Guidelines for intraoperative care in cesarean delivery Dr





























- Slides: 97

Guidelines for intraoperative care in cesarean delivery Dr. M. Moshfeghi OBS&GYN fellowship of perinatology Shariati. Hospital , TUMS RUYAN INSTITUTE
Enhanced Recovery After Surgery Society Recommendations (ERAS) is a standardized, perioperative care program include colorectal, urologic, gynecologic, hepatobiliary surgery. American Journal of Obstetrics & Gynecology DECEMBER 2018

ERAS result clinical benefits (reductions in length of stay, complications, and readmissions) health system benefits (reduction in cost)
ERAS guideline/pathway. for scheduled and unscheduled surgery starting from 30 -60 minutes before skin incision to maternal discharge preoperative elements, intraoperative elements, postoperative elements

Specifics of the intraoperative care prophylactic antibiotics before CS appropriate Pt warming intraoperatively blunt expansion of the transverse uterine hysterotomy skin closure with subcuticular sutures delayed cord clamping.
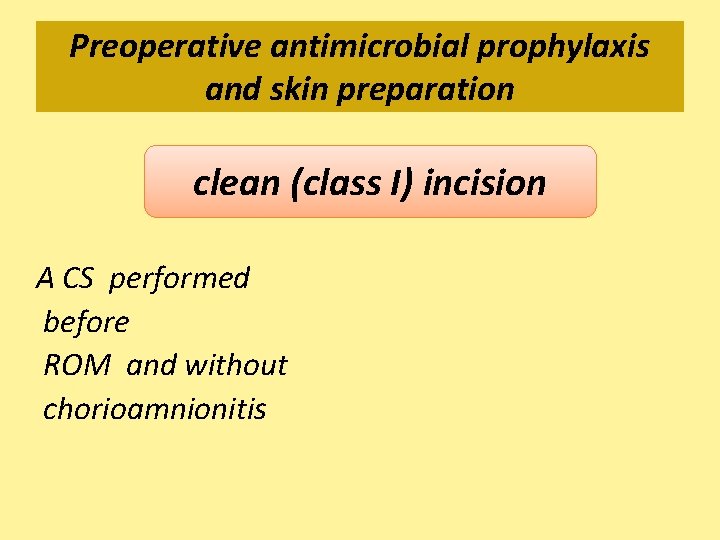
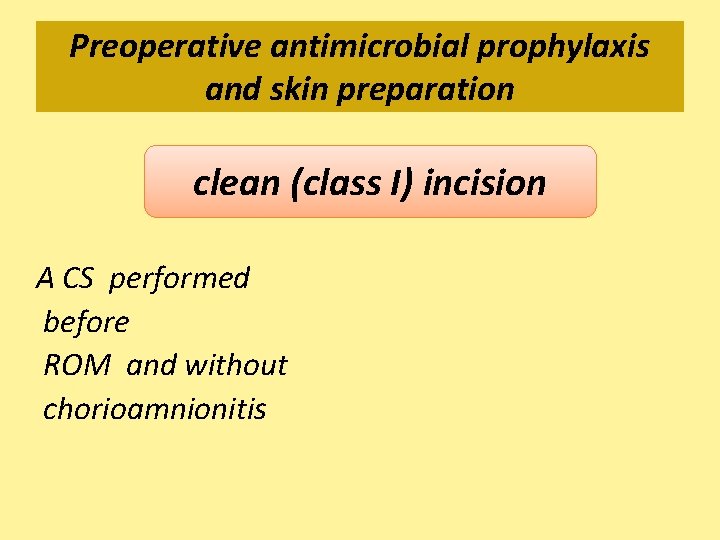
Preoperative antimicrobial prophylaxis and skin preparation clean (class I) incision A CS performed before ROM and without chorioamnionitis
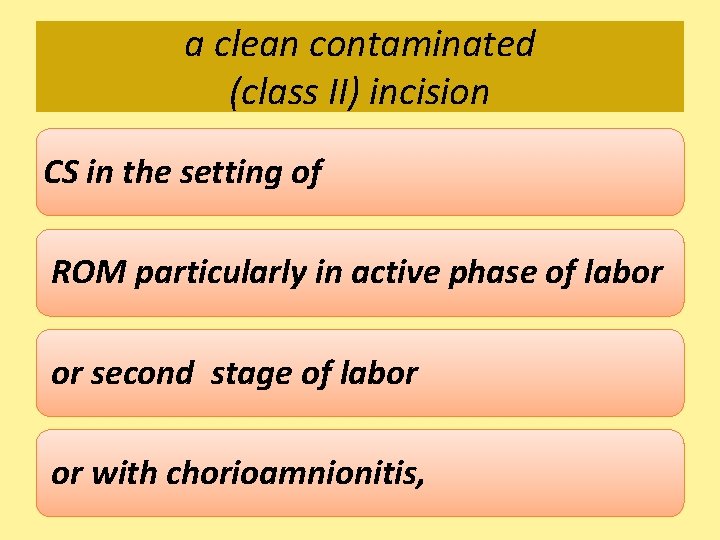
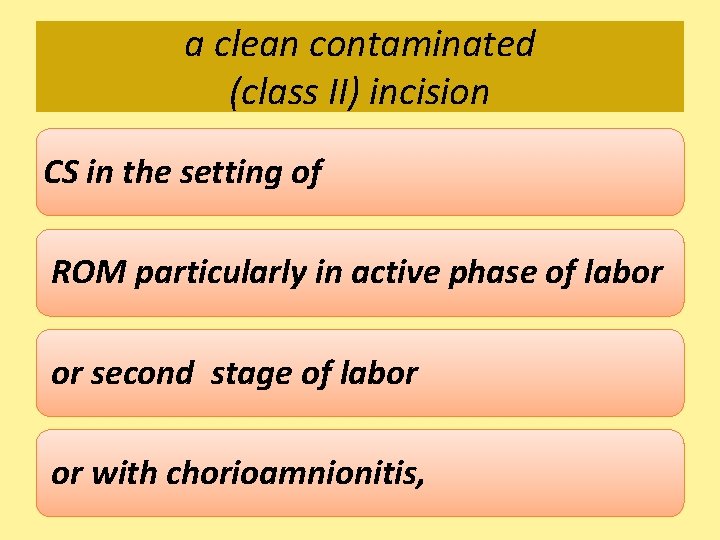
a clean contaminated (class II) incision CS in the setting of ROM particularly in active phase of labor or second stage of labor or with chorioamnionitis,
contaminated (class III) incisions at least, some of these latter incisions are contaminated (class III) incisions.
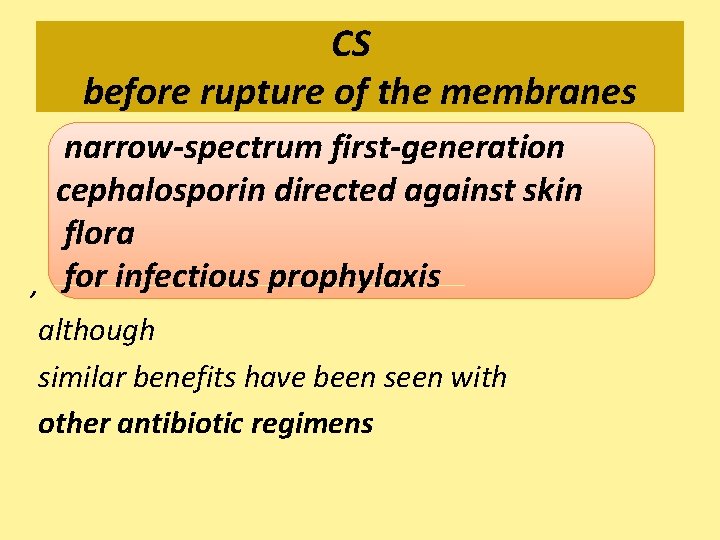
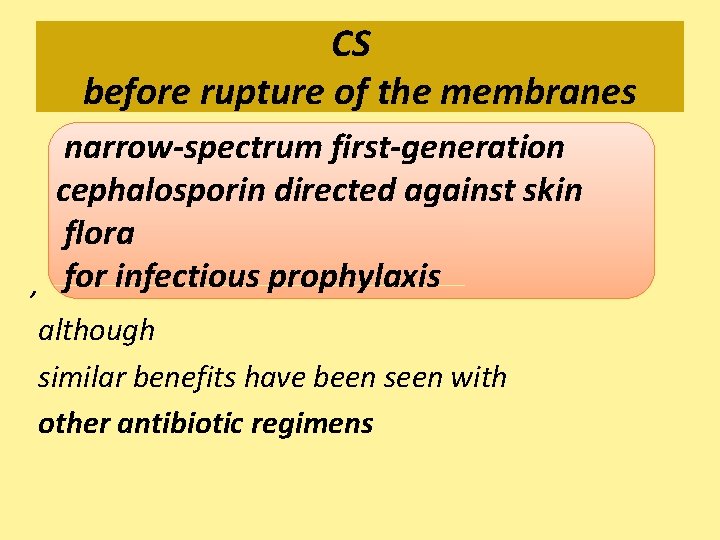
CS before rupture of the membranes narrow-spectrum first-generation cephalosporin directed against skin flora , for infectious prophylaxis although similar benefits have been seen with other antibiotic regimens

