Assisted vaginal delivery via vacuum extraction Unit 3

- Slides: 39

Assisted vaginal delivery via vacuum extraction Unit 3: Introductory knowledge for the vacuum extraction procedure Refresher course for health care providers working in crisis settings
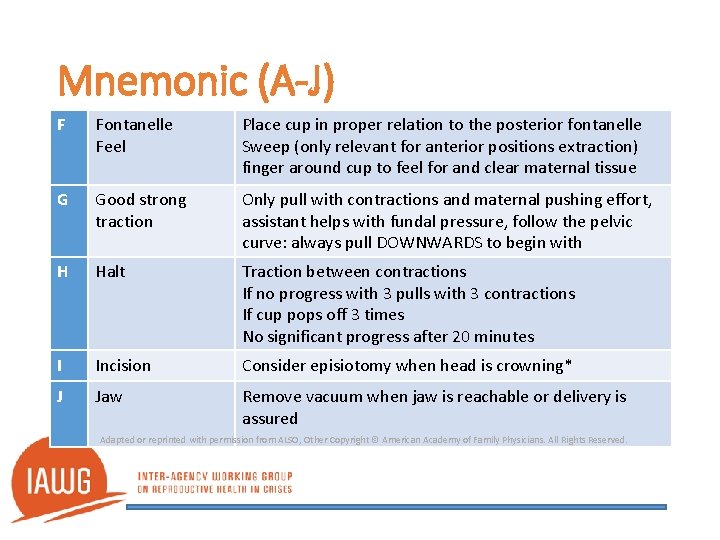
Anatomy of the fetal head World Health Organization. Managing complications in pregnancy and childbirth: A guide for midwives and doctors. Section 1 Clinical Principles.
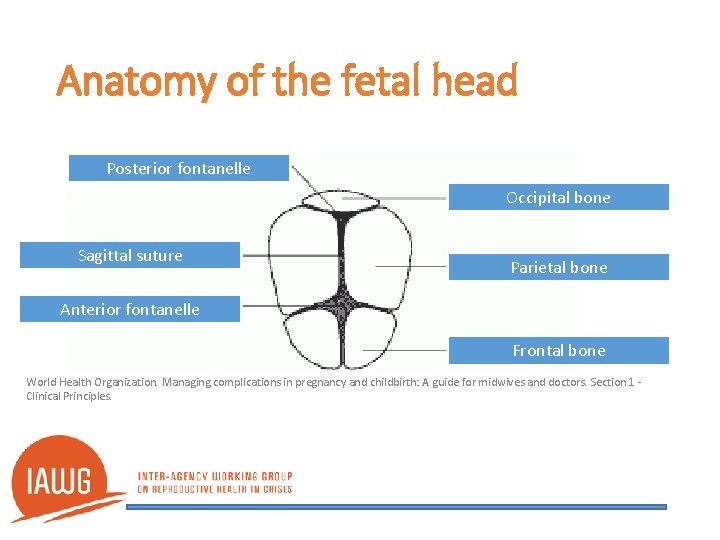
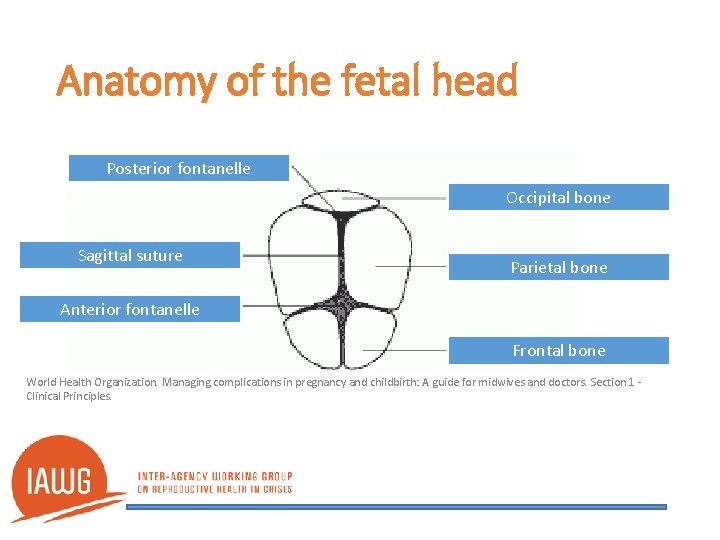
Anatomy of the fetal head Posterior fontanelle Occipital bone Sagittal suture Parietal bone Anterior fontanelle Frontal bone World Health Organization. Managing complications in pregnancy and childbirth: A guide for midwives and doctors. Section 1 Clinical Principles.
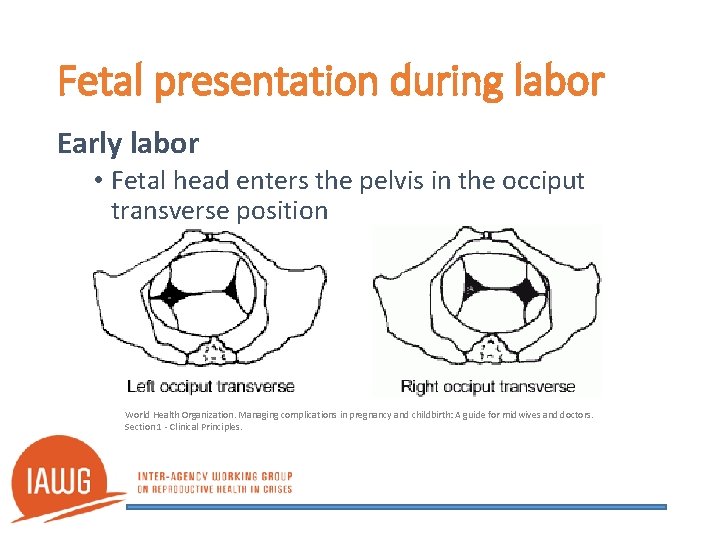
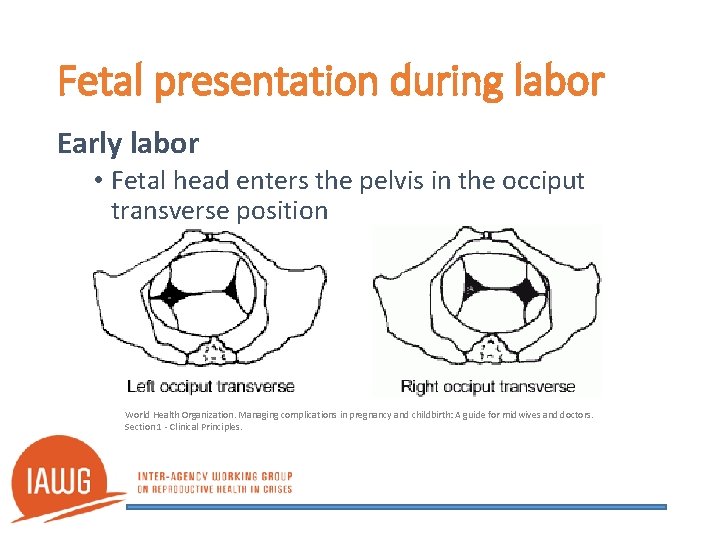
Fetal presentation during labor Early labor • Fetal head enters the pelvis in the occiput transverse position World Health Organization. Managing complications in pregnancy and childbirth: A guide for midwives and doctors. Section 1 - Clinical Principles.
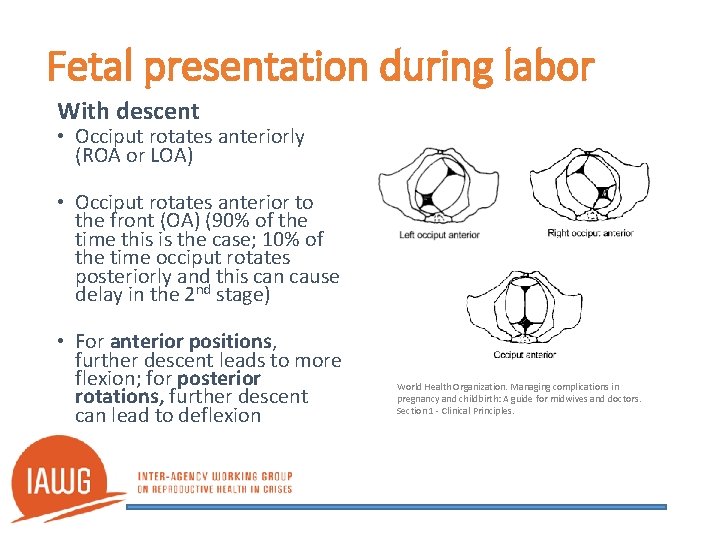
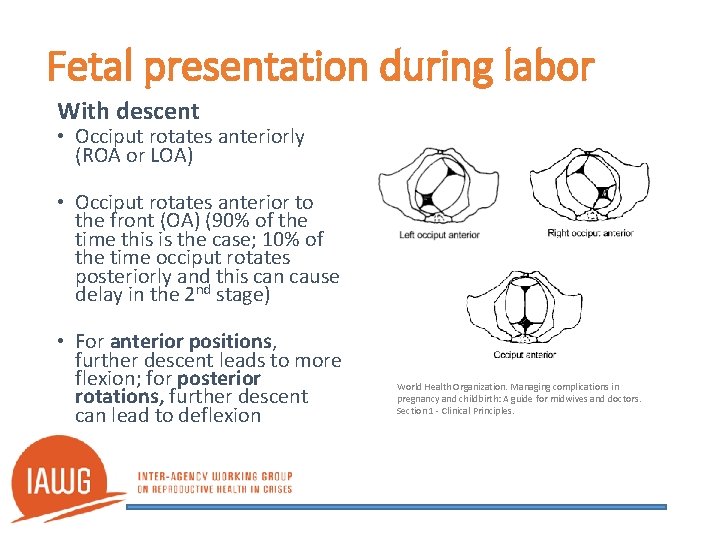
Fetal presentation during labor With descent • Occiput rotates anteriorly (ROA or LOA) • Occiput rotates anterior to the front (OA) (90% of the time this is the case; 10% of the time occiput rotates posteriorly and this can cause delay in the 2 nd stage) • For anterior positions, further descent leads to more flexion; for posterior rotations, further descent can lead to deflexion World Health Organization. Managing complications in pregnancy and childbirth: A guide for midwives and doctors. Section 1 - Clinical Principles.
