Update on Diagnosis and Treatment of Osteoporosis Sophia









- Slides: 26
Update on Diagnosis and Treatment of Osteoporosis Sophia Ish-Shalom Rambam Medical Center Technion Faculty of Medicine
Diagnosis of Osteoporosis What do we want to know about risk? How likely is that this individual with osteoporosis will sustain a fracture over a finite period of time?

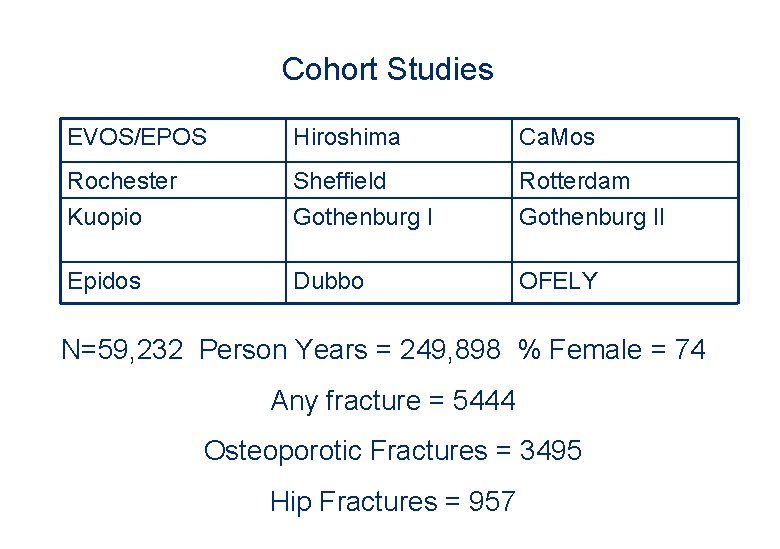
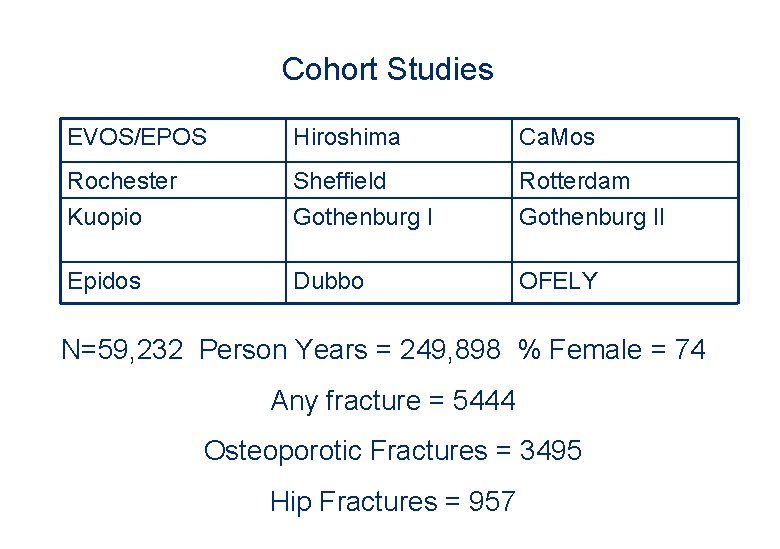
Cohort Studies EVOS/EPOS Hiroshima Ca. Mos Rochester Kuopio Sheffield Gothenburg I Rotterdam Gothenburg II Epidos Dubbo OFELY N=59, 232 Person Years = 249, 898 % Female = 74 Any fracture = 5444 Osteoporotic Fractures = 3495 Hip Fractures = 957
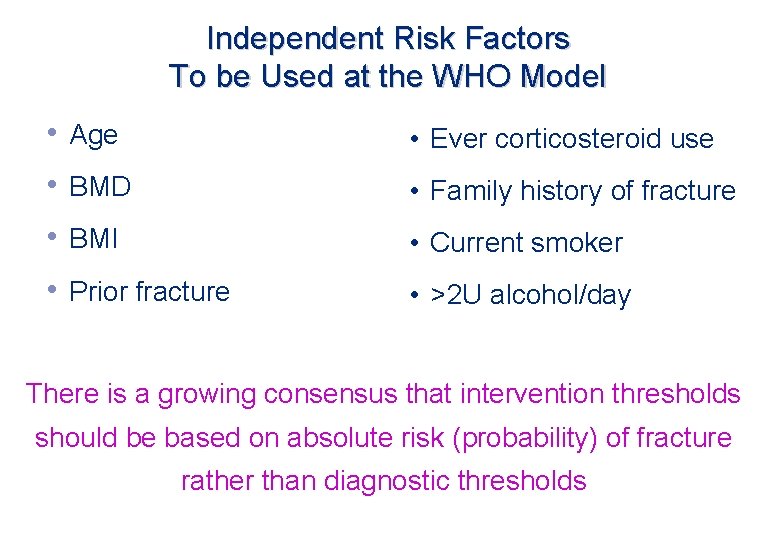
Independent Risk Factors To be Used at the WHO Model • Age • Ever corticosteroid use • BMD • Family history of fracture • BMI • Current smoker • Prior fracture • >2 U alcohol/day There is a growing consensus that intervention thresholds should be based on absolute risk (probability) of fracture rather than diagnostic thresholds
