. peroxide) Manual (suture scissors, scrubbing) Surgical (scrubbing under anesthesia (burns) Scar Assessment Hypertrophic Tenodermodesis Contracture- wound or scar crossing a joint Mature- flat and softer and has neutral color, does not blanch to touch 11/30/09 OT 460 A 25
Evaluation Vascular Assessment Cyanosis, erythemia, pallor, gangrene, grayish, blanching within 2 seconds of release of pressure Edema Circumferential measurement Volumeter Range of Motion PROM, ROM TAM or TROM 11/30/09 OT 460 A 26

Evaluation (continued) Grip and Pinch 10 -15% difference in strength between dominant and non-dominant hands No relationship w/increase and increase function Bell shaped curve MMT Sensibility Dexterity and Hand function Jebsen MMRT Box and Block Purdue Pegboard Nine Hole 11/30/09 OT 460 A 27
Clinical Decision Making ADL and functional Implications Goals Quality of movement Structures Joint vs. musculotendinous Lag vs. contracture (extensor lag in spite of PROM available) Intrinsic vs. extrinsic tightness (PROM of DIP vs. PIP) Tightness of extrinsic extensors or extrinsic flexors 11/30/09 OT 460 A 28
Interventions Edema Elevation Compression Manual edema mobilization (different than retrograde massage) Lymphedema pumps 11/30/09 OT 460 A 29
Intervention (continued) Scar management Compression Silicone gel Manual edema mobilization vs. friction massage Tendon Gliding exercises (figure 42. 3) Blocking exercises Place and Hold End feel and Splinting 11/30/09 OT 460 A 30
Interventions Splinting Blocking Buddy strapping Dynamic vs. static 11/30/09 OT 460 A 31

Common conditions Stiff hand Result of fracture Decrease PROM/AROM if painful or swollen Static splinting during acute inflammatory phase, dynamic when joint has a soft end feel Tendonitis More than half of occupational illnesses Tx= RICE (rest, ice, compression, elevation) Splinting @ night Gradual mobilization balanced w/rest Prevent reinjury though education 11/30/09 OT 460 A 32
Types of Tendonitis Lateral Epicondylitis Proximal conditioning and scapular stabilizing Built up handles Splinting Counterforce strap-reduces load on the tendon Medial epicondylitis- Golfers elbow Involves the FCR Proximal conditioning, avoid end ranges, built up handles, and splinting as well as counterforce strap 11/30/09 OT 460 A 33
Types of Tendonitis De. Quervains Disease APL and EPB at first dorsal compartment Avoid wrist deviation (esp w/pinching) Forearm thumb spica Others (less common) Intersection syndrome EPL tendonitis ECU, FCR, FCU tendonitis Flexor Tendonsynovitis or trigger finger 11/30/09 OT 460 A 34

Nerve Injuries Median nerve compression- CTS Steroid injection Night splinting in neutral Exercises for tendon gliding Aerobic exercises Proximal conditioning Ergonomic modification Postural training 11/30/09 OT 460 A 35
Nerve Injuries (continued) Cubital Tunnel Syndrome Between the medial epicondyle and the olecranon Ulnar nerve entrapment Proximal and medial forearm pain Radial Nerve Compression Purely motor, inability to ext MP jts. Can be entrapped at the supinator muscle Nerve laceration Surgical intervention w/protective splinting Sensory re-ed Reduction/prevention of a neuroma 11/30/09 OT 460 A 36
Types of nerve injuries Low median- OP and APB of thumb Hi Median- FDP to IF and MF and DGS to all digits and pronation Low ulnar- intrinsic loss= claw hand Hi Ulnar- FDP of RF and SF and FDU Low radial-MP ext is affected Hi Radial-supinator, wrist and finger ext out 11/30/09 OT 460 A 37
Fractures Distal Radius fx- most common Scaphoid- FOOSH, may accompany EPL and EPB stretching and ligamentous injury. Avascular necrosis is a risk. Non Articular Hand Fx Distal phalanx, Middle, Proximal, Metacarpal Fx (Fixation with wires, screws) 11/30/09 OT 460 A 38
Collateral Ligament Injury PIP joint sprain Skier Thumb-collateral ligament of the thumb w/acute radial deviation Flexor Tendon Injury Zones of the hand Passive Flexion-active extension protocol Chow advocates early motion Extensor Tendon Injury Less common 7 zones in the dorsum of the hand In zones 3 and 4 can lead to boutonniere deformity Tenolysis- surgical procedure to release tendon adhesion. Therapy begins a few hours after surgery 11/30/09 OT 460 A 39

