Head injury anaesthetic concerns Dr S Parthasarathy MD





- Slides: 45
Head injury- anaesthetic concerns Dr. S. Parthasarathy MD. , DA. , DNB, MD (Acu), Dip. Diab. DCA, Dip. Software statistics, Phd (physio) Mahatma Gandhi Medical college and research institute puducherry , India
What is this ? ? �Head injury can be defined as any trauma to the head, other than superficial facial injuries. �This term is often used interchangeably with both brain injury and traumatic brain injury. (TBI)

Incidence and classification � 1 million / year in UK � 1 % of all adult deaths �In India one person dies every 10 minutes due to TBI, and this will treble by 2020. � 80% -- Mild - == GCS 13 -15 � 10 -15 % –Moderate 9 -12 � 5 -10% - Severe < 8 ( mortality of 25 % )
One more classification �Primary �Instantaneous neuronal injury at the impact time �Can we do something ? ? �Secondary �We can do something !! Why does it happen ? ?
We want to decrease it !!

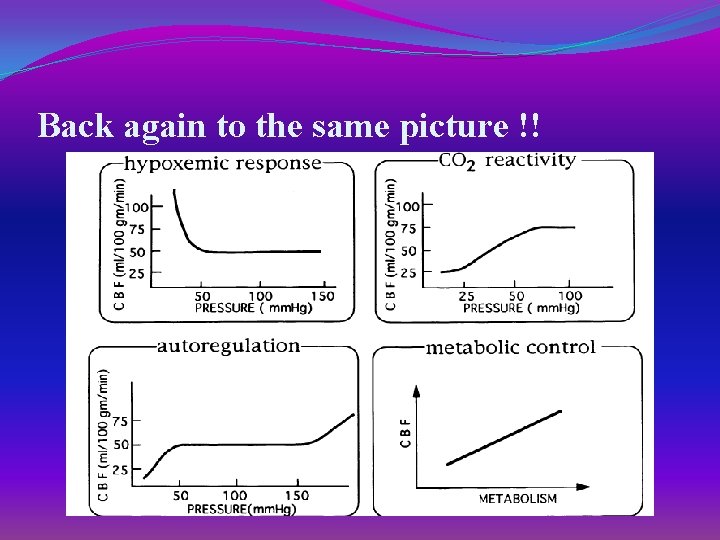
TBI itself causes these !! �. 1 DECREASE CBF[ ESP < 18 CC/100 G/MIN[ �. 2 IMPAIR AUTOREGULATION �. 3 INCREASE ICP � 4. HYPERTENSION � 5. IRREGULAR RESPIRATION � 6. HYPERTHERMIA Response to head injury
Types of injuries �Haemorhagic contusion �Intracerebral hematomas �Subdural hematomas �Extradural hematomas �Vascular injuries �Diffuse axonal injuries �Skull fractures
Look for �Chest injuries �Bleeding profuse external injuries �Abdominal injuries �Spine injuries �Ophthalmic injuries �Vitals �Breathing and airway injuries
