When to Use IVUS When to Use FFR










- Slides: 45
When to Use IVUS, When to Use FFR and When to Use OCT Ron Waksman, MD, Itsik Ben-Dor, MD, Augusto D. Pichard, MD Division of Cardiology, Washington Hospital Center, Washington, DC
Ron Waksman, MD § Consulting Fees – – Abbott Laboratories Boston Scientific Corporation Medtronic, Inc. Biotronik § Speakers’ Bureau – – Abbott Laboratories Boston Scientific Corporation Medtronic, Inc. Volcano I intend to reference off label or unapproved uses of drugs or devices in my presentation.

When OCT IVUS FFR ? ? ?
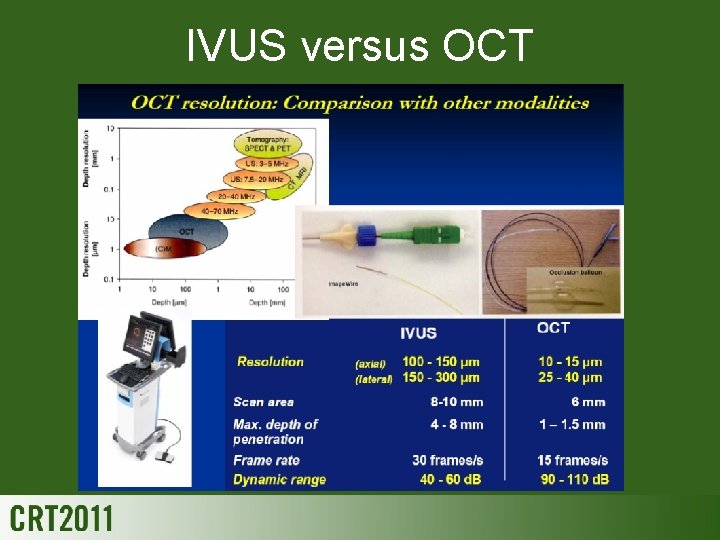
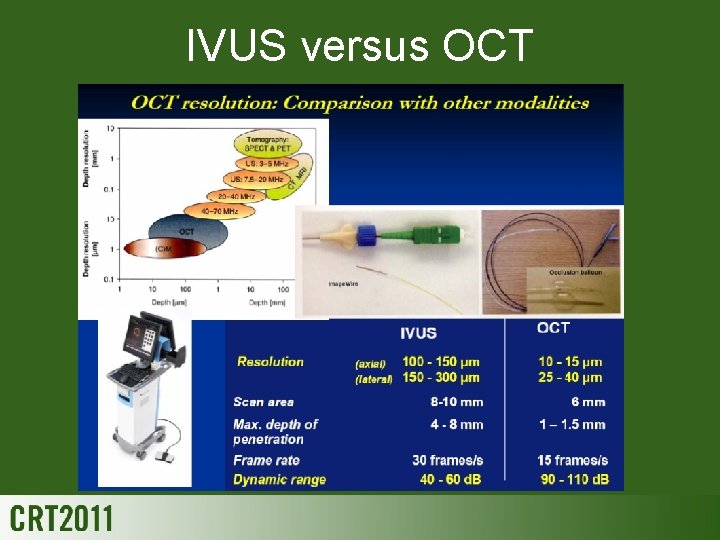
IVUS versus OCT
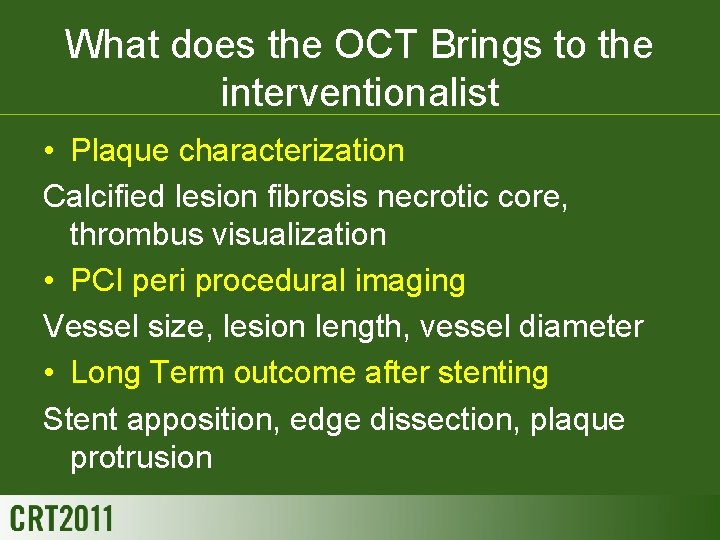
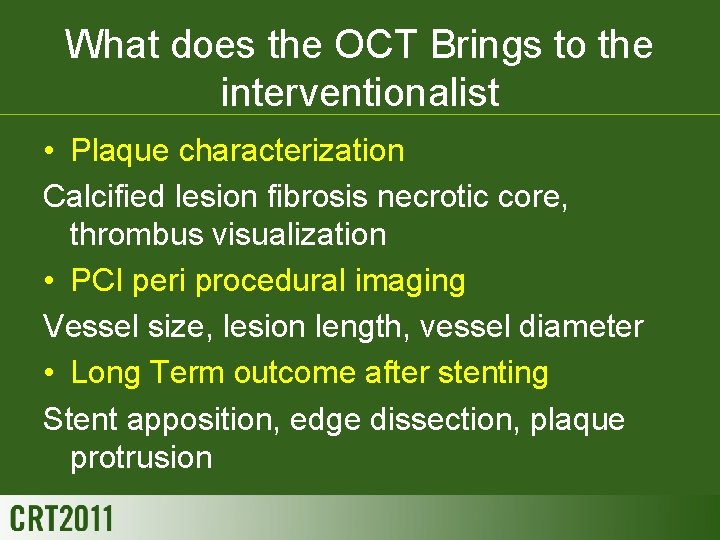
What does the OCT Brings to the interventionalist • Plaque characterization Calcified lesion fibrosis necrotic core, thrombus visualization • PCI peri procedural imaging Vessel size, lesion length, vessel diameter • Long Term outcome after stenting Stent apposition, edge dissection, plaque protrusion

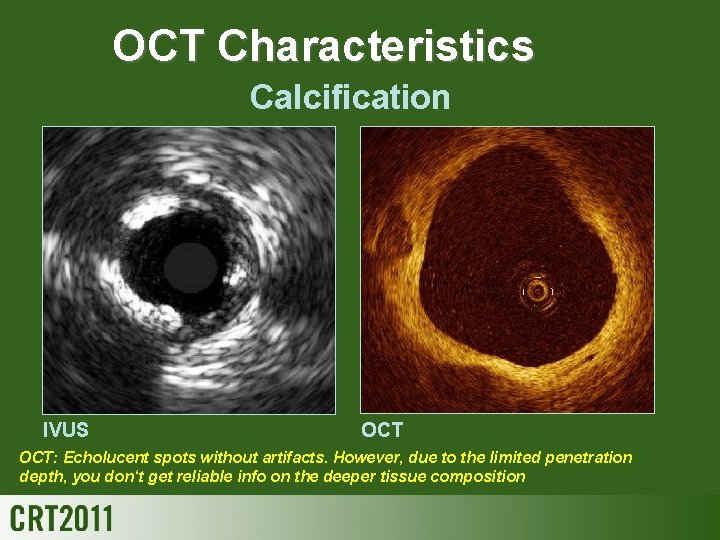
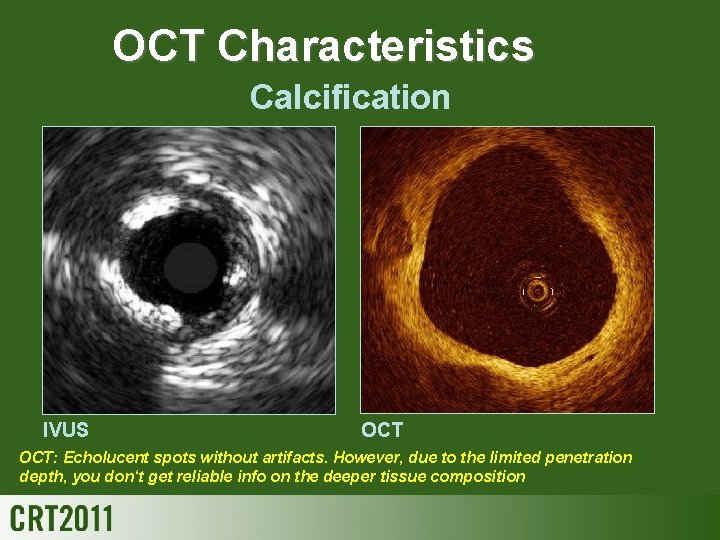
