Hypertriglyceridemia Vishwanath Pattan MD Endocrinology Wyoming Medical Center








- Slides: 83
Hypertriglyceridemia Vishwanath Pattan, MD Endocrinology Wyoming Medical Center
Disclosure �Holdings in Amarin Corporation
Objectives �Triglyceride rich lipoproteins (TRLs) �Genetic causes of hypertriglyceridemia (HTG) �Hypertriglyceridemia induced pancreatitis �Management of hypertriglyceridemia
What is the most common cause of pancreatitis in during pregnancy? um ar id av gr es is em er yp H 0 em ia ce ly ig yp er tr a es on st Ga ll rid ic ed m nd nd a on es st ll Ga 0 at in sm ok on l s t al g nd a ho l co Al 7 0. . . 0 g 0 es 4. 5. Alcohol and gall stones Gall stones and smoking Gall stones and medication induced pancreatitis Hypertriglyceridemia Hyperemesis gravidarum H 1. 2. 3.
What is the risk of developing acute pancreatitis when triglyceride level is <500 vs triglyceride level >2000 mg/dl? 0 0 nd <5 5 % % 5% and resp a 5 - ec nd 10 t. . <5 5 %. % 0% re s 5% and res. . . a 10 pec nd -2. 7 0%. . 0% r re e. . . sp ec. . . 0 a 7 2% and 5% respectively <5% and 5 -10% respectively 5% and 50% respectively <5% and 10 -20% respectively 5% and 70% respectively 2% A. B. C. D. E.
All are therapeutic targets for management of hypertriglyceridemia except: to in hi II C eas lip n ei ot pr po Li bi o Ad bi in hi T 3 GL AN 0 en to to bi in hi III C o. Ap 7 0. . . 0 Ap o- 0 r 4. Apo-C III inhibitor ANGLT 3 inhibitors Lipoprotein lipase-Adeno associated virus vecotor Apo-C II inhibito rs 1. 2. 3.
55 yo. Male nondiabetic patient presented with severe acute pancreatitis with triglyceride 5, 640 mg/dl lipase 5 times the upper limit of normal. What is the best treatment? . . . m a N su lin a nd g lu la s N PO , I n ra he , T N PO 7 0 0 co PO N se P i. , O In N. . , H PO su ep lin , F ar en an in of d ib he ra pa te rin a nd in su l. . . 0 pe 3. 4. 5. p 2. NPO, Therapeutic plasma exchange NPO, Insulin and glucose infusion NPO, Heparin NPO, Insulin and heparin NPO, Fenofibrate and insulinglucose infusion ut ic 1.
The highest risk of acute pancreatitis is with: cr H D L L a D ed H D ec re as ed as re ec D . . . an d in nd d an L D L ed at ev 0 in cr L D VL VL at ed ev El 0. . . 0 D n ro ic El hy c ed at ev El 7 0 L 0 lo 5. Elevated chylomicron Elevated VLDL Elevated LDL and VLDL Decreased HDL and increased IDL m 1. 2. 3. 4.

Triglyceride rich lipoproteins (TRLs)
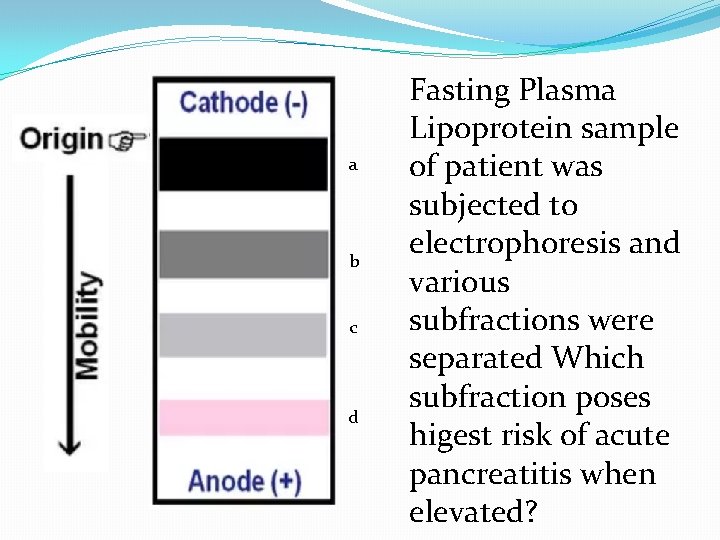
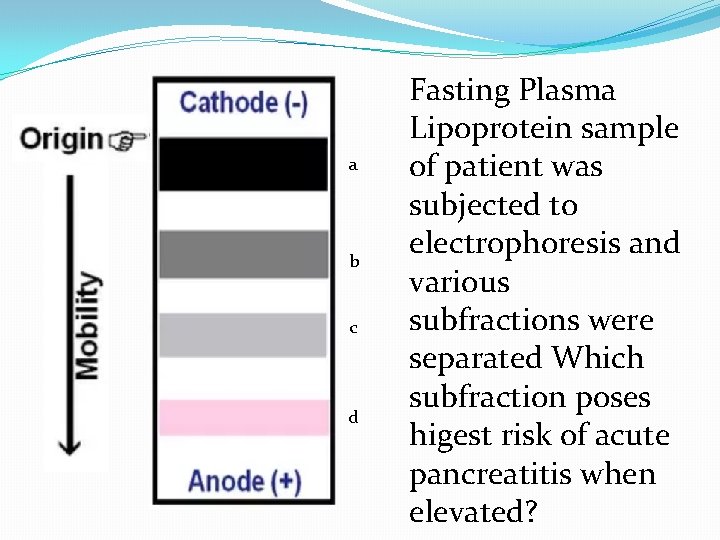
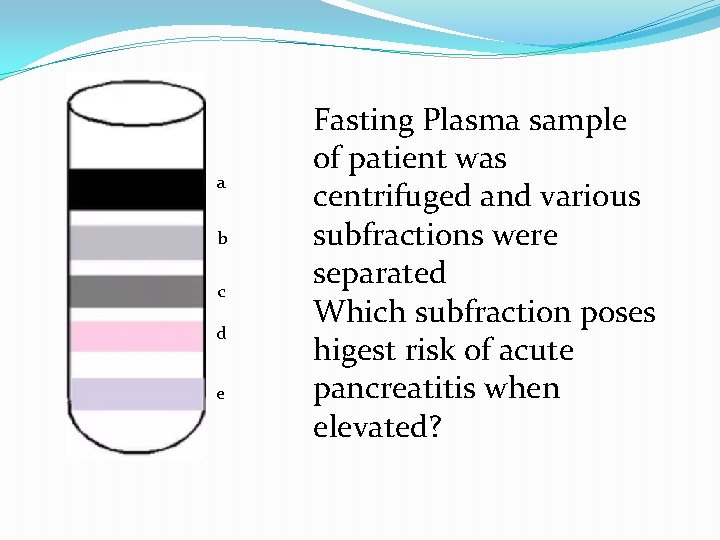
a b c d Fasting Plasma Lipoprotein sample of patient was subjected to electrophoresis and various subfractions were separated Which subfraction poses higest risk of acute pancreatitis when elevated?
