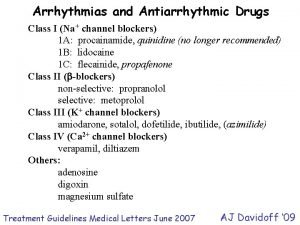
ANTIARRHYTMIC DRUGS Classification of antiarrhythmic drugs Vaughn Williams
- Slides: 29
ANTI-ARRHYTMIC DRUGS
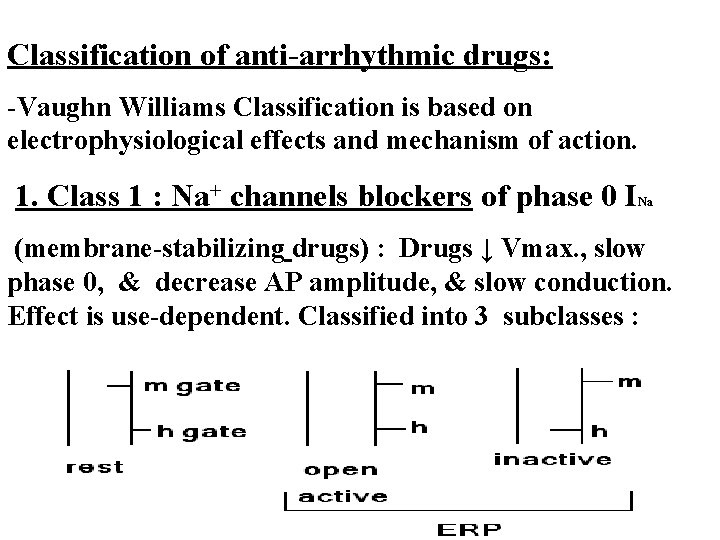
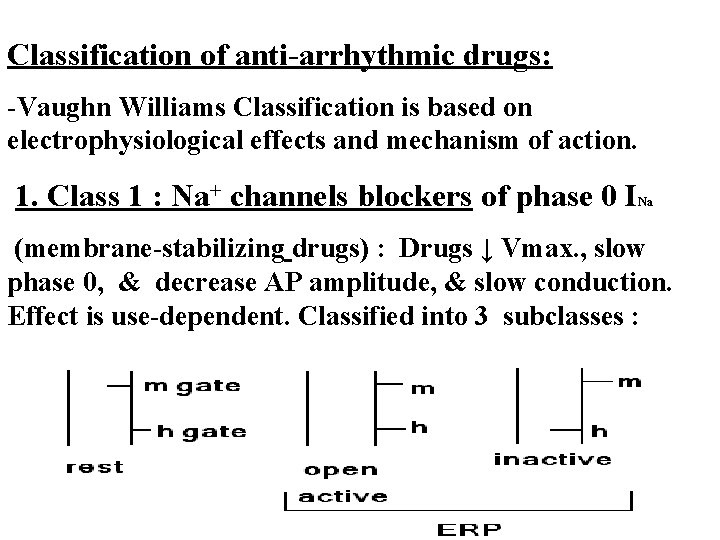
Classification of anti-arrhythmic drugs: -Vaughn Williams Classification is based on electrophysiological effects and mechanism of action. 1. Class 1 : Na+ channels blockers of phase 0 I Na (membrane-stabilizing drugs) : Drugs ↓ Vmax. , slow phase 0, & decrease AP amplitude, & slow conduction. Effect is use-dependent. Classified into 3 subclasses :
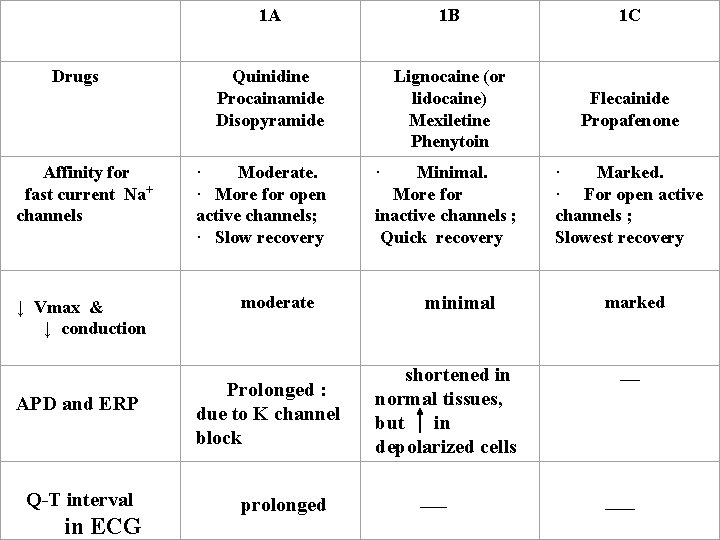
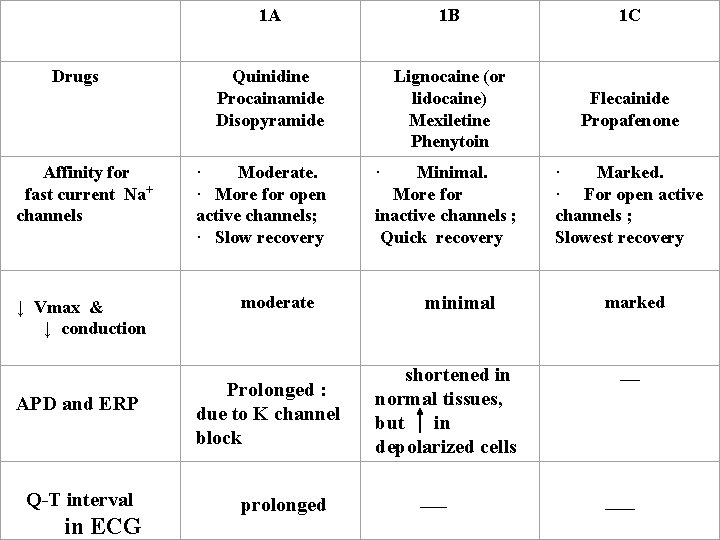
Drugs Affinity for fast current Na+ channels ↓ Vmax & ↓ conduction APD and ERP Q-T interval in ECG 1 A 1 B 1 C Quinidine Procainamide Disopyramide Lignocaine (or lidocaine) Mexiletine Phenytoin Flecainide Propafenone Minimal. More for inactive channels ; Quick recovery · Marked. · For open active channels ; Slowest recovery · Moderate. · More for open active channels; · Slow recovery moderate Prolonged : due to K channel block prolonged · minimal shortened in normal tissues, but in depolarized cells ___ marked __ ___