OCT Characteristics Calcification IVUS OCT: Echolucent spots without artifacts. However, due to the limited penetration depth, you don‘t get reliable info on the deeper tissue composition
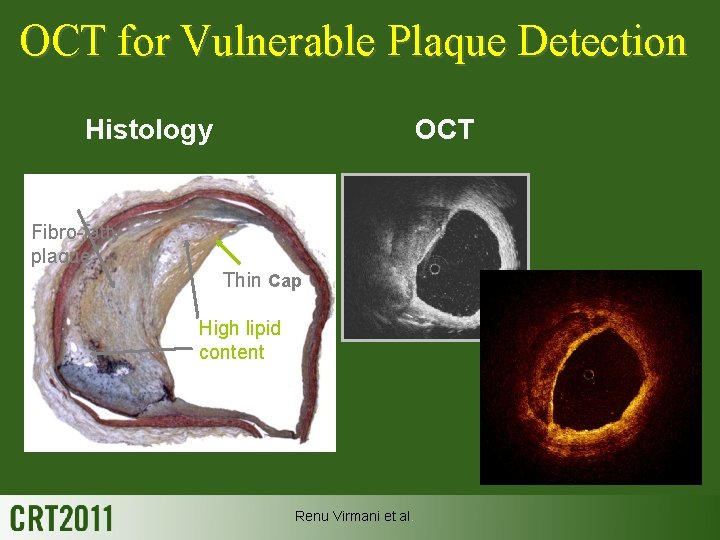
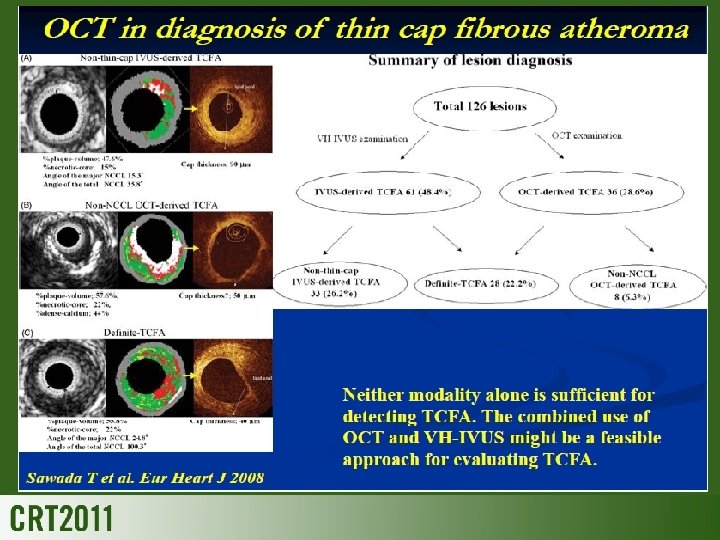
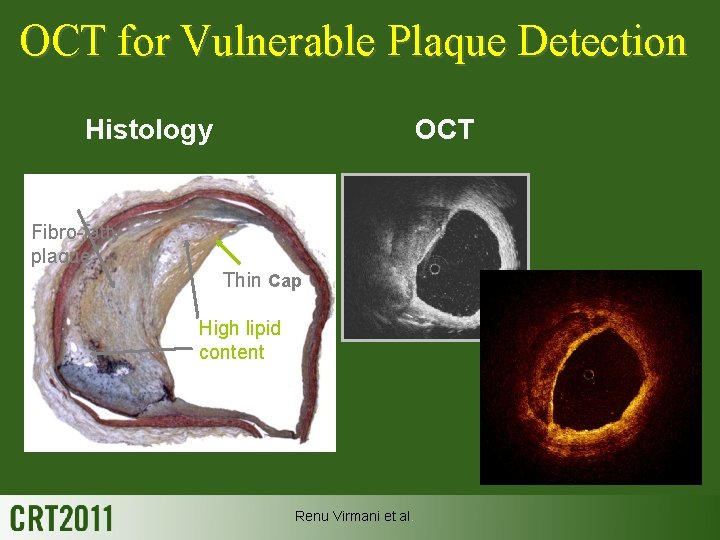
OCT for Vulnerable Plaque Detection Histology OCT Fibro-fatty plaque Thin Cap High lipid content Renu Virmani et al.
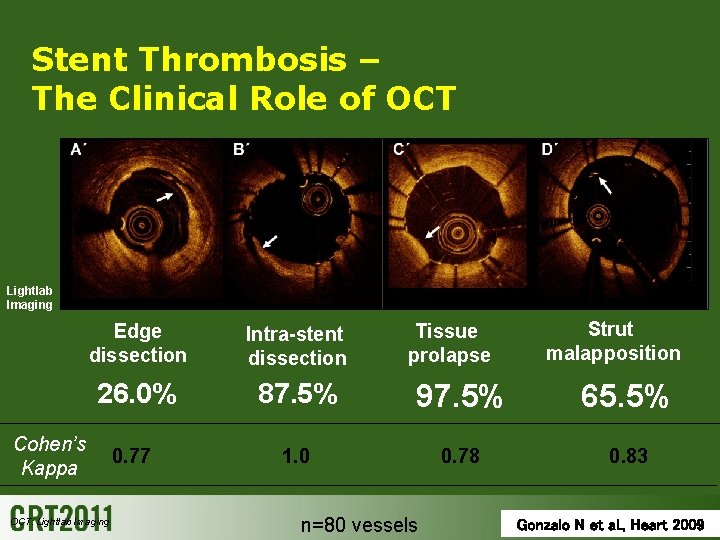
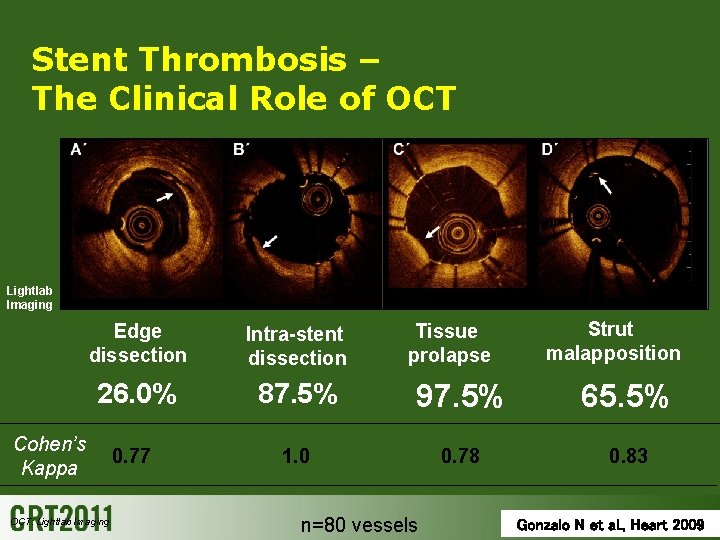
Stent Thrombosis – The Clinical Role of OCT Lightlab Imaging Intra-stent dissection 26. 0% 87. 5% 97. 5% 65. 5% 0. 77 1. 0 0. 78 0. 83 Cohen’s Kappa OCT: Lightlab Imaging Tissue prolapse Strut malapposition Edge dissection n=80 vessels Gonzalo N et al. , Heart 2009
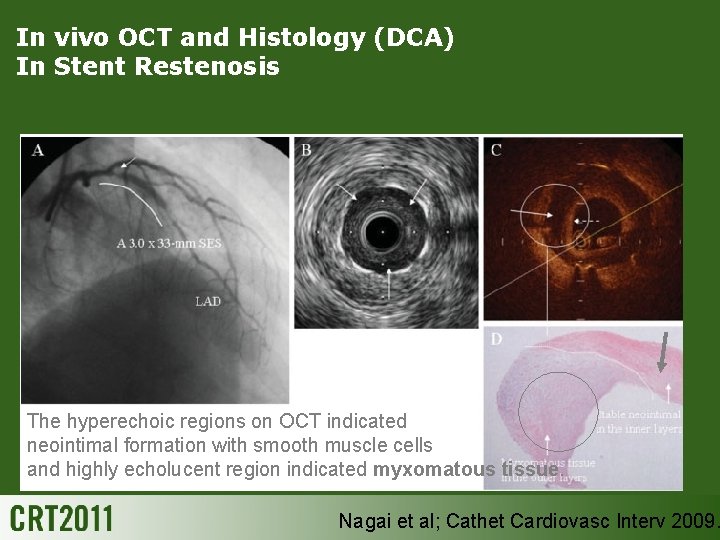
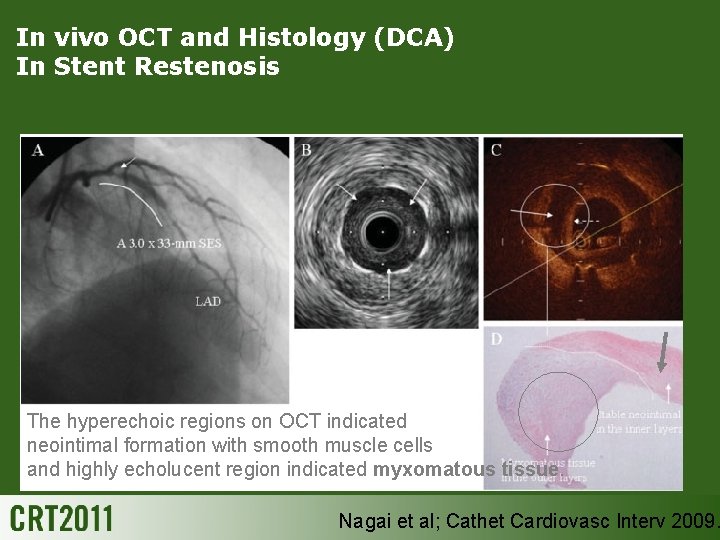
In vivo OCT and Histology (DCA) In Stent Restenosis The hyperechoic regions on OCT indicated neointimal formation with smooth muscle cells and highly echolucent region indicated myxomatous tissue. Nagai et al; Cathet Cardiovasc Interv 2009.
