CHOLINERGIC SYSTEM AND DRUGS CHOLINOMIMETICS PARASYMPATHOMIMETICS MS Nageswararao















- Slides: 50
CHOLINERGIC SYSTEM AND DRUGS (CHOLINOMIMETICS, PARASYMPATHOMIMETICS) MS. Nageswararao Dept. of Pharmacology
• Acetylcholine(Ach) is the Quaternary ammonium compound and main neurotransmitter in the cholinergic system. • The neurons that synthesize , store and release Ach are called cholinergic neurons.


• CHOLINESTERASE: There are two types of cholinesterases. 1) A specific (Acetylcholinesterase - ACh. E or true cholinesterase) : ACh. E is strategically located at all cholinergic neurones, ganglia, RBC, and NMJ. serves to inactivate acetyl choline instantaneously 2) A nonspecific (Butyrylcholinesterase – Bu. Ch. E or pseudocholinesterase): Bu. Ch. E present in plasma, liver and glial cells. and probably serves to metabolize ingested esters
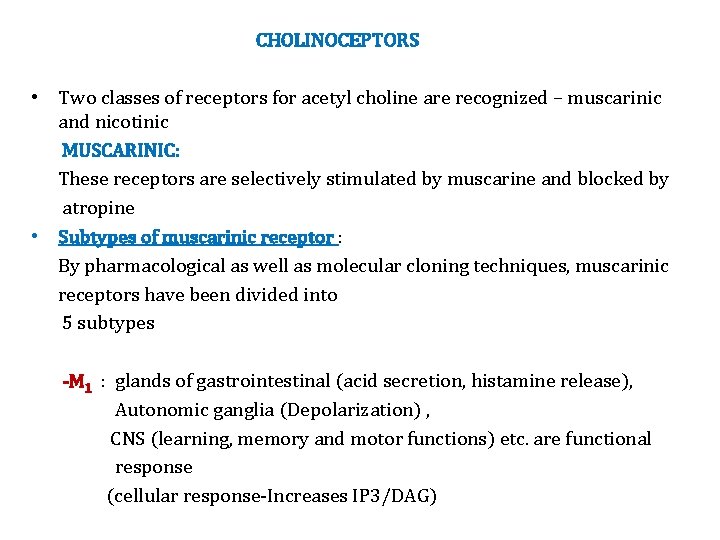
CHOLINOCEPTORS • Two classes of receptors for acetyl choline are recognized – muscarinic and nicotinic MUSCARINIC: These receptors are selectively stimulated by muscarine and blocked by atropine • Subtypes of muscarinic receptor : By pharmacological as well as molecular cloning techniques, muscarinic receptors have been divided into 5 subtypes -M 1 : glands of gastrointestinal (acid secretion, histamine release), Autonomic ganglia (Depolarization) , CNS (learning, memory and motor functions) etc. are functional response (cellular response-Increases IP 3/DAG)

