1 Intracanal medicaments Nilesh Deshpande JRII Department of
- Slides: 71
1 Intracanal medicaments Nilesh Deshpande JR-II Department of pediatric and preventive dentistry
2 INTRODUCTION • An important objective of endodontic therapy is the removal of necrotic infected pulp and dentinal debris from the root canal system of infected or non-vital teeth. • Failure to use an irrigating solution during BMP results in considerable amount of debris to be left behind in the root canal system ultimately leading to endodontic failure. • Hence for obtaining an optimum level of disinfection of the root canal system chemo-mechanical preparation is a must.
3 HISTORY Prior to 1940’s Water was the most commonly used irrigant as it was: 1. Readily available. 2. Inexpensive. 3. Provided a lubricating effect during instrumentation.
4 ØDuring 1940’s proteolytic enzymes like streptokinase, streptodomase, papain, etc. were being used as irrigating solutions because of their tissue dissolving property. ØIn 1943, Grossman introduced the concept of using oxidizing agents as irrigants. ØIn 1945, Daniel formulated an irrigating solution comprising of a amino-acridine. ØIn 1970’s chelating agents were used increasingly because of their biologically acceptable properties.
5 IDEAL REQUIREMENTS • It should be an effective germicide and fungicide. • It should be non-irritating to the periapical tissues. • It should remain stable in solution. • It should have prolonged antimicrobial effect • It should be active in the presence of blood, serum and protein derivatives of tissues. • It should have low surface tension. • It should not interfere with repair of periapical tissues. • It should not stain tooth structure • It should not induce cell mediated immune response. • It should be capable of inactivation in a culture medium.
6 CATEGORIES OF USE That is conditions or situations for which intracanal medicaments have been advocated. • Elimination microorganisms. • Rendering contents of canal inert • Prevention or control of post treatment pain • Enhancing Anesthesia • Control of persistent periapical abscess
7 CLASSIFICATIONS A. According to DCNA 1. 2. 3. 4. 5. 6. 7. Phenolics - Eugenol - Camphorated monoparachlorophenol (CMCP) - Parachlorophenol (PCP) - Camphorated parachlorophenol (CPC) - Metacresylacetate (Cresatin) - Cresol - Creosote (Beechwood) - Thymol Aldehydes - Formocresol - Glutaraldehyde Halides - Sodium hypochlorite - Iodine - Potassium iodide Steroids Calcium hydroxide Antibiotics Combinations
8 B. According to Grossman 1. Essential oils - Eugenol 2. Phenolic compound - Phenol - Para chlorophenol - Camphorated para chlorophenol - Formocresol - Glutaraldehyde - Cresatin 3. Halogens - sodium hypochlorite - Iodides 4. Quaternary Ammonium compounds - 9 -amino acridine
9 INDIVIDUAL INTRACANAL MEDICAMENTS
10 Physiologic Saline From a biological stand point, sterile normal saline is the best irrigant to use because it causes. I. Least apical tissue irritation or damage. II. Biocompatible. III. Least amount of cell lysis.
11 Disadvantages: ØDoes not remove the smear layer. ØFlushes out some of the superficial debris from the root canal system. ØHas poor antibacterial properties. ØHowever irrigation followed by ultrasonic and sonic instrumentation have been reported to be almost as effective as 0. 5 to 2. 5% sodium hypochlorite irrigation in reducing the number of bacteria in infected root canals.
12 Phenol • It is the oldest compound for controlling microorganisms. • It was introduced by Lord Lister in 1867. • It is white crystalline substance, and has a characteristic odor derived from coal tar. • Phenol is a protoplasmic poison and produces necrosis of soft tissues by its ability to penetrate and disrupt the cell wall of bacteria and subsequently the protoplasm. • Liquefied phenol consists of 9 parts of phenol and 1 part water. • Highly effective in 1 to 2% concentration.
