LAPAROSCOPY IN INFERTILITY DR E SH TEHRANI NEJAD

- Slides: 67
LAPAROSCOPY IN INFERTILITY DR. E. SH. TEHRANI NEJAD ASSOCIATE PROFESSOR OF TEHRAN UNIVERSITY OF MEDICAL SCIENCES
The availability of ART has reduced the need for reproductive surgery as a primary surgical treatment of infertility. When fertility surgery is indicated, laparoscopy is the tool of choice. 2
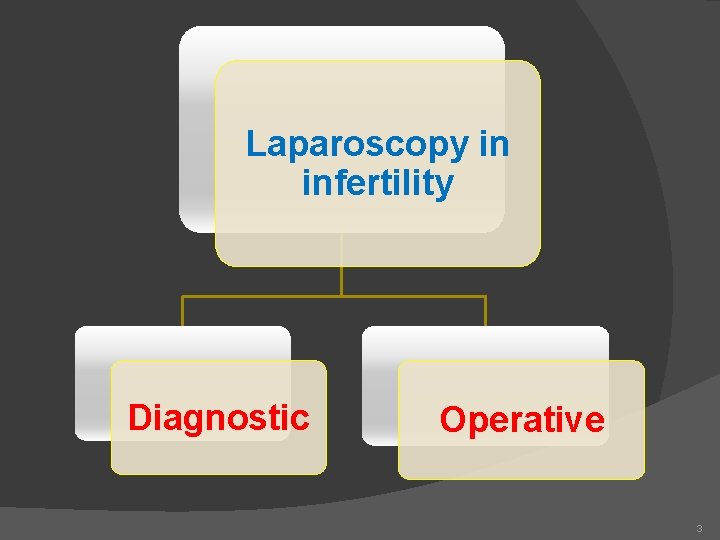
Laparoscopy in infertility Diagnostic Operative 3
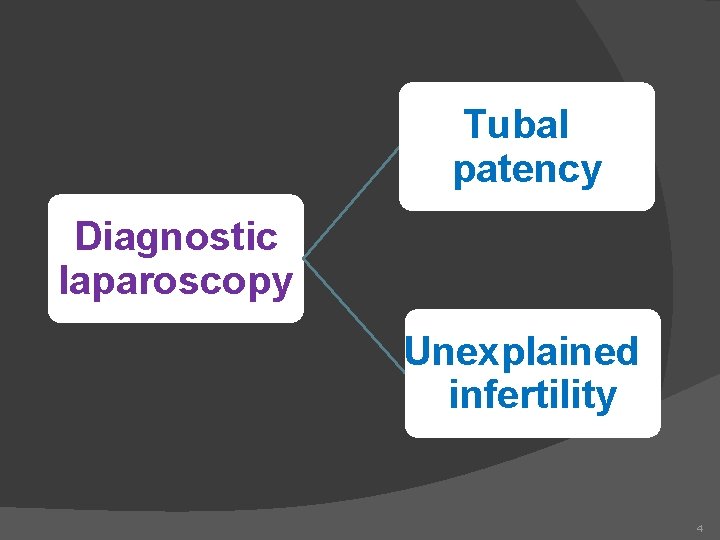
Tubal patency Diagnostic laparoscopy Unexplained infertility 4
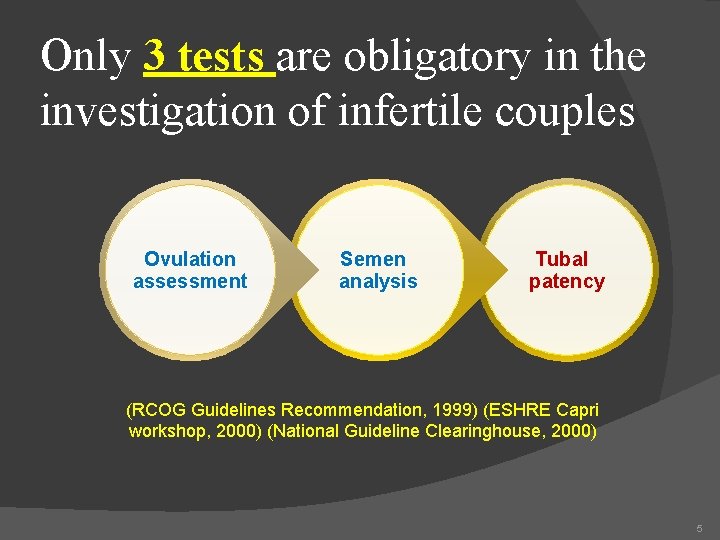
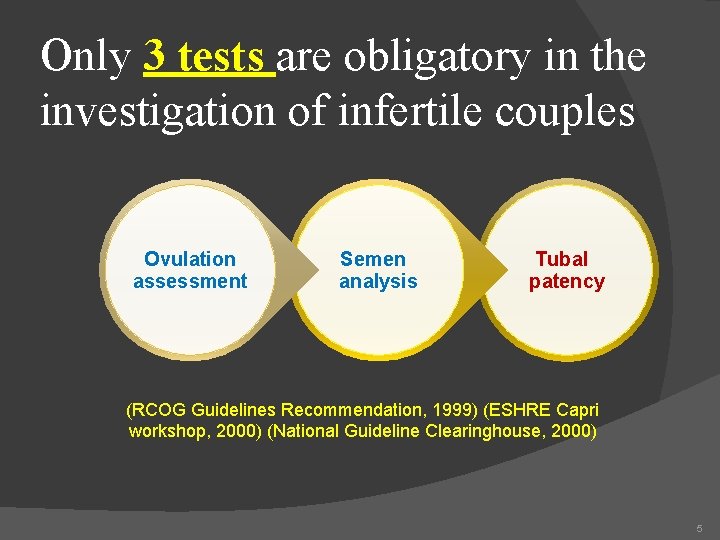
Only 3 tests are obligatory in the investigation of infertile couples Ovulation assessment Semen analysis Tubal patency (RCOG Guidelines Recommendation, 1999) (ESHRE Capri workshop, 2000) (National Guideline Clearinghouse, 2000) 5
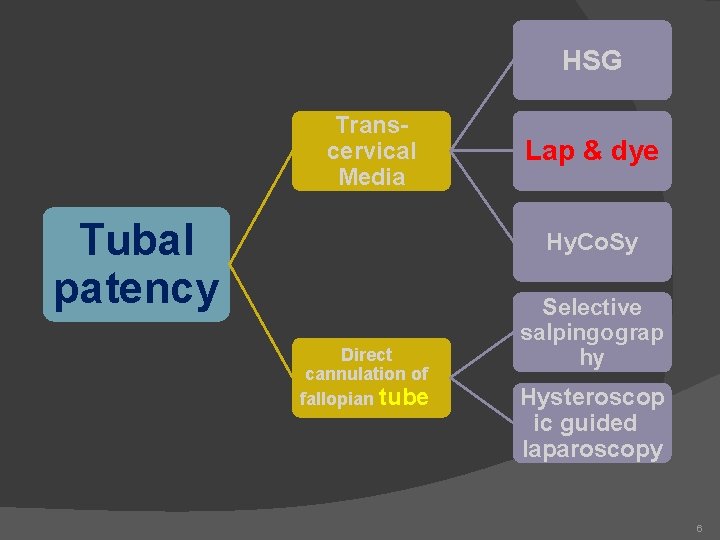
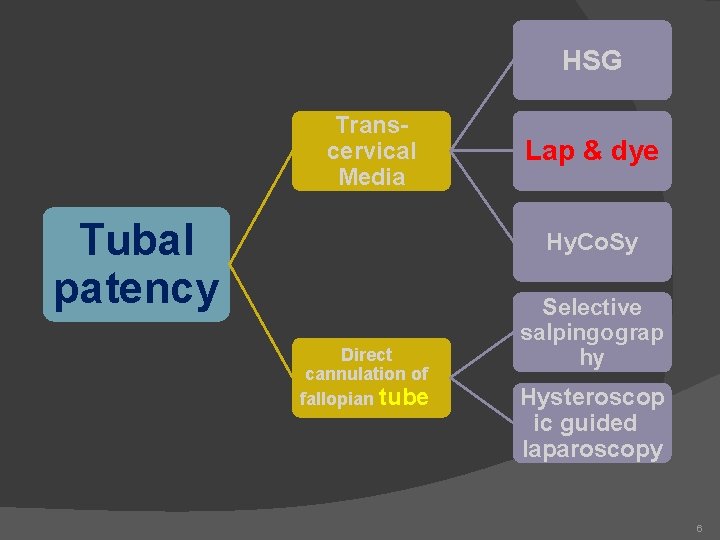
HSG Transcervical Media Tubal patency Lap & dye Hy. Co. Sy Direct cannulation of fallopian tube Selective salpingograp hy Hysteroscop ic guided laparoscopy 6
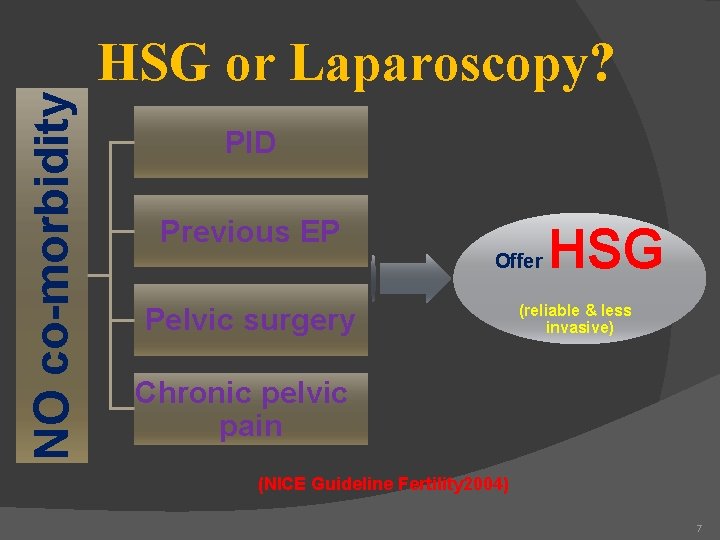
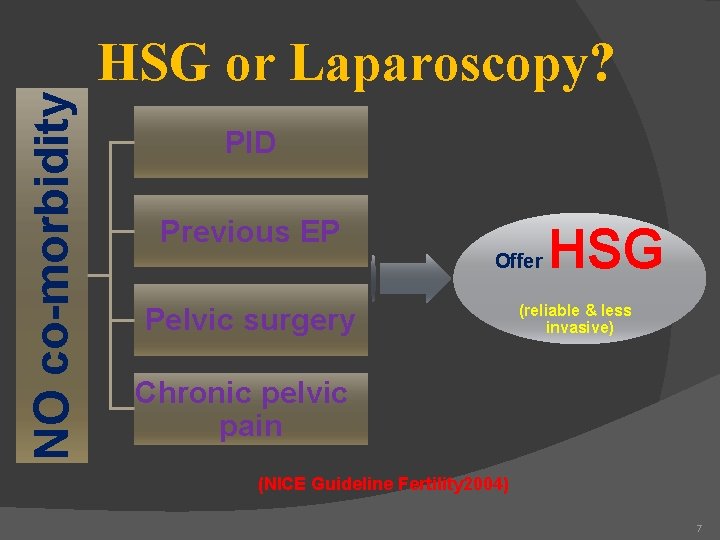
NO co-morbidity HSG or Laparoscopy? PID Previous EP Offer Pelvic surgery HSG (reliable & less invasive) Chronic pelvic pain (NICE Guideline Fertility 2004) 7
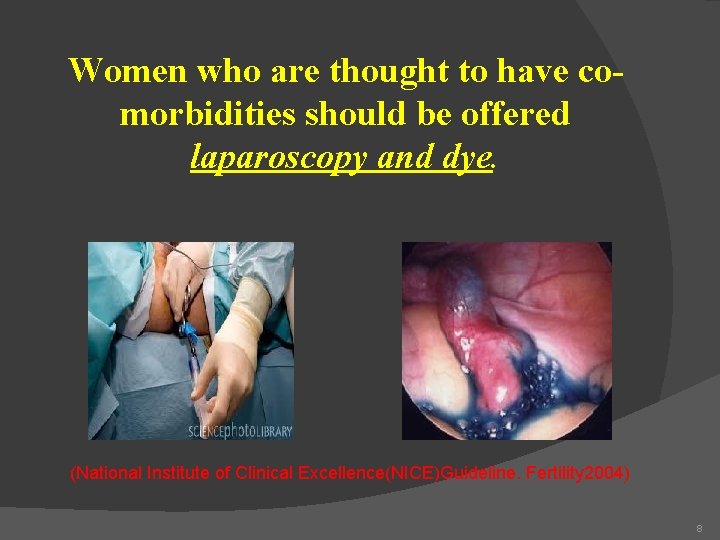
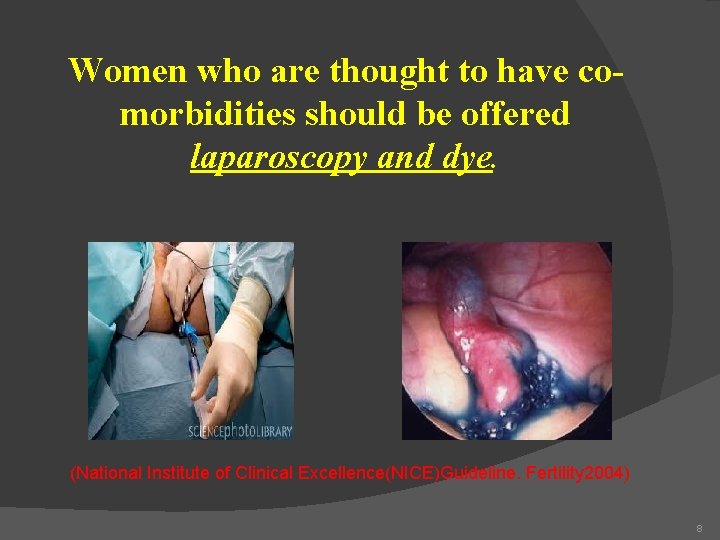
Women who are thought to have comorbidities should be offered laparoscopy and dye. (National Institute of Clinical Excellence(NICE)Guideline. Fertility 2004) 8
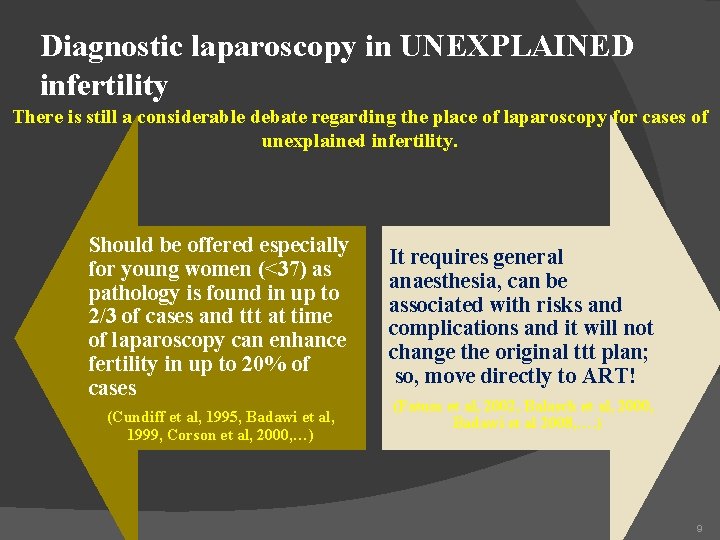
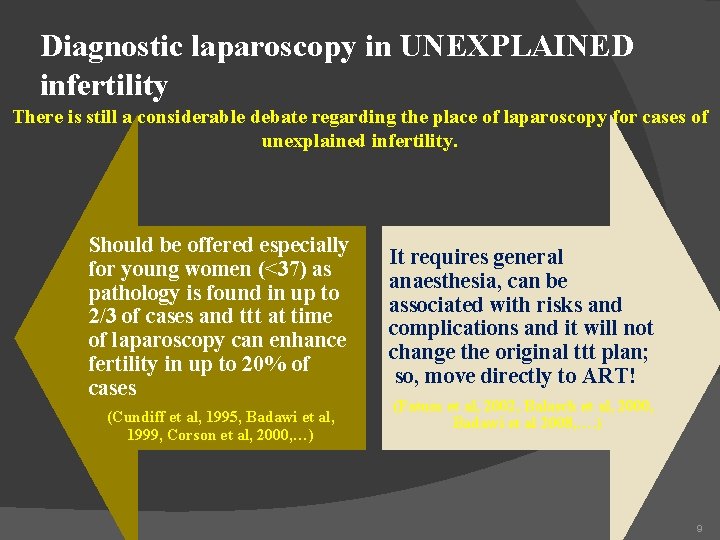
Diagnostic laparoscopy in UNEXPLAINED infertility There is still a considerable debate regarding the place of laparoscopy for cases of unexplained infertility. Should be offered especially for young women (<37) as pathology is found in up to 2/3 of cases and ttt at time of laparoscopy can enhance fertility in up to 20% of cases (Cundiff et al, 1995, Badawi et al, 1999, Corson et al, 2000, …) It requires general anaesthesia, can be associated with risks and complications and it will not change the original ttt plan; so, move directly to ART! (Fatum et al, 2002, Balasch et al, 2000, Badawi et al 2008, …. ) 9
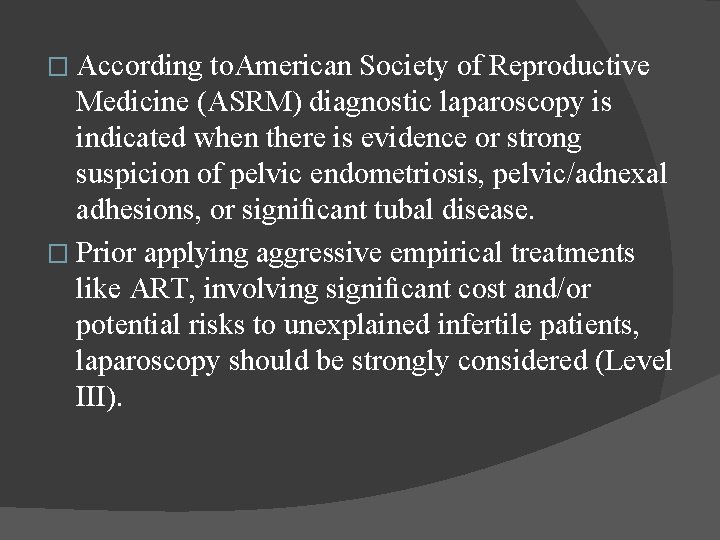