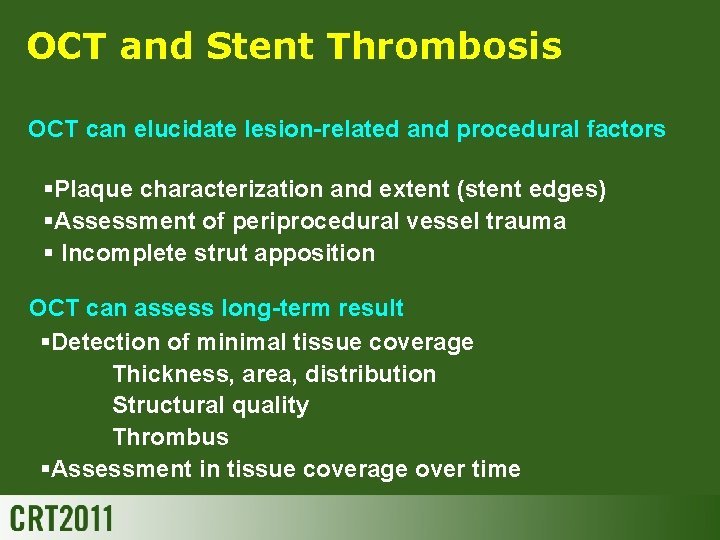
OCT and Stent Thrombosis OCT can elucidate lesion-related and procedural factors §Plaque characterization and extent (stent edges) §Assessment of periprocedural vessel trauma § Incomplete strut apposition OCT can assess long-term result §Detection of minimal tissue coverage Thickness, area, distribution Structural quality Thrombus §Assessment in tissue coverage over time

Importance of IVUS Guidance Lesion Assessment Appropriate Expansion Adequate stent apposition Full lesion coverage
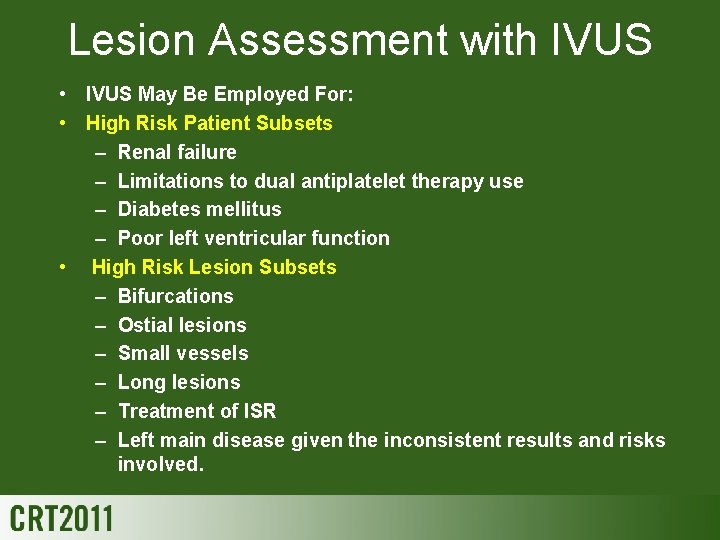
Lesion Assessment with IVUS • IVUS May Be Employed For: • High Risk Patient Subsets – Renal failure – Limitations to dual antiplatelet therapy use – Diabetes mellitus – Poor left ventricular function • High Risk Lesion Subsets – Bifurcations – Ostial lesions – Small vessels – Long lesions – Treatment of ISR – Left main disease given the inconsistent results and risks involved.

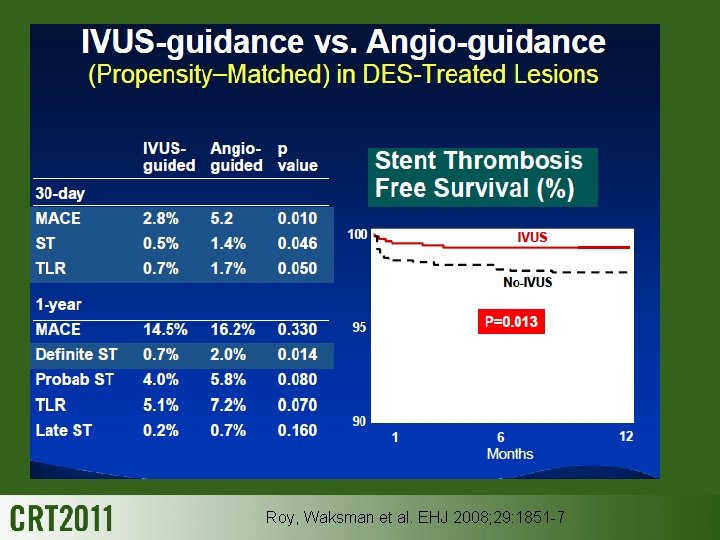
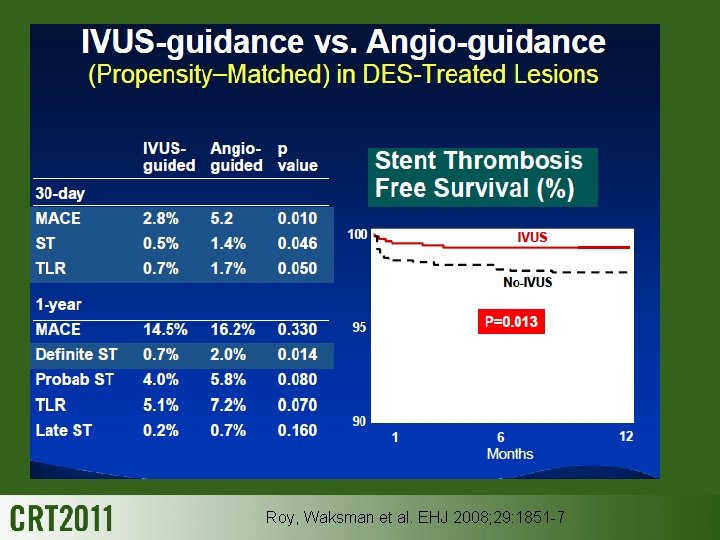
Roy, Waksman et al. EHJ 2008; 29: 1851 -7
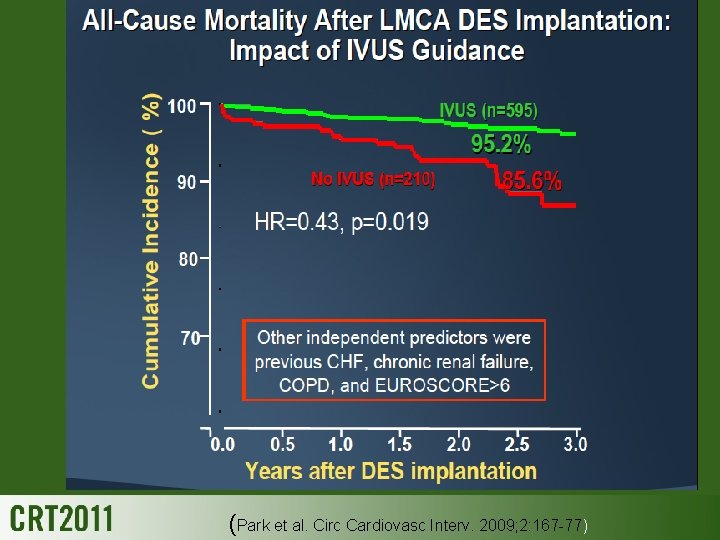
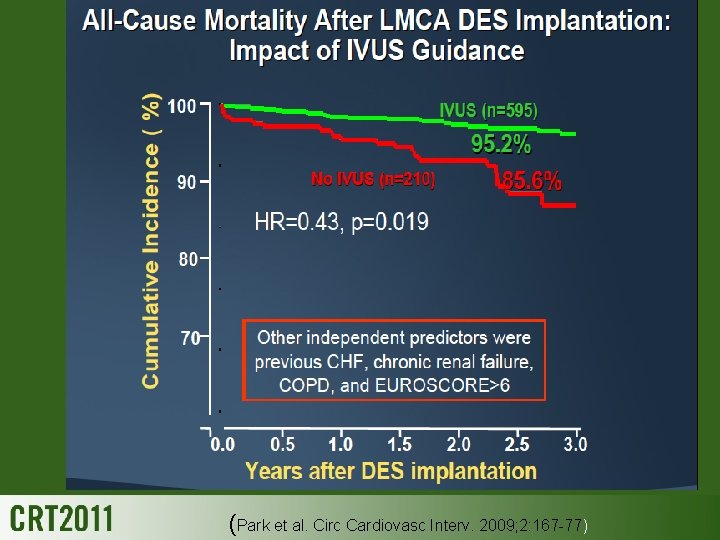
(Park et al. Circ Cardiovasc Interv. 2009; 2: 167 -77)

Intravascular Ultrasound Versus Fractional Flow Reserve for PCI with DES
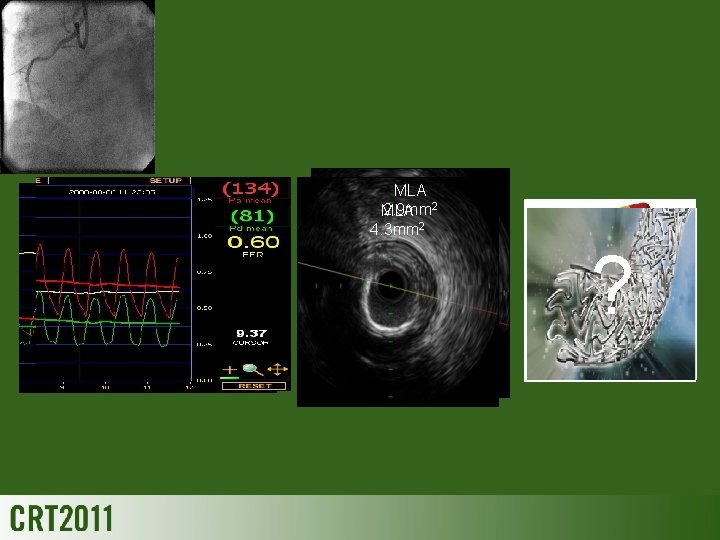
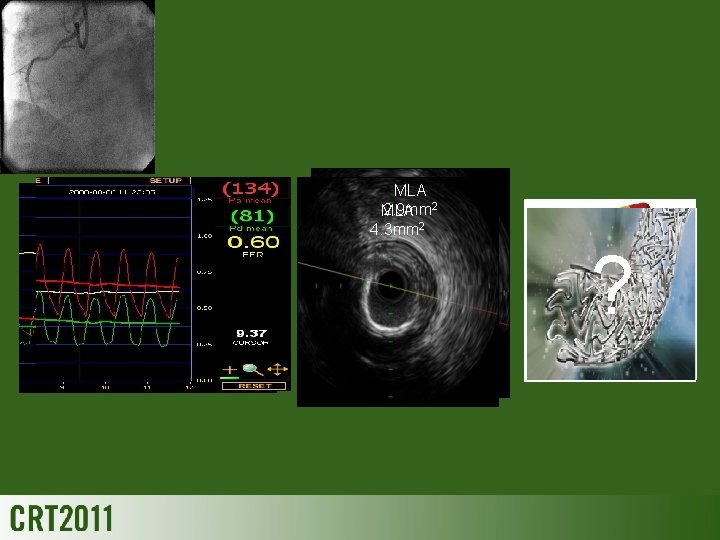
MLA 2. 9 mm 2 MLA 4. 3 mm 2 ?

