UNIVERSITA CATTOLICA DEL SACRO CUORE Facolta di Medicina







- Slides: 75
UNIVERSITA’ CATTOLICA DEL SACRO CUORE Facolta di Medicina e Chirurgia “A. Gemelli” UOC DI MEDICINA INTERNA E GASTROENTEROLOGIA direttore Prof. A Gasbarrini “La disbiosi indotta da antibiotici a breve e a lungo termine: dalla patogenesi al trattamento” Franco Scaldaferri, MD, Ph. D Department of internal Medicine, Gastroenterology Division IBD Unit – “Policlinico “A. Gemelli” Hospital Catholic University of Sacred Hearth Rome, Italy francoscaldaferri@gmail. com
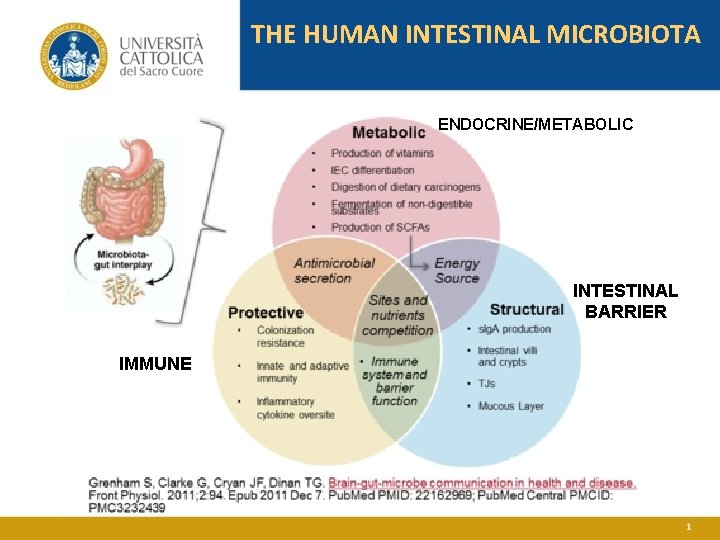
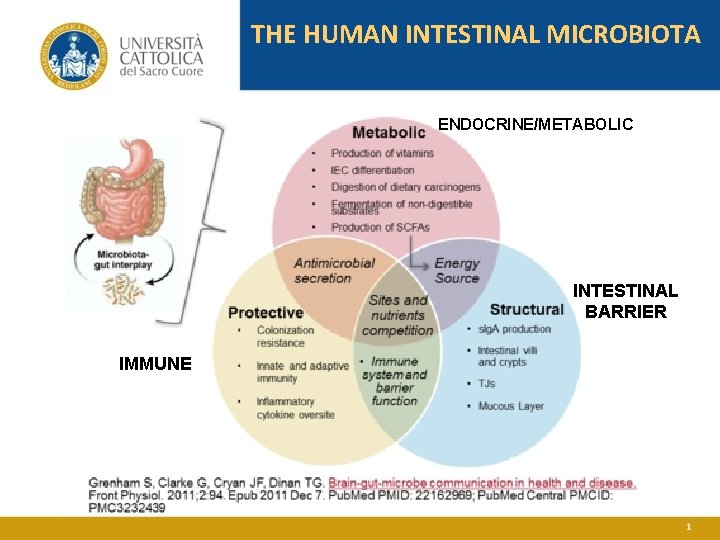
THE HUMAN INTESTINAL MICROBIOTA ENDOCRINE/METABOLIC INTESTINAL BARRIER IMMUNE
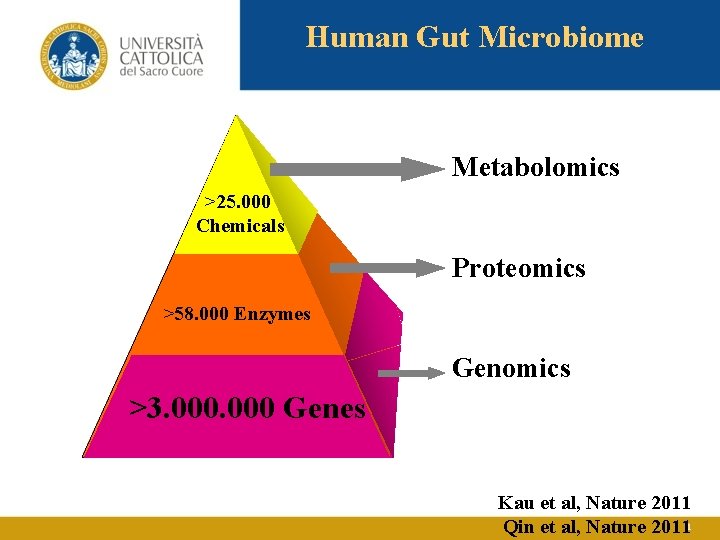
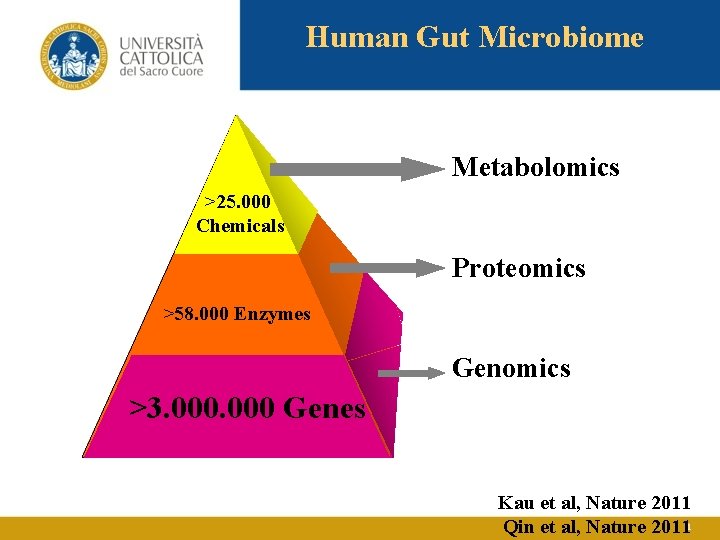
Human Gut Microbiome Metabolomics >25. 000 Chemicals Proteomics >58. 000 Enzymes Genomics >3. 000 Genes Kau et al, Nature 2011 Qin et al, Nature 2011
