GMC Standards Confidentiality delegation and referral raising concerns


- Slides: 29
GMC Standards Confidentiality, delegation and referral, raising concerns Rachel Woodall, GMC Regional Liaison Adviser
Snapshot of this evening § Brief overview of current guidance and online resources § Raising and acting on concerns § Confidentiality § Delegation and referral
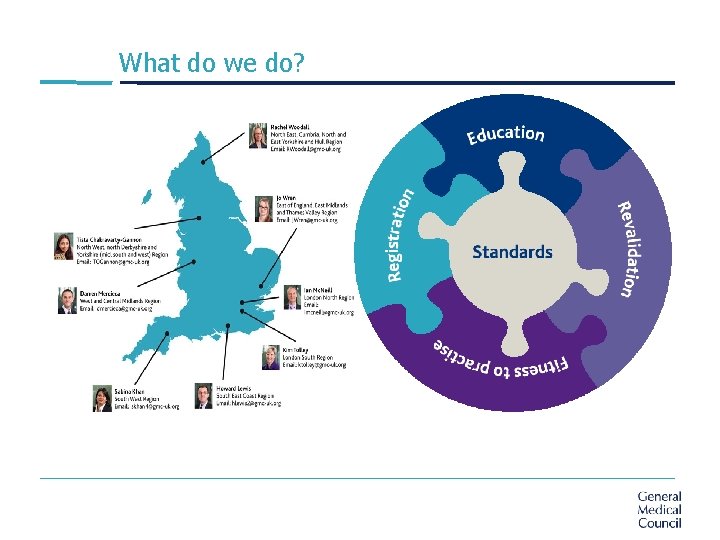
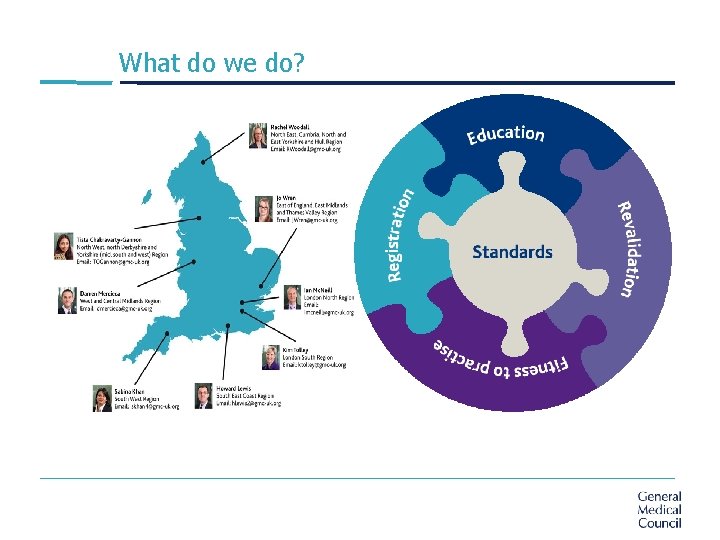
What do we do?
What guidance?
Online resources

Raising concerns
The duty § There is duty on all doctors to raise concerns where they believe that § patient safety § dignity, or § care § is compromised by the practice of colleagues or the systems, policies and procedures in the places in which they work.
The guidance § Part 1: Raising a concern gives advice on raising a concern that patients might be at risk of serious harm, and on the help and support available to doctors. § Part 2: Acting on a concern explains doctors’ responsibilities when colleagues or others raise concerns with them and how those concerns should be handled.