13 Camphorated Phenol • This contains 30% phenol, 60% camphor, 10% ethyl alcohol. • It is the least toxic of the phenolic compounds. • It has excellent antimicrobial effect and also relieves pain. • Camphorating process aims at developing a less caustic medicament as a result of the slow release of phenol. • Camphor serves as a vehicle and diluent.
14 Monochlorophenol (MCP) -It is a derivative of phenol and has three isomers of which paramonochlorophenol is the most effective. - Mono chlorophenol is more effective antiseptic and is also more toxic than phenol.
15 Camphorated Paramonochlorophenol (CMPCP) (Developed by Walkhoff 1891) - Contains : 35% monochlorophenol 65% camphor - Its antimicrobial effect is good. - Highly toxic to the tissues. - It is used in the form of vapor forming intracanal medicament. The vapors can pass through the apical foramen.
16 Formocresol Developed by BUCKLEY in 1906 Contents : 19% formaldehyde 35% cresol 46% water Glycerine. or is a combination of formalin and cresol in the proportion of 1: 2 ØFormocresol combines the protein - coagulating effect of phenolic compounds with the alkylating effect of formaldehyde. ØThe bactericidal effect of formocresol is good at levels as low as 2%.
17 ØIt is a strong poison and causes widespread destruction of living tissue followed by a persistent inflammatory reaction. ØStudies have reported that formocresol treated tissue produced a cell mediated immune response.
18 Glutaraldehyde -It is a colorless slightly soluble in H 2 O. -Slightly acidic -It is a strong disinfectant and fixative -Used in concentration of 2% - Extent of toxicity is less compared to formaldehyde. Its molecular weight is high compared to formaldehyde hence does not penetrate into the periapical tissues.
19 Glutaraldehyde was preferred to formaldehyde: ØIrreversible bonding with proteins. ØLimited diffusion into tooth structure. ØNo periapical irritation. ØAppears to cause a softening of dentin for limited duration, facilitating the mechanical preparation of the root canal. ØGreater reduction in microorganisms with glutaraldehyde 2% can be attributed to the fixative property rendering the microorganisms inert and nontoxic.
20 Cresatin ØAlso known as metacresylacetate ØIt is a clear, stable, oily liquid of low volatility. ØIt has both antiseptic and obtundant properties ØCompared to formocresol or camphorated parachlorophenol the antimicrobial effect of cresatin is less
21 Creosote ØIt is a mixture of phenol and phenol derivatives ØBeachwood creosote has long been used in endodontic therapy. ØThere are several reports on severe tissue irritation and necrosis
22 Alcohols ØEthyl alcohol and Isopropyl alcohol are used. ØThese denature protiens in high concentration. ØDenaturing takes place in presence of water, hence 70% is prefered to 95% ØThey are not recommended as intracanal medicament
23 Eugenol Ø It is the chemical essence of oil of clove. Ø It is related to phenol Ø It is both an antiseptic and an obtundant Ø It is slightly more irritating than oil of clove. ØStudies have reported that eugenol inhibited intradental nerve impulses Ø A few reports of allergy to eugenol have been reported.
24 Heavy metal salts ØSalts of silver, copper and mercury are used. ØThey coagulate protiens and act as enzyme inhibitors. ØThey are toxic. ØThe mercury salts are rendered less effective by the tissue fluid proteins present in the root canal. Hence they are not often used.
25 N 2 Contains : It ms Paraformaldehyde Phenylmercuric borate Eugenol. Additional ingredients like lead, corticosteroids, antibiotics. sealer and unusual antimicrobial properties have been denied by the council on Dental Therapeutics of the American Dental Association. week to 10 days.
26 SODIUM HYPOCHLORITE Is one of the most popular irrigating solutions. It has been used as an irrigant for well over 4 decades. ØIt was first recommended as an antiseptic solution by HENRY DAKIN in 1915 and was called as DAKIN’s SOLUTION during the time of World War-I (Na. OCl buffered with sodium bicarbonate). Ø 0. 5% Na. OCl solution was then used as a treatment for infected wounds.
