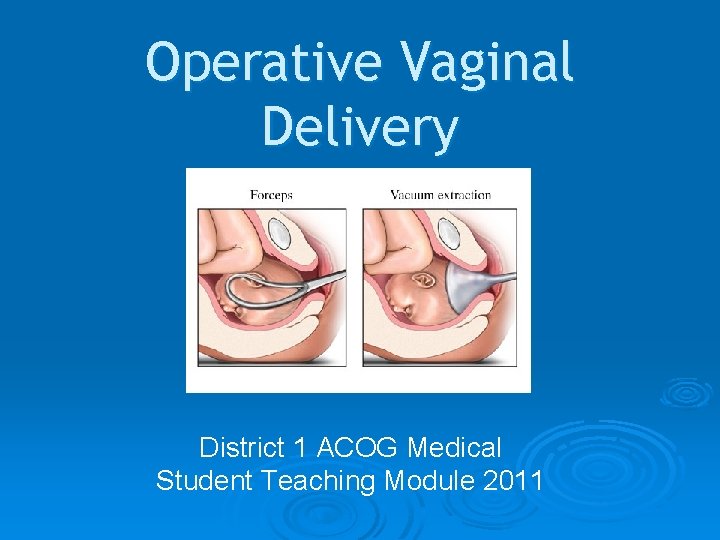
Operative Vaginal Delivery District 1 ACOG Medical Student
- Slides: 14
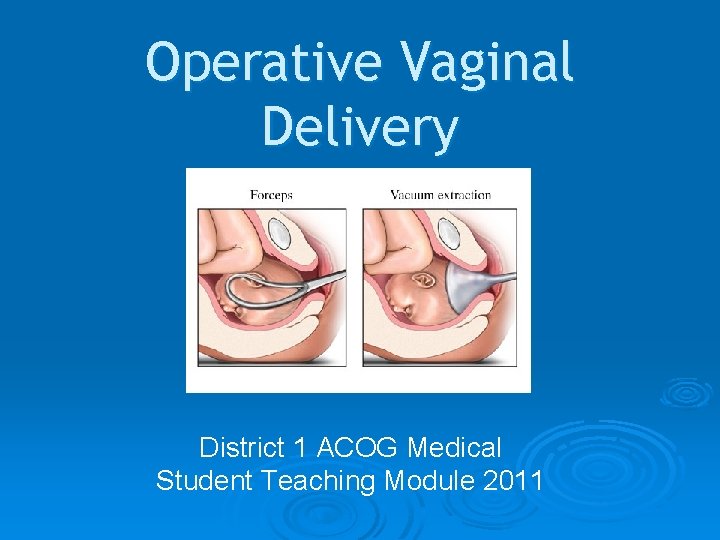
Operative Vaginal Delivery District 1 ACOG Medical Student Teaching Module 2011
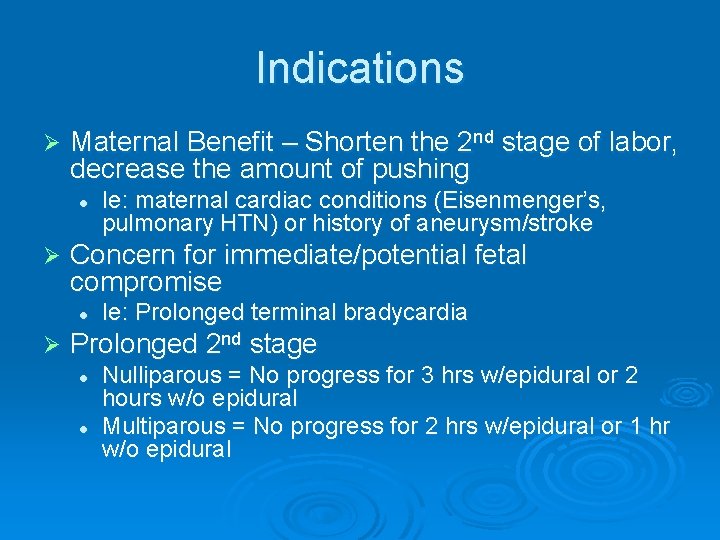
Indications Ø Maternal Benefit – Shorten the 2 nd stage of labor, decrease the amount of pushing l Ø Concern for immediate/potential fetal compromise l Ø Ie: maternal cardiac conditions (Eisenmenger’s, pulmonary HTN) or history of aneurysm/stroke Ie: Prolonged terminal bradycardia Prolonged 2 nd stage l l Nulliparous = No progress for 3 hrs w/epidural or 2 hours w/o epidural Multiparous = No progress for 2 hrs w/epidural or 1 hr w/o epidural
