Ventricular Tachycardia Mohammad Hajjiri MD FACC FHRS Director


- Slides: 40
Ventricular Tachycardia Mohammad Hajjiri, MD FACC FHRS Director, Interventional Electrophysiology Ohio. Health Medical Center, Mansfield, OH Assistant Professor of Medicine Ohio University
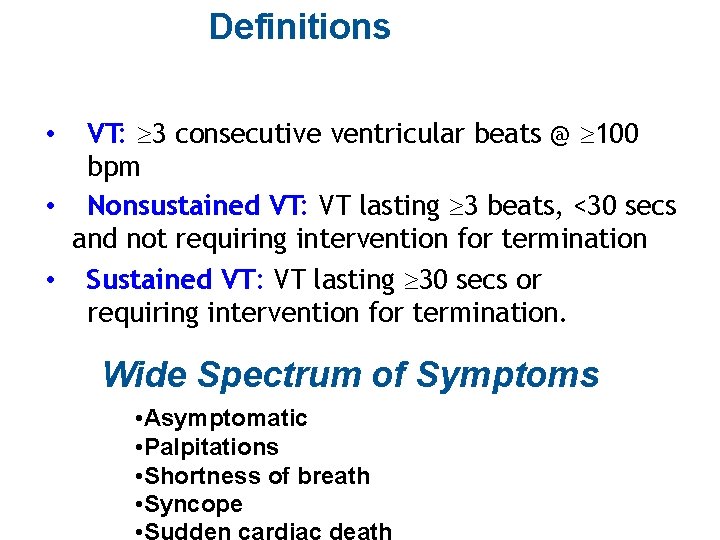
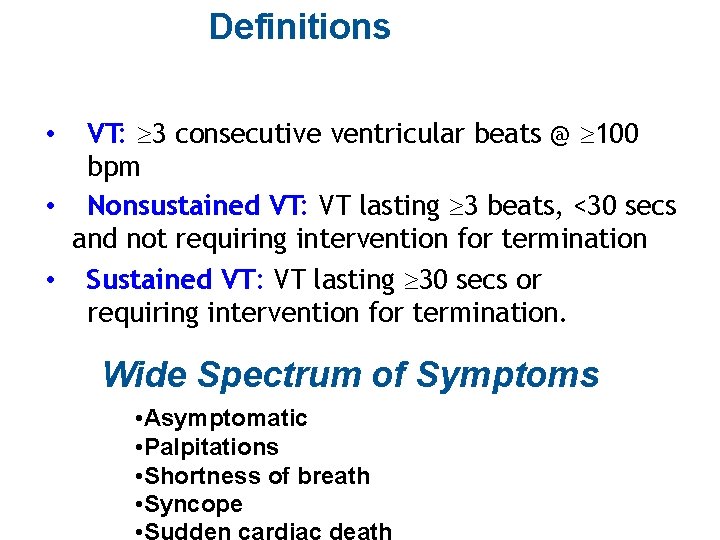
Definitions VT: ³ 3 consecutive ventricular beats @ ³ 100 bpm • Nonsustained VT: VT lasting ³ 3 beats, <30 secs and not requiring intervention for termination • Sustained VT: VT lasting ³ 30 secs or requiring intervention for termination. • Wide Spectrum of Symptoms • Asymptomatic • Palpitations • Shortness of breath • Syncope • Sudden cardiac death
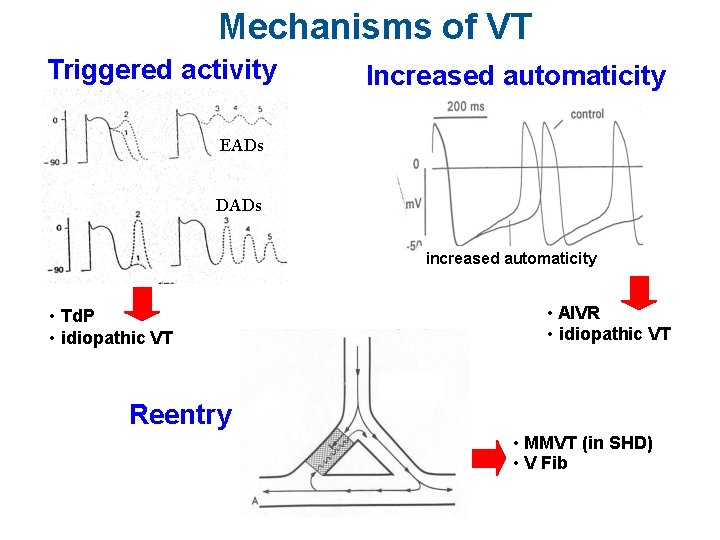
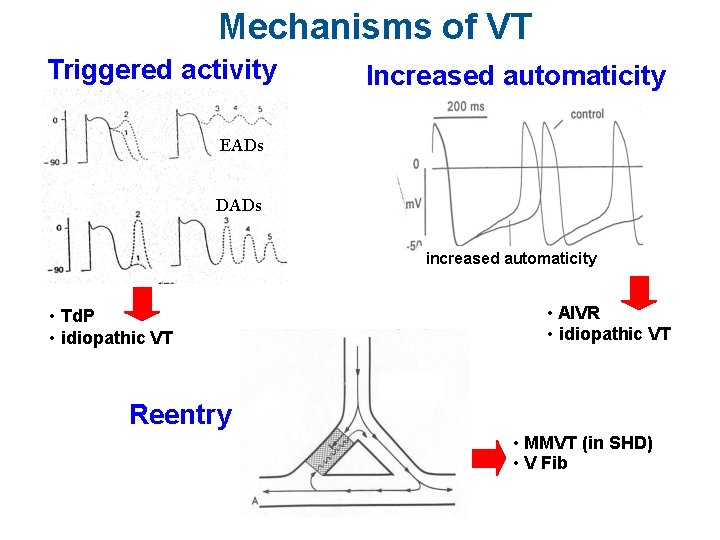
Mechanisms of VT Triggered activity Increased automaticity EADs DADs increased automaticity • Td. P • idiopathic VT • AIVR • idiopathic VT Reentry • MMVT (in SHD) • V Fib
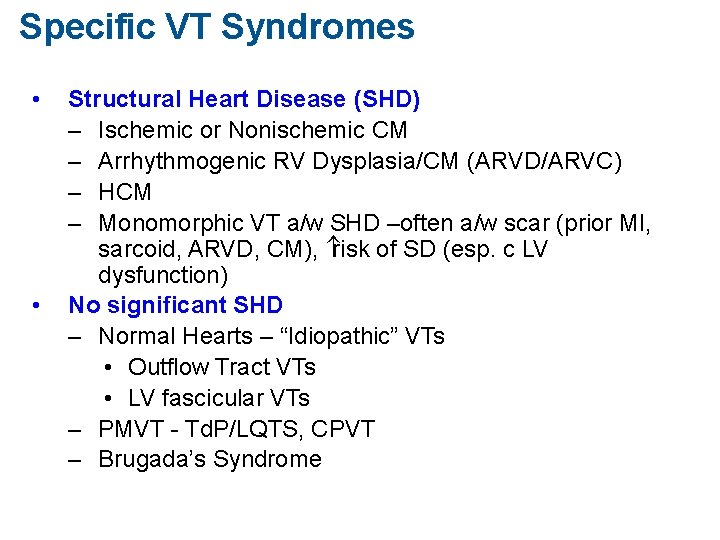
Specific VT Syndromes • • Structural Heart Disease (SHD) – Ischemic or Nonischemic CM – Arrhythmogenic RV Dysplasia/CM (ARVD/ARVC) – HCM – Monomorphic VT a/w SHD –often a/w scar (prior MI, sarcoid, ARVD, CM), risk of SD (esp. c LV dysfunction) No significant SHD – Normal Hearts – “Idiopathic” VTs • Outflow Tract VTs • LV fascicular VTs – PMVT - Td. P/LQTS, CPVT – Brugada’s Syndrome
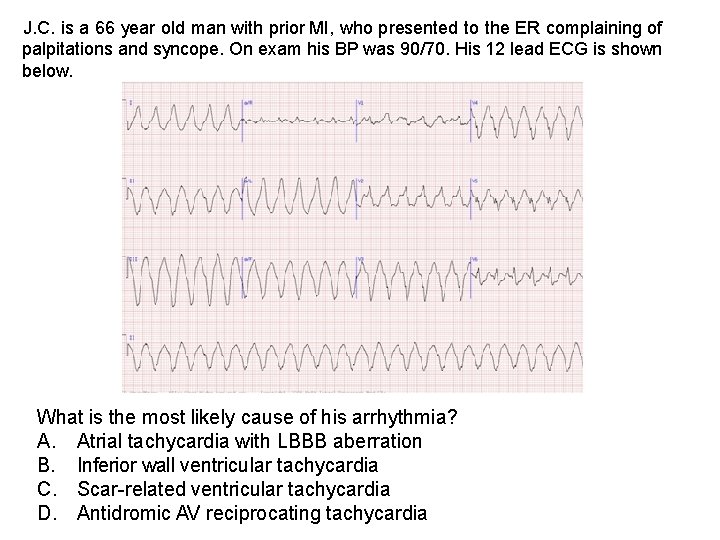
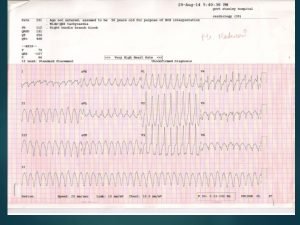
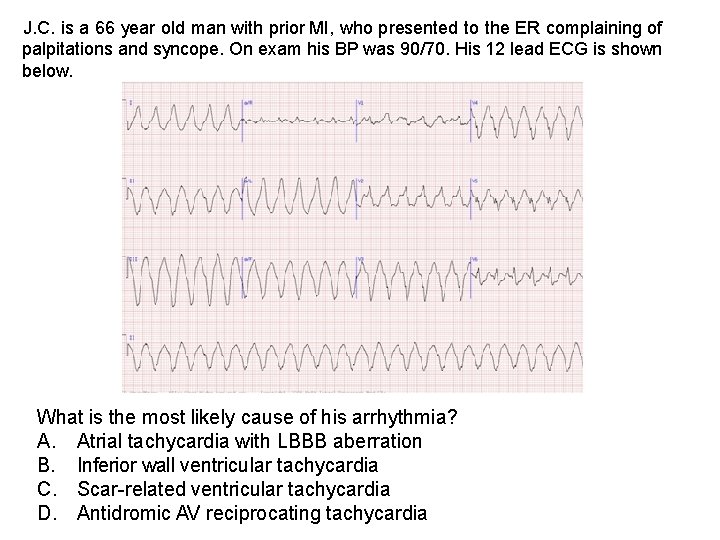
J. C. is a 66 year old man with prior MI, who presented to the ER complaining of palpitations and syncope. On exam his BP was 90/70. His 12 lead ECG is shown below. What is the most likely cause of his arrhythmia? A. Atrial tachycardia with LBBB aberration B. Inferior wall ventricular tachycardia C. Scar-related ventricular tachycardia D. Antidromic AV reciprocating tachycardia


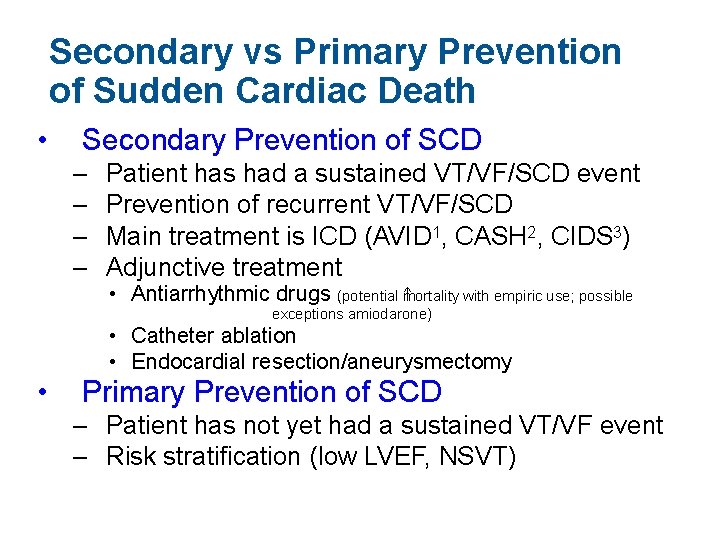
Secondary vs Primary Prevention of Sudden Cardiac Death • Secondary Prevention of SCD – – Patient has had a sustained VT/VF/SCD event Prevention of recurrent VT/VF/SCD Main treatment is ICD (AVID 1, CASH 2, CIDS 3) Adjunctive treatment • Antiarrhythmic drugs (potential m ortality with empiric use; possible exceptions amiodarone) • Catheter ablation • Endocardial resection/aneurysmectomy • Primary Prevention of SCD – Patient has not yet had a sustained VT/VF event – Risk stratification (low LVEF, NSVT) AVID Investigators NEJM 1997; 337: 1576 -84; 2 Kuck et al Circulation 2000; 102: 748 -54; 3 Connolly et al Circulaton 2000; 101: 1297 -1302 1
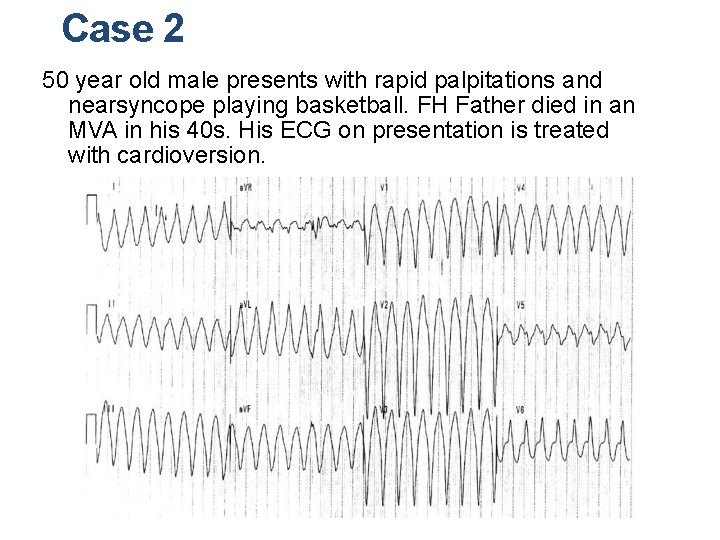
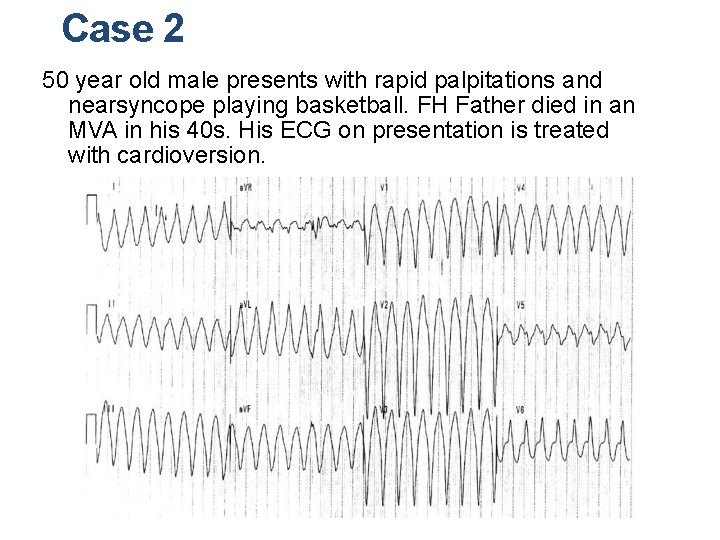
Case 2 50 year old male presents with rapid palpitations and nearsyncope playing basketball. FH Father died in an MVA in his 40 s. His ECG on presentation is treated with cardioversion.
