Laparoscopy anaesthetic concerns Dr S Parthasarathy MD DA









- Slides: 54
Laparoscopy- anaesthetic concerns Dr. S. Parthasarathy MD. , DA. , DNB, MD (Acu), Dip. Diab. DCA, Dip. Software statistics Ph. D (physio) Mahatma Gandhi medical college and research institute , puducherry – India
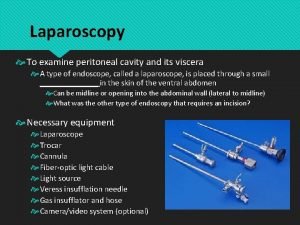
What is it ? ? • Laparoscopy (or peritoneoscopy) is a “minimally invasive” procedure allowing endoscopic access to the peritoneal cavity after insufflation of a gas (CO 2) to create space between the anterior abdominal wall and the viscera. • Laparoscopic surgery can also be extraperitoneal. It can also be gasless with abdominal wall retraction, • Hand assisted

Some history • • • Laparoscopy introduced in 20 th Century 1975 : first laparoscopic salpingectomy 1970 -- 80 : used for gyne procedures 1981: Semm, from Germany, 1 st lap appendectomy 1989: laparoscopic cholecystectomy
All surgeries including laparoscopic autopsies

Why ? ?
major benefits Small incision reduced postoperative discomfort, shortened recovery rates, lower incidence of post operative wound infections • Less post op pulmonary complications • shorter in-patient stay • •