Operative Vaginal Delivery Ø Incidence: 4. 5% of vaginal deliveries Ø Forceps deliveries = 0. 8% Ø Vacuum deliveries = 3. 7% Ø Success Rate = 99% l Reflects appropriate choice of candidates
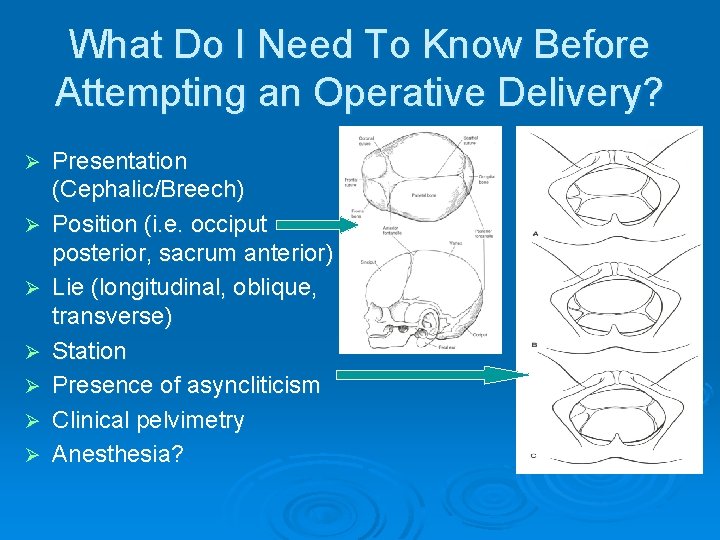
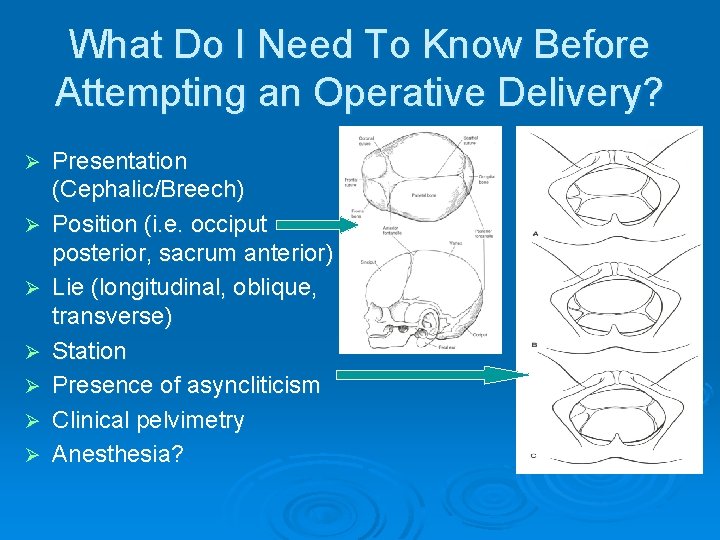
What Do I Need To Know Before Attempting an Operative Delivery? Ø Ø Ø Ø Presentation (Cephalic/Breech) Position (i. e. occiput posterior, sacrum anterior) Lie (longitudinal, oblique, transverse) Station Presence of asyncliticism Clinical pelvimetry Anesthesia?
