1 1 2 hapter 193 1 Non syndromic



- Slides: 65

1 1
2 hapter 193: 1 Non syndromic Craniosynostosis Introduction and Single-Suture Synostosis Farzad zallaghi january 2018
3 1 bone growth in the skull occurred primarily at suture lines and that when this growth site was prematurely bridged with bone, an abnormal skull shape developed. This was characterized by the skull’s growth in a plane perpendicular to the plane of the fused suture
4 1 Growth restriction occurred at the closed suture, and compensatory growth occurred elsewhere in the skull to accommodate the growing brain
5 1 Premature fusion of calvarial sutures 1 in 2500 live births Nonsyndromic type: The more common variant Often had single-suture synostosis Without other abnormalities Syndromic type: Often had multiple sutures fused Other associated skeletal abnormalities Strong family history Genetic abnormalities based on the autosomal dominant
6 1 NONSYNDROMIC CRANIOSYNOSTOSIS Ø 85% of cases of craniosynostosis Ø The most commonly affected is the sagittal suture, followed by the unilateral coronal, bilateral coronal, metopic, and lambdoid sutures. Ø Cranial vault suture, not cranial base, pathology is of primary importance in the development of skull shape pathology in nonsyndromic craniosynostosis. Ø Preoperative and postoperative computed tomography (CT) shows that surgical treatment of the cranial vault alone results in improvement of not only cranial vault but also cranial base pathology
7 1 DIAGNOSIS: Non syndromic craniosynostosis involving a single vault suture is ordinarily diagnosed by the observation of a typically deformed skull shape, with radiographs serving as confirmatory evidence.
8 1
9 1
10 1
11 1
12 1
13 1
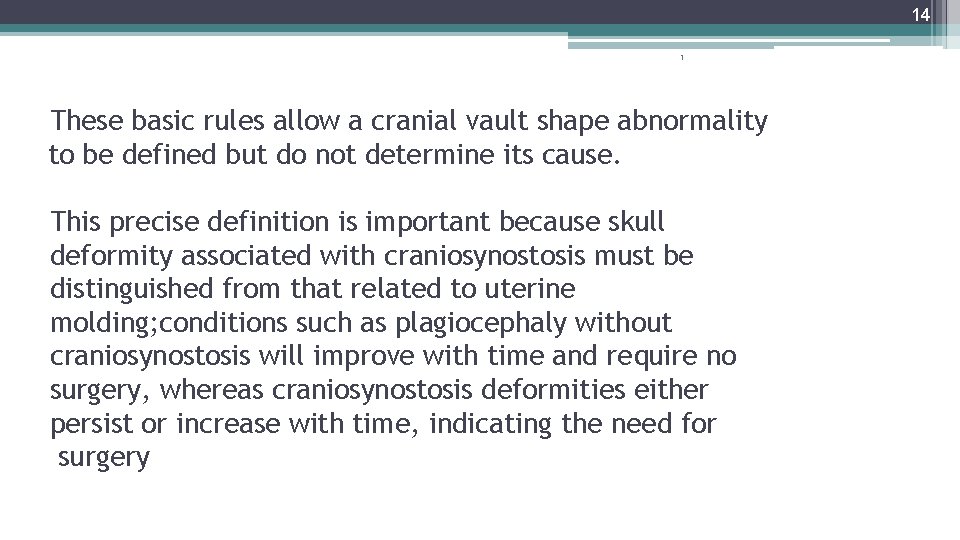
14 1 These basic rules allow a cranial vault shape abnormality to be defined but do not determine its cause. This precise definition is important because skull deformity associated with craniosynostosis must be distinguished from that related to uterine molding; conditions such as plagiocephaly without craniosynostosis will improve with time and require no surgery, whereas craniosynostosis deformities either persist or increase with time, indicating the need for surgery
15 1 There is controversy regarding the advisability of CT scans in patients being evaluated for craniosynostosis. It has been reported that CT scans performed early in infancy are associated with an increased likelihood of malignancy later in life
16 1 A recent prospective multicenter study demonstrated that a correct diagnosis of craniosynostosis could be derived as accurately by simple physical examination as by CT scan. Nevertheless, there remains a role for advanced imaging when the diagnosis of craniosynostosis is in doubt, for preoperative planning (particularly venous imaging for patients who will undergo occipital remodeling),
17 1 OPERATIVE TIMING AND APPROACHES ØA common question asked by parents is whether the condition is progressive? ØMore significant degrees of improvement were noted in some patients who underwent surgery when younger than 6 months. ØLimited craniectomy procedures of few sutures appear to be beneficial in very young patients with mild deformities,
18 1 The endoscopic approach has wide appeal in the treatment of craniosynostosis, particularly for patients’ families, owing to the limited scar, brevity of surgery, shortened hospital stay, decreased rate of blood loss and transfusion, and potentially minimally invasive operative intervention. Endoscopic strip craniectomy procedures have not yielded consistently good skull forms, even when supported by postoperative skull-molding helmets
19 1 ETIOLOGY OF NEUROCOGNTIVE DISABILITIES Ø There are several hypothetical mechanisms by which craniosynostosis might affect brain development adversely: global intracranial hypertension, focal brain hypoperfusion, mechanical deformation of neuroanatomic structures Ø Inverse correlation between preoperative ICP and DQ or IQ. Ø Chronic elevations in ICP may lead to ophthalmologic deficits and perhaps headaches, but the impact on cognition has not been established.
20 Diagnosis of elevated ICP 1 ØElevated ICP was recorded in : - 8% of cases of sagittal synostosis, - 6% of metopic synostosis, - 12% of unilateral coronal synostosis, - more prevalent in patients with multiple suture involvement and among syndromic cases. . Øfunduscopic examination has a high specificity in all age groups but does not have a high sensitivity until children are older than 8 years.
21 1 EFFECT OF SURGICAL TECHNIQUE AND TIMING there has been increasing confusion about what is the optimal management of infants with isolated nonsyndromic craniosynostosis. The priorities in care, in thetreatment of these children, relate primarily to two factors: 1. intellectual function 2. skull shape
22 1 ØThe children operated on before 6 months of age did better neurologically than those operated on after 6 months of age. ØEarly surgery (i. e. , <6 months of age) with a more comprehensive approach yielded a better neurological outcome than strip craniectomy (endoscopic or otherwise) before 3 months of age. ØCranioplasty is recommended between 4 and 6 months of age (typically closer to 6 months), depending on the weight and health of the child. ØRegardless of surgica. L technique or timing of surgery Children with single-suture craniosynostosis have a higher incidence of learning disabilities than the normal population.
23 1 OPERATIVE TREATMENT
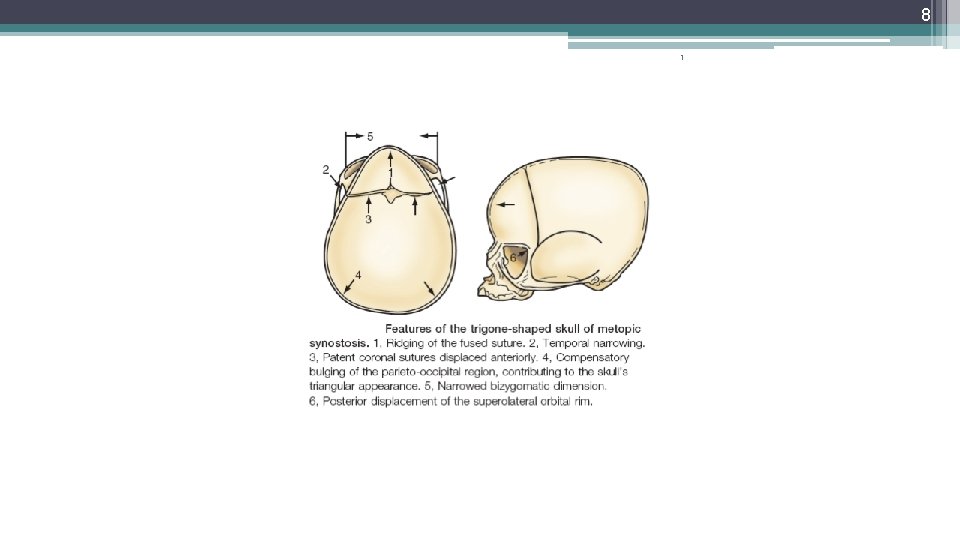
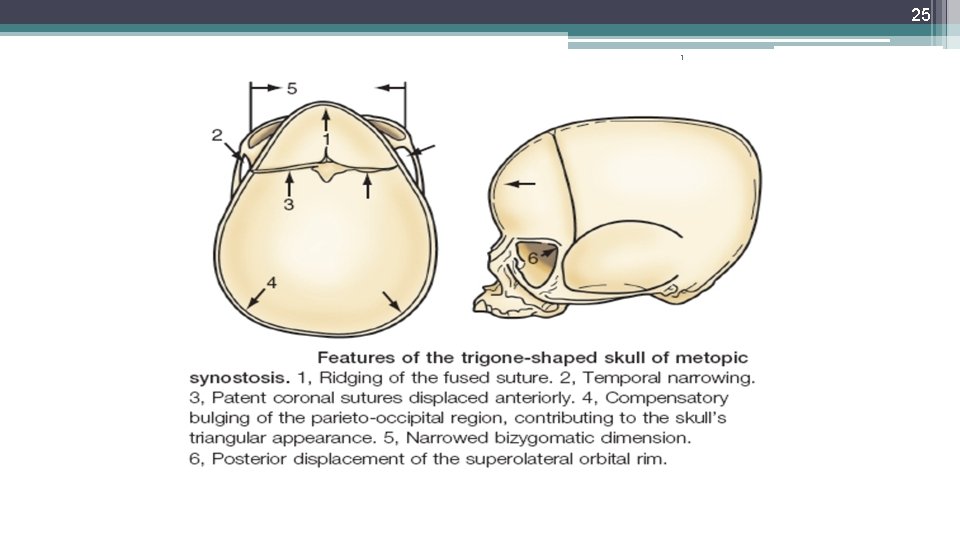
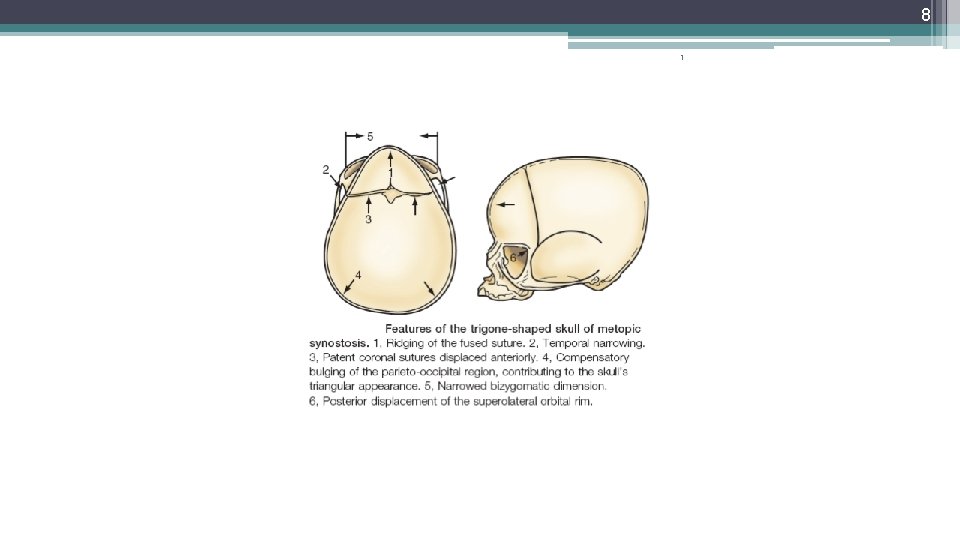
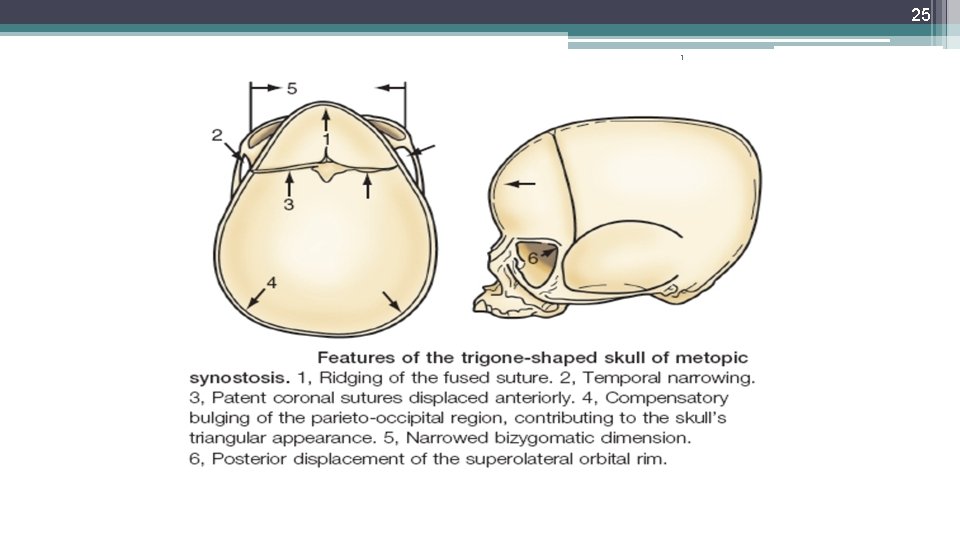
24 Metopic Synostosis: 1 1 -metopic suture ridging 2 -bilateral flattening of the frontal bones 3 -anterior displacement of the coronal sutures 4 -lateral flaring of the posterior parietal regions 5 -Hypotelorism 6 -flattening of the supraorbital ridges stic triangular shape known as trigonocephaly.
