2017 PARAMEDIC REFRESHER COURSE Paramedic Refresher Module V

















- Slides: 110
2017 PARAMEDIC REFRESHER COURSE

Paramedic Refresher Module V Medical Emergencies 1 ENDOCRINE/DIABETIC TOXOCOLOGICAL/OPIOID IMMUNOLOGICAL PHARMACOLOGY PAIN MANAGEMENT
Module V Objectives ▪ Explain role glucose plays on the cells ▪ Explain role of insulin ▪ Discuss S/S commonly associated with hypo/hyperglycemia ▪ Identify commonly prescribed medications for diabetes ▪ Explain management of hypo/hyperglycemia ▪ Discuss metabolic syndrome ▪ Discuss functions of different insulin pumps ▪ Discuss common synthetic stimulants and natural or synthetic THC
Module V Objectives Cont. ▪ Discuss common opioids ▪ Explain common treatment options for opioid overdose ▪ Discuss the causes of an allergic reaction/anaphylaxis ▪ Differentiate between mild/localized allergic reaction and anaphylaxis ▪ Explain the actions of medications used to treat anaphylaxis ▪ Discuss different routes of medication delivery and rates of absorption ▪ Discuss pharmacological and non-pharmacological pain management
Module V Objectives Cont. ▪ Determine the differences between acute and chronic pain management ▪ Discuss the role of QA/QI, medical direction, and importance of documentation of pain management ▪ Discuss reassessment/re-evaluation of pain and management
Endocrine and Diabetic Emergencies ▪ Glucose ▪ Sugar ▪ Your body gets glucose primarily from the food you eat ▪ Usually carbohydrate rich foods ▪ Breads, pastas, etc… ▪ Fuels the cells
Endocrine and Diabetic Emergencies ▪ Brain and cells require proper amounts of glucose to function ▪ Change in glucose levels can cause alteration in behavior ▪ Seen as changes in mental status and consciousness ▪ Could exhibit stroke like symptoms ▪ Acting abnormally per friends or family ▪ Delayed responses or actions ▪ Confusion ▪ Lack of muscle coordination
Endocrine and Diabetic Emergencies ▪ Glucose is regulated by the pancreas ▪ Body attempts to keep blood glucose in a narrow range ▪ This function is performed by the pancreas through the release of hormones ▪ The hormones responsible for blood glucose maintenance are ▪ Insulin ▪ Secreted by beta islet cells of the pancreas ▪ High blood glucose stimulates insulin production ▪ Absorb glucose out of the blood ▪ Glucagon ▪ Secreted by alpha islet cells of the pancreas ▪ Low blood glucose stimulates glucagon secretion ▪ Effects the liver to release its glucose stores into the blood stream
Endocrine and Diabetic Emergencies ▪ Diabetes ▪ Disease characterized by nonexistent, minimal, or non-functioning insulin production ▪ Untreated diabetes leads to high blood glucose levels ▪ Two types of diabetes ▪ Insulin dependent (IDDM, Type 1) ▪ ▪ ▪ Early age of onset Lack of insulin production Requires use of insulin injections to maintain glucose levels Failure to administer insulin results in high glucose levels Failure to administer insulin in proper amounts could result in high or low glucose levels
Endocrine and Diabetic Emergencies ▪ Diabetes ▪ Non-Insulin Dependent (NIDDM, Type 2) ▪ ▪ Later age of onset Associated with obesity Some cases resolve with weight loss Cells become less sensitive to glucose ▪ Take medications to improve insulin sensitivity ▪ Metformin, Chlorpropamide, Glyburide ▪ Some may take insulin ▪ The pancreas produces extra insulin to make up for the insulin resistance ▪ Over time the pancreas is not able to make enough insulin
Endocrine and Diabetic Emergencies ▪ Hypoglycemia ▪ Presents with ▪ ▪ ▪ ▪ Rapid onset and changes in mental status Diaphoresis Hunger Tachycardia Rapid, shallow respirations Seizures possible Abnormal patient behavior ▪ Stroke mimic ▪ Hypoglycemia is a common stroke mimic ▪ Be alert for possible stroke when assessing possible hypoglycemia
Endocrine and Diabetic Emergencies ▪ Hypoglycemia management ▪ ▪ ▪ Ensure open and patent airway Adequate respiration Adequate circulation Check blood glucose level Be alert for insulin pumps Administer medication as necessary ▪ ▪ Oral glucose D 50 for >2 years D 25 for >1 month <2 years D 10 for <1 month ▪ Supportive care

Endocrine and Diabetic Emergencies ▪ Dextrose solutions ▪ D 50 is commonly carried and readily available for administration ▪ D 25 can be carried but is not as common ▪ To mix D 25 from D 50 aspirate 25 ml of D 50 ▪ Then draw 25 ml of normal saline into the D 50 vial ▪ D 10 can be carried and is still less common ▪ To mix D 10 from D 50 aspirate 40 ml of D 50 ▪ Then draw 40 ml of normal saline into the D 50 vial
Endocrine and Diabetic Emergencies ▪ Hyperglycemia ▪ Presents with ▪ ▪ ▪ ▪ ▪ Slower onset and changes in mental status Rapid breathing Possible presence of ketones on breath Dehydration Weakness Nausea/Vomiting Weak rapid pulse Polydipsia Polyuria Polyphagia

Endocrine and Diabetic Emergencies ▪ Hyperglycemia management ▪ ▪ Ensure open and patent airway Adequate respiration Adequate circulation Determine blood glucose level ▪ Glucose monitors vary on how high a level they can read ▪ Some strips determine the high level of the monitor ▪ Determine which method your monitor uses and become familiar with the limits ▪ A reading of HI is above the upper limit of the monitor or strips capability
Endocrine and Diabetic Emergencies ▪ Hyperglycemia management ▪ Supportive care ▪ Blood sugar needs to be lowered slowly in a monitored setting ▪ Patients may need to be monitored on an insulin drip in ICU ▪ Field management will consist of combating dehydration ▪ Transport ▪ All hyperglycemic patients should be transported to the ED for further evaluation ▪ If the patient present alert and wishes to refuse take you time and explain your concerns to the patient in an effort to convince them to go ▪ Ultimately there is little to be done at home and hospital evaluation and treatment should be the minimum standard for hyperglycemic patients

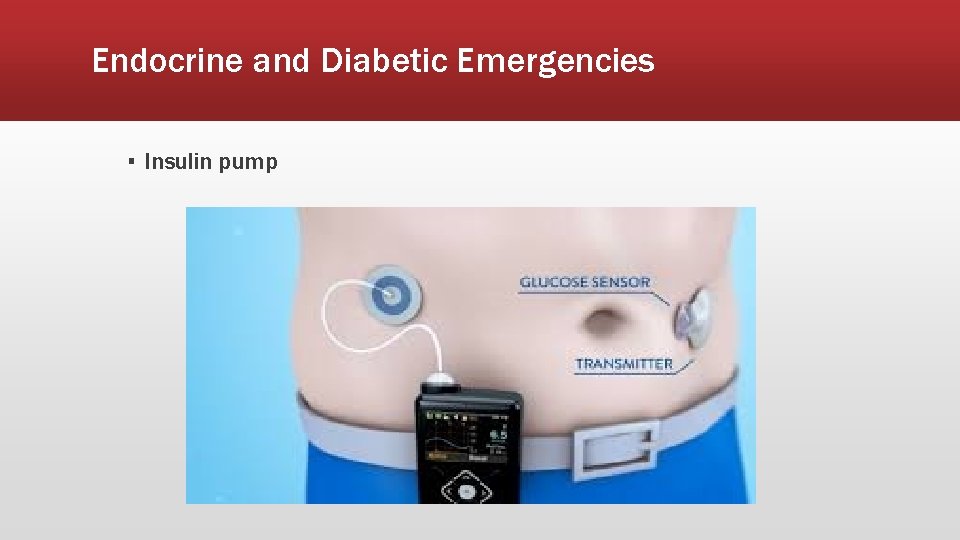
Endocrine and Diabetic Emergencies ▪ Insulin pumps ▪ ▪ About the size a an Altoid tin with a button or touch screen interface Secrete short acting insulin over 24 hours Attached SQ via a catheter attached from the pump to the patient Suspend pump administration or disconnect when treating hypoglycemic patients ▪ If unfamiliar with insulin pump use get the assistance of a family member of care taker ▪ Treating hypoglycemia while an insulin pump is active is pointless ▪ Tracks and stores info ▪ If familiar with insulin pumps or someone familiar is available it can provide helpful information in determining when or why this issue may have occurred

