Autism Law Summit 2020 Legal Refresher Daniel R









- Slides: 46

Autism Law Summit 2020 Legal Refresher Daniel R. Unumb. Esq. Autism Legal Resource Center LLC Danunumb. alrc@gmail. com © Dan Unumb 2020

3

Refresher? ! But I Came for the Party!

The Basics Healthcare Coverage Mandates Mental Health Parity ERISA Medicaid ADA/Section 504 (Schools)
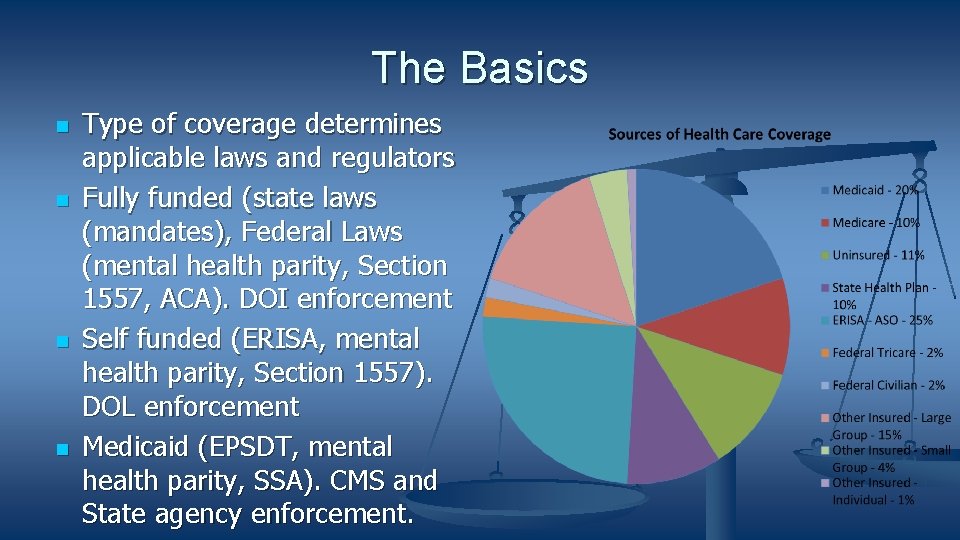
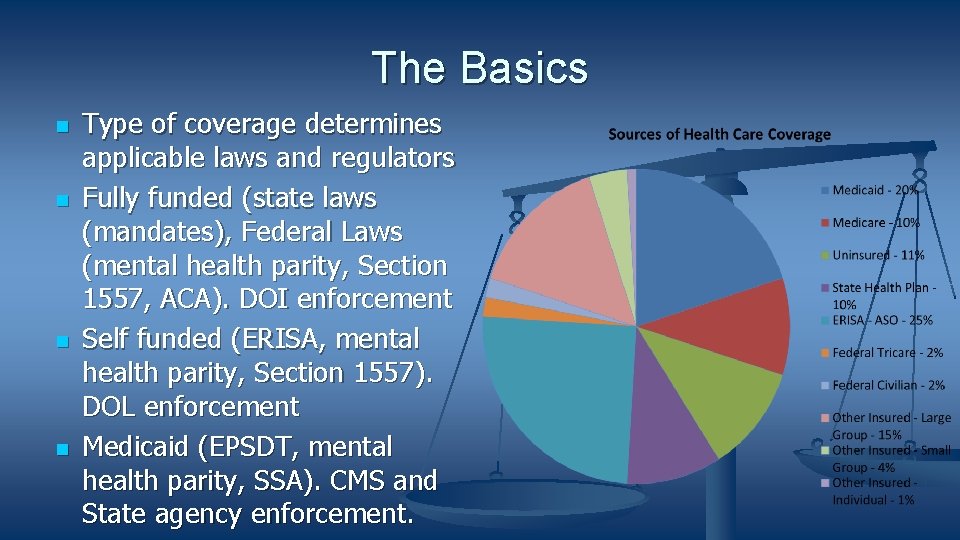
The Basics Type of coverage determines applicable laws and regulators Fully funded (state laws (mandates), Federal Laws (mental health parity, Section 1557, ACA). DOI enforcement Self funded (ERISA, mental health parity, Section 1557). DOL enforcement Medicaid (EPSDT, mental health parity, SSA). CMS and State agency enforcement.
