Arrhythmias and Antiarrhythmic Drugs Class I Na channel

![Digoxin: Cardiac effects: Increases intracellular [Na+], increases in Ca 2+ (via NCX) more Ca Digoxin: Cardiac effects: Increases intracellular [Na+], increases in Ca 2+ (via NCX) more Ca](https://slidetodoc.com/presentation_image_h/0ee8b15a1b4344a6467184e9b4fde2f9/image-29.jpg)
![Triggered activity due too much intracellular Ca 2+ [Ca 2+]i Mg 2+ (for torsades) Triggered activity due too much intracellular Ca 2+ [Ca 2+]i Mg 2+ (for torsades)](https://slidetodoc.com/presentation_image_h/0ee8b15a1b4344a6467184e9b4fde2f9/image-31.jpg)

- Slides: 36
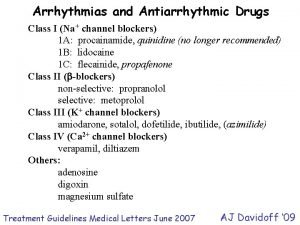
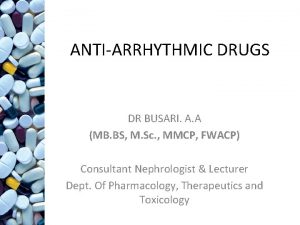
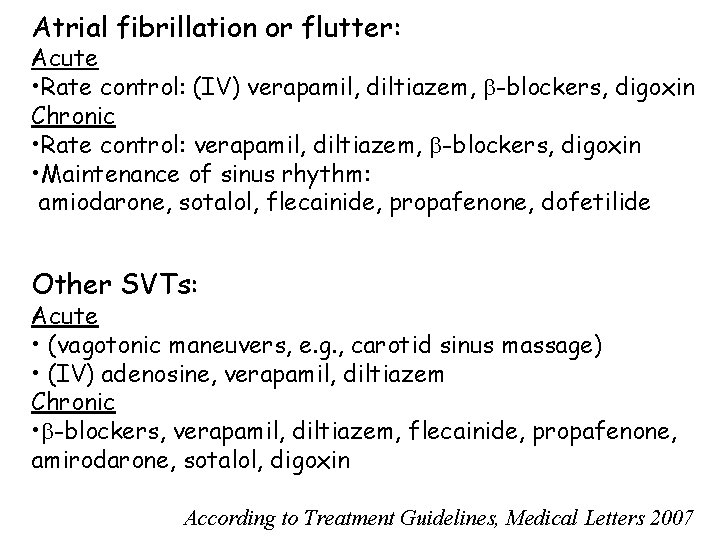
Arrhythmias and Antiarrhythmic Drugs Class I (Na+ channel blockers) 1 A: procainamide, quinidine (no longer recommended) 1 B: lidocaine 1 C: flecainide, propafenone Class II ( -blockers) non-selective: propranolol selective: metoprolol Class III (K+ channel blockers) amiodarone, sotalol, dofetilide, ibutilide, (azimilide) Class IV (Ca 2+ channel blockers) verapamil, diltiazem Others: adenosine digoxin magnesium sulfate Treatment Guidelines Medical Letters June 2007 AJ Davidoff ‘ 09
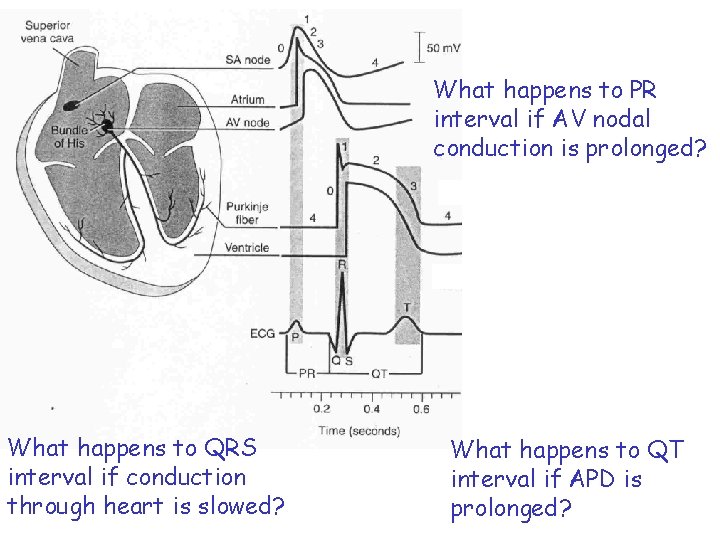
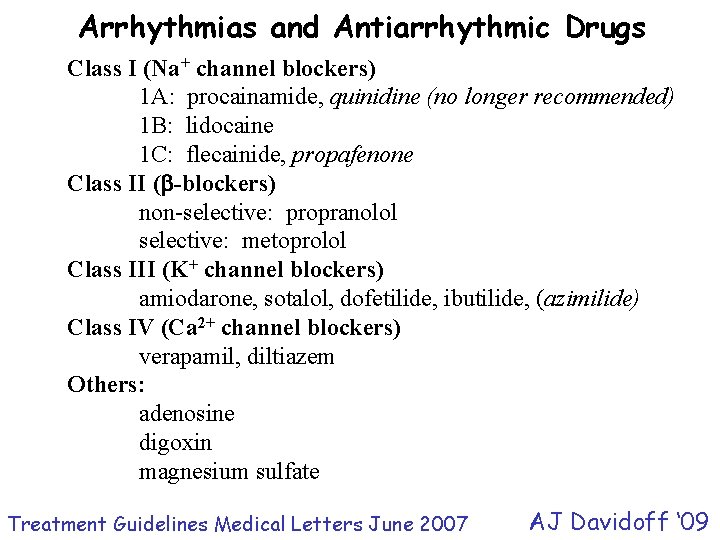
What happens to PR interval if AV nodal conduction is prolonged? What happens to QRS interval if conduction through heart is slowed? What happens to QT interval if APD is prolonged?
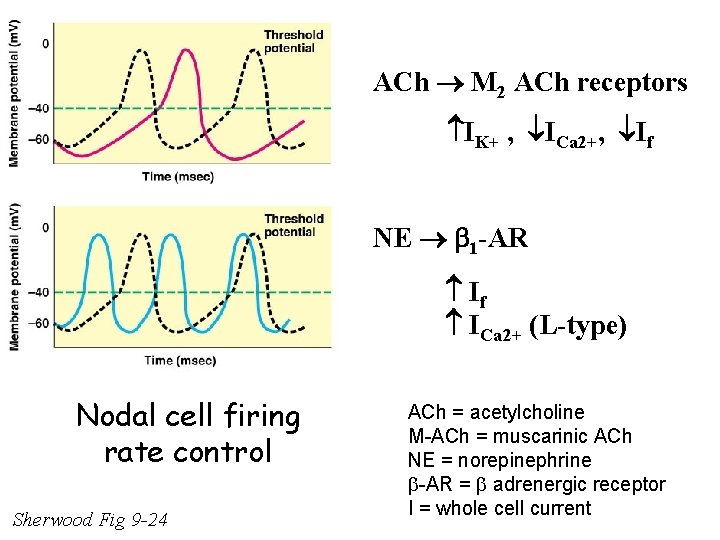
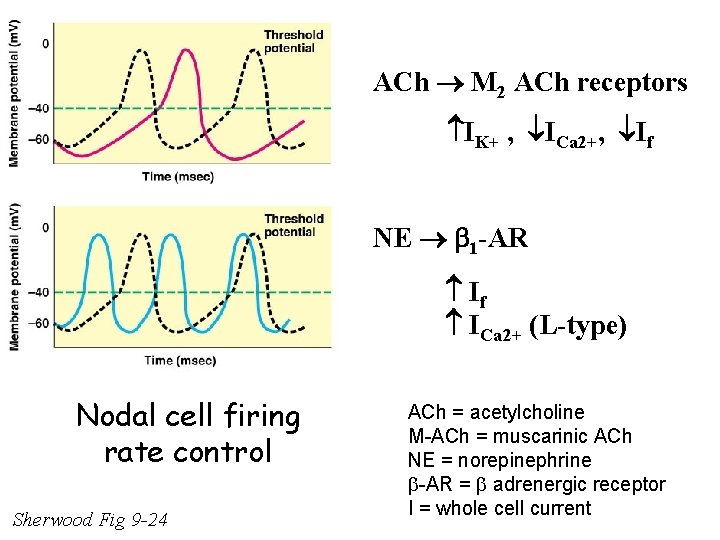
ACh M 2 ACh receptors IK+ , ICa 2+, If NE 1 -AR If ICa 2+ (L-type) Nodal cell firing rate control Sherwood Fig 9 -24 ACh = acetylcholine M-ACh = muscarinic ACh NE = norepinephrine -AR = adrenergic receptor I = whole cell current
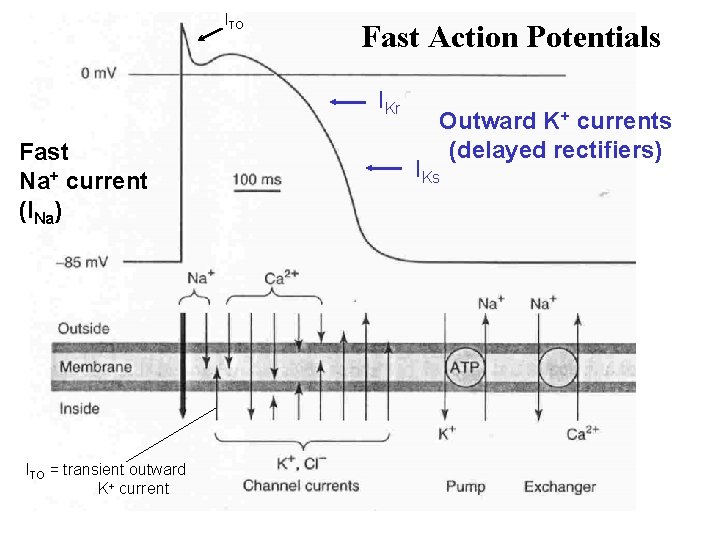
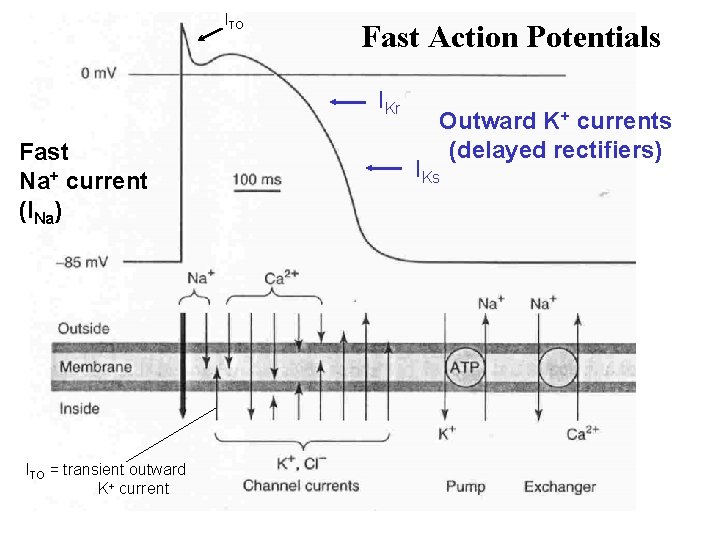
ITO Fast Action Potentials IKr Fast Na+ current (INa) ITO = transient outward K+ current Outward K+ currents (delayed rectifiers) IKs
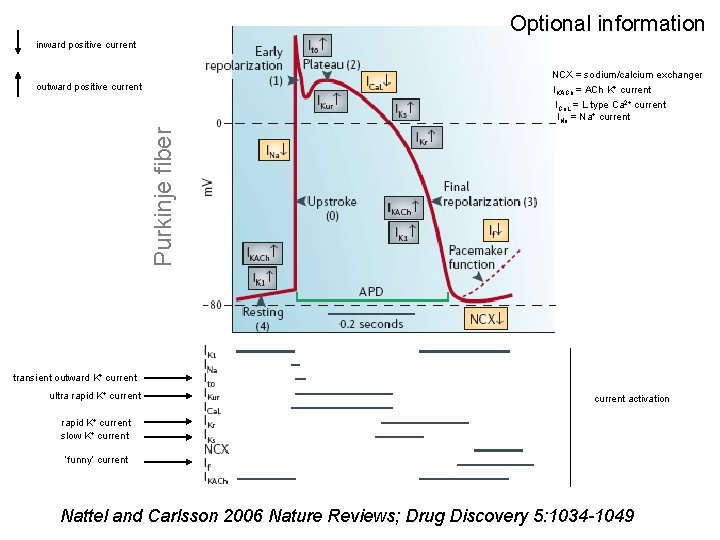
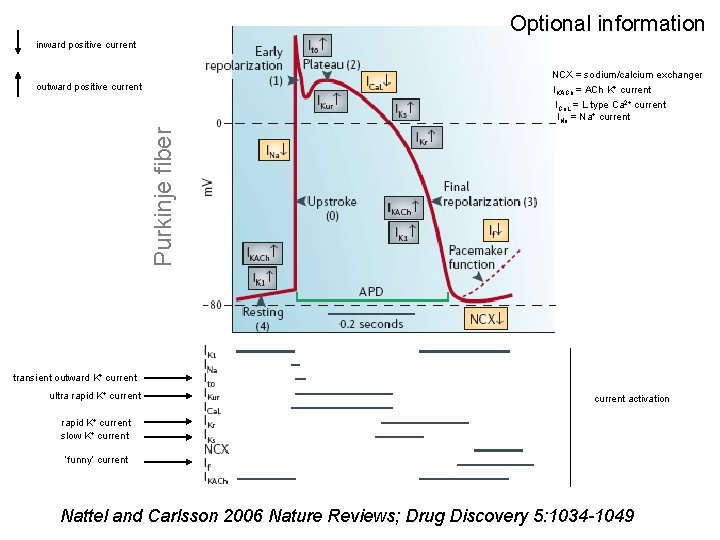
Optional information inward positive current NCX = sodium/calcium exchanger IKACh = ACh K+ current outward positive current Purkinje fiber ICa. L = L type Ca 2+ current INa = Na+ current transient outward K+ current ultra rapid K+ current activation rapid K+ current slow K+ current ‘funny’ current Nattel and Carlsson 2006 Nature Reviews; Drug Discovery 5: 1034 -1049