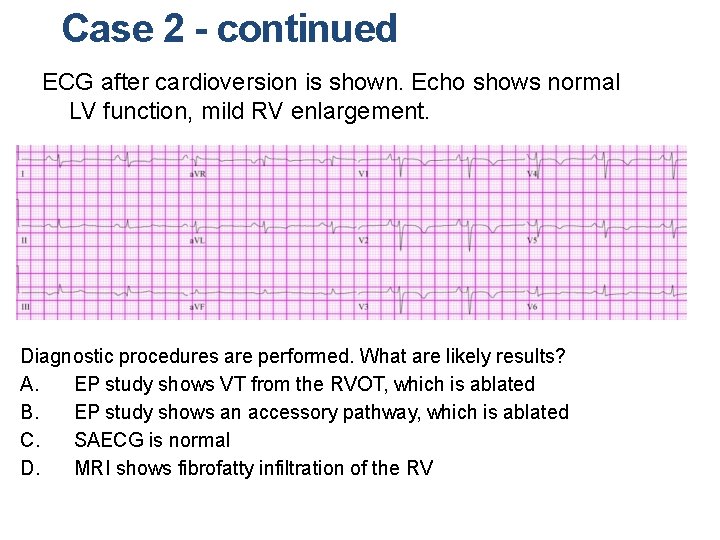
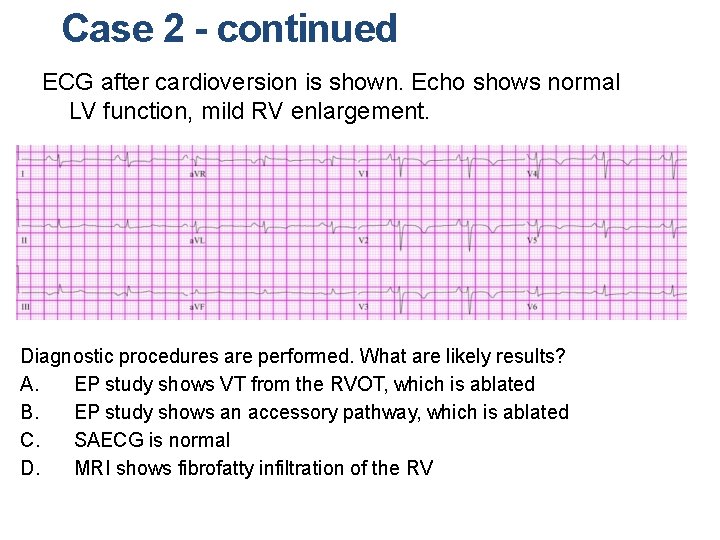
Case 2 - continued ECG after cardioversion is shown. Echo shows normal LV function, mild RV enlargement. Diagnostic procedures are performed. What are likely results? A. EP study shows VT from the RVOT, which is ablated B. EP study shows an accessory pathway, which is ablated C. SAECG is normal D. MRI shows fibrofatty infiltration of the RV
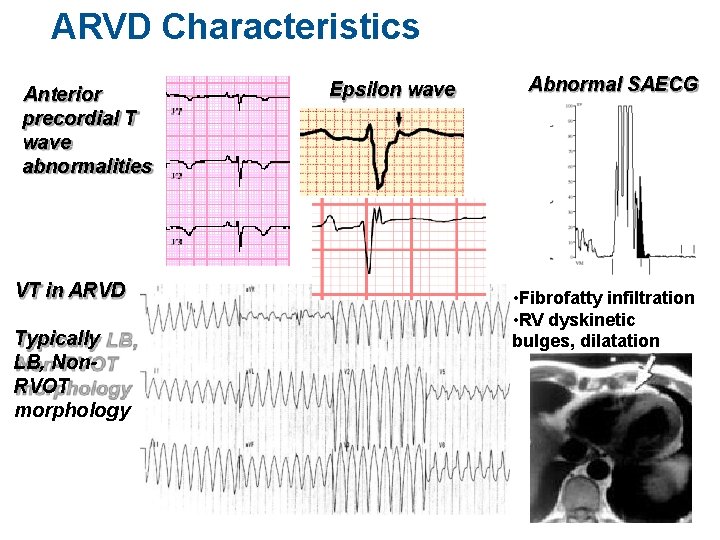
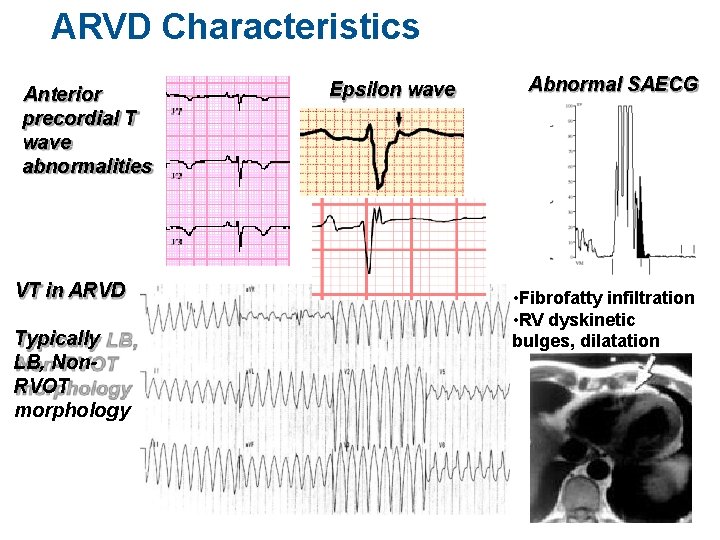
ARVD Characteristics Anterior precordial T wave abnormalities VT in ARVD Typically LB, Non. RVOT morphology Epsilon wave Abnormal SAECG From: Mc. Rae et al, CCJM 68: 459 -67, 2001 • Fibrofatty infiltration • RV dyskinetic bulges, dilatation T. H.