27 Manufactured: It is made by bubbling chlorine gas through Na. OH to form equal amounts of sodium hypochlorite and sodium chloride (Na. OH gas Na. OCl + Na. Cl 2)
28 Properties of Na. OCl: ØAntibacterial action ØStrong dissolution property: Fresh tissue Necrotic tissue Fixed tissue ØLubricant – for effective instrumentation. ØBleaching action on discolored teeth. ØNa. OCl has been used in various concentrations ranging from 0. 5 -5. 25%. ØMost commonly used concentration – 2. 5%
29 ACTIONS: Antibacterial: Na. OCl exerts its antibacterial action either by: 1. Direct contact with microorganisms. 2. Vapour action. Destruction of the bacteria takes place in two phases: • Penetration into the bacterial cell. • Chemical combination with the protoplasm of the bacterial cell that destroys it.
30 ØSodium hypochlorite at 5. 25% is an extremely effective antimicrobial agent. ØStudies have shown that this solution will destroy most of the microorganisms found in the root-canal system after exposure of 1 minute or less.
31 FACTORS AFFECTING THE ANTIMICROBIAL PROPERTIES OF Na. OCl: • Diluting 5. 25% significantly. Na. OCl inhibits antimicrobial property • Bactericidal effectiveness of 5. 25% Na. OCl decreases over time. Martin suggested a storage shelf-life of 3 months for undiluted preparations. • The antimicrobial property may be achieved in a significantly lesser time by prewarming the solution (room temperature 22°Cbody temperature 37°C).
32 • It maintains a remarkable degree of antimicrobial activity in the presence of organic matter such as blood and serum albumin. ** Briseno (1992) and coworkers demonstrated that the irrigation of the root canal with 1% Na. OCl (manual) was more effective against the test organisms (E-edi + S. mutans) than irrigation of the root canal with 2% Na. OCl + ultrasound.
33 TISSUE SOLVENT PROPERTY ØNa. OCl possesses strong tissue dissolution property for fresh vital tissue, necrotic tissue and fixed tissues. This tissue dissolving capacity equals to that shown by H 2 SO 4 and HCl. ØThe solvent action of Na. OCl has been attributed to its high alkalinity. ØThe removal of organic tissue by Na. OCl is by the release of hypochlorous acid which reacts with insoluble proteins to form soluble polypeptides, aminoacids and other by products.
34 • Na. OCl – hypochlorus acid + insoluble proteins – soluble polypeptides, aminoacids and byproducts. • Grossman has shown that it can dissolve an entire pulp in 20 minutes to 2 hours. • 5. 25% of Na. OCl is capable of penetrating into the dentinal tubules and dissolving the contents of the tubules adjacent to the main canal.
35 Na. OCl and Smear layers Na. OCl alone is not very effective in removal of the smear layer, but when used in conjunction with other solutions or with ultrasonics it has shown to remove the smear layer effectively. Yamada and associates (2003) reported that a final flushing of 17% EDTA, followed by 10 ml of 5. 25% Na. OCl, was more effective in removing both inorganic and organic debris. These authors concluded, that flushing with a chelating agent removed the final calcific sludge that remained on the canal walls.
36 ØFlushing with 10 ml Na. OCl removed any remaining organic tissue, thus leaving patent dentinal tubules on the surface of the canal walls. Ø(Lengiz in 97) showed that the use of 0. 5% Na. OCl in combination with Ca(OH)2 preparation and ultrasonics in the root canal can effectively remove the smear layer. Also this is considered to be more safer than the use of Na. OCl solution is 5% concentration which is proved to be highly toxic.
37 TOXICITY OF Na. OCl TO PERIAPICAL TISSUE Causes: 1. Severe pain. 2. Edema. 3. Profuse haemorrhage both interstitially and through the tooth. This may be followed by (for several days) 1. Increasing edema. 2. Ecchymosis. 3. Tissue necrosis. 4. Parasthesia. 5. Secondary infection (rarely). Majority of cases, have shown complete resolution within a couple of weeks. In some cases they may be long-term parasthesia or scarring.