Most arrhythmias result from altered conduction and/or automaticity Conduction abnormalities Typically arise from partial depolarization due to injury (e. g. , over stretch, ischemia) or abnormal anatomy Partial or complete block Accessory conduction pathways e. g. , Wolff-Parkinson-White (WPW) Syndrome Re-entry Fibrillation (multi-re-entry loops)
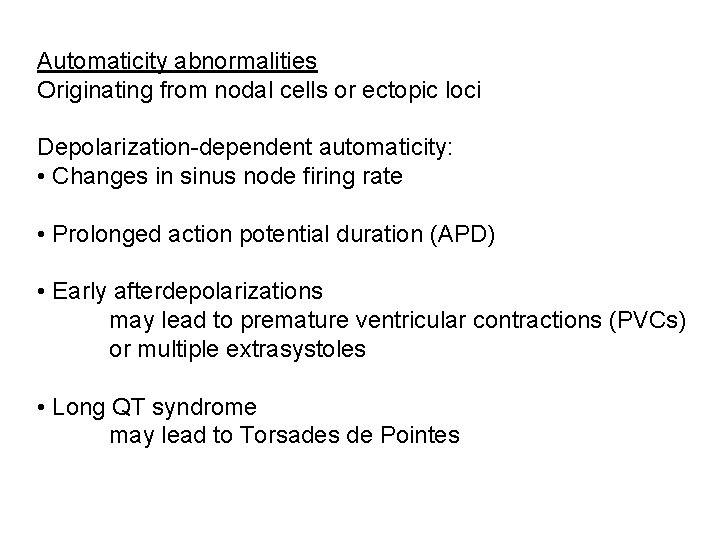
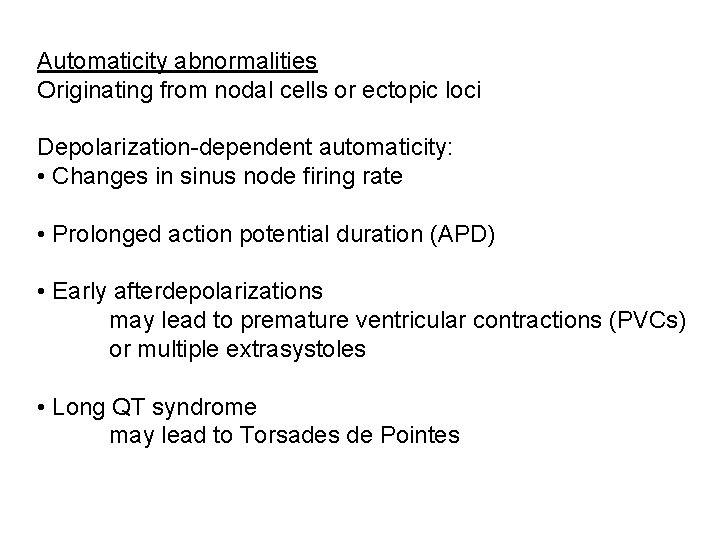
Automaticity abnormalities Originating from nodal cells or ectopic loci Depolarization-dependent automaticity: • Changes in sinus node firing rate • Prolonged action potential duration (APD) • Early afterdepolarizations may lead to premature ventricular contractions (PVCs) or multiple extrasystoles • Long QT syndrome may lead to Torsades de Pointes
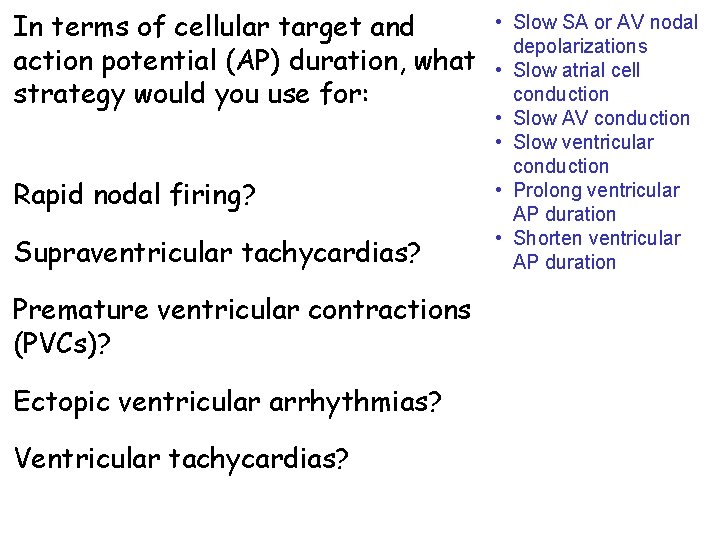
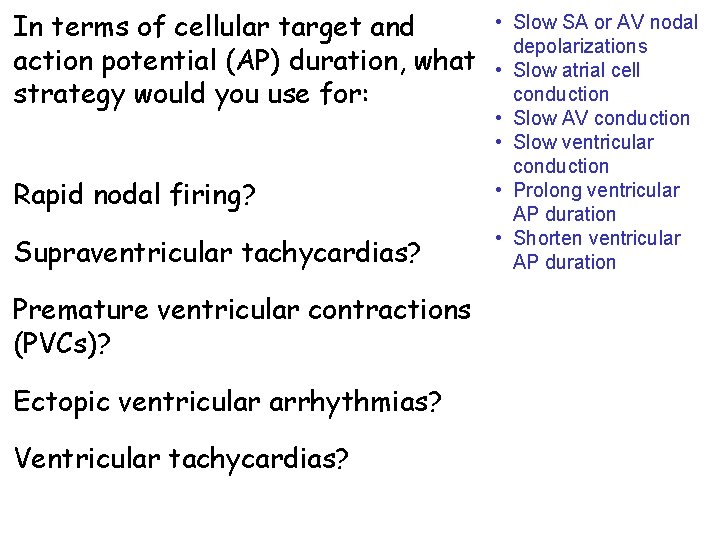
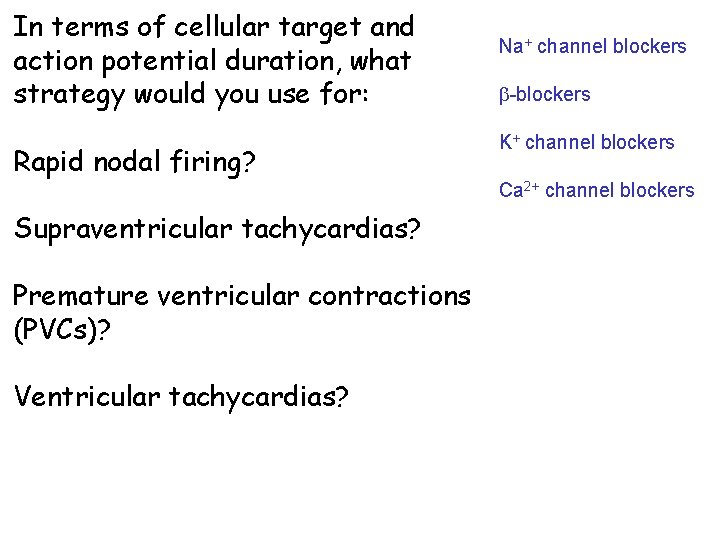
In terms of cellular target and action potential (AP) duration, what strategy would you use for: Rapid nodal firing? Supraventricular tachycardias? Premature ventricular contractions (PVCs)? Ectopic ventricular arrhythmias? Ventricular tachycardias? • Slow SA or AV nodal depolarizations • Slow atrial cell conduction • Slow AV conduction • Slow ventricular conduction • Prolong ventricular AP duration • Shorten ventricular AP duration
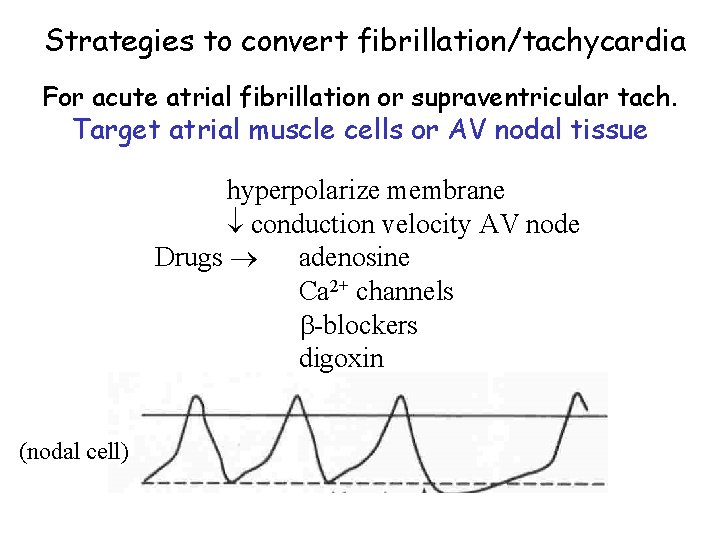
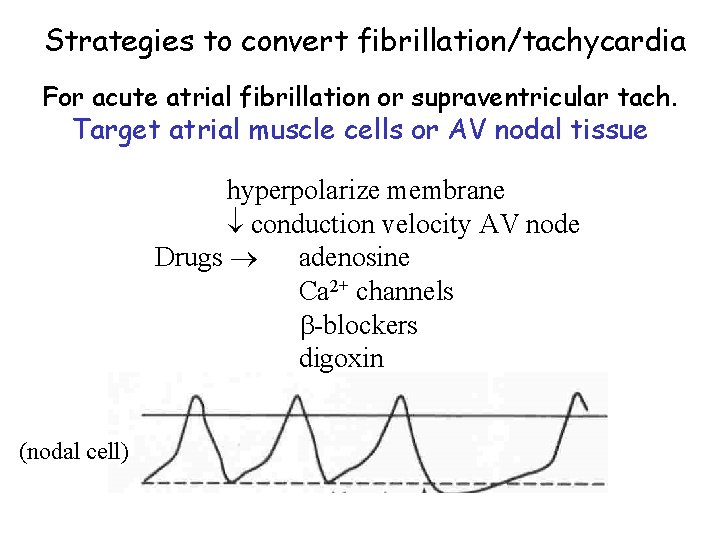
Strategies to convert fibrillation/tachycardia For acute atrial fibrillation or supraventricular tach. Target atrial muscle cells or AV nodal tissue hyperpolarize membrane conduction velocity AV node Drugs adenosine Ca 2+ channels -blockers digoxin (nodal cell)
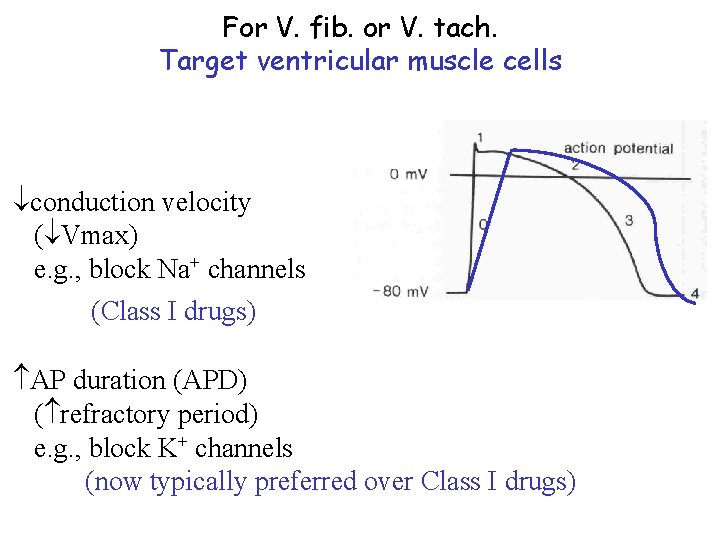
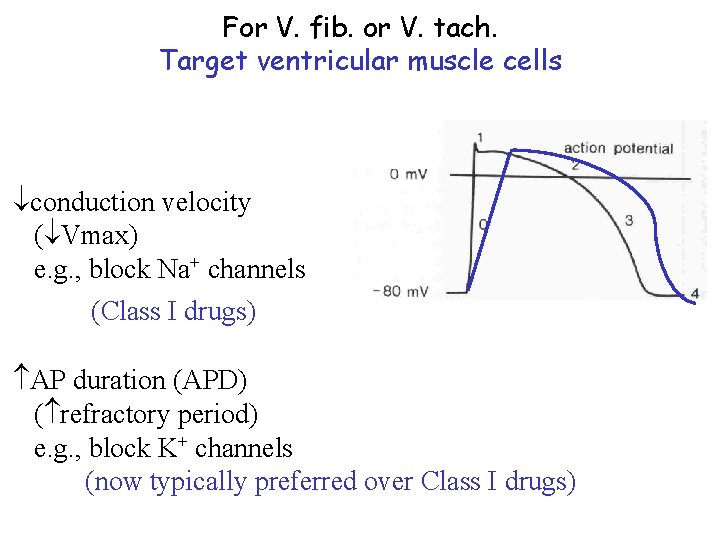
For V. fib. or V. tach. Target ventricular muscle cells conduction velocity ( Vmax) e. g. , block Na+ channels (Class I drugs) AP duration (APD) ( refractory period) e. g. , block K+ channels (now typically preferred over Class I drugs)
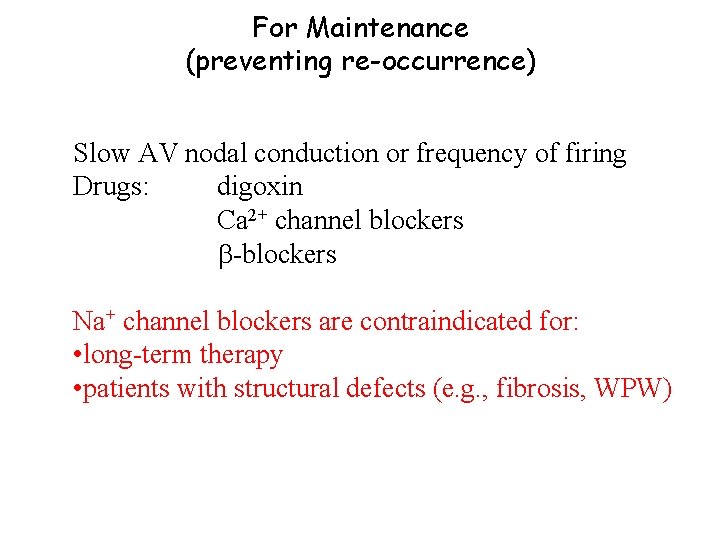
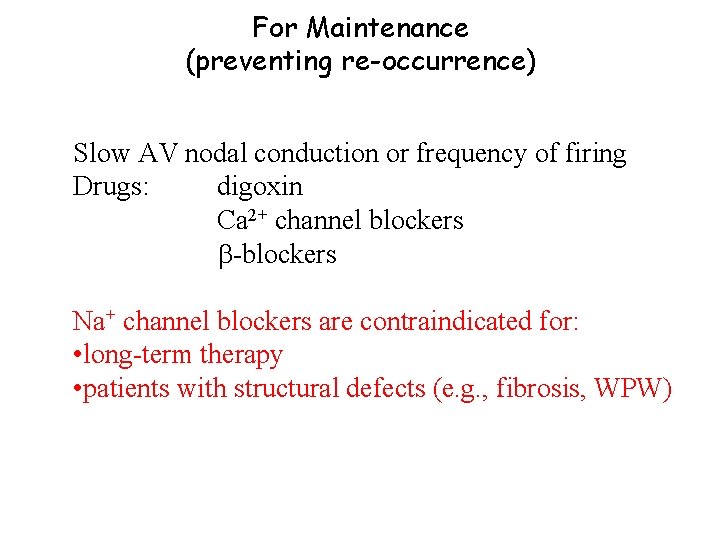