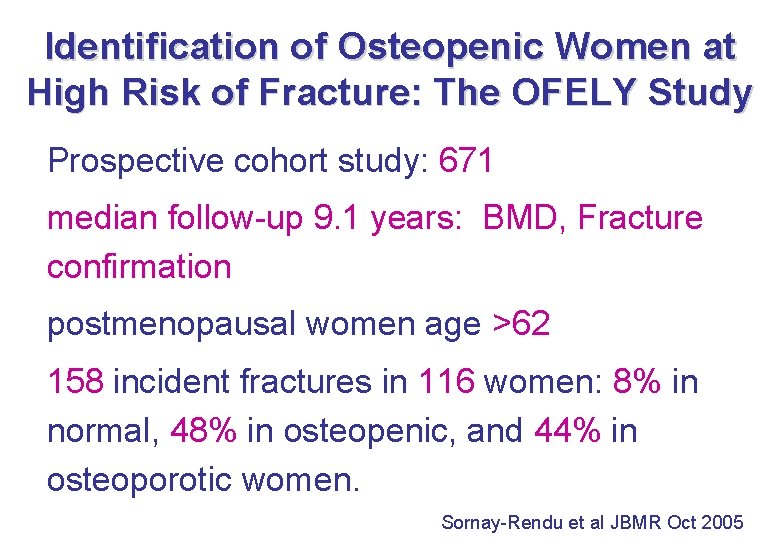
Identification of Osteopenic Women at High Risk of Fracture: The OFELY Study Prospective cohort study: 671 median follow-up 9. 1 years: BMD, Fracture confirmation postmenopausal women age >62 158 incident fractures in 116 women: 8% in normal, 48% in osteopenic, and 44% in osteoporotic women. Sornay-Rendu et al JBMR Oct 2005
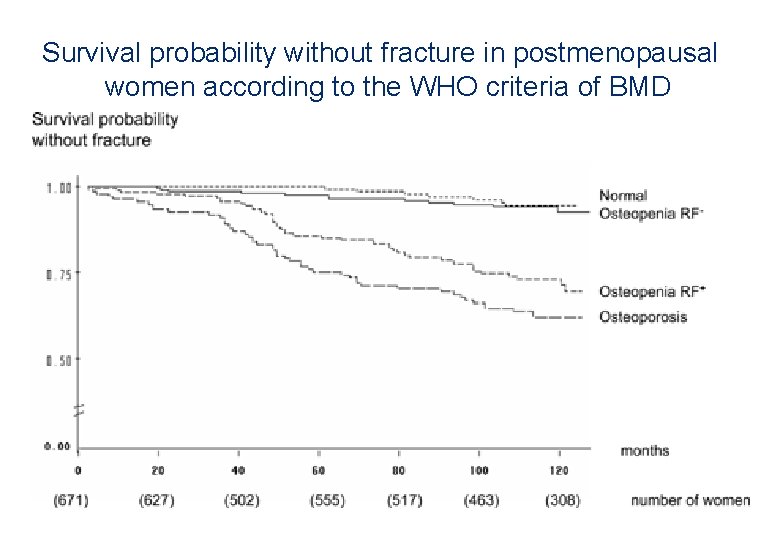
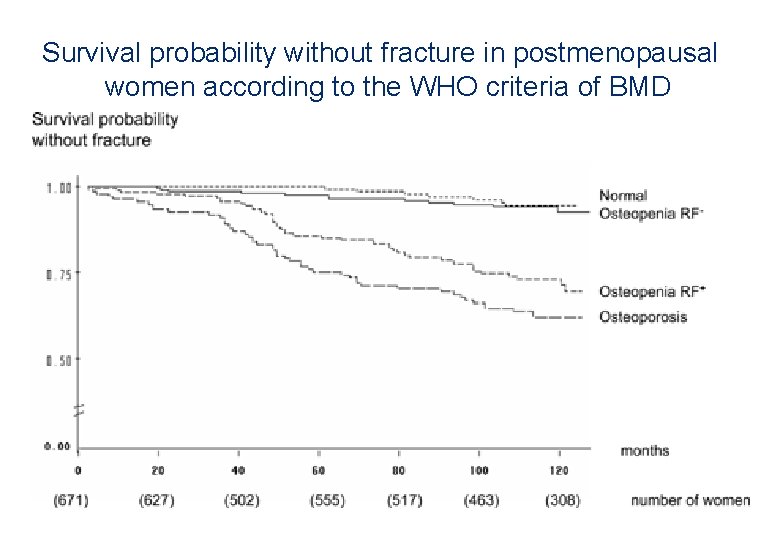
Survival probability without fracture in postmenopausal women according to the WHO criteria of BMD

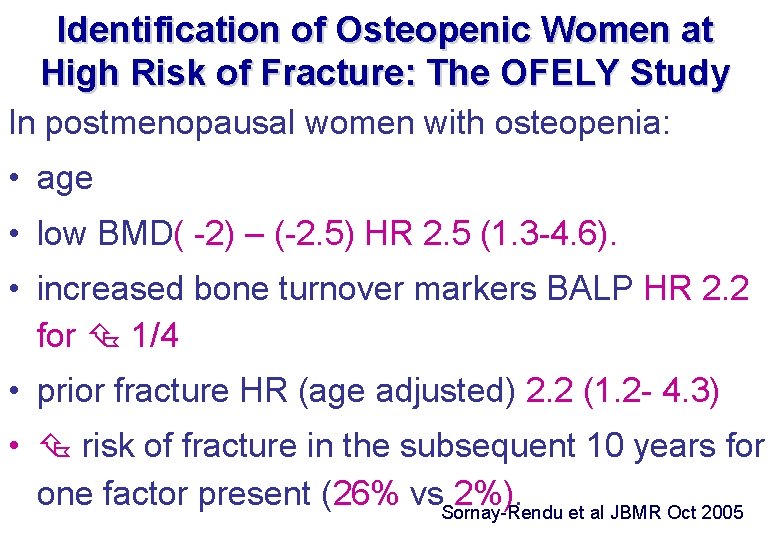
Identification of Osteopenic Women at High Risk of Fracture: The OFELY Study In postmenopausal women with osteopenia: • age • low BMD( -2) – (-2. 5) HR 2. 5 (1. 3 -4. 6). • increased bone turnover markers BALP HR 2. 2 for 1/4 • prior fracture HR (age adjusted) 2. 2 (1. 2 - 4. 3) • risk of fracture in the subsequent 10 years for one factor present (26% vs. Sornay-Rendu 2%). et al JBMR Oct 2005