Endocrine and Diabetic Emergencies ▪ Insulin pump
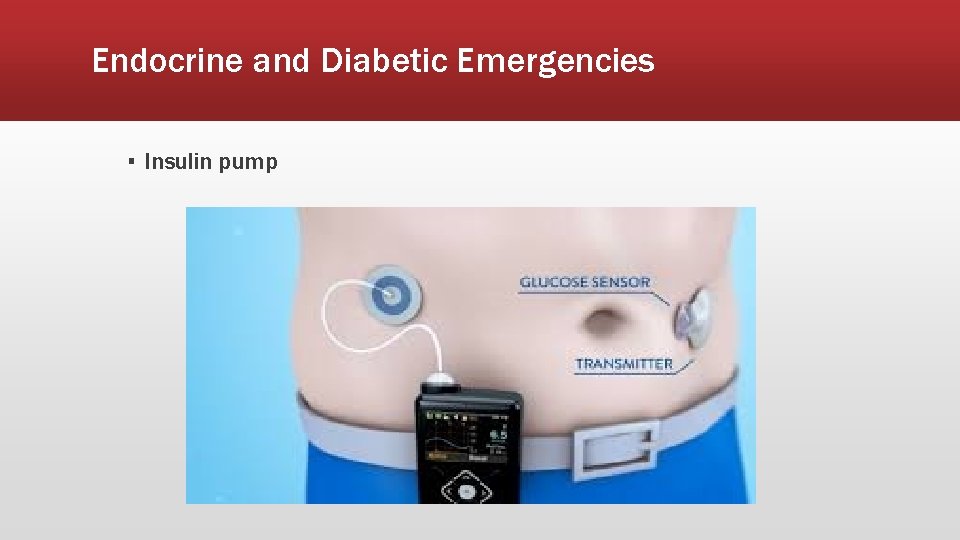
Endocrine and Diabetic Emergencies ▪ Insulin pump
Endocrine and Diabetic Emergencies ▪ Metabolic Syndrome ▪ Group of risk factors that increase risks for CAD, stroke, and Type 2 diabetes ▪ Central Obesity ▪ Extra weight around the middle and upper parts of the body ▪ “Apple shaped” appearance ▪ Insulin resistance ▪ Body is unable to use insulin as efficiently as normal ▪ Insulin helps to control the level of sugar in the body ▪ Blood sugar and fat levels rise

Endocrine and Diabetic Emergencies ▪ Metabolic Syndrome ▪ Increased long-term risk for development of ▪ Heart disease ▪ Increased risk MI and angina ▪ Type 2 diabetes ▪ Insulin resistance leads to poor insulin production after time ▪ Stroke ▪ PVD and sedentary lifestyle associated with obesity can lead to stroke ▪ Kidney disease ▪ Diabetes over time leads to kidney disease and failure ▪ Poor circulation to the legs
Endocrine and Diabetic Emergencies ▪ Adrenal Hypoplasia ▪ Addison’s Disease ▪ Primary adrenal insufficiency ▪ Adrenal glands do not produce enough steroid hormones ▪ Symptoms ▪ Typically slow onset ▪ Abdominal pain, weakness, and weight loss ▪ Darkening of the skin, in certain areas, may also occur ▪ Adrenal Crisis ▪ Can be triggered by stress, injury, or infection ▪ Presents with ▪ Hypotension, vomiting, low back pain, and loss of consciousness
Endocrine and Diabetic Emergencies ▪ Congenital adrenal hyperplasia ▪ Can affect all adrenal hormones ▪ Can cause hypo/hyperadrenalism ▪ Hyperadrenalism ▪ Overproduction of any or all ▪ Androgen hormones ▪ Corticosteroids ▪ Aldosterone ▪ Hypoadrenalism ▪ Adrenal insufficiency ▪ Underproduction of adrenal hormones ▪ Can cause ▪ Fatigue, dizziness, nausea, loss of appetite

Endocrine and Diabetic Emergencies ▪ Waterhouse Friderichsen Syndrome ▪ Can present with life threatening hypoglycemia and hypotension during adrenal crisis ▪ Out of hospital treatment ▪ ▪ Fluid bolus to treat hypotension Dextrose administration for hypoglycemia Transport to the ED Patient may carry an emergency kit containing hydrocortisone or dexamethasone ▪ Neither of these medications are currently in the WVOEMS scope of practice ▪ Family or caretaker may be familiar with the administration procedures ▪ Contact medical command for further guidance
Toxicological and Opioid Emergencies ▪ Synthetic stimulants ▪ Effects of synthetic stimulants ▪ Psychological ▪ ▪ ▪ ▪ ▪ Agitation Insomnia Irritability Dizziness Depression Paranoia Delusions Suicidal ideation Seizures Panic attacks
Toxicological and Opioid Emergencies ▪ Synthetic stimulants ▪ Effects of synthetic stimulants ▪ Somatic ▪ Hyperthermia ▪ Even with normal ambient temperature ▪ Tachycardia ▪ Can lead to MI and stroke ▪ ▪ Chest pain Diaphoresis Epistaxis Nausea/Vomiting

