Chapter 24 Hematologic Emergencies National EMS Education Standard
- Slides: 88
Chapter 24 Hematologic Emergencies
National EMS Education Standard Competencies Medicine Integrates assessment findings with principles of epidemiology and pathophysiology to formulate a field impression and implement a comprehensive treatment/disposition plan for a patient with a medical complaint.
National EMS Education Standard Competencies Hematology • Anatomy, physiology, pathophysiology, assessment, and management of: − Sickle cell crisis − Clotting disorders
National EMS Education Standard Competencies • Anatomy, physiology, epidemiology, pathophysiology, psychosocial impact, presentations, prognosis, and management of common or major hematological diseases and/or emergencies − − Sickle cell crisis Blood transfusion complications Hemostatic disorders Lymphomas
National EMS Education Standard Competencies • Anatomy, physiology, epidemiology, pathophysiology, psychosocial impact, presentations, prognosis, and management of common or major hematological diseases and/or emergencies (cont’d) − Red blood cell disorders − White blood cell disorders − Coagulopathies
Introduction • EMS systems rarely respond to hematologic emergencies. • Hematologic disorder: any disorder of the blood − Hemolytic disorders − Hemostatic disorders
Introduction • Hematopoietic system − Organs and tissues involved in the production of blood components
Blood and Plasma • Blood performs the following functions: − Respiratory − Nutritional − Excretory − Regulatory − Defensive
Blood and Plasma • Blood is made of: − Plasma: • 92% water • 55% of total blood volume − Formed elements: • 45% of total blood volume • Includes RBCs, WBCs, and platelets
Blood and Plasma • The production of RBCs occurs within stem cells. − Stimulated by erythropoietin − Five days to mature • Average life span: 4 months − Hemoglobin carries oxygen to the tissues.
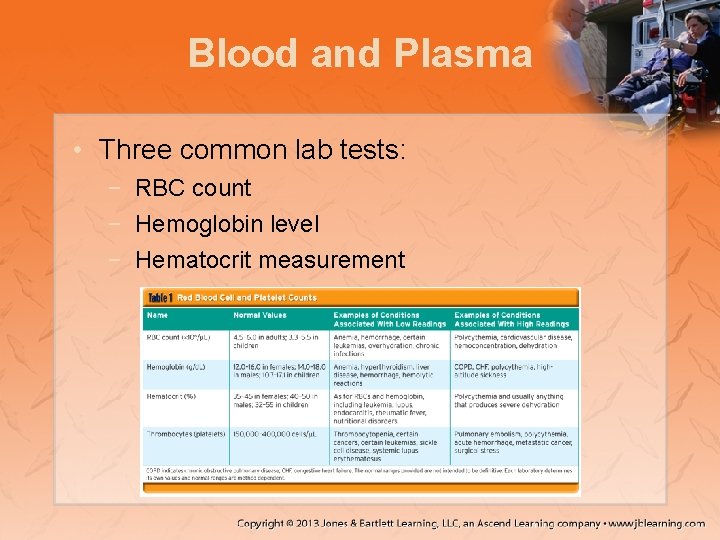
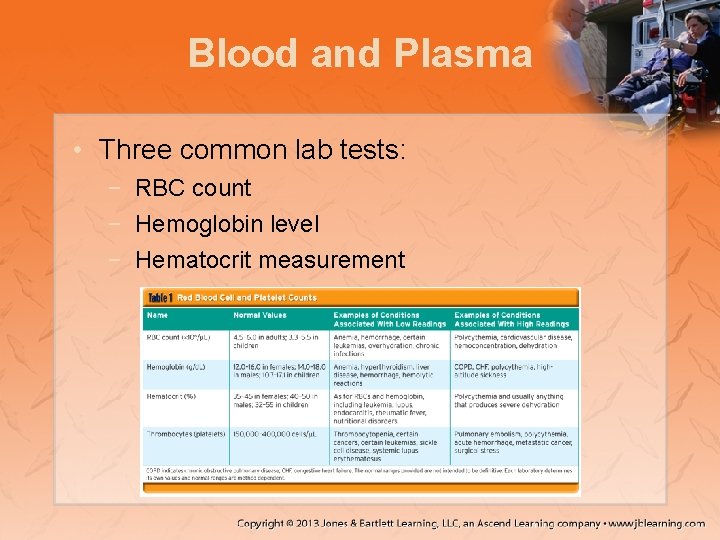
Blood and Plasma • Three common lab tests: − RBC count − Hemoglobin level − Hematocrit measurement
Blood and Plasma • White blood cells − Larger than RBCs − Immunity against “foreign invaders” − Derived from stem cells − Several types • Platelets − Smallest formed element − Clot the blood • Hemostasis − Two thirds circulate through the blood.