TIME fetal exposure, antibiotics were often given after cord clamping. it is now recommended to give the antibiotics 30 -60 min before CS when possible
reduction in composite maternal infectious morbidity women who received preoperative prophylactic antibiotics as compared with women who received prophylactic antibiotics at the time of cord clamping
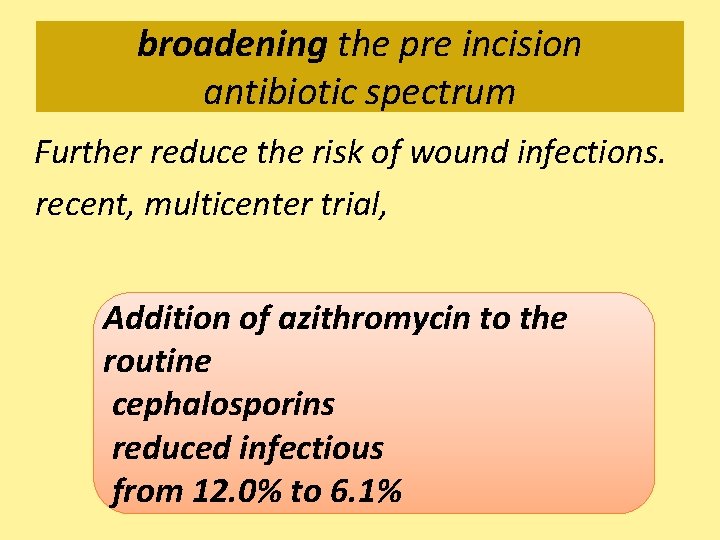
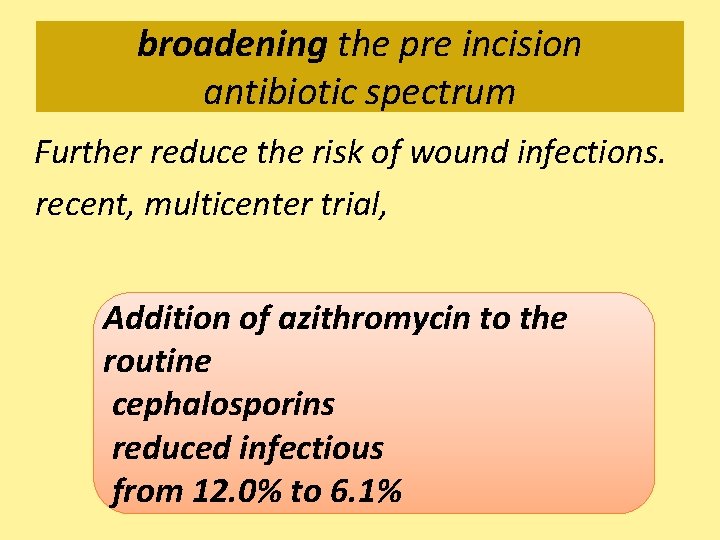
broadening the pre incision antibiotic spectrum Further reduce the risk of wound infections. recent, multicenter trial, Addition of azithromycin to the routine cephalosporins reduced infectious from 12. 0% to 6. 1%
drapes use of antibiotic infused drapes without adequate evidence to support routine use
Obese women increased risk of wound complications and the potential of higher blood volume for the antibiotic distribution.

obese women no differences . between 2 -g and 3 -g dosing of cephazolin further evidence must be collected before increased dosing of prophylactic antibiotics in obese women is routinely recommended.