-M 2 : Heart (-chronotropic(HR) , -inotropic(FOC) and –dromotropic (A. V) effects are the functional response. cellular response: Decreases c. AMP &opens K+ channels -M 3 : Smooth muscles(contractions), Exocrine glands(secretion), Vascular endothelial cells (release of NO- vasodilatation) (cellular response-Increases IP 3/DAG) -M 4 : (cellular response: Decreases c. AMP &opens K+ channels) -M 5 : are present mainly on nerve endings in certain areas of the brain and regulate the release of other neurotransmitters (cellular response-Increases IP 3/DAG)
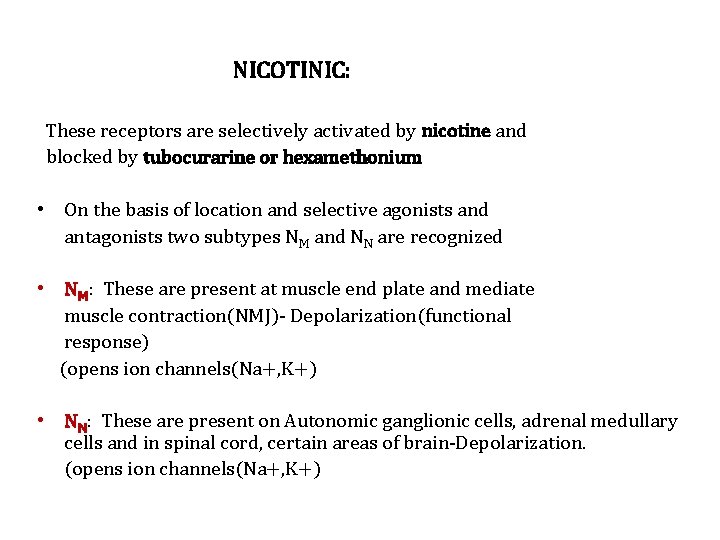
NICOTINIC: These receptors are selectively activated by nicotine and blocked by tubocurarine or hexamethonium • On the basis of location and selective agonists and antagonists two subtypes NM and NN are recognized • NM: These are present at muscle end plate and mediate muscle contraction(NMJ)- Depolarization(functional response) (opens ion channels(Na+, K+) • NN: These are present on Autonomic ganglionic cells, adrenal medullary cells and in spinal cord, certain areas of brain-Depolarization. (opens ion channels(Na+, K+)
Classification of cholinergic agents: • These are drugs which produce actions similar to that of ACh, either by directly interacting with cholinergic receptors (cholinergic agonists) or by increasing availability of ACh at these sites (anticholinesterases)

CHOLINERGIC DRUGS Directly acting Choline esters • Ach • Bethanechol • Carbachol Methacholine Indirectly acting (Anticholinesterases) Alkaloids Pilocarpine Muscarine , Arecoline REVERSIBLE Carbamates Physostigmine (Esirine) Neostigmine Pyridostigmine Edrophonium , Donepezil Rivastigmine , Galantamine IRREVERSIBLE Carbamates Carbaryl propoxur (prolonged action) OP compounds Prathion, Dyflos Melathion Nerve gases Echothiophate Diazinon
Pharmacological actions (of ACh as prototype) • Depending on the type of receptor through which it is mediated, the peripheral actions of ACh are classified as muscarinic or nicotinic.

