Chapter 10 Medical Emergencies National EMS Education Standard

- Slides: 70
Chapter 10: Medical Emergencies
National EMS Education Standard Competencies (1 of 6) Medicine Recognizes and manages life threats based on assessment findings of a patient with a medical emergency while awaiting additional emergency response.
National EMS Education Standard Competencies (2 of 6) Medical Overview Assessment and management of a • Medical complaint Neurology Anatomy, presentations, management of • Decreased level of responsiveness • Seizure • Stroke
National EMS Education Standard Competencies (3 of 6) Abdominal and Gastrointestinal Disorders • Anatomy, presentations, and management of shock associated with abdominal emergencies • Gastrointestinal bleeding Endocrine Disorders Awareness that • Diabetic emergencies cause altered mental status (AMS)
National EMS Education Standard Competencies (4 of 6) Cardiovascular Anatomy, signs, symptoms, and management • Chest pain • Cardiac arrest
National EMS Education Standard Competencies (5 of 6) Respiratory Anatomy, signs, symptoms, and management of respiratory emergencies including those that affect the • Upper airway • Lower airway
National EMS Education Standard Competencies (6 of 6) Genitourinary/Renal • Blood pressure assessment in hemodialysis patients
Introduction (1 of 2) • Common medical conditions include – Angina pectoris – Heart attack – Dyspnea – Asthma – Stroke – Hypoglycemia and diabetic coma – Abdominal pain
Introduction (2 of 2) • Emergency medical responders (EMRs) can prepare to treat medical patients by studying the signs, symptoms, and treatments of each condition.
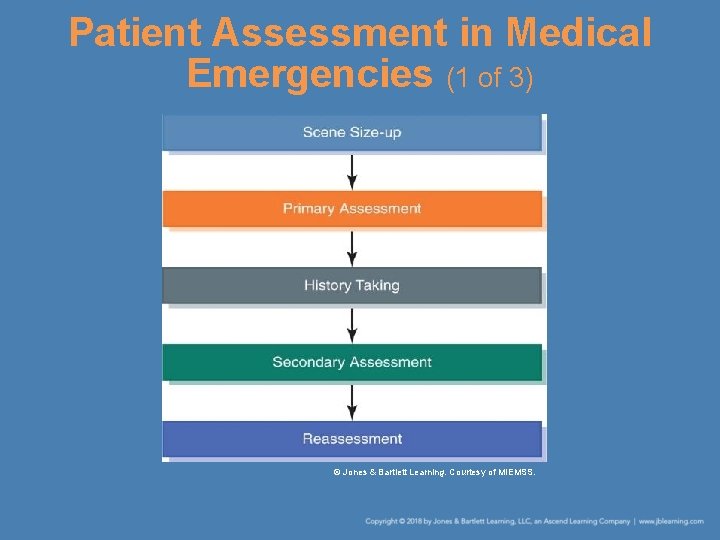
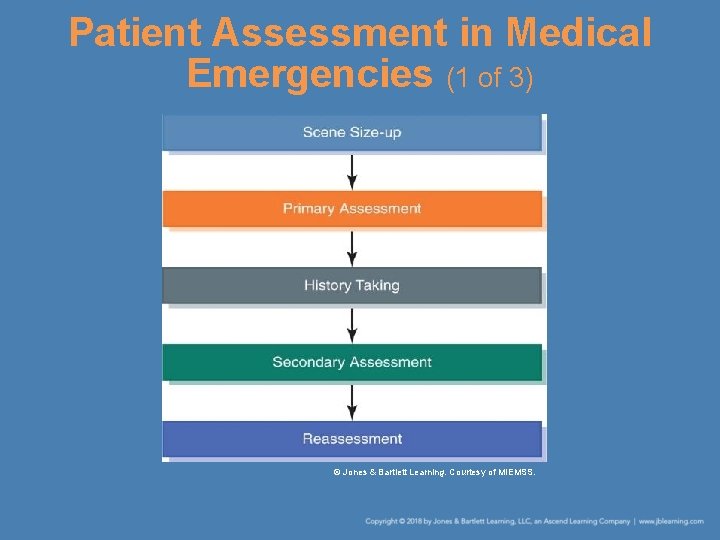
Patient Assessment in Medical Emergencies (1 of 3) © Jones & Bartlett Learning. Courtesy of MIEMSS.