preoperative antimicrobial prophylaxis and skin preparation 1. IV antibiotics should be administered routinely within 60 min before the CS skin incision. In all women, a first-generation cephalosporin is recommended; in women in labor or with ruptured membranes, the addition of azithromycin additional reduction in postoperative infections. Strong
Chlorhexidine-alcohol OR aqueous povidone-iodine Chlorhexidinealcohol is preferred to aqueous povidone-iodine cleansing before CS (evidence level: low/recommendation grade: strong).
Vaginal preparation povidine-iodine solution should be considered for the reduction of Post CS infections. Weak
Vaginal preparation antimicrobial vaginal preparation with a povidone-iodine before CS in women in labor or with rupture of membranes reduces the risk of infectious complications evidence level: moderate/grade: weak
Wound preparation Even before the hospital admission for scheduled CS , it is recommended shower with an antimicrobial soap if possible
Pre- and intraoperative anesthetic management Regional anesthesia is the preferred for CS as part of an enhanced recovery protocol strong
general anesthesia higher maternal blood loss greater potential for postoperative sedation,
spinal and epidural anesthesia Outcomes are similar the onset time for an effective block is shorter incidence of intraoperative pain is lower for spinal than for epidural anesthesia
Combined spinal epidural anesthesia rapid motor recovery than spinal anesthesia the presence of an epidural catheter provides a capability to extend or prolong an inadequate spinal block
intrathecal morphine improved postoperative analgesia But the risk of side-effects (nausea, vomiting, and pruritis) increases with the dosage used optimal dose is not established.
Prevention of intraoperative hypothermia Perioperative hypothermia 50 -80% of patients who undergo spinal anesthesia for CS
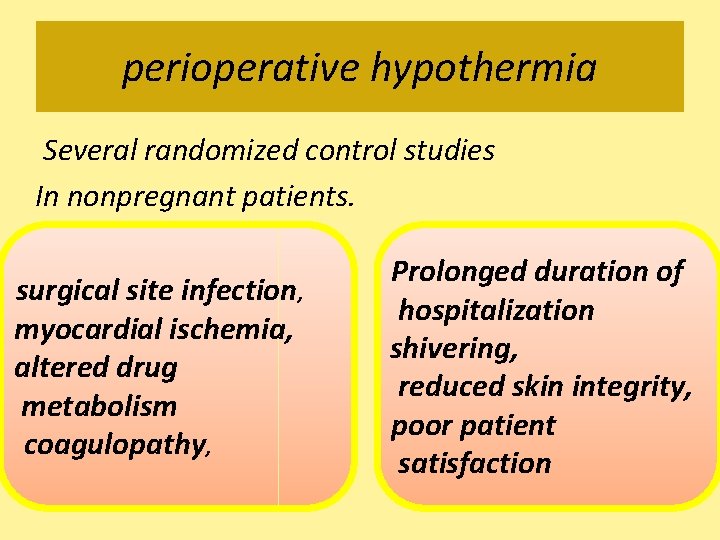
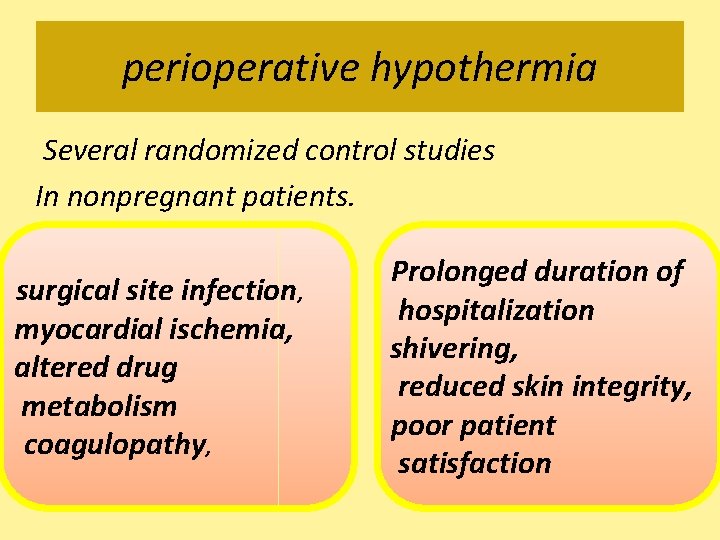
perioperative hypothermia Several randomized control studies In nonpregnant patients. surgical site infection, myocardial ischemia, altered drug metabolism coagulopathy, Prolonged duration of hospitalization shivering, reduced skin integrity, poor patient satisfaction

Hypothermia adverse effects on neonates, such as temperature, p. H umbilical , Apgar score
operating room temperature 23. 0 C resulted in significantly lower maternal hypothermia when compared with the operating room temperature at 20. 0 C.
1. Appropriate patient temperature monitoring is needed to apply warming devices and avoid hypothermia (evidence level: low/recommendation grade: strong). Forcedair airwarming, intravenous 2. 2. Forced fluidwarming, and andincreasingoperating fluid roomtemperatureare room allrecommendedtotopreventhypothermia all during. CS CS during (evidence level: moderate/recommendation grade: strong).
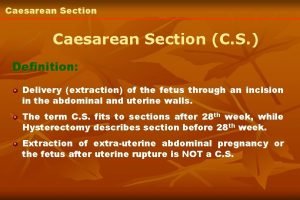
Cesarean delivery surgical techniques/ considerations Despite its worldwide spread, consensus on the most appropriate CS technique to use has not yet been reached.

Surgical incision traditional the Pfannenstiel skin incision that is made sharply through the subcutaneous tissue, sharply through the fascia, and sharply entering the parietal peritoneum

The Kerr hysterotomy made sharply in a transverse fashion into the uterus A bladder flap commonly was created to dissect the bladder, although a recent metaanalysis does not support this being performed routinely


Joel-Cohen incision The. subcutaneous tissue is left undisturbed apart from the midline, and the abdominal fascia is incised only at the midline in a transvers fashion. The rectus sheath is separated along its fibers with blunt dissection, and the rectus muscles are separated by pulling. The parietal peritoneum is opened digitally at the upper level of the intermuscular space and stretched in a cranialcaudal direction. A small transverse incision is made into the uterus with a scalpel, 2 cm above the vesical-uterine fold until the membranes bulge, and 2 index fingers are inserted to stretch the opening laterally
the Joel-Cohen approach has been associated with lower operative times and lower blood loss


Blunt expansion of a transverse uterine hysterotomy is recommended to reduce surgical blood loss evidence level: moderate/recommendation grade: weak.
Repair of incision The uterine incision is repaired commonly in 1 or 2 layers with a continuous unlocked suture

higher rate of uterine rupture after a previous cesarean delivery with hysterotomies closed in a single layer.
the most recent Cochrane review did not find a difference in outcomes between 1 - or 2 -layer closure
Closure of the hysterotomy in 2 layers may be associated with a lower rate of uterine rupture (evidence level: low/ recommendation grade: weak).
suture The use of a delayed absorbable monofilament (Monocryl; has been described, as has chromic catgut and Vicryl, without strong evidence to support a particular suture.
blunt vs sharp needles do not demonstrate benefit to patients In such studies, a reduction in glove perforations is seen but providers are less satisfied with blunt needles.

the visceral and parietal peritoneum Historically, were closed; , in systematic reviews, no evidence that outcomes such as intraabdominal adhesions are different Operative times are shorter leaving the peritoneum open
The peritoneum does not need to be closed because closure is not associated with improved outcomes and increases operative times (evidence level: low / recommendation grade: weak).
the rectus muscles commonly were sutured, but there is no evidence to support closure, there is concern that intramuscular sutures will tear through

The abdominal fascia is usually closed with a continuous suture, PDS or Vicryl

In women with 2 cm of subcutaneous tissue, reapproximation of that tissue layer should be performed (evidence level: moderate/recommendation grade: weak).
in women whose subcutaneous tissue is 2 cm in thickness, reapproximation with catgut or Vicryl subcutaneous drain wounds >4 cm not improve outcomes

skin closure closed with subcuticular suture in most Cases evidence level: moderate/ recommendation grade: weak) subcuticular suture rather than staples

