Dementia It is defined as a chronic confusional
- Slides: 26
Dementia • It is defined as a chronic confusional state characterized by an acquired deterioration in cognitive abilities that impairs the successful performance of activities of daily living. • Memory is the most common cognitive ability lost with dementia • Other mental faculties are also affected in dementia, such as language, visuospatial ability, calculation, judgment, and problem solving
• Confusion is the disorientation in space & time. • In dementia there is chronic (long) history of disorientation without fluctuation in level of consciousness while in acute confusional state there is short history of disorientation associated with fluctuation in level of consciousness.
• Approximately 15% of the population over 65 years of age suffer from Alzheimer disease. At the age of 85 & above, this rises to over 45%.
Common Causes of Dementia Alzheimer disease (60 – 70%) of the cases • Vascular dementia (10 – 20%) which is of 2 types : - Multi-infarct (large vessels & small vessels) - Diffuse white matter disease (Binswanger’s disease) • Parkinson’s disease (in ~25% of cases) • Alcoholism • Drug intoxication
Reversible causes of dementia • About 10% of cases of dementia are reversible (treatable), their diagnosis, thus, is extremely vital. • These include: - Normal pressure hydrocephalus - Intracranial mass lesions like tumors - Chronic subdural hematoma - Vitamin B 12 deficiency - Hypothyroidism - Neurosyphilis
Other causes of dementia • • • Huntington disease Korsakoff syndrome Progressive supra-nuclear palsy Multi system atrophy Dementia pugilistica (Head injuries in boxers lead to diffuse brain damage) • Dialysis Dementia • Chronic renal failure • Prion diseases like Creutzfeldt-Jakob disease & caw madness.
Pseudo-dementia • About 15% of patients referred for evaluation of possible dementia instead have a functional disorder, such as endogenous depression. • Note: In real dementia (organic causes) the patient will give wrong answers during mental state examination while in pseudodementia he will give “I don’t know” response.
ALZHEIMER DISEASE • • most common cause of dementia in western countries. occurring mostly in patients over 45 years. Approximately 1% of cases are familial most often presents with subtle onset of memory loss followed by a slowly progressive dementia that spreading to language and visuospatial deficits over several years. • In the late stages delusions are common, & usually simple. 10% of patients develop the Capgras syndrome, believing that a caregiver has been replaced by an impostor. • In end-stage, patients become rigid, mute, incontinent, and bedridden. Myoclonus & generalized seizures may also occur • It’s typical duration is 5 to 10 years, but the course can range from 1 to 25 years.
Risk factors for Alzheimer disease: - increase age - female sex - family history - sleep deprivation - depression - low educational level - smoking - diabetes - obesity - hypertension - fatty diet
Factors favorably affect the risk of Alzheimer disease - cognitive engagement - physical activity - a low-fat and vegetable-rich diet - light to moderate alcohol intake
Pathologically there are: - Grossly: diffuse atrophy of the cerebral cortex with secondary enlargement of the ventricular system. - Microscopically: there are neuritic plaques containing amyloid, silver-staining neurofibrillary tangles (NFTs) in neuronal cytoplasm, and accumulation of amyloid in arterial walls of cerebral blood vessels - Biochemically: Cholinergic neurons are lost and the acetylcholine-synthesizing enzyme choline acetyltransferase is markedly depleted in the cerebral cortex and hippocampus. Degeneration of (1) the nucleus basalis of Meynert (the principal origin of cortical cholinergic innervation) and of (2) the cholinergic septal-hippocampal tract may underlie this biochemical abnormality
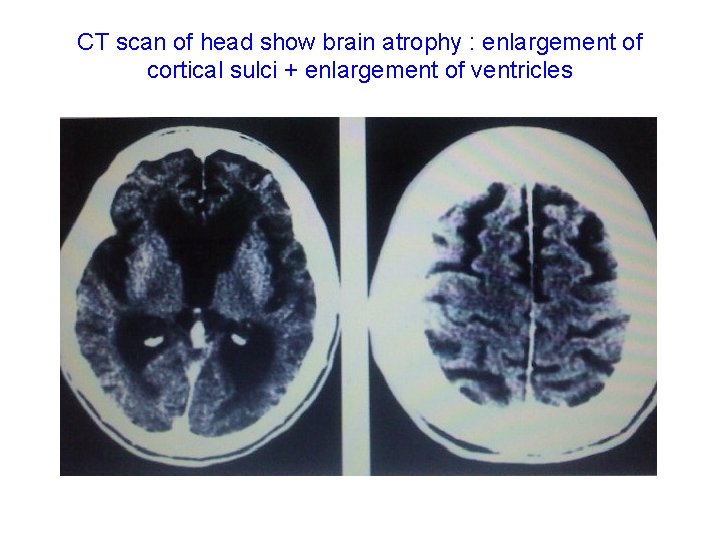
Investigations: CT scan & MRI: early in the course of the disease may be normal. But as the disease progress they will show diffuse atrophy of cerebral cortex (more posteriorly) + atrophy of hippocampus.