Then come to brain
Initial assessment �Conscious status – GCS – pupils �Cervical spine injuries _ 5 % �Extra cranial injuries upto 50 % !! �GCS – 8 or below – intubate �Don’t sedate any patient with head injury for CT scan if uncooperative �Better intubate and control �Good dose of thio will obliterate scoline induced ICP problem !!
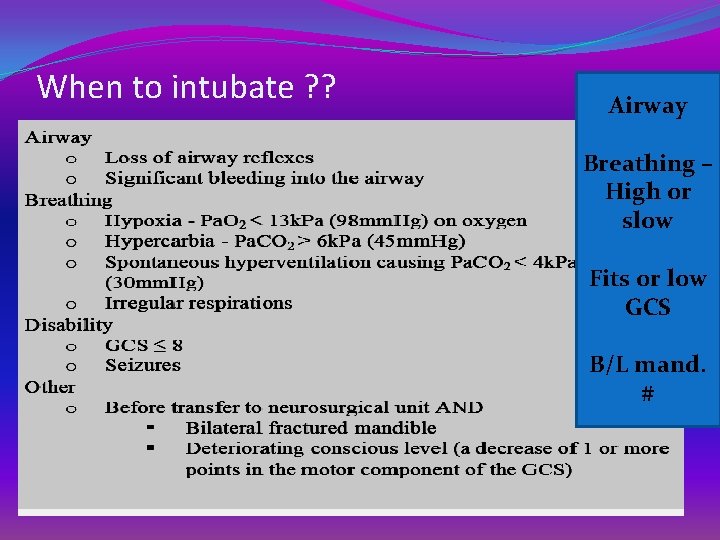
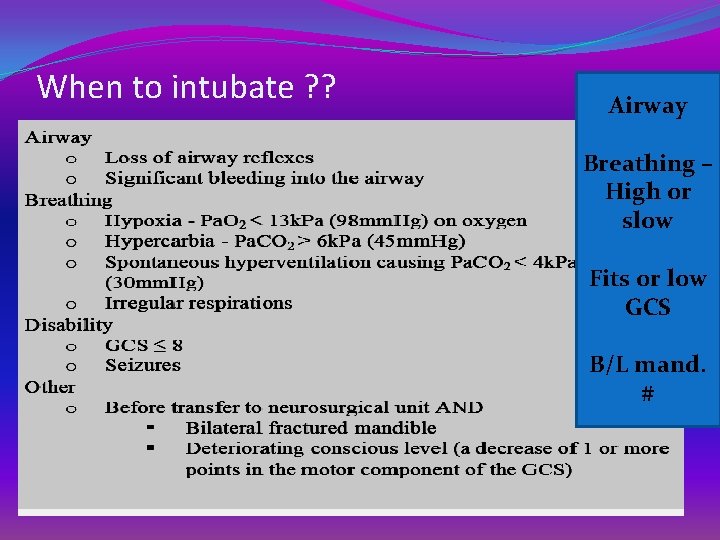
When to intubate ? ? Airway Breathing – High or slow Fits or low GCS B/L mand. #
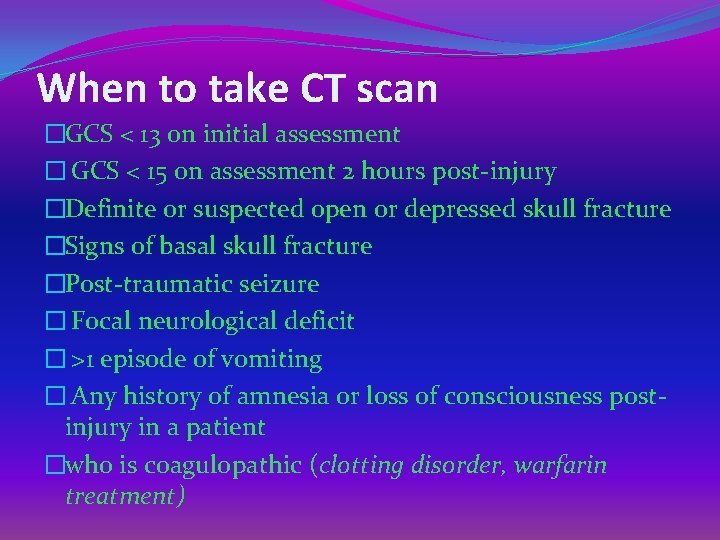
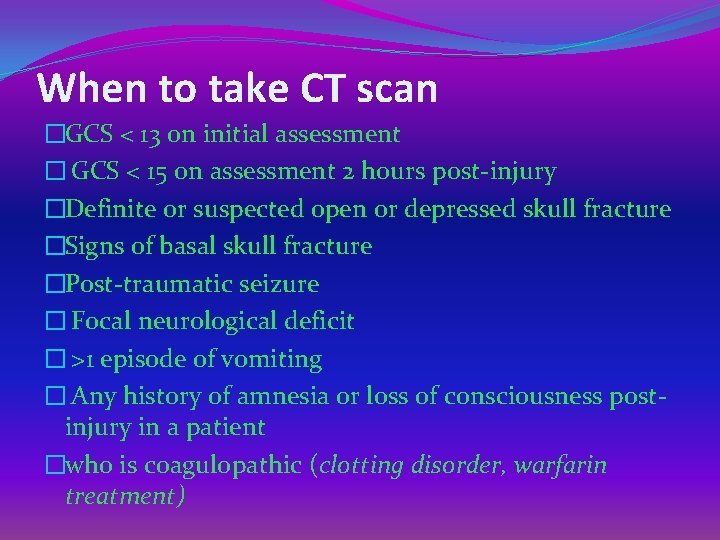
When to take CT scan �GCS < 13 on initial assessment � GCS < 15 on assessment 2 hours post-injury �Definite or suspected open or depressed skull fracture �Signs of basal skull fracture �Post-traumatic seizure � Focal neurological deficit � >1 episode of vomiting � Any history of amnesia or loss of consciousness postinjury in a patient �who is coagulopathic (clotting disorder, warfarin treatment)
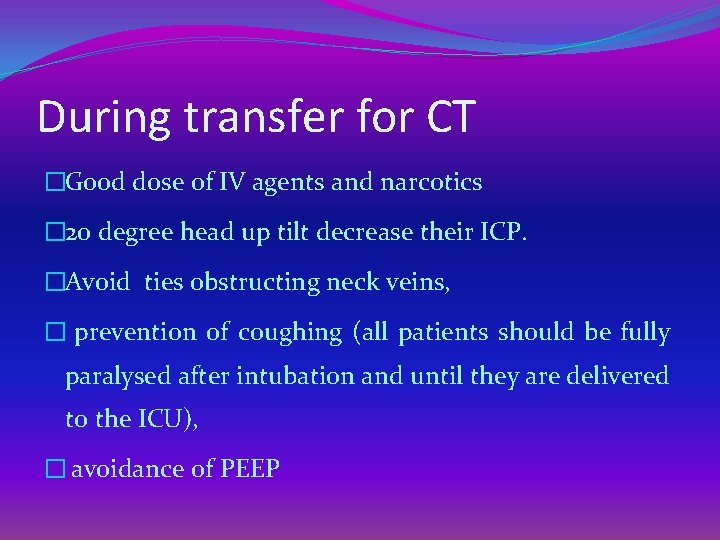
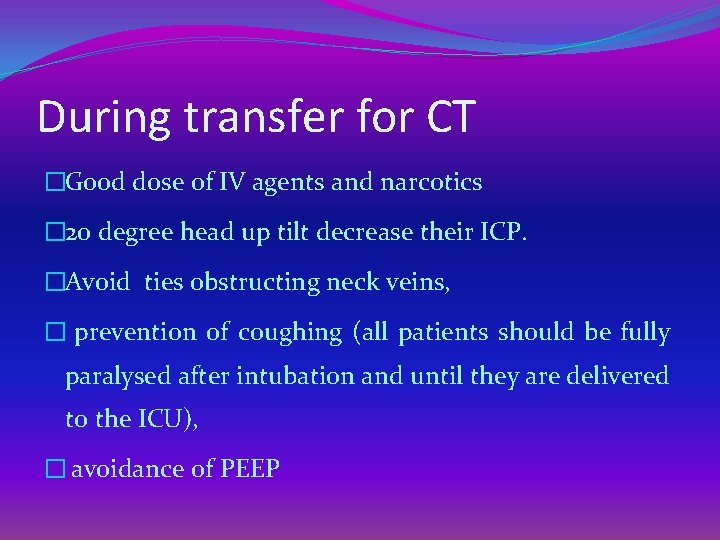
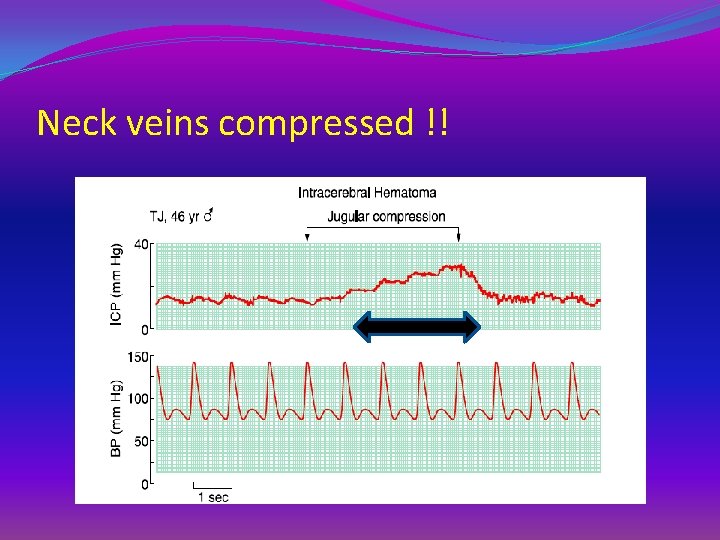
During transfer for CT �Good dose of IV agents and narcotics � 20 degree head up tilt decrease their ICP. �Avoid ties obstructing neck veins, � prevention of coughing (all patients should be fully paralysed after intubation and until they are delivered to the ICU), � avoidance of PEEP
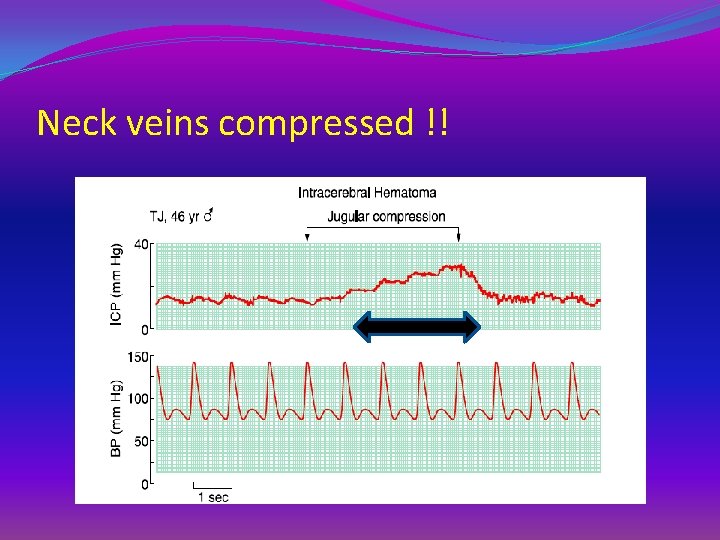
Neck veins compressed !!