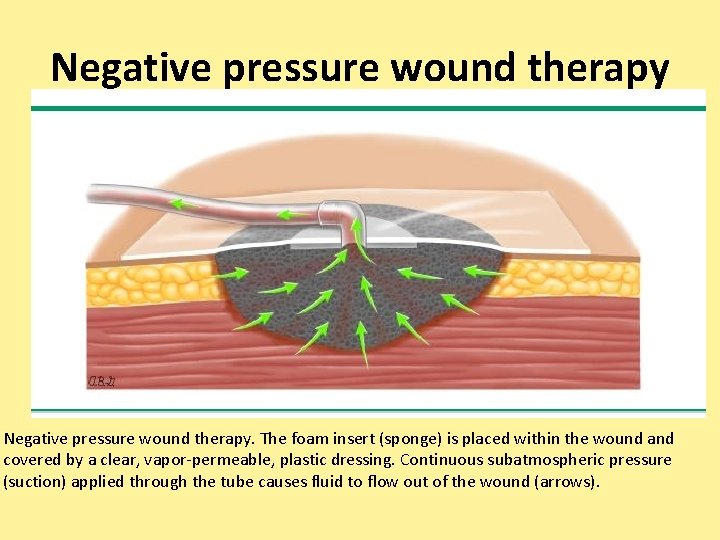
negative-pressure dressing several ongoing trials at this time; thus, although it would be reasonable for a clinician to use this technology, there is a need for additional research to fully address this question
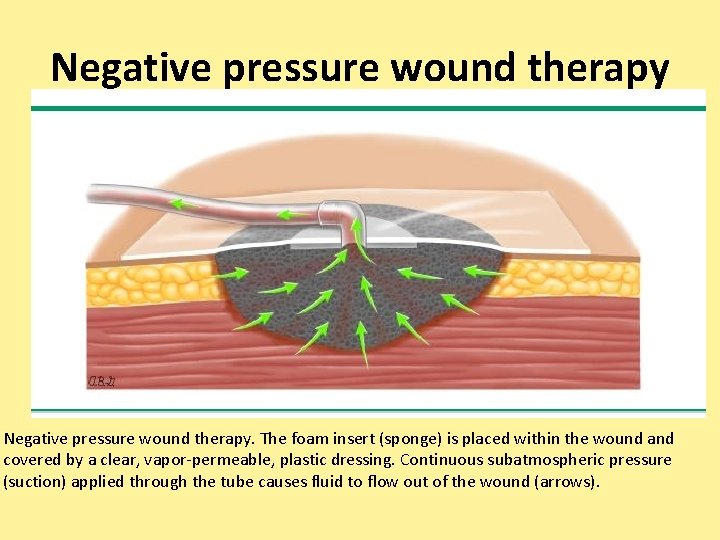
Negative pressure wound therapy. The foam insert (sponge) is placed within the wound and covered by a clear, vapor-permeable, plastic dressing. Continuous subatmospheric pressure (suction) applied through the tube causes fluid to flow out of the wound (arrows).
Perioperative fluid management Intravascular volume determines not only blood pressure but also cardiac output and oxygen delivery. optimize fetal oxygenation and prevent acidosis but also deliver nutrients and eliminate waste products from the uterine myometrium
Perioperative fluid overload increased cardiovascular work and pulmonary edema Maternal overload can result in newborn infant weight loss during the first 3 days after birth
combination of vasopressors and adequate fluid therapy effective in reducing the incidence and severity of hypotension

prophylactic phenylephrine infusions intravenous fluids alone have limited efficacy many clinicians now administer prophylactic phenylephrine infusions, which not only prevent hypertension but also reduce the risk of fetal acidosis
Preoperative and intraoperative euvolemia are important factors in patient perioperative care and appear to lead to improved maternal and neonatal outcomes after cesarean delivery (evidence level: low to moderate/recommendation grade: strong).

Neonate pathway Immediate care of the newborn infant To promote safe transition from fetal to neonatal life,
For the vigorous infant, interventions in the operating room. optimal timing of umbilical cord clamping , hypothermia prevention, facilitating onset of breathing, maternal-neonatal skin-to-skin contact
Delay of clamping of the umbilical cord for at least 1 min after term delivery decreases anemia and improves neurodevelopmental outcomes. In CS , the infant can be placed on the maternal abdomen or legs or held by the surgeon or assistant close to the level of the placenta until the umbilical cord is clamped.
Delayed cord clamping for at least 1 minute at a term delivery is recommended (evidence level: moderate/ recommendation grade: strong).

Delayed cord clamping In preterm infants at least 30 seconds less need for transfusion less IVH, and lower risk for NEC than after immediate cord clamping (evidence level: lowmoderate/ recommendation grade: strong).

Immediate cord clamping should be restricted to infants with immediate need of resuscitation or when placental circulation is not intact.

Immediate drying and covering of the infant’s head Use of exothermic heaters or open bed incubators, transwarmer mattresses, plastic wraps/bags, and caps all keep preterm infants warmer and
Body temperature should be measured maintained at between 36. 5 C and 37. 5 C after birth, through admission and stabilization (evidence level: low-moderate/ recommendation grade: strong).
stimulating for first breath or cry are recommended. 85% of babies who are born at term will initiate spontaneous respirations within 10 -30 seconds of birth; 10% will respond during drying and stimulation, 5% need some form of assisted ventilation
Routine suctioning of the airway or gastric aspiration should be avoided and used only for symptoms of an obstructive airway (by secretions or meconium; evidence level: low/ recommendation grade: strong).
Routine neonatal supplementation with room air is recommended because the use of inspired air with oxygen is not recommended and may be associated with harm (evidence level: low-moderate/ recommendation grade: strong).
immediate neonatal resuscitation In all settings that perform cesarean delivery, a capacity for immediate neonatal resuscitation is mandatory (evidence level: high/recommendation grade: strong).
the most common indication for admission to the hospital is childbirth, and themost common surgery is a cesarean delivery. With this clinical volume of obstetric surgical activity, it seems appropriate that the ERAS process be applied to this surgical care
Antibiotic prophylaxis Regimen — For all women undergoing • cesarean delivery, we administer a single dose of cefazolin in the • 60 minutes before making the skin incision, and add a single dose of azithromycin 500 mg intravenously to those in labor or with ruptured membranes.
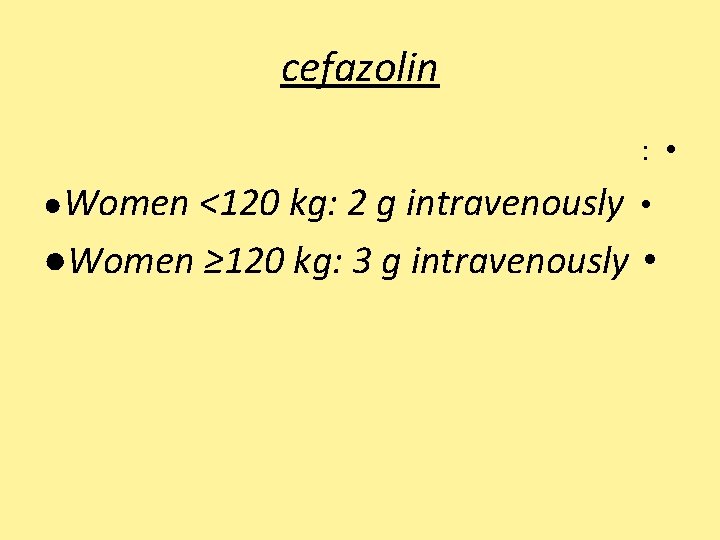
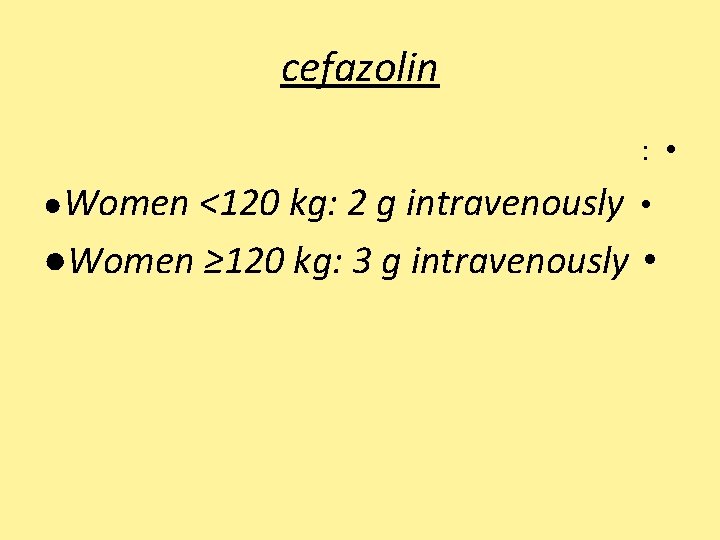
cefazolin : • ●Women <120 kg: 2 g intravenously • ●Women ≥ 120 kg: 3 g intravenously •