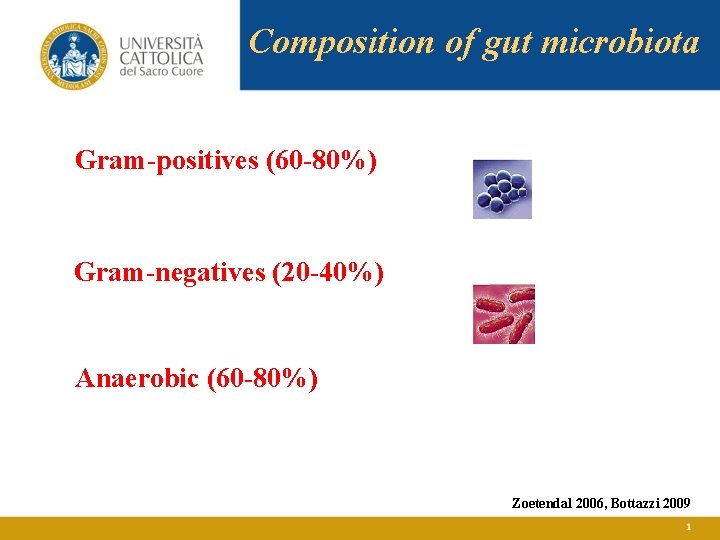
Composition of gut microbiota Gram-positives (60 -80%) Gram-negatives (20 -40%) Anaerobic (60 -80%) Zoetendal 2006, Bottazzi 2009
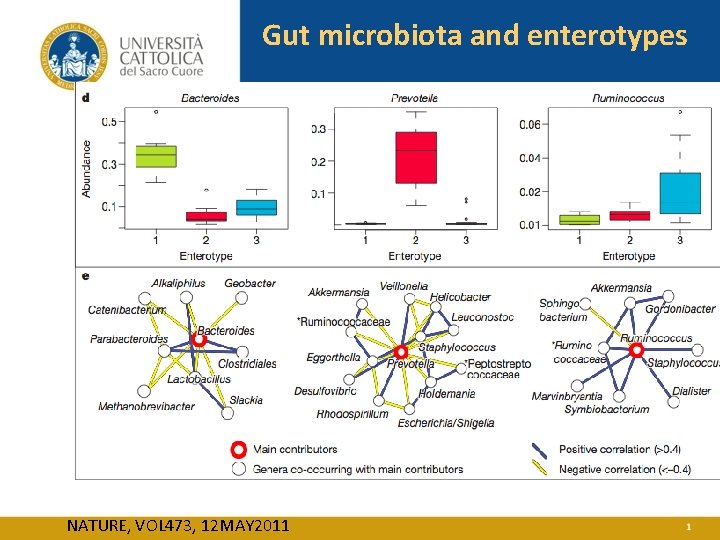
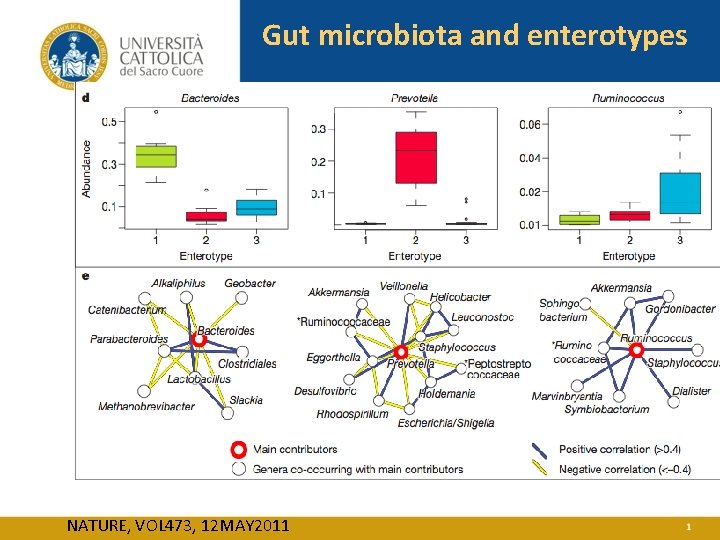
Gut microbiota and enterotypes NATURE, VOL 473, 12 MAY 2011
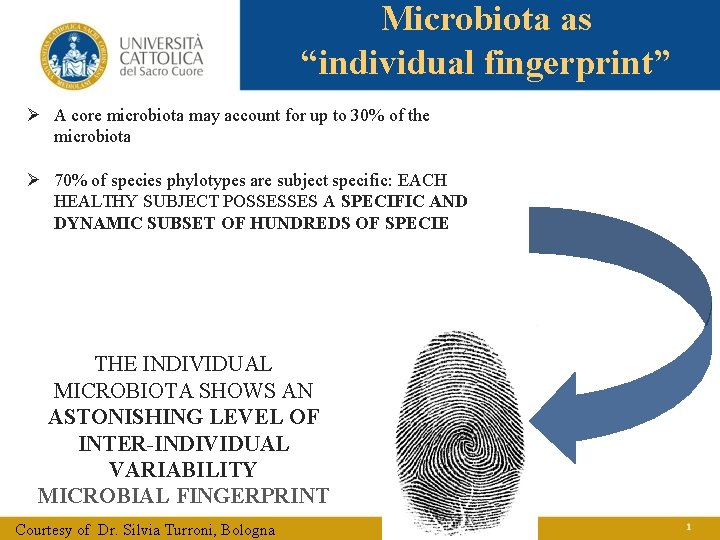
Microbiota as “individual fingerprint” Ø A core microbiota may account for up to 30% of the microbiota Ø 70% of species phylotypes are subject specific: EACH HEALTHY SUBJECT POSSESSES A SPECIFIC AND DYNAMIC SUBSET OF HUNDREDS OF SPECIE THE INDIVIDUAL MICROBIOTA SHOWS AN ASTONISHING LEVEL OF INTER-INDIVIDUAL VARIABILITY MICROBIAL FINGERPRINT Courtesy of Dr. Silvia Turroni, Bologna
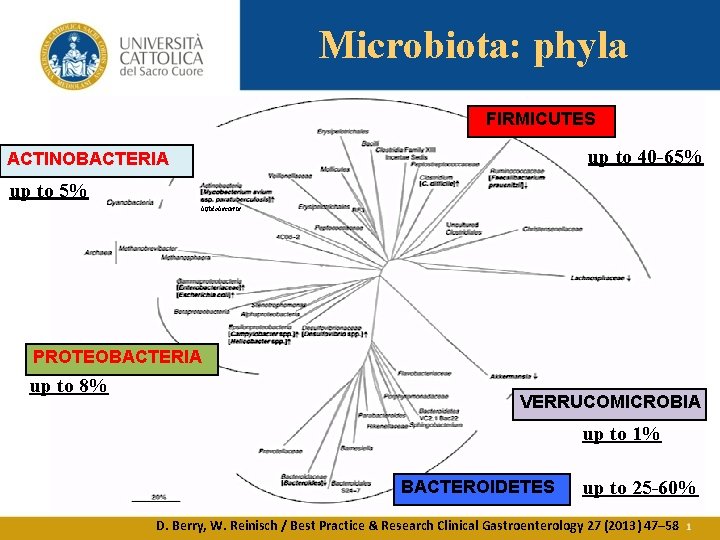
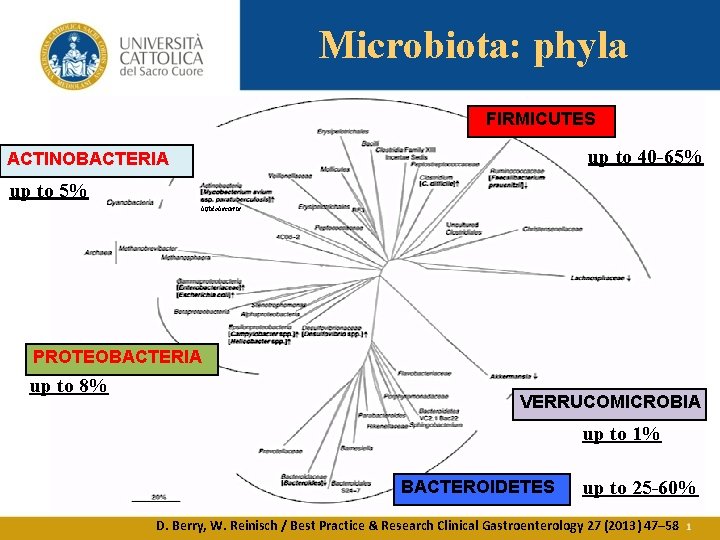
Microbiota: phyla FIRMICUTES up to 40 -65% ACTINOBACTERIA up to 5% bifidobacteria PROTEOBACTERIA up to 8% VERRUCOMICROBIA up to 1% BACTEROIDETES up to 25 -60% D. Berry, W. Reinisch / Best Practice & Research Clinical Gastroenterology 27 (2013) 47– 58
