Antiarrhythmic Drugs Dr Naza M Ali Lec 5












- Slides: 41

Antiarrhythmic Drugs Dr. Naza M. Ali Lec. 5 -6 May 21 -2017
Objective and Outlines Cardiac arrhythmias Nature of Arrhythmias Phases of action potential Classification of antiarrhythmic drugs
• Cardiac arrhythmias commonly occur in the presence of preexisting heart disease. • They are the most common cause of death in patient with MI or terminal heart failure. • They are also the most serious manifestation of digitalis toxicity and are often associated with anesthesia, hyperthyroidism, electrolyte disorders.
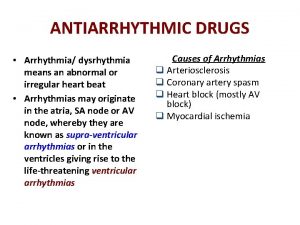
• Any rhythm that is not normal sinus rhythm is an arrhythmia. Arrhythmia: is an abnormality of heart rhythm 1. Heart rate increased/ decreased Tachycardia when heart rate fast >100 beats/min Bradycardia when heart rate slow< 60 beats/min 2. Heart rhythm ( regular / irregular) 3. Site of origin ( supraventricular / ventricular)
Nature of Arrhythmias Normal electrical cardiac function (normal sinus rhythm) • Is dependent on generation of an impulse in the normal SA node pacemaker & its conduction through the atrial muscle, through the AV node, through the Purkinje conduction system, to the ventricular muscle. • Thus, require normal action potentials (dependent on sodium, calcium, and potassium channel activity) under appropriate autonomic control.


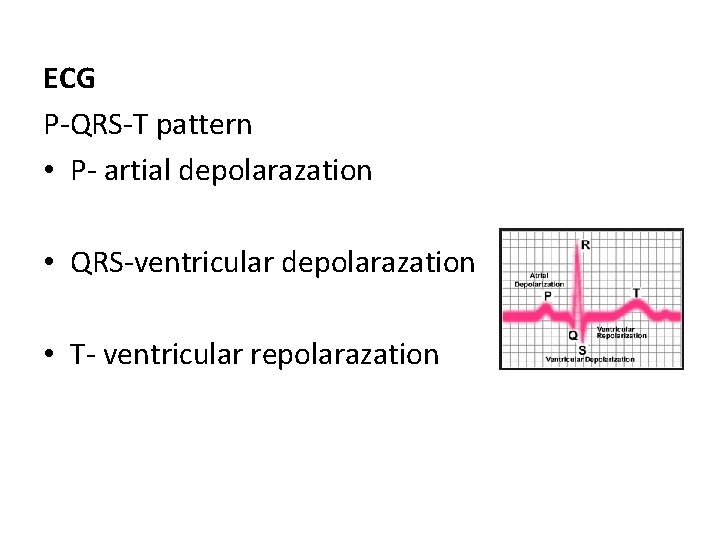
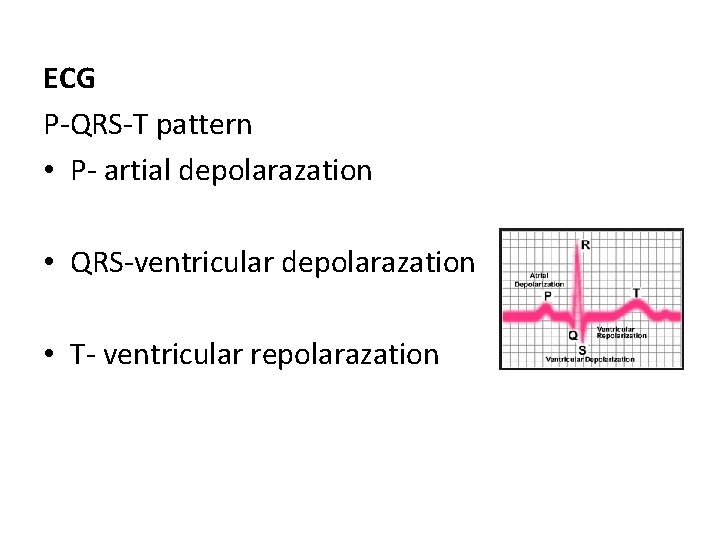
ECG P-QRS-T pattern • P- artial depolarazation • QRS-ventricular depolarazation • T- ventricular repolarazation
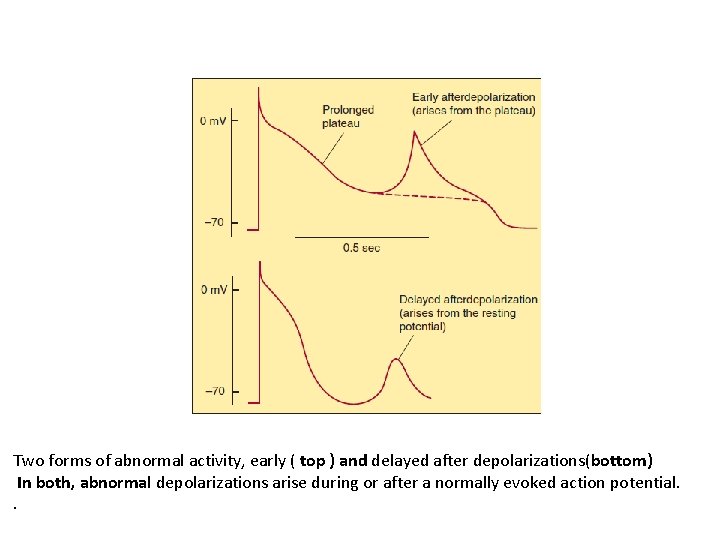
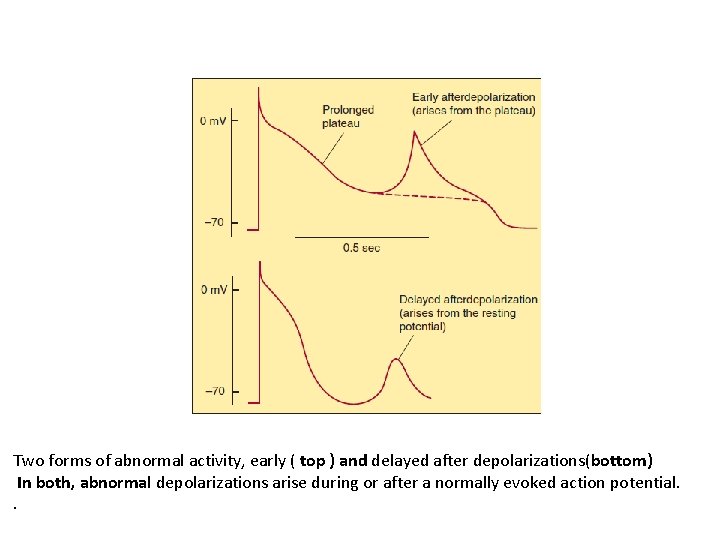
Two forms of abnormal activity, early ( top ) and delayed after depolarizations(bottom) In both, abnormal depolarizations arise during or after a normally evoked action potential. .