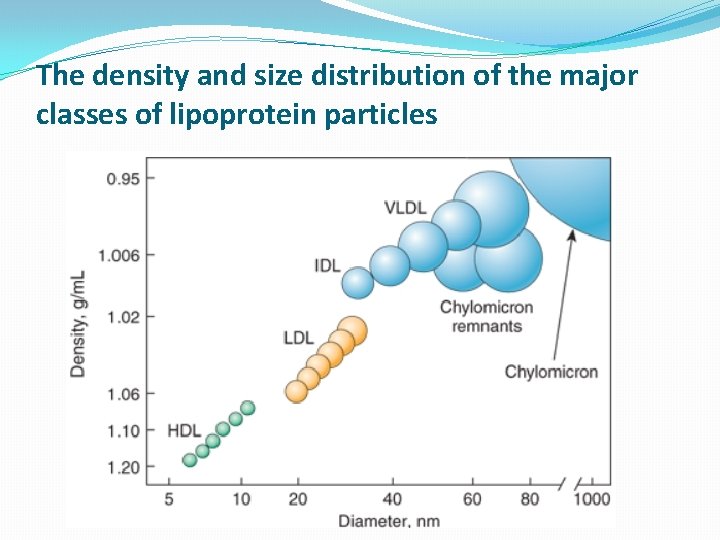
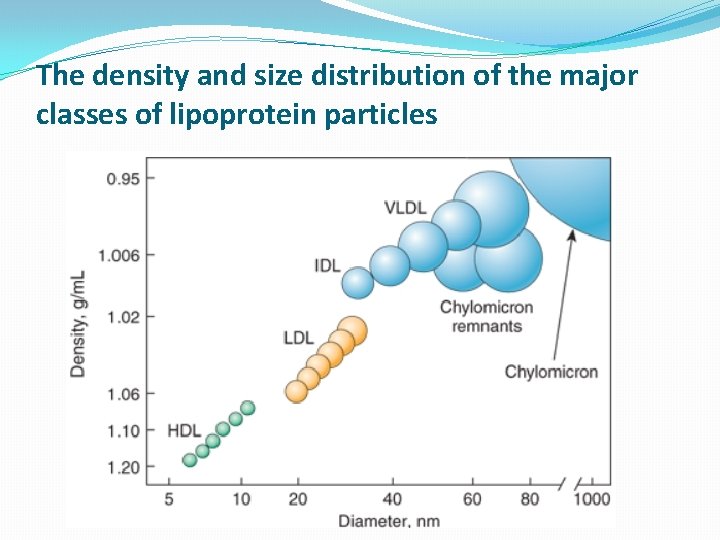
The density and size distribution of the major classes of lipoprotein particles

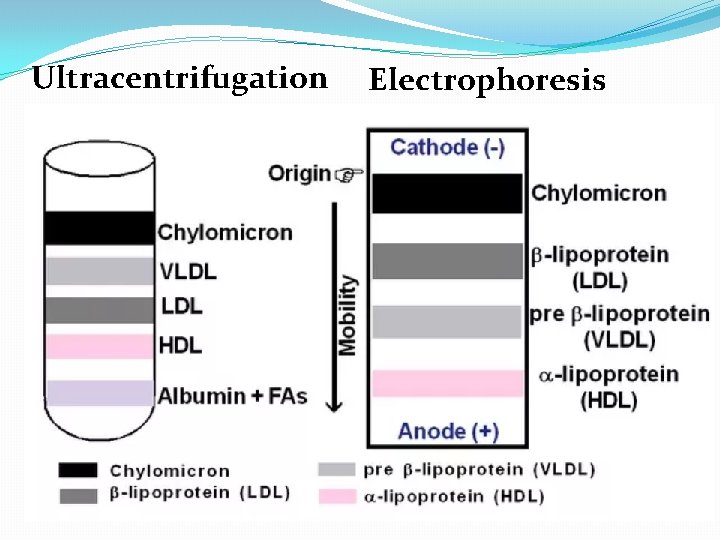
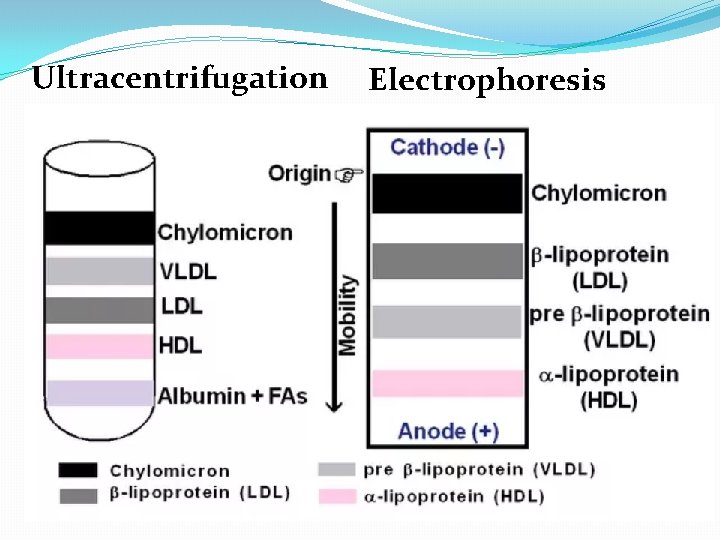
Ultracentrifugation Electrophoresis
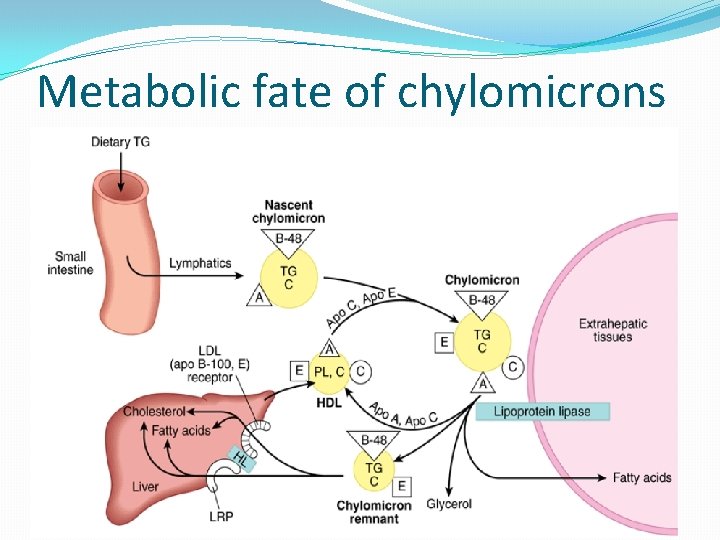
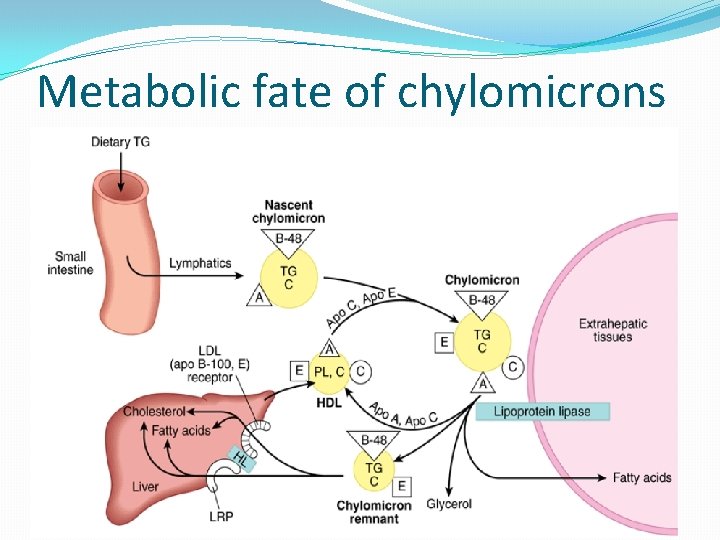
Metabolic fate of chylomicrons
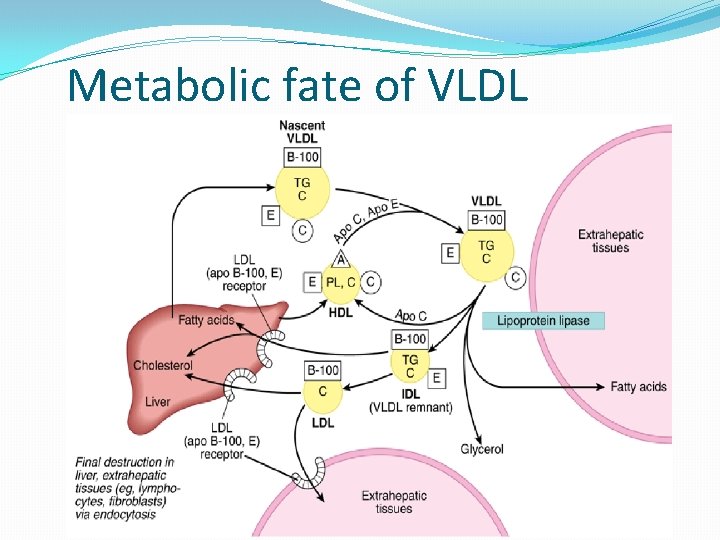
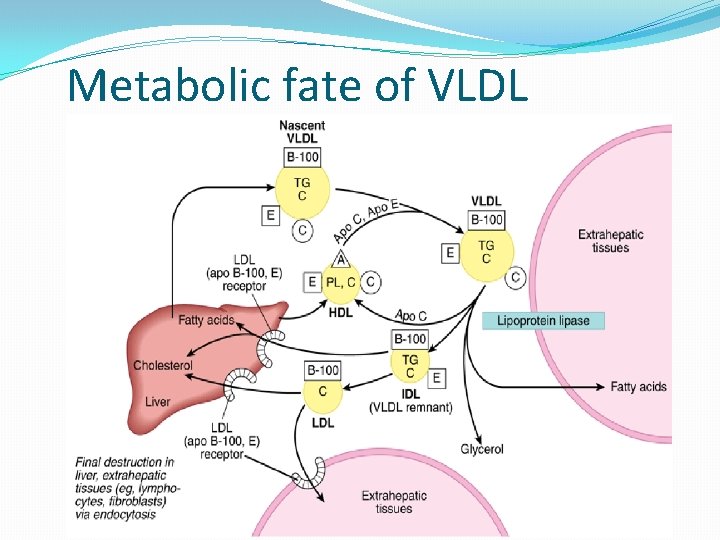
Metabolic fate of VLDL


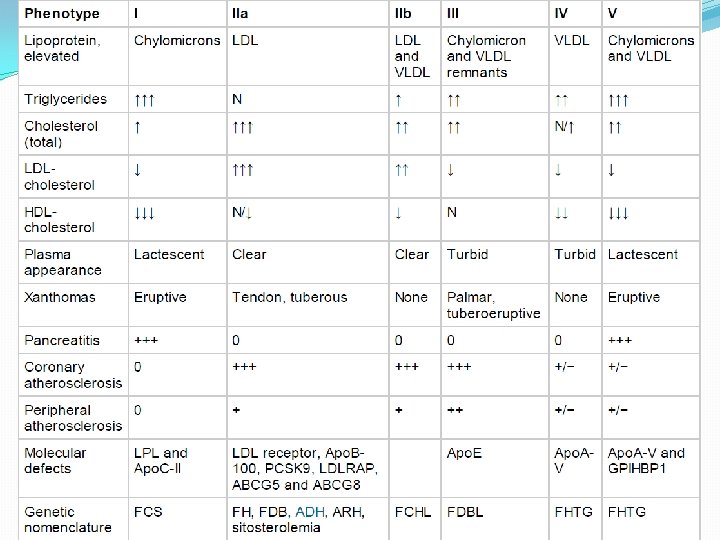
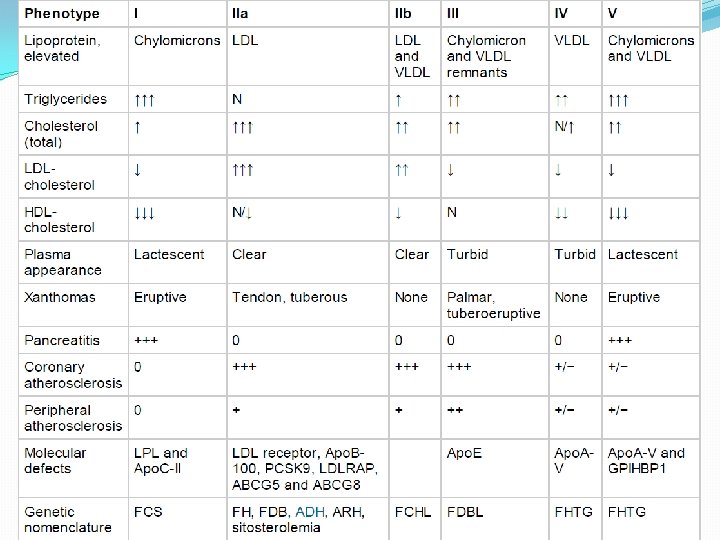
Genetic causes of HTG
Most common cause of monogenic chylomicronemia is a. Familial LPL Deficiency b. Familial Apo. C-II Deficiency c. Familial GPIHBP 1 deficiency d. Familial LMF 1 deficiency e. Familial Apo. A-V Deficiency

All are therpeutic targets for management of hypertriglyceridemia except �Apo-C III inhibitor �ANGPLT 3 inhibitors �Lipoprotein lipase-Adeno associated virus vector �Apo C II inhibitor
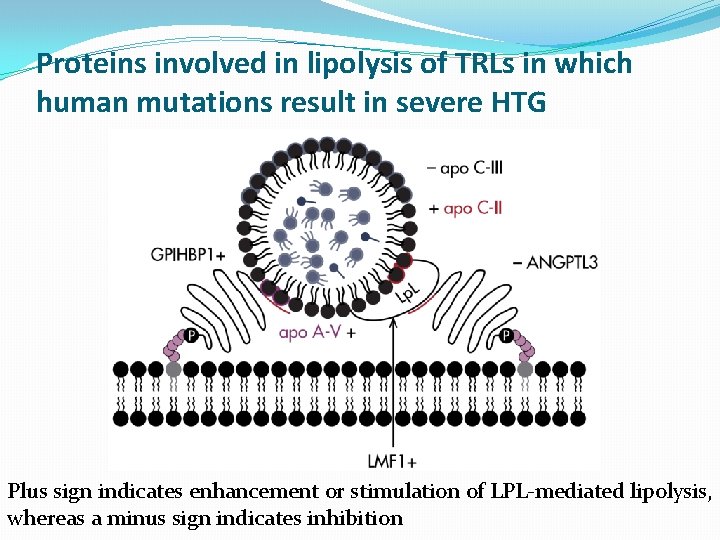
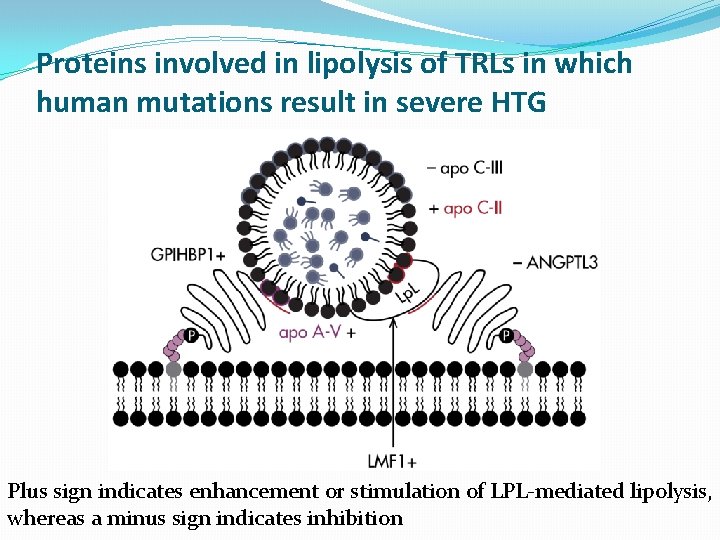
Proteins involved in lipolysis of TRLs in which human mutations result in severe HTG Plus sign indicates enhancement or stimulation of LPL-mediated lipolysis, whereas a minus sign indicates inhibition