Patient Assessment in Medical Emergencies (2 of 3) • Review the dispatch information. • Carefully assess the scene to identify safety issues. • As you perform the primary assessment – Try to form an impression of the problem first. – Then, determine the patient’s responsiveness, introduce yourself, check the ABCs, and acknowledge the chief complaint.
Patient Assessment in Medical Emergencies (3 of 3) • Usually, it is best to obtain a medical history on a medical patient before you perform the secondary assessment. – Use the SAMPLE history format. – Obtain the patient’s vital signs. • Monitor the patient through ongoing reassessment. • Remember to reassure the patient.
General Medical Conditions • General medical conditions may have different causes, yet result in similar signs and symptoms. • Initial treatment can stabilize the patient until other emergency medical services (EMS) and hospital personnel can take over.
Altered Mental Status (1 of 5) • Sudden or gradual decrease in the patient’s level of responsiveness • Use the AVPU scale to assess mental status: – Alert – Verbal – Pain – Unresponsive

Altered Mental Status (2 of 5) • When assessing the patient’s mental status, consider two factors: – The patient’s initial level of consciousness – Any change in that level of consciousness
Altered Mental Status (3 of 5) • Conditions causing an altered level of consciousness – Head injury – Shock – Decreased level of oxygen to the brain – Stroke – Slow heart rate – High fever
Altered Mental Status (4 of 5) • Conditions causing an altered level of consciousness (cont’d) – Infection – Poisoning – Low level of blood glucose – Insulin reaction – Psychiatric condition
Altered Mental Status (5 of 5) • Initial treatment – Maintain the patient’s ABCs and normal body temperature. – Keep the patient from additional harm. – If the patient is unconscious and has not sustained trauma, place the patient in the recovery position or use an airway adjunct. – Be prepared to suction.
Seizures (1 of 6) • Caused by sudden episodes of uncontrolled electrical impulses in the brain • Generalized seizures – Produce shaking movements – Involve the entire body – Last 1 to 2 minutes – Usually leave patients unconscious
Seizures (2 of 6) • Generalized seizures caused by a sudden high fever – Called febrile seizures – Occur in infants and young children • Absence seizures – Result in only a brief lapse of consciousness – Patients may blink, stare vacantly, or jerk one part of their body
Seizures (3 of 6) • Monitor the patient’s ABCs and arrange for transport. • Seizures can be caused by – Epilepsy – Trauma – Head injury – Stroke – Shock
Seizures (4 of 6) • Seizures can be caused by (cont’d) – Decreased level of oxygen to the brain – High fever – Infection – Poisoning – Overdose of drugs or alcohol – Brain tumor or infection – Diabetic emergencies – Complication of pregnancy
Seizures (5 of 6) • Treatment – Usually, the seizure will be over by the time you arrive at the scene. – If it has not ended, focus on protecting the patient from injury. – Once the seizure stops, ensure an open airway and place the patient in the recovery position.
Seizures (6 of 6) • Treatment (cont’d) – If the patient does not resume breathing, begin mouth-to-mask or mouth-to-mouth breathing. – Administer supplemental oxygen as soon as it is available. – After the seizure, move the patient to a more comfortable, private place.
Specific Medical Conditions • You will find it helpful to be knowledgeable about some of the more specific medical conditions you may encounter as an EMR. • This information will help you assess, treat, and communicate more effectively with patients.
Heart Conditions • The heart must receive a constant supply of oxygen or it will die. • The heart receives its oxygen through a complex system of coronary arteries. – These arteries may narrow as a result of atherosclerosis. – Progressive atherosclerosis can cause angina pectoris, heart attack, and cardiac arrest.
Angina Pectoris (1 of 2) • Chest pain caused by an inadequate flow of blood and oxygen to the heart muscle • Often described as pressure or heavy discomfort • The patient is often short of breath and sweating, is extremely frightened, and has a sense of doom.