Advantages • Obesity and bariatric surgery • Pulmonary diseases
There are some disadvantages also
Disadvantages • Higher equipment costs • May be longer time of surgery • Cannot do • Positioning and Pneumoperitoneum cardiopulmonary effects
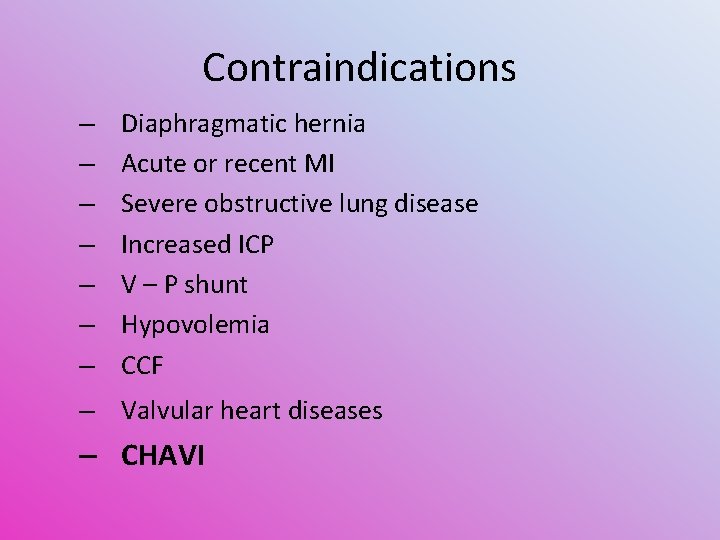
Contraindications – – – – Diaphragmatic hernia Acute or recent MI Severe obstructive lung disease Increased ICP V – P shunt Hypovolemia CCF – Valvular heart diseases – CHAVI
Three specific problems • Positioning • Pneumoperitoneum • CO 2 insufflation
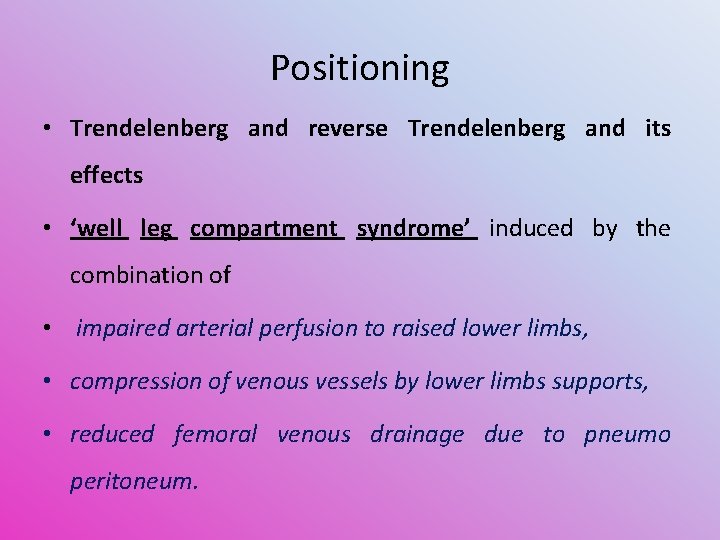
Positioning • Trendelenberg and reverse Trendelenberg and its effects • ‘well leg compartment syndrome’ induced by the combination of • impaired arterial perfusion to raised lower limbs, • compression of venous vessels by lower limbs supports, • reduced femoral venous drainage due to pneumo peritoneum.
Risk factors • Risk factors include surgery > 4 h duration, muscular lower limbs, obesity, peripheral vascular disease, hypotension, and steep Trendelenburg positioning Get up after two hours and go back again
pneumoperitoneum • CO 2 insufflation --- intra-abdominal pressure (IAP) climbs. • Normal IAP = 0 – 5 mm. Hg • Upto 10 – ok • More than 15 – problems start • Individual systems affected
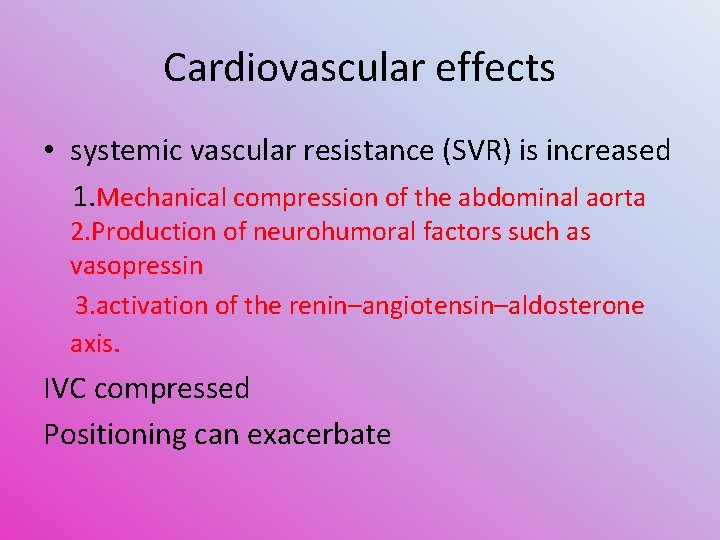
Cardiovascular effects • systemic vascular resistance (SVR) is increased 1. Mechanical compression of the abdominal aorta 2. Production of neurohumoral factors such as vasopressin 3. activation of the renin–angiotensin–aldosterone axis. IVC compressed Positioning can exacerbate

Steps to decrease CVS effects • Healthy patients appear to tolerate these hemodynamic effects well • What will decrease? ? • the lowest insufflation pressure • vasodilating agents, centrally acting alpha-2 agonists. • appropriate intravenous fluid loading
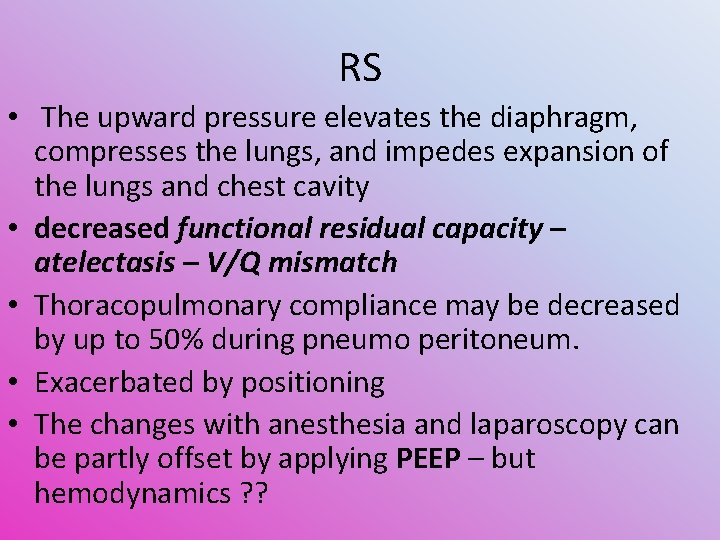
RS • The upward pressure elevates the diaphragm, compresses the lungs, and impedes expansion of the lungs and chest cavity • decreased functional residual capacity – atelectasis – V/Q mismatch • Thoracopulmonary compliance may be decreased by up to 50% during pneumo peritoneum. • Exacerbated by positioning • The changes with anesthesia and laparoscopy can be partly offset by applying PEEP – but hemodynamics ? ?