25 1
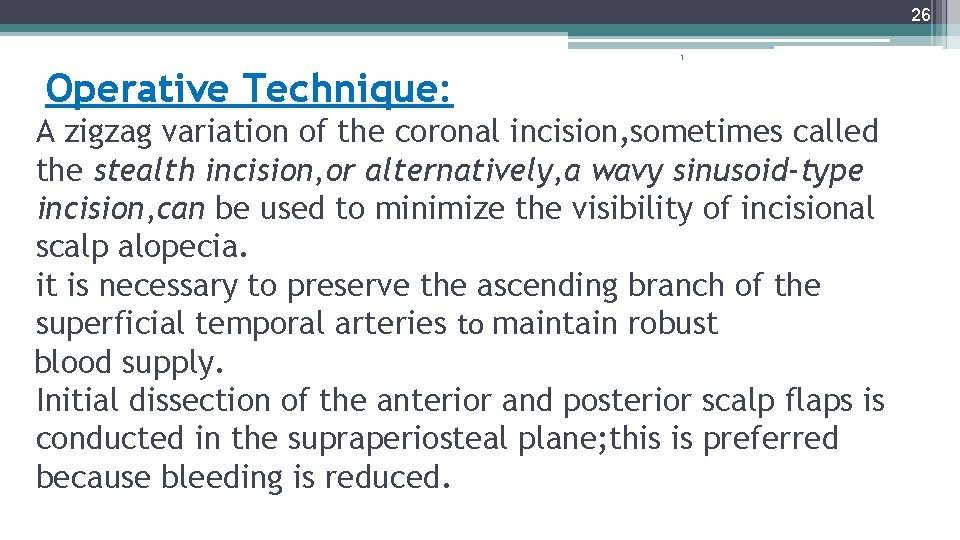
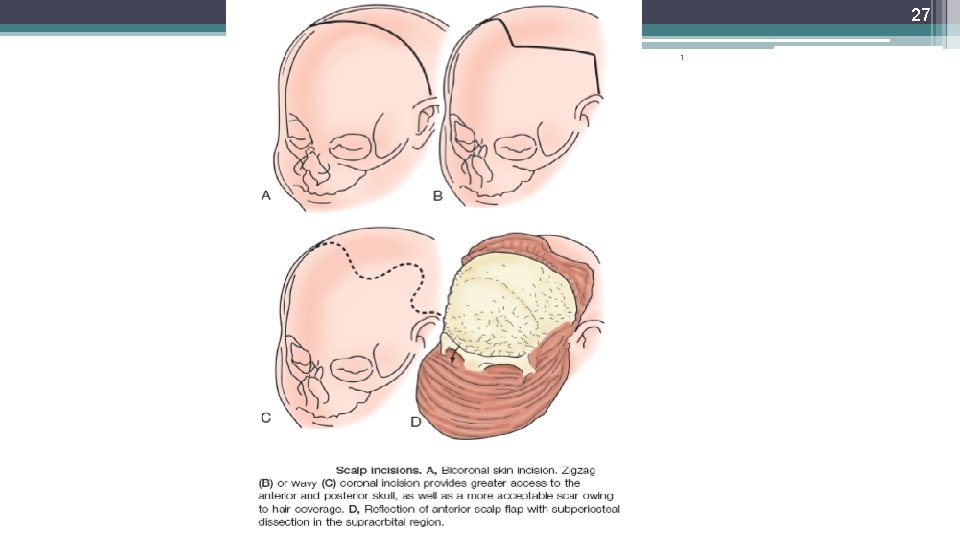
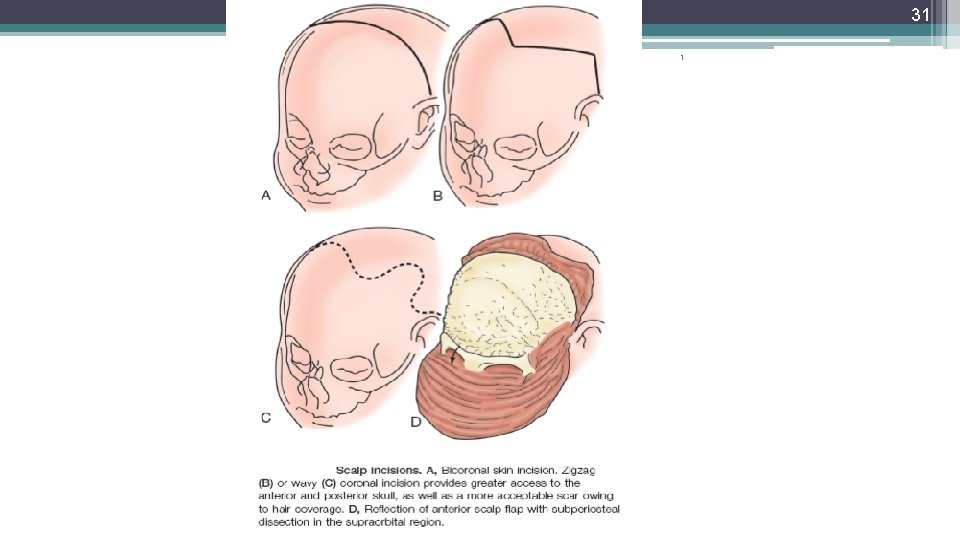
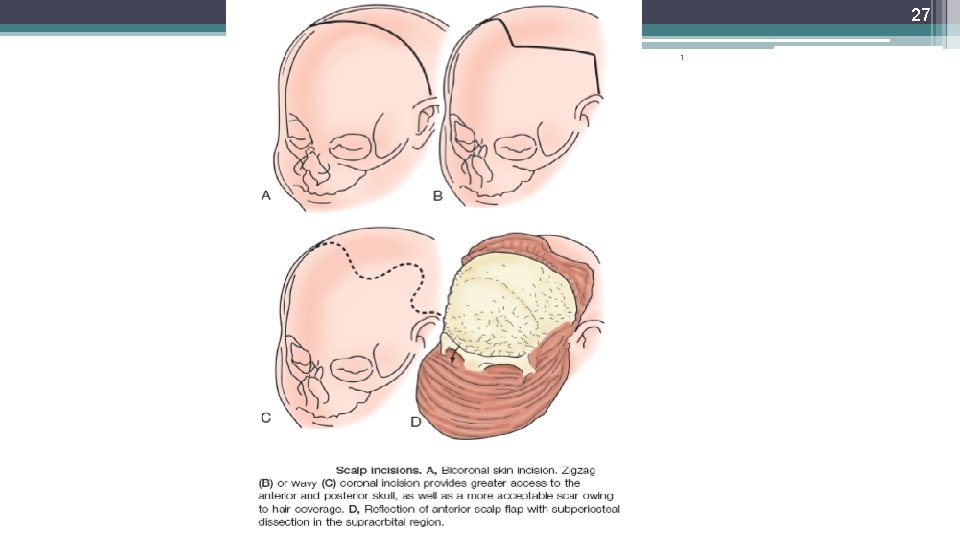
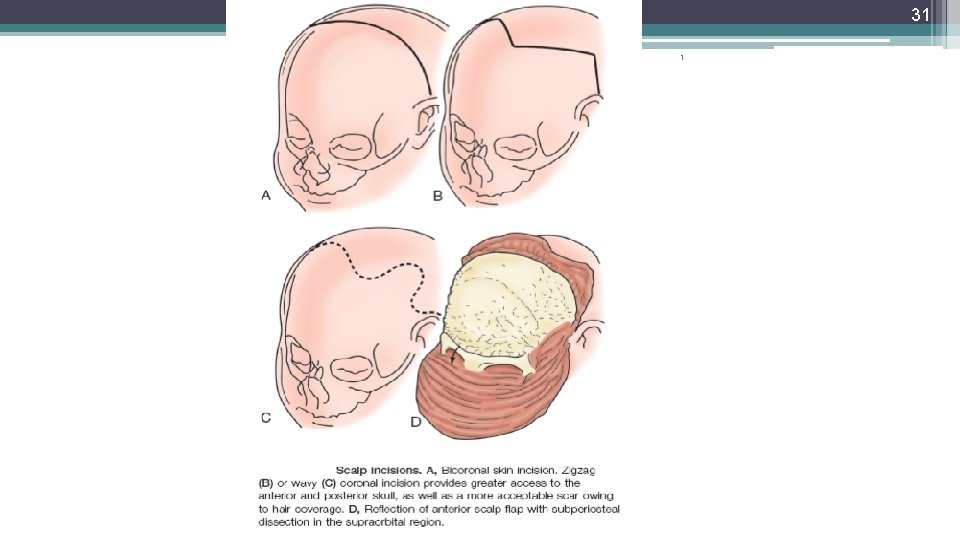
26 1 Operative Technique: A zigzag variation of the coronal incision, sometimes called the stealth incision, or alternatively, a wavy sinusoid-type incision, can be used to minimize the visibility of incisional scalp alopecia. it is necessary to preserve the ascending branch of the superficial temporal arteries to maintain robust blood supply. Initial dissection of the anterior and posterior scalp flaps is conducted in the supraperiosteal plane; this is preferred because bleeding is reduced.