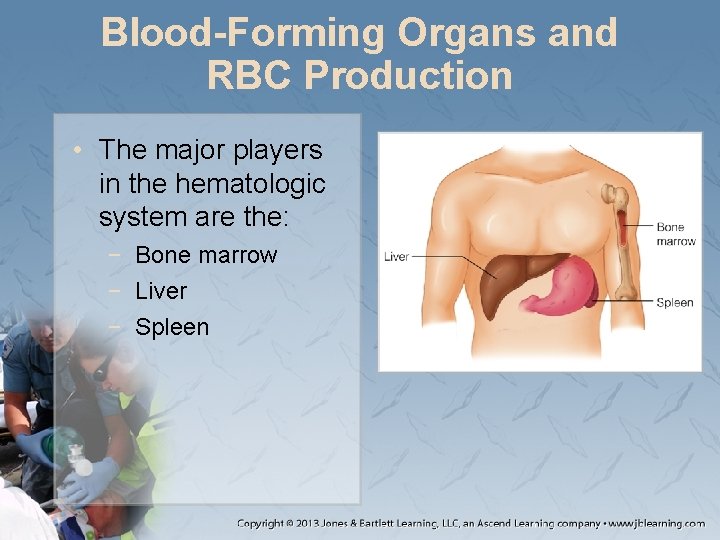
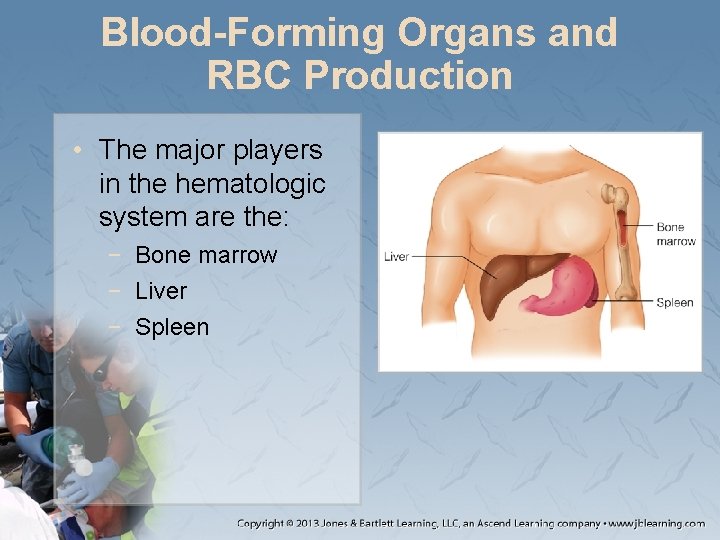
Blood-Forming Organs and RBC Production • The major players in the hematologic system are the: − Bone marrow − Liver − Spleen
The Inflammatory Process • All of the body’s cells and blood contain antigens at birth. − Antigens activate the immune system. • Autoimmune diseases − Identify the body’s own antigen as foreign
The Immune System • Processes protect against pathogens and other unwanted materials. − Must distinguish between: • Body’s own tissue • Outside organs
The Immune System • Native immunity − Nonspecific, maximal response − First line of defense − Associated with initial inflammatory response • Acquired immunity − Specific to vertebrates − A pathogenspecific response
The Immune System • Humoral immunity − Secretion of immunoglobins • Recognizes a specific antigen • Cell-mediated immunity − Macrophages and T-cells destroy pathogens.