For Maintenance (preventing re-occurrence) Slow AV nodal conduction or frequency of firing Drugs: digoxin Ca 2+ channel blockers -blockers Na+ channel blockers are contraindicated for: • long-term therapy • patients with structural defects (e. g. , fibrosis, WPW)
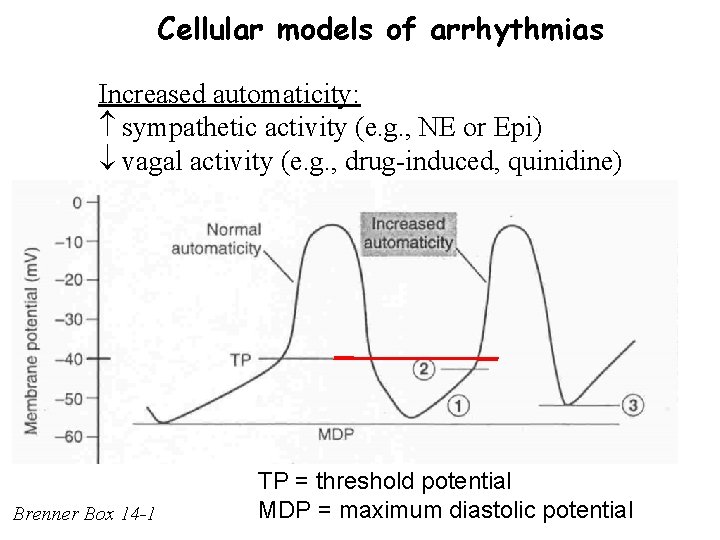
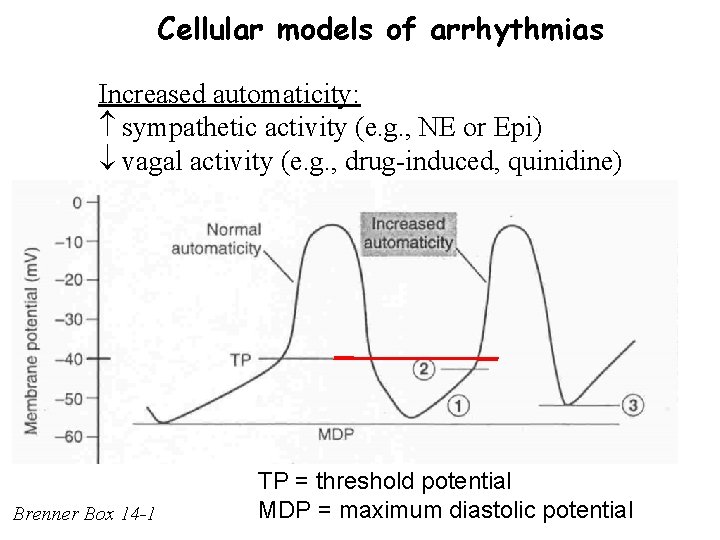
Cellular models of arrhythmias Increased automaticity: sympathetic activity (e. g. , NE or Epi) vagal activity (e. g. , drug-induced, quinidine) Brenner Box 14 -1 TP = threshold potential MDP = maximum diastolic potential
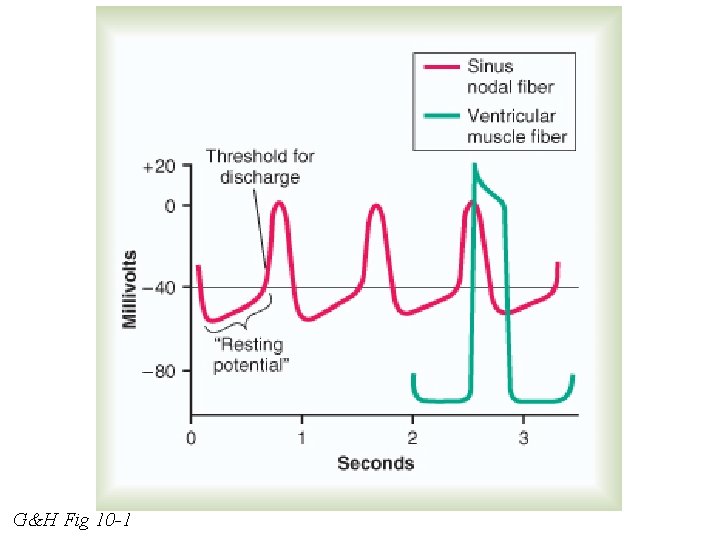
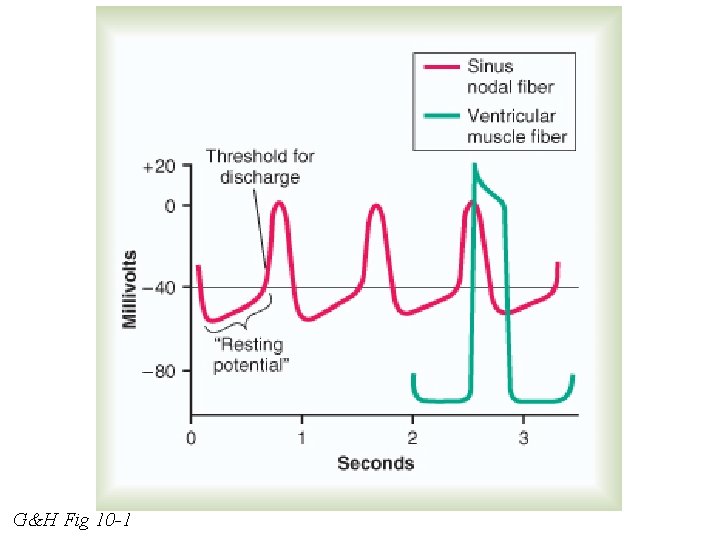
G&H Fig 10 -1
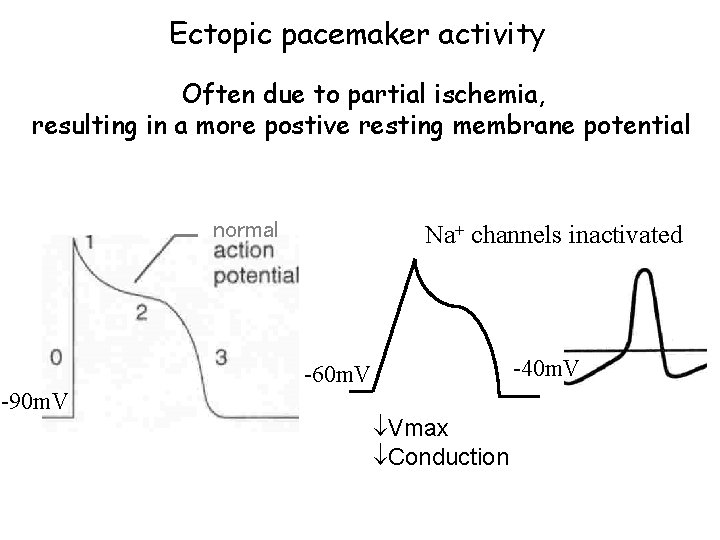
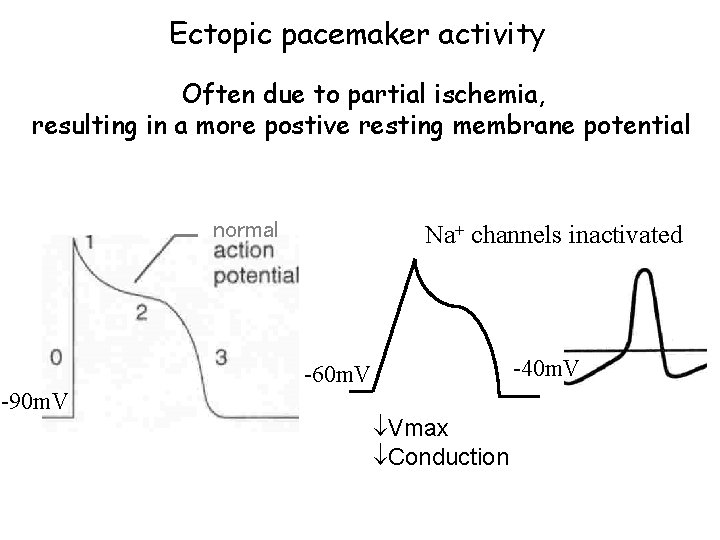
Ectopic pacemaker activity Often due to partial ischemia, resulting in a more postive resting membrane potential normal Na+ channels inactivated -40 m. V -60 m. V -90 m. V Vmax Conduction
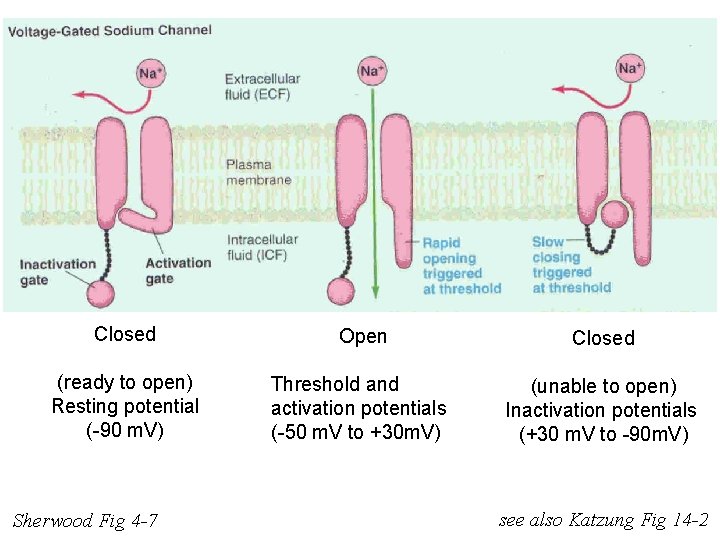
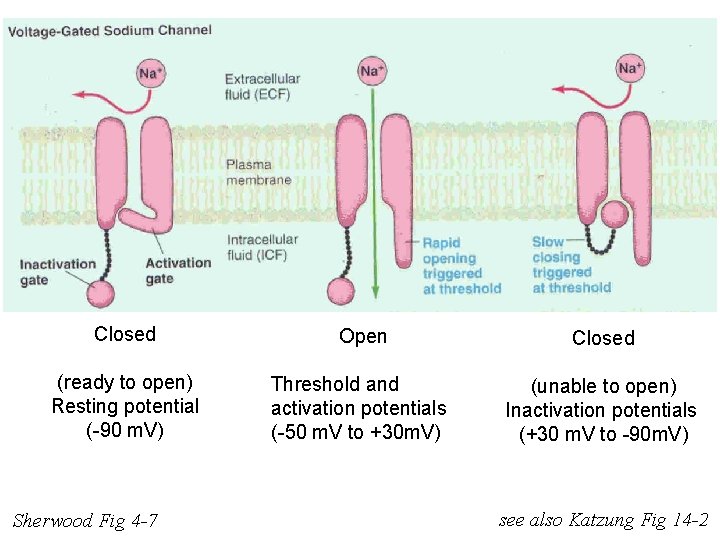
Closed Open Closed (ready to open) Resting potential (-90 m. V) Threshold and activation potentials (-50 m. V to +30 m. V) (unable to open) Inactivation potentials (+30 m. V to -90 m. V) Sherwood Fig 4 -7 see also Katzung Fig 14 -2
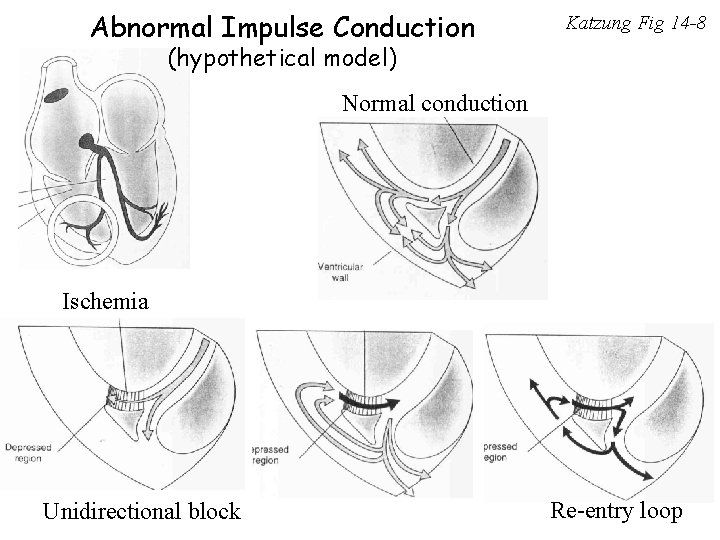
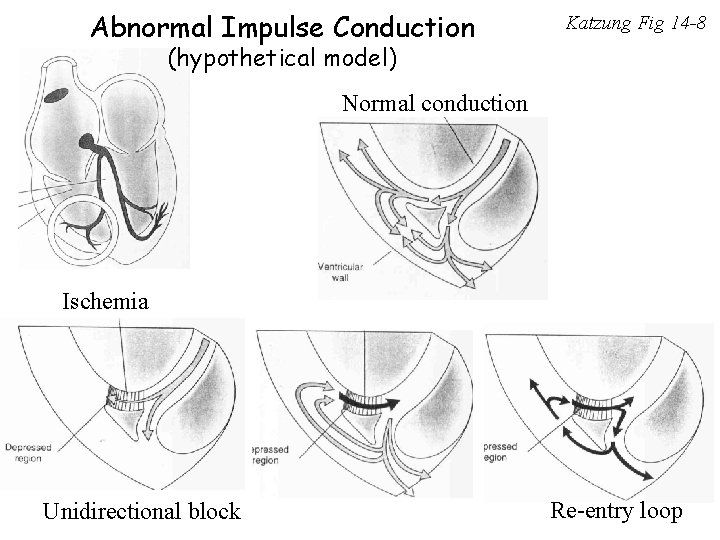
Abnormal Impulse Conduction Katzung Fig 14 -8 (hypothetical model) Normal conduction Ischemia Unidirectional block Re-entry loop
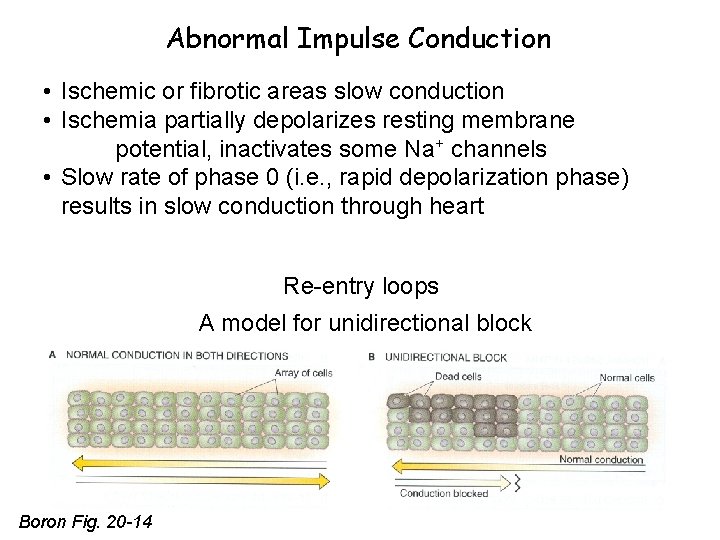
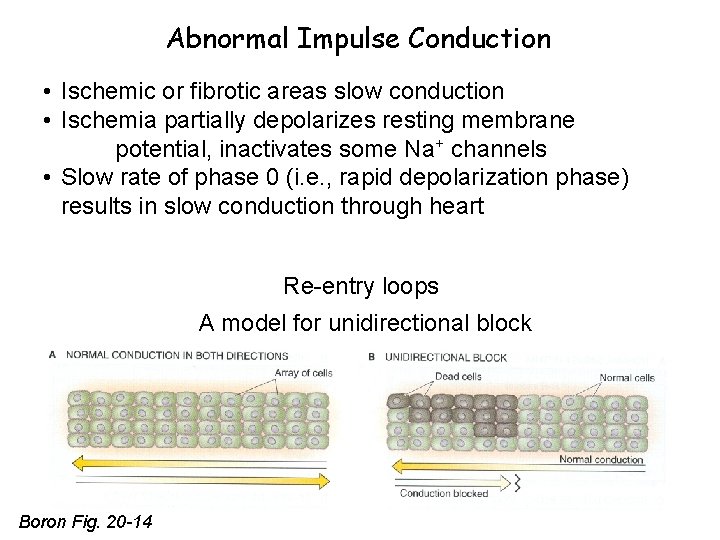
Abnormal Impulse Conduction • Ischemic or fibrotic areas slow conduction • Ischemia partially depolarizes resting membrane potential, inactivates some Na+ channels • Slow rate of phase 0 (i. e. , rapid depolarization phase) results in slow conduction through heart Re-entry loops A model for unidirectional block Boron Fig. 20 -14
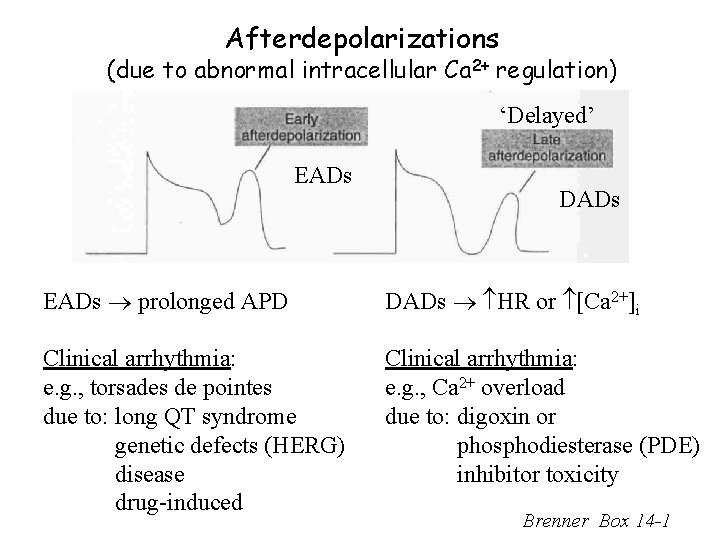
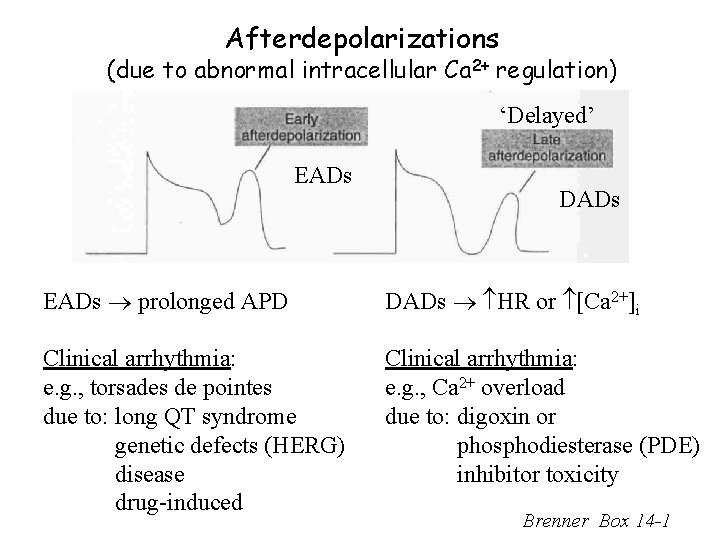
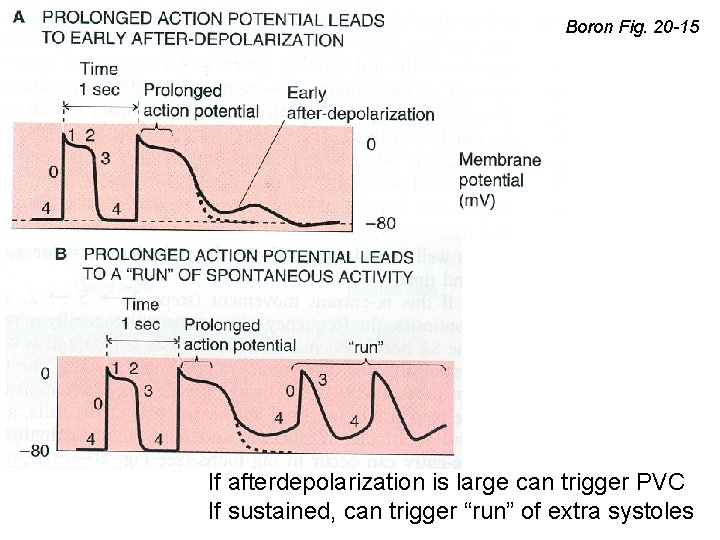
Afterdepolarizations (due to abnormal intracellular Ca 2+ regulation) ‘Delayed’ EADs DADs EADs prolonged APD DADs HR or [Ca 2+]i Clinical arrhythmia: e. g. , torsades de pointes due to: long QT syndrome genetic defects (HERG) disease drug-induced Clinical arrhythmia: e. g. , Ca 2+ overload due to: digoxin or phosphodiesterase (PDE) inhibitor toxicity Brenner Box 14 -1