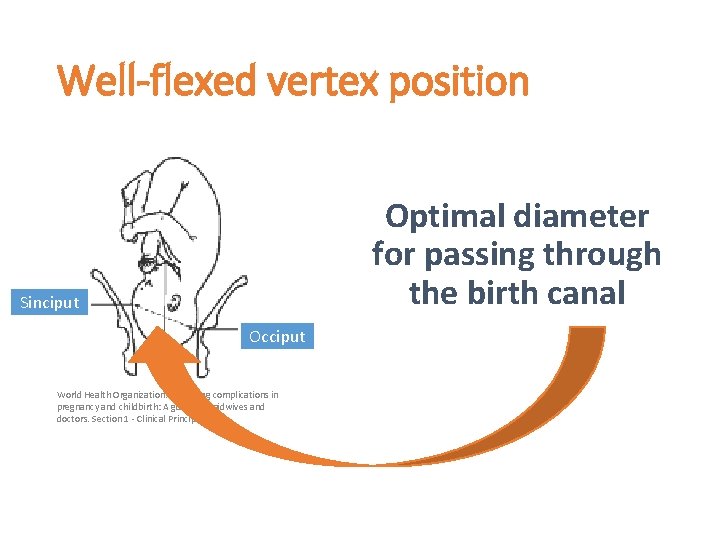
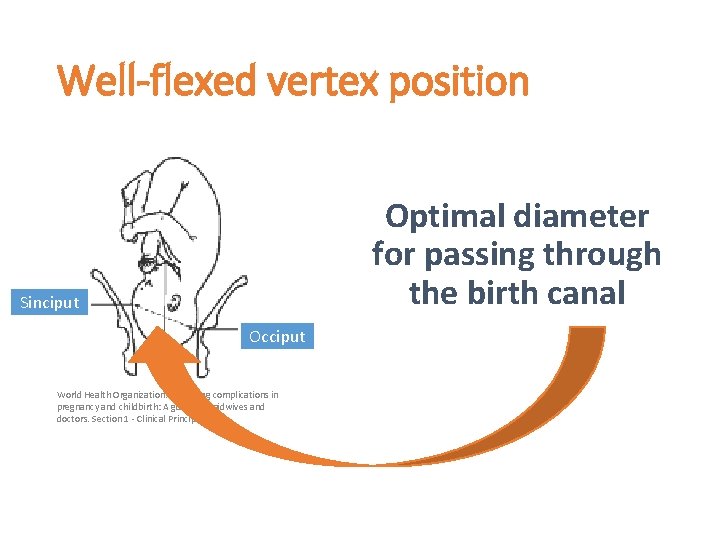
Well-flexed vertex position Optimal diameter for passing through the birth canal Sinciput Occiput World Health Organization. Managing complications in pregnancy and childbirth: A guide for midwives and doctors. Section 1 - Clinical Principles.
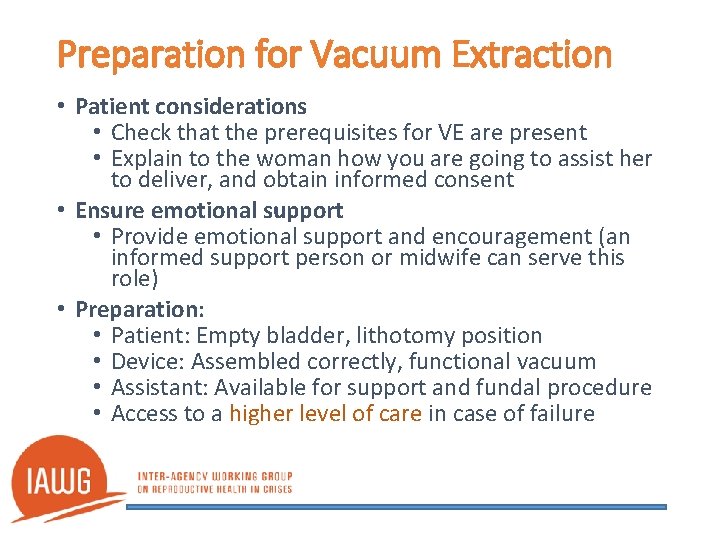
Preparation for Vacuum Extraction • Patient considerations • Check that the prerequisites for VE are present • Explain to the woman how you are going to assist her to deliver, and obtain informed consent • Ensure emotional support • Provide emotional support and encouragement (an informed support person or midwife can serve this role) • Preparation: • Patient: Empty bladder, lithotomy position • Device: Assembled correctly, functional vacuum • Assistant: Available for support and fundal procedure • Access to a higher level of care in case of failure
Pre-requisites for Vacuum Extraction • Gestation >34 weeks, Cephalic presentation • Strong contractions (Frequency = 3 in 10, Duration >45 seconds); strengthen contractions with oxytocin drip if contractions are not adequate • Head is in the pelvis. No more than 1/5 palpable above the brim on bimanual palpation and vaginal station below spine • Fully dilated cervix and empty bladder (drain with a catheter if bladder is not empty)
Procedure Check if the requirements/prequisites are present • Locate the flexion point by palpating the fontanelle(s) of the fetal head • Apply the cup up under the fetal head to the flexion point • Create a vacuum; wait 2 minutes for chignon to form • Apply traction only during a contraction in conjunction with maternal pushing efforts
Flexion point What is it? • Landmark for placement of the center of the vacuum cup • Proper placement of the cup on the flexion point promotes flexion, descent, and autorotation of fetal head during traction
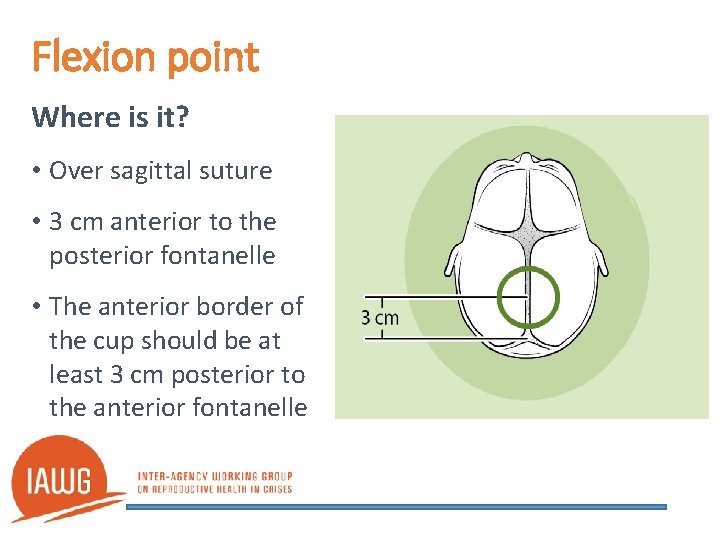
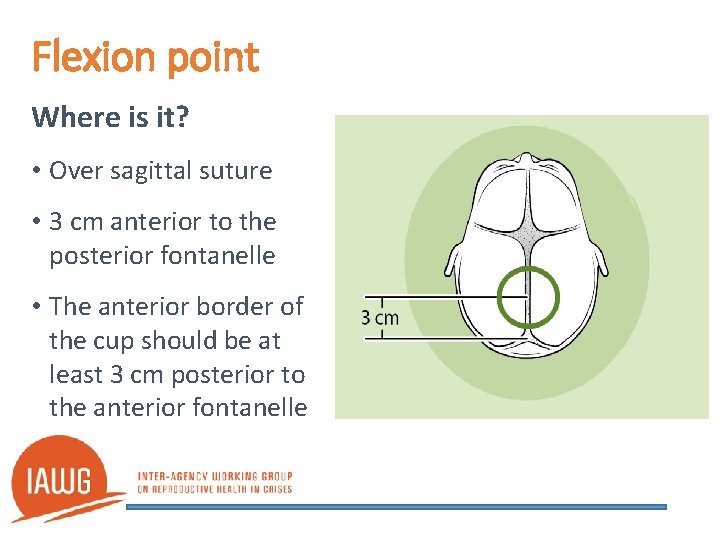
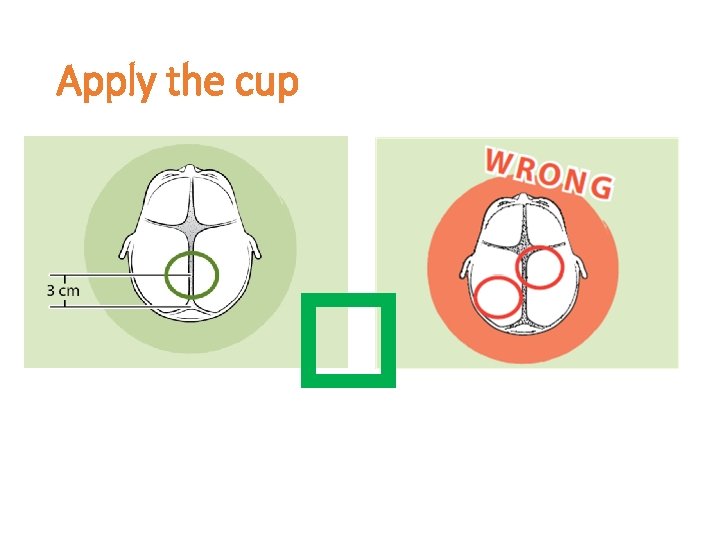
Flexion point Where is it? • Over sagittal suture • 3 cm anterior to the posterior fontanelle • The anterior border of the cup should be at least 3 cm posterior to the anterior fontanelle
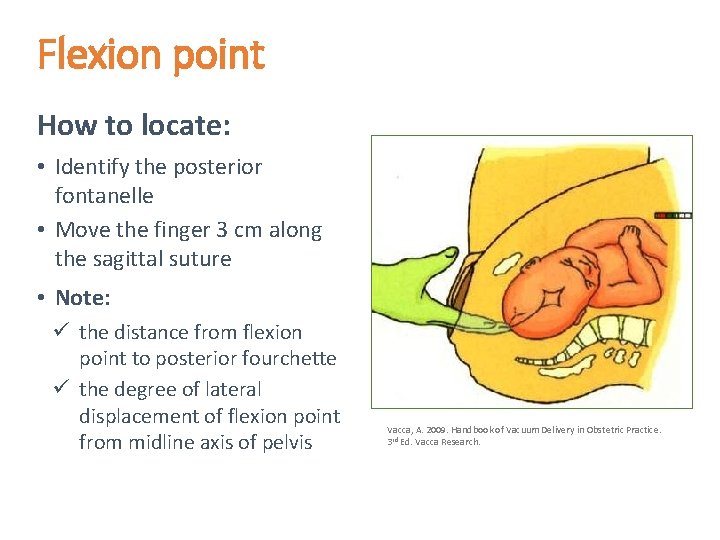
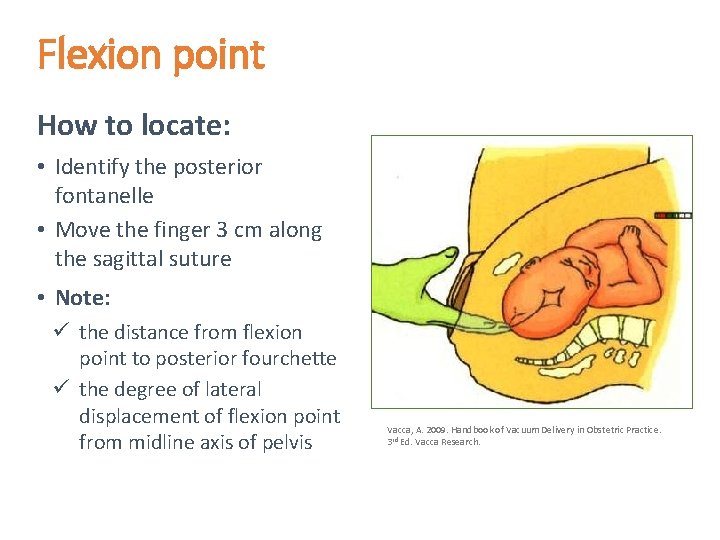
Flexion point How to locate: • Identify the posterior fontanelle • Move the finger 3 cm along the sagittal suture • Note: ü the distance from flexion point to posterior fourchette ü the degree of lateral displacement of flexion point from midline axis of pelvis Vacca, A. 2009. Handbook of Vacuum Delivery in Obstetric Practice. 3 rd Ed. Vacca Research.