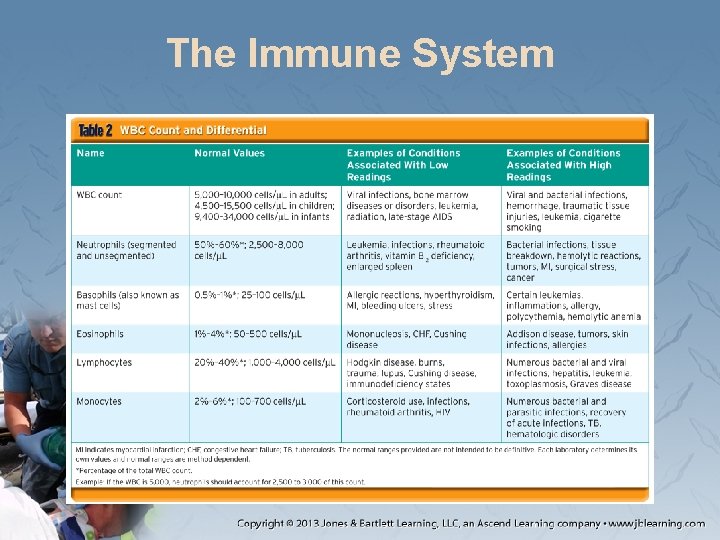
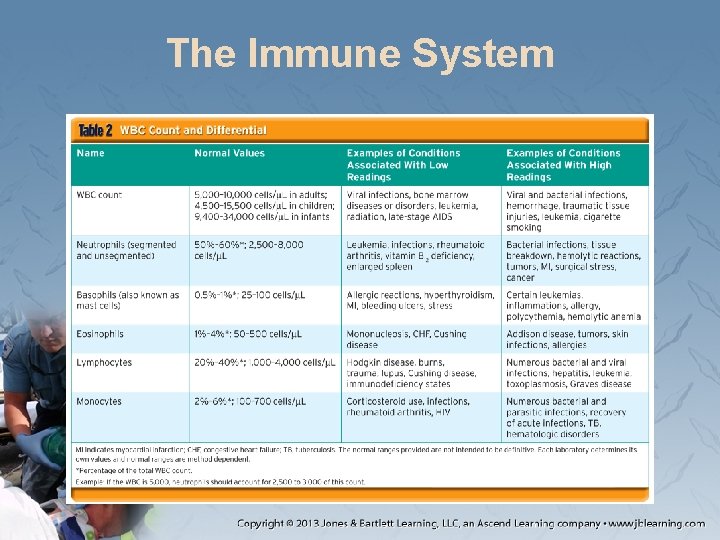
The Immune System • White blood cells − Produced in the bone marrow − Laboratory values provide information on the immune system. − Baseline count is normally 5, 000– 10, 000 cells/µL.
The Immune System
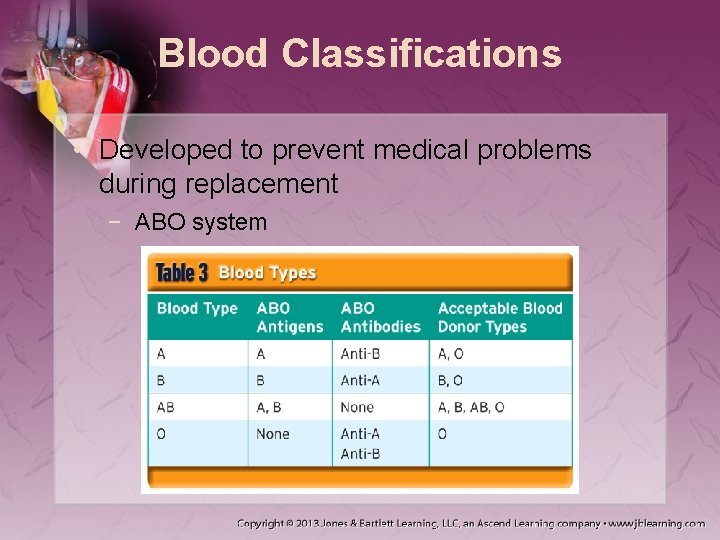
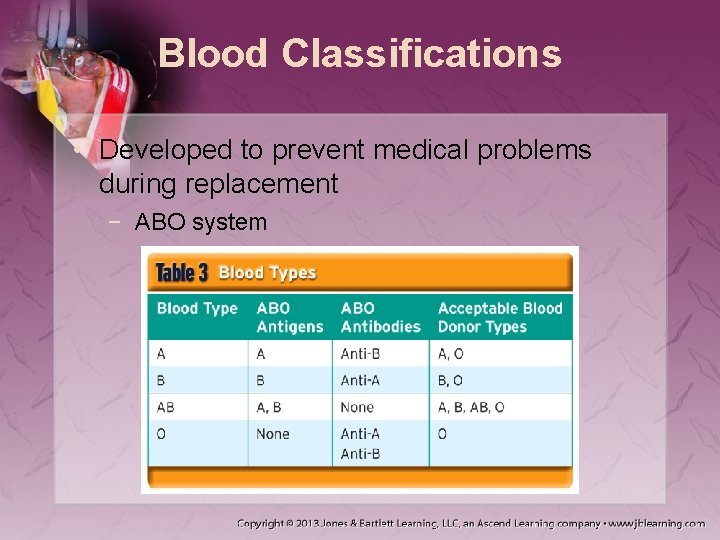
Blood Classifications • Developed to prevent medical problems during replacement − ABO system
Blood Classifications • Blood contains a secondary antigen called the Rh antigen. − Possible complications in pregnancy • Hemolytic disease
Hemostasis • The process of stopping bleeding through: − Vasoconstriction (immediate response) − Platelet plugging − Coagulation • Clots are made up of fibrin.
