CAESAREAN SECTION History According to legend Julius Caesar

- Slides: 36
CAESAREAN SECTION -
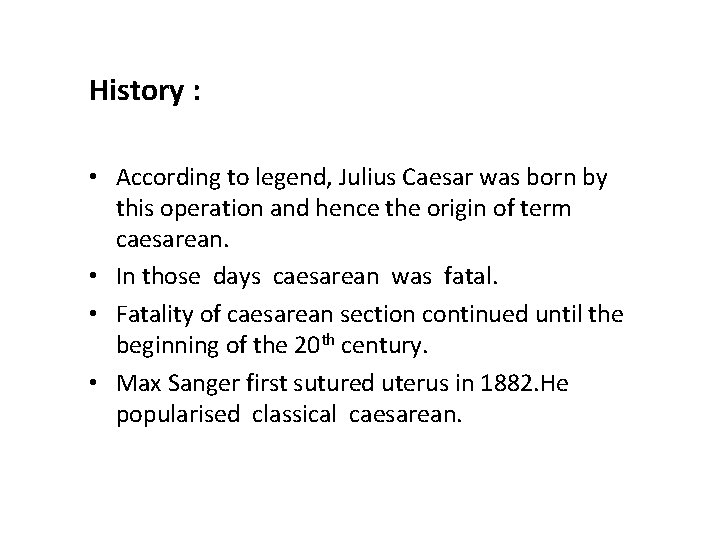
History : • According to legend, Julius Caesar was born by this operation and hence the origin of term caesarean. • In those days caesarean was fatal. • Fatality of caesarean section continued until the beginning of the 20 th century. • Max Sanger first sutured uterus in 1882. He popularised classical caesarean.
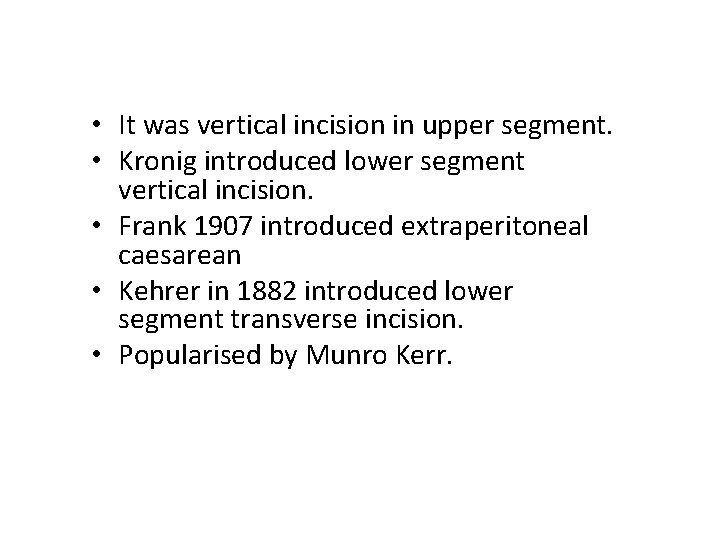
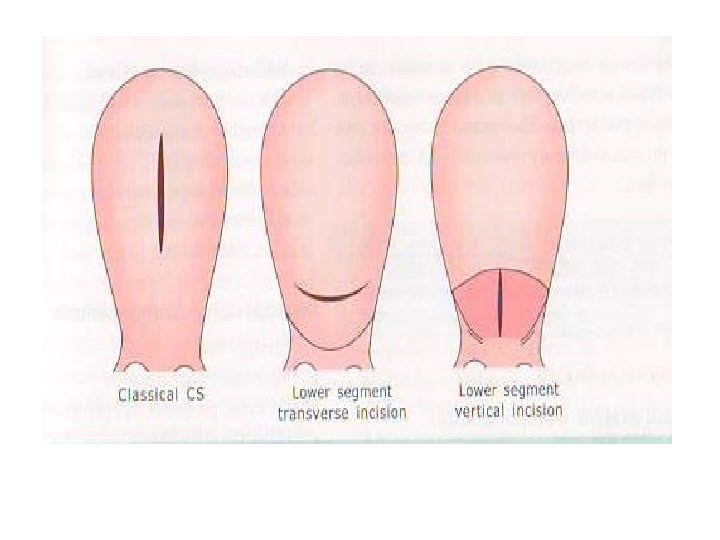
• It was vertical incision in upper segment. • Kronig introduced lower segment vertical incision. • Frank 1907 introduced extraperitoneal caesarean • Kehrer in 1882 introduced lower segment transverse incision. • Popularised by Munro Kerr.
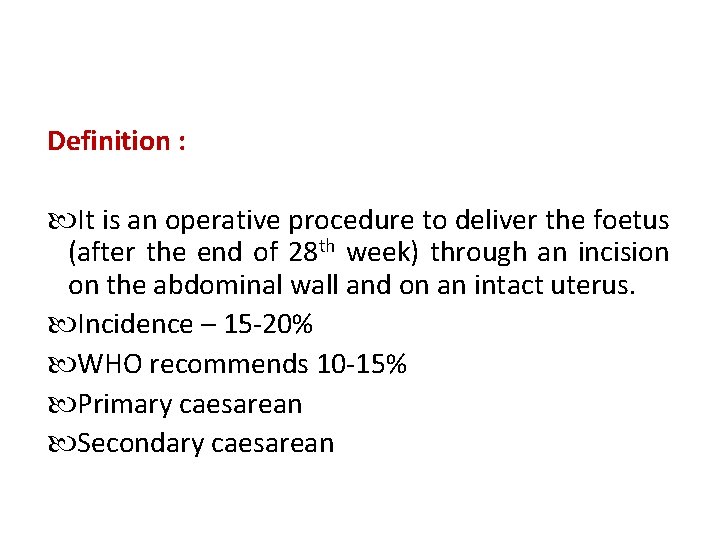
Definition : It is an operative procedure to deliver the foetus (after the end of 28 th week) through an incision on the abdominal wall and on an intact uterus. Incidence – 15 -20% WHO recommends 10 -15% Primary caesarean Secondary caesarean
INDICATIONS : Indications Maternal indications i) Central placenta praevia ◦ Grade III placenta praevia ◦ Grade II post placenta praevia ii) Contracted pelvis iii) Vaginal atresia or stenosis iv) Pelvic mass causing obstruction (cervical or broad ligament fibroid ovarian tumours impacted in the pelvis)
• • • CPD Obstructed labour Macrosomia Tumours complicating pregnancy Foetal distress , cord prolapse Cervical dysocia Abruptio placenta Malpresentations – shoulder, breech brow Failed induction of labour, failure to progress in labour.