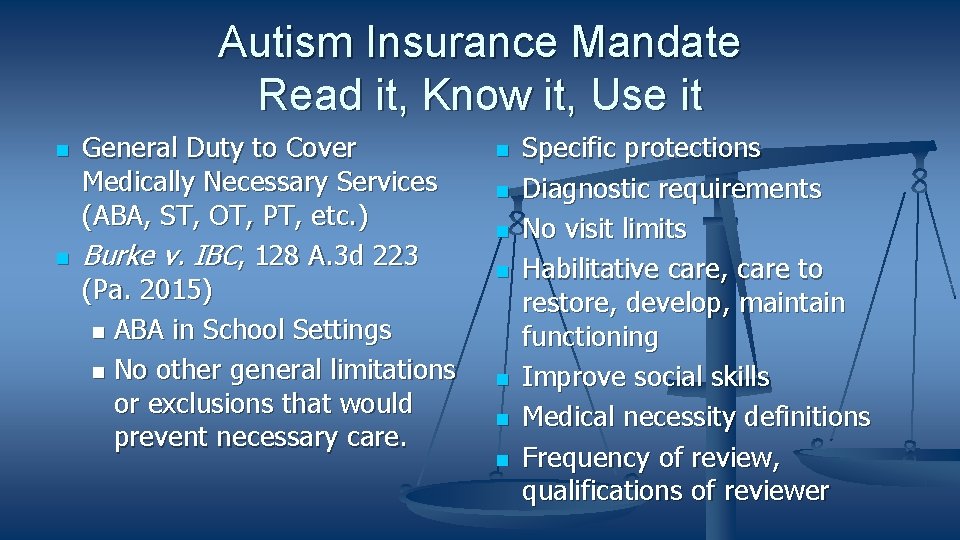
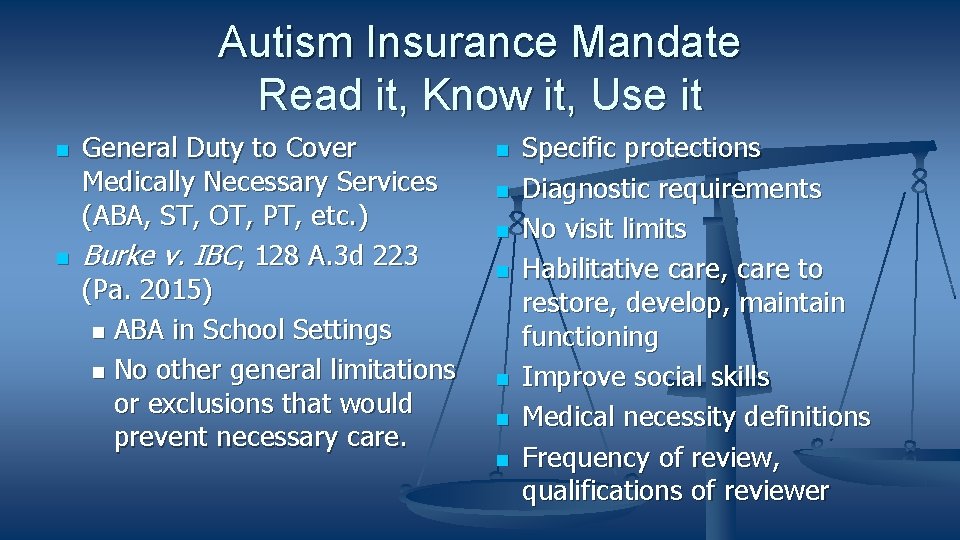
Autism Insurance Mandate Read it, Know it, Use it General Duty to Cover Medically Necessary Services (ABA, ST, OT, PT, etc. ) Burke v. IBC, 128 A. 3 d 223 (Pa. 2015) ABA in School Settings No other general limitations or exclusions that would prevent necessary care. Specific protections Diagnostic requirements No visit limits Habilitative care, care to restore, develop, maintain functioning Improve social skills Medical necessity definitions Frequency of review, qualifications of reviewer
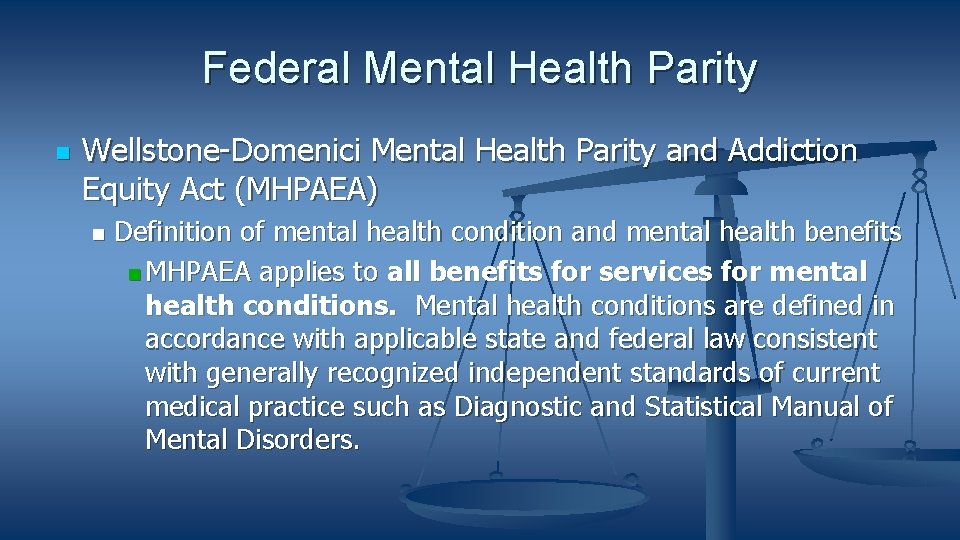
Federal Mental Health Parity Wellstone-Domenici Mental Health Parity and Addiction Equity Act (MHPAEA) Definition of mental health condition and mental health benefits MHPAEA applies to all benefits for services for mental health conditions. Mental health conditions are defined in accordance with applicable state and federal law consistent with generally recognized independent standards of current medical practice such as Diagnostic and Statistical Manual of Mental Disorders.