• A. MUSCARINIC 1. Heart: • The effect of Ach are similar to those following vagal stimulation. • Ach , by stimulating M 2 receptors of the heart , opens the potassium channels and thus causes hyperpolarization. ACh hyperpolarizes the SA nodal cells and decreases the rate of diastolic depolarization. As a result, rate of impulse generation is reduced – bradycardia or even cardiac arrest may occur •
• 2. Blood vessels: All blood vessels are dilated, Fall in BP and flushing, especially in the blush area occurs • Muscarinic receptors(M 3) are present on vascular endothelial cells: vasodilatation is primarily mediated through the release of an endothelium dependent relaxing factor (EDRF) which is nitric oxide (NO) • Stimulation of cholinergic nerves to the penis causes erection by releasing NO and dilating cavernosal vessels through muscarinic receptors(M 3)
3. Smooth muscle: (M 3 receptors). • GIT: Smooth muscle in most organs is contracted. Tone, peristalsis and GI secretions in the gastrointestinal tract is increased and sphincters relax → abdominal cramps and evacuation of bowel • Urinary bladder: Peristalsis in ureter is increased. The detrusor muscle contracts while the bladder trigone and sphincter relaxes→ voiding of bladder(causes urination) • Bronchi: Bronchial muscles constrict(bronchospasm), increases tracheobronchial secretions. asthmatics are highly sensitive → dyspnoea, precipitation of an attack of bronchial asthma
• 4. Exocrine Glands: (M 3 receptor) Secretion from all parasympathetically innervated glands is increased: sweating, salivation, lacrimation, tracheobronchial and gastric secretion • The effect on pancreatic and intestinal glands is not marked. Secretion of milk and bile is not affected
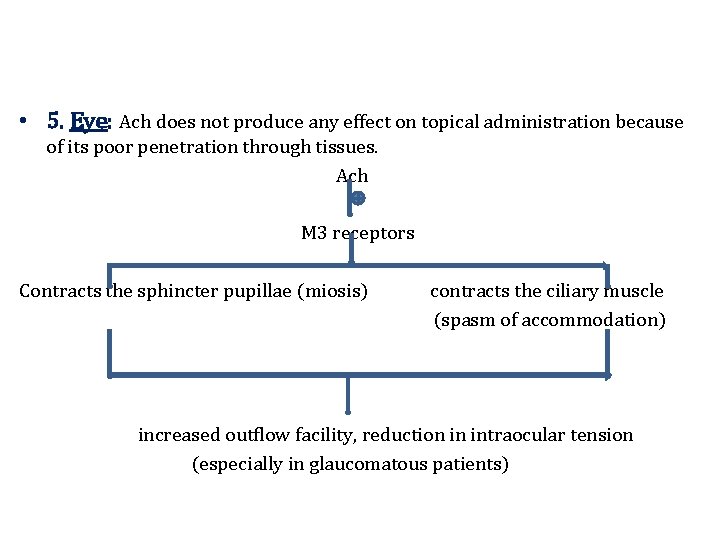
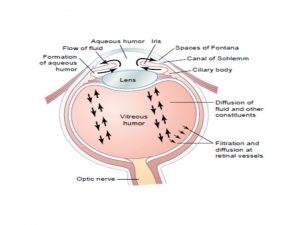
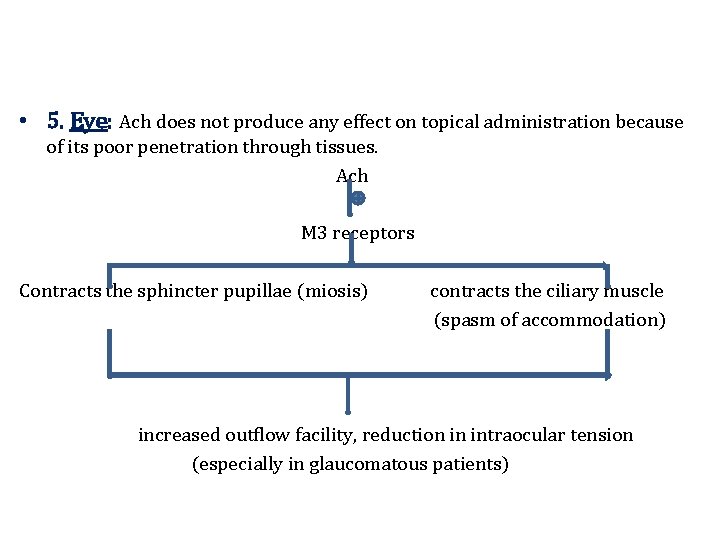
• 5. Eye: Ach does not produce any effect on topical administration because of its poor penetration through tissues. Ach M 3 receptors Contracts the sphincter pupillae (miosis) contracts the ciliary muscle (spasm of accommodation) increased outflow facility, reduction in intraocular tension (especially in glaucomatous patients)