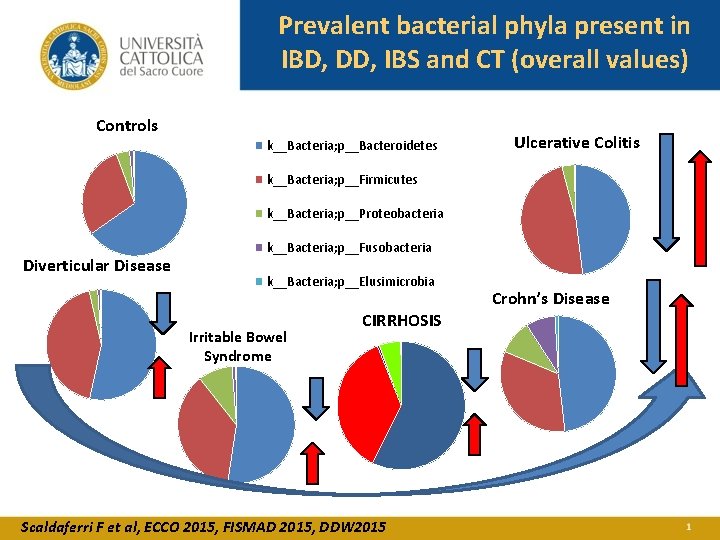
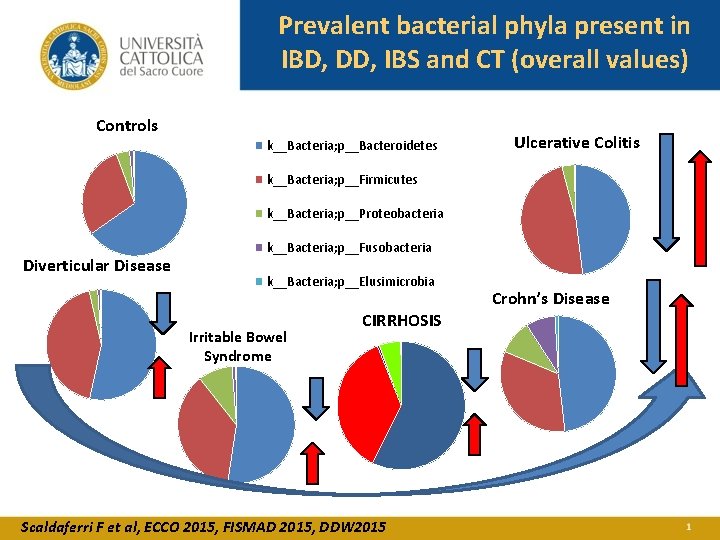
Prevalent bacterial phyla present in IBD, DD, IBS and CT (overall values) Controls k__Bacteria; p__Bacteroidetes Ulcerative Colitis k__Bacteria; p__Firmicutes k__Bacteria; p__Proteobacteria Diverticular Disease k__Bacteria; p__Fusobacteria k__Bacteria; p__Elusimicrobia Irritable Bowel Syndrome CIRRHOSIS Scaldaferri F et al, ECCO 2015, FISMAD 2015, DDW 2015 Crohn’s Disease
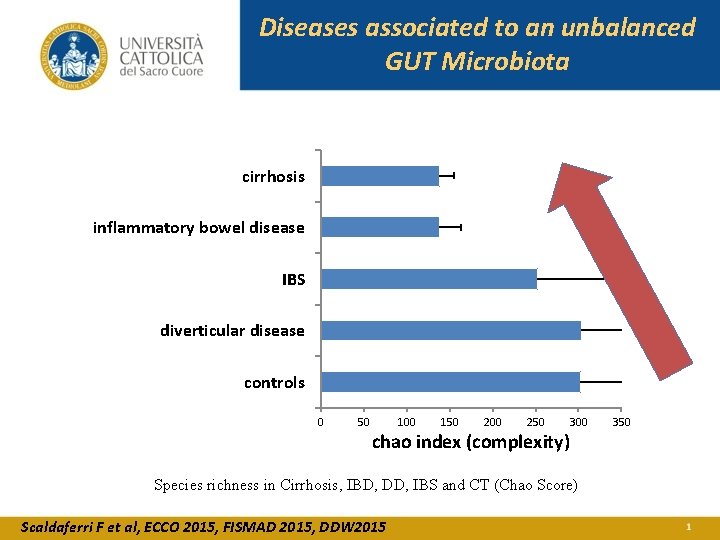
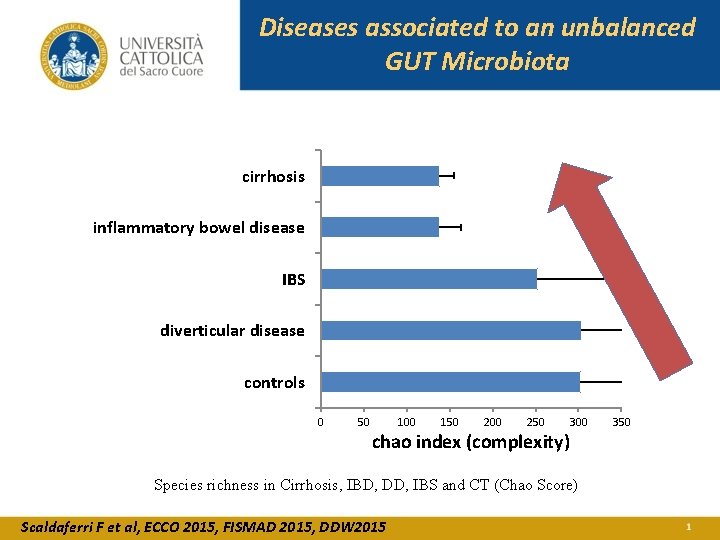
Diseases associated to an unbalanced GUT Microbiota cirrhosis inflammatory bowel disease IBS diverticular disease controls 0 50 100 150 200 250 300 chao index (complexity) Species richness in Cirrhosis, IBD, DD, IBS and CT (Chao Score) Scaldaferri F et al, ECCO 2015, FISMAD 2015, DDW 2015 350