Contraindications Ø GA < 34 weeks (contraindication for vacuum due to risk of fetal IVH) Ø Known bone demineralization condition (e. g. osteogenesis imperfecta) or bleeding disorder, ie: VWD) Ø Fetal head unengaged Ø Position of fetal head unknown
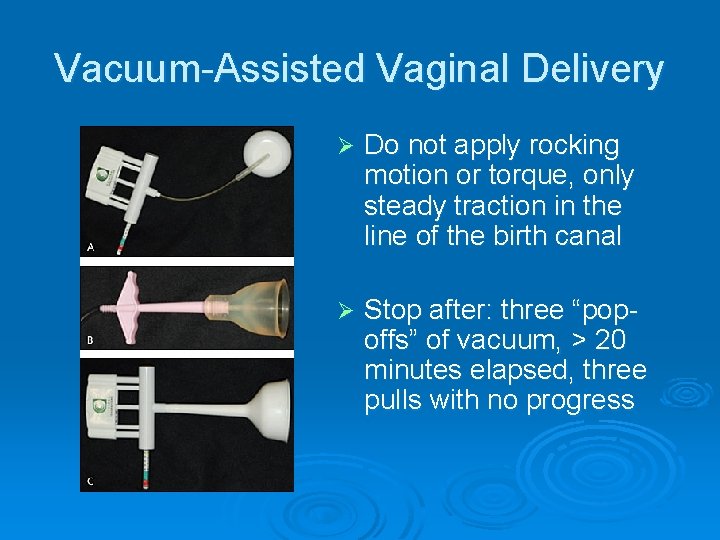
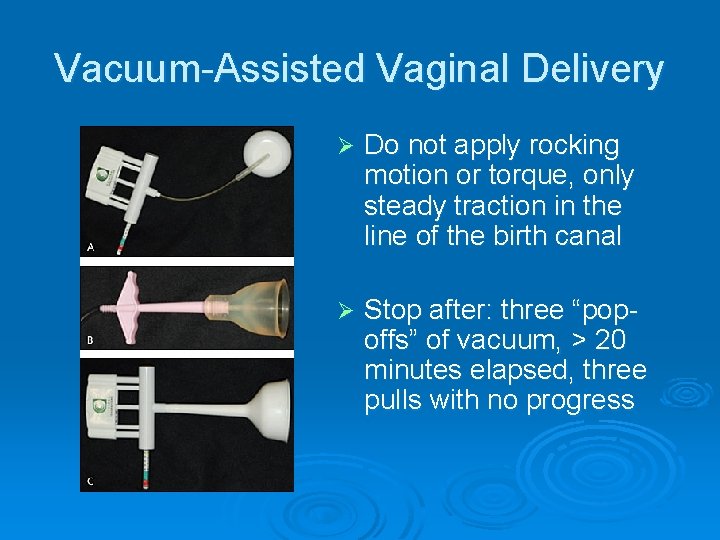
Vacuum-Assisted Vaginal Delivery Ø Do not apply rocking motion or torque, only steady traction in the line of the birth canal Ø Stop after: three “popoffs” of vacuum, > 20 minutes elapsed, three pulls with no progress
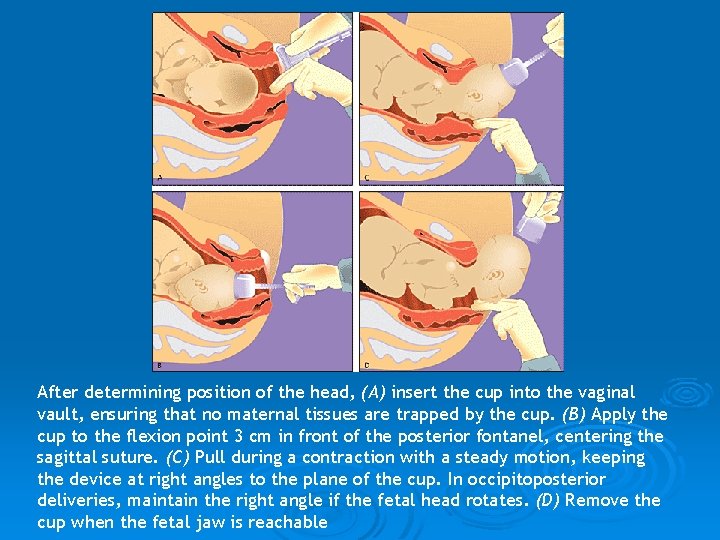
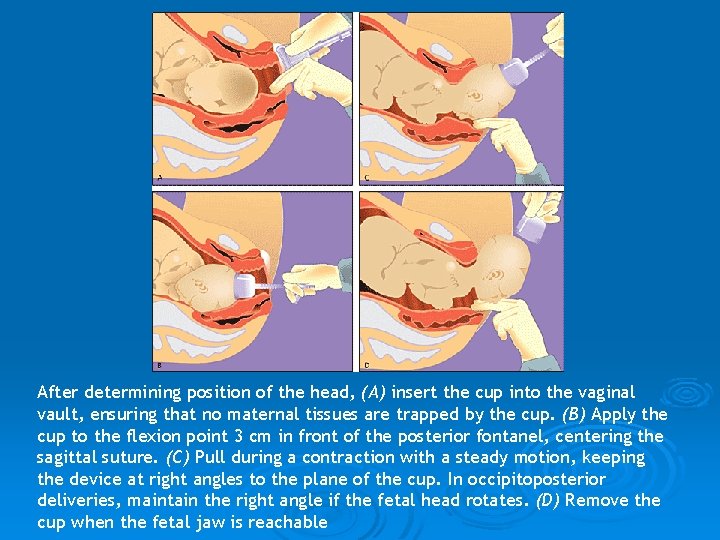