Toxicological and Opioid Emergencies ▪ Types of synthetic stimulants ▪ Bath salts ▪ Known as: ▪ Bliss, Blue silk, Ivory wave, White dove, White knight, White lightning ▪ Delivered as: ▪ Typically in powdered form ▪ Can be in a capsule ▪ White to off-white in color ▪ Administered: ▪ Typically nasal ▪ Can also be taken orally, IV, or smoked
Toxicological and Opioid Emergencies ▪ Types of synthetic stimulants ▪ Methamphetamine ▪ Known as ▪ Crank, Crystal meth, Glass, Ice, Tweak, Yaba ▪ Delivered as ▪ Usually in crystal form or crystalline powder ▪ White to off-white in color ▪ Yellow or red in powder form ▪ Administered ▪ Typically smoked, snorted, or IV
Toxicological and Opioid Emergencies ▪ Types of synthetic stimulants ▪ Methylenedioxymethamphetamine (MDMA) ▪ Known as ▪ Ecstasy, E, X, XTC, Smarties, Scooby-snacks, Skittles ▪ Delivered as ▪ Typically tablets or capsules ▪ Can be liquid ▪ Can be any color ▪ Administered ▪ Oral liquid drops, snorted, smoked
Toxicological and Opioid Emergencies ▪ Tetrahydrocannabinol (THC) ▪ Natural ▪ Known as ▪ Weed, bud, doobie, Mary-Jane, pot, blunt, herb, grass, hemp ▪ Delivered as ▪ A green, brown, or gray mixture of dried, shredded leaves, stems, seeds, and flowers of the hemp plant ▪ Administered ▪ Usually smoked in a cigarette or pipe
Toxicological and Opioid Emergencies ▪ Tetrahydrocannabinol (THC) ▪ Synthetic ▪ Known as ▪ K 2, spice, black mamba, Bombay blue, genie, zohai ▪ Delivered as ▪ Similar appearance to natural ▪ Administered ▪ Same as natural ▪ Can cause psychosis
Toxicological and Opioid Emergencies ▪ Tetrahydrocannabinol (THC) ▪ Effects of THC ▪ Impaired short term memory ▪ Decreased concentration ▪ Decreased attention ▪ Impaired coordination ▪ Tachycardia ▪ Increased BP ▪ Increased appetite
Toxicological and Opioid Emergencies ▪ Synthetic or semi-synthetic opioids ▪ Act as CNS depressant ▪ Decrease perception of pain ▪ Decrease reaction to pain ▪ Increase pain tolerance ▪ May be prescribed for acute or chronic pain ▪ Prolonged use may lead to tolerance and/or addiction ▪ Abused to induce euphoria
Toxicological and Opioid Emergencies ▪ Synthetic or semi-synthetic opioids ▪ Common effects ▪ ▪ ▪ ▪ Respiratory depression Drowsiness Constipation Constricted pupils Dry mouth Itching Nausea/Vomiting
Toxicological and Opioid Emergencies ▪ Synthetic or semi-synthetic opioids ▪ Common opioids ▪ Heroin ▪ Made from morphine ▪ Can be a white or brown powder ▪ Can also be a black sticky substance ▪ Commonly known as Big H, horse, hell dust, or smack ▪ Can be injected, snorted, or smoked ▪ Speedballing is administering a mix of heroin and crack cocaine
Toxicological and Opioid Emergencies ▪ Synthetic or semi-synthetic opioids ▪ Common opioids ▪ Morphine ▪ Oxycodone (Percocet) ▪ Codeine ▪ Fentanyl ▪ Hydrocodone (Vicodin) ▪ Hydromorphone (Dilaudid) ▪ Meperidine (Demerol) ▪ Methadone
Toxicological and Opioid Emergencies ▪ Treatment for opioid emergencies ▪ Naloxone (Narcan) ▪ Opioid antagonist ▪ Blocks opioid receptors by locking onto opioid receptors without activating them ▪ Reverses CNS and respiratory depression caused by opioid use ▪ Naloxone has a greater affinity for the opioid receptor than the opioid itself knocking the opioid from the receptor and deactivating the receptor in the process ▪ If opioid was taken with additional non-opioid drug substances or alcohol it may take additional time or possibly require additional dosing. ▪ If opioid was taken with non-opioid drug substances those drug effects will remain
Toxicological and Opioid Emergencies ▪ Treatment for opioid emergencies ▪ Naloxone (Narcan) ▪ Not effective on non-opioid drugs ▪ Due to the mechanism of action for Naloxone non-opioid drugs would not be effected but the administration of Naloxone. ▪ Availability ▪ The WV Board of Pharmacy allows any Pharmacist, Pharmacist Intern, or Pharmacy Intern to dispense Nalaxone without a prescription as long as counseling is provided to the recipient regarding: ▪ Administration ▪ When and why to contact EMS ▪ The risks of not contacting EMS following administration
Toxicological and Opioid Emergencies ▪ Treatment for opioid emergencies ▪ Naloxone (Narcan) ▪ Administration ▪ Narcan is available for administration via ▪ Intranasal ▪ Used by EMS and public with training ▪ Can be either a prefilled cartridge with an atomizer or a one time use nasal spray ▪ One time use nasal spray received by the public is dispensed as 4 mg ▪ IV/IO ▪ Used by EMS and higher trained medical personnel ▪ Can be either a prefilled cartridge or a multi-dose vial ▪ IM ▪ Used by general public with training ▪ Works like an EPI-PEN with a retractable needle system ▪ One time use dispensed as 2 mg ▪ May have a longer activation time due to the IM route
Immunological Emergencies ▪ Allergic reactions are a hyperactive localized immune response to an allergen ▪ Some histamine is released but not in excessive amounts ▪ Usually requires only minimal supportive therapy ▪ Repeat exposures to an allergen may cause anaphylaxis
Immunological Emergencies ▪ Allergic reaction ▪ Symptoms ▪ Mild reactions ▪ Redness ▪ At and around the sight of allergen contact ▪ Swelling ▪ At and around the sight of allergen contact ▪ Hives ▪ May be present in multiple areas ▪ Itching ▪ At the sight and any areas where hives are present
Immunological Emergencies ▪ Allergic reaction ▪ Treatment ▪ Mild reactions ▪ Usually involves some slight increase in respiratory effort but does not involve wheezing or stridor ▪ Remove mechanism of administration if present (i. e. : stinger) ▪ Provide O 2 therapy and supportive care ▪ Administer Diphenhydramine ▪ Adults ▪ 25 mg IM or SLOW IV/IO push q 30 if necessary ▪ Pediatric ▪ 1 mg/kg IM or SLOW IV push to max of 25 mg
Immunological Emergencies ▪ Allergic reaction ▪ Symptoms ▪ Moderate reactions ▪ Presence of same symptoms of mild reactions ▪ Possibly to a greater extent on redness, hives, and itching ▪ Also present with ▪ Significant increase in work of breathing ▪ Wheezing may be evident ▪ Stridor may be evident ▪ Abnormal breath sounds may be evident
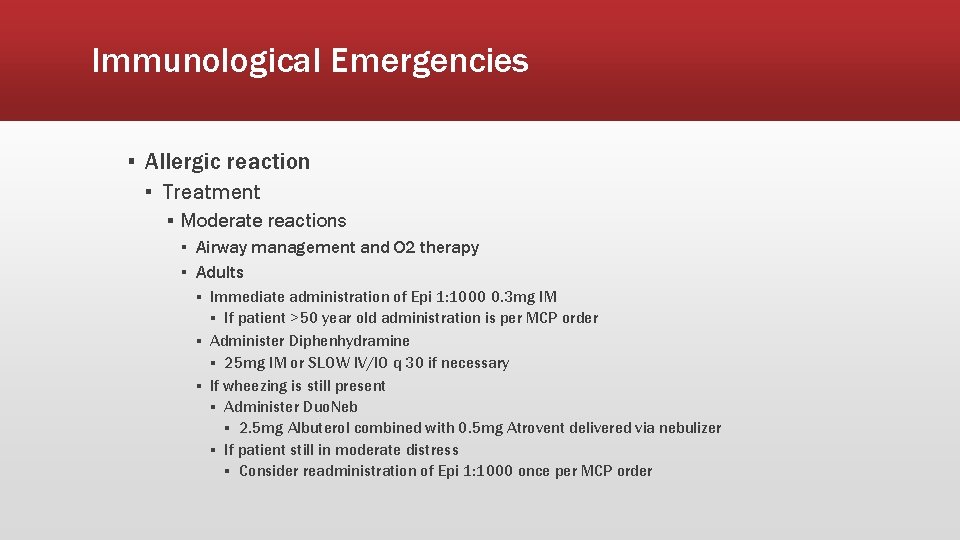
Immunological Emergencies ▪ Allergic reaction ▪ Treatment ▪ Moderate reactions ▪ Airway management and O 2 therapy ▪ Adults ▪ Immediate administration of Epi 1: 1000 0. 3 mg IM ▪ If patient >50 year old administration is per MCP order ▪ Administer Diphenhydramine ▪ 25 mg IM or SLOW IV/IO q 30 if necessary ▪ If wheezing is still present ▪ Administer Duo. Neb ▪ 2. 5 mg Albuterol combined with 0. 5 mg Atrovent delivered via nebulizer ▪ If patient still in moderate distress ▪ Consider readministration of Epi 1: 1000 once per MCP order
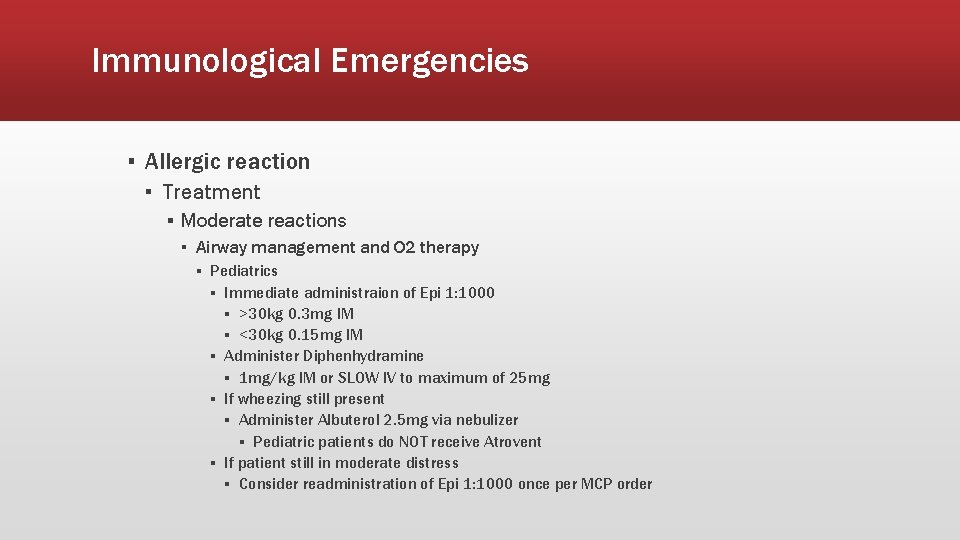
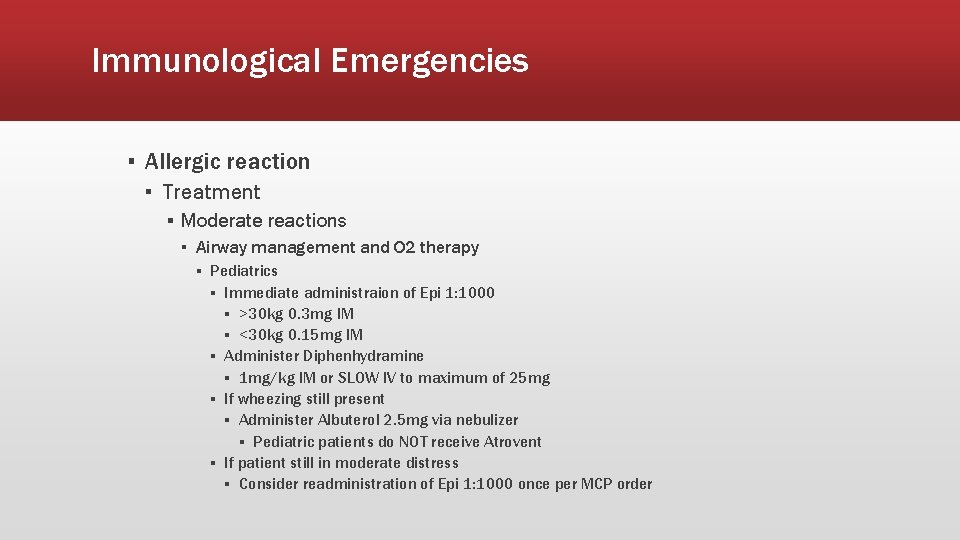
Immunological Emergencies ▪ Allergic reaction ▪ Treatment ▪ Moderate reactions ▪ Airway management and O 2 therapy ▪ Pediatrics ▪ Immediate administraion of Epi 1: 1000 ▪ >30 kg 0. 3 mg IM ▪ <30 kg 0. 15 mg IM ▪ Administer Diphenhydramine ▪ 1 mg/kg IM or SLOW IV to maximum of 25 mg ▪ If wheezing still present ▪ Administer Albuterol 2. 5 mg via nebulizer ▪ Pediatric patients do NOT receive Atrovent ▪ If patient still in moderate distress ▪ Consider readministration of Epi 1: 1000 once per MCP order
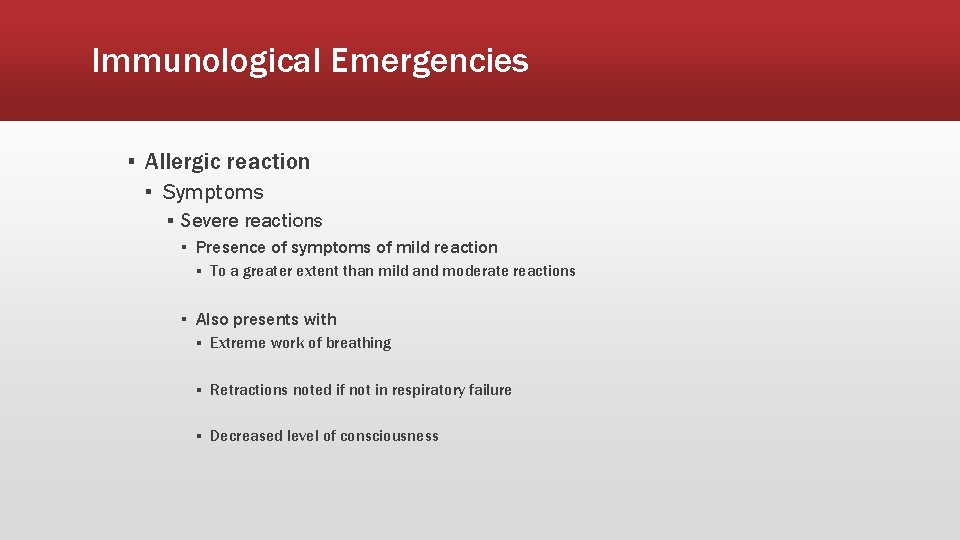
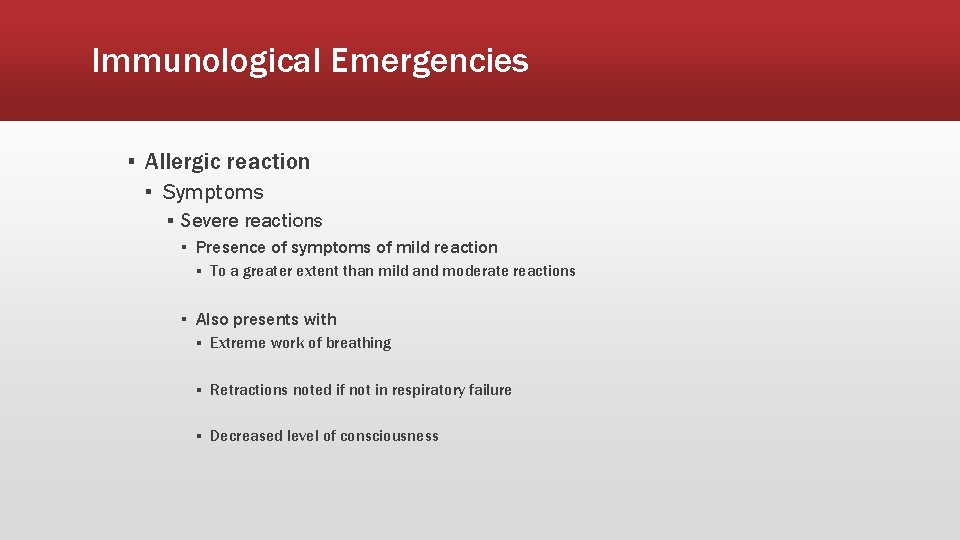
Immunological Emergencies ▪ Allergic reaction ▪ Symptoms ▪ Severe reactions ▪ Presence of symptoms of mild reaction ▪ To a greater extent than mild and moderate reactions ▪ Also presents with ▪ Extreme work of breathing ▪ Retractions noted if not in respiratory failure ▪ Decreased level of consciousness
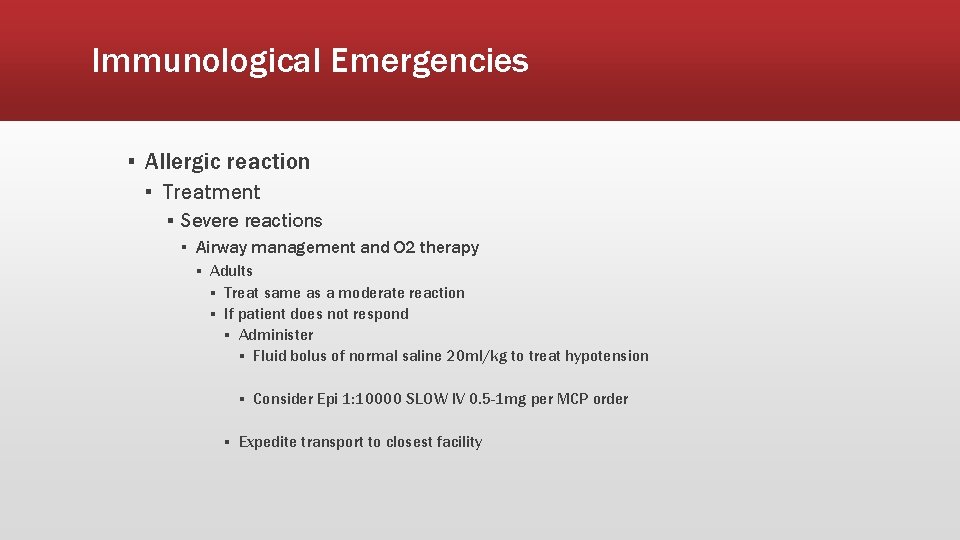
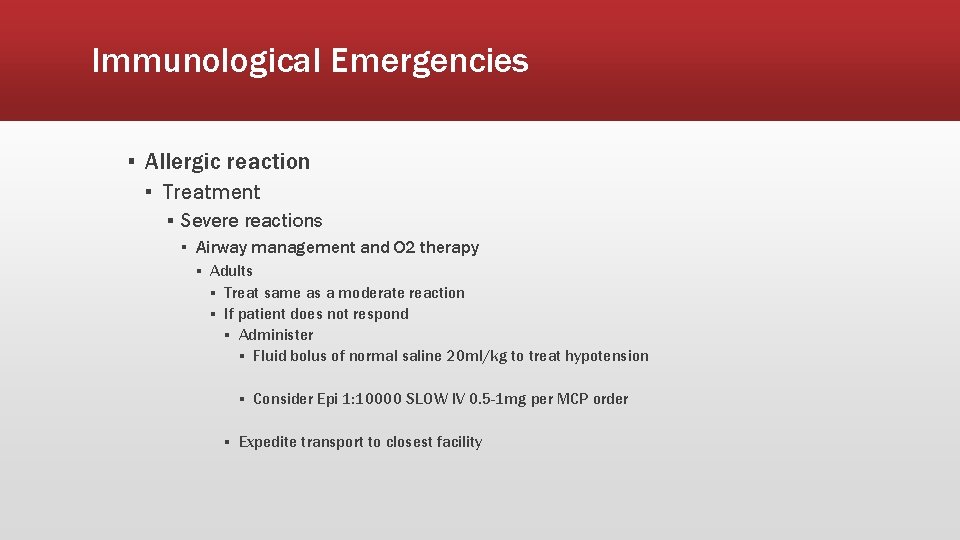
Immunological Emergencies ▪ Allergic reaction ▪ Treatment ▪ Severe reactions ▪ Airway management and O 2 therapy ▪ Adults ▪ Treat same as a moderate reaction ▪ If patient does not respond ▪ Administer ▪ Fluid bolus of normal saline 20 ml/kg to treat hypotension ▪ Consider Epi 1: 10000 SLOW IV 0. 5 -1 mg per MCP order ▪ Expedite transport to closest facility
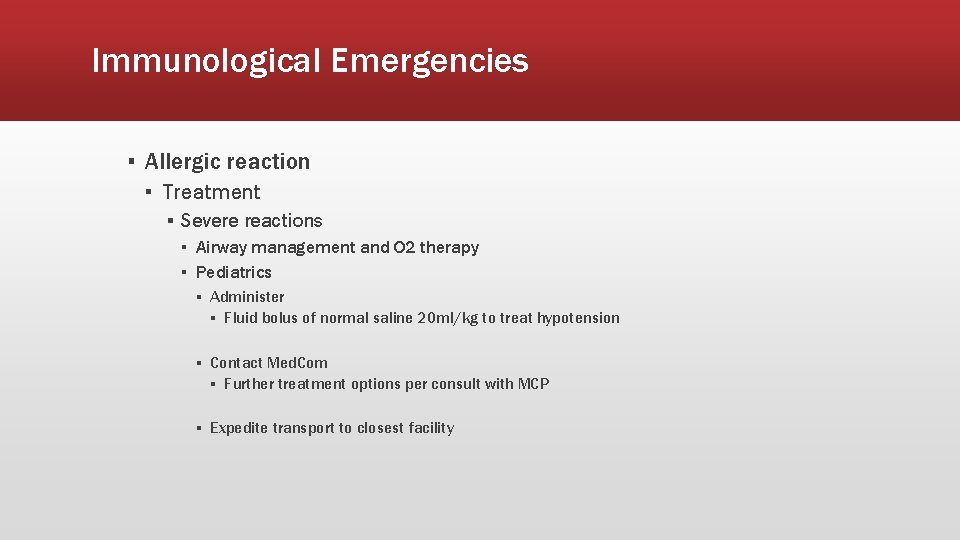
Immunological Emergencies ▪ Allergic reaction ▪ Treatment ▪ Severe reactions ▪ Airway management and O 2 therapy ▪ Pediatrics ▪ Administer ▪ Fluid bolus of normal saline 20 ml/kg to treat hypotension ▪ Contact Med. Com ▪ Further treatment options per consult with MCP ▪ Expedite transport to closest facility
Immunological Emergencies ▪ Anaphylaxis ▪ Allergic reaction affecting multiple body systems ▪ Potentially life threatening immune reaction to an allergen ▪ Large amounts of histamine release throughout the body ▪ Causes vasodiltation and increased capillary permiability
Immunological Emergencies ▪ Anaphylaxis ▪ Can lead to distributive shock ▪ Increased bronchoconstriction and mucus production ▪ Increased respiratory distress ▪ Swelling of the upper airway ▪ Causes wheezing and stridor ▪ Possible airway obstruction ▪ Could be mucus or the airway constricting completely on itself
Immunological Emergencies ▪ Anaphylaxis ▪ Treatment ▪ First line is Epi ▪ Reverses bronchodilation and vasoconstriction ▪ Requires continuous reassessment ▪ May require addition dosing due to short half-life ▪ Second line is Diphenhyramine ▪ Blocks histamine receptors ▪ Inhibits further histamine release ▪ Third line is Duo. Neb ▪ Bronchodilation ▪ Used is wheezing still present post Epi administration