Mental Health Parity-MHPAEA No treatment limitations imposed only on MH conditions or only on ASD
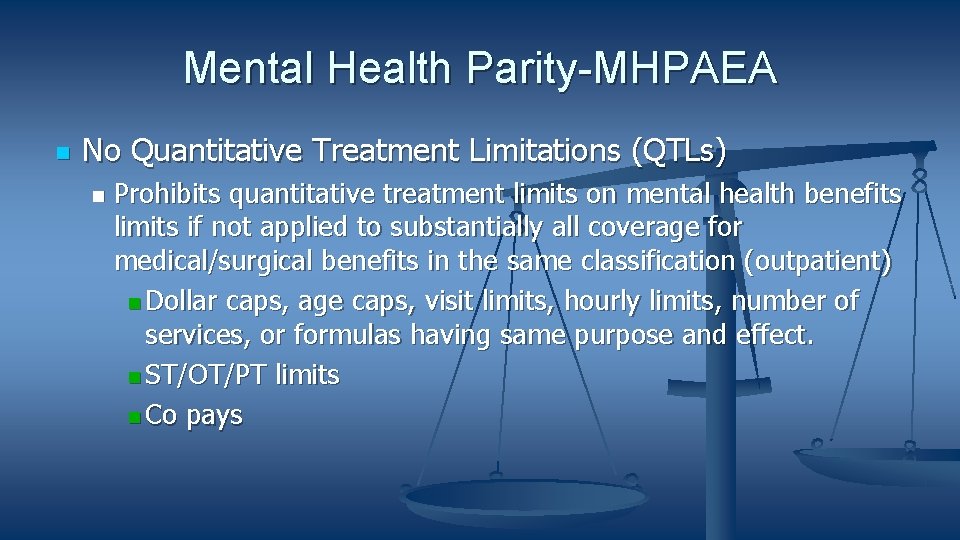
Mental Health Parity-MHPAEA No Quantitative Treatment Limitations (QTLs) Prohibits quantitative treatment limits on mental health benefits limits if not applied to substantially all coverage for medical/surgical benefits in the same classification (outpatient) Dollar caps, age caps, visit limits, hourly limits, number of services, or formulas having same purpose and effect. ST/OT/PT limits Co pays
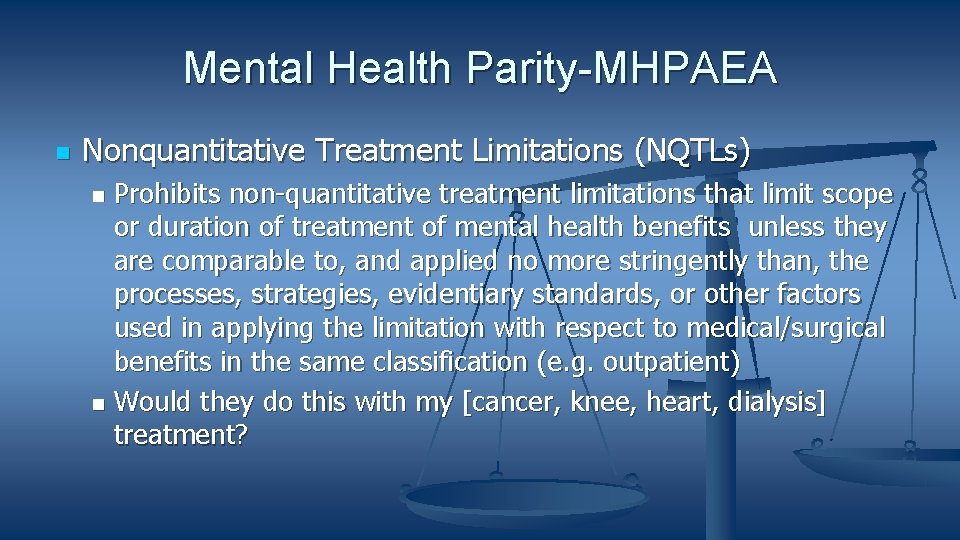
Mental Health Parity-MHPAEA Nonquantitative Treatment Limitations (NQTLs) Prohibits non-quantitative treatment limitations that limit scope or duration of treatment of mental health benefits unless they are comparable to, and applied no more stringently than, the processes, strategies, evidentiary standards, or other factors used in applying the limitation with respect to medical/surgical benefits in the same classification (e. g. outpatient) Would they do this with my [cancer, knee, heart, dialysis] treatment?
Mental Health Parity NQTLS Medical management/medical necessity criteria provider networks, provider admission standards and reimbursement formulas, in-network and out-of-network coverage. Treatment plan requirements, parent participation requirements, conditioning coverage on likelihood of improvement within set time period, review procedures, who, when, what.
NQTLs Conditioning access to treatment on obtaining an ASD diagnosis using overly restrictive diagnostic criteria and tests not required for diagnosis by professionals acting within the scope of license and accepted standards. Mandatory requirements for parent or caregiver participation imposed as a condition for access to treatment. Restrictions on access to medically necessary treatment locations such as clinics, schools, or community locations. Restrictions based on age or school attendance. Restrictions on the range of ASD symptoms treated or conditioning access to treatment on demonstration of certain symptoms such as self-injurious behavior or aggression.
Mental Health Parity ABA Exclusions A. F. v. Providence, 35 F. Supp. 3 d 1298 (D. Or. 2014) (developmental disability exclusion). Idaho Department of Insurance Bulletin No. 18 -02, April 2, 2018 (exclusion violates MHPAEA and ACA 1557). North Dakota Insurance Department Bulletin 2018 -1, July 10, 2018 (exclusion violates MHPAEA).
ERISA Duties and Contract Provisions Wit v. UBH , Case No. 14 -cv-02346 (N. D. Cal. March 4, 2019) Challenging internal level of care and coverage determination guidelines for chronic mental illness that are more restrictive than generally accepted standards and general policy terms. Note: provider contracts typically obligate provider to deliver care in accordance with professional standards. Wit analysis would also likely apply to MHPAEA claim. Cover medical/surgical in accordance with generally accepted standards.
Wit v. UBH Sought coverage of residential treatment for mental health/substance use disorder. Denied based on UBH level of care guidelines/coverage determination guidelines. UBH administered employer self-funded plans and employer fully funded plans.