Hemostasis • Clotting cascade − Can be initiated through: • Intrinsic pathway • Extrinsic pathway − Coagulopathy: process that interferes with the clotting cascade or hemostasis
Patient Assessment • Note any lifethreatening signs or symptoms. − Ask about patient’s history and SAMPLE history. − A nonjudgmental approach is essential.
Scene Size-Up • Ensure the scene is safe for entry. • Consider the mechanism of injury. • Determine the number of patients. • Assess for hazards.
Primary Assessment • An African American or Mediterranean patient reporting severe pain may have sickle cell disease. − Perform cervical spine stabilization if necessary.
Primary Assessment • Form a general impression. − Perform a rapid scan and determine LOC. • Airway and breathing − Inadequate breathing or altered mental status should receive high-flow oxygen or ventilation.
Primary Assessment • Circulation − Manage life-threatening conditions. − If hemophilia is suspected, watch for: • Acute blood loss • Bleeding of unknown origin • Hypoxia or shock
Primary Assessment • Transport decision − Depends on severity and patient’s wishes − Transport to the closest facility if: • Sickle cell crisis • Uncontrolled bleeding
History Taking • Obtain patient and SAMPLE history. • Do not take a sickle cell crisis lightly. − Life-threatening situations, characterized by: • Signs of pneumonia • Swelling of fingers and toes • Jaundice
History Taking • Look for: − − − Changes in LOC Vertigo Feelings of fatigue Syncope Dyspnea Chest pain − Changes in pulse rate and rhythm − Coughing up blood − Visual disturbances − Muscle pain − Stiffness
History Taking • Is pain isolated or felt throughout? • Has the patient experienced: − − − Skin changes? Bleeding? History of liver problems? Pain for unknown reasons? Genitourinary or gastrointestinal problems?
History Taking • If known sickle cell disease, ask: − − Have you had a crisis before? When was the last time? How did it resolve? Have you had any illness, unusual amount of activity, or stress lately?