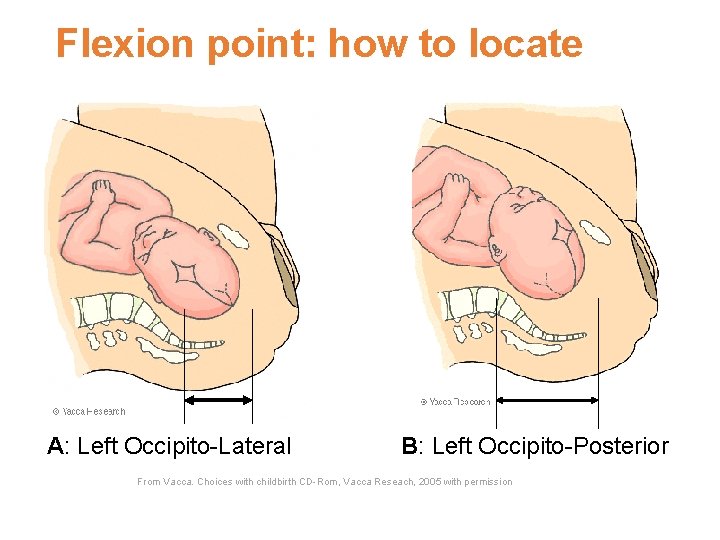
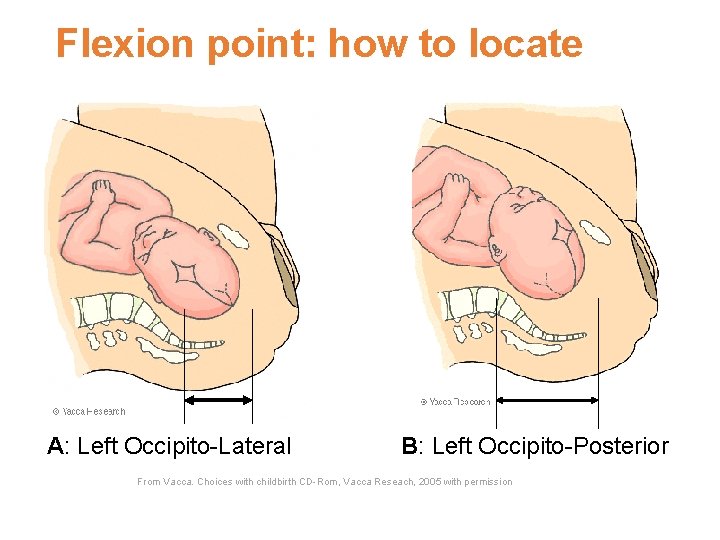
Flexion point: how to locate A: Left Occipito-Lateral B: Left Occipito-Posterior From Vacca. Choices with childbirth CD-Rom, Vacca Reseach, 2005 with permission
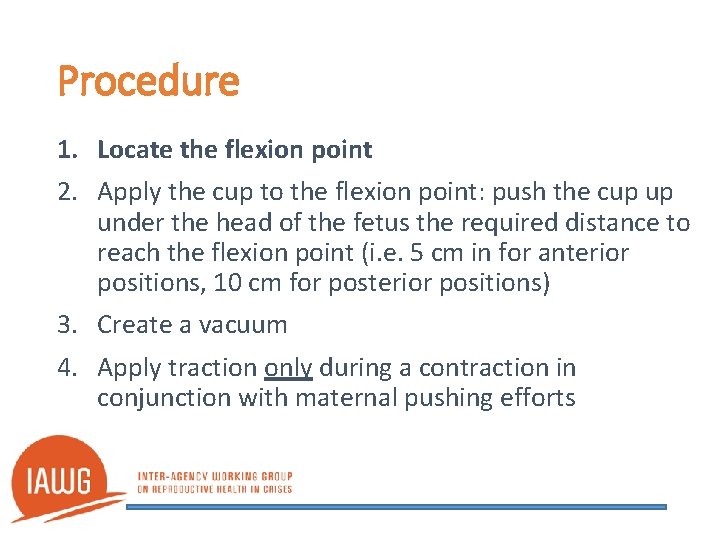
Procedure 1. Locate the flexion point 2. Apply the cup to the flexion point: push the cup up under the head of the fetus the required distance to reach the flexion point (i. e. 5 cm in for anterior positions, 10 cm for posterior positions) 3. Create a vacuum 4. Apply traction only during a contraction in conjunction with maternal pushing efforts
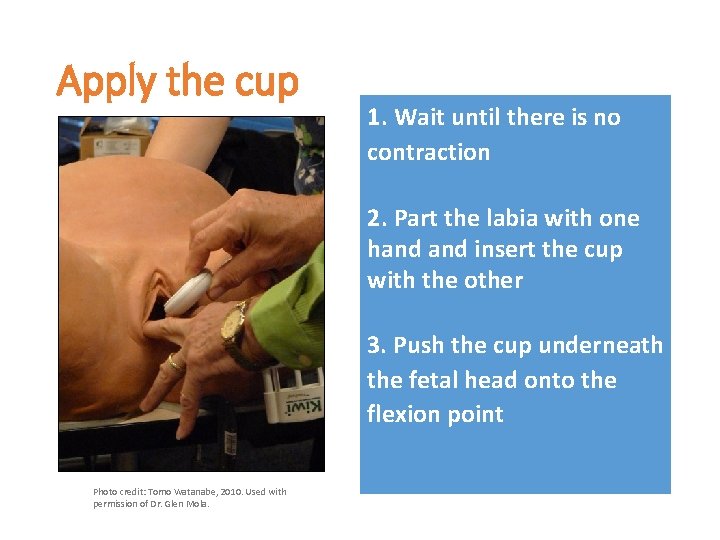
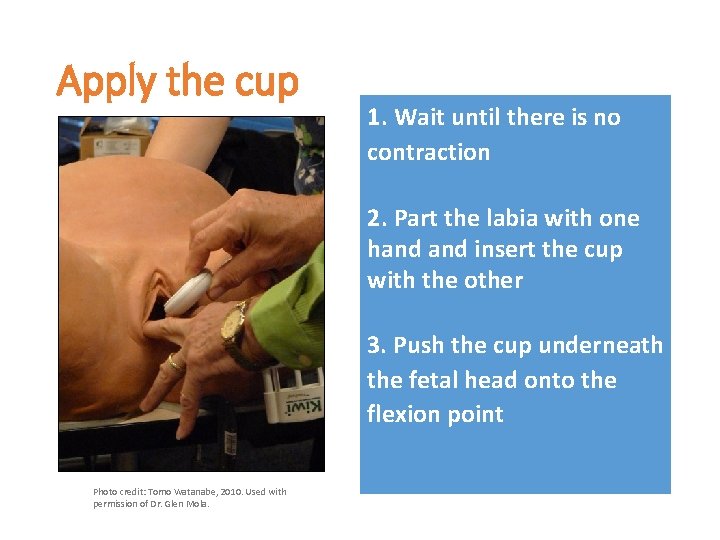
Apply the cup 1. Wait until there is no contraction 2. Part the labia with one hand insert the cup with the other 3. Push the cup underneath the fetal head onto the flexion point Photo credit: Tomo Watanabe, 2010. Used with permission of Dr. Glen Mola.
