ANAESTHETIC MANAGEMENT OF TURP Dr S Parthasarathy MD
![HYPOOSMOLALITY • Hypoosmolality is more important than hyponatremia • 2[Na+] + [Glucose]/18 + [ HYPOOSMOLALITY • Hypoosmolality is more important than hyponatremia • 2[Na+] + [Glucose]/18 + [](https://slidetodoc.com/presentation_image_h2/1aa0400a3af0be1773aab4e2b2252677/image-26.jpg)

- Slides: 44
ANAESTHETIC MANAGEMENT OF TURP Dr. S. Parthasarathy MD. , DA. , DNB, MD (Acu), Dip. Diab. DCA, Dip. Software statistics Ph. D. (physiology) Mahatma Gandhi medical college and research institute , puducherry – India
HOW COMMON ? ? • Approximately 40 000 transurethral resections • of the prostate (TURP) are performed annually • in the UK. • In pondicherry • 60 – 70 / month
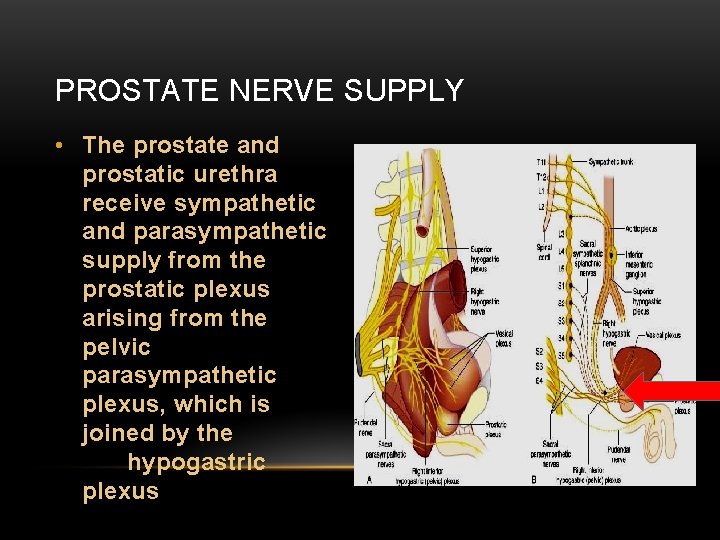
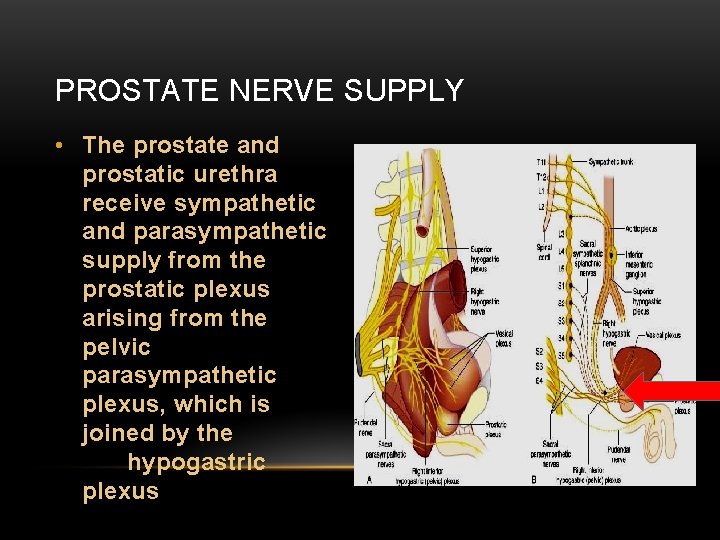
PROSTATE NERVE SUPPLY • The prostate and prostatic urethra receive sympathetic and parasympathetic supply from the prostatic plexus arising from the pelvic parasympathetic plexus, which is joined by the hypogastric plexus
NERVE AND BLOOD • Pain from prostate – sacral nerves S 2 – S 4 • But bladder distension – sympathetic – T 11 – L 2 • It has a rich blood supply and venous drainage is via the large, thin-walled sinuses adjacent to the capsule.
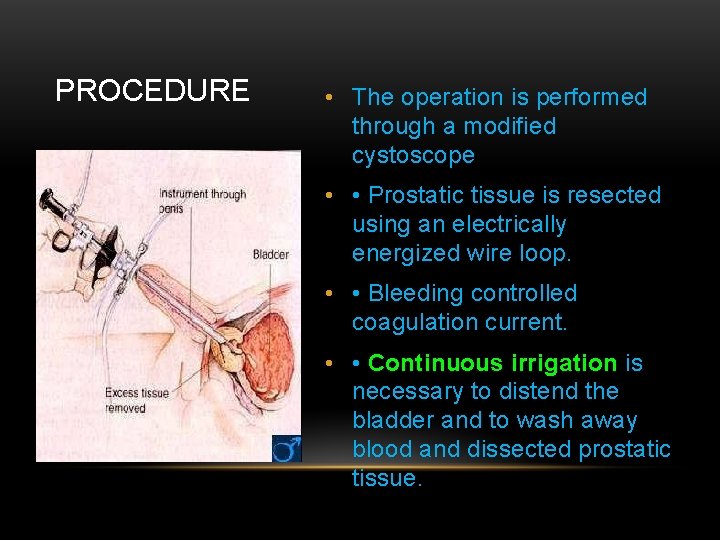
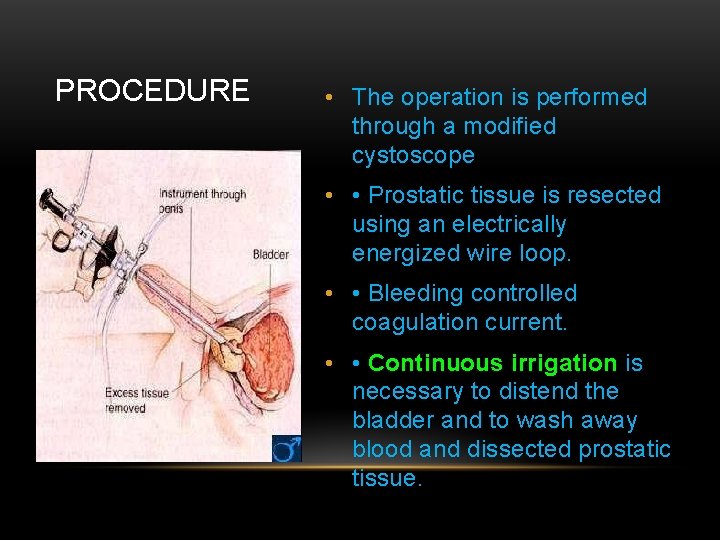
PROCEDURE • The operation is performed through a modified cystoscope • • Prostatic tissue is resected using an electrically energized wire loop. • • Bleeding controlled coagulation current. • • Continuous irrigation is necessary to distend the bladder and to wash away blood and dissected prostatic tissue.
