What is Familial Chylomicronemia Syndrome Familial Chylomicronemia Syndrome




- Slides: 35




What is Familial Chylomicronemia Syndrome? • Familial Chylomicronemia Syndrome (FCS) – Rare genetic disorder characterized by severe elevations in circulating triglycerides – Triglyceride levels are commonly from 10 to 100 times greater than normal – Fat is commonly deposited in skin, eyes, and other organs – Severe hypertriglyceridemia predisposes to pancreatitis Al Azkawi H, et al. Case Rep Med. 2010; 2010: 807434. Gaudet D, et al. N Engl J Med. 2014; 371: 2200 -2206.
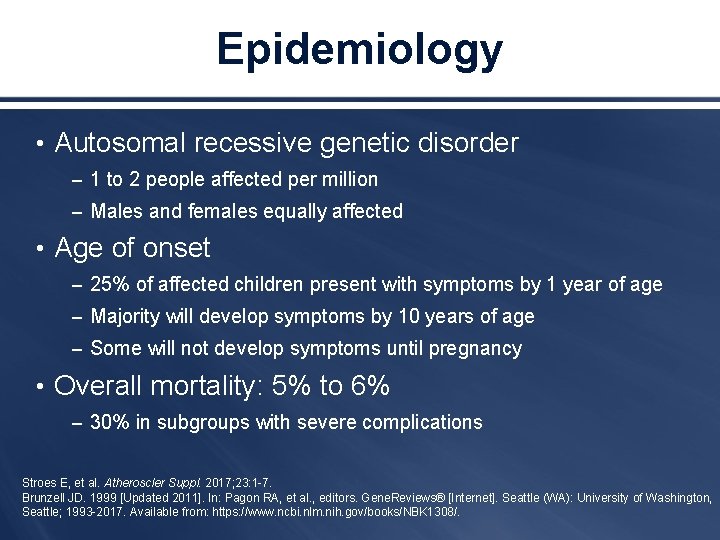
Epidemiology • Autosomal recessive genetic disorder – 1 to 2 people affected per million – Males and females equally affected • Age of onset – 25% of affected children present with symptoms by 1 year of age – Majority will develop symptoms by 10 years of age – Some will not develop symptoms until pregnancy • Overall mortality: 5% to 6% – 30% in subgroups with severe complications Stroes E, et al. Atheroscler Suppl. 2017; 23: 1 -7. Brunzell JD. 1999 [Updated 2011]. In: Pagon RA, et al. , editors. Gene. Reviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993 -2017. Available from: https: //www. ncbi. nlm. nih. gov/books/NBK 1308/.
Mechanisms of Disease • Mutations in lipoprotein lipase (LPL) gene – Encodes the enzyme responsible for catabolism of TGs or • Genes related to LPL function – Apo. C 2, apo. A 5, LMF 1, and GPIHBP 1 • Patients are unable to clear circulating TGs, resulting in plasma chylomicron accumulation TGs = triglycerides; Apo = apolipoprotein; LMF 1 = lipase maturation factor 1; GPIHBP 1 = glycosylphosphatidylinositol anchored high density lipoprotein binding protein 1. Chokshi N, et al. J Clin Lipidol. 2014; 8: 287– 295.
Identification of Patients with FCS: Symptom Recognition and Differential Diagnosis
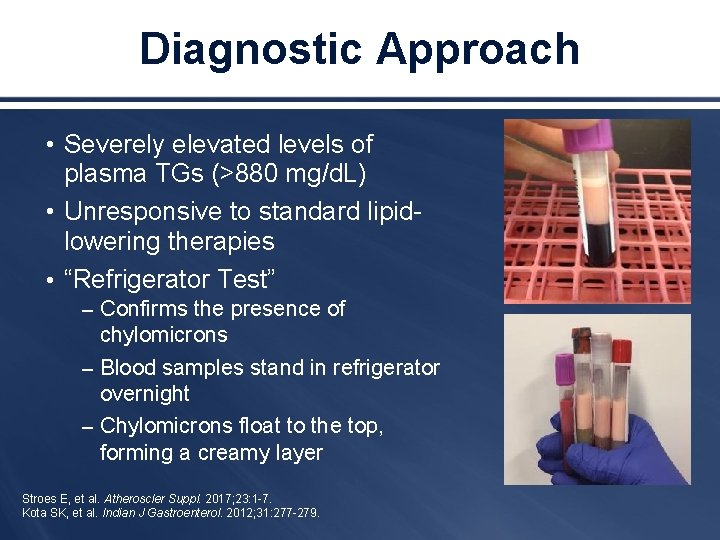
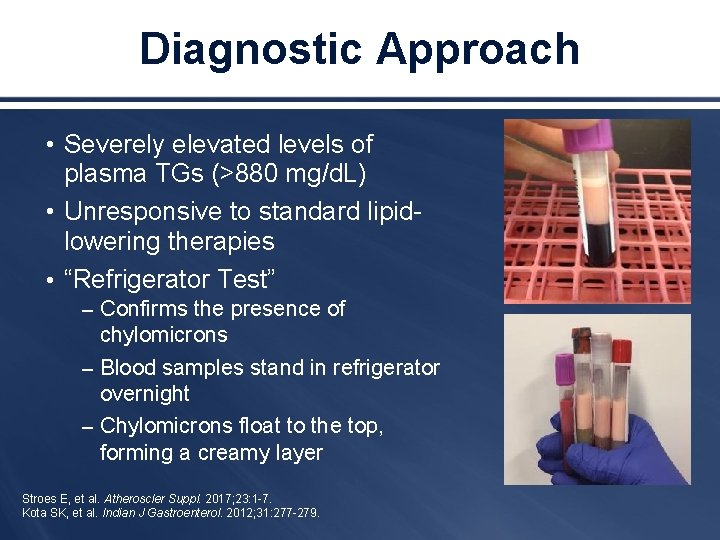
Diagnostic Approach • Severely elevated levels of plasma TGs (>880 mg/d. L) • Unresponsive to standard lipidlowering therapies • “Refrigerator Test” – Confirms the presence of chylomicrons – Blood samples stand in refrigerator overnight – Chylomicrons float to the top, forming a creamy layer Stroes E, et al. Atheroscler Suppl. 2017; 23: 1 -7. Kota SK, et al. Indian J Gastroenterol. 2012; 31: 277 -279.