Sinus rhythm • Sinoatrial node is cardiac pacemaker • Is controlled by autonomic nervous system • Parasympathetic system predominantes (M 2 muscarinic receptors) • Sympathetic system (β 1 receptors) -increased heart rate (positive chronotropic effect) -Increased automaticity -Facilitation of conduction of AV node
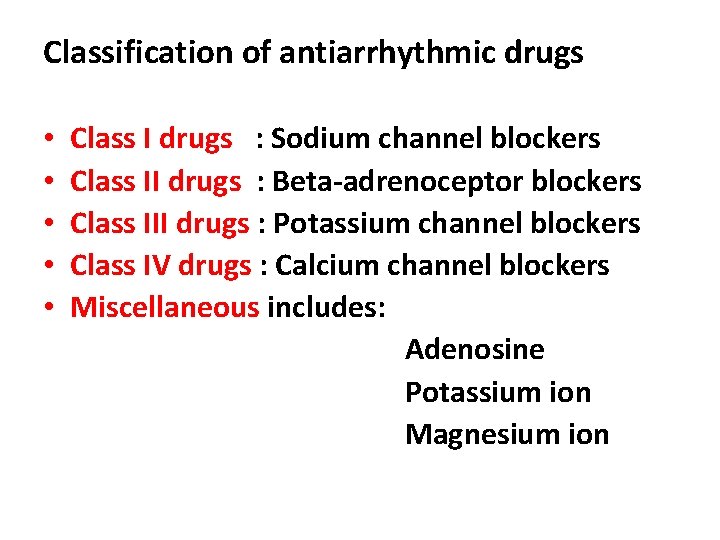
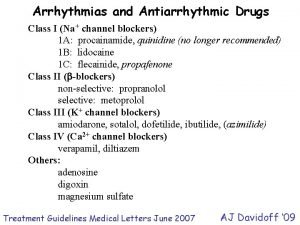
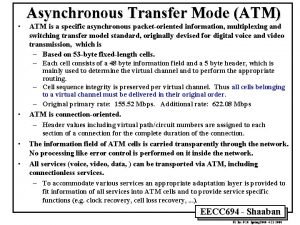
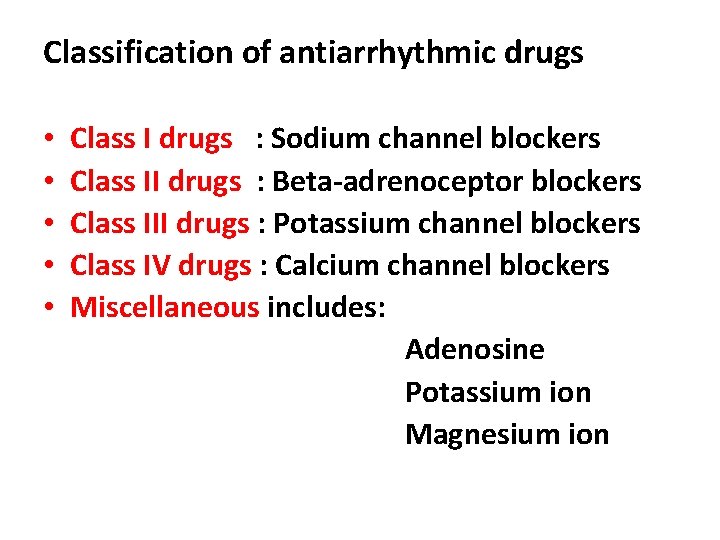
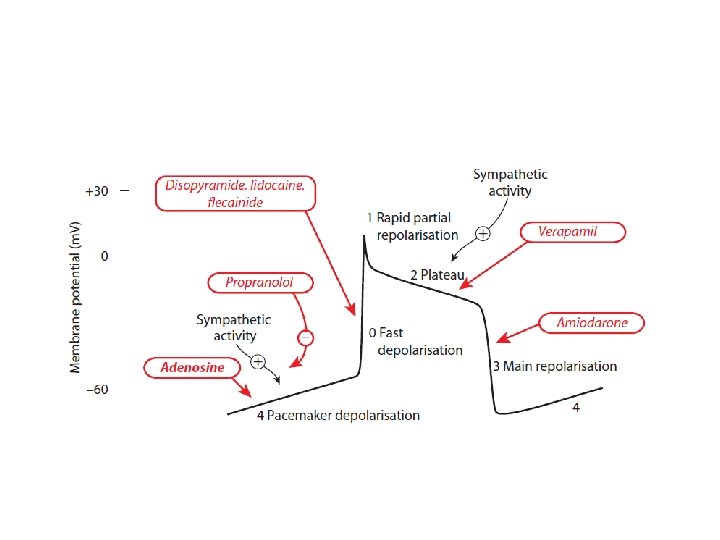
Classification of antiarrhythmic drugs • • • Class I drugs : Sodium channel blockers Class II drugs : Beta-adrenoceptor blockers Class III drugs : Potassium channel blockers Class IV drugs : Calcium channel blockers Miscellaneous includes: Adenosine Potassium ion Magnesium ion
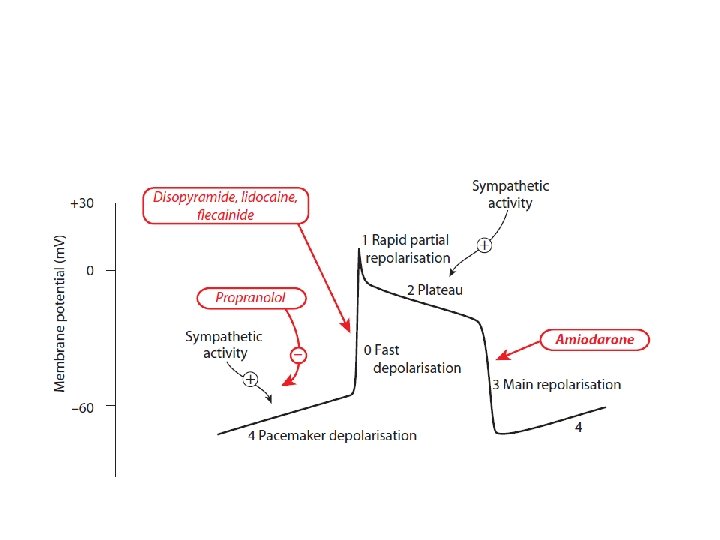
Class I drugs : Sodium channel blockers • • They are the oldest group With local anesthetic action Block sodium channels Reduce the sodium current, I Na
The central concept is of use–dependent channel block • It is this characteristic that enables all class I drugs to block the high frequency excitation of the myocardium that occurs in tachyarrhythmias, without preventing the heart from beating at normal frequencies. • Na channels exist in three distinct functional states resting , open and inactivated. • Channels switch rapidly from resting to open in response to depolarization this is known as activation.