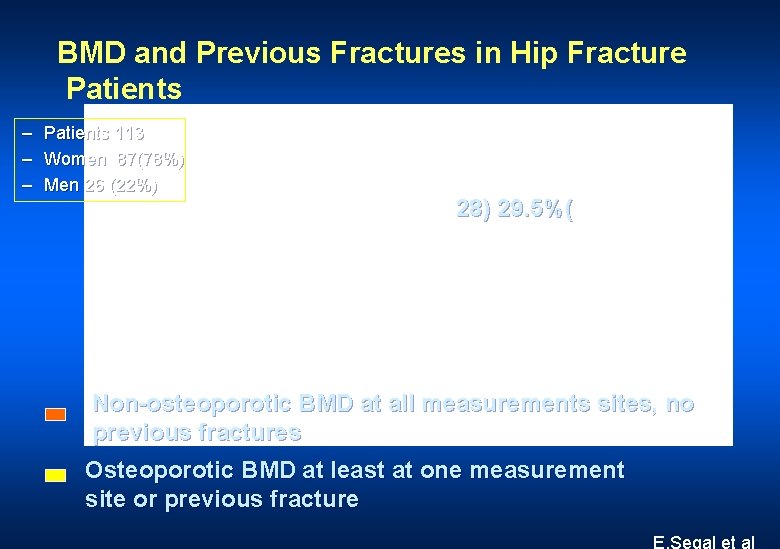
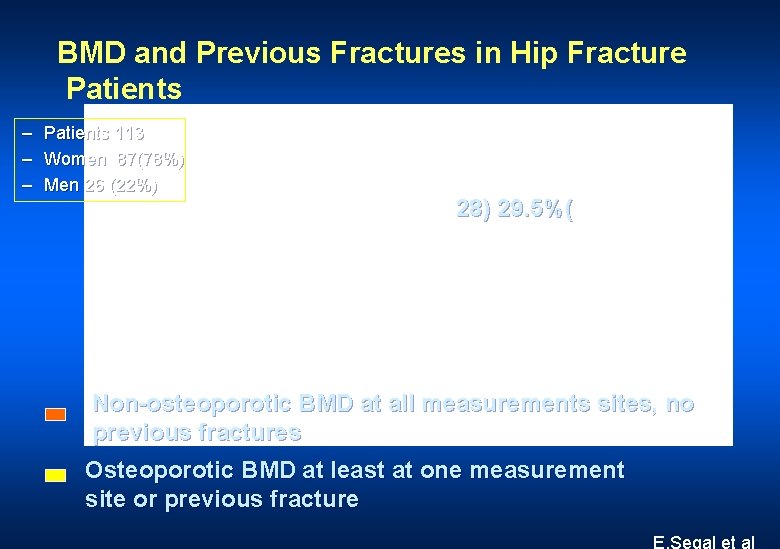
BMD and Previous Fractures in Hip Fracture Patients – – – Patients 113 Women 87(78%) Men 26 (22%) 28) 29. 5%( Non-osteoporotic BMD at all measurements sites, no previous fractures Osteoporotic BMD at least at one measurement site or previous fracture E. Segal et al
Better Lighting to Reduce Falls and Fracture? A Comment on de Boer et al. (2004): Different Aspects of Visual Impairment as Risk Factors for Falls and Fractures in Older Men and Women Aart C Kooijman and Frans W Cornelissen JBMR November 2005, Volume 20, Number 11 Investments in the daily living conditions and improving the visibility of the elderly visual environment will presumably reduce their risk of falling and fractures, in turn resulting in savings on medical and care expenses.