• B. NICOTINIC • There are thick fibrous tissue sheath around the nicotinic receptors. As the Ach has poor penetration through tissues, larger doses are required to elicit nicotinic action. • 1. Autonomic ganglia: (NN RECEPTOR) • Higher doses of Ach produce dangerous muscarinic effects especially on the heart. Hence , the prior administration of atropine is necessary to elicit nicotinic actions. • Both sympathetic and parasympathetic ganglia are stimulated. and causing tachycardia and rise in BP due to sympathetic ganglia stimulation and release of catecholamines. This effect is manifested a higher doses
• 2. Skeletal muscles: (NM RECEPTOR) Iontophoretic application of ACh to muscle endplate causes contraction of the fibre. • Intra-arterial injection of high dose can cause twitching and fasciculation's, followed by the prolonged depolarization of NMJ and paralysis. But i. v. injection is generally without any effect (due to rapid hydrolysis of ACh) • C. CNS • ACh injected i. v. does not penetrate blood brain barrier and no central effects are seen However, direct injection into the brain, or other cholinergic drugs which enter brain, produce a complex pattern of stimulation followed by depression • USES: Choline esters are rarely, if ever, clinically used • ACh is not used because of evanescent and nonselective action
• BETHANECHOL has been used in postoperative / postpartum non obstructive urinary retention, neurogenic bladder, paralytic ileum. • Mainly preffered because: wide margin of safety it has no nicotinic actions its muscarinic actions completely antagonized by atropine • Side effects are prominent: belching, colic, involuntary urination / defecation, flushing, sweating, fall in BP, bronchospasm • DOSE: 10 -40 mg oral, 2. 5 -5 mg s. c.
• CHOLINOMIMETIC ALKALOIDS: • They mimic the actions of acetylcholine. • PILOCARPINE: it is a tertiary amine. It is obtained from the leaves of Pilocarpus microphyllus • It produces muscarinic and nicotinic effects by directly interacting with the receptors. • It has a predominant muscarinic action especially on secretory activity.
• Pilocarpine causes marked sweating, salivation and increases other secretions as well • The cardiovascular effects are complex • Small doses generally cause fall in BP (muscarinic), but higher doses elicit rise in BP and tachycardia which is probably due to ganglionic stimulation (through ganglionic muscarinic receptors) • Applied to the eye, it penetrates cornea and promptly causes miosis, ciliary muscle contraction and fall in intraocular tension lasting 4 -8 hours