After determining position of the head, (A) insert the cup into the vaginal vault, ensuring that no maternal tissues are trapped by the cup. (B) Apply the cup to the flexion point 3 cm in front of the posterior fontanel, centering the sagittal suture. (C) Pull during a contraction with a steady motion, keeping the device at right angles to the plane of the cup. In occipitoposterior deliveries, maintain the right angle if the fetal head rotates. (D) Remove the cup when the fetal jaw is reachable
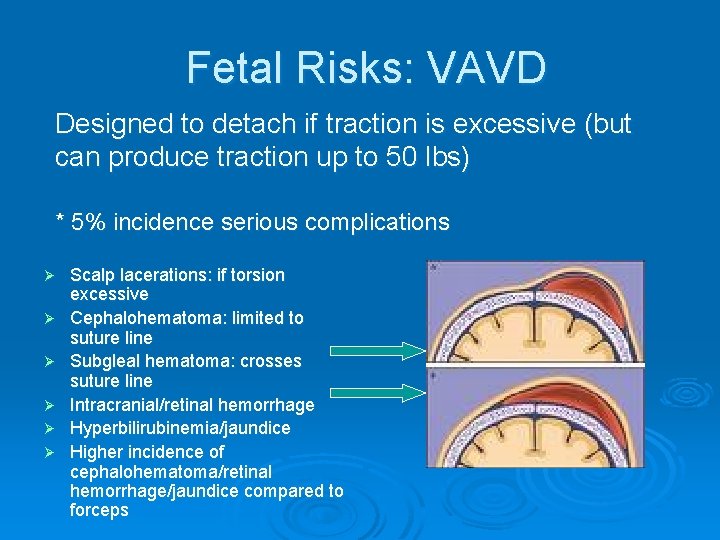
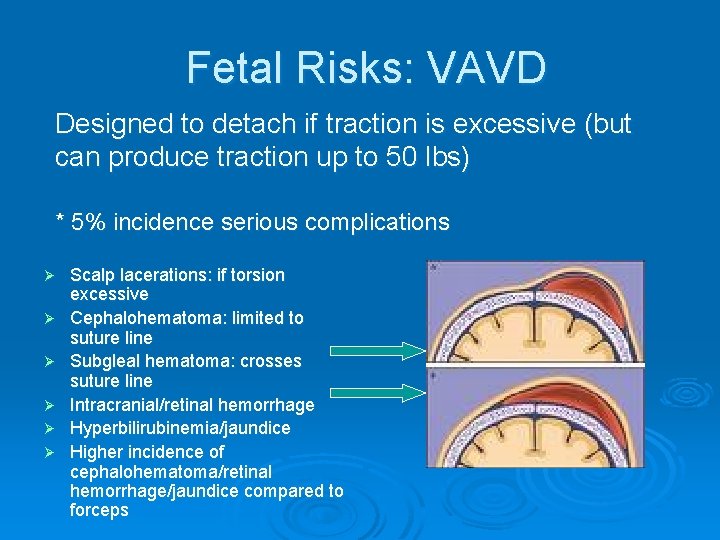
Fetal Risks: VAVD Designed to detach if traction is excessive (but can produce traction up to 50 lbs) * 5% incidence serious complications Ø Ø Ø Scalp lacerations: if torsion excessive Cephalohematoma: limited to suture