• Maintained depolarization as in ischemic muscle, cause channels to change more slowly from open to inactivated • Class I bind to channels most strongly when they are either in the open or the inactivated state, less strongly to channels in resting state. • Their action therefore shows the property of use dependence( the more frequently the channels are activated, the greater degree of block produced).
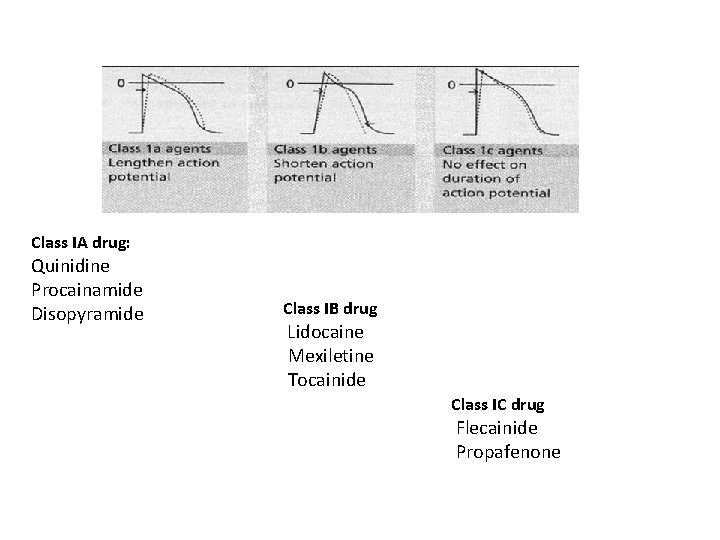
• The Class I drugs are subdivide on the basis of their effects on action potential duration. Class IA drug: Quinidine, Procainamide Disopyramide Class IB drug Lidocaine Mexiletine Tocainide Class IC drug Flecainide Propafenone
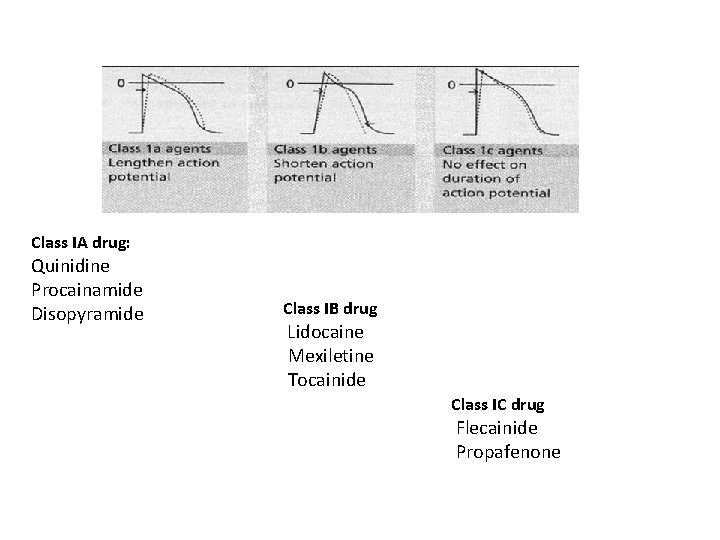
Class IA drug: Quinidine Procainamide Disopyramide Class IB drug Lidocaine Mexiletine Tocainide Class IC drug Flecainide Propafenone
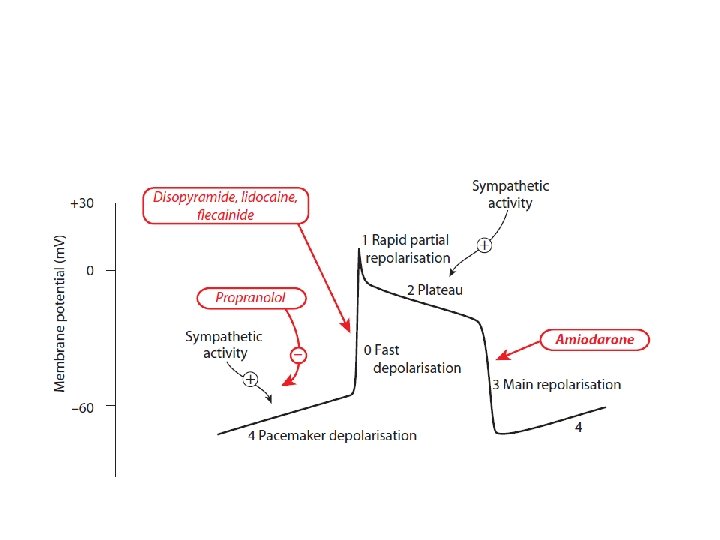
Mechanism of action of Class IA Quinidine • binds to open and inactivated sodium channels and prevents sodium influx, • It decreases the slope of Phase 4 spontaneous depolarization and inhibit potassium channels. • The IA drugs block potassium current
Class IA action Quinidine • Cinchona plant • Block Na channel • Use for atrial fibrillation • Ventricular tachycardia • Half life 6 -8 hrs. Side effects -GIT / NVD -A syndrome of headache, dizziness, and tinnitus (cinchonism) is observed at toxic drug concentration -Hypersensitivity reactions

Class I
Class IB action Lidocaine • Rapidly associate and dissociate from sodium channels. • decreases the duration of the action potential • Drug of choice for emergency treatment of cardiac arrhythmias. • is useful in treating ventricular arrhythmias arising during myocardial ischemia • Lidocaine IV ( because of extensive first-pass transformation)
Class IC action Flecainide • Have no effect on AP duration • Powerful depressants of sodium currents • slowly dissociate from resting sodium channels • Several studies by CAST a large clinical trial of the prophylactic use of class IC drugs in MI survivors. • The trail results showed that class IC drugs caused greater mortality than placebo. • For this reason , are now restricted to use in persistent arrhythmias that fail to responds to other drugs.
Class II drugs: β-adrenergic Blockers • Diminish Phase 4 depolarization, and decreasing heart rate and contractility. • useful in treating tachyarrhythmias caused by increased sympathetic activity. • They are also used for atrial flutter and fibrillation and for AV-nodal reentrant tachycardia.
Propranolol • Reduces incidence of sudden arrhythmic death after MI • Use as prophylactic in patient who have had a MI Metoprolol • Reduce the risk of bronchospasm Esmolol • is a very short-acting used IV in acute arrhythmias that occur during surgery or emergency situations.