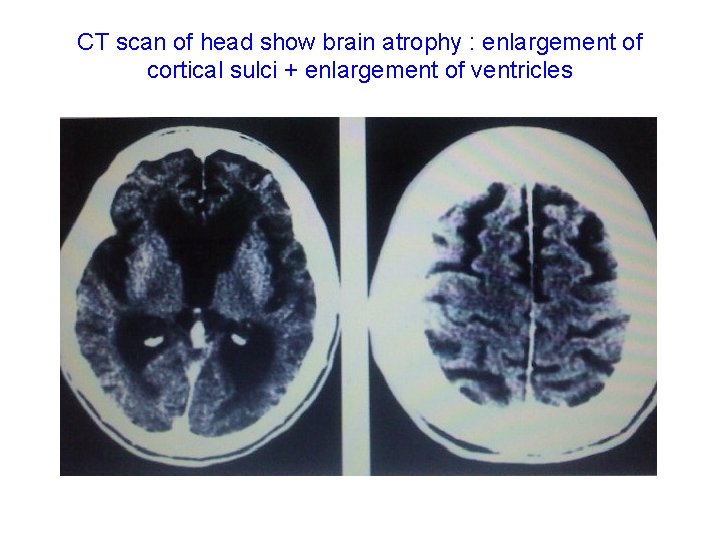
CT scan of head show brain atrophy : enlargement of cortical sulci + enlargement of ventricles
Treatment: • There is no curative treatment. • Just symptomatic. • Anticholinesterases such as Donepezil (5 mg/day for 1 month then increase to 10 mg/day), Rivastigmine (Exelon)® 1. 5– 6 mg/day and Galantamine 4– 12 mg/day. • The N-methyl D-aspartate receptor antagonist, Memantine (Ebixa)® 5 mg/day for 1 week then increased in steps of 5 mg at weekly intervals up to 20 mg/day in 2 divided doses shown some benefit. • All above drugs produce small improvement (about 5% only) in tests of cognitive function, for only 3 – 6 months then become placebo! • Ginkgo biloba 1 – 2 cap. /day lead to modest improvement in cognitive function by increase cerebral blood flow. • Piracetam (Nootropil)® 4. 8 g/day in divided doses for 3 weeks then reduced to 2. 4 g/day (or some time to 1. 2 g/day) in divided doses. • Behavioral disturbances respond to antipsychotics like Haloperidol (Serenace)® 0. 5 - 4 mg x 4 or novel antipsychotic like Risperidone (Risperidal)® 2 -4 mg/day in single non divided dose, antidepressants like Citalopram (Celexa)® (10, 20, 40 mg tab. ) 2040 mg/day, & anxiolytics.
Fronto-temporal Dementia • The fronto-temporal dementia, including Pick disease, sometimes can be distinguished from Alzheimer disease during life by: - their generally earlier onset, - more prominent behavioral (personality) than cognitive (memory) dysfunction at presentation, - preferential atrophy of the frontal and anterior temporal lobes on CT scan or MRI of the brain. • Definitive diagnosis is usually not possible during life, and relies instead on histo-pathological features which include the presence of Pick cells and Pick inclusion bodies, the absence of amyloid plaques and neurofibrillary tangles characteristic of Alzheimer disease, and the inclusions in neurons and glia that contain the microtubuleassociated protein, tau. • Familial occurrence of fronto-temporal dementia has been documented. • There is no specific treatment, just symptomatic.