Wit v. UBH owed fiduciary duty to administer plans solely in the interest of the participants with care and skill in accordance with plan documents. Breached by using guidelines more restrictive than generally accepted standards as required by plans and prioritizing cost savings over members interests.
Wit v. UBH breached duty to use due care by arbitrarily and capriciously denying benefits using guidelines that were more restrictive than generally accepted standards.
Wit v. UBH Standards adopted and used by UBH were more restrictive than generally accepted standards. Generally accepted standards include services to maintain functioning and prevent deterioration. Multidimensional taking into account a wide range of patient information. UBH standards placed excessive emphasis on acuity and crises stabilization. UBH standards pushed patients to lower of care when safe to do so even if would be less effective. UBH standards failed to take into account developmental state of children.
Wit v. UBH Care should not be denied on grounds that patient not responding to treatment where patient has potential to respond to treatment. Whether care can be denied as “custodial” should not be based on rehabilitation potential or degree of functional limitation. Financial incentives “infected” Guideline development process.
Wit v. UBH Fact that Guidelines were riddled with requirements that provided narrower coverage than is consistent with generally accepted standards of care gives rise to a strong inference that UBH’s financial interests interfered with the Guideline development process. The overemphasis on moving members to a “less restrictive setting” in the Guidelines. . . was influenced, at least in part, by cost considerations.
Insurer Medical Necessity Guidelines In-house Commercial
Wit v. UBH Generally accepted standards of care the standards that have achieved widespread acceptance among behavioral health professionals. Multiple sources, including: peer-reviewed studies; consensus guidelines from professional organizations; Guidelines and materials distributed by government agencies. American Association of Community Psychiatrists, American Academy of Child and Adolescent Psychiatry, APA, CMS. ABA?
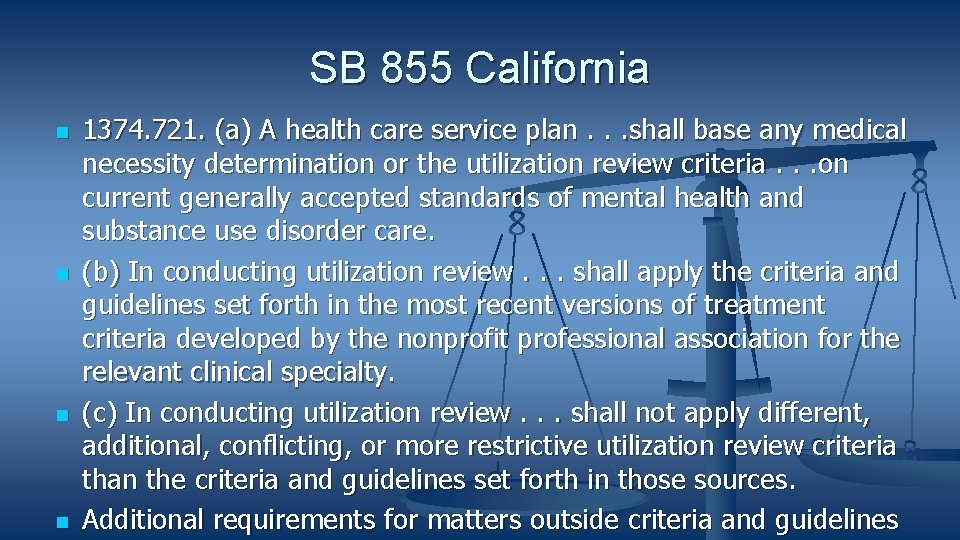
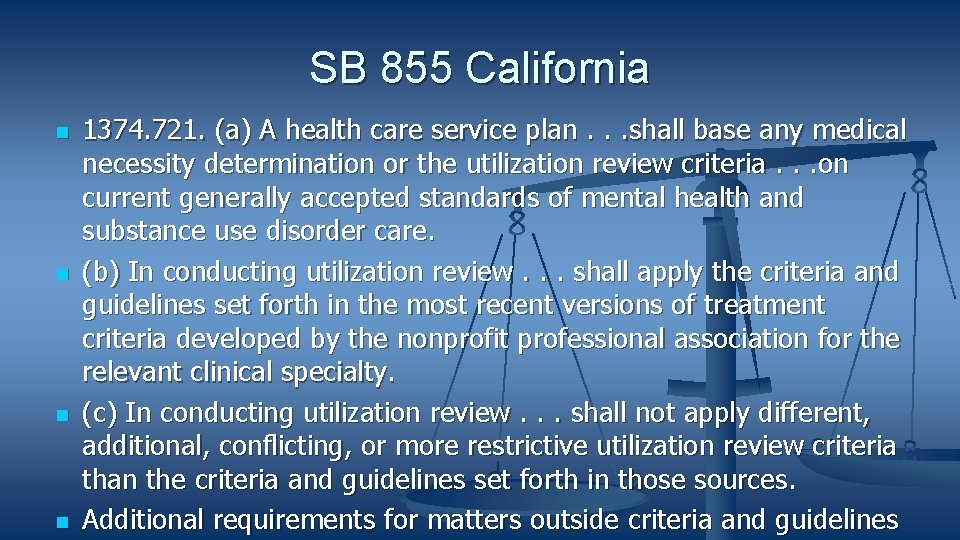