Angina Pectoris (2 of 2) • Ask if the patient is already being treated for a heart condition and has nitroglycerin. – Assist the patient in taking one pill or administering the aerosol spray. – If the pain has not lessened 5 minutes after the first dose, help the patient take another. – If the pain has not lessened 5 minutes after the second dose, assume the patient is having a heart attack and transport promptly.
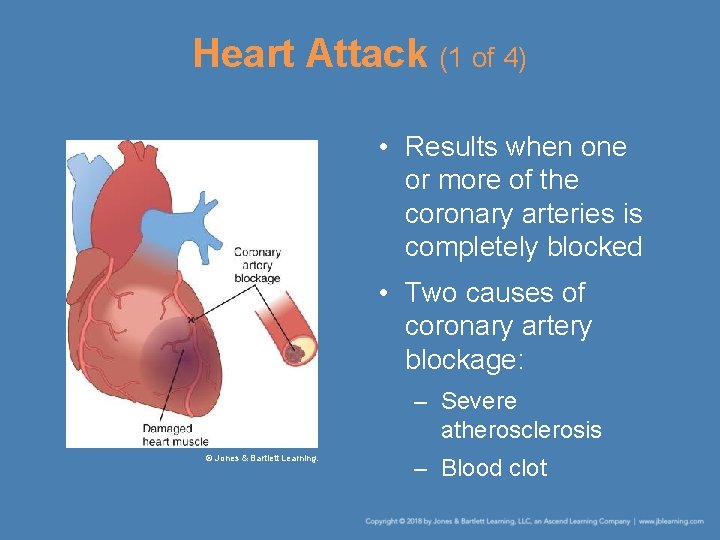
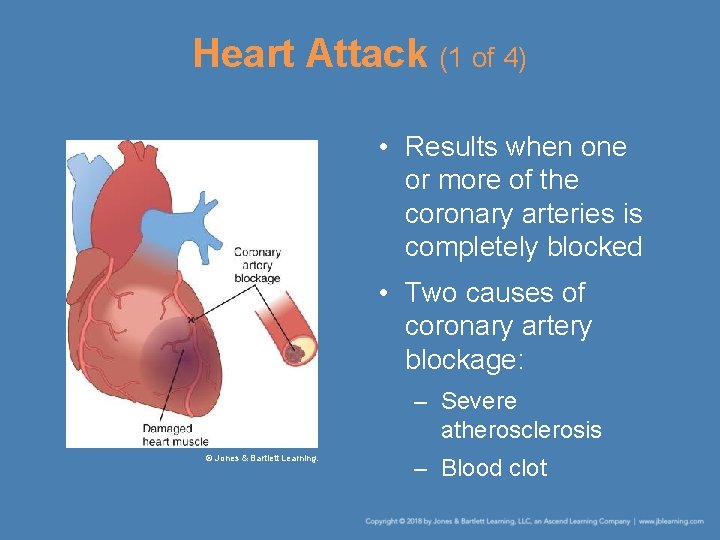
Heart Attack (1 of 4) • Results when one or more of the coronary arteries is completely blocked • Two causes of coronary artery blockage: – Severe atherosclerosis © Jones & Bartlett Learning. – Blood clot
Heart Attack (2 of 4) • Signs of heart attack include – The patient suffers immediate and severe pain. – The pain may radiate from the chest to the left arm or to the jaw or to the back. – The patient is usually short of breath, weak, sweating, and nauseated and may vomit. – If the blocked area is critical or large, the heart may stop completely.
Heart Attack (3 of 4) • Complete cessation of heartbeat is called cardiac arrest. – Cardiopulmonary resuscitation (CPR) is your first emergency treatment. • Take the following actions: – Summon additional help. – Talk to the patient to relieve his or her anxiety. – Touch the patient to establish a bond. – Reassure the patient.
Heart Attack (4 of 4) • Take the following actions: (cont’d) – Move the patient as little as possible. – Place the patient in the most comfortable position. – Help the patient take one adult aspirin or 2 -4 low -dose aspirins. – Administer oxygen if it is available. – Be prepared to administer CPR. – If an automated external defibrillator (AED) is available, have it brought to the patient and make sure it is ready for use.