Microbiota and antibiotics Ø Antibiotics act on single germ level
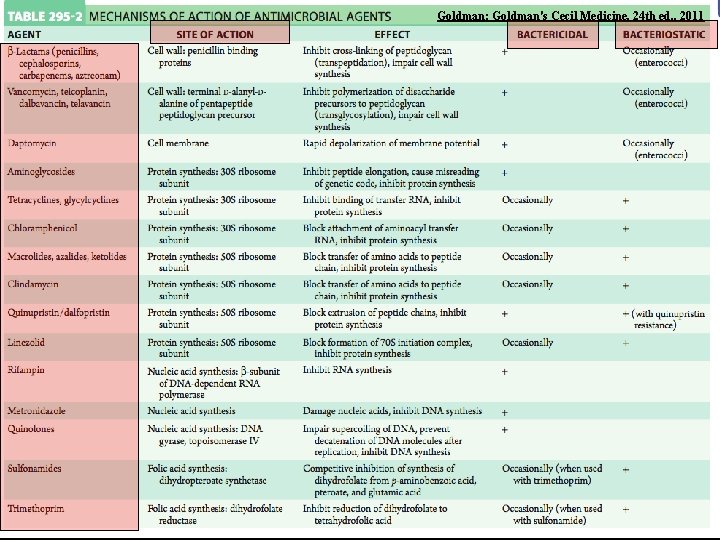
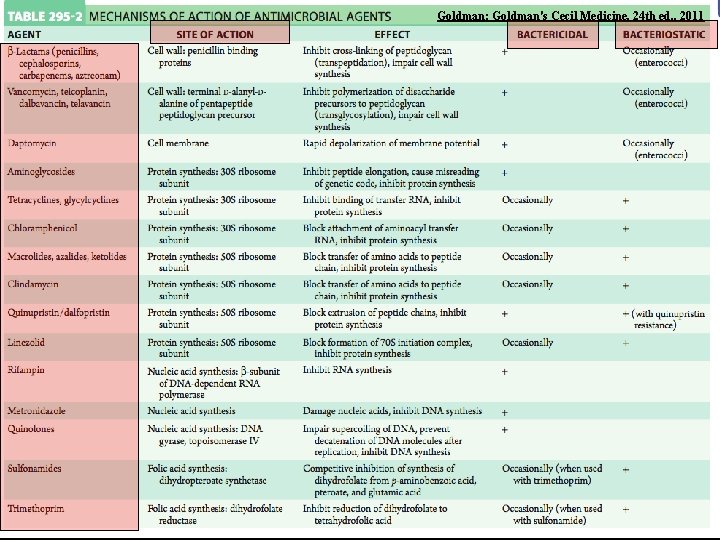
Goldman: Goldman's Cecil Medicine, 24 th ed. , 2011


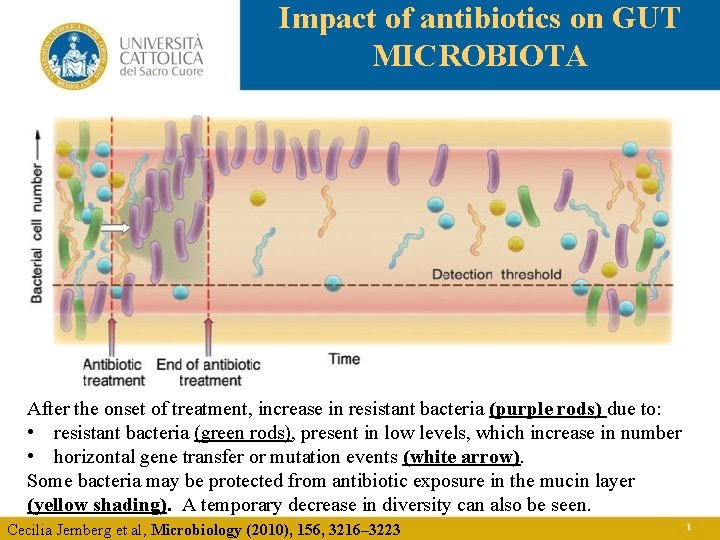
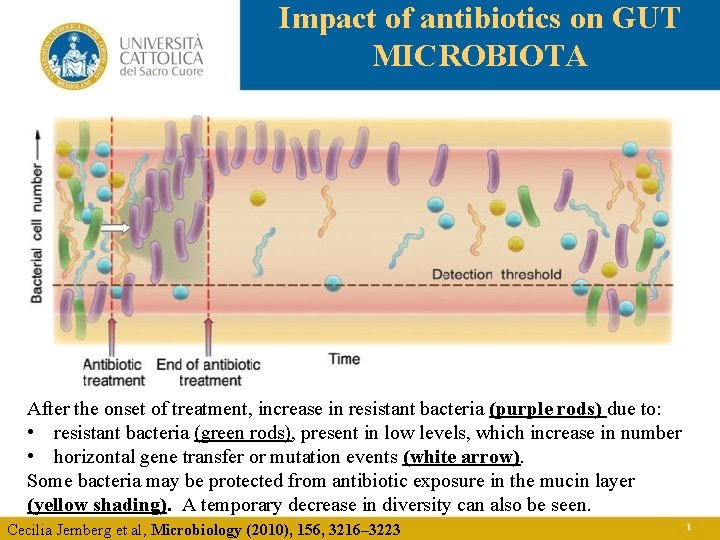
Impact of antibiotics on GUT MICROBIOTA After the onset of treatment, increase in resistant bacteria (purple rods) due to: • resistant bacteria (green rods), present in low levels, which increase in number • horizontal gene transfer or mutation events (white arrow). Some bacteria may be protected from antibiotic exposure in the mucin layer (yellow shading). A temporary decrease in diversity can also be seen. Cecilia Jernberg et al, Microbiology (2010), 156, 3216– 3223
Impact of antibiotics on GUT MICROBIOTA • Antibiotic concentration in blood ? • Antibiotic concentration within gut lumen? • Antibiotic concentration within gut mucus? • Subject variability?