Lewy Body dementia Parkinson disease is accompanied by dementia in ~25% of cases. Patients who develop dementia at least 1 year after the onset of motor symptoms (tremor, rigidity, bradykinesia, postural instability) are classified as having Parkinson disease with dementia, whereas those in whom dementia has its
In diffuse Lewy body disease, pathology similar to that found in the substantia nigra in Parkinson's disease is found in the cerebral cortex (i. e: Lewy bodies – an αsynuclein protein - exist in cerebral cortex also). This condition usually presents as cognitive impairment in the context of an extrapyramidal syndrome, and the cognitive features may be indistinguishable from those of Alzheimer disease. Patients' cognitive state often fluctuates; they have a high incidence of visual hallucinations, and are particularly sensitive to the sideeffects of anti-parkinsonian medications and also to neuroleptic medications. There is no specific treatment for this condition, although there may be clinical benefit with memantine & anticholinesterase agents such as Rivastigmine (Exelon)®
Wernicke-Korsakoff disease • Deficiency of thiamin (vitamin B 1) usually presents with an acute confusional state (Wernicke's encephalopathy) and brain-stem abnormalities such as ataxia, nystagmus and extraocular muscle weakness, particularly lateral rectus weakness. • If inadequately treated, this results in a dementia characterized by a profound disturbance of short-term memory associated with a tendency to confabulate (i. e: tendency to full the gabs in memory by imaginary events created by the patient), called Korsakoff's syndrome. • The deficiency can arise as a result of malnutrition (particularly when due to chronic alcohol misuse), malabsorption or even protracted vomiting (as in hyperemesis gravidarum). • The diagnosis is usually made clinically. • Because it is potentially treatable at the stage of Wernicke’s encephalopathy, the condition must be considered