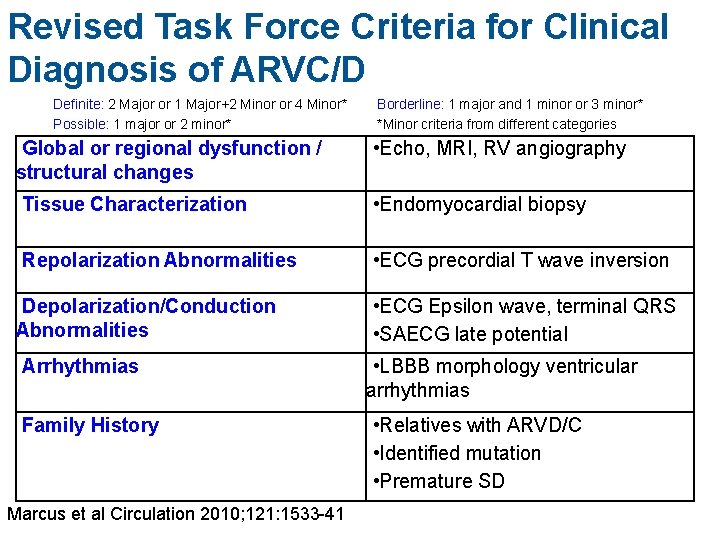
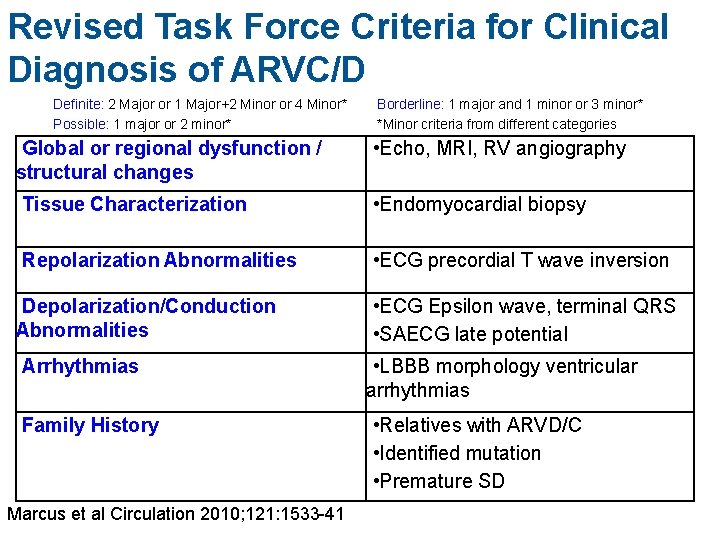
Revised Task Force Criteria for Clinical Diagnosis of ARVC/D Definite: 2 Major or 1 Major+2 Minor or 4 Minor* Possible: 1 major or 2 minor* Global or regional dysfunction / structural changes Borderline: 1 major and 1 minor or 3 minor* *Minor criteria from different categories • Echo, MRI, RV angiography Tissue Characterization • Endomyocardial biopsy Repolarization Abnormalities • ECG precordial T wave inversion Depolarization/Conduction Abnormalities Arrhythmias Family History Marcus et al Circulation 2010; 121: 1533 -41 • ECG Epsilon wave, terminal QRS • SAECG late potential • LBBB morphology ventricular arrhythmias • Relatives with ARVD/C • Identified mutation • Premature SD
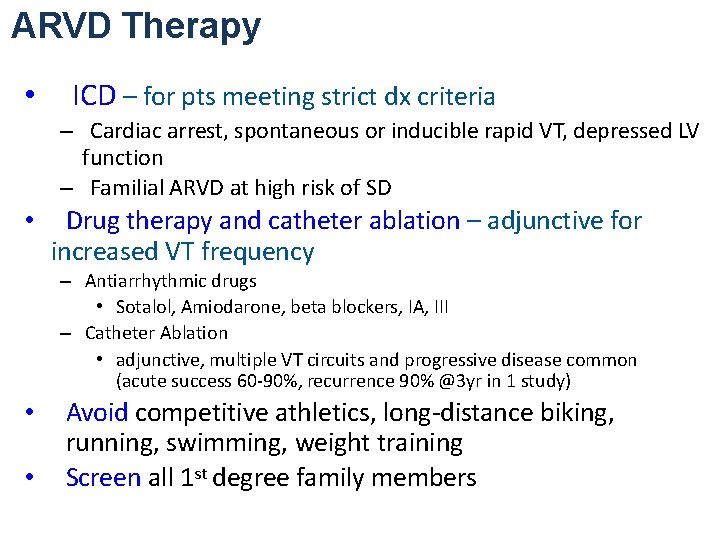
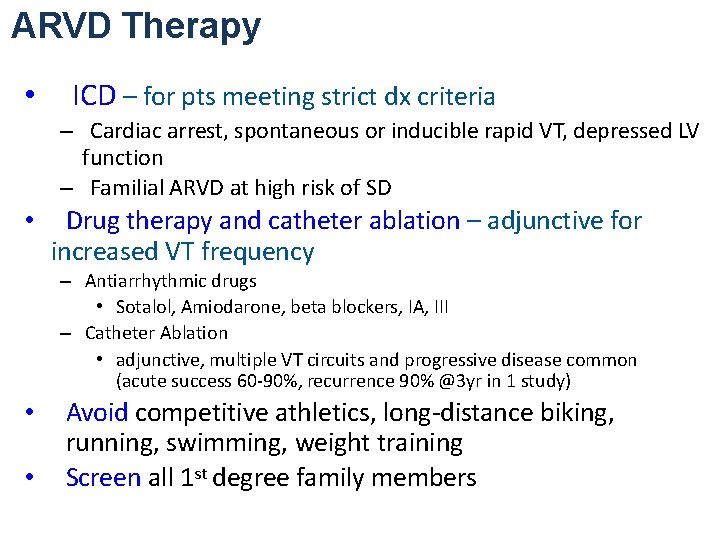
ARVD Therapy • ICD – for pts meeting strict dx criteria – Cardiac arrest, spontaneous or inducible rapid VT, depressed LV function – Familial ARVD at high risk of SD • Drug therapy and catheter ablation – adjunctive for increased VT frequency – Antiarrhythmic drugs • Sotalol, Amiodarone, beta blockers, IA, III – Catheter Ablation • adjunctive, multiple VT circuits and progressive disease common (acute success 60 -90%, recurrence 90% @3 yr in 1 study) • • Avoid competitive athletics, long-distance biking, running, swimming, weight training Screen all 1 st degree family members
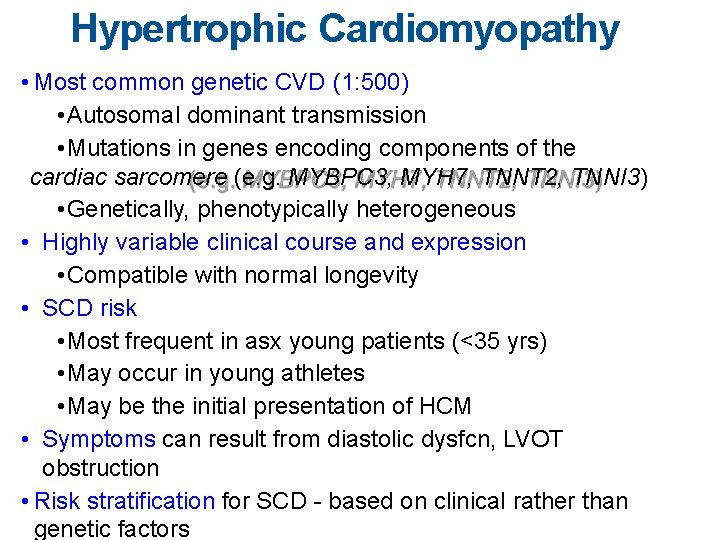
Hypertrophic Cardiomyopathy • Most common genetic CVD (1: 500) • Autosomal dominant transmission • Mutations in genes encoding components of the cardiac sarcomere (e. g. MYBPC 3, MYH 7, TNNT 2, TNNI 3) • Genetically, phenotypically heterogeneous • Highly variable clinical course and expression • Compatible with normal longevity • SCD risk • Most frequent in asx young patients (<35 yrs) • May occur in young athletes • May be the initial presentation of HCM • Symptoms can result from diastolic dysfcn, LVOT obstruction • Risk stratification for SCD - based on clinical rather than genetic factors
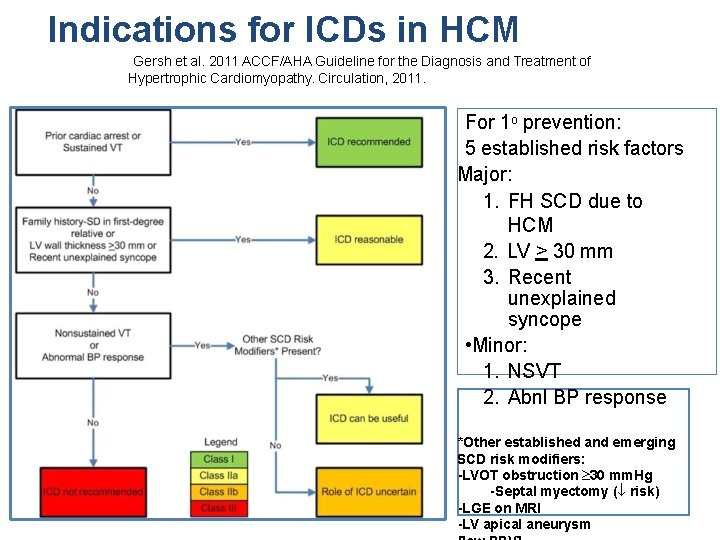
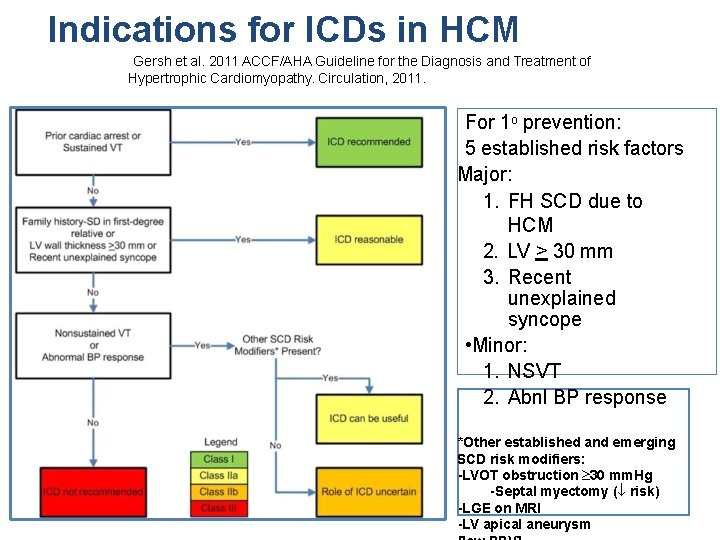
Indications for ICDs in HCM Gersh et al. 2011 ACCF/AHA Guideline for the Diagnosis and Treatment of Hypertrophic Cardiomyopathy. Circulation, 2011. For 1 o prevention: 5 established risk factors Major: 1. FH SCD due to HCM 2. LV > 30 mm 3. Recent unexplained syncope • Minor: 1. NSVT 2. Abnl BP response *Other established and emerging SCD risk modifiers: -LVOT obstruction ³ 30 mm. Hg -Septal myectomy (¯ risk) -LGE on MRI -LV apical aneurysm
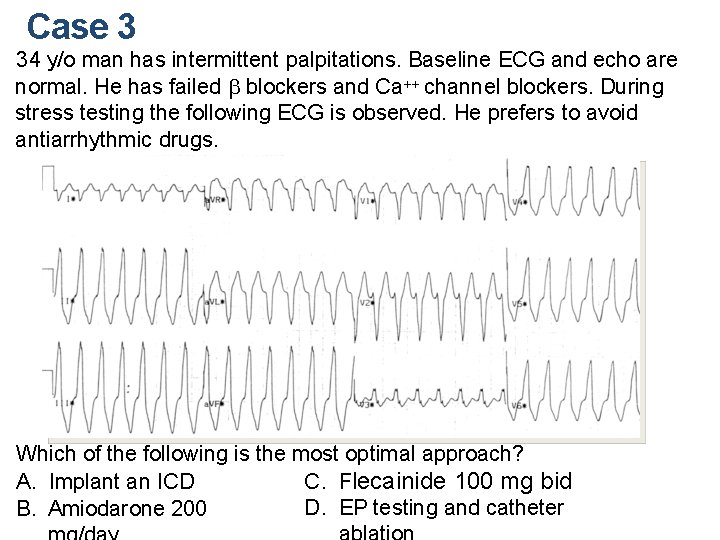