�HTG within a family does not typically follow classical Mendelian patterns of inheritance �HTG does not consistently show vertical transmission across generations in family pedigrees �Although some cases do cluster in some families, they are usually not monogenic Endocrine Reviews, February 2015, 36(1): 131– 147

Primary Hypertriglyceridemias �Familial LPL Deficiency �Familial Apo. C-II Deficiency �Familial GPIHBP 1 Deficiency �Familial Apo. A-V Deficiency
Familial Hypertriglyceridemia (FHTG) �Is a polygenic hypertriglyceridemia �FHTG is characterized by elevated fasting TGs without a clear secondary cause, average to below average LDL-C levels, low HDL-C levels, and a family history of hypertriglyceridemia �Apo. B levels are not elevated
�Patients with very severe HTG (TG 2000 mg/d. L) are almost certain to have one or more genetic defects together with coexisting secondary conditions Endocrine Reviews, February 2015, 36(1): 131– 147
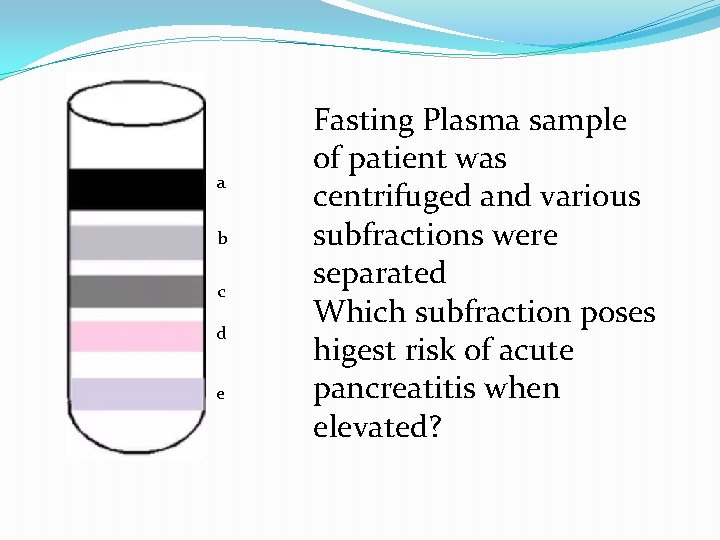
a b c d e Fasting Plasma sample of patient was centrifuged and various subfractions were separated Which subfraction poses higest risk of acute pancreatitis when elevated?