PREOP - SYSTEMIC ILLNESS • • • Age – 69 Diabetes, musculo skeletal , Neuro, renal CVS GI , COPD , airway • Occasionly patients are dehydrated and depleted of essential electrolytes (long-term diuretic therapy and restricted fluid intake).
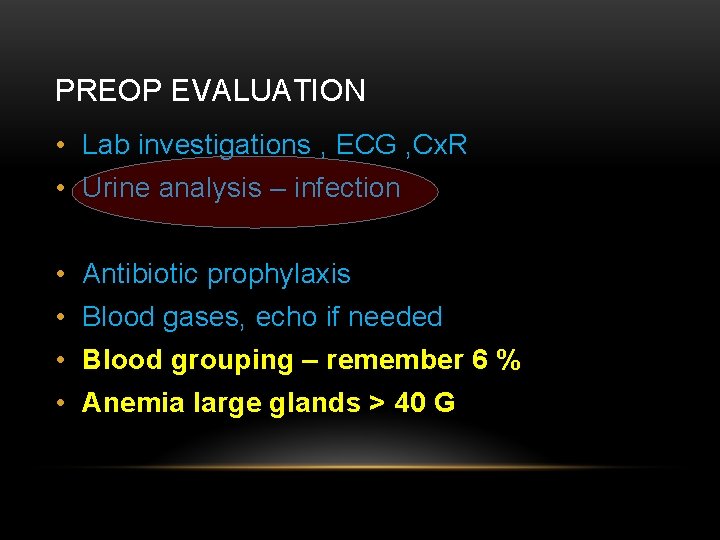
PREOP EVALUATION • Lab investigations , ECG , Cx. R • Urine analysis – infection • Antibiotic prophylaxis • Blood gases, echo if needed • Blood grouping – remember 6 % • Anemia large glands > 40 G
DRUGS • antihypertensive and antianginal drugs should be continued until the day of surgery. • Beta blockers • ACE inhibitors • Bronchodilators • Anti diabetic drugs • Warfarin
PREMEDICATION • Antibiotics, drugs and benzodiazepines • Anesthesia • Regional / GA
ANESTHESIA • Spinal anaesthesia is regarded as the technique of choice for TURP • 2. 5– 3. 0 ml of 0. 5% plain or hyperbaric bupivacaine may be used. • Level T 10 • Why ? ? - bladder, capsular sign !! • Why spinal ? ?
FOR SPINAL • for patients with significant respiratory disease. • good postoperative analgesia , blood loss less • may reduce the stress response to surgery. • spinal anaesthesia allows the anaesthetist to monitor the patient’s level of consciousness, which makes it easier to detect the early signs of TURP syndrome. • Early recognition of capsular tears and bladder perforation is also possible