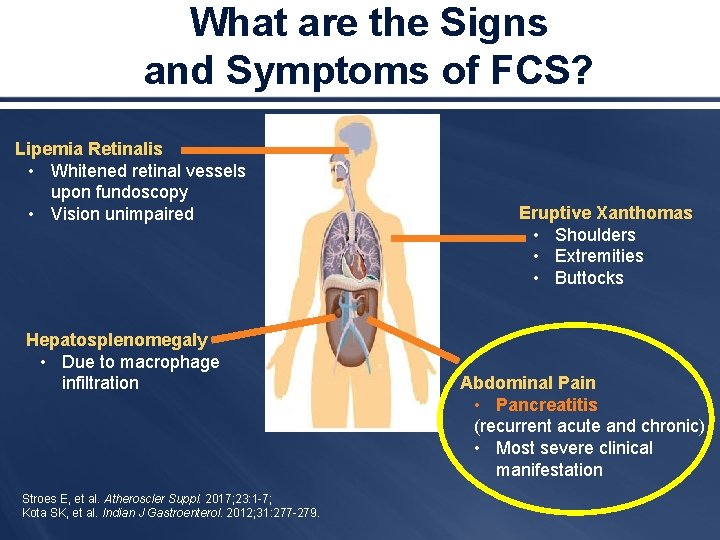
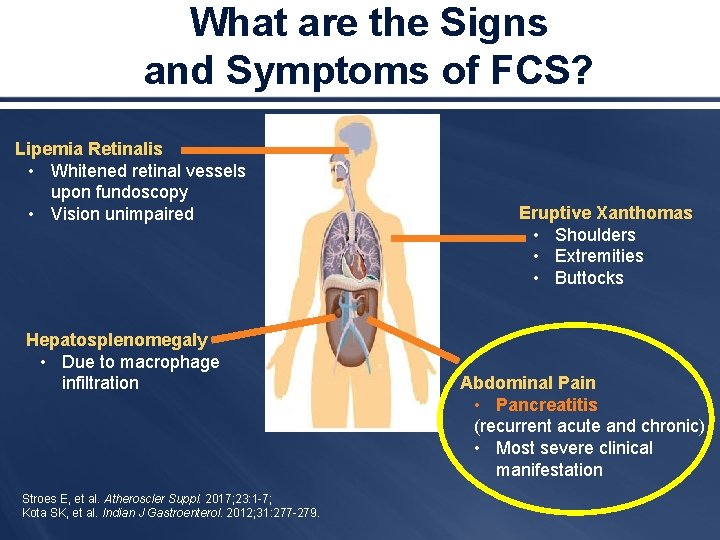
What are the Signs and Symptoms of FCS? Lipemia Retinalis • Whitened retinal vessels upon fundoscopy • Vision unimpaired Hepatosplenomegaly • Due to macrophage infiltration Stroes E, et al. Atheroscler Suppl. 2017; 23: 1 -7; Kota SK, et al. Indian J Gastroenterol. 2012; 31: 277 -279. Eruptive Xanthomas • Shoulders • Extremities • Buttocks Abdominal Pain • Pancreatitis (recurrent acute and chronic) • Most severe clinical manifestation
When Do Symptoms of FCS Occur? • Generally presents in late childhood or adolescence • Infants – Acute pancreatitis in infants can present in 25% of cases – Cases in neonates have been reported § Consider symptoms: anemia, jaundice, pallor, irritability, diarrhea Stroes E, et al. Atheroscler Suppl. 2017; 23: 1 -7. Kota SK, et al. Indian J Gastroenterol. 2012; 31: 277 -279.
When Should FCS be Suspected? ü Severe HTG presenting in childhood or infancy – Secondary causes (eg, uncontrolled diabetes, alcohol abuse) have been ruled out ü TG levels >1000 mg/d. L (fasting) or 2000 mg/d. L (non-fasting) – Low or normal LDL, normal HDL ü Recurrent episodes of abdominal pain, with or without recurrent pancreatitis ü Presence of other symptoms, such as fatigue, malaise, and cognitive impairment ü Family history of FCS Ahmad Z, et al. Expert Rev Clin Pharm. 2017; 10: 1 -3; Al Azkawi H, et al. Case Rep Med. 2010; 2010: 807434; Brunzell JD. 1999 [Updated 2011]. In: Pagon RA, et al. , editors. Gene. Reviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993 -2017. Available from: https: //www. ncbi. nlm. nih. gov/books/NBK 1308/
Confirming a Diagnosis of FCS • Refer to lipid specialist • Diagnostic gold standard: – Full LPL gene sequencing – Cofactor gene sequencing § LMF 1, GPIHBP 1, apo. C 2, apo. A 5 • When a patient is diagnosed with FCS, at-risk siblings should also be tested Stroes E, et al. Atheroscler Suppl. 2017; 23: 1 -7; Brunzell JD. 1999 [Updated 2011]. In: Pagon RA, et al. , editors. Gene. Reviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993 -2017. Available from: https: //www. ncbi. nlm. nih. gov/books/NBK 1308/.