27 1


29 1
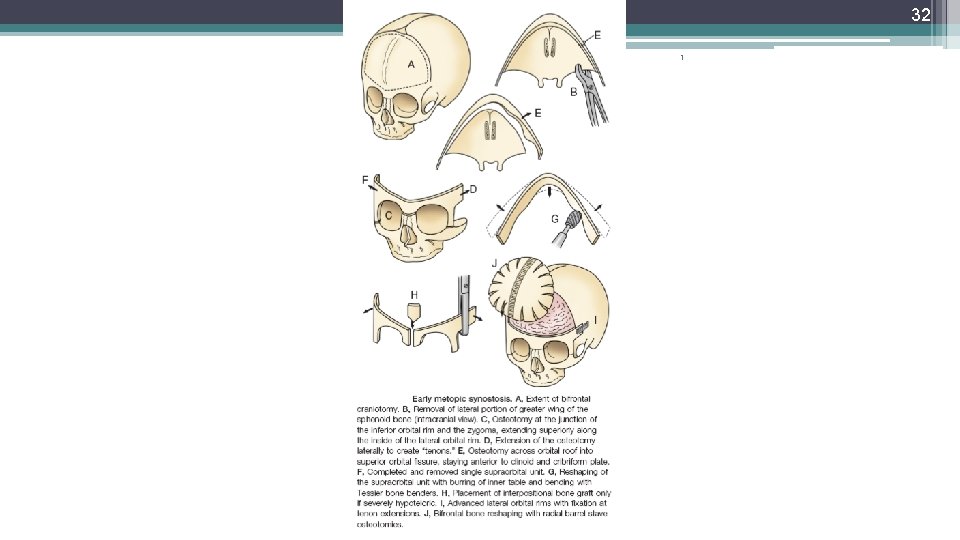
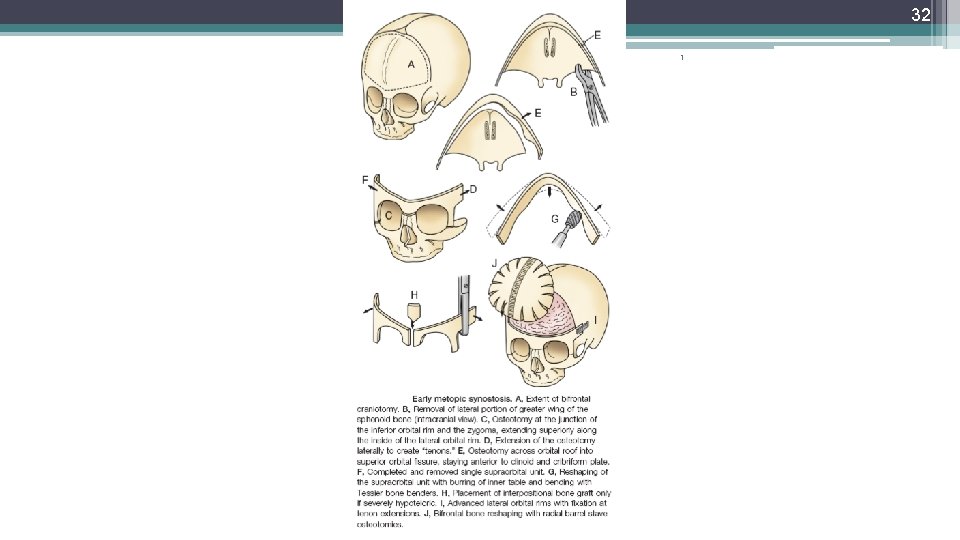
30 1 A bifrontal craniotomy is performed, the posterior extent of which is determined at the point where the narrowing deformity of the skull is first noted. The lateral portions of the sphenoid wings are removed to allow unimpeded brain expansion and to provide greater access to the middle cranial fossa during the orbital osteotomies.
31 1
32 1
33 1 The frontal bone is fixed with a combination of absorbable plates and screws and sutures to the adjoining bones, and the scalp flap is then replaced and closed in layers. No suction drains are used to avoid a cerebrospinal fluid siphoning effect, in which there is a continuous cerebrospinal fluid leak from superficial microabrasions of the underlying dura during the craniotomies.
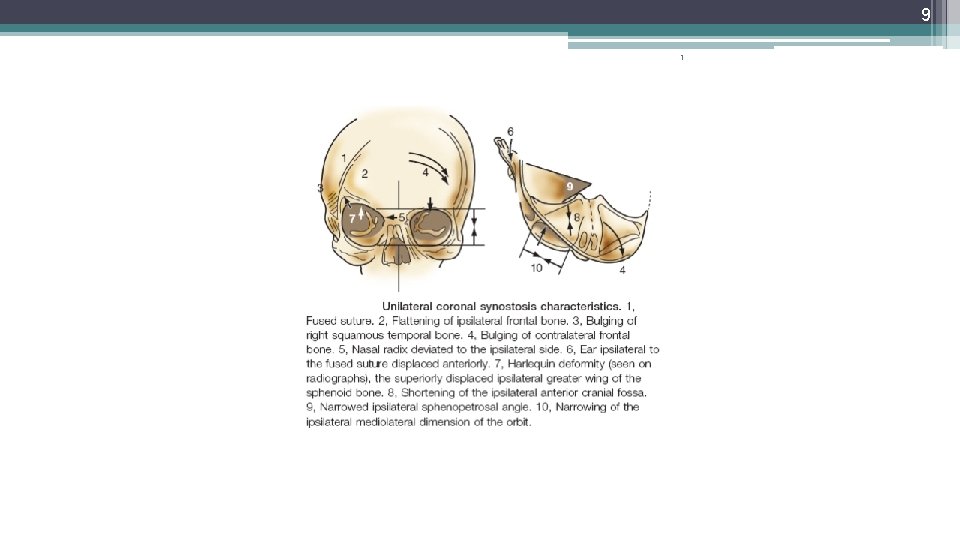
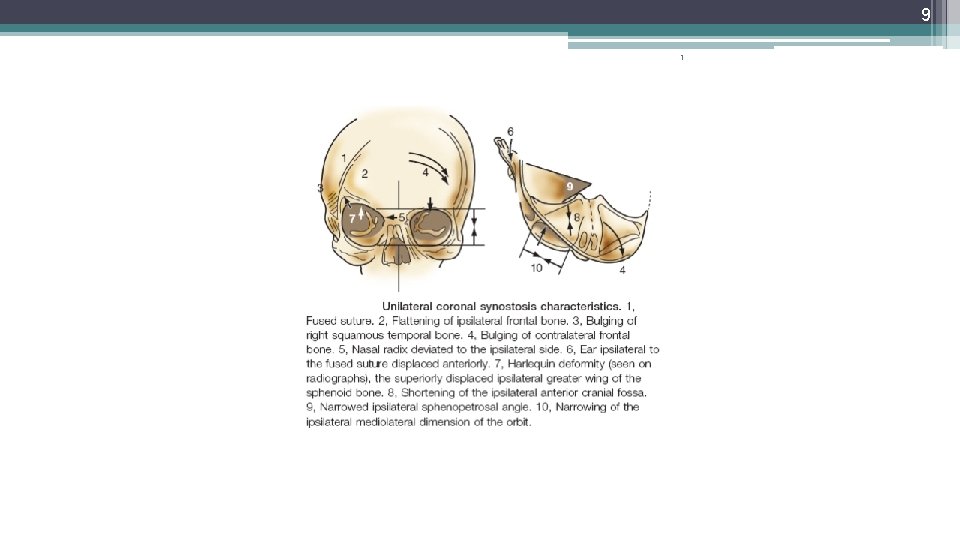
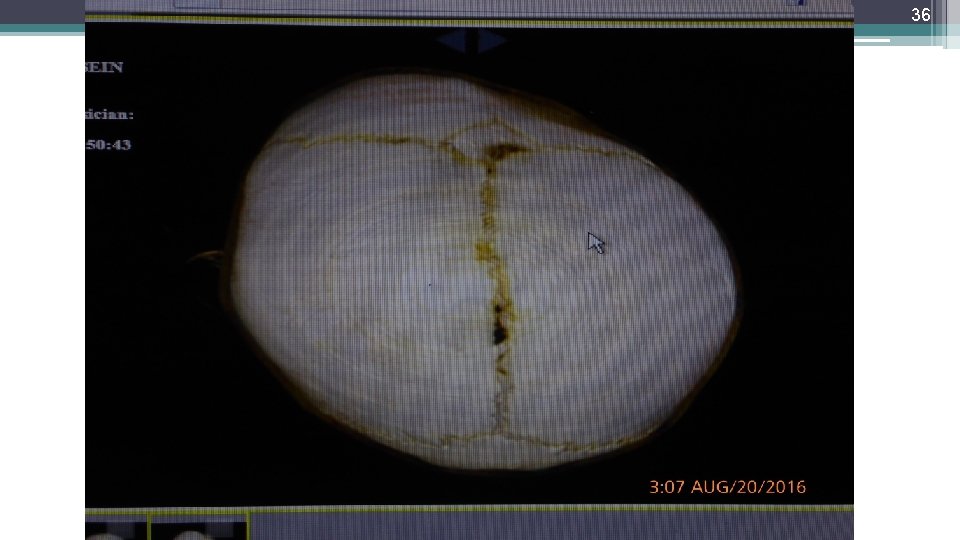
34 Unilateral Coronal Synostosis: 1_ridging of the prematurely fused half of the coronal suture 1 2_flattening of the ipsilateral frontal and parietal bones 3_bulging of the ipsilateral squamous portion of the temporal bone 4_bulging of the contralateral frontal and parietal bones 5_The bony orbit on the affected side is significantly distorted
35 1 6_ Nasal radix deviated to the ipsilateral side. 7_ Ear ipsilateral to the fused suture displaced anteriorly. 8_Harlequin deformity(seen on radiographs)the superiorly displaced ipsilateral greater wing of the sphenoid bone. 9_Shortening of the ipsilateral anterior cranial fossa. 10_ Narrowed ipsilateral sphenopetrosal angle.
36 1
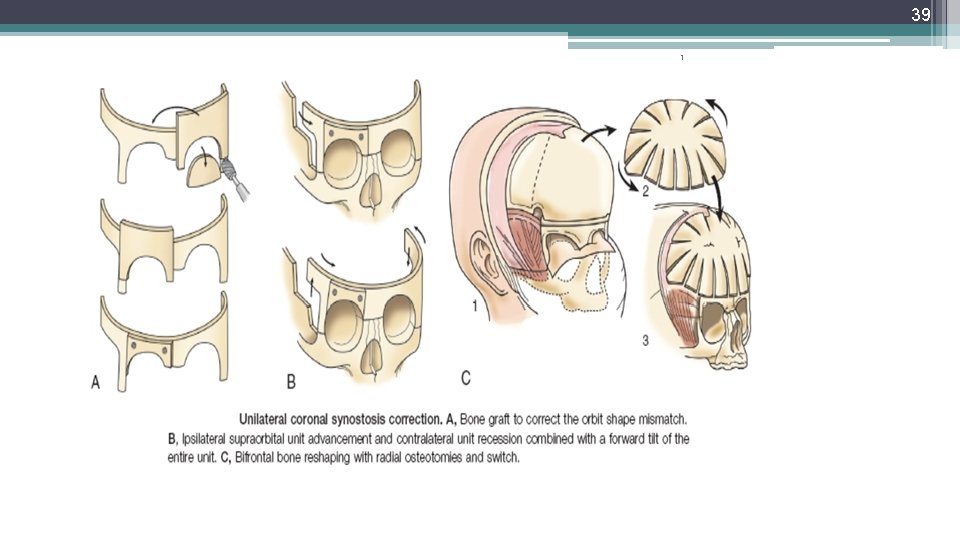
37 1 Operative Technique: The patient is placed in a supine position, and a modified zigzag(occipital or coronal)or wavy line coronal incision is carried out. The anterior scalp flap is dissected in the supraperiosteal plane to approximately 2 cm above the superior orbital rims.