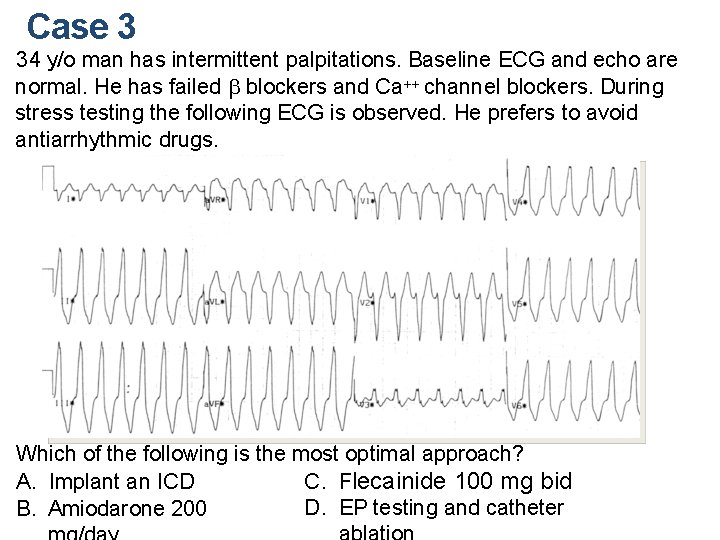
Case 3 34 y/o man has intermittent palpitations. Baseline ECG and echo are normal. He has failed b blockers and Ca++ channel blockers. During stress testing the following ECG is observed. He prefers to avoid antiarrhythmic drugs. Which of the following is the most optimal approach? C. Flecainide 100 mg bid A. Implant an ICD D. EP testing and catheter B. Amiodarone 200
“Idiopathic” VT in NORMAL HEARTS • • Outflow Tract VT (e. g. RVOT, LVOT, aortic cusp) Idiopathic LV (fascicular) VT
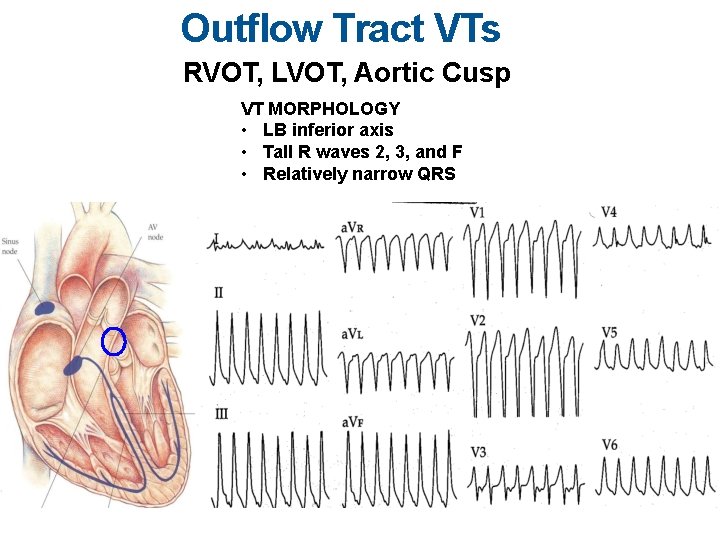
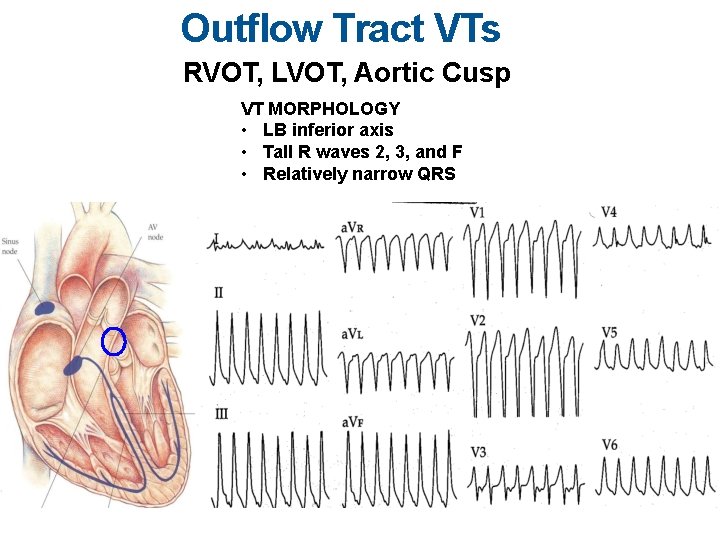
Outflow Tract VTs RVOT, LVOT, Aortic Cusp VT MORPHOLOGY • LB inferior axis • Tall R waves 2, 3, and F • Relatively narrow QRS
Repetitive Monomorphic Idiopathic VT VT pattern • Frequent PVCs • Repetitive runs of NSVT • Sustained VT
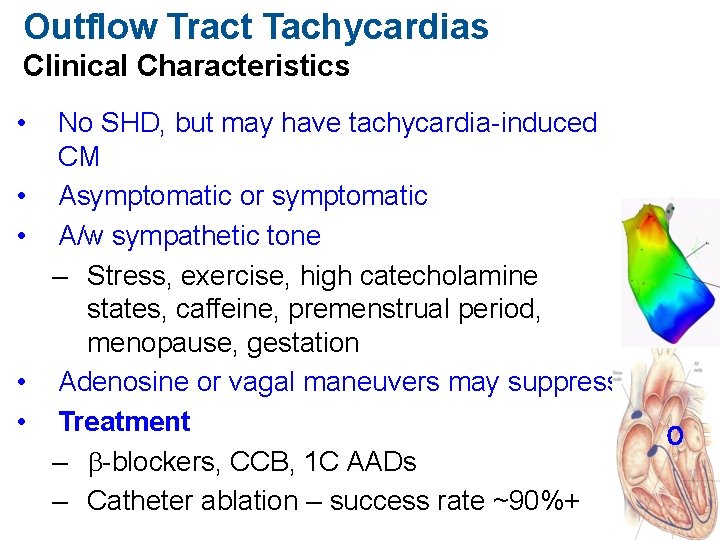
Outflow Tract Tachycardias Clinical Characteristics • • • No SHD, but may have tachycardia-induced CM Asymptomatic or symptomatic A/w sympathetic tone – Stress, exercise, high catecholamine states, caffeine, premenstrual period, menopause, gestation Adenosine or vagal maneuvers may suppress Treatment – b-blockers, CCB, 1 C AADs – Catheter ablation – success rate ~90%+
VT in normal hearts #2 Idiopathic LV or Fascicular VT (ILVT) • Paroxysmal VT • Reentry in Ca++ dependent Purkinje-fascicular fibers • Potentiated, though not typically precipitated by exercise • RBBB morphology – Most common RB/LSA (LAD, - in II, a. VF) • No definite SHD; normal SAECG • Terminated or suppressed by verapamil or diltiazem – NOT usually adenosine sensitive • Ablation: sites where the VT is preceded by a Purkinje/fascicular potential – Most common site – LV inferior septum (mid-apical)
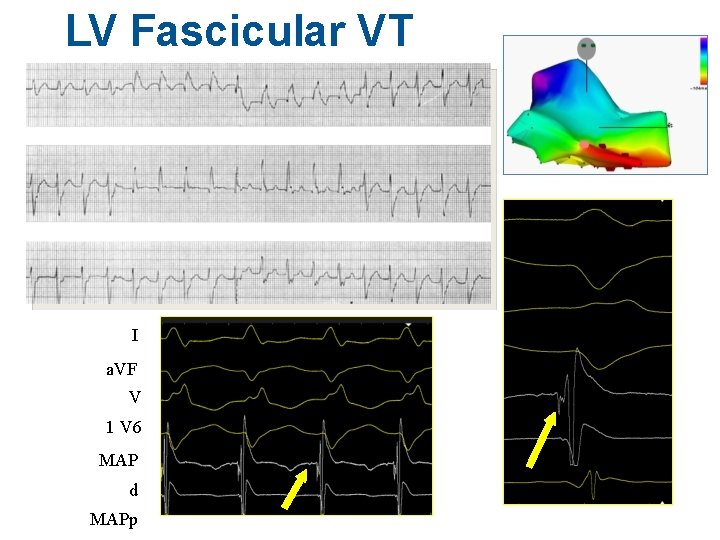
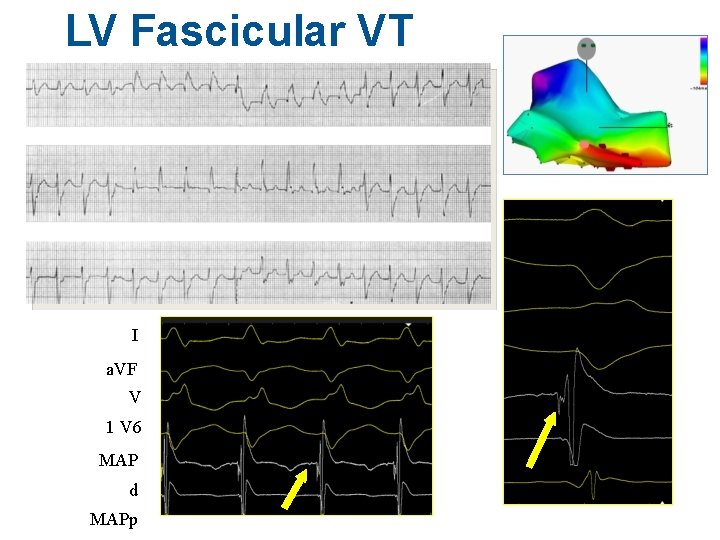
LV Fascicular VT I a. VF V 1 V 6 MAP d MAPp
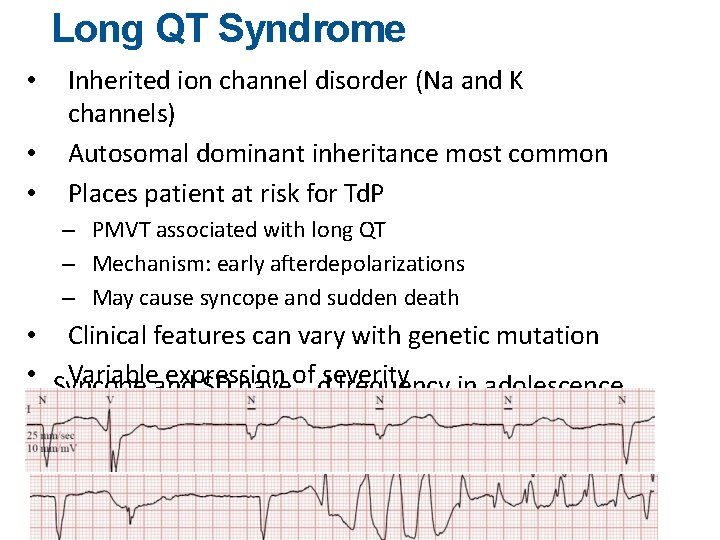
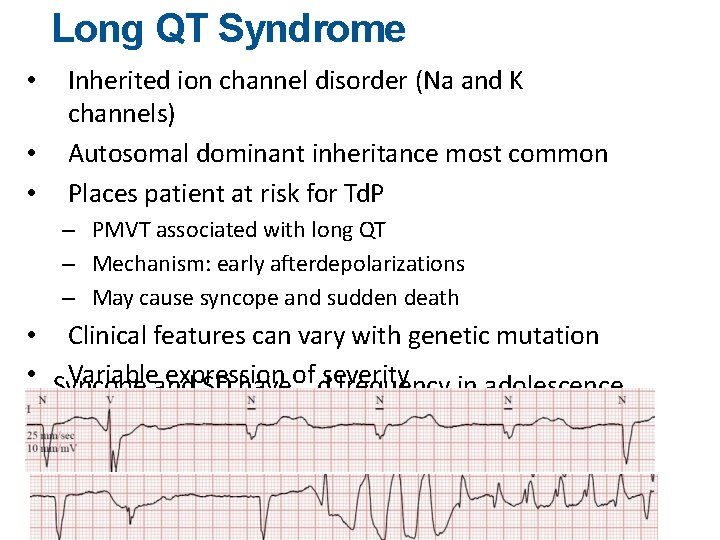
Long QT Syndrome • • • Inherited ion channel disorder (Na and K channels) Autosomal dominant inheritance most common Places patient at risk for Td. P – PMVT associated with long QT – Mechanism: early afterdepolarizations – May cause syncope and sudden death • Clinical features can vary with genetic mutation • Syncope Variableand expression SD haveof dseverity frequency in adolescence •
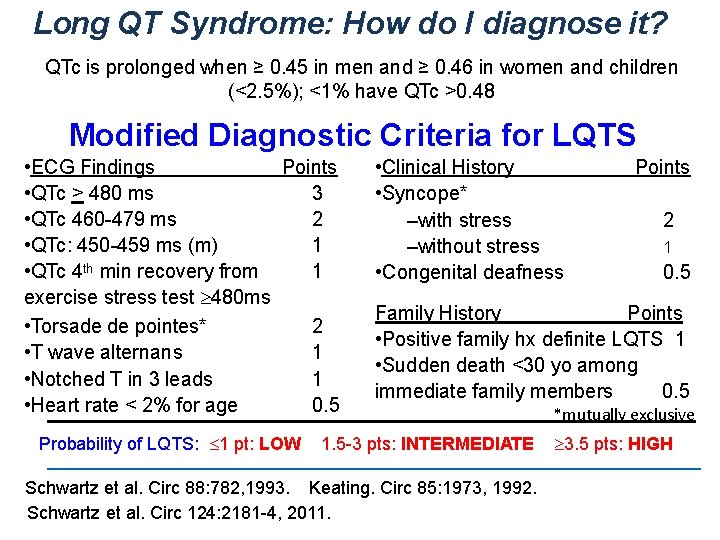
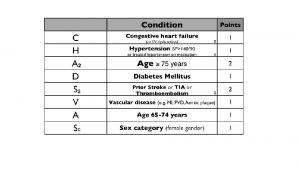
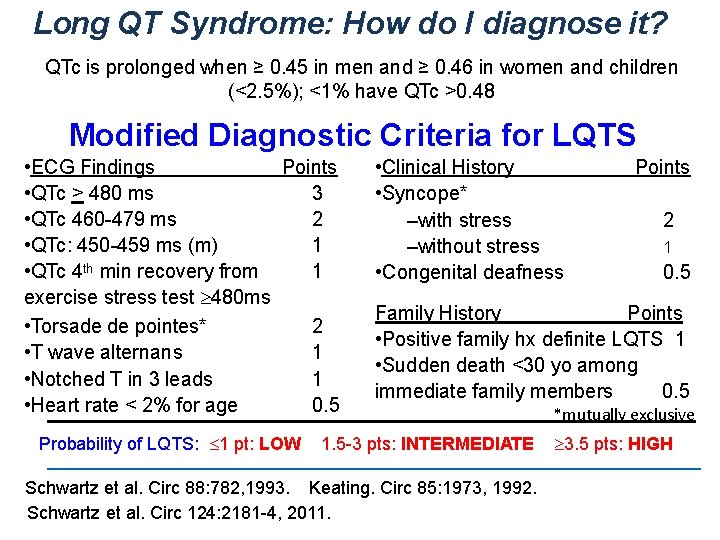