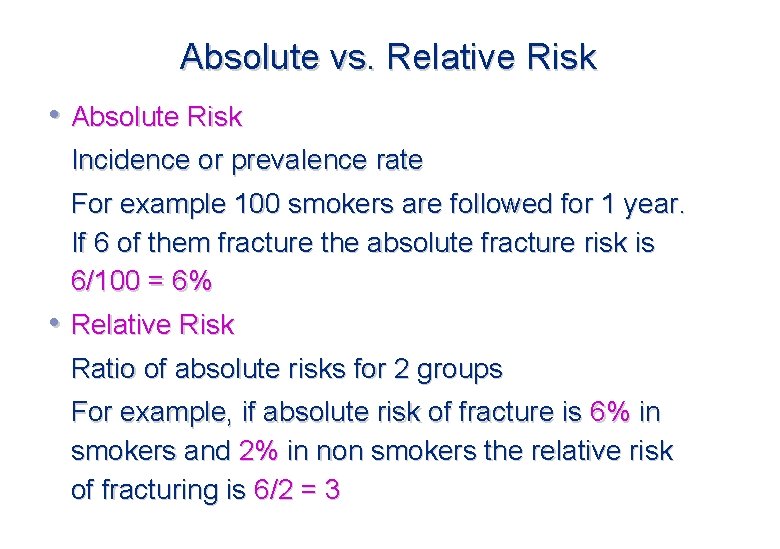
Absolute vs. Relative Risk • Absolute Risk Incidence or prevalence rate For example 100 smokers are followed for 1 year. If 6 of them fracture the absolute fracture risk is 6/100 = 6% • Relative Risk Ratio of absolute risks for 2 groups For example, if absolute risk of fracture is 6% in smokers and 2% in non smokers the relative risk of fracturing is 6/2 = 3



It Often Takes Time to Reach the Diagnosis S Ish-Shalom
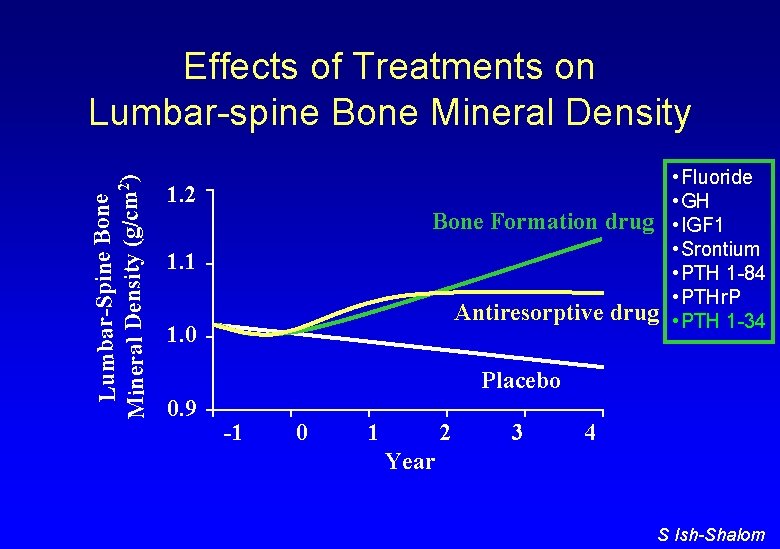
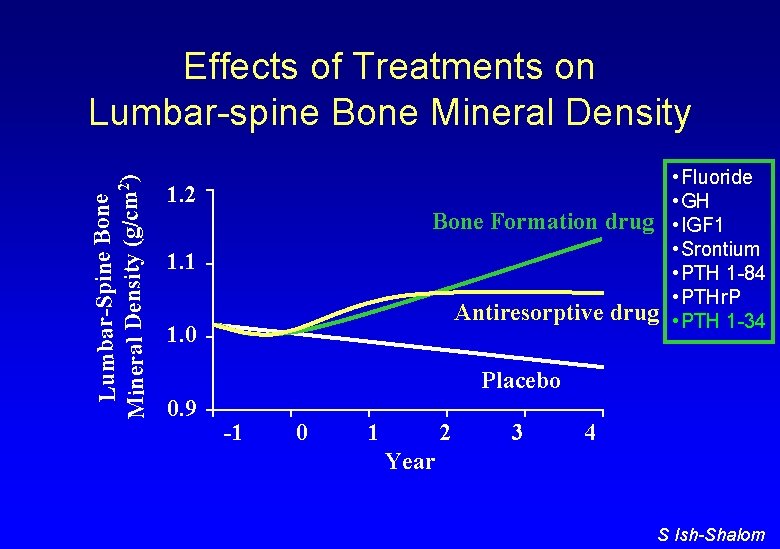
Lumbar-Spine Bone 2) m /c (g ty si en D al er in M Effects of Treatments on Lumbar-spine Bone Mineral Density • Fluoride • GH Bone Formation drug • IGF 1 • Srontium • PTH 1 -84 • PTHr. P Antiresorptive drug • PTH 1 -34 1. 2 1. 1 1. 0 Placebo 0. 9 -1 0 1 2 3 4 Year S Ish-Shalom
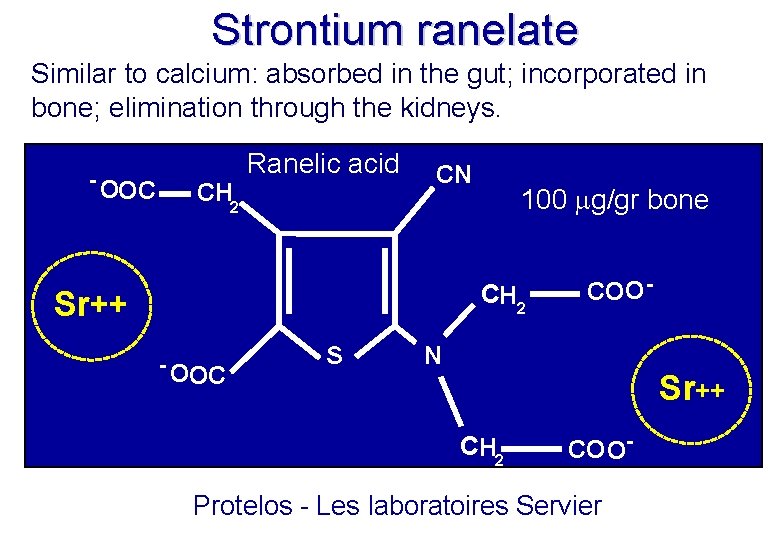
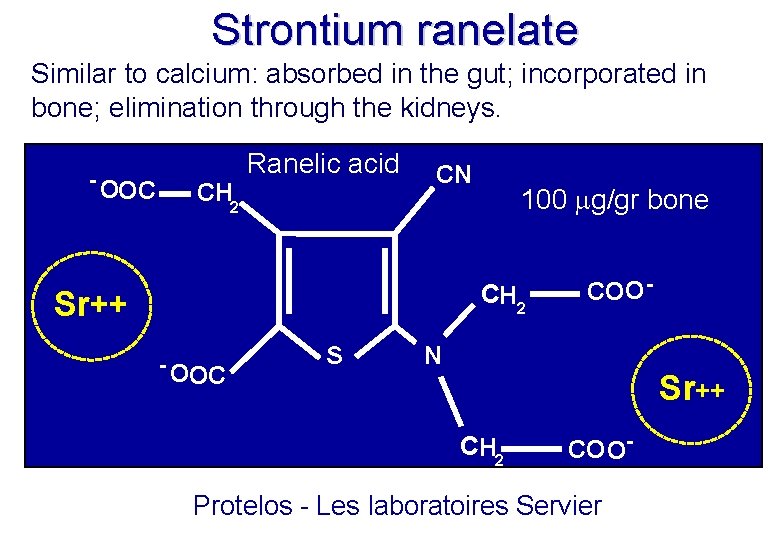
Strontium ranelate Similar to calcium: absorbed in the gut; incorporated in bone; elimination through the kidneys. - OOC CH 2 Ranelic acid CN 100 g/gr bone CH 2 Sr++ - OOC S COO - N Sr++ CH 2 CO O- Protelos - Les laboratoires Servier

Strontium - Bone Retention • In the short term the strontium atoms are adsorbed on to the surface of hydroxyapatite crystals • In the longer term some strontium will exchange with calcium in the bone mineral and may remain bound in the skeleton for years • The exchange is limited with maximum replacement by strontium, when given in high doses, of one in every ten calcium atoms.

Strontium – Bone Retention • ICRP model predicts that at 3 months, 1 year, and 3 years after a single oral dose of strontium, the skeleton retains 20%, 15%, and 11%, respectively, of the strontium absorbed by the gut • Three-year treatment with strontium ranelate at 2 g/day total strontium intake of 750 g. 25% absorption by the gut • Using the ICRP model to calculate the average long-term retention after a 3 -year treatment, there is 30 g of strontium in the skeleton. • Expressed as a molar fraction of the total calcium content in bone =1% (i. e. , after 3 years of treatment with strontium ranelate, there is 1 strontium atom for every 100 calcium atoms in bone tissue).