Immunological Emergencies ▪ Mild allergic reaction
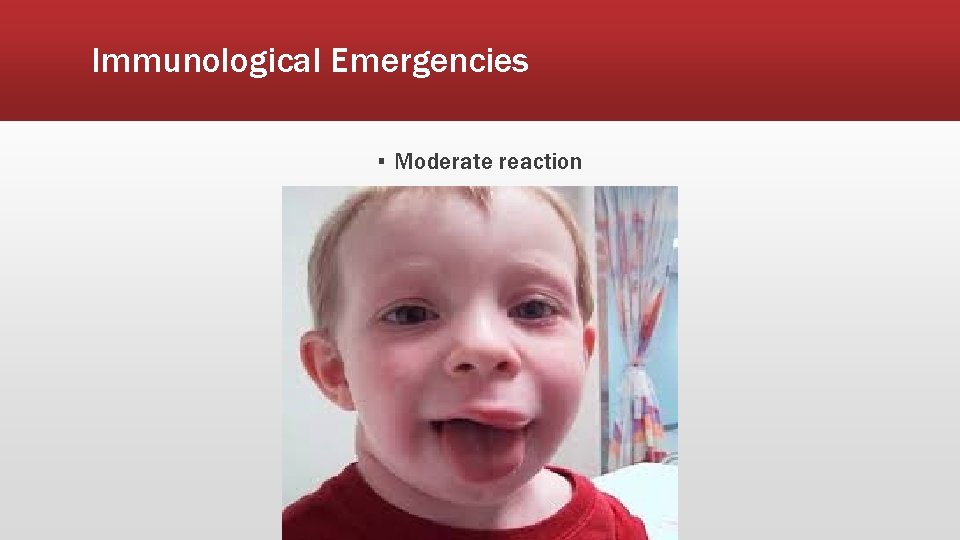
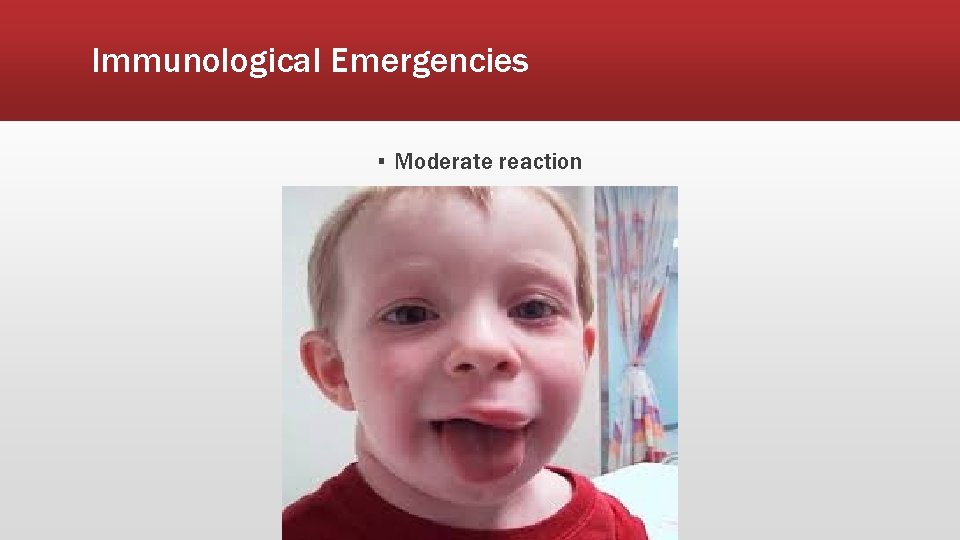
Immunological Emergencies ▪ Moderate reaction