Long QT Syndrome: How do I diagnose it? QTc is prolonged when ≥ 0. 45 in men and ≥ 0. 46 in women and children (<2. 5%); <1% have QTc >0. 48 Modified Diagnostic Criteria for LQTS • ECG Findings Points • QTc > 480 ms 3 • QTc 460 -479 ms 2 • QTc: 450 -459 ms (m) 1 • QTc 4 th min recovery from 1 exercise stress test ³ 480 ms • Torsade de pointes* 2 • T wave alternans 1 • Notched T in 3 leads 1 • Heart rate < 2% for age 0. 5 Probability of LQTS: £ 1 pt: LOW • Clinical History • Syncope* –with stress –without stress • Congenital deafness Points 2 1 0. 5 Family History Points • Positive family hx definite LQTS 1 • Sudden death <30 yo among immediate family members 0. 5 1. 5 -3 pts: INTERMEDIATE Schwartz et al. Circ 88: 782, 1993. Keating. Circ 85: 1973, 1992. Schwartz et al. Circ 124: 2181 -4, 2011. *mutually exclusive ³ 3. 5 pts: HIGH
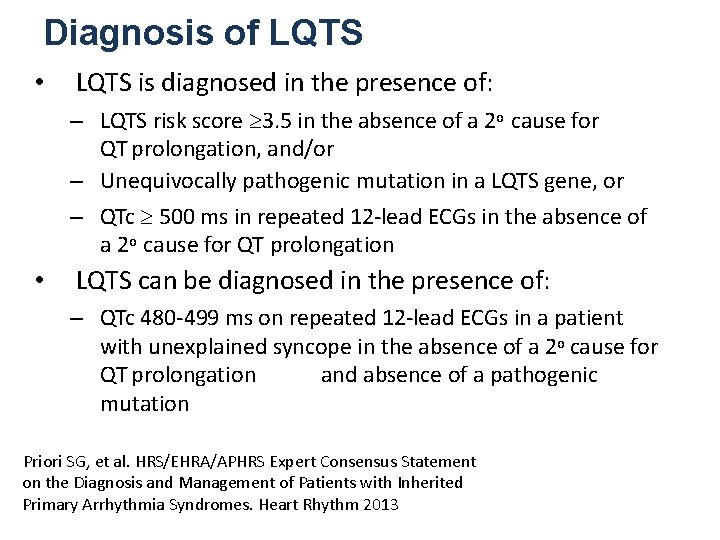
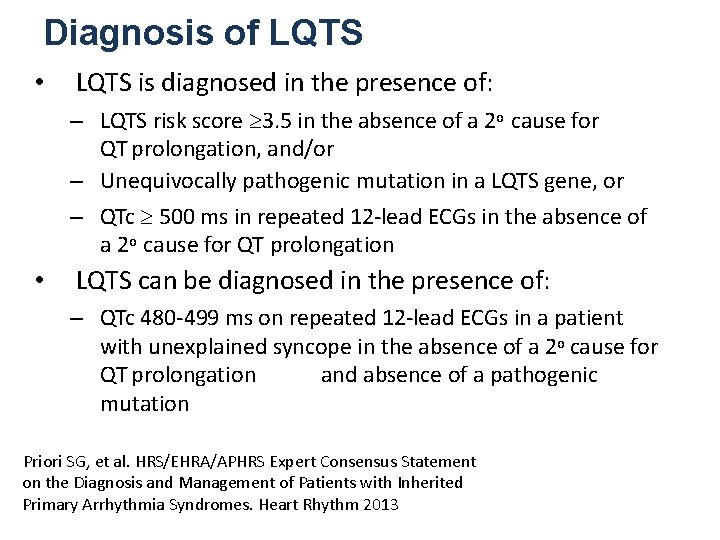
Diagnosis of LQTS • LQTS is diagnosed in the presence of: – LQTS risk score ³ 3. 5 in the absence of a 2 o cause for QT prolongation, and/or – Unequivocally pathogenic mutation in a LQTS gene, or – QTc ³ 500 ms in repeated 12 -lead ECGs in the absence of a 2 o cause for QT prolongation • LQTS can be diagnosed in the presence of: – QTc 480 -499 ms on repeated 12 -lead ECGs in a patient with unexplained syncope in the absence of a 2 o cause for QT prolongation and absence of a pathogenic mutation Priori SG, et al. HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes. Heart Rhythm 2013
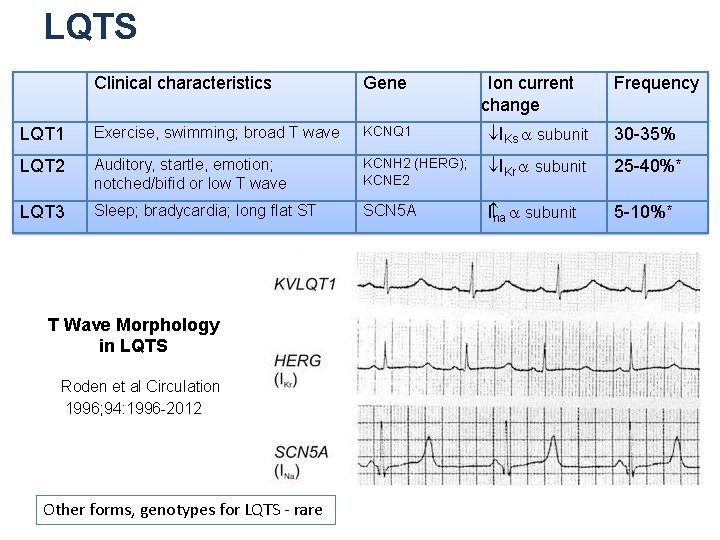
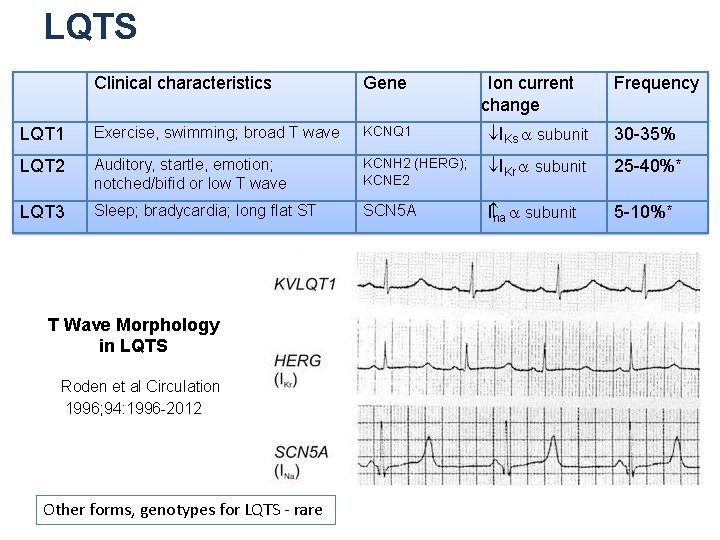
LQTS Clinical characteristics Gene LQT 1 Exercise, swimming; broad T wave KCNQ 1 ¯IKs a subunit 30 -35% LQT 2 Auditory, startle, emotion; notched/bifid or low T wave KCNH 2 (HERG); KCNE 2 ¯IKr a subunit 25 -40%* LQT 3 Sleep; bradycardia; long flat ST SCN 5 A I na a subunit 5 -10%* T Wave Morphology in LQTS Roden et al Circulation 1996; 94: 1996 -2012 Other forms, genotypes for LQTS - rare Ion current change Frequency
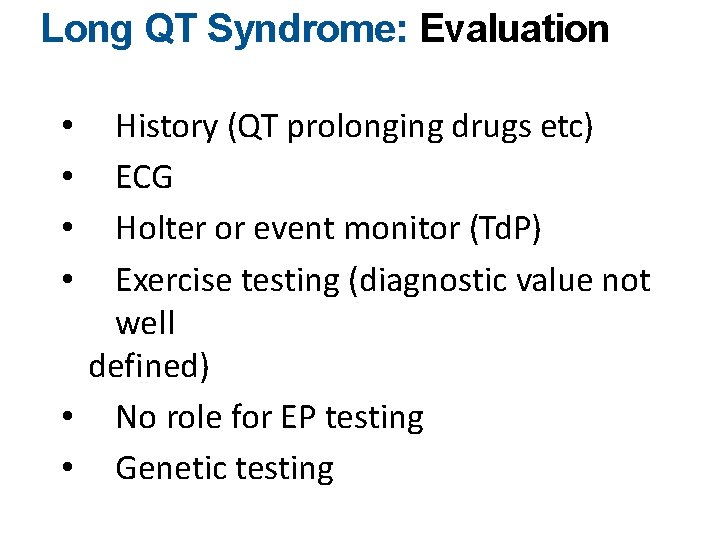
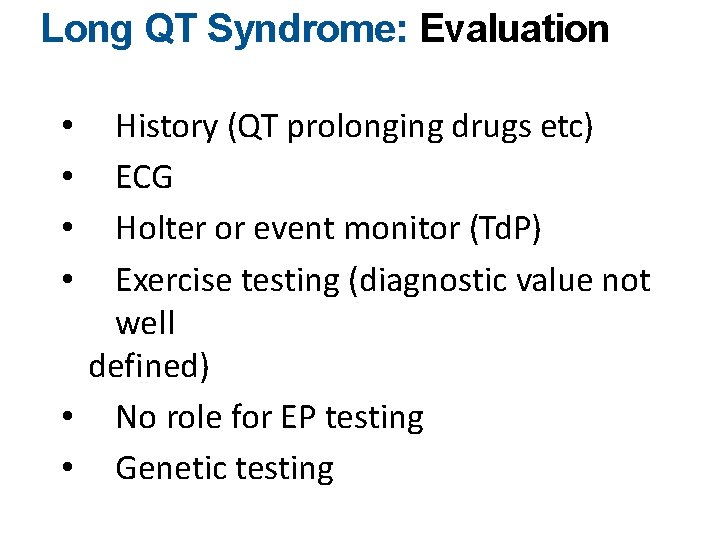
Long QT Syndrome: Evaluation History (QT prolonging drugs etc) ECG Holter or event monitor (Td. P) Exercise testing (diagnostic value not well defined) • No role for EP testing • Genetic testing • •
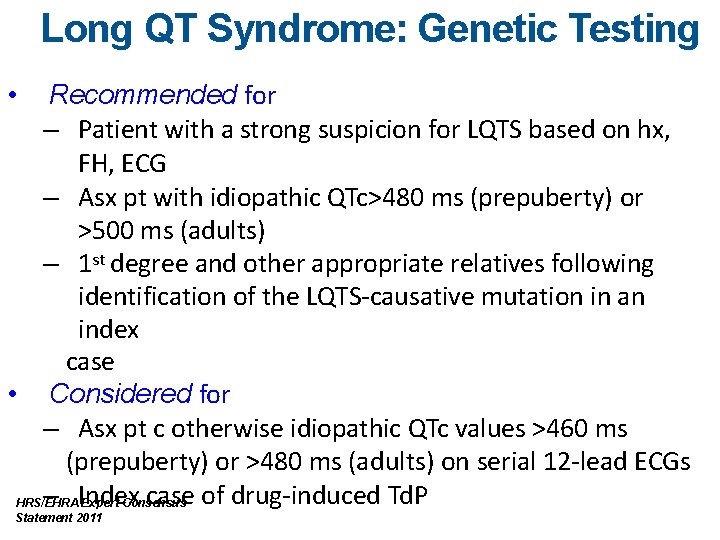
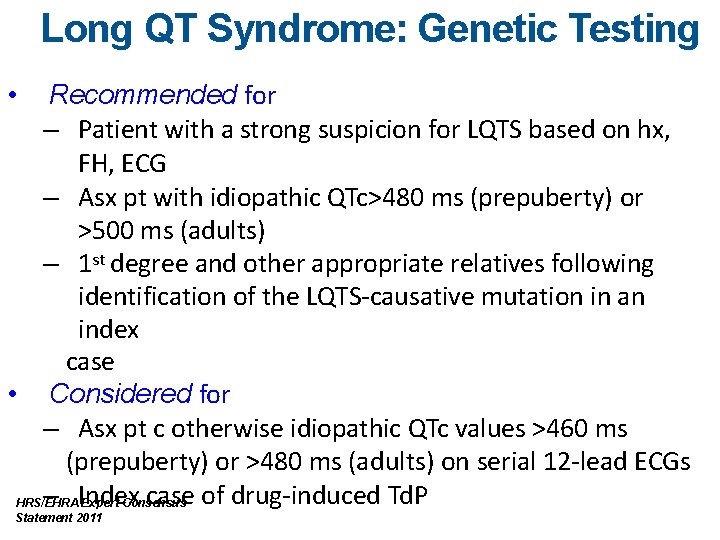
Long QT Syndrome: Genetic Testing Recommended for – Patient with a strong suspicion for LQTS based on hx, FH, ECG – Asx pt with idiopathic QTc>480 ms (prepuberty) or >500 ms (adults) – 1 st degree and other appropriate relatives following identification of the LQTS-causative mutation in an index case • Considered for – Asx pt c otherwise idiopathic QTc values >460 ms (prepuberty) or >480 ms (adults) on serial 12 -lead ECGs – Index case of drug-induced Td. P HRS/EHRA Expert Consensus • Statement 2011
