FORCEPS DELIVERY AND VACUUM EXTRACTION Prof S P


- Slides: 113
FORCEPS DELIVERY AND VACUUM EXTRACTION Prof. S. P. Jaiswar Department of Obst. & Gynae. K. G. Medical University, Lucknow
INTRODUCTION • Forceps delivery is an operative delivery conducted with the help of obstetric forceps • Obstetrics forceps is a pair of instruments specially designed to assist extraction of fetal head and thereby accomplishing delivery of the fetus.
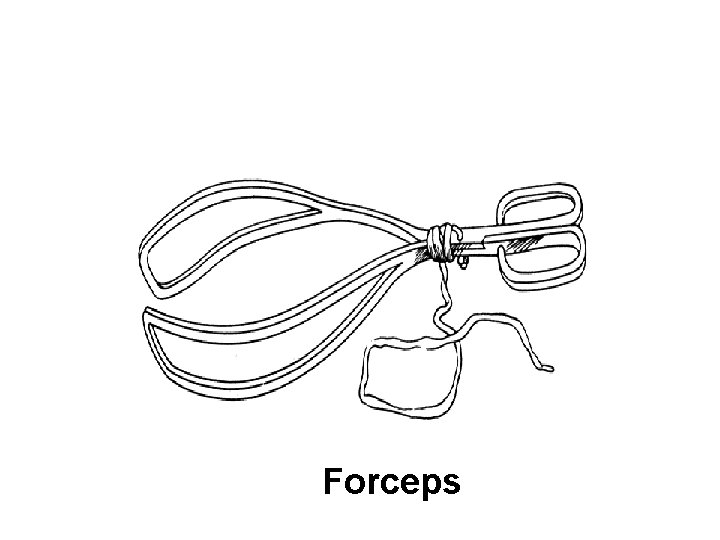
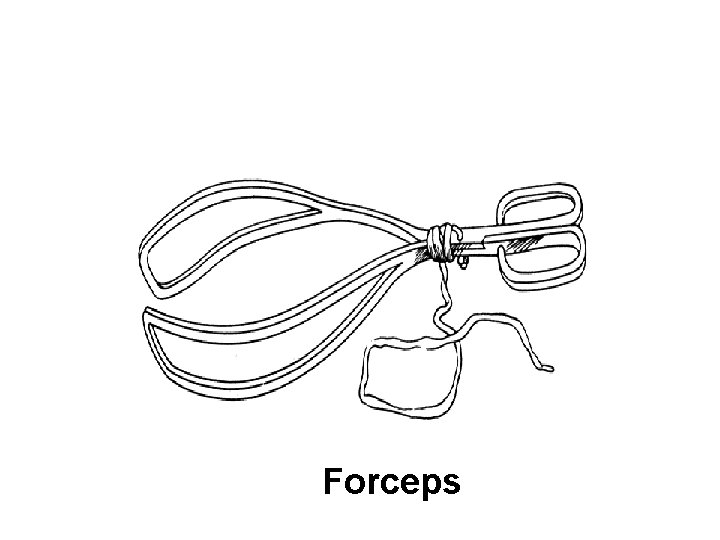
Forceps
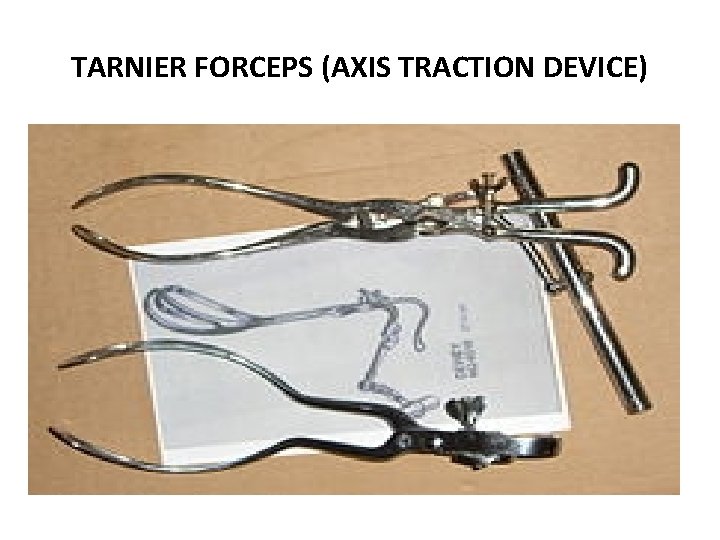
HISTORY OF FORCEPS • The credit for design and early use of forceps goes to Chamberlen of England. • The credit for using pelvic curve – Levert (1747) • Smellie gave us the English lock • Tarnier -axis traction device.
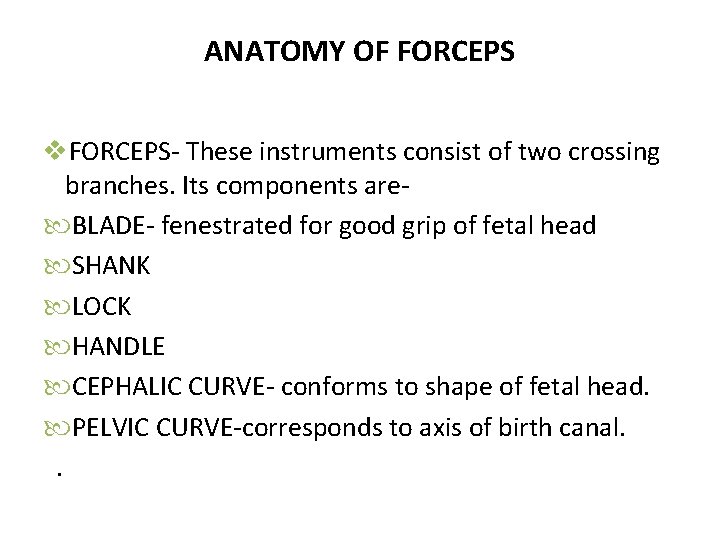
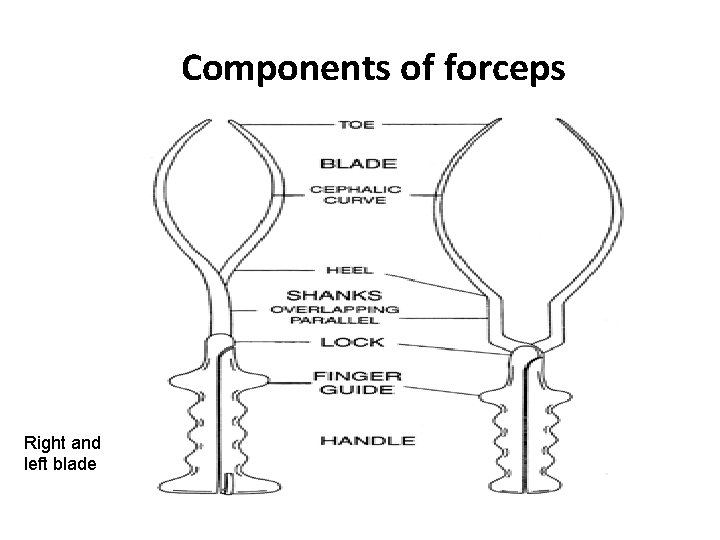
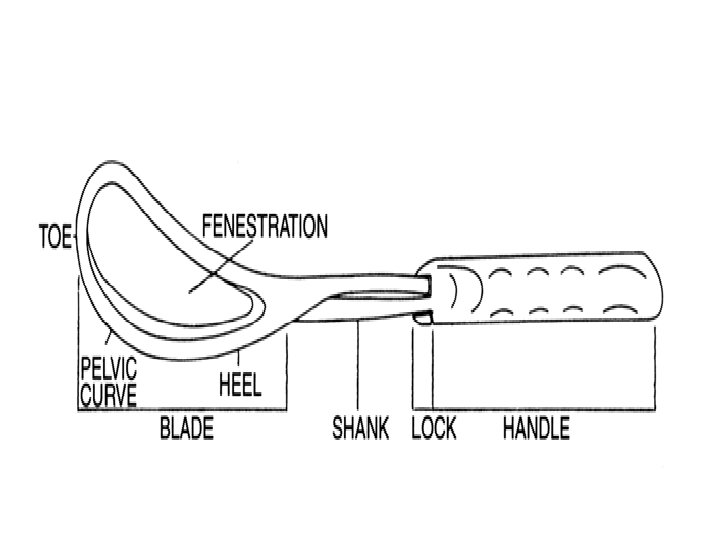
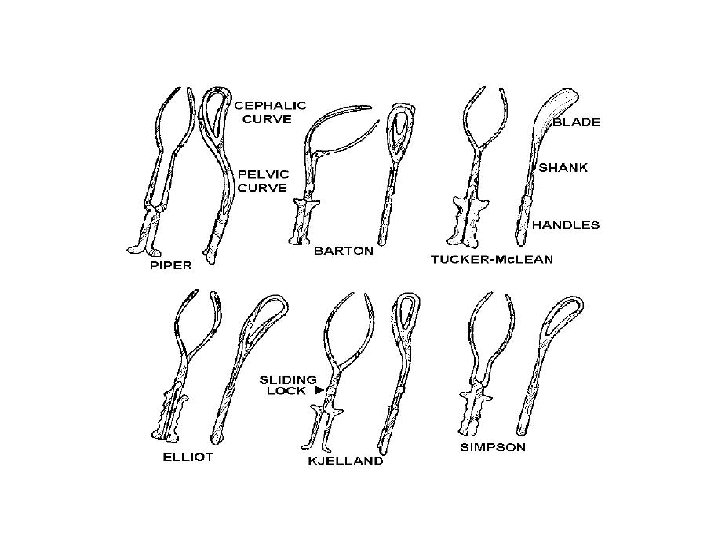
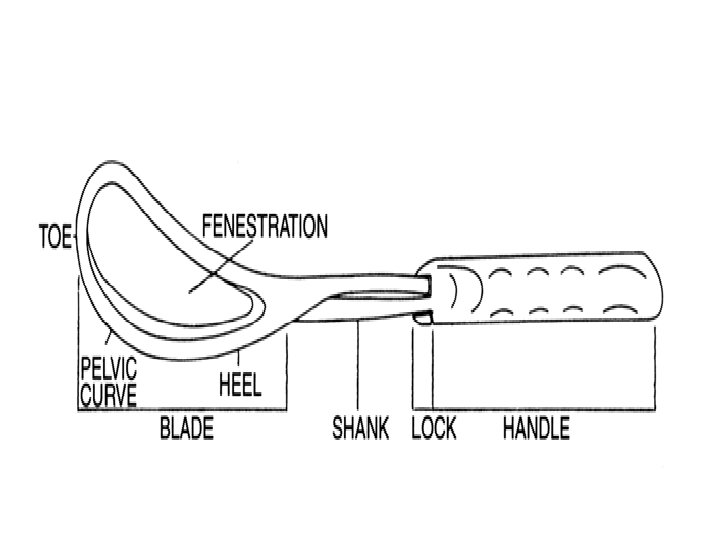
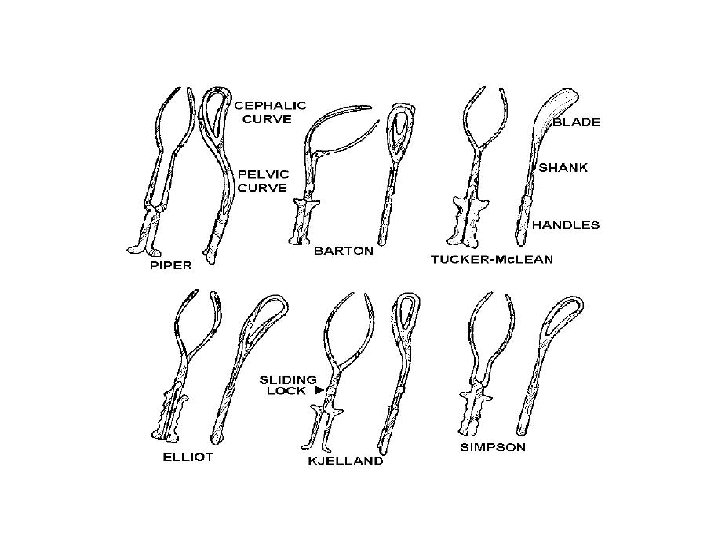
ANATOMY OF FORCEPS v. FORCEPS- These instruments consist of two crossing branches. Its components are BLADE- fenestrated for good grip of fetal head SHANK LOCK HANDLE CEPHALIC CURVE- conforms to shape of fetal head. PELVIC CURVE-corresponds to axis of birth canal. .
ANATOMY OF FORCEPS contd. . • A sliding lock is used in Kielland forceps. • Total length of long obstetric forceps is 37 cm. • The distance between two tips - 2. 5 cm (when locked). • The widest diameter between blade is 9 cm.