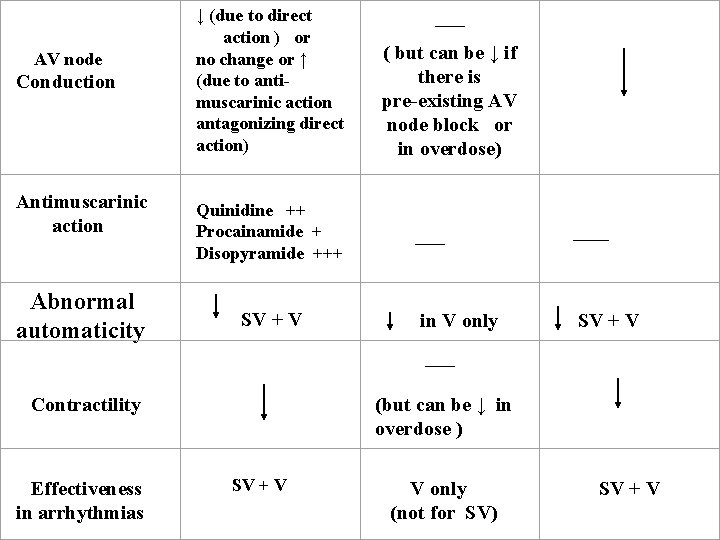
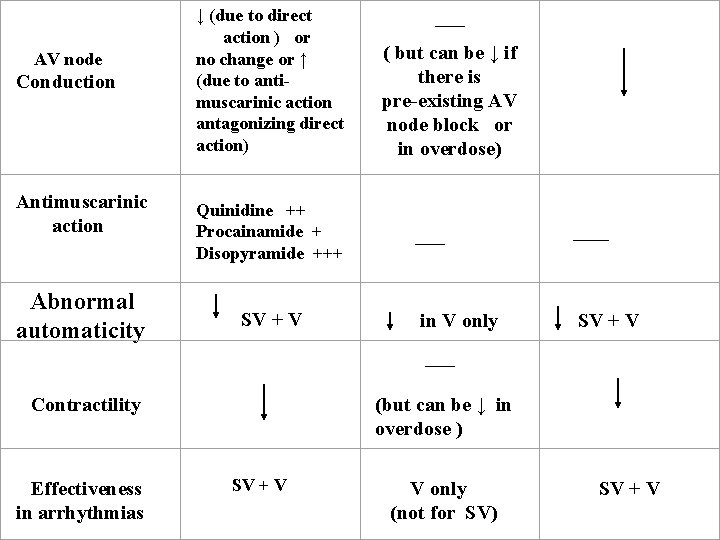
AV node Conduction Antimuscarinic action Abnormal automaticity ↓ (due to direct action ) or no change or ↑ (due to antimuscarinic action antagonizing direct action) Quinidine ++ Procainamide + Disopyramide +++ SV + V ___ ( but can be ↓ if there is pre-existing AV node block or in overdose) ____ in V only SV + V ___ Contractility Effectiveness in arrhythmias (but can be ↓ in overdose ) SV + V V only (not for SV) SV + V
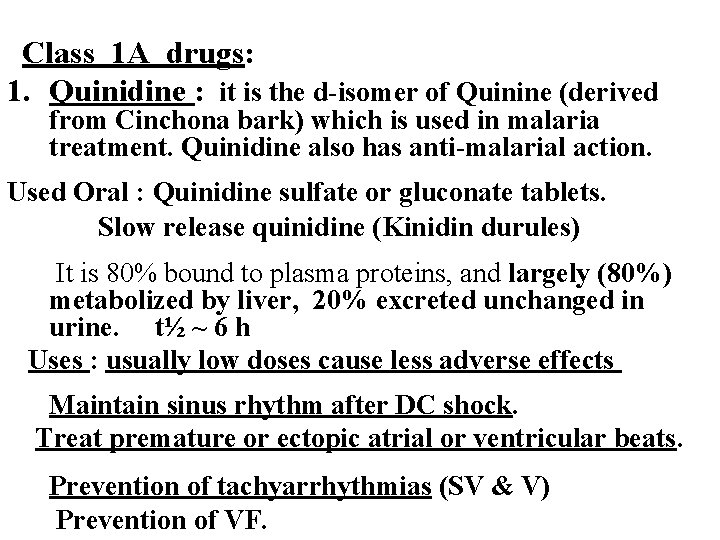
Class 1 A drugs: 1. Quinidine : it is the d-isomer of Quinine (derived from Cinchona bark) which is used in malaria treatment. Quinidine also has anti-malarial action. Used Oral : Quinidine sulfate or gluconate tablets. Slow release quinidine (Kinidin durules) It is 80% bound to plasma proteins, and largely (80%) metabolized by liver, 20% excreted unchanged in urine. t½ ~ 6 h Uses : usually low doses cause less adverse effects Maintain sinus rhythm after DC shock. Treat premature or ectopic atrial or ventricular beats. Prevention of tachyarrhythmias (SV & V) Prevention of VF.