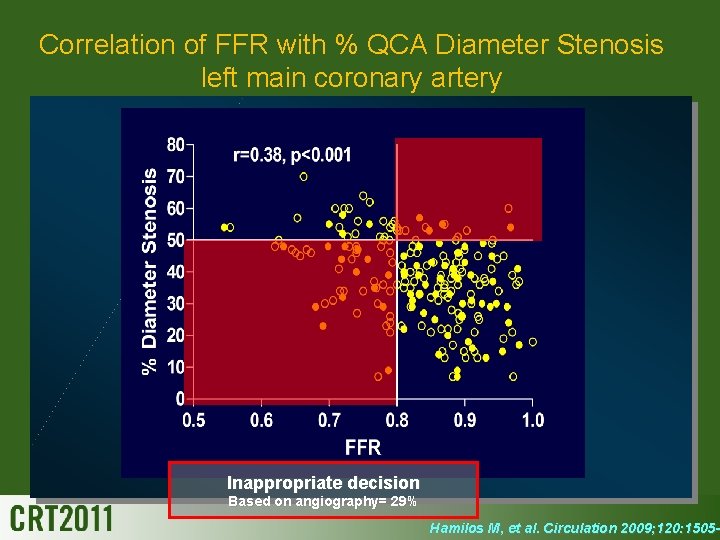
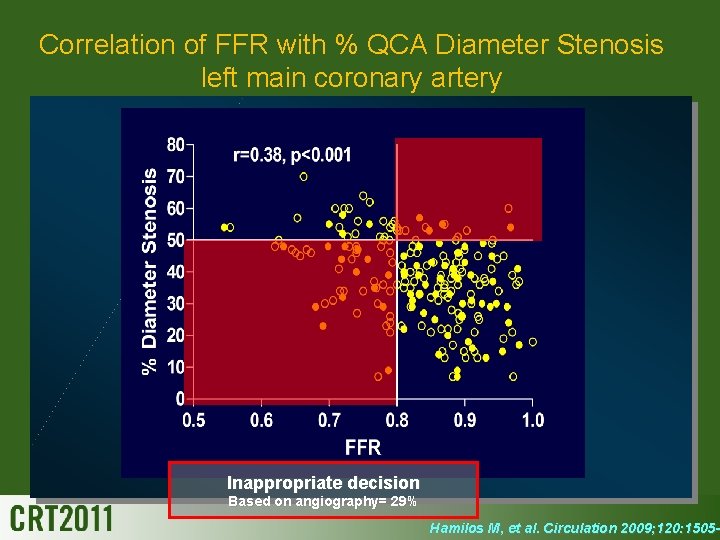
Correlation of FFR with % QCA Diameter Stenosis left main coronary artery Inappropriate decision Based on angiography= 29% Hamilos M, et al. Circulation 2009; 120: 1505 -1 2009; 120: 1505 -

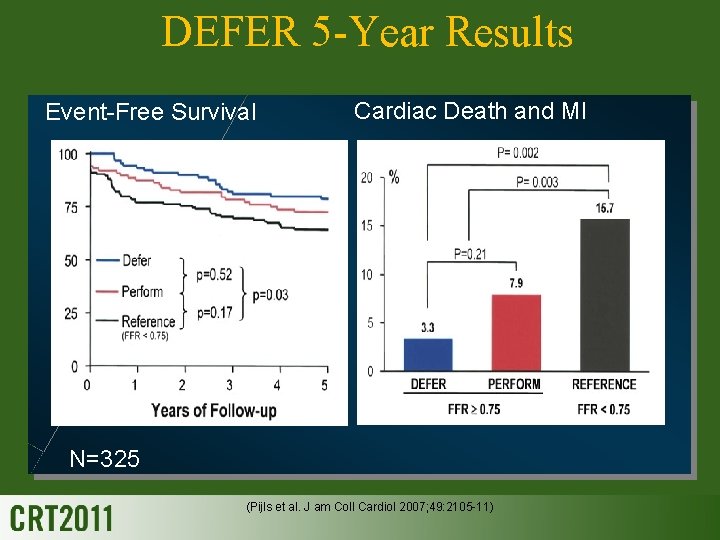
Clinical outcome-FFR DEFER
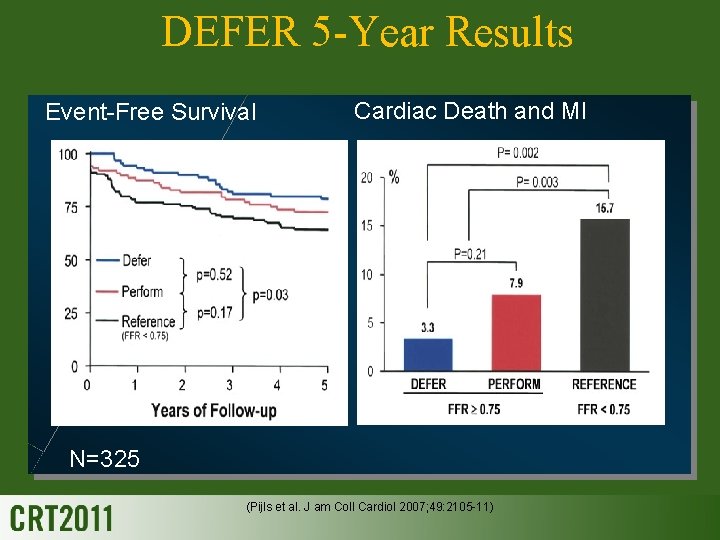
DEFER 5 -Year Results Event-Free Survival Cardiac Death and MI N=325 (Pijls et al. J am Coll Cardiol 2007; 49: 2105 -11)

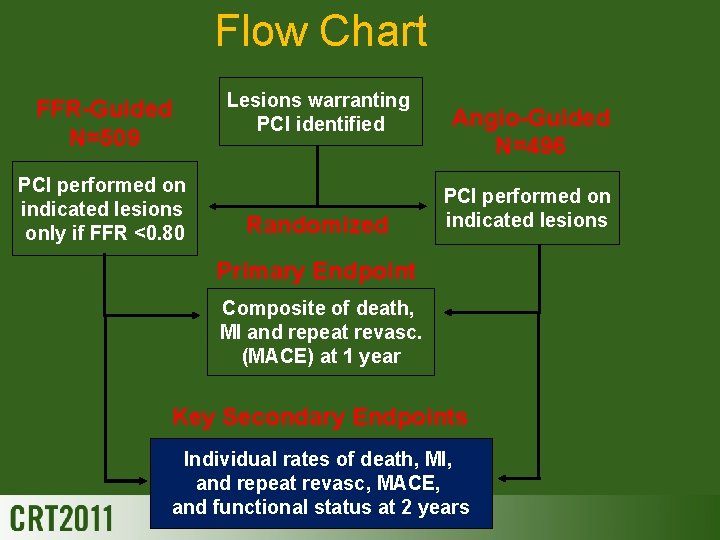
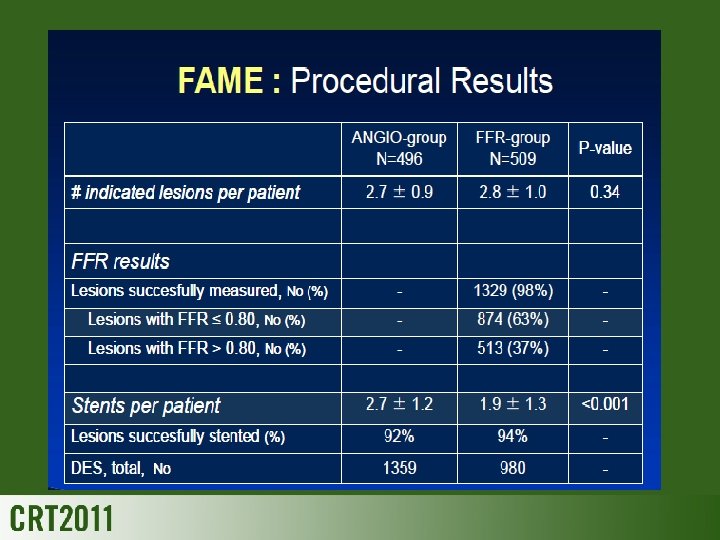
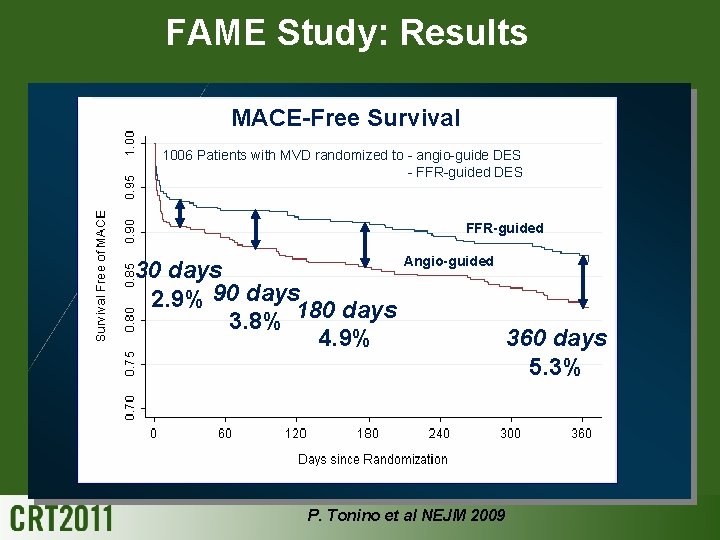
Clinical outcome-FFR FAME
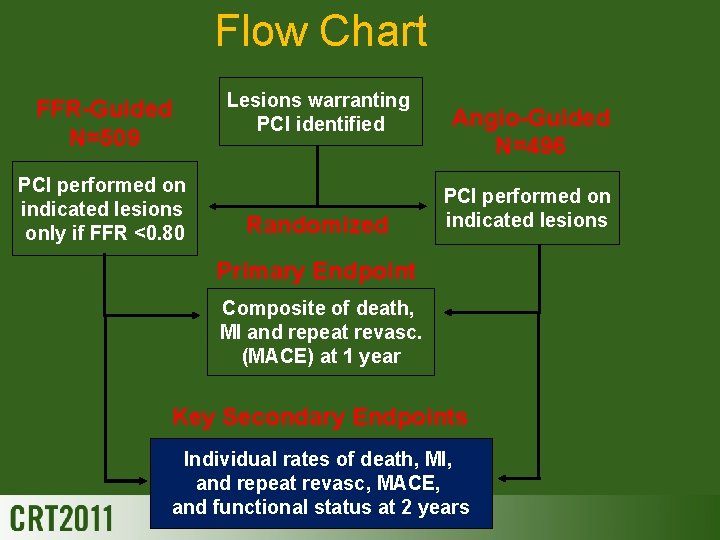
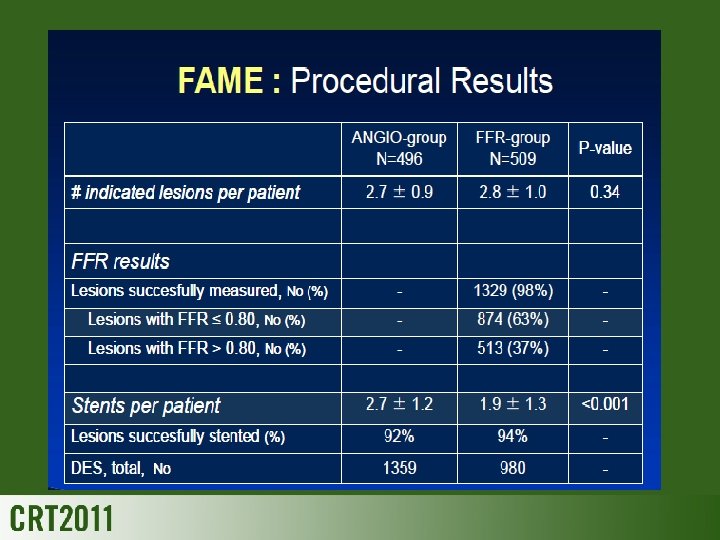
Flow Chart FFR-Guided N=509 PCI performed on indicated lesions only if FFR <0. 