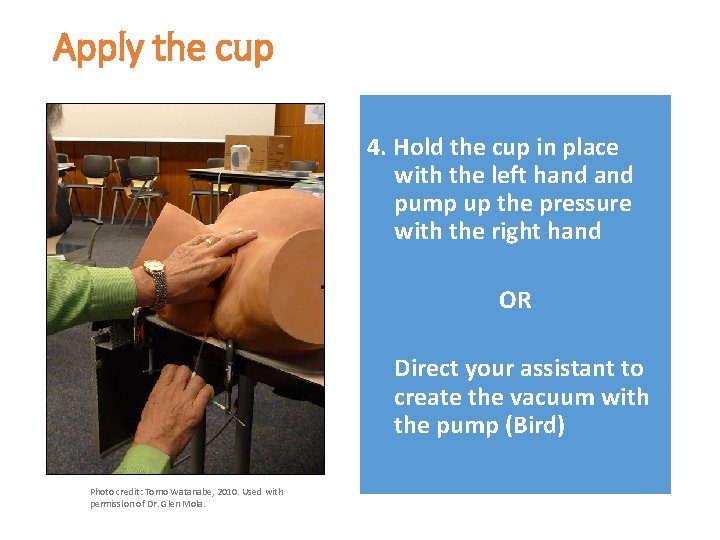
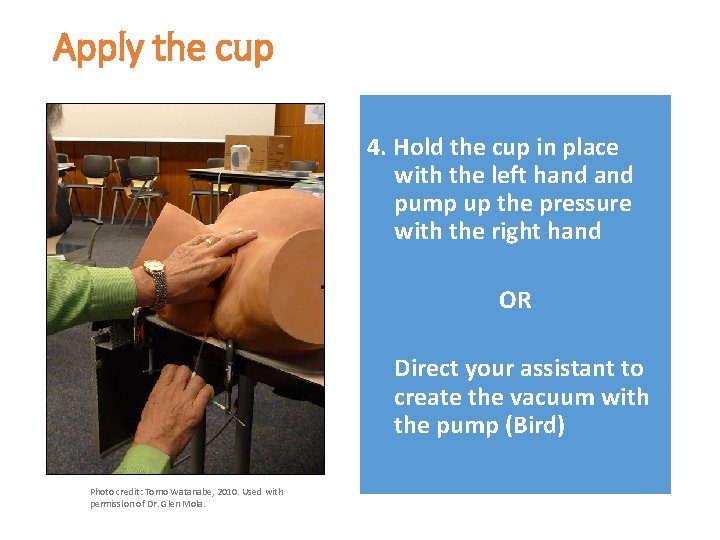
Apply the cup 4. Hold the cup in place with the left hand pump up the pressure with the right hand OR Direct your assistant to create the vacuum with the pump (Bird) Photo credit: Tomo Watanabe, 2010. Used with permission of Dr. Glen Mola.
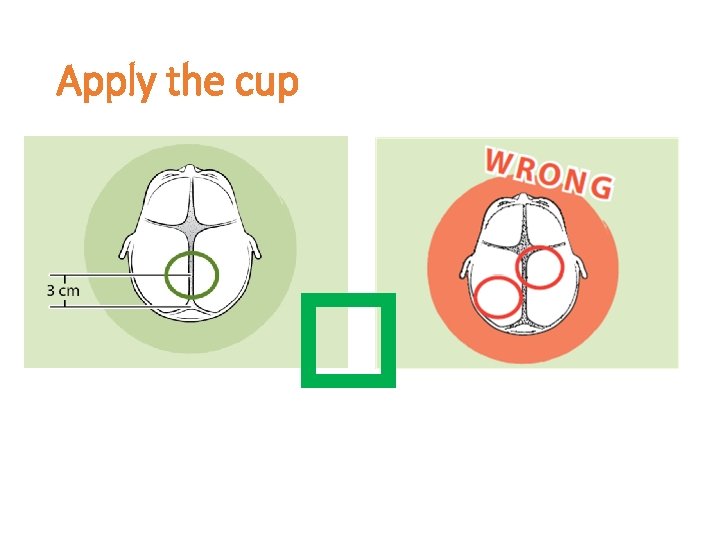
Apply the cup �
Procedure 1. Locate the flexion point 2. Apply the cup to the flexion point 3. Create a vacuum and wait 2 minutes for the chignon to form inside the cup 4. Apply traction only during a contraction in conjunction with maternal pushing efforts
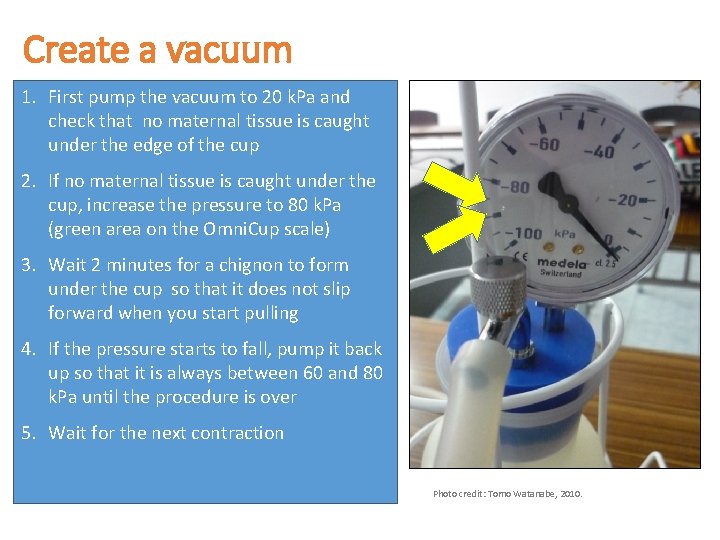
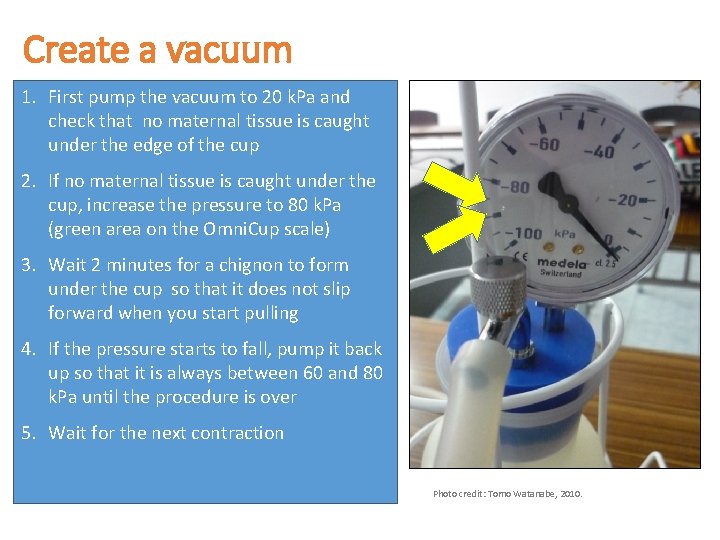
Create a vacuum 1. First pump the vacuum to 20 k. Pa and check that no maternal tissue is caught under the edge of the cup 2. If no maternal tissue is caught under the cup, increase the pressure to 80 k. Pa (green area on the Omni. Cup scale) 3. Wait 2 minutes for a chignon to form under the cup so that it does not slip forward when you start pulling 4. If the pressure starts to fall, pump it back up so that it is always between 60 and 80 k. Pa until the procedure is over 5. Wait for the next contraction Photo credit: Tomo Watanabe, 2010.
Procedure 1. Locate the flexion point 2. Apply the cup to the flexion point 3. Create a vacuum and wait 2 minutes for the chignon to form inside the cup 4. Apply traction only during a contraction in conjunction with maternal pushing efforts
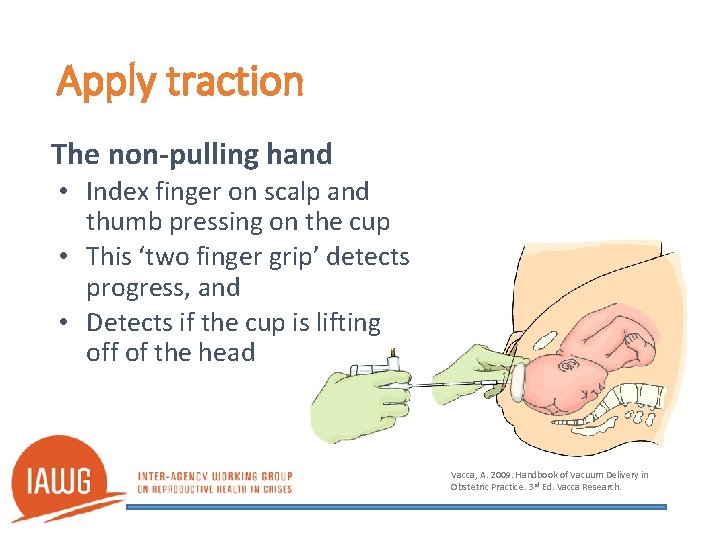
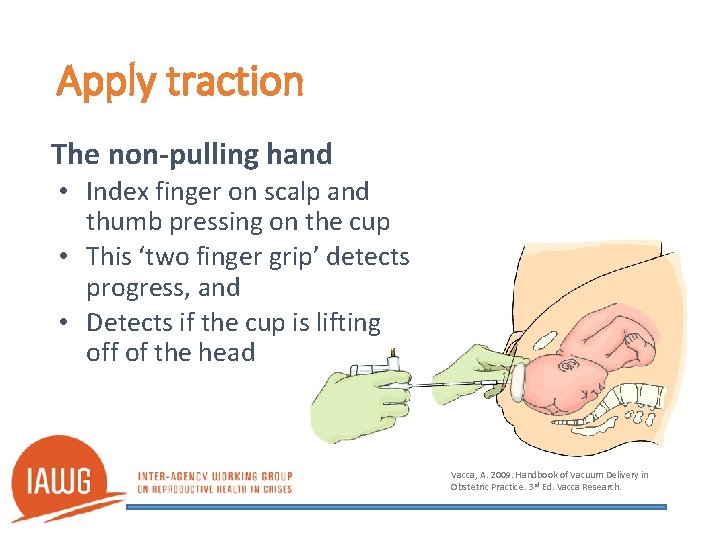
Apply traction The non-pulling hand • Index finger on scalp and thumb pressing on the cup • This ‘two finger grip’ detects progress, and • Detects if the cup is lifting off of the head Vacca, A. 2009. Handbook of Vacuum Delivery in Obstetric Practice. 3 rd Ed. Vacca Research.