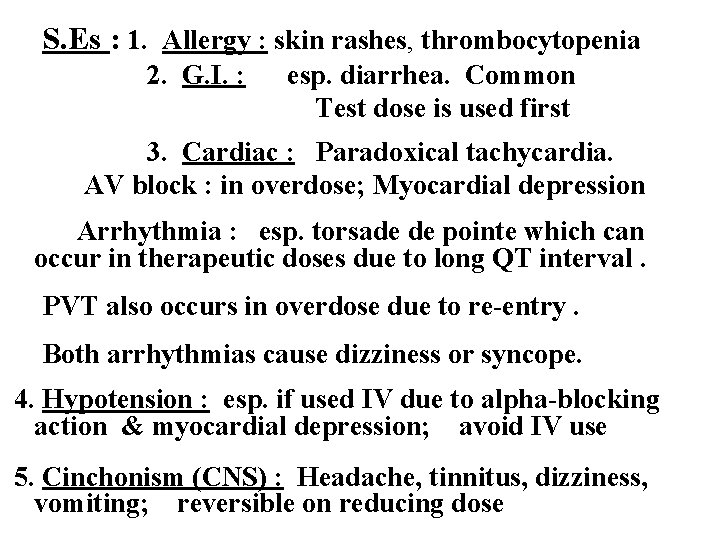
S. Es : 1. Allergy : skin rashes, thrombocytopenia 2. G. I. : esp. diarrhea. Common Test dose is used first 3. Cardiac : Paradoxical tachycardia. AV block : in overdose; Myocardial depression Arrhythmia : esp. torsade de pointe which can occur in therapeutic doses due to long QT interval. PVT also occurs in overdose due to re-entry. Both arrhythmias cause dizziness or syncope. 4. Hypotension : esp. if used IV due to alpha-blocking action & myocardial depression; avoid IV use 5. Cinchonism (CNS) : Headache, tinnitus, dizziness, vomiting; reversible on reducing dose
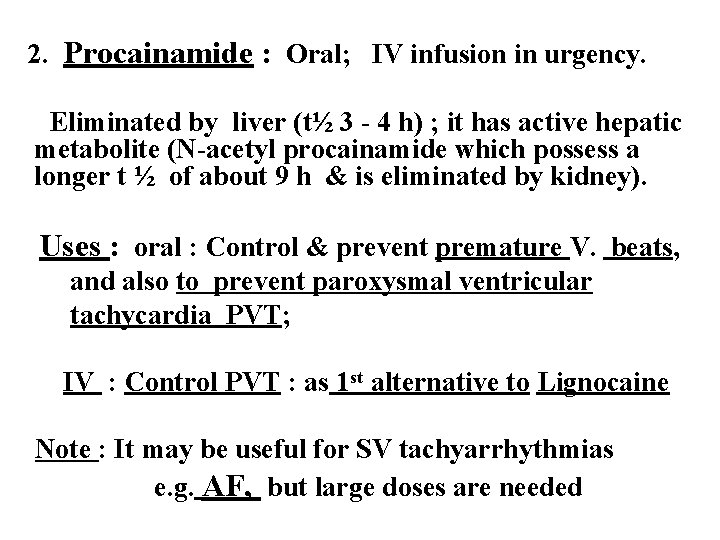
2. Procainamide : Oral; IV infusion in urgency. Eliminated by liver (t½ 3 - 4 h) ; it has active hepatic metabolite (N-acetyl procainamide which possess a longer t ½ of about 9 h & is eliminated by kidney). Uses : oral : Control & prevent premature V. beats, and also to prevent paroxysmal ventricular tachycardia PVT; IV : Control PVT : as 1 st alternative to Lignocaine Note : It may be useful for SV tachyarrhythmias e. g. AF, but large doses are needed
S. Es : 1. CNS : depression, hallucinations. 2. Cardiac : arrhythmia; myocardial depression 3. Hypotension : if given IV, largely due to ganglion-blocking action 4. Allergy & cross-allergy with procaine 5. If used longer than 6 weeks orally, then positive anti-nuclear factor (ANF) titer can develop, and about 30% of cases progress to SLE ( reversible usually on stopping drug use ).
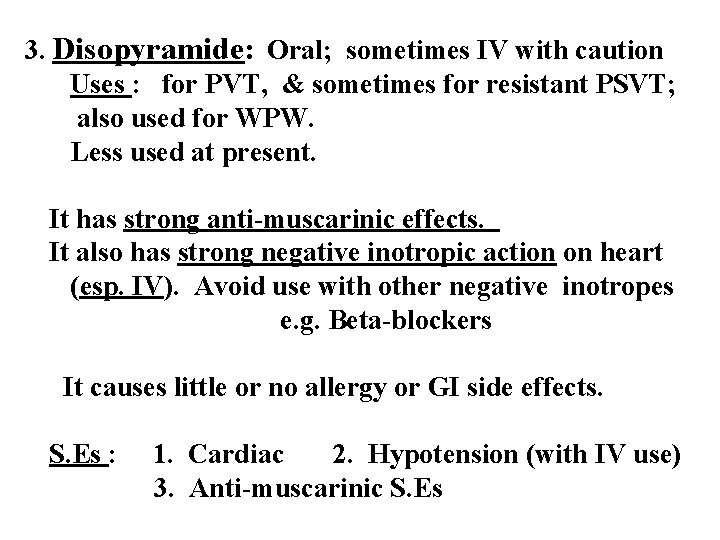
3. Disopyramide: Oral; sometimes IV with caution Uses : for PVT, & sometimes for resistant PSVT; also used for WPW. Less used at present. It has strong anti-muscarinic effects. It also has strong negative inotropic action on heart (esp. IV). Avoid use with other negative inotropes e. g. Beta-blockers It causes little or no allergy or GI side effects. S. Es : 1. Cardiac 2. Hypotension (with IV use) 3. Anti-muscarinic S. Es