alter Regimen: Ampicillin-sulbactam 3 g IV • Regimen: Clindamycin 900 mg IV◊ • Vancomycin¶ 15 mg/kg IV (not to exceed 2 g • per dose) PLUS one of the following • : Gentamicin 5 mg/kg IV (if overweight or • obese, based on dosing weight)§
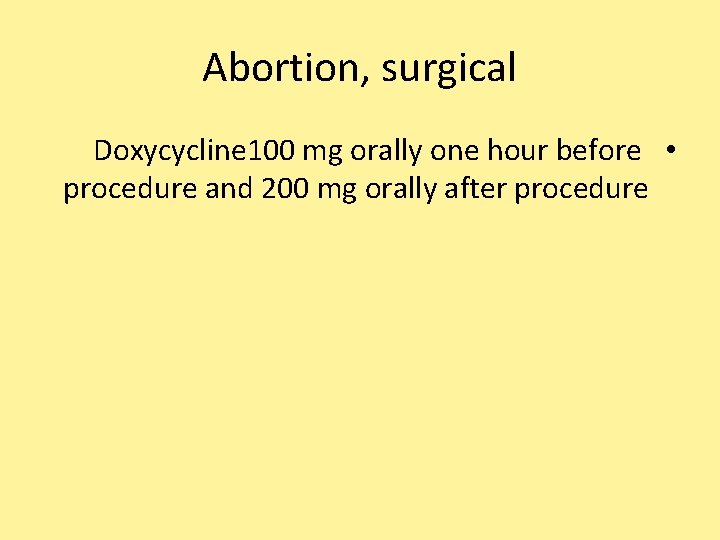
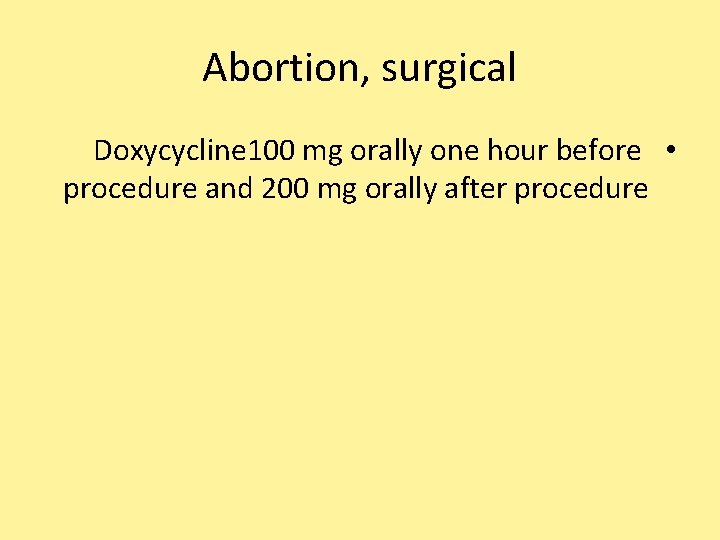
Abortion, surgical Doxycycline 100 mg orally one hour before • procedure and 200 mg orally after procedure
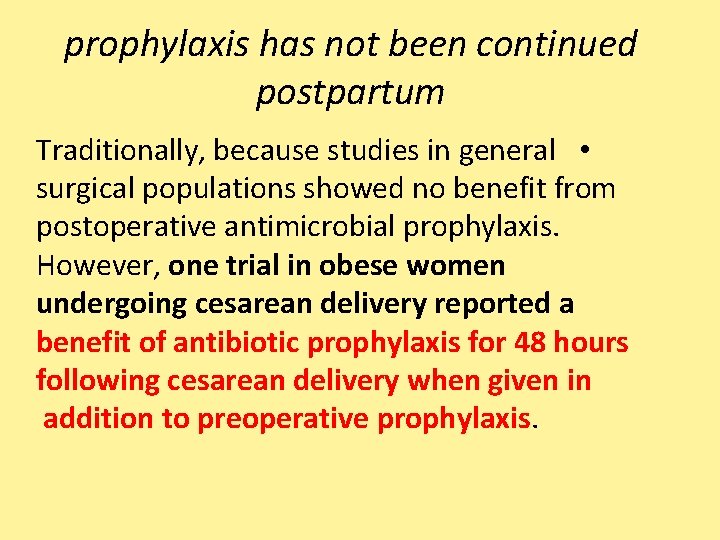
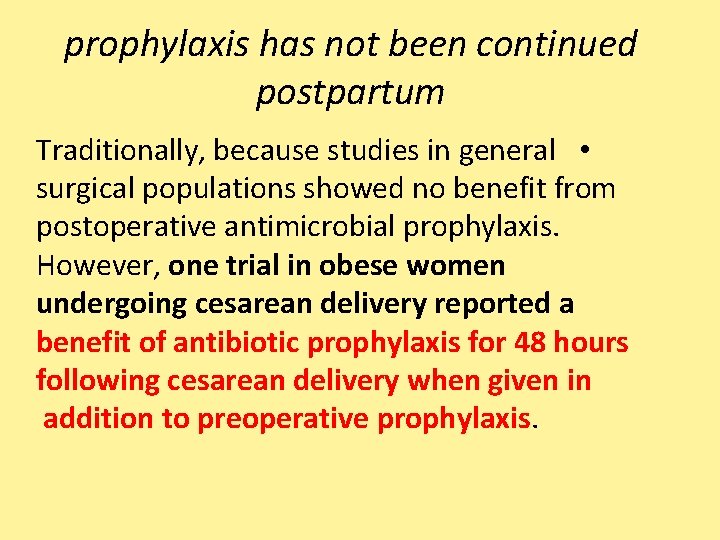
prophylaxis has not been continued postpartum Traditionally, because studies in general • surgical populations showed no benefit from postoperative antimicrobial prophylaxis. However, one trial in obese women undergoing cesarean delivery reported a benefit of antibiotic prophylaxis for 48 hours following cesarean delivery when given in addition to preoperative prophylaxis.
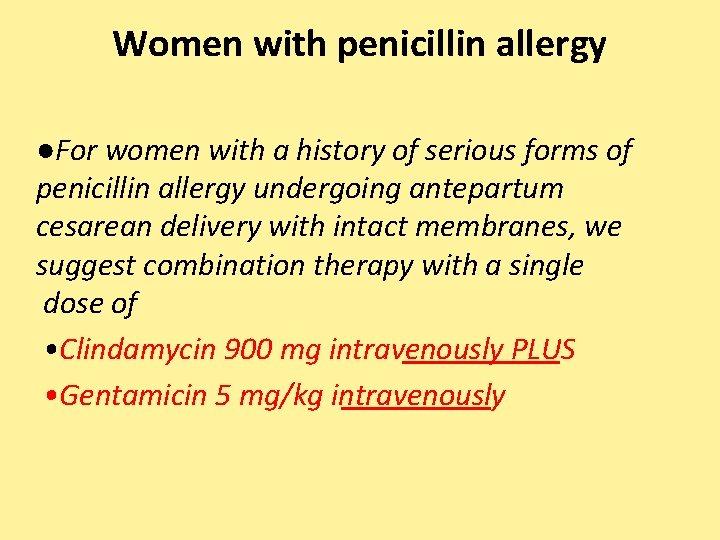
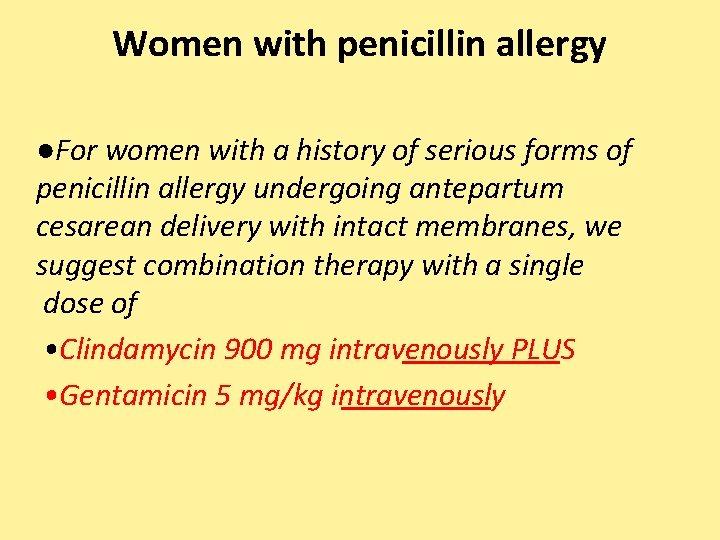
Women with penicillin allergy ●For women with a history of serious forms of penicillin allergy undergoing antepartum cesarean delivery with intact membranes, we suggest combination therapy with a single dose of • Clindamycin 900 mg intravenously PLUS • Gentamicin 5 mg/kg intravenously
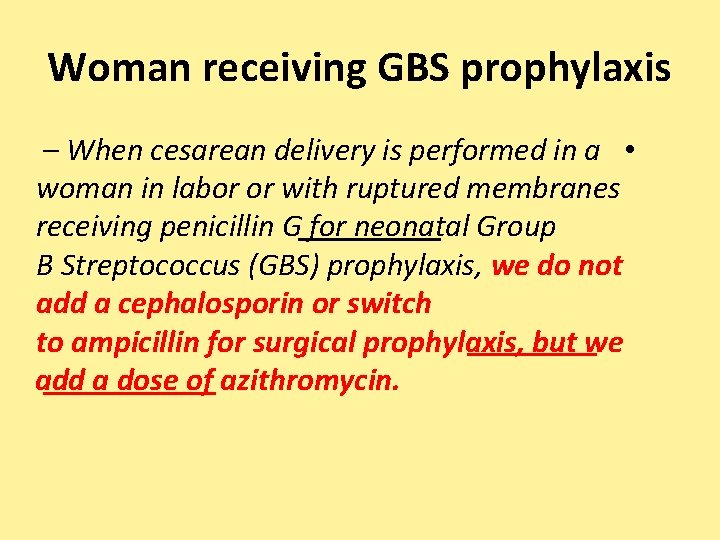
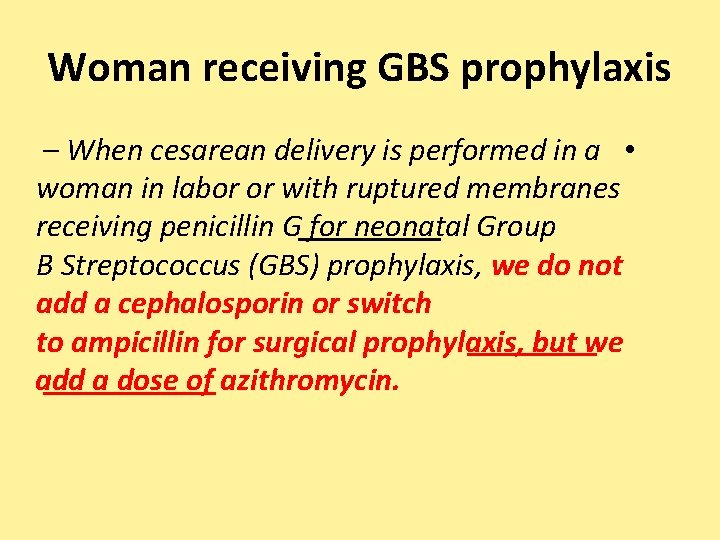
Woman receiving GBS prophylaxis – When cesarean delivery is performed in a • woman in labor or with ruptured membranes receiving penicillin G for neonatal Group B Streptococcus (GBS) prophylaxis, we do not add a cephalosporin or switch to ampicillin for surgical prophylaxis, but we add a dose of azithromycin.
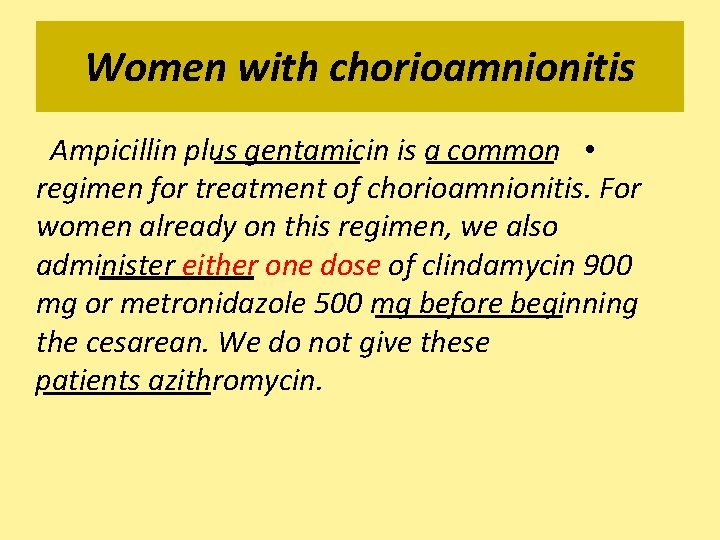
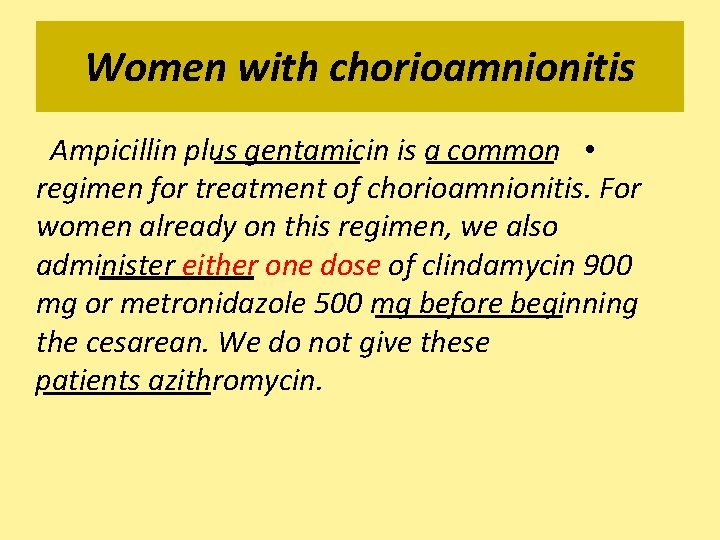