80 Lesions warranting PCI identified Randomized Angio-Guided N=496 PCI performed on indicated lesions Primary Endpoint Composite of death, MI and repeat revasc. (MACE) at 1 year Key Secondary Endpoints Individual rates of death, MI, and repeat revasc, MACE, and functional status at 2 years
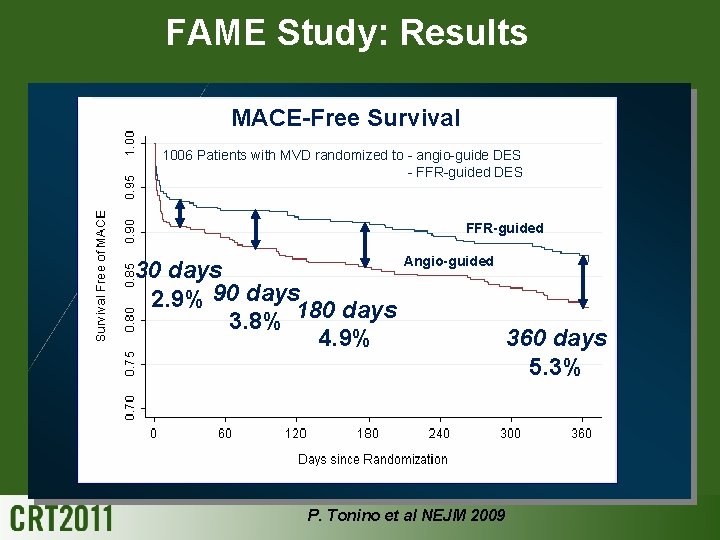
FAME Study: Results MACE-Free Survival 1006 Patients with MVD randomized to - angio-guide DES - FFR-guided DES FFR-guided Angio-guided 30 days 2. 9% 90 days 180 days 3. 8% 360 days 4. 9% 5. 3% P. Tonino et al NEJM 2009
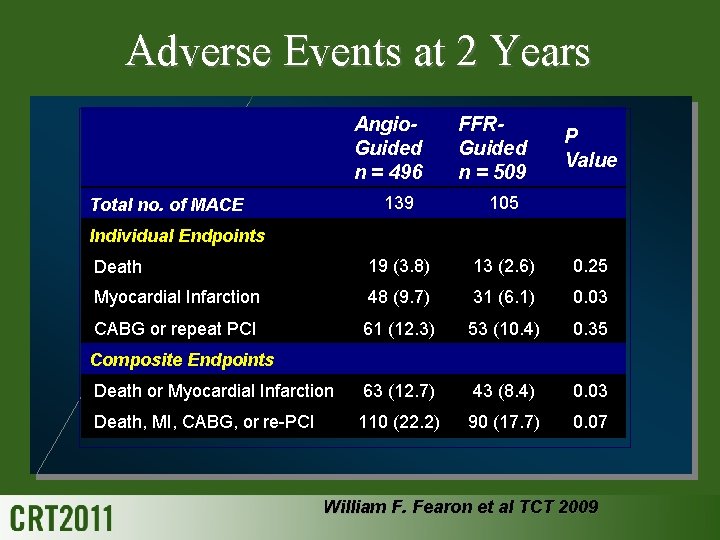
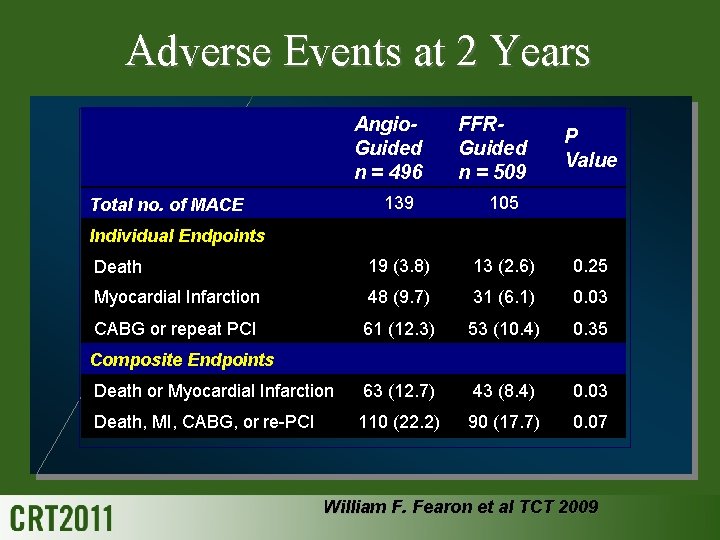
Adverse Events at 2 Years Angio. Guided n = 496 FFRGuided n = 509 P Value 139 105 Death 19 (3. 8) 13 (2. 6) 0. 25 Myocardial Infarction 48 (9. 7) 31 (6. 1) 0. 03 CABG or repeat PCI 61 (12. 3) 53 (10. 4) 0. 35 Death or Myocardial Infarction 63 (12. 7) 43 (8. 4) 0. 03 Death, MI, CABG, or re-PCI 110 (22. 2) 90 (17. 7) 0. 07 Total no. of MACE Individual Endpoints Composite Endpoints William F. Fearon et al TCT 2009
IVUS & FFR correlation ?
