Urticaria Angioedema Prof Dr Yehia ElGarem MD Definition








- Slides: 32
Urticaria & Angioedema Prof. Dr. Yehia El-Garem, MD
Definition Superficial itchy swellings of the skin due to transient plasma leakage from small blood vessels are known as weals. Deeper swellings of the skin and alimentary tract are called angio-oedema. These may be painful rather than itchy and tend to last longer. Weals and angiooedema often coexist but either may occur alone.
Pathophysiology • Histamine is the most important mediator of urticaria. Histamine is produced and stored in mast cells. There are several mechanisms for histamine release: • Immunologic (Ig. E mediated) • Non immunologic



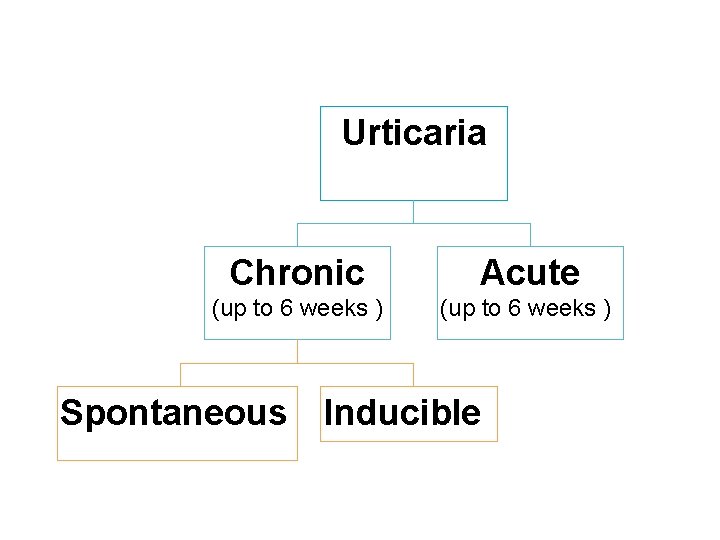
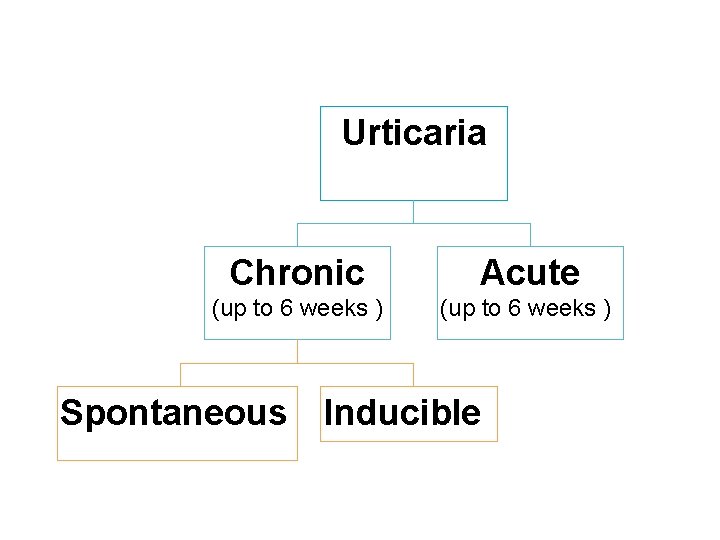
Urticaria Chronic Acute (up to 6 weeks ) Spontaneous Inducible
Causes of Acute urticaria • Idiopathic (50%) • Food: tree nuts, legumes, fish, eggs, milk, soy, wheat…. • Drugs: penicillin, cephalosporin, aspirin, NSAIDs (Ig. E mediated), Acetylsalicylic acid • Infections, mostly acute viral upper respiratory infections (40%)
Causes of Chronic urticaria • • § § Inducible (Physical) Spontaneous: Autoimmune chronic urticaria Idiopathic chronic urticaria
Chronic inducible urticaria (induced by the same physical stimulus): • Cold contact urticaria : Eliciting factor: cold objects/air/ fluids/wind • Delayed pressure urticaria : Eliciting factor: vertical pressure (weals arising with a 3– 12 h latency) • Heat contact urticaria: Eliciting factor: localised heat • Solar urticaria : Eliciting factor: UV and/or visible light • Dermographic urticaria : Eliciting factor: mechanical shearing forces. Unknown cause, whealing usually develops within 5 -10 minutes of stroking the skin and persists for 15 -30 minutes.
• Aquagenic urticaria: Eliciting factor: water • Cholinergic urticaria: Elicitation by increase in body core temperature due to physical exercises, spicy food. (allergy to sweat or decrease sweat with increase ACH mast cell)Characterized by: small papules mainly on the trunk, with pricky sensation • Contact urticaria: Elicitation by contact with urticariogenic substance • Vibratory Urticaria
Causes of Chronic spontaneous urticaria • Idiopathic • Autoreactivity: autoimmune CU with anti-Ig. E and anti-Ig. E antibodies, associated with autoimmune disorders (thyroiditis), characterized by long duration and high disease activity. • Infection: bacterial (streptococci, helicobacter pylori), parasitic • Intolerance: (Pseudoallergic) non-allergic, dosedependent and delayed (4– 12 h) onset hypersensitivity to food pseudoallergens such as food colorants, preservatives, taste intensifiers. CU due to intolerance is diagnosed in patients who show decreased disease activity following a 3– 4 week diet low in pseudoallergens
Clinical Manifestations • A wheal consists of three typical features: • A central swelling of variable size, almost invariably surrounded by a reflex erythema; • Associated itching rubbing in character or sometimes burning sensations • A fleeting nature (EVANESCENT), with the skin returning to its normal appearance, usually within 1– 24 h. • Clinical variants: • Polycyclic (annular) with peripheral extension and central clearing • Vesiculobullous