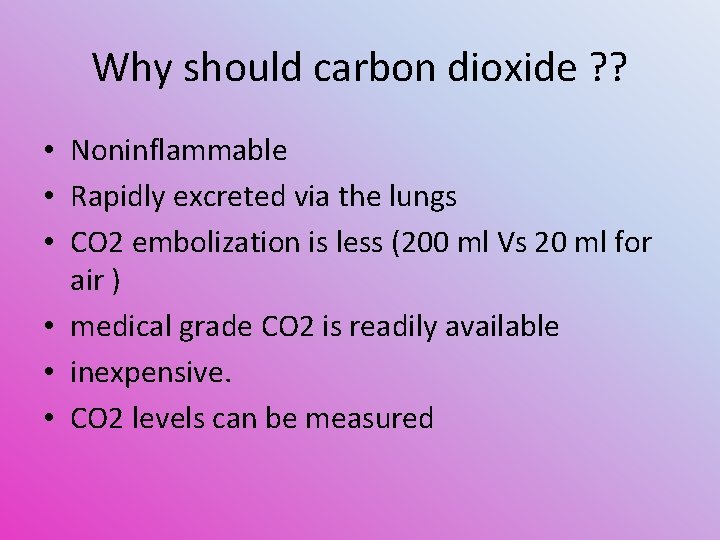
Why should carbon dioxide ? ? • Noninflammable • Rapidly excreted via the lungs • CO 2 embolization is less (200 ml Vs 20 ml for air ) • medical grade CO 2 is readily available • inexpensive. • CO 2 levels can be measured
But CO 2 is not inert • It gets converted to carbonic acid in moist peritoneum – local pain • it can remain in gaseous form intra peritoneal after laparoscopy, causing referred shoulder pain. • Blood - Hypercarbia -- hypertension, tachycardia, cerebral vasodilation, and respiratory acidosis. Insufflations flow rate should be low, initially 1 -1. 5 Ltr/min of CO 2
Back to increased IAP
Splanchnic effects • Blood flow to the kidney and liver is significantly compromised with increasing IAP • 20 mm Hg ---- 25 % GFR decrease
Neurological effects • An elevated IAP causes an increase in intracerebral pressure (ICP) by limiting cerebral venous drainage as a consequence of raised intra-thoracic pressure CPP ? ? On cardiac output POCD !!
Be awake like her
Preanaesthetic preparation • Consent and readiness for laparotomy • The cardiac and pulmonary status of all patients should be carefully assessed • Premedication is usually not necessary except in anxious patients. • Atropine can be used for premedication to prevent vagally mediated brady arrhythmias • PONV prophylaxis • PONV
Monitoring • • Pulse rate Continuous ECG Intermittent NIBP Pulse oximetry (Sp. O 2) Capnography (Et. CO 2) Temperature Intra abdominal pressure Pulmonary airway pressure • Others --- be vigilant like
Controlled GA with ETT – WHY ? ? • Less gastric acid aspiration, • allows optimal control of CO 2 • facilitates surgical access -------------------- • No mask ventilation • Ryles tube – gastric distension for view, prevention of gastric injuries
• zone 4 opened , zone 3 increased, zone 2 becomes three in increased IAP. • The application of PEEP prior to Pneumo peritoneum is supposed to stop the lung changes • All so called changes due to PEEP will be acceptable if we have adequate intravascular status
laryngeal mask airway (LMA) • controversial due to the increased risk of aspiration • difficulties encountered when trying to maintain effective gas transfer while delivering the higher airway pressures • Still a lot of RCT s prove the use of proseal LMAs in lap surgeries
nitrous oxide • • The use of nitrous oxide- controversial produce bowel distension during surgery increase in PONV Halothane increases the incidence of arrhythmia during laparoscopic surgery, especially in the presence of hypercarbia
Remifentanyl – PCV • Extremely painful - insufflation • But surgery is short hence remifentanyl is ideal. • Pressure controlled modalities affords higher instantaneous flow peaks, • minimizing peak pressures, • improved alveolar recruitment and oxygenation in laparoscopic surgery for obese patients
Combined spinal epidural anesthesia for laparoscopic appendectomy in adults: A case series management of pneumo peritoneum, achieving adequate level of analgesia Problem of shoulder tip pain, provision of postoperative pain relief prevent deterioration of respiratory mechanics, • ambulation as early as possible. • Possible with GA ? ? • • •