• • Medical disorders – Eclampsia – uncontrolled fits. Severe preeclampsia Uncontrolled diabetes mellitus. With unfavourable cervix previous caesarean section, PROM, PPROM. Chorioamnionitis
• • Following VVF repair RVF repair Previous 2 caesarean section (LSCS) Previous classical caesarean or – Hysterotomy – Myomectomy (where cavity was opened) – HIV infections – Maternal request – Failed forceps or vacuum
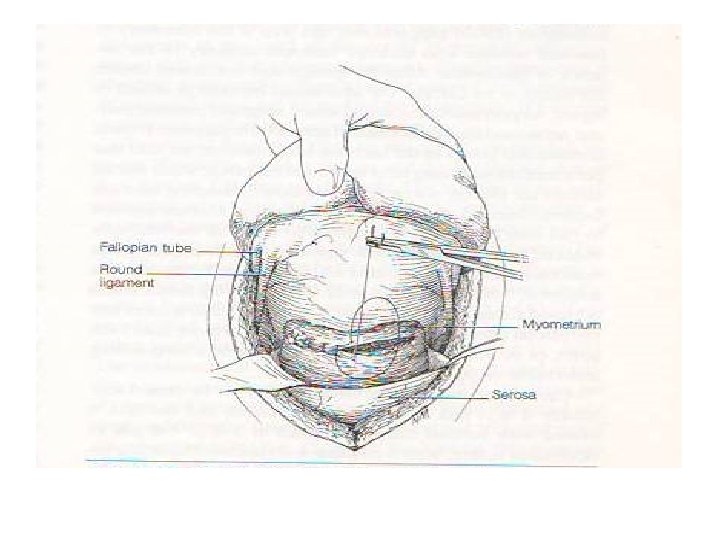
Lower segment : • • Pre-op preparation Anaesthesia Abdominal incisions Pfannensteil incision Joel Cohen incision Maylard incision Midline vertical incision

Transverse incision Vertical incision • Cosmetic appeal More Less appearing • Postoperative pain Less More • Wound dehiscence Less chance More chance • Incisional hernia Differences • Technical skill • Time taken Less chance between transverse. More andchance vertical More