Upper Respiratory Tract Infections Saudi Diploma in Family
- Slides: 42
Upper Respiratory Tract Infections Saudi Diploma in Family Medicine Center of Post Graduate Studies in Family Medicine Dr. Zekeriya Aktürk zekeriya. akturk@gmail. com www. aile. net 1 / 42 Utilized work: Dr. Aynur Engin, Cumhuriyet University, Sivas, Turkey and Dr. Ela Eker, Trakya University, Edirne, Turkey
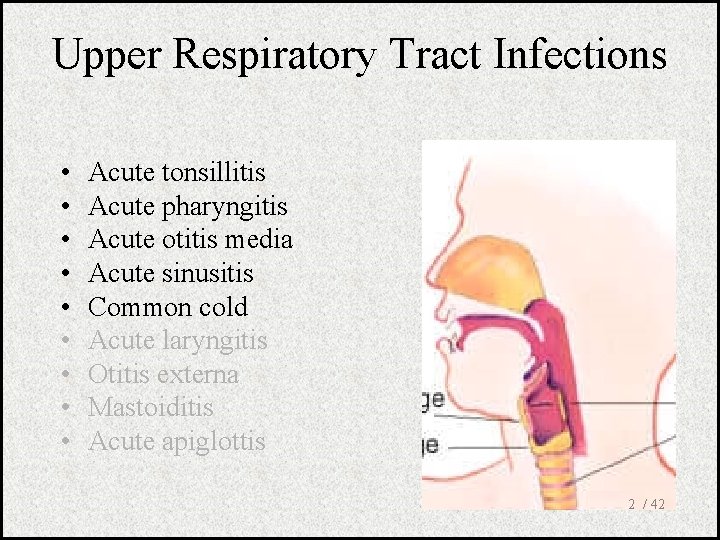
Upper Respiratory Tract Infections • • • Acute tonsillitis Acute pharyngitis Acute otitis media Acute sinusitis Common cold Acute laryngitis Otitis externa Mastoiditis Acute apiglottis 2 / 42
Objectives • At the end of this session, the participants should be able to; – List upper respiratory tract infections – Make differential diagnosis between URTI – Define criteria for antibiotic use – Apply and interpret the Mc. Isaac scoring 3 / 42
Tonsilitis-pharyngitis • Bacteria – S. pyogenes – C. diphteriae – N. gonorrhoeae • Viruses – Epstein-Barr virus – Adenovirus – Influenza A, B – Coxsackie A – Parainfluenzae 4 / 42
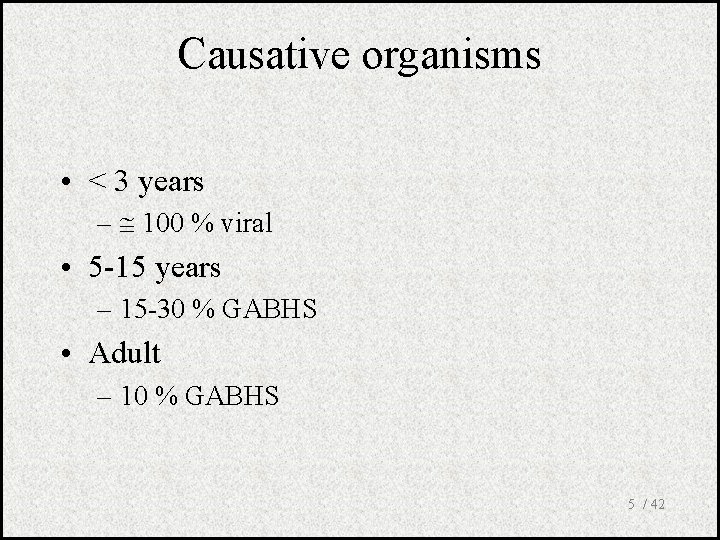
Causative organisms • < 3 years – 100 % viral • 5 -15 years – 15 -30 % GABHS • Adult – 10 % GABHS 5 / 42
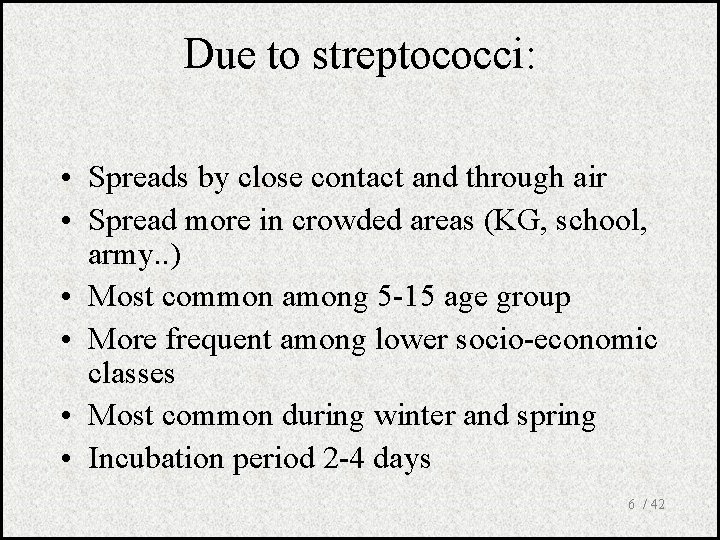
Due to streptococci: • Spreads by close contact and through air • Spread more in crowded areas (KG, school, army. . ) • Most common among 5 -15 age group • More frequent among lower socio-economic classes • Most common during winter and spring • Incubation period 2 -4 days 6 / 42
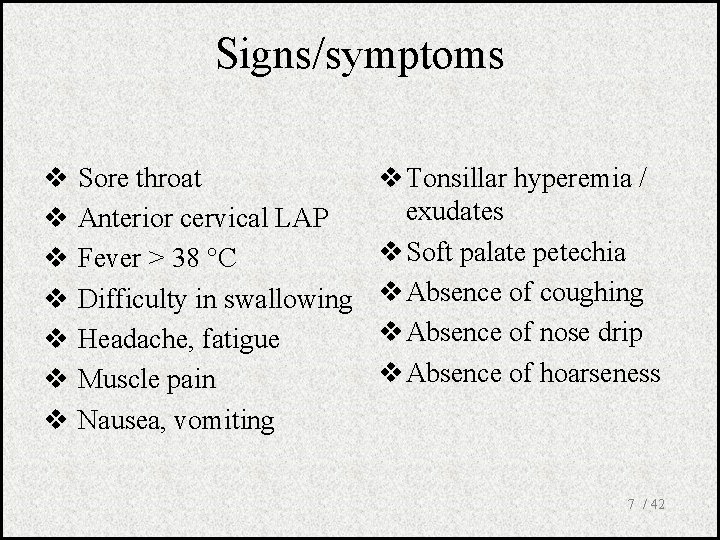