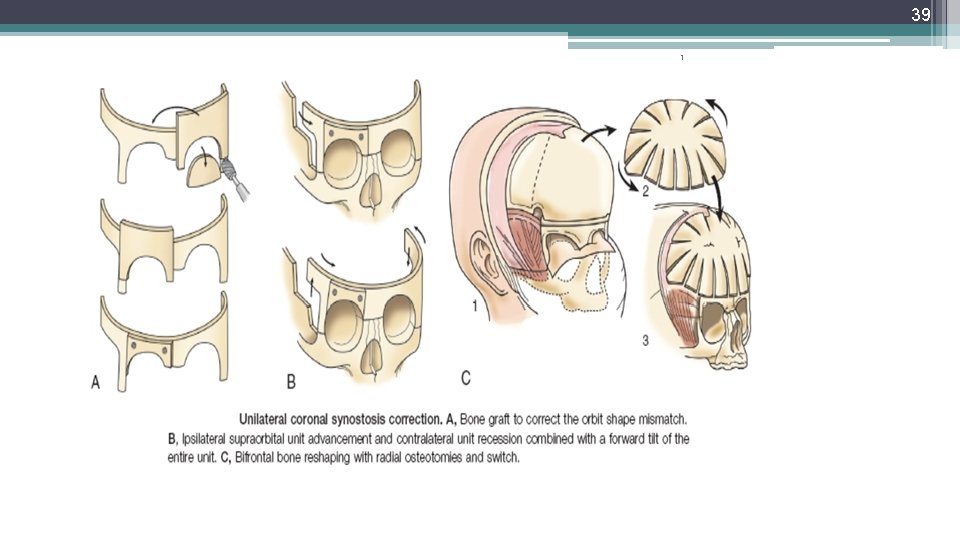
38 1 A bifrontal craniotomy is performed with the posterior extent of the cuts posterior to both the fused and nonfused coronal sutures. Similar cuts are performed to separate the bilateral supraorbital units, as was done with metopic synostosis
39 1
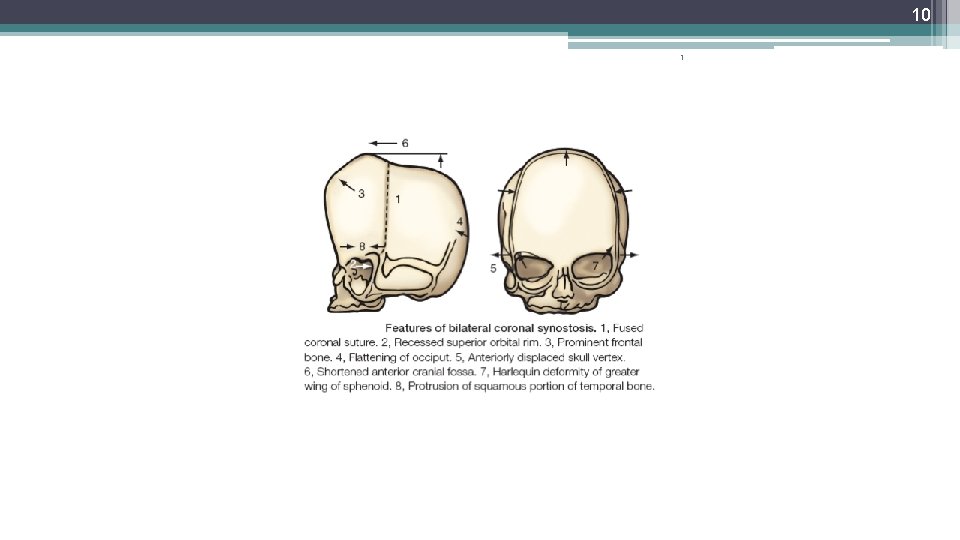
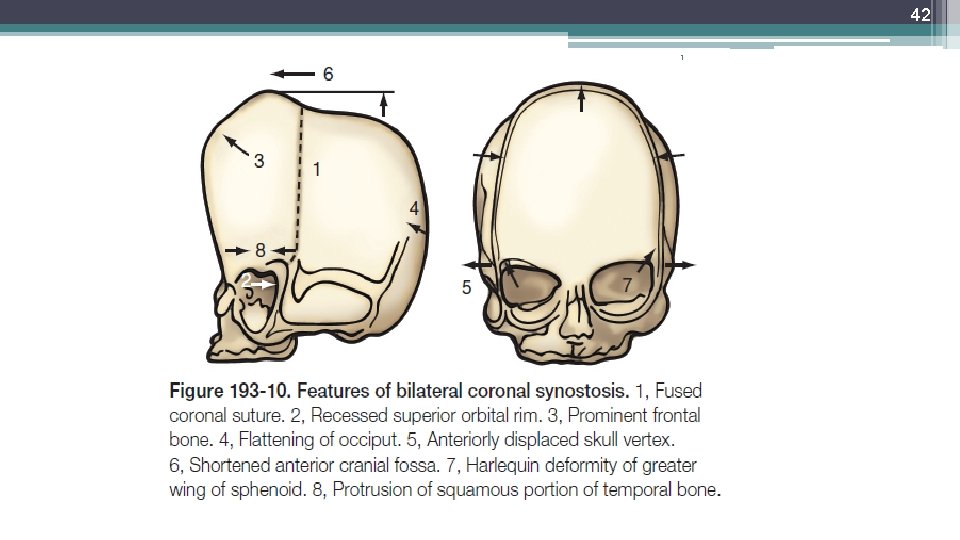
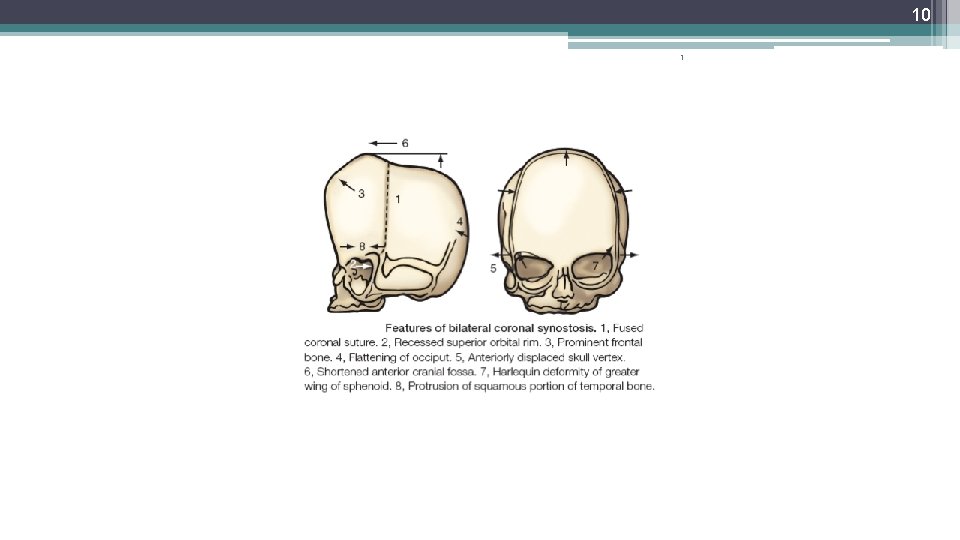
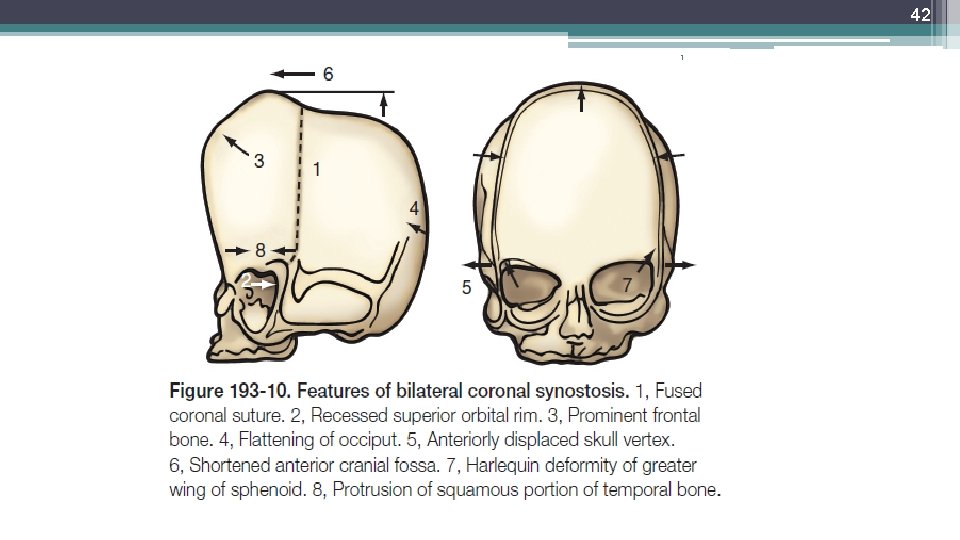
40 1 Bilateral Coronal Synostosis: 1. Fused coronal suture. 2. Recessed superior orbital rim. 3. Prominent frontal bone. 4. Flattening of occiput. 5. Anteriorly displaced skull vertex. 6. Shortened anterior cranial fossa. 7. Harlequin deformity of greater wing of sphenoid. 8. Protrusion of squamous portion of temporal bone
41 1 This characteristic head shape is referred to as turribrachycephaly to describe the excessive vertical height, increased overall width, and often severely truncated anteroposterior dimension of the skull
42 1
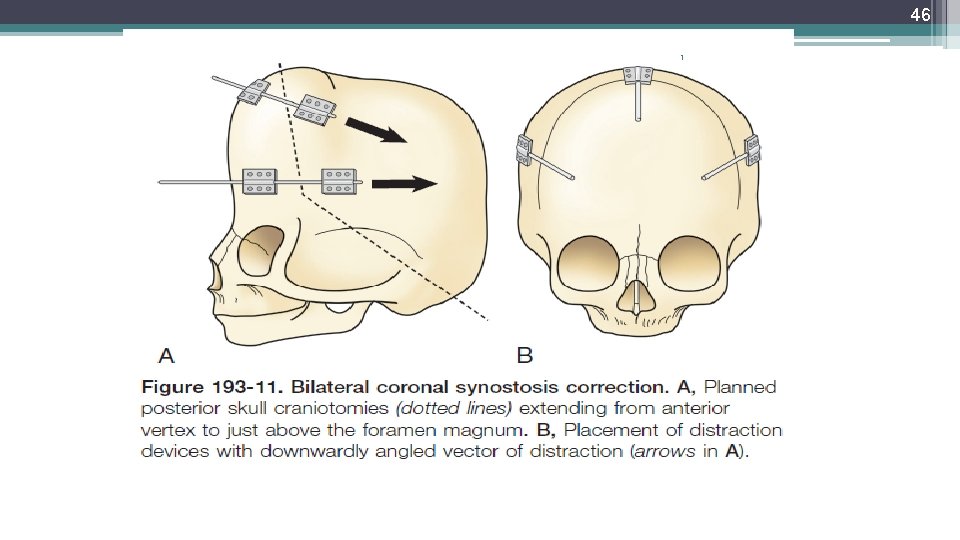
43 1 Operative Technique: Because the abnormalities of coronal synostosis are situated both anteriorly and posteriorly within the skull, a different approach to the surgical correction is indicated. A two-stage approach should be selected, with first addressing the posterior skull deformity followed at a later time by the second addressing the anterior deformity.