Complications of FCS: Focus on Pancreatitis
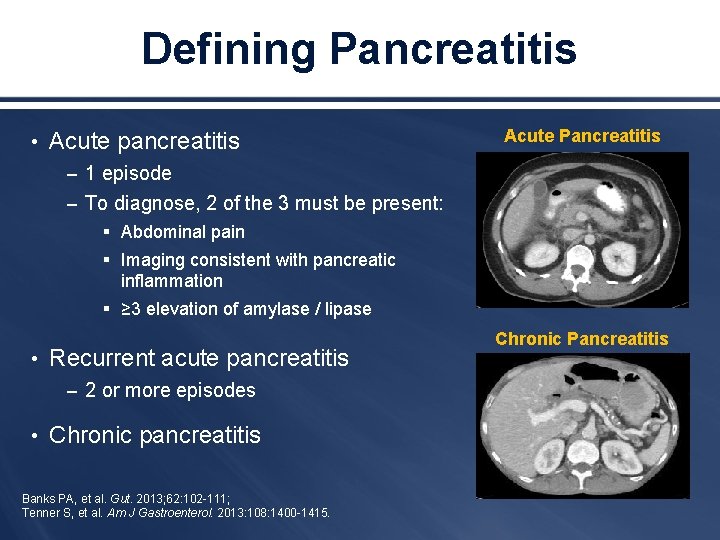
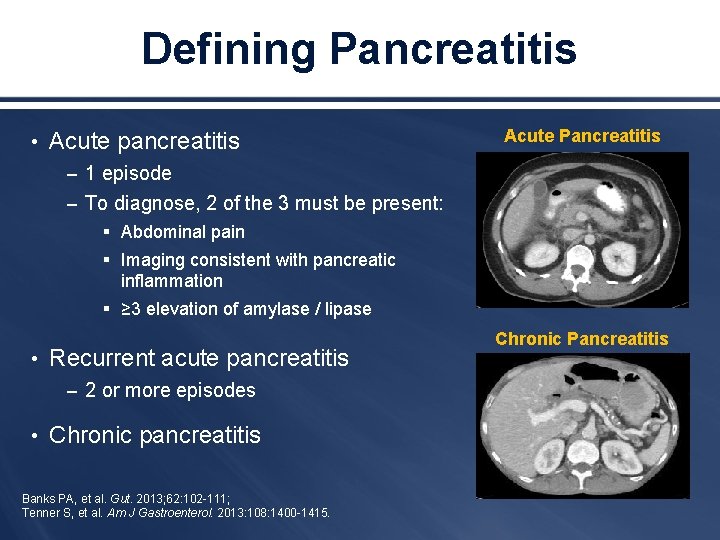
Defining Pancreatitis • Acute pancreatitis Acute Pancreatitis – 1 episode – To diagnose, 2 of the 3 must be present: § Abdominal pain § Imaging consistent with pancreatic inflammation § ≥ 3 elevation of amylase / lipase • Recurrent acute pancreatitis – 2 or more episodes • Chronic pancreatitis Banks PA, et al. Gut. 2013; 62: 102 -111; Tenner S, et al. Am J Gastroenterol. 2013: 108: 1400 -1415. Chronic Pancreatitis
Pancreatitis: Life-threatening Complication of FCS • Pancreatitis is a life-threatening complication of FCS. • FCS accounts for approximately 7% of all pancreatitis cases (or more). • Recurrent pancreatitis can lead to chronic pancreatitis. • Important to reduce triglycerides to prevent episodes of pancreatitis. • Standard of care and pain management is recommended for acute pancreatitis. Al Azkawi H, et al. Case Rep Med. 2010; 2010: 807434; Sisman G, et al. Hepatobiliary Pancreat Dis Int. 2014; 13: 209 -214; Gardner TB, et al. Pancreas. 2010; 39: 498 -501; Brunzell JD. 1999 [Updated 2011]. In: Pagon RA, et al. , editors. Gene. Reviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993 -2017. Available from: https: //www. ncbi. nlm. nih. gov/books/NBK 1308/.
How Does FCS Triggers Pancreatitis? • Increased pancreatic lipase secretion due to overstimulation: – Fatty meals – Alcohol abuse • Hypoperfusion due to: – High plasma viscosity – Erythrocyte aggregation induced by high plasma chylomicron and VLDL concentrations VLDL = very-low-density lipoprotein. Lennertz A, et al. Ther Apher. 1999; 3: 227 -233; Tenner S, et al. Am J Gastroenterol. 2013: 108: 1400 -1415.
Pancreatitis: Patient Presentation • Severe epigastric pain – Radiates to flank and/or back – Frequently triggered by meals or excessive alcohol intake • Nausea, vomiting • If severe, can present with organ failure (respiratory, kidney, vascular) Banks PA, et al. Gut. 2013; 62: 102 -111; Tenner S, et al. Am J Gastroenterol. 2013: 108: 1400 -1415.
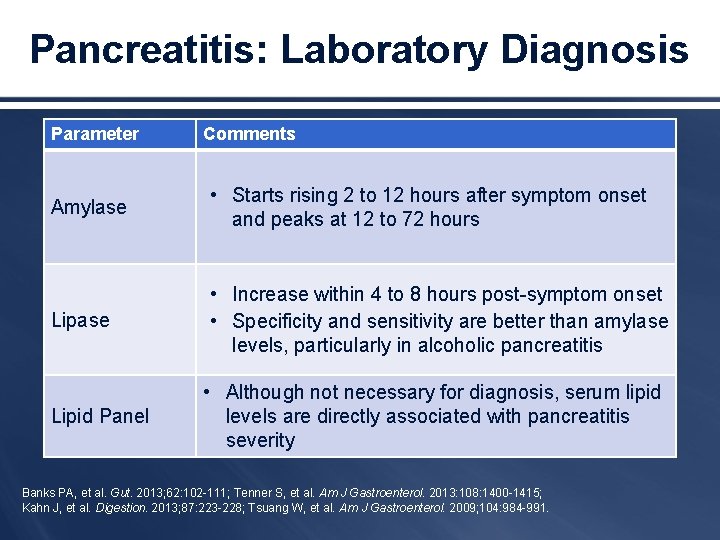
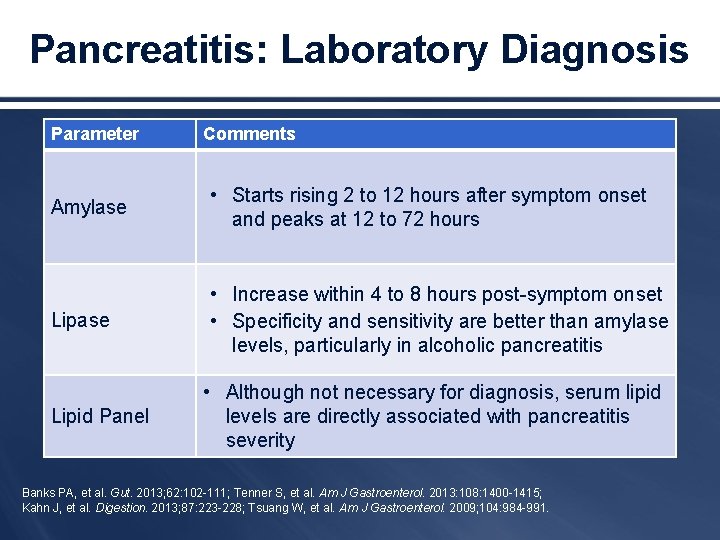
Pancreatitis: Laboratory Diagnosis Parameter Comments Amylase • Starts rising 2 to 12 hours after symptom onset and peaks at 12 to 72 hours Lipase • Increase within 4 to 8 hours post-symptom onset • Specificity and sensitivity are better than amylase levels, particularly in alcoholic pancreatitis Lipid Panel • Although not necessary for diagnosis, serum lipid levels are directly associated with pancreatitis severity Banks PA, et al. Gut. 2013; 62: 102 -111; Tenner S, et al. Am J Gastroenterol. 2013: 108: 1400 -1415; Kahn J, et al. Digestion. 2013; 87: 223 -228; Tsuang W, et al. Am J Gastroenterol. 2009; 104: 984 -991.