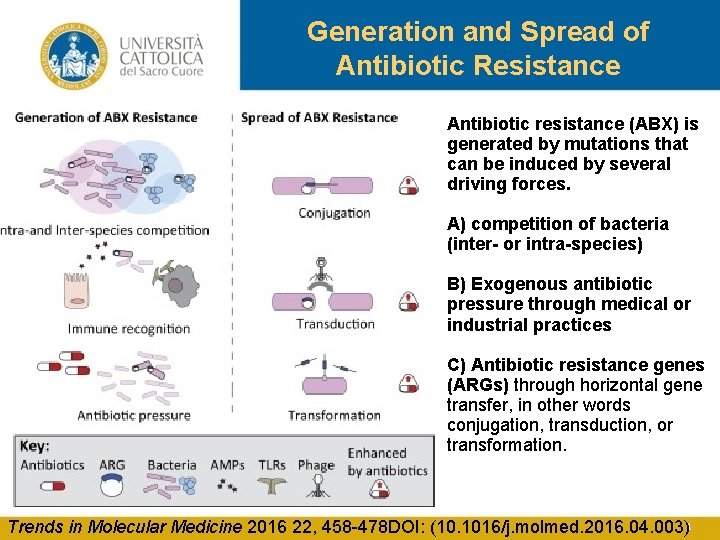
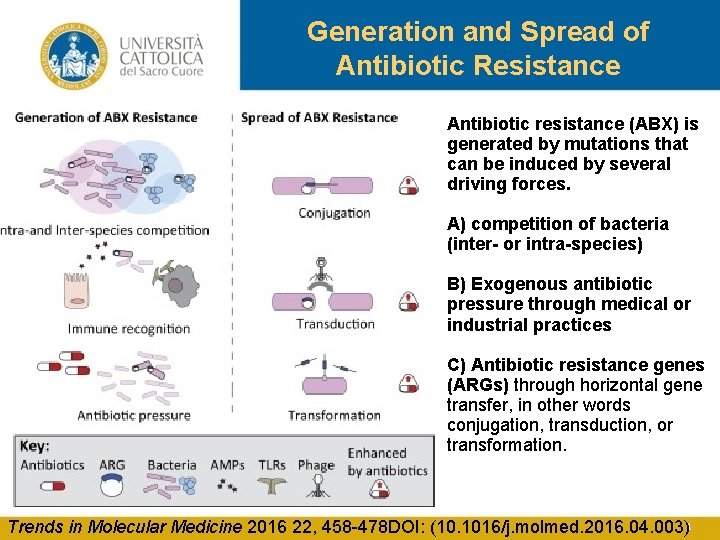
Generation and Spread of Antibiotic Resistance Antibiotic resistance (ABX) is generated by mutations that can be induced by several driving forces. A) competition of bacteria (inter- or intra-species) B) Exogenous antibiotic pressure through medical or industrial practices C) Antibiotic resistance genes (ARGs) through horizontal gene transfer, in other words conjugation, transduction, or transformation. Trends in Molecular Medicine 2016 22, 458 -478 DOI: (10. 1016/j. molmed. 2016. 04. 003)
Microbiota and antibiotics Ø Antibiotics act on single germ level Ø Antibiotics act on gut microbiota composition
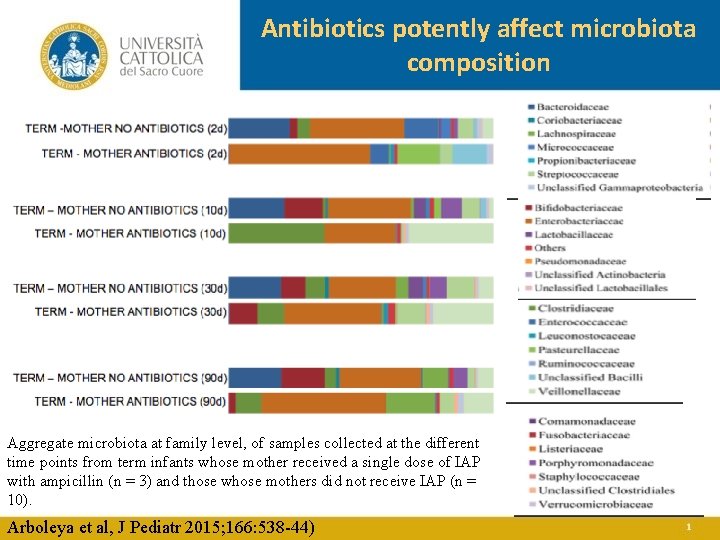
16 S ribosomal RNA gene sequence-based microbiota analysis quantitative polymerase chain reaction to evaluate the establishment of the intestinal microbiota preterm infants (n = 27) compared with full-term babies (n = 13). Arboleya et al, J Pediatr 2015; 166: 538 -44)