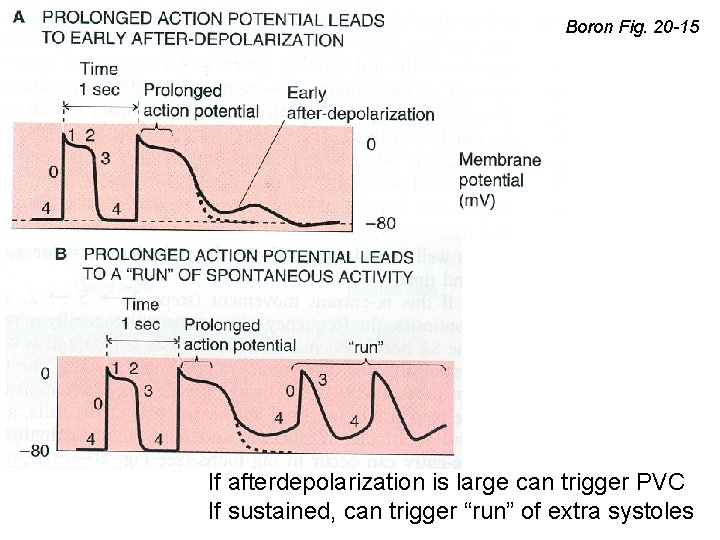
Boron Fig. 20 -15 If afterdepolarization is large can trigger PVC If sustained, can trigger “run” of extra systoles
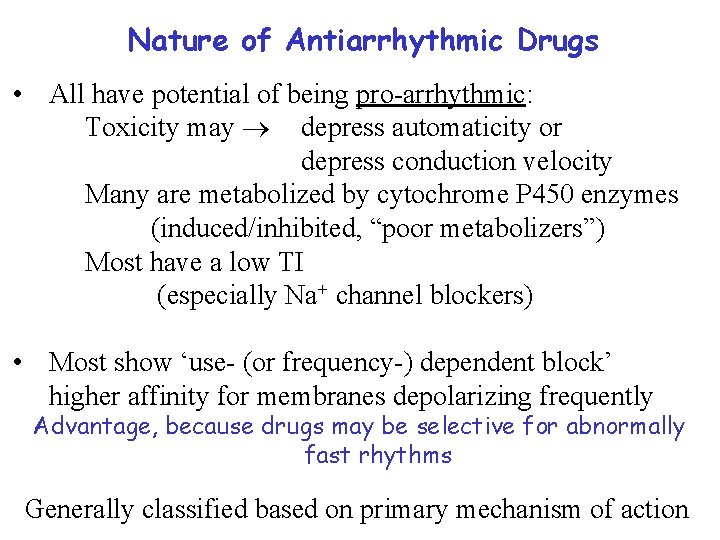
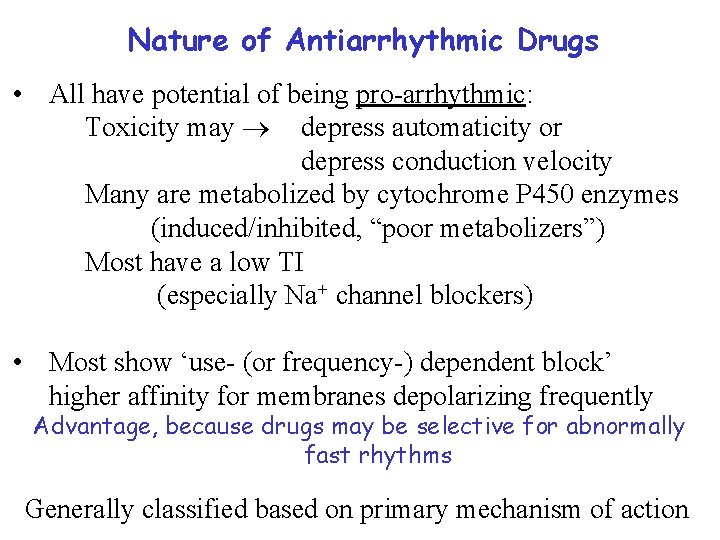
Nature of Antiarrhythmic Drugs • All have potential of being pro-arrhythmic: Toxicity may depress automaticity or depress conduction velocity Many are metabolized by cytochrome P 450 enzymes (induced/inhibited, “poor metabolizers”) Most have a low TI (especially Na+ channel blockers) • Most show ‘use- (or frequency-) dependent block’ higher affinity for membranes depolarizing frequently Advantage, because drugs may be selective for abnormally fast rhythms Generally classified based on primary mechanism of action
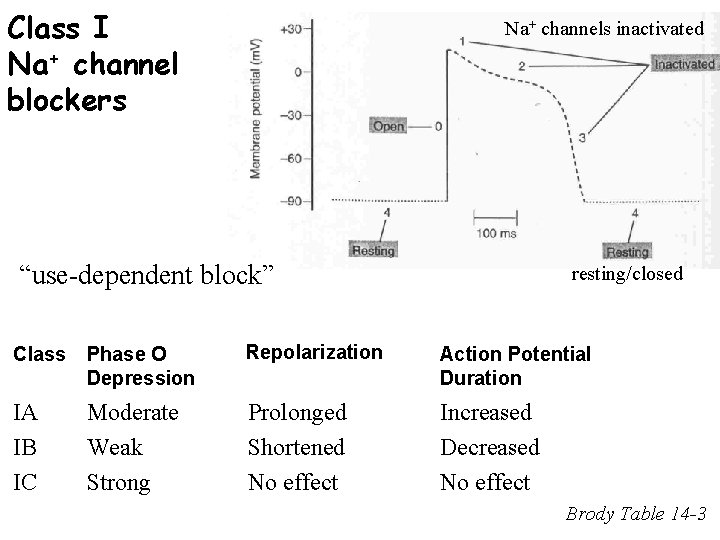
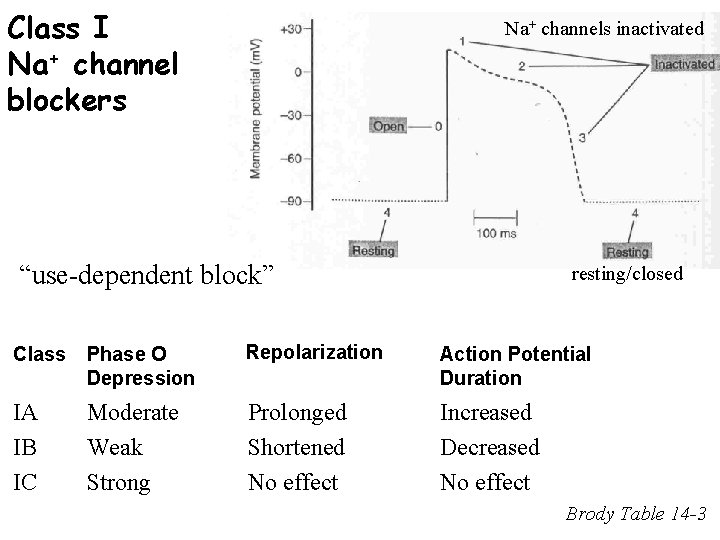
Class I Na+ channel blockers Na+ channels inactivated “use-dependent block” resting/closed Class Phase O Depression Repolarization Action Potential Duration IA IB IC Moderate Weak Strong Prolonged Shortened No effect Increased Decreased No effect Brody Table 14 -3
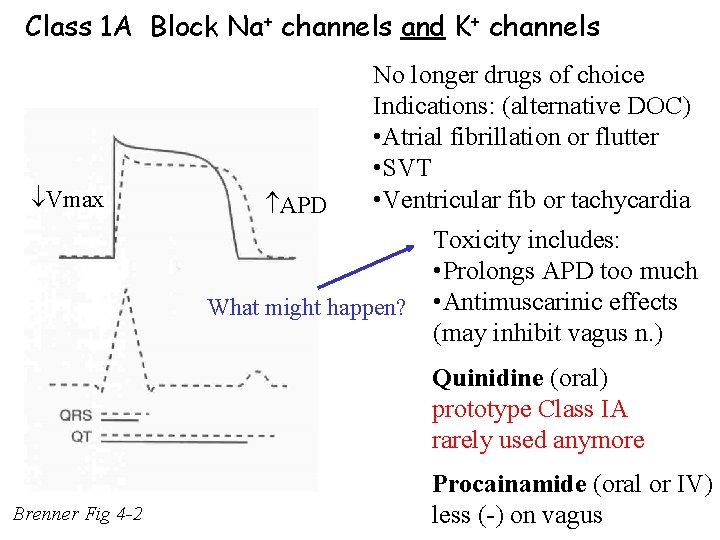
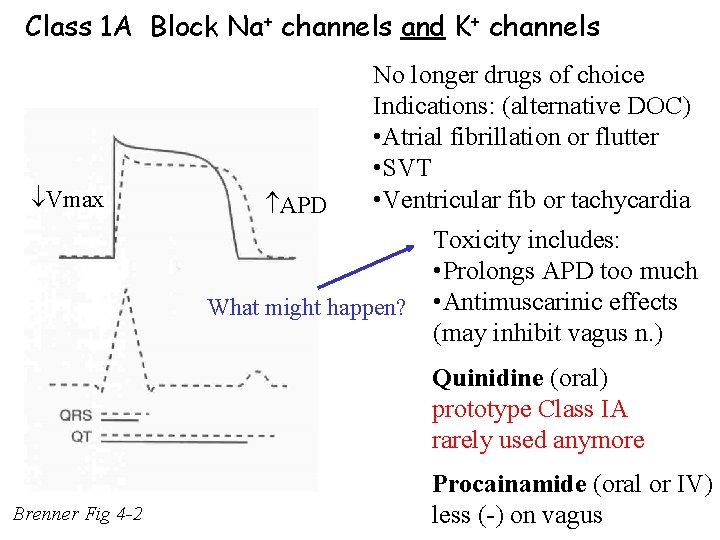
Class 1 A Block Na+ channels and K+ channels Vmax APD No longer drugs of choice Indications: (alternative DOC) • Atrial fibrillation or flutter • SVT • Ventricular fib or tachycardia What might happen? Toxicity includes: • Prolongs APD too much • Antimuscarinic effects (may inhibit vagus n. ) Quinidine (oral) prototype Class IA rarely used anymore Brenner Fig 4 -2 Procainamide (oral or IV) less (-) on vagus
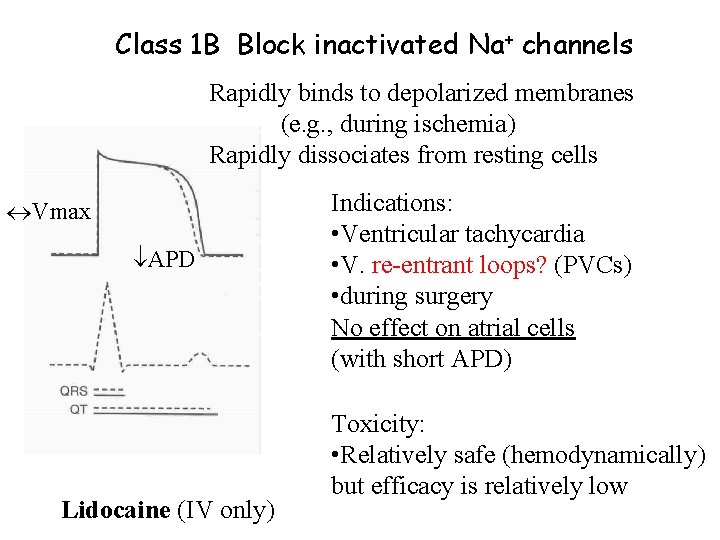
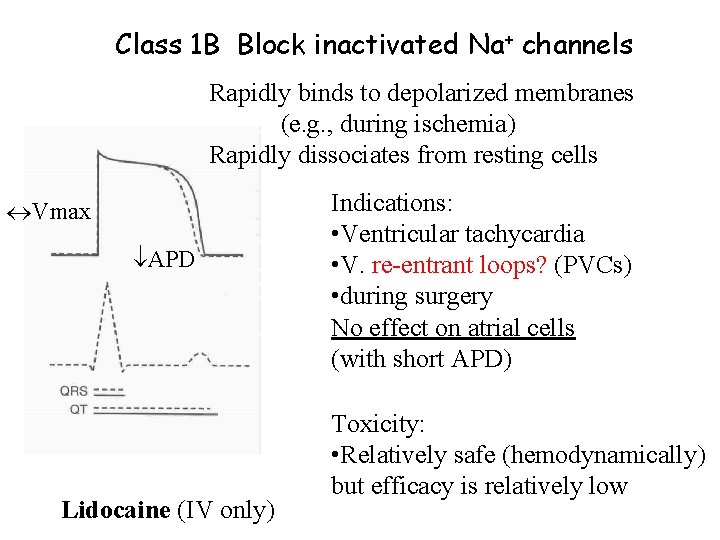
Class 1 B Block inactivated Na+ channels Rapidly binds to depolarized membranes (e. g. , during ischemia) Rapidly dissociates from resting cells Vmax APD Lidocaine (IV only) Indications: • Ventricular tachycardia • V. re-entrant loops? (PVCs) • during surgery No effect on atrial cells (with short APD) Toxicity: • Relatively safe (hemodynamically) but efficacy is relatively low
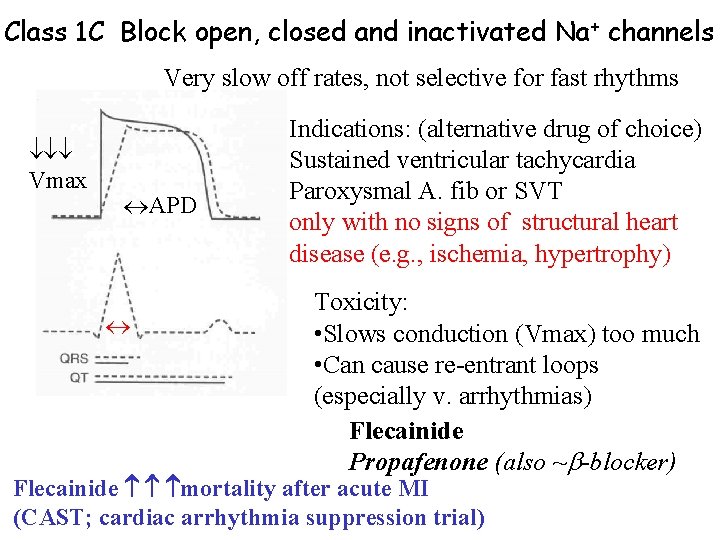
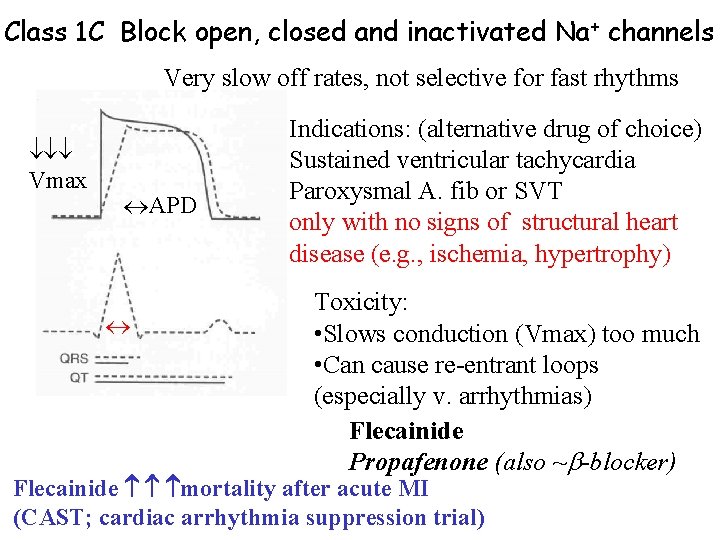