TIPS ABOUT SPINAL • Intraoperative fluid overload less • DVT less • Use vasopressors for hypotension – add fentanyl. • Technically easy than epidural • Sacral sparing – no • USE NS than RL – more osmolar and more sodium • Warm IVF •
GENERAL ANAESTHESIA • Contraindication to spinal • Cant lie down for longer times • Cough during lying down. • ETT or proseal LMA • Dilutional hyponatremia – prolong NM blockers • Post op caudal • Rarely done under LA
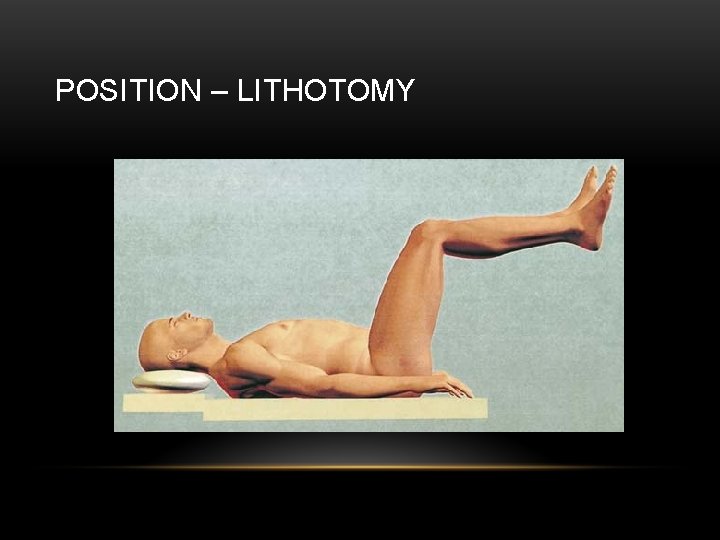
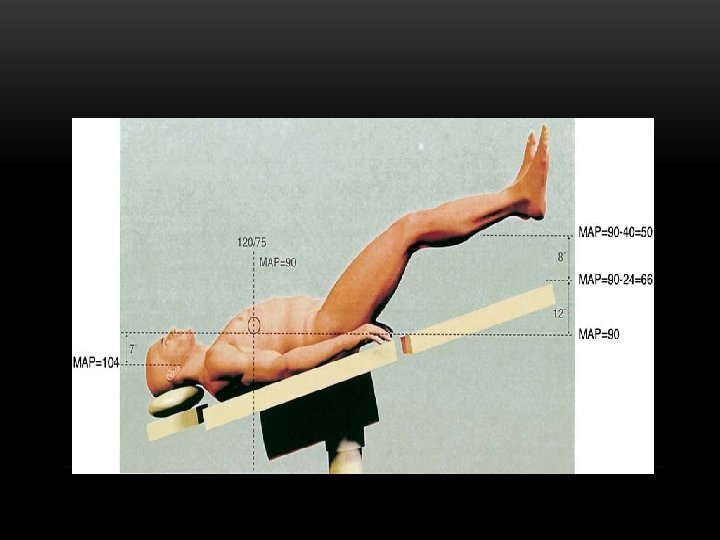
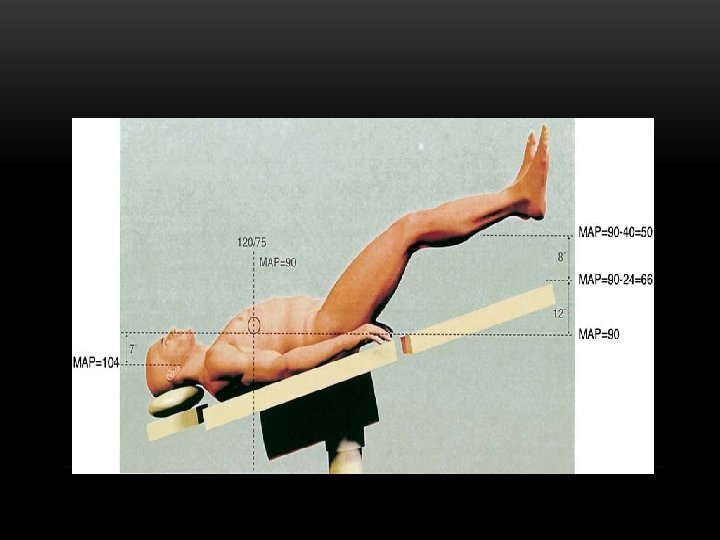
LITHOTOMY • Significant amount of intravascular volume is added to the central circulation. • Perfusion pressure of lower extremities = 10 – 15 mm. Hg – compression – compartment syndrome • Nerve compressions • Respiratory changes
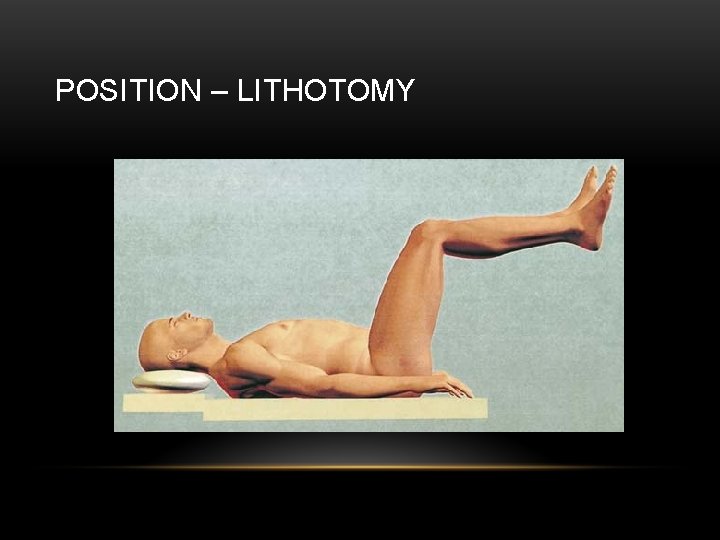
POSITION – LITHOTOMY
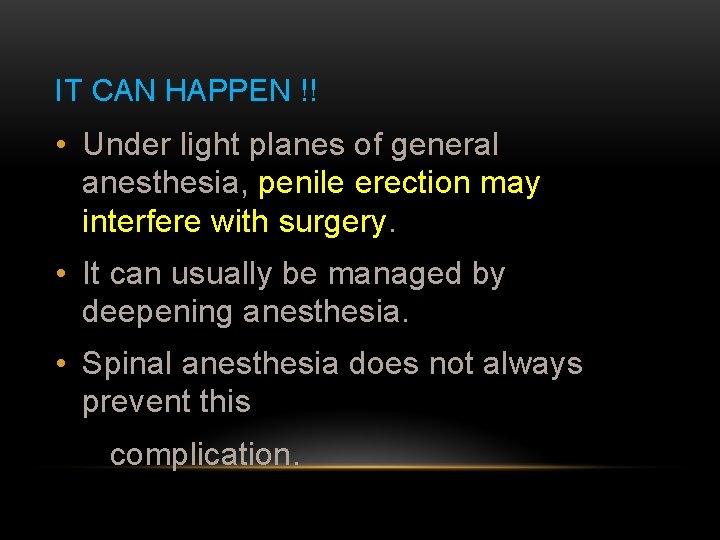
IT CAN HAPPEN !! • Under light planes of general anesthesia, penile erection may interfere with surgery. • It can usually be managed by deepening anesthesia. • Spinal anesthesia does not always prevent this complication.