in any confused or demented patient; if there is any doubt, it is usually better to treat anyway. Treatment consists of intravenous thiamin 100 mg before or with dextrose to avoid exacerbating the disease. Parenteral thiamin should continue till patient regain the ability for normal dieting. In addition we should treating the underlying cause. • Once Korsakoff’s syndrome develop the condition became irreversible.
Normal-pressure hydrocephalus (NPH) • Uncommon. • consisting of an abnormal gait (gait apraxia), dementia (usually mild to moderate), and urinary incontinence. • Neuroimaging findings in NPH are those of a communicating (non-obstructive) hydrocephalus with a patent aqueduct of Sylvius. In many cases periventricular edema is present. There is no evidence of cortical or hippocampal atrophy. • Lumbar puncture findings include an opening pressure in the high-normal range and normal CSF sugar, cells, protein.
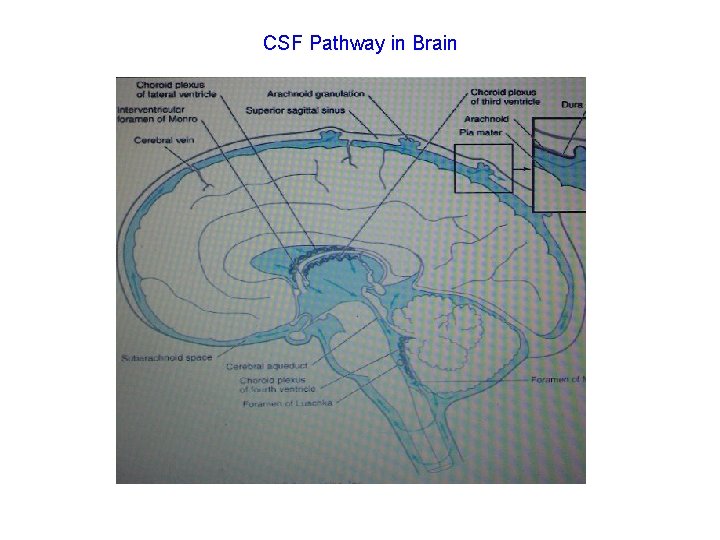
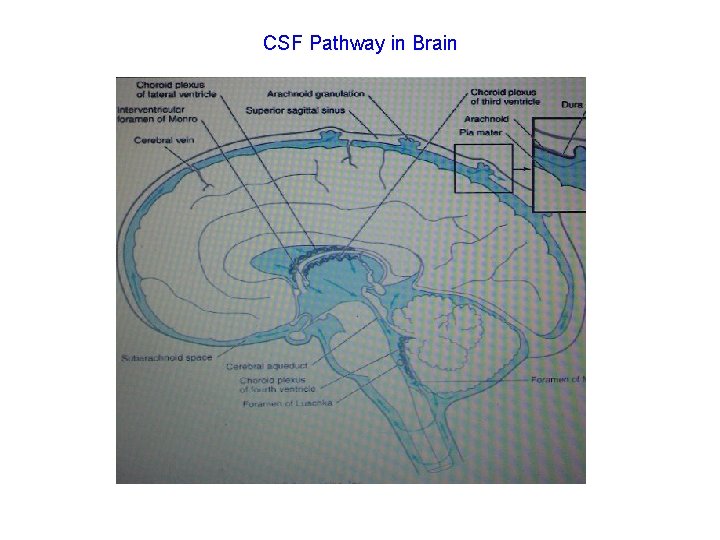
CSF Pathway in Brain
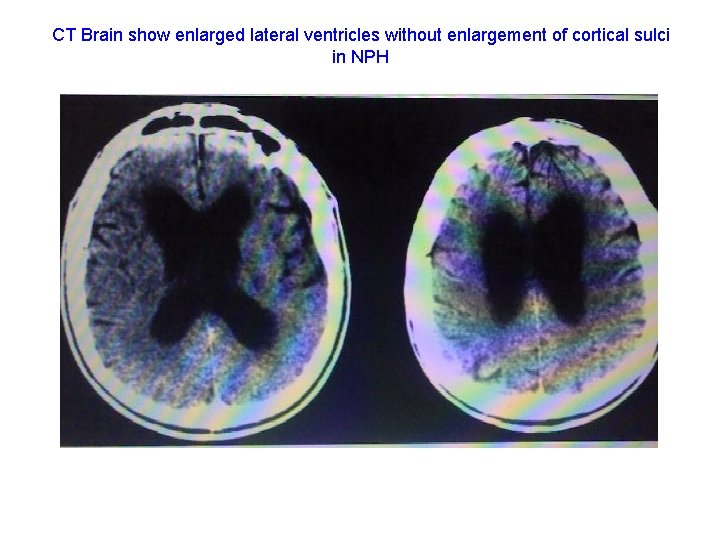
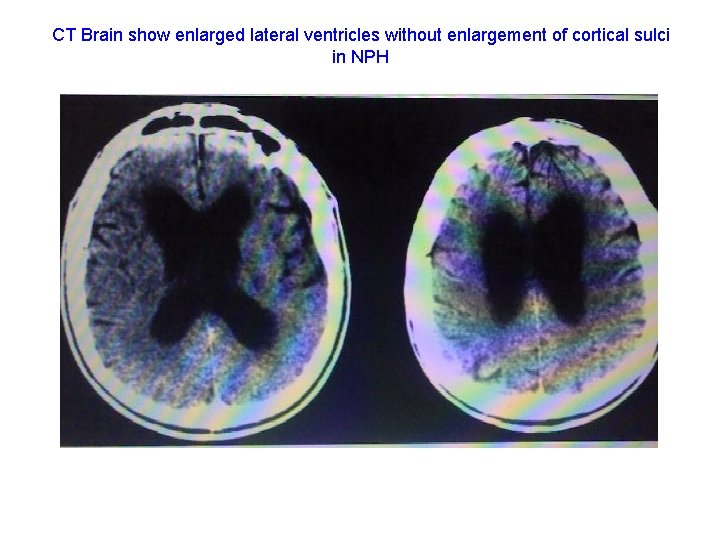
CT Brain show enlarged lateral ventricles without enlargement of cortical sulci in NPH
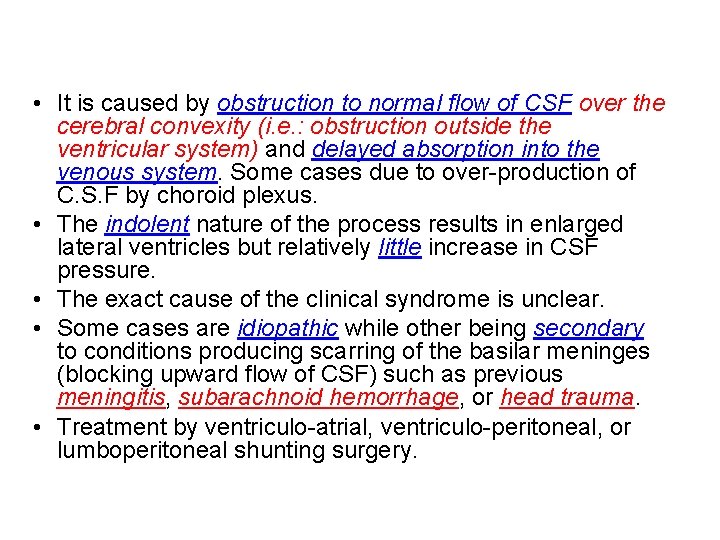
• It is caused by obstruction to normal flow of CSF over the cerebral convexity (i. e. : obstruction outside the ventricular system) and delayed absorption into the venous system. Some cases due to over-production of C. S. F by choroid plexus. • The indolent nature of the process results in enlarged lateral ventricles but relatively little increase in CSF pressure. • The exact cause of the clinical syndrome is unclear. • Some cases are idiopathic while other being secondary to conditions producing scarring of the basilar meninges (blocking upward flow of CSF) such as previous meningitis, subarachnoid hemorrhage, or head trauma. • Treatment by ventriculo-atrial, ventriculo-peritoneal, or lumboperitoneal shunting surgery.