� According to. American Society of Reproductive Medicine (ASRM) diagnostic laparoscopy is indicated when there is evidence or strong suspicion of pelvic endometriosis, pelvic/adnexal adhesions, or significant tubal disease. � Prior applying aggressive empirical treatments like ART, involving significant cost and/or potential risks to unexplained infertile patients, laparoscopy should be strongly considered (Level III).
However, the presence and absence of risk factors related to infertility does not always indicate a patient’s need for diagnostic laparoscopy; � it should be strongly considered by the clinicians when they encounter with an abnormal HSG result, a past history of pelvic infection, pelvic surgery and/or unexplained secondary infertility during management of an unexplained infertile couple. � A laparoscopist should also be capable of performing operative procedures like adhesiolysis and endometriosis surgery during diagnostic laparoscopy especially for secondary unexplained infertile patients. � 11
� Omitting diagnostic laparoscopy after a normal HSG in infertile patients with UI and without risk factors for pelvic pathologies related to infertility is reasonable because the majority became pregnant after several cycles of ovulation induction, and/or ART treatment while diagnostic laparoscopy is indicated when pelvic endometriosis and/ or tubal pathology is strongly suspected. Based on the current literature, when HSG is normal, one cannot recommend laparoscopy as the first line diagnostic tool for infertility work-up due to lack of cost-effectiveness, so diagnostic laparoscopy could be postponed until several ovarian stimulation and intrauterine insemination attempts had been found to be unsuccessful in achieving pregnancy. �
Unfortunately, there a few randomised controlled studies to investigate the value of diagnostic laparoscopy in unexplained infertile couples and the heterogeneity of published articles regarding pregnancy outcomes based on different follow- up durations of the patients. � Diagnostic laparoscopy should be considered when there abnormal HSG results, a past history of pelvic infection, pelvic surgery and/or unexplained secondary infertility during management of an �
for female infertility 14
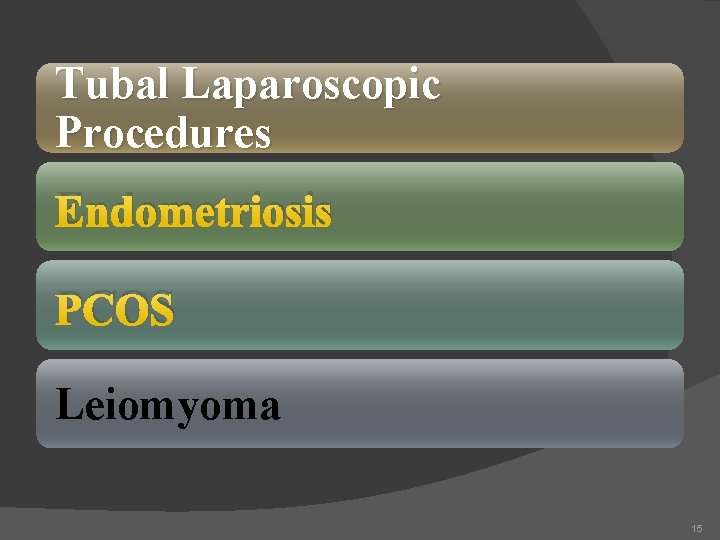