Irrigation fluid
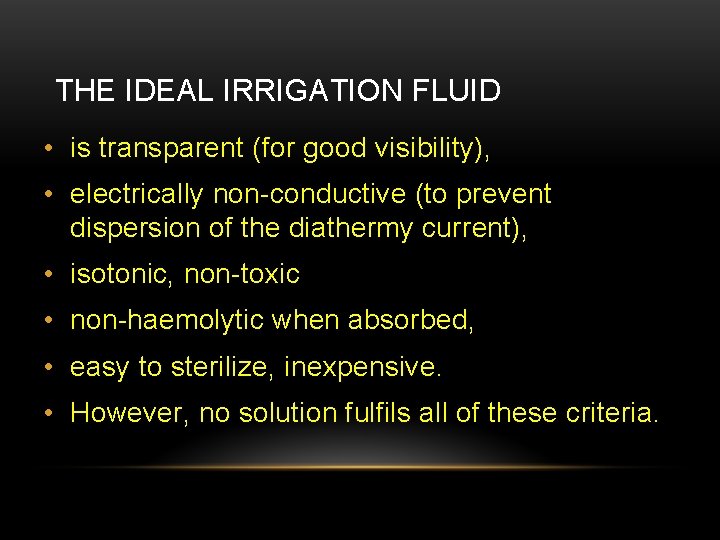
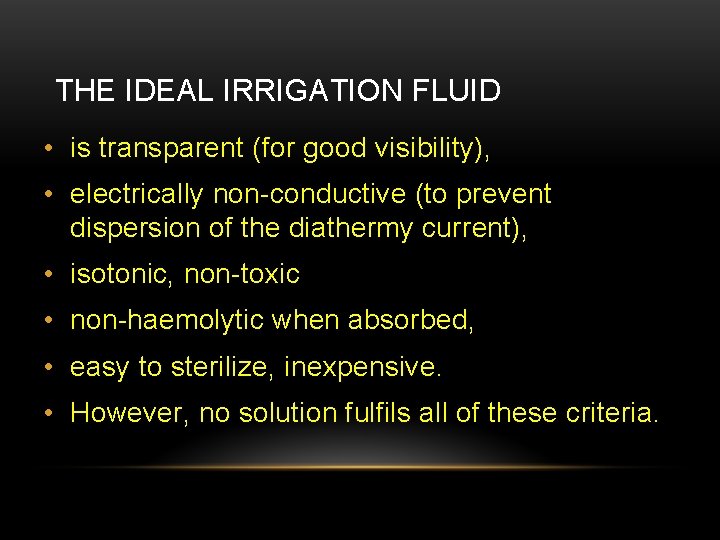
THE IDEAL IRRIGATION FLUID • is transparent (for good visibility), • electrically non-conductive (to prevent dispersion of the diathermy current), • isotonic, non-toxic • non-haemolytic when absorbed, • easy to sterilize, inexpensive. • However, no solution fulfils all of these criteria.
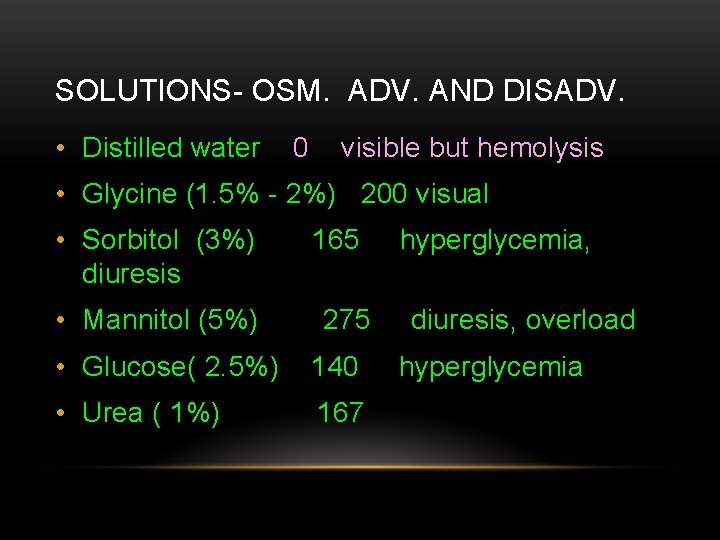
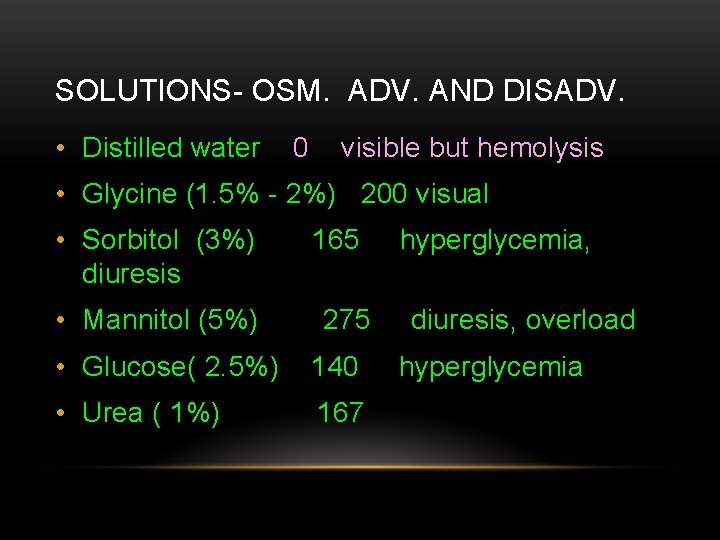
SOLUTIONS- OSM. ADV. AND DISADV. • Distilled water 0 visible but hemolysis • Glycine (1. 5% - 2%) 200 visual • Sorbitol (3%) diuresis • Mannitol (5%) 165 275 • Glucose( 2. 5%) 140 • Urea ( 1%) 167 hyperglycemia, diuresis, overload hyperglycemia
TURP SYNDROME
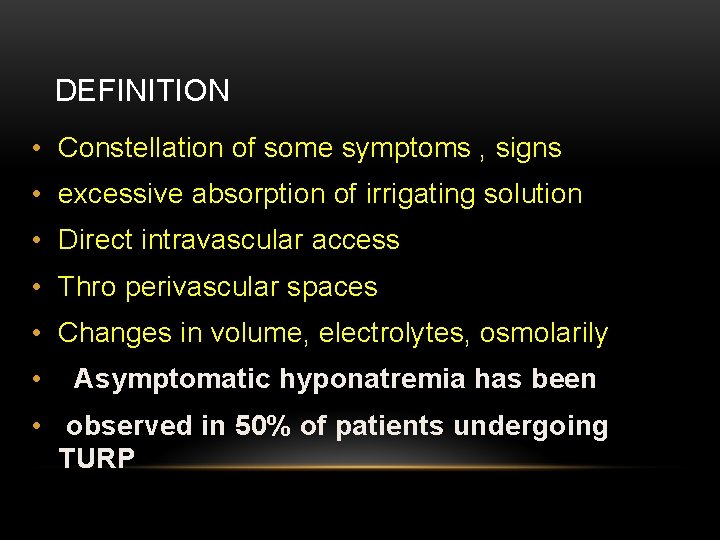
DEFINITION • Constellation of some symptoms , signs • excessive absorption of irrigating solution • Direct intravascular access • Thro perivascular spaces • Changes in volume, electrolytes, osmolarily • Asymptomatic hyponatremia has been • observed in 50% of patients undergoing TURP