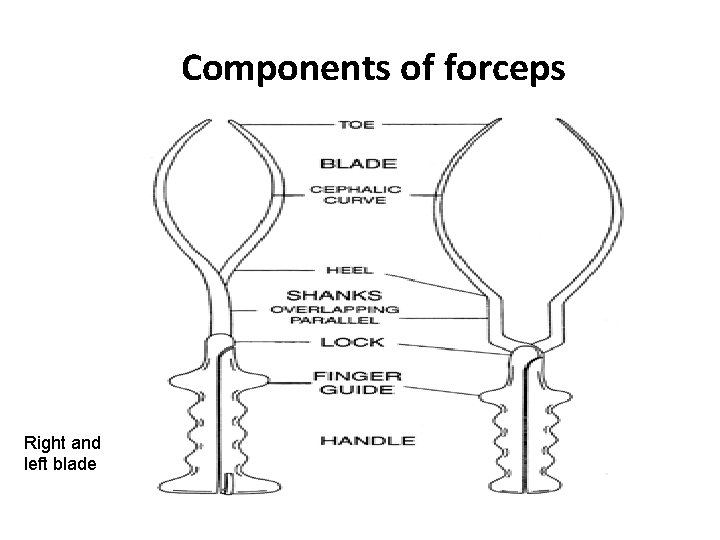
Components of forceps Right and left blade
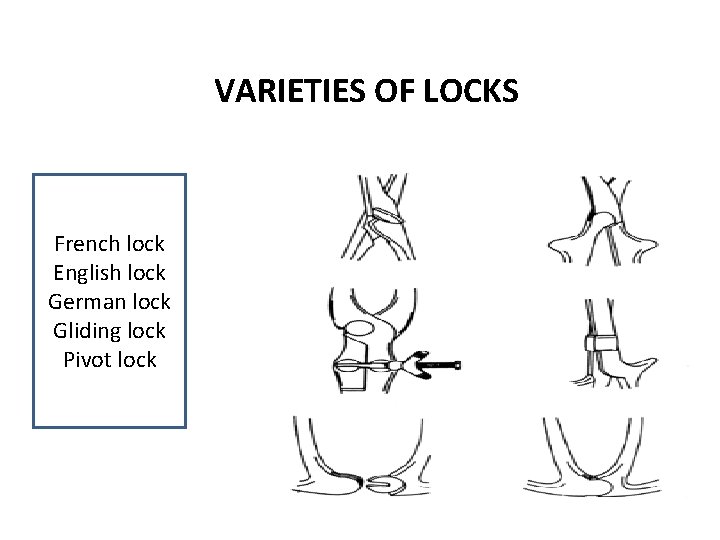
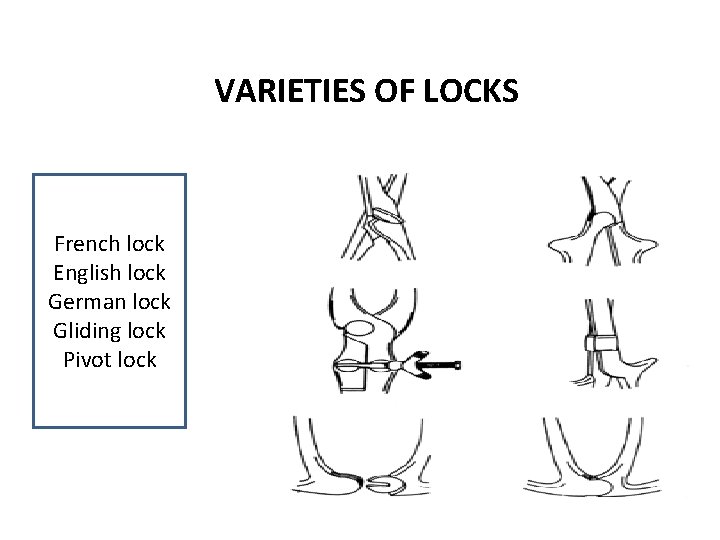
VARIETIES OF LOCKS French lock English lock German lock Gliding lock Pivot lock
VARIETIES OF OBSTETRIC FORCEPS • CONVENTIONAL TRACTION FORCEPS • SHORT FORCEPSWrigleys, Short Simpson • LONG FORCEPS-Das Simpson • LONG FORCEPS with AXIS TRACTIONMilne Murray, Haig Fergusen, Nevelles Barnes
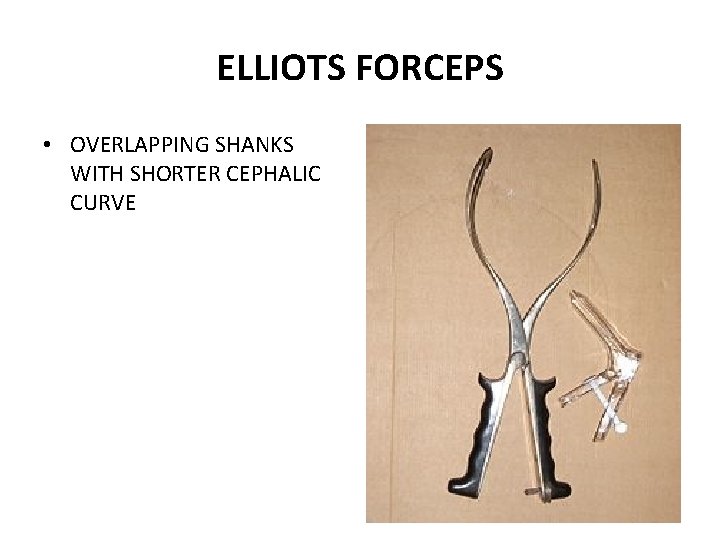
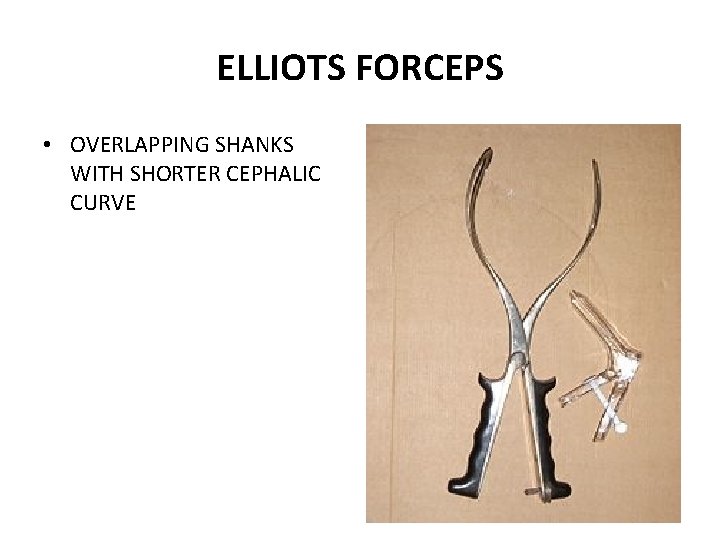
ELLIOTS FORCEPS • OVERLAPPING SHANKS WITH SHORTER CEPHALIC CURVE
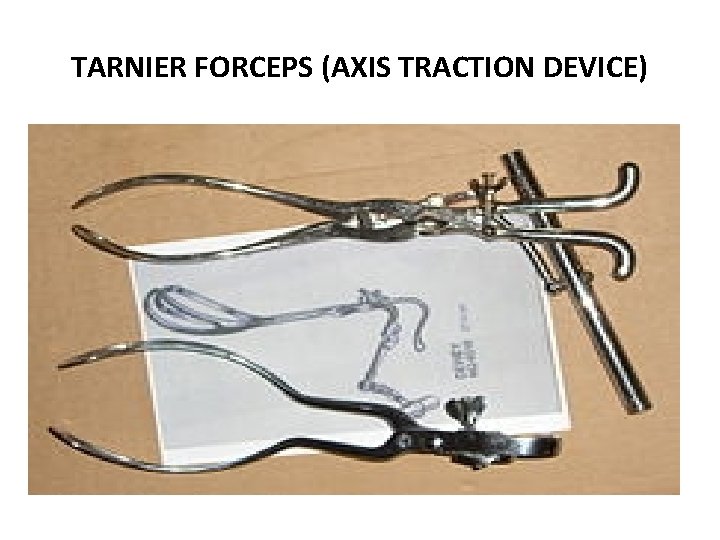
TARNIER FORCEPS (AXIS TRACTION DEVICE)
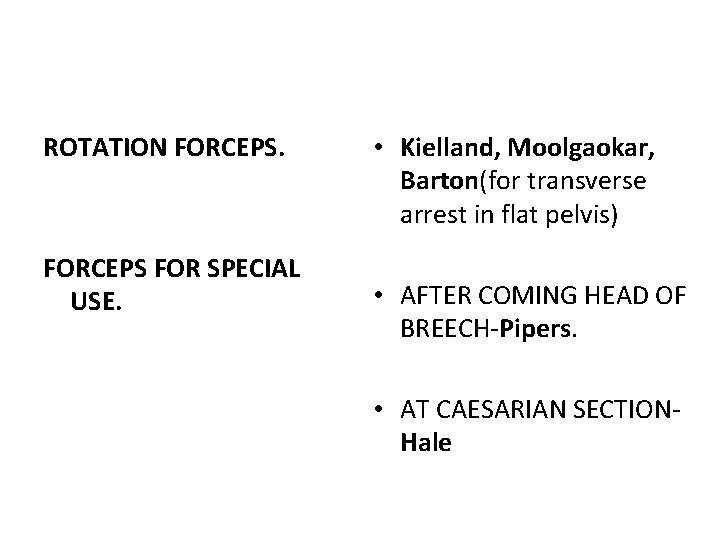
ROTATION FORCEPS FOR SPECIAL USE. • Kielland, Moolgaokar, Barton(for transverse arrest in flat pelvis) • AFTER COMING HEAD OF BREECH-Pipers. • AT CAESARIAN SECTIONHale
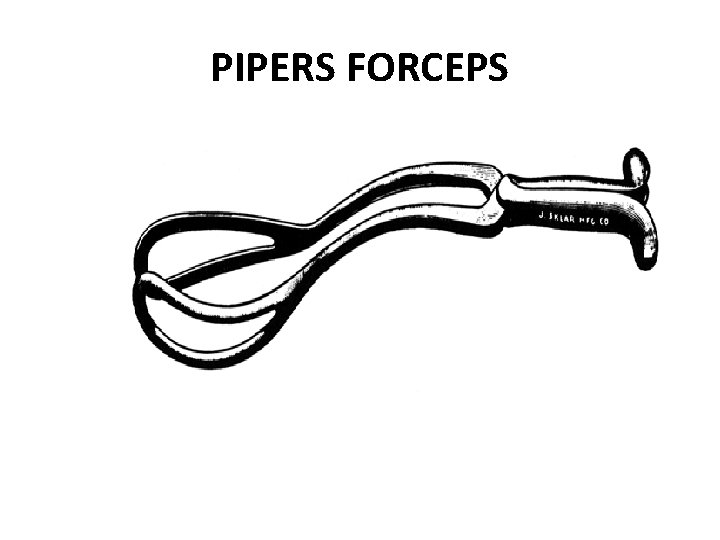
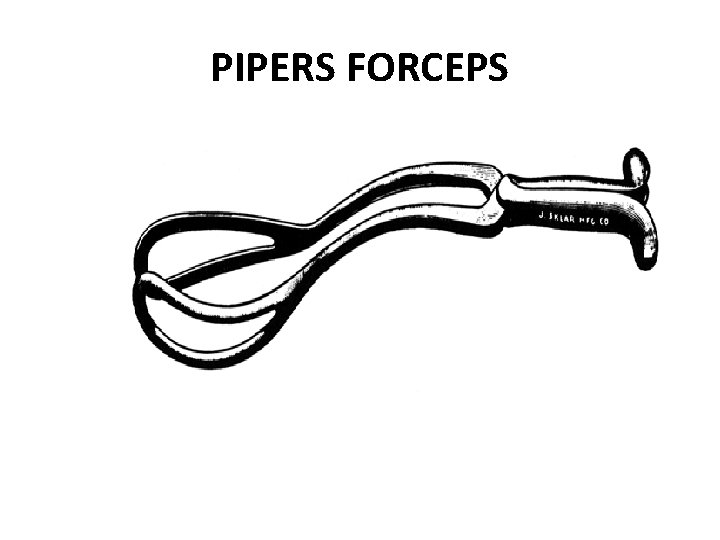
PIPERS FORCEPS
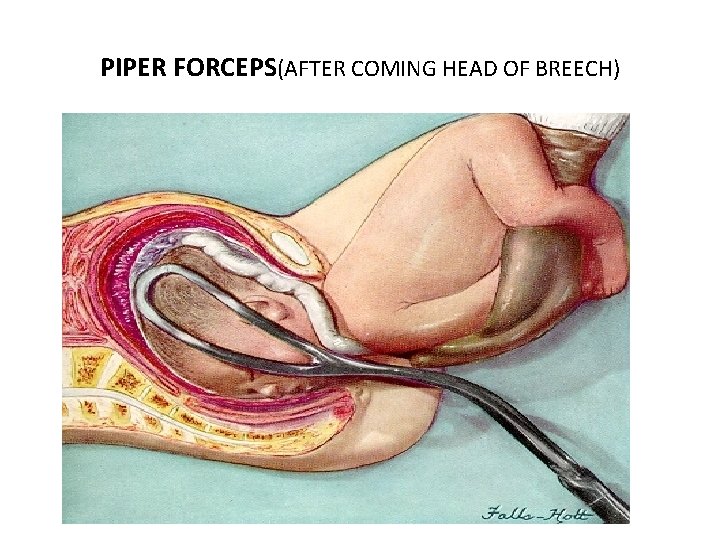
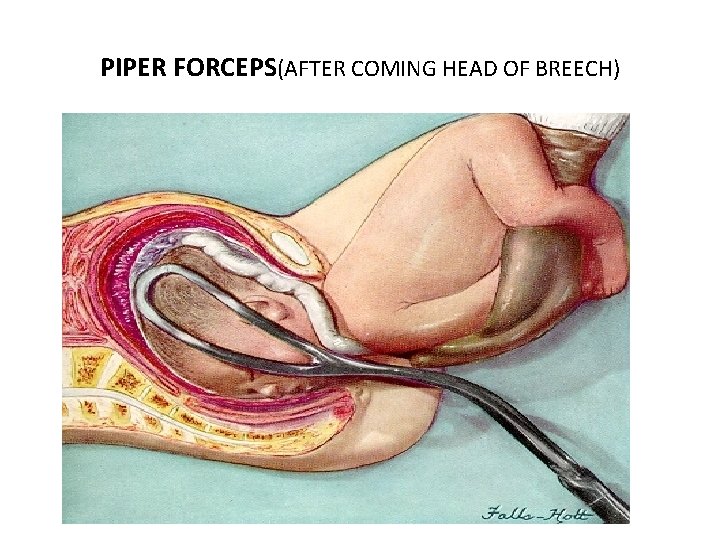
PIPER FORCEPS(AFTER COMING HEAD OF BREECH)
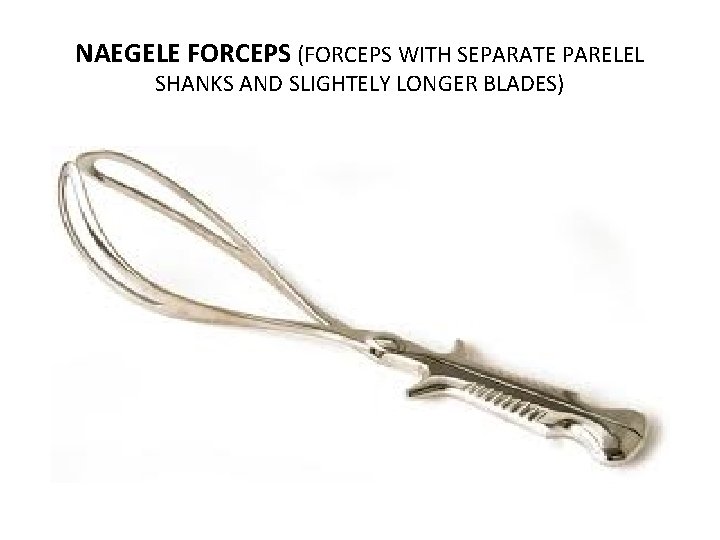
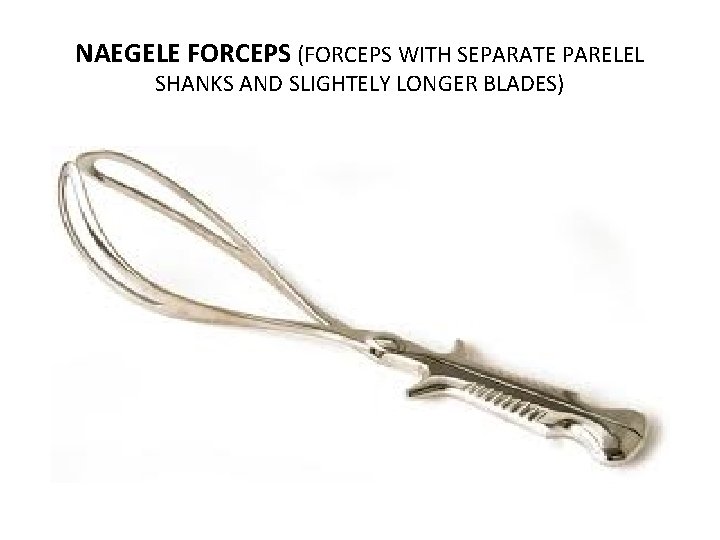
NAEGELE FORCEPS (FORCEPS WITH SEPARATE PARELEL SHANKS AND SLIGHTELY LONGER BLADES)
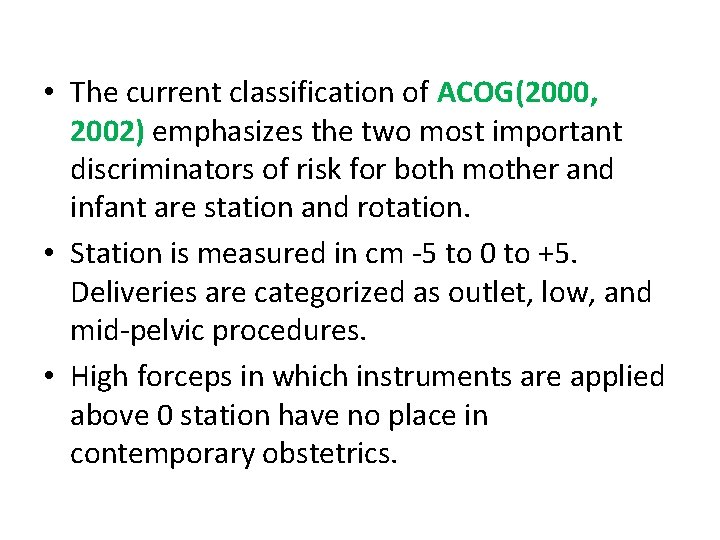
• The current classification of ACOG(2000, 2002) emphasizes the two most important discriminators of risk for both mother and infant are station and rotation. • Station is measured in cm -5 to 0 to +5. Deliveries are categorized as outlet, low, and mid-pelvic procedures. • High forceps in which instruments are applied above 0 station have no place in contemporary obstetrics.
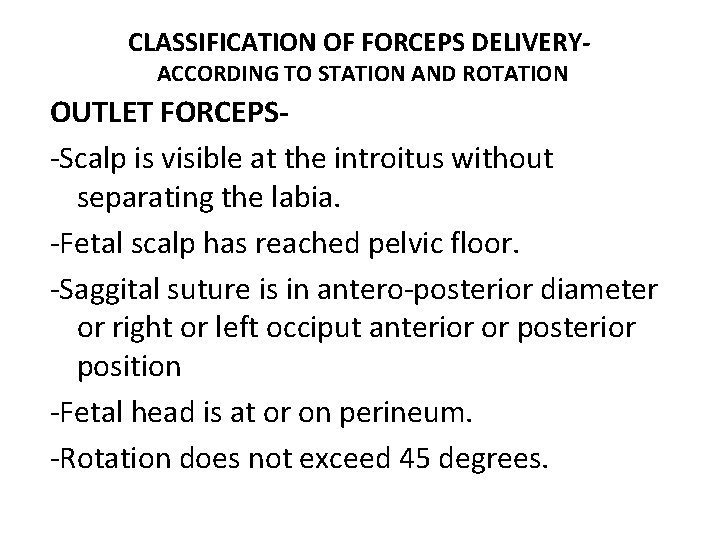
CLASSIFICATION OF FORCEPS DELIVERYACCORDING TO STATION AND ROTATION OUTLET FORCEPS-Scalp is visible at the introitus without separating the labia. -Fetal scalp has reached pelvic floor. -Saggital suture is in antero-posterior diameter or right or left occiput anterior or posterior position -Fetal head is at or on perineum. -Rotation does not exceed 45 degrees.
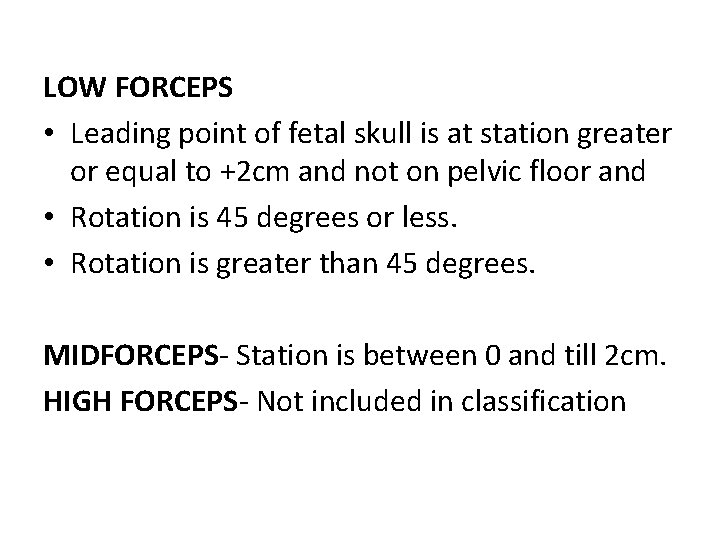
LOW FORCEPS • Leading point of fetal skull is at station greater or equal to +2 cm and not on pelvic floor and • Rotation is 45 degrees or less. • Rotation is greater than 45 degrees. MIDFORCEPS- Station is between 0 and till 2 cm. HIGH FORCEPS- Not included in classification
FUNCTIONS OF FORCEPS • The most important function of forceps is traction but can be used for rotation for occiput transverse and posterior positions. • To provide a protective cage for the head in premature baby or to control delivery of after coming head of breech to lessen dangers of sudden decompression. • One forceps blade may be used as a vectis to assist delivery of head in caesarian section.
IDENTIFICATION OF BLADE OF FORCEPS • Take the blade of forceps • Place it infront of maternal pelvis, tip of the forceps directed towards maternal head, concavity of pelvic curve directed toward the midline of pelvis • The blade which correspond to left side of mother is left blade and right side right blade.
INDICATION OF FORCEPS MATERNAL INDICATIONS-Maternal exhaustion following prolonged labour. -Prolonged second stage of labour. -Maternal distress as shown by maternal tachycardia, dehydration, mild pyrexia -Maternal medical disorder( like cardiac disease, severe anaemia, tuberculosis, pregnancy induced hypertension, eclampsia ) To shorten the second stage or obviate the need for prolonged bearing down. -Failure of decent or internal rotation for 2 hrs in primigravida and 1 hr in multigravida in second stage of labour.