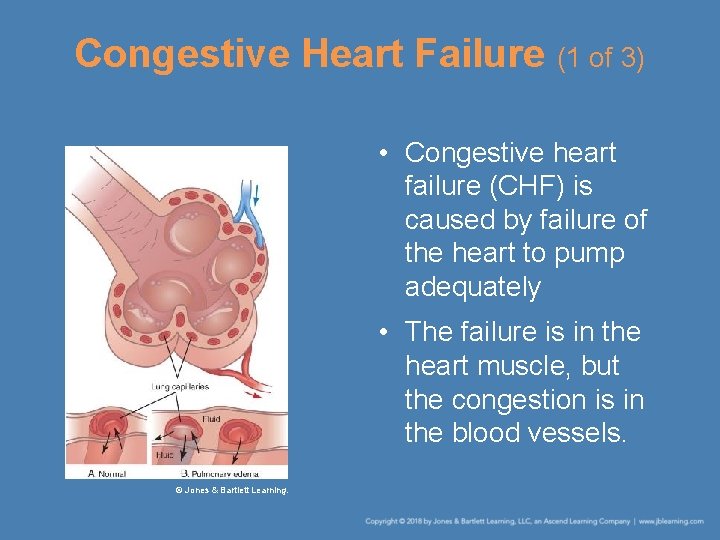
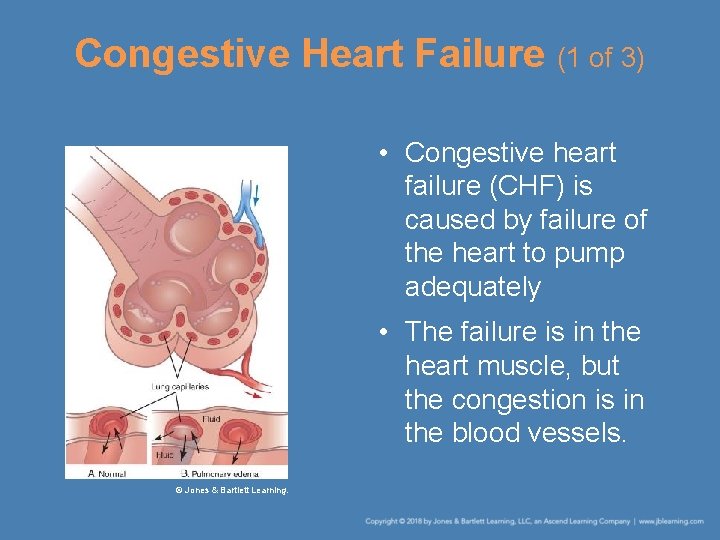
Congestive Heart Failure (1 of 3) • Congestive heart failure (CHF) is caused by failure of the heart to pump adequately • The failure is in the heart muscle, but the congestion is in the blood vessels. © Jones & Bartlett Learning.
Congestive Heart Failure (2 of 3) • Signs and symptoms – Breathing difficulty (major symptom) – Rapid, shallow breathing – Moist or gurgling respirations – Profuse sweating – Enlarged neck veins – Swollen ankles – Anxiety
Congestive Heart Failure (3 of 3) • Take these actions: – Place the patient in a sitting position with the legs down to drain some of the fluid back into the lower parts of the body. – Administer oxygen in large quantities and at a high flow rate. – Summon additional help. – Arrange for prompt transport.
Dyspnea (1 of 4) • Shortness of breath or difficulty breathing • Usually associated with serious heart or lung disease – Heart-related causes: angina pectoris, heart attack, and CHF – Other causes: pulmonary disease such as as chronic obstructive pulmonary disease (COPD), emphysema, chronic bronchitis, pneumonia, and asthma
Dyspnea (2 of 4) • General treatment – Check the patient’s airway to be sure it is not obstructed. – Check the rate and depth of breathing. – Place the patient in a comfortable position. – Provide reassurance. – Loosen any tight clothing. – Administer oxygen if it is available.