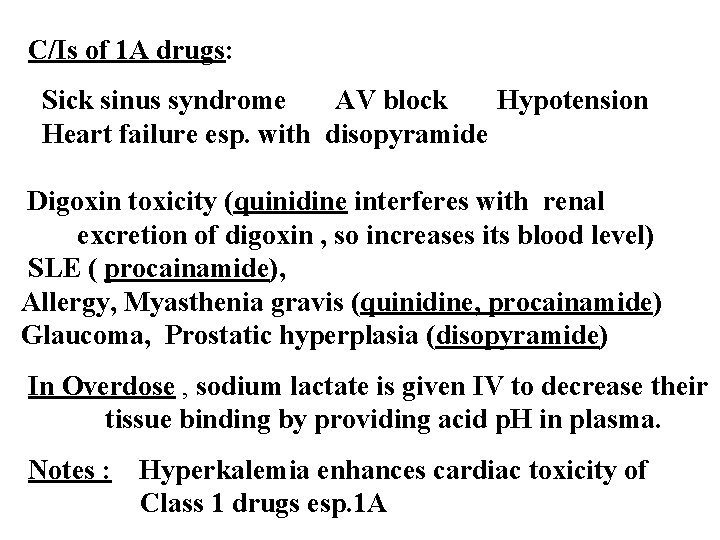
C/Is of 1 A drugs: Sick sinus syndrome AV block Hypotension Heart failure esp. with disopyramide Digoxin toxicity (quinidine interferes with renal excretion of digoxin , so increases its blood level) SLE ( procainamide), Allergy, Myasthenia gravis (quinidine, procainamide) Glaucoma, Prostatic hyperplasia (disopyramide) In Overdose , sodium lactate is given IV to decrease their tissue binding by providing acid p. H in plasma. Notes : Hyperkalemia enhances cardiac toxicity of Class 1 drugs esp. 1 A
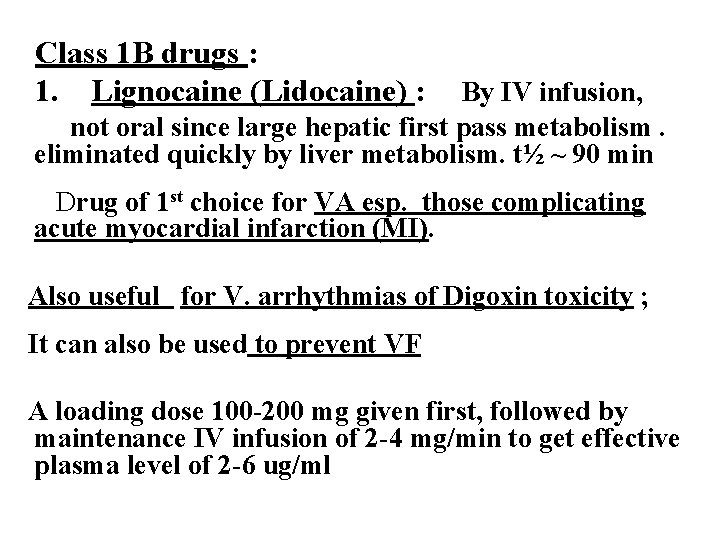
Class 1 B drugs : 1. Lignocaine (Lidocaine) : By IV infusion, not oral since large hepatic first pass metabolism. eliminated quickly by liver metabolism. t½ ~ 90 min Drug of 1 st choice for VA esp. those complicating acute myocardial infarction (MI). Also useful for V. arrhythmias of Digoxin toxicity ; It can also be used to prevent VF A loading dose 100 -200 mg given first, followed by maintenance IV infusion of 2 -4 mg/min to get effective plasma level of 2 -6 ug/ml
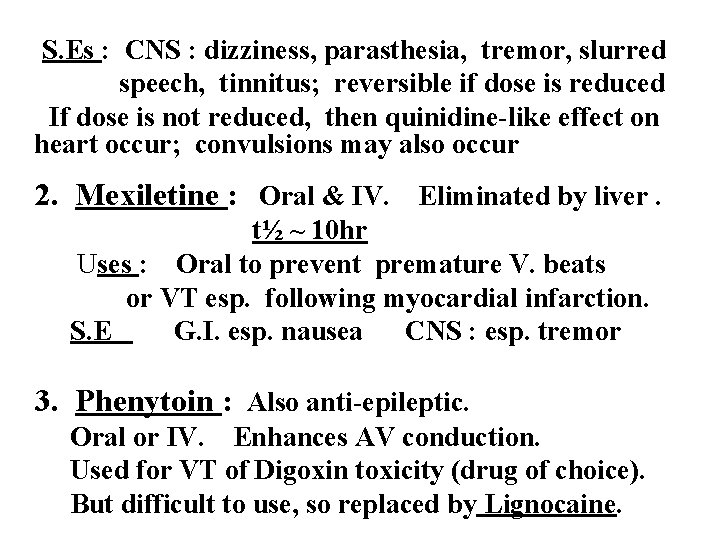
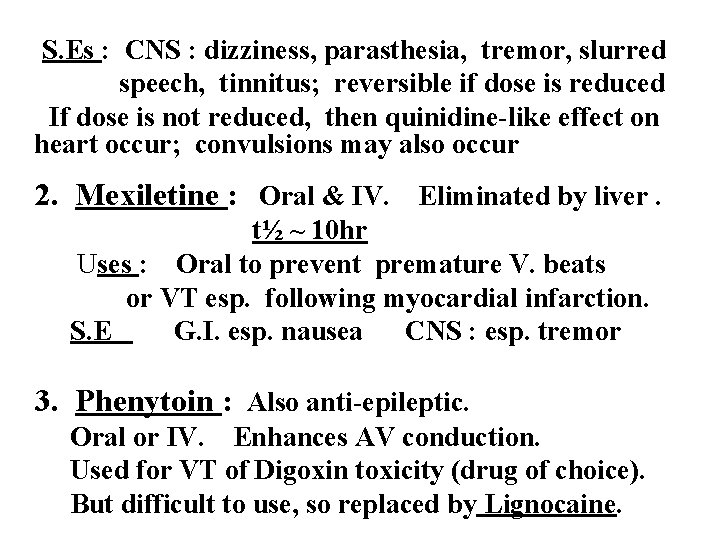
S. Es : CNS : dizziness, parasthesia, tremor, slurred speech, tinnitus; reversible if dose is reduced If dose is not reduced, then quinidine-like effect on heart occur; convulsions may also occur 2. Mexiletine : Oral & IV. Eliminated by liver. t½ ~ 10 hr Uses : Oral to prevent premature V. beats or VT esp. following myocardial infarction. S. E G. I. esp. nausea CNS : esp. tremor 3. Phenytoin : Also anti-epileptic. Oral or IV. Enhances AV conduction. Used for VT of Digoxin toxicity (drug of choice). But difficult to use, so replaced by Lignocaine.