Signs/symptoms v v v v Sore throat Anterior cervical LAP Fever > 38 C Difficulty in swallowing Headache, fatigue Muscle pain Nausea, vomiting v Tonsillar hyperemia / exudates v Soft palate petechia v Absence of coughing v Absence of nose drip v Absence of hoarseness 7 / 42
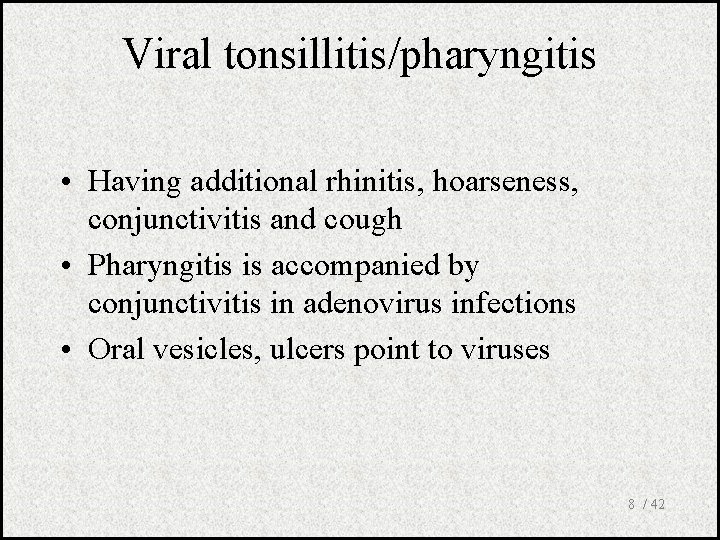
Viral tonsillitis/pharyngitis • Having additional rhinitis, hoarseness, conjunctivitis and cough • Pharyngitis is accompanied by conjunctivitis in adenovirus infections • Oral vesicles, ulcers point to viruses 8 / 42
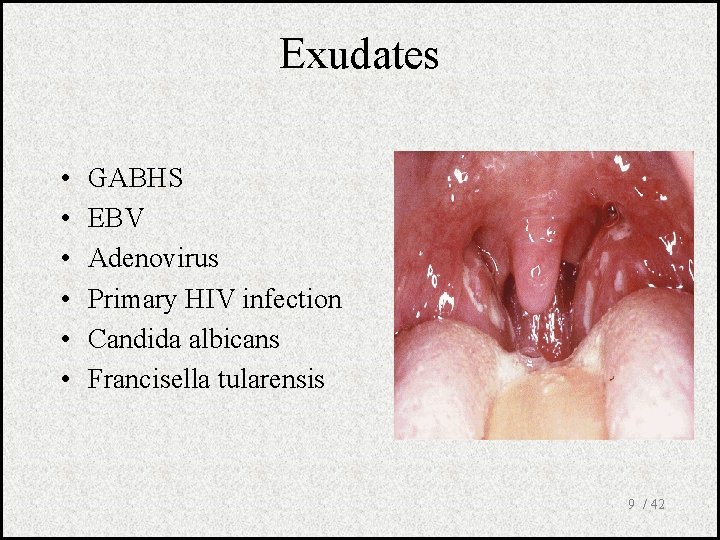
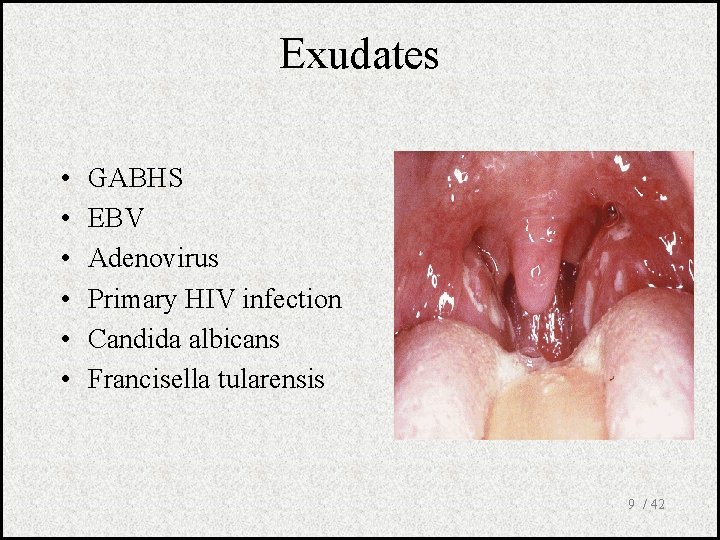
Exudates • • • GABHS EBV Adenovirus Primary HIV infection Candida albicans Francisella tularensis 9 / 42
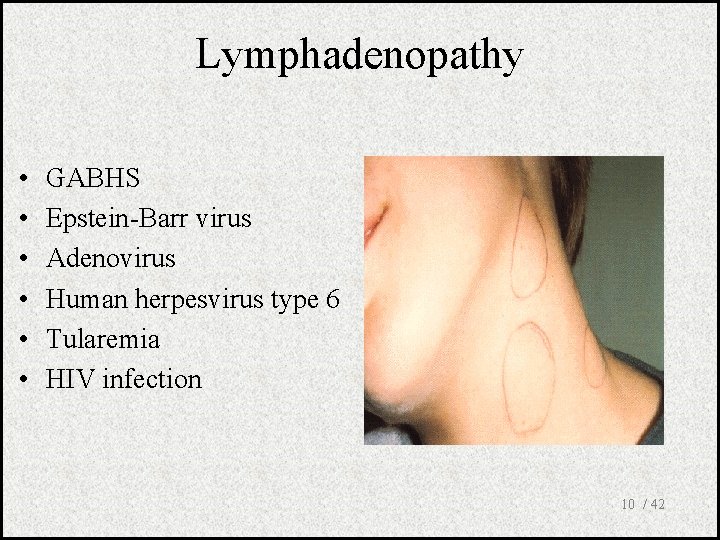
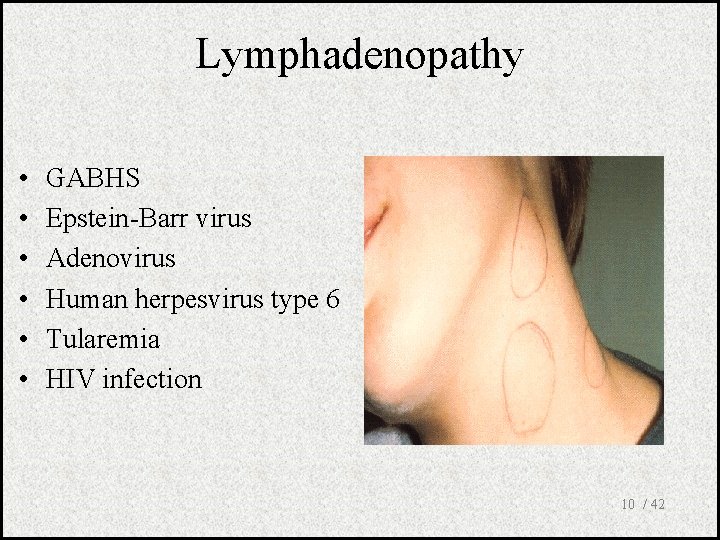
Lymphadenopathy • • • GABHS Epstein-Barr virus Adenovirus Human herpesvirus type 6 Tularemia HIV infection 10 / 42
Laboratory • Throat swab – Gold standard • Rapid antigen test – If negative need swab • ASO – May remain + for 1 year • WBC count • Peripheral smear 11 / 42
Throat Culture • Pathogens looked for – Group A beta hemolytic streptococci – C. diphteriae (rare) – N. gonorrhoeae (rare) • If GABHS do we need antibiogram? – Is there resistence to penicilline? 12 / 42
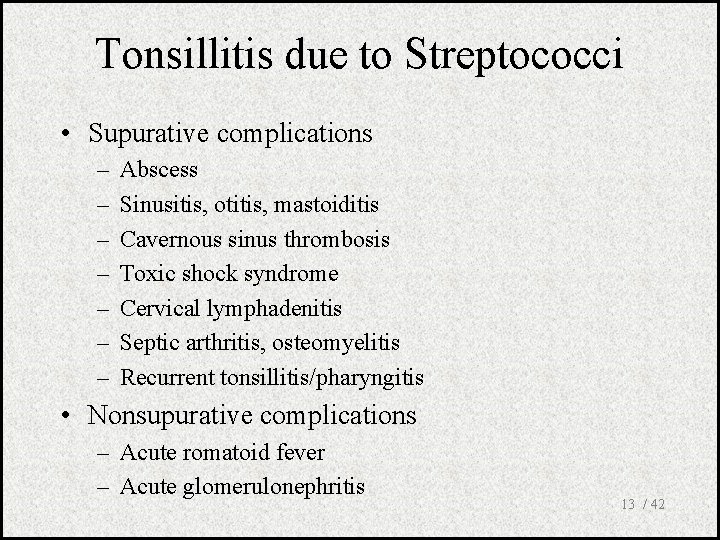
Tonsillitis due to Streptococci • Supurative complications – – – – Abscess Sinusitis, otitis, mastoiditis Cavernous sinus thrombosis Toxic shock syndrome Cervical lymphadenitis Septic arthritis, osteomyelitis Recurrent tonsillitis/pharyngitis • Nonsupurative complications – Acute romatoid fever – Acute glomerulonephritis 13 / 42