Immunological Emergencies ▪ Anaphylactic reaction
Pharmacology and Medication Delivery ▪ Routes of administration ▪ Parenteral ▪ Intramuscular (IM) ▪ ▪ ▪ Faster than oral onset Absorption rate depends on site and circulation Onset usually within 10 -20 minutes but can be quicker Must use needle long enough to reach striated muscle tissue Injection sites ▪ Deltoid ▪ Volume up to 2 m. L ▪ Faster than other sites ▪ Gluteus Maximus ▪ Volume up to 5 m. L ▪ Vastus lateralus ▪ Volume up to 5 m. L
Pharmacology and Medication Delivery ▪ Routes of administration ▪ Parenteral ▪ Subcutaneous (SQ) ▪ ▪ Slower than IM or IV Absorption rate depends on circulation Onset 15 -30 minutes Injection sites ▪ Arm ▪ Volume ≤ 0. 5 m. L ▪ Vastus lateralus ▪ Volume ≤ 2 m. L ▪ Injection angle ▪ 15 -20 degrees
Pharmacology and Medication Delivery ▪ Routes of administration ▪ Parenteral ▪ Intravenous (IV) ▪ ▪ Injection straight into the systemic circulation most common parenteral route bypasses absorption barriers and first-pass metabolism used when a rapid effect is required, continuous administraction and large volumes ▪ Onset various based on the drug of use
Pharmacology and Medication Delivery ▪ Routes of administration ▪ Enteral ▪ Per Os (PO) ▪ Passes into blood through GI tract ▪ Onset rates vary for multiple reasons ▪ Type of medication ▪ Rate of absorption in GI tract ▪ Extent of absorption in GI tract ▪ Bioavailability ▪ Based on the rate and completeness of absorption ▪ Rate is based on the type of medication ▪ Solution ▪ Suspension ▪ Capsule ▪ Tablet ▪ Coated tablet
Pharmacology and Medication Delivery ▪ Routes of administration ▪ Enteral ▪ Sublingual (SL) ▪ Administered beneath the tongue ▪ To be dissolved, not chewed/swallowed ▪ Blood vessels in the mouth bypass the liver ▪ Passes directly into the systemic circulation following absorption ▪ Rate of dissolution various depending on the moisture content in the mouth ▪ Typically reserved for nitrates
Pharmacology and Medication Delivery ▪ Routes of administration ▪ Other ▪ Intranasal (IN) ▪ ▪ ▪ ▪ Absorbed circulation through mucus membranes Atomizer must be used for full dispersal of medication Ease of administration Rapid absorption rate Ideal volume per nostril 0. 3 ml Higher volume per nostril could cause “runoff” Severely clogged nasal passages (i. e. : mucus, emesis) could cause delays in absorption
Pharmacology and Medication Delivery ▪ Routes of administration ▪ Other ▪ Inhalation ▪ Nebulized medications ▪ Rapid delivery across the mucous membranes of the respiratory tract ▪ Rapid onset, similar to IV rates ▪ Decreased tidal volume could reduce the effect of the medication ▪ Repeated dosing may be required
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Acetaminophen (Tylenol), 160 mg/5 m. L oral suspension ▪ ▪ ▪ Antipyretics, nonopioid analgesics PO treatment for fever Onset 0. 5 -1 hour Peak 1 -5 hours Half life varies by age If temperature is > 102° F ▪ Facilitate passive cooling by removing excess clothing and blankets ▪ If child has not been given Acetaminophen in the last four (4) hours, administer Acetaminophen at 15 mg/kg
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Albuterol 2. 5 mg/3 m. L unit dose ▪ Bronchodilators ▪ Binds to beta 2 -adrenergic receptors in airway smooth muscle ▪ Nebulized ▪ Onset 5 -15 minutes ▪ Peak 1 -1. 5 hours ▪ Duration 3 -6 hours ▪ Use caution in cardiac disease ▪ Beta blockers may negate therapeutic effect
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Ipratropium ▪ Bronchodilator ▪ Inhibits cholinergic receptors in bronchial smooth muscle ▪ Nebulized ▪ Onset 1 -3 minutes ▪ Peak 1 -2 hours ▪ Duration 4 -6 hours
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Amiodarone ▪ Antiarrhythmics ▪ Prolongs action potential and refractory period ▪ Contraindicated in ▪ Cardiogenic shock ▪ 2 nd degree AV block ▪ 3 rd degree AV block ▪ Onset 1 -30 minutes ▪ Peak 30 minutes