• Pilocarpine is used only in the eye as 0. 5 -4% drops • It is a third-line drug in open angle glaucoma and narrow angle glaucoma. An initial stinging sensation in the eye and painful spasm of accommodation are frequent side effects • Pilocarpine ocusert that releases the drug slowly over 7 days is available. • Also used to reverse the pupillary dilatation after refraction testing • Pilocarpine can be used cautiously by oral route in Xerostomia (dry mouth) that follows head and neck radiation treatment. • A/E: salivation, sweating , bradycardia, diarrhoea, bronchospasm and painfull spasm of accommodation. • PREP: 1%, 2%, 4% eye drops
• Muscarine: • It is an active ingradient of poisonous mushroom, Amanita muscaria and Inocybe species. • It has only muscarinic actions and not used therapeutically but is of toxicological importance. • Arecoline: It is an alkaloid obtained from arecanut. and its muscarinic and nicotinic actions are similar to choline esters.
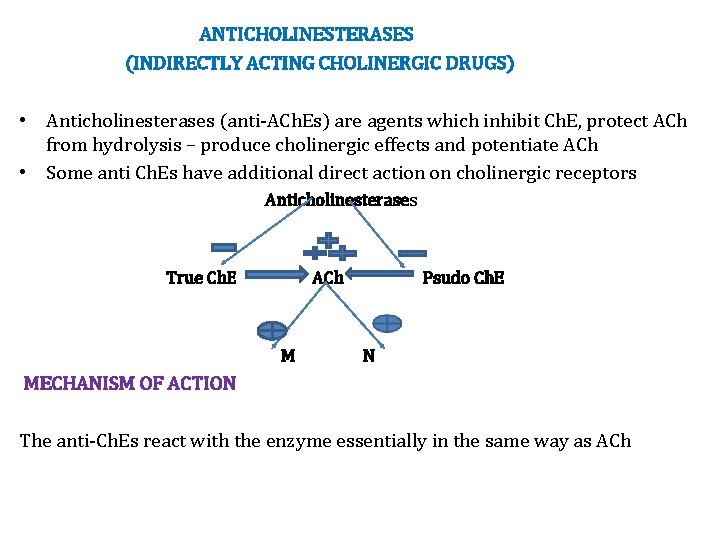
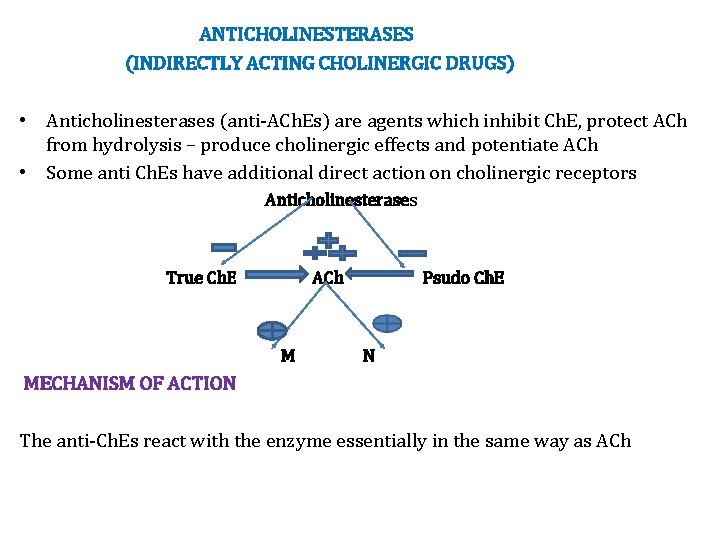
ANTICHOLINESTERASES (INDIRECTLY ACTING CHOLINERGIC DRUGS) • Anticholinesterases (anti-ACh. Es) are agents which inhibit Ch. E, protect ACh from hydrolysis – produce cholinergic effects and potentiate ACh • Some anti Ch. Es have additional direct action on cholinergic receptors Anticholinesterases True Ch. E ACh M Psudo Ch. E N MECHANISM OF ACTION The anti-Ch. Es react with the enzyme essentially in the same way as ACh
• REVERSIBLE • Carbamates: Physostigmine (Eserine), Neostigmine, Pyridostigmine, Edrophonium, Rivastigmine, Donepezil, Galantamine • Acridine: Tacrine • IRREVERSIBLE • Organophosphates: Dyflos (DFP), Echothiopate, Parathion, Malathion, Diazinon , Tabun, sarin, soman Carbamates: Carbaryl, Propoxur
• PHARMACOLOGICAL ACTIONS • The actions of anti-Ch. Es are qualitatively similar to that of directly acting cholinoceptor stimulants • They do not penetrate CNS and have no central effects
• Ganglia: • Anti-Ch. Es stimulate ganglia primarily through muscarinic receptors present there • CVS: Cardiovascular effects are complex. Where as muscarinic action would produce bradycardia and hypotension, ganglionic stimulation would tend to increase heart rate and BP • Skeletal muscles: After treatment with anti-Ch. Es, the ACh released by a single nerve impulse is not immediately destroyed • Rebinds to the same receptor, diffuses to act on neighboring receptors and activates prejunctional fibres → repetitive firing → twitching and fasciculation
• Higher doses cause persistent depolarization of end plates resulting in blockade of neuromuscular transmission → weakness and paralysis • Other effects: These result from stimulation of smooth muscles and glands of the gastrointestinal, respiratory, urinary tracts and in the eye • PHARMACOKINETICS • Physostigmine: It is rapidly absorbed from g. i. t. and parenteral sites • Applied to the eye, it penetrates cornea freely. • It crosses blood brain barrier and is disposed after hydrolysis by Ch. E
• Neostigmine and congeners: • These are poorly absorbed orally; oral dose is 20 -30 times higher than parenteral dose • They do not effectively penetrate cornea or cross blood brain barrier • Organophosphates : These are absorbed from all sites including intact skin and lungs • They are hydrolyzed as well as oxidized in the body and little is excreted unchanged