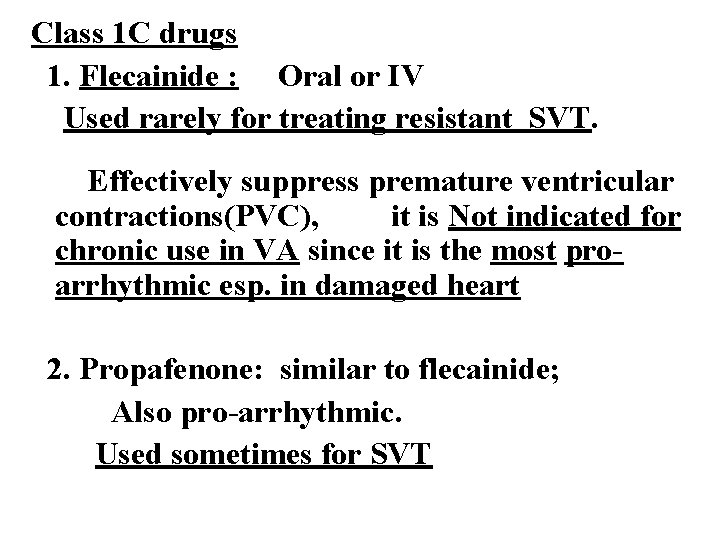
Class 1 C drugs 1. Flecainide : Oral or IV Used rarely for treating resistant SVT. Effectively suppress premature ventricular contractions(PVC), it is Not indicated for chronic use in VA since it is the most proarrhythmic esp. in damaged heart 2. Propafenone: similar to flecainide; Also pro-arrhythmic. Used sometimes for SVT
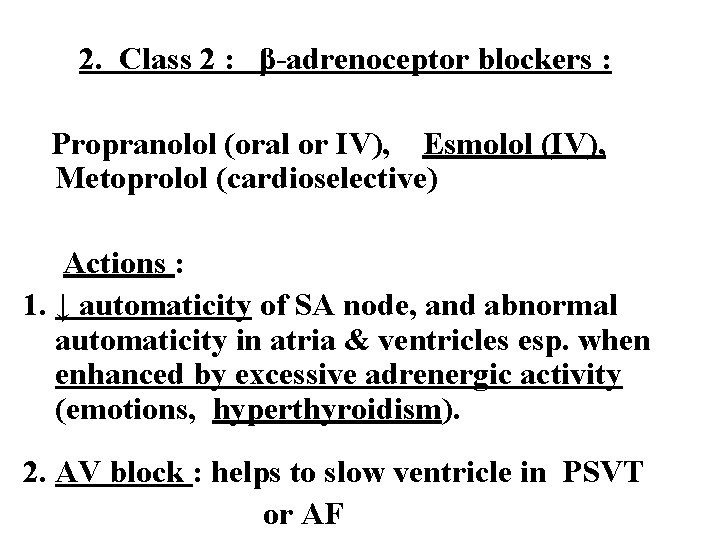
2. Class 2 : β-adrenoceptor blockers : Propranolol (oral or IV), Esmolol (IV), Metoprolol (cardioselective) Actions : 1. ↓ automaticity of SA node, and abnormal automaticity in atria & ventricles esp. when enhanced by excessive adrenergic activity (emotions, hyperthyroidism). 2. AV block : helps to slow ventricle in PSVT or AF
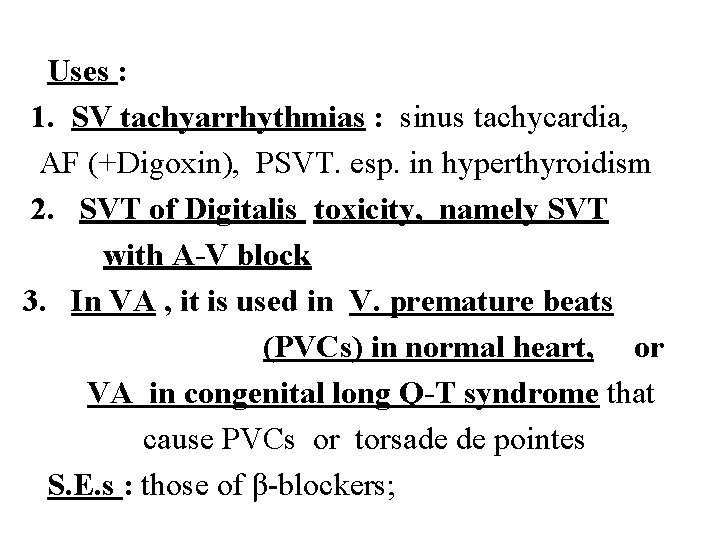
Uses : 1. SV tachyarrhythmias : sinus tachycardia, AF (+Digoxin), PSVT. esp. in hyperthyroidism 2. SVT of Digitalis toxicity, namely SVT with A-V block 3. In VA , it is used in V. premature beats (PVCs) in normal heart, or VA in congenital long Q-T syndrome that cause PVCs or torsade de pointes S. E. s : those of β-blockers;
Class 3 : Drugs that prolong repolarization, APD and ERP. - Block K+ channels responsible for phase 3 rectifier K+ current , thus prolong Q-T interval. 1. Amiodarone : Also blocks Na+ channels, and blocks non- specifically Ca++ channels and β-receptors. Oral; in urgency IV. Uses: In urgency in AF or PSVT or VT, Resistant SVT or VT : control & prevention Best drug to control arrhythmias due Wolf-Parkinson-White syndrome). Also can prevent VF after use of defibrillator
Disadvantages : a. Cumulative : t ½ ~ 2 -3 weeks; stored in fat & many tissues and eliminated in bile and urine. b. Many adverse effects : Corneal micro-deposits (may be reversible). Photosensitivity. Cardiac toxicity ( torsade de pointes is least likely). Stop drug if : Thyroid (hyper- or hypo-thyroidism). Pulmonary fibrosis : very serious and can be fatal Liver toxicity. Peripheral neuropathy. 2. Sotalol is a beta-blocker that has also class 3 action. d-Sotalol lacks beta-blocking action but retains class 3 effect. It prolongs Q-T interval, & can cause torsades de pointes. Available as racemic dl-mixture for oral use.
3. Ibutilide : Prolong APD by blocking delayed rectifier K+ current. It prolongs QT interval, and may cause torsade de pointes. Used IV for acute conversion of flutter (more effective) or atrial fibrillation to normal sinus rhythm. Rapidly eliminated by liver; t ½ is 6 h. Dofetilide : similar to ibutilide, but is orally effective. It is useful to maintain sinus rhythm after conversion of atrial fibrillation or flutter. Eliminated by kidney.
4. Class 4 Drugs : Cardioactive calcium channel blockers : anti-arrhythmic effect is due block of T- type Ca++ channel in AV node causing AV block. Include : Verapamil & Diltiazem Uses : Prevention of PSVT due to AVnodal re-entry S. E. s Bradycardia, ↓ BP esp. IV, Constipation. Note : They decrease myocardial contractility, so Avoid use with Β-blockers or disopyramide C/Is : HF. AV block. Sick sinus syndrome. Hypotension. Digoxin toxicity. VT
5. Miscellaneous drugs: 1. Adenosine : Drug of 1 st choice for quick control of PSVT due to AV node re-entry : given IV Stimulates Adenosine receptors (Pi) in AV node; also decreases calcium currents. Its anti-arrhythmic action is due to the hyperpolarization of AV node, and prolongation of its ERP, thus stops re-entry in AV node and produces AVblock. t½ is very short (~10 sec) acting due to rapid uptake by cells including endothelium and inactivation by adenine deaminase. Dose , if not effective, can be repeated after 1 min
Its uptake is inhibited by dipyridamole, while its receptors are blocked by theophylline and caffeine S. E. s : flushing, transient hypotension (due to vasodilation) , bradycardia, bronchospasm. AF is rarely induced by short ERP in atrium ( due to activation of Ach-sensitive K channels in atria) 2. Digoxin : It was drug of 1 st choice for atrial fibrillation (AF) or flutter. Oral or IV. It slows fast irregular ventricle in AF by increasing the ERP of AV node due to its selective cardiac vagal stimulant action. Atrium remains in fibrillating unless cause is removed. Slowing of ventricle will also help to relieve heart failure.