Pharmacology and Medication Delivery ▪ Pharmacology ▪ Aspirin ▪ ▪ ▪ ▪ Analgesics Salicylates Well absorbed from the upper small intestine Contraindicated hypersensitivity to aspirin or other salicylates Onset 5 -30 minutes Peak 1 -3 hours Duration 3 -6 hours
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Adenosine ▪ Antiarrhythmic ▪ Conversion of SVT/PSVT to normal sinus rhythm when vagal maneuvers are unsuccessful ▪ Restores normal sinus rhythm by interrupting re-entrant pathways in the AV node ▪ Contraindicated in hypersensitivity, 2 nd or 3 rd degree AV block, or sick sinus syndrome ▪ Onset immediate ▪ Peak unknown ▪ Duration 1 -2 minutes ▪ Adenosine 6 mg IVP If no conversion in 1 - 2 min then Adenosine 12 mg IVP
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Atropine ▪ ▪ ▪ ▪ ▪ Antiarrhythmics Treatment of sinus bradycardia and heart block Increased heart rate May alter response to beta-blocker Onset immediate Peak 2 -4 minutes Duration 4 -6 hours 0. 5 mg IV q 3 - 5 minutes as necessary to max of 3 mg Atropine administration should not delay implementation of external pacing for patients
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Dextrose ▪ ▪ ▪ ▪ Caloric sources Prevention and treatment of hypoglycemia Administered PO or IV Onset rapid Peak rapid Duration brief If blood glucose is < 60 mg/dl D 50 25 grams IVP May be repeated once q 5 minutes if patient remains hypoglycemic
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Diltiazem ▪ ▪ ▪ Antiarrhythmic Calcium channel blocker Inhibits transport of calcium into myocardial cells Reduction of ventricular rate in atrial fibrillation or flutter If Symptomatic Atrial Fibrillation or Atrial Flutter consider Diltiazem 0. 25 mg/kg slow IVP q 15 at 0. 35 mg/kg slow IVP per MCP order
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Diphenhydramine ▪ ▪ ▪ ▪ Antihistamine Relief of allergic symptoms caused by histamine release Antagonizes the effects of histamine at H 1 -receptor sites Onset rapid Peak unknown Duration 4 -8 hours 25 mg IM or slow IV/IO q 30 minutes if symptoms persist
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Dopamine ▪ Inotropic, vasopressor ▪ Adjunct to standard measures to improve BP and Cardiac output ▪ Larger doses 2– 10 mcg/kg/min stimulate dopaminergic and beta 1 adrenergic receptors, producing cardiac stimulation ▪ Contraindicated in tachyarrhythmias ▪ If hypotension (BP < 90 systolic) and other signs and symptoms of shock persist after administration of second 20 ml/kg normal saline bolus ▪ consider Dopamine IV drip infusion at 5 micrograms/kg/minute per MCP order ▪ Titrate Dopamine drip at 5 - 20 micrograms/kg per minute in an effort to improve perfusion per MCP order
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Epinephrine ▪ Adrenergic ▪ Affects both beta 1(cardiac) adrenergic receptors and beta 2 (pulmonary) adrenergic receptor sites ▪ Onset rapid ▪ Peak 20 minutes ▪ Duration 20 -30 minutes ▪ Cardiac arrest Epinephrine 1 mg q 3 – 5 until ROSC or termination ▪ Anaphylaxis administer Epinephrine, 1: 1000 0. 3 mg IM, If > 50 per MCP order
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Fentanyl ▪ ▪ ▪ ▪ Opioid analgesic Schedule II Binds to opiate receptors in the CNS Onset 1 -2 minutes Peak 3 -5 minutes Duration 0. 5 -1 hour Administer Fentanyl 1 mcg/kg up to 100 mcg max single dose slow IV If no pain relief after 2 minutes may repeat per MCP order at 1 mcg/kg to 100 mcg max per dose
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Lasix ▪ Diuretic ▪ Inhibits the reabsorption of sodium and chloride from the loop of Henle and distal renal tubule ▪ Increases renal excretion of water, sodium, chloride, magnesium, potassium, and calcium ▪ Onset 5 minutes ▪ Peak 30 minutes ▪ Duration 2 hours ▪ If patient DOES NOT take Lasix and systolic BP remains > 100 post Nitro administer 40 mg IV/IO ▪ If patient DOES take Lasix and systolic BP remains > 100 post Nitro administer 80 mg IV/IO
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Glucagon ▪ Hormone ▪ Acute management of severe hypoglycemia if administration of glucose is not available ▪ Stimulates hepatic production of glucose from glycogen stores ▪ Onset within 10 minutes ▪ Peak 30 minutes ▪ If unable to initiate an IV and blood glucose is < 60 mg/dl administer Glucagon 1 mg IM (if over 25 kg) or 0. 5 mg IM (if < 25 kg)
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Haldol ▪ Antipsychotic ▪ Acute and chronic psychotic disorders including schizophrenia, manic states, drug induced psychoses ▪ Alters the effects of dopamine in the CNS ▪ If patient remains agitated or aggressive post Versed in 5 minutes administer Haldol 5 mg IM ▪ If dystonic reaction (dyskinesia) is noted secondary to Haldol administer diphenhydramine 25 mg IV or IM