44 1 In the first stage, a posterior skull craniotomy is performed and distraction osteogenesis is employed A standard coronal incision(zigzag or wavy)is performed, and posterior supraperiosteal dissection is carried out.
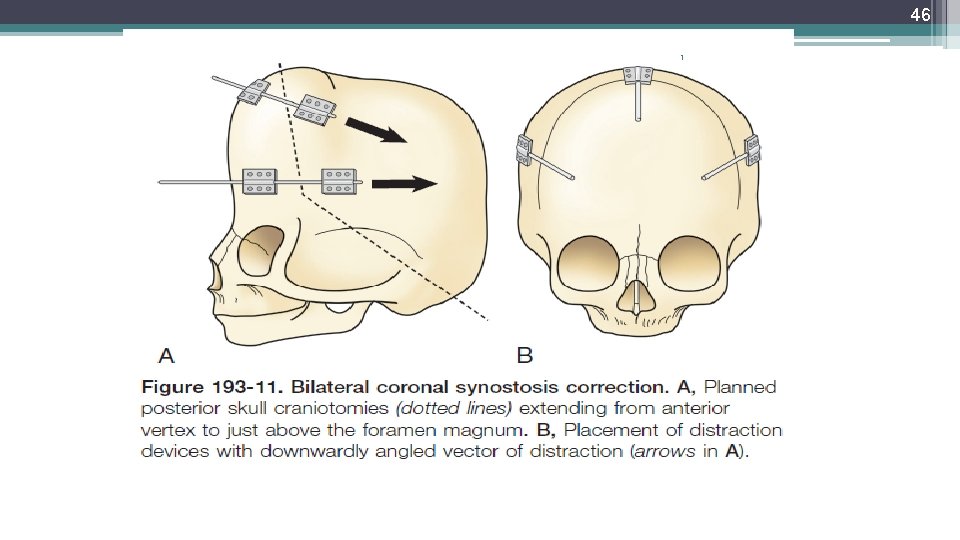
45 1 After the full extent of the posterior deformity is exposed, craniotomies are carefully planned starting superiorly just anterior to the highest point of the vertex, then running laterally along the widest portion of the skull where the temporal bone is most prominent, and finally angling posteriorly and inferiorly as low as possible staying 1 to 2 cm above the foramen magnum
46 1
47 1 After these cuts are completed, the external distraction devices are placed. Usually, three are needed to create the necessary stability for a posteriorly directed vector and to prevent unintended canting of the bone segment during the distraction. Two devices are placed laterally and one superiorly.
48 1 The distraction protocol is the standard one, with a latency period of 1 to 2 days, followed by active distraction at a rate of 1 mm per day, until a noticeable reduction in the vertex has occurred.
49 1 After the distraction and consolidation period have been completed, the patient is then brought back to the operating room for a standard fronto-orbital advancement in a manner similar to the unicoronal synostotic skull, and the anterior skull is then reshaped and reconstructed with simultaneous supraorbital advancement.
50 In bilateral coronal synostosis, the occipital cranioplasty may be done in the supine position or in the modified prone positition some limitations exist related to its effectiveness 1. if a ventriculoperitoneal shunt is in place 1 2. in syndromic patients if a tracheostomy is in place 3. redo cranioplasty 4. syndromic cases with large posterior venous sinus anomalies or prominent Arnold-Chiari malformation
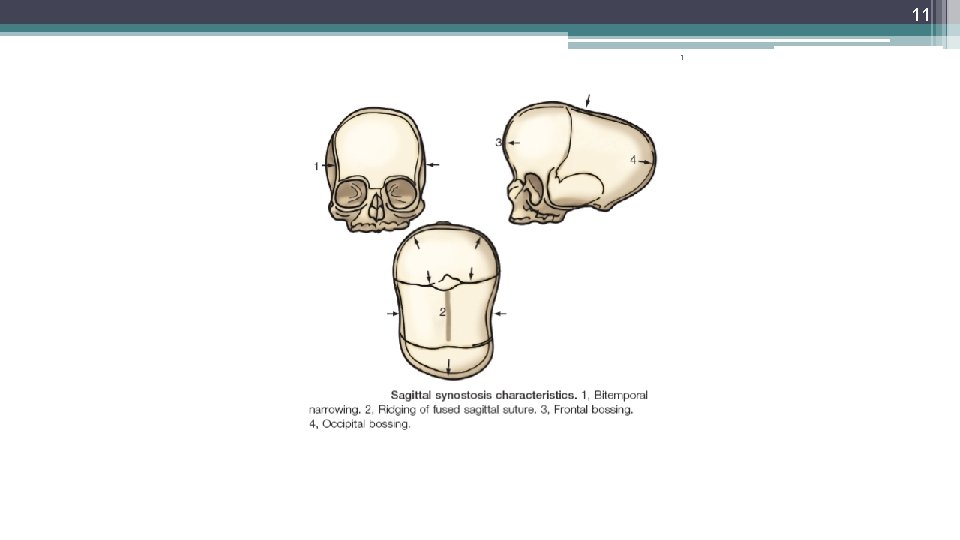
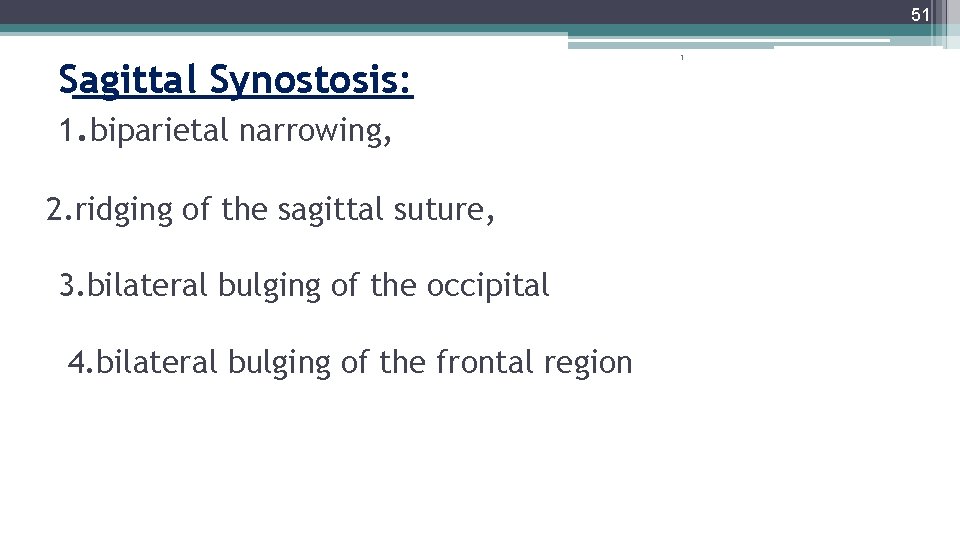
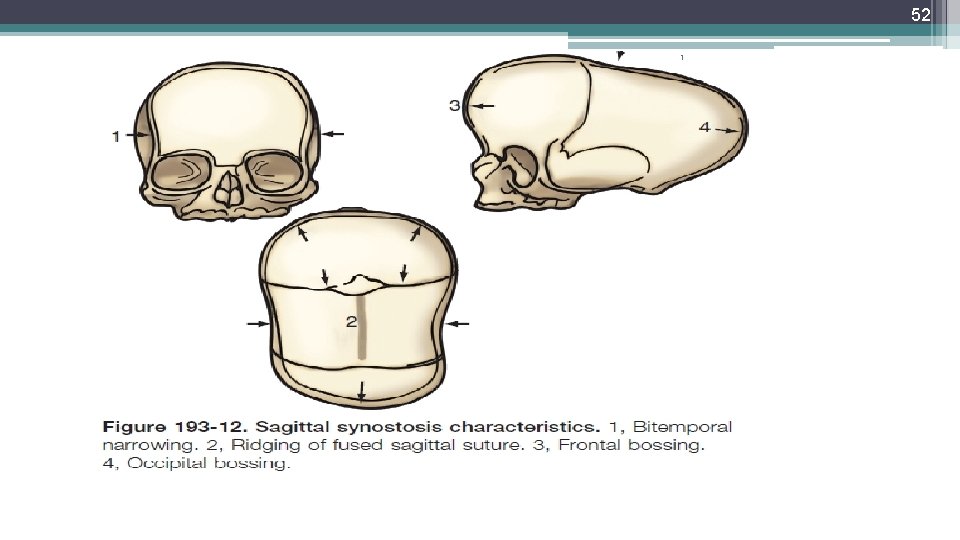
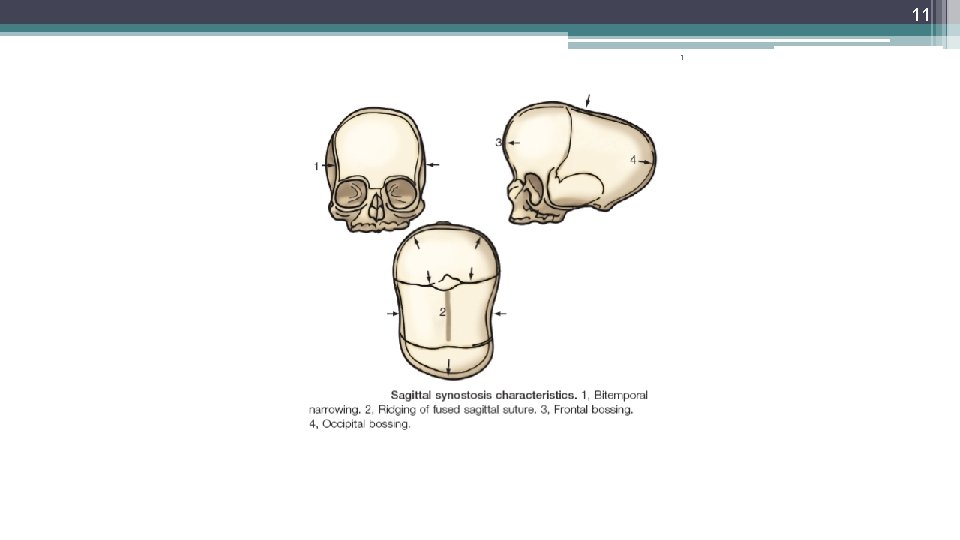
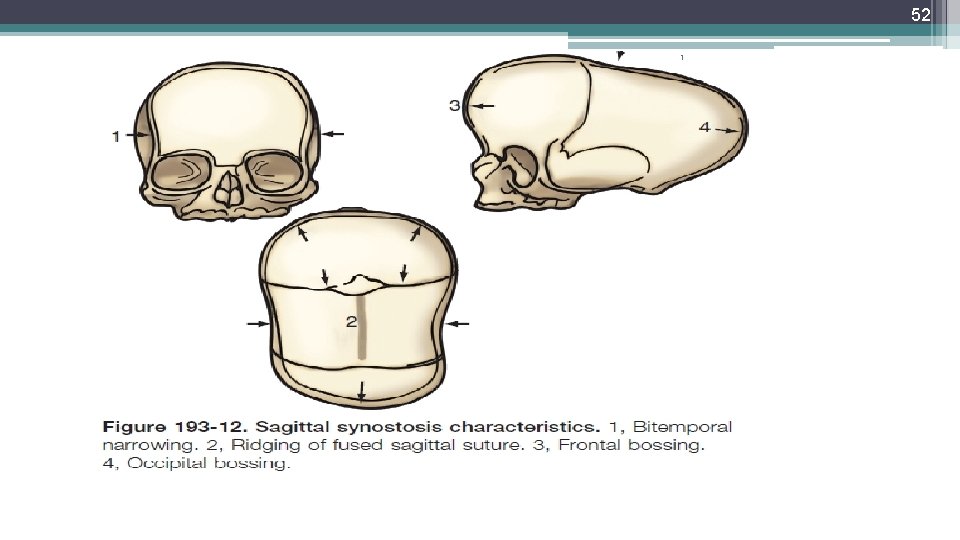
51 Sagittal Synostosis: 1. biparietal narrowing, 2. ridging of the sagittal suture, 3. bilateral bulging of the occipital 4. bilateral bulging of the frontal region 1