Women with chorioamnionitis Ampicillin plus gentamicin is a common • regimen for treatment of chorioamnionitis. For women already on this regimen, we also administer either one dose of clindamycin 900 mg or metronidazole 500 mg before beginning the cesarean. We do not give these patients azithromycin.
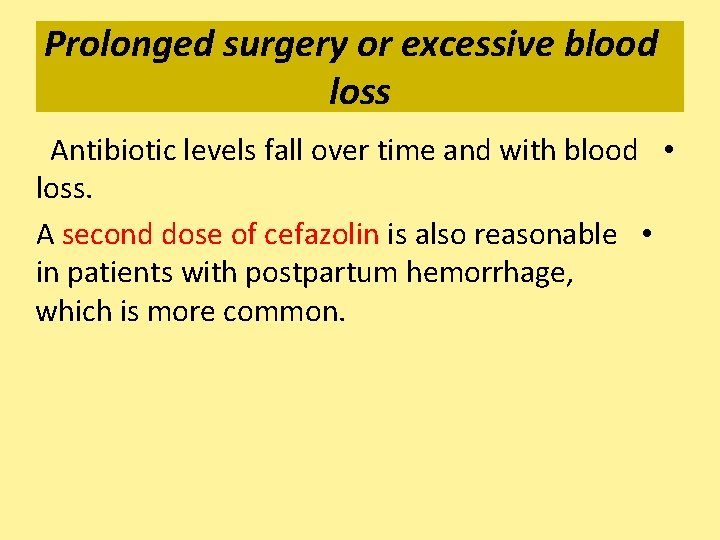
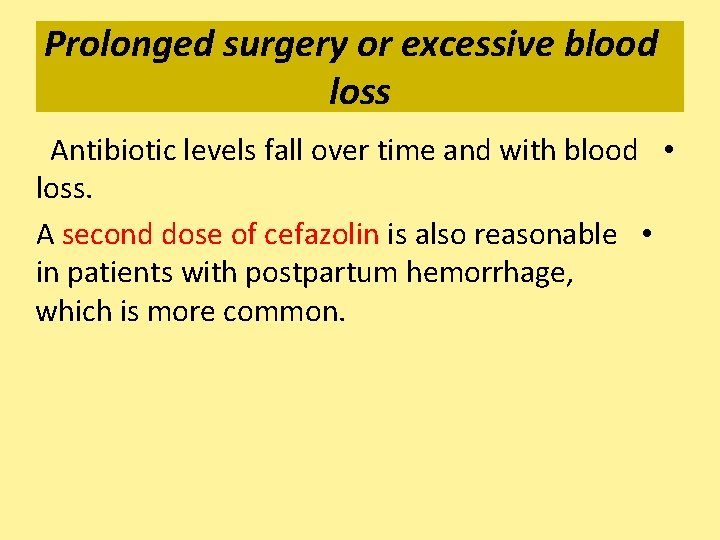
Prolonged surgery or excessive blood loss Antibiotic levels fall over time and with blood • loss. A second dose of cefazolin is also reasonable • in patients with postpartum hemorrhage, which is more common.
For all women undergoing cesarean • delivery, we suggest mechanical thromboprophylaxis
Drapes — The surgical site is draped with nonadhesive drapes in a lower rate of wound infection than adhesive drapes
Bladder catheterization maintain bladder drainage and thereby • improve visualization • during surgery and minimize bladder injury. • there is no high quality evidence that routine placement of an indwelling catheter is advantageous
Hair removal no difference in the rate of surgical site infection in those who had hair removed prior to surgery versus those who did not If hair needs to be removed, it should be clipped rather than shaved as patients who are shaved are more likely to develop surgical site infection. depilatory cream is also preferable to shaving. Clipping should be performed just before surgery
FETOPLACENTAL ASSESSMENT scheduled cesarean the value of continuous or intermittent fetal heart rate monitoring following admission is unclear If the pregnancy is high risk and has been undergoing antepartum fetal testing, it is reasonable to perform an admission nonstress test and discontinue monitoring if the tracing is reactive. If there is an excessive delay between anesthetic placement and abdominal preparation for surgery, it is appropriate to recheck the fetal heart rate during this interval.