• INDIVIDUAL COMPOUNDS • PHYSOSTIGMINE eye drops are usually prepared freshly by ophthalmology departments • PREP: 0. 25%, 0. 5% eye drops, 1 mg/ml for i. m/i. v use • Also used for Atropine and other antimuscarinic drug poisoning. • NEOSTIGMINE: 15 mg tab, 0. 5 mg/ml in 1 ml and 5 ml inj( oral, SC, IM) Indirect action- inhibit Ch. E Direct action- directly stimulates NM receptors at NMJ (quaternary ammonium compound) • PYRIDOSTIGMINE: Resembles neostigmine in all respects but is dose to dose less potent and longer acting, less frequent dosing (twice daily in sustained release form)is required in myasthenia gravis. And better tolerated by these patients. PREP: 60 mg tab, 1 -3 tab TDS

• EDROPHONIUM: quaternary ammonium compound, rapid onset but short duration of action (5 -15 minutes) • It is used in diagnosis of myasthenia gravis • Also used in differentiate myasthenic crisis from cholinergic crisis. • Curare poisoning.
• RIVASTIGMINE: This lipophilic relatively cerebroselective Ch. E inhibitor has been introduced for Alzheimer's disease (AD)-Degenerative disease of the cerebral cortex • DONEPEZIL: Another centrally acting anti-ACh. E that has produced cognitive and behavioral improvement in AD • It is long acting and suitable for once daily administration • GALANTAMINE: This natural alkaloid inhibitor of cerebral ACh. E has in addition weak agonistic action on nicotinic receptors • It is being used to afford symptomatic relief in AD • Alzheimer's disease: it is degenerative disease of the cerebral cortex. These drugs increases cerebral levels of Ach and have shown to produce some benefit in these patients.
• Anti-Ch. E are contraindicated in • • • Sick sinus A-V conduction defects Hypotensive states Peptic ulcer and Asthma and COPD • Seizure patients.
• USES • 1. AS MIOTIC • (a) In Glaucoma: Miotics increase the tone of ciliary muscle (attached to scleral spur) and sphincter pupillae which pull on and somehow improve alignment of the trabeculae so that outflow facility is increased→ i. o. t falls in open angle glaucoma • On chronic use , it accelerates cataract formation, hence it is rarely used in glaucoma. • Pilocarpine is the preferred miotic. The action is rapid and short lasting (46 hr); 6 -8 hourly instillation is required and even then i. o. t. may fluctuate in between • A/E: Diminution of vision, especially in dim light (due to constricted pupil), spasm of accomodation and brow pain are frequent side effects
• Systemic effects – nausea, diarrhoea, sweating and bronchospasm may occur with higher concentration eye drops • Physostigmine (0. 1%) is used only to supplement pilocarpine
• 2. MYASTHENIA GRAVIS • Myasthenia gravis is an autoimmune disorder affecting about 1 in 10, 000 population • It is due to development of antibodies directed to nicotinic receptors (NR) at the muscle end plate → reduction in number of free NM cholinoceptors to 1/3 of normal or less and • Structural damage to the neuromuscular junction → weakness and easy fatigability on repeated activity, with recovery after rest • Neostigmine and its congeners improve muscle contraction by allowing ACh released from prejunctional endings to accumulate and act on receptors over a larger area, and by directly depolarizing the endplate

• Treatment is usually started with neostigmine 15 mg orally 6 hourly; dose and frequency is then adjusted according to response • Pyridostigmine is an alternative which needs less frequent dosing (twice daily) because of longer duration. • If intolerable muscarinic side effects are produced, atropine can be added to block them

