Anesthesia Considerations in Thoracic Trauma Patients 2009 11













- Slides: 48
Anesthesia Considerations in Thoracic Trauma Patients 張婉玲 醫師 嘉義長庚醫院 麻醉科 2009. 11. 21.
Introduction • Mortality from chest injuries is around 10% • The majority of patients with thoracic trauma can be managed conservatively • Require thoracotomy: ® Blunt trauma: 10 % ® Penetrating trauma: 15 %~ 30 %

Initial Management Plan • Airway maintenance with cervical spine protection • Breathing: ventilation and oxygenation • Circulation with hemorrhage control
Initial Assessment Ø Primary Survey: –AIRWAY • Always assume a cervical spine injury exists until proven • Jaw-thrust maneuver
Initial Assessment • ALWAYS ASSUME FULL STOMACH PRECAUTIONS---RAPID SEQUENCE INTUBATION

• Indications for intubation: –Airway obstruction –Pa. O 2 < 80 mm. Hg or Sp. O 2 < 90% with O 2 –Shock with SBP < 90 mm. Hg –Severe head injury or unconscious (GCS <9) –Anticipated surgery with multisystem injury
Initial Assessment • Awake intubation: local, topical superior laryngeal nerve blocks • Awake fiberoptic: may be too bloody • Awake cricothyrotomy/tracheostomy • Know your difficult airway algorithm!
Initial Assessment • BREATHING – 100 % O 2 –Always verify correct position of ETT.
Initial Assessment • Circulation –Control hemorrhage first! –Crystalloids vs. colloids vs. blood products?
Secondary survey • After primary survey complete, attempt to complete a head-to-toe assessment
Preop assessment • Cardiac: S/S shock, EKG changes • Respiratory: Breath sounds, crepitus, respiratory patterns/distress, CXR • Neurologic: GCS, LOC; assume C-spine injury until ruled out Lateral C-spine Xray, palpate neck • Renal: monitor urine output, amount and color
Preop assessment • Gastrointestional: FULL STOMACH!!!! • Endocrine: release of stress hormones (catecholaminesand glucose) • Hematologic: hypovolemicshock; coagulopathies
Laboratory/diagnostic tests • CBC, electrolytes, urinalysis, PT/PTT, lactate, baseline ABG (as condition permits) • CXR, lateral C-spine, CT/MRI • 12 lead EKG • FAST: focused abdominal sonography for trauma
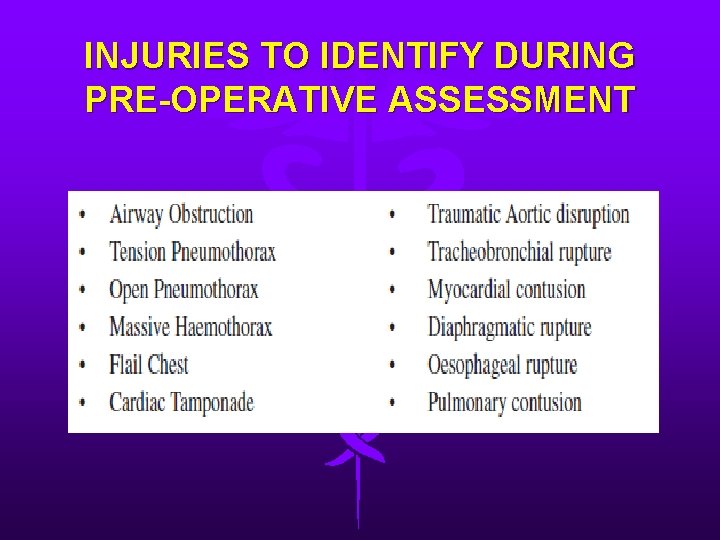
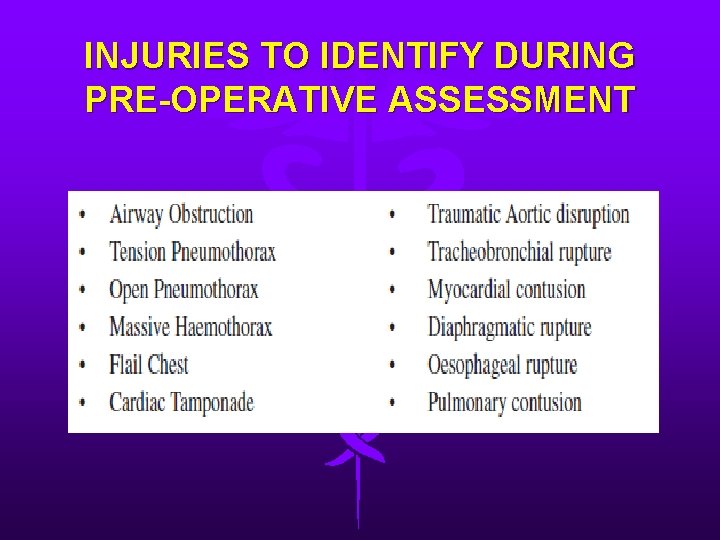
INJURIES TO IDENTIFY DURING PRE-OPERATIVE ASSESSMENT
AIRWAY INJURY/OBSTRUCTION • Intrathoracic tracheobronchial injuries are less common than upper airway injuries. • High mortality. • A definitive airway can usually be secured using a fiber-optic bronchoscope
Pneumothorax • Accumulation of air between parietal and visceral pleura • Results in severe V/Q mismatch and hypoxia • S/S: –chest wall hyperresonant to percussion –Breath sounds decreased or absent unilaterally –Subcutaneous emphysema –CXR confirms
Tension pneumothorax • Diagnosis of tension pneumothorax is clinical rather than radiological - Absent breath sounds - Hyper-resonant percussion - No chest movement - Tracheal deviation to the injured side - Distended neck veins (may not be seen if the patient is hypovolaemic). - Severe dyspnoea, tachycardia and hypotension