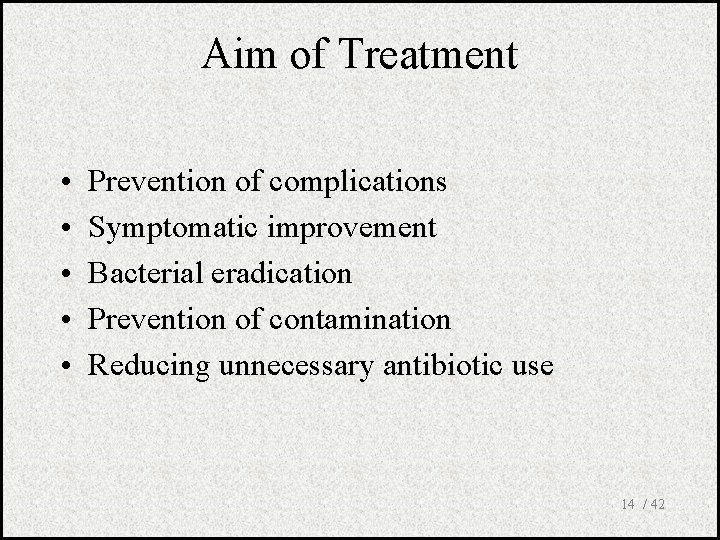
Aim of Treatment • • • Prevention of complications Symptomatic improvement Bacterial eradication Prevention of contamination Reducing unnecessary antibiotic use 14 / 42
Treatment • Many different antibiotics can eradicate GABHS from pharynx • Starting treatment within 9 days is enough to prevent ARF 15 / 42
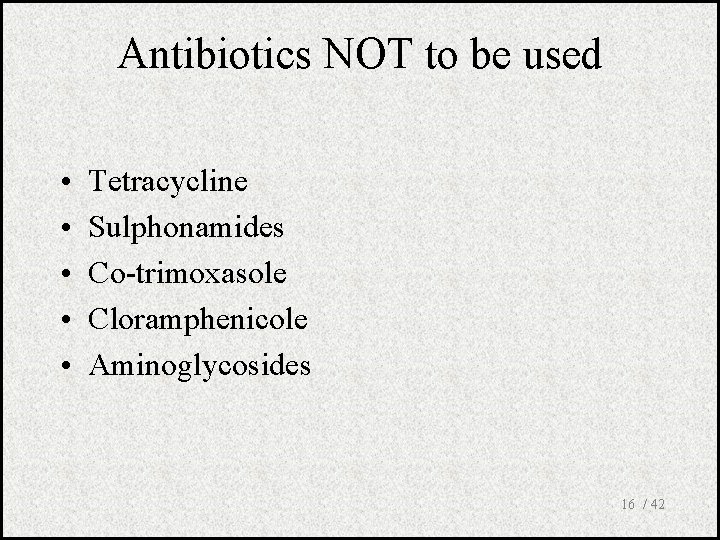
Antibiotics NOT to be used • • • Tetracycline Sulphonamides Co-trimoxasole Cloramphenicole Aminoglycosides 16 / 42
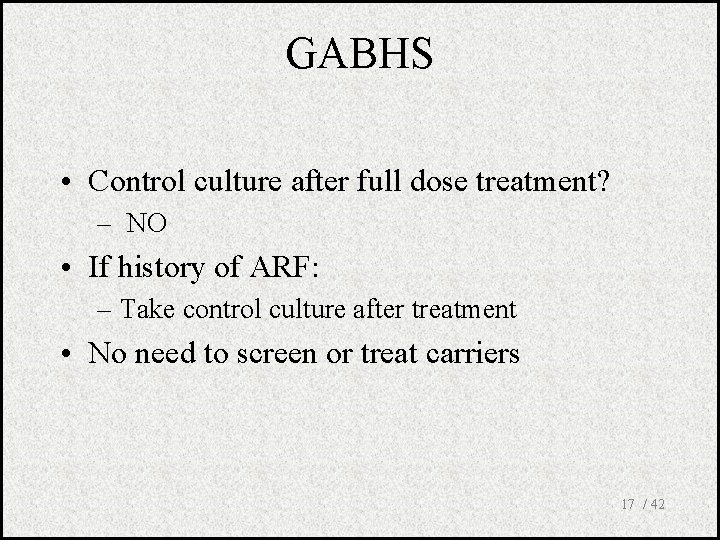
GABHS • Control culture after full dose treatment? – NO • If history of ARF: – Take control culture after treatment • No need to screen or treat carriers 17 / 42
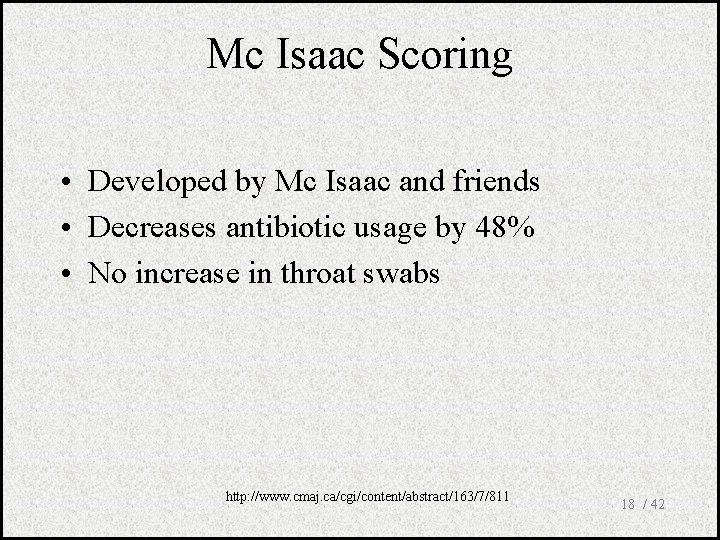
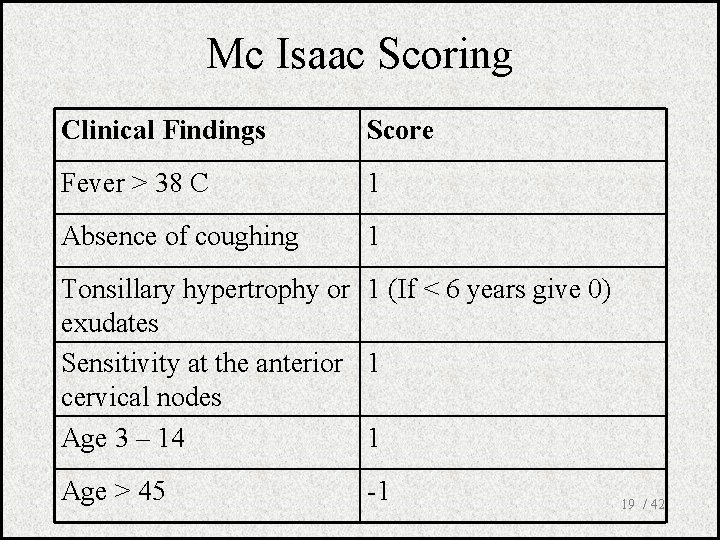
Mc Isaac Scoring • Developed by Mc Isaac and friends • Decreases antibiotic usage by 48% • No increase in throat swabs http: //www. cmaj. ca/cgi/content/abstract/163/7/811 18 / 42
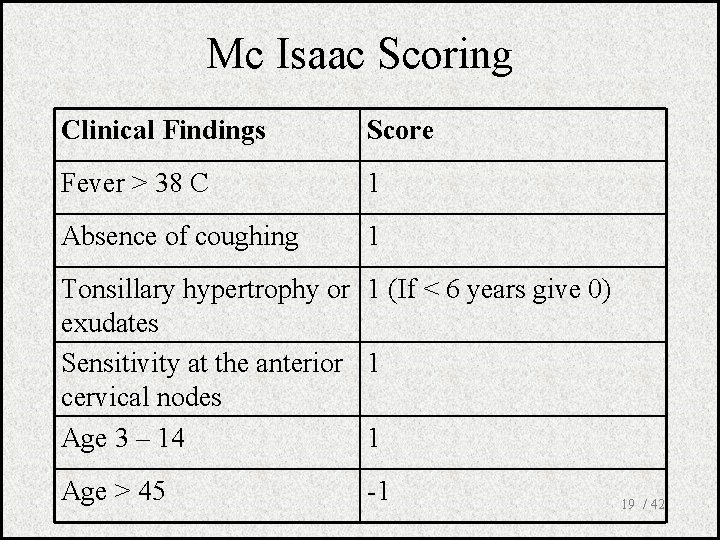
Mc Isaac Scoring Clinical Findings Score Fever > 38 C 1 Absence of coughing 1 Tonsillary hypertrophy or 1 (If < 6 years give 0) exudates Sensitivity at the anterior 1 cervical nodes Age 3 – 14 1 Age > 45 -1 19 / 42
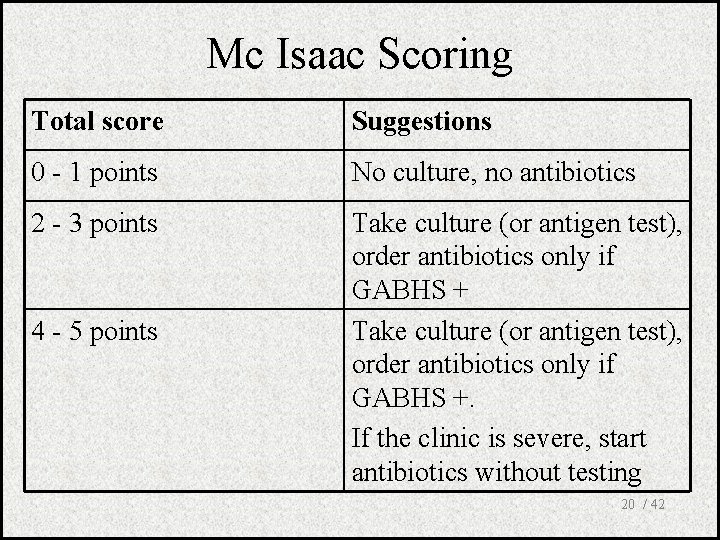
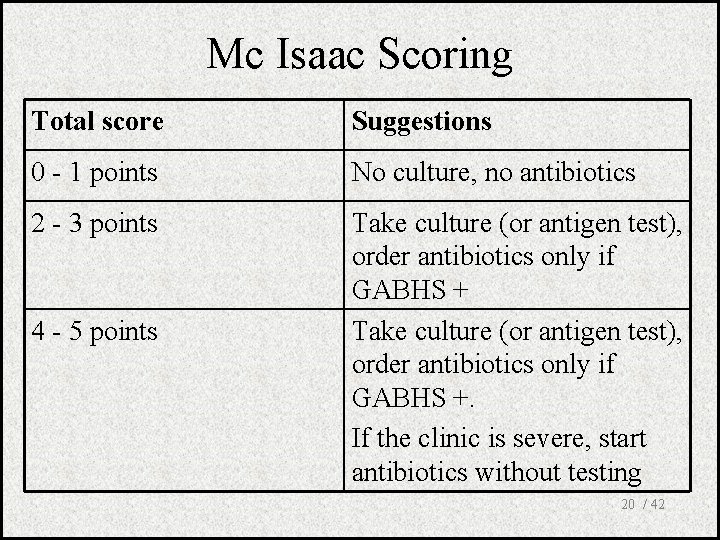
Mc Isaac Scoring Total score Suggestions 0 - 1 points No culture, no antibiotics 2 - 3 points Take culture (or antigen test), order antibiotics only if GABHS +. If the clinic is severe, start antibiotics without testing 4 - 5 points 20 / 42
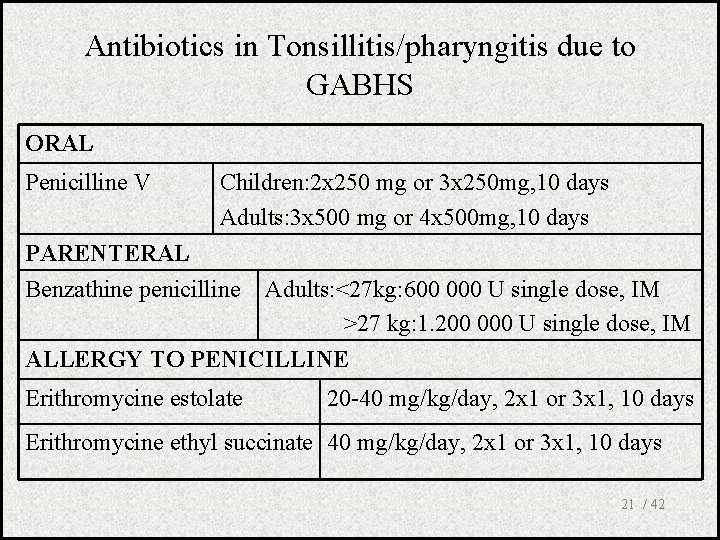