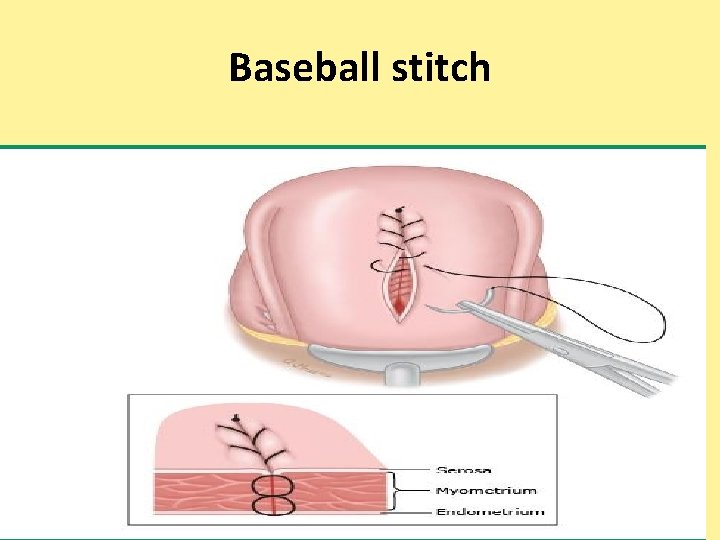
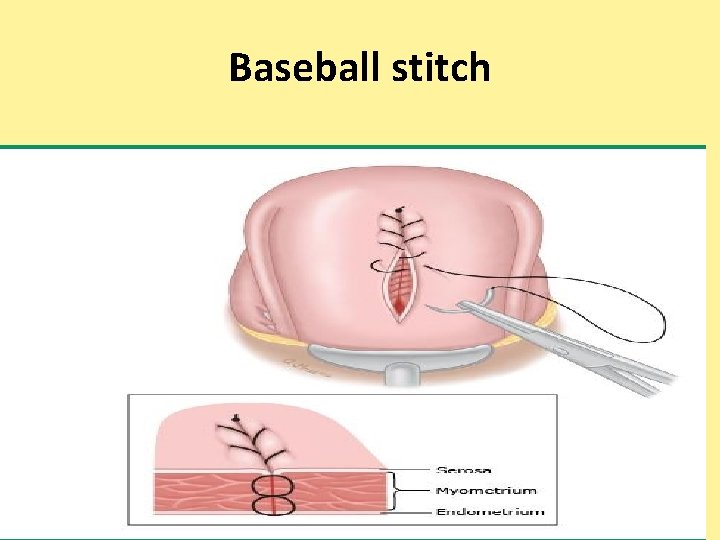
Baseball stitch