• Corticosteroids afford considerable improvement in such cases by their immunosuppressant action • They inhibit production of NR-antibodies and may increase synthesis of NRs • Prednisolone 30 -60 mg/day induces remission in about 80% of the advanced cases; 10 mg daily or on alternate days can be used for maintenance therapy • Myasthenic crisis is characterized by acute weakness of respiratory muscles • It is managed by tracheal intubation and mechanical ventilation
• 3. POSTOPERATIVE PARALYTIC ILEUS/URINARY RETENTION: • This can be relieved by 0. 5 -1 mg s. c. neostigmine, provided no organic obstruction is present • 4. POSTOPERATIVE DECURARIZATION: • Neostigmine 0. 5 -2. 0 mg i. v. , preceded by atropine to block muscarinic effects, rapidly reverses muscle paralysis induced by competitive neuromuscular blockers
• 5. COBRA BITE: Cobra venom has a curare like neurotoxin. Though specific antivenom serum is the primary treatment, neostigmine + atropine prevent respiratory paralysis • 6. BELLADONNA POISONING: Physostigmine 0. 5 -2 mg i. v. repeated as required is the specific antidote for poisoning with belladonna or other anticholinergics • It penetrates blood brain barrier and antagonizes both central and peripheral actions • 7. ALZHEIMER’DISEASE: Characterized by progressive dementia, is a neurogenerative disorder, primarily affecting cholinergic neurones in the brain • The relatively cerebroselective anti-Ch. Es rivastigmine, donepezil and galantamine have been approved for clinical use

• ANTICHOLINESTERASE POISONING • All OP compounds except Echothiophate have no therapeutic applications. Echothiophate is rarely used in resistant cases of glaucoma. • OP have only toxicological importance. And most common poisoning all over the world. • Anticholinesterases are easily available and extensively used as agricultural and household insecticides; accidental as well as suicidal and homicidal poisoning is common • Local muscarinic manifestations at the site of exposure (skin, eye, g. i. t. ) occur immediately and are followed by complex systemic effects due to muscarinic, nicotinic and central actions. They are
• Muscarinic effects: Irritation of eye, lacrimation, salivation, sweating, copious tracheobronchial secretions, miosis, blurring of vision, breathlessness, colic, involuntary defecation and urination , Fall in BP, bradycardia and tachycardia, cardiac arrhythmias, vascular collapse • Nicotinic effects: Muscular fasciculations, weakness, respiratory paralysis (central as well as peripheral) due to prolonged depolarization. • Central effects: Excitement, tremor, ataxia, convulsions, coma and death( death is usually due to respiratory failure) • Death is generally due to respiratory failure
• Diagnosis: history of exposure, characteristic signs and symptoms • Estimation of cholinesterase activity in the blood, which is reduced to less than 50% of normal. • TREATMENT • 1. Termination of further exposure to the poison – fresh air, wash the skin and mucous membranes with soap and water, gastric lavage according to need • 2. Maintain patent airway, positive pressure respiration if it is failing • 3. Supportive measures – maintain BP, hydration, control of convulsions with judicious use of diazepam
• 4. Specific antidotes – • (a) Atropine: It is highly effective in counteracting the muscarinic symptoms, but higher doses are required to antagonize the central effects • It does not reverse peripheral muscular paralysis which is a nicotinic action • All cases of anti-Ch. E poisoning must be promptly given atropine 2 mg i. v. repeated every 10 minutes till dryness of mouth or other signs of atropinization appear • Continued treatment with maintenance doses may be required for 1 -2 weeks

• (b) Cholinesterase reactivators: • Oximes are used to restore neuromuscular transmission in case of organophosphate anti-Ch. E poisoning • OP compounds inactivate cholinesterases by phosphorylating the esteratic site of the enzyme. Oximes bind with high affinity to anionic site and dephosphorylate the enzymes at the esteratic site , thus reactivate them. • Pralidoxime has a quaternary nitrogen: attaches to the anionic site of the enzyme.
• Its oxime end reacts with the phosphorus atom attached to the esteratic site: the oxime-phosphonate so formed diffuses away leaving the reactivated Ch. E • Early administration of oximes is necessary before the phosphorylated enzyme undergoes “aging” and becomes resistant to reactivation.