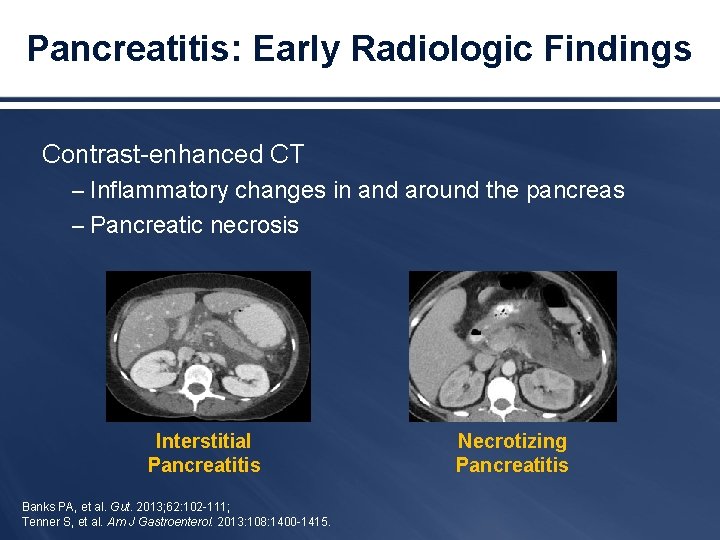
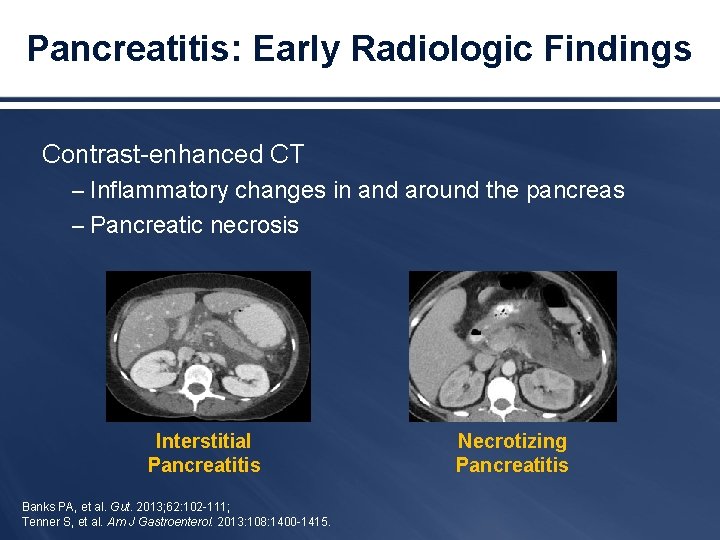
Pancreatitis: Early Radiologic Findings Contrast-enhanced CT – Inflammatory changes in and around the pancreas – Pancreatic necrosis Interstitial Pancreatitis Banks PA, et al. Gut. 2013; 62: 102 -111; Tenner S, et al. Am J Gastroenterol. 2013: 108: 1400 -1415. Necrotizing Pancreatitis
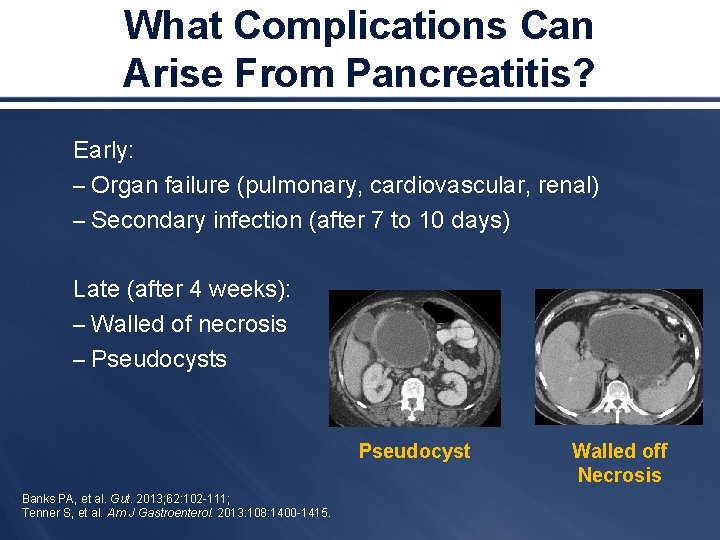
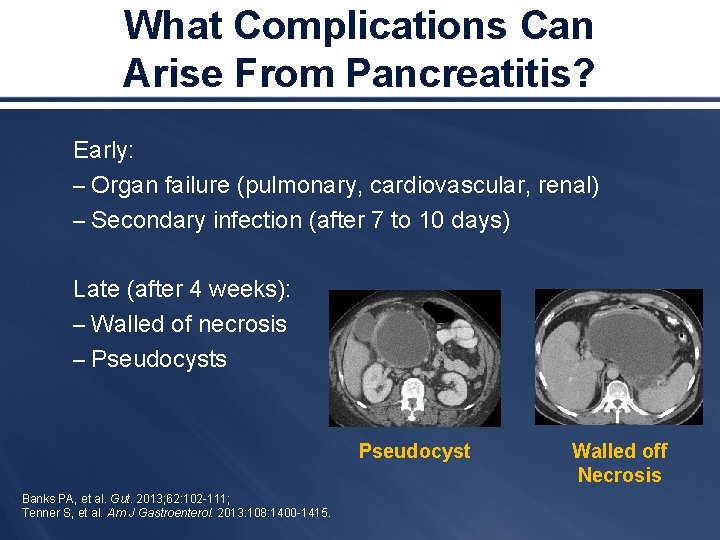
What Complications Can Arise From Pancreatitis? Early: – Organ failure (pulmonary, cardiovascular, renal) – Secondary infection (after 7 to 10 days) Late (after 4 weeks): – Walled of necrosis – Pseudocysts Pseudocyst Banks PA, et al. Gut. 2013; 62: 102 -111; Tenner S, et al. Am J Gastroenterol. 2013: 108: 1400 -1415. Walled off Necrosis
Pancreatitis: General Management • Supportive therapy – Aggressive IV rehydration – Analgesia – Antiemetic – Enteral feeding in some patients • No proven medical therapies currently exist for acute pancreatitis Tenner S, et al. Am J Gastroenterol. 2013: 108: 1400 -1415; Wu BU, et al. Gastroenterology. 2009; 137: 129 -135.