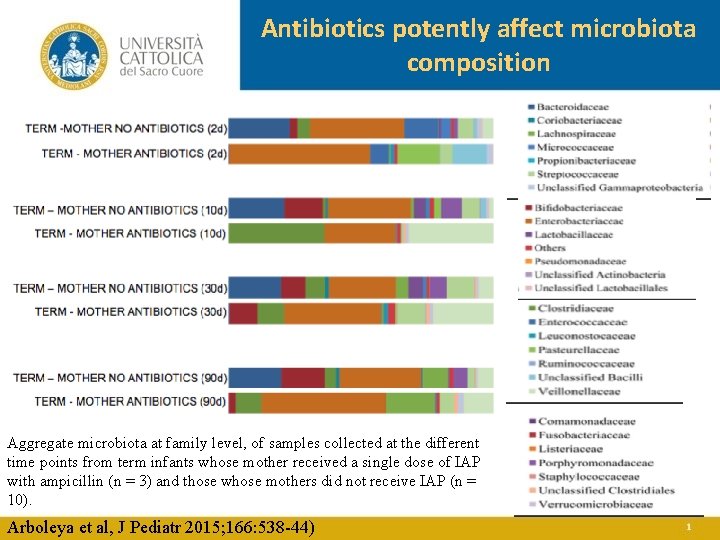
Antibiotics potently affect microbiota composition Aggregate microbiota at family level, of samples collected at the different time points from term infants whose mother received a single dose of IAP with ampicillin (n = 3) and those whose mothers did not receive IAP (n = 10). Arboleya et al, J Pediatr 2015; 166: 538 -44)
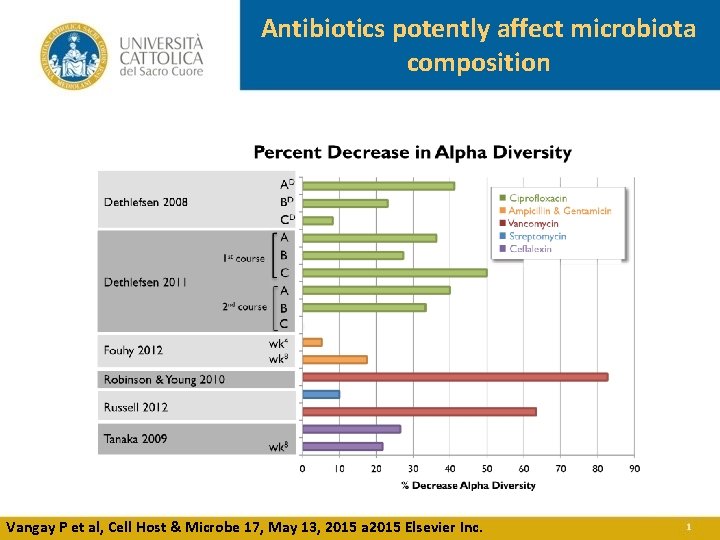
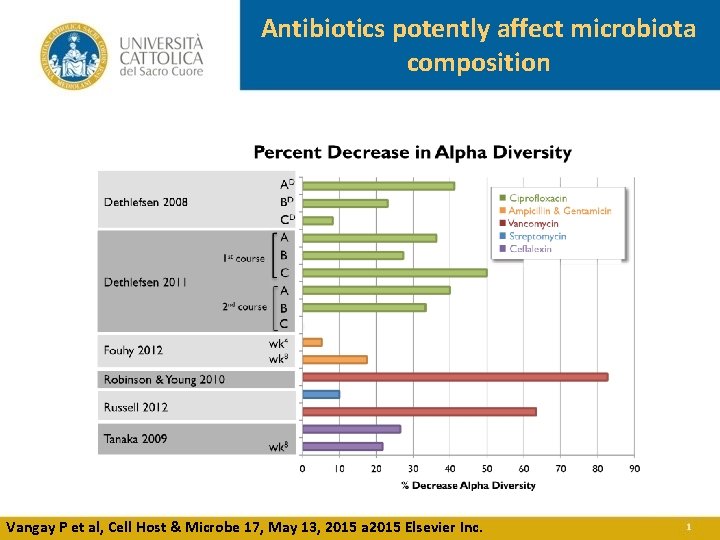
Antibiotics potently affect microbiota composition Vangay P et al, Cell Host & Microbe 17, May 13, 2015 a 2015 Elsevier Inc.
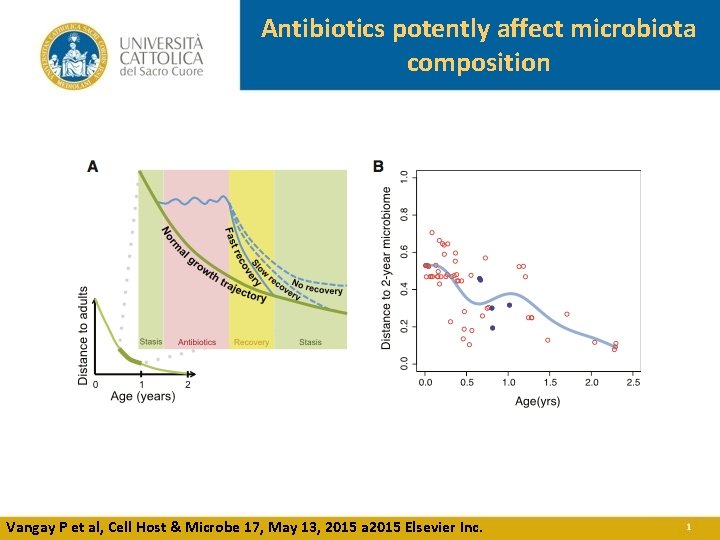
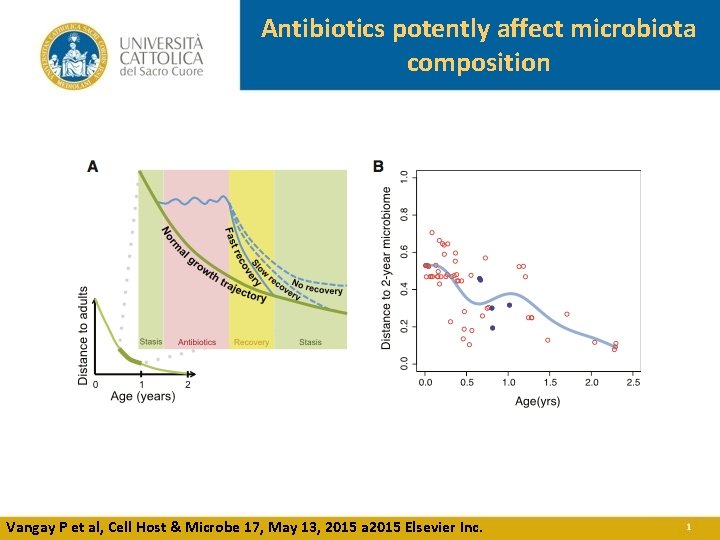
Antibiotics potently affect microbiota composition Vangay P et al, Cell Host & Microbe 17, May 13, 2015 a 2015 Elsevier Inc.