Complex Regional Pain Syndrome CRPS- used to be called RSD Type 1 - follows noxious event, pain, edema, abnormal skin color, pseudomotor activity Type 2 -develops after a nerve injury Pain is disproportionate to the injury Four cardinal symptoms Pain, swelling, stiffness, discoloration Secondary symptoms Osseous demineralization Sudomotor and temperature changes Trophic changes Vasomotor instability Palmar fascitis Pilomotor activity 11/30/09 OT 460 A 40
Management of CRPS Management of pain through medications, sympathetic blocks, modalities Vaso motor challenge through stress loading (scrubbing) change positions, temperature biofeedback, contrast, vibration, desensitization, water aerobics Patient Directed therapy 11/30/09 OT 460 A 41
Arthritis Osteoarthritis or DJD Heberden’s nodes (@ DIP) Bouchard’s nodes at the PIP Thumb CMC arthroplasty is common TX includes splinting, pain mgmt, jt. Prot. Rheumatoid (a systemic disease) Tx reduce inflammation Jt. Protection Splinting, Energy Conservation 11/30/09 OT 460 A 42
 Preventing hand injuries
Preventing hand injuries Lippman's test
Lippman's test Bragard test
Bragard test Uva template powerpoint
Uva template powerpoint 2 minute orthopedic exam
2 minute orthopedic exam Orthopedic search engine optimization
Orthopedic search engine optimization Orthopedic history taking
Orthopedic history taking Schepelmann's test
Schepelmann's test Dr. craig shank orthopedic surgery
Dr. craig shank orthopedic surgery Orthopedic icats
Orthopedic icats Causes of orthopedic impairment
Causes of orthopedic impairment Orthopedic case presentation
Orthopedic case presentation Orthopedic case presentation
Orthopedic case presentation Idea orthopedic impairment
Idea orthopedic impairment Lokmanya tilak hospital chinchwad
Lokmanya tilak hospital chinchwad Pediatric orthopedics near tracy
Pediatric orthopedics near tracy Dr wilcox orthopedic
Dr wilcox orthopedic What is it
What is it An hour hand
An hour hand Interrosei
Interrosei Mother father sister brother
Mother father sister brother Gang process chart
Gang process chart Abendrot eichendorff
Abendrot eichendorff Hand in hand module 1
Hand in hand module 1 Technology tools and equipment names
Technology tools and equipment names Put your left hand in
Put your left hand in Father mother sister brother hand in hand with one another
Father mother sister brother hand in hand with one another Right hand in the air left hand in the air
Right hand in the air left hand in the air Ape hand vs hand of benediction
Ape hand vs hand of benediction The push and pull method
The push and pull method Ulnar nerve special test
Ulnar nerve special test Hand by hand
Hand by hand Handsoft pro
Handsoft pro Unit 15:8 providing first aid for cold exposure
Unit 15:8 providing first aid for cold exposure A short backboard or vest-style immobilization
A short backboard or vest-style immobilization Chapter 21 caring for head and spine injuries
Chapter 21 caring for head and spine injuries Chapter 15 injuries to muscles and bones
Chapter 15 injuries to muscles and bones Chapter 14 promotion of safety
Chapter 14 promotion of safety Chapter 14 bleeding shock and soft tissue injuries
Chapter 14 bleeding shock and soft tissue injuries Chapter 13:2 preventing accidents and injuries
Chapter 13:2 preventing accidents and injuries Chapter 11 assessment and evaluation of sports injuries
Chapter 11 assessment and evaluation of sports injuries Chapter 12 lesson 3 planning a personal activity program
Chapter 12 lesson 3 planning a personal activity program Common track and field injuries
Common track and field injuries