SB 855 California 1374. 721. (a) A health care service plan. . . shall base any medical necessity determination or the utilization review criteria. . . on current generally accepted standards of mental health and substance use disorder care. (b) In conducting utilization review. . . shall apply the criteria and guidelines set forth in the most recent versions of treatment criteria developed by the nonprofit professional association for the relevant clinical specialty. (c) In conducting utilization review. . . shall not apply different, additional, conflicting, or more restrictive utilization review criteria than the criteria and guidelines set forth in those sources. Additional requirements for matters outside criteria and guidelines
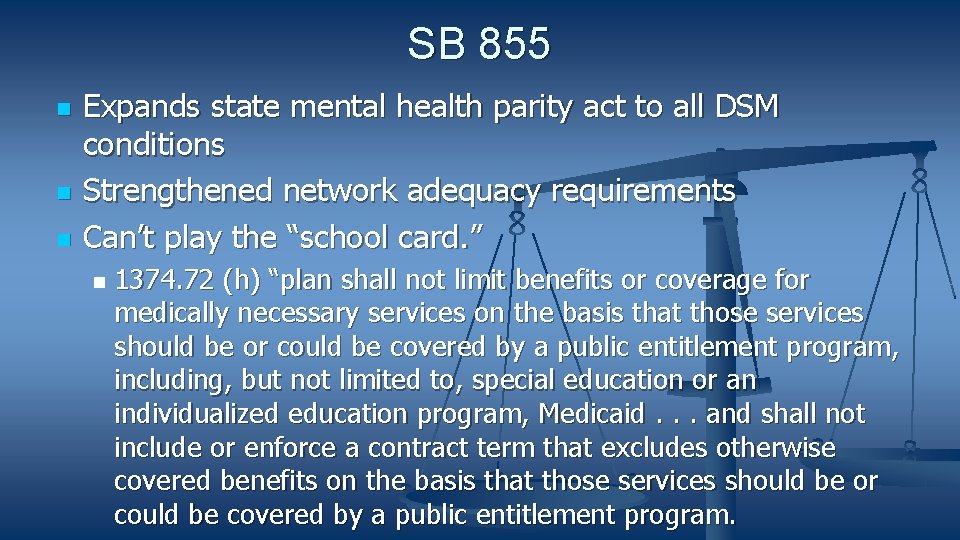
SB 855 Expands state mental health parity act to all DSM conditions Strengthened network adequacy requirements Can’t play the “school card. ” 1374. 72 (h) “plan shall not limit benefits or coverage for medically necessary services on the basis that those services should be or could be covered by a public entitlement program, including, but not limited to, special education or an individualized education program, Medicaid. . . and shall not include or enforce a contract term that excludes otherwise covered benefits on the basis that those services should be or could be covered by a public entitlement program.
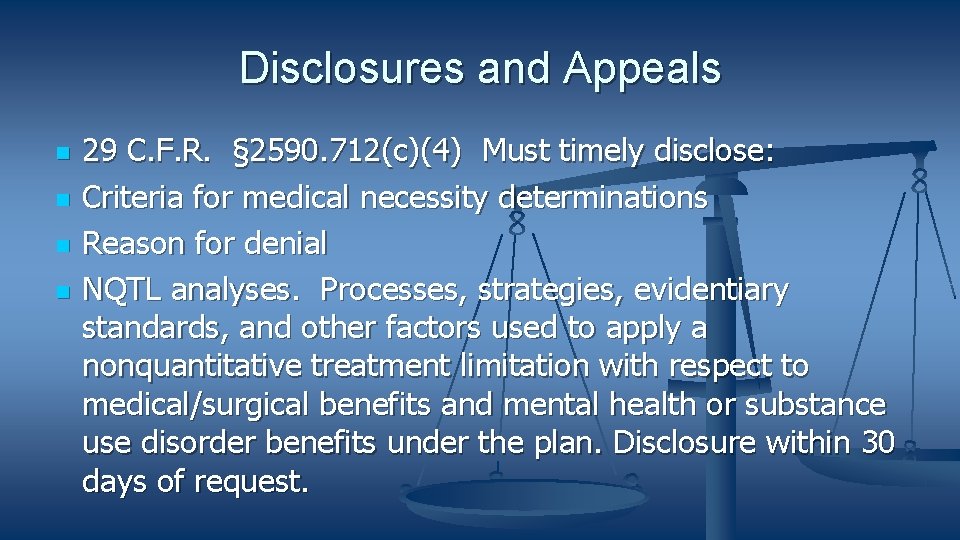
Disclosures and Appeals 29 C. F. R. § 2590. 712(c)(4) Must timely disclose: Criteria for medical necessity determinations Reason for denial NQTL analyses. Processes, strategies, evidentiary standards, and other factors used to apply a nonquantitative treatment limitation with respect to medical/surgical benefits and mental health or substance use disorder benefits under the plan. Disclosure within 30 days of request.
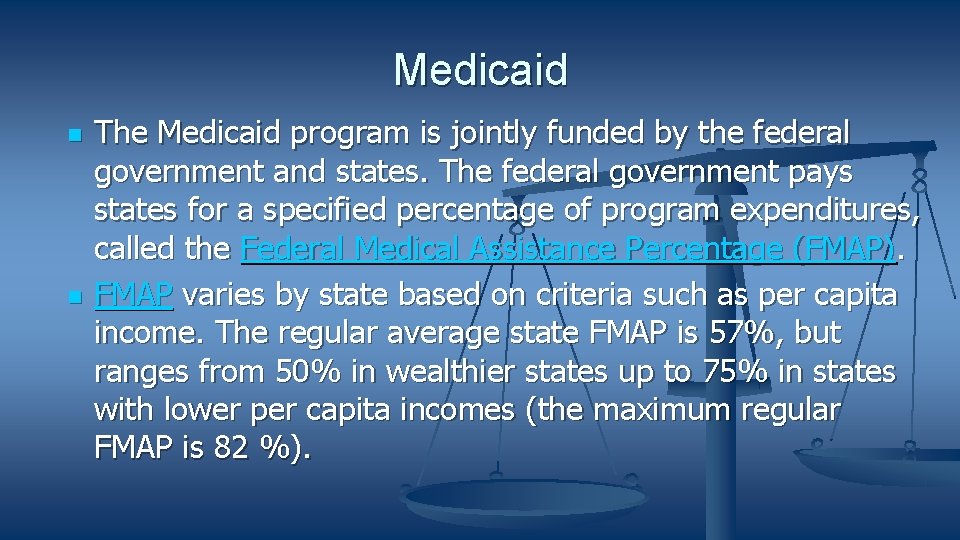
Medicaid The Medicaid program is jointly funded by the federal government and states. The federal government pays states for a specified percentage of program expenditures, called the Federal Medical Assistance Percentage (FMAP). FMAP varies by state based on criteria such as per capita income. The regular average state FMAP is 57%, but ranges from 50% in wealthier states up to 75% in states with lower per capita incomes (the maximum regular FMAP is 82 %).