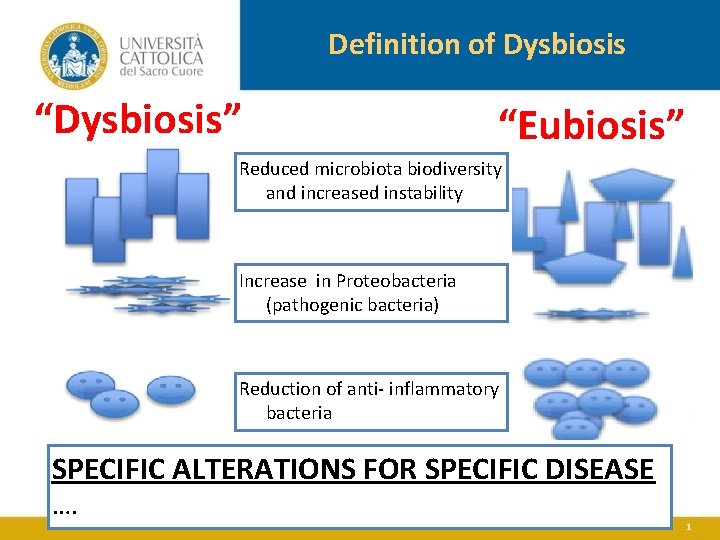
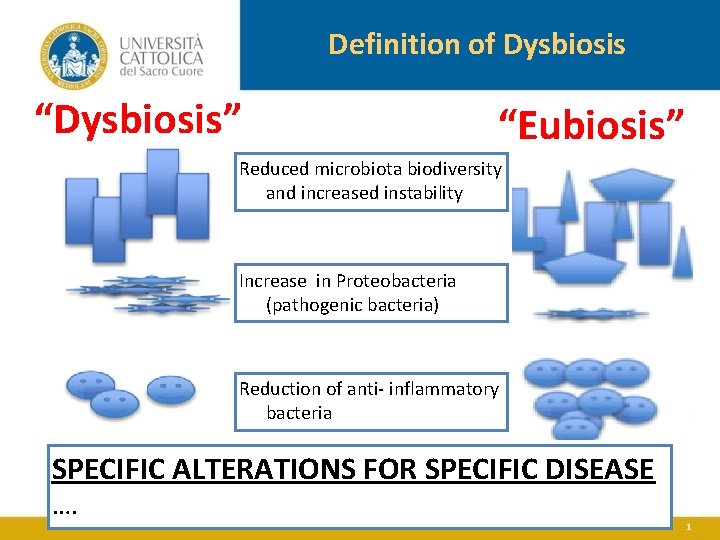
Definition of Dysbiosis “Dysbiosis” “Eubiosis” Reduced microbiota biodiversity and increased instability Increase in Proteobacteria (pathogenic bacteria) Reduction of anti- inflammatory bacteria SPECIFIC ALTERATIONS FOR SPECIFIC DISEASE ….
Microbiota and antibiotics Ø Antibiotics act on single germ level Ø Antibiotics act on gut microbiota Ø Antibiotics impact on gut microbiota functions within the GI tract
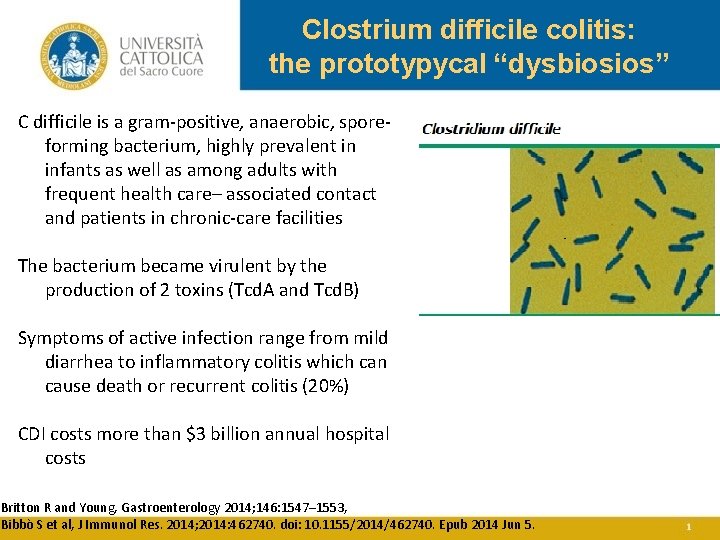
Clostrium difficile colitis: the prototypycal “dysbiosios” C difficile is a gram-positive, anaerobic, sporeforming bacterium, highly prevalent in infants as well as among adults with frequent health care– associated contact and patients in chronic-care facilities The bacterium became virulent by the production of 2 toxins (Tcd. A and Tcd. B) Symptoms of active infection range from mild diarrhea to inflammatory colitis which can cause death or recurrent colitis (20%) CDI costs more than $3 billion annual hospital costs Britton R and Young, Gastroenterology 2014; 146: 1547– 1553, Bibbò S et al, J Immunol Res. 2014; 2014: 462740. doi: 10. 1155/2014/462740. Epub 2014 Jun 5.
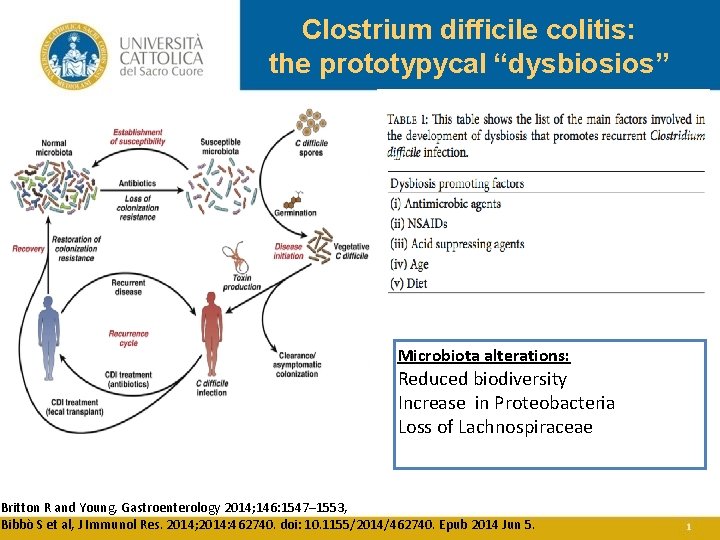
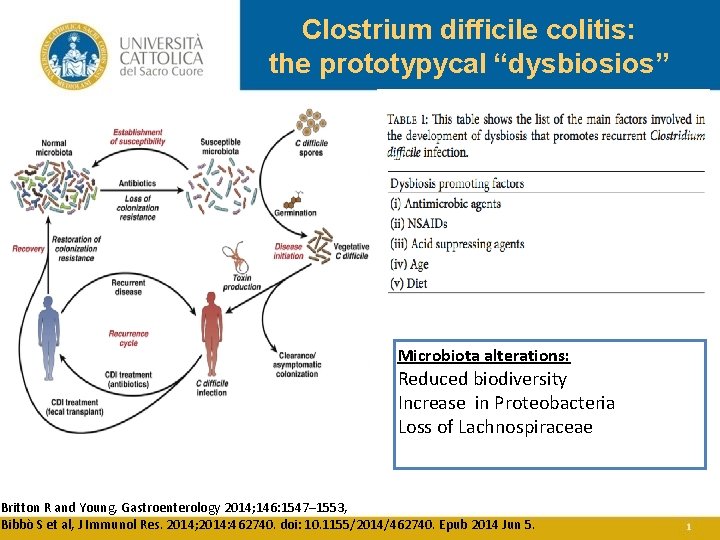
Clostrium difficile colitis: the prototypycal “dysbiosios” Microbiota alterations: Reduced biodiversity Increase in Proteobacteria Loss of Lachnospiraceae Britton R and Young, Gastroenterology 2014; 146: 1547– 1553, Bibbò S et al, J Immunol Res. 2014; 2014: 462740. doi: 10. 1155/2014/462740. Epub 2014 Jun 5.