Class 1 C Block open, closed and inactivated Na + channels Very slow off rates, not selective for fast rhythms Vmax APD Indications: (alternative drug of choice) Sustained ventricular tachycardia Paroxysmal A. fib or SVT only with no signs of structural heart disease (e. g. , ischemia, hypertrophy) Toxicity: • Slows conduction (Vmax) too much • Can cause re-entrant loops (especially v. arrhythmias) Flecainide Propafenone (also ~ -blocker) Flecainide mortality after acute MI (CAST; cardiac arrhythmia suppression trial)
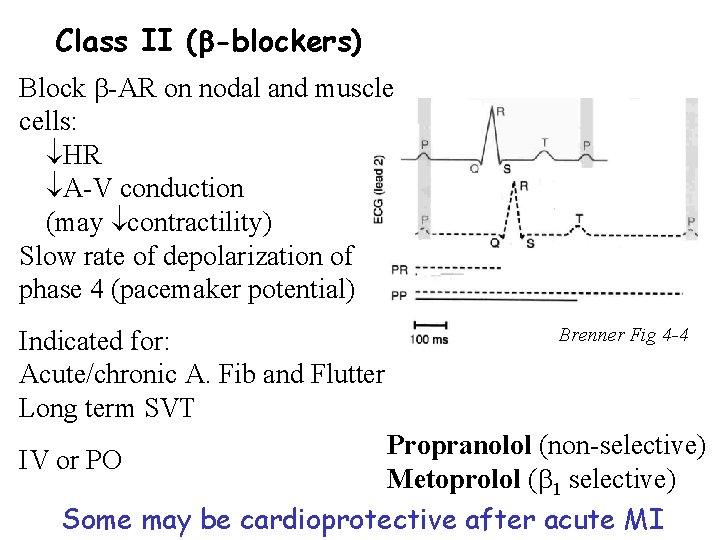
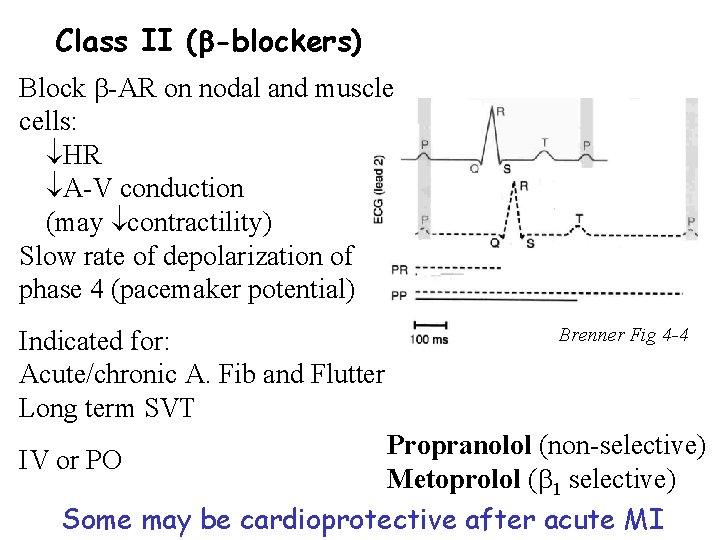
Class II ( -blockers) Block -AR on nodal and muscle cells: HR A-V conduction (may contractility) Slow rate of depolarization of phase 4 (pacemaker potential) Indicated for: Acute/chronic A. Fib and Flutter Long term SVT Brenner Fig 4 -4 Propranolol (non-selective) IV or PO Metoprolol ( 1 selective) Some may be cardioprotective after acute MI
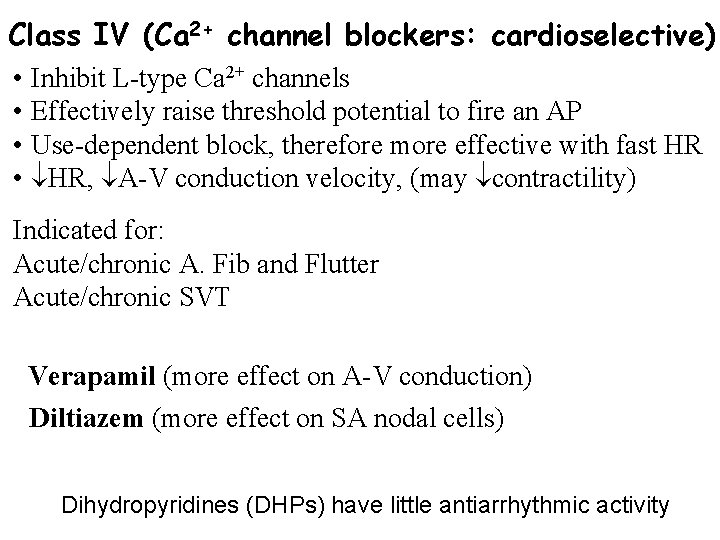
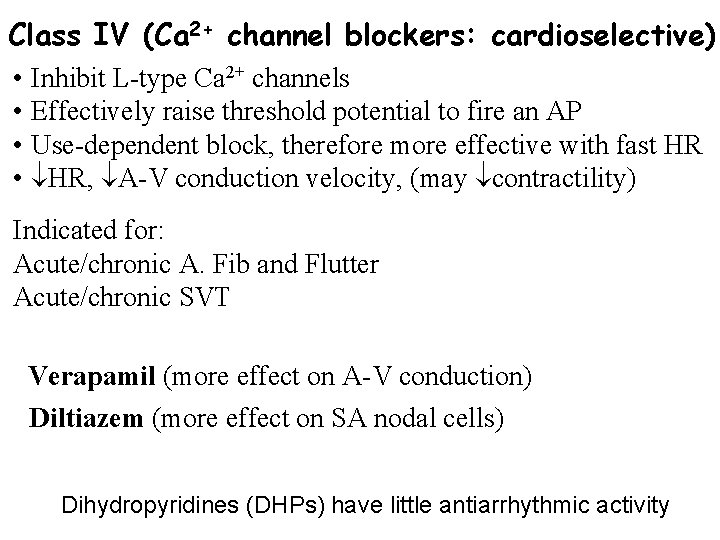
Class IV (Ca 2+ channel blockers: cardioselective) • Inhibit L-type Ca 2+ channels • Effectively raise threshold potential to fire an AP • Use-dependent block, therefore more effective with fast HR • HR, A-V conduction velocity, (may contractility) Indicated for: Acute/chronic A. Fib and Flutter Acute/chronic SVT Verapamil (more effect on A-V conduction) Diltiazem (more effect on SA nodal cells) Dihydropyridines (DHPs) have little antiarrhythmic activity
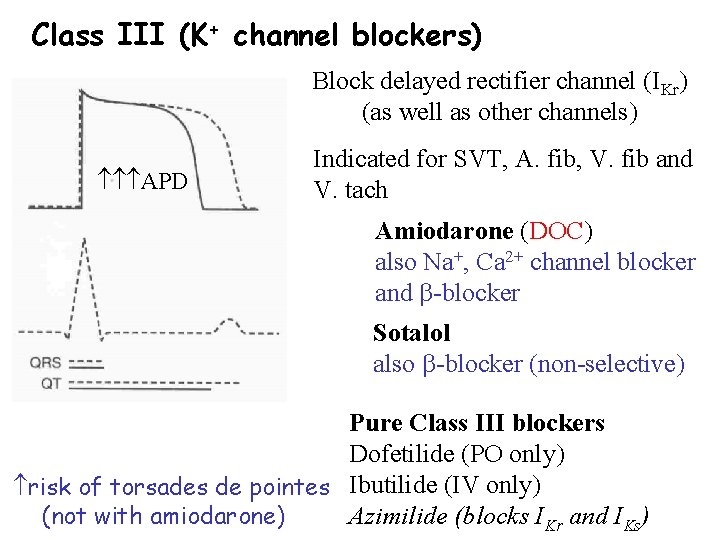
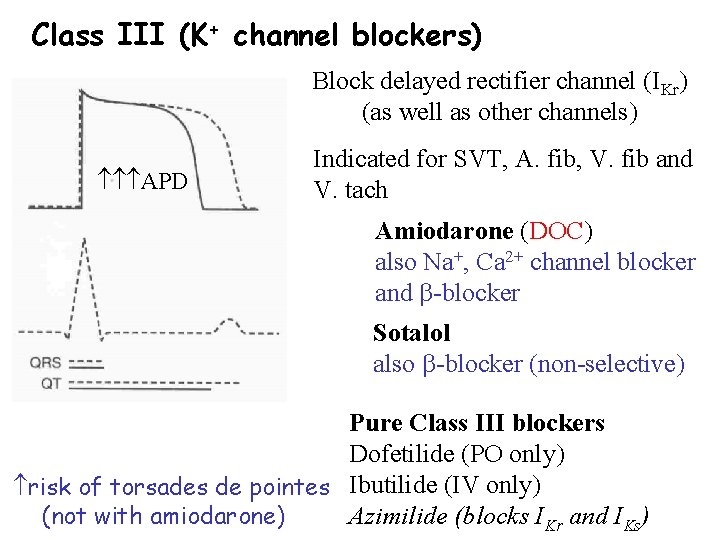
Class III (K+ channel blockers) Block delayed rectifier channel (IKr) (as well as other channels) APD Indicated for SVT, A. fib, V. fib and V. tach Amiodarone (DOC) also Na+, Ca 2+ channel blocker and -blocker Sotalol also -blocker (non-selective) Pure Class III blockers Dofetilide (PO only) risk of torsades de pointes Ibutilide (IV only) (not with amiodarone) Azimilide (blocks IKr and IKs)
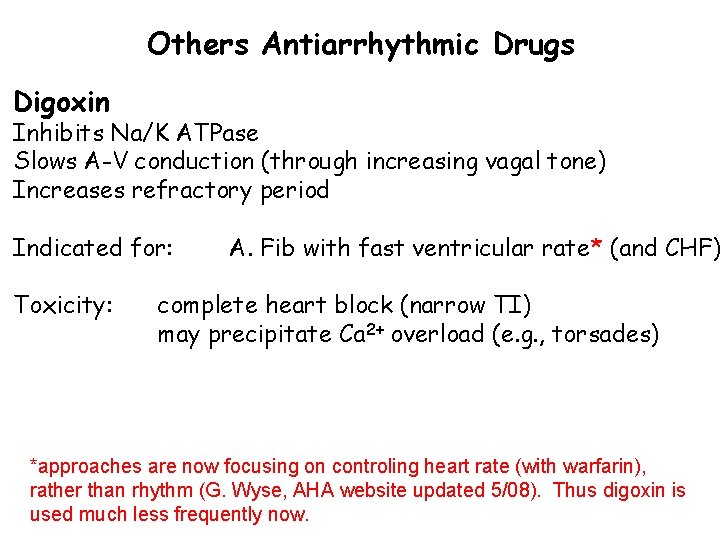
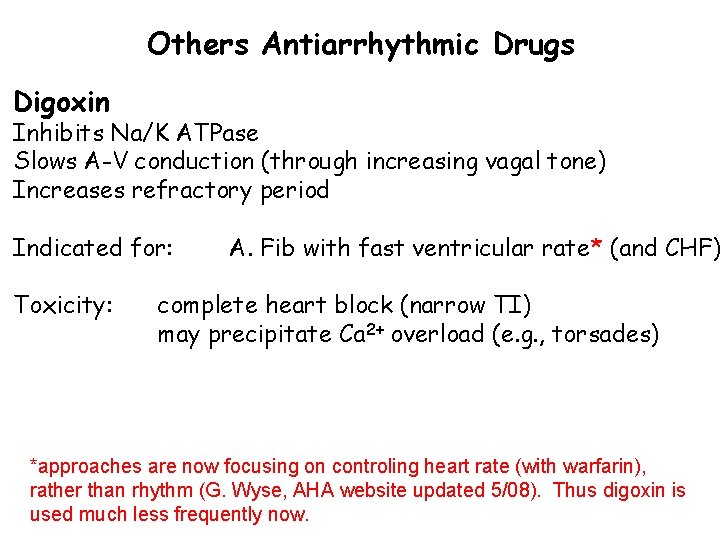
Others Antiarrhythmic Drugs Digoxin Inhibits Na/K ATPase Slows A-V conduction (through increasing vagal tone) Increases refractory period Indicated for: Toxicity: A. Fib with fast ventricular rate* (and CHF) complete heart block (narrow TI) may precipitate Ca 2+ overload (e. g. , torsades) *approaches are now focusing on controling heart rate (with warfarin), rather than rhythm (G. Wyse, AHA website updated 5/08). Thus digoxin is used much less frequently now.