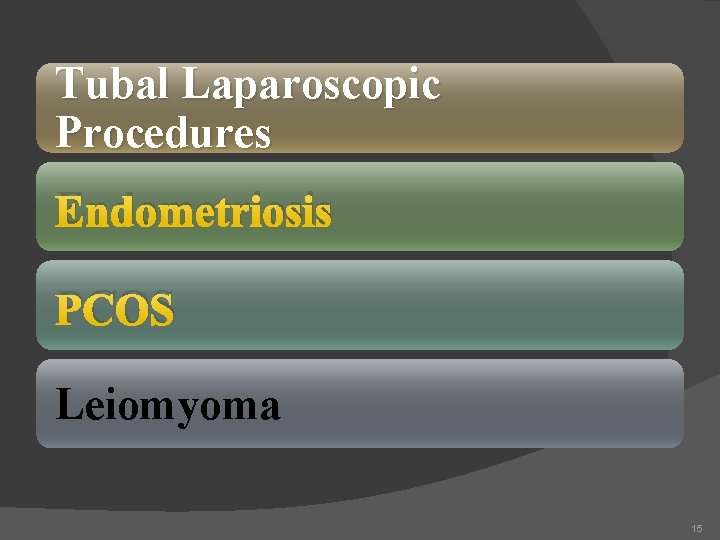
Tubal Laparoscopic Procedures Endometriosis PCOS Leiomyoma 15
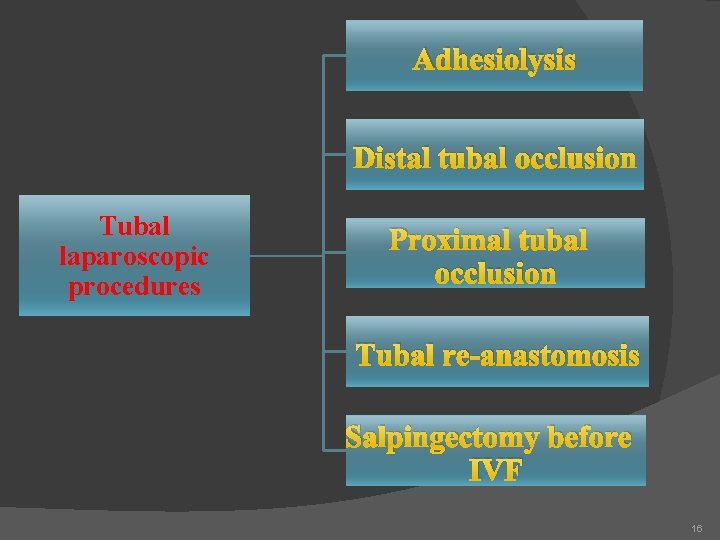
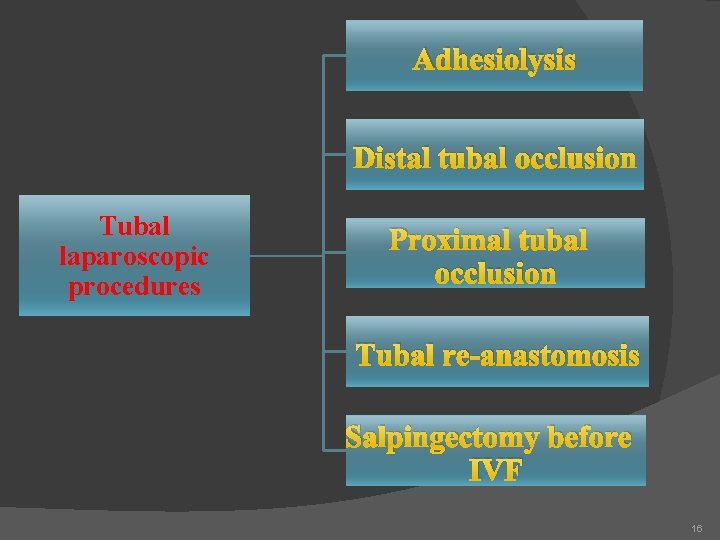
Adhesiolysis Distal tubal occlusion Tubal laparoscopic procedures Proximal tubal occlusion Tubal re-anastomosis Salpingectomy before IVF 16
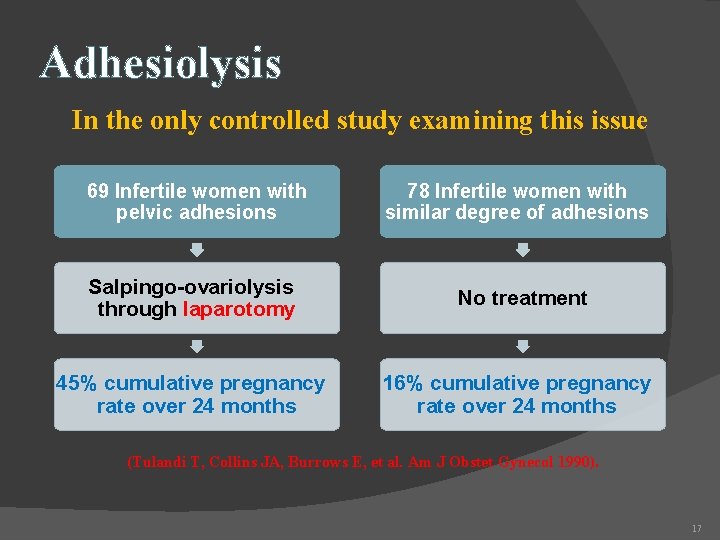
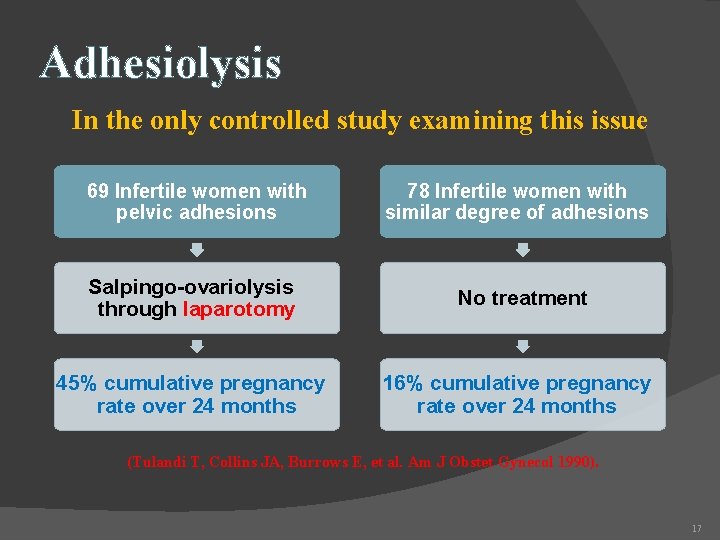
Adhesiolysis In the only controlled study examining this issue 69 Infertile women with pelvic adhesions 78 Infertile women with similar degree of adhesions Salpingo-ovariolysis through laparotomy No treatment 45% cumulative pregnancy rate over 24 months 16% cumulative pregnancy rate over 24 months (Tulandi T, Collins JA, Burrows E, et al. Am J Obstet Gynecol 1990). 17
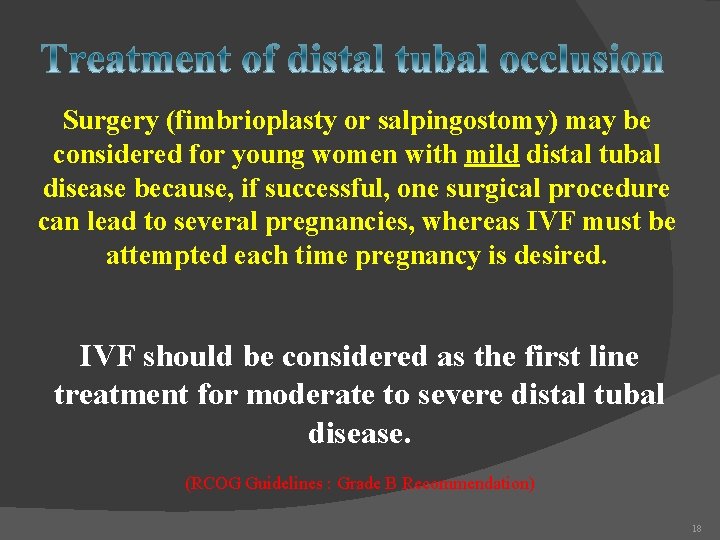
Surgery (fimbrioplasty or salpingostomy) may be considered for young women with mild distal tubal disease because, if successful, one surgical procedure can lead to several pregnancies, whereas IVF must be attempted each time pregnancy is desired. IVF should be considered as the first line treatment for moderate to severe distal tubal disease. (RCOG Guidelines : Grade B Recommendation) 18
Proximal tubal occlusion (Cornual Obstruction) The incidence of true cornual occlusion is low and surgical treatment (resection and anastomosis) is not highly successful 19
Tubal re-anastomosis Indications include: • Reversal of sterilization • Mid-tubal block • Previous ectopic Sterilization reversal can be considered in young women (<37) with more than 4 cm of residual tube and prior ring or clip sterilization. In other women, IVF may be a better option. (Boeckxstaens A, Devroey P, Collins J, Tournaye H. Getting pregnant after tubal sterilization: surgical reversal or IVF? Hum Reprod 2007; 22: 2660). 20
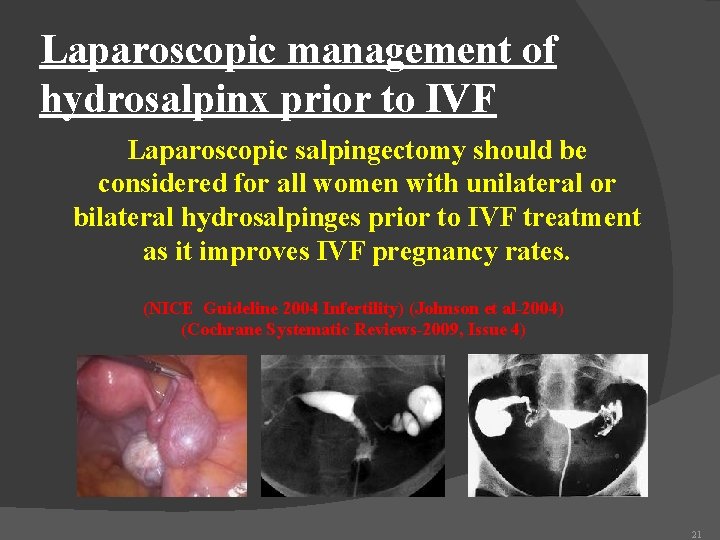
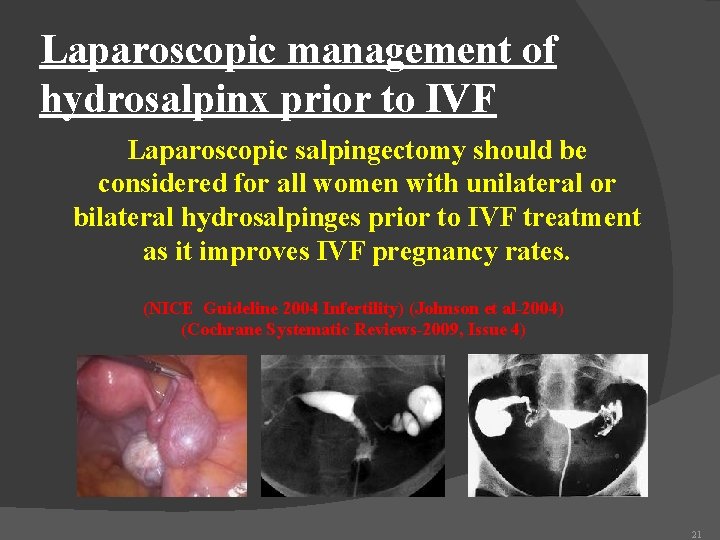
Laparoscopic management of hydrosalpinx prior to IVF Laparoscopic salpingectomy should be considered for all women with unilateral or bilateral hydrosalpinges prior to IVF treatment as it improves IVF pregnancy rates. (NICE Guideline 2004 Infertility) (Johnson et al-2004) (Cochrane Systematic Reviews-2009, Issue 4) 21
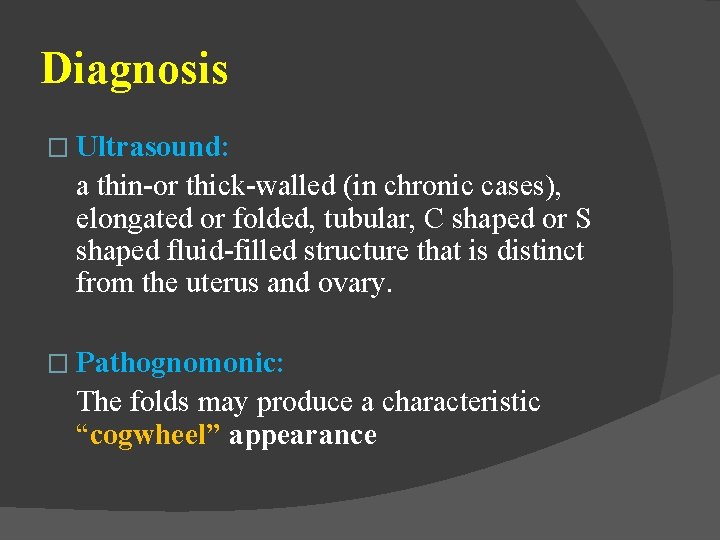
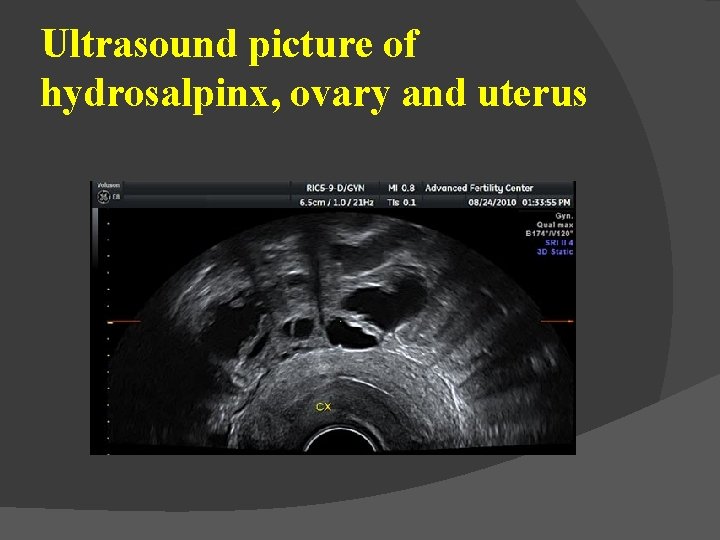