Clinical outcome-IVUS No prospective randomized study has ever shown better PCI outcome by using IVUS
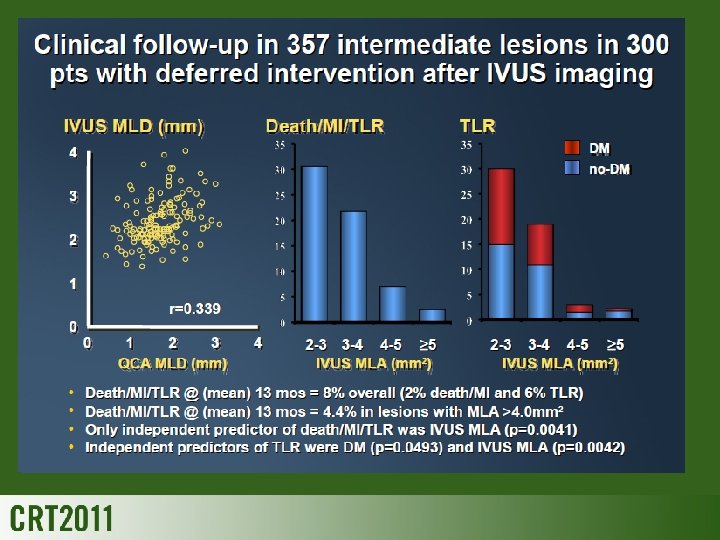
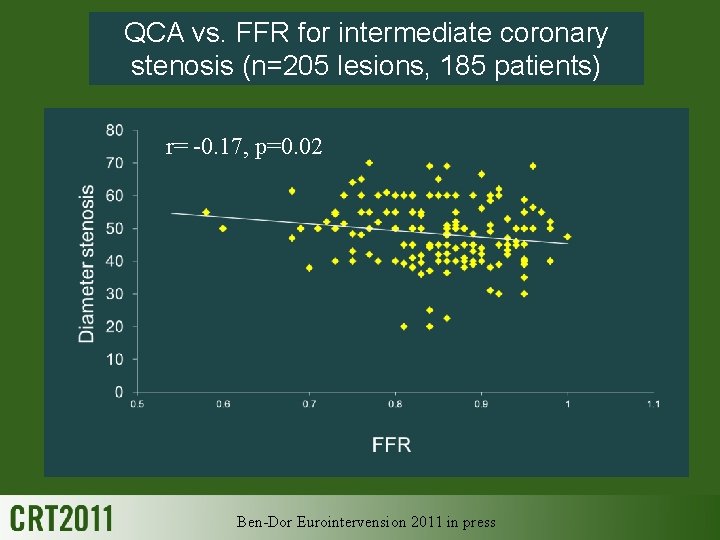
QCA vs. FFR for intermediate coronary stenosis (n=205 lesions, 185 patients) r= -0. 17, p=0. 02 Ben-Dor Eurointervension 2011 in press
IVUS & FFR correlation ?
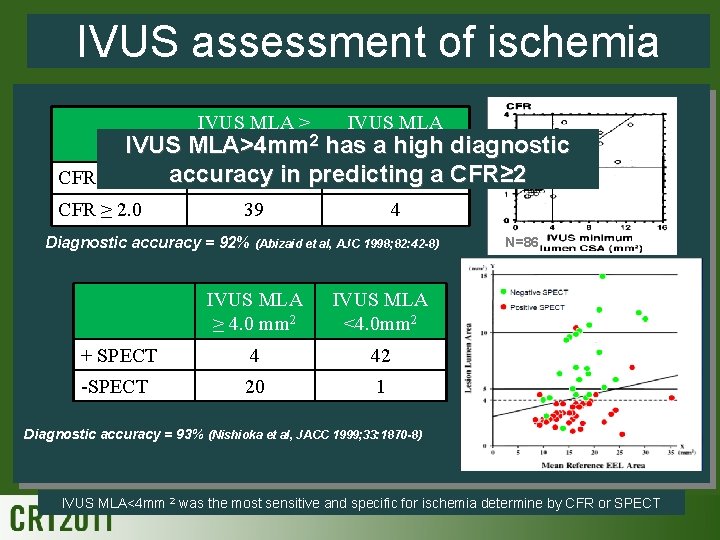
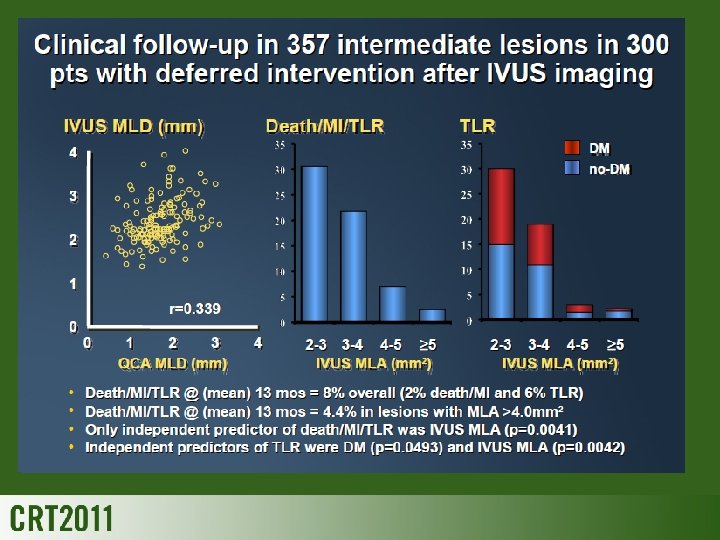
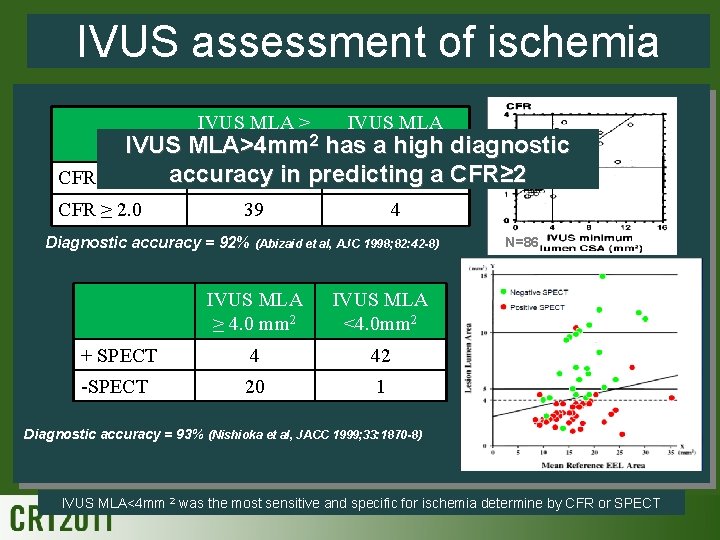
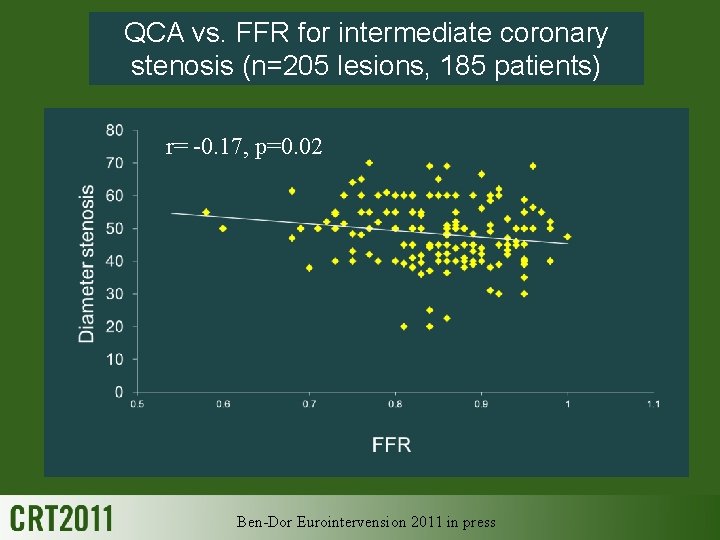
IVUS assessment of ischemia IVUS MLA ≥ 4. 0 mm 2 2 IVUS MLA>4 mm CFR < 2. 0 CFR ≥ 2. 0 IVUS MLA 2 diagnostic has<4. 0 mm a high accuracy 2 in predicting 27 a CFR≥ 2 39 4 Diagnostic accuracy = 92% (Abizaid et al, AJC 1998; 82: 42 -8) IVUS MLA ≥ 4. 0 mm 2 IVUS MLA <4. 0 mm 2 + SPECT 4 42 -SPECT 20 1 N=86 Diagnostic accuracy = 93% (Nishioka et al, JACC 1999; 33: 1870 -8) IVUS MLA<4 mm 2 was the most sensitive and specific for ischemia determine by CFR or SPECT

IVUS vs. FFR N=43 N=42 mm 2 IVUS MLA<3 and an area stenosis >60% were predictive of an FFR <0. 75 Sensitivity Specificity Area stenosis >70% 100% 68% MLD <1. 8 mm 100% 66% MLA <4. 0 mm 2 82% 56% Length >10 mm 41% 80% (Takagi, et al. Circulation 1999; 100: 250 -5) (Briguori, et al. AJC 2001; 87: 136 -41)
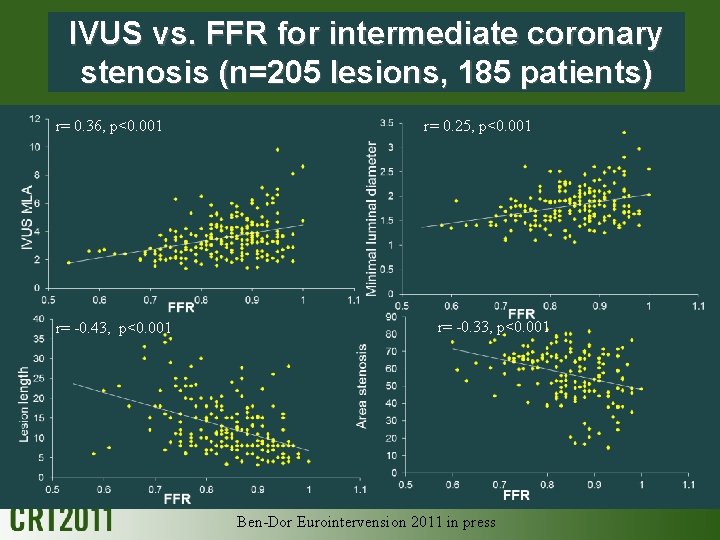