HOW MUCH AND WHEN • 1– 8% • 15 minutes to after 24 hours • Direct vascular or bladder rupture and absorption • Mortality around 0. 2% - 0. 8%
CLINICAL FEATURES • Acute fluid overload --- hypertension and reflex bradycardia • Later on equilibration from ECF, hypotension and hypovolumia • Sympathetic block of spinal • Can precipitate pulmonary edema
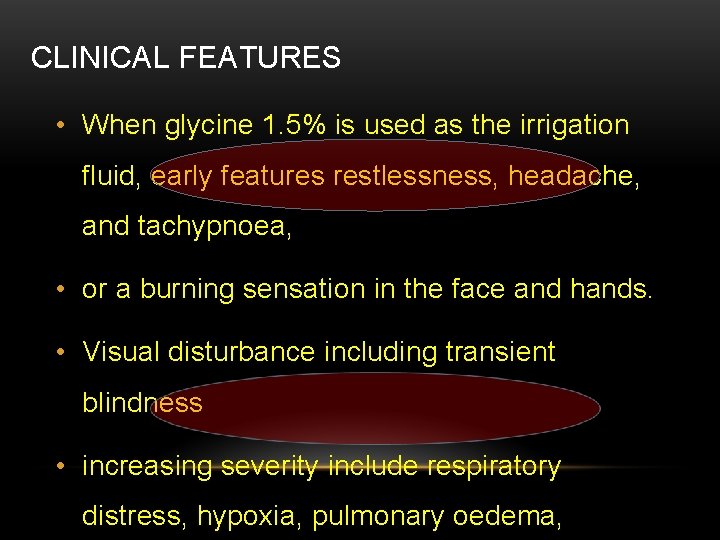
CLINICAL FEATURES • When glycine 1. 5% is used as the irrigation fluid, early features restlessness, headache, and tachypnoea, • or a burning sensation in the face and hands. • Visual disturbance including transient blindness • increasing severity include respiratory distress, hypoxia, pulmonary oedema,
![HYPOOSMOLALITY Hypoosmolality is more important than hyponatremia 2Na Glucose18 HYPOOSMOLALITY • Hypoosmolality is more important than hyponatremia • 2[Na+] + [Glucose]/18 + [](https://slidetodoc.com/presentation_image_h2/1aa0400a3af0be1773aab4e2b2252677/image-26.jpg)
HYPOOSMOLALITY • Hypoosmolality is more important than hyponatremia • 2[Na+] + [Glucose]/18 + [ BUN ]/2. 8 • Effective pore size of BBB is 8 A – permeable to water than sodium