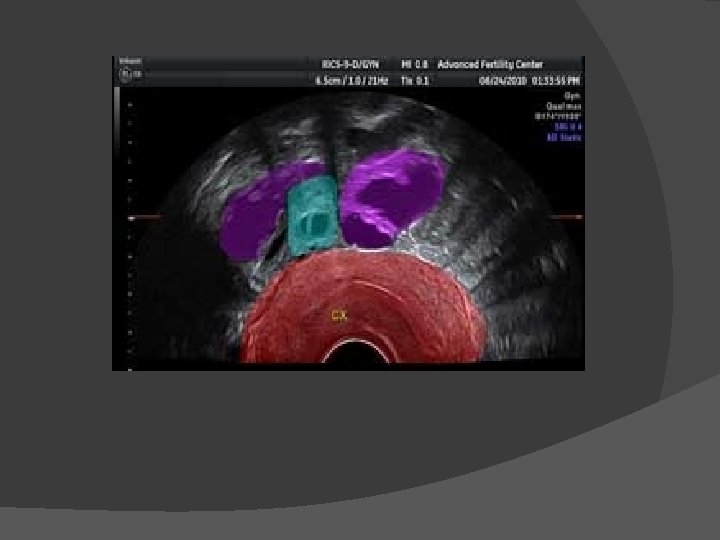
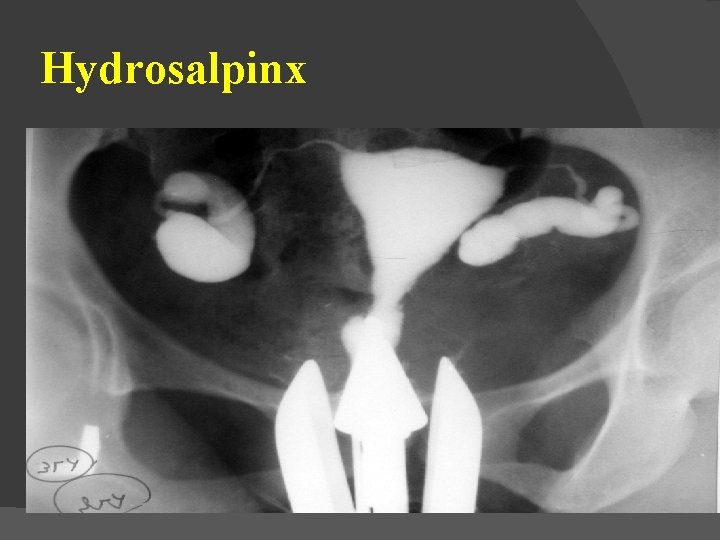
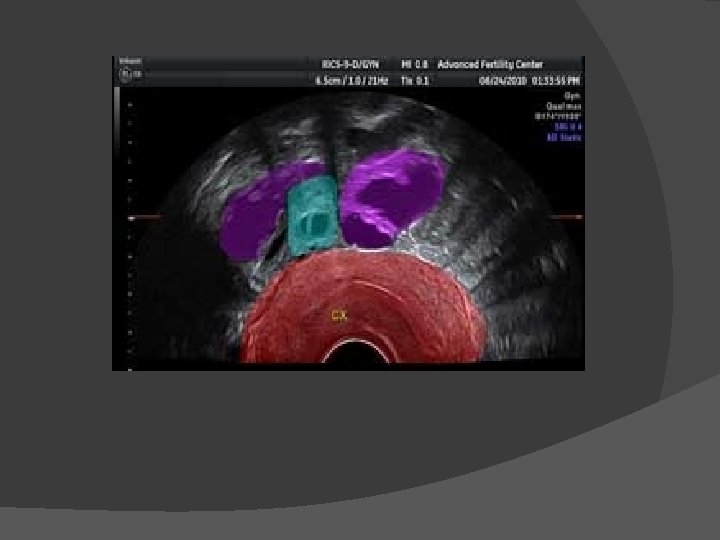
Diagnosis � Ultrasound: a thin-or thick-walled (in chronic cases), elongated or folded, tubular, C shaped or S shaped fluid-filled structure that is distinct from the uterus and ovary. � Pathognomonic: The folds may produce a characteristic “cogwheel” appearance
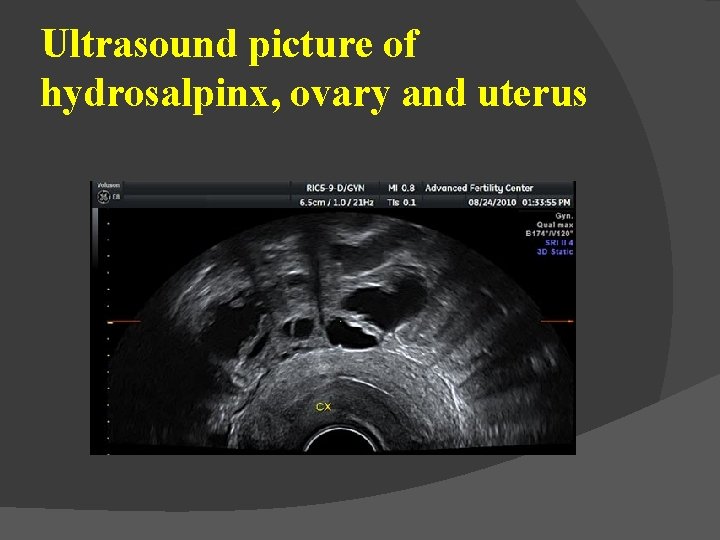
Ultrasound picture of hydrosalpinx, ovary and uterus
Diagnosis � CT � HSG � MRI � Laparoscopy
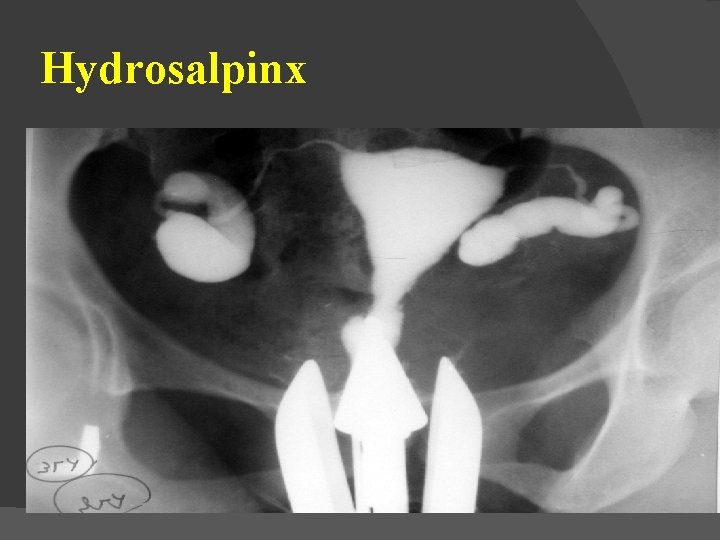
Hydrosalpinx
� In the beginning : (IVF) tubal factor infertility was the sole indication for the treatment. � NOW tubal disease : as little as 20%. � tubal factor : yield worse results than other causes of infertility. � tubal factor infertility : independently negative predictive factor of pregnancy and birth, as compared with all other indications
Pregnancy rates were significantly lower (15%) in Visible compared with hydrosalpinges not visible (31 %). � presence of Bilateral to unilateral hydrosalpinx significantly lower pregnancy (12% vs. 24%) and implantation rates (5% vs. 11%). � � These findings suggest that the total amount of fluid in the hydrosalpinges is negatively correlated to the chance of achieving a pregnancy
MECHANISM OF HYDROSALPINX � Directly on the transferred embryos � on the endometrium and its receptivity for implantation, � Embryotoxic Properties
INTERVENTIONS AGAINST HYDROSALPINX Any surgical intervention interrupting the communication to the uterus would remove the leakage of the hydrosalpingeal fluid and restore pregnancy rates. � Salpingectomy � tubal ligation � transvaginal aspiration
Salpingectomy �A multicenter study in Scandinavia compared laparoscopic salpingectomy to no intervention prior to the first IVF cycle; Significant improvement in pregnancy and birth rates after salpingectomy in patients with hydrosalpinges that were large enough to be visible on ultrasound. � Clinical pregnancy rates were 46% versus 22% (p = 0. 049), and birth rates were 40% versus 17% (p = 0. 040)
�A systematic review in the Cochrane Library included meta-analyses demonstrating a significant improvement in ongoing pregnancy (OR 2. 2, 95% CI 1. 3 -3. 8) after IVF if salpingectomy was performed compared with no surgical intervention.