CSEA
Spinal • Spinal anaesthesia with Hyperbaric Bupivacaine and Fentanyl is adequate and safe for elective laparoscopic appendectomy in healthy patients but careful evaluation of the method is needed particularly in cardio respiratory conditions. • Saudi Journal of Anaesthesia Vol. 6, Issue 1, January. March 2012
M Ravishankar et al • In a conscious patient undergoing laparoscopy with pneumoperitoneum, under spinal anaesthesia, the preserved inspiratory diaphragmatic activity maintains ventilation and, the gas exchange within physiological limits. Hence it is a safe alternative to general anaesthesia. Who said this ? ? • J Anaesthesiol Clin Pharmacol. 2010 Oct-Dec; 26(4): 475– 479. • Respiratory Changes During Spinal Anaesthesia for Gynaecological Laparoscopic Surgery

Yes we can do it !!
Single shot epidural + GA
Previous slide and concepts 1 Mechanical compression of the abdominal aorta 2. Production of neurohumoral factors such as vasopressin 3. activation of the renin–angiotensin– aldosterone axis. Using epidural and cutting off all symp. Afferents will correct all the above instead of using separate hypotensives
• Ephedrine ok • Phenylephrine ? ?
Complications • CO 2 emphysema • Capnothorax • CO 2 embolism • Trochar may cause abdominal vessel injury, GIT perforation, hepatic and splenic tear and omental injury. • Extraperitoneal insufflation of CO 2 • Pneumothorax pneumomediastinum and pneumopericardium • IPEEP
Treatment • • Most of these cases – 100 % oxygen. , Cut off nitrous IVF and supportive measures
Other complications
Endobronchial intubation • Cephalad displacement of the diaphragm during pneumoperitoneum result in cephalad movement of carina leading to endobronchial intubation
GAS EMBOLISM • Direct insufflation of gas into a vessel by misplaced trochar or veress needle. • Small bubble of gas carried through injured vein at operative site • Large gas absorption into portal circulation may be caused by very fast rate of gas flow and very high intra abdominal pressure
CARDIAC ARYHTHMIAS • Patient undergoing laparoscopy are prone to develop cardiac arrythmias due to high PCO 2 and raised vagal tone. • Other complications • Darkness in the OR • Regurgitation • DARE – IPEEP