Pharmacology and Medication Delivery ▪ Pharmacology ▪ Labetalol ▪ ▪ Antihypertensive Blocks stimulation of beta 1 and beta 2 adrenergic receptor sites Treatment goal reduce MAP by 10 - 15% of initial value Measure blood pressure manually every five (5) minutes. If two (2) successive readings have a systolic > 240 or a diastolic >120 mm. Hg ▪ Per MCP order ▪ Initial 10 mg slow IV push over 2 minutes ▪ Repeat in 10 minutes at 20 mg if BP remains > 180/120 and symptoms remain
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Lidocaine ▪ Antiarrhythmics ▪ Ventricular arrhythmias ▪ Suppresses automaticity and spontaneous depolarization of the ventricles during diastole ▪ VF/VT arrest 1. 0 – 1. 5 mg/kg IV/IO repeated at 0. 5 – 0. 75 mg/kg IV/IO at 10 minute intervals to a max dose of 3 mg/kg ▪ Wide complex tachycardia 0. 5 to 0. 75 mg/kg every 5 - 10 minutes with maximum total dose of 3 mg/kg
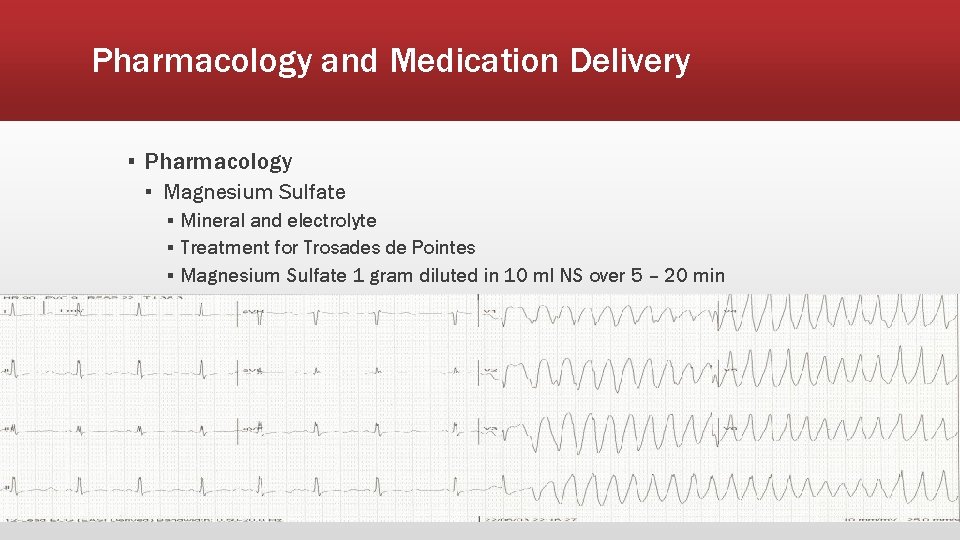
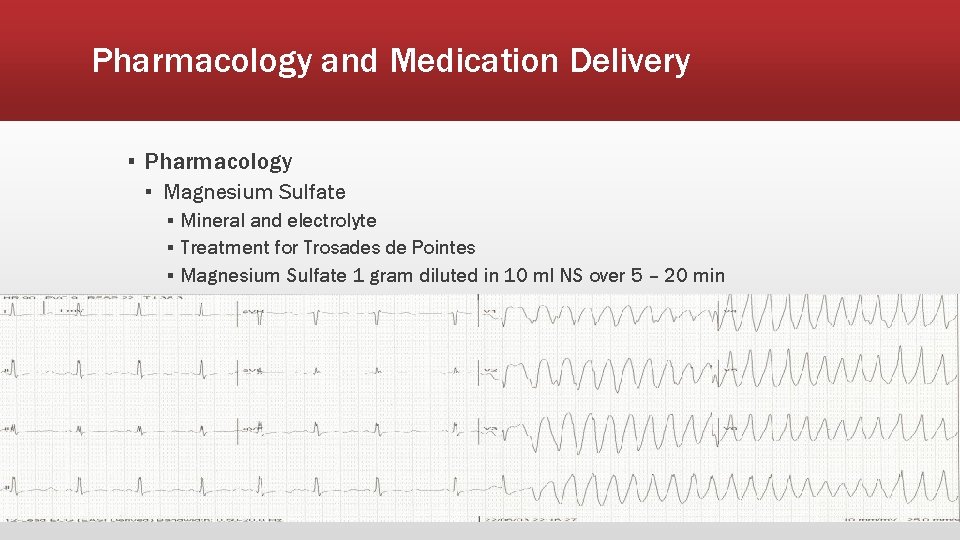
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Magnesium Sulfate ▪ Mineral and electrolyte ▪ Treatment for Trosades de Pointes ▪ Magnesium Sulfate 1 gram diluted in 10 ml NS over 5 – 20 min
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Versed ▪ Benzodiazepine ▪ Acts at many levels of the CNS to produce generalized CNS depression ▪ If seizure lasts longer than 5 minutes or 2 or more episodes of seizure activity occur between which the patient does not regain consciousness, administer Versed 2 mg IV/IO/IM or 5 mg IN ▪ > 55 years old administer Versed 1 mg IV/IO/IM or 5 mg IN ▪ If agitation is suspected administer Versed 5 mg IV/IM/IN ▪ > 55 years old administer Versed 2 mg IV/IM or 5 mg IN
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Morphine ▪ Opioid ▪ Management of moderate to severe chronic pain ▪ Binds to opiate receptors in the CNS. Alters the perception of and response to painful stimuli while producing generalized CNS depression ▪ Administer Morphine 2 mg slow IV q 5 as necessary to max total dose 10 mg or pain relief ▪ DO NOT administer Morphine Sulfate to children less than 12 years old without MCP order pediatric dose of Morphine Sulfate is 0. 05 mg/kg ▪ > 55 years old administer Morphine 1 mg slow IV q 5 to max total dose 10 mg or pain is relief
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Naloxone ▪ Opioid antagonist ▪ Reversal of CNS depression and respiratory depression because of suspected opioid overdose ▪ Competitively blocks the effects of opioids ▪ Administer Naloxone up to 2 mg IV titrated slowly at 0. 4 mg/minute to restore the respiratory drive. If patient does not show signs of improvement administer up to an additional 2 mg IV titrated slowly at 0. 4 mg/minute ▪ If unable to obtain IV access, give Naloxone 2 mg IN 1 mg per nostril. If patient does not show signs of administer an additional 2 mg IN
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Nitroglycerin ▪ Nitrate ▪ Increases coronary blood flow by dilating coronary arteries and improving collateral flow to ischemic regions ▪ If patient has a BP < 90 DO NOT administer nitroglycerin ▪ If 12 lead ECG indicates Inferior Wall AMI a 12 lead ECG should be obtained using right chest leads (V 4 R at a minimum). If right chest leads show ST Segment elevation, DO NOT administer sublingual Nitroglycerin ▪ If blood pressure is > 90 mm/hg systolic and patient has not taken erectile dysfunction medication within 24 -72 hours administer Nitroglycerin 0. 4 mg SL q 3 - 5 to a maximum of 3 doses or pain is relief
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Zofran ▪ Antiemetic ▪ Prevention of nausea and vomiting ▪ Administer Zofran 4 mg ODT Tablet PO dissolved in mouth or 4 mg undiluted IVP over 4 minutes or IM ▪ Administration of Zofran is contraindicated in preexisting prolonged QT interval
Pharmacology and Medication Delivery ▪ Pharmacology ▪ Thiamine ▪ ▪ Vitamin Prevention of Wernicke’s encephalopathy Required for carbohydrate metabolism Use caution in Wernicke’s encephalopathy as condition may be worsened unless thiamine is administered before glucose ▪ If patient is malnourished, has HIV/AIDS, receives dialysis, is a known alcoholic, or has other grossly impaired nutritional status, administer Thiamine 100 mg slow IVP over 1 minute, prior to Dextrose administration, or Thiamine 100 mg IM prior to Glucagon administration
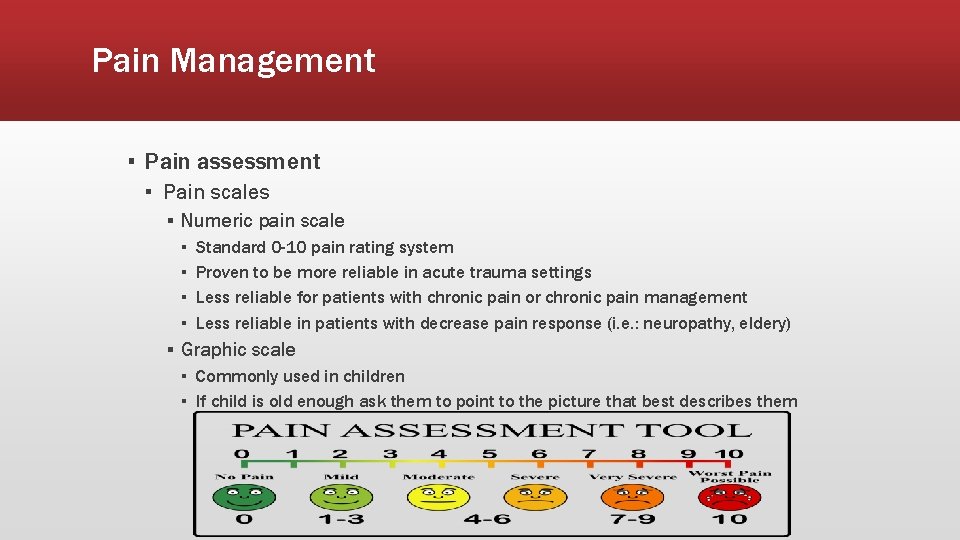
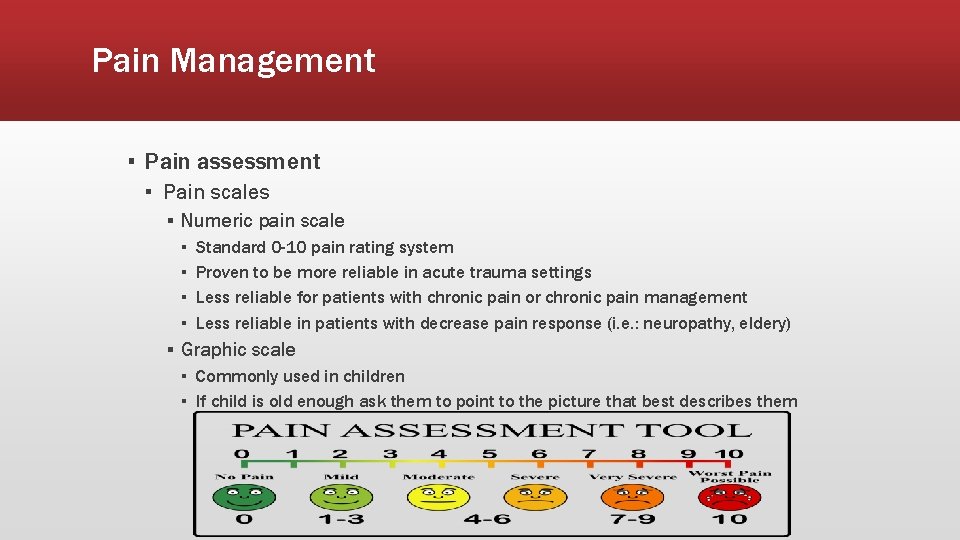
Pain Management ▪ Pain assessment ▪ Pain scales ▪ Numeric pain scale ▪ ▪ Standard 0 -10 pain rating system Proven to be more reliable in acute trauma settings Less reliable for patients with chronic pain or chronic pain management Less reliable in patients with decrease pain response (i. e. : neuropathy, eldery) ▪ Graphic scale ▪ Commonly used in children ▪ If child is old enough ask them to point to the picture that best describes them
Pain Management ▪ Pain assessment ▪ When using a pain scale assessment you must use the same scale for reassessments that was used for primary assessment ▪ When assessing pain be alert for the various dimensions of pain ▪ Physiologic ▪ Acute response to pain ▪ Somatic pain ▪ Skin, muscles, connective tissue, bones, joints ▪ Visceral pain ▪ Organs, gastrointestinal tract
Pain Management ▪ Pain assessment ▪ Dimensions of pain ▪ Psychological ▪ How a patient responds to pain ▪ Some patients may actively work to calm themselves reducing the perception of pain ▪ Some patients may be unable to calm themselves and require assistance to focus their attentions somewhere else ▪ Patient could have psychological issues that exacerbate response to pain ▪ Patients with anxiety or that experience syncope with high stress events ▪ Being able to calm the patient will have an impact on pain management
Pain Management ▪ Pain assessment ▪ Dimensions of pain ▪ Emotional ▪ The emotional response to pain cause variances in the presentation of pain ▪ Injuries that create any amount of physical pain can also create an emotional response that occurs at time of incident or later ▪ Pain that is chronic or physically disfiguring injuries can cause greater emotional responses leading to ▪ Stress ▪ Anxiety ▪ Depression
Pain Management ▪ Pain assessment ▪ Dimensions of pain ▪ Behavioral ▪ Mostly observed in chronic pain patients ▪ Interaction between the patient and their environment ▪ Made up of three dimensions and nine components ▪ Dimensions ▪ Withdrawal approach ▪ High-arousal/Low-arousal ▪ Visible-audible ▪ Components ▪ anxiety, attention seeking, verbal pain complaints, medication use, general verbal complaints, distorted posture and mobility, fatigue, insomnia, and depressive mood
Pain Management ▪ Pain assessment ▪ Assessment ▪ Commonly pain is undertreated by EMS due to an underestimation of the patients needs ▪ Providers should base their management on a combination of the patient’s ▪ ▪ Presentation Pain scale rating How well the patient is managing the various dimensions of pain How well the provider can mitigate the responses from the dimensions of pain ▪ Providers should also use their prior experience to help in the determination of pain management
Pain Management ▪ Pain assessment ▪ Documentation ▪ Providers should be sure to thoroughly documents ▪ Presence of pain ▪ When, Where, Why ▪ Intensity of pain ▪ How bad is the pain ▪ Treatments for pain ▪ Any and all treatments administered for pain ▪ Be sure to include any additional treatments (i. e. : O 2, splinting, positioning, etc) ▪ Change in pain after treatment ▪ Did they pain and to what degree ▪ Any adverse effects to the patient with treatment