technical skill Less technical skill incisions More time consuming Less time consuming • Access to upper abdomen Less access Good access and can be extended if needed
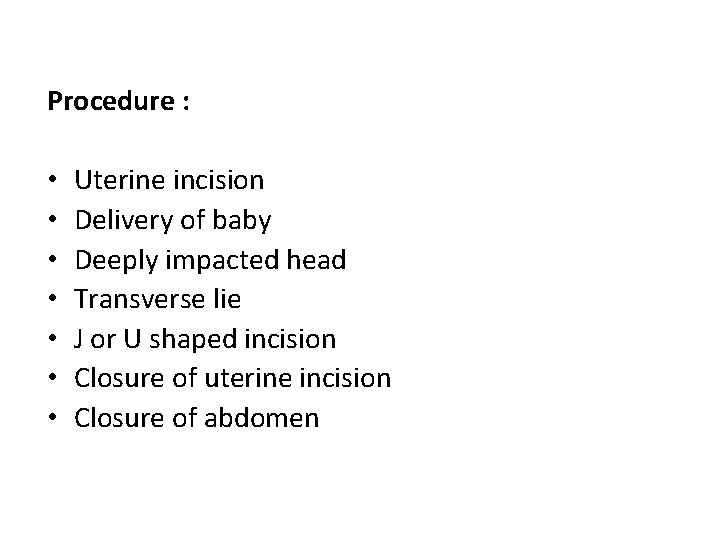
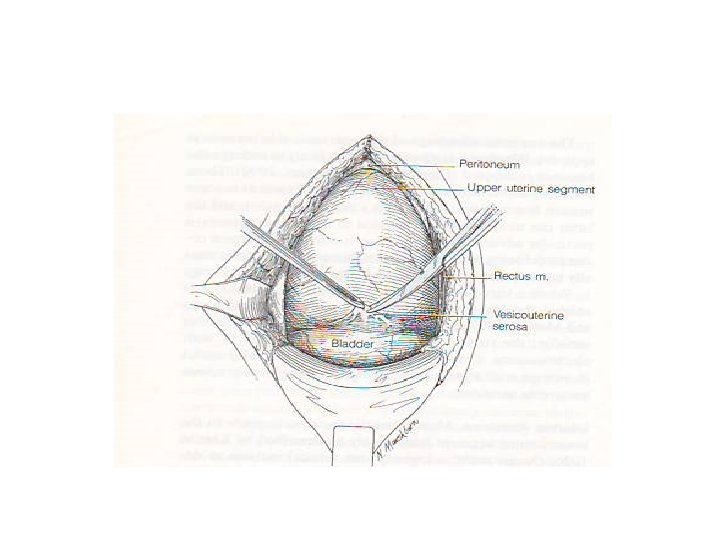
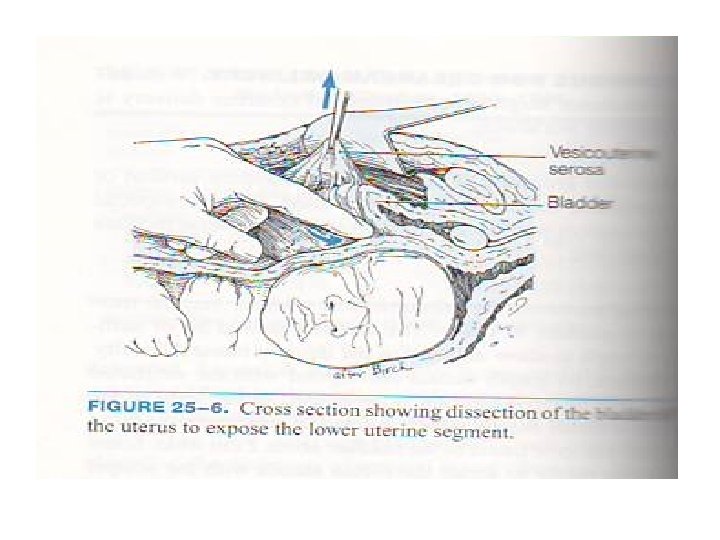
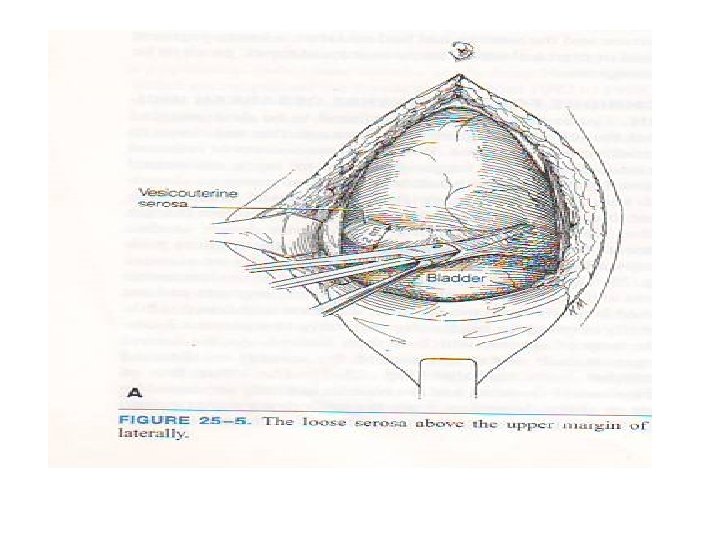
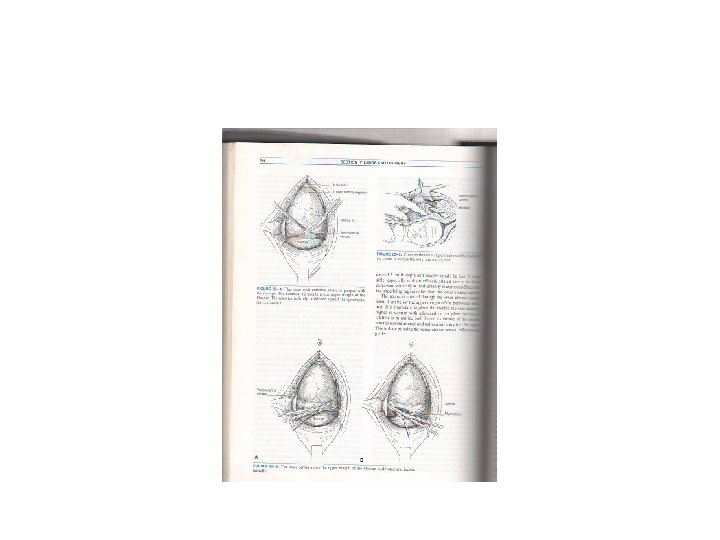
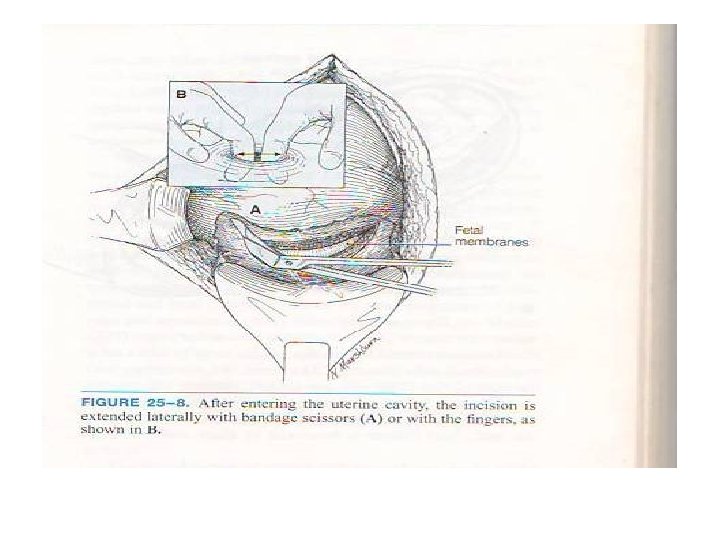
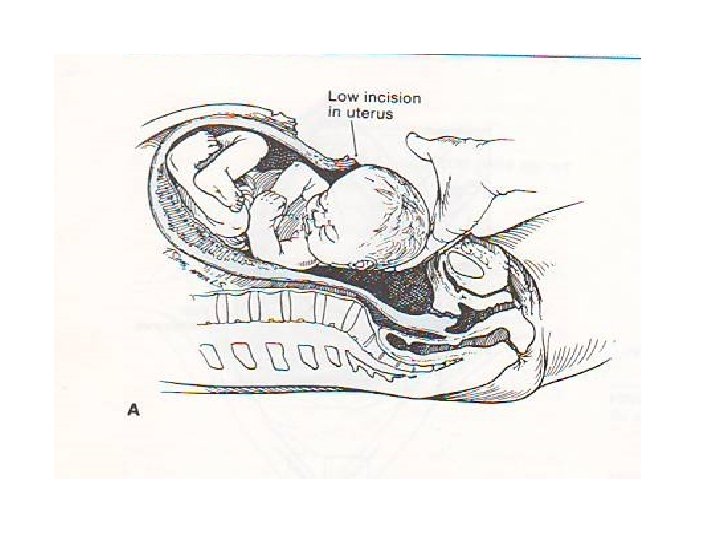
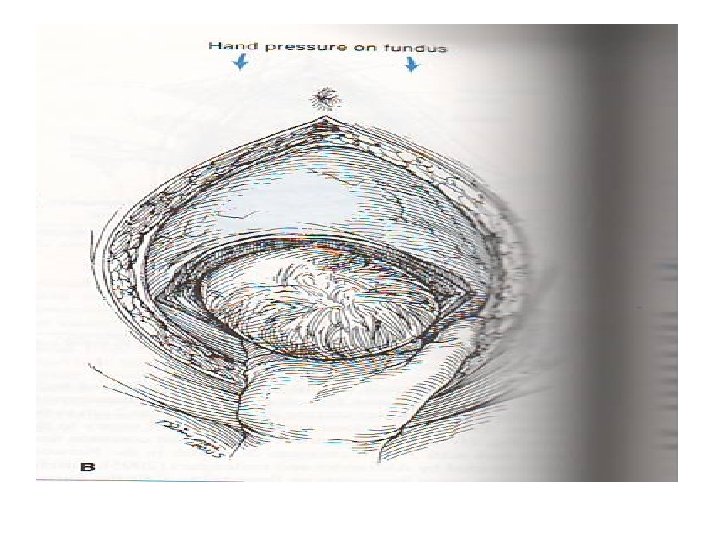
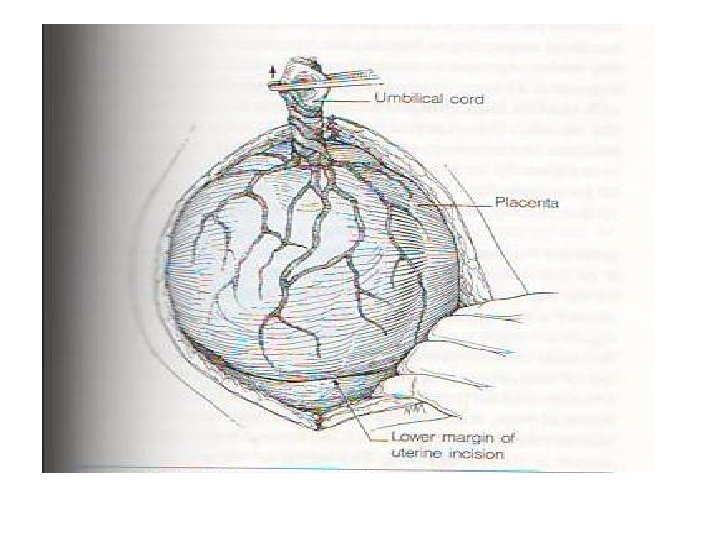
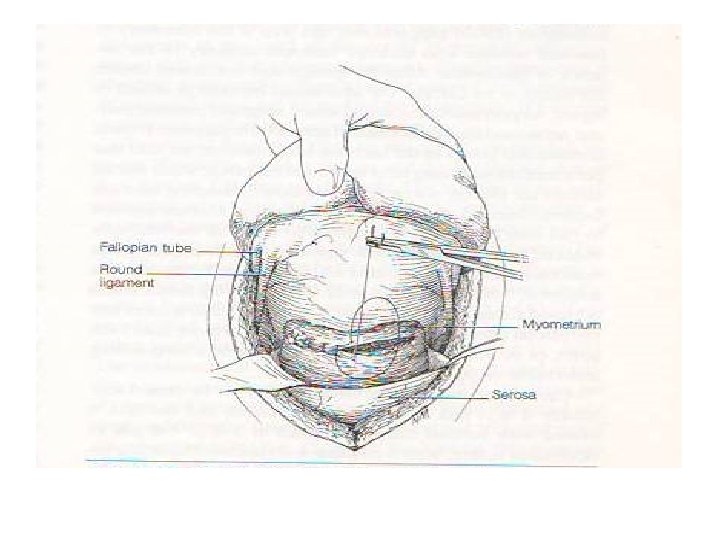
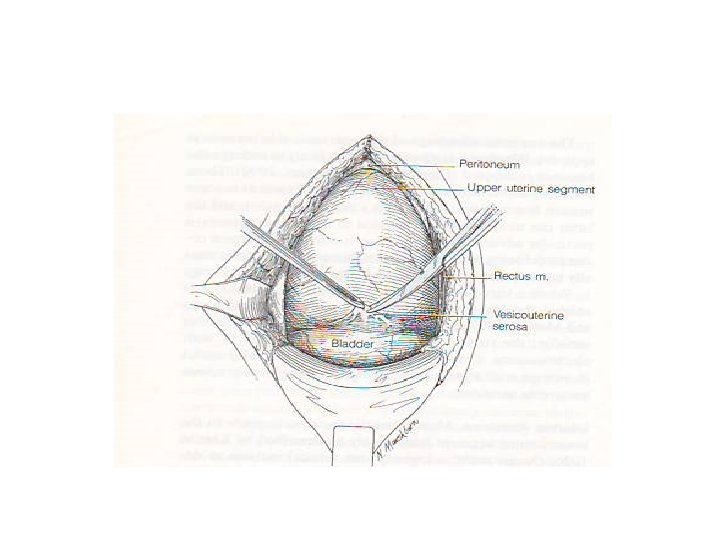
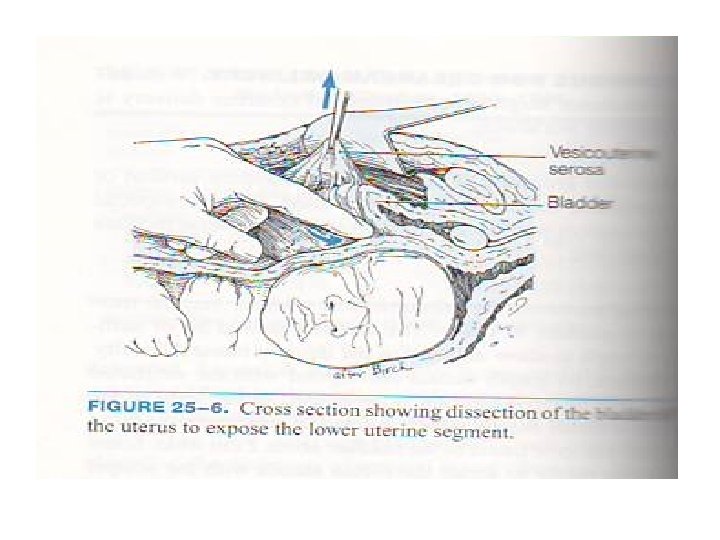
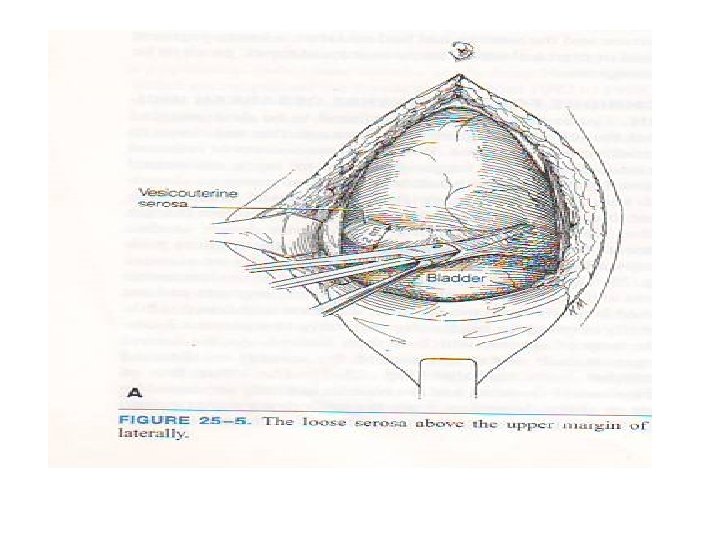
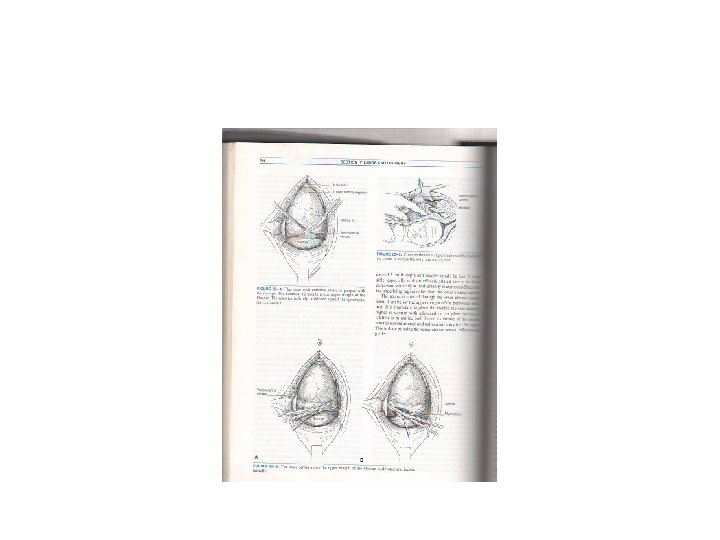
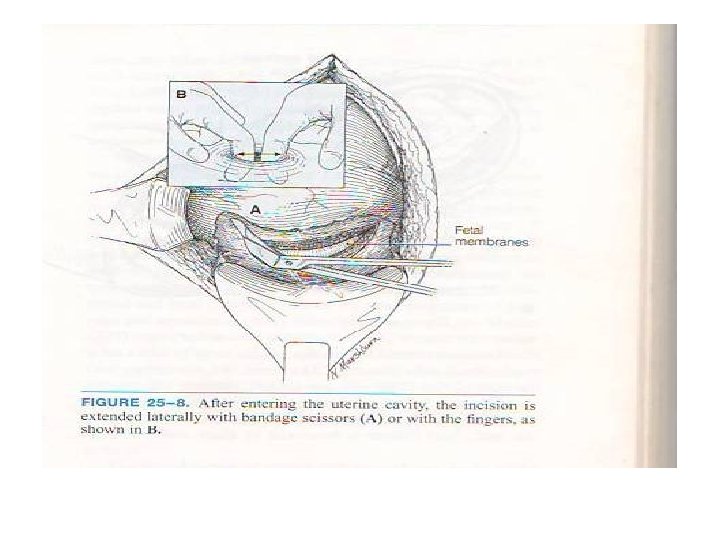
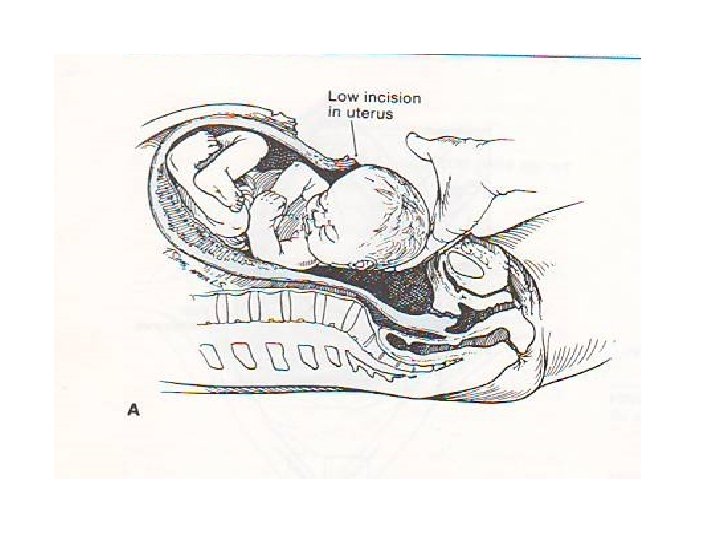
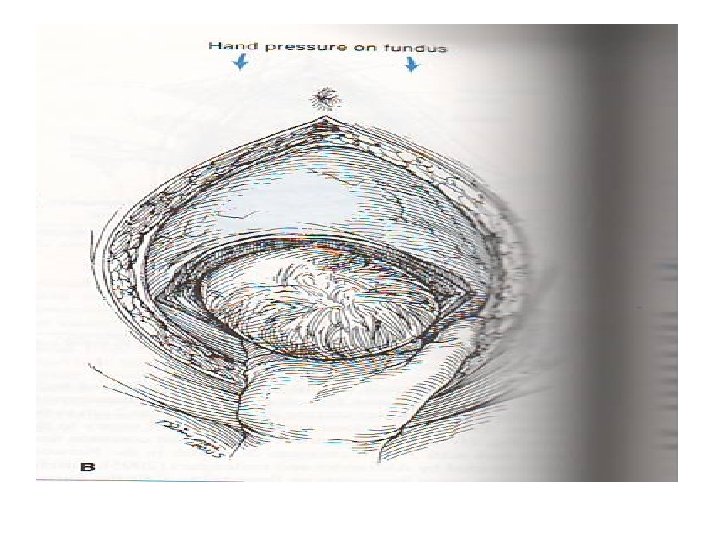