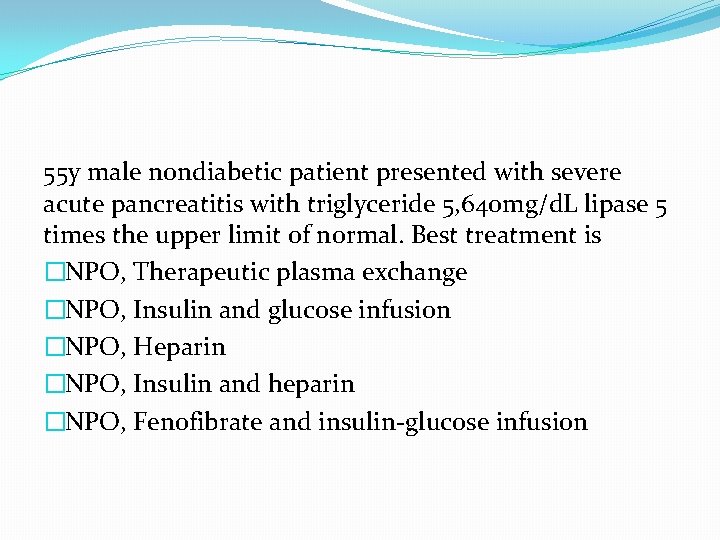
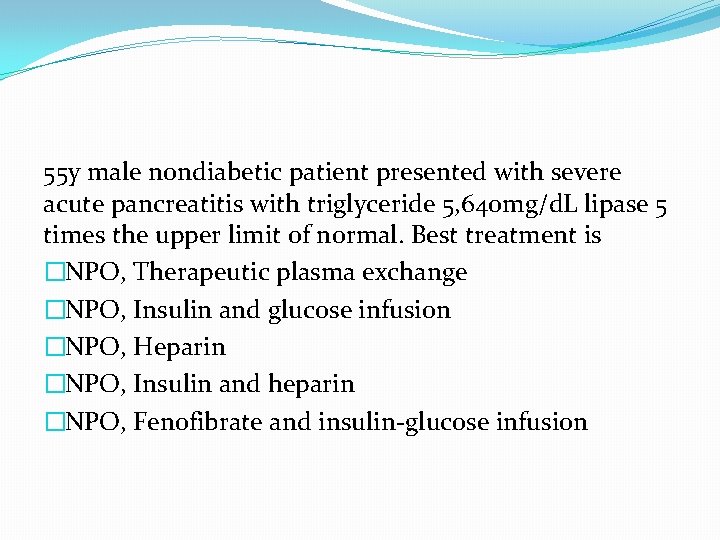
55 y male nondiabetic patient presented with severe acute pancreatitis with triglyceride 5, 640 mg/d. L lipase 5 times the upper limit of normal. Best treatment is �NPO, Therapeutic plasma exchange �NPO, Insulin and glucose infusion �NPO, Heparin �NPO, Insulin and heparin �NPO, Fenofibrate and insulin-glucose infusion
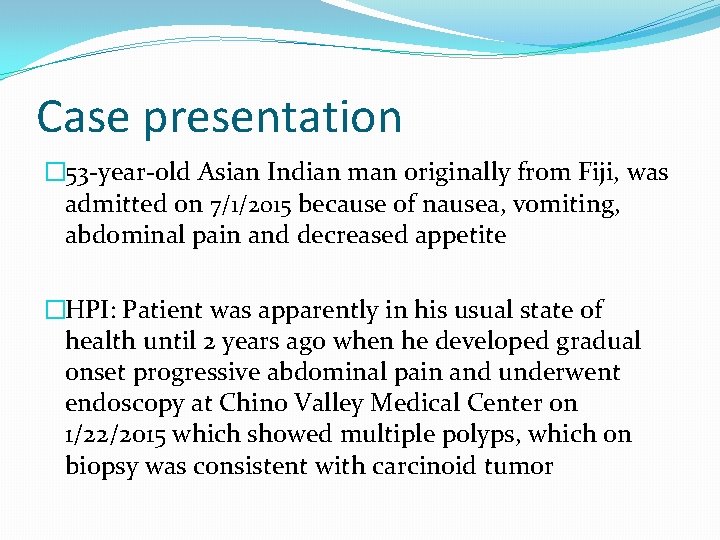
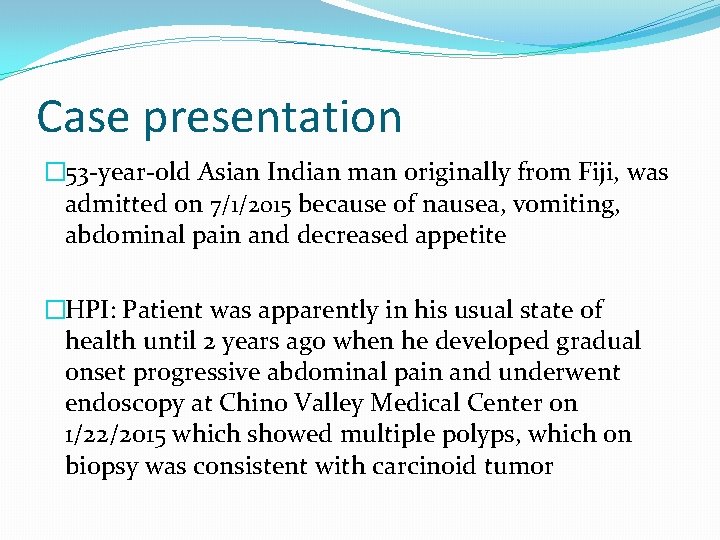
Case presentation � 53 -year-old Asian Indian man originally from Fiji, was admitted on 7/1/2015 because of nausea, vomiting, abdominal pain and decreased appetite �HPI: Patient was apparently in his usual state of health until 2 years ago when he developed gradual onset progressive abdominal pain and underwent endoscopy at Chino Valley Medical Center on 1/22/2015 which showed multiple polyps, which on biopsy was consistent with carcinoid tumor
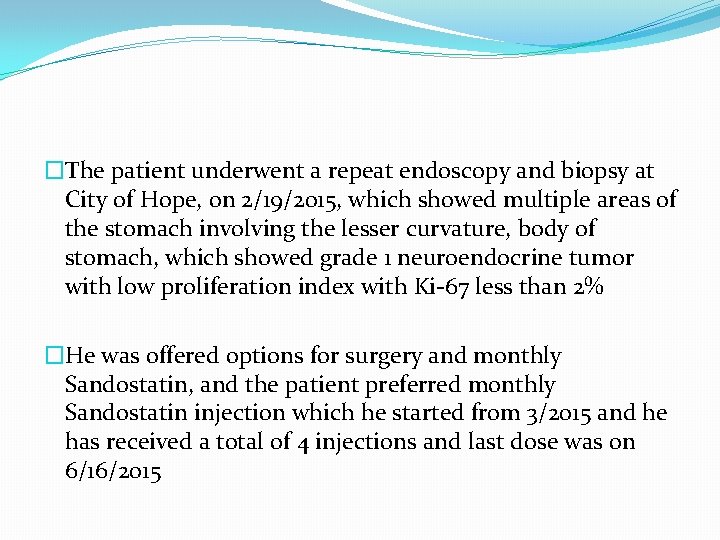
�The patient underwent a repeat endoscopy and biopsy at City of Hope, on 2/19/2015, which showed multiple areas of the stomach involving the lesser curvature, body of stomach, which showed grade 1 neuroendocrine tumor with low proliferation index with Ki-67 less than 2% �He was offered options for surgery and monthly Sandostatin, and the patient preferred monthly Sandostatin injection which he started from 3/2015 and he has received a total of 4 injections and last dose was on 6/16/2015
�Patient was admitted for severe abdominal pain on 3/21/2015 and was found to have acute pancreatitis confirmed on CT scan and with elevated lipase �Ultrasound on 3/22/16 did not show gallstones and due to Hx of alcohol use it was presumed to be either alcohol induced and /or passed gallstones(patient had elevated ALP 301, AST 335, ALT 109, Ca 7. 2, albumin 3. 3)
�Octreoscan, on 3/27/2015, which was negative for any evidence of metastases �CT imaging, on 6/16/2015, showed near complete resolution of features of pancreatitis, which was previously seen �The patient has been drinking alcohol for the last 30 years �The patient says that he takes at least scotch 1 -2 drinks daily and usually 4 drinks per day
PAST MEDICAL HISTORY: �Neuroendocrine tumor involving the stomach �Hypertension �Fatty liver disease �Chronic alcoholism �Elevated liver enzyme, probably secondary to alcohol use �History of acute pancreatitis
PAST SURGICAL HISTORY: �Gastric submucosal biopsy in 2/2015 and 1/2015. FAMILY HISTORY: �No history of diabetes or thyroid problems in the family. �No history of cancers in the family. �No history of neuroendocrine tumor in the family.
SOCIAL HISTORY �The patient is married. He denies smoking but he drinks alcohol, one or two drinks daily for the last 30 years. No illicit drug use. No known drug allergies
HOME MEDICATIONS: �Hydrochlorothiazide 25 mg daily �Lisinopril 30 mg daily �Omega-3 fatty acid 1 g 3 times daily �Compazine 10 mg orally 3 times daily �Ecitalopram 10 mg daily �Ondansetron 8 mg every 8 hours as needed for nausea, vomiting �Oxycodone 5 mg tablet every 6 hours as needed for pain