3. Potassium : Hypokalemia increases ectopic pacemaker activity and also enhances after-deplarizations, especially in presence of Digoxin Hyperkalemia depresses ectopic pacemakers (due to ↑ in their K+ permeability which stabilizes their membrane potentials) and slows conduction. Marked hyperkalemia can cause cardiac arrest in diastole. So, K+ salts (oral, or in urgent cases IV slowly) are important in treating arrhythmias associated with hypokalemia, esp. in digitalis-induced arrhythmias
4. Magnesium : Exact mechanism is not known, but Mg++ is known to influence Na+/K+ ATPase & ionic channels for Na+ , K+ , and Ca++ It may be given as magnesium sulfate (1 g IV) slowly over 20 min. (may be repeated once, if necessary) for : Digitalis-induced arrhythmias associated with hypomagnesaemia. Some patients with torsades de pointes (caused by EADs)
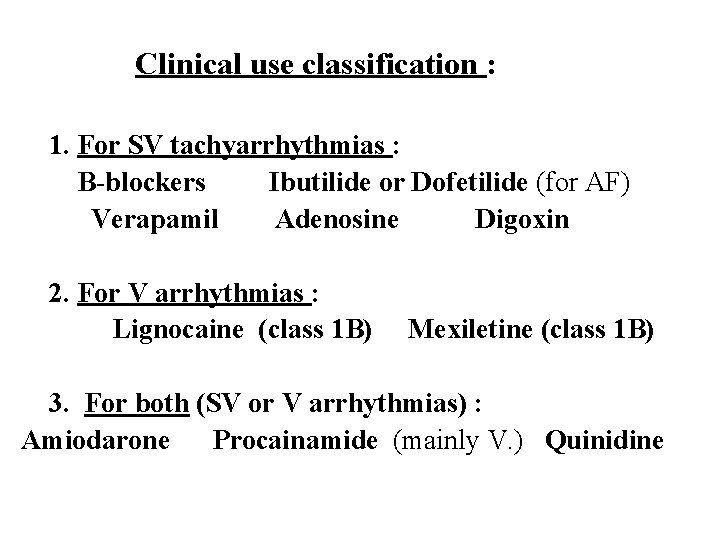
Clinical use classification : 1. For SV tachyarrhythmias : Β-blockers Ibutilide or Dofetilide (for AF) Verapamil Adenosine Digoxin 2. For V arrhythmias : Lignocaine (class 1 B) Mexiletine (class 1 B) 3. For both (SV or V arrhythmias) : Amiodarone Procainamide (mainly V. ) Quinidine
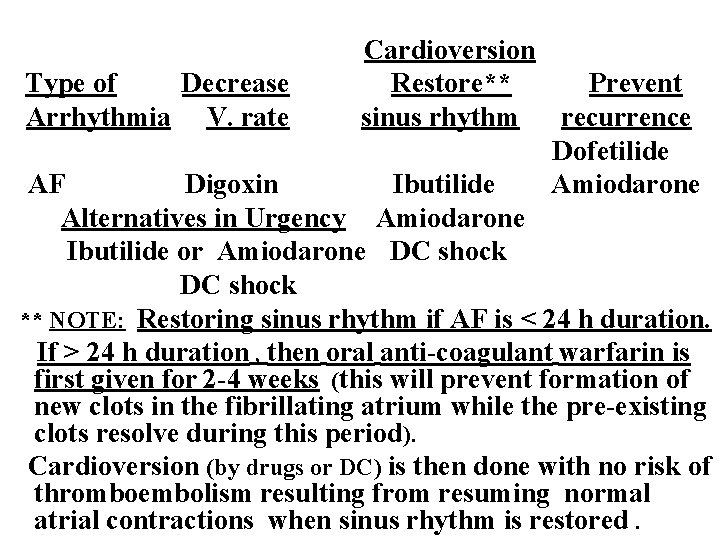
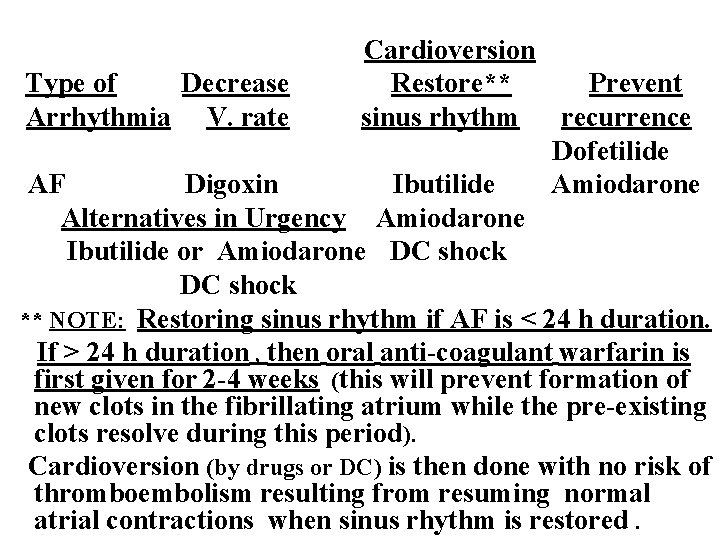
Cardioversion Type of Decrease Restore** Prevent Arrhythmia V. rate sinus rhythm recurrence Dofetilide AF Digoxin Ibutilide Amiodarone Alternatives in Urgency Amiodarone Ibutilide or Amiodarone DC shock ** NOTE: Restoring sinus rhythm if AF is < 24 h duration. If > 24 h duration , then oral anti-coagulant warfarin is first given for 2 -4 weeks (this will prevent formation of new clots in the fibrillating atrium while the pre-existing clots resolve during this period). Cardioversion (by drugs or DC) is then done with no risk of thromboembolism resulting from resuming normal atrial contractions when sinus rhythm is restored.