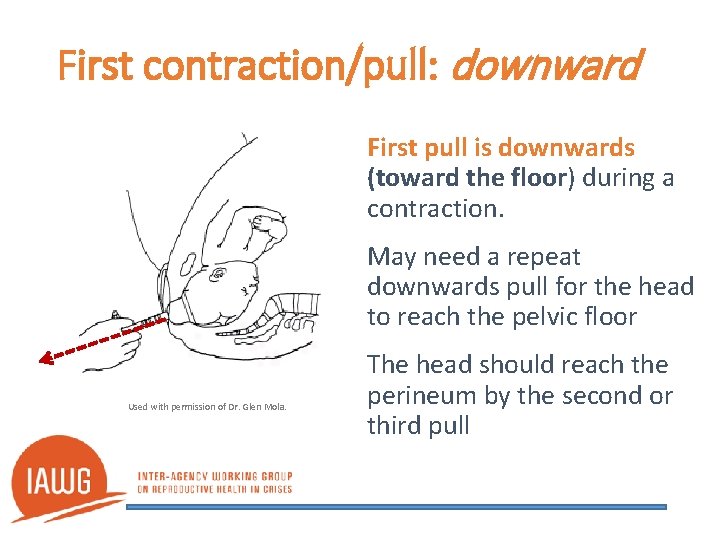
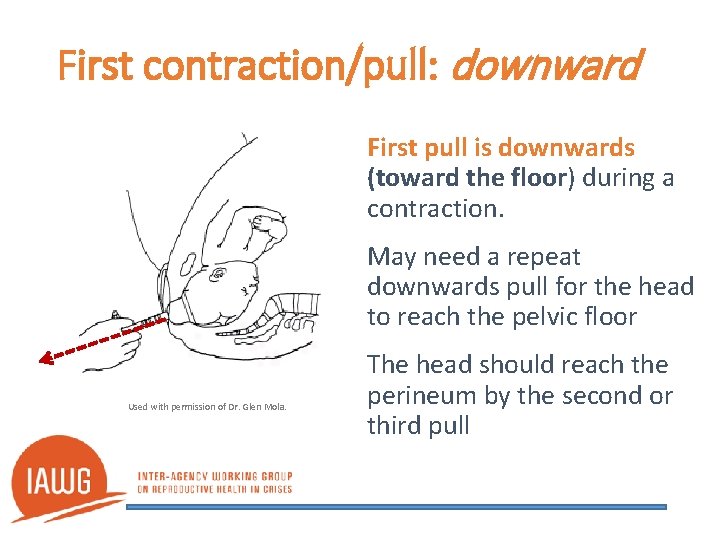
First contraction/pull: downward First pull is downwards (toward the floor) during a contraction. May need a repeat downwards pull for the head to reach the pelvic floor Used with permission of Dr. Glen Mola. The head should reach the perineum by the second or third pull
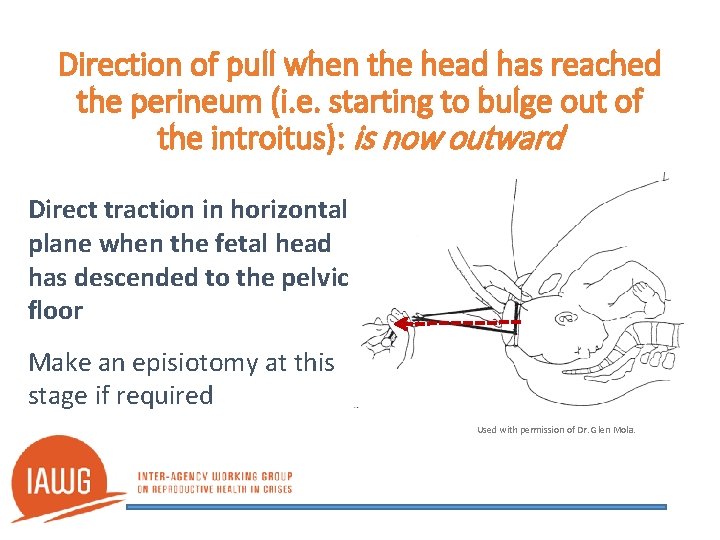
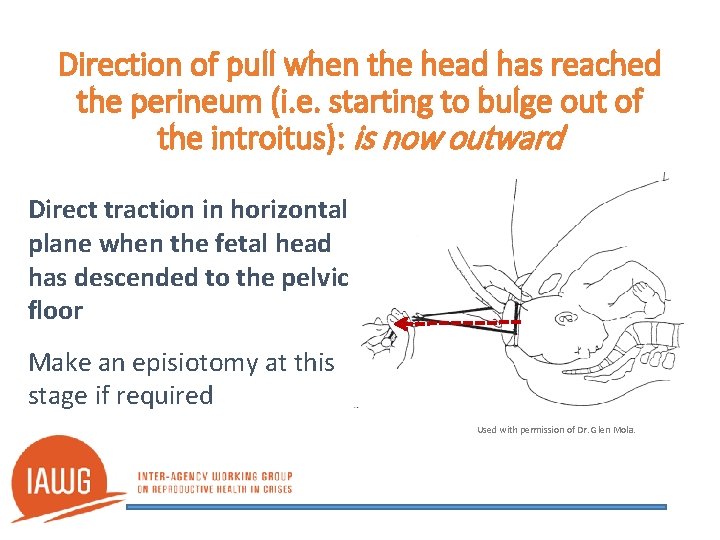
Direction of pull when the head has reached the perineum (i. e. starting to bulge out of the introitus): is now outward Direct traction in horizontal plane when the fetal head has descended to the pelvic floor Make an episiotomy at this stage if required Used with permission of Dr. Glen Mola.
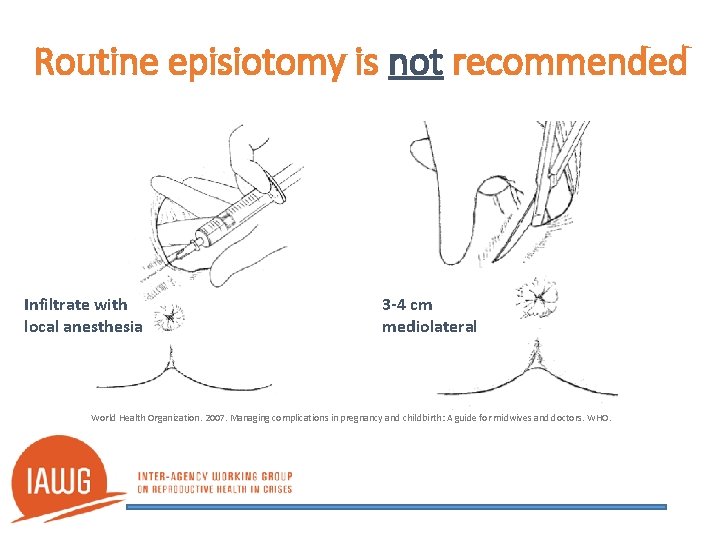
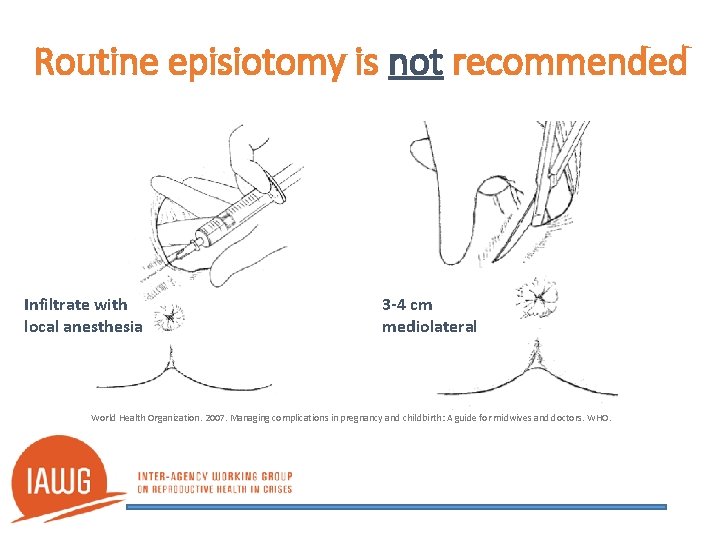
Routine episiotomy is not recommended Infiltrate with local anesthesia 3 -4 cm mediolateral World Health Organization. 2007. Managing complications in pregnancy and childbirth: A guide for midwives and doctors. WHO.
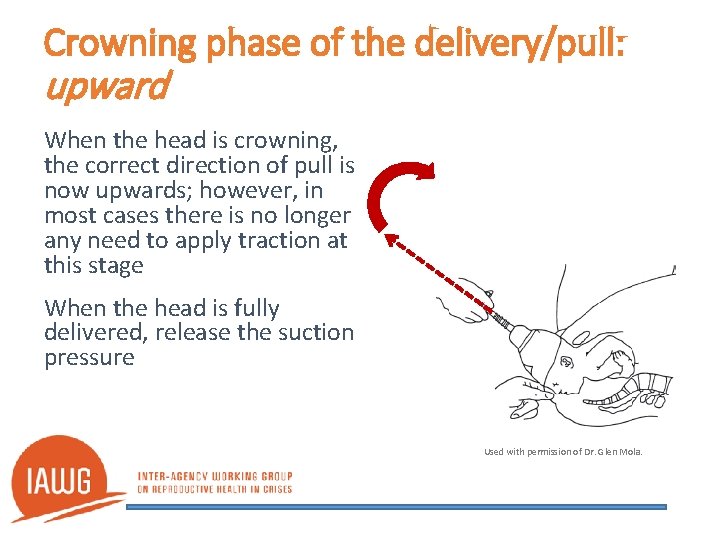
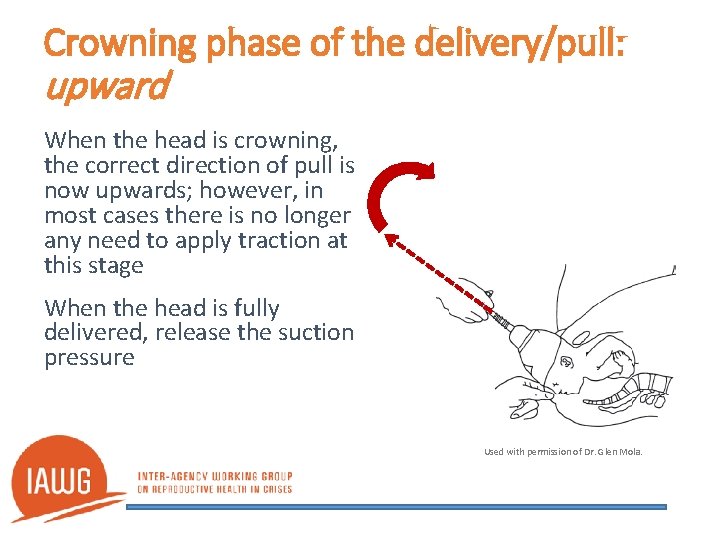
Crowning phase of the delivery/pull: upward When the head is crowning, the correct direction of pull is now upwards; however, in most cases there is no longer any need to apply traction at this stage When the head is fully delivered, release the suction pressure Used with permission of Dr. Glen Mola.