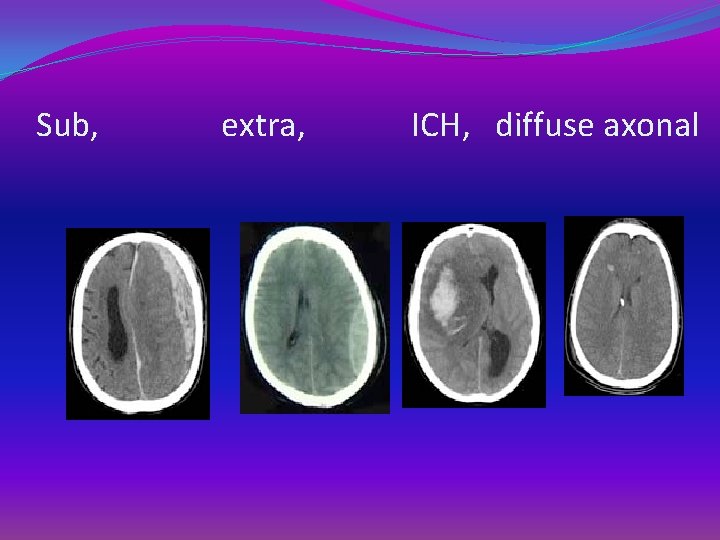
Sub, extra, ICH, diffuse axonal
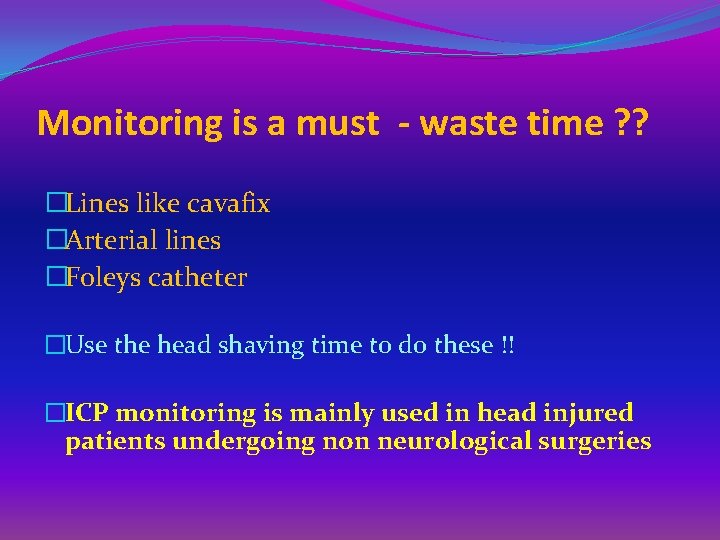
Monitoring is a must - waste time ? ? �Lines like cavafix �Arterial lines �Foleys catheter �Use the head shaving time to do these !! �ICP monitoring is mainly used in head injured patients undergoing non neurological surgeries
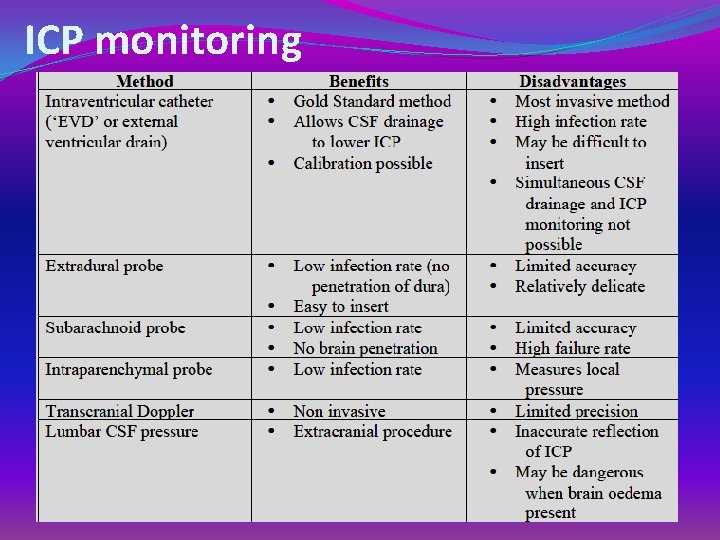
ICP monitoring
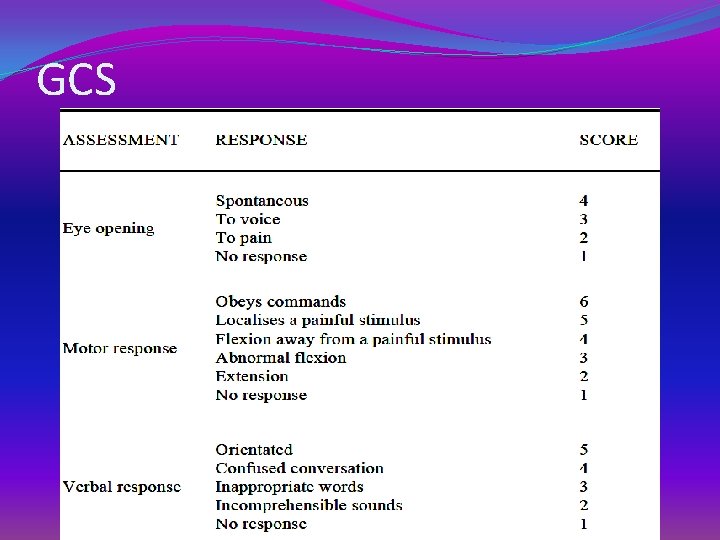
GCS
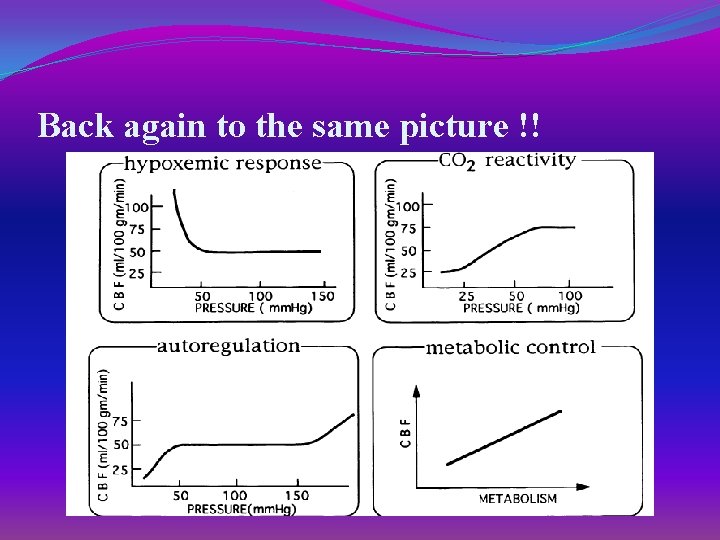
Back again to the same picture !!