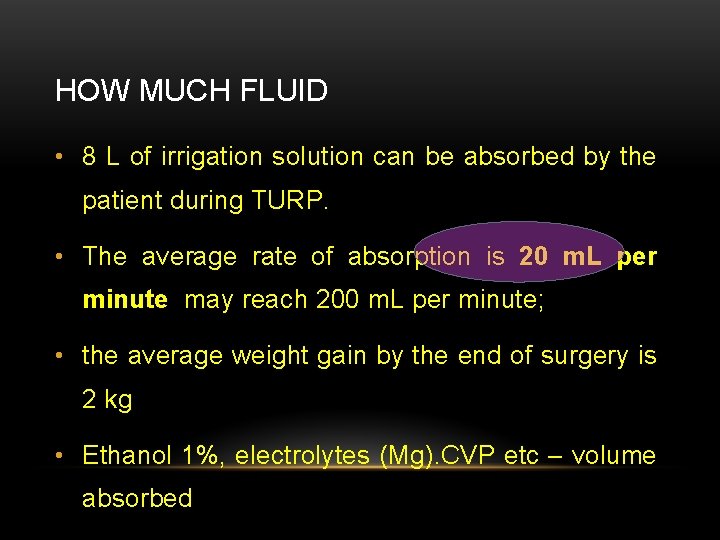
HOW MUCH FLUID • 8 L of irrigation solution can be absorbed by the patient during TURP. • The average rate of absorption is 20 m. L per minute may reach 200 m. L per minute; • the average weight gain by the end of surgery is 2 kg • Ethanol 1%, electrolytes (Mg). CVP etc – volume absorbed
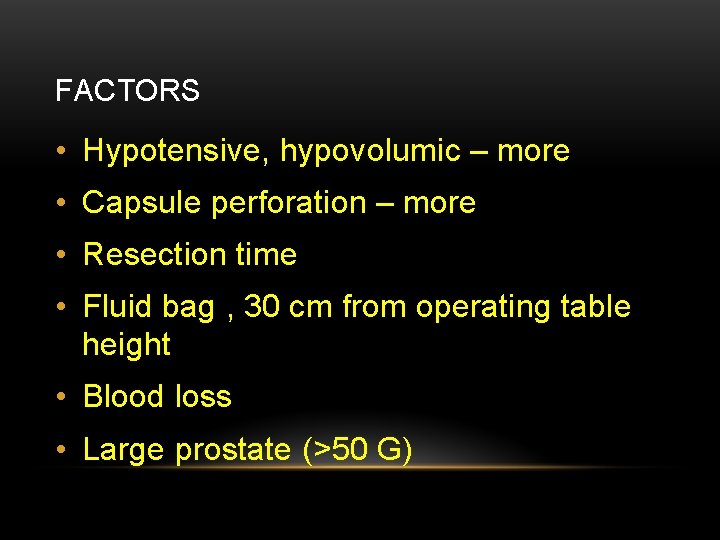
FACTORS • Hypotensive, hypovolumic – more • Capsule perforation – more • Resection time • Fluid bag , 30 cm from operating table height • Blood loss • Large prostate (>50 G)
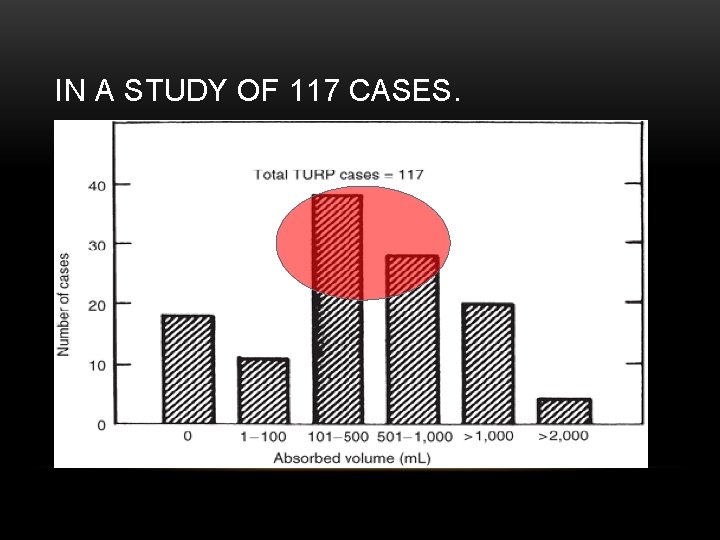
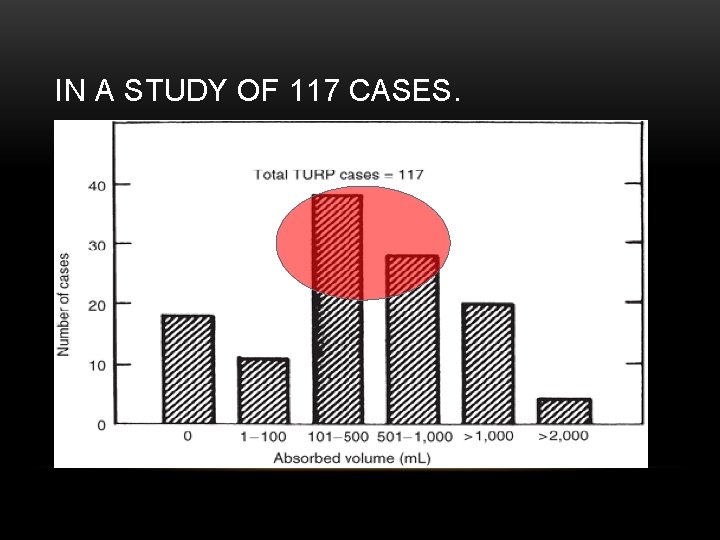
IN A STUDY OF 117 CASES.
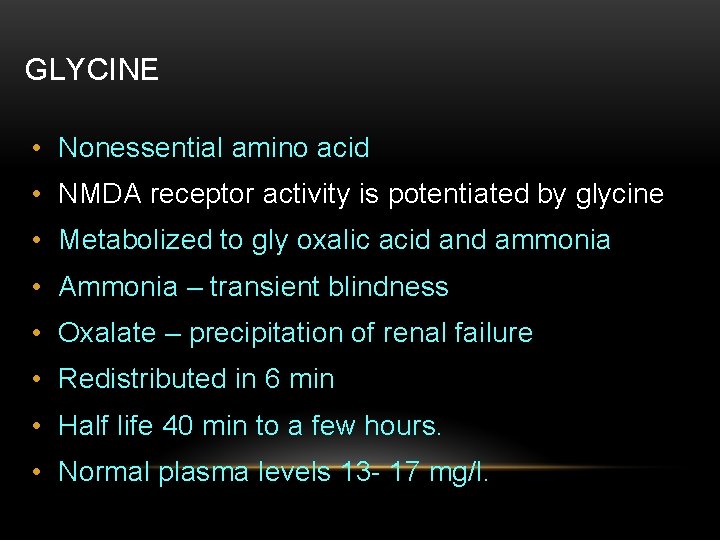
GLYCINE • Nonessential amino acid • NMDA receptor activity is potentiated by glycine • Metabolized to gly oxalic acid and ammonia • Ammonia – transient blindness • Oxalate – precipitation of renal failure • Redistributed in 6 min • Half life 40 min to a few hours. • Normal plasma levels 13 - 17 mg/l.