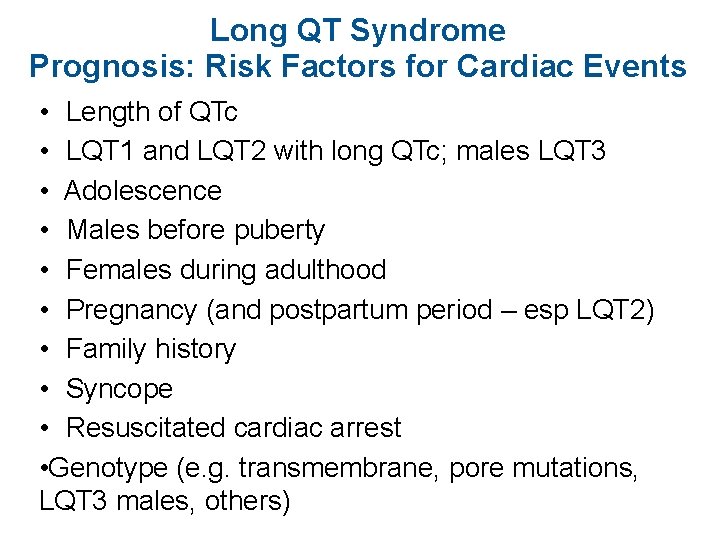
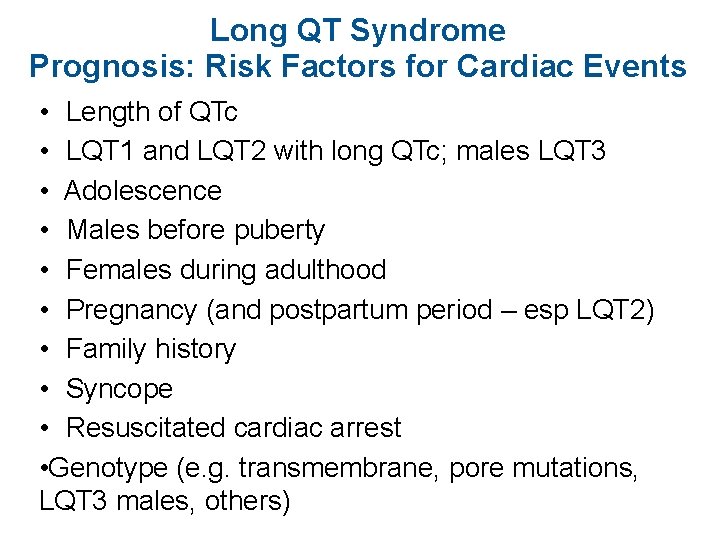
Long QT Syndrome Prognosis: Risk Factors for Cardiac Events • Length of QTc • LQT 1 and LQT 2 with long QTc; males LQT 3 • Adolescence • Males before puberty • Females during adulthood • Pregnancy (and postpartum period – esp LQT 2) • Family history • Syncope • Resuscitated cardiac arrest • Genotype (e. g. transmembrane, pore mutations, LQT 3 males, others)
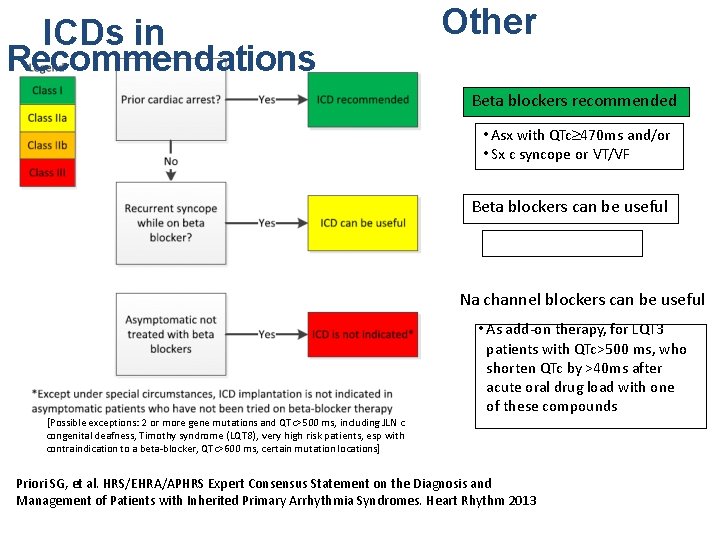
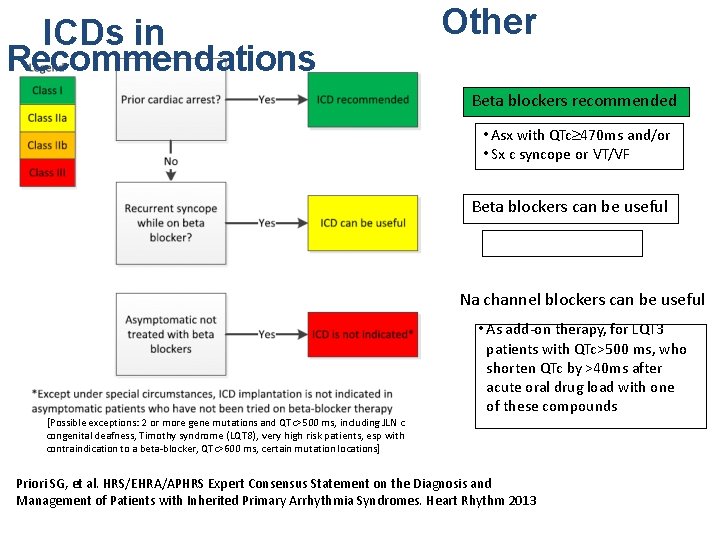
ICDs in Recommendations LQTS Other Beta blockers recommended • Asx with QTc³ 470 ms and/or • Sx c syncope or VT/VF Beta blockers can be useful • Asx with QTc£ 470 ms Na channel blockers can be useful • As add-on therapy, for LQT 3 patients with QTc>500 ms, who shorten QTc by >40 ms after acute oral drug load with one of these compounds [Possible exceptions: 2 or more gene mutations and QTc>500 ms, including JLN c congenital deafness, Timothy syndrome (LQT 8), very high risk patients, esp with contraindication to a beta-blocker, QTc>600 ms, certain mutation locations] Priori SG, et al. HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes. Heart Rhythm 2013
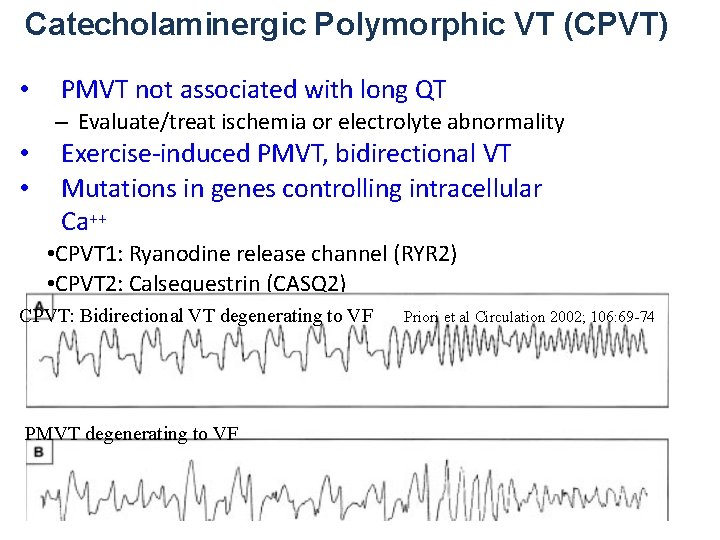
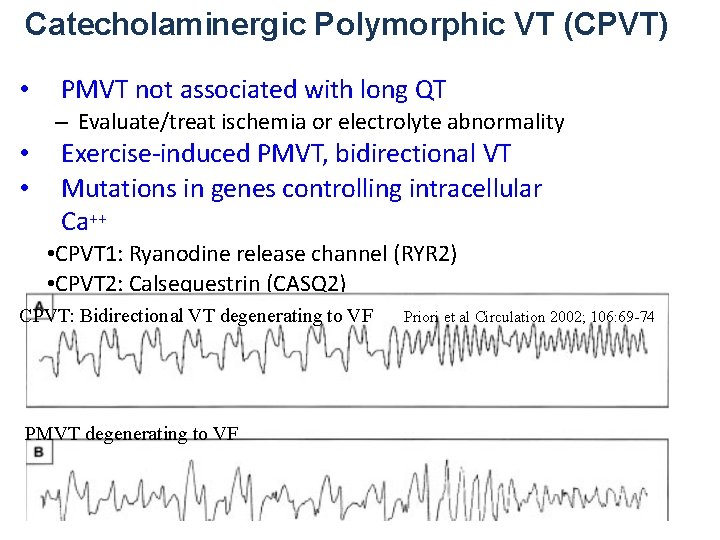
Catecholaminergic Polymorphic VT (CPVT) • PMVT not associated with long QT – Evaluate/treat ischemia or electrolyte abnormality • • Exercise-induced PMVT, bidirectional VT Mutations in genes controlling intracellular Ca++ • CPVT 1: Ryanodine release channel (RYR 2) • CPVT 2: Calsequestrin (CASQ 2) • Other loci postulated CPVT: Bidirectional VT degenerating to VF Priori et al Circulation 2002; 106: 69 -74 PMVT degenerating to VF
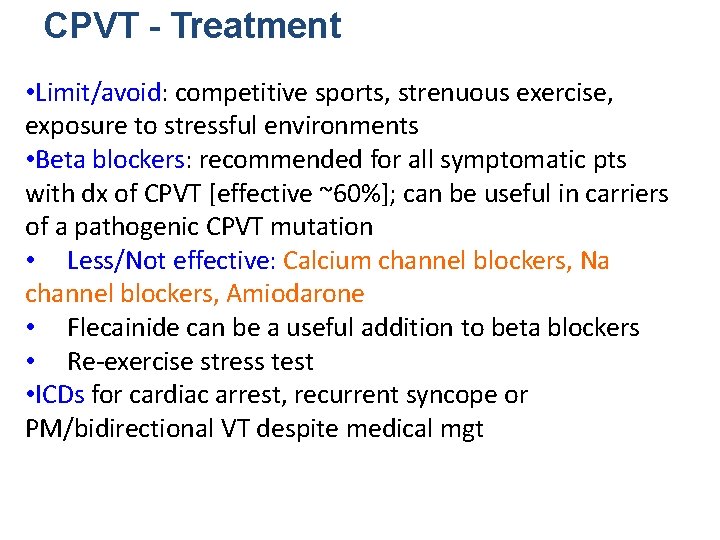
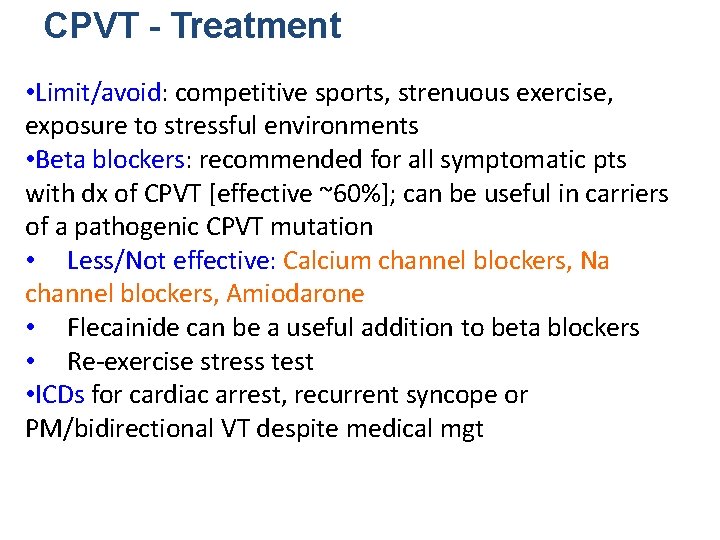
CPVT - Treatment • Limit/avoid: competitive sports, strenuous exercise, exposure to stressful environments • Beta blockers: recommended for all symptomatic pts with dx of CPVT [effective ~60%]; can be useful in carriers of a pathogenic CPVT mutation • Less/Not effective: Calcium channel blockers, Na channel blockers, Amiodarone • Flecainide can be a useful addition to beta blockers • Re-exercise stress test • ICDs for cardiac arrest, recurrent syncope or PM/bidirectional VT despite medical mgt
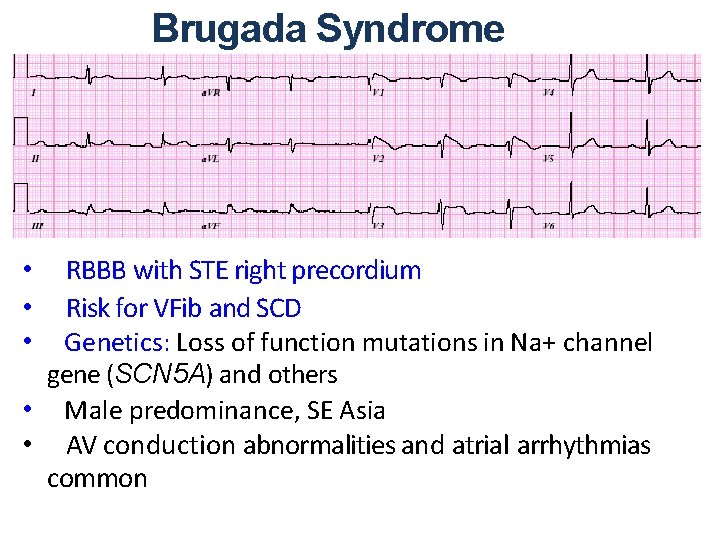
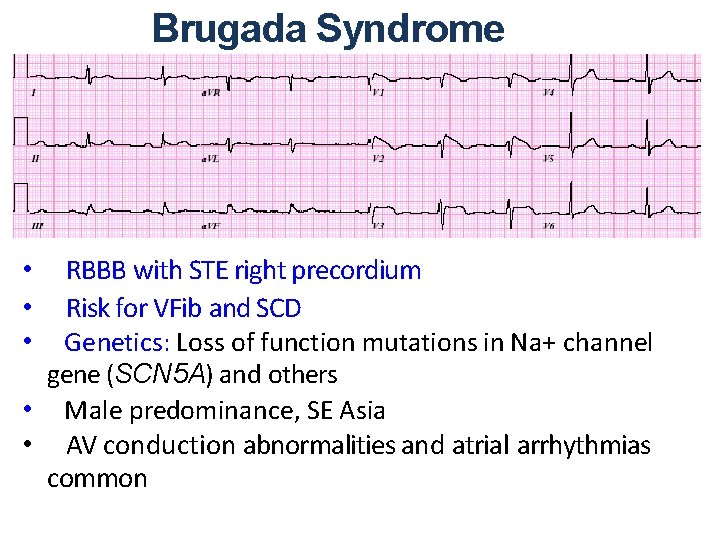
Brugada Syndrome RBBB with STE right precordium Risk for VFib and SCD Genetics: Loss of function mutations in Na+ channel gene (SCN 5 A) and others • Male predominance, SE Asia • AV conduction abnormalities and atrial arrhythmias common • • •