FETAL INDICATIONS -Fetal distress in second stage of labour. -After coming head of breech. -Acute emergencies e. g. cord prolapse or cord loops around the neck causing severe hypoxia.
PROLONGED SECOND STAGE OF LABOUR-(ACCORDING TO ACOG 2002) • IN NULLIPARA- more than three hour with or more than two hour without regional analgesia. • IN MULTIPARAS- more than two hours with or more than one hour without regional anaesthesia.
Indications for operative vaginal delivery (RCOG Guideline) • Fetal - Presumed fetal compromise • Maternal - To shorten and reduce the effects of the second stage of labour on medical conditions • Cardiac disease -Class III or IV (N Y H Association Classification) • • • Hypertensive crises, Myasthenia gravis, Spinal cord injury Patients at risk of autonomic dysreflexia, Proliferative retinopathy
Indications for operative vaginal delivery (RCOG Guideline) contd. . • Inadequate progress • Nulliparous women – Lack of continuing progress for 3 hours (total of active and passive second-stage labour) with regional anaesthesia, or 2 hours without regional anaesthesia • Multiparous women – lack of continuing progress for 2 hours (total of active and passive second-stage labour) • With regional anaesthesia, or 1 hour without regional anaesthesia • Maternal fatigue/exhaustion
PREREQUISITES FORCEPS APPLICATION The cervix must be completely dilated. The membranes must be ruptured. The head must be engaged. The fetus must be vertex, or present a face with chin anterior. • The position of the fetal head must be known. • •
PREREQUISITES FORCEPS APPLICATION • • • contd. . There must be no cephalopelvic disproportion. Bladder must be emptied. Adequate analgesia Experienced operator Verbal or written consent.
Prerequisites for operative vaginal delivery (RCOG Green top guidelines) Head is ≤ 1/5 th palpable per abdomen vaginal examination Vertex presentation. Cervix is fully dilated and the membranes ruptured. Exact position of the head can be determined so proper placement of the instrument can be achieved. • Assessment of caput and moulding. • Pelvis is deemed adequate. Irreducible moulding may indicate cephalo–pelvic disproportion. • •
Prerequisites for operative vaginal delivery (RCOG Green top guidelines)contd. . • Preparation of mother- Clear explanation should be given and informed consent obtained. • Appropriate analgesia is in place for mid-cavity rotational deliveries. This will usually be a regional block. • A pudendal block may be appropriate, particularly in the context of urgent delivery. • Maternal bladder has been emptied recently. In-dwelling catheter should be removed or balloon deflated. • Aseptic technique.
Prerequisites for operative vaginal delivery (RCOG Green top guidelines)contd. . • Preparation of staff- Operator must have the knowledge, experience and skill necessary. • Adequate facilities are available (appropriate equipment, bed, lighting). • Back-up plan in place in case of failure to deliver. When conducting mid-cavity deliveries, theatre staff should be immediately available to allow a caesarean section to be performed without delay (less than 30 minutes).