Class III drugs: Potassium channel blockers Dofetilide Ibutilide Amiodarone Dronedarone Sotalol
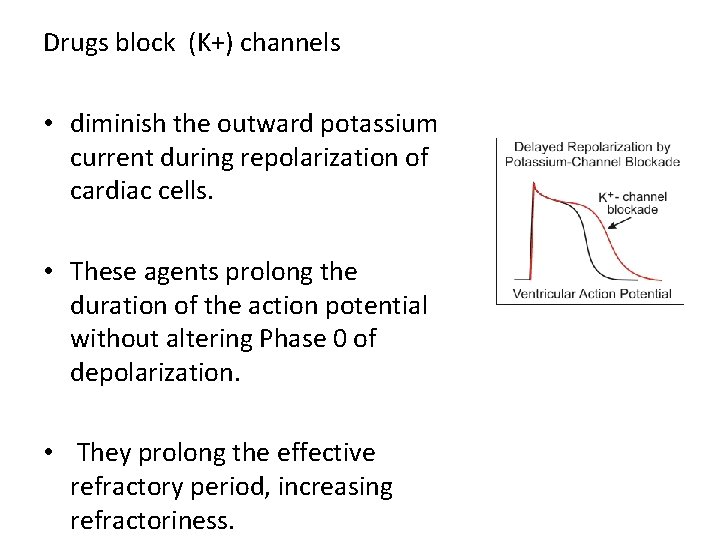
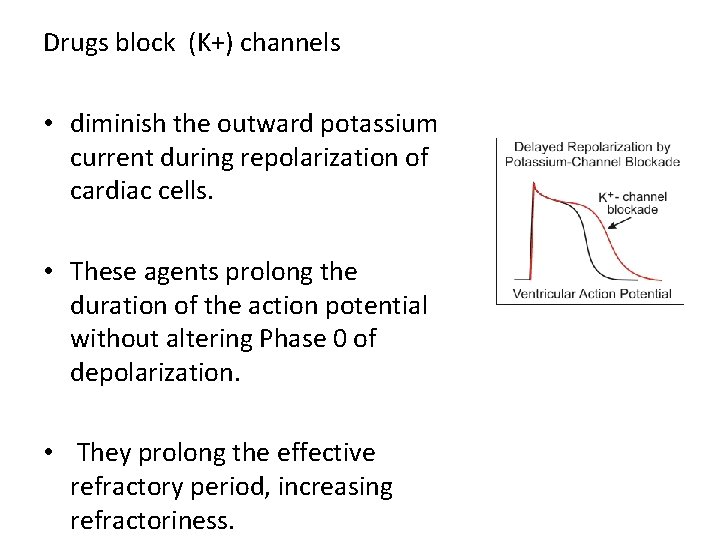
Drugs block (K+) channels • diminish the outward potassium current during repolarization of cardiac cells. • These agents prolong the duration of the action potential without altering Phase 0 of depolarization. • They prolong the effective refractory period, increasing refractoriness.


Amiodarone • It has complex effects, showing Class I, III & IV actions. • Its multiple classes of action • Its dominant effect is prolongation of action potential duration and the refractory period. • use in the treatment of severe refractory supraventricular and ventricular tachyarrhythmias. • its broad spectrum of antiarrhythmic action, it is very extensively used for a wide variety of arrhythmias.
• Incompletely absorbed after oral administration. • The drug have a prolonged half life of several weeks, and it distributes extensively in adipose tissue. • Full clinical effects may not be achieved until 6 weeks after initiation of treatment, unless loading doses are employed. • The drug accumulates in many tissues, including the heart (10– 50 times more so than in plasma), lung, liver, and skin, and is concentrated in tears.

Amiodarone shows a variety of toxic effects: Pulmonary fibrosis, hyper- or hypothyroidism, blue skin discoloration caused by iodine accumulation in the skin.
Dronedarone • Amiodarone derivative, which is less lipophilic, has lower tissue accumulation, and has a shorter serum half-life than amiodarone. • It does not have the iodine moieties that are responsible for thyroid dysfunction associated with amiodarone. • Like amiodarone, it has class I, III, and IV actions. • Currently, dronedarone is used to maintain sinus rhythm in atrial fibrillation or flutter, but it is less effective than amiodarone.