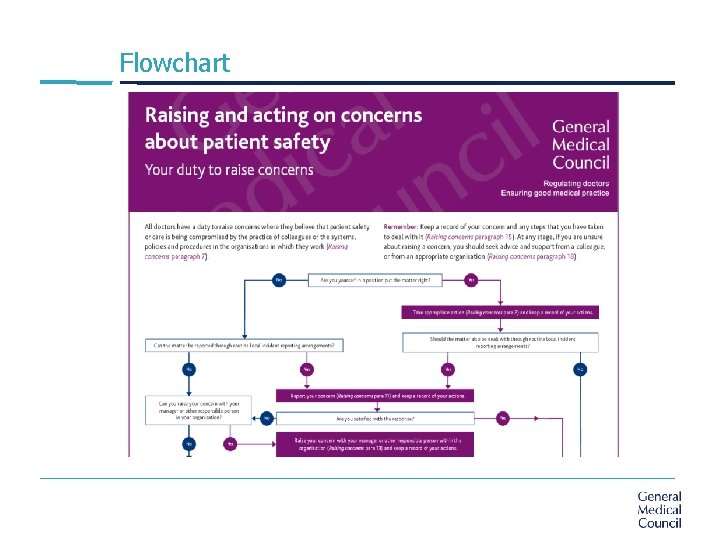
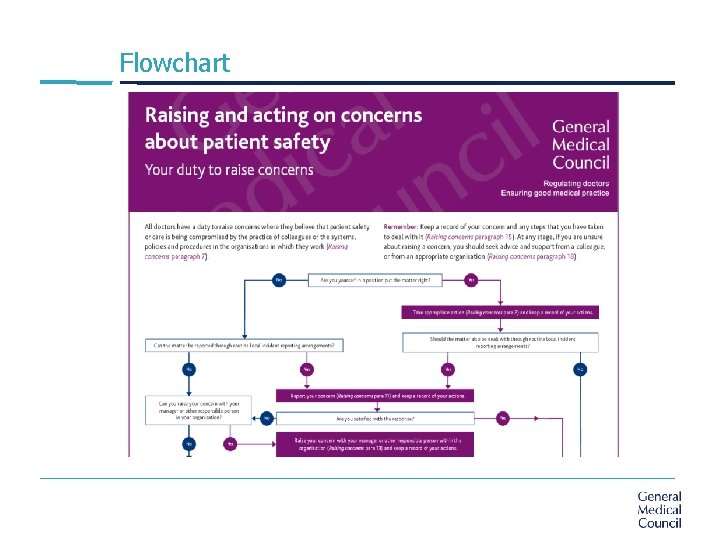
Flowchart
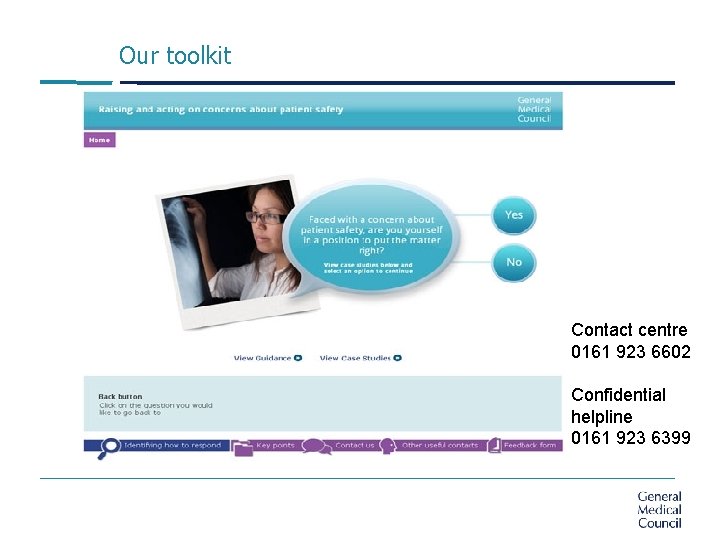
Our toolkit Contact centre 0161 923 6602 Confidential helpline 0161 923 6399
Yes or no 1. The law provides protection against victimisation or dismissal for individuals who raise concerns? 2. All doctors are responsible for encouraging and supporting a culture in which staff can raise concerns openly and safely? 3. You have to wait for proof and gather evidence before reporting? 4. Don’t delay – report to GMC straightaway?