38 Treatment a) For immediate relief of pain – nerve block and L. A. b) Wet, cold, compress – continually applied to the face – for relief of pain and burning sensation and minimize swelling (for upto 6 hours). c) Analgesics – after emergency treatment. d) To control inflammation – corticosteroids immediately i. v. for 3 days. e) To prevent infection – antibiotics (1 wk). Heat packs and warm mouth rinse (after initial treatment). To improve circulation to the area.
39 ØAdvise the patient concerning the anticipated swelling and ecchymosis. ØGive the patient both verbal and written instructions. ØReassure the patient that he will regain his normal appearance within a short period.
40 HYDROGEN PEROXIDE 3% H 2 O 2 was recommended as a canal irrigant because of: a) Its effervescent action. b) Disinfecting properties.
41 ØEffervescent action was specially indicated in mandibular teeth where the bubbling of the peroxide was thought to lift debris from the canal system almost defying gravity. Ø H 2 O 2 does not possess tissue dissolution properties Not effective as a lubricant. Ø Hence, alternate use of H 2 O 2 + Na. OCl irrigating solutions was recommended by Grossman.
42 This alternate irrigation regimen during Chemo-mechanical preparation produces: a) Transient but energetic effervescence that mechanically forces out debris and microorganisms out of the canal. b) At the same time the O 2 that is liberated in an active state assists in destroying the anaerobic microorganisms. c) The permeability of dentinal tubules is increased allowing deeper penetration of intracanal medicament. d) Increases the bleaching action on discolored teeth.
43 CHELATING AGENTS ØAid in the mechanical enlargement of difficult root canals by softening the root canal dentin walls. ØEDTA – Ethylene diamine tetra-acetic acid composed by Disodium salt of EDTA distilled water 100 ml, 5 N Na. OH 4. 25 ml. ØThis was 1 st described for use in endodontics by Ostby.
44 Functions a) It has certain dentin dissolving effects desirable in all kinds of root canal therapy – ease in instrumentation. b) It reduced the time necessary for debridement and disinfection. c) It aided in enlarging narrow / obstructed canals. d) It helped make possible the bypassing of broken instruments in the canals. e) Removed the inorganic component of smear layer. f) Had no corrosive effects on the instruments.
45 Action The sodium salts of EDTA are capable of forming soluble non-ionic chelates with large number of metallic ions viz. calcium ions. Because EDTA would seek the calcium metal ion in the hydroxyapatite crystals of dentin in a chelate and thereby act to demineralize dentin and enamel. ü Ostby and associates found that EDTA decalcified dentin to a depth of 20 -30µm in 5 minutes. ü Franklin et al in 2004 reported that it is possible to overchelate a canal which can lead to perforation.
46 ØEDTA is known to remain active within the canal for 5 days. ØIf not inactivated the solution may seep into the periapical tissues and damage the bone. ØTherefore at the completion of appointment, the canal must be irrigated with Na. OCl.
47 RC Preparation It’s a combination of 17% EDTA + urea peroxide 10%, developed by Stewart and colleagues. Effective lubricating and cleaning agent. 1. It allows deeper penetration of the medicament into the dentin. 2. It is not water-soluble. 3. It is popularly used in combination with Na. OCl. 4. Because it is thought to produce a bubbling action helps loosen and float out dentinal debris.
48 Studies have shown RC preparation might affect the apical seal. Cook and associates in 1998 reported twice as much leakage in canals obturated with GP or silver cones following cleaning and shaping with RC preparation Na. OCl than with Na. OCl alone.
49 EDTA-c (commercial name) Quaternary ammonium compound to EDTA + Cetavlon which has greater germicidal acitivity and disinfecting properties. REDTA – A quaternary ammonium bromide + EDTA solution. To reduce the surface tension + increase the permeability of the solution.
50 SALVIZOL Another chelating agent is salvizol based on aminoquinaldinum diacetate. Properties: • It has surface acting property similar to quaternary ammonium groups. • Chelating action. • Organic debridement. • Bactericidal activity.