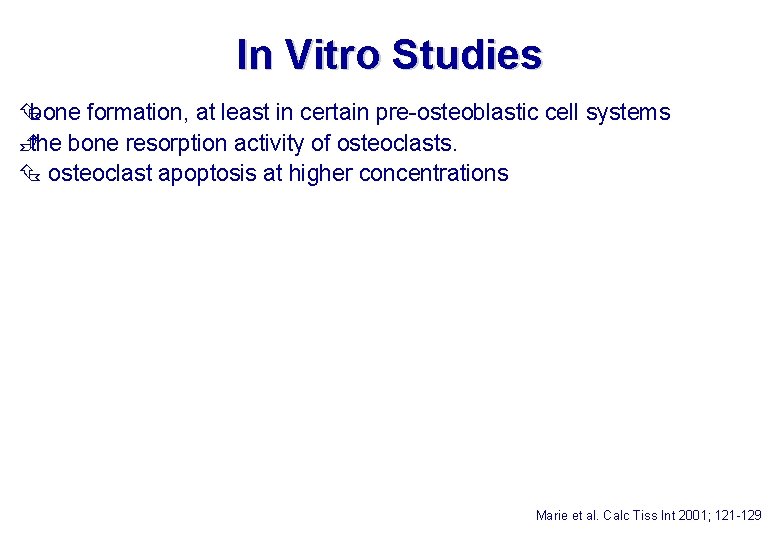
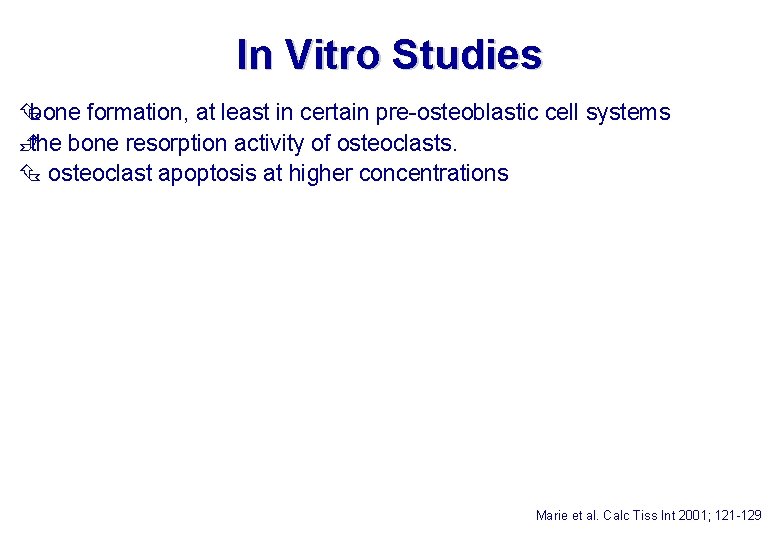
In Vitro Studies bone formation, at least in certain pre-osteoblastic cell systems È the bone resorption activity of osteoclasts. osteoclast apoptosis at higher concentrations Marie et al. Calc Tiss Int 2001; 121 -129
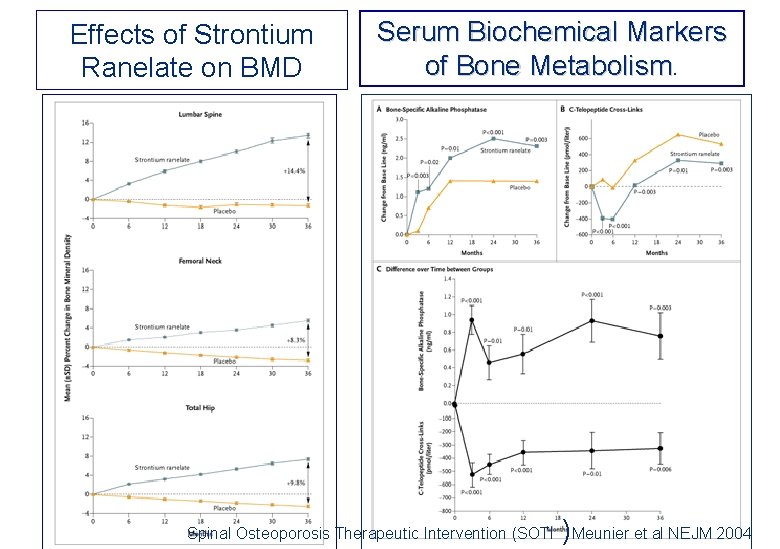
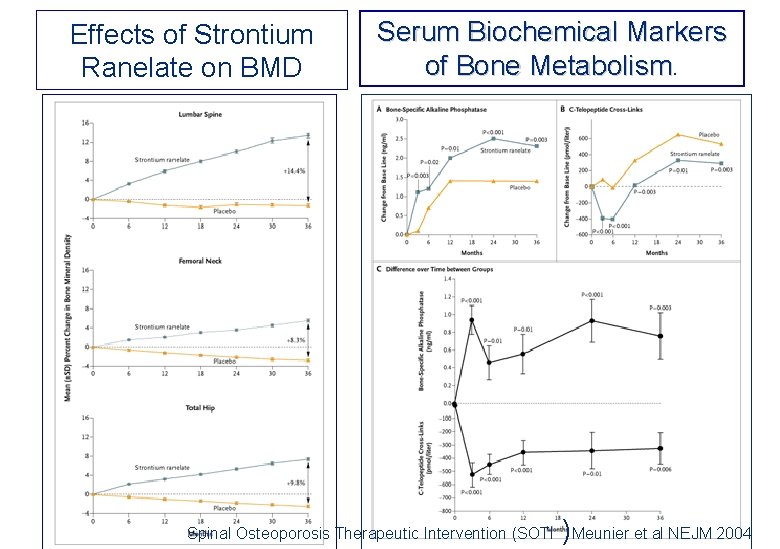
Effects of Strontium Ranelate on BMD Serum Biochemical Markers of Bone Metabolism Spinal Osteoporosis Therapeutic Intervention (SOTI )Meunier et al NEJM 2004
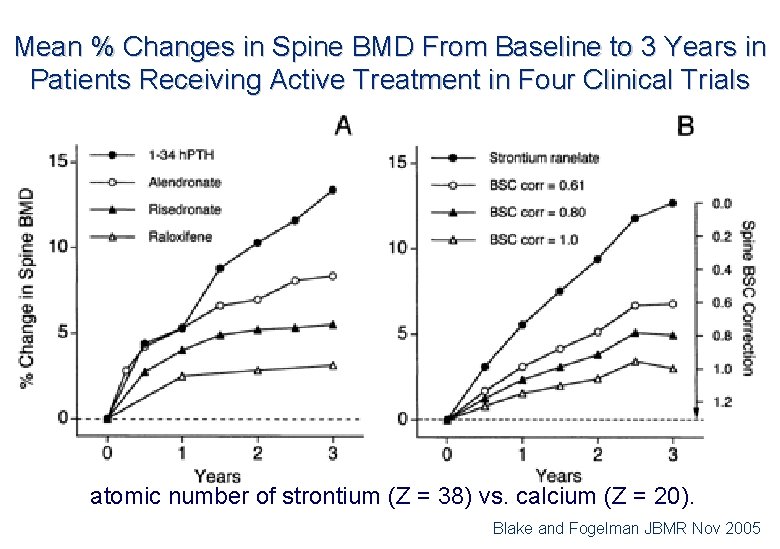
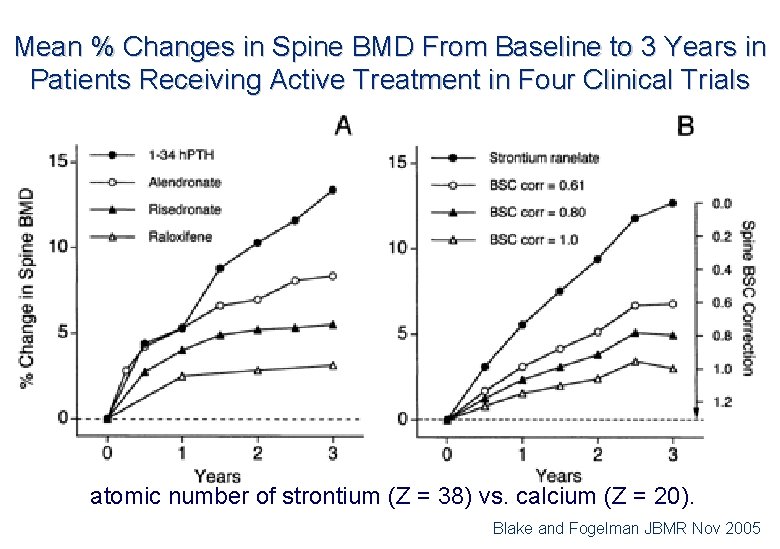
Mean % Changes in Spine BMD From Baseline to 3 Years in Patients Receiving Active Treatment in Four Clinical Trials atomic number of strontium (Z = 38) vs. calcium (Z = 20). Blake and Fogelman JBMR Nov 2005
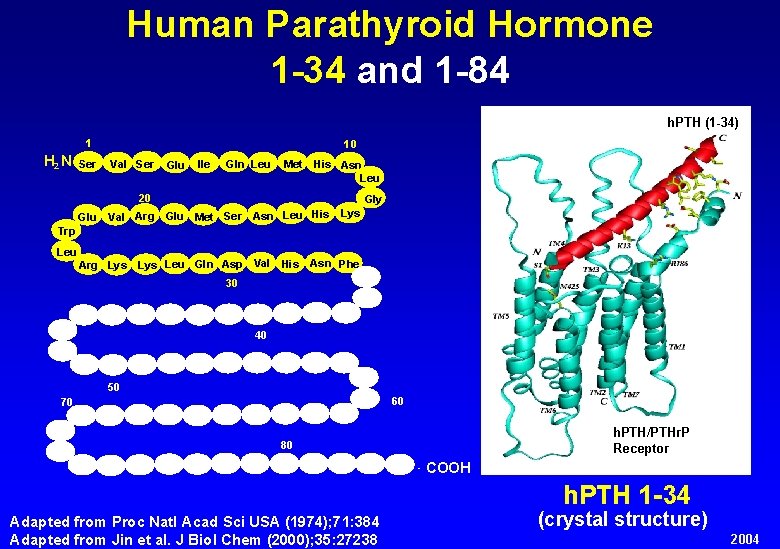
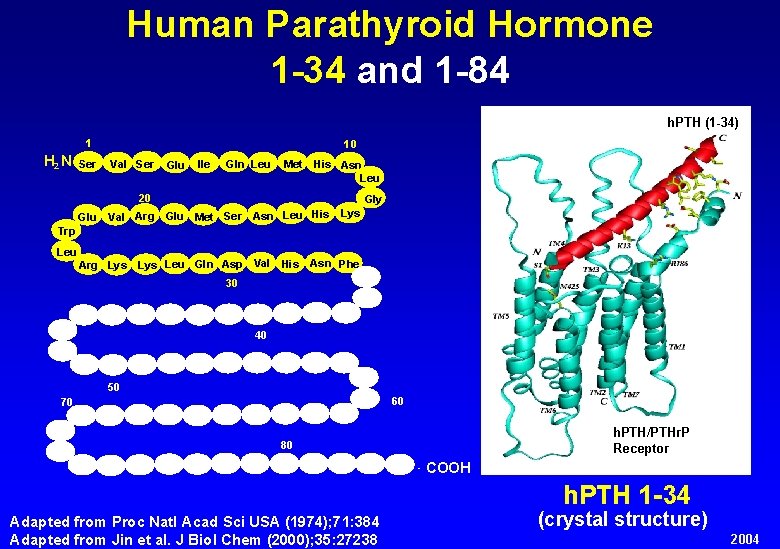
Human Parathyroid Hormone 1 -34 and 1 -84 h. PTH (1 -34) 1 H 2 N -Ser 10 Val Ser Glu Ile Gln Leu Met His Asn Leu 20 Glu Val Arg Gly Glu Met Ser Asn Leu His Lys Trp Leu Arg Lys Leu Gln Asp Val His