Does it always have to be the nuclear option?
Dr Singh § Dr Hargreaves, a GP in the practice you are working, has recently returned to work following the death of his wife. He has been the subject of a complaint from Mr Wood, to whom he mistakenly prescribed penicillin in spite of the fact that his penicillin allergy was on record § The surgery receptionist, Jenny, says to you “Dr Singh, I gave him the patient records for this morning's surgery and he just looks awful - I can't imagine he's getting any sleep at all. And I'm sure I caught a whiff of alcohol too, though that might be from last night - Mark said he saw him coming out of the White Hart”
Dr Singh § You speak to the GP Partner who says “Well he's had a lot to deal with recently. I'd suggest he had more time off but he keeps saying that work's the only thing that's keeping him going” § You aren’t happy with this response, you and Jenny are concerned that he might make another mistake and are worried about his state of mind § You must support colleagues who have problems with their performance or health. But you must put patient safety first at all times(Good Medical Practice paragraph 43)
Dr Smith-Jones § Dr Smith-Jones is on a visit to a nursing home in the area, to see a resident, Jack, who is receiving palliative care. He is concerned to hear from relatives that Jack is not receiving the oxygen prescribed for him and Dr Smith-Jones can see Jack is losing weight quicker than expected. He has faeces stuck under his fingernails, has food stains down his bed covers and does not appear to have his hygiene needs looked after. § While there you can see the home appears understaffed, buzzers are going unanswered. As you go to the lift to try and speak to the manager, you hear a relative complaining to a member of staff that her elderly mother has burnt her chest after being given a cup of tea that was far too hot. She says ‘you know my mother shakes, why was she left with this at all? ’
Key points to understand: § your duty to protect patients § the steps to raise a concern where you work § your legal rights and the protections available to you § the difference between raising a concern and raising a personal grievance § Seek advice and support from a senior colleague, professional organisation, medical defence body or regulator, or Public Concern at work § Keep a record of your concerns and actions taken § Remember that you will be able to justify raising a concern if you do so honestly, on the basis of reasonable belief and through appropriate channels, even if you are mistaken
Confidentiality
The guidance § Emphasis remains firmly on obtaining consent where possible for disclosures of identifiable information and anonymising or coding data where possible § Disclosures should be kept to the minimum necessary § You must make sure all patient information that you hold or control is stored securely and used appropriately in line with the Data Protection Act § Duty continues after a patient’s death
Exceptions to the general duty: § Law (statute and judge-ordered) § Consent (implied or express) § Public interest § Does the public interest in disclosure of a patient’s personal information outweigh both the public interest and the patients’ interest in a confidential health service?
Explanatory guidance § Reporting concerns about patients to the DVLA § Disclosing records for financial and administrative purposes § Reporting gunshot and knife wounds § Disclosing information about serious communicable diseases § Disclosing information for insurance, employment and similar purposes § Disclosing information for education and training purposes § Responding to criticism in the press
Disclosures § The police want you to disclose if a man fitting the description of your patient came in today as they are investigating a road traffic accident. § Amy is a 15 year old patient and you can see from her records she was recently prescribed contraception when she visited on her own. She comes in to see you with her mother regarding headaches. § A patient has signed a consent form to release their full medical records as their insurance company require further information about back pain. § Mr Harris is 52 and has had epilepsy following a head injury 2 years ago. He has not had a fit for the past 6 months. He is the main carer for his disabled wife. He mentioned that he had driven to the surgery. What are your obligations?
Delegation and referral
Key points - delegation § When you delegate care you are still responsible for the overall management of the patient. § You XXXXX be satisfied that the person to whom you delegate has the knowledge, skills and experience to provide the care or treatment; or that the person will be adequately supervised.
Key points - referrals § Usually referrals will be made to another doctor or healthcare professional registered with a statutory regulatory body. Where this is not the case, you XXXXX be satisfied that systems are in place to assure the safety and quality of care provided, for example the services have been commissioned through an NHS commissioning process.