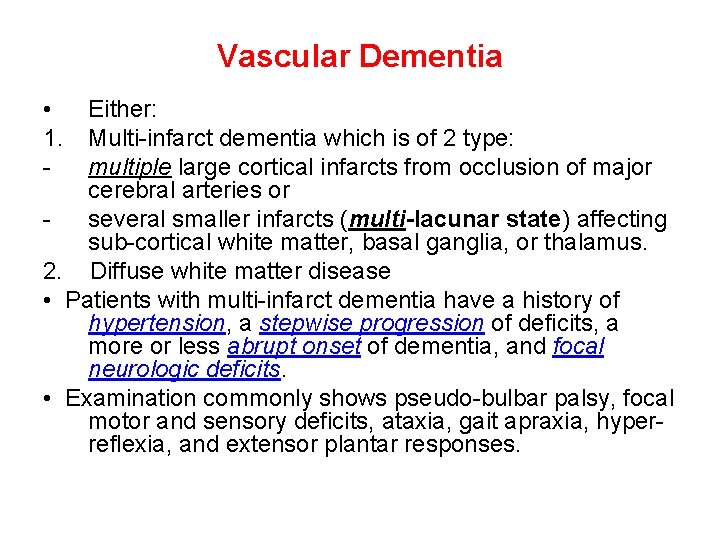
Vascular Dementia • 1. - Either: Multi-infarct dementia which is of 2 type: multiple large cortical infarcts from occlusion of major cerebral arteries or several smaller infarcts (multi-lacunar state) affecting sub-cortical white matter, basal ganglia, or thalamus. 2. Diffuse white matter disease • Patients with multi-infarct dementia have a history of hypertension, a stepwise progression of deficits, a more or less abrupt onset of dementia, and focal neurologic deficits. • Examination commonly shows pseudo-bulbar palsy, focal motor and sensory deficits, ataxia, gait apraxia, hyperreflexia, and extensor plantar responses.
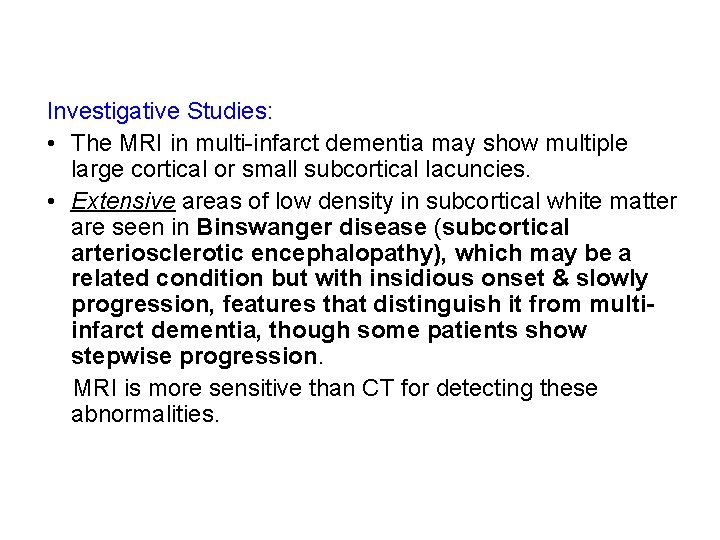
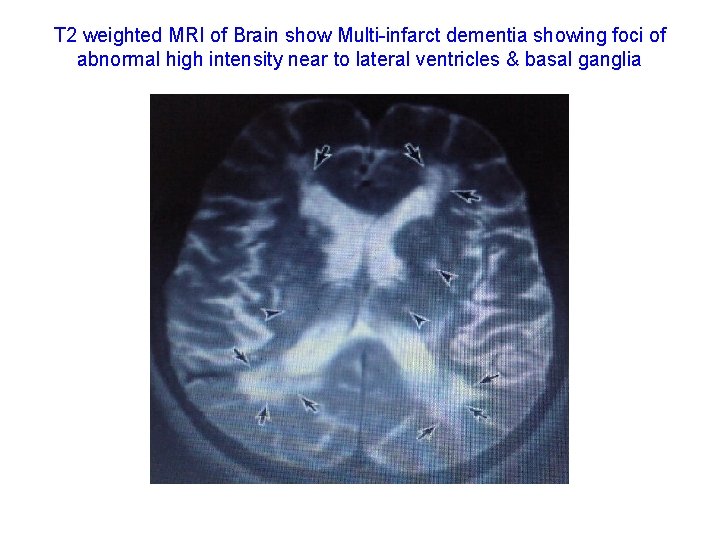
Investigative Studies: • The MRI in multi-infarct dementia may show multiple large cortical or small subcortical lacuncies. • Extensive areas of low density in subcortical white matter are seen in Binswanger disease (subcortical arteriosclerotic encephalopathy), which may be a related condition but with insidious onset & slowly progression, features that distinguish it from multiinfarct dementia, though some patients show stepwise progression. MRI is more sensitive than CT for detecting these abnormalities.