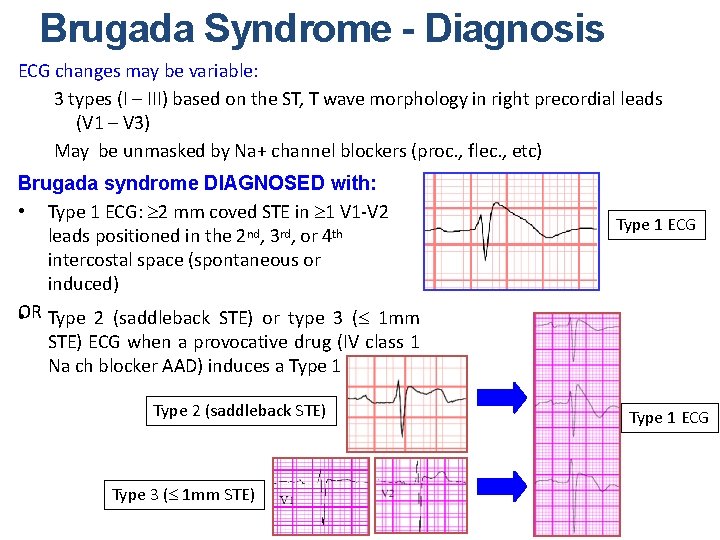
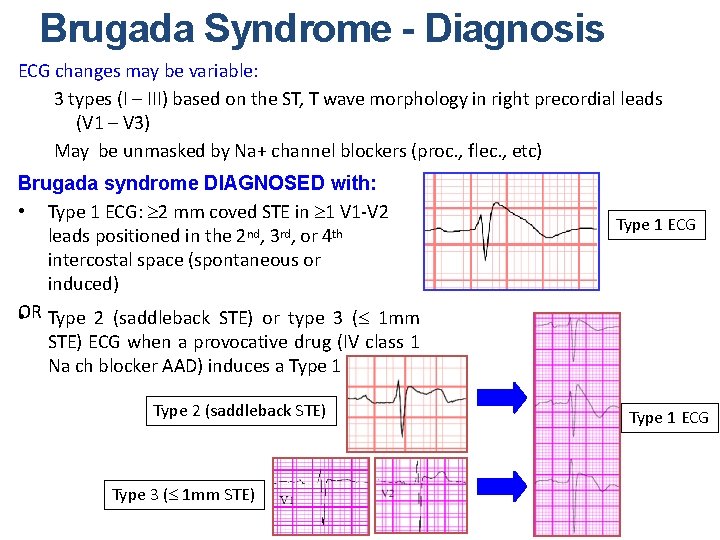
Brugada Syndrome - Diagnosis ECG changes may be variable: 3 types (I – III) based on the ST, T wave morphology in right precordial leads (V 1 – V 3) May be unmasked by Na+ channel blockers (proc. , flec. , etc) Brugada syndrome DIAGNOSED with: • Type 1 ECG: ³ 2 mm coved STE in ³ 1 V 1 -V 2 leads positioned in the 2 nd, 3 rd, or 4 th intercostal space (spontaneous or induced) OR • Type 2 (saddleback STE) or type 3 (£ 1 mm Type 1 ECG STE) ECG when a provocative drug (IV class 1 Na ch blocker AAD) induces a Type 1 ECG Type 2 (saddleback STE) Type 3 (£ 1 mm STE) Type 1 ECG
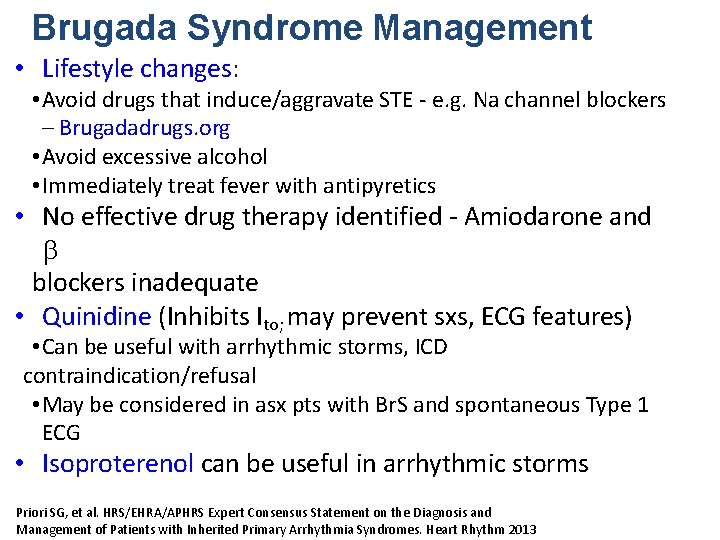
Brugada Syndrome Management • Lifestyle changes: • Avoid drugs that induce/aggravate STE - e. g. Na channel blockers – Brugadadrugs. org • Avoid excessive alcohol • Immediately treat fever with antipyretics • No effective drug therapy identified - Amiodarone and b blockers inadequate • Quinidine (Inhibits Ito; may prevent sxs, ECG features) • Can be useful with arrhythmic storms, ICD contraindication/refusal • May be considered in asx pts with Br. S and spontaneous Type 1 ECG • Isoproterenol can be useful in arrhythmic storms Priori SG, et al. HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes. Heart Rhythm 2013
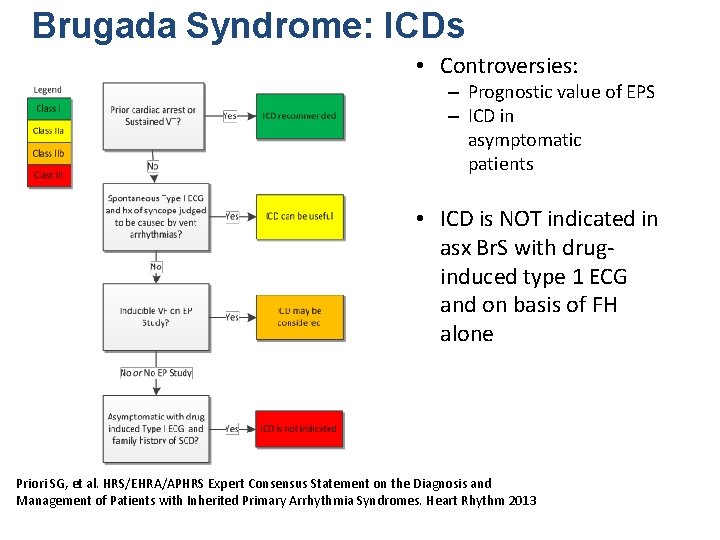
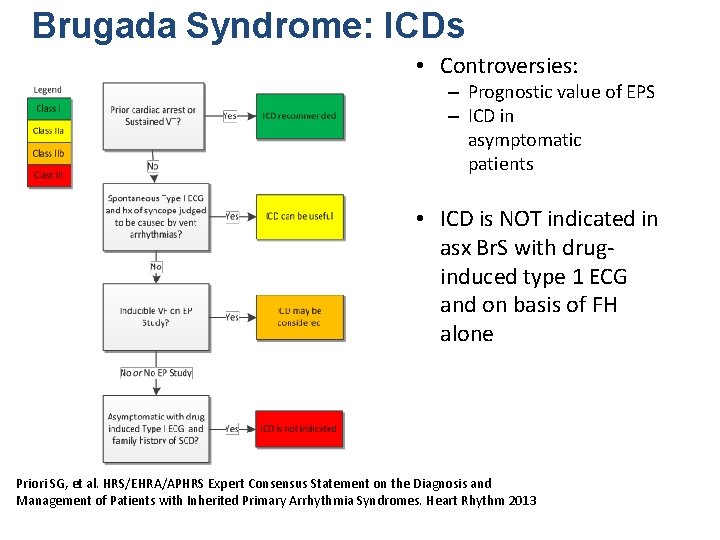
Brugada Syndrome: ICDs • Controversies: – Prognostic value of EPS – ICD in asymptomatic patients • ICD is NOT indicated in asx Br. S with druginduced type 1 ECG and on basis of FH alone Priori SG, et al. HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes. Heart Rhythm 2013
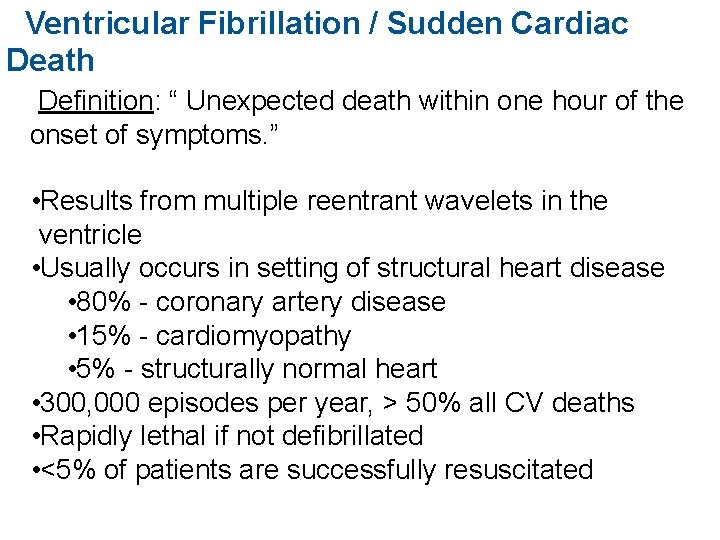
Ventricular Fibrillation / Sudden Cardiac Death Definition: “ Unexpected death within one hour of the onset of symptoms. ” • Results from multiple reentrant wavelets in the ventricle • Usually occurs in setting of structural heart disease • 80% - coronary artery disease • 15% - cardiomyopathy • 5% - structurally normal heart • 300, 000 episodes per year, > 50% all CV deaths • Rapidly lethal if not defibrillated • <5% of patients are successfully resuscitated
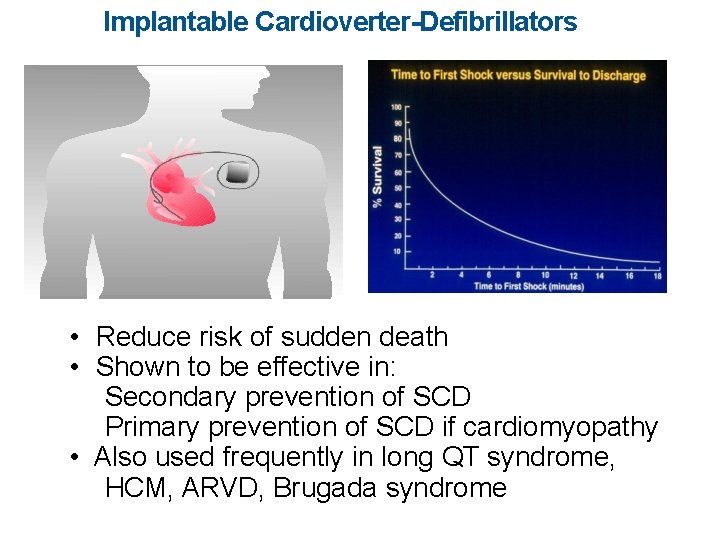
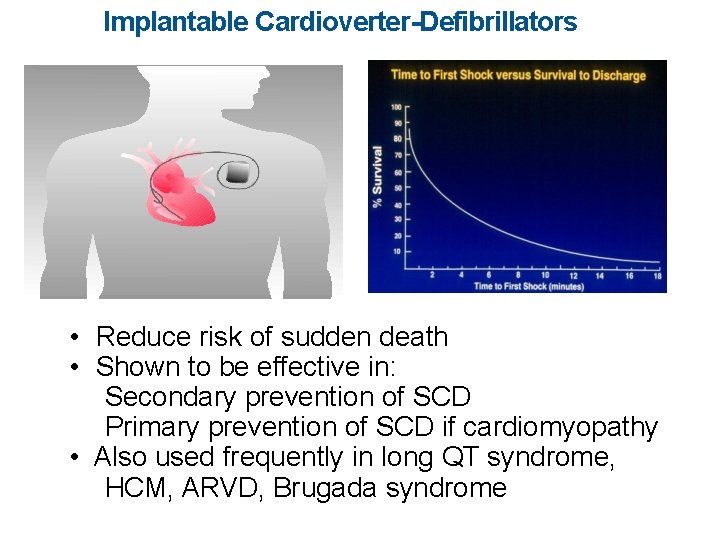
Implantable Cardioverter-Defibrillators • Reduce risk of sudden death • Shown to be effective in: Secondary prevention of SCD Primary prevention of SCD if cardiomyopathy • Also used frequently in long QT syndrome, HCM, ARVD, Brugada syndrome
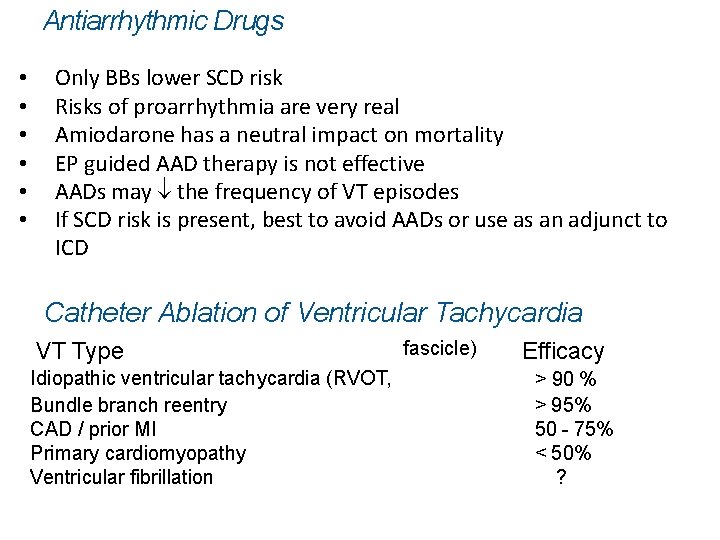
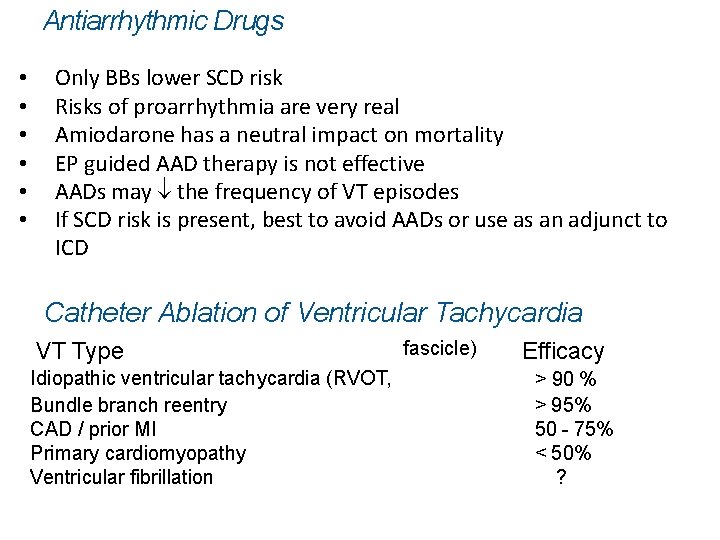