Pancreatitis in FCS: Special Considerations • Interventions – Dietary management – Exercise – Avoidance of alcohol and tobacco – Lipid-lowering medication (poor results) – Repeated plasmapheresis § Used as a prophylactic measure in patients unresponsive to diet and medicine – Endoscopic treatment if complications from pancreatitis present Sisman G, et al. Hepatobiliary Pancreat Dis Int. 2014; 13: 209 -214.
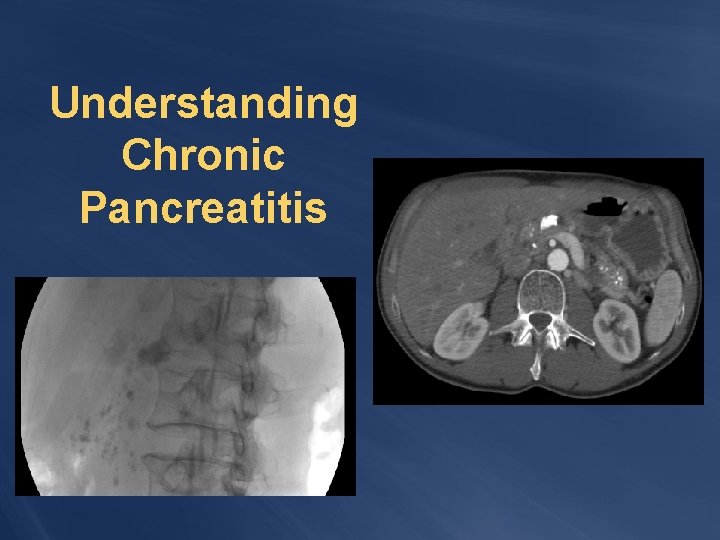
Understanding Chronic Pancreatitis
From Chronic Pancreatitis Presentation and Complications • Pain can be mild-to-severe / debilitating • Type 3 c diabetes mellitus • Exocrine pancreatic insufficiency – Treated with pancreatic enzyme replacement therapy • Others: – Vitamin deficiency – Metabolic bone disease Fieker A, et al. Clin Exp Gastroenterol. 2011; 4: 55 -73; Rickels MR, et al. Pancreatology. 2013; 13: 336 -342; Ewald N, et al. World J Gastroenterol. 2013; 19: 7276 -7281; Malka D, et al. Gastroenterology. 2000; 119: 1324 -1332.
From Chronic Pancreatitis to Pancreatogenic Diabetes • Diabetes secondary to chronic pancreatitis • Classified as Type 3 c diabetes mellitus • Complex metabolic situation, with destruction of: – Islet cells due to pancreatic inflammation – Glucagon secreting alpha-cells – Pancreatic polypeptide secreting cells Rickels MR, et al. Pancreatology. 2013; 13: 336 -342. Ewald N, et al. World J Gastroenterol. 2013; 19: 7276 -7281.
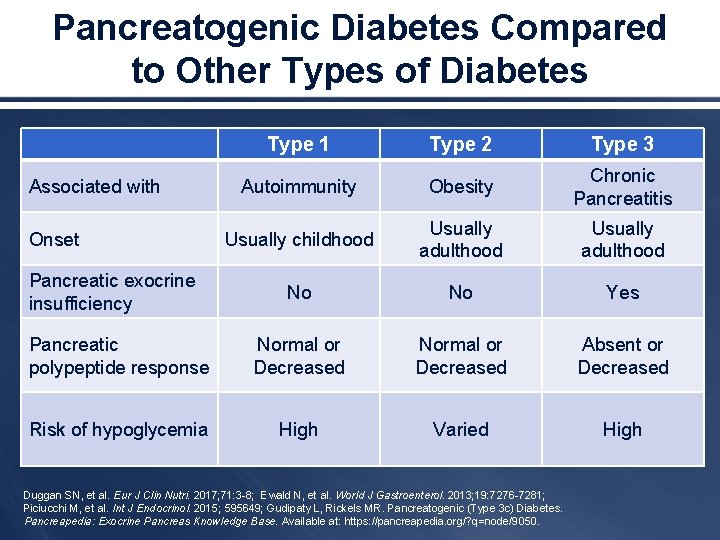
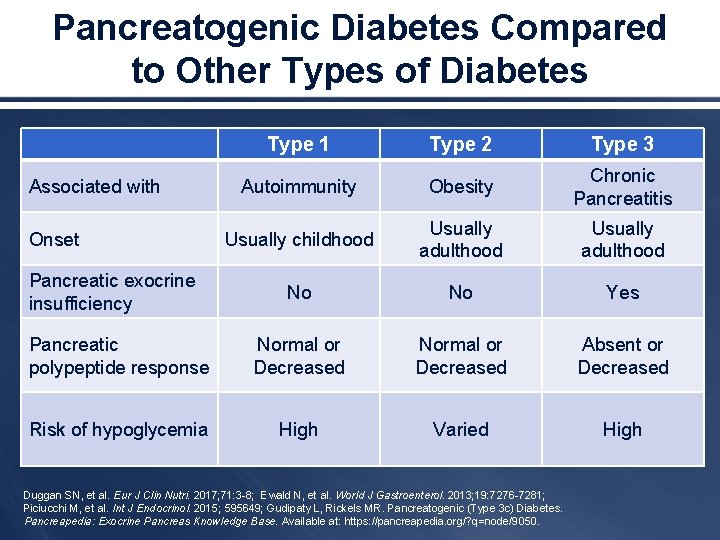
Pancreatogenic Diabetes Compared to Other Types of Diabetes Type 1 Type 2 Type 3 Autoimmunity Obesity Chronic Pancreatitis Usually childhood Usually adulthood No No Yes Pancreatic polypeptide response Normal or Decreased Absent or Decreased Risk of hypoglycemia High Varied High Associated with Onset Pancreatic exocrine insufficiency Duggan SN, et al. Eur J Clin Nutri. 2017; 71: 3 -8; Ewald N, et al. World J Gastroenterol. 2013; 19: 7276 -7281; Piciucchi M, et al. Int J Endocrinol. 2015; 595649; Gudipaty L, Rickels MR. Pancreatogenic (Type 3 c) Diabetes. Pancreapedia: Exocrine Pancreas Knowledge Base. Available at: https: //pancreapedia. org/? q=node/9050.