Dyspnea (3 of 4) • Asthma – Acute spasm of the air passage associated with excess mucus production and swelling of the lining of the respiratory passage – Can be caused by • An allergic reaction • Severe emotional stress • Exercise • Respiratory infections
Dyspnea (4 of 4) • Asthma (cont’d) – Asthma attacks killed 3, 630 in the United States in 2013. – Patients will have great difficulty exhaling and a wheezing sound will be heard. – Follow the treatment steps for dyspnea and instruct the patient to perform pursed-lip breathing. – If ALS is not available, transport promptly.
Stroke (1 of 6) • Leading cause of brain injury and disability in adults • Most strokes are caused by a blood clot that blocks blood supply to a part of the brain. • Signs and symptoms – Headache – Numbness or paralysis on one side of the body – Dizziness – Confusion
Stroke (2 of 6) • Signs and symptoms (cont’d) – Drooling – Inability to speak – Difficulty seeing – Unequal pupil size – Unconsciousness – Seizures – Respiratory arrest – Incontinence – Unresponsiveness
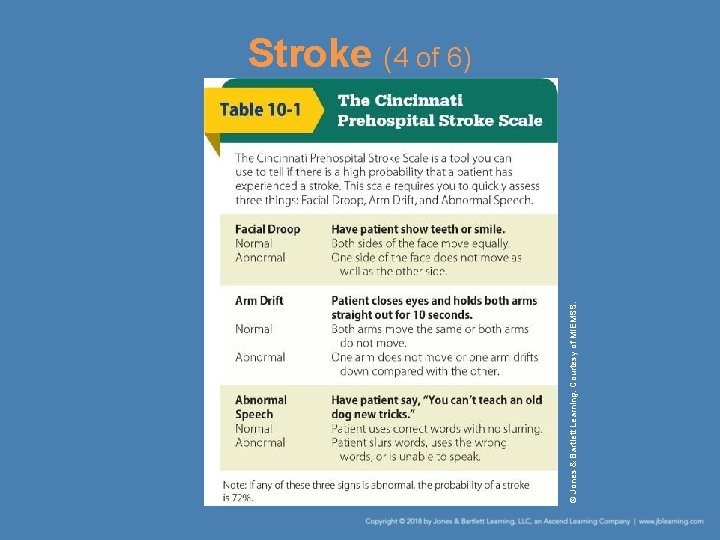
Stroke (3 of 6) • Cincinnati Prehospital Stroke Scale – Used to determine whether a patient may have experienced a stroke – Requires no special equipment
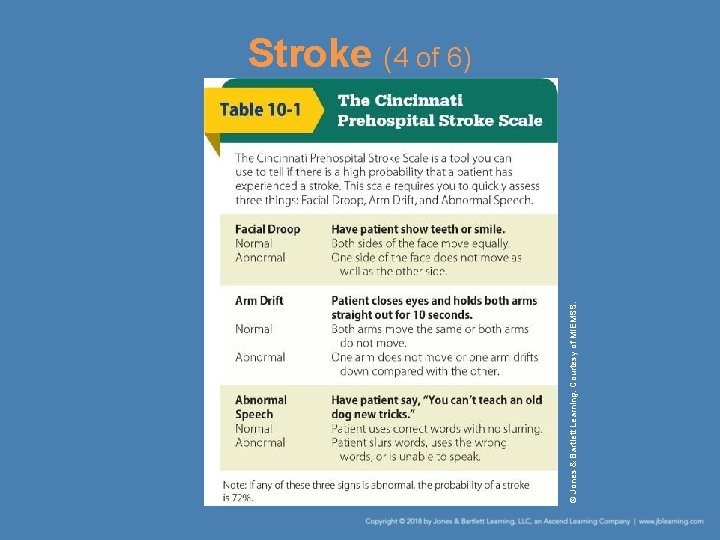
© Jones & Bartlett Learning. Courtesy of MIEMSS. Stroke (4 of 6)
Stroke (5 of 6) • Treatment – The first priority is to maintain an open airway. – Administer oxygen using a nonrebreathing face mask. – If the patient is having a seizure, try to prevent further injury. – Be prepared to administer rescue breathing.