Tension pneumothorax • Immediate chest decompression is required. • During anaesthesia ü In pressure controlled modes: ↓ tidal volume ü In volume controlled modes: ↑ peak airway pressure

OPEN PNEUMOTHORAX • >2/3 rd the diameter of the trachea. • This results in paradoxical breathing with collapse of the lung on the affected side during inspiration. • This results in increased intra-pulmonary shunt, decreased venous return and progressive hypoxaemia and hypercapnia. • Administration of oxygen, covering the wound and chest drain insertion.

Hemothorax • Can be caused from bleeding of intercostal vessels, pulmonary arteries or veins, avulsion of mediastinal vessels or penetrating cardiac injury. • Differentiated from pneumothorax by dullness to percussion with absent breath sounds


Hemothorax • The choice and dose of anaesthetic induction agent is determined by the severity of the shock and any preexisting medical co-morbidity • Fluid load before chest tube placement • Thoracotomy may be needed if drainage is more than 250 mls per hour, or the patient’s physiological status continues to deteriorate despite fluid replacement.
Flail chest • Results from two or more ribs fracture in two or more places • Accompanied by hemothorax or pulmonary contusion • Patients with 3 or more rib fractures have greater likelihood of hepatic or splenicinjury
Flail chest • S/S –Paradoxical chest wall movement • Treatment –O 2 –Pain control

Cardiac tamponade • Life-threatening emergency • Bleeding into pericardial space, which restricts cardiac filling during diastole and creates a low cardiac output state • Initial symptoms - Dyspnea – Orthopnea – tachycardia
Cardiac tamponade • Classic symptoms –Beck’s triad neck vein distention, hypotension, muffled heart sounds –Pulsus paradoxus: > 10 mm. Hg decrease in blood pressure during spontaneous inspiration • May not be evident in hypovolemia

Cardiac tamponade • Echocardiography provides the definitive diagnosis.
ANAESTHESIA FOR RESUSCITATIVE THORACOTOMY • Penetrating cardiac injury may rapidly lead to cardiac arrest. • Induction of anaesthesia may lead to a dramatic loss of blood pressure and care should be taken with the choice of induction agent.

AORTIC DISRUPTION • A wide mediastinum on chest X-ray may be the only indication that the injury has occurred • Spiral contrast CT is now performed more frequently than angiography
TRACHEOBRONCHIAL INJURY • high mortality • In blunt trauma the majority of injuries occur within a 2 – 3 cm of the carina • Signs include haemoptysis, subcutaneous emphysema and persisting pneumothorax or broncho-pleural fistula following chest drain insertion.
TRACHEOBRONCHIAL INJURY • Low tidal volume, permissive hypercapnia ventilatory strategies are required until surgical intervention has occurred. • Once intubated fibre optic bronchoscopy is needed to identify the site of the leak.
OESOPHAGEAL DISRUPTION • very rare • most frequently occurring in the lower oesophagus
DIAPHRAGMATIC RUPTURE • most commonly after blunt abdominal trauma. • Usually on the left side. • Classically the stomach, nasogastric tube or colon is noted to be in the left side of the chest on chest X-ray.

