Device and Antiarrhythmic Drugs Advantages and Pitfalls Teresa
- Slides: 12
Device and Antiarrhythmic Drugs: Advantages and Pitfalls Teresa Menendez Hood, M. D.
Implantable cardioverter defibrillators (ICDs) and antiarrhythmic drugs (AAD) • ICDs have been proven successful in treating life-threatening ventricular arrhythmias • Antiarrhythmic drug therapy now has a palliative role in the treatment of ventricular arrhythmias • The use of both results in beneficial and adverse interactions
Trends of AAD use in patients with ICDs • Decrease in use of AAD in patients with ICDs over the last 10 years – The largest decrease has been in Class 1 agents while the Class 3 agents have actually increased (amiodarone and sotalol) • Currently, about 20% - 40% of patients with an ICD are also on an AAD – The most common reason that a patient gets put on an AAD is frequent ICD shocks • More of a decline in AAD is seen in patients with cardiac arrest and syncope than in patients with sustained VT • Amiodarone is the most common AAD used with ICDs
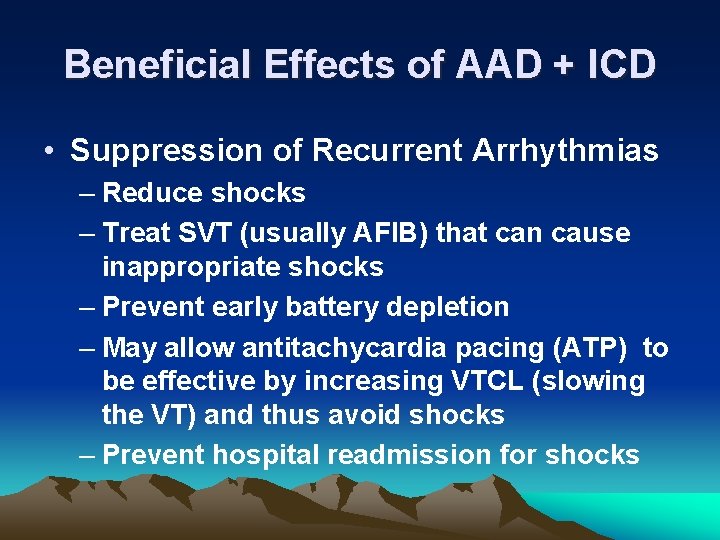
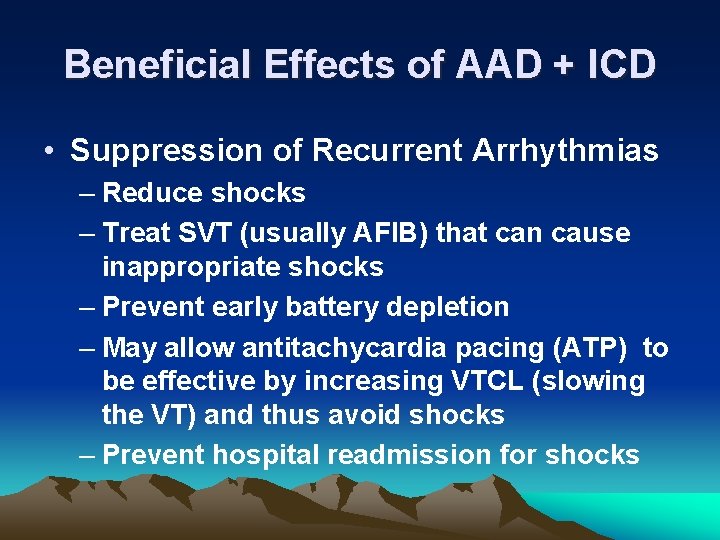
Beneficial Effects of AAD + ICD • Suppression of Recurrent Arrhythmias – Reduce shocks – Treat SVT (usually AFIB) that can cause inappropriate shocks – Prevent early battery depletion – May allow antitachycardia pacing (ATP) to be effective by increasing VTCL (slowing the VT) and thus avoid shocks – Prevent hospital readmission for shocks
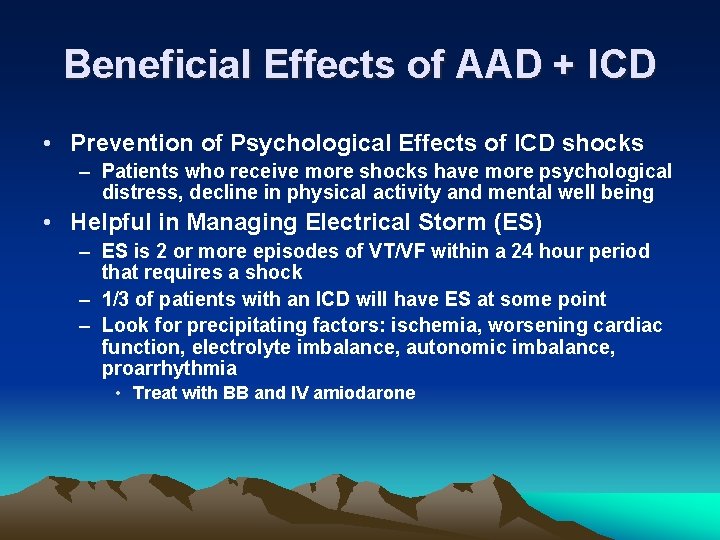
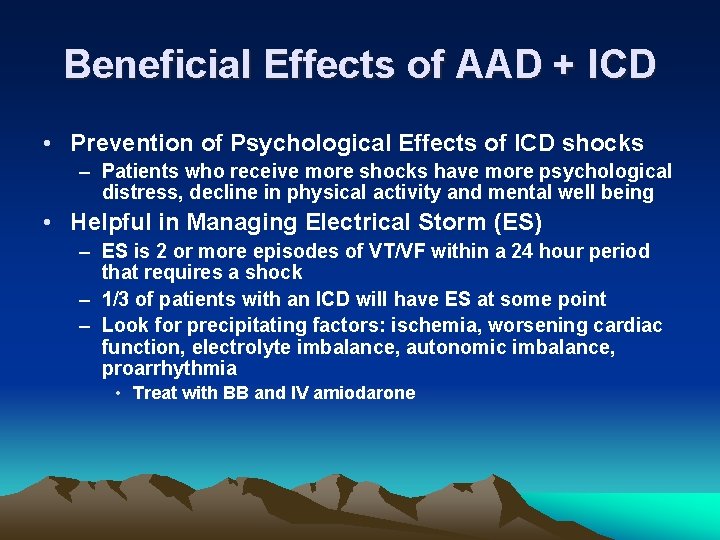
Beneficial Effects of AAD + ICD • Prevention of Psychological Effects of ICD shocks – Patients who receive more shocks have more psychological distress, decline in physical activity and mental well being • Helpful in Managing Electrical Storm (ES) – ES is 2 or more episodes of VT/VF within a 24 hour period that requires a shock – 1/3 of patients with an ICD will have ES at some point – Look for precipitating factors: ischemia, worsening cardiac function, electrolyte imbalance, autonomic imbalance, proarrhythmia • Treat with BB and IV amiodarone