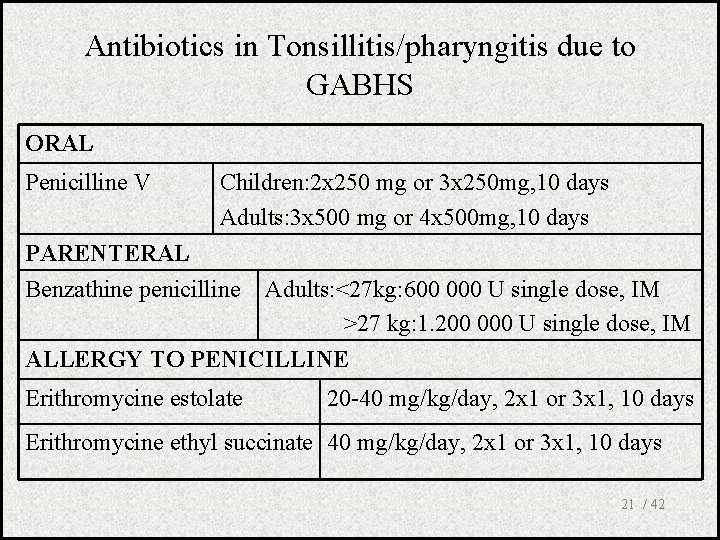
Antibiotics in Tonsillitis/pharyngitis due to GABHS ORAL Penicilline V Children: 2 x 250 mg or 3 x 250 mg, 10 days Adults: 3 x 500 mg or 4 x 500 mg, 10 days PARENTERAL Benzathine penicilline Adults: <27 kg: 600 000 U single dose, IM >27 kg: 1. 200 000 U single dose, IM ALLERGY TO PENICILLINE Erithromycine estolate 20 -40 mg/kg/day, 2 x 1 or 3 x 1, 10 days Erithromycine ethyl succinate 40 mg/kg/day, 2 x 1 or 3 x 1, 10 days 21 / 42
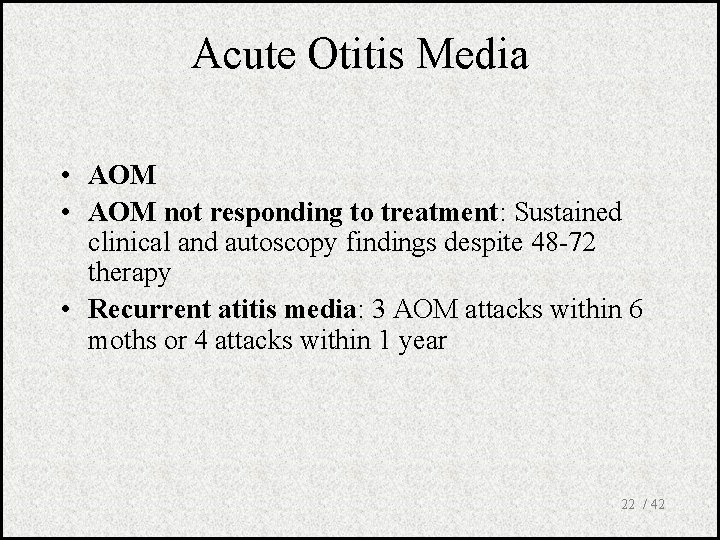
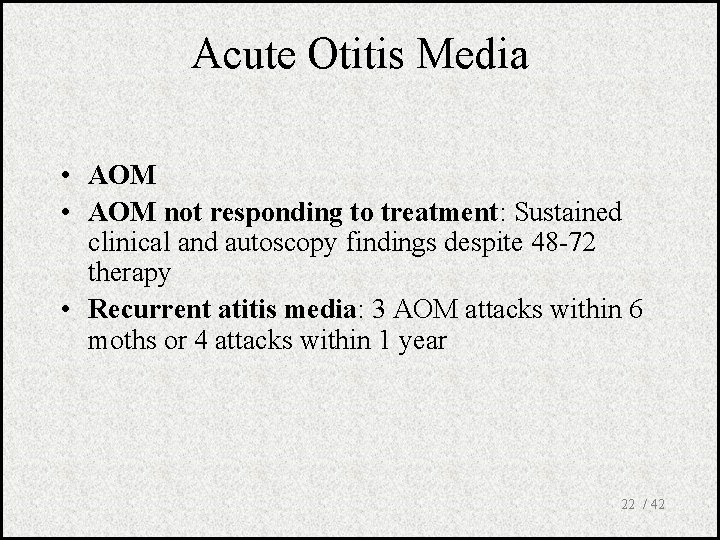
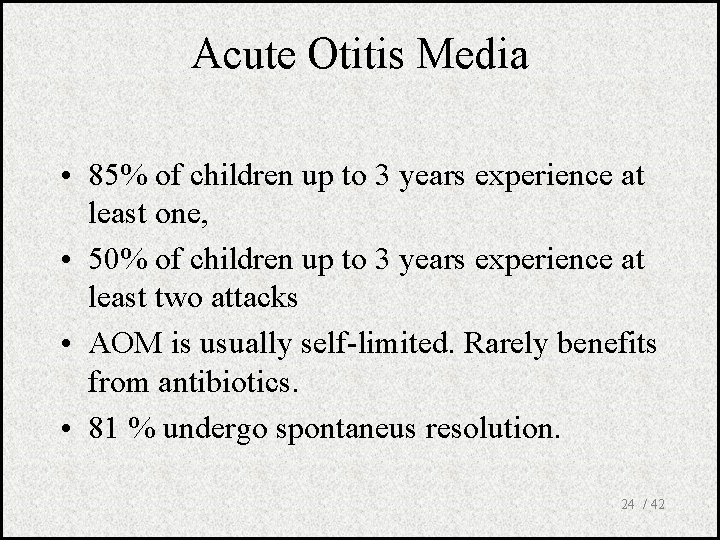
Acute Otitis Media • AOM not responding to treatment: Sustained clinical and autoscopy findings despite 48 -72 therapy • Recurrent atitis media: 3 AOM attacks within 6 moths or 4 attacks within 1 year 22 / 42
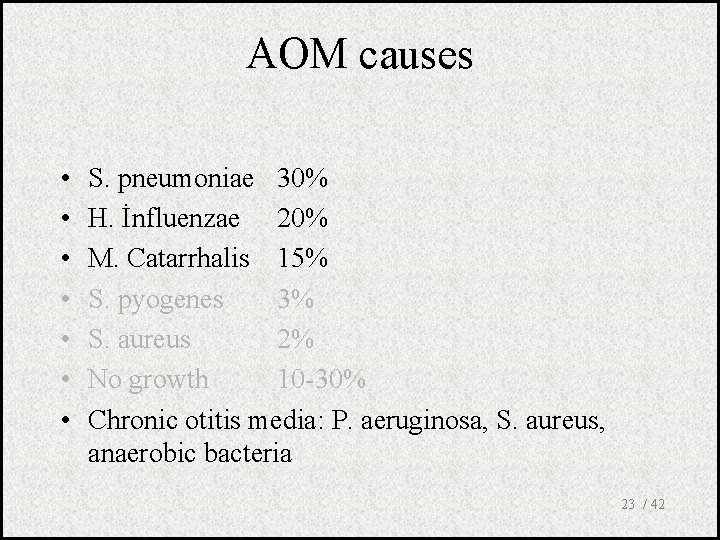
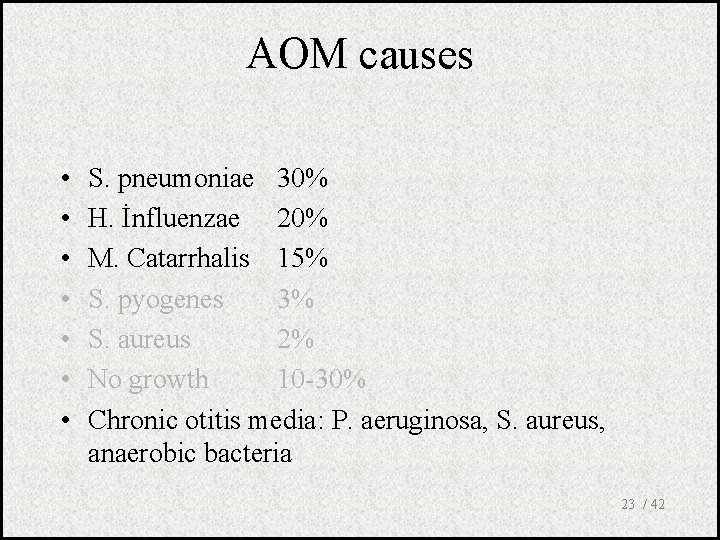
AOM causes • • S. pneumoniae 30% H. İnfluenzae 20% M. Catarrhalis 15% S. pyogenes 3% S. aureus 2% No growth 10 -30% Chronic otitis media: P. aeruginosa, S. aureus, anaerobic bacteria 23 / 42
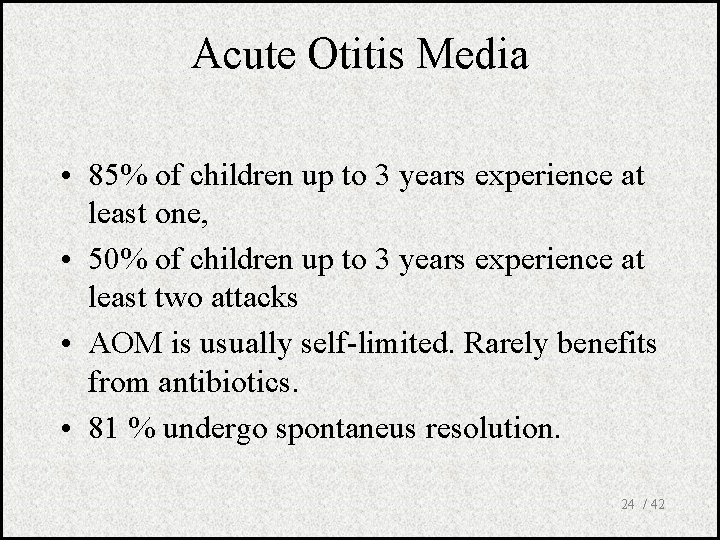
Acute Otitis Media • 85% of children up to 3 years experience at least one, • 50% of children up to 3 years experience at least two attacks • AOM is usually self-limited. Rarely benefits from antibiotics. • 81 % undergo spontaneus resolution. 24 / 42
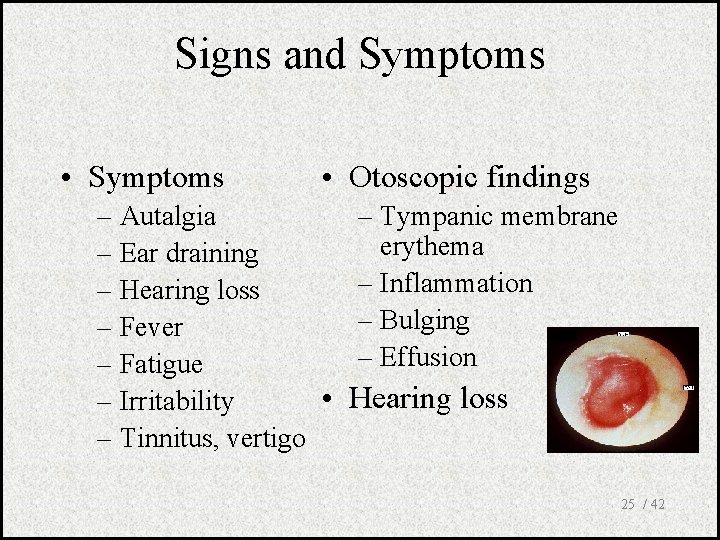
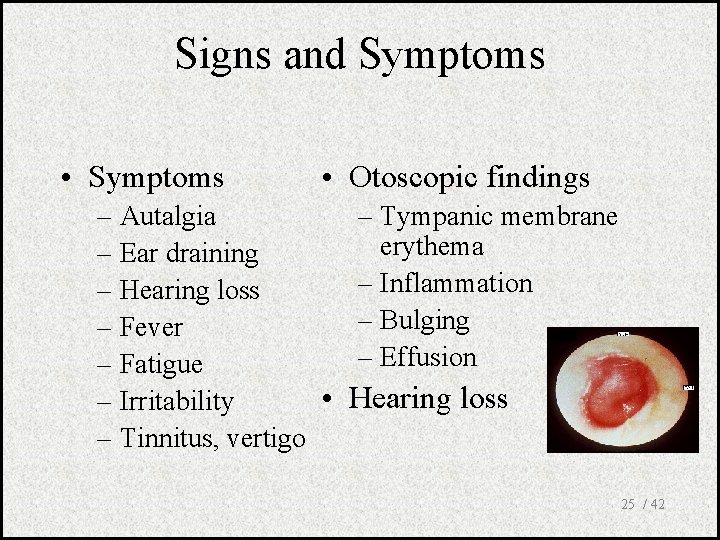
Signs and Symptoms • Symptoms • Otoscopic findings – Autalgia – Ear draining – Hearing loss – Fever – Fatigue • – Irritability – Tinnitus, vertigo – Tympanic membrane erythema – Inflammation – Bulging – Effusion Hearing loss 25 / 42