52 1
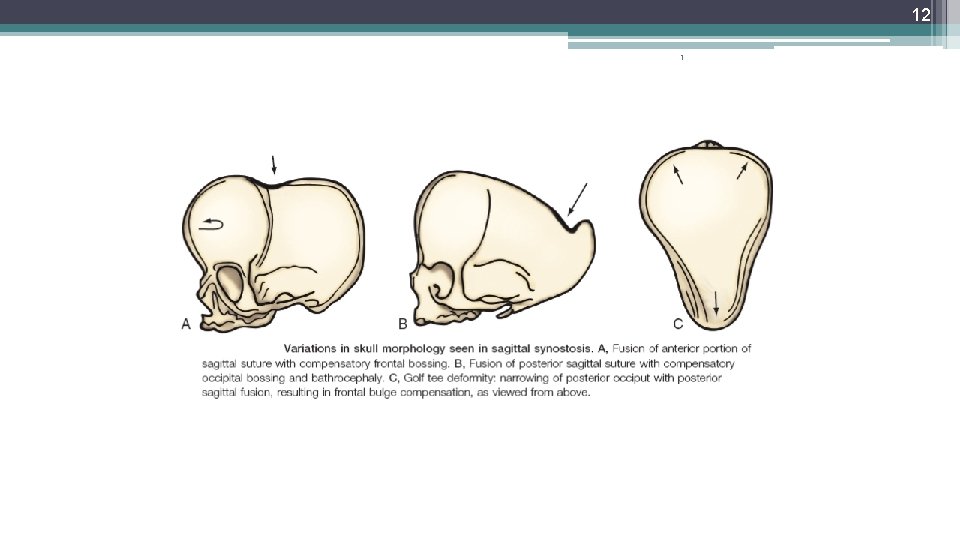
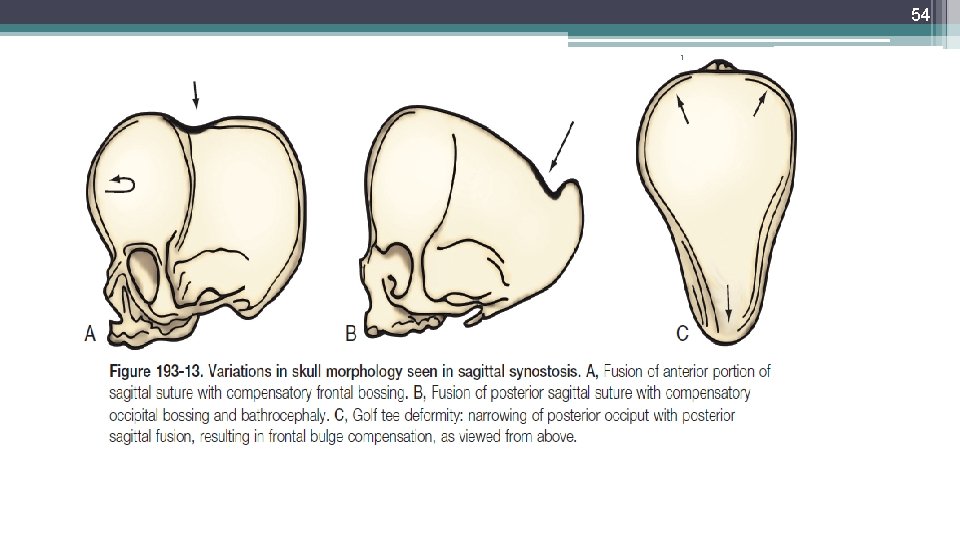
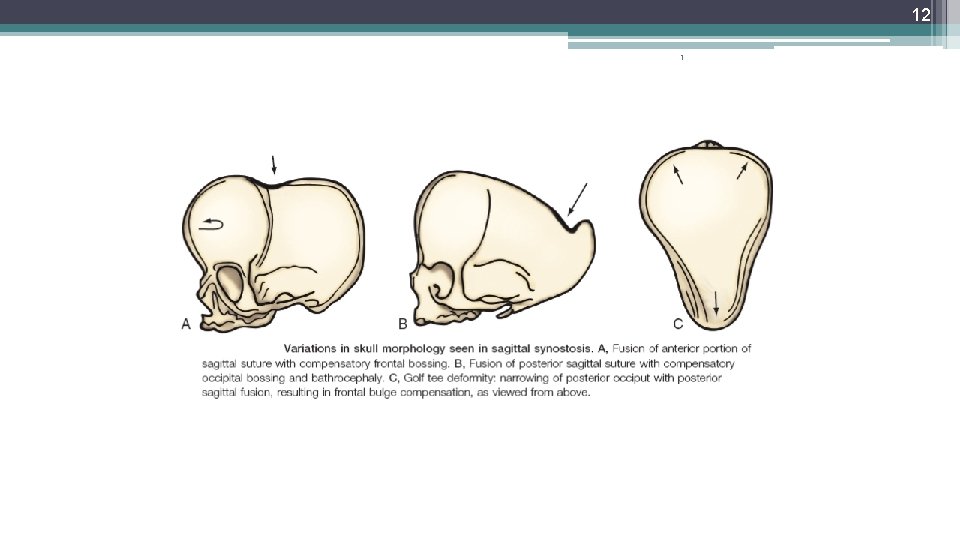
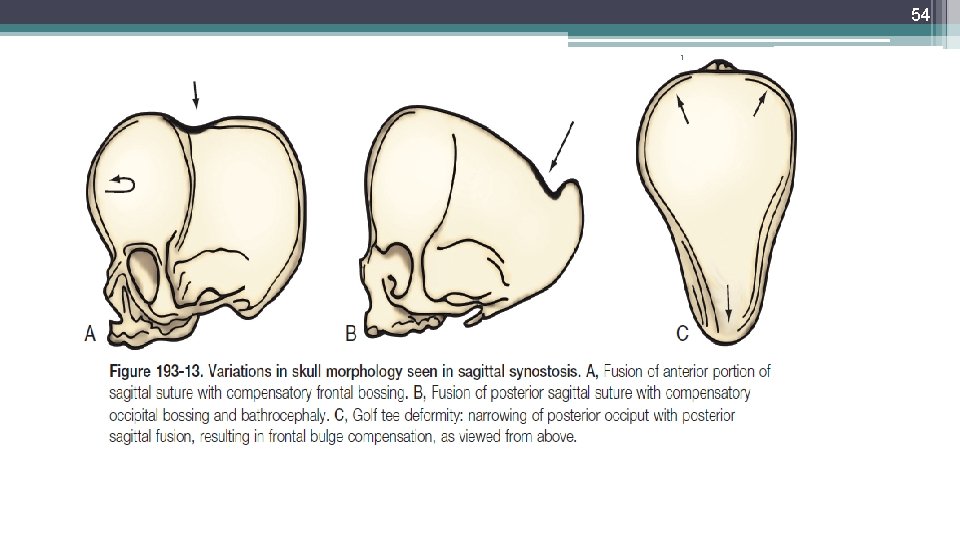
53 1 Usually, one of three varieties of sagittal synostosis predominates: >anterior compensation >posterior compensation >the “golf tee” or bathyrocephalic deformity
54 1
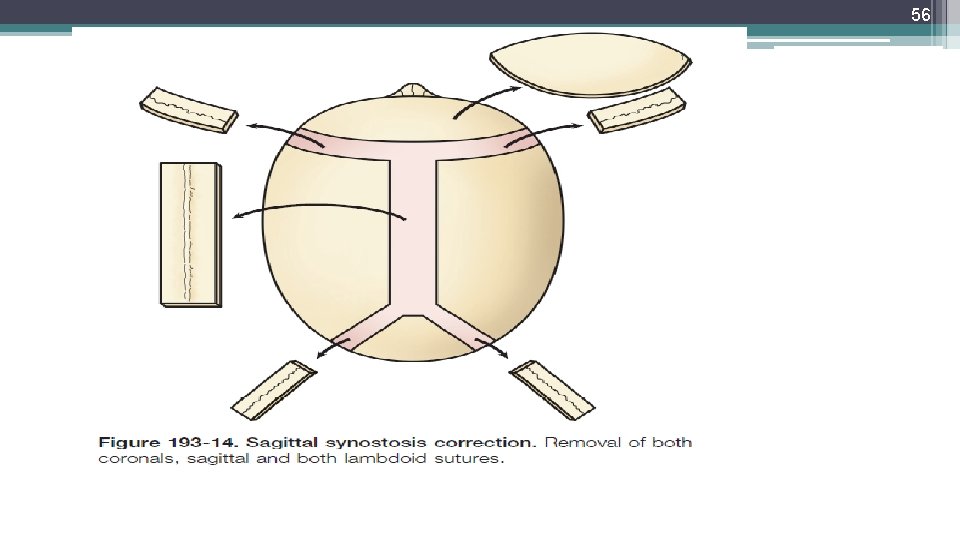
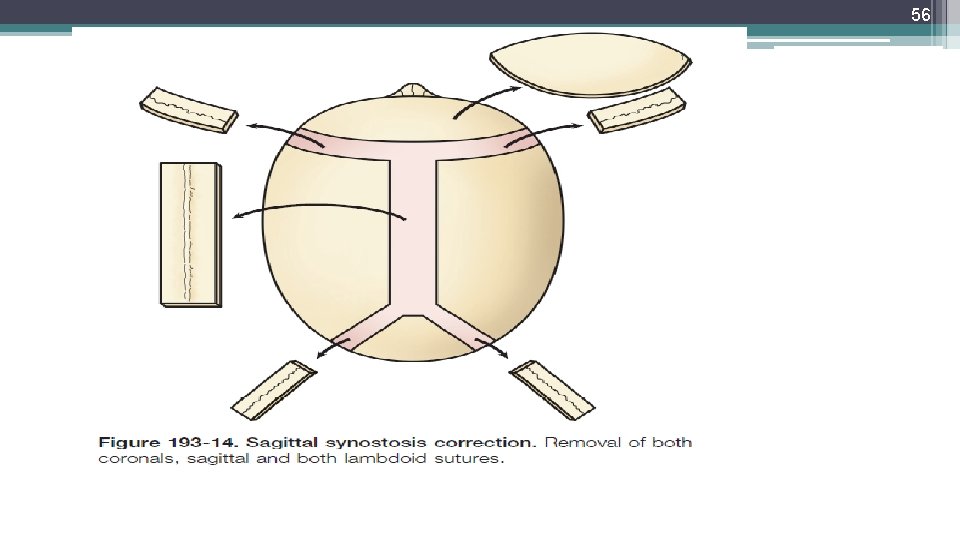
55 1 Operative Technique: In general, treatment is directed at the most salient deformity—that is, the variety of sagittal synostosis that predominates: . anterior compensation. posterior compensation. golf tee deformity After exposure of the skull, the individual sutures(e. g. , the coronals, sagittal, and lambdoid) are each removed separately
56 1
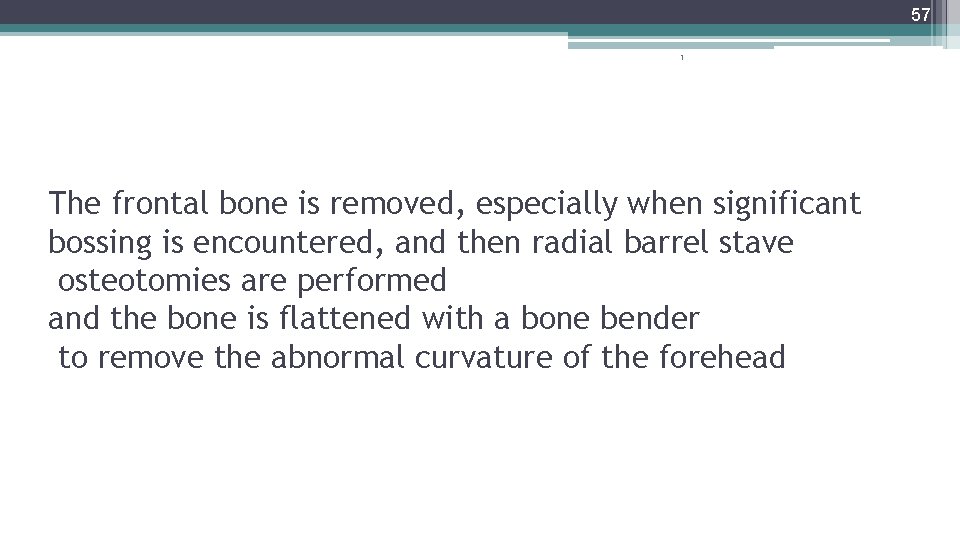
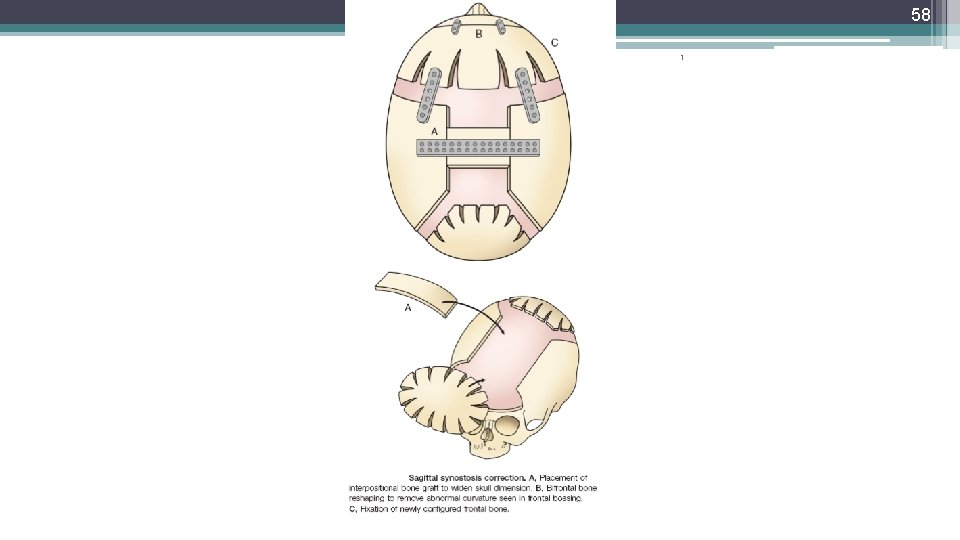
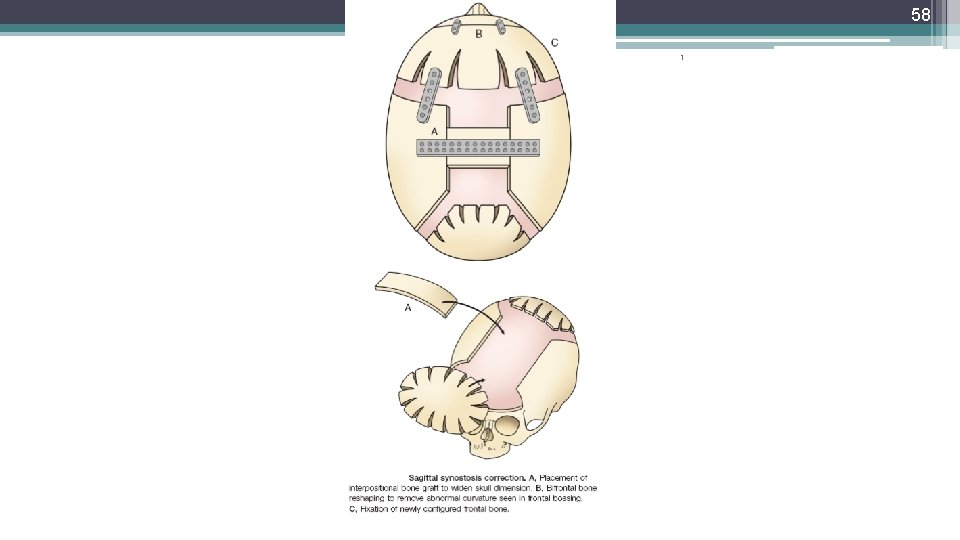
57 1 The frontal bone is removed, especially when significant bossing is encountered, and then radial barrel stave osteotomies are performed and the bone is flattened with a bone bender to remove the abnormal curvature of the forehead
58 1
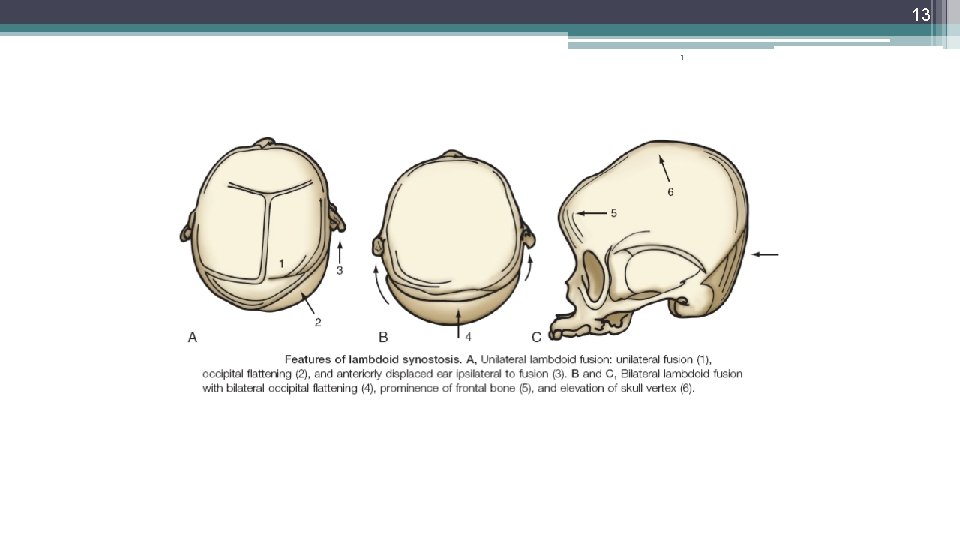
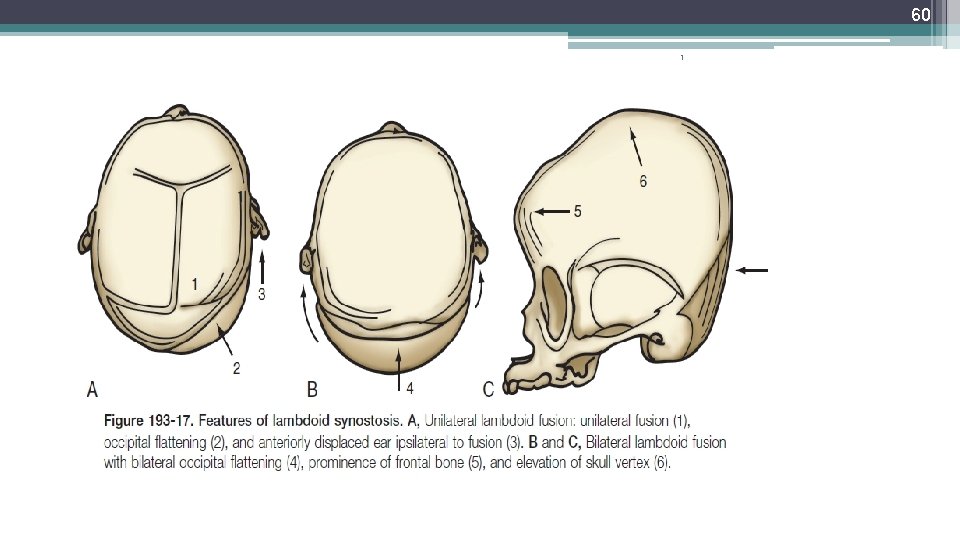
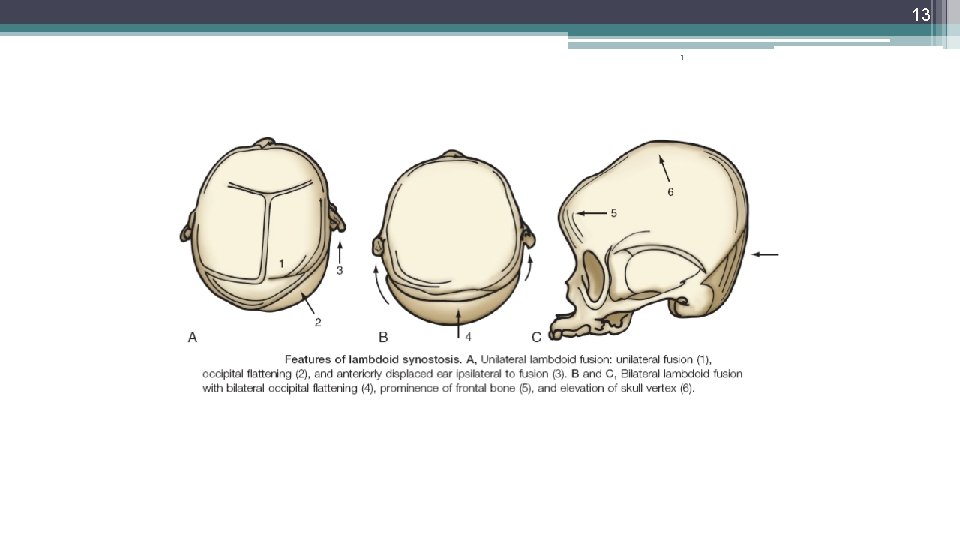
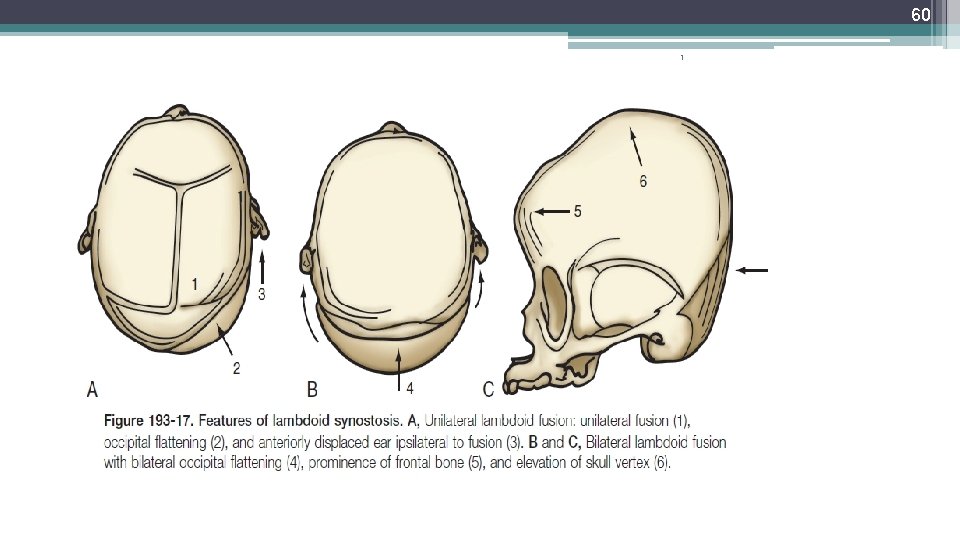
59 1 Lambdoid Synostosis: 1. flattening of the parietal and occipital regions ipsilateral to the fused portion 2. contralateral bulging evident in the parietal occiput or mastoid region. The ipsilateral ear is pulled backward toward the fused suture 4. If bilateral synostosis has occurred, symmetrical flattening of the occiput is seen
60 1
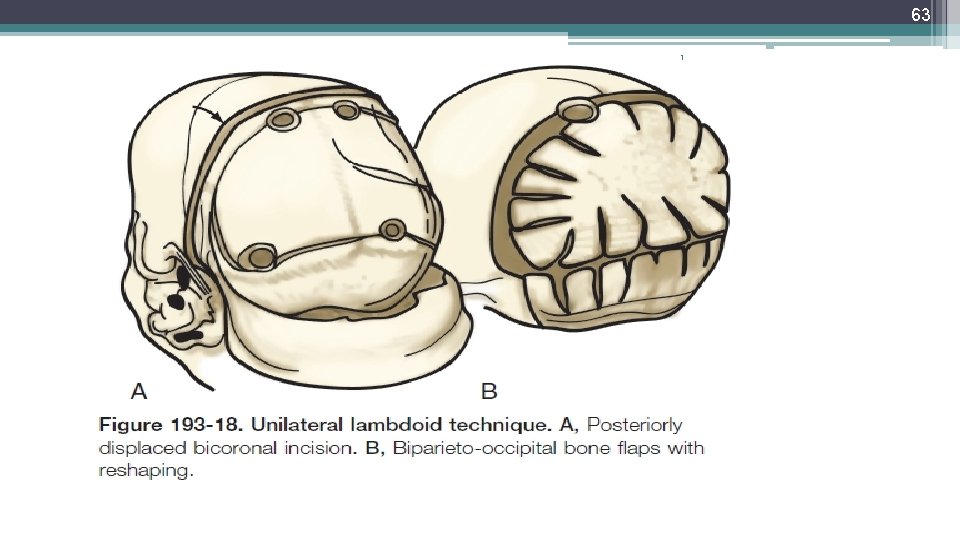
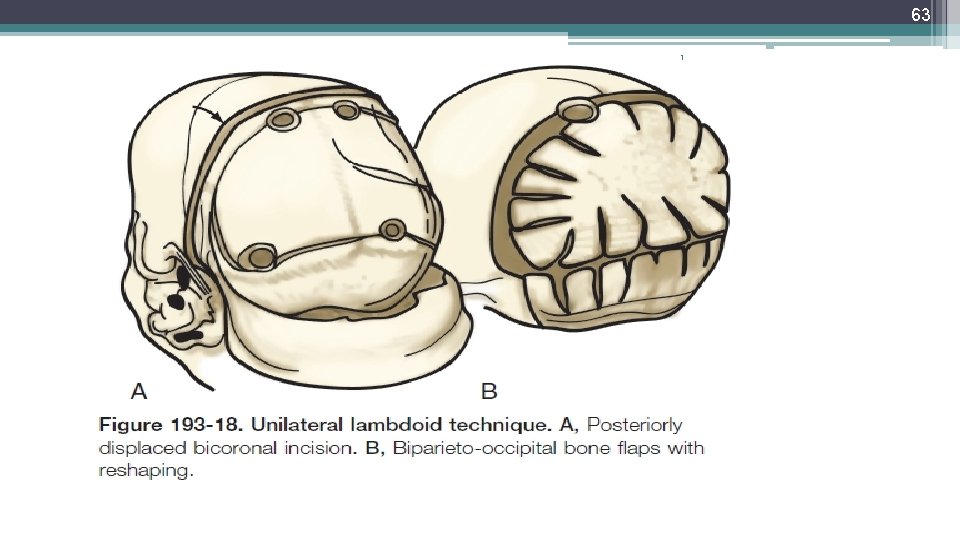
61 1 Operative Technique: most deformities can be satisfactorily corrected with the patient in the prone position and surgical manipulations in the occipital bone. A patient with an occipital deformity is placed in the prone position, and a posteriorly“displaced”coronal incision is carried out