Stroke (6 of 6) • Treatment (cont’d) – Place an unresponsive patient in the recovery position. – Provide emotional support by talking to and touching the patient. – Some patients can be treated with drugs to dissolve the blood clot in their brain. – Arrange for prompt transport.
Diabetes (1 of 8) • Caused by the body’s inability to process and use glucose • The body produces insulin, which enables glucose to move into individual cells. – If the body does not produce enough insulin, the cells become “starved” for glucose and diabetes results.
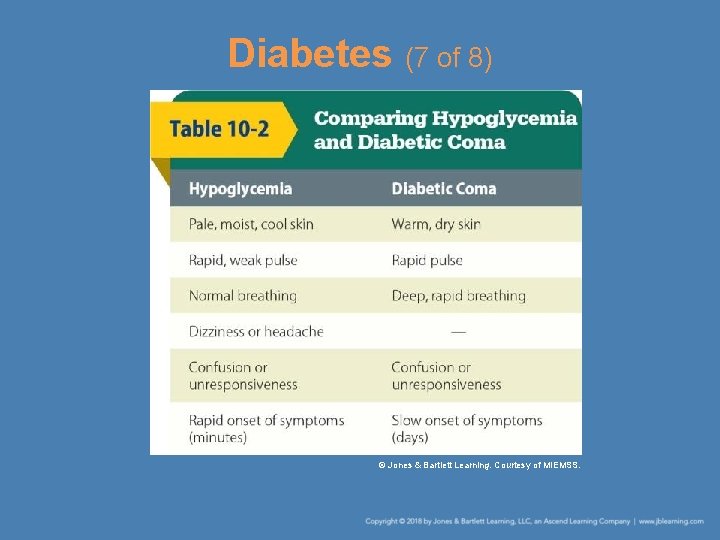
Diabetes (2 of 8) • Hypoglycemia – Occurs if the body has enough insulin but not enough blood glucose – Signs and symptoms • Pale, moist, cool skin • Rapid, weak pulse • Dizziness or headache • Confusion or unconsciousness • Sweating
Diabetes (3 of 8) • Hypoglycemia (cont’d) – Signs and symptoms (cont’d) • Hunger • Rapid onset of symptoms (within minutes) – A person experiencing hypoglycemia may appear to be drunk. – If the patient is able to swallow, have him or her eat or drink something sweet.
Diabetes (4 of 8) • Hypoglycemia (cont’d) – If the patient is unconscious, open the airway and assist breathing and circulation. Courtesy of Paddock Laboratories, Inc. – Do not administer fluids by mouth. – Some EMRs carry a tube of oral glucose gel or tablets that can be placed inside the cheek.
Diabetes (5 of 8) • Diabetic coma – Occurs when the body has too much blood glucose and not enough insulin – Signs and symptoms • History of diabetes • Warm, dry skin • Rapid pulse • Deep, rapid breathing • Fruity odor on the patient’s breath
Diabetes (6 of 8) • Diabetic coma (cont’d) – Signs and symptoms (cont’d) • Weakness, nausea, and vomiting • Increased hunger, thirst, and urination • Slow onset of symptoms (days) – Misdiagnosis is common—it is not always easy to distinguish between hypoglycemia and diabetic coma.
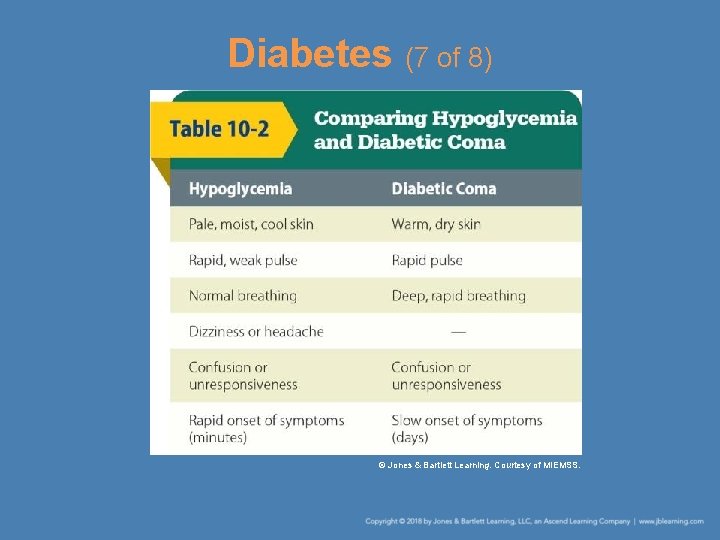
Diabetes (7 of 8) © Jones & Bartlett Learning. Courtesy of MIEMSS.