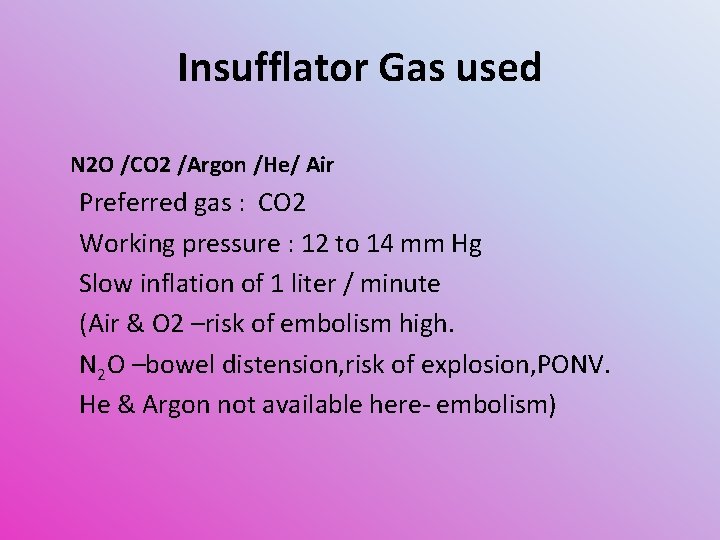
Insufflator Gas used N 2 O /CO 2 /Argon /He/ Air Preferred gas : CO 2 Working pressure : 12 to 14 mm Hg Slow inflation of 1 liter / minute (Air & O 2 –risk of embolism high. N 2 O –bowel distension, risk of explosion, PONV. He & Argon not available here- embolism)
Post op management • O 2 administration for couple of hours to prevent alveolar hypoxia as CO 2 excretion continues • Energetic care for prevention of sickness must be taken as PONV can jeopardize all the benefits of laparoscopy and anesthesiologist gets total blame. • Proper warming of patient. • Attention must be paid for pain relief.
Post op pain – same on day 1 • instillation of bupivacaine into the peritoneum • interpleural injection of bupivacaine. • Rigorous surgical washout at the end of the procedure. • Nonsteroidal anti-inflammatory drugs • When used in combination with a regular paracetamol, there is a considerable reduction in the requirement for opioid analgesia
Post op pain • • • Local infiltration of the incision Expel as gas as possible TAP block Epidural Pre op dexa – pain and PONV

Summary • • Definition, advantages , disadvantages, CI Surgeries Three musketeers Premed Technique – monitoring Complications Postop
• Thank you all
 Ramya parthasarathy
Ramya parthasarathy Ramya parthasarathy
Ramya parthasarathy Maya parthasarathy
Maya parthasarathy Addressing concerns and earning commitment
Addressing concerns and earning commitment Macbeth questions and answers
Macbeth questions and answers Escalating concerns in nursing
Escalating concerns in nursing Thematic concerns
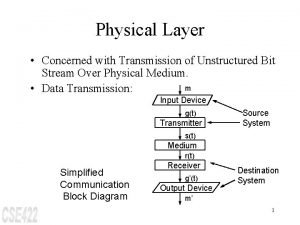
Thematic concerns The physical layer concerns with
The physical layer concerns with Southwest airlines ethics and social responsibility
Southwest airlines ethics and social responsibility Cross-cutting concerns
Cross-cutting concerns Gmc confidentiality
Gmc confidentiality When a choice concerns matters of personal value or taste
When a choice concerns matters of personal value or taste Ddd cross cutting concerns
Ddd cross cutting concerns Gianna emanuela molla
Gianna emanuela molla What happened in 1777
What happened in 1777 Macmillan concerns checklist
Macmillan concerns checklist It concerns many sociologists
It concerns many sociologists How does banquo describe the witches
How does banquo describe the witches Identify concerns
Identify concerns Earning commitment
Earning commitment Software design separation of concerns
Software design separation of concerns Comfort food psychology
Comfort food psychology Joys and concerns images
Joys and concerns images Layouts that can handle varied processing requirements
Layouts that can handle varied processing requirements Lumi sps
Lumi sps Design concerns
Design concerns Health concerns
Health concerns Boreal forest features
Boreal forest features Joys and concerns
Joys and concerns Social process theories criminology
Social process theories criminology The network layer is concerned with of data.
The network layer is concerned with of data. Macbeth discussion questions
Macbeth discussion questions Vocopher
Vocopher Piping and instrumentation diagrams
Piping and instrumentation diagrams Cbam model
Cbam model Dwrfism
Dwrfism Health concerns
Health concerns Joys and concerns prayer
Joys and concerns prayer The main issue in designing process layouts concerns what
The main issue in designing process layouts concerns what