62 1 A biparietal occipital bone graft is elevated in patients with unilateral synostosis or bilateral lambdoid synostosis, with care taken to avoid injuring the transverse sinus. In unilateral synostosis, the convex side is made flatter, and the flatter side is made more convex with the use of greenstick fractures.
63 1
64 1 OPERATIVE COMPLICATIONS
65 The most serious problems associated with cranioplasty procedures are ØBlood loss, ØAir embolus, Ø Infection. 1 The incidence of infection is quite low, with reported incidencesvarying from 2. 5% to 6. 5%.
 Expenditure cycle
Expenditure cycle Hapter 11
Hapter 11 Syndromic surveillance
Syndromic surveillance Texas syndromic surveillance
Texas syndromic surveillance Cms-r-193
Cms-r-193 Cs 193
Cs 193 A 193 kg curtain needs to be raised
A 193 kg curtain needs to be raised Types of inverse
Types of inverse Item 193
Item 193 Uiuc applied aerodynamics group
Uiuc applied aerodynamics group A 193 kg curtain needs to be raised
A 193 kg curtain needs to be raised Kinetic energy equation
Kinetic energy equation 193 brand
193 brand Art 193 clt
Art 193 clt Aku hendak tetap berhati tulus
Aku hendak tetap berhati tulus Mr antolini's advice to holden
Mr antolini's advice to holden Veux-tu briser du péché le pouvoir parole
Veux-tu briser du péché le pouvoir parole Canto 27
Canto 27 Bene non escludibile e non rivale
Bene non escludibile e non rivale Non mihi
Non mihi Assiomi della comunicazione
Assiomi della comunicazione Non air atau non air
Non air atau non air Non erodible channels
Non erodible channels Sifat barang publik
Sifat barang publik Lên non mới biết non cao lội sông mới biết
Lên non mới biết non cao lội sông mới biết Chi non stima la vita non la merita
Chi non stima la vita non la merita Chi non stima la vita non la merita
Chi non stima la vita non la merita Non fidarti di chi non chiude gli occhi quando ti bacia
Non fidarti di chi non chiude gli occhi quando ti bacia Non posse non peccare
Non posse non peccare Non nobis domine non nobis sed nomini tuo da gloriam
Non nobis domine non nobis sed nomini tuo da gloriam Non nobis domine non nobis sed nomini tuo ad gloriam
Non nobis domine non nobis sed nomini tuo ad gloriam Behavioral-rational approach to curriculum
Behavioral-rational approach to curriculum Non quia difficilia sunt