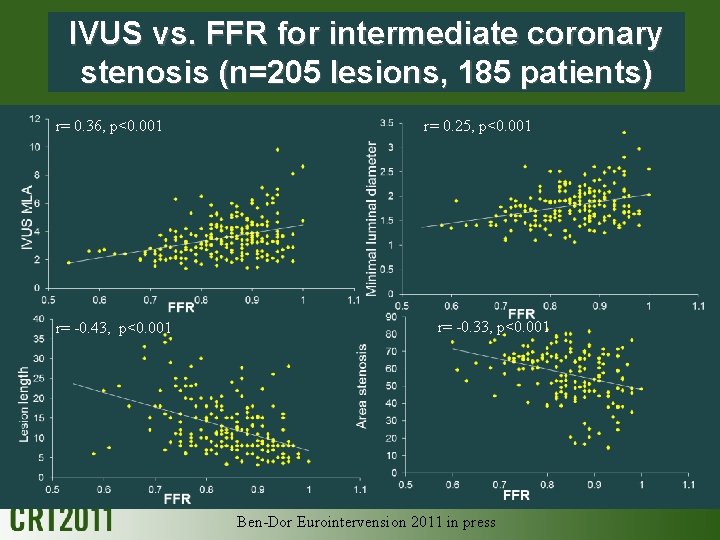
IVUS vs. FFR for intermediate coronary stenosis (n=205 lesions, 185 patients) r= 0. 36, p<0. 001 r= -0. 43, p<0. 001 r= 0. 25, p<0. 001 r= -0. 33, p<0. 001 Ben-Dor Eurointervension 2011 in press

IVUS cutoff for ischemic FFR<0. 8 Percentage 3. 09 mm 2 (sensitivity 69. 2%, specificity 71. 5%) Ben-Dor Eurointervension 2011 in press C=0. 73
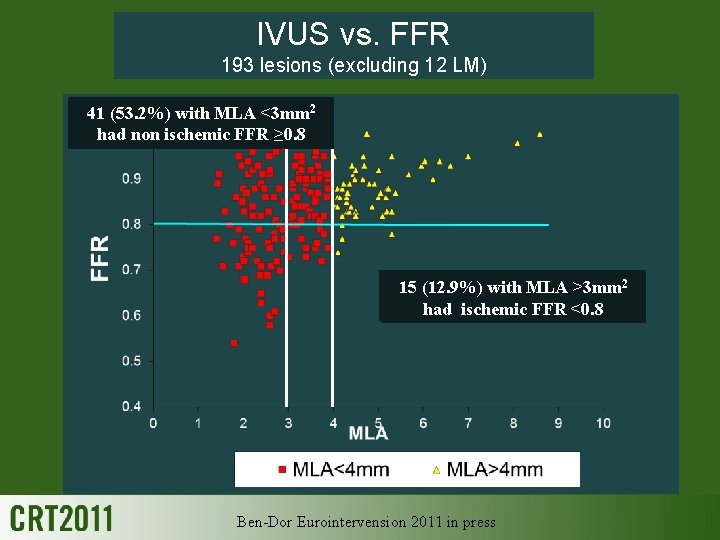
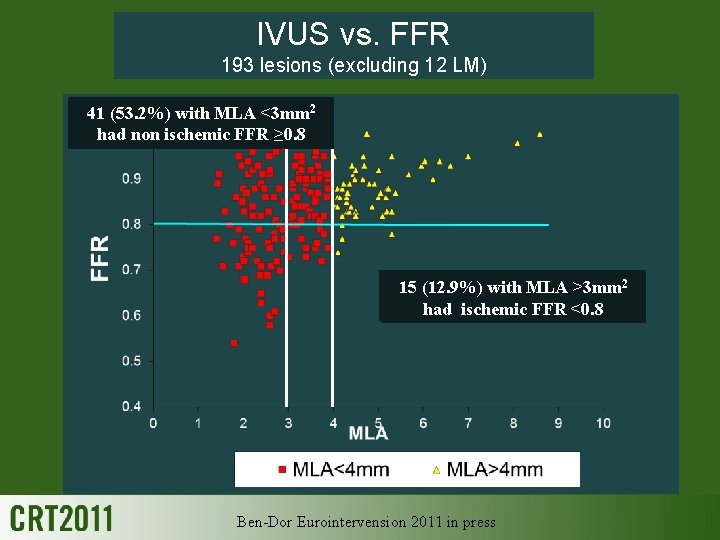
IVUS vs. FFR 193 lesions (excluding 12 LM) 41 (65. 7%) (53. 2%) with MLA <4 mm <3 mm 2 92 had non ischemic FFR ≥ 0. 8 2 had 2 315 (5. 6%) with MLA >4 mm (12. 9%) MLA >3 mm ischemic FFR <0. 8 had ischemic FFR <0. 8 Ben-Dor Eurointervension 2011 in press
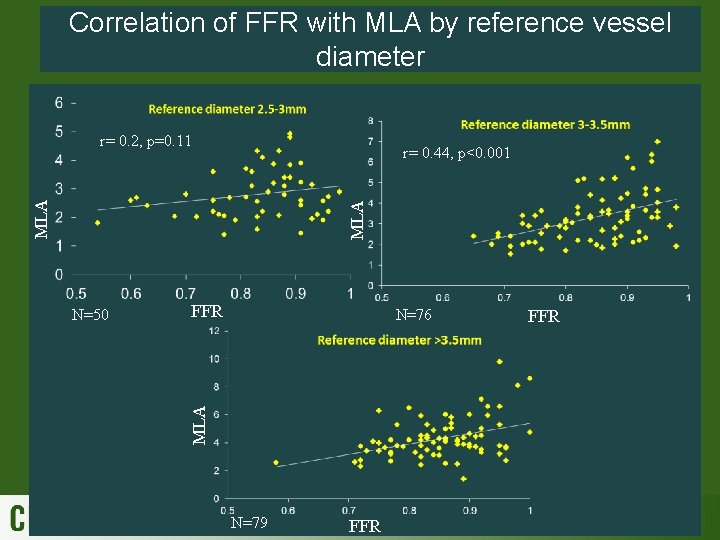
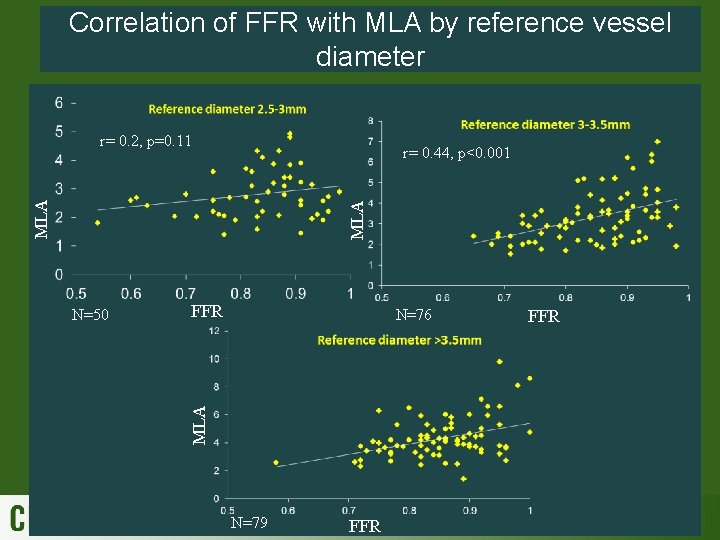
Correlation of FFR with MLA by reference vessel diameter r= 0. 2, p=0. 11 MLA r= 0. 44, p<0. 001 FFR N=76 MLA N=50 N=79 FFR
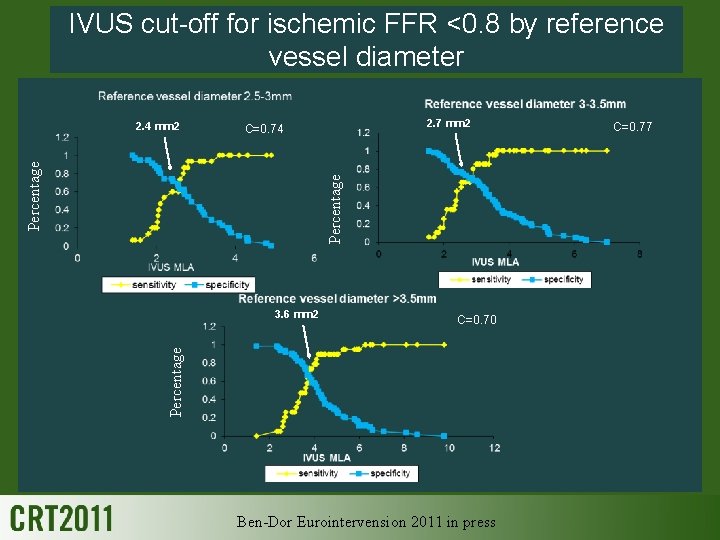
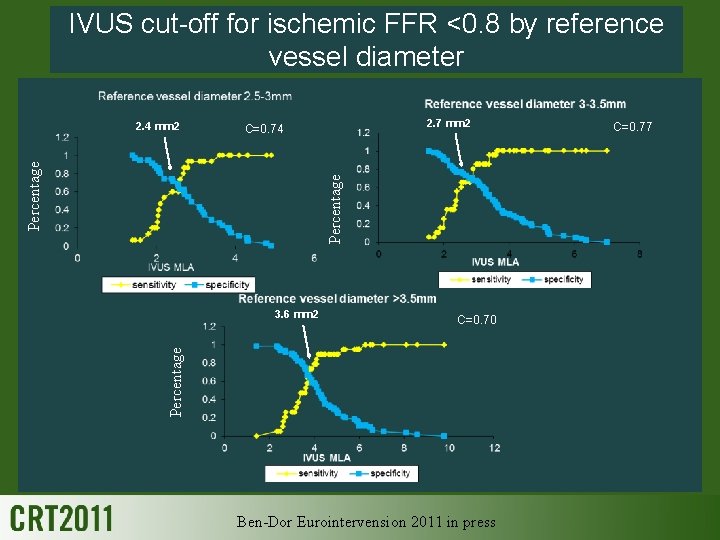
IVUS cut-off for ischemic FFR <0. 8 by reference vessel diameter 2. 7 mm 2 C=0. 74 Percentage 2. 4 mm 2 C=0. 70 Percentage 3. 6 mm 2 Ben-Dor Eurointervension 2011 in press C=0. 77
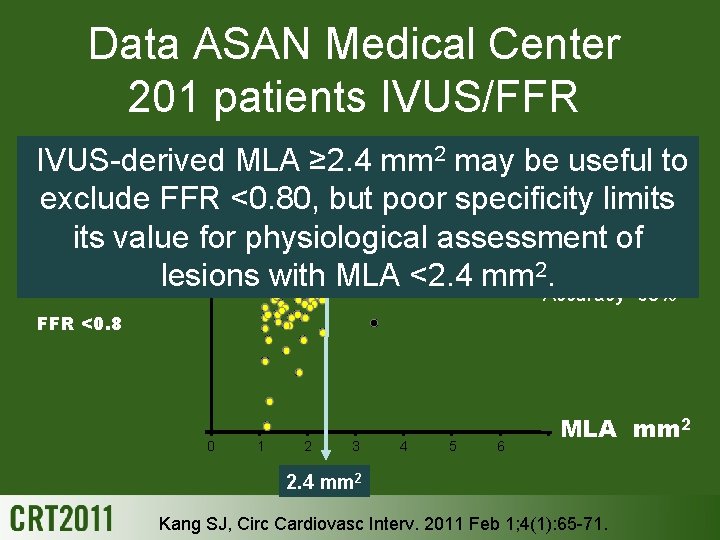
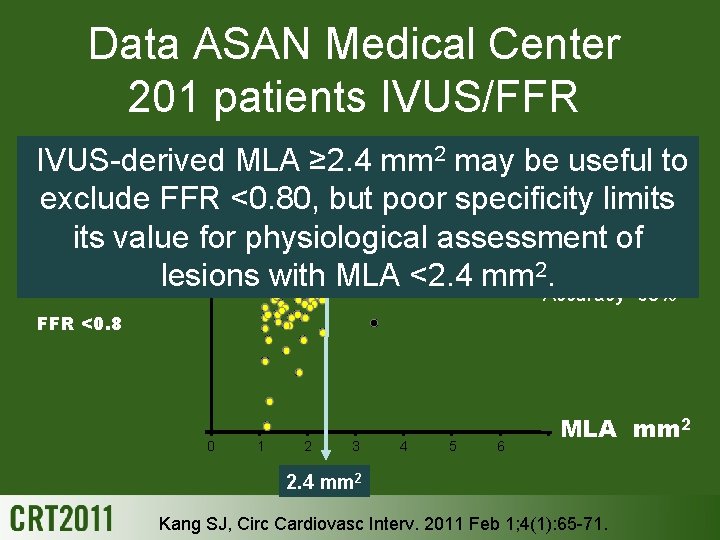