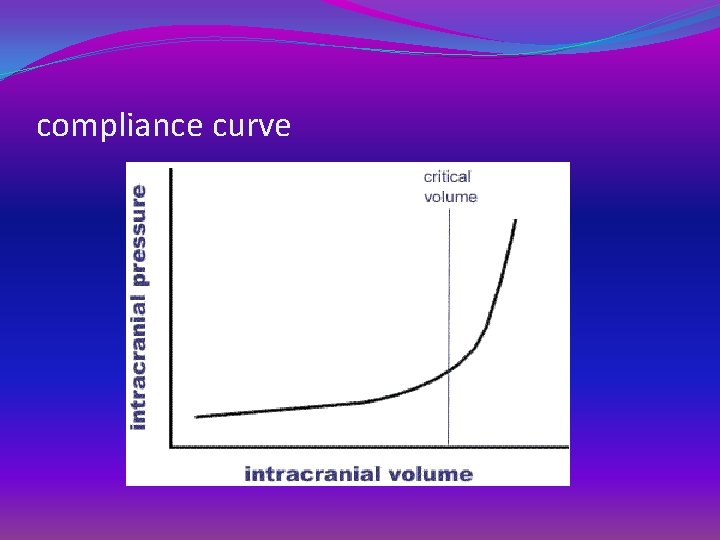
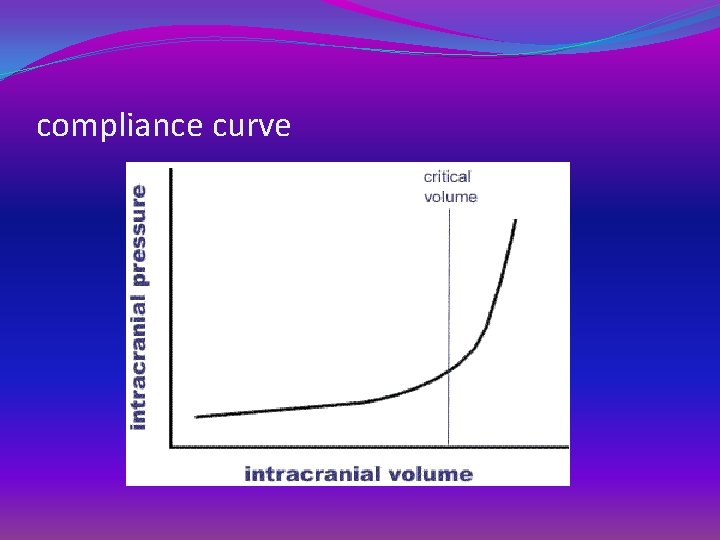
compliance curve
Preoperative preparation �Routine investigations �Blood grouping and reservation �Coagulation profile �Possible neuroprotective role �Potassium �Magnesium �Female gender hormones
Aims of anaesthesia �Avoid secondary brain damage �Optimize cerebral perfusion and oxygenation �Provide adequate surgical conditions for the neurosurgeons.
Induction �Usually intubated �If not start propofol/thio / suxa / intubation �Difficult airway – awake fibreoptic �Glidescope �Never allow hypoxemia. Hypercarbia etc. . �Be aggressive
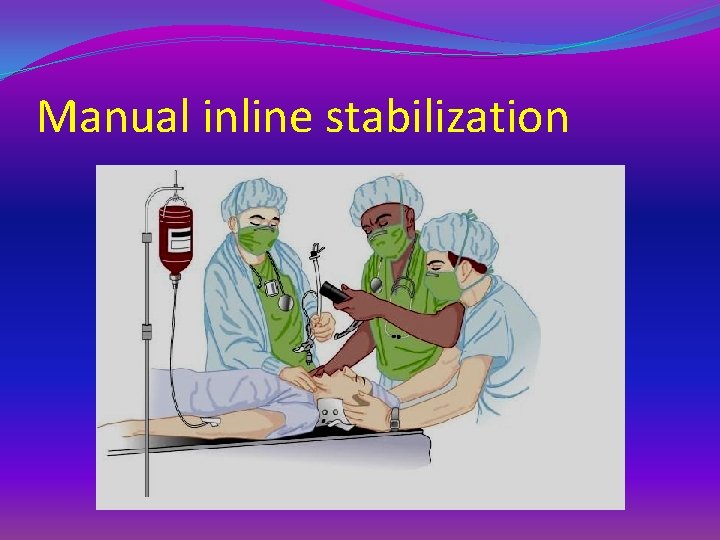
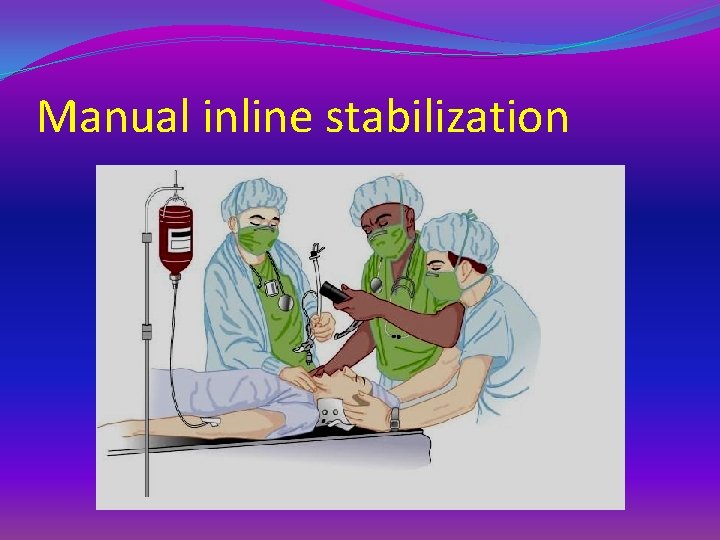
Manual inline stabilization
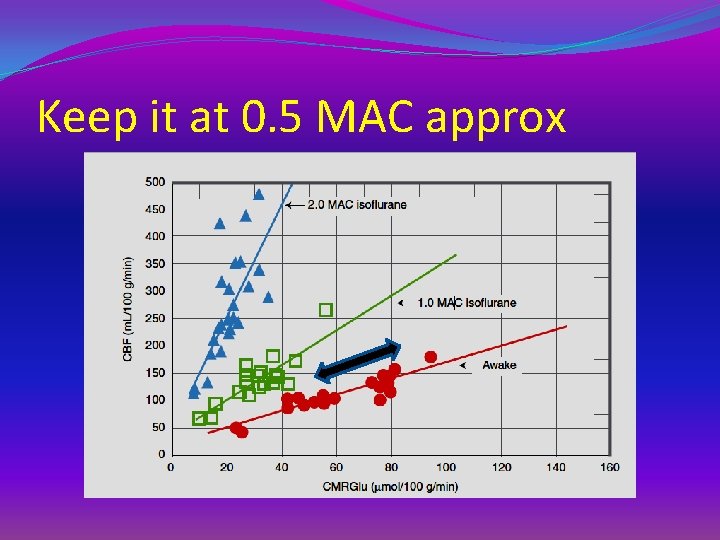
Maintanance �Ketamine Can be avoided �Studies say – can coadminister with propofol �Continue propofol infusion with hemodynamic stability �Nitrous oxide can increase CMRO 2 and cause cerebral vasodialation and increased ICP and should be avoided �Inhalational agents with titration( < 1 MAC ) – OK �tight brain – stop and switch over to IV agents
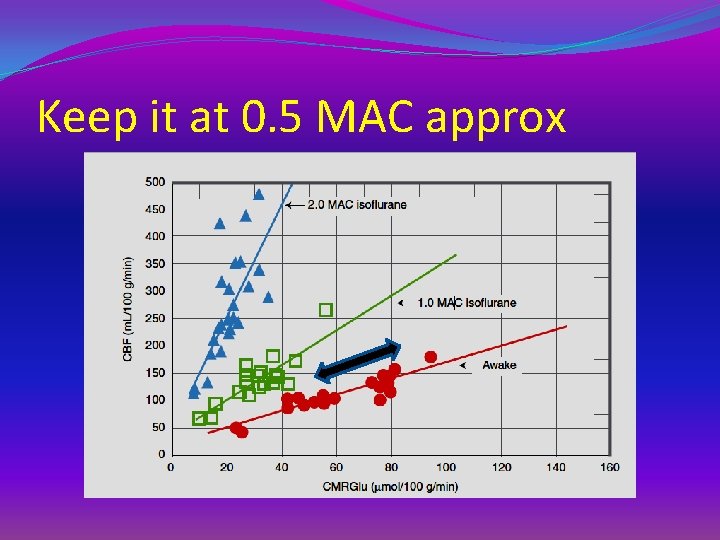
Keep it at 0. 5 MAC approx
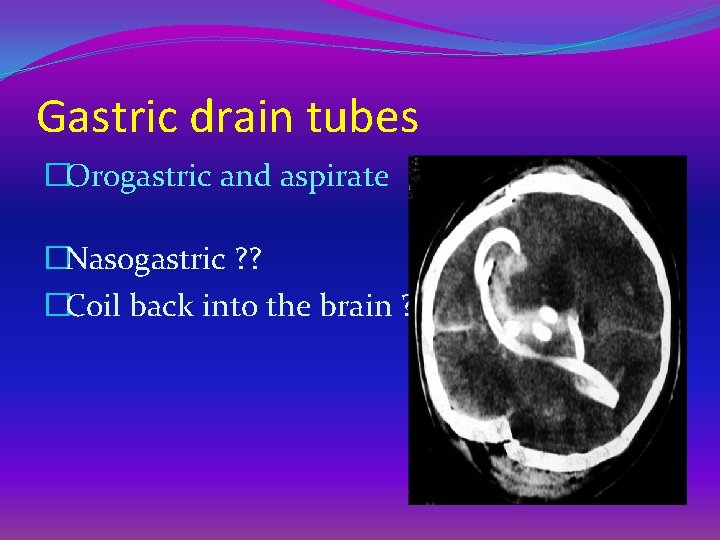
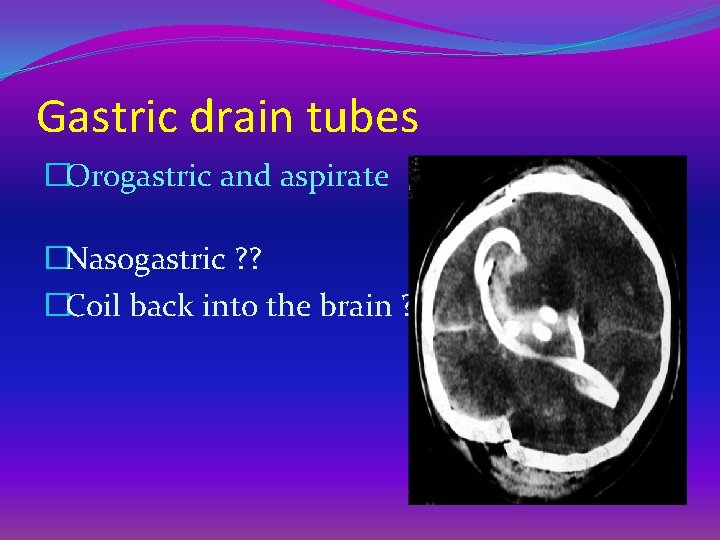
Gastric drain tubes �Orogastric and aspirate �Nasogastric ? ? �Coil back into the brain ?
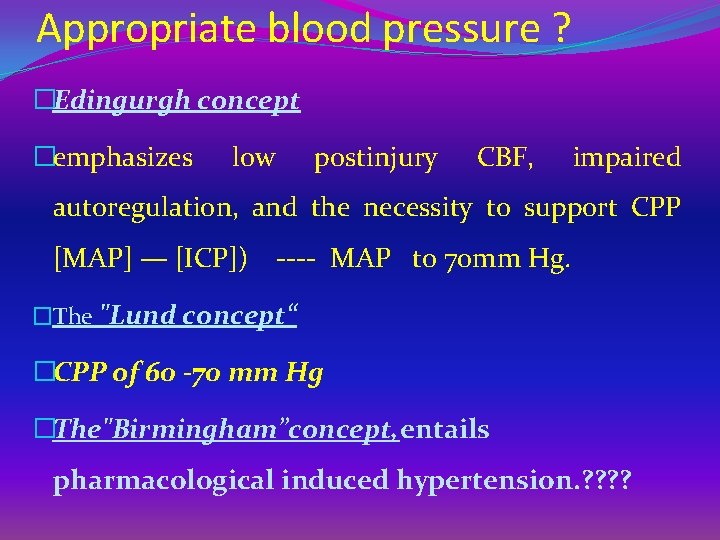
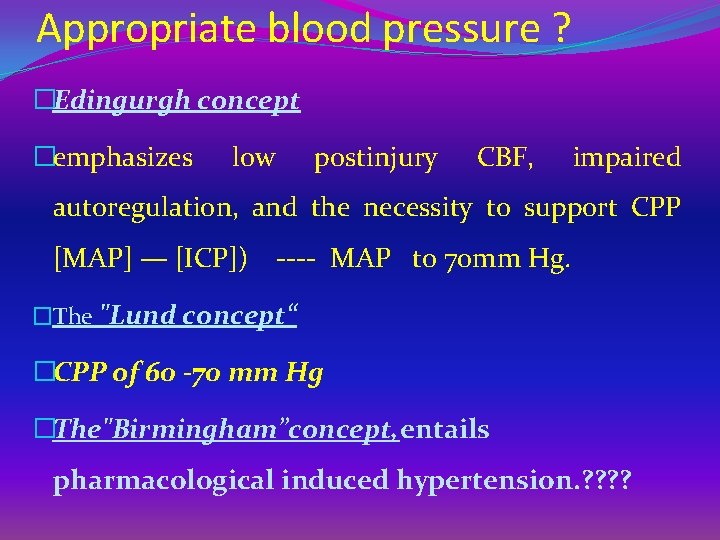
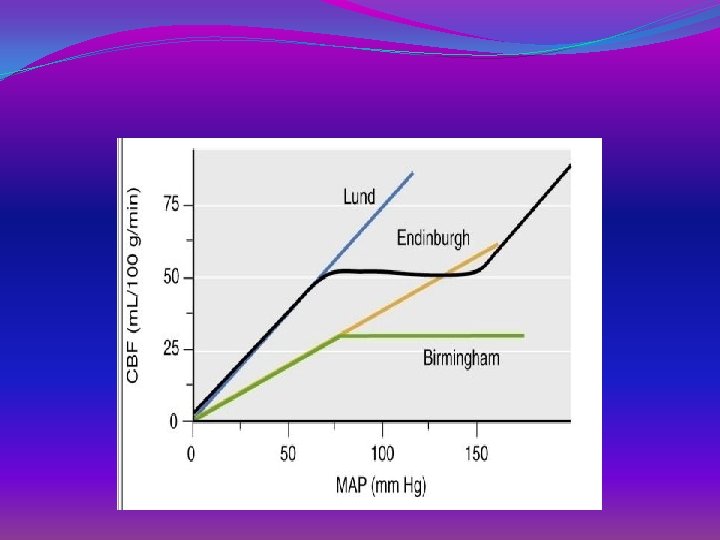
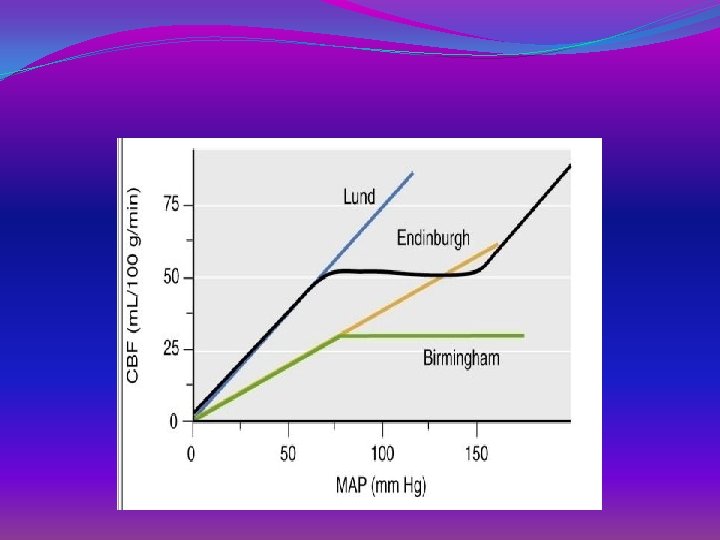
Appropriate blood pressure ? �Edingurgh concept �emphasizes low postinjury CBF, impaired autoregulation, and the necessity to support CPP [MAP] — [ICP]) ---- MAP to 70 mm Hg. �The "Lund concept“ �CPP of 60 -70 mm Hg �The"Birmingham”concept, entails pharmacological induced hypertension. ? ?