line Subgleal hematoma: crosses suture line Intracranial/retinal hemorrhage Hyperbilirubinemia/jaundice Higher incidence of cephalohematoma/retinal hemorrhage/jaundice compared to forceps
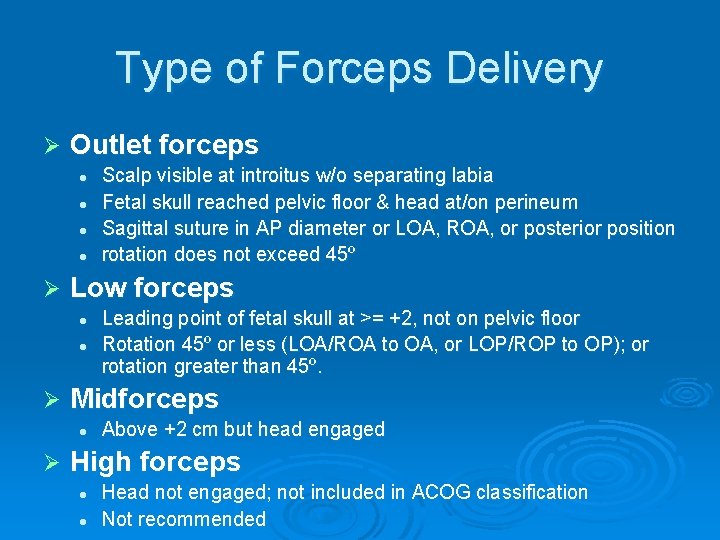
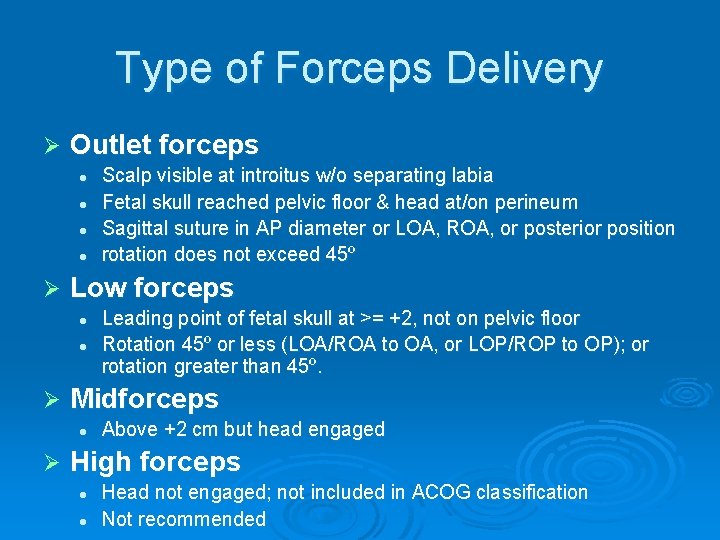
Type of Forceps Delivery Ø Outlet forceps l l Ø Low forceps l l Ø Leading point of fetal skull at >= +2, not on pelvic floor Rotation 45º or less (LOA/ROA to OA, or LOP/ROP to OP); or rotation greater than 45º. Midforceps l Ø Scalp visible at introitus w/o separating labia Fetal skull reached pelvic floor & head at/on perineum Sagittal suture in AP diameter or LOA, ROA, or posterior position rotation does not exceed 45º Above +2 cm but head engaged High forceps l l Head not engaged; not included in ACOG classification Not recommended
