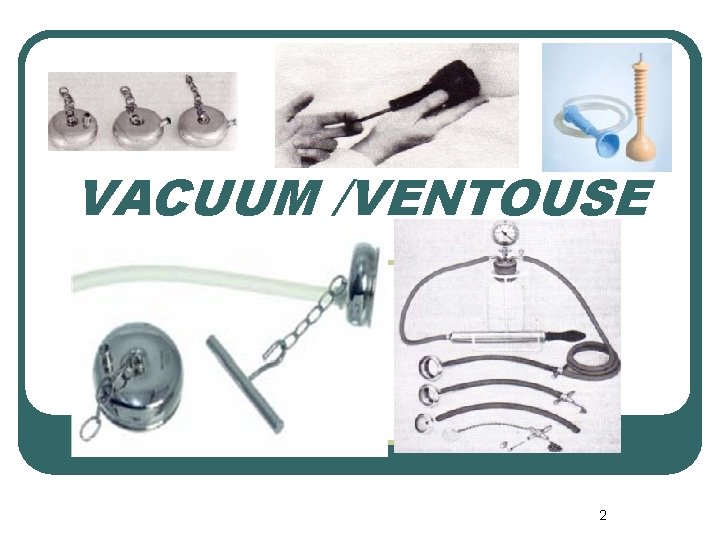
Operative Vaginal Delivery cesarean 1 VACUUM VENTOUSE 2


- Slides: 43

Operative Vaginal Delivery & cesarean 1
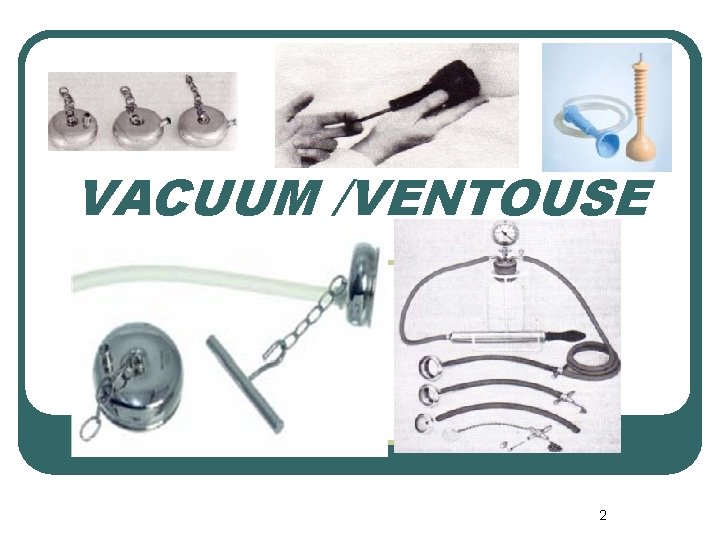
VACUUM /VENTOUSE 2

FORCEPS 3
l early 20 th century when almost 50% of all deliveries were with forceps. Over the last three decades this has changed and worldwide there has been a decrease in the use of operative techniques. This has been accompanied by a relative increase in abdominal delivery. 4
There are various explanations for this trend including: l development of more effective anesthesia techniques, l introduction of antibiotics, , l development of improved surgical techniques 5
Caput Succedaneum l l l Commonly referred to as caput, caput succedaneum aponeurosis and periosteum) over lying the leading part of the skull. This is a normal occurrence , the result of pressure from the cervix interrupting venous and lymphatic drainage from the scalp during labor. There are varying degrees of caput and these are described subsequently. Caput usually disappears within hours after birth. 6
Cephalhematoma l l l A cephalhematoma is a collection of blood between the periosteum and the skull bone. The extent of the bleed is limited by the periosteal attachments at the suture lines but can still be significant. Cephalhematomas usually take hours to develop and weeks to reabsorb. 7
Suhgaleal (Subaponeurotic) Hemorrhage l l l emissary veins are damaged and blood accumulates in the potential space between the galea aponeurotica and the periosteum of the skull subgaleal hematoma may extend from the orbital ridges to the nape of the neck. dangerous , life-threatening hemorrhage. Subgaleal bleeding presents with diffuse swelling of the head and signs of hypovolemic shock (e. g. , pallor, hypotension, tachycardia, and increased respiration rate). The signs may be present at delivery or may not become clinically apparent until several hours or up to a few days 8