Antiarrhythmic Drugs • • • Only BBs lower SCD risk Risks of proarrhythmia are very real Amiodarone has a neutral impact on mortality EP guided AAD therapy is not effective AADs may ¯ the frequency of VT episodes If SCD risk is present, best to avoid AADs or use as an adjunct to ICD Catheter Ablation of Ventricular Tachycardia VT Type Idiopathic ventricular tachycardia (RVOT, Bundle branch reentry CAD / prior MI Primary cardiomyopathy Ventricular fibrillation fascicle) Efficacy > 90 % > 95% 50 - 75% < 50% ?
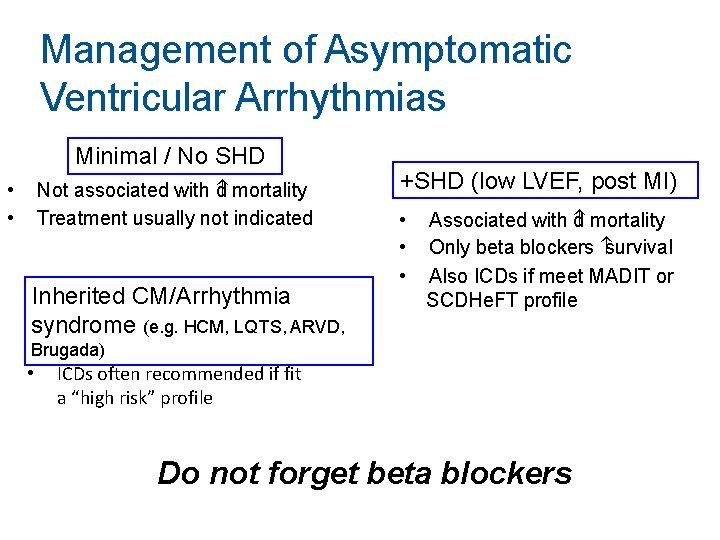
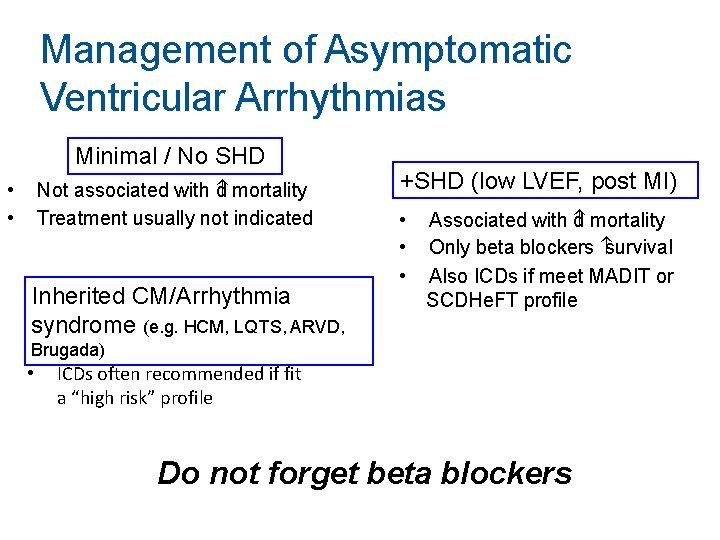
Management of Asymptomatic Ventricular Arrhythmias Minimal / No SHD Not associated with d mortality Treatment usually not indicated • • Inherited CM/Arrhythmia syndrome (e. g. HCM, LQTS, ARVD, +SHD (low LVEF, post MI) • • • Associated with d mortality Only beta blockers survival Also ICDs if meet MADIT or SCDHe. FT profile Brugada) • ICDs often recommended if fit a “high risk” profile Do not forget beta blockers
 Ventricular tachycardia治療
Ventricular tachycardia治療 Narrow qrs complex
Narrow qrs complex Junctional bradycardia
Junctional bradycardia Vagal maneuvers
Vagal maneuvers Acls bradycardia algorithm
Acls bradycardia algorithm Als2 tachycardia algorithm
Als2 tachycardia algorithm Junctional dysrhythmia
Junctional dysrhythmia Private als courses
Private als courses Normal qrs interval
Normal qrs interval Dc cardioversion pals
Dc cardioversion pals Orthodromic reciprocating tachycardia
Orthodromic reciprocating tachycardia Sharif
Sharif Mohammad ghoreishi
Mohammad ghoreishi Mohammad ali abtahi
Mohammad ali abtahi Phynetoin
Phynetoin Dr mohammad aman
Dr mohammad aman Mohammad keshavarz
Mohammad keshavarz Refrances
Refrances Mohammad ali javidian
Mohammad ali javidian Anovulation who classification
Anovulation who classification Pearo-nn
Pearo-nn Mohammad irfan bowdoin
Mohammad irfan bowdoin Vlsi
Vlsi Mohammad sharifkhani
Mohammad sharifkhani Pelvic girdle
Pelvic girdle Dr nur mohammad hadi zahalan
Dr nur mohammad hadi zahalan Dr. mohammad diab
Dr. mohammad diab Dr mohammad khan
Dr mohammad khan Kongres melayu 1939 dan 1940
Kongres melayu 1939 dan 1940 Mohammad arjomand
Mohammad arjomand Mohammad sadegh rasooli
Mohammad sadegh rasooli Shaik mohammad tajuddin
Shaik mohammad tajuddin Mohammad sharifkhani
Mohammad sharifkhani Mohammad alomar
Mohammad alomar Mohammad sharifkhani
Mohammad sharifkhani Dr mohammad aman
Dr mohammad aman Mohammad alipour
Mohammad alipour Mohammad ridwan bkn
Mohammad ridwan bkn Laringocele
Laringocele Ventricular system
Ventricular system Fine vs coarse v fib
Fine vs coarse v fib