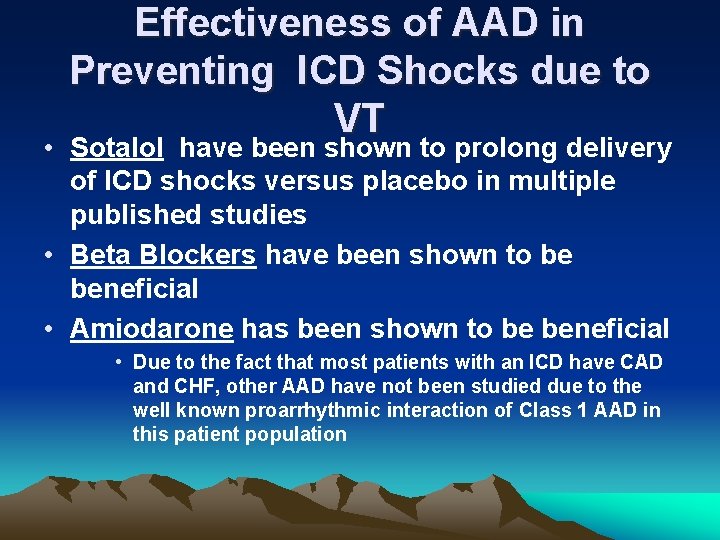
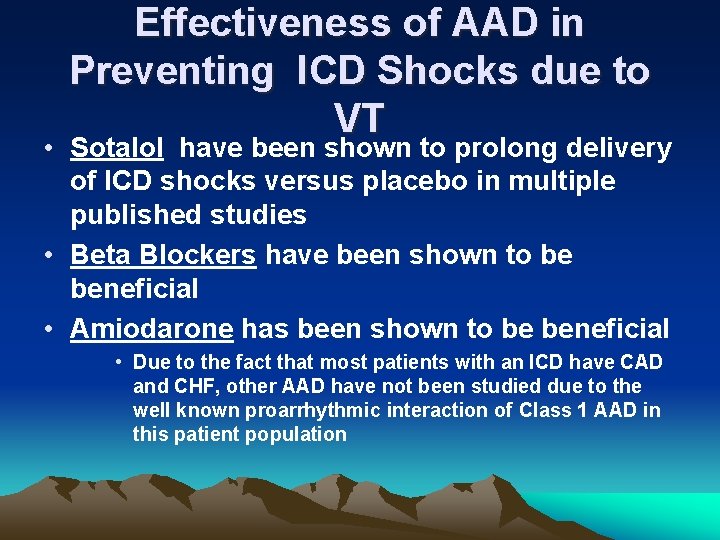
Effectiveness of AAD in Preventing ICD Shocks due to VT • Sotalol have been shown to prolong delivery of ICD shocks versus placebo in multiple published studies • Beta Blockers have been shown to be beneficial • Amiodarone has been shown to be beneficial • Due to the fact that most patients with an ICD have CAD and CHF, other AAD have not been studied due to the well known proarrhythmic interaction of Class 1 AAD in this patient population
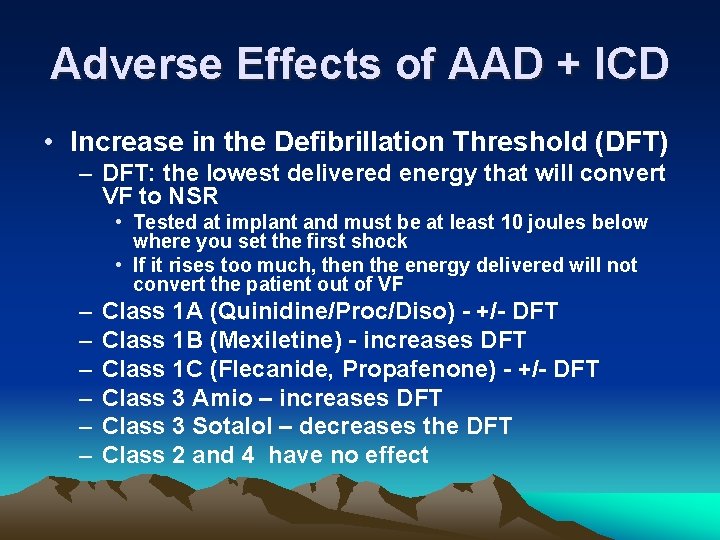
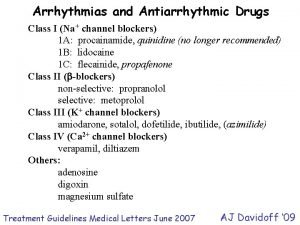
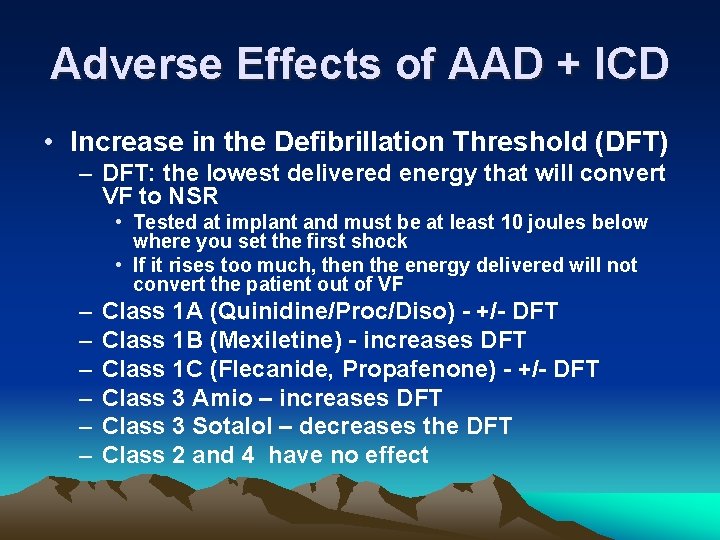
Adverse Effects of AAD + ICD • Increase in the Defibrillation Threshold (DFT) – DFT: the lowest delivered energy that will convert VF to NSR • Tested at implant and must be at least 10 joules below where you set the first shock • If it rises too much, then the energy delivered will not convert the patient out of VF – – – Class 1 A (Quinidine/Proc/Diso) - +/- DFT Class 1 B (Mexiletine) - increases DFT Class 1 C (Flecanide, Propafenone) - +/- DFT Class 3 Amio – increases DFT Class 3 Sotalol – decreases the DFT Class 2 and 4 have no effect