Molding l Molding is an expected deformation of the fetal head that occurs during the delivery process. A small amount of occipitoparietal molding is normal during the second stage of labor but excessive skull bone molding (particularly parieto-parietal molding) is abnormal during the first stage of labor. 9
Prerequisites for an operative vaginal delivery l F Favorable head position (OA/AP <45 degrees from the AP diameter)—unless intended rotational delivery -Fetal assessment (weight and status) l O Open Os (completely dilated cervix) l R, Ruptured membranes l C Contractions present, Consent (verbal or written) 10
l E Engaged head, Empty bladder, Epidural or other form of adequate anesthesia l P Prepared for cesarean section, if needed Prepared for neonatal resuscitation, if needed Pelvimetry (clinical) adequate Preoperative note written l S Stirrups and lithotomy position with attention paid to pressure points and prevention of hyperflexion at the hips (to avoid femoral nerve 11 apraxia)
Indications for vacuum-assisted delivery l Maternal indications l l Need to avoid voluntary maternal expulsive effort (e. g. , the mother has cardiac or cerebrovascular disease) Inadequate maternal expulsive efforts Maternal exhaustion or lack of cooperation l Fetal indications l Nonreassuring fetal heart tracing Prolonged Second stage of labor Failure to progress in second stage of labor l l l 12
Relative contraindications for vacuum Extraction l l l l Operator inexperience Fetal prematurity (<34 wks of gestation) Fetal scalp trauma Unengaged head Incomplete cervical dilation Uncertain fetal head position Active bleeding or suspected fetal coagulation defects Suspected macrosomia Inability to achieve proper application Prior failed forceps delivery Nonvertex presentation or other malpresentation Cephalopelvic disproportion Delivery requiring rotation or excessive traction Inadequate anesthesia 13
OBSTETRIC FORCEPS Anatomy of Forceps -Handle -Shank -Lock -Blade 14
forceps have four potential actions: 1. Correction of deflexion, asynclitism, or positional abnormalities of the fetal head that impedes or retards descent, rotation, and accommodation within the pelvis. 2. Extraction, which includes augmenting or replacing the expulsive force generated by uterine contractions and voluntary pushing. 15