![Digoxin Cardiac effects Increases intracellular Na increases in Ca 2 via NCX more Ca Digoxin: Cardiac effects: Increases intracellular [Na+], increases in Ca 2+ (via NCX) more Ca](https://slidetodoc.com/presentation_image_h/0ee8b15a1b4344a6467184e9b4fde2f9/image-29.jpg)
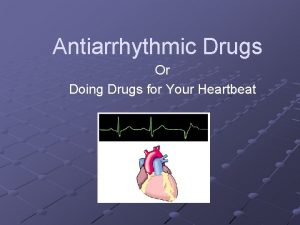
Digoxin: Cardiac effects: Increases intracellular [Na+], increases in Ca 2+ (via NCX) more Ca 2+ to trigger SR Ca 2+ release, increases contraction (positive inotropic effects, discussed in heart failure lecture) Decreases intracellular [K+], depolarizes membrane potential partially inactivates Na+ channels in fast fibers, reduces excitability, slows conduction High affinity to vagus nerve (particularly at the AV node), increases vagal tone slows AV nodal conduction Binds to, and inhibits Na+/K+ ATPase pumps in other tissues (noncardiac toxicities include visual distrubances -yellow hues), with highest affinity to cardiac and vagal nerve.
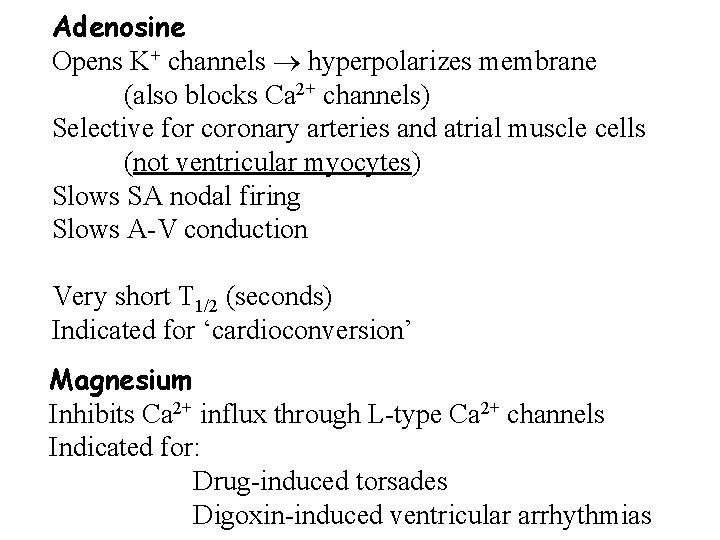
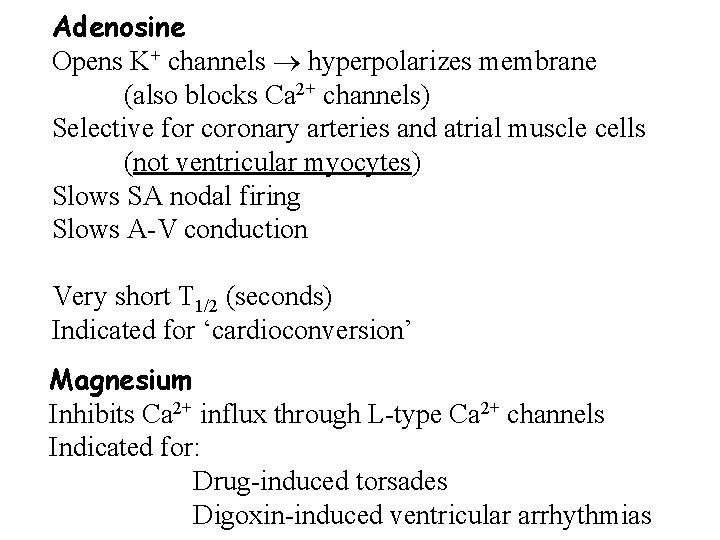
Adenosine Opens K+ channels hyperpolarizes membrane (also blocks Ca 2+ channels) Selective for coronary arteries and atrial muscle cells (not ventricular myocytes) Slows SA nodal firing Slows A-V conduction Very short T 1/2 (seconds) Indicated for ‘cardioconversion’ Magnesium Inhibits Ca 2+ influx through L-type Ca 2+ channels Indicated for: Drug-induced torsades Digoxin-induced ventricular arrhythmias
![Triggered activity due too much intracellular Ca 2 Ca 2i Mg 2 for torsades Triggered activity due too much intracellular Ca 2+ [Ca 2+]i Mg 2+ (for torsades)](https://slidetodoc.com/presentation_image_h/0ee8b15a1b4344a6467184e9b4fde2f9/image-31.jpg)
Triggered activity due too much intracellular Ca 2+ [Ca 2+]i Mg 2+ (for torsades) Na/Ca exchange (3 Na+(in): 1 Ca 2+(out)) Open L-type Ca 2+ channels [Na+]i (depolarize membrane)
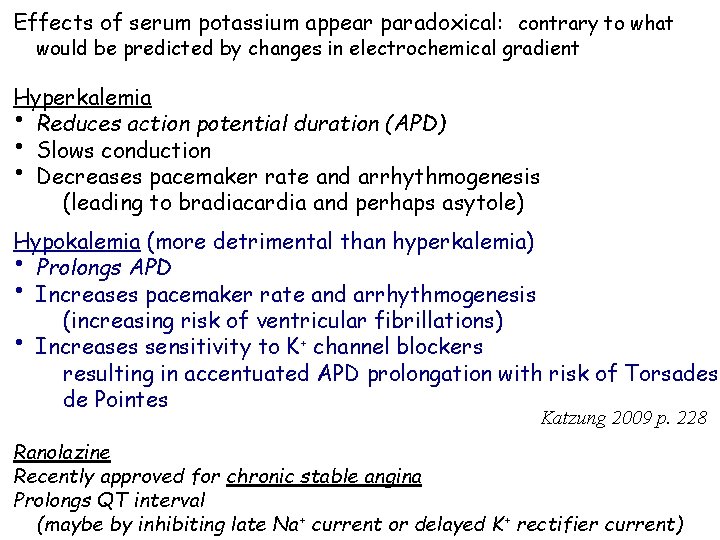
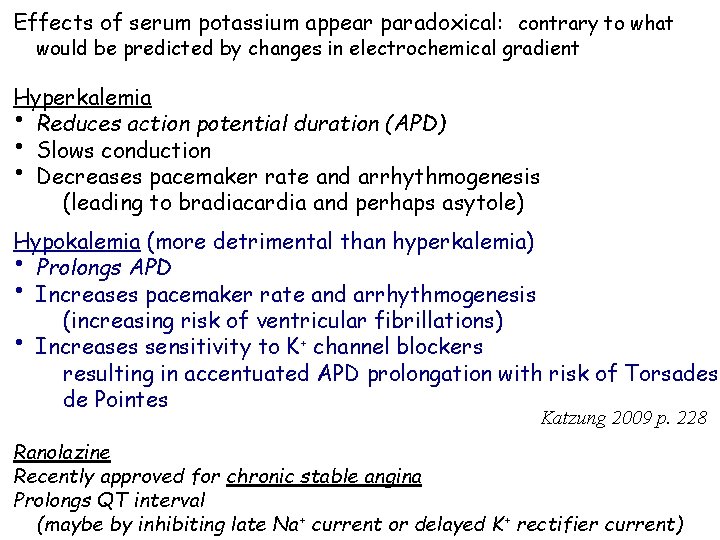