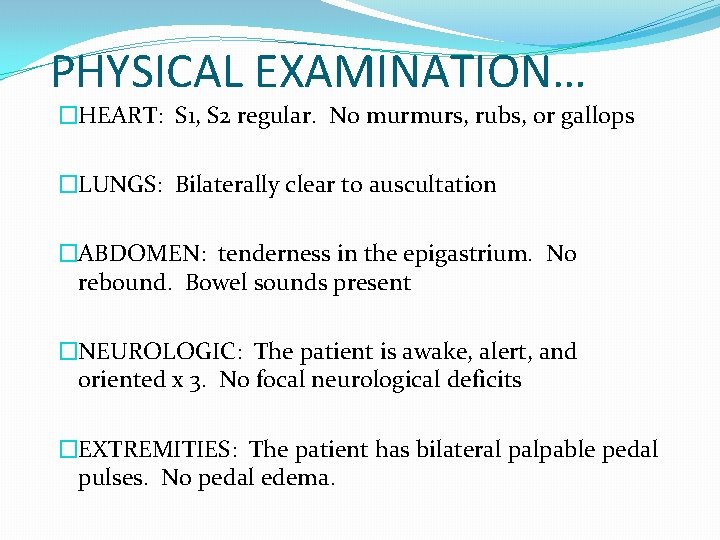
PHYSICAL EXAMINATION �GENERAL: The patient is lying on bed, not in acute distress �SKIN: no xanthelasma, no eruptive xanthomas �VITAL SIGNS: HR 80, BP 127/95, RR 18, T 98. 2 F, saturating 96% on room air, body weight 76. 8 kg, height 180 cm, BMI 23. 7 kg/m 2 �HEENT: Pupils equal and reactive to light. Extraocular movements intact �NECK: Supple. No thyromegaly
PHYSICAL EXAMINATION… �HEART: S 1, S 2 regular. No murmurs, rubs, or gallops �LUNGS: Bilaterally clear to auscultation �ABDOMEN: tenderness in the epigastrium. No rebound. Bowel sounds present �NEUROLOGIC: The patient is awake, alert, and oriented x 3. No focal neurological deficits �EXTREMITIES: The patient has bilateral palpable pedal pulses. No pedal edema.
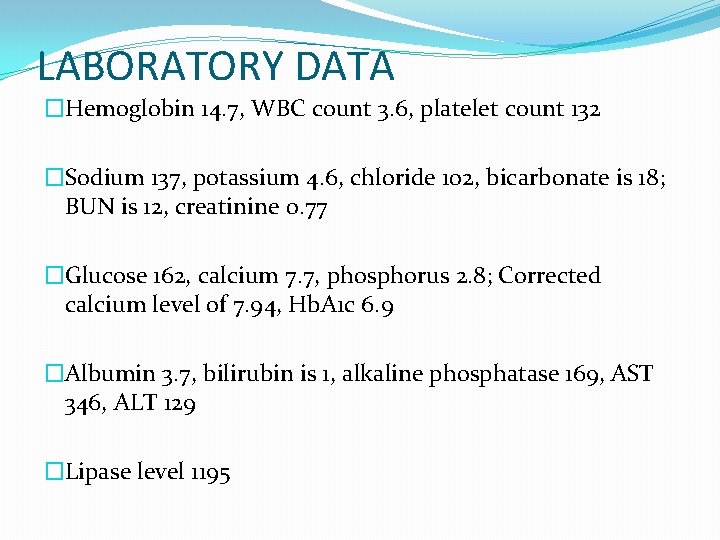
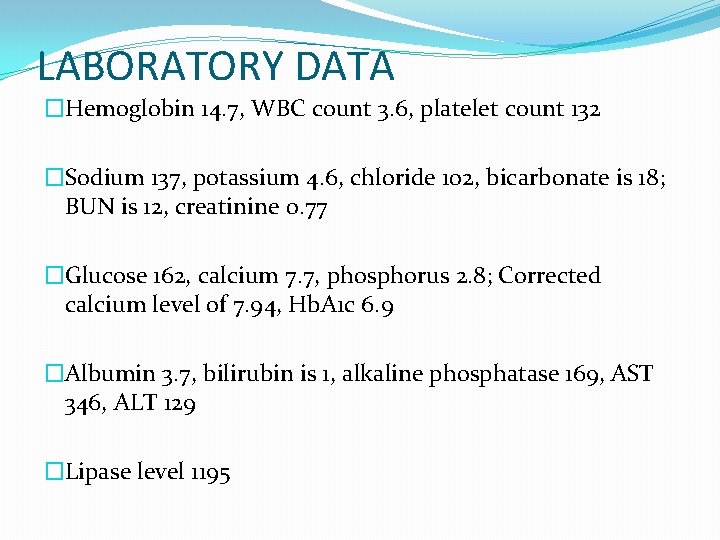
LABORATORY DATA �Hemoglobin 14. 7, WBC count 3. 6, platelet count 132 �Sodium 137, potassium 4. 6, chloride 102, bicarbonate is 18; BUN is 12, creatinine 0. 77 �Glucose 162, calcium 7. 7, phosphorus 2. 8; Corrected calcium level of 7. 94, Hb. A 1 c 6. 9 �Albumin 3. 7, bilirubin is 1, alkaline phosphatase 169, AST 346, ALT 129 �Lipase level 1195
�Endo consult for elevated Hb. A 1 c 6. 9 and new onset type 2 diabetes
�New lab orders- Triglyceride level
�Triglyceride 5016 mg/d. L
ASSESSMENT AND PLAN �SEVERE HYPERTRIGLYCERIDEMIA PRECIPITATED BY ALCOHOL USE, COMPLICATED WITH ACUTE PANCREATITIS �NPO �IV fluids �Therapeutic plasma exchange was recommended to manage hypertriglyceridemia in this patient with acute pancreatitis �Our goal was to decrease triglyceride to <500 mg/d. L
�After 1 session of therapeutic plasma exchange triglyceride level improved from 5016 mg/d. L to 1192 mg/Dl �After 2 nd session of therapeutic plasma exchange plasma triglycerides decreased from 1192 mg/d. L to 312 mg/d. L �Patient was pain free and started on clear liquids on day 3 and diet was advanced
Hypertriglyceridemia induced pancreatitis
�Hypertriglyceridemia is an important cause of pancreatitis that is often missed �The risk of developing acute pancreatitis is approximately 5 percent with TG >1000 mg/d. L and 10 to 20 percent with TG >2000 mg/d. L J Clin Gastroenterol. 2014; 48(3): 195 �Alcohol increases serum triglyceride concentrations in a "dose-dependent" manner
�In women, pregnancy-induced HTG has been found to be responsible for up to 56 percent of cases of acute pancreatitis occurring during pregnancy Pancreas. 2017; 46(4): 504 �Persistent hyperchylomicronemia may lead to the formation of eruptive xanthomas over the extensor surfaces of the arms, legs, buttocks, and back; lipemia retinalis; and hepatosplenomegaly from fatty infiltration of the liver
�Patients with HTG induced pancreatitis tend to have severe pancreatitis as compared with patients with other causes of pancreatitis Lipids Health Dis. 2017; 16(1): 124