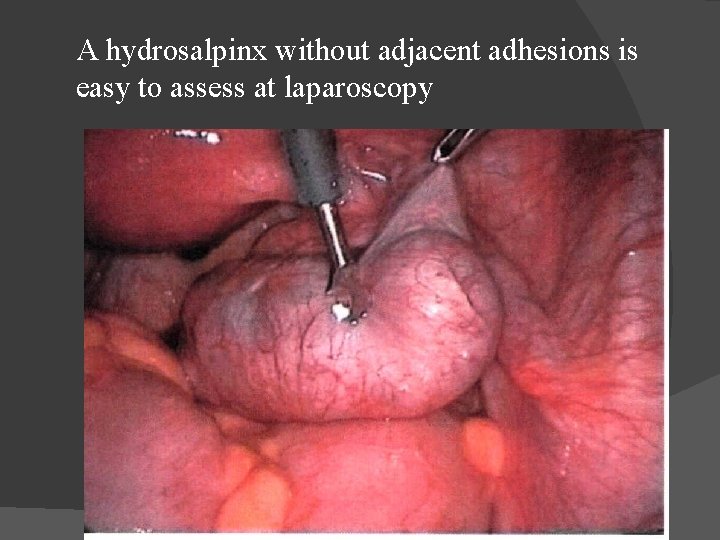
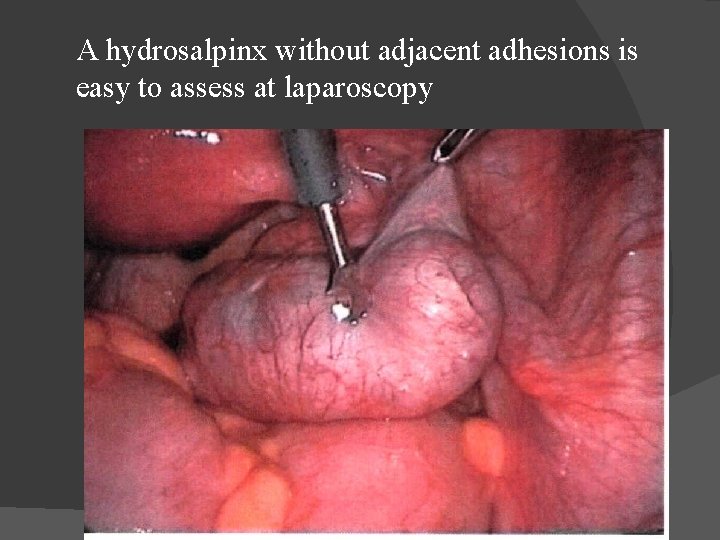
A hydrosalpinx without adjacent adhesions is easy to assess at laparoscopy
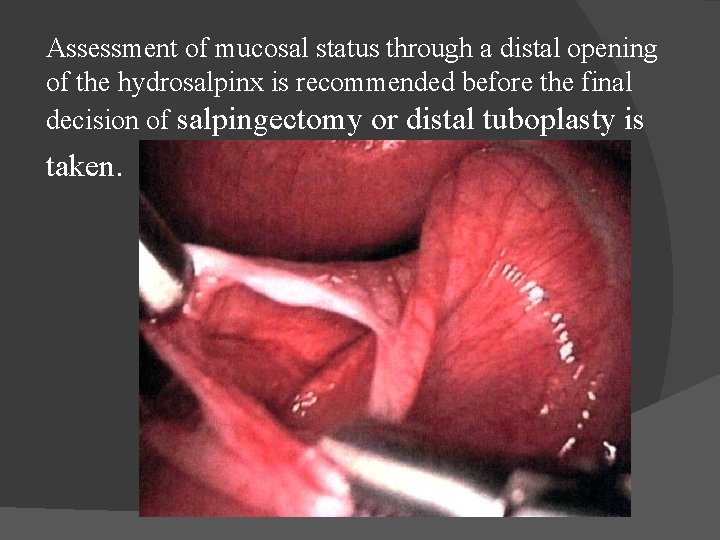
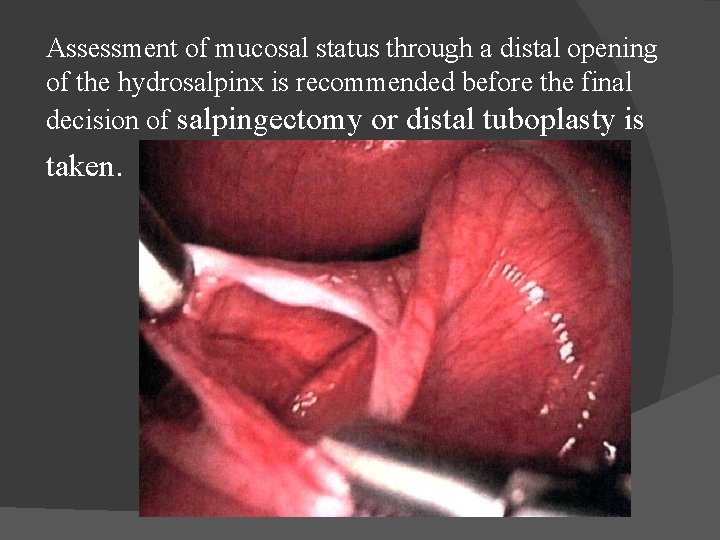
Assessment of mucosal status through a distal opening of the hydrosalpinx is recommended before the final decision of salpingectomy or distal tuboplasty is taken.
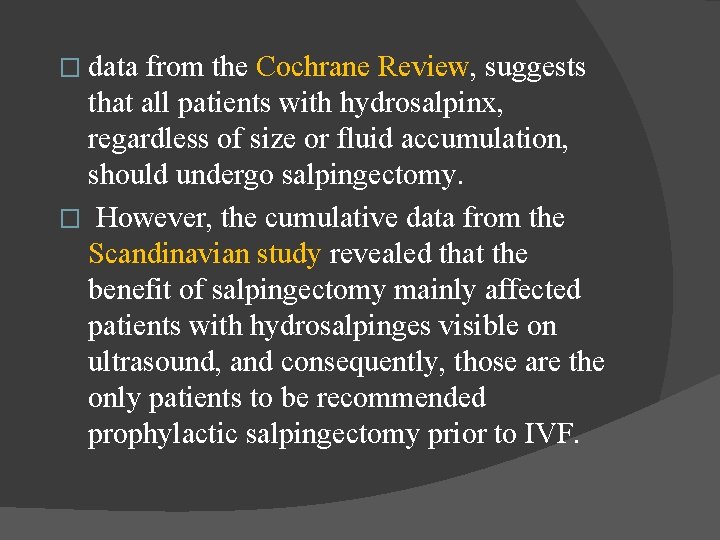
� data from the Cochrane Review, suggests that all patients with hydrosalpinx, regardless of size or fluid accumulation, should undergo salpingectomy. � However, the cumulative data from the Scandinavian study revealed that the benefit of salpingectomy mainly affected patients with hydrosalpinges visible on ultrasound, and consequently, those are the only patients to be recommended prophylactic salpingectomy prior to IVF.
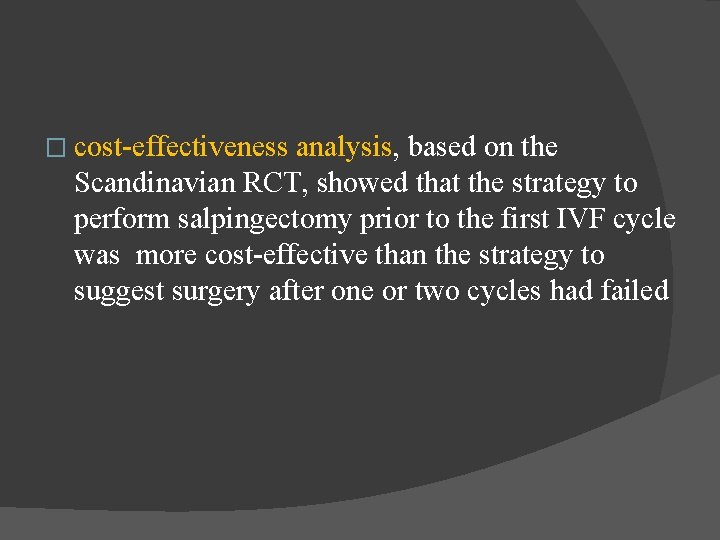
� cost-effectiveness analysis, based on the Scandinavian RCT, showed that the strategy to perform salpingectomy prior to the first IVF cycle was more cost-effective than the strategy to suggest surgery after one or two cycles had failed
Ovarian Function after Salpingectomy � None of them demonstrate an effect on the overall performance although one study has shown a decreased response in the ovary, ipsilateral to the salpingectomy
� In the Scandinavian RCT on salpingectomy prior to IVF, there was no difference in the number of retrieved oocytes � the effect of salpingectomy on the ovarian performance was examined by measuring the need for follicle-stimulating hormone (FSH) and the number of retrieved oocytes
� From the results, we cannot conclude that patients with a low ovarian reserve are at greater risk to suffer from poor response after salpingectomy. � However, theoretically, it seems important to be very careful not to damage the vascular and nervous supply when performing a salpingectomy.
� laparoscopic salpingectomy should be performed with cautious use of electrocautery, with no unnecessary excision of the mesosalpinx. � Resection very close to the actual tube to avoid damage to the medial tubal artery; it is preferable to leave a portion of an adherent tube on the ovary rather than to perform an excessively radical salpingectomy.
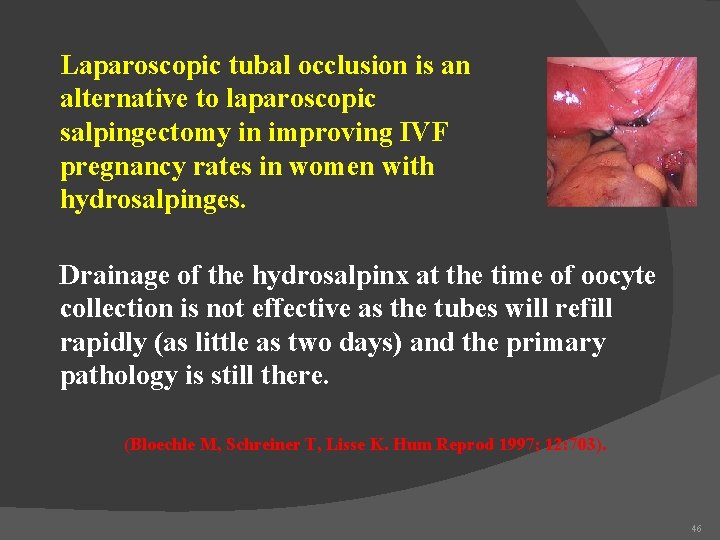
Tubal Occlusion by laparoscopy also includes proximal ligation and salpingostomy. � One randomized trial, in which 115 patients with hydrosalpinx were allocated to proximal tubal occlusion, salpingectomy, or no surgery prior to IVF. � Salpingectomy but not tubal ligation demonstrated significantly higher ongoing pregnancy rates (49% and 38%, respectively) compared to women having no surgery (7%), analysed on an intention-to-treat basis. �
� According to theory of the hydrosalpingeal fluid affecting the endometrium negatively , the procedure of tubal ligation is likely to be effective in improving pregnancy results. The procedure is currently recommended when pelvic adhesions are too extensive to perform a salpingectomy.
Tubal Occlusion by Hysteroscopy � when laparoscopy is contraindicated, like in cases with severe obesity or frozen pelvis. � The first case (Essureı) has been followed by a case series of 10 patients, reporting a live birth rate of 20% after one IVF cycle and/or frozen embryo transfer method can be performed in local anesthesia.
Salpingostomy � Salpingostomy is naturally the method of choice if the tube is suitable for reconstructive surgery. � The selection of patients suitable for surgical repair has to be based on the evaluation of the tubal mucosa through an endoscopic technique, and tubes with more than half of the mucosa in a good condition may have a fair chance of spontaneous conception
� These patients should be given sufficient time to await spontaneous conception, although the woman's age may hasten the need for IVF.