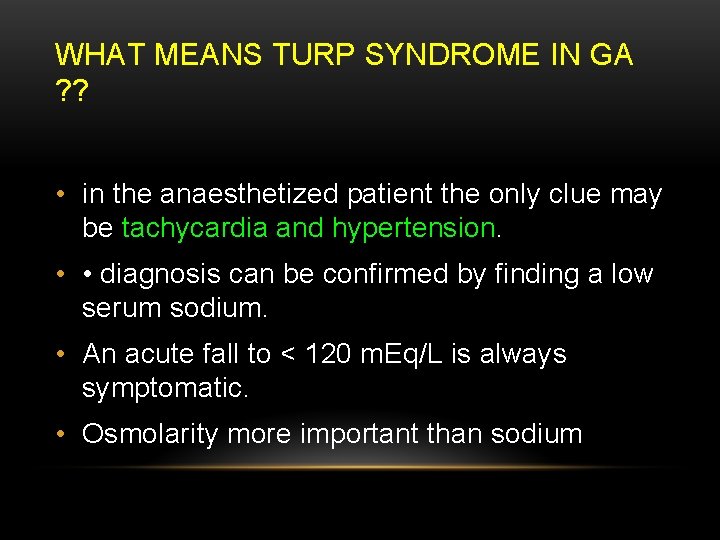
WHAT MEANS TURP SYNDROME IN GA ? ? • in the anaesthetized patient the only clue may be tachycardia and hypertension. • • diagnosis can be confirmed by finding a low serum sodium. • An acute fall to < 120 m. Eq/L is always symptomatic. • Osmolarity more important than sodium
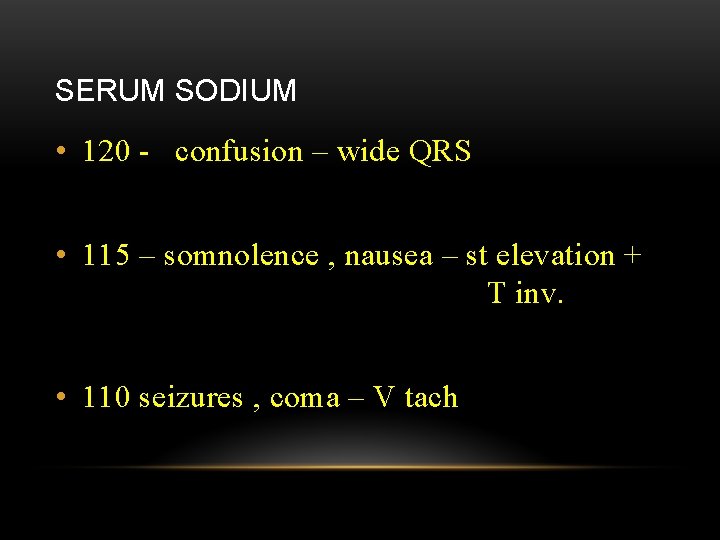
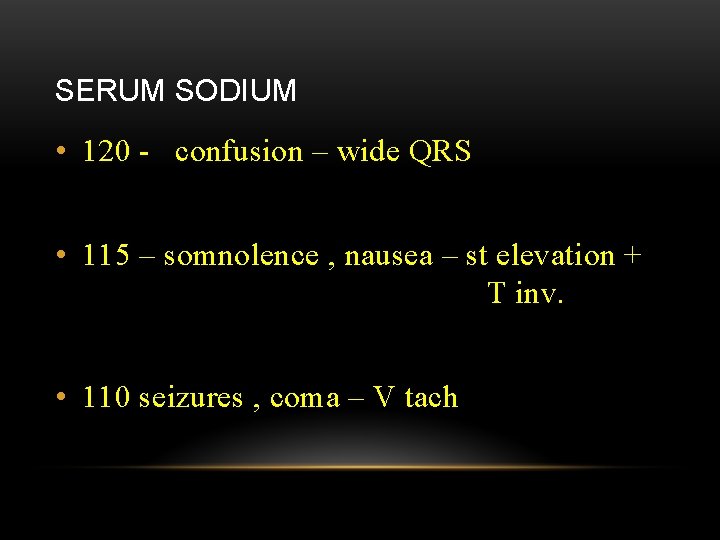
SERUM SODIUM • 120 - confusion – wide QRS • 115 – somnolence , nausea – st elevation + T inv. • 110 seizures , coma – V tach
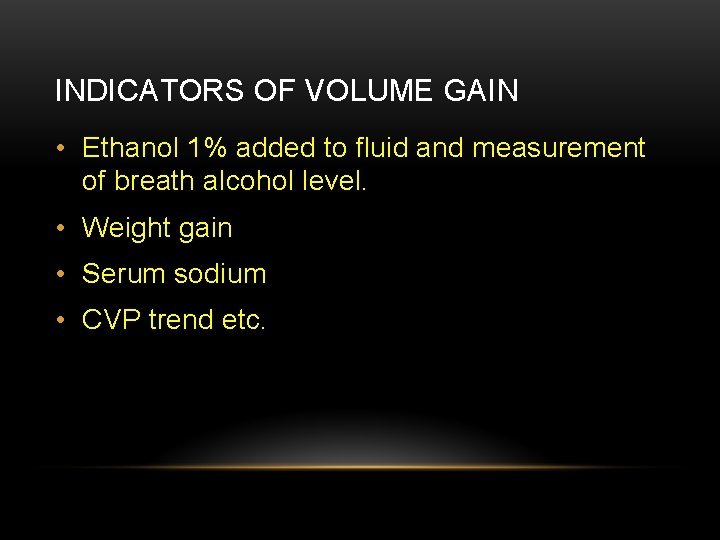
INDICATORS OF VOLUME GAIN • Ethanol 1% added to fluid and measurement of breath alcohol level. • Weight gain • Serum sodium • CVP trend etc.