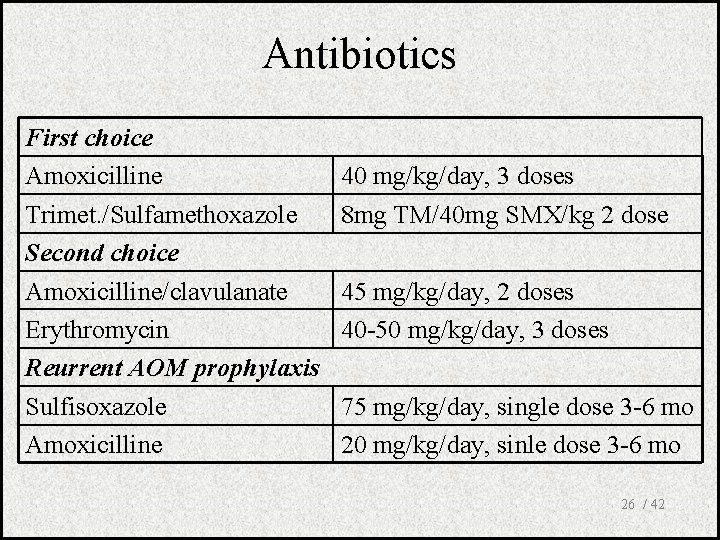
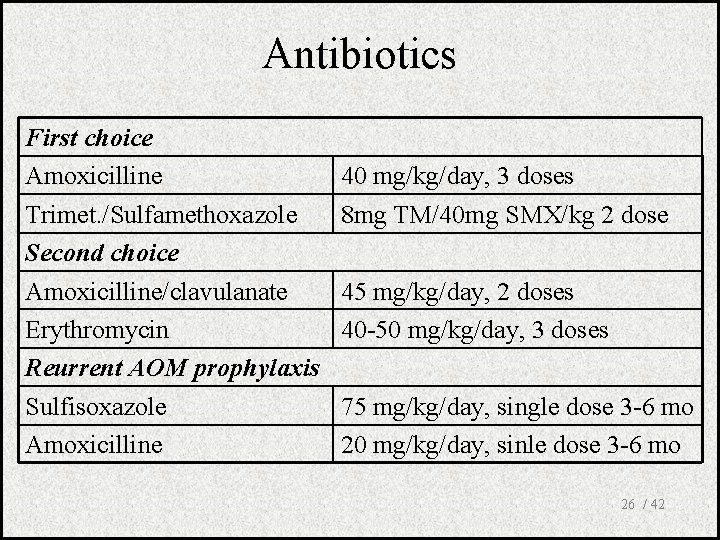
Antibiotics First choice Amoxicilline Trimet. /Sulfamethoxazole Second choice Amoxicilline/clavulanate Erythromycin Reurrent AOM prophylaxis Sulfisoxazole Amoxicilline 40 mg/kg/day, 3 doses 8 mg TM/40 mg SMX/kg 2 dose 45 mg/kg/day, 2 doses 40 -50 mg/kg/day, 3 doses 75 mg/kg/day, single dose 3 -6 mo 20 mg/kg/day, sinle dose 3 -6 mo 26 / 42
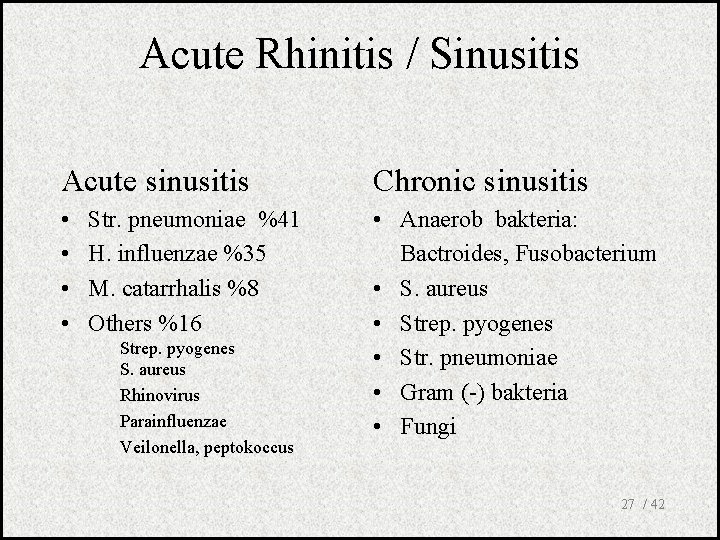
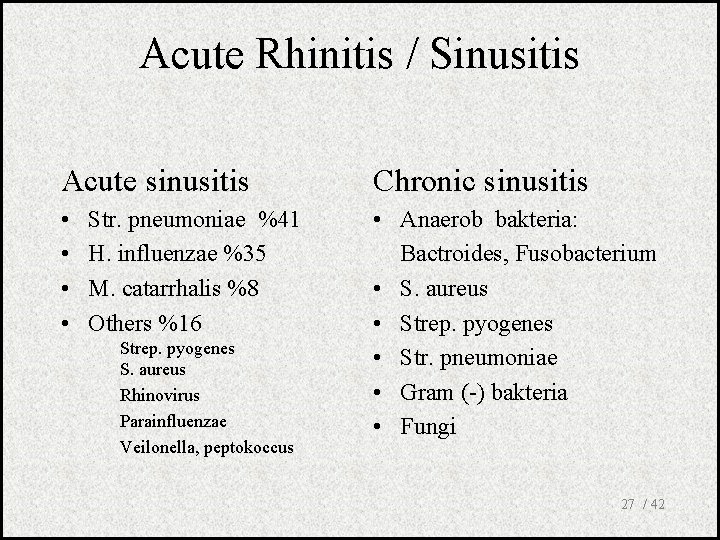
Acute Rhinitis / Sinusitis Acute sinusitis Chronic sinusitis • • • Anaerob bakteria: Bactroides, Fusobacterium • S. aureus • Strep. pyogenes • Str. pneumoniae • Gram (-) bakteria • Fungi Str. pneumoniae %41 H. influenzae %35 M. catarrhalis %8 Others %16 Strep. pyogenes S. aureus Rhinovirus Parainfluenzae Veilonella, peptokoccus 27 / 42
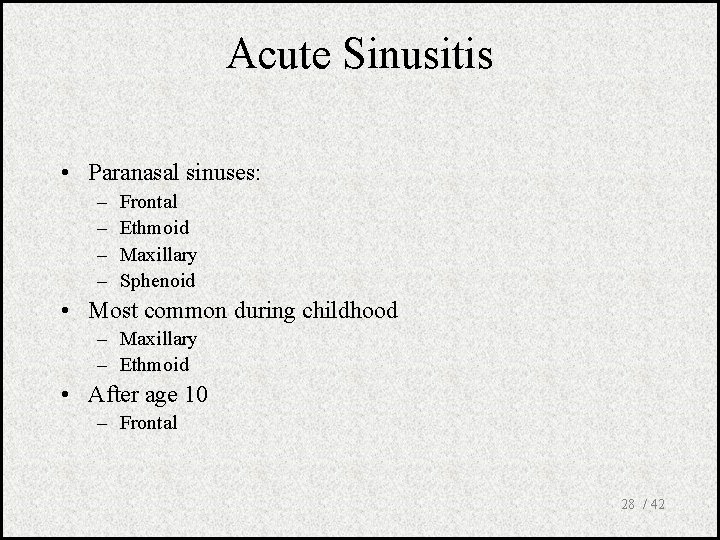
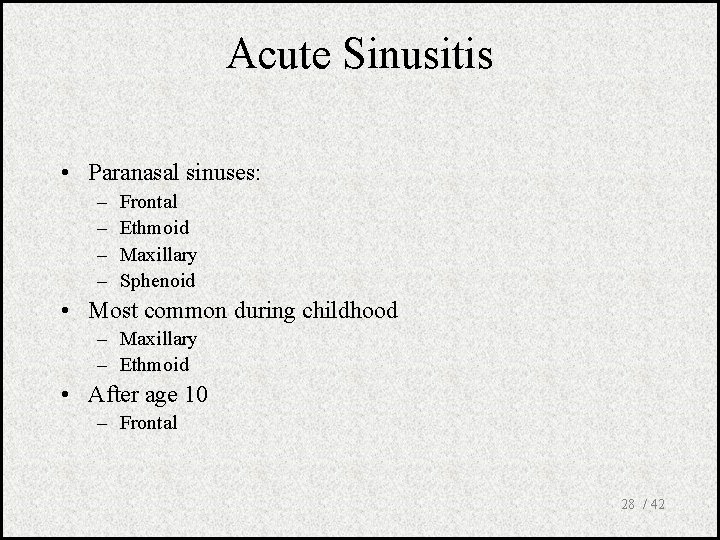
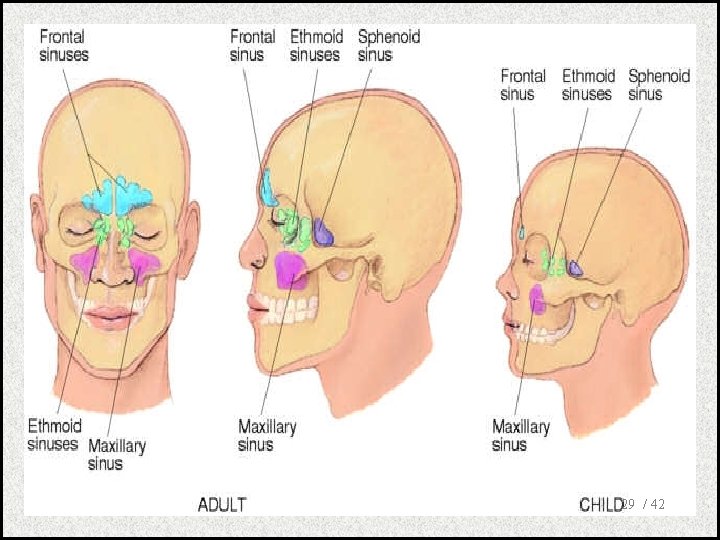
Acute Sinusitis • Paranasal sinuses: – – Frontal Ethmoid Maxillary Sphenoid • Most common during childhood – Maxillary – Ethmoid • After age 10 – Frontal 28 / 42
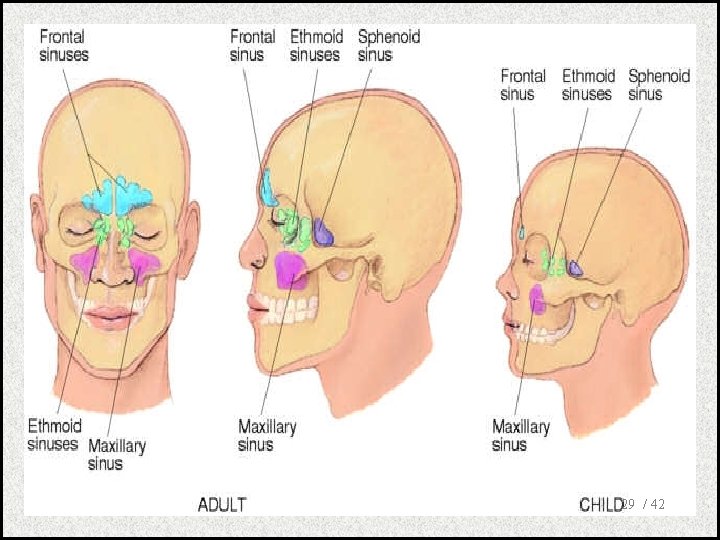
29 / 42
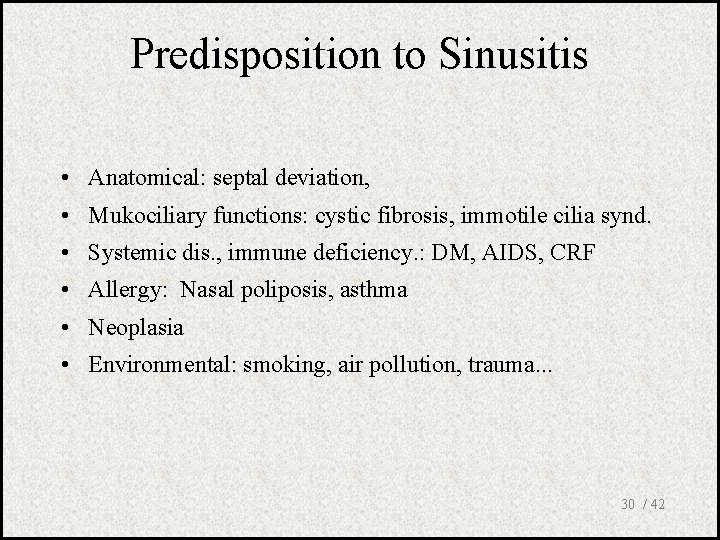
Predisposition to Sinusitis • Anatomical: septal deviation, • Mukociliary functions: cystic fibrosis, immotile cilia synd. • Systemic dis. , immune deficiency. : DM, AIDS, CRF • Allergy: Nasal poliposis, asthma • Neoplasia • Environmental: smoking, air pollution, trauma. . . 30 / 42