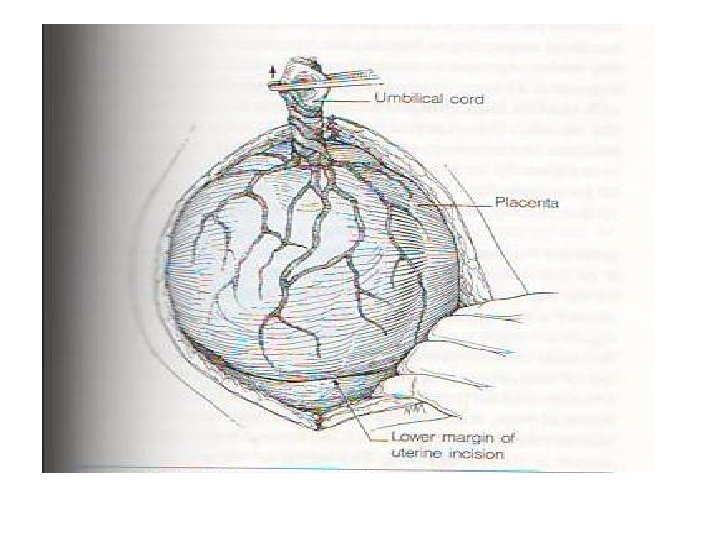
Procedure : • • Uterine incision Delivery of baby Deeply impacted head Transverse lie J or U shaped incision Closure of uterine incision Closure of abdomen
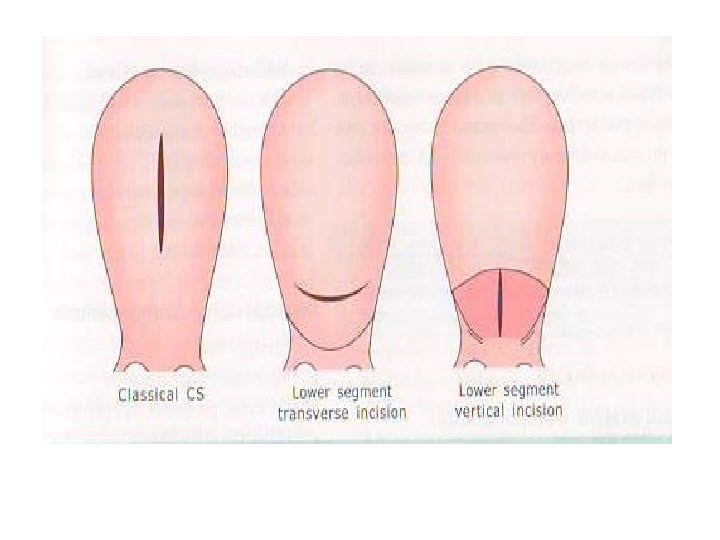
• Postoperative care • • Other types of caesarean section Lower segment vertical incision Classical caesarean Extraperitoneal caesarean section
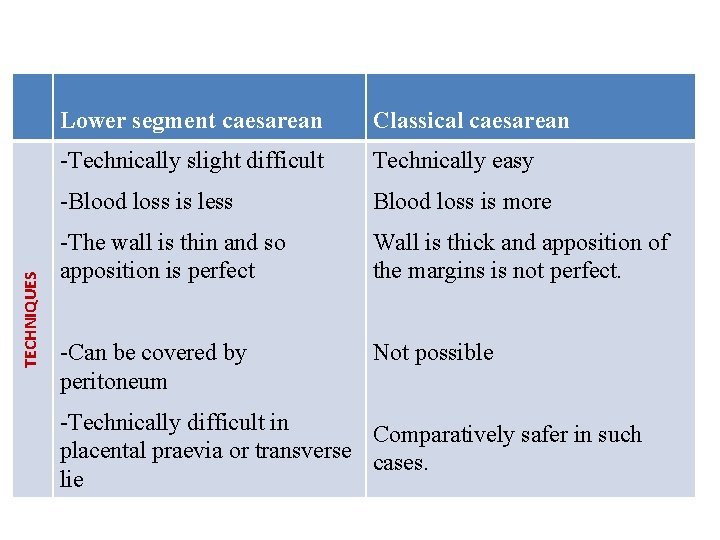
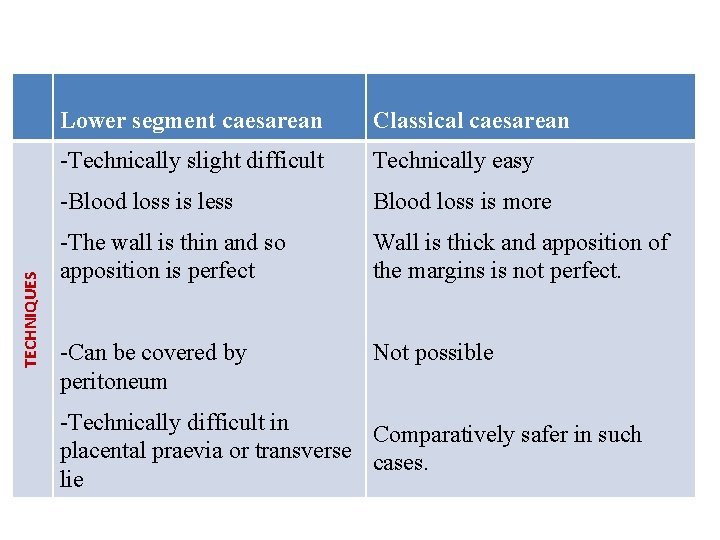
TECHNIQUES Lower segment caesarean Classical caesarean -Technically slight difficult Technically easy -Blood loss is less Blood loss is more -The wall is thin and so apposition is perfect Wall is thick and apposition of the margins is not perfect. -Can be covered by peritoneum Not possible -Technically difficult in Comparatively safer in such placental praevia or transverse cases. lie
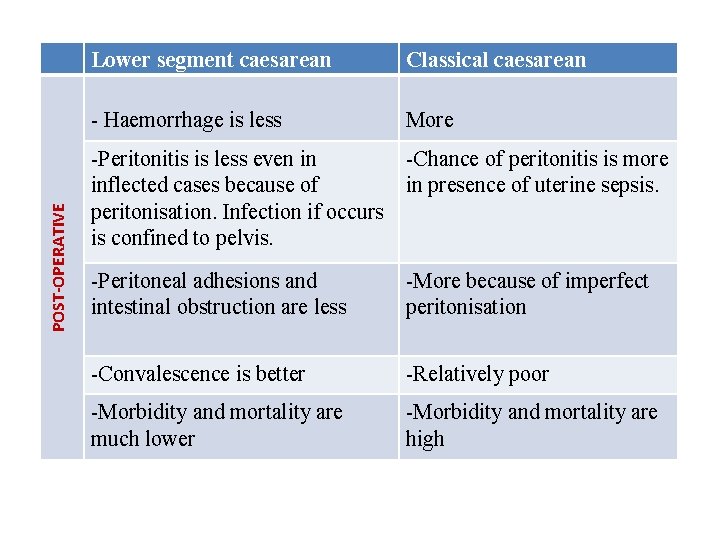