Diabetes (8 of 8) • Diabetic coma (cont’d) – In general, give conscious diabetic patients sugar by mouth and arrange for prompt transport. – If the diabetic patient is unconscious, arrange for prompt transport.
Abdominal Pain (1 of 5) • The contents of the abdomen are divided into hollow and solid structures. – Hollow structures are really tubes through which contents pass. – Solid structures produce substances. • Abdominal pain is a common complaint.
Abdominal Pain (2 of 5) • Acute abdomen – Caused by irritation of the abdominal wall – May result from infection or the presence of blood in the abdominal cavity – Pain can be referred to other parts of the body. – The abdomen may feel as hard as a board. – Patients may have nausea and vomiting, fever, and diarrhea as well as pain.
Abdominal Pain (3 of 5) • Some patients will vomit blood because they are bleeding from the esophagus or stomach. • If a patient has abdominal pain: – Monitor vital signs. – Treat symptoms of shock. – Keep the patient comfortable. – Arrange for transport.
Abdominal Pain (4 of 5) • Abdominal aortic aneurysm (AAA) – One cause of acute abdomen – Occurs when one or more layers of the aorta become weakened and separate from other layers of the aorta – Risk factors: diabetes, high blood pressure, atherosclerosis, and heavy smoking
Abdominal Pain (5 of 5) • Treatment for AAA – Place the patient in a comfortable position. – Treat the patient for shock. – Handle these patients gently. – Arrange for prompt transport.
Kidney Dialysis Patients (1 of 3) • People with certain types of kidney disease are unable to filter waste products from their bloodstream. • Many patients with chronic renal failure must undergo hemodialysis. – The patient’s blood passes through a machine that filters out the waste products and returns the cleansed blood to the patient.
Kidney Dialysis Patients (2 of 3) • Hemodialysis (cont’d) – Most hemodialysis patients have a shunt implanted in their arm or leg. – A shunt is a surgically created connection between an artery and a vein. – If the patient has a shunt, take the patient’s blood pressure in the arm without the shunt.
Kidney Dialysis Patients (3 of 3) • Patients may experience emergencies related to their dialysis treatment. – Low blood pressure due to the changes in their body – Shock due to decreased blood pressure – Internal bleeding – Abnormal levels of electrolytes, which can cause cardiac arrhythmias
Summary (1 of 3) • General medical conditions may have different causes, yet result in similar signs and symptoms. • Usually, it is best to collect a medical history on the patient experiencing a medical problem before you perform a physical examination.
Summary (2 of 3) • Altered mental status (AMS) is a sudden or gradual decrease in the patient’s level of responsiveness. When assessing AMS in a patient, use the AVPU scale. • Seizures are caused by sudden episodes of uncontrolled electrical impulses in the brain.
Summary (3 of 3) • Specific medical conditions include angina pectoris, heart attack, congestive heart failure, dyspnea, stroke, hypoglycemia, diabetic coma, and abdominal pain.
Review 1. Signs and symptoms of stroke include all of the following EXCEPT: A. numbness or paralysis. B. high fever. C. drooling. D. unequal pupil size.
Review Answer: B. high fever.
Review 2. Which of the following actions would NOT be appropriate when managing a patient who is suffering a heart attack? A. Place the patient in the most comfortable position. B. Administer oxygen if it is available. C. Be prepared to administer CPR. D. Move the patient as quickly as possible to the ambulance for transport.
Review Answer: D. Move the patient as quickly as possible to the ambulance for transport.