Medicaid Medical Assistance 42 USC 1396 d(a) Mandatory services (e. g. physician services, hospital services, EPSDT). Optional services (e. g. case management, other licensed practitioner). State Plan Services Equivalent amount, duration and scope for all enrollees Statewide Freedom of choice in providers
Medicaid Waiver Coverage Waiver services (e. g. home and community based services). Typical requirements are waived. Can be limited to certain populations, geographic areas and locations, can have age caps, hour caps, limited treatment focus, provider limitations.

Medicaid State Plan Services Mandatory coverage Optional coverage EPSDT (Early Periodic Screening Diagnosis and Treatment) is a mandatory service. Identify and treat illnesses and conditions so child enters adulthood as healthy and functional as possible. Prevent/limit disability.
Medicaid EPSDT Coverage Not waiver coverage. For all Medicaid eligible children under 21. All Medical Assistance whether or not in the current State Plan to correct or ameliorate defects, conditions or illnesses. Must be provided to all eligible children with reasonable promptness. Single case agreements if no current provider type.
Medicaid-EPSDT Must provide all medically necessary ABA services to correct or ameliorate a child’s ASD deficits and conditions. No caps on services, no limits on symptoms treated, no age, hour caps, no location restrictions, no mandatory parent participation requirements Determinations must be based on individualized assessment of needs. State agency remains responsible for compliance regardless of delegations to MCOs or other agencies.
Medicaid Eligibility Income based Disability based TEFRA Meet LOC No waiting list Katie Becket Meet waiver requirements Waiting list Medicaid buy-in.

Red Flags in Medicaid Coverage Improper limitations on medical necessity such as requiring that child exhibits aggressive or selfinjurious behavior or behaviors that interfere with community activities. EPSDT requires all necessary care to correct or ameliorate the deficits and conditions of a child’s ASD. Attempts to impose “fail first” or “step therapy” regimes before providing recommended ABA treatment.

Red Flags in Medicaid Coverage Overly restrictive or burdensome prior authorization requirements or gateway requirements such as requirement for evaluation by multidisciplinary “team. ” Imposing limits on hours at levels below general standards of care and requiring additional authorization to exceed those levels. Overly restrictive provider requirements, Failing to allow LABAs, overly stringent requirements on paraprofessionals.
Red Flags in Medicaid Coverage Imposing fixed, mandatory parental participation requirements that discriminate against working parents, parents with disabilities, single parent families, etc. Limitations on location of services such as schools. Requiring severe behaviors as a condition for treatment, restricting range of symptoms and deficits treated.
MHPAEA and Medicaid Applies if any part of services is delivered through MCOs State determines if condition is MH for purposes of MHPAEA but determination must be consistent with generally recognized independent standards of medical practice. Children—Red flags for EPSDT Adults--Requirements beyond State Plan. Must provide additional coverage when necessary to comply with MHPAEA.
Section 1557 of the ACA Prohibits discrimination in healthcare on the vbsis of , including discrimination on the basis of race, color, national origin, sex, age, or disability, including discrimination in benefit design Applies to entities with federal health care funding nexus including insurers. Applies to Medicaid.
ADA/504 ABA in Schools Section 504 of the federal Rehabilitation Act applies to entities which receive federal financial assistance and prohibits discrimination of the basis of disability. The ADA (Americans with Disabilities Act) was passed after Section 504 and applies to private institutions, workplaces, state-funded entities and other institutions that were not covered under section 504.
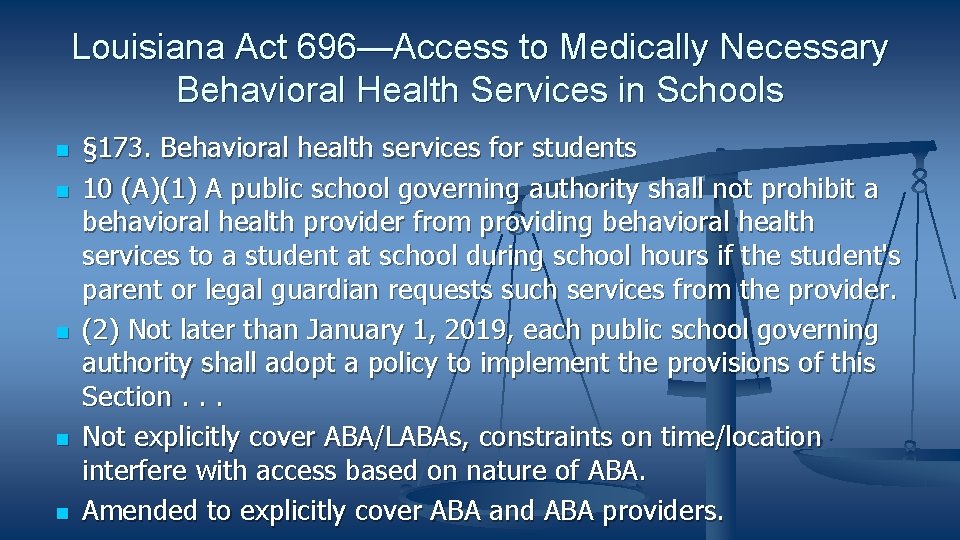
Louisiana Act 696—Access to Medically Necessary Behavioral Health Services in Schools § 173. Behavioral health services for students 10 (A)(1) A public school governing authority shall not prohibit a behavioral health provider from providing behavioral health services to a student at school during school hours if the student's parent or legal guardian requests such services from the provider. (2) Not later than January 1, 2019, each public school governing authority shall adopt a policy to implement the provisions of this Section. . . Not explicitly cover ABA/LABAs, constraints on time/location interfere with access based on nature of ABA. Amended to explicitly cover ABA and ABA providers.