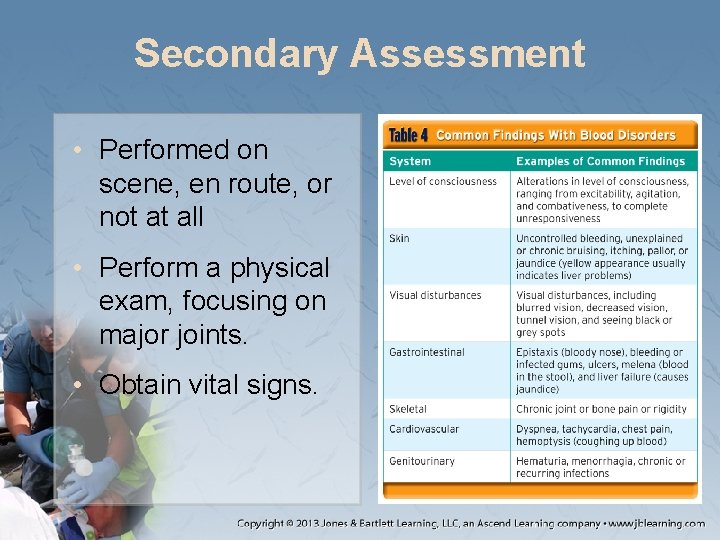
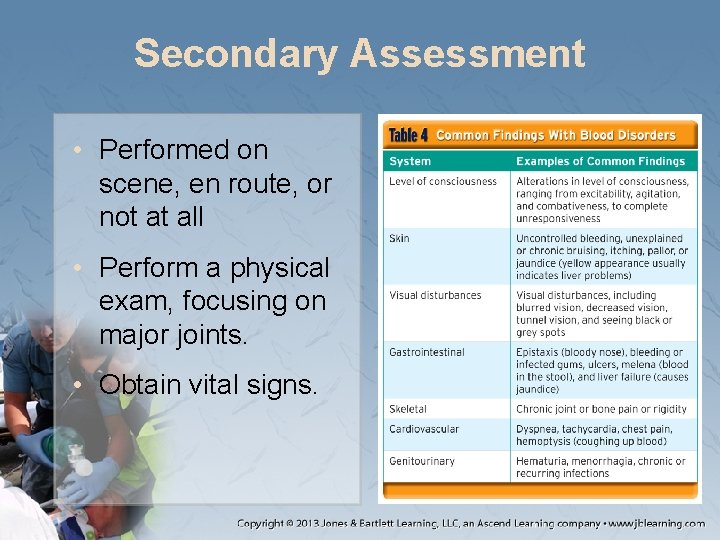
Secondary Assessment • Performed on scene, en route, or not at all • Perform a physical exam, focusing on major joints. • Obtain vital signs.
Secondary Assessment • Evaluate and documental status. • In patients experiencing a sickle cell crisis: − Respirations are normal to rapid. − Pulse is weak and rapid. − Skin is pale and clammy with low blood pressure.
Reassessment • Reassess frequently. • Administer supplemental oxygen. • Provide ventilation as appropriate. • Cover to maintain body temperature.
Reassessment • According to local protocol, administer: − IV fluid − Nitrous oxide • Prehospital care for hemophilia can include IV therapy.
Reassessment • Inform hospital staff about: − Patient history − Present situation − Assessment findings − Interventions and their results • Document: − − Each assessment Your findings Treatment Time of interventions − Changes in patient condition
Emergency Medical Care • Emergency medical care should include: − − − Oxygen Fluids ECG Comfort Pharmacology Support
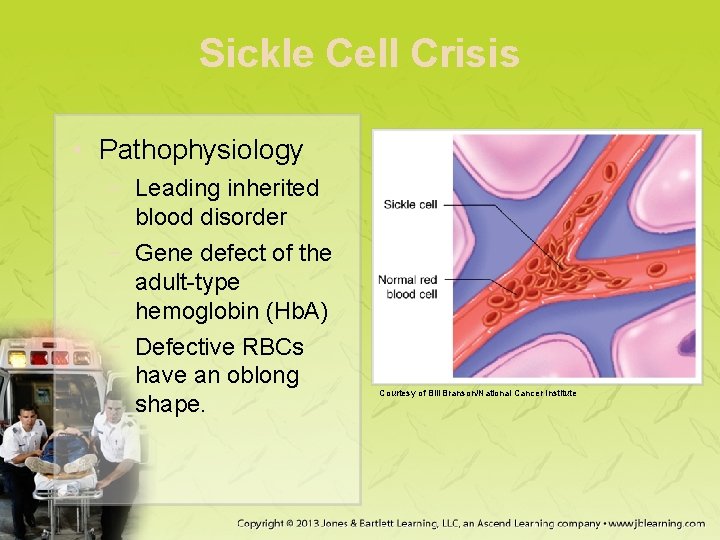
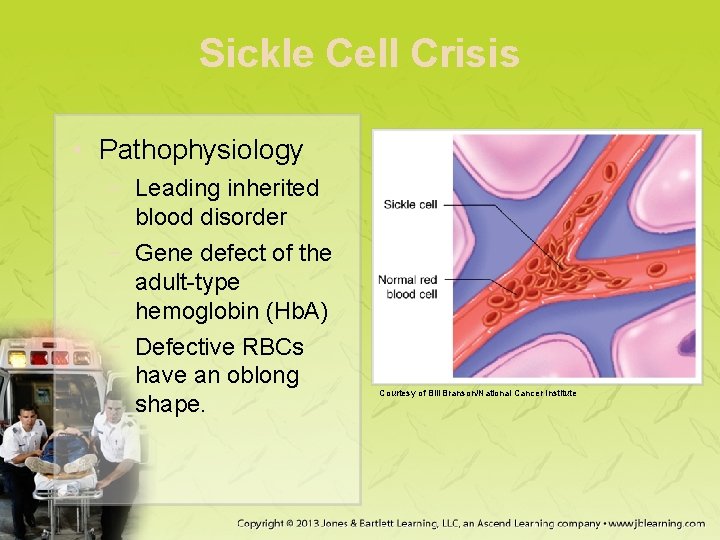
Sickle Cell Crisis • Pathophysiology − Leading inherited blood disorder − Gene defect of the adult-type hemoglobin (Hb. A) − Defective RBCs have an oblong shape. Courtesy of Bill Branson/National Cancer Institute
Sickle Cell Crisis • Pathophysiology (cont’d) − Can lead to: • Aplastic crisis: RBC production temporarily stops. • Hemolytic crisis: Acute RBC destruction
Sickle Cell Crisis • Pathophysiology (cont’d) − May manifest as: • Vaso-occlusive crisis • Acute chest syndrome • Splenic sequestration crisis
Sickle Cell Crisis • Assessment − Characterizations may include: • • Shortness of breath Inadequate perfusion of the skin Jaundice Mild dehydration
Sickle Cell Crisis • Assessment (cont’d) − Patients may have significant pain. • Pediatric patients typically present with pain in the hands and feet. • Adults typically report back and proximal extremity pain.
Sickle Cell Crisis • Management − − − Administer high levels of oxygen. Rapidly transport patient. Consider IV fluid therapy. Maintain patient’s body temperature. Recommend that patient rest.