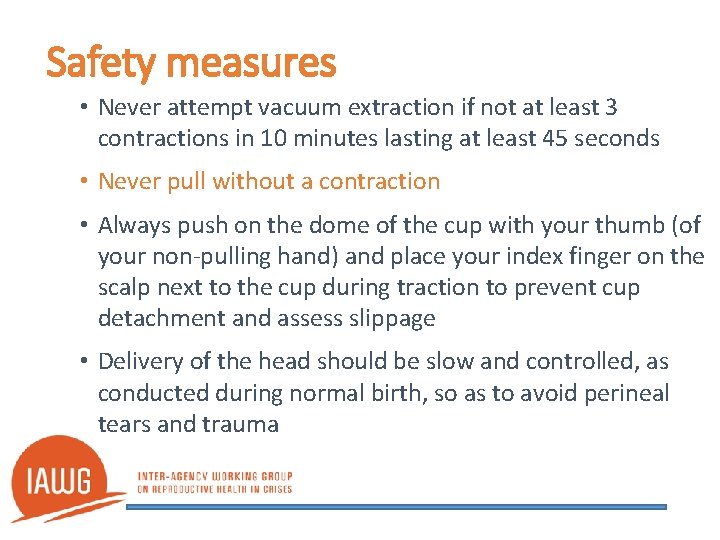
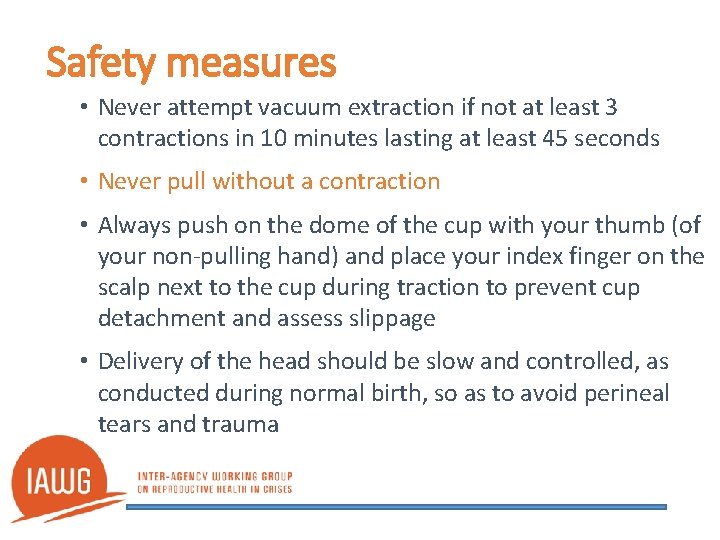
Safety measures • Never attempt vacuum extraction if not at least 3 contractions in 10 minutes lasting at least 45 seconds • Never pull without a contraction • Always push on the dome of the cup with your thumb (of your non-pulling hand) and place your index finger on the scalp next to the cup during traction to prevent cup detachment and assess slippage • Delivery of the head should be slow and controlled, as conducted during normal birth, so as to avoid perineal tears and trauma
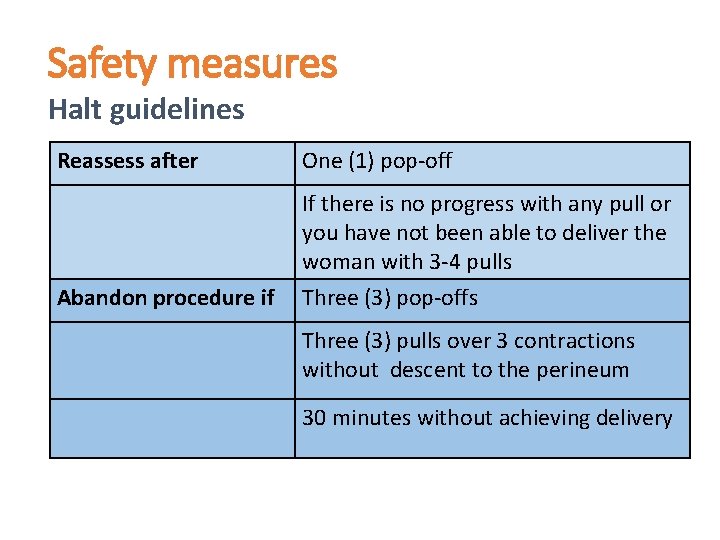
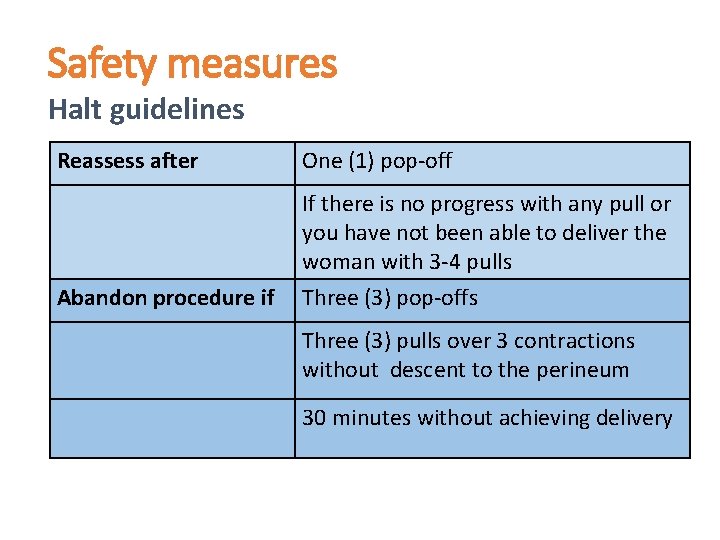
Safety measures Halt guidelines Reassess after One (1) pop-off Abandon procedure if If there is no progress with any pull or you have not been able to deliver the woman with 3 -4 pulls Three (3) pop-offs Three (3) pulls over 3 contractions without descent to the perineum 30 minutes without achieving delivery
Safety measures if procedure has failed Stop the procedure: • Turn off the oxytocin and put up IV of normal saline • Roll the mother onto her left side • Analgesia • Prepare to perform symphysiotomy* or refer urgently for cesarean *Perform symphysiotomy, depending on clinical skills
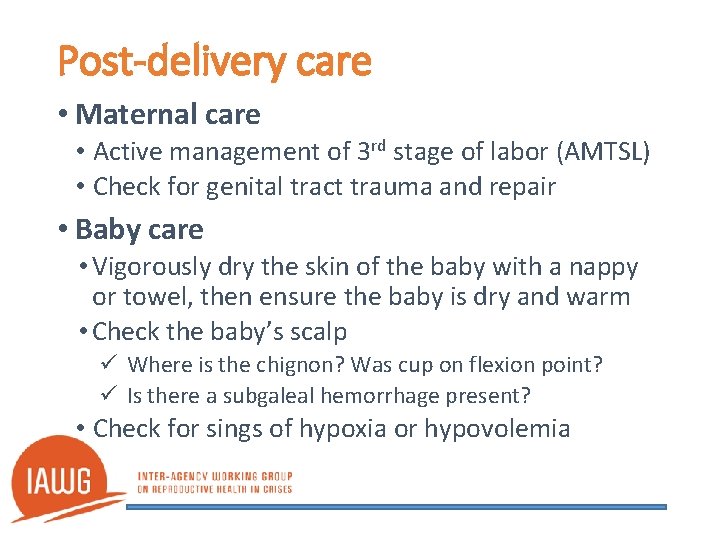
Post-delivery care • Maternal care • Active management of 3 rd stage of labor (AMTSL) • Check for genital tract trauma and repair • Baby care • Vigorously dry the skin of the baby with a nappy or towel, then ensure the baby is dry and warm • Check the baby’s scalp ü Where is the chignon? Was cup on flexion point? ü Is there a subgaleal hemorrhage present? • Check for sings of hypoxia or hypovolemia
Complications • Usually result from: Ø Not observing the conditions of cup application Ø Continuing traction beyond the halt guidelines • Maternal Ø Tears to the cervix and vagina • Fetal Ø Innocuous scalp markings Ø subgaleal hemorrhage > 30 m. Ls in size needs urgent resuscitation with normal saline drip (IV or intraosseous)
Safety measures after delivery • Be ready to prevent/manage PPH: • Risk factors: long second stage, big baby, febrile? • Consider AMTSL and extra measures: • Fundal massage for longer • Consider IV oxytocin infusion for 2 -4 hours • Keep the bladder empty • Consider insertion of misoprostol 3 tablets into the maternal rectum
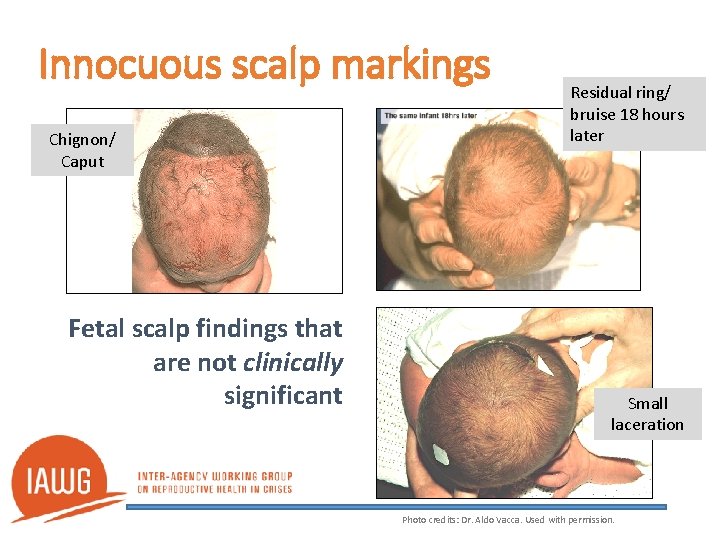
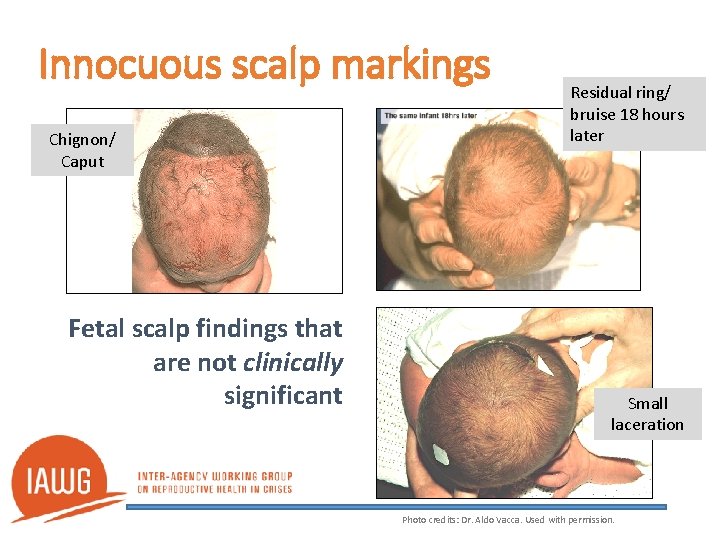
Innocuous scalp markings Chignon/ Caput Fetal scalp findings that are not clinically significant Residual ring/ bruise 18 hours later Small laceration Photo credits: Dr. Aldo Vacca. Used with permission.