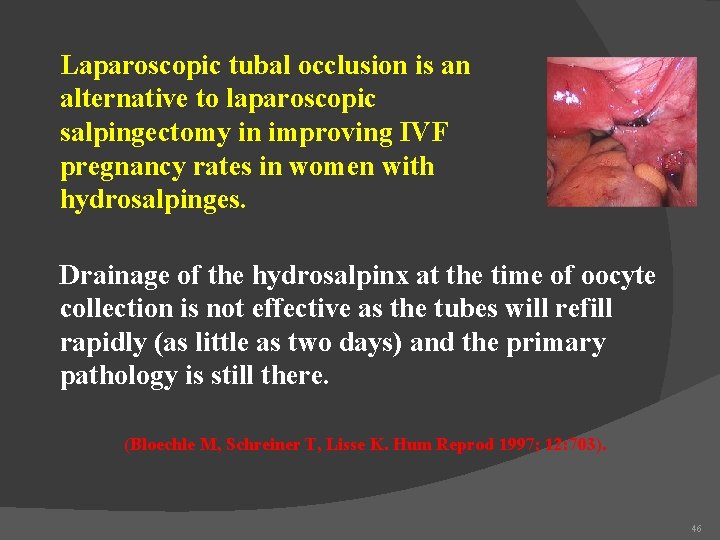
Laparoscopic tubal occlusion is an alternative to laparoscopic salpingectomy in improving IVF pregnancy rates in women with hydrosalpinges. Drainage of the hydrosalpinx at the time of oocyte collection is not effective as the tubes will refill rapidly (as little as two days) and the primary pathology is still there. (Bloechle M, Schreiner T, Lisse K. Hum Reprod 1997; 12: 703). 46
Transvaginal Aspiration � Whatever the exact mechanism of the negative influence of hydrosalpinx fluid, the treatment options concern the disposal of the fluid. � The simplest way, vaginal aspiration of fluid, has been evaluated in an RCT comparing transvaginal aspiration to no aspiration
� Unfortunately, the study was stopped in advance due to recruitment difficulties. The study was thus underpowered including 66 patients and the difference in clinical pregnancy rate (31% vs. 18%) did not reach statistical significance.
� transvaginal aspiration before ovarian stimulation was initiated and demonstrated that there was no improvement in pregnancy rates. � It can be concluded that transvaginal aspiration of hydrosalpingeal fluid at the time of oocyte collection is a treatment option, particularly if there is a contraindication or nonacceptance for surgery, or if a hydrosalpinx develops during ovarian stimulation.
Antibiotic Treatment � One retrospective study suggested that extended doxycycline treatment during an IVF cycle would minimize the detrimental effect of hydrosalpinx.
� Not allow for any recommendation of antibiotic treatment as an effective treatment. The method is, however, advantageously cheap and simple, but its benefit still needs to be evaluated in a prospective trial.
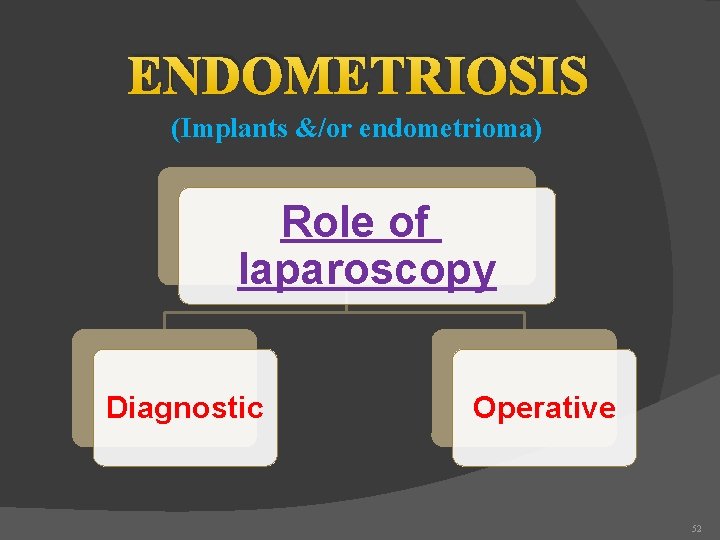
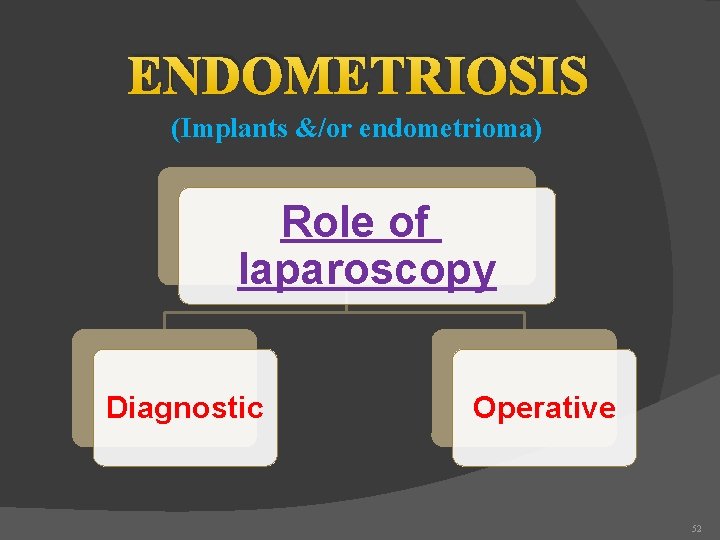
ENDOMETRIOSIS (Implants &/or endometrioma) Role of laparoscopy Diagnostic Operative 52
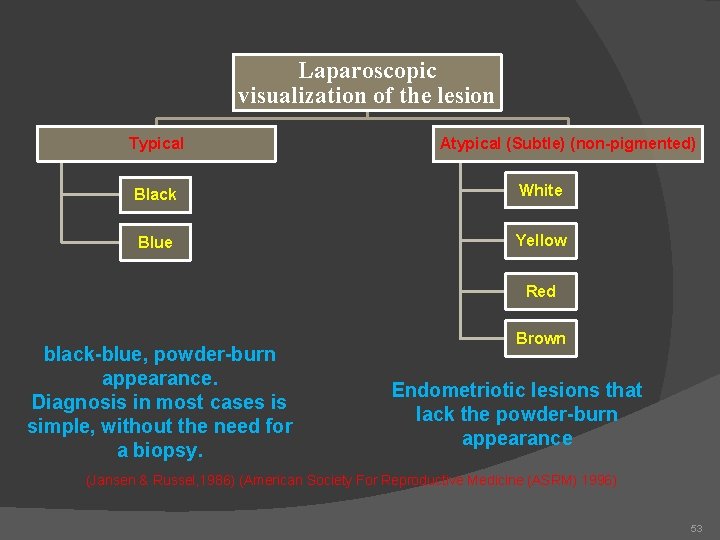
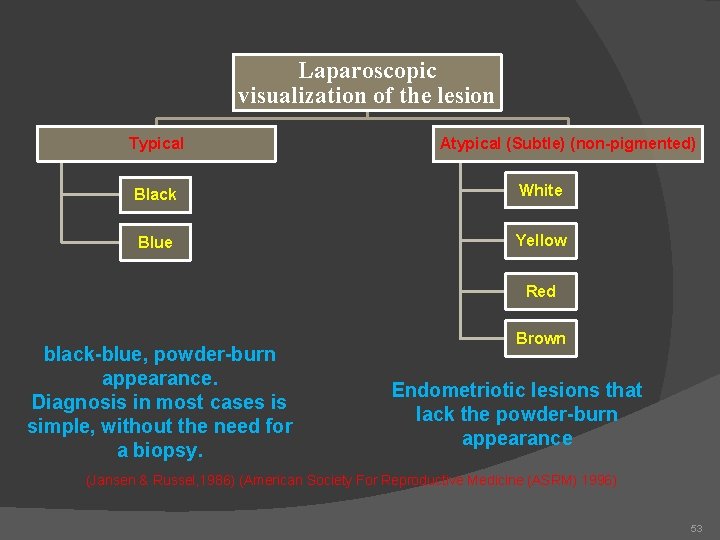
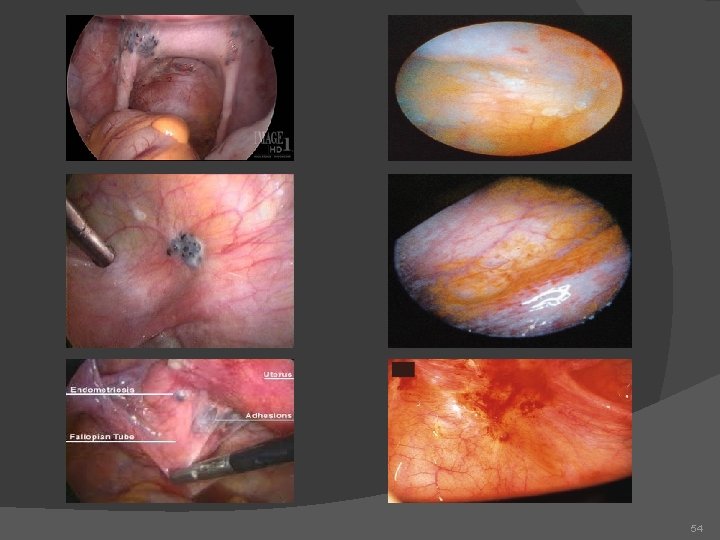