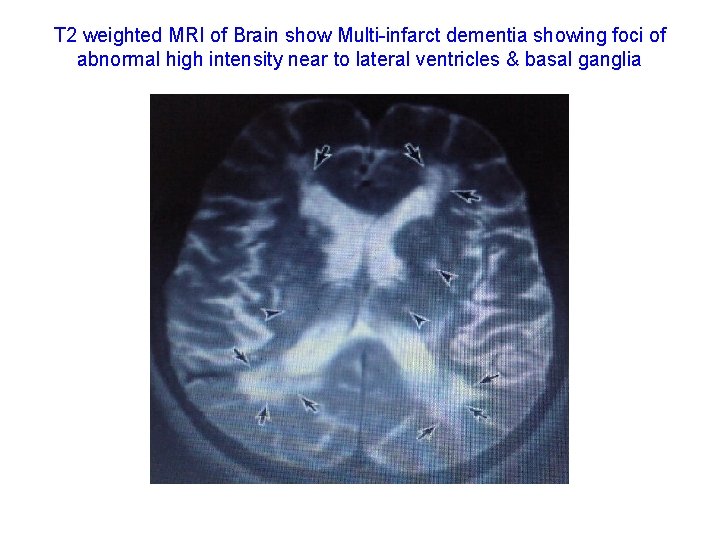
T 2 weighted MRI of Brain show Multi-infarct dementia showing foci of abnormal high intensity near to lateral ventricles & basal ganglia
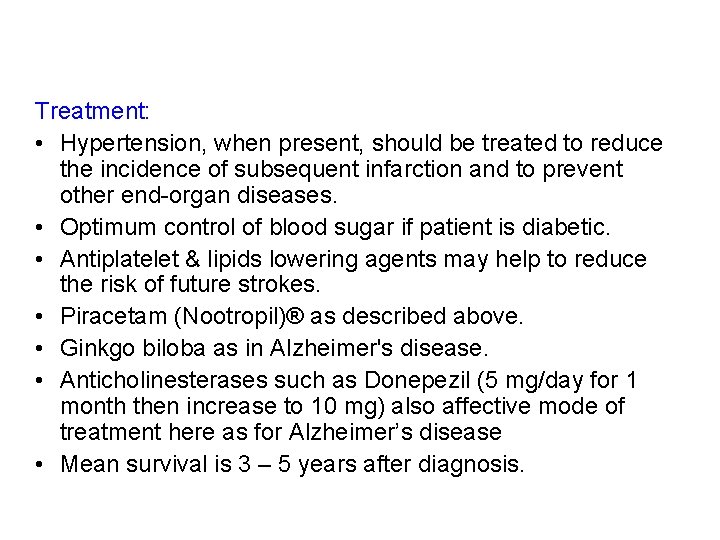
Treatment: • Hypertension, when present, should be treated to reduce the incidence of subsequent infarction and to prevent other end-organ diseases. • Optimum control of blood sugar if patient is diabetic. • Antiplatelet & lipids lowering agents may help to reduce the risk of future strokes. • Piracetam (Nootropil)® as described above. • Ginkgo biloba as in Alzheimer's disease. • Anticholinesterases such as Donepezil (5 mg/day for 1 month then increase to 10 mg) also affective mode of treatment here as for Alzheimer’s disease • Mean survival is 3 – 5 years after diagnosis.