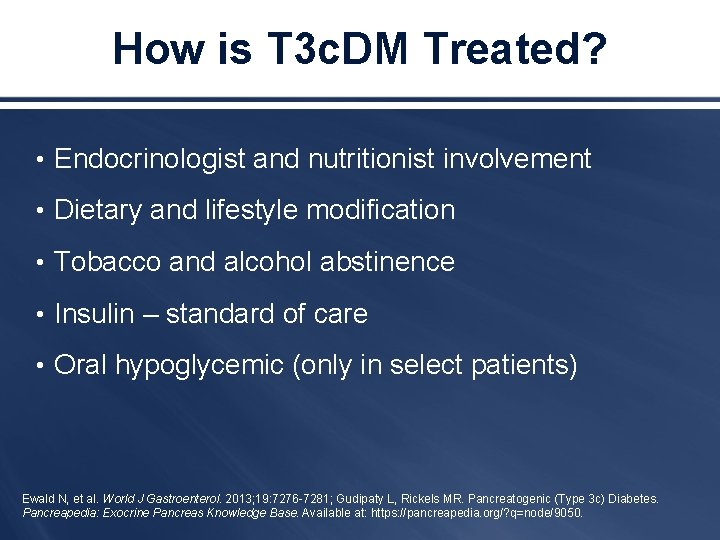
How is T 3 c. DM Treated? • Endocrinologist and nutritionist involvement • Dietary and lifestyle modification • Tobacco and alcohol abstinence • Insulin – standard of care • Oral hypoglycemic (only in select patients) Ewald N, et al. World J Gastroenterol. 2013; 19: 7276 -7281; Gudipaty L, Rickels MR. Pancreatogenic (Type 3 c) Diabetes. Pancreapedia: Exocrine Pancreas Knowledge Base. Available at: https: //pancreapedia. org/? q=node/9050.
Management of Patients with FCS: Available and Emerging Interventions
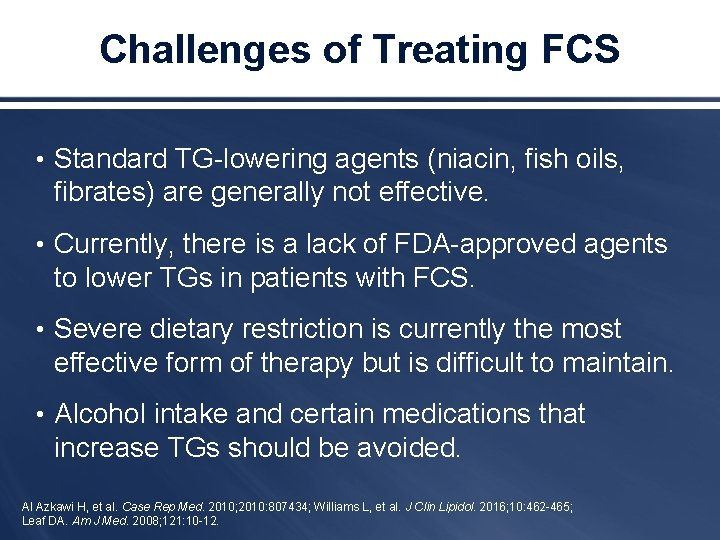
Challenges of Treating FCS • Standard TG-lowering agents (niacin, fish oils, fibrates) are generally not effective. • Currently, there is a lack of FDA-approved agents to lower TGs in patients with FCS. • Severe dietary restriction is currently the most effective form of therapy but is difficult to maintain. • Alcohol intake and certain medications that increase TGs should be avoided. Al Azkawi H, et al. Case Rep Med. 2010; 2010: 807434; Williams L, et al. J Clin Lipidol. 2016; 10: 462 -465; Leaf DA. Am J Med. 2008; 121: 10 -12.
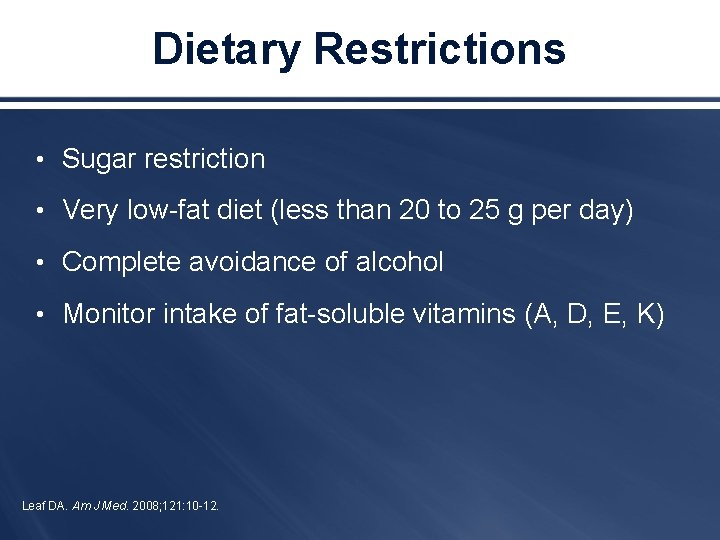
Dietary Restrictions • Sugar restriction • Very low-fat diet (less than 20 to 25 g per day) • Complete avoidance of alcohol • Monitor intake of fat-soluble vitamins (A, D, E, K) Leaf DA. Am J Med. 2008; 121: 10 -12.