�In patients who develop Hypertriglyceridemia induced pancreatitis, the treatment includes conventional treatment of acute pancreatitis, and management of serum triglyceride levels with an initial goal of <500 mg/d. L �Maintenance of triglyceride levels below 500 mg/d. L has been seen in multiple case series to expedite clinical improvement
�Therapeutic plasma exchange(TPE) is the removal of plasma and replacement with a colloid solution (eg, albumin or plasma) �TPE should be considered for hypertriglyceridemiainduced acute pancreatitis especially when serum triglyceride level >1000 mg/d. L plus lipase >3 times the upper limit of normal and signs of hypocalcemia, lactic acidosis, or signs of worsening inflammation or organ dysfunction
�Severe or very severe HTG plus high lipase levels (>3 times the upper limit of normal) are associated with very high FFA levels and can further be complicated by systemic inflammation from both acute pancreatitis and direct activation of TLR 2 and TLR 4 by FFA
Chylomicronemia �Chylomicronemia — Commonly due to partial LPL deficiency, where the type V phenotype (in which chylomicrons are present in the supernatant, and the infranatant is cloudy due to VLDL particles) is brought out be one of the exacerbating factors � Type V phenotype shows Fasting triglyceride levels above the 99 th percentile �Marked hypertriglyceridemia (>1000 mg/d. L ) may lead to chylomicronemia syndrome which can manifest with recent memory loss, abdominal pain and/or pancreatitis, dyspnea, eruptive xanthoma, flushing with alcohol, and lipemia retinalis
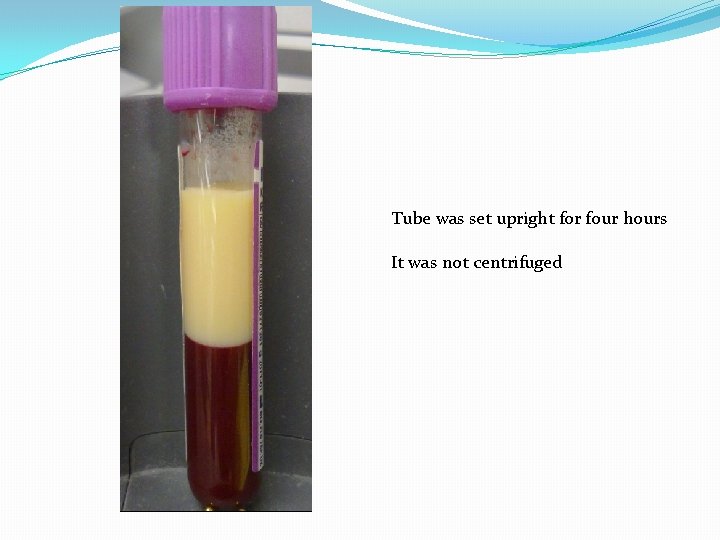
Chylomicronemia… �There is also a primary form of type V hyperlipoproteinemia in which there is no deficiency in LPL or its ligand apo C-II �The underlying defect in this disorder is uncertain but apo E 4, which is a ligand for the hepatic chylomicron and VLDL remnant receptor, may play a role �Fasting chylomicronemia can be diagnosed by confirming the presence of chylomicrons and excess VLDL on agarose gel electrophoresis or ultracentrifugal analysis �A simple technique is to refrigerate plasma overnight and examine the specimen for a creamy supernatant from chylomicrons and a turbid VLDL-rich infranatant
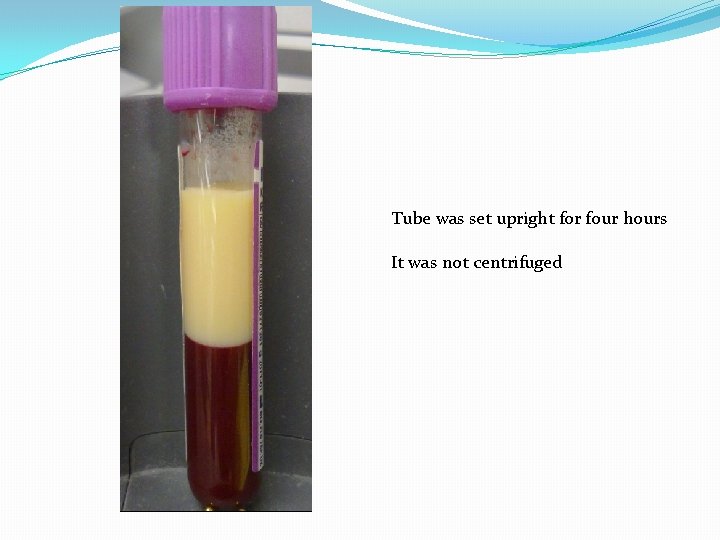
Tube was set upright for four hours It was not centrifuged
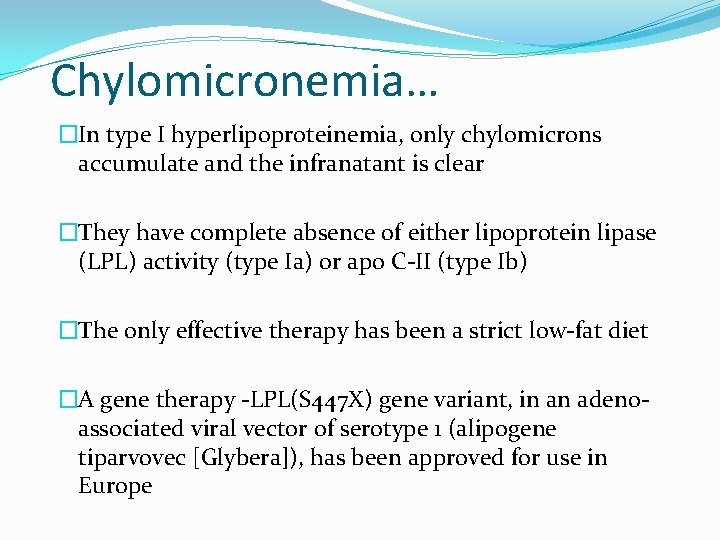
Chylomicronemia… �In type I hyperlipoproteinemia, only chylomicrons accumulate and the infranatant is clear �They have complete absence of either lipoprotein lipase (LPL) activity (type Ia) or apo C-II (type Ib) �The only effective therapy has been a strict low-fat diet �A gene therapy -LPL(S 447 X) gene variant, in an adenoassociated viral vector of serotype 1 (alipogene tiparvovec [Glybera]), has been approved for use in Europe
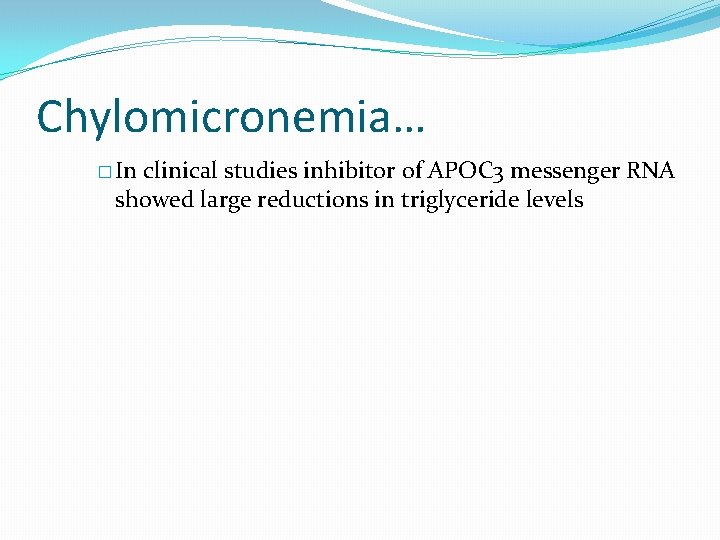
Chylomicronemia… � In clinical studies inhibitor of APOC 3 messenger RNA showed large reductions in triglyceride levels