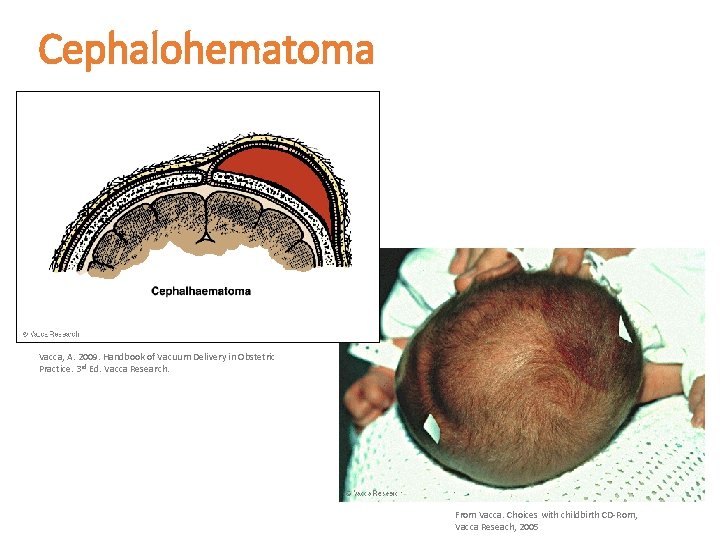
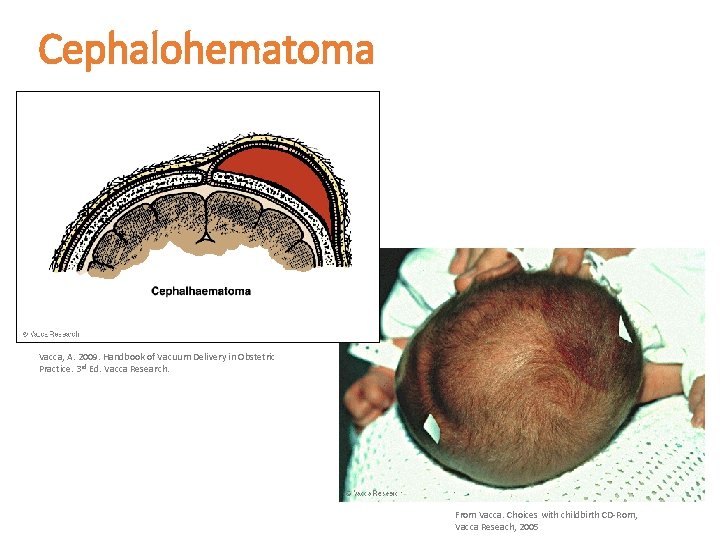
Cephalohematoma Vacca, A. 2009. Handbook of Vacuum Delivery in Obstetric Practice. 3 rd Ed. Vacca Research. From Vacca. Choices with childbirth CD-Rom, Vacca Reseach, 2005
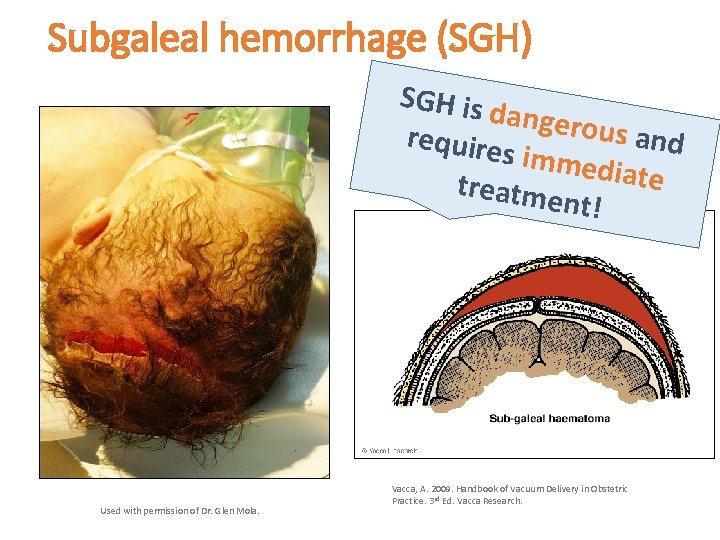
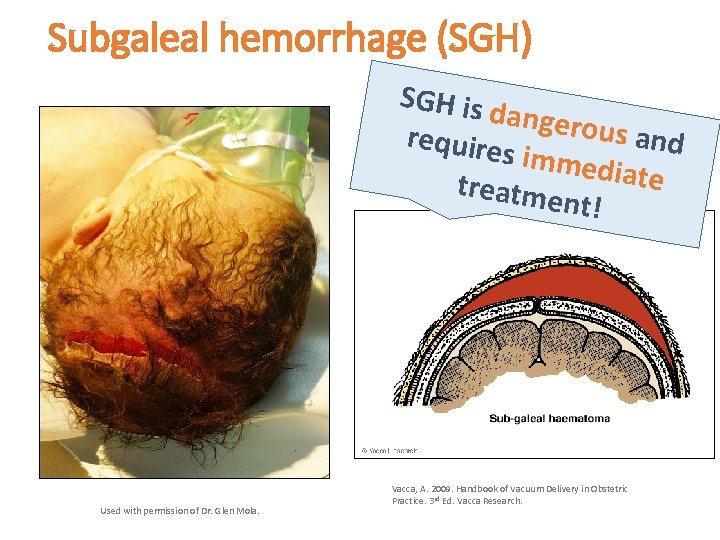
Subgaleal hemorrhage (SGH) SGH is d angerou s and require s imme d iate treatme nt! Used with permission of Dr. Glen Mola. Vacca, A. 2009. Handbook of Vacuum Delivery in Obstetric Practice. 3 rd Ed. Vacca Research.