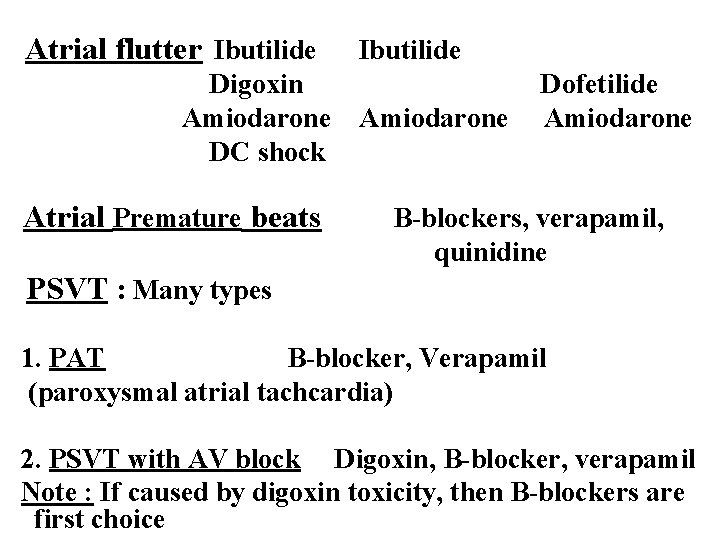
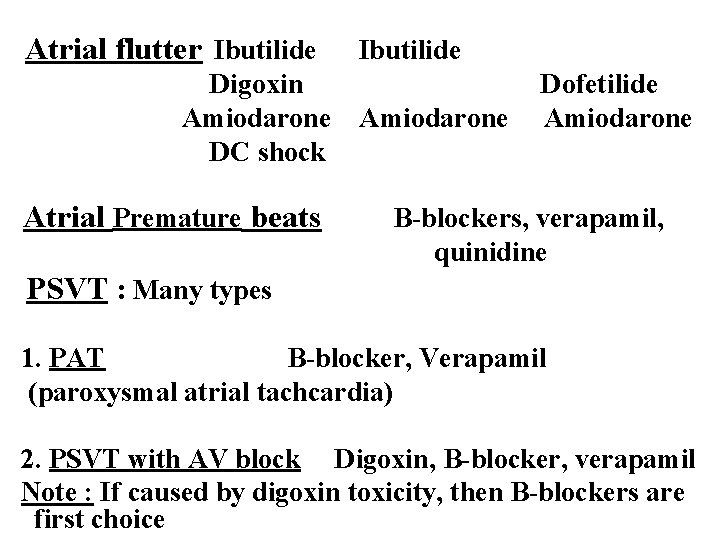
Atrial flutter Ibutilide Digoxin Amiodarone DC shock Atrial Premature beats Ibutilide Amiodarone Dofetilide Amiodarone B-blockers, verapamil, quinidine PSVT : Many types 1. PAT B-blocker, Verapamil (paroxysmal atrial tachcardia) 2. PSVT with AV block Digoxin, B-blocker, verapamil Note : If caused by digoxin toxicity, then B-blockers are first choice
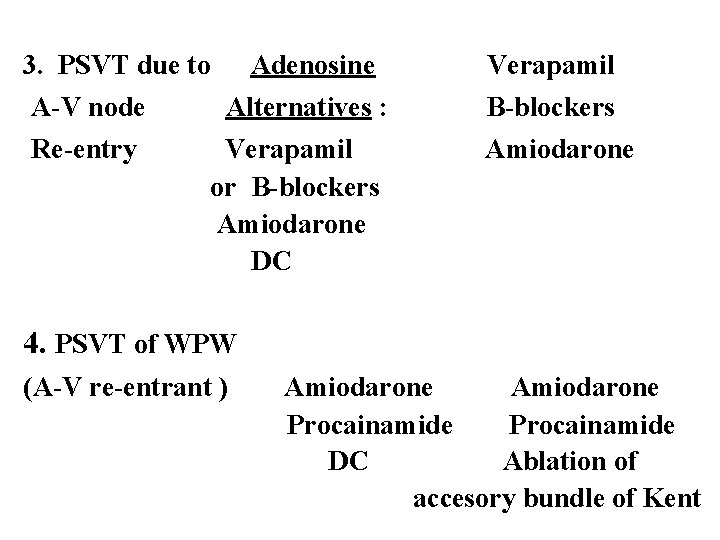
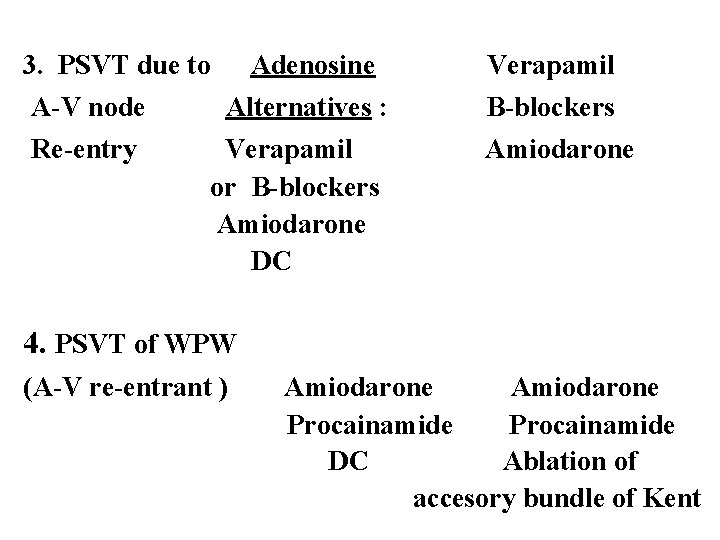
3. PSVT due to A-V node Re-entry Adenosine Verapamil Alternatives : B-blockers Verapamil or B-blockers Amiodarone DC Amiodarone 4. PSVT of WPW (A-V re-entrant ) Amiodarone Procainamide DC Ablation of accesory bundle of Kent
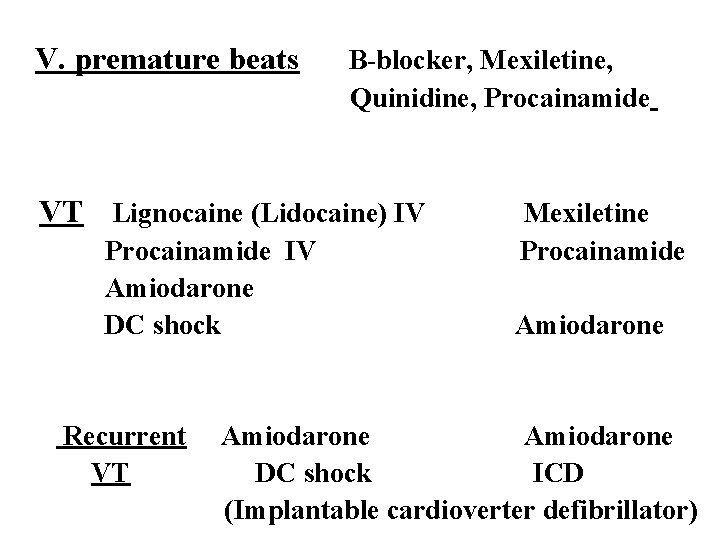
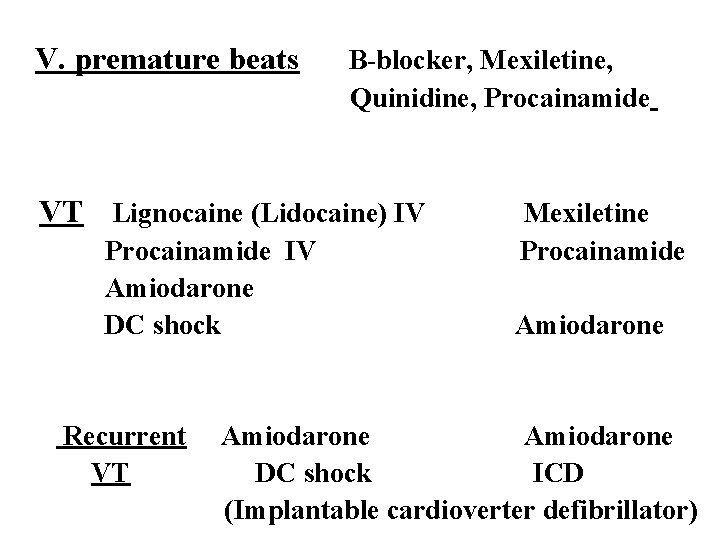
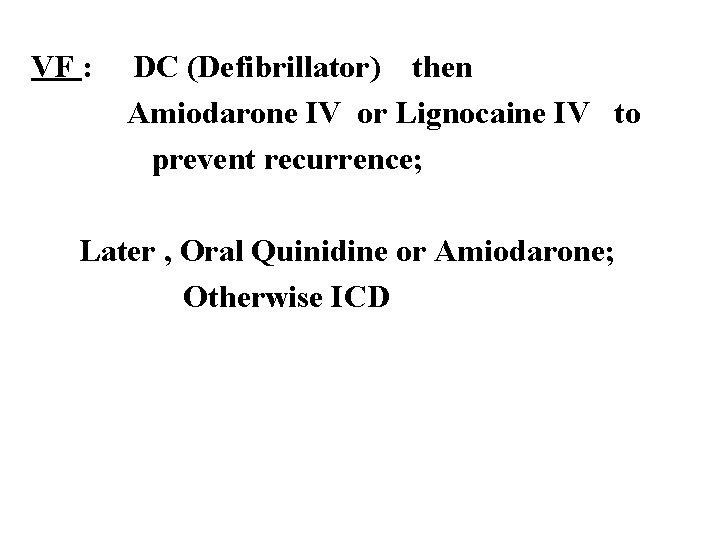
V. premature beats B-blocker, Mexiletine, Quinidine, Procainamide VT Lignocaine (Lidocaine) IV Procainamide IV Amiodarone DC shock Recurrent VT Mexiletine Procainamide Amiodarone DC shock ICD (Implantable cardioverter defibrillator)
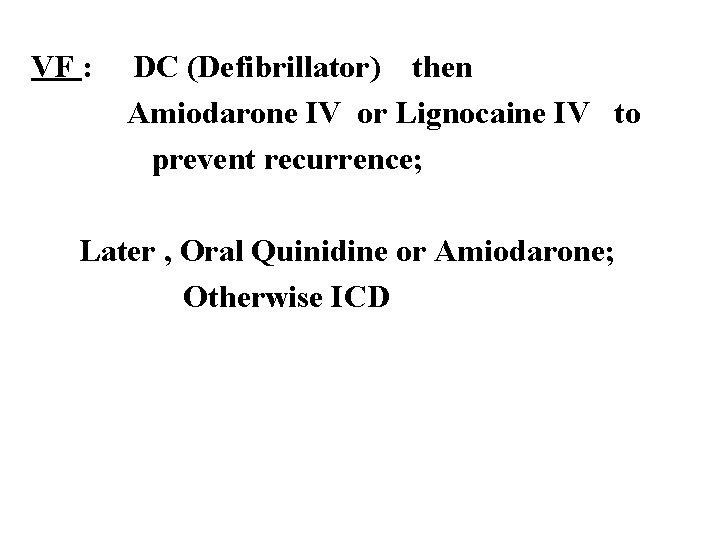
VF : DC (Defibrillator) then Amiodarone IV or Lignocaine IV to prevent recurrence; Later , Oral Quinidine or Amiodarone; Otherwise ICD
 Classification of antiarrhythmic drugs with examples
Classification of antiarrhythmic drugs with examples Classification of antiarrhythmic drugs
Classification of antiarrhythmic drugs Antiarrhythmic classification
Antiarrhythmic classification Antiarrhythmic drugs classification