Be liberal in vasopressors
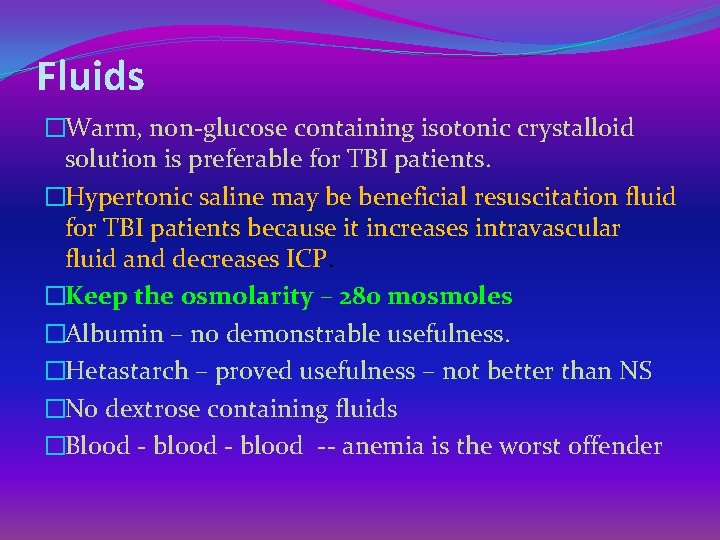
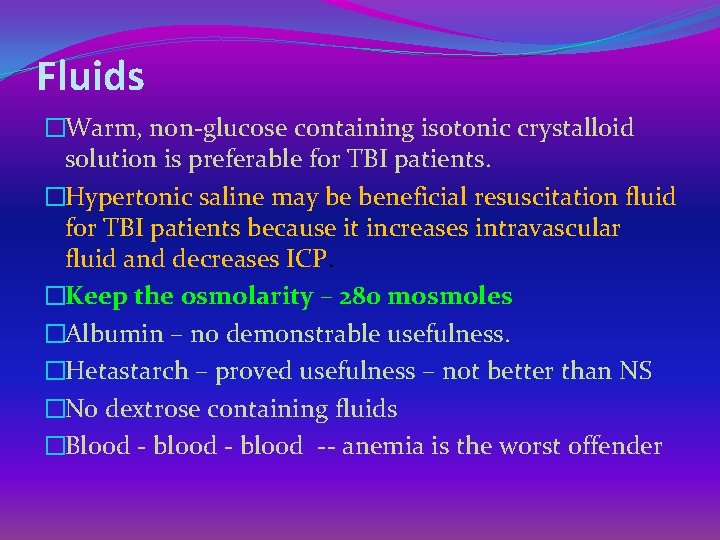
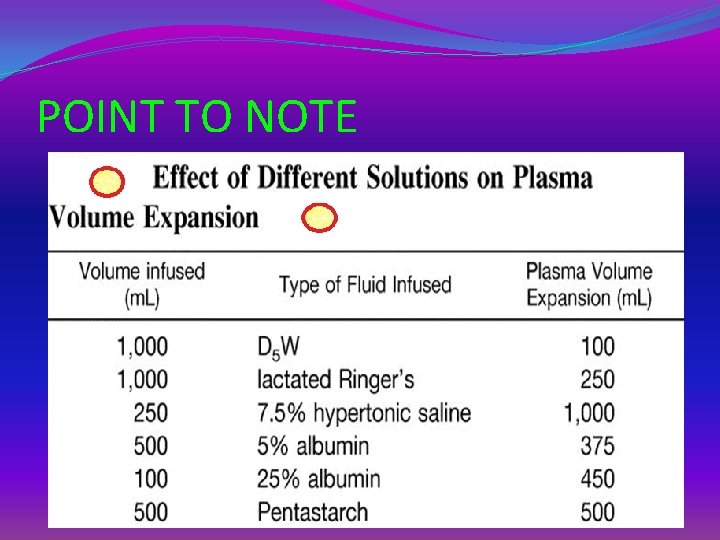
Fluids �Warm, non-glucose containing isotonic crystalloid solution is preferable for TBI patients. �Hypertonic saline may be beneficial resuscitation fluid for TBI patients because it increases intravascular fluid and decreases ICP. �Keep the osmolarity – 280 mosmoles �Albumin – no demonstrable usefulness. �Hetastarch – proved usefulness – not better than NS �No dextrose containing fluids �Blood - blood -- anemia is the worst offender
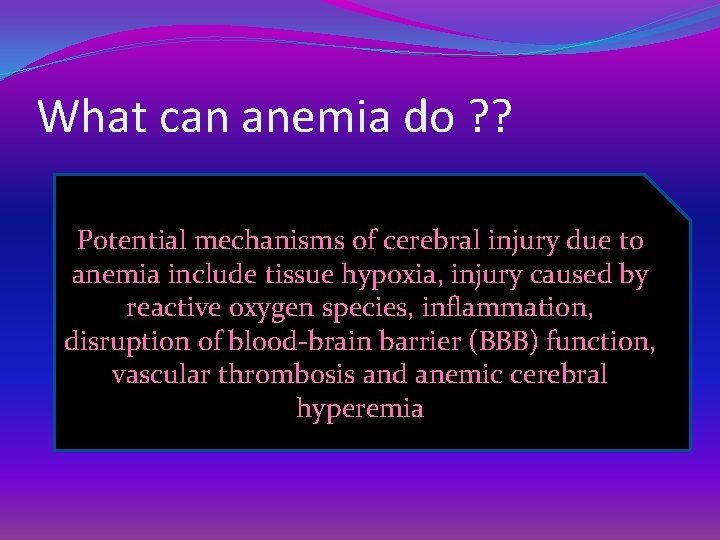
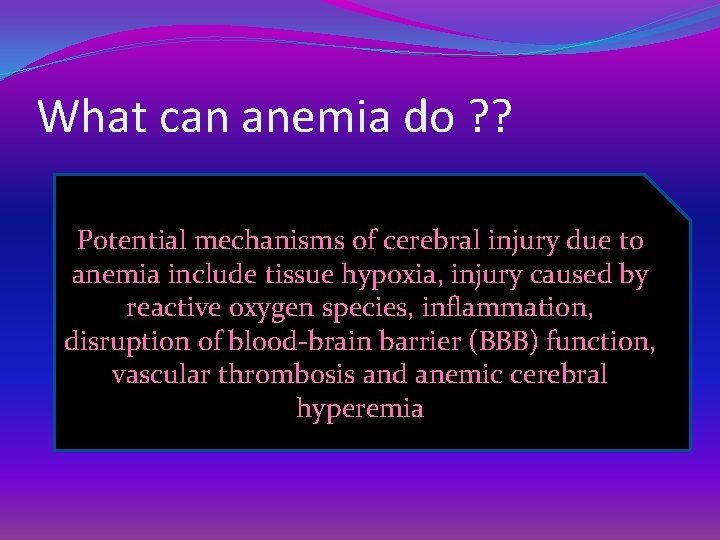