• Pralidoxime (500 mg/20 ml infusion, 1 g/vial for inj) is injected i. v. slowly in a dose of 1 -2 g (children 20 -40 mg/kg) • Treatment should be started as early as possible (within 24 hours) • Doses may be repeated according to need (max. 12 g in first 24 hours, lower doses according to symptoms for 1 -2 weeks) • The use of oximes in organophosphate poisoning is secondary to that of atropine • Other oximes are obidoxime (more potent than pralidoxime) and diacetyl-monooxime

THANK YOU
 M cholinomimetic drugs examples
M cholinomimetic drugs examples Atropine hallucinations
Atropine hallucinations How do indirect-acting cholinergic agonists work
How do indirect-acting cholinergic agonists work Anticholinergic effects
Anticholinergic effects Structure activity relationship of cholinergic drugs
Structure activity relationship of cholinergic drugs Blocking muscarinic receptors would
Blocking muscarinic receptors would Classification of cholinergic drugs
Classification of cholinergic drugs Indirect acting cholinergic drugs
Indirect acting cholinergic drugs Anticholinergic examples
Anticholinergic examples Anticholinesterase
Anticholinesterase Ans
Ans Anticholinergic
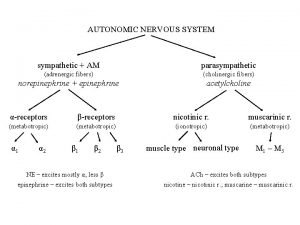
Anticholinergic Adrenergic and cholinergic difference
Adrenergic and cholinergic difference Adrenergic vs cholinergic
Adrenergic vs cholinergic Cholinergic crisis
Cholinergic crisis Cholinergic crisi
Cholinergic crisi Acetylcholine crisis
Acetylcholine crisis Dumbbells cholinergic
Dumbbells cholinergic Parasympathetic drugs classification
Parasympathetic drugs classification Cholinergic agents
Cholinergic agents Cholinergic agents
Cholinergic agents Adrenergic fibers sympathetic or parasympathetic
Adrenergic fibers sympathetic or parasympathetic Cholinergic crisi
Cholinergic crisi Cholinergic toxidrome
Cholinergic toxidrome Cholinergic toxidrome
Cholinergic toxidrome Cholinergic
Cholinergic Cholinergic interneurons striatum
Cholinergic interneurons striatum Cholinergic
Cholinergic Cholinergic
Cholinergic Section 35-4 the senses
Section 35-4 the senses Pharmacology of drugs acting on respiratory system
Pharmacology of drugs acting on respiratory system Remains simon armitage context
Remains simon armitage context Open closed and isolated systems
Open closed and isolated systems Circularory system
Circularory system Mydriatics and miotics drugs
Mydriatics and miotics drugs Rate and rhythm control drugs
Rate and rhythm control drugs Neurotransmitters and drugs
Neurotransmitters and drugs Organised and unorganised crude drugs
Organised and unorganised crude drugs Rate and rhythm control drugs
Rate and rhythm control drugs Chapter 19 vocabulary glencoe health
Chapter 19 vocabulary glencoe health Chapter 7 alcohol other drugs and driving
Chapter 7 alcohol other drugs and driving Clarke's analysis of drugs and poisons
Clarke's analysis of drugs and poisons Drugs and alcohol toolbox talk
Drugs and alcohol toolbox talk Remains simon armitage text
Remains simon armitage text Drugs that alter moods thoughts and sense perceptions
Drugs that alter moods thoughts and sense perceptions Why must we put all chemicals and drugs in locked cupboards
Why must we put all chemicals and drugs in locked cupboards Psychedelic drugs that distort perceptions and evoke
Psychedelic drugs that distort perceptions and evoke Drugs that alter moods, thoughts, and sense perceptions
Drugs that alter moods, thoughts, and sense perceptions First pass effect
First pass effect Chapter 15 alcohol other drugs and driving
Chapter 15 alcohol other drugs and driving Chemistry food and drugs
Chemistry food and drugs