Antiarrhythmic drugs classification Af begets af
Af begets af Inotropic effect
Inotropic effect Amiodarone mechanism of action
Amiodarone mechanism of action Antiarrhythmic drugs mechanism of action
Antiarrhythmic drugs mechanism of action Verna and sam case study health and social care
Verna and sam case study health and social care Andy williams robert williams
Andy williams robert williams Robbie williams janet williams
Robbie williams janet williams The hard way out by terry vaughn
The hard way out by terry vaughn Cholemesis medical term
Cholemesis medical term Kaitlin barr
Kaitlin barr Vaughn whittaker
Vaughn whittaker Christy vaughn
Christy vaughn Safest antiarrhythmic drug
Safest antiarrhythmic drug Antithyroid drugs classification
Antithyroid drugs classification Dumbbells antimuscarinic
Dumbbells antimuscarinic Oral hypoglycemic drugs classification
Oral hypoglycemic drugs classification Classification of diuretics
Classification of diuretics Serotaxonomy classification of crude drugs
Serotaxonomy classification of crude drugs M cholinomimetic drugs
M cholinomimetic drugs Anticancer drugs classification
Anticancer drugs classification Antifungal drugs classification
Antifungal drugs classification Lamotrigine mechanism of action
Lamotrigine mechanism of action Classification of antiemetic drugs
Classification of antiemetic drugs Anticholinergic drugs classification
Anticholinergic drugs classification Tropicamaide
Tropicamaide Classification of anticholinergic drugs
Classification of anticholinergic drugs