The frequency of a cesarean delivery has increased from 4. 5% in 1970 to 31. 9% in 2015 in the United States.
IV AB should be administered routinely within 60 min before CS skin incision. In all women, a first generation cephalosporin is recommended; in women in labor or with ruptured membranes, the addition of azithromycin confers additional reduction in postoperative infections (evidence level: high/recommendation grade: strong).
Chlorhexidine-alcohol is preferred to aqueous povidone-iodine solution for abdominal skin cleansing before cesarean delivery (evidence level: low/recommendation grade: strong).

Vaginal preparation with povidoneiodine solution should be considered for the reduction of infections after cesarean delivery (evidence level: moderate/recommendation grade: weak).
Maternal-Fetal Medicine Unit Network: primary indications (dystocia 37%; nonreassuring fetal heart rate 25%; abnormal fetal presentation 20%; other 15%; failed forceps or vacuum delivery ; (3%
patient core temperature is monitored poorly during neuraxial anesthesia. Skin temperature monitoring can be used during neuraxial anesthesia, but the temperatures are 2. 0 -4. 0 C less than the core temperature. Axillary temperatures can be measured if the sensor is placed over the axillary artery with arms adducted to the side
 Splint incision
Splint incision Perioperative definition
Perioperative definition Complications of c section
Complications of c section Types of cesarean section
Types of cesarean section Intraoperative cholangiogram
Intraoperative cholangiogram Perioperative vs intraoperative
Perioperative vs intraoperative Choledocholithiasis
Choledocholithiasis Complications c section
Complications c section Cesarean instruments list with pictures
Cesarean instruments list with pictures Types of cesarean section
Types of cesarean section Cesarean hysterectomy steps
Cesarean hysterectomy steps Icd 10 fraktur clavicula
Icd 10 fraktur clavicula Cesarean julius caesar
Cesarean julius caesar Baseball stitch classical cesarean
Baseball stitch classical cesarean Primary secondary tertiary health care definition
Primary secondary tertiary health care definition What is the website for accenture delivery suite?
What is the website for accenture delivery suite? Who guidelines for primary eye care
Who guidelines for primary eye care Who guidelines for primary eye care
Who guidelines for primary eye care Integrated care delivery system
Integrated care delivery system The objective for health service delivery is to
The objective for health service delivery is to Open for delivery meaning
Open for delivery meaning Introduction of health care delivery system
Introduction of health care delivery system Modular nursing method
Modular nursing method Care delivery value chain
Care delivery value chain Modular nursing advantages and disadvantages
Modular nursing advantages and disadvantages Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Påbyggnader för flakfordon
Påbyggnader för flakfordon A gastrica
A gastrica Egg för emanuel
Egg för emanuel Beräkna standardavvikelse
Beräkna standardavvikelse Rutin för avvikelsehantering
Rutin för avvikelsehantering Presentera för publik crossboss
Presentera för publik crossboss Treserva lathund
Treserva lathund Myndigheten för delaktighet
Myndigheten för delaktighet Mall debattartikel
Mall debattartikel Tack för att ni lyssnade
Tack för att ni lyssnade En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Tack för att ni lyssnade bild
Tack för att ni lyssnade bild Mall för referat
Mall för referat Tack för att ni har lyssnat
Tack för att ni har lyssnat Byggprocessen steg för steg
Byggprocessen steg för steg Karttecken brant
Karttecken brant Mitos steg
Mitos steg Rbk-mätning
Rbk-mätning Lufttryck formel
Lufttryck formel Elektronik för barn
Elektronik för barn Var 1721 för stormaktssverige
Var 1721 för stormaktssverige Förklara densitet för barn
Förklara densitet för barn Tack för att ni har lyssnat
Tack för att ni har lyssnat Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Fimbrietratt
Fimbrietratt Trög för kemist
Trög för kemist Magnetsjukhus
Magnetsjukhus Multiplikation med decimaltal uppgifter
Multiplikation med decimaltal uppgifter Kassaregister ideell förening
Kassaregister ideell förening Toppslätskivling dos
Toppslätskivling dos Vad står k.r.å.k.a.n för
Vad står k.r.å.k.a.n för Redogör för vad psykologi är
Redogör för vad psykologi är Borra hål för knoppar
Borra hål för knoppar Mat för unga idrottare
Mat för unga idrottare Bris för vuxna
Bris för vuxna Argument för teckenspråk som minoritetsspråk
Argument för teckenspråk som minoritetsspråk Ledarskapsteorier
Ledarskapsteorier Offentlig förvaltning
Offentlig förvaltning Antika plagg
Antika plagg Indikation för kejsarsnitt på moderns önskan
Indikation för kejsarsnitt på moderns önskan Datorkunskap för nybörjare
Datorkunskap för nybörjare Steg för steg rita
Steg för steg rita Kontinuitetshantering i praktiken
Kontinuitetshantering i praktiken Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Sju principer för tillitsbaserad styrning
Sju principer för tillitsbaserad styrning Geometri för barn
Geometri för barn Bästa kameran för astrofoto
Bästa kameran för astrofoto Bunden till c-dur
Bunden till c-dur Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Varför kallas perioden 1918-1939 för mellankrigstiden
Varför kallas perioden 1918-1939 för mellankrigstiden Personlig tidbok för yrkesförare
Personlig tidbok för yrkesförare Handledning reflektionsmodellen
Handledning reflektionsmodellen Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Jätte råtta
Jätte råtta Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Vem räknas som jude
Vem räknas som jude Kolposkopi, px
Kolposkopi, px Urban torhamn
Urban torhamn Stig kerman
Stig kerman Strategi för svensk viltförvaltning
Strategi för svensk viltförvaltning Sju för caesar
Sju för caesar Verksamhetsanalys exempel
Verksamhetsanalys exempel Novell typiska drag
Novell typiska drag Matematisk modellering eksempel
Matematisk modellering eksempel Tack för att ni har lyssnat
Tack för att ni har lyssnat Läkarutlåtande för livränta
Läkarutlåtande för livränta Shivaismen
Shivaismen Cks
Cks Health and social care unit 2
Health and social care unit 2 Care certificate duty of care
Care certificate duty of care Care sunt simturile prin care sunt evocate
Care sunt simturile prin care sunt evocate