Acute Rhinosinusitis • Most important: Headache and postnasal dripping • Face congestion • Fever, fatigue, headache increased by leaning forward • Nose obstruction • Nose dripping • Purulent secretions (rhinoscopy) • Sensitivity over the sinuses • Halitosis 31 / 42
Acute rhinosinusitis Rhinitis • Increased symptoms after 5 days • Symptoms lasting > 10 days • Decreasing viral symptoms, nasal secretion becoming more purulent are indicative for acute rhinosinusitis 32 / 42
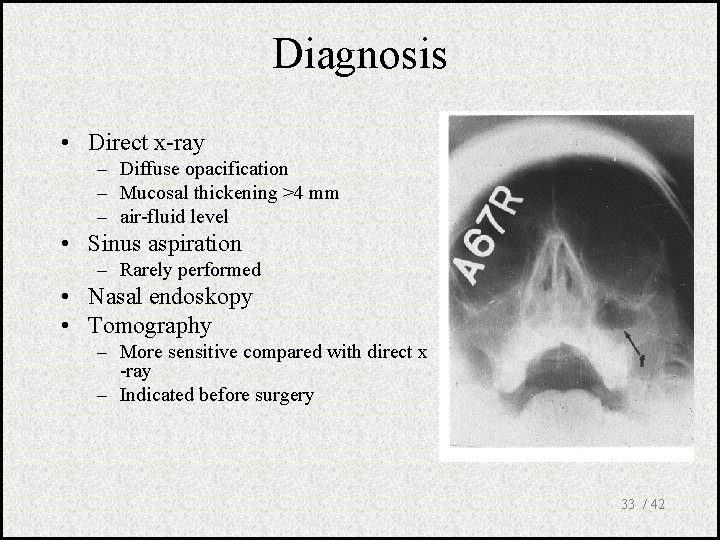
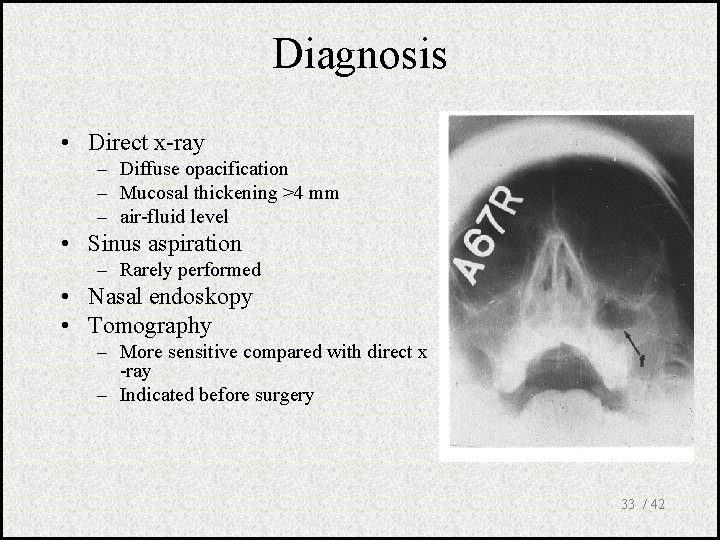
Diagnosis • Direct x-ray – Diffuse opacification – Mucosal thickening >4 mm – air-fluid level • Sinus aspiration – Rarely performed • Nasal endoskopy • Tomography – More sensitive compared with direct x -ray – Indicated before surgery 33 / 42
Treatment • Ampirical – Specific microbiologic diagnosis difficult • Primary pathogens – S. pneumoniae – H. influenzae 34 / 42
Treatment • Antibiotics questionable • Stalman: 192 patients. No difference between placebo and doxycycline. • Van Buchem: 214 patients. No difference between amoxycilline and placebo. • Lindbaek: 130 patients. compared Pen V, Amoxycilline and placebo. 86 % of patients receiving antibiotics and 57% of patients receiving placebo improved. 35 / 42
Antibiotics for Sinusitis • Amoxycilline (Alfoxil) 3 x 500 mg/d PO 10 d • Amoxycilline/clavulonate (Augmentin) 3 x 625 mg/d PO 10 d • Sefprosil(Serozil) 2 x 1000 mg/d PO 10 d • Sefuroxim (Zinnat) 2 x 250 mg/d PO 10 d • Azithromycine (Zitromax) First day 1 x 500 mg, then 1 x 250 mg/d PO 5 d 36 / 42