51 ORGANIC ACIDS The use of organic acid irrigants to irrigate and debride root canals is as old as root canal therapy itself. CITRIC ACID: Has been recommended as a canal irrigant because of its ability to demineralize and remove the smear layer effectively. 2 observations were made: • It acts as a chelating agent on dentine. • Therefore, it occurs naturally in the body, it is more acceptable biologically than other acids ((Jenkin and Dawer 1963).
52 The chelating action of citric acid softens the dentin and facilitates easy removal of the smear layer. CA has been used effectively in concentration of 10, 25 and 50% as RC irrigant. Disadvantages: C. A. may leave precipitated crystals (calcium and phosphate containing crystals) in the canal wall. Which may be a disadvantage. 1. Citric acid has been used in combination with Na. OCl to effectively clean the R. C. 2. C. A. removes smear layer better than many acids like poly acrylic acid, lactic acid and phosphoric acid.
53 TANNIC ACID Tannic acid is another cleansing agent for root canal preparation was suggested by Graham Mount. It has been extensively used in the treatment of burns (more than 100 years old). Action: It acts as a surface coagulant by precipitating proteins. *Studies have shown that the use of tannic acid in the root canal as an irrigant cleansed the canal more effectively than the conventional combination of Na. OCl + H 2 O 2.
54 CHLORHEXIDINE GLUCONATE Chlorhexidine has become recognized as an effective antimicrobial agent and its use as a potential endodontic irrigant has been demonstrated in the last decade. Recently, it has been accepted as a root canal irrigant in endodontics. Advantages: • Has a broad spectrum antimicrobial action. • Relative absence of toxicity. Disadvantage – it is not known to possess a tissue dissolving property.
55 Structure is a symmetrical cationic molecule consisting of: 4 -chlorophenyl rings and 2 biguanide groups Connected by a central hexamethylene chain Specturm of activity Chlorhexidine is bactericidal and effective against gram +ve, gram-ve, yeast, Candida albicans.
56 Action: Acts by adsorbing into the cell wall of the microorganisms and causing leakage of the intracellular components. At low concentration has bacteriostatic effect. At higher concentration, chlorhexidine is bactericidal because of precipitation or coagulation of the cytoplasm caused by protein cross linking. The bacteriostatic effect of chlorhexidine is considered to be more effective. The bound chlorhexidine molecule is slowly released for upto 24 hours, as the concentration decrease.
57 According to Klimn et al When used as an intra canal irrigant in the endodontic treatment for periapical lesions: • Clinical relief of symptoms. • Sterility. • Reduction in the size of periapical lesions. All at a mean follow up of 24 months. In another study (O hara et al) showed that chlorhexidine was the most efficient antibacterial agent when compared to 3% H 2 O 2, 5. 25% Na. OCl, saline REDTA 17%.
58 Iodides : mild effect on living tissue. loosely bound manner so its penetration is not impeded. 94% distilled water has excellent antimicrobial activity and minimal toxicity and tissue irritating qualities.
59 Cationic detergents tension and good cleansing effect. The antimicrobial effect of these compounds are not strong. positevely charged and the microorganisms are negatively charged. Thus a surface active effect results in which the compound clings to the microorganism and reverses the charge. These compounds may delay wound healing he centrations -These compounds inused between are 0. 1 to 1% for root canal irrigation, but rarely as intracanal dressings root canal instrumentation It has chelating effect Salvizol causes some degree of tissue irritation
60 9 -AMINOACRIDINE • • The efficacy of 9 -aminoacridine has been reviewed by Schmitz. Properties: 1. Antibacterial action. 2. Low toxicity. 3. Osteogenic potential. Disadvantage: Not a chelator. Not a tissue solvent. It use is not widespread.