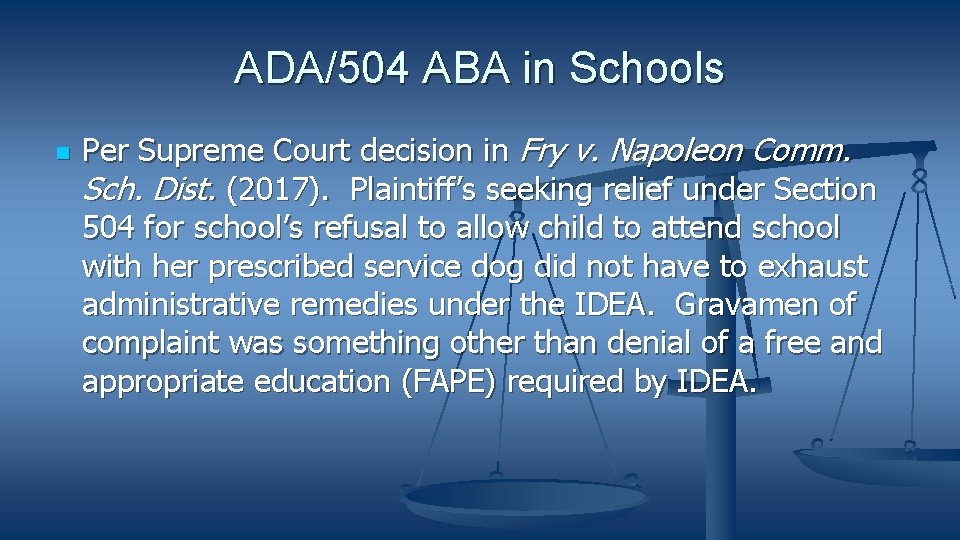
ADA/504 ABA in Schools Per Supreme Court decision in Fry v. Napoleon Comm. Sch. Dist. (2017). Plaintiff’s seeking relief under Section 504 for school’s refusal to allow child to attend school with her prescribed service dog did not have to exhaust administrative remedies under the IDEA. Gravamen of complaint was something other than denial of a free and appropriate education (FAPE) required by IDEA.
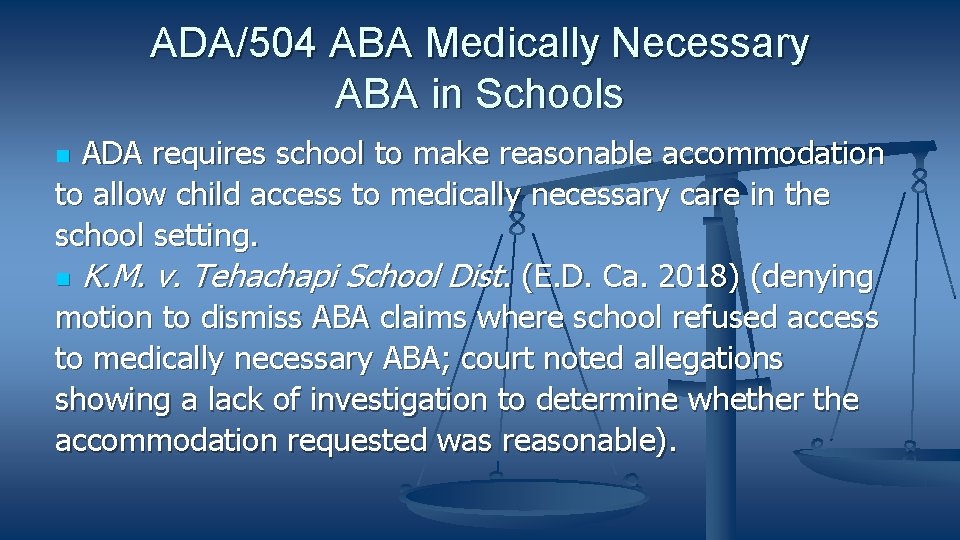
ADA/504 ABA Medically Necessary ABA in Schools ADA requires school to make reasonable accommodation to allow child access to medically necessary care in the school setting. K. M. v. Tehachapi School Dist. (E. D. Ca. 2018) (denying motion to dismiss ABA claims where school refused access to medically necessary ABA; court noted allegations showing a lack of investigation to determine whether the accommodation requested was reasonable).