3. Reduction of the friction between the fetal head and the birth canal. 4. Transient, artificial enlargement of the soft tissue of the birth canal which reduces the resistance of the outlet. 16
Classification of forceps deliveries Outlet forceps: 1. Scalp is visible at the introitus without separating labia 2. Fetal skull has reached pelvic floor 3. Sagittal suture is in AP diameter or right or left OA or OP position 4. Fetal head is at or on perineum 5. Rotation does not exceed 45 degrees Low forceps: Leading point of fetal skull is at station = or >_2 cm and not on the pelvic floor a. Rotation = or <45 degrees (left or right OA to OA, or left or right OP to OP) b. Rotation >45 degrees Midlerceps: Station above +2 cm but head engaged 17
Indications for operative vaginal delivery Standard indications: apply to the patient in whom the fetal head is engaged and the cervix is fully dilated: 1. Delayed second stage: 2. Suspicion of immediate or potential fetal compromise. 3. Elective shortening of the second state for maternal and fetal benefit 18
Indications for operative vaginal delivery Special indications: 1. Delayed second stage due to malposition or asynclitism of the fetal head where there may be correctable borderline disproportion due to the abnormal head position. 2. Prolapse of the umbilical cord at complete dilation. 19
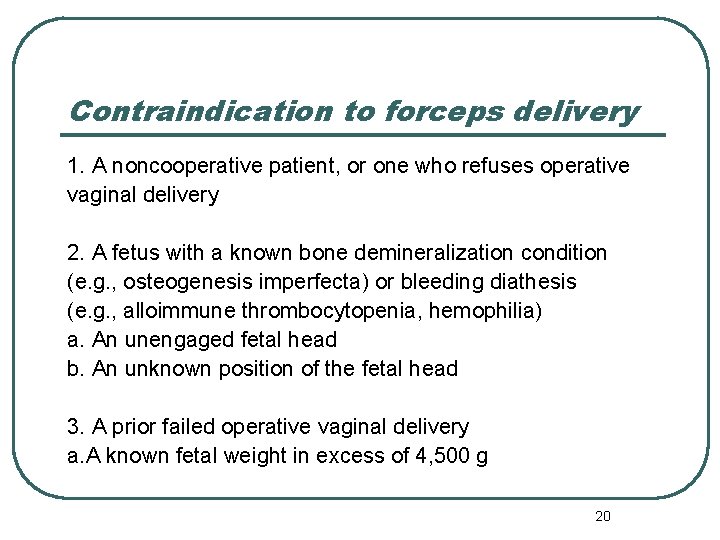
Contraindication to forceps delivery 1. A noncooperative patient, or one who refuses operative vaginal delivery 2. A fetus with a known bone demineralization condition (e. g. , osteogenesis imperfecta) or bleeding diathesis (e. g. , alloimmune thrombocytopenia, hemophilia) a. An unengaged fetal head b. An unknown position of the fetal head 3. A prior failed operative vaginal delivery a. A known fetal weight in excess of 4, 500 g 20
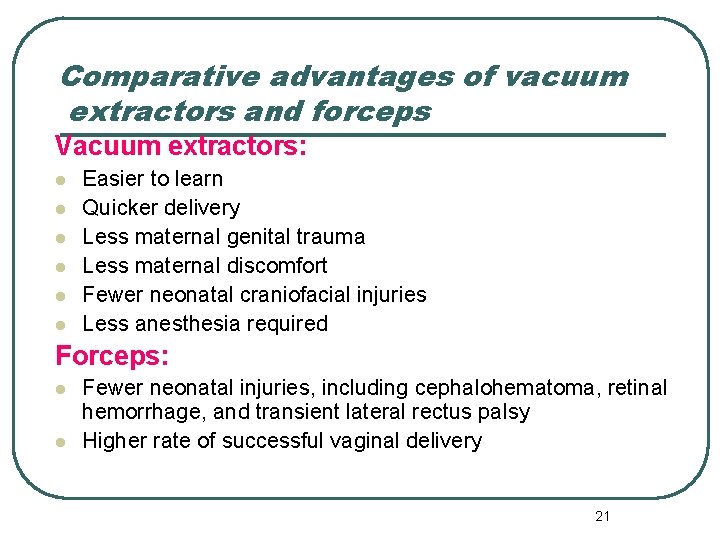