What can anemia do ? ? Potential mechanisms of cerebral injury due to anemia include tissue hypoxia, injury caused by reactive oxygen species, inflammation, disruption of blood-brain barrier (BBB) function, vascular thrombosis and anemic cerebral hyperemia
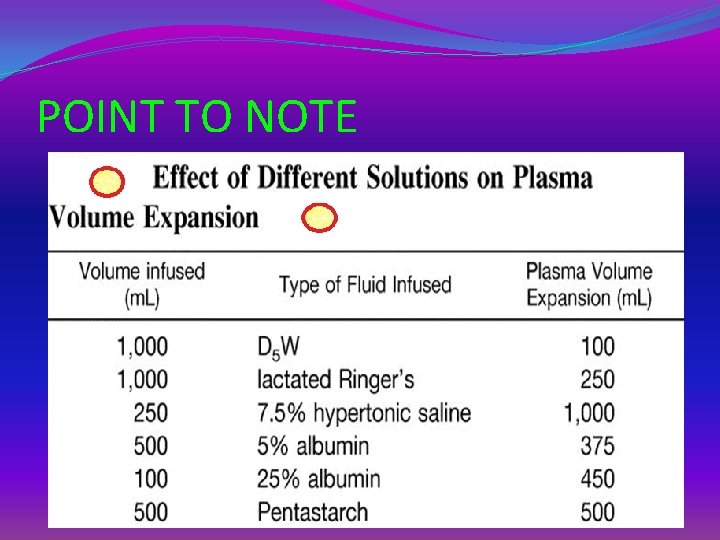
POINT TO NOTE
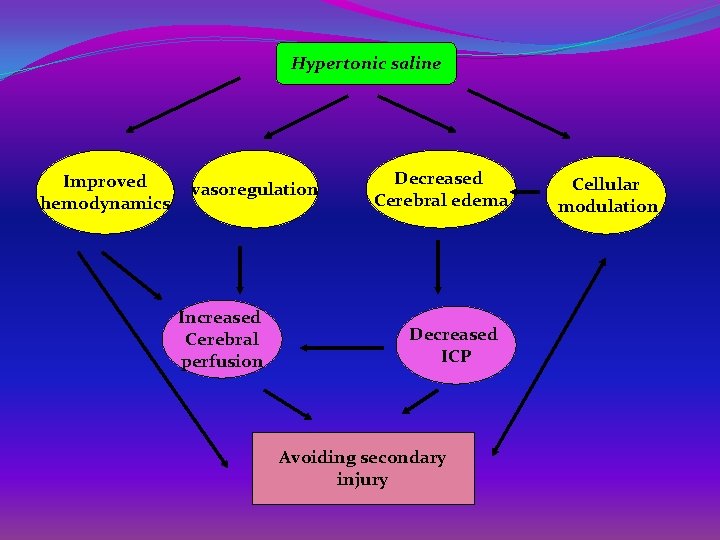
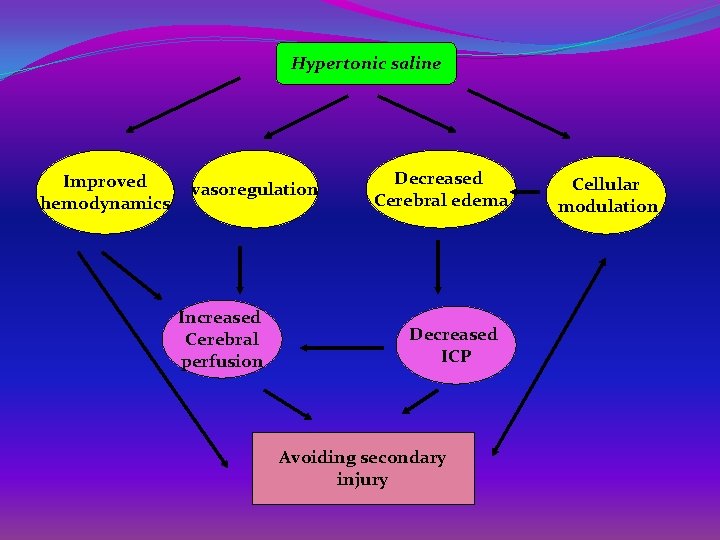
Hypertonic saline Improved hemodynamics vasoregulation Increased Cerebral perfusion Decreased Cerebral edema Decreased ICP Avoiding secondary injury Cellular modulation
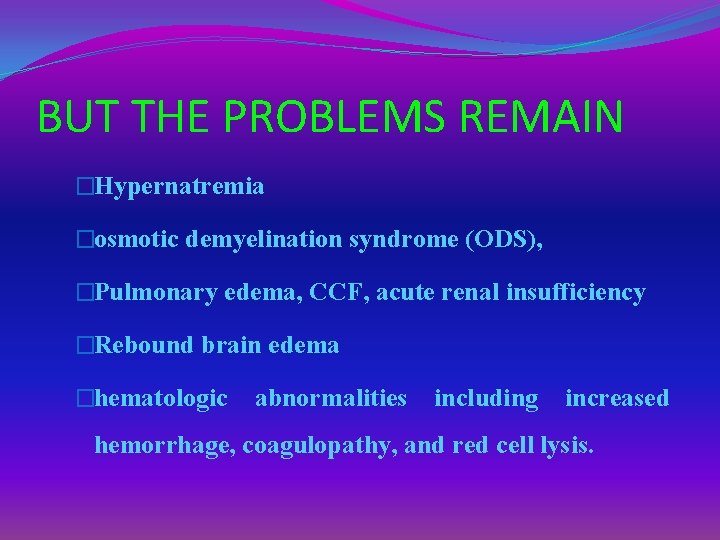
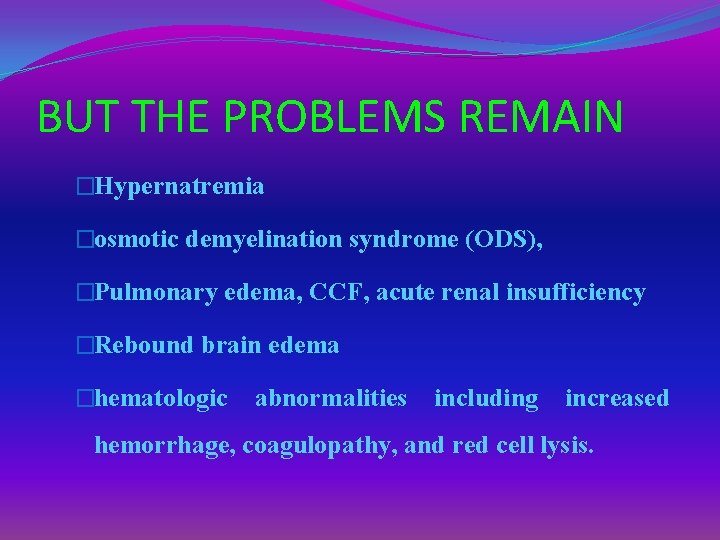
BUT THE PROBLEMS REMAIN �Hypernatremia �osmotic demyelination syndrome (ODS), �Pulmonary edema, CCF, acute renal insufficiency �Rebound brain edema �hematologic abnormalities including increased hemorrhage, coagulopathy, and red cell lysis.