Prerequisites for operative vaginal delivery (RCOG Green top guidelines)contd. . • A senior obstetrician competent in performing midcavity deliveries should be present if a junior trainee is performing the delivery. • Anticipation of complications that may arise (e. g. shoulder dystocia, postpartum haemorrhage) • Personnel present that are trained in neonatal resuscitation. RCOG Green-top Guideline No. 26 5 of 19 © Royal College of Obstetricians and Gynaecologists
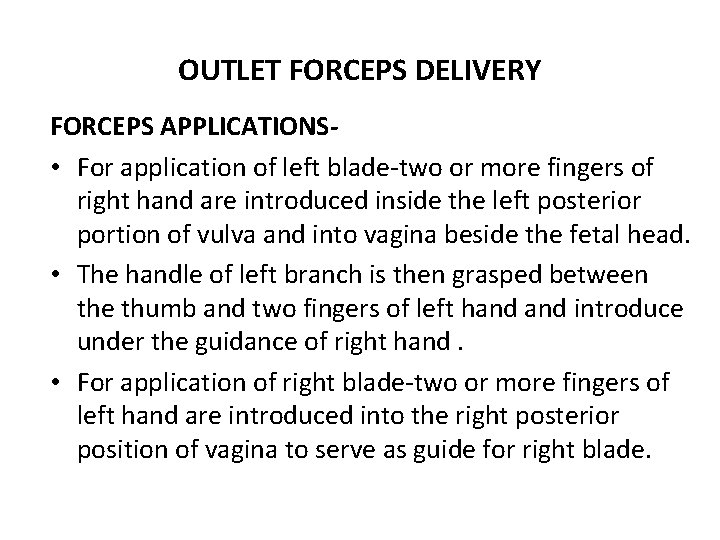
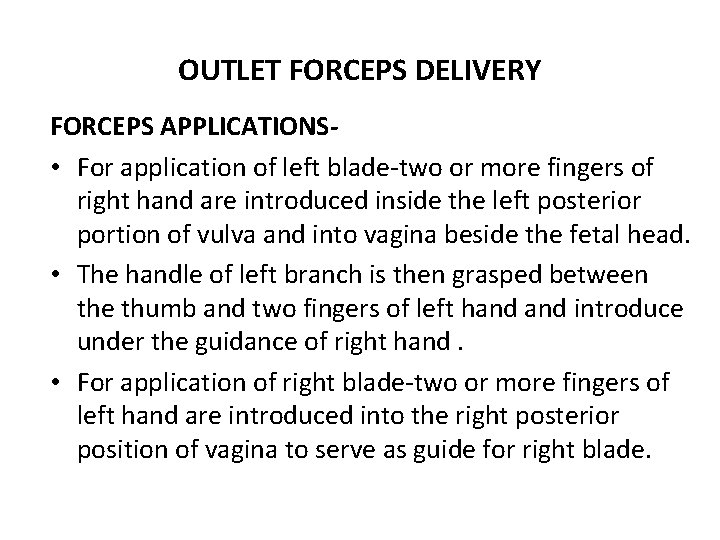
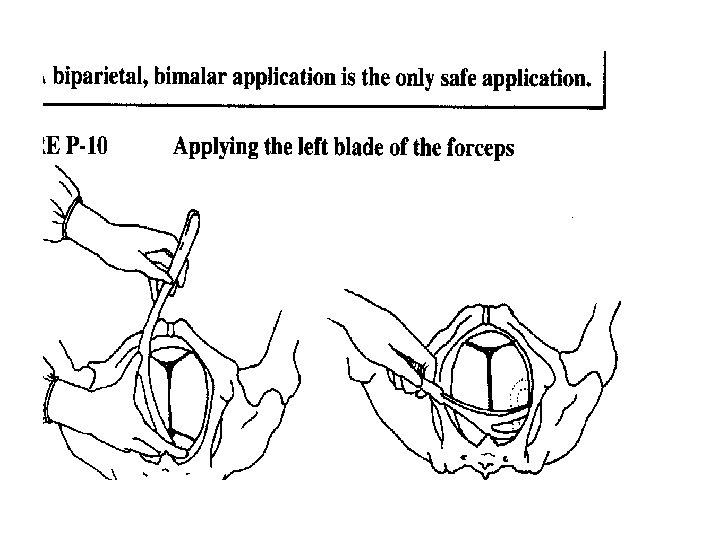
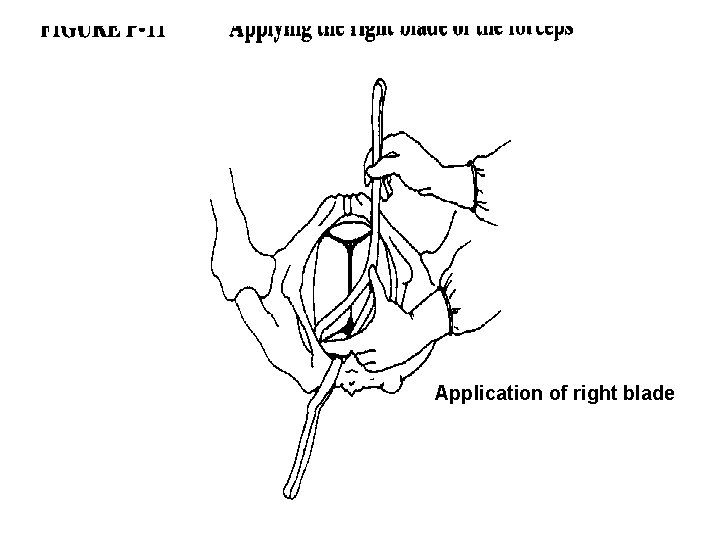
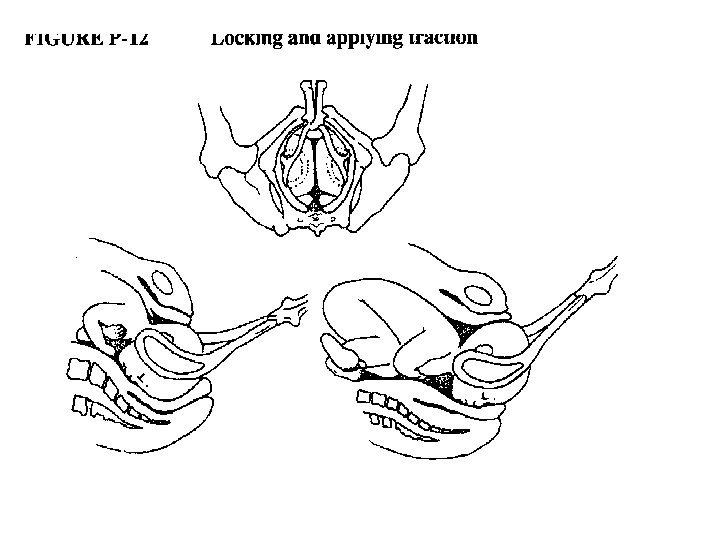
OUTLET FORCEPS DELIVERY FORCEPS APPLICATIONS • For application of left blade-two or more fingers of right hand are introduced inside the left posterior portion of vulva and into vagina beside the fetal head. • The handle of left branch is then grasped between the thumb and two fingers of left hand introduce under the guidance of right hand. • For application of right blade-two or more fingers of left hand are introduced into the right posterior position of vagina to serve as guide for right blade.
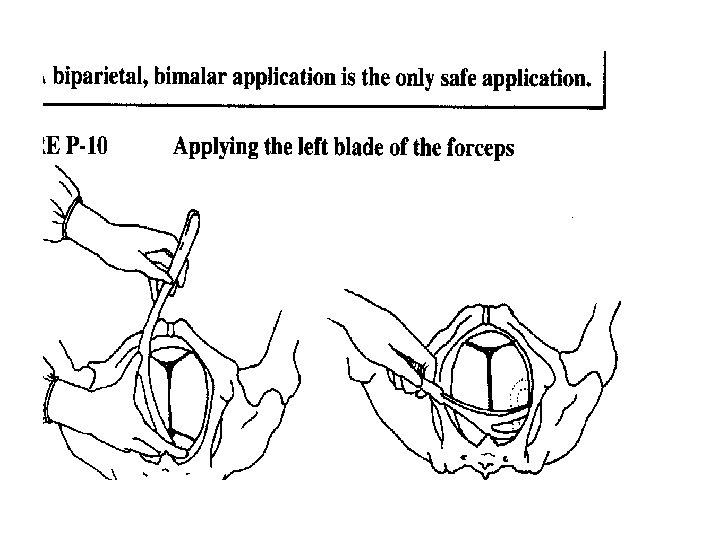
Application of right blade
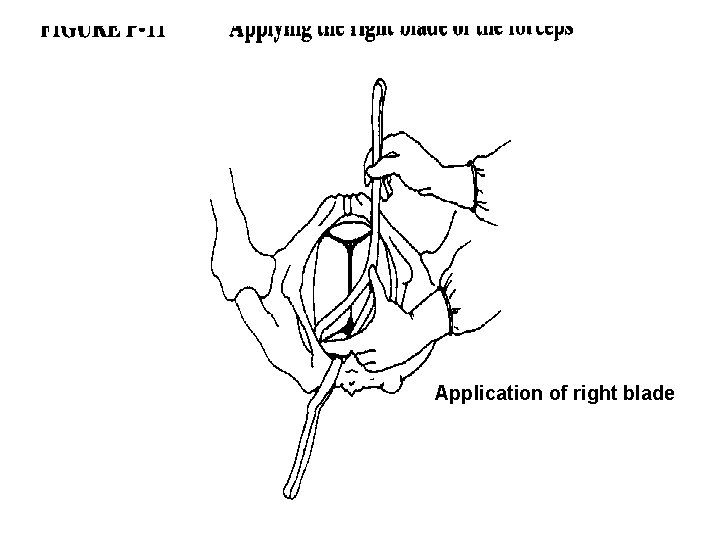
APPLICATIONS OF BLADES • The biparietal diameter corresponds to the greatest distance between appropriately applied blades. • The head of fetus is perfectly grasped only when long axis of blades corresponds to occipitomental diameter. • If one blade is applied over brow and other on occiput, instrument cannot be locked and if locked , blades will slip off when traction is applied.
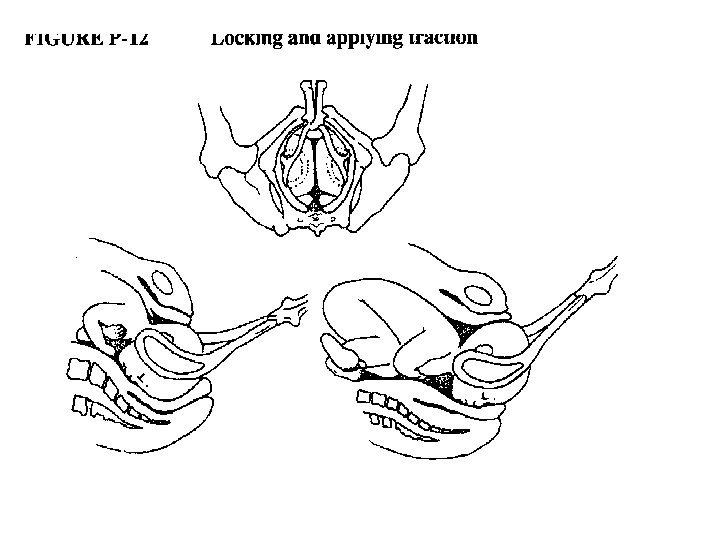
TRACTION When it is certain that blades are applied satisfactorily then gentle , intermittent, horizontal traction is exerted until perineum begins to bulge. • With traction when vulva is distended by the occiput, an episiotomy may be given if indicated.
TRACTION contd… • Additional horizontal traction is applied, and the handles are elevated, pointing directly upwards as parietal bone emerge. • As handles are raised, head is extended. During birth of head, spontaneous delivery should be simulated as closely as possible.
TRACTION contd. . • Traction should be intermittent , and head should be allowed to recede in intervals as in spontaneous labour except in cases of fetal bradycardia. • It is preferable to apply traction only with each uterine contraction. • Maximum permissible force is 45 lb(20 kg) in the nullipara or 30 lb(13 kg)in multipara.