Effects of serum potassium appear paradoxical: contrary to what would be predicted by changes in electrochemical gradient Hyperkalemia • Reduces action potential duration (APD) • Slows conduction • Decreases pacemaker rate and arrhythmogenesis (leading to bradiacardia and perhaps asytole) Hypokalemia (more detrimental than hyperkalemia) • Prolongs APD • Increases pacemaker rate and arrhythmogenesis (increasing risk of ventricular fibrillations) • Increases sensitivity to K+ channel blockers resulting in accentuated APD prolongation with risk of Torsades de Pointes Katzung 2009 p. 228 Ranolazine Recently approved for chronic stable angina Prolongs QT interval (maybe by inhibiting late Na+ current or delayed K+ rectifier current)
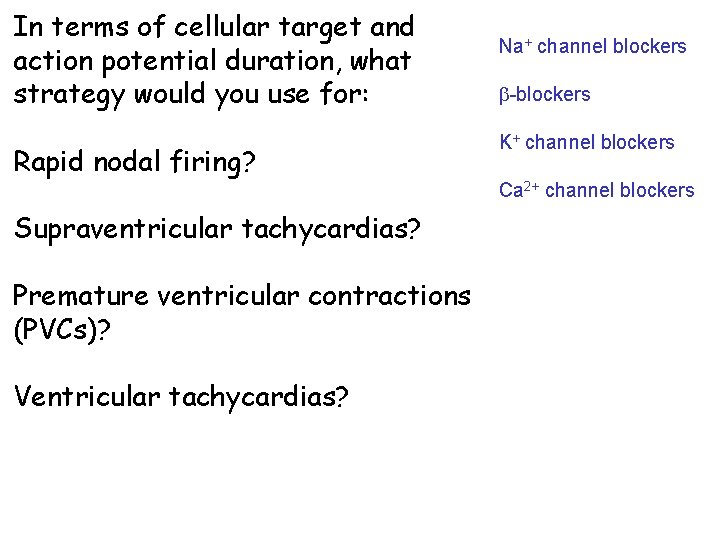
In terms of cellular target and action potential duration, what strategy would you use for: Rapid nodal firing? Na+ channel blockers -blockers K+ channel blockers Ca 2+ channel blockers Supraventricular tachycardias? Premature ventricular contractions (PVCs)? Ventricular tachycardias?
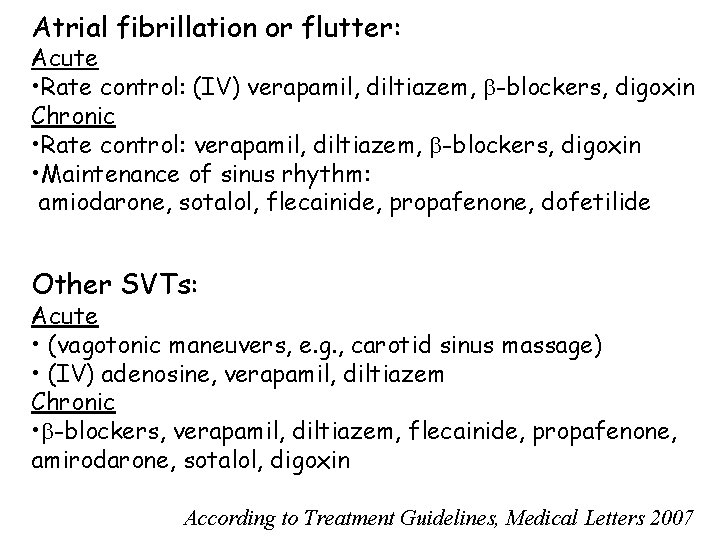
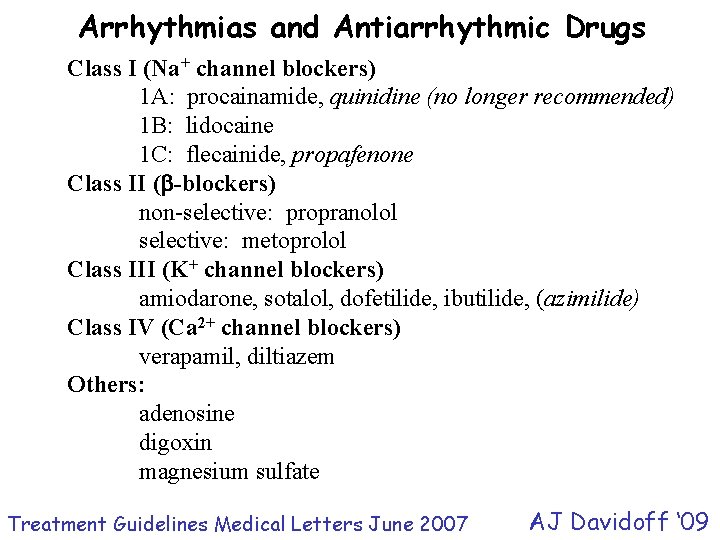
Atrial fibrillation or flutter: Acute • Rate control: (IV) verapamil, diltiazem, -blockers, digoxin Chronic • Rate control: verapamil, diltiazem, -blockers, digoxin • Maintenance of sinus rhythm: amiodarone, sotalol, flecainide, propafenone, dofetilide Other SVTs: Acute • (vagotonic maneuvers, e. g. , carotid sinus massage) • (IV) adenosine, verapamil, diltiazem Chronic • -blockers, verapamil, diltiazem, flecainide, propafenone, amirodarone, sotalol, digoxin According to Treatment Guidelines, Medical Letters 2007

PVCs or non-sustained V. tach: Asymptomatic • no therapy Symptomatic (flecainide is contraindicated post-MI) • -blockers (post MI improves mortality rates) Sustained V. tach. or V. fib: Acute DC cardioversion is safest • amiodarone Chronic • Implantable cardiac defribillator (ICD) (NEJM Jan 20, 2005) • amiodarone, plus a -blocker According to Medical Letters
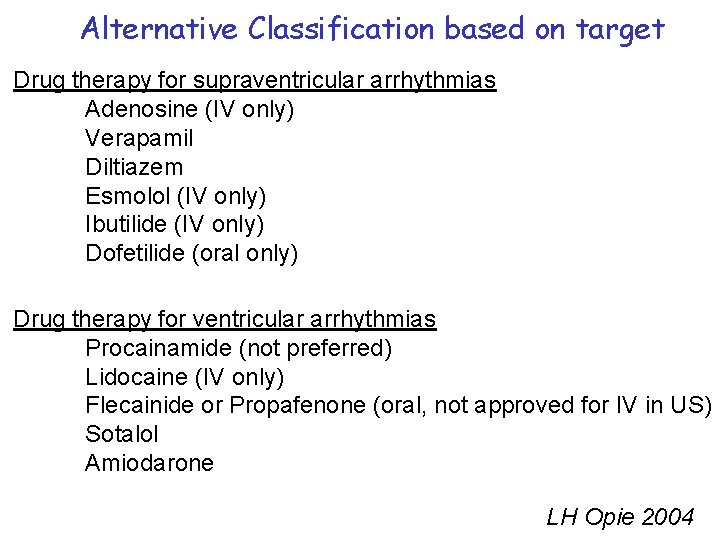
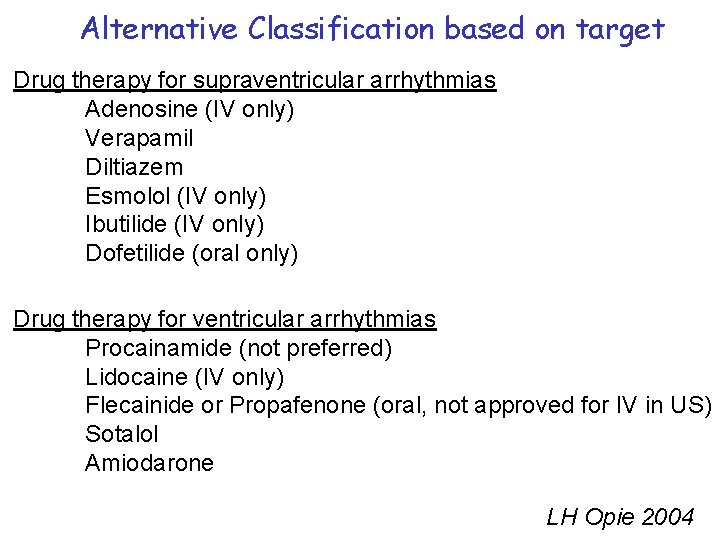
Alternative Classification based on target Drug therapy for supraventricular arrhythmias Adenosine (IV only) Verapamil Diltiazem Esmolol (IV only) Ibutilide (IV only) Dofetilide (oral only) Drug therapy for ventricular arrhythmias Procainamide (not preferred) Lidocaine (IV only) Flecainide or Propafenone (oral, not approved for IV in US) Sotalol Amiodarone LH Opie 2004
 Chronotropic