Laparoscopic visualization of the lesion Typical Atypical (Subtle) (non-pigmented) Black White Blue Yellow Red black-blue, powder-burn appearance. Diagnosis in most cases is simple, without the need for a biopsy. Brown Endometriotic lesions that lack the powder-burn appearance (Jansen & Russel, 1986) (American Society For Reproductive Medicine (ASRM) 1996) 53
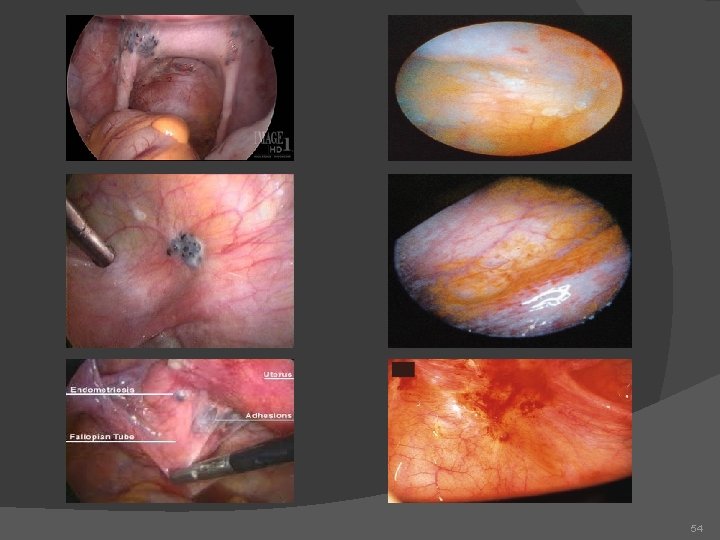
54
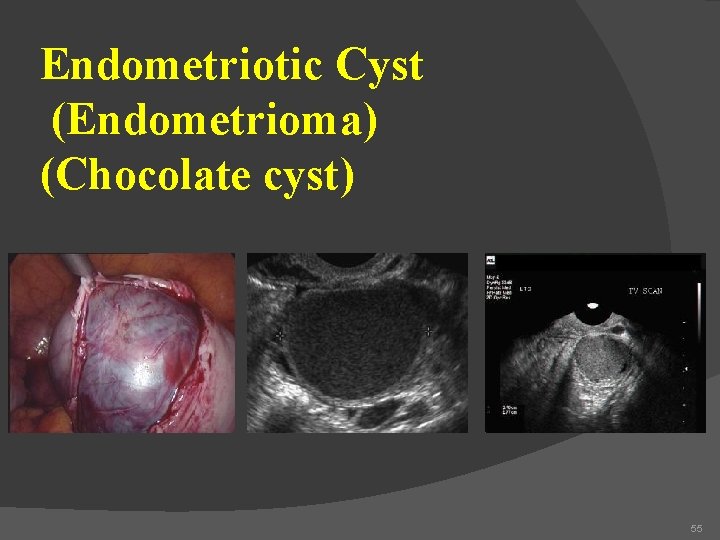
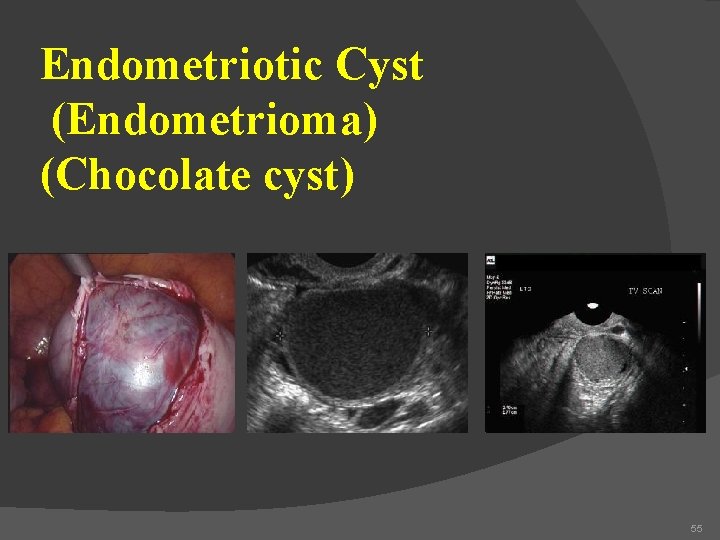
Endometriotic Cyst (Endometrioma) (Chocolate cyst) 55
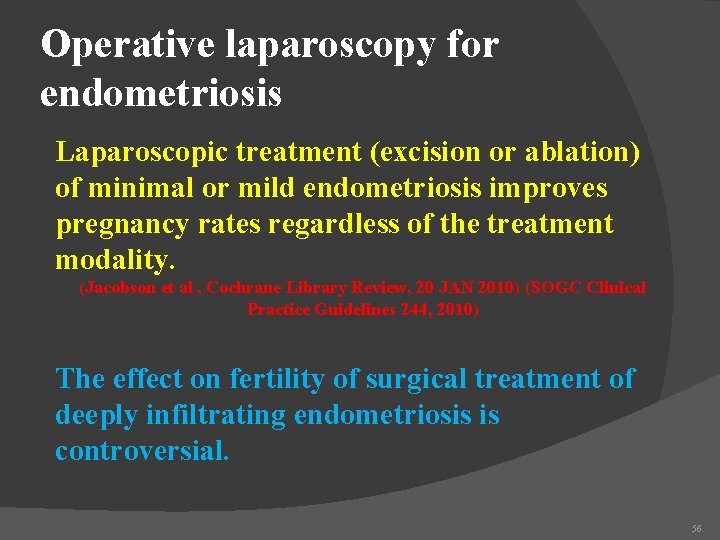
Operative laparoscopy for endometriosis Laparoscopic treatment (excision or ablation) of minimal or mild endometriosis improves pregnancy rates regardless of the treatment modality. (Jacobson et al , Cochrane Library Review, 20 JAN 2010) (SOGC Clinical Practice Guidelines 244, 2010) The effect on fertility of surgical treatment of deeply infiltrating endometriosis is controversial. 56
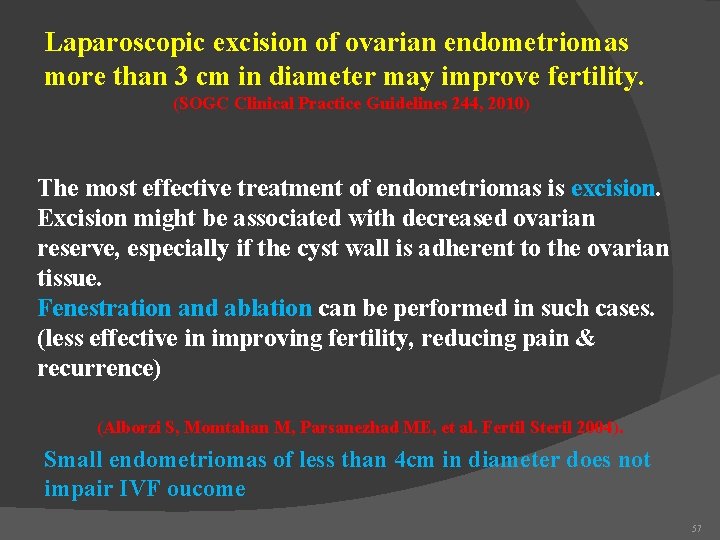
Laparoscopic excision of ovarian endometriomas more than 3 cm in diameter may improve fertility. (SOGC Clinical Practice Guidelines 244, 2010) The most effective treatment of endometriomas is excision. Excision might be associated with decreased ovarian reserve, especially if the cyst wall is adherent to the ovarian tissue. Fenestration and ablation can be performed in such cases. (less effective in improving fertility, reducing pain & recurrence) (Alborzi S, Momtahan M, Parsanezhad ME, et al. Fertil Steril 2004). Small endometriomas of less than 4 cm in diameter does not impair IVF oucome 57
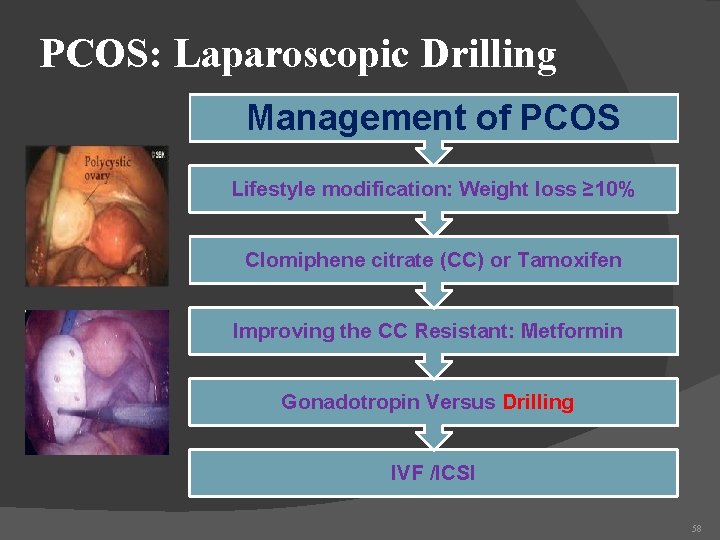
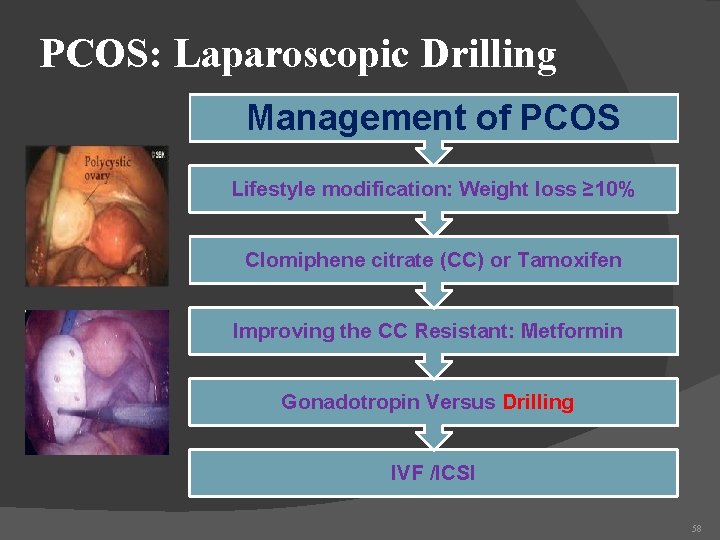
PCOS: Laparoscopic Drilling Management of PCOS Lifestyle modification: Weight loss ≥ 10% Clomiphene citrate (CC) or Tamoxifen Improving the CC Resistant: Metformin Gonadotropin Versus Drilling IVF /ICSI 58
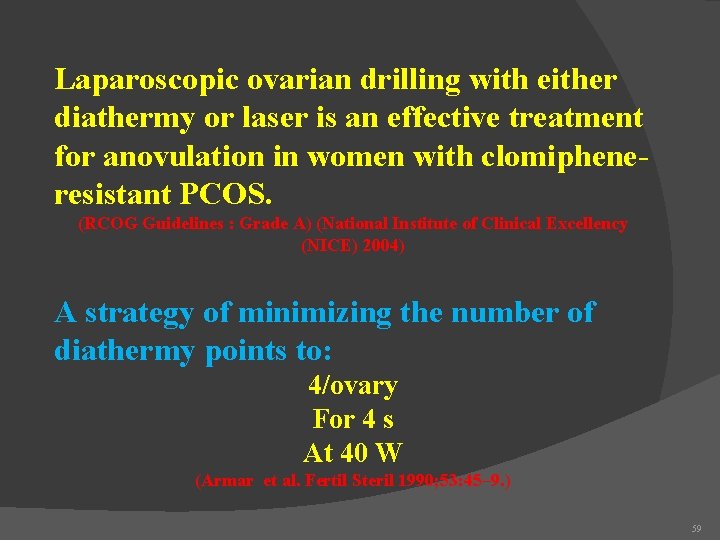
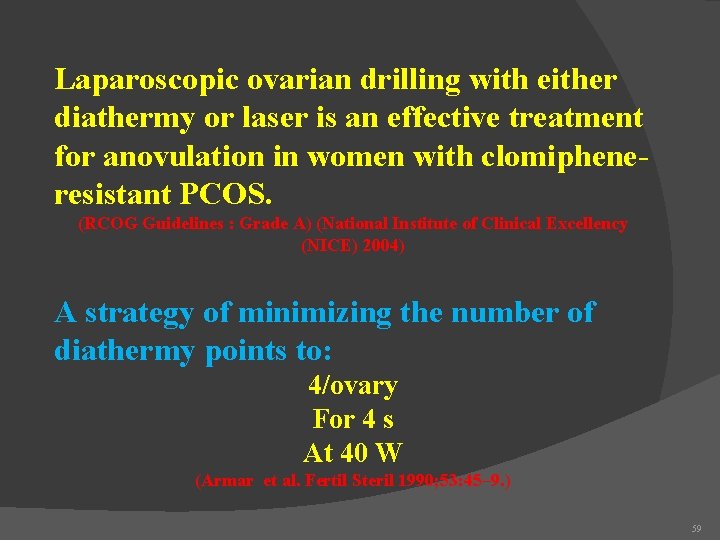
Laparoscopic ovarian drilling with either diathermy or laser is an effective treatment for anovulation in women with clomipheneresistant PCOS. (RCOG Guidelines : Grade A) (National Institute of Clinical Excellency (NICE) 2004) A strategy of minimizing the number of diathermy points to: 4/ovary For 4 s At 40 W (Armar et al. Fertil Steril 1990; 53: 45– 9. ) 59