61 Mechanism of action: Disruption of cellular metabolic pathways of microorganisms: -Inhibition of cells, protein synthesis. -Inhibition of DNA synthesis. Use: a) Management of endodontically involved teeth with large periapical abscess. b) Recommended as pressure irrigation of the periapical tissues via the canals. c) The drug may be sealed in the canal as an interim medication ( low inflammatory potential)
62 Glyoxide is an irrigation solution i. e. comprised of 10% urea peroxide (Carbamide peroxide) in a vehicle of anhydrous glycerol. Use: • Narrow and curved canals where slippery effect of glycerol is maximized for instrumentation.
63 Action: a) Antibacterial activity that is more potent than 3% H 2 O 2. b) Enhances root canal lubrication without softening the dentin. (less chance of root perforation) a) It is less toxic to periapical tissues than Na. OCl. b) It also has greater solvent action than 3% H 2 O 2.
64 DOXYCYCLINE HYDROCHLORIDE A hydroxy derivative of tetracycline. It is the most potent anticollagenase antibiotic among commercially available tetracyclines. Advantages: a) The dentin surface is capable of acting as a reservoir by adsorbing and slowly releasing antibacterial levels of doxycycline into the adjacent environment for several days following topical applications of this antibiotic solutions. b) Inhibit extracellular collagenase activity and bone resorption.
65 Metronidazole ØAntibiotic spectrum confined solely to obligate anaerobes. ØActive against bacteroides, porphyromonas fusibacterium, clostridium and peptococci and peptostreptococci. Barnett and Tronstad in 2002 reported the successful use of metranidazole in controlling infections by bacterioides spp and pseudomonas spp colonized at root ends of endodontically treated teeth that had failed to heal and remained refractory to all other treatment.
66 Adverse reactions: 1. Nausea. 2. Headache. 3. Metallic taste. 4. Xerostomia.
67 Calcium hydroxide ØHermann introduced Ca(OH)2 paste as an intra canal medicament in 1920. ØThick suspension of Ca(OH)2 powder in sterile water or saline. ØThe high p. H of calcium hydroxide paste is responsible for the destructive effect on bacterial cell membranes and protein structures. ØAid directly or indirectly in the dissolution of necrotic pulp tissue. Tissue submerged in Ca(OH)2 for a day is more easily dissolved with Na. OCl than is untreated tissue. Bystrom et al showed that Ca(OH)2 paste effectively eliminated all microorganisms in infected root canals when the dressing was maintained for 4 weeks.
68 Mode of application : Ø The paste is introduced into the root canal with a lentulo spiral, dried with coarse absorbent points and packed with appropriately sized root canal pluggers. ØTemporary cement is then placed for an effective seal.
69 Antibiotics ØAntibiotics are indicated in a small minority of cases when root canal infection persists despite other antiseptics. ØLadermix paste or polyantibiotic paste (PBSC) are used
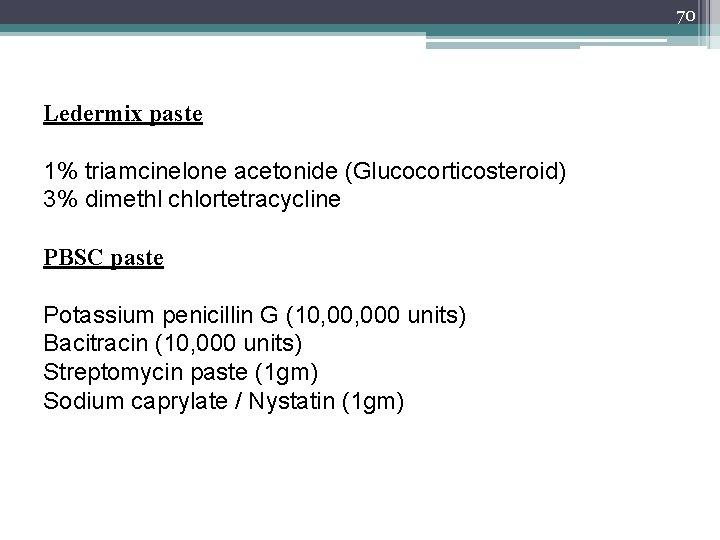
70 Ledermix paste 1% triamcinelone acetonide (Glucocorticosteroid) 3% dimethl chlortetracycline PBSC paste Potassium penicillin G (10, 000 units) Bacitracin (10, 000 units) Streptomycin paste (1 gm) Sodium caprylate / Nystatin (1 gm)
71 Conclusion ØDebridement of the root canal systems is essential for a predictably successful endodontic treatment. ØThe identification and elimination of bacteria, removed of other necrotic products from the canal with appropriate irrigating solutions with proper technique ensures definite fulfillment of one of the objectives of root canal therapy.