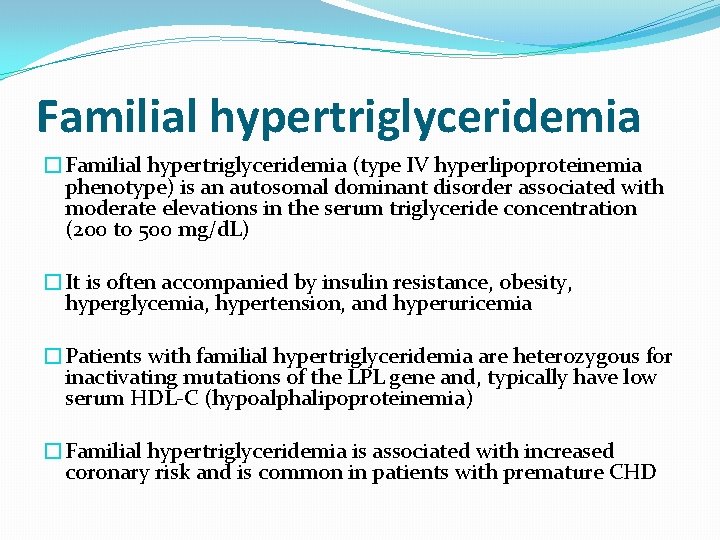
Familial hypertriglyceridemia �Familial hypertriglyceridemia (type IV hyperlipoproteinemia phenotype) is an autosomal dominant disorder associated with moderate elevations in the serum triglyceride concentration (200 to 500 mg/d. L) �It is often accompanied by insulin resistance, obesity, hyperglycemia, hypertension, and hyperuricemia �Patients with familial hypertriglyceridemia are heterozygous for inactivating mutations of the LPL gene and, typically have low serum HDL-C (hypoalphalipoproteinemia) �Familial hypertriglyceridemia is associated with increased coronary risk and is common in patients with premature CHD
Most common acquired causes �Diabetes �Alcohol �Pregnancy �Drug- induced hypertriglyceridemia �Diet-induced hypertriglyceridemia
Severe Hypertriglyceridemia (Type V) �Most individuals with severe hypertriglyceridemia have type V hyperlipoproteinemia, signifying an increase in both chylomicrons and VLDL-C �The need to lower TG levels in these individuals is urgent to prevent acute pancreatitis and chylomicronemia syndrome
Borderline Hypertriglyceridemia �When moderate hypertriglyceridemia (150 -199 mg/d. L) in association with increased serum cholesterol or low HDLC levels is the primary disorder, physical activity, weight control, smoking cessation, and other lifestyle changes are first-line therapy �The approach to treatment of accompanying elevated LDL -C does not need to be modified � However, if the individual also has decreased HDL-C, the selection of secondary drug therapy may be affected

�The criteria developed for the Endocrine Society guidelines focus on the ability to assess risk for premature CVD vs. risk for pancreatitis �The designations of mild and moderate hypertriglyceridemia correspond to the range of levels predominant in risk assessment for premature CVD, and this range includes the vast majority of subjects with hypertriglyceridemia
�In addition, these levels suggest different etiologies �Presence of mild or moderate hypertriglyceridemia is commonly due to a dominant underlying cause in each patient, whereas severe or very severe hypertriglyceridemia is more likely due to several contributing factors
�Recommend screening adults for hypertriglyceridemia as part of a lipid panel at least every 5 years (1/ ⊕⊕oo) �Recommend basing the diagnosis of hypertriglyceridemia on fasting triglyceride levels and not on nonfasting triglyceride levels (1/ ⊕⊕⊕o) �Recommend against the routine measurement of lipoprotein particle heterogeneity in patients with hypertriglyceridemia (1/ ⊕⊕oo)
Management of Hypertriglyceridemia
Endocrine Society Clinical Practice Guideline 2012 �Strong recommendations use the phrase “we recommend” and the number 1, and weak recommendations use the phrase “we suggest” and the number 2 �Cross-filled circles indicate the quality of the evidence, such that ⊕ooo denotes very low-quality evidence; ⊕⊕oo, low quality; ⊕⊕⊕o, moderate quality; and ⊕⊕⊕⊕, high quality.