Non quia difficilia sunt Non fare ad altri ciò che non vorresti fosse fatto a te
Non fare ad altri ciò che non vorresti fosse fatto a te How to mix aggregate and non aggregate tableau
How to mix aggregate and non aggregate tableau Whats proportional relationship
Whats proportional relationship Rumus vout
Rumus vout Non-maleficence in medical ethics
Non-maleficence in medical ethics Non recursive algorithm
Non recursive algorithm Tenses exercises with answers
Tenses exercises with answers Partial non hunting gear ratio
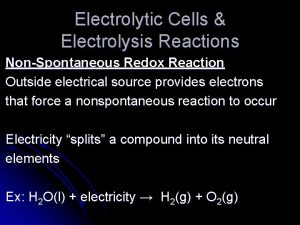
Partial non hunting gear ratio Non spontaneous redox reaction
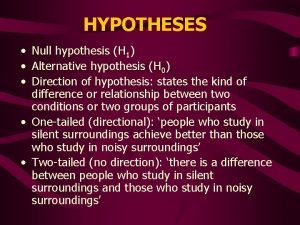
Non spontaneous redox reaction Directional and non directional hypothesis
Directional and non directional hypothesis Ncic restricted files list
Ncic restricted files list Unkompetitif
Unkompetitif Non banking statutory financial organization
Non banking statutory financial organization Non segmental phonology
Non segmental phonology Contoh mesin non konvensional
Contoh mesin non konvensional Non spontaneous reaction examples
Non spontaneous reaction examples Non spontaneous process
Non spontaneous process Non-fatal injury evaluation
Non-fatal injury evaluation Fibrinopeptide a
Fibrinopeptide a How to write a testable question
How to write a testable question Statutory and non statutory welfare measures
Statutory and non statutory welfare measures Lerman non invasive halo
Lerman non invasive halo 12 neutrons metallic 11 electrons
12 neutrons metallic 11 electrons Terminal and non terminal in compiler design
Terminal and non terminal in compiler design Fotosintesis terjadi di
Fotosintesis terjadi di Non accidental death
Non accidental death Contoh analisis fungsional
Contoh analisis fungsional Tunjangan bahaya radiasi
Tunjangan bahaya radiasi Ferrous vs non ferrous
Ferrous vs non ferrous Arginine amino acid essential
Arginine amino acid essential Rachele piange i suoi figli e non vuole essere consolata
Rachele piange i suoi figli e non vuole essere consolata Importance of nonverbal communication
Importance of nonverbal communication Where the dummy nodes added in the branch with unity gain
Where the dummy nodes added in the branch with unity gain