 Silver point dental
Silver point dental Cmcp intracanal medicament
Cmcp intracanal medicament Dragonal médicaments
Dragonal médicaments Nilesh samani
Nilesh samani Himanshu deshpande
Himanshu deshpande Anand deshpande house
Anand deshpande house Nilesh gambhava
Nilesh gambhava Pooja harekoppa
Pooja harekoppa Shirish deshpande mumbai grahak panchayat
Shirish deshpande mumbai grahak panchayat General counsel legal department structure chart
General counsel legal department structure chart Virginia department of historical resources
Virginia department of historical resources Oklahoma department of career and technology education
Oklahoma department of career and technology education Altaeros bat
Altaeros bat Edenton recreation department
Edenton recreation department Hse department organization chart
Hse department organization chart Ponzi scheme vs pyramid scheme
Ponzi scheme vs pyramid scheme Flagler hospital billing
Flagler hospital billing National audit department
National audit department Support department adalah
Support department adalah Department of homeland security minnesota
Department of homeland security minnesota Department of us
Department of us East syracuse police department
East syracuse police department Cern edh
Cern edh Department of work and pensions
Department of work and pensions Based department
Based department Pakistan metrology department
Pakistan metrology department Front office department responsibilities
Front office department responsibilities Samsung business structure
Samsung business structure Miami dade county internal services department
Miami dade county internal services department Michigan department of education teacher certification
Michigan department of education teacher certification Department of veterans affairs office
Department of veterans affairs office Calhr 752
Calhr 752 Sierra madre planning department
Sierra madre planning department Wisconsin department
Wisconsin department Virtual enterprises international
Virtual enterprises international Education and literacy department sindh
Education and literacy department sindh Central islip fire dept
Central islip fire dept Femur borders
Femur borders Vermont department of health
Vermont department of health Department of local affairs
Department of local affairs Several leveled flowchart adalah
Several leveled flowchart adalah Retail institutions by store-based strategy mix
Retail institutions by store-based strategy mix Objectives of customer satisfaction
Objectives of customer satisfaction Department of transportation
Department of transportation Tum
Tum Ohio department of taxation morse road
Ohio department of taxation morse road Department strategy
Department strategy Fishers health department
Fishers health department Bucket check in hotel
Bucket check in hotel Pakistan meteorological department satellite images
Pakistan meteorological department satellite images What is job zone
What is job zone Accounting department workflow
Accounting department workflow Cern hr department
Cern hr department Department of electronics & information technology
Department of electronics & information technology Athletic department budget presentation
Athletic department budget presentation Bulloch county bus garage
Bulloch county bus garage Www.fldoe.org login
Www.fldoe.org login Animal quarantine and certification service
Animal quarantine and certification service Banquet department in hotel
Banquet department in hotel Department of labor and training
Department of labor and training Nyc department of youth
Nyc department of youth Pfizer human resources department
Pfizer human resources department Department tf
Department tf State of texas emergency assistance registry
State of texas emergency assistance registry Operational planning is also known as
Operational planning is also known as Guthrie health department
Guthrie health department Physics 121 njit
Physics 121 njit It department
It department Eacademics iitd student login
Eacademics iitd student login Deped order no. 30 s. 2019
Deped order no. 30 s. 2019 Indiana department revenue
Indiana department revenue Das honigkuchenherz
Das honigkuchenherz