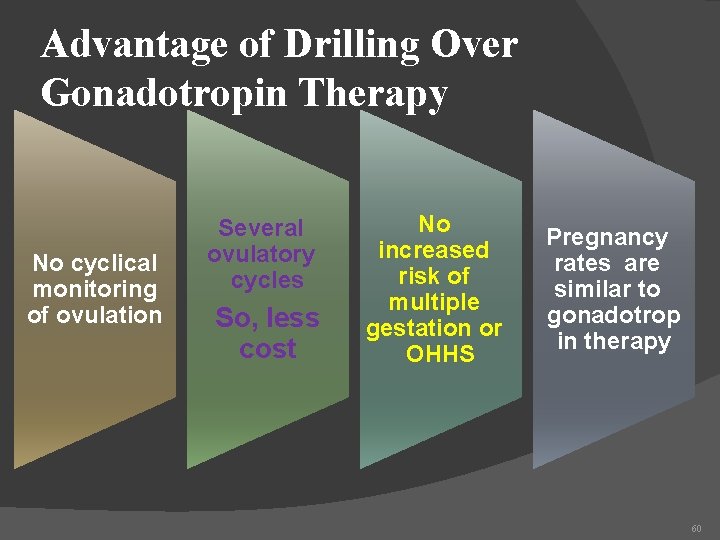
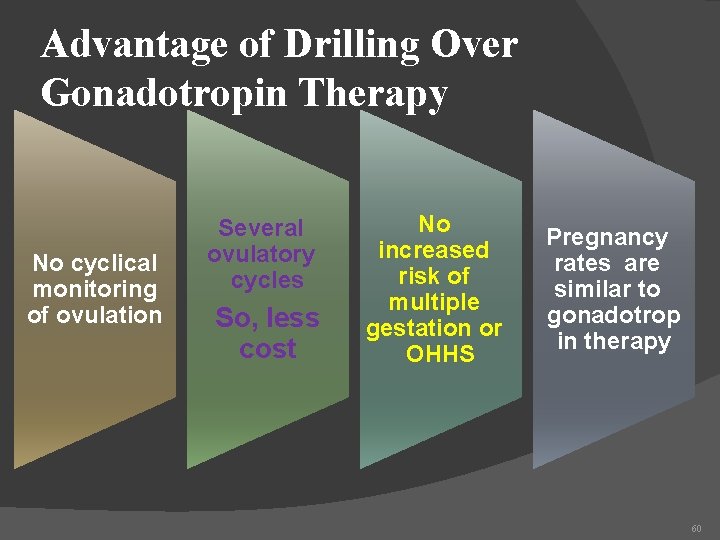
Advantage of Drilling Over Gonadotropin Therapy No cyclical monitoring of ovulation Several ovulatory cycles So, less cost No increased risk of multiple gestation or OHHS Pregnancy rates are similar to gonadotrop in therapy 60
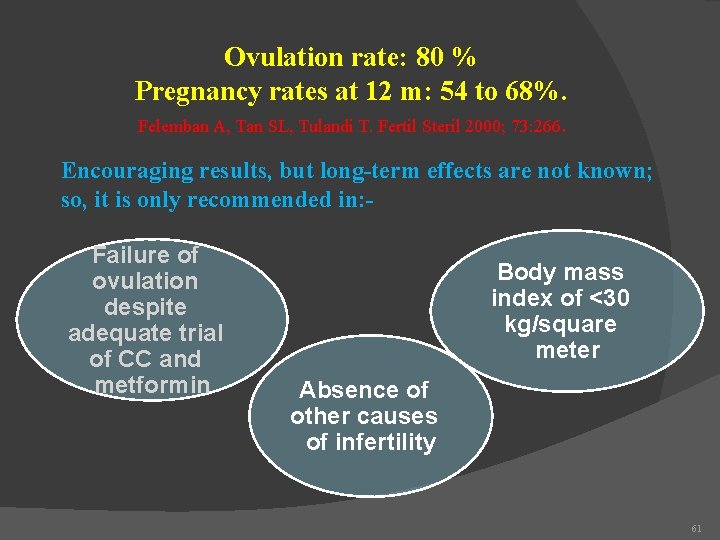
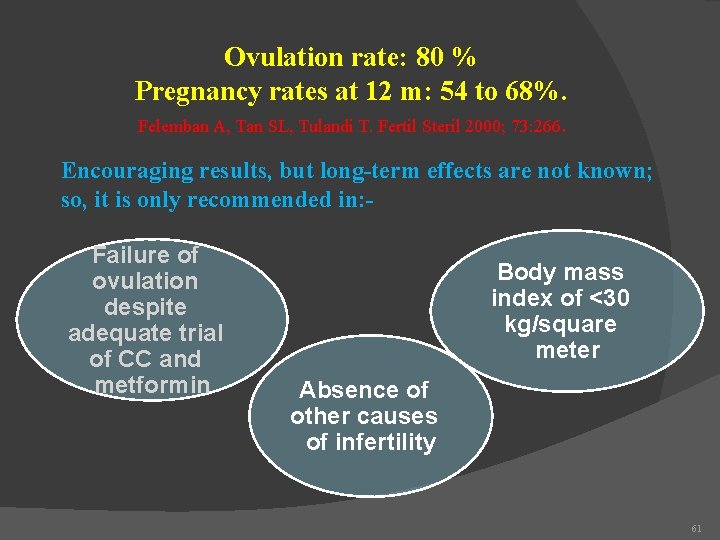
Ovulation rate: 80 % Pregnancy rates at 12 m: 54 to 68%. Felemban A, Tan SL, Tulandi T. Fertil Steril 2000; 73: 266. Encouraging results, but long-term effects are not known; so, it is only recommended in: Failure of ovulation despite adequate trial of CC and metformin Body mass index of <30 kg/square meter Absence of other causes of infertility 61
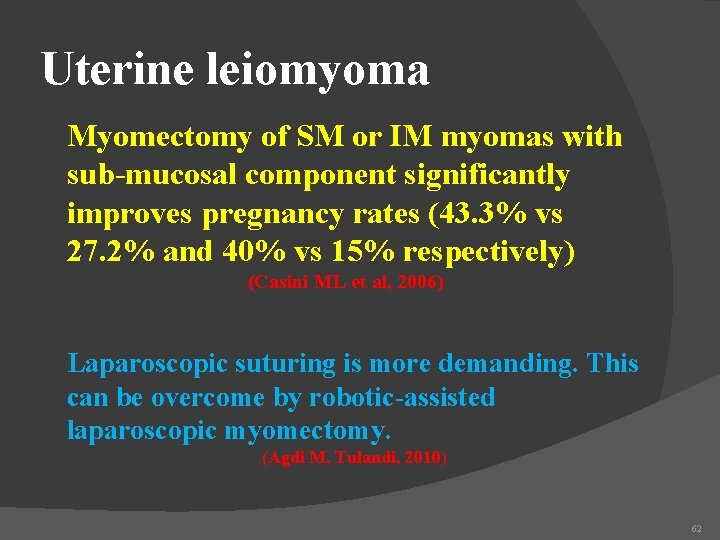
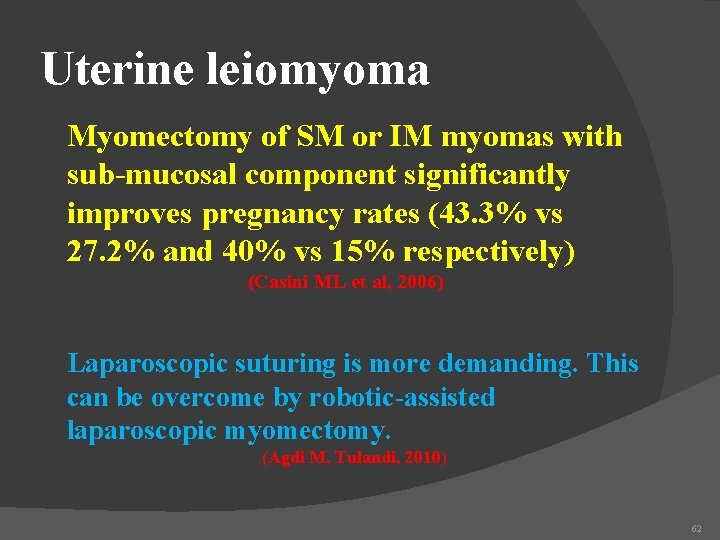
Uterine leiomyoma Myomectomy of SM or IM myomas with sub-mucosal component significantly improves pregnancy rates (43. 3% vs 27. 2% and 40% vs 15% respectively) (Casini ML et al, 2006) Laparoscopic suturing is more demanding. This can be overcome by robotic-assisted laparoscopic myomectomy. (Agdi M, Tulandi, 2010) 62
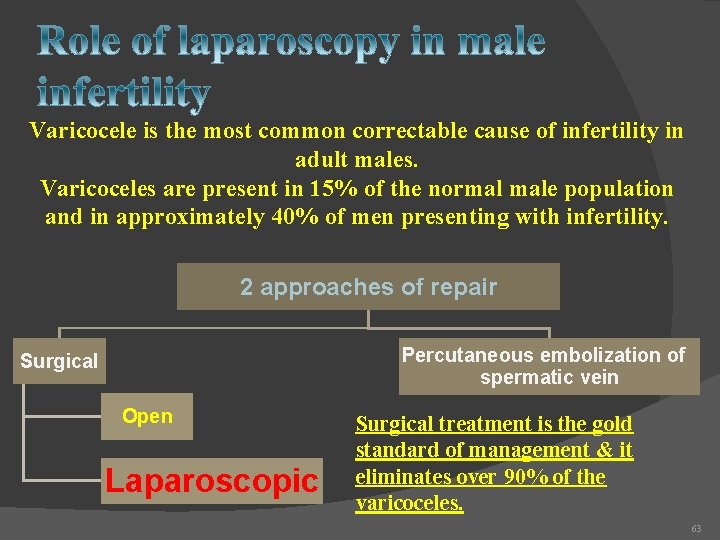
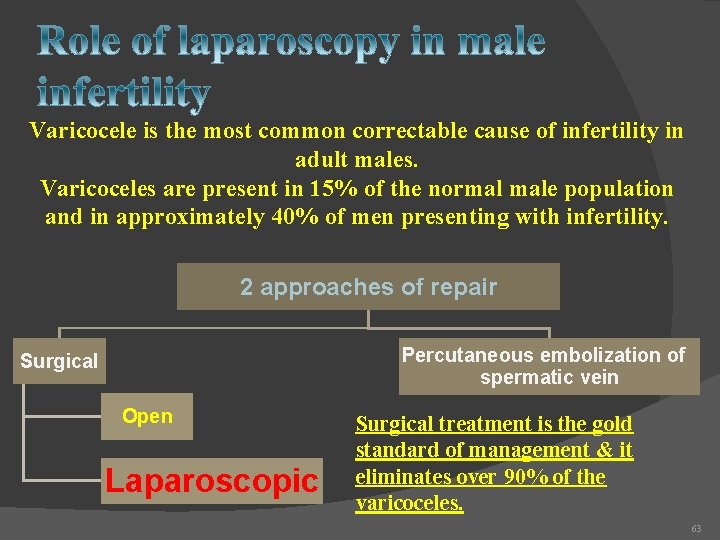
Varicocele is the most common correctable cause of infertility in adult males. Varicoceles are present in 15% of the normal male population and in approximately 40% of men presenting with infertility. 2 approaches of repair Percutaneous embolization of spermatic vein Surgical Open Laparoscopic Surgical treatment is the gold standard of management & it eliminates over 90% of the varicoceles. 63
Conclusion I The role of diagnostic laparoscopy in management of infertility is limited. However, it can be useful in infertility evaluation of young women with a history of PID, EP, pelvic surgery or chronic pelvic pain 64
Conclusion II Certainly, some women would have a correctable problem found at laparoscopy that would not be discovered with any other fertility screening test. 65
Conclusion III A significant number of patients, such as those with tubal factor and endometriosis, can benefit from operative laparoscopy. 66

6/19/2021 Dr Mohammad Khalil DR A DEWIDAR 67