Urticarial vasculitis • Urticarial vasculitis is characterized by pruritic, burning or painfully raised, superficial, erythematous or edematous, circumscribed wheals • The individual urticarial lesions last frequently more than 24 hours and leave a residual transient hyperpigmentation. • Associated features include fever, malaise, myalgia and specific organ involvement. • Skin biopsy revealed vasculitic changes.

Papular urticaria • Papular urticaria is atypical response to the bites of a number of arthropods, including biting flies, mosquitoes, mites, fleas. • The lesions are small urticated papules, often surrounded by a tiny vesicle, and are so itchy that their tops are rapidly excoriated. • They arise as a result of a hypersensitivity response to antigens in the arthropods.

Angioedema • Angioedema, is characterized by nonpitting, edematous swelling that involves subcutaneous tissues (e. g. , face (lips, periorbital), hands, genitals) • Symptoms of Laryngeal edema • Symptoms of GIT edema
Angioedema is characterized by: • Sudden, pronounced swelling of the lower dermis and subcutis; • ill defined • Pale rather than red • Sometimes pain rather than itching; • Frequent involvement of mucous membranes • Resolution that is slower than for wheals and can take up to 72 h.

Clinical types • Idiopathic angioedema • Drug induced: NSAIDs, ACE inhibitor-induced angioedema • Angioedema caused by C 1 inhibitor deficienc): LOW (C 4) • Hereditary angioedema • Acquired angioedema: decrease of C 1 -INH due to increase metabolism as in lyhmphoproliferative disorders, autoantibodies against C 1 -INH. • Allergic angioedema: often associated with acute or chronic urticaria. • Vibratory angioedema
Diagnosis • History • Physical examination • Differential blood count, ESR, CRP: to exclude major internal condition • Stool analysis for helicobacter and parasites • Antinuclear antibody, thyroid tests • Autologous serum skin test (ASST): (anti Ig. E antibodies) • Skin prick test (SPT): to measure the presence of Ig. E antibodies for the suspect food. • C 4 for angioedema without wheals • C 1 esterase inhibitor level and function
Differential Diagnosis • • • Atopic dermatitis Contact or allergic dermatitis Pityriasis rosea Drug eruption Erythema multiform
Treatment • General measures: • Patients should be advised to avoid factors that trigger relapses: eg, food, drugs. • Treatment with calamine lotion, 1% menthol in aqueous cream have been proved to suppress histamine induced itching.
• • Symptomatic treatment: Antihistamines: Second-generation H 1 -receptor antagonist: Cetirizine, 5 to 10 mg per day for several weeks, Fexofenadine, 180 mg per day or 60 mg twice daily Desloratadine , 5 mg per day Loratadine, 10 mg per day First-generation sedating H 1 -receptor antagonist: • Hydroxyzine, 10 to 50 mg at night • Diphenhydramine, 25 to 50 mg at night