Anemia • Pathophysiology − Low hemoglobin or erythrocyte level − Usually associated with an underlying disease
Anemia • Iron deficiency anemia − Most common type − Causes include: • Gastrointestinal blood loss • Menstrual bleeding • Frequent donations or diagnostic test
Anemia • Pathophysiology (cont’d) − May be caused by an inherited hemolytic disorder or a hematologic disorder − Can have serious consequences in high altitudes
Anemia • Assessment − Patients may feel: • • Worn down Lack of energy Overexerted Unable to “catch their breath” − Patients may have: • Anginal-type chest pain • Leukopenia • Thrombocytopenia
Anemia • Management − − Check and monitor airway breathing. Check vital signs frequently. For chest pain, apply a cardiac monitor. Blood pressure management and fluid replacement may be needed.
Anemia • Management (cont’d) − Allow the patient to rest. − Consider rapid transport for: • Abrupt change in consciousness • Hypotension • Significant perfusion inadequacies
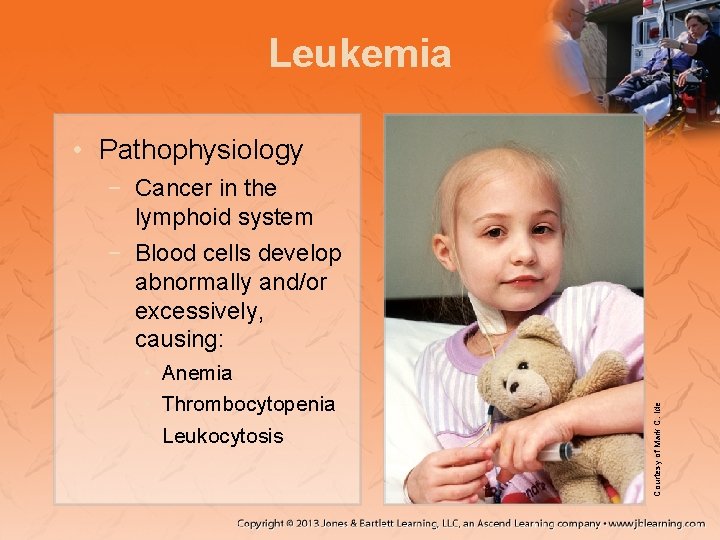
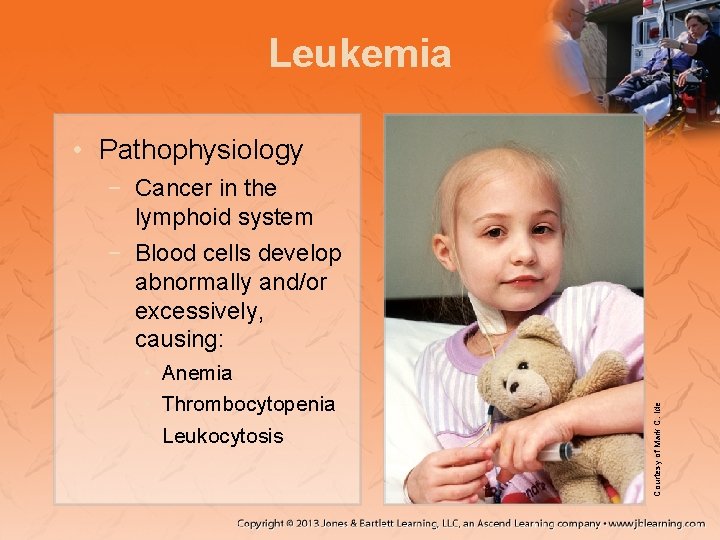
Leukemia • Pathophysiology • Anemia • Thrombocytopenia • Leukocytosis Courtesy of Mark C. Ide − Cancer in the lymphoid system − Blood cells develop abnormally and/or excessively, causing:
Leukemia • Pathophysiology (cont’d) − Acute leukemia: Bone marrow is replaced with abnormal lymphoblasts − Chronic leukemia: Abnormal cells accumulate in: • • Bone marrow Lymph nodes Spleen Peripheral blood
Leukemia • Pathophysiology (cont’d) − Survival depends on several factors: • Stage of detection • Underlying medical condition • Response to treatment − Treated with chemotherapy and radiation
Leukemia • Assessment − Patient presentation depends on: • Stage of leukemia • Current treatment − Patients may present with: • • Fatigue Headaches Bone pain Unexplained bleeding
Leukemia • Management − As appropriate, provide: • • • Airway support Oxygen therapy IV fluid therapy Analgesics Positive support
Leukemia • Management (cont’d) − You may be called because loved ones are uncertain about what to do. • Discuss with medical control. • Document all findings. • Have a refusal/release form signed.