Sotalol • has potent nonselective β-blocker activity. • has 2 stereoisomers with different pharmacological activity • The levorotatory isomer ( l-sotalol) is responsible for the β-blocker activity • d-sotalol for the Class III antiarrhythmic action. • Sotalol blocks a rapid outward potassium current

• Used for long-term therapy to decrease the rate of sudden death following an acute MI • β-Blockers have a modest ability to suppress ectopic beats and to reduce myocardial oxygen demand. • Sotalol was more effective in preventing recurrence of arrhythmia
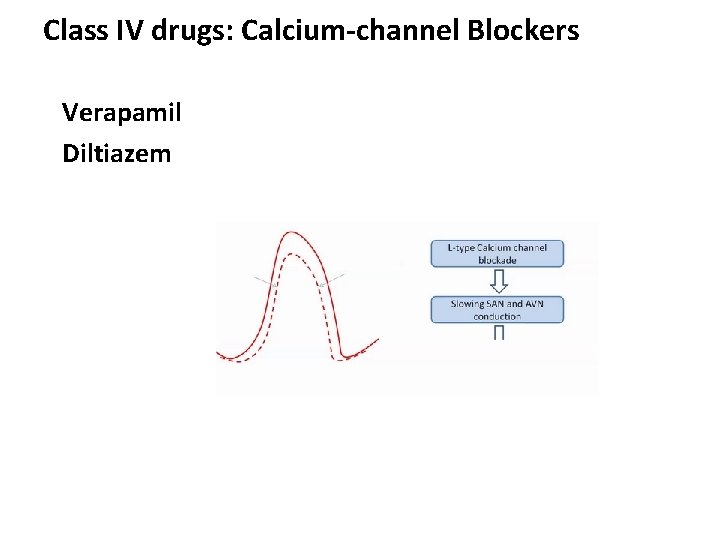
Class IV drugs: Calcium-channel Blockers Verapamil Diltiazem

• They decrease the inward current carried by (Ca 2+), • Slow conduction in tissues that are dependent on calcium currents, such as the AV node • are more effective against atrial than against ventricular arrhythmias.


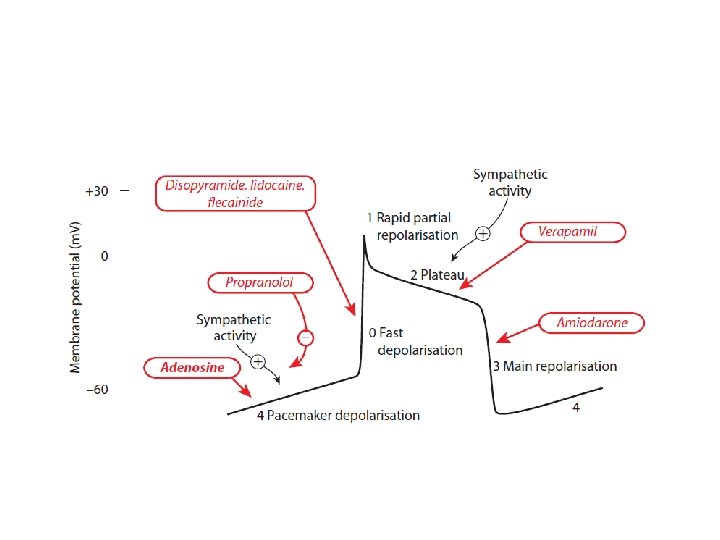
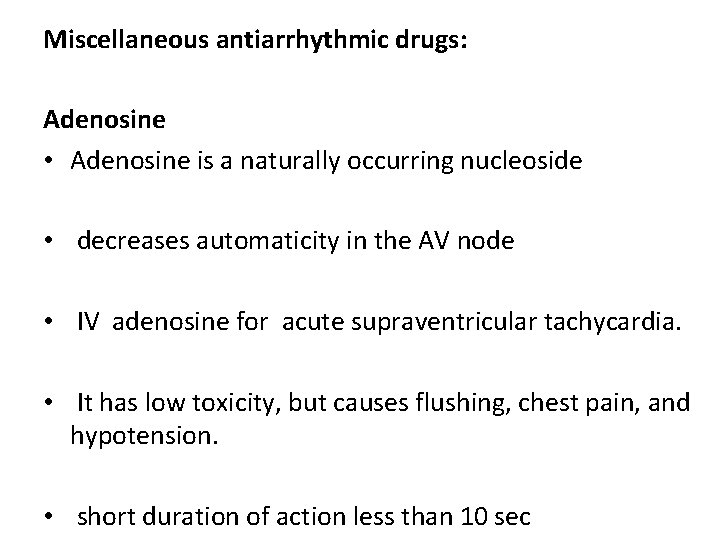
Miscellaneous antiarrhythmic drugs: Adenosine • Adenosine is a naturally occurring nucleoside • decreases automaticity in the AV node • IV adenosine for acute supraventricular tachycardia. • It has low toxicity, but causes flushing, chest pain, and hypotension. • short duration of action less than 10 sec
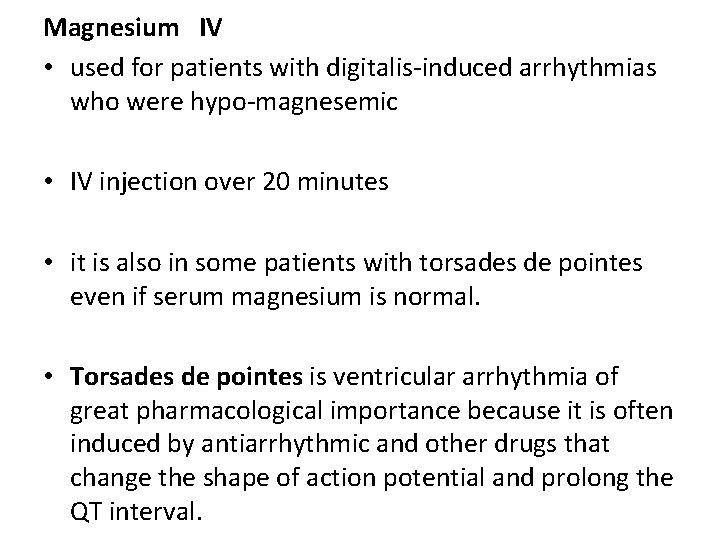
Magnesium IV • used for patients with digitalis-induced arrhythmias who were hypo-magnesemic • IV injection over 20 minutes • it is also in some patients with torsades de pointes even if serum magnesium is normal. • Torsades de pointes is ventricular arrhythmia of great pharmacological importance because it is often induced by antiarrhythmic and other drugs that change the shape of action potential and prolong the QT interval.
Potassium • Hypokalemia results in an increased risk of early and delayed after depolarizations, and ectopic pacemaker activity, especially in the presence of digitalis. • Hyperkalemia depresses ectopic pacemakers