Chronotropic Flecainide mechanism of action
Flecainide mechanism of action M
M Classification of antiarrhythmic drugs with examples
Classification of antiarrhythmic drugs with examples Cardioversion anticoagulation
Cardioversion anticoagulation Antiarrhythmic drugs mechanism of action
Antiarrhythmic drugs mechanism of action Svt pregnancy
Svt pregnancy Antiarrhythmic drugs classification
Antiarrhythmic drugs classification Amirodarone
Amirodarone Multichannel retail
Multichannel retail Signal space analysis in digital communication
Signal space analysis in digital communication Determine id
Determine id Examples of class c drugs in uganda
Examples of class c drugs in uganda Abstract class vs concrete class
Abstract class vs concrete class Abstract concrete class relationship
Abstract concrete class relationship 7 rights of medication administration in order
7 rights of medication administration in order Static vs dynamic class loading
Static vs dynamic class loading Remains poem summary
Remains poem summary What about today's class
What about today's class Putting a package together
Putting a package together Lower class boundary of the modal class
Lower class boundary of the modal class Class i vs class ii mhc
Class i vs class ii mhc How do i find the class width
How do i find the class width Response class vs stimulus class
Response class vs stimulus class Discriminative stimulus psychology definition
Discriminative stimulus psychology definition Class maths student student1 class student string name
Class maths student student1 class student string name Unordered stem and leaf plot
Unordered stem and leaf plot In greenfoot, you can cast an actor class to a world class?
In greenfoot, you can cast an actor class to a world class? Class 0 esd
Class 0 esd Static class diagram
Static class diagram Class 2 class 3
Class 2 class 3 Public class test subject extends test class
Public class test subject extends test class Package mypackage class first class body
Package mypackage class first class body Class third class
Class third class C++ class implementation
C++ class implementation Component class has composite class as collaborator
Component class has composite class as collaborator Intradermal drug administration
Intradermal drug administration