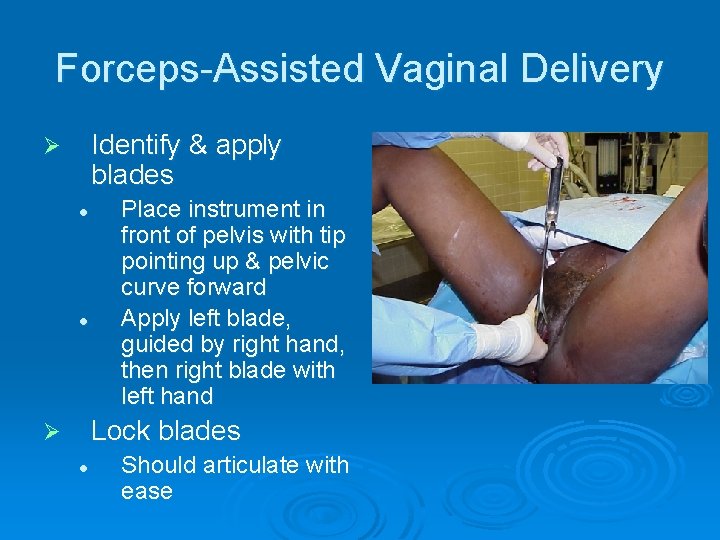
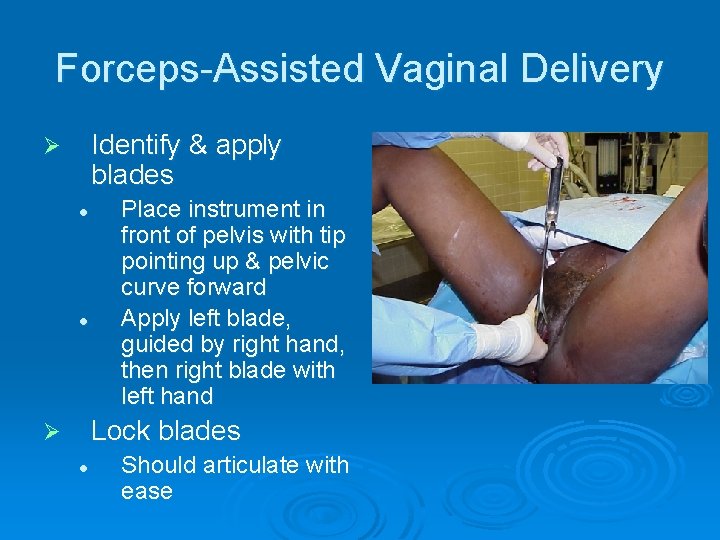
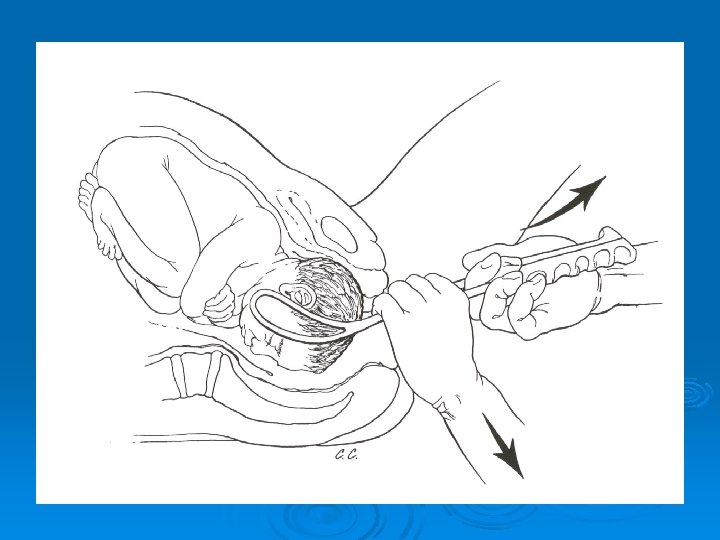
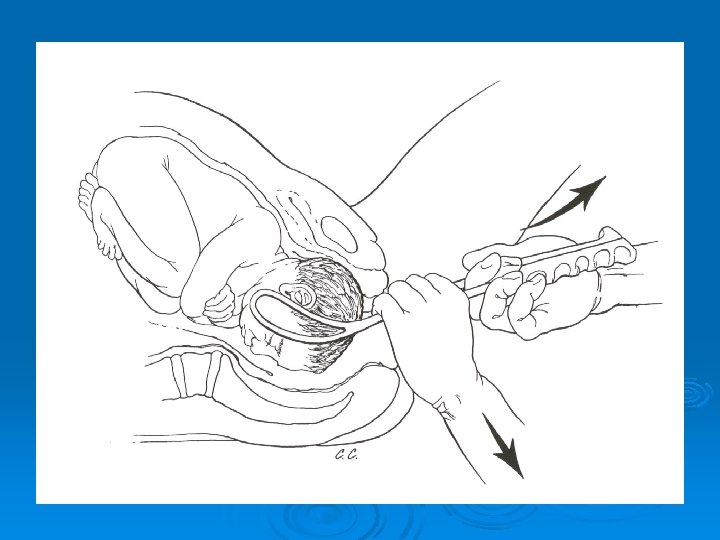
Forceps-Assisted Vaginal Delivery Identify & apply blades Ø l l Place instrument in front of pelvis with tip pointing up & pelvic curve forward Apply left blade, guided by right hand, then right blade with left hand Lock blades Ø l Should articulate with ease
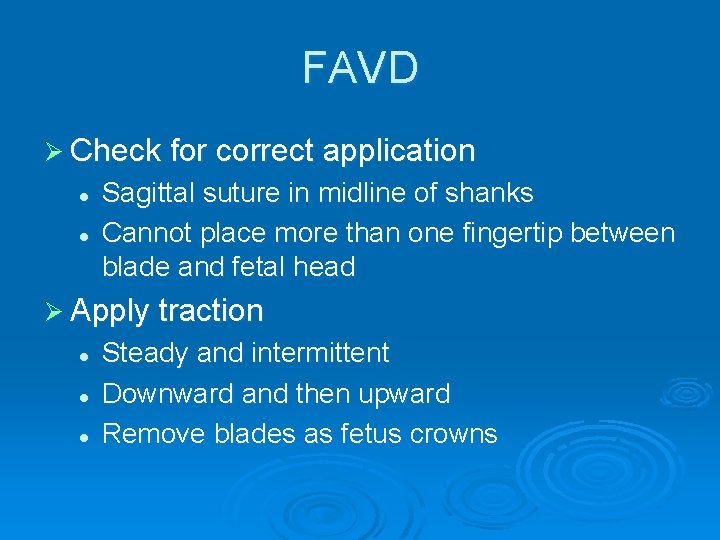
FAVD Ø Check for correct application l l Sagittal suture in midline of shanks Cannot place more than one fingertip between blade and fetal head Ø Apply traction l l l Steady and intermittent Downward and then upward Remove blades as fetus crowns