Review 3. Hypoglycemia occurs when a patient A. consumes too many high-fat foods. B. has enough insulin but not enough blood glucose. C. suffers severe dehydration. D. has too much blood glucose and not enough insulin.
Review Answer: B. has enough insulin but not enough blood glucose.
 National ems standards
National ems standards Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Environmental emergencies emt
Environmental emergencies emt Chapter 23 gynecologic emergencies
Chapter 23 gynecologic emergencies The term behavioral crisis is most accurately defined as
The term behavioral crisis is most accurately defined as Chapter 19 endocrine and hematologic emergencies
Chapter 19 endocrine and hematologic emergencies Chapter 18 neurologic emergencies
Chapter 18 neurologic emergencies Emt chapter 18 gastrointestinal and urologic emergencies
Emt chapter 18 gastrointestinal and urologic emergencies Chapter 28 first aid and emergencies
Chapter 28 first aid and emergencies Chapter 16 respiratory emergencies
Chapter 16 respiratory emergencies Gems diamond geriatric assessment
Gems diamond geriatric assessment Chapter 13 handling emergencies
Chapter 13 handling emergencies Chapter 12 behavioral emergencies
Chapter 12 behavioral emergencies Chapter 32 environmental emergencies
Chapter 32 environmental emergencies Chapter 17 cardiovascular emergencies
Chapter 17 cardiovascular emergencies A 41 year old man presents with slow irregular breathing
A 41 year old man presents with slow irregular breathing National ems advisory council
National ems advisory council Quiz
Quiz Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Lesson 6: cardiac emergencies and using an aed
Lesson 6: cardiac emergencies and using an aed Leukostasis symptoms
Leukostasis symptoms Psychiatric emergency
Psychiatric emergency Qut security emergency extension number
Qut security emergency extension number Immunologic emergencies
Immunologic emergencies Chapter 1 ems systems
Chapter 1 ems systems Ems systems chapter 1
Ems systems chapter 1 Ptal california medical board
Ptal california medical board Gbmc medical records
Gbmc medical records Hepburn osteometric board
Hepburn osteometric board Torrance memorial hospital medical records
Torrance memorial hospital medical records Cartersville medical center medical records
Cartersville medical center medical records Standard error in statistics
Standard error in statistics Language
Language Difference between actual cost and standard cost
Difference between actual cost and standard cost Bahagian pembangunan kurikulum dskp kssm
Bahagian pembangunan kurikulum dskp kssm National board for medical interpreters
National board for medical interpreters National hospital ambulatory medical care survey
National hospital ambulatory medical care survey Abu ali sina university peshawar
Abu ali sina university peshawar M.gorky donetsk national medical university
M.gorky donetsk national medical university Seoul national university medical school
Seoul national university medical school Mongolian national university of medical sciences
Mongolian national university of medical sciences National core standards domains
National core standards domains Nqs assessment and rating
Nqs assessment and rating Dsmith
Dsmith National standard 1
National standard 1 Nfpa 1600 standard
Nfpa 1600 standard Nsmc chart
Nsmc chart User applied labelling
User applied labelling National healthy housing standard
National healthy housing standard Nfpa 1600
Nfpa 1600 National standard practice manual
National standard practice manual National unification and the national state
National unification and the national state Helen hynes
Helen hynes Corbs model of feedback
Corbs model of feedback Epa medical education
Epa medical education The medical rehabilitation education foundation reports
The medical rehabilitation education foundation reports Current trends in medical education
Current trends in medical education Target institute of medical education and research
Target institute of medical education and research Define blime
Define blime Ethics in medical education
Ethics in medical education Continuing medical education
Continuing medical education American association of continuing medical education
American association of continuing medical education Continuing medical education
Continuing medical education Belarusian medical academy of postgraduate education
Belarusian medical academy of postgraduate education Medical education reform programme
Medical education reform programme Medical education and drugs department
Medical education and drugs department International standard classification of education
International standard classification of education Career education standard
Career education standard National forum on education statistics
National forum on education statistics What is malaysia education blueprint
What is malaysia education blueprint National environmental education action plan
National environmental education action plan