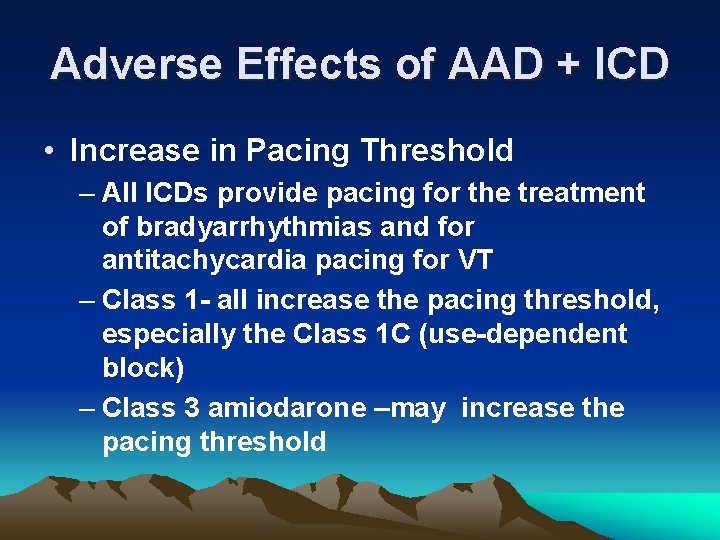
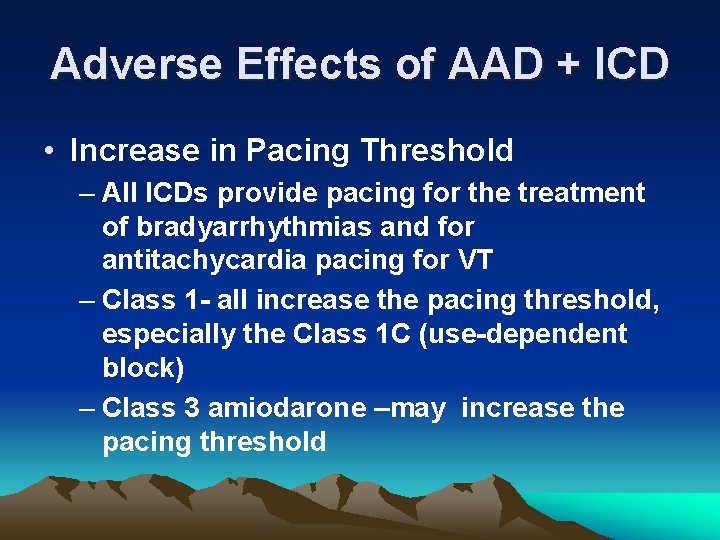
Adverse Effects of AAD + ICD • Increase in Pacing Threshold – All ICDs provide pacing for the treatment of bradyarrhythmias and for antitachycardia pacing for VT – Class 1 - all increase the pacing threshold, especially the Class 1 C (use-dependent block) – Class 3 amiodarone –may increase the pacing threshold
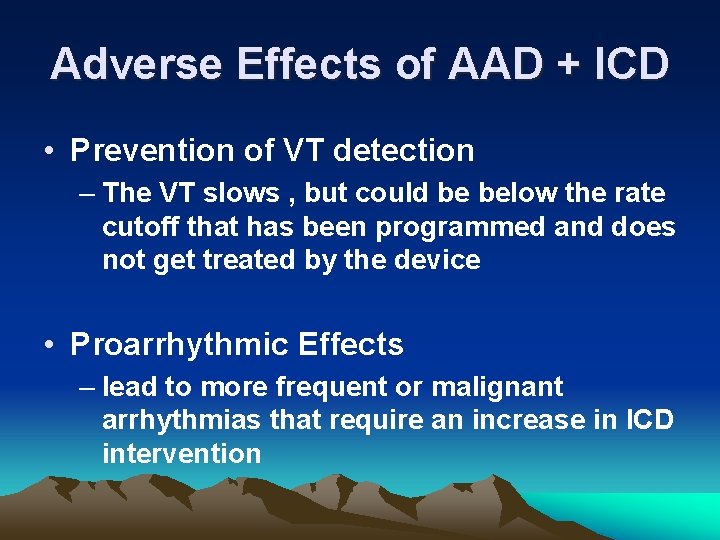
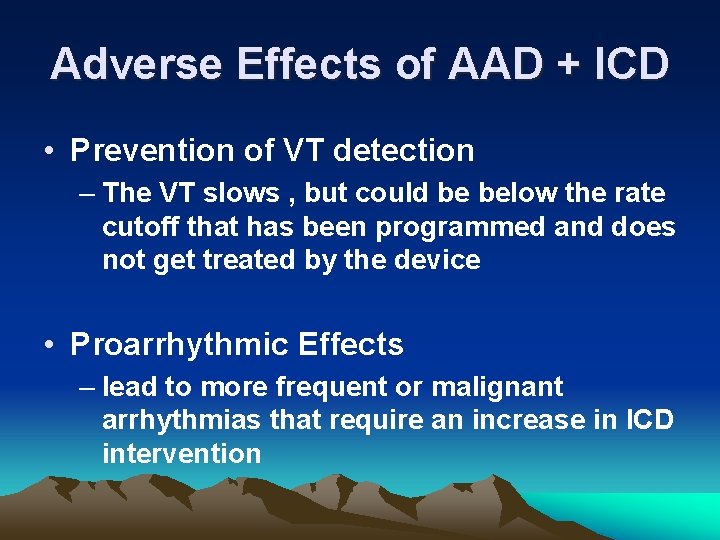
Adverse Effects of AAD + ICD • Prevention of VT detection – The VT slows , but could be below the rate cutoff that has been programmed and does not get treated by the device • Proarrhythmic Effects – lead to more frequent or malignant arrhythmias that require an increase in ICD intervention
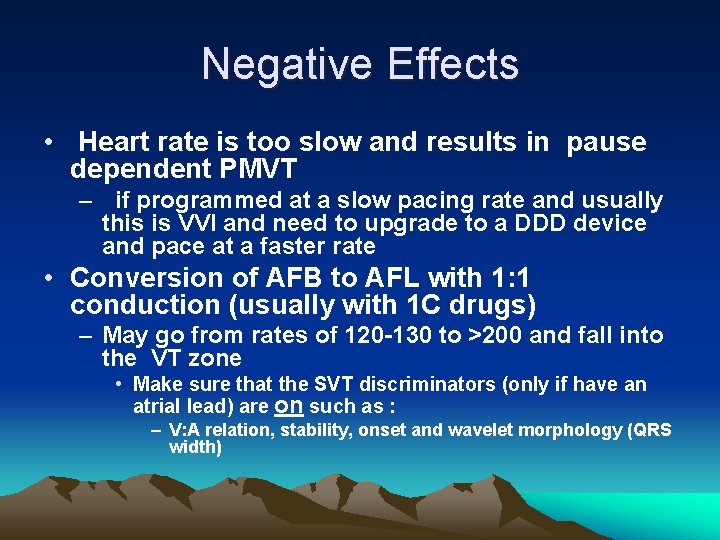
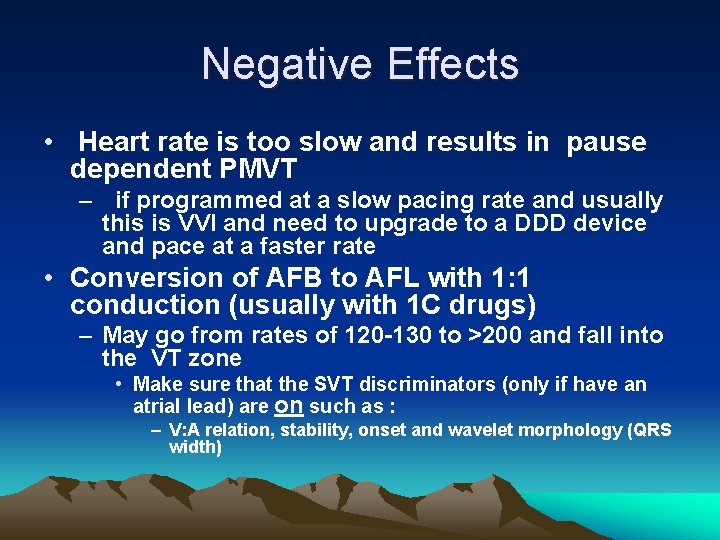