Antibiotic associated diarrhea • Antibiotic associated diarrhea (AAD)ranges from mild diarrhea to inflammatory colitis to pseudomembranous colitis • AAD may occur while taking antibiotics, or develop as much as 8 weeks afterwards. • Duration of AAD ranges from 1 day to several months, being recurrent in up to 20 -50% of patients Mc Farland VL, Future Microbiology. 3. 5 (Oct. 2008)
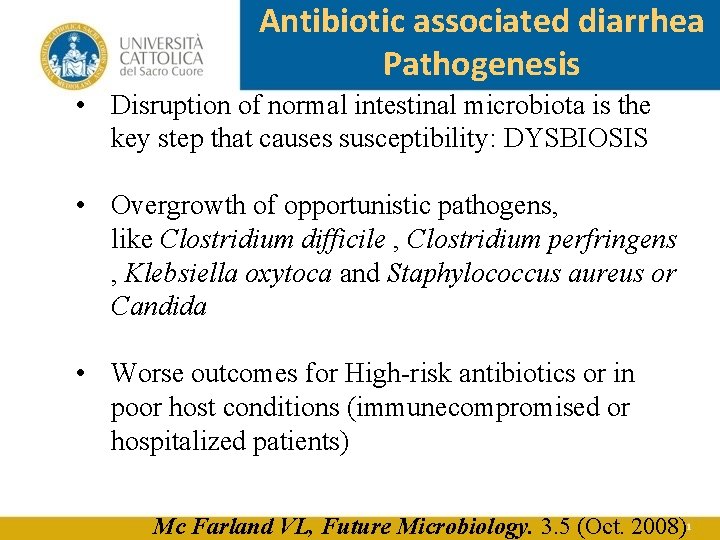
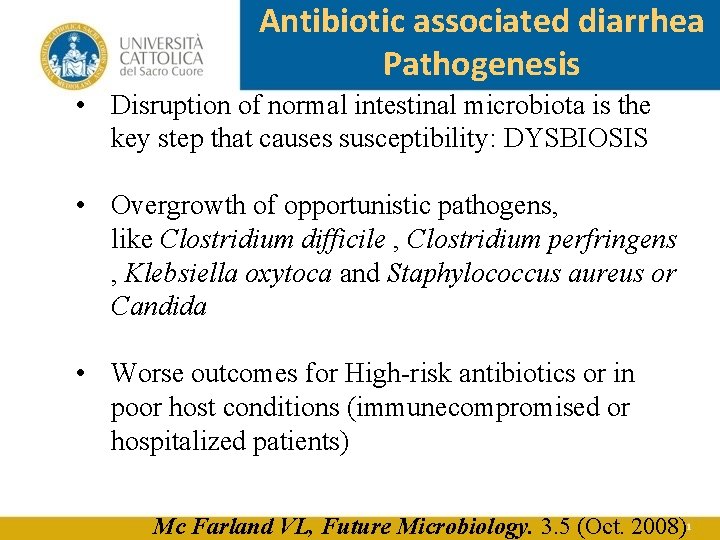
Antibiotic associated diarrhea Pathogenesis • Disruption of normal intestinal microbiota is the key step that causes susceptibility: DYSBIOSIS • Overgrowth of opportunistic pathogens, like Clostridium difficile , Clostridium perfringens , Klebsiella oxytoca and Staphylococcus aureus or Candida • Worse outcomes for High-risk antibiotics or in poor host conditions (immunecompromised or hospitalized patients) Mc Farland VL, Future Microbiology. 3. 5 (Oct. 2008)
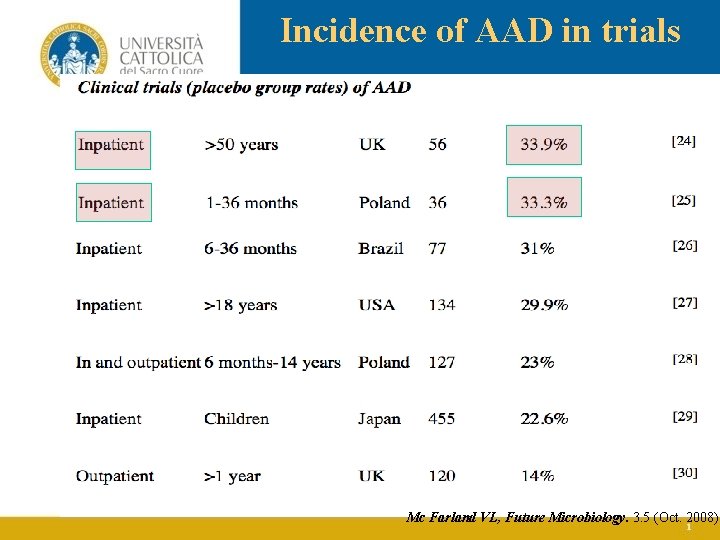
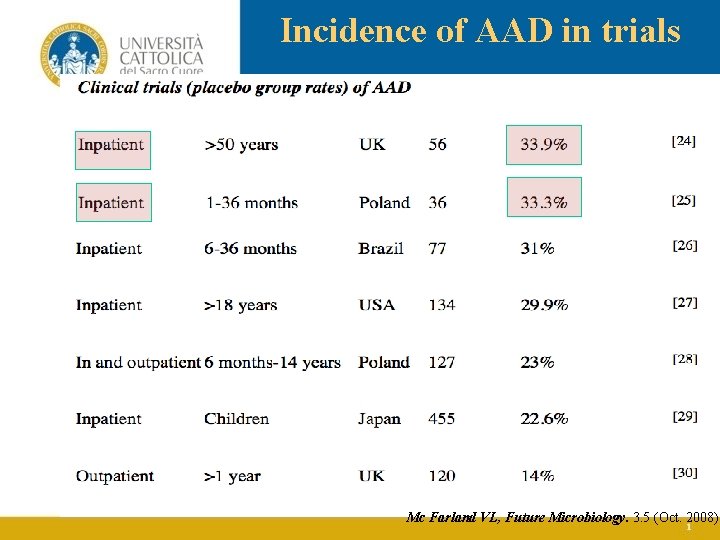
Incidence of AAD in trials Mc Farland VL, Future Microbiology. 3. 5 (Oct. 2008)