Endocrine Society Clinical Practice Guideline 2012 �Recommend lifestyle therapy, including dietary counseling to achieve appropriate diet composition, physical activity, and a program to achieve weight reduction in overweight and obese individuals as the initial treatment of mild-to-moderate hypertriglyceridemia (1/ ⊕⊕OO) �For severe and very severe hypertriglyceridemia (1000 mg/dl), we recommend combining reduction of dietary fat and simple carbohydrate intake with drug treatment to reduce the risk of pancreatitis (1/ ⊕⊕⊕⊕) �Recommend that the treatment goal for patients with moderate hypertriglyceridemia be a non-high-density lipoprotein (HDL) cholesterol level in agreement with NCEP ATP guidelines (1/ ⊕⊕OO)
Management of hypertriglyceridemia � Recommend that a fibrate be used as a first-line agent for reduction of triglycerides in patients at risk for triglyceride-induced pancreatitis (1/ ⊕⊕⊕O) � Suggest that three drug classes (fibrates, niacin, n-3 fatty acids) alone or in combination with statins be considered as treatment options in patients with moderate to severe triglyceride levels (2/ ⊕⊕OO) � We recommend that statins not be used as monotherapy for severe or very severe hypertriglyceridemia. However, statins may be useful for the treatment of moderate hypertriglyceridemia when indicated to modify cardiovascular risk (1/ ⊕⊕OO)
Diet �The Omni. Heart study compared the effects of healthful dietary patterns based on the DASH diet that lowered blood pressure and LDL cholesterol �These dietary patterns all emphasize fruits, vegetables, and low-fat dairy products; include whole grains, poultry, fish, and nuts; use unsaturated vegetable oils; and contain smaller amounts of red meat, sweets, and sugar-containing beverages than typical diets in the United States
Diet �Compared with a diet that emphasized carbohydrate, a similar diet that emphasized protein decreased triglyceride levels further, and this decrease was about twice the effect of a diet that emphasized unsaturated fat �African-Americans have lower serum triglyceride levels than other racial or ethnic groups. The Omni. Heart study, in which 50% of the population was African-American, found that diet modification had less effect on triglyceride levels in this ethnic group than in a Caucasian population when matching baseline triglyceride levels
Exercise �The minimum exercise required to reduce a postprandial triglyceride increase has not been determined, but a period of 30 – 60 min of intermittent aerobic exercise or mild resistance exercise has been shown to be effective in lowering plasma and VLDL triglycerides
�We do not recommend the use of heparin infusions or plasmapheresis in the treatment of very severe hypertriglyceridemia with pancreatitis �The treatment of underlying causes including dietary fat restriction and use of long-term fibrate therapy should suffice
Fibrates �Fibrates decrease triglyceride levels by 30 – 50% and sometimes increase HDL cholesterol �A response to fibrates is seen as early as two weeks into therapy with a maximal effect in six to eight weeks Expert Rev Cardiovasc Ther. 2008; 6(10): 1319
Fish oil �Lovaza (4 g/day) reduced triglyceride levels by 45 percent but raised LDL-C levels by 31 percent J Cardiovasc Risk. 1997 Oct; 4(5 -6): 385 -91 �Another commercial preparation, Vascepa, is more than 95 percent icosapent-ethyl, the ethyl ester of eicosapentaenoic acid Am J Cardiol. 2012; 110(7): 984
�Icosapent-ethyl (4 g/day) also reduced triglyceride levels by up to 45 percent, but did not significantly affect LDL-C levels Am J Cardiol. 2011 Sep; 108(5): 682 -90 �The majority of the response with nicotinic acid is seen in six weeks and with fish oil in two weeks
AACE 2017 guidelines Omega-3 Fish Oil �R 63. Prescription omega-3 oil, 2 to 4 g daily, should be used to treat severe hypertriglyceridemia (TG >500 mg/d. L). (Grade A, BEL 1) �Dietary supplements are not FDA-approved for treatment of hypertriglyceridemia and generally are not recommended for this purpose
Conclusions �Hypertriglyceridemia is an important cause of pancreatitis that is often missed �Patients with HTG induced pancreatitis tend to have severe pancreatitis as compared with patients with other causes of pancreatitis �Therapeutic Plasma Exhange should be considered for hypertriglyceridemia-induced acute pancreatitis especially when serum triglyceride level >1000 mg/d. L plus lipase >3 times the upper limit of normal and signs of hypocalcemia, lactic acidosis, or signs of worsening inflammation or organ dysfunction
�At the present time, genetic testing for rare mutations rarely provides useful information to guide clinical therapy, but it is very relevant for understanding the pathophysiology of hypertriglyceridemic states �With greater understanding of genetic and environmental causes and their interaction, therapy can be intelligently targeted in the future
References �J Clin Gastroenterol. 2014; 48(3): 195 �Endocrine Reviews, February 2015, 36(1): 131– 147 �Lipids Health Dis. 2017; 16(1): 124 �Pancreas. 2008; 37(1): 13. �Expert Rev Cardiovasc Ther. 2008; 6(10): 1319 �J Cardiovasc Risk. 1997 Oct; 4(5 -6): 385 -91 �Am J Cardiol. 2011 Sep; 108(5): 682 -90 �Am J Cardiol. 2012; 110(7): 984 �Endocrine Society Clinical Practice Guideline 2012 �AACE 2017 guidelines
Thank You
 Vishwanath pattan
Vishwanath pattan Tabel kelenjar endokrin dan hormon yang dihasilkan
Tabel kelenjar endokrin dan hormon yang dihasilkan Familial hypertriglyceridemia
Familial hypertriglyceridemia Vishwanath alluri
Vishwanath alluri Sriram vishwanath
Sriram vishwanath Vishwanath joshi
Vishwanath joshi Endocrinology of pregnancy
Endocrinology of pregnancy Endocrinology of pregnancy
Endocrinology of pregnancy Pediatric endocrinology near cameron park
Pediatric endocrinology near cameron park Reproductive biology and endocrinology
Reproductive biology and endocrinology Reproductive endocrinology near campbell
Reproductive endocrinology near campbell Endocrinology
Endocrinology Greater baltimore medical center medical records
Greater baltimore medical center medical records Torrance memorial medical center medical records
Torrance memorial medical center medical records Cartersville medical center medical records
Cartersville medical center medical records Wyoming medicaid portal
Wyoming medicaid portal Wyoming medicaid providers
Wyoming medicaid providers Wyoming egi
Wyoming egi Water rights wyoming
Water rights wyoming Wyoming medicaid travel reimbursement
Wyoming medicaid travel reimbursement Atlantic city project wyoming
Atlantic city project wyoming Wyoming lottery corporation
Wyoming lottery corporation Wyoming counseling association
Wyoming counseling association Wyoming county dss
Wyoming county dss Stephanie cashion wyoming
Stephanie cashion wyoming Wyoming medicaid dental coverage
Wyoming medicaid dental coverage Daniel timins
Daniel timins Wyoming smart capital
Wyoming smart capital Removals to wyoming
Removals to wyoming Wyoming medicaid trust
Wyoming medicaid trust Steve wolff wyoming
Steve wolff wyoming Ancillary probate colorado
Ancillary probate colorado There are many types of lethal venom in the animal kingdom
There are many types of lethal venom in the animal kingdom Simon tolbert
Simon tolbert Wyoming pipeline authority
Wyoming pipeline authority Wyoming csd
Wyoming csd Wyoming infrastructure authority
Wyoming infrastructure authority California medical license application
California medical license application Difference between medical report and medical certificate
Difference between medical report and medical certificate Wyndham+houston+medical+center
Wyndham+houston+medical+center Umass nurse residency program
Umass nurse residency program Makati medical center charity program
Makati medical center charity program Nipt test kuwait
Nipt test kuwait Jacobi medical center building 4
Jacobi medical center building 4 Queens medical center internship
Queens medical center internship Berkshire medical center program
Berkshire medical center program Durham va pharmacy
Durham va pharmacy Vanderbilt neurology residency
Vanderbilt neurology residency Empp university medical center
Empp university medical center Duke medical library
Duke medical library Ospital ng maynila emergency number
Ospital ng maynila emergency number Chinle wellness center
Chinle wellness center Chafford hundred medical center
Chafford hundred medical center Maribor gluten free
Maribor gluten free Anchorage va medical center
Anchorage va medical center Ku medical center histology slides
Ku medical center histology slides Outpatient medical center leesville la
Outpatient medical center leesville la Columbia university medical center
Columbia university medical center Mercy regional medical center lorain
Mercy regional medical center lorain Dr suhail allaqaband
Dr suhail allaqaband Columbia university medical center
Columbia university medical center Suny downstate medical center
Suny downstate medical center Sinai samaritan
Sinai samaritan Easc usc
Easc usc Arden medical center
Arden medical center Tufts anesthesiology residency
Tufts anesthesiology residency Islamic medical center kuwait
Islamic medical center kuwait Joint special operations medical training center
Joint special operations medical training center Woodlane medical centre
Woodlane medical centre Meritus family medicine
Meritus family medicine Iakentro athens
Iakentro athens Unm sandoval regional medical center billing
Unm sandoval regional medical center billing Wvmc my chart
Wvmc my chart Medical manuscript writing
Medical manuscript writing Three types of word parts
Three types of word parts Wootton medical centre
Wootton medical centre Tifr medical section
Tifr medical section Flat thoracic spine
Flat thoracic spine Patient centered medical home conference
Patient centered medical home conference Queen anne medical electrolysis and laser
Queen anne medical electrolysis and laser Conectados swiss medical beneficios
Conectados swiss medical beneficios Chapter 11 medical terminology
Chapter 11 medical terminology Pcs medizin
Pcs medizin Ivf maribor
Ivf maribor