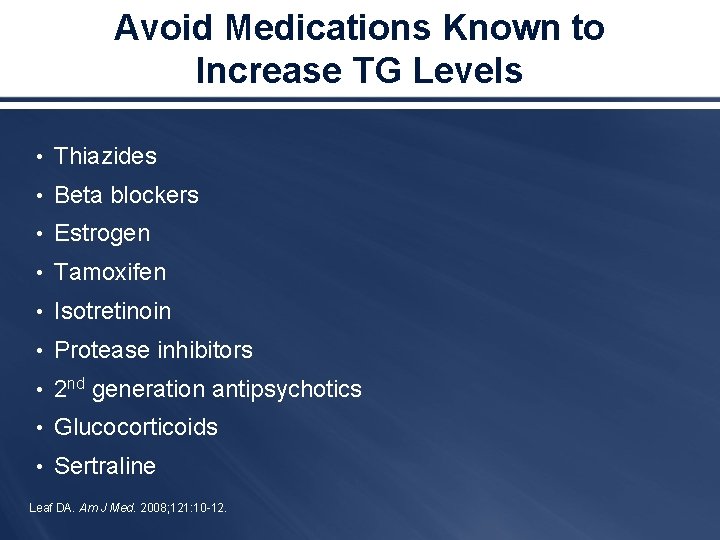
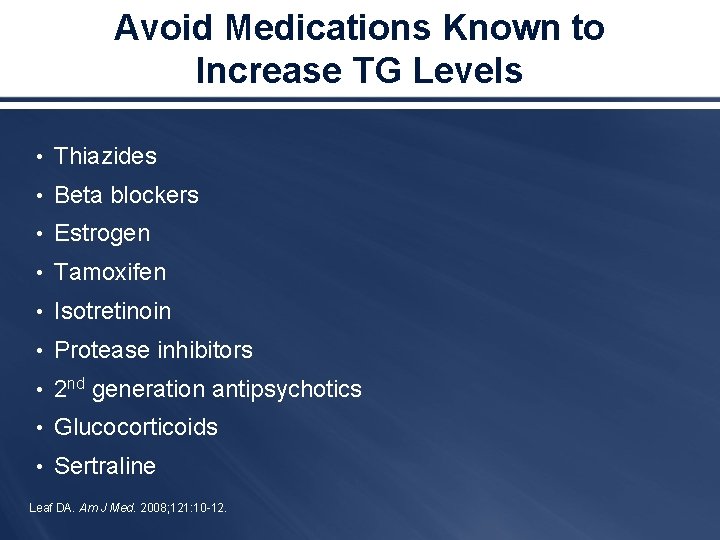
Avoid Medications Known to Increase TG Levels • Thiazides • Beta blockers • Estrogen • Tamoxifen • Isotretinoin • Protease inhibitors • 2 nd generation antipsychotics • Glucocorticoids • Sertraline Leaf DA. Am J Med. 2008; 121: 10 -12.
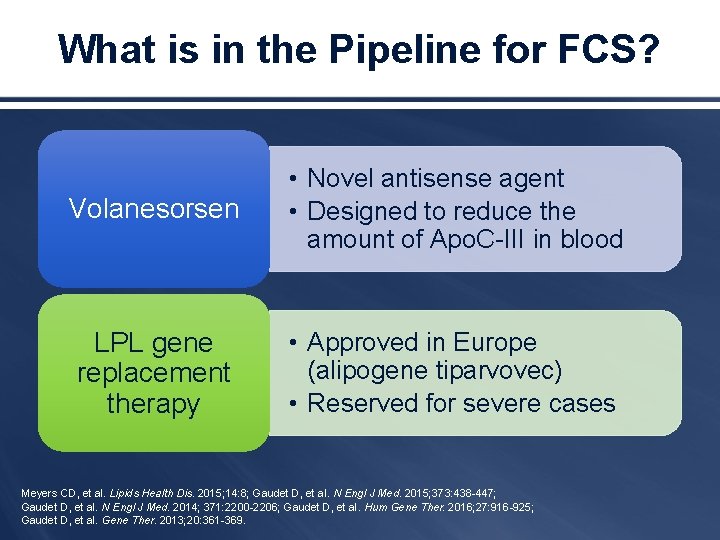
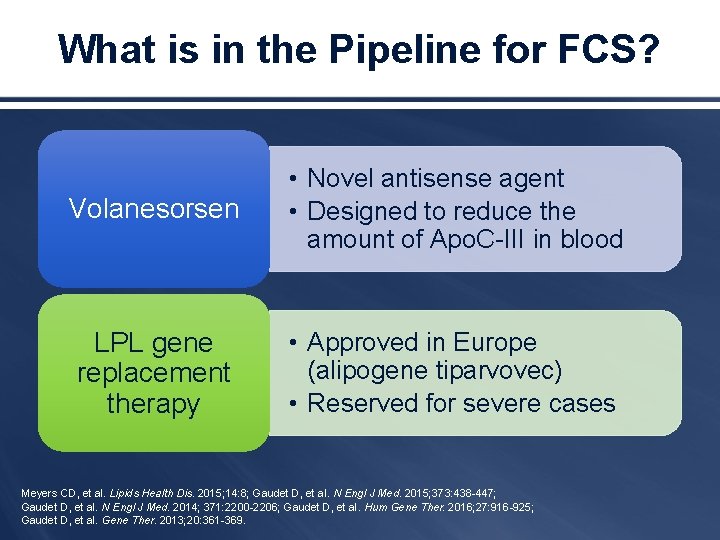
What is in the Pipeline for FCS? Volanesorsen • Novel antisense agent • Designed to reduce the amount of Apo. C-III in blood LPL gene replacement therapy • Approved in Europe (alipogene tiparvovec) • Reserved for severe cases Meyers CD, et al. Lipids Health Dis. 2015; 14: 8; Gaudet D, et al. N Engl J Med. 2015; 373: 438 -447; Gaudet D, et al. N Engl J Med. 2014; 371: 2200 -2206; Gaudet D, et al. Hum Gene Ther. 2016; 27: 916 -925; Gaudet D, et al. Gene Ther. 2013; 20: 361 -369.