Pulmonary contusion • Intra-alveolar hemorrhage and edema resulting from sudden increase in intraalveolar pressure and rupture of alveolar-capillary interface • Difficult to diagnosis
ARDS • Later pulmonary complication • Attributed to direct thoracic injury, sepsis, aspiration, head injury, massive transfusion, oxygen toxicity, and fat embolism • Mortality rate reaching 50%
INTRA-OPERATIVE LUNG PROTECTIVE STRATEGIES • LUNG PROTECTIVE VENTILATION ü tidal volume 6 - 8 mls/kg ü trans alveolar pressure is kept below 35 cm of water (plateau airway pressure of 35 - 45 cm of water).
INTRA-OPERATIVE LUNG PROTECTIVE STRATEGIES • INTRA-OPERATIVE LUNG RECRUITMENT ü Extrinsic PEEP ü a single large tidal breath and holding end inspiration for 20 seconds
Myocardial contusion • Associated with blunt trauma • Contusion most often right ventricle since lies directly posterior to sternum • S/S –Dysrhythmias: heart block to Vfib; ST segment elevation –Elevated CPK-MB; ? Troponin elevation –CHF –Anginal pain which may or may not respond to nitrates
Anesthetic management • The general principles of trauma anesthesia such as oxygenation, restoration of circulating volume, correction of hypothermia and coagulopathy.
Anesthetic management Ø Induction • Standard monitors • Preoxygenation • direct laryngoscopy + RSI • Invasive monitors as indicated
Induction agents • Thiopental 3 -4 mg/kg; reduce doses in unstable patients • Ketamine 0. 5 -1 mg/kg; useful for burn and hypovolemic patients; avoid with head injuried • Etomidate 0. 1 -0. 3 mg/kg; reduce doses with hypovolemia • Propofol 1 -2 mg/kg in stable patients; reduce doses in hypovolemia

Muscle relaxants • Succinylcholine: 1 -2 mg/kg; useful for RSI • Rocuronium: 1 mg/kg

ONE LUNG ANAESTHESIA • Double-lumen tubes are often difficult to insert during rapid sequence intubation and are commonlyassociated with malposition.
Maintenance • Low-dose volatile agent with fentanyl and nondepolarizing muscle relaxant is usually suitable. • Avoid Nitrous oxide. • Bispectral index monitor
Conclusion • Blunt or penetrating thoracic injuries present a particular challenge as a result of complex, dynamic and lifethreatening injuries • The roles of the anesthesiologist and anesthetist are critical.
 Gastrectomy anesthesia considerations
Gastrectomy anesthesia considerations Eswl anesthesia considerations
Eswl anesthesia considerations Lippincott williams & wilkins
Lippincott williams & wilkins Management of patients with neurologic trauma
Management of patients with neurologic trauma Examples of consideration
Examples of consideration Pricing considerations and approaches
Pricing considerations and approaches Database design considerations
Database design considerations Fluid intake pdhpe
Fluid intake pdhpe Collaboration design considerations
Collaboration design considerations Data warehouse considerations
Data warehouse considerations Appendix sample
Appendix sample Pre-analytical considerations in phlebotomy
Pre-analytical considerations in phlebotomy Retromylohyoid muscle
Retromylohyoid muscle Atm kiosk software
Atm kiosk software Hach wims
Hach wims Contrasting acquisition
Contrasting acquisition Ethical consideration in experimental research sample
Ethical consideration in experimental research sample Freedom of displacement in tooth preparation
Freedom of displacement in tooth preparation Azure landing zone considerations
Azure landing zone considerations Simple mask
Simple mask Web security considerations
Web security considerations Bioreactor considerations for animal cell culture
Bioreactor considerations for animal cell culture Dogso e spa
Dogso e spa Three considerations of societal marketing concept
Three considerations of societal marketing concept Ethical consideration in research
Ethical consideration in research What is cloud delivery model
What is cloud delivery model Identify the device
Identify the device What are the general considerations in machine design
What are the general considerations in machine design Anatomical considerations
Anatomical considerations Dissect the broad area into sub-areas
Dissect the broad area into sub-areas Ethical considerations examples
Ethical considerations examples Practical considerations for costume design might include
Practical considerations for costume design might include Mechanical considerations of transmission line
Mechanical considerations of transmission line Final design icon
Final design icon Azure landing zone considerations
Azure landing zone considerations Writing strategies and ethical considerations
Writing strategies and ethical considerations Design considerations for mobile computing
Design considerations for mobile computing Tax considerations for setting up a new business
Tax considerations for setting up a new business Biopharmaceutic considerations in drug product design
Biopharmaceutic considerations in drug product design Santa fe pain and spine
Santa fe pain and spine Thoracic outlet wedge pillow
Thoracic outlet wedge pillow Angle of louis
Angle of louis Plumb line posture
Plumb line posture Mitral stenosis chest x ray
Mitral stenosis chest x ray Lumbar vertebrae characteristics
Lumbar vertebrae characteristics Thoracic lumbar fascia
Thoracic lumbar fascia Rib tubercle
Rib tubercle Thoracic cavity labeled
Thoracic cavity labeled Diaphragm thoracic level
Diaphragm thoracic level