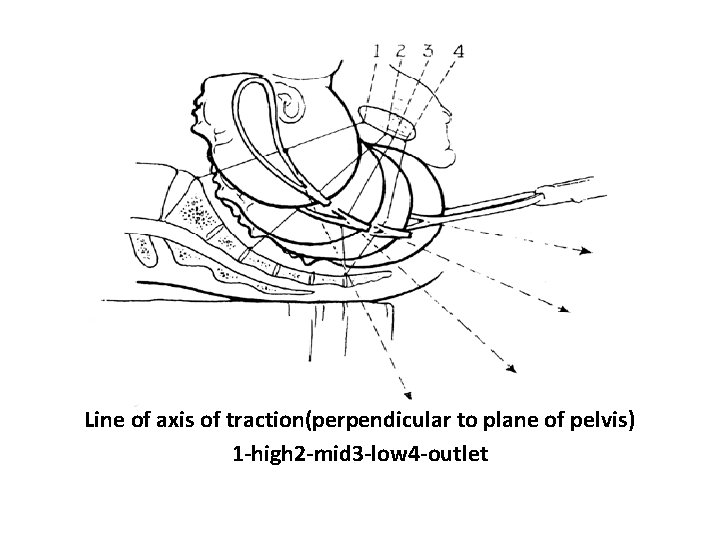
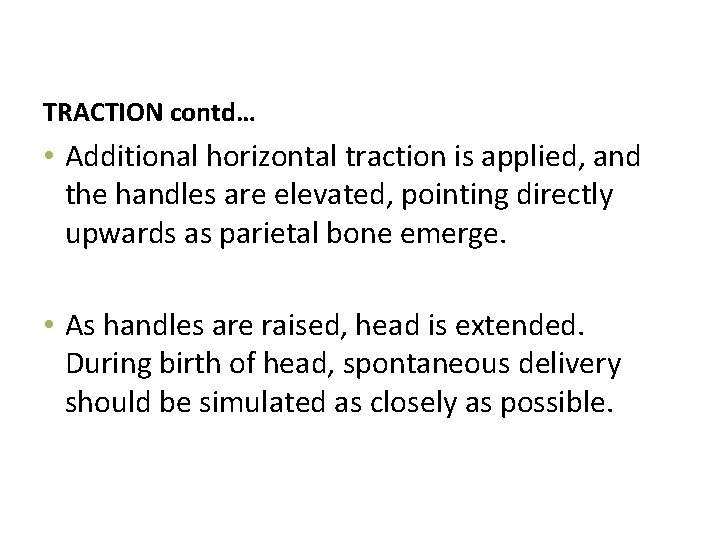
Line of axis of traction(perpendicular to plane of pelvis) 1 -high 2 -mid 3 -low 4 -outlet
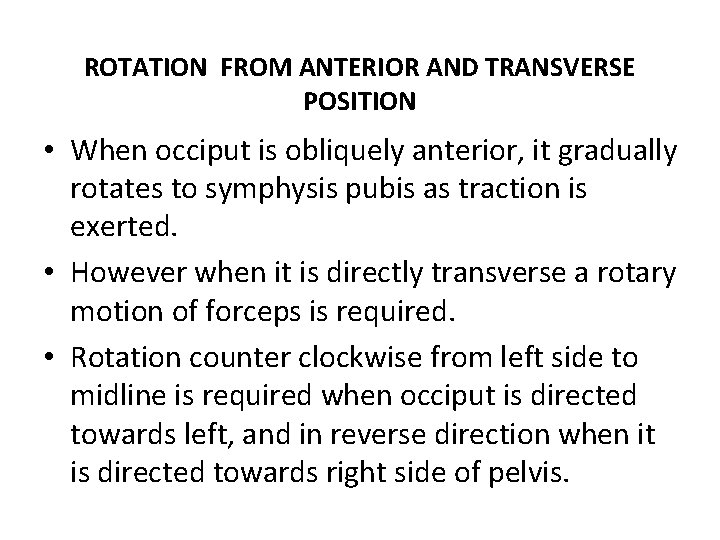
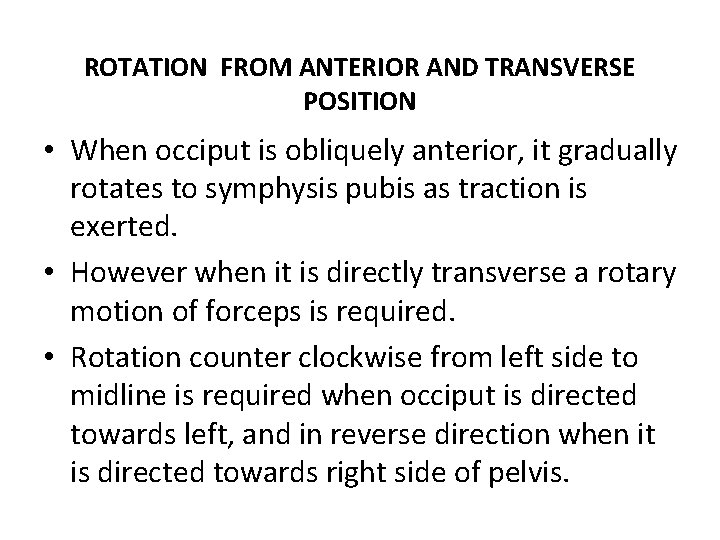
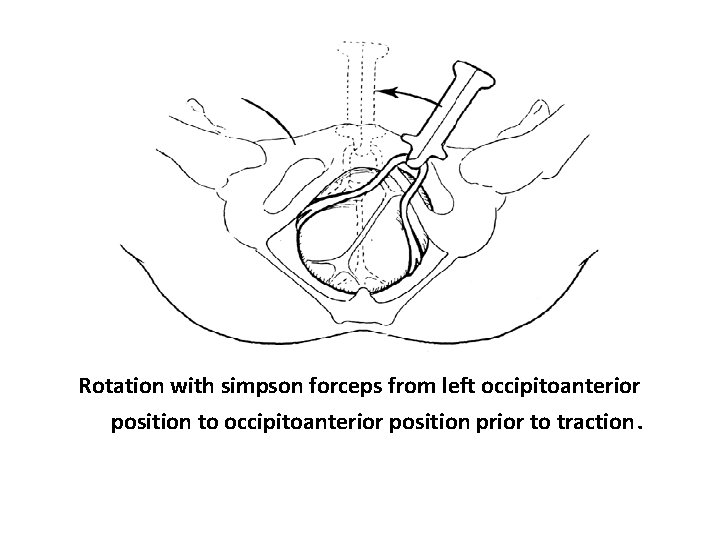
ROTATION FROM ANTERIOR AND TRANSVERSE POSITION • When occiput is obliquely anterior, it gradually rotates to symphysis pubis as traction is exerted. • However when it is directly transverse a rotary motion of forceps is required. • Rotation counter clockwise from left side to midline is required when occiput is directed towards left, and in reverse direction when it is directed towards right side of pelvis.
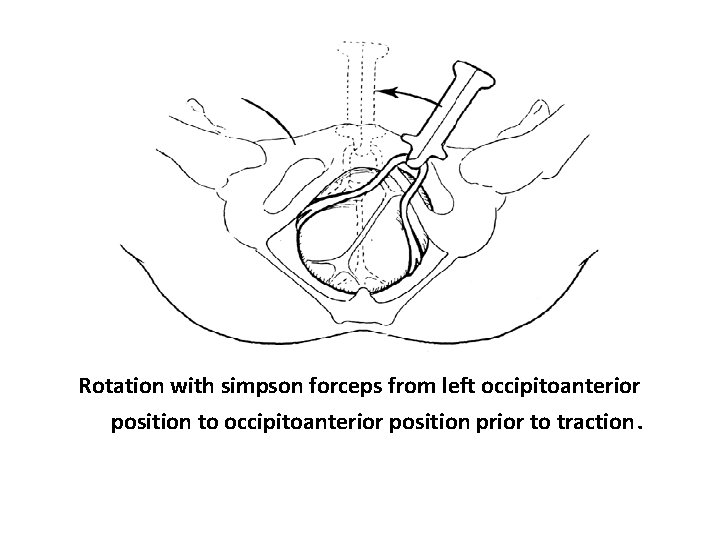
Rotation with simpson forceps from left occipitoanterior position to occipitoanterior position prior to traction.
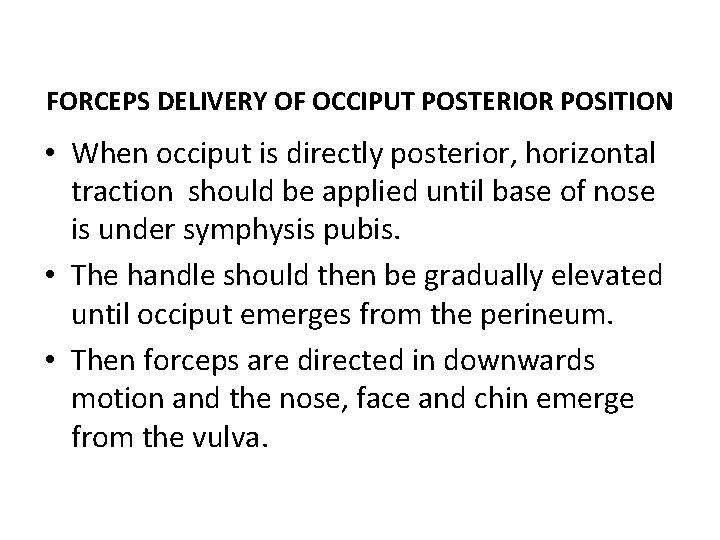
FORCEPS DELIVERY OF OCCIPUT POSTERIOR POSITION • When occiput is directly posterior, horizontal traction should be applied until base of nose is under symphysis pubis. • The handle should then be gradually elevated until occiput emerges from the perineum. • Then forceps are directed in downwards motion and the nose, face and chin emerge from the vulva.
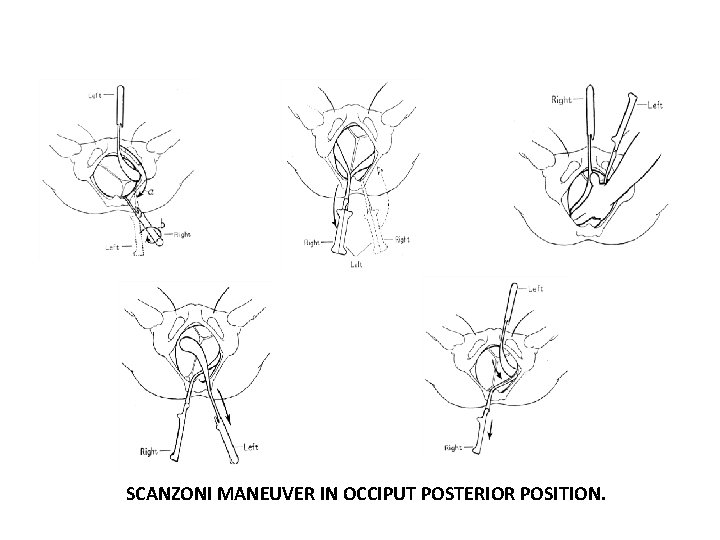
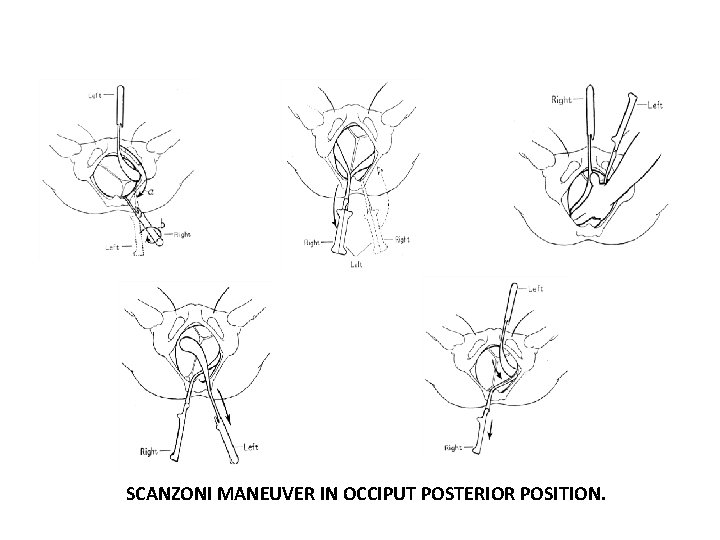
SCANZONI MANEUVER IN OCCIPUT POSTERIOR POSITION.
OCCIPUT POSTERIOR POSITION- COMPLICATION • OCCIPUT POSTERIOR group had higher incidence of perineal lacerations and extensive episiotomy as compared to OCCIPUT ANTERIOR group. • There is also high incidence of operative delivery in OCCIPUT POSTERIOR group • Infants delivered from OCCIPUT POSTERIOR group had high incidence of ERBS and FACIAL NERVE PALSY.
FACE PRESENTATION FORCEPS DELIVERY • With mentum anterior face presentation, forceps can be used to affect vaginal delivery. • The blades are applied to the sides of head along the occipitomental diameter with pelvic curve directed towards neck. • Downwards traction is applied until chin appears under the symphysis. Then by upward movement the face is slowly extracted with nose, eyes, brow and occiput appearing in close succession over anterior margin of perineum.
FORCEPS SHOULD NEVER BE APPLIED TO MENTUM POSTERIOR PRESENTATION BECOZ VAGINAL DELIVERY IS IMPOSSIBLE.
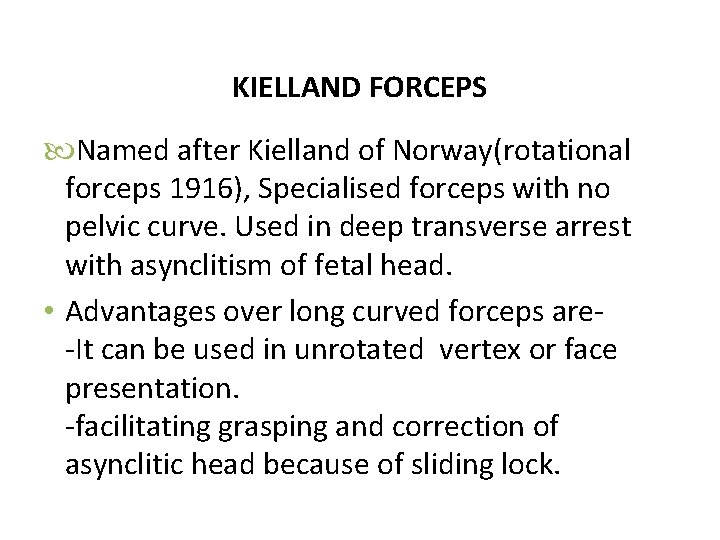
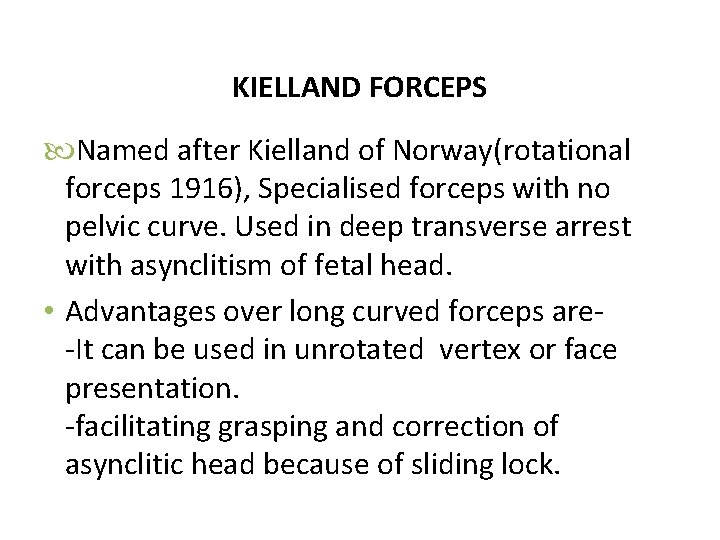
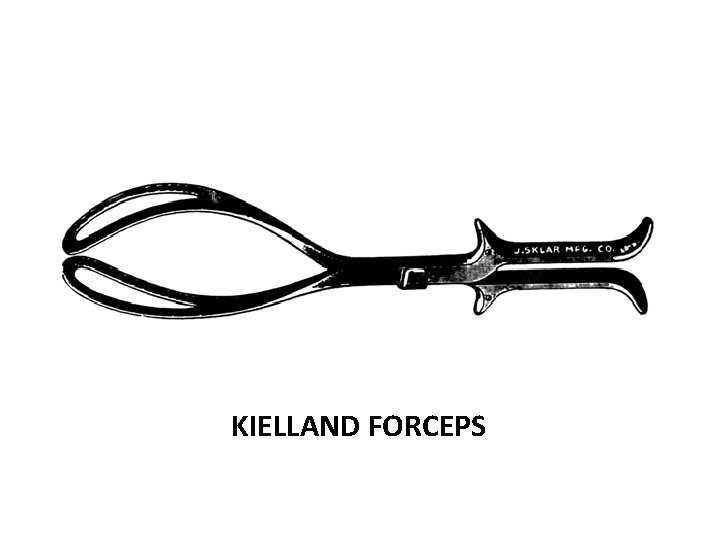
KIELLAND FORCEPS Named after Kielland of Norway(rotational forceps 1916), Specialised forceps with no pelvic curve. Used in deep transverse arrest with asynclitism of fetal head. • Advantages over long curved forceps are-It can be used in unrotated vertex or face presentation. -facilitating grasping and correction of asynclitic head because of sliding lock.