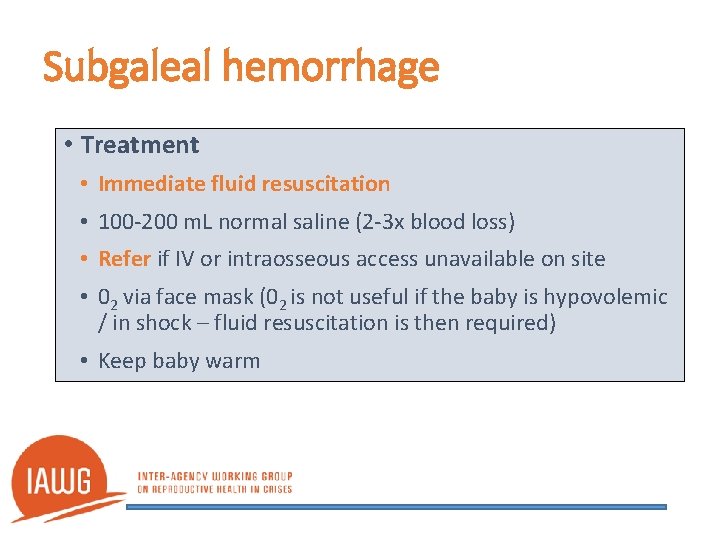
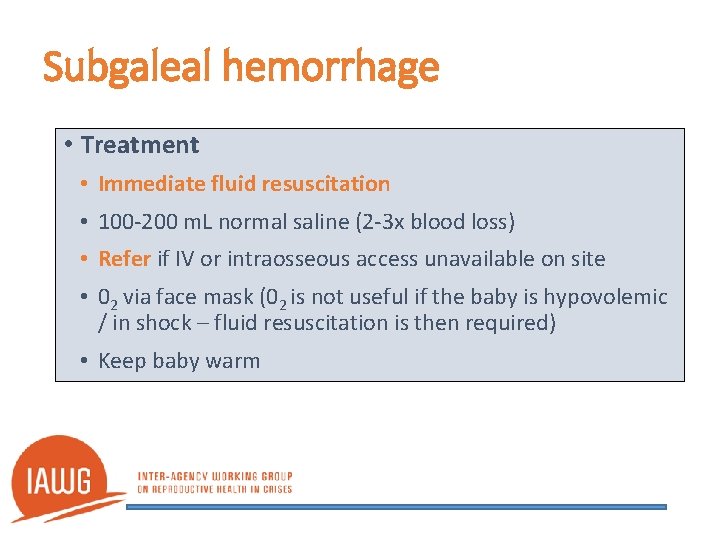
Subgaleal hemorrhage • Treatment • Immediate fluid resuscitation • 100 -200 m. L normal saline (2 -3 x blood loss) • Refer if IV or intraosseous access unavailable on site • 02 via face mask (02 is not useful if the baby is hypovolemic / in shock – fluid resuscitation is then required) • Keep baby warm
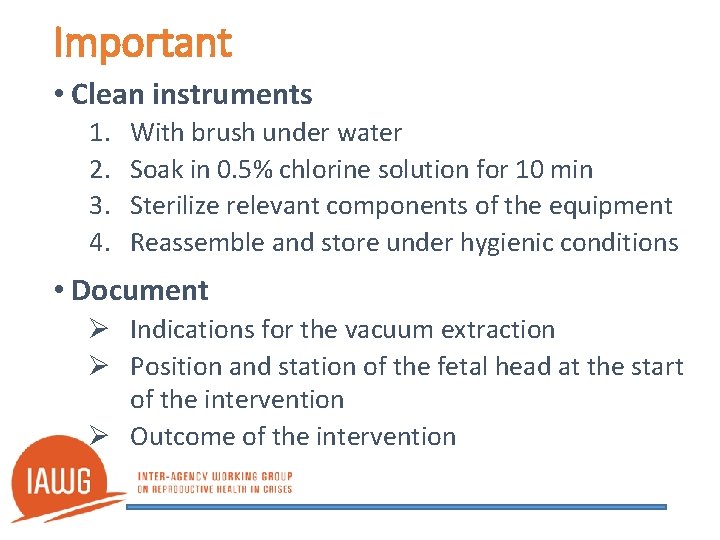
Important • Clean instruments 1. 2. 3. 4. With brush under water Soak in 0. 5% chlorine solution for 10 min Sterilize relevant components of the equipment Reassemble and store under hygienic conditions • Document Ø Indications for the vacuum extraction Ø Position and station of the fetal head at the start of the intervention Ø Outcome of the intervention
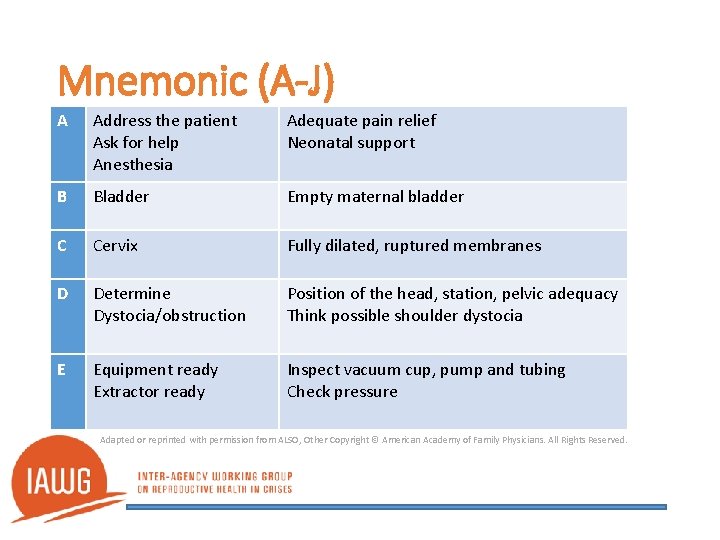
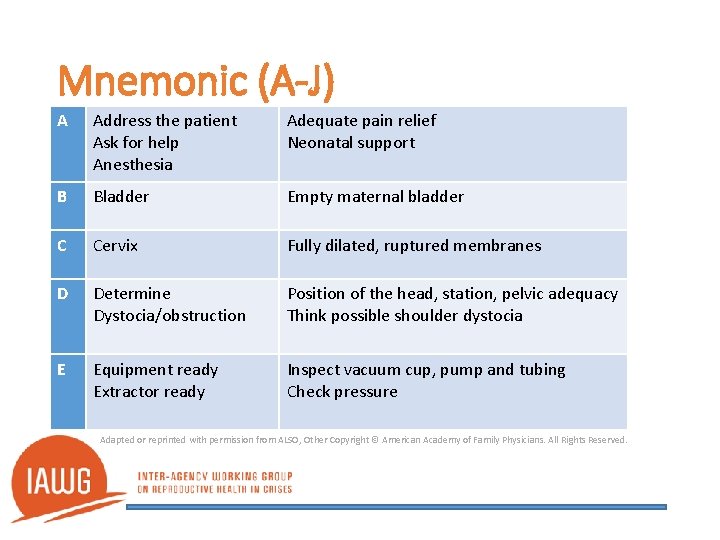
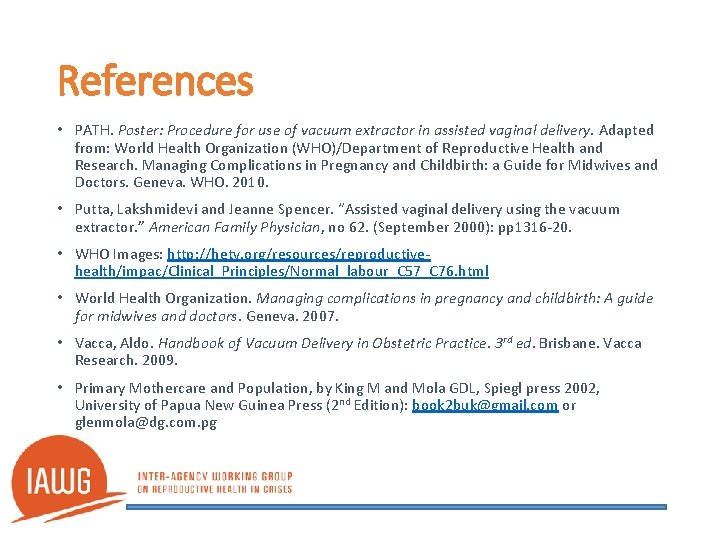
Mnemonic (A-J) A Address the patient Ask for help Anesthesia Adequate pain relief Neonatal support B Bladder Empty maternal bladder C Cervix Fully dilated, ruptured membranes D Determine Dystocia/obstruction Position of the head, station, pelvic adequacy Think possible shoulder dystocia E Equipment ready Extractor ready Inspect vacuum cup, pump and tubing Check pressure Adapted or reprinted with permission from ALSO, Other Copyright © American Academy of Family Physicians. All Rights Reserved.
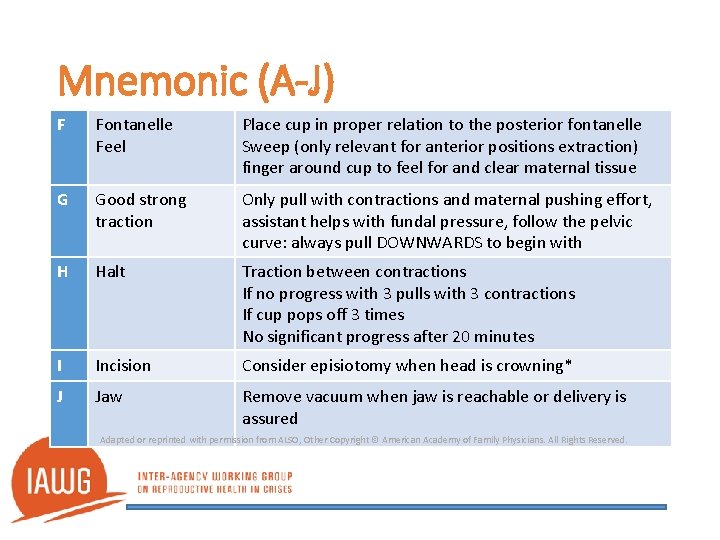
Mnemonic (A-J) F Fontanelle Feel Place cup in proper relation to the posterior fontanelle Sweep (only relevant for anterior positions extraction) finger around cup to feel for and clear maternal tissue G Good strong traction Only pull with contractions and maternal pushing effort, assistant helps with fundal pressure, follow the pelvic curve: always pull DOWNWARDS to begin with H Halt Traction between contractions If no progress with 3 pulls with 3 contractions If cup pops off 3 times No significant progress after 20 minutes I Incision Consider episiotomy when head is crowning* J Jaw Remove vacuum when jaw is reachable or delivery is assured Adapted or reprinted with permission from ALSO, Other Copyright © American Academy of Family Physicians. All Rights Reserved.
References • PATH. Poster: Procedure for use of vacuum extractor in assisted vaginal delivery. Adapted from: World Health Organization (WHO)/Department of Reproductive Health and Research. Managing Complications in Pregnancy and Childbirth: a Guide for Midwives and Doctors. Geneva. WHO. 2010. • Putta, Lakshmidevi and Jeanne Spencer. “Assisted vaginal delivery using the vacuum extractor. ” American Family Physician, no 62. (September 2000): pp 1316 -20. • WHO Images: http: //hetv. org/resources/reproductivehealth/impac/Clinical_Principles/Normal_labour_C 57_C 76. html • World Health Organization. Managing complications in pregnancy and childbirth: A guide for midwives and doctors. Geneva. 2007. • Vacca, Aldo. Handbook of Vacuum Delivery in Obstetric Practice. 3 rd ed. Brisbane. Vacca Research. 2009. • Primary Mothercare and Population, by King M and Mola GDL, Spiegl press 2002, University of Papua New Guinea Press (2 nd Edition): book 2 buk@gmail. com or glenmola@dg. com. pg