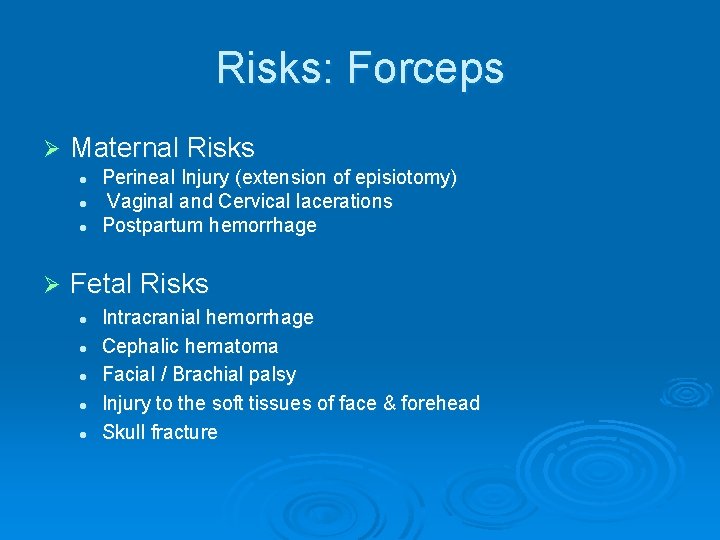
Risks: Forceps Ø Maternal Risks l l l Ø Perineal Injury (extension of episiotomy) Vaginal and Cervical lacerations Postpartum hemorrhage Fetal Risks l l l Intracranial hemorrhage Cephalic hematoma Facial / Brachial palsy Injury to the soft tissues of face & forehead Skull fracture
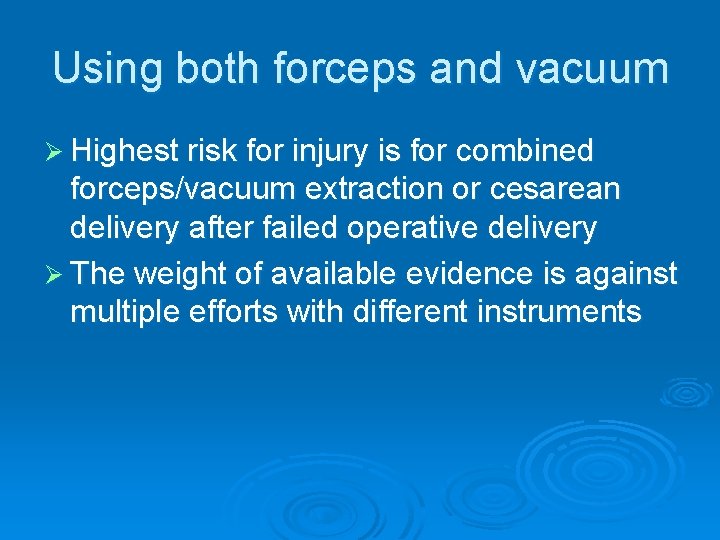
Using both forceps and vacuum Ø Highest risk for injury is for combined forceps/vacuum extraction or cesarean delivery after failed operative delivery Ø The weight of available evidence is against multiple efforts with different instruments
 Shoulder dystocia helper
Shoulder dystocia helper Criteria for normal vaginal delivery
Criteria for normal vaginal delivery Contraindications for vaginal delivery
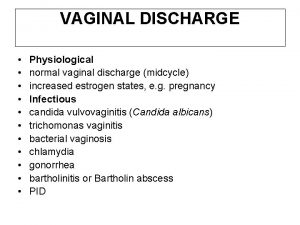
Contraindications for vaginal delivery Chlamydia symptoms bleeding
Chlamydia symptoms bleeding Palm coein acog
Palm coein acog Oligoaminios
Oligoaminios Acog flowsheet
Acog flowsheet Blighted ovum criteria acog
Blighted ovum criteria acog Acog thyroid pregnancy
Acog thyroid pregnancy Website to access accenture delivery suite
Website to access accenture delivery suite Vaginal process
Vaginal process Pathologie vaginale
Pathologie vaginale Depo-provera
Depo-provera Haivn
Haivn Structure of spermatic cord
Structure of spermatic cord