METHODS OF APPLICATION 1 -Classical(obslete) 2 -Wandering 3 -Direct.
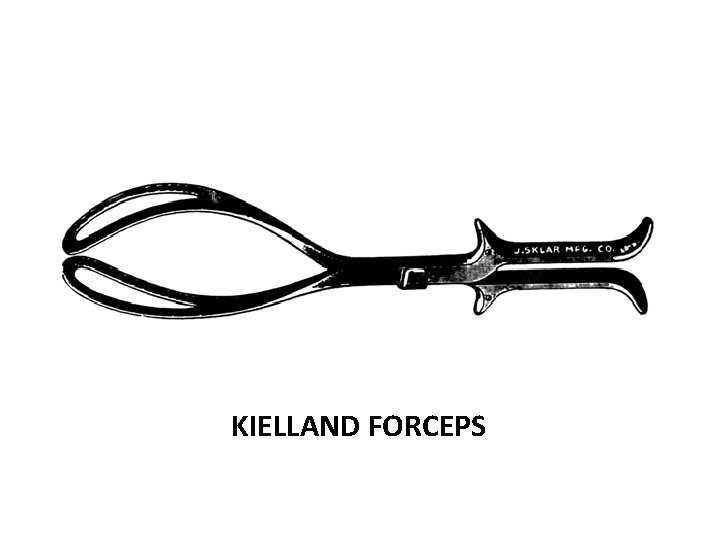
KIELLAND FORCEPS
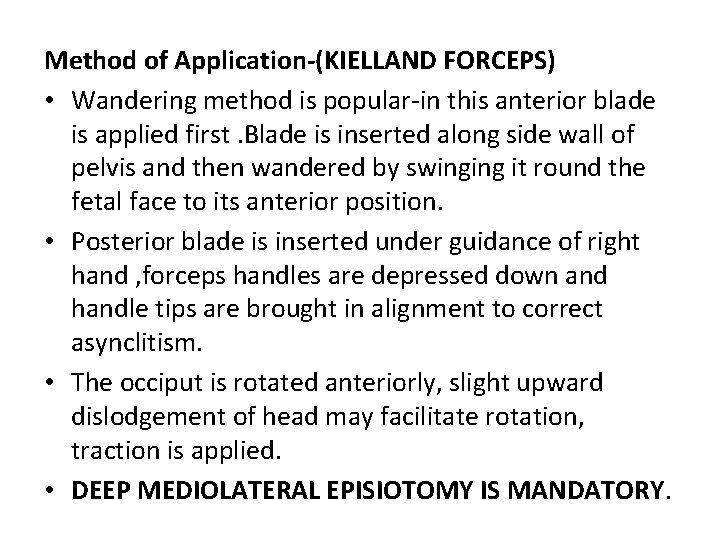
Method of Application-(KIELLAND FORCEPS) • Wandering method is popular-in this anterior blade is applied first. Blade is inserted along side wall of pelvis and then wandered by swinging it round the fetal face to its anterior position. • Posterior blade is inserted under guidance of right hand , forceps handles are depressed down and handle tips are brought in alignment to correct asynclitism. • The occiput is rotated anteriorly, slight upward dislodgement of head may facilitate rotation, traction is applied. • DEEP MEDIOLATERAL EPISIOTOMY IS MANDATORY.
MATERNAL MORBIDITY FROM FORCEPS -The greater the rotation, greater will be the morbidity in form of laceration and blood loss. -Forceps deliveries are associated with higher episiotomy rates and third and fourth degrees lacerations. -Postpartum urinary retention and bladder dysfunction. -Anal sphincter dysfunction -Infection -Pelvic haematoma. -Traumatic post partum haemorrhage and shock.
FETAL MORBIDITY -Cephalhaematoma, skull fracture and intracranial haemorrhage. -Brain damage -Marked depression of respiration and asphyxia. -Facial palsy, brachial palsy. -soft tissue injury to face, bruising and laceration, Cord compression, convulsions.
CONTRAINDICATIONS FORCEPS -Absence of full dilatation of cervix. -In case of cephalopelvic disproportion. -High station of fetal head. -If uterine contraction cease. -Lack of experience of operator. -Mentum posterior face presentation. -Hydrocephalic infant. -Brow presentation.
TRIAL OF FORCEPS It is a tentative attempt of forceps delivery in case of suspected midpelvic contraction with a declaration of abandoning it in favor of caesarean section if moderate traction fails to overcome the resistance. Such an operation must be undertaken on a operating table in properly equipped operating theatre with an anaesthetist present. If there is difficulty at any stage from introduction of blades, locking of device or resistance to gentle traction then undue force is not used forceps withdrawn and caesarian section done.
FAILED FORCEPS When a deliberate attempt in vaginal delivery with forceps has failed to expedite the process, it is called failed forceps. FORCEPS FAILED IF- Fetal head does not advance with each pull. Fetus is undelivered after three pulls with no descent or after 30 minutes If forceps fails caesarian section is performed.
Higher rates of failure associated with: • maternal body mass index over 30 • estimated fetal weight over 4000 g or clinically big baby • occipito-posterior position • mid-cavity delivery or when 1/5 th of the head palpable per abdomen • African American race, increased maternal age. • Diabetes, polyhydramnios, • Dysfuctional labour, induction of labour
PROPHYLACTIC FORCEPS(ELECTIVE) • Named after De. Lee. It refers to forceps delivery only to shorten the second stage of labour when maternal and or fetal complications are anticipated. • INDICATIONS –Eclampsia, heart disease , previous history of caesarean section, postmaturity, lowbirth weight baby, to curtail the painful second stage, patient under epidural analgesia. • Prophylactic forceps should not be applied until the criteria of low forceps are fulfilled.
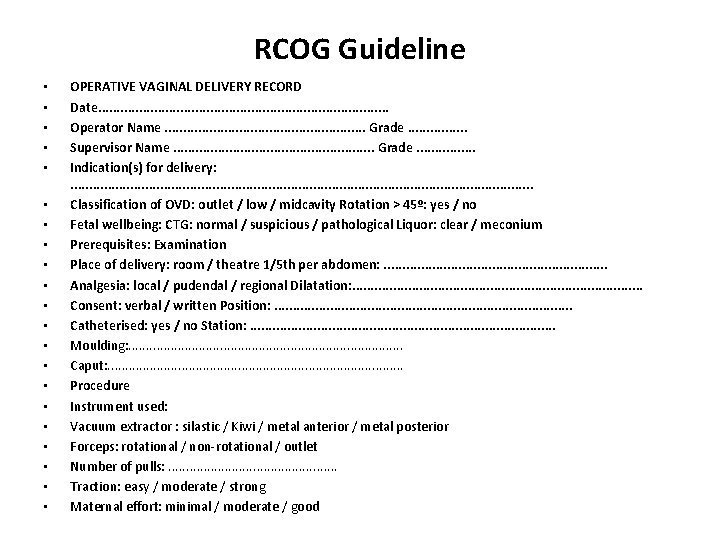
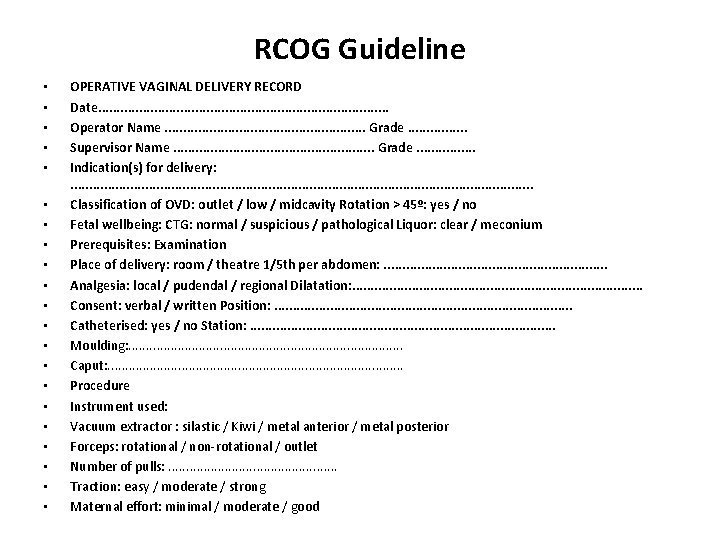
RCOG Guideline • • • • • • OPERATIVE VAGINAL DELIVERY RECORD Date. . . . . Operator Name. . . . Grade. . . . Supervisor Name. . . . Grade. . . . Indication(s) for delivery: . . . . . . . . Classification of OVD: outlet / low / midcavity Rotation > 45º: yes / no Fetal wellbeing: CTG: normal / suspicious / pathological Liquor: clear / meconium Prerequisites: Examination Place of delivery: room / theatre 1/5 th per abdomen: . . . . Analgesia: local / pudendal / regional Dilatation: . . . . . Consent: verbal / written Position: . . . . . Catheterised: yes / no Station: . . . . . Moulding: . . . . . Caput: . . . . . Procedure Instrument used: Vacuum extractor : silastic / Kiwi / metal anterior / metal posterior Forceps: rotational / non-rotational / outlet Number of pulls: . . . Traction: easy / moderate / strong Maternal effort: minimal / moderate / good
Placenta: CCT/ manual Episiotomy: yes / no Perineal tear: 1 st degree 2 nd degree 3 rd / 4 th degree (complete pro forma) Other (complete suturing pro forma if necessary) EBL: . . . . Baby: M / F Birth weight: . . (kg) Apgar: 1. . . 5. . . 10. . . Cord p. H: Arterial. . Venous. . Post-delivery care: Level of care: routine / high dependency Syntocinon infusion: yes / no Catheter: yes / no Remove. . . . Vaginal pack: yes / no Remove. . . . Diclofenac 100 mg PR: yes / no Analgesia prescribed: yes / no Thromboembolic risk: low / medium / high Thromboprophylaxis prescribed: yes / no Signature: . . . . . . Date: . . . Patient Details Multiple instrument use: yes / no Examination before second instrument 1/5 th per abdomen: . . . . Position: . . . Station: . . . Moulding: . . . Caput: . . . Reasons for second instrument: . . . . . . . . . . .
Vacuum Extraction (Ventouse)
Vacuum Extraction (Ventouse) • It is an instrumental device designed to assist delivery by creating a vacuum between it and the fetal scalp • In the United states the device is referred to as the vacuum extractor whereas in Europe it is called as Ventouse- from the french word literally meaning soft cup.
Historical background • In 1705, Yonge described an attempted vaginal delivery using a cupping glass • In 1848 Simpson devised a bell shaped device called an “air tractor vacuum extractor” • In 1953 a metal cup extractor was developed by Malmstrom.