 Antiarrhythmic drugs classification
Antiarrhythmic drugs classification Classes of antiarrhythmic drugs
Classes of antiarrhythmic drugs Af begets af
Af begets af Lidocaine in cardiac arrest
Lidocaine in cardiac arrest Class 1a antiarrhythmic drugs
Class 1a antiarrhythmic drugs Negative chronotropic effect of digoxin
Negative chronotropic effect of digoxin Antiarrhythmic drugs mechanism of action
Antiarrhythmic drugs mechanism of action Classification of antiarrhythmic drugs with examples
Classification of antiarrhythmic drugs with examples Lektira nosac samuel sve price
Lektira nosac samuel sve price Dr naza
Dr naza Safest antiarrhythmic drug
Safest antiarrhythmic drug Lec ditto
Lec ditto Tura analítica
Tura analítica Lec hardver
Lec hardver August lec 250
August lec 250 Diesel lec
Diesel lec Lec
Lec Componentes del lec
Componentes del lec History of software development life cycle
History of software development life cycle Scoreboarding computer architecture
Scoreboarding computer architecture Sekisui slec
Sekisui slec Lec renal
Lec renal Lec 16
Lec 16 Scoreboard architecture
Scoreboard architecture 132000 lec
132000 lec Xyloprin
Xyloprin 11th chemistry thermodynamics lec 10
11th chemistry thermodynamics lec 10 416 lec
416 lec 252 lec
252 lec Lec 1
Lec 1 Lec promotion
Lec promotion 11th chemistry thermodynamics lec 13
11th chemistry thermodynamics lec 13 Ir.ac.kashanu.register://h
Ir.ac.kashanu.register://h Lec barbate
Lec barbate Lec element
Lec element Lec
Lec Art 455 lec
Art 455 lec Lec anatomia
Lec anatomia Storage and maintenance of drugs
Storage and maintenance of drugs Atropine substitutes mnemonic
Atropine substitutes mnemonic Duvadilan drip preterm labour
Duvadilan drip preterm labour Bronchodilators
Bronchodilators