Negative Effects • Heart rate is too slow and results in pause dependent PMVT – if programmed at a slow pacing rate and usually this is VVI and need to upgrade to a DDD device and pace at a faster rate • Conversion of AFB to AFL with 1: 1 conduction (usually with 1 C drugs) – May go from rates of 120 -130 to >200 and fall into the VT zone • Make sure that the SVT discriminators (only if have an atrial lead) are on such as : – V: A relation, stability, onset and wavelet morphology (QRS width)
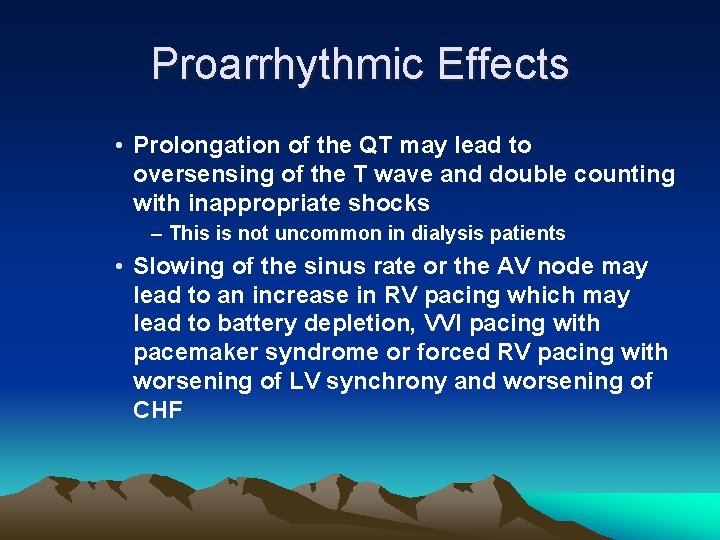
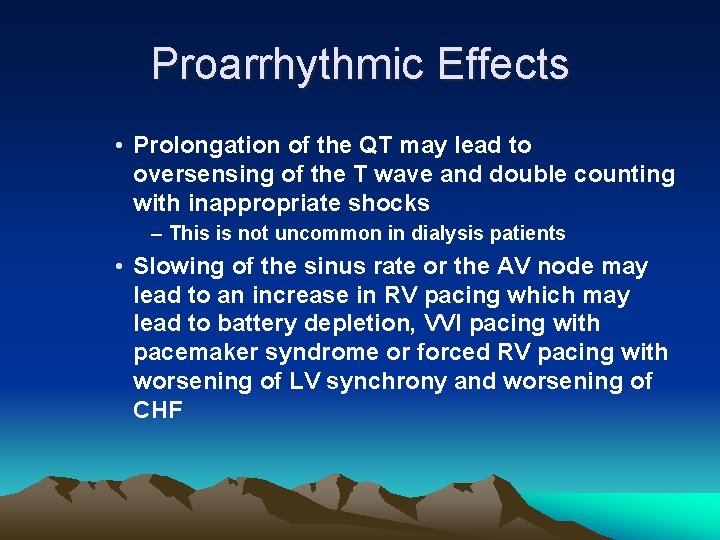
Proarrhythmic Effects • Prolongation of the QT may lead to oversensing of the T wave and double counting with inappropriate shocks – This is not uncommon in dialysis patients • Slowing of the sinus rate or the AV node may lead to an increase in RV pacing which may lead to battery depletion, VVI pacing with pacemaker syndrome or forced RV pacing with worsening of LV synchrony and worsening of CHF
Summary • ICDs are the treatment of choice for primary and secondary prevention of lethal ventricular arrhythmias • At least 1/3 will require adjuvant AAD therapy • Class 3 agents appear to be the best tolerated drugs in this patient population • This hybrid therapy has potential pitfalls that need to be recognized and may require reprogramming of the ICD for patient safety
 Lidocaine in cardiac arrest
Lidocaine in cardiac arrest Positive vs negative inotropes
Positive vs negative inotropes Classification of antiarrhythmic drugs
Classification of antiarrhythmic drugs Class 3 antiarrhythmic drugs mechanism of action
Class 3 antiarrhythmic drugs mechanism of action Class 1a antiarrhythmic drugs
Class 1a antiarrhythmic drugs Antiarrhythmic drugs mechanism of action
Antiarrhythmic drugs mechanism of action Antiarrhythmic drugs classification
Antiarrhythmic drugs classification Antiarrhythmic drugs classification
Antiarrhythmic drugs classification Cpu output device
Cpu output device Safest antiarrhythmic drug
Safest antiarrhythmic drug C traps and pitfalls
C traps and pitfalls Nitcar
Nitcar First pass effect in pharmacology
First pass effect in pharmacology