Lymphomas • Pathophysiology − Group of malignant diseases within the lymphoid system − Classified in two categories
Lymphomas • Non-Hodgkin − Any age − Can be hereditary − Characterized by progression • Indolent • Aggressive • Highly aggressive • Hodgkin: − Progressive enlargement of lymphoid glands − Highly rare − Peaks between: • 15– 35 years of age • After age 55– 60
Lymphomas • Assessment − Require chemotherapy or radiation. − Signs and symptoms may include: • • Pallor Feeling hot and then cold or both Inadequate perfusion Abnormal ECG rhythms
Lymphomas • Management − Aggressive pain management − Treat inadequate perfusion and abnormal heart rhythms. − Initiate rapid transport if condition does not improve.
Polycythemia • Pathophysiology − − Overabundance or overproduction of RBCs Multiple causes Can lead to other conditions Treatment usually includes phlebotomy or cancer-type therapy
Polycythemia • Assessment − Findings may widely vary − Note the extent and duration of dyspnea. − Has the patient experienced pruritus or changes in skin temperature?
Polycythemia • Management − Consists of supportive care and transport to the appropriate facility. − Administer oxygen and establish IV as needed.
Disseminated Intravascular Coagulation • Pathophysiology − Number of causes − Two stages: • Defibrination • Uncontrolled hemorrhage − High mortality rate
Disseminated Intravascular Coagulation • Assessment − Identify associated signs and symptoms. − Patients may have: • Respiratory difficulty • Signs of shock • Skin changes
Disseminated Intravascular Coagulation • Management − Identify underlying cause and establish treatment early. − Maintain an airway. − Treat for shock.
Hemophilia • Pathophysiology − A bleeding disorder in which clotting: • Does not occur • Occurs insufficiently − Two primary types: A and B
Hemophilia • Pathophysiology (cont’d) − Signs and symptoms may include: • Acute and chronic bleeding − Patients may require: • Hospitalization for transfusion • Infusion of factors VIII and IX
Hemophilia • Assessment − − Take care of the ABCs. Be alert for signs of acute blood loss. Note any bleeding of unknown origin. Patients may show signs of hypoxia.