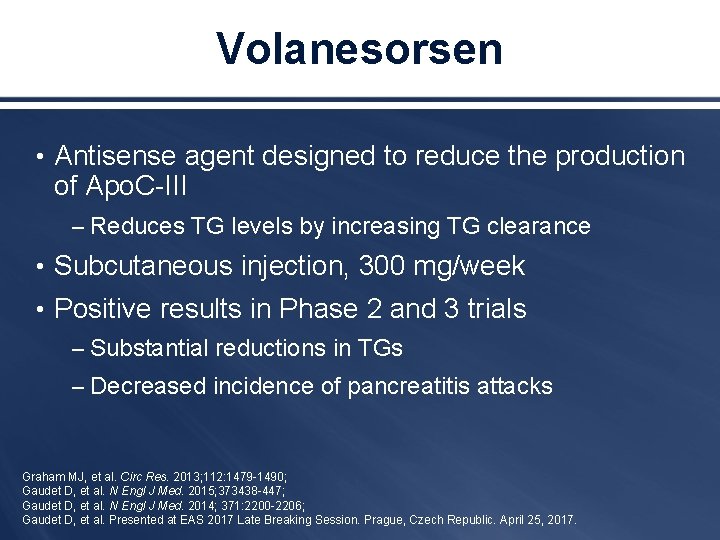
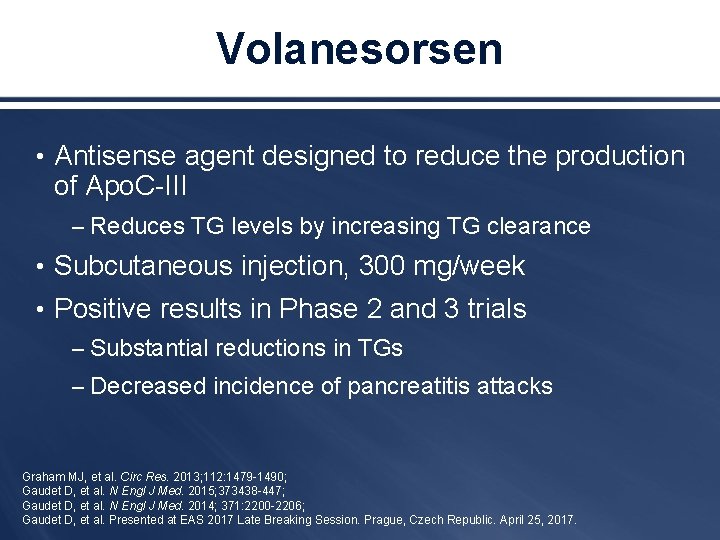
Volanesorsen • Antisense agent designed to reduce the production of Apo. C-III – Reduces TG levels by increasing TG clearance • Subcutaneous injection, 300 mg/week • Positive results in Phase 2 and 3 trials – Substantial reductions in TGs – Decreased incidence of pancreatitis attacks Graham MJ, et al. Circ Res. 2013; 112: 1479 -1490; Gaudet D, et al. N Engl J Med. 2015; 373438 -447; Gaudet D, et al. N Engl J Med. 2014; 371: 2200 -2206; Gaudet D, et al. Presented at EAS 2017 Late Breaking Session. Prague, Czech Republic. April 25, 2017.
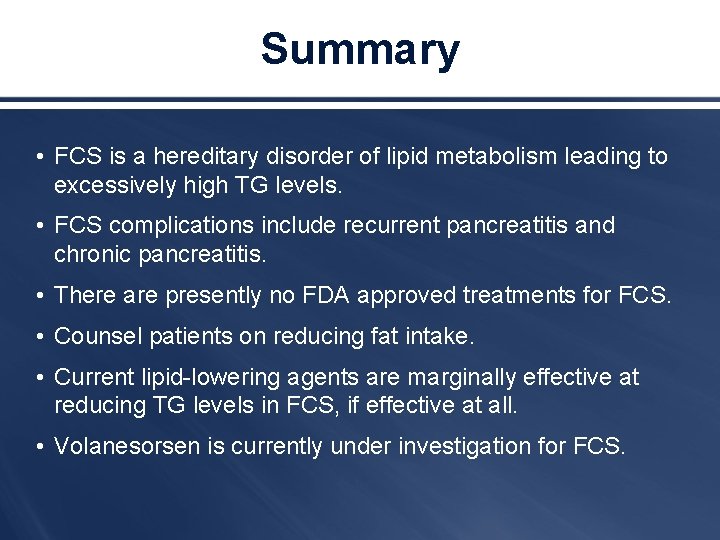
Summary • FCS is a hereditary disorder of lipid metabolism leading to excessively high TG levels. • FCS complications include recurrent pancreatitis and chronic pancreatitis. • There are presently no FDA approved treatments for FCS. • Counsel patients on reducing fat intake. • Current lipid-lowering agents are marginally effective at reducing TG levels in FCS, if effective at all. • Volanesorsen is currently under investigation for FCS.
 Familial down syndrome
Familial down syndrome Monoploidy
Monoploidy Familial down syndrome
Familial down syndrome Danette format familial
Danette format familial Dr pattan casper wy
Dr pattan casper wy Communauté universelle
Communauté universelle Familial hypocalciuric hypercalcemia
Familial hypocalciuric hypercalcemia Familial roots
Familial roots Familial hypertriglyceridemia
Familial hypertriglyceridemia Mild hypercalcemia
Mild hypercalcemia Fetal valproate syndrome
Fetal valproate syndrome Marfan syndrome face
Marfan syndrome face Joint hypermobility syndrome symptoms
Joint hypermobility syndrome symptoms Assistive devices for carpal tunnel syndrome
Assistive devices for carpal tunnel syndrome Mackler triad boerhaave's syndrome
Mackler triad boerhaave's syndrome Angiocholite
Angiocholite Concept map of assessment
Concept map of assessment Livedo mortis
Livedo mortis Reflow syndrome
Reflow syndrome Waist circumference metabolic syndrome
Waist circumference metabolic syndrome Mgt411
Mgt411 Wernicke-korsakoff syndrome
Wernicke-korsakoff syndrome Sheehan syndrome
Sheehan syndrome Introduction of liver
Introduction of liver Syndrome
Syndrome Syndrome de chilaiditi traitement
Syndrome de chilaiditi traitement Voie motrice pyramidale
Voie motrice pyramidale Patm syndrome
Patm syndrome Acute glomerulonephritis causes
Acute glomerulonephritis causes Syndrome hepato renal
Syndrome hepato renal Mast cell activation syndrome
Mast cell activation syndrome Critique of feifer assessment of reading
Critique of feifer assessment of reading Crush syndrome
Crush syndrome Photo maladie de cushing
Photo maladie de cushing Geriatric syndrome
Geriatric syndrome Fhf
Fhf