• • • H 1 - plus H 2 -receptor antagonist: Doxepin, 10 to 50 mg at night Cyproheptadine, 4 mg, up to three times daily Cimetidine, titrated to 400 mg three times daily Immunosuppressive drugs: Patients with autoimmune urticaria. Cyclosporine is recommended only for patients with severe disease refractory to high doses of oral antihistamines.
• Oral corticosteroid: (Prednisone) as shortterm therapy (3 to 7 days) in acute, severe, generalized urticarial unresponsive to antihistamines. Not indicated in chronic urticaria. • Mast cell stabilizer: in some cases of cholinergic urticarial • Leukotriene modifier: Montelukast, 10 mg: Antileukotrienes may be taken in addition to an H 1 antihistamine for poorly controlled urticaria but there is little evidence that they are useful as monotherapy.
• Omalizumab binds to free Ig. E in the blood and interstitial space, forming biologically inactive Ig. E complexes that are unable to bind to receptor on the surface of mast cells and basophils.
Angioedema • Severe cases: Subcutaneous epinephrine (adrenaline) is the main treatment • Moderate cases: • Close monitoring is often necessary. • Diphenhydramine (50) mg intramuscular (IM)/intravenous (IV). • Hydrocortisone (200 mg) may reduce the possibility of relapse.
• For laryngeal swelling and airway obstruction, close monitoring of the airway is mandatory. Epinephrine (1: 1000) should be administrated subcutaneous or intramuscular. • Prevention of attacks : The administration of androgen derivatives (Danazol) or antifibrinolytics (Tranexamic acid) may be considered.
 Angioedema
Angioedema Angioedema classification
Angioedema classification Types of angioedema
Types of angioedema Angioedema
Angioedema Angioedema pictures
Angioedema pictures Angioedema anaphylaxis
Angioedema anaphylaxis Urticaria einkenni
Urticaria einkenni Omalizumab urticaria
Omalizumab urticaria Chronic inducible urticaria
Chronic inducible urticaria Chest thightness
Chest thightness Chronic inducible urticaria
Chronic inducible urticaria Prof. dr. marcus eckert
Prof. dr. marcus eckert Prof agamenon roberto
Prof agamenon roberto Prof david toback
Prof david toback What is this in english
What is this in english Dr suganda
Dr suganda Th
Th Domanda motivazionale tfa sostegno come rispondere
Domanda motivazionale tfa sostegno come rispondere Conclusion partielle texte argumentatif
Conclusion partielle texte argumentatif Jakim gatunkiem literackim są syzyfowe prace
Jakim gatunkiem literackim są syzyfowe prace Prof. grace schneider
Prof. grace schneider Edna st. vincent millay, ‘sonnet 29’
Edna st. vincent millay, ‘sonnet 29’ Akuisita
Akuisita Prof dr orhan canbolat
Prof dr orhan canbolat Obsatar sinaga
Obsatar sinaga Pem dereceleri
Pem dereceleri Professor mark ferguson
Professor mark ferguson Bellioni otorino
Bellioni otorino Prof ramli musa
Prof ramli musa Prof aris sudiyanto
Prof aris sudiyanto Prof agamenon roberto
Prof agamenon roberto Prof dr bilgin arda
Prof dr bilgin arda Epinoryum
Epinoryum