Hemophilia • Management − − Patients may need high-flow oxygen. Note ECG findings. IV therapy may be necessary. Analgesics may be appropriate.
Multiple Myeloma • Pathophysiology − Number of plasma cells in the bone marrow increase abnormally • Forms tumors in the bone • Results in anemia and susceptibility to infection
Multiple Myeloma • Pathophysiology (cont’d) − Neoplastic cells may accelerate protein development in the bloodstream. − Patients may have weakness in the bones. − Chemotherapy and other anticancer treatment may be given.
Multiple Myeloma • Assessment − Findings depend on stage − Early stage: • Fatigue • Mild pain − Later stage: • • Hemorrhage Weight loss Bone fractures Pain
Multiple Myeloma • Management: − IV therapy − Pain management − Supportive care
Transfusion Reactions • Pathophysiology − Similar to anaphylactic reaction − Monitor a patient receiving a blood transfusion very closely for the first 30– 60 minutes − Occurs when a patient receives a blood type different than their own
Transfusion Reactions • Assessment − Symptoms can be subtle in patients who are unresponsive or intubated. − An acute reaction may include a rapid onset of: • Chills • Back pain • Hypotension
Transfusion Reactions • Assessment (cont’d) − Complications include: • • • Hemolytic Febrile Allergic Transfusion-related lung injury Circulatory overload Bacterial infection
Transfusion Reactions • Management − Immediately stop the transfusion. − Provide hemodynamic supportive care. − Maximize kidney perfusion.
Transfusion Reactions • Management (cont’d) − A hemodynamically unstable patient requires: • Early invasive monitoring • Vasopressors • Promotion of diuresis − Administer high-flow oxygen.
Summary • Most EMS systems rarely respond to hematologic emergencies. • Blood performs respiratory, nutritional, excretory, regulatory, and defensive functions. • Blood is made up of plasma and formed elements, including RBCs, WBCs, and platelets.
Summary • Common lab blood tests are RBC count, hemoglobin level, and hematocrit measurement. • Blood tests measuring subtypes of WBCs can provide valuable information about the status of the immune system. • The ABO system is commonly used to classify blood types.
Summary • During the primary assessment, note any signs and symptoms that may be immediately life threatening. • While taking a history and during the secondary assessment, look for changes in the level of consciousness. • General blood disorder management should include oxygen, fluids, ECG, transport, medications, and psychological support.
Summary • Hematologic disorders include sickle cell crisis, anemia, leucopenia, thrombocytopenia, leukemia, lymphomas, polycythemia, DIC, hemophilia, multiple myeloma, and complications of blood transfusions.
Summary • A patient experiencing a sickle cell crisis will experience significant pain. • A patient with anemia has a low hemoglobin or RBC level. • Leukopenia is a reduction in the number of WBCs. Thrombocytopenia is a reduction in the number of platelets. • Leukemia is a cancer that affects the production of WBCs.
Summary • Lymphomas are a group of malignant disorders that occur within the lymphoid system. The two types are non-Hodgkin (most common) and Hodgkin lymphoma. • Polycythemia is an overabundance or overproduction of RBCs. • Disseminated intravascular coagulation (DIC) may result from a massive injury, sepsis, or obstetric complications.
Summary • Hemophilia is a bleeding disorder in which clotting does not happen or is insufficient. • Multiple myeloma is a cancer of the bone marrow caused by malignant plasma cells. • Complications of blood transfusions are similar to anaphylactic reactions. They are caused by a mismatch of the patient’s blood type to that received, or an allergic reaction to preservatives or agents in the transfused product.
Credits • Chapter opener: © Monkey Business Images/Shutter. Stock, Inc. • Backgrounds: Orange—© Keith Brofsky/ Photodisc/Getty Images; Blue—Courtesy of Rhonda Beck; Lime—© Photodisc; Purple— Courtesy of Rhonda Beck. • Unless otherwise indicated, all photographs and illustrations are under copyright of Jones & Bartlett Learning, courtesy of Maryland Institute for Emergency Medical Services Systems, or have been provided by the American Academy of Orthopaedic Surgeons.