Pain Management ▪ Pain management ▪ Non-pharmacological ▪ Appropriate wording ▪ Be sure to speak calmly and effectively to patients ▪ While it can be easy to become excited or anxious ourselves in the presence of major injury remember you demeanor affects your patients ▪ Distraction ▪ Attempt to have the patient focus on other things ▪ Ask the patient to focus on respiratory rate ▪ Conversation ▪ Engage the patient in conversation not related to the injury when possible ▪ Parents ▪ If the patient is a child the presence of a parent of care giver may help to calm the patient
Pain Management ▪ Pain management ▪ Non-pharmacological ▪ Traditional techniques ▪ Immobilization ▪ Remember to immobilize all swollen joints to prevent further bone or soft tissue damage ▪ Elevation ▪ Ice ▪ Padding ▪ Pad the spaced in any immobilization device ▪ Pad the injured where it comes into contact with the resting surface
Pain Management ▪ Pain management ▪ Pharmacological ▪ Narcotic pain management ▪ Morphine ▪ ▪ ▪ Opioid Schedule II IV use is rapid onset peaking at 20 minutes with a duration of 4 -5 hours Use caution in head trauma, severe renal disease, decrease hepatic function Use caution in patients taking MAOIs within last 14 days Administer Morphine 2 mg slow IV q 5 to total of 10 mg or pain relief, whichever is first If systolic BP drops below 90 mm/Hg discontinue analgesic administration and administer IV fluid bolus 250 m. L Normal Saline ▪ DO NOT administer Morphine to children less than 12 years old without MCP order. Pediatric dose of Morphine is 0. 05 mg/kg per MCP order ▪ If patient >55 years old administer Morphine 1 mg slow IV q 5 to total of 10 mg or pain relief, whichever is first
Pain Management ▪ Pain management ▪ Pharmacological ▪ Narcotic pain management ▪ Fentanyl ▪ ▪ ▪ Opioid Schedule II IV use is onset 1 -2 minutes, peaks at 3 -5 minutes with a duration of 0. 5 -1 hour Use caution in head trauma, severe renal disease, decrease hepatic function Use caution in patients taking MAOIs within last 14 days Administer Fentanyl 1 mcg/kg slow IV up to 100 mcg max single dose If no pain relief after 2 minutes, may repeat Fentanyl per MCP at 1 mcg/kg up to 100 mcg max per dose ▪ DO NOT administer Fentanyl to children less than 12 years old without MCP order. Pediatric dose is 1 mcg/kg max dose of 50 mcg per MCP order ▪ If patient >55 years old administer Fentanyl 0. 5 mcg/kg up to a max initial dose of 100 mcg. Providers may repeat this dose 1 time as a standing order. Additional doses require MCP order
Pain Management ▪ Pain management ▪ Pharmacological ▪ Narcotic pain management ▪ It is important to note that when treating with narcotic pain medications the patient may become nauseas and/or vomit ▪ Consider the administration of Zofran 4 mg IV/IM slowly over 4 minutes ▪ Pediatric dose of Zofran is 0. 15 mg/kg IV to a max of 4 mg ▪ Special considerations ▪ If the patient is on chronic pain medication they may experience a decreased effect from the administration of these medications ▪ Some patients may request not to be treated with narcotic pain medication due to previous drug issues ▪ Consider additional non-pharmacological pain management techniques to be used in conjunction with pharmacological pain management
Pain Management ▪ Monitoring and documentation ▪ Analgesic treatment ▪ It is important to document the patient’s presentation both before and after analgesic treatments ▪ Vital signs ▪ Level of consciousness ▪ Before and after treatment ▪ Note any additional measures taken outside of analgesic administration and their effects ▪ Heart rate, BP, and Sp. O 2 ▪ Baseline vitals are required prior to any analgesic treatments ▪ Vitals should be reassessed after each intervention and at regular intervals throughout ▪ Document ▪ Any change in the patients clinical status positive or negative ▪ Corrective actions taken for any possible negative effects
Pain Management ▪ Monitoring and documentation ▪ Analgesic treatment ▪ Any pain medication not used during EMS intervention must be wasted ▪ A narcotic waste form should be filled out by the paramedic administering and wasting the medication ▪ If possible the waste should be witnessed by a third party medical provider (i. e. : nurse at receiving facility) and signed by the witness that the medication wasted in their presence ▪ All paperwork for the wasting of narcotics should be filed with your department for tracking and DEA records ▪ A copy of the waste form should be attached to the EPCR as part of the record
Pain Management ▪ Quality improvement and medical oversight ▪ Systems with established QI programs have a proven better compliance record with pain management protocols ▪ Training ▪ Each EMS organization various in size and staffing. It is important to ensure that the department is up-to-date on all protocols and procedures for use and handling of analgesics ▪ Departments should take steps to prevent mishaps by having recurring training in the use and administration of pain management techniques ▪ Tracking plan ▪ Each department should track the use of pain medication and review the EPCR for patients receiving pain medication ▪ Maybe more importantly departments should review the lack of pain medication use where significant levels of pain were reported to ensure that patients are being treated appropriately for their pain levels
Pain Management ▪ Quality improvement and medical oversight ▪ Feedback and discussion ▪ ED staff ▪ When possible the crew or a department representative should attempt to speak with ED staff as to the state of patients being brought into the ED and whether or not they are receiving proper treatment ▪ ED staff can sometimes advise when a patient was over or undertreated ▪ Medical Director ▪ ED feedback is an excellent tool but has a broader reach when used in discussion with the agency medical director to enhance trainings or identify trends ▪ Patient follow up if the patient is willing provides a great insight into how the patient felt they were treated and why they felt they may have been under/overtreated which can have significant value to the crews and departments
Pain Management ▪ Acute vs. chronic pain management ▪ Drug dependence ▪ A physical condition in which the body has adapted to the presence of a drug. If an individual with drug dependence stops taking that drug suddenly, that person will experience predictable and measurable symptoms, known as a withdrawal syndrome. ▪ Drug abuse ▪ Habitual use of drugs not needed for therapeutic purposes, solely to alter one’s mood, affect, or state of consciousness. ▪ Addiction ▪ Chronic, relapsing brain disease that is characterized by compulsive drug seeking and use, despite harmful consequences and this compulsion is long -lasting and can return unexpectedly after a period of improvement.
Pain Management ▪ Acute vs. chronic pain management ▪ Perform a thorough assessment prior to administration of pain medications ▪ Pain management should be dependent on objective evidence ▪ Does the patient present with pain ▪ Does the pain improve with non-pharmacologic interventions ▪ Does the patient’s complaint of pain match the patient’s clinical presentation ▪ Pain is subjective to each patient ▪ Each person perceives pain differently ▪ A patient not have much pain even with significant injury ▪ Do not assume your patient is overestimating pain just because you “think” it should not be that high of a rating

Pain Management ▪ Monitoring ▪ Analgesia ▪ Fentanyl ▪ ▪ ▪ Ideal pain management for EMS Rapid onset Short duration Multiple routes of administration (IV/IO for WV) Hemodynamically stable

Pain Management ▪ Monitoring ▪ Analgesia ▪ Morphine ▪ ▪ ▪ Long standing use in EMS Rapid onset Longer peak time Longer duration Not as hemodynamically stable as Fentanyl
Pain Management ▪ Monitoring ▪ Analgesia ▪ Ketamine ▪ At low doses ▪ ▪ ▪ Safe Hemodynamically stable No dissociation No respiratory compromise No gag reflex impairment Can be used in conjunction with opioids to enhance their effects in patients with significant injury or tolerance to medication
Pain Management ▪ Failure to treat ▪ EMS providers as a whole tend to undertreat patients complaining of pain ▪ This tends to occur more in abdominal pain patients ▪ EMS should not withhold pain medications from abdominal pain patients for fear of masking the pain ▪ The EMS provider’s job is to treat and care for patients and treating abdominal pain in the field should not lead to a failed diagnosis of the patient’s condition

Pain Management ▪ Sedation and chemical restraint ▪ Versed ▪ ▪ ▪ Optimal pre-hospital medication for agitation Rapid onset Multiple administration routes (IV/IM/IN in WV) Can cause respiratory depression Use caution in elderly

Pain Management ▪ Sedation and chemical restraint ▪ Ketamine ▪ ▪ ▪ In dissociative dose Rapid onset Hemodynamically stable Leaves gag reflex intact In rare cases causes laryngospasm Be familiar with the treatment of laryngospasm ▪ Larson maneuver ▪ Firmly push the soft tissue just behind the earlobes of the patient’s ears. Be sure not to go too inferiorly along the ramus of the mandible. You want to push at a point as superior as you can go in this notch. Push both sides firmly inward towards the skull base. Simultaneously, push anteriorly similar to a jaw-thrust maneuver. This should break the laryngospasm within 1 -2 breaths.