Data ASAN Medical Center 201 patients IVUS/FFR IVUS-derived MLA ≥ 2. 4 mm 2 may be useful to Sensitivity=90% exclude FFR <0. 80, but poor specificity limits Specificity=60% FFR >0. 8 its value for physiological assessment of PPV=37% 0. 8 lesions with MLA <2. 4 mm 2 NPV=96%. Accuracy=68% FFR <0. 8 0 1 2 3 4 5 6 MLA mm 2 2. 4 mm 2 Kang SJ, Circ Cardiovasc Interv. 2011 Feb 1; 4(1): 65 -71.
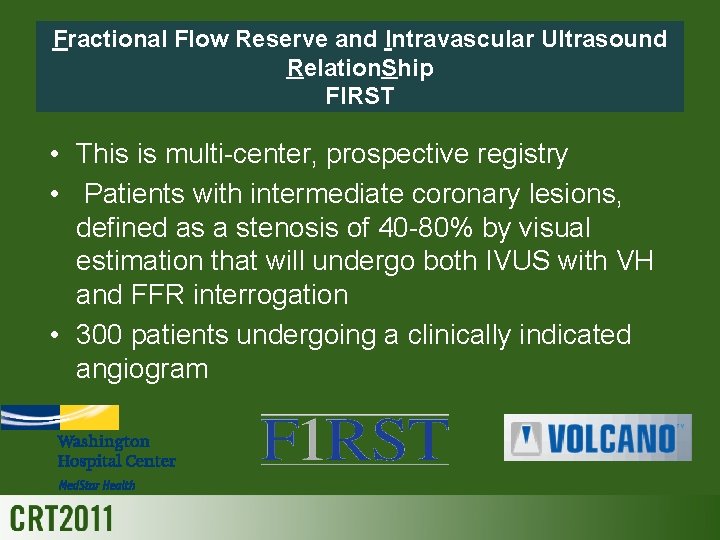
Fractional Flow Reserve and Intravascular Ultrasound Relation. Ship FIRST • This is multi-center, prospective registry • Patients with intermediate coronary lesions, defined as a stenosis of 40 -80% by visual estimation that will undergo both IVUS with VH and FFR interrogation • 300 patients undergoing a clinically indicated angiogram
Conclusions IVUS/FFR correlation • Anatomic parameters of intermediate coronary lesions obtained by IVUS showed a moderate correlation to the FFR values in medium and large vessel diameters • IVUS cut-off parameter for ischemia: Major epicardial coronary artery: changes with reference vessel diameter and MLA <4 mm 2 does not always imply physiological ischemia • Anatomic parameters of intermediate coronary lesions obtained by IVUS should take into account the reference vessel size
Conclusions IVUS/FFR correlation • Incorrect: “less than four, let`s stent some more” • Correct: “more than four, let`s head for the door”