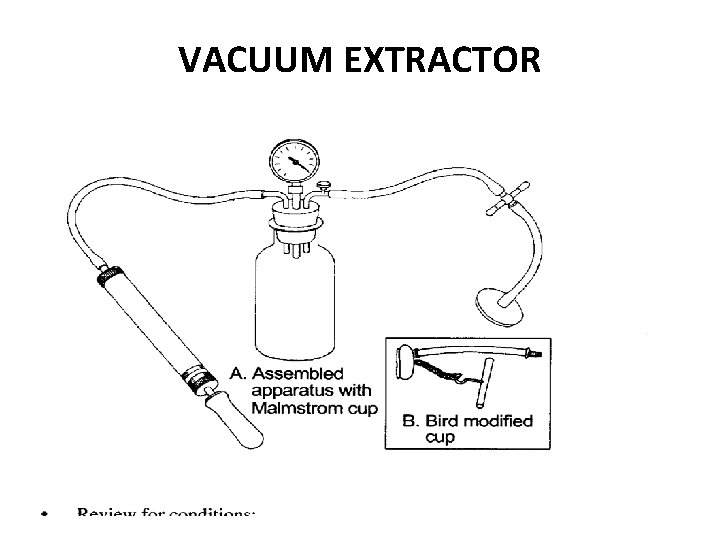
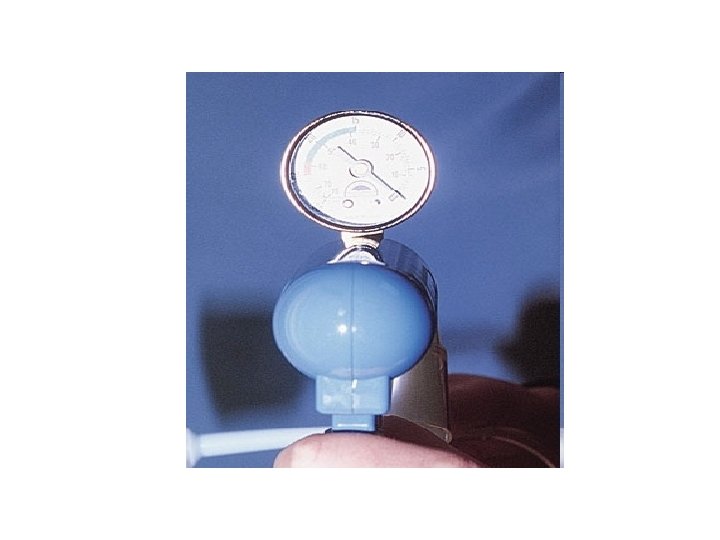
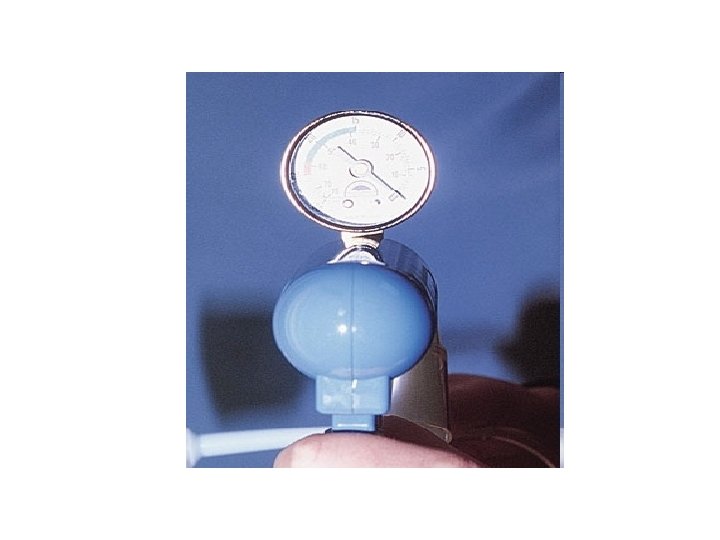
Description • Vacuum extractor is composed of: • A specially designed cup with a diameter of 3, 4, 5 or 6 cm. • A rubber tube attaching the cup to a glass bottle with a screw in between to release the negative pressure. • A manometer fitted in the mouth of the glass bottle to declare the negative pressure. • Another rubber tube connecting the bottle to a suction piece which may be manual or electronic creating a negative pressure that should not exceed 0. 8 kg per cm 2.
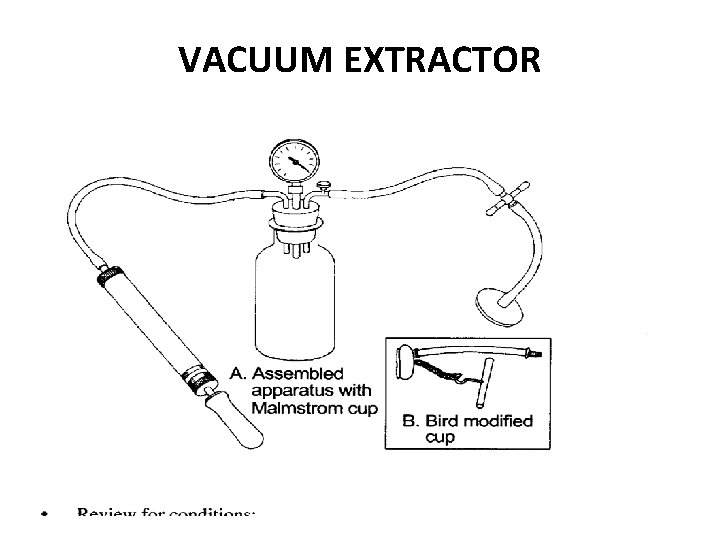
VACUUM EXTRACTOR

Types of vacuum extractors Vacuum extractors are divided on the basis of the type of cup-metal or plastic 1. Metal cup vacuum extractors 2. Soft cup vacuum extractors
Metal cup • The metal-cup vacuum extractor is a mushroomshaped metal cup varying from 40 to 60 mm in diameter. • Metal-cup vacuum extractors have a higher success rate and easier cup placement in the occipitoposterior (OP) position, • The rigidity of metal cups can make application difficult and uncomfortable, and their use is associated with an increased risk of fetal scalp injuries.
Soft cup • Traditionally soft cups are bell or funnel shaped. • Soft-cup instruments can be used with a manual vacuum pump or an electrical suction device. Soft-cup vacuum extractors may be disposable or reusable. • Compared with metal-cup devices, soft-cup vacuum extractors cause fewer neonatal scalp injuries. However, these instruments have a higher failure rate.
Indications of vacuum extraction • Generally vacuum extraction is reserved for fetuses who have attained a gestational age of 34 weeks. • Otherwise, the indications and pre-requisites for its use are the same as forceps delivery(American College of obstetricians and Gynecologists
Contraindications • • Operator inexperience Inability to assess fetal position High station(above 0 station) Suspicion of cephalopelvic disproportion Other presentations than vertex. Premature fetus(<34 weeks). Intact membranes.
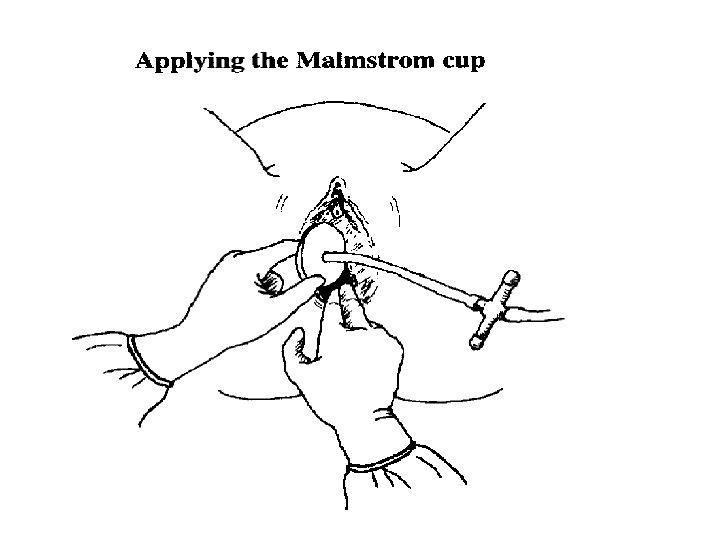
Pre-requisites of the Procedure • Procedure should be explained to the patient and consent should be taken • Emotional support and encouragement • Lithotomy position. • Bladder should be emptied. • Antiseptic measures for the vagina, vulva and perineum. • Vaginal examination to check pelvic capacity, cervical dilatation, presentation, position, station and degree of flexion of the head and that the membranes are ruptured.
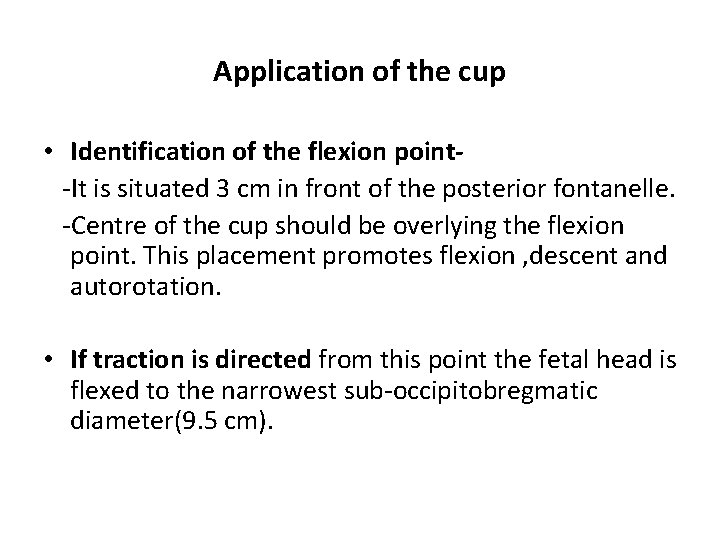
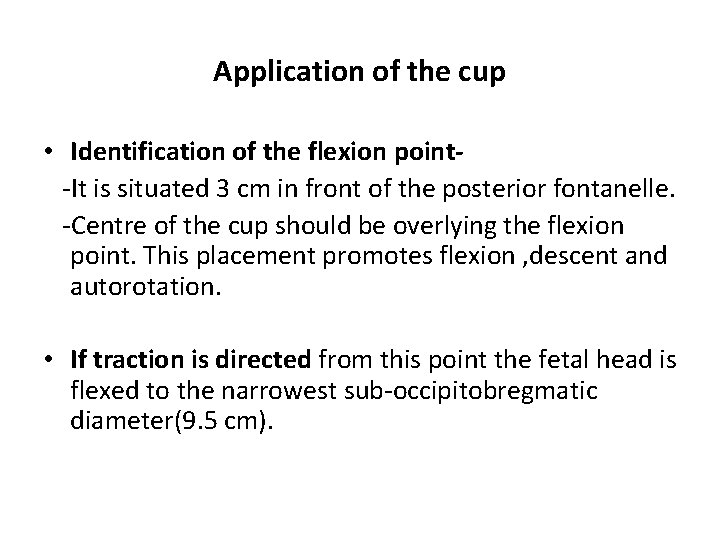
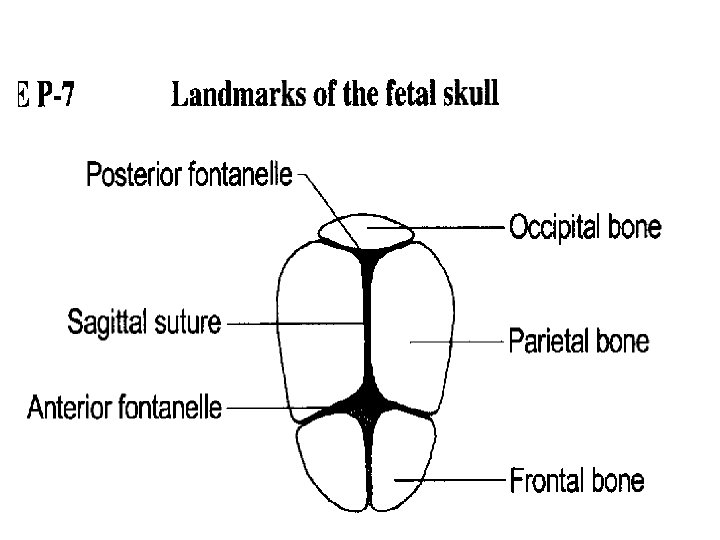
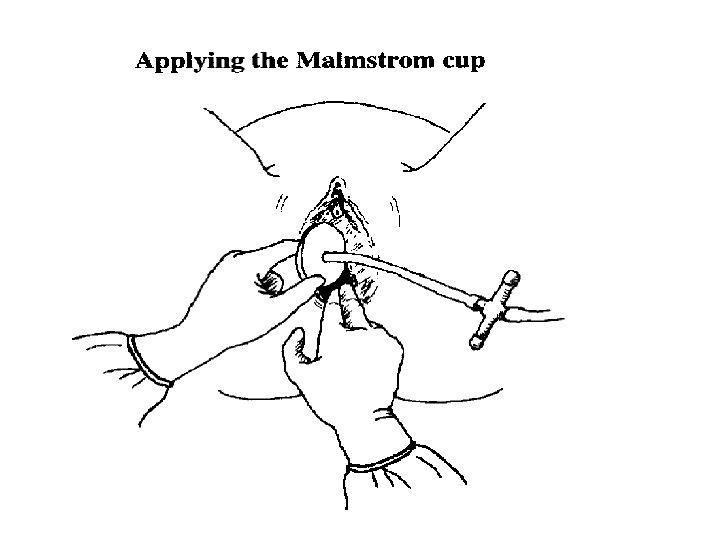
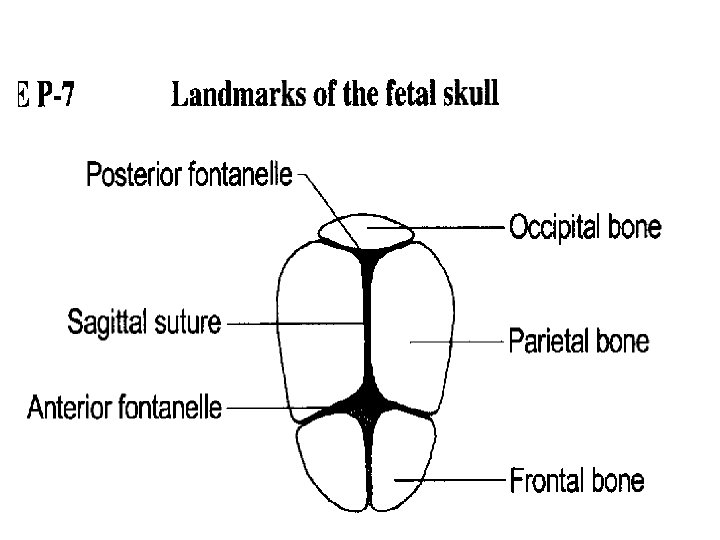
Application of the cup • Identification of the flexion point-It is situated 3 cm in front of the posterior fontanelle. -Centre of the cup should be overlying the flexion point. This placement promotes flexion , descent and autorotation. • If traction is directed from this point the fetal head is flexed to the narrowest sub-occipitobregmatic diameter(9. 5 cm).