Asn Phe 30 40 50 60 70 h. PTH/PTHr. P Receptor 80 - COOH h. PTH 1 -34 Adapted from Proc Natl Acad Sci USA (1974); 71: 384 Adapted from Jin et al. J Biol Chem (2000); 35: 27238 (crystal structure) 2004

Cumulative Proportion Of Women Enrolled In The Follow-up Study Who Had One Or More Nonvertebral Fragility Fractures After Baseline By Kaplan-Meier Analysis Prince et al JBMR Sep 2005
Doctors are men who prescribe medicines of which they know little, to cure diseases of which they know less, in human beings of whom they know nothing. Francois-Marie Arouet - Voltaire 1694 - 1778

 Subjective data for osteoporosis
Subjective data for osteoporosis Backup and recovery techniques
Backup and recovery techniques Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Types of nursing diagnosis
Types of nursing diagnosis Nursing process objectives
Nursing process objectives Charting exercise chapter 28
Charting exercise chapter 28 Lateral throat form classification neil
Lateral throat form classification neil Endodontic diagnosis and treatment planning
Endodontic diagnosis and treatment planning Chapter 28 oral diagnosis and treatment planning
Chapter 28 oral diagnosis and treatment planning Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Pes statement for osteoporosis
Pes statement for osteoporosis Dual energy x ray absorptiometry (dexa)
Dual energy x ray absorptiometry (dexa) Is osteoporosis hypokinetic or hyperkinetic
Is osteoporosis hypokinetic or hyperkinetic Loss defination
Loss defination Woc atrial fibrilasi
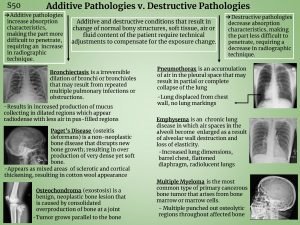
Woc atrial fibrilasi Additive pathology
Additive pathology Royal osteoporosis society leaflets
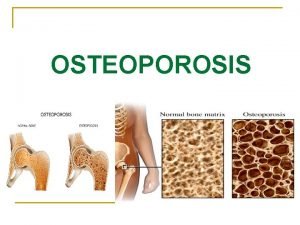
Royal osteoporosis society leaflets Osteoporosis
Osteoporosis Eva decroli
Eva decroli Alendronate mechanism
Alendronate mechanism Tbs osteoporosis
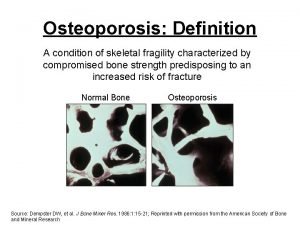
Tbs osteoporosis Osteoporosis definition
Osteoporosis definition International osteoporosis foundation
International osteoporosis foundation Whole muscle
Whole muscle Philia sophia philia nikea
Philia sophia philia nikea Josef a high school student tells his therapist
Josef a high school student tells his therapist