Support Therapy • Decongestants – Short duration 3 -5 days • Antihistamines – If allergy • Normal saline • Local steroids 37 / 42
Common Cold • Adults Rhinovirus • Children Parainfluenzae and RSV 38 / 42
Common Cold • • • Fatigue Feeling cold, shuddering Nose burning, obstruction, running Sneezing Fever 39 / 42
Influenza (flu) • Causes epidemics and pandemics • Highly contagious • Viral infection. 40 / 42
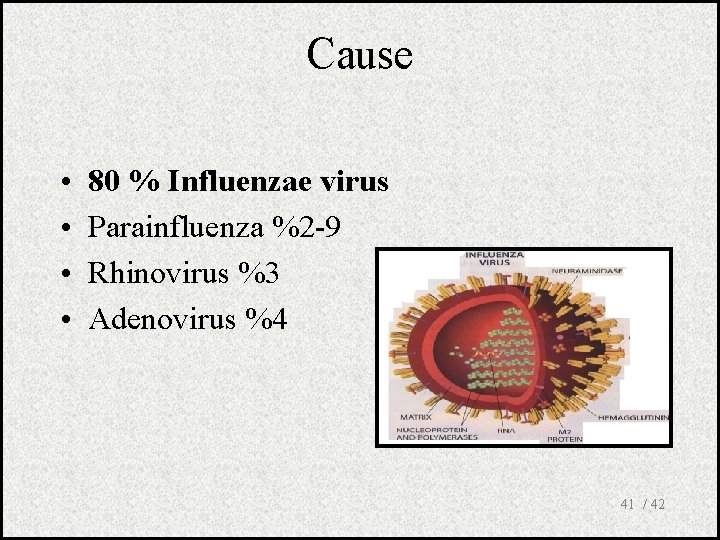
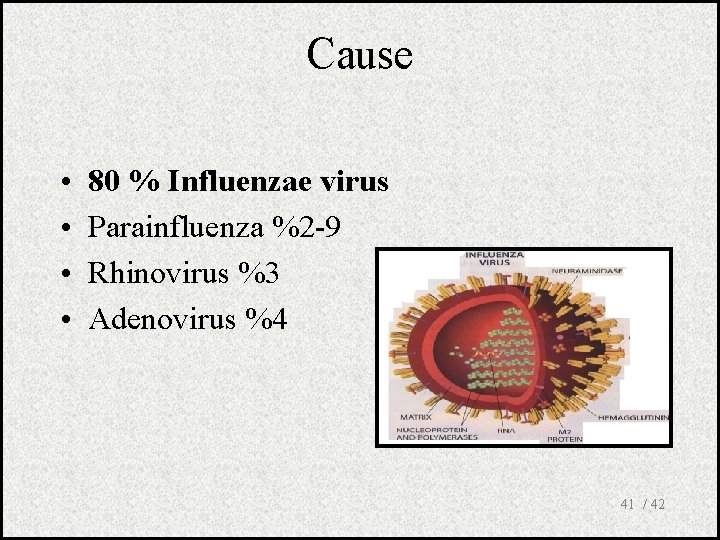
Cause • • 80 % Influenzae virus Parainfluenza %2 -9 Rhinovirus %3 Adenovirus %4 41 / 42
Influenza • Sudden onset after 12 -24 hours incubation • General weakness and fatigue • Feeling cold, shivering, temp. Up to 39 -40 C • No sore throat or running nose • Severe back, muscle and joint pain 42 / 42
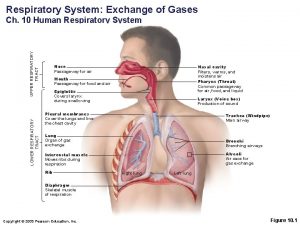
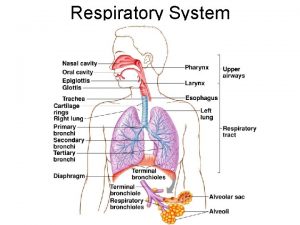
 What is the major function of the respiratory system
What is the major function of the respiratory system Anatomy of the upper respiratory tract
Anatomy of the upper respiratory tract Carina nasal
Carina nasal Physiology of lungs
Physiology of lungs Upper respiratory tract definition
Upper respiratory tract definition Classification of upper respiratory tract infection
Classification of upper respiratory tract infection Upper rti
Upper rti Upper and lower respiratory tract
Upper and lower respiratory tract Extrapyramidal tract function
Extrapyramidal tract function Dorsal reticulospinal tract
Dorsal reticulospinal tract The air passageway
The air passageway Pneumonia classification
Pneumonia classification Conclusion of respiratory tract infection