For both § You XXXXX make sure the patient is informed about who is responsible for their overall care and if the transfer is temporary or permanent. You XXXXX make sure the patient knows who to contact if they have questions or concerns about their care. § You XXXXX pass on to the healthcare professional involved: 1. Relevant information about the patient’s condition and history, 2. The purpose of transferring care and/or the investigation, care or treatment the patient needs.
Dr Gibbs § Dr Gibbs works as a GP in a rural practice. He receives a letter from the local hospital concerning an elderly patient, Mr Brown who has an inflammatory lung condition. Mr Brown's care in hospital has been managed by Consultant Respiratory Physician, Dr Santu. § The letter from Dr Santu explains that he has put Mr Brown on a course of azathioprine to reduce inflammation in the lungs and requests that Dr Gibbs continue the prescription. The letter states that Mr Brown will have a blood test when seen in the follow up clinic 4 weeks after discharge.
Dr Gibbs § Dr Gibbs notes that the date for the clinic appointment was four weeks ago but the letter was only sent within the last week. Dr Gibbs is aware that azathioprine can reduce white cells in the blood, reducing immunity and lead to an increased susceptibility to infection. He also notes that the hospital's shared care protocol which should have been included with the letter is missing. § Dr Gibbs tries to call Dr Santu's secretary and then Dr Santu directly but can not reach them. He immediately rings Mr Brown to check how he is doing and learns that he has not had a blood test since starting azathioprine.
Dr Mayer § Dr Mayer is a locum GP working at a busy inner-city practice. He sees Lucy, a 14 year old who has been persuaded to come in by her sister after taking an overdose. Her sister says that she thinks Lucy is being bullied. Dr Mayer notices evidence of previous cuts on Lucy’s wrists. When Lucy’s father arrives Dr Mayer feels that he is highly critical of Lucy, describing her as a “trouble-maker” and apologises for wasting time. § Dr Mayer’s surgery have Teresa, a final year medical student working with them. Dr Mayer passes her in the corridor and she looks stressed, so asks her if things are ok? She says “I’m ok, just a bit nervous, the secretary has just asked me to do a cervical smear as everyone is busy”

Rachel Woodall Regional Liaison Adviser 0161 250 6832 07787006390 rwoodall@gmc-uk. org @Woodall. Rach
 Gmc confidentiality
Gmc confidentiality Gmc inspire automation
Gmc inspire automation Wbpa rcgp
Wbpa rcgp Green turtle grease interceptor
Green turtle grease interceptor Health education north west
Health education north west Gmc translation
Gmc translation Paul buckley gmc
Paul buckley gmc Jane mamelok gmc
Jane mamelok gmc Dr peter rubin
Dr peter rubin Gmdtranslations
Gmdtranslations Conventional encryption and message confidentiality
Conventional encryption and message confidentiality Confidentiality and privacy controls
Confidentiality and privacy controls La netiquette mail
La netiquette mail Prayer is the raising of one's heart and mind to god
Prayer is the raising of one's heart and mind to god Trussed beam ladder
Trussed beam ladder Addressing concerns and earning commitment
Addressing concerns and earning commitment Earning commitment
Earning commitment Joys and concerns images
Joys and concerns images Joys and concerns prayer
Joys and concerns prayer Joys and concerns images
Joys and concerns images Hard customer defined standards
Hard customer defined standards Purpose of delegation
Purpose of delegation Advantages of delegation
Advantages of delegation Leadership and delegation in nursing
Leadership and delegation in nursing Continuum of participation
Continuum of participation Elements of delegation
Elements of delegation Why is confidentiality important
Why is confidentiality important Confidentiality using symmetric encryption
Confidentiality using symmetric encryption Texas address confidentiality program
Texas address confidentiality program Matthew seavey
Matthew seavey