Hyperventilation �MAY BE USEFUL �acute increases in ICP �need to improve surgical exposure �Paco 2 can decrease ICP but cerebral ischemia ? ? – �short lived action of hypocarbia �Studies – beneficial Paco 2 is around 30 -35
Miscellaneous �Routine stress ulcer prophylaxis is required. �Seizure prophylaxis is currently recommended for 7 days following the injury in patients with severe TBI. �The agent most commonly recommended is phenytoin, �loading dose of 18 mg/kg �maintenance dose of 5 mg/kg/d �serum drug levels 10 to 20 mg/L. Hyponatremia, hypomagnesemia !!
Miscellaneous �Both hypoglycaemia and hyperglycaemia can worsen brain injury. �A blood glucose of 4 – 8 mmol/l is targeted �majority of studies indicate that 15 -30°head elevation reduces ICP without compromising CPP or cerebral oxygenation. � Marked degrees of head elevation (>30°) may actually increase ICP in some patients by causing autoregulatory vasodilatation �Keep it at 20
Miscellaneous �Mild hypothermia (32 -34°C) is beneficial in head injuries. �It reduces CMR, CBF, ICP and improves outcome �Steroids have no role in head injury !! �Diuretics have definite role – detailed earlier �Mannitol – 1 gm/kg followed by frusemide – ICP, ? Brain herniation, slackness
Coagulopathy �Coagulation disorder could result from TBI and cause secondary brain injury. �A recent review reported that the overall prevalence of coagulopathy was 32. 7% after TBI and more than 60% in severe TBI �presence of coagulopathy was associated with an increased mortality and poor outcome. �Novoseven. Tranexamic acid
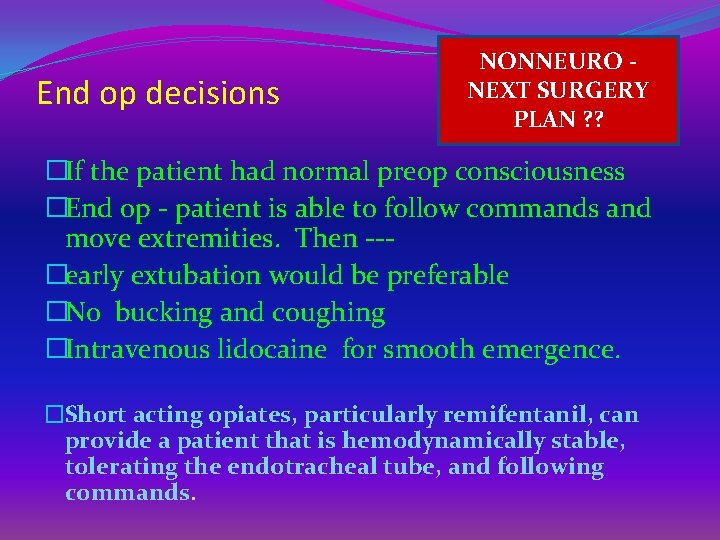
End op decisions NONNEURO NEXT SURGERY PLAN ? ? �If the patient had normal preop consciousness �End op - patient is able to follow commands and move extremities. Then --�early extubation would be preferable �No bucking and coughing �Intravenous lidocaine for smooth emergence. �Short acting opiates, particularly remifentanil, can provide a patient that is hemodynamically stable, tolerating the endotracheal tube, and following commands.

DURING TRANSFER �VENTILATION, OXYGENATION, CPP MUST BE CAREFULLY MAINTAINED. �MONITOR BP, CAPNOGRAPHY, Sa. O 2, ICP �EMERGENCE CAN RESULT IN INCREASE IN BP, ICP, ADDITIONAL SEDATIVE, NARCOTIC, LABETALOL MAY BE REQUIRED �ALVEOLAR VENTILATION MUST BE CAREFULLY SUPPORTED AND MONITORED UNTIL TO ICU

Summary �Definition �Intubate ? �CT scan ? �Aggressive �Other injuries �Aims of anaesthesia �Induction and intubation �Recovery OTHER INJURIES PREVENT SECONDARY BRAIN INJURY
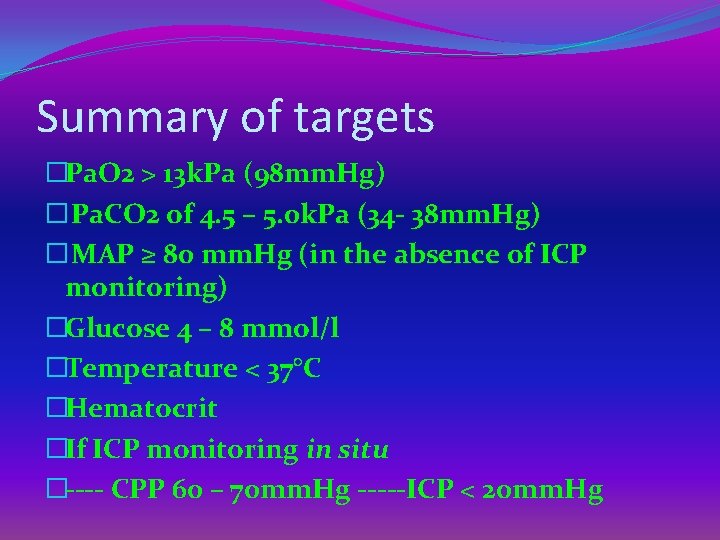
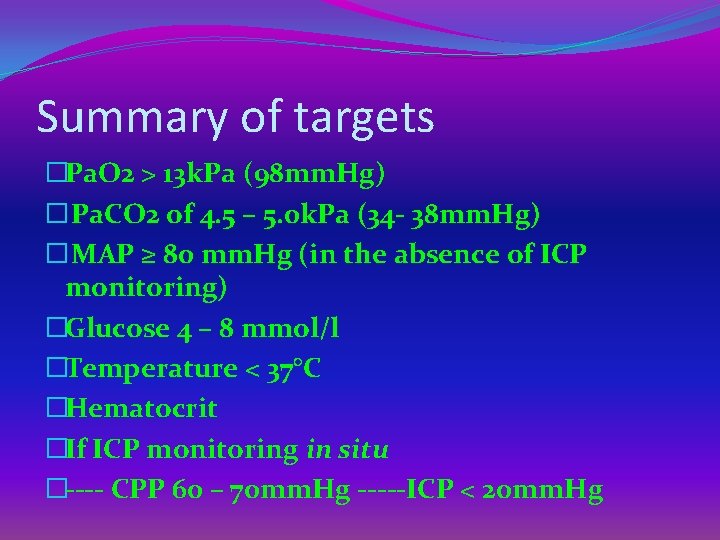
Summary of targets �Pa. O 2 > 13 k. Pa (98 mm. Hg) � Pa. CO 2 of 4. 5 – 5. 0 k. Pa (34 - 38 mm. Hg) � MAP ≥ 80 mm. Hg (in the absence of ICP monitoring) �Glucose 4 – 8 mmol/l �Temperature < 37°C �Hematocrit �If ICP monitoring in situ �---- CPP 60 – 70 mm. Hg -----ICP < 20 mm. Hg
Carry home message