Conclusion of respiratory tract infection Normal flora of respiratory tract
Normal flora of respiratory tract Chassard lapine
Chassard lapine Respiratory zone
Respiratory zone Acute upper respiratory infection unspecified คือ
Acute upper respiratory infection unspecified คือ Neurosiphyllis
Neurosiphyllis Methotrexate yeast infection
Methotrexate yeast infection Genital infections
Genital infections Classification of acute gingival infections
Classification of acute gingival infections Storch infections
Storch infections Eye infections
Eye infections Opportunistic infections
Opportunistic infections Storch infections
Storch infections Amber blumling
Amber blumling Postpartum infections
Postpartum infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Bone and joint infections
Bone and joint infections Opportunistic infections
Opportunistic infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections Phagocytr
Phagocytr Understanding the mirai botnet
Understanding the mirai botnet Saudi arabia oligarchy
Saudi arabia oligarchy Mobile number portability saudi arabia
Mobile number portability saudi arabia Peta arab saudi dan palestina
Peta arab saudi dan palestina Ang mga likas na yaman sa hilagang asya
Ang mga likas na yaman sa hilagang asya Saudi energy efficiency program
Saudi energy efficiency program Agency in law definition
Agency in law definition Saudi standards, metrology and quality organization
Saudi standards, metrology and quality organization Saudi arabia
Saudi arabia Gbs saudi arabia
Gbs saudi arabia Engineering corner for inspection
Engineering corner for inspection