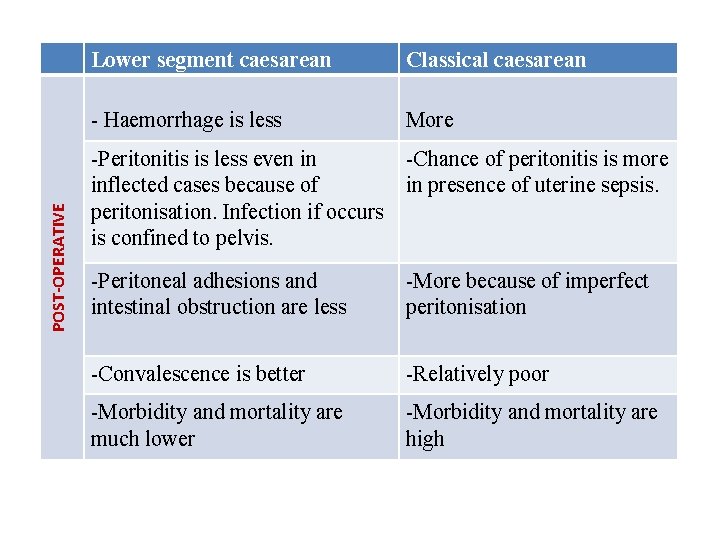
POST-OPERATIVE Lower segment caesarean Classical caesarean - Haemorrhage is less More -Peritonitis is less even in -Chance of peritonitis is more inflected cases because of in presence of uterine sepsis. peritonisation. Infection if occurs is confined to pelvis. -Peritoneal adhesions and intestinal obstruction are less -More because of imperfect peritonisation -Convalescence is better -Relatively poor -Morbidity and mortality are much lower -Morbidity and mortality are high
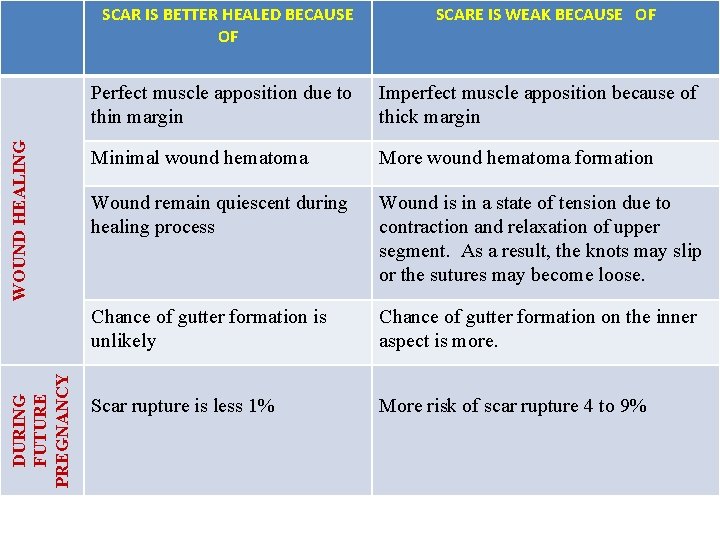
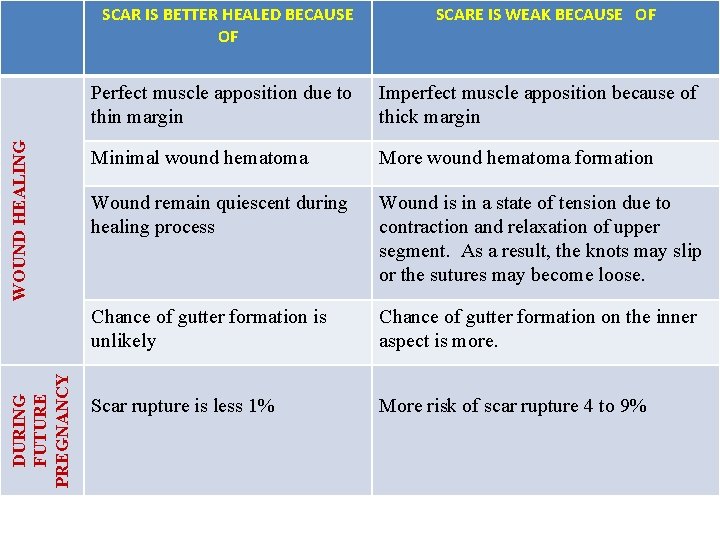
DURING FUTURE PREGNANCY WOUND HEALING SCAR IS BETTER HEALED BECAUSE OF SCARE IS WEAK BECAUSE OF Perfect muscle apposition due to thin margin Imperfect muscle apposition because of thick margin Minimal wound hematoma More wound hematoma formation Wound remain quiescent during healing process