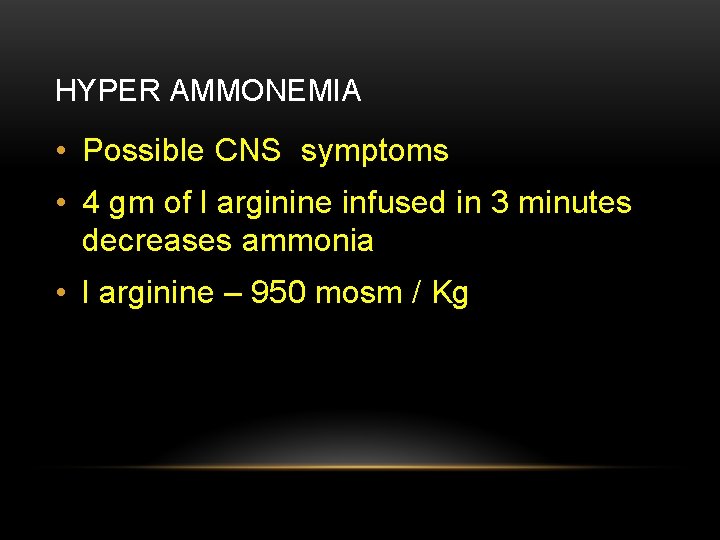
HYPER AMMONEMIA • Possible CNS symptoms • 4 gm of l arginine infused in 3 minutes decreases ammonia • l arginine – 950 mosm / Kg
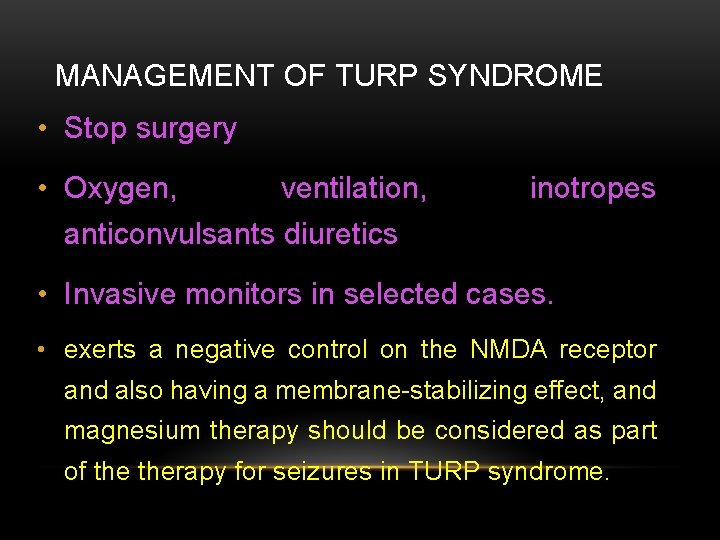
MANAGEMENT OF TURP SYNDROME • Stop surgery • Oxygen, ventilation, inotropes anticonvulsants diuretics • Invasive monitors in selected cases. • exerts a negative control on the NMDA receptor and also having a membrane-stabilizing effect, and magnesium therapy should be considered as part of therapy for seizures in TURP syndrome.
INVESTIGATIONS • Blood , BUN, glucose , ABG , electrolytes • CXR, ECG, Hematocrit • Severe cases of symptomatic hyponatremia • 3 % hypertonic saline 2 * 0. 6 * Weight • 2 *42 = 84 ml of 3% hypertonic saline – I meq. / l • I F we correct fast – • Osmotic demyelination syndrome.
INTRAOPERATIVE • Myocardial ischaemia - can occur in up to 25% of patients during TURP, with myocardial infarction occurring in 1 -3% • Hypothermia. . Warmed irrigation fluid has NOT been shown to increase blood loss by local vasodilation. • warm i. v. fluids, active patient warming devices. • • Perforation of prostatic capsule, urethra or bladder with the resectoscope. • • Bleeding
BLOOD LOSS • blood loss should lie within the range of 7 -20 ml per gram of resected tissue. • Or • 2 - 5 ml / minute
FACTORS - 1 % • Large gland • Time , Infection • Pre op catheter • TRANEXAMIC ACID 15 MG / KG - useful • Prostate can release thromboplastin to cause fibrinolysis. -- EACA
BLADDER PERFORATION • Peri umbilical pain • Hypotension sweating restlessness • Hiccups • Rarely shoulder pain • Spinal identifies
POST OPERATIVE PROBLEMS • Pain – not severe. - rare use opioids • Bladder spasm • Clot retention – • precipitate bradycardia • TURP syndrome • Cognition impairment
DVT AND PE • compression stockings are usually adequate as prophylaxis. • Low-molecular-weight heparin should be considered in patients at higher risk • (poor mobility, malignancy, inter current illness, and obesity).
SUMMARY - TURP • High number • Preop disease , antibiotics • spinal , level, Position ( GA / LA) • TURP syndrome – irrigation fluid 20 ml/ min. , factors • Hypoosmolarity – NS , inotropes, stop surgery • Blood loss, perforation bladder • Pain ? ?

THANK YOU ALL
 Mturp
Mturp Ramya parthasarathy
Ramya parthasarathy Ramya parthasarathy
Ramya parthasarathy Maya parthasarathy
Maya parthasarathy Top management middle management first line management
Top management middle management first line management Management pyramid
Management pyramid Middle level management
Middle level management Time management human resources
Time management human resources Performance management network definition
Performance management network definition Managing assets vs asset management
Managing assets vs asset management Configuration management project management
Configuration management project management Crm and scm
Crm and scm Organized retailing
Organized retailing Principles of project cost management
Principles of project cost management Behavioural management theory
Behavioural management theory Network accounting management
Network accounting management Literal sense in hrm
Literal sense in hrm Contoh sales management
Contoh sales management Quality management in operations management
Quality management in operations management Traditional management vs entrepreneurial management
Traditional management vs entrepreneurial management Erp in supply chain management ppt
Erp in supply chain management ppt Sequence of a typical manufacturing supply chain
Sequence of a typical manufacturing supply chain Configuration management in software project management
Configuration management in software project management Operations management chapter 12 inventory management
Operations management chapter 12 inventory management Gplms grade 3
Gplms grade 3 Introduction for project
Introduction for project Demand management and capacity management
Demand management and capacity management What is project integration management
What is project integration management Introduction to network management
Introduction to network management Network management definition
Network management definition Operations management with total quality management book
Operations management with total quality management book Workflow management with calendar
Workflow management with calendar C srinivasan waste management
C srinivasan waste management Cmmi level 3 documentation templates
Cmmi level 3 documentation templates Snmpc management console
Snmpc management console Project procurement management lecture notes
Project procurement management lecture notes Genesis management and market research
Genesis management and market research Employers claim management
Employers claim management Wvu risk management
Wvu risk management Windows server 2008 ip address management
Windows server 2008 ip address management Data management concepts
Data management concepts Operating cycle formula
Operating cycle formula Management accounting subject code
Management accounting subject code Acme workflow management
Acme workflow management Workers participation in management
Workers participation in management