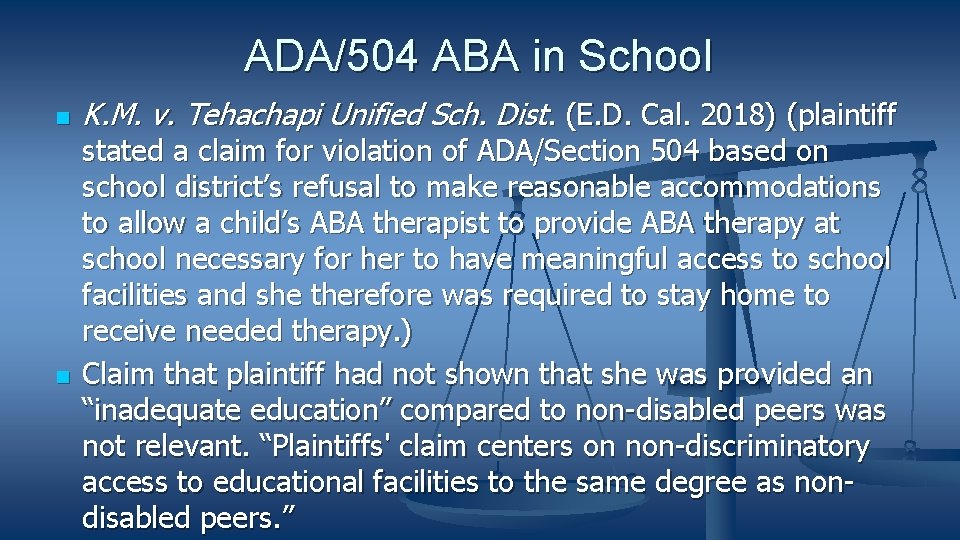
ADA/504 ABA in School K. M. v. Tehachapi Unified Sch. Dist. (E. D. Cal. 2018) (plaintiff stated a claim for violation of ADA/Section 504 based on school district’s refusal to make reasonable accommodations to allow a child’s ABA therapist to provide ABA therapy at school necessary for her to have meaningful access to school facilities and she therefore was required to stay home to receive needed therapy. ) Claim that plaintiff had not shown that she was provided an “inadequate education” compared to non-disabled peers was not relevant. “Plaintiffs' claim centers on non-discriminatory access to educational facilities to the same degree as nondisabled peers. ”
K. M. v. Tehachapi Settlement (2019) Licensed Lindamood Bell providers, Orton-Gillingham providers, or STAR Haynes NPA 1: 1 instructional services will be provided to K. M. during school hours for an hour each school day (inclusive of Extended School Year (“ESY”)), through 12 th grade, 200 school days per year totaling roughly 1510 hours, for a total cost of between roughly $135, 900. 00 and $196, 300. BCBA behavior support and training of staff, at up to 15 hours per month, at $300. 00 per hour, for a total of 10. 5 months per year, as long as she remains in school - worth roughly: $355, 500.
And More on ABA and Schools Graham v. Friedlander, 334 Conn. 564 (Conn. 2020) Claims against Board of Education for negligent hiring and supervision of unqualified autism service provider to serve children in school did not have to be exhausted through IDEA procedures Basis of complaint was regression and inability to communicate effectively caused by time children were under care of uncertified and unqualified behavior analyst and same claim could have been brought at public facility that was not a school.

Thanks! Danunumb. alrc@gmail. com
 Autism law summit
Autism law summit Dan unumb
Dan unumb Newton's first law and second law and third law
Newton's first law and second law and third law Newton's first law
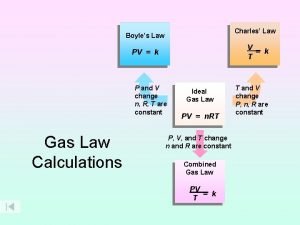
Newton's first law Boyle's law charles law avogadro's law
Boyle's law charles law avogadro's law How to calculate boyle's law
How to calculate boyle's law Sql refresher
Sql refresher Vocabulary refresher group a answers
Vocabulary refresher group a answers Gdpr refresher training
Gdpr refresher training What is v/q mismatch
What is v/q mismatch Annual security refresher
Annual security refresher Information security program refresher training
Information security program refresher training Caution radioactive material
Caution radioactive material Object oriented programming java exercises
Object oriented programming java exercises Confined space refresher
Confined space refresher Java programming refresher
Java programming refresher Ipv refresher course
Ipv refresher course Rt-130
Rt-130 Confined space refresher training
Confined space refresher training Ifr refresher
Ifr refresher Saeta refresher course 2021
Saeta refresher course 2021 Refresher training example
Refresher training example Hazmat training alaska
Hazmat training alaska Biology refresher
Biology refresher Positive law vs natural law
Positive law vs natural law Legal aid townsville
Legal aid townsville Unit 1 introduction to law and the legal system
Unit 1 introduction to law and the legal system The autism iceberg
The autism iceberg Core symptoms of autism
Core symptoms of autism Many faces of autism
Many faces of autism Autism range severity
Autism range severity The big a autism
The big a autism Special needs
Special needs Central coherence theory autism
Central coherence theory autism Puberty and autism spectrum disorders
Puberty and autism spectrum disorders Physical education adaptations for autism
Physical education adaptations for autism What is pdd-nos
What is pdd-nos Ace aba software
Ace aba software Tratament pentru autism infantil
Tratament pentru autism infantil Fallbeskrivning autism
Fallbeskrivning autism Autism spectrum disorders added authorization
Autism spectrum disorders added authorization Does sheldon cooper have autism
Does sheldon cooper have autism Macey hensley autism
Macey hensley autism Social pragmatic communication disorder
Social pragmatic communication disorder Hackney autism service
Hackney autism service Aspergers vs autism
Aspergers vs autism Autism nivå 3 barn
Autism nivå 3 barn