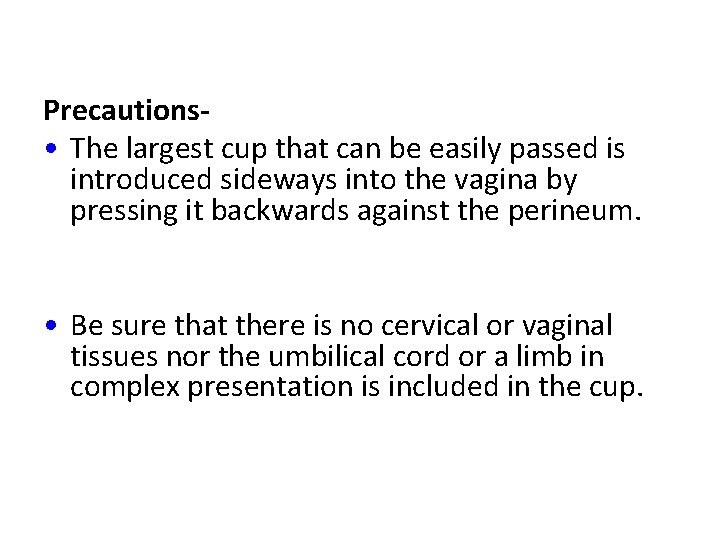
Precautions • The largest cup that can be easily passed is introduced sideways into the vagina by pressing it backwards against the perineum. • Be sure that there is no cervical or vaginal tissues nor the umbilical cord or a limb in complex presentation is included in the cup.
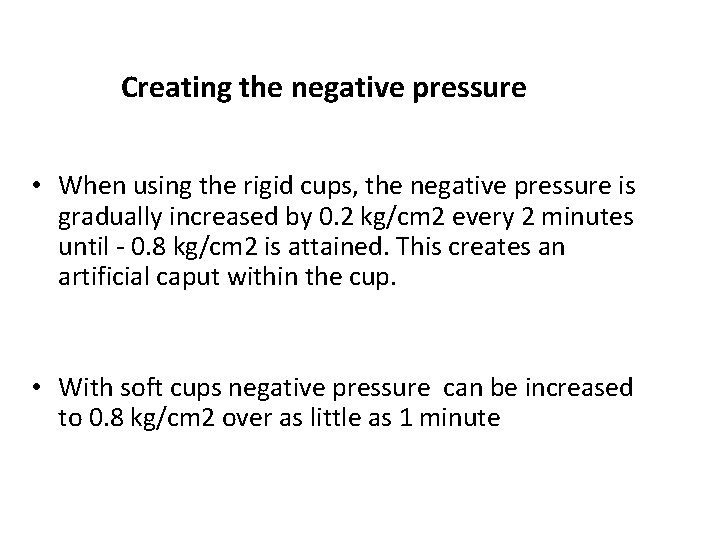
Creating the negative pressure • When using the rigid cups, the negative pressure is gradually increased by 0. 2 kg/cm 2 every 2 minutes until - 0. 8 kg/cm 2 is attained. This creates an artificial caput within the cup. • With soft cups negative pressure can be increased to 0. 8 kg/cm 2 over as little as 1 minute
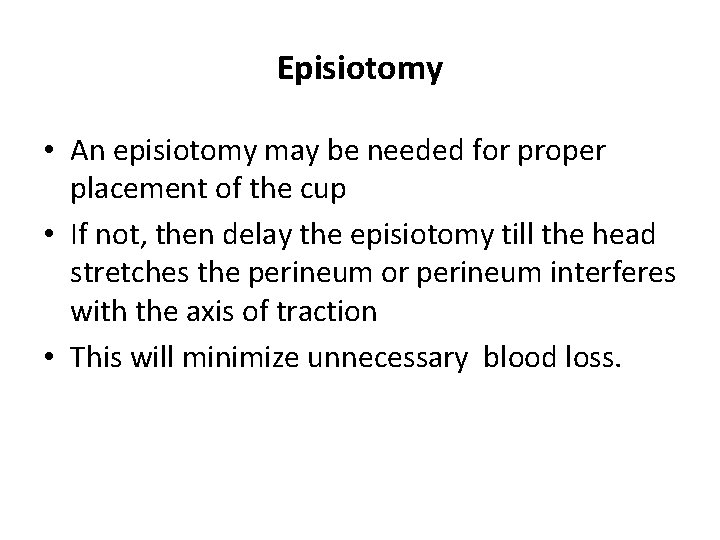
Episiotomy • An episiotomy may be needed for proper placement of the cup • If not, then delay the episiotomy till the head stretches the perineum or perineum interferes with the axis of traction • This will minimize unnecessary blood loss.
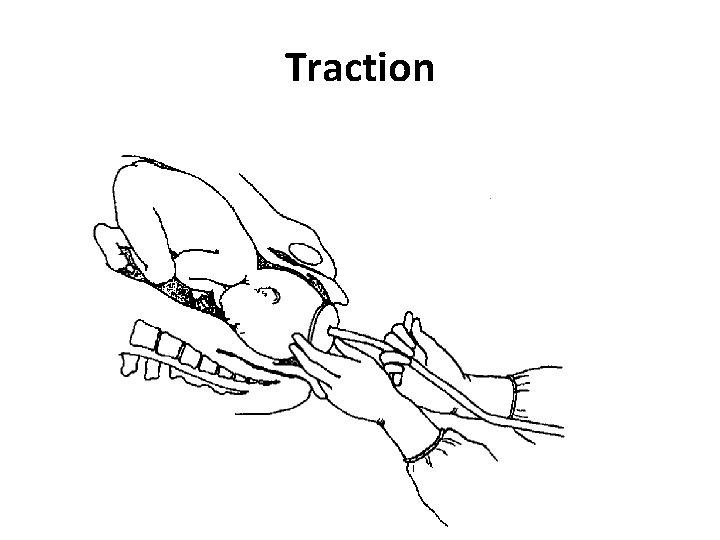
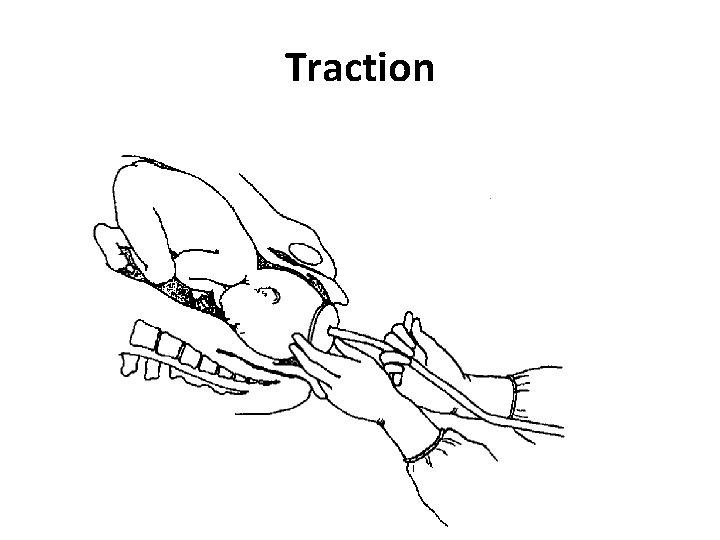
Traction • Traction should be intermittent and coordinated with maternal expulsive efforts and with uterine contractions. • Traction should be in line of the pelvic axis and perpendicular to the plane of the cup
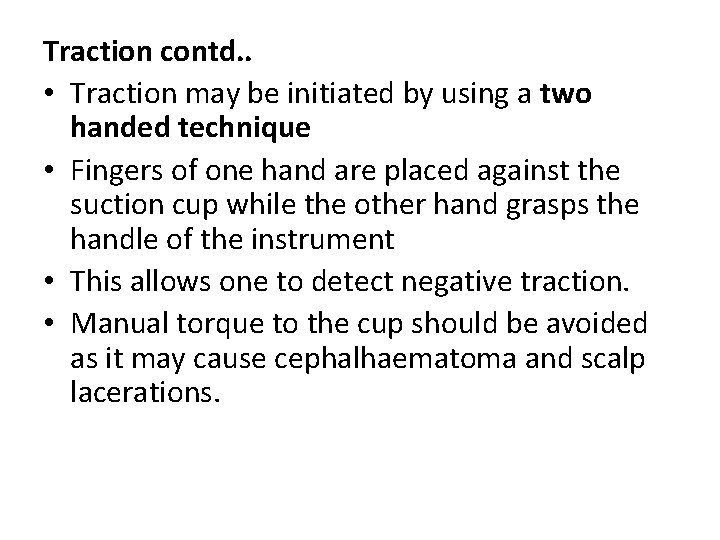
Traction contd. . • Traction may be initiated by using a two handed technique • Fingers of one hand are placed against the suction cup while the other hand grasps the handle of the instrument • This allows one to detect negative traction. • Manual torque to the cup should be avoided as it may cause cephalhaematoma and scalp lacerations.
Traction
Traction contd. . • Between contractions, check for fetal heart rate and proper application of the cup • Check for sacral hand wedge if the head has descended to the perineum with traction but further progress is slow.
Release • When the head is delivered the vacuum is reduced as slowly as it was created using the screw as this diminishes the risk of scalp damage. • The chignon should be explained to the patient and the relatives.
Reapplication of the cup If the cup detaches for the first time, reassess the situation. If favorable , then reapply. If cup detaches for the second time, reassess if vaginal delivery is safe or move to caesarean section Caesarean section is necessary if there is inadequate descent and rotation
Failure of vacuum • Vacuum extraction is considered failed if-fetal head does not advance with each pull -fetus is undelivered after 3 pulls with no descent or after 30 minutes -cup slips off the head twice at the proper direction of pull with the maximum negative pressure.
Advantages of Vacuum over Forceps Regional Anaesthesia is not required so it is preferred in cardiac and pulmonary patient. The ventouse is not occupying a space beside the head as forceps. Less compression force (0. 77 kg/cm 2) compared to forceps (1. 3 kg/cm 2) so injuries to the head is less common. Less genital tract lacerations. Can be applied before full cervical dilatation. It can be applied on non-engaged head.
Complications Maternal Perineal, vaginal , labial, periurethral and cervical lacerations. Annular detachment of the cervix when applied with incompletely dilated cervix. Cervical incompetence and future prolapse if used with incompletely dilated cervix.
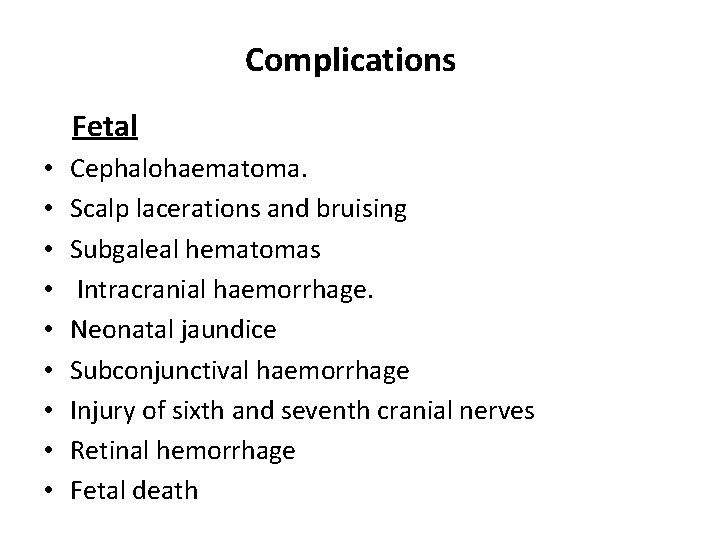
Complications Fetal • • • Cephalohaematoma. Scalp lacerations and bruising Subgaleal hematomas Intracranial haemorrhage. Neonatal jaundice Subconjunctival haemorrhage Injury of sixth and seventh cranial nerves Retinal hemorrhage Fetal death

Instrumental deliveries Questionaire
1) In current obstetrics, forceps deliveries are categorized in one of the following three groups: a) High forceps, mid forceps, low forceps b) Mid forceps, low forceps, outlet forceps c) Inlet forceps, mid forceps, outlet forceps d) Inlet forceps, low forceps, outlet forceps
B ( mid forceps, low forceps, outlet forceps)
2) In general, the categories of forceps delivery are defined by which of the following: a) Fetal station b) Type of forceps used c) maternal pelvic shape d) Degree of fetal moulding
A (fetal station)
3) Which of the following describes forceps that are applied to the fetal head with the scalp visible at the introitus without manual separation of the labia: a) mid forceps b) Low forceps c) Inlet forceps d) Outlet forceps
D ( OUTLET FORCEPS)
4)Prerequisites forceps application include all except which of the following: a) Head is engaged b) Membranes are ruptured c) Cervix is fully dilated d) Late fetal heart rate deccelerations are absent
D ( late fetal heart rate deccelerations are absent)
5) In general, vacuum extraction would be contraindicated in all except in : a) 30 week fetus b) Fetal thrombocytopenia c) Occiput transverse presentation d) Inability to assess fetal head position
C ( Occipito transverse position)
6) Ventouse is contraindicated in all except: a) Fetal distress b) Face presentation c) Transverse lie d) Anemia
D ( Anemia)
7) The effective pressure to be achieved in vacuum extraction is: a) 0. 1 kg/cm 2 b) 0. 8 kg/cm 2 c) 0. 4 kg/cm 2 d) 1. 2 kg/cm 2
B ( 0. 8 kg/cm 2)
8) Forceps is applied in all the following except: a) After coming head of breech b) Face presentation c) Occipitoposterior d) Brow presentation
D ( Brow presentation)
9) Contraindication to ventouse delivery is all except: a) Fetal coagulopathies b) Extreme prematurity c) Mento transverse position d) Occipito transverse position
D ( occipito transverse)
10) Maternal morbidity with forceps delivery is most closely predicted by which of the following: a) Fetal head station b) Maternal parity c) Degree of fetal distress d) Degree of fetal head moulding
A ( Fetal head station)
THANK YOU