Wound is in a state of tension due to contraction and relaxation of upper segment. As a result, the knots may slip or the sutures may become loose. Chance of gutter formation is unlikely Chance of gutter formation on the inner aspect is more. Scar rupture is less 1% More risk of scar rupture 4 to 9%
• Caesarean hysterectomy • Perimortem caesarean section
COMPLICATIONS OF CAESAREAN SECTION : Intra operative : Difficulty in delivery of head Primary haemorrhage • Extension of uterine incision to one or both the sides. May involve the uterine vessels to cause severe haemorrhage, may lead to broad ligament haematoma formation. • Extension laterally or inferiorly into the vagina. • Bladder injury
• Ureteral injury (Rare) occurs during control of bleeding from lateral extensions. • GIT injury rare unless prior pelvic/abdominal adhesions. • Bleeding – Atonic PPH – Traumatic PPH • Combined
• Morbidly adherent placenta (Placenta accreta) commonly seen in placenta praevia who had prior caesarean. Total hysterectomy often needed to control haemorrhage. • Anesthetic hazards – Mendelssohn's syndrome – Hypotension – Cardiac arrest
Post-operative complications : Immediate : • PPH – may lead to shock • Infections : – Endometrites – UTI – Peritonitis – Abdominal wound infection
• Intestinal obstruction – may be mechanical due to adhesions or bands or paralytic ileus following peritonitis. • DVT, septic thromboplebitis.
Remote complications : • • Chronic pelvic pain Incisional hernia Intestinal obstruction due to adhesions and bands. Future pregnancy – risk of scar rupture. VVF Scar endometriosis Placenta praevia and adherent placenta in next pregnancy Increased incidence of bladder injury at a repeat caesarean or at hysterectomy later
Foetal complications : • Injuries • Scalp • During breech extraction - intracranial haemorrhage • Prematurity – iatrogenic • Birth asphyxia may be preexisting (foetal distress being indication for caesarean section)
• MMR following caesarean section – 6 to 22 per 1 lack procedures. • Perinatal mortality rate – 5 to 8%
Rising caesarean rates Worldwide increase Decreased VBAC Decreased instrumental deliveries Decreased breech deliveries Increased diagnosis of intrapartum fetal distress Increased diagnosis of prolonged labour Increased induction of labour Prevalence of obesity Increased number of older women and women with medical problems getting pregnant • Pregnancies following ART procedures • Fear of litigation • Maternal request • • •
• Though caesarean rate is increased, no much improvement in perinatal outcome. • Maternal morbidity and mortality increased due to adherent placenta