Comparative advantages of vacuum extractors and forceps Vacuum extractors: l l l Easier to learn Quicker delivery Less maternal genital trauma Less maternal discomfort Fewer neonatal craniofacial injuries Less anesthesia required Forceps: l l Fewer neonatal injuries, including cephalohematoma, retinal hemorrhage, and transient lateral rectus palsy Higher rate of successful vaginal delivery 21
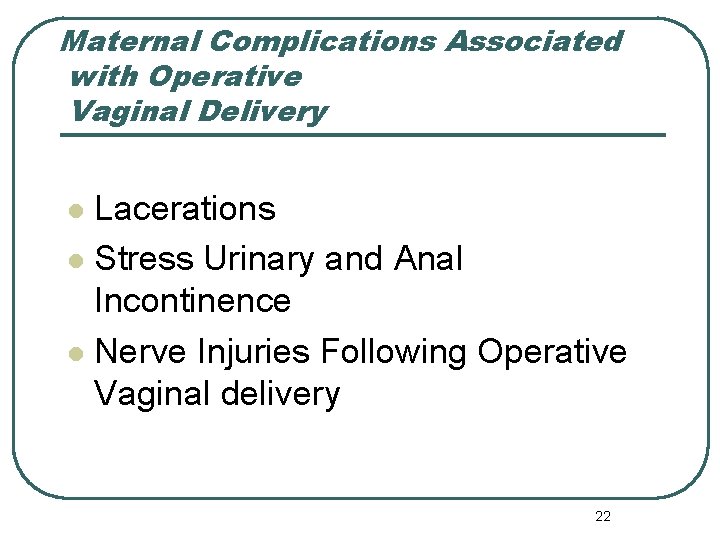
Maternal Complications Associated with Operative Vaginal Delivery Lacerations l Stress Urinary and Anal Incontinence l Nerve Injuries Following Operative Vaginal delivery l 22
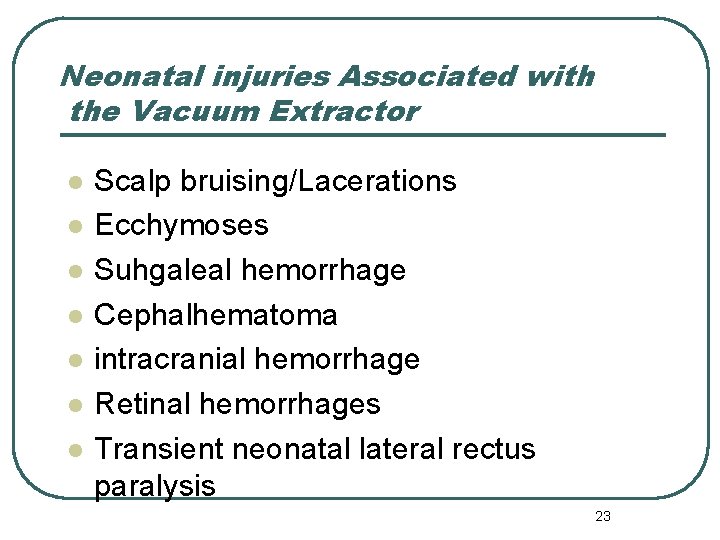
Neonatal injuries Associated with the Vacuum Extractor l l l l Scalp bruising/Lacerations Ecchymoses Suhgaleal hemorrhage Cephalhematoma intracranial hemorrhage Retinal hemorrhages Transient neonatal lateral rectus paralysis 23
Vacuum extraction is associated with a higher rate of neonatal jaundice than is spontaneous delivery or forceps procedures, and this is possibly related to the higher rate of cephalhematoma. 24
Neonatal Injuries Associated with Forceps l l l Superficial Scalp and Facial Markings Facial Nerve Injury Cephalhematoma Retinal Hemorrhage Corneal Abrasions/External Ocular Trauma Intracranial Bleeds 25
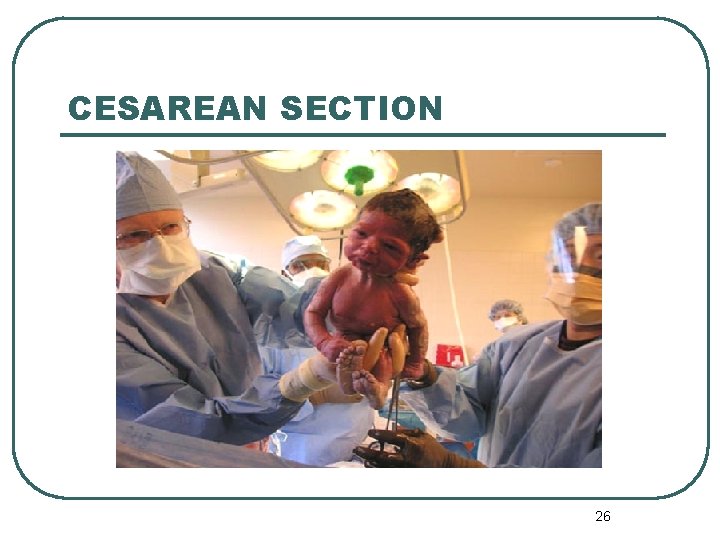
CESAREAN SECTION 26
Cesarean Delivery Cesarean section: delivery of a viable fetus through an incision in the abdominal wall (laparotomy) and the uterus (hysterotomy) Cesarean delivery has played a major role in lowering both maternal and perinatal morbidity and mortality rates during the past century 27
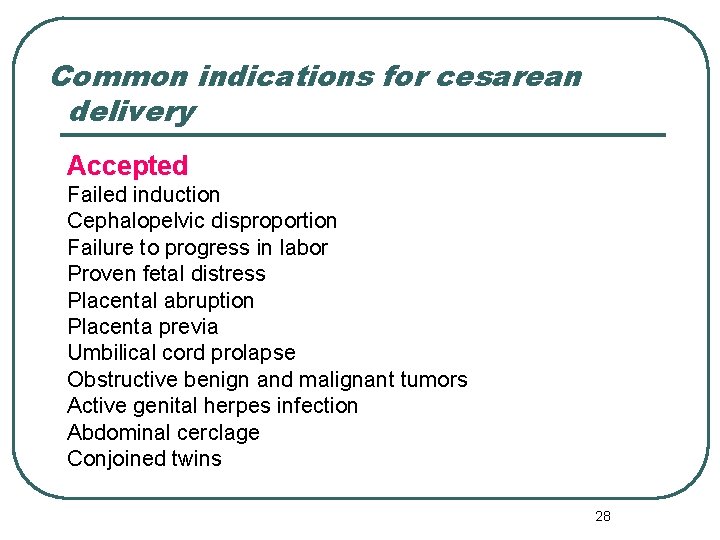
Common indications for cesarean delivery Accepted Failed induction Cephalopelvic disproportion Failure to progress in labor Proven fetal distress Placental abruption Placenta previa Umbilical cord prolapse Obstructive benign and malignant tumors Active genital herpes infection Abdominal cerclage Conjoined twins 28
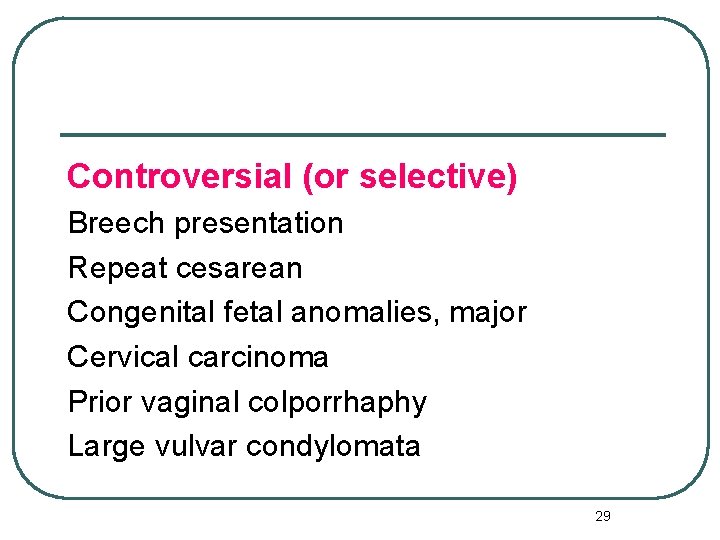
Controversial (or selective) Breech presentation Repeat cesarean Congenital fetal anomalies, major Cervical carcinoma Prior vaginal colporrhaphy Large vulvar condylomata 29
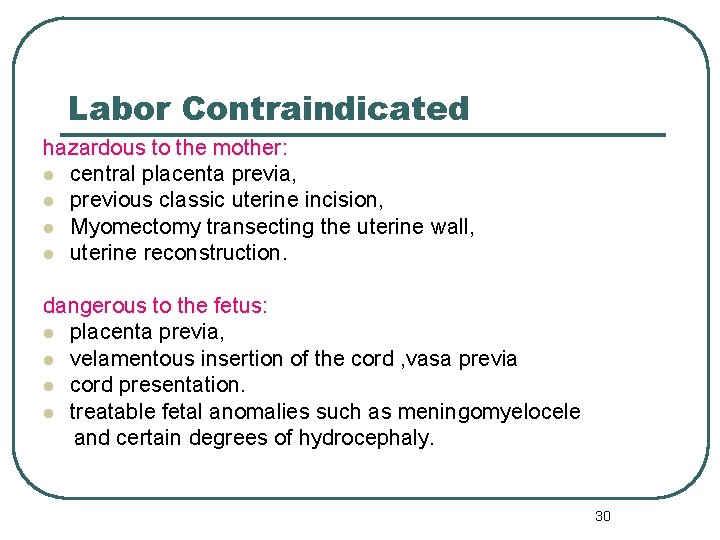
Labor Contraindicated hazardous to the mother: l central placenta previa, l previous classic uterine incision, l Myomectomy transecting the uterine wall, l uterine reconstruction. dangerous to the fetus: l placenta previa, l velamentous insertion of the cord , vasa previa l cord presentation. l treatable fetal anomalies such as meningomyelocele and certain degrees of hydrocephaly. 30
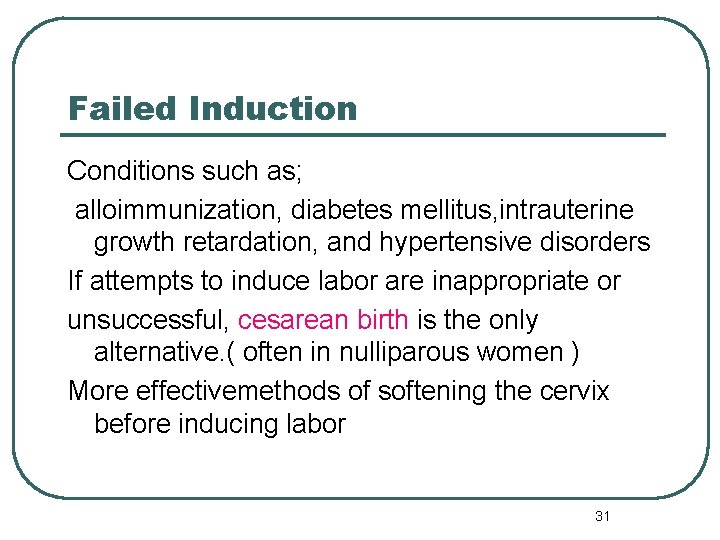
Failed Induction Conditions such as; alloimmunization, diabetes mellitus, intrauterine growth retardation, and hypertensive disorders If attempts to induce labor are inappropriate or unsuccessful, cesarean birth is the only alternative. ( often in nulliparous women ) More effectivemethods of softening the cervix before inducing labor 31
Dystocia Mechanical problems of the uterus, fetus, or birth canal or ineffective uterine contractions that result in unsuccessful progress of labor and vaginal delivery are referred to collectively as dystocia. (failure to progress, CPD, dysfunctional labor, soft tissue tumors , abnormal fetal presentations) 32
Intrapartum Fetal Heart Rate Abnormalities Electronic fetal monitoring improves the chance of detecting fetal compromise, but its inaccuracy (false-positive rate) has also contributed to the increased number of cesarean births. Many clinicians have replaced vaginal breech deliveries with cesarean delivery to avoid the risk of intrapartum asphyxia or delivery-related trauma from head entrapment and umbilical cord prolapse. 33
Maternal or Fetal Emergency Such circumstances include: severe placental abruption, hemorrhage from placenta previa, prolapse of the umbilical cord, active genital herpes, impending maternal death. 34
COMPLICATIONS postpartum complications including: nonexplained fever, endometritis, wound infection, hemorrhage, aspiration, atelectasis, urinary tract infection, venous thromboembolism (up to 25%). cesarean-related maternal death rates: less than 1 per 1, 000 operations many deaths are related to an underlying maternal illness or anesthetic complications. 35
Late maternal complications -intestinal obstruction from adhesions, - dehiscence of the uterine incision in subsequent pregnancie ( more common with the classic incision ) - abnormal myometrial invasion of the placenta (accreta, increta, percreta) in subsequent pregnancies( increases with each cesarean) -cesarean hysterectomy ( placenta previa and a history of cesarean) 36
TYPES OF CESAREAN OPERATIONS -classic incision -low transverse incision -J-shaped incision -T-shaped incision (to avoid extension into the broad ligament) 37
ANESTHESIA Not candidates for spinal or epidural anesthetic techniques: -immediate delivery (fetal distress, hemorrhage, shock) - previous injury or surgery to the spine, skin infections of the lower back, or coagulopathy. Not good candidates for inhalation anesthesia: - active pulmonary disease( pneumonia or tuberculosis) - difficult intubation Choice: the urgency of delivery, patient choice, and skill of the anesthesiologist. 38
- inferior vena cava syndrome induction-to-delivery time: 5 to 15 minutes 39
Fetal maturity assessment before elective repeat cesarean delivery -FHR for 20 weeks by nonelectronic fetoscope or for 30 weeks by Doppler -36 weeks since a positive serum or urine HCG - ultrasonographic measurement of CRL (5 -11 wks) GA >39 wks -Ultrasonography ( 12 to 20 wks) GA >39 WKS 40
vaginal birth after Cesarean (VBAC) 1. One or two prior cesarean deliveries 2. Clinically adequate pelvis in relation to fetal size 3. No other uterine scars, anomalies, or previous rupture 4. Patient consent Physician capable of monitoring labor and performing an emergency cesarean delivery immediately available throughout active labor 6. Availability of anesthesia and personnel for emergency cesarean 41
Contraindications to VBAC 1. Prior classic or T-shaped incision or other transmural uterine surgery 2. Contracted pelvis 3. Medical or obstetric complication that precludes vaginal delivery 4. Patient refusal 5. Inability to immediately perform emergency cesarean because of unavailable surgeon or anesthesia personnel, inadequate staff or facility 42
Towards a safe motherhood 43
 Lower segment caesarean section ppt
Lower segment caesarean section ppt Criteria for normal vaginal delivery
Criteria for normal vaginal delivery Vacuum delivery indication
Vacuum delivery indication Advantages of ventouse over forceps
Advantages of ventouse over forceps Forceps delivery ppt
Forceps delivery ppt Cesarean hysterectomy steps
Cesarean hysterectomy steps Icd 10 fraktur clavicula
Icd 10 fraktur clavicula Nursing care for cesarean section ppt
Nursing care for cesarean section ppt Cesarean julius caesar
Cesarean julius caesar Baseball stitch classical cesarean
Baseball stitch classical cesarean Complications after cesarean section
Complications after cesarean section Sindications
Sindications Types of cesarean section
Types of cesarean section How many levels does adm have accenture
How many levels does adm have accenture Obstetrics instrument
Obstetrics instrument Vaginal hydrocele
Vaginal hydrocele Vulvar intraepithelial neoplasia (vin) grade 3
Vulvar intraepithelial neoplasia (vin) grade 3 Processus vaginalis
Processus vaginalis Anel vaginal
Anel vaginal Tipos de himem
Tipos de himem Menopause definition
Menopause definition Sistem penghantaran obat vaginal
Sistem penghantaran obat vaginal Vaginal discharge
Vaginal discharge What is receptive vaginal sex
What is receptive vaginal sex Hrt side effects
Hrt side effects Vaginal ring
Vaginal ring Tricomoniasis sintomas
Tricomoniasis sintomas Speculum
Speculum Schlussel urology
Schlussel urology Vaginal neoplasia
Vaginal neoplasia Mamas turgidas
Mamas turgidas Anel vaginal
Anel vaginal Simpexioni
Simpexioni Bivalve vaginal speculum
Bivalve vaginal speculum Dt56a side effects
Dt56a side effects Vaginal vault prolapse
Vaginal vault prolapse Bernie brenner
Bernie brenner Processus vaginalis anatomy
Processus vaginalis anatomy периниум
периниум What is vaginal ring
What is vaginal ring Vaginal bleeding
Vaginal bleeding Sterile gloves
Sterile gloves Sims anterior vaginal wall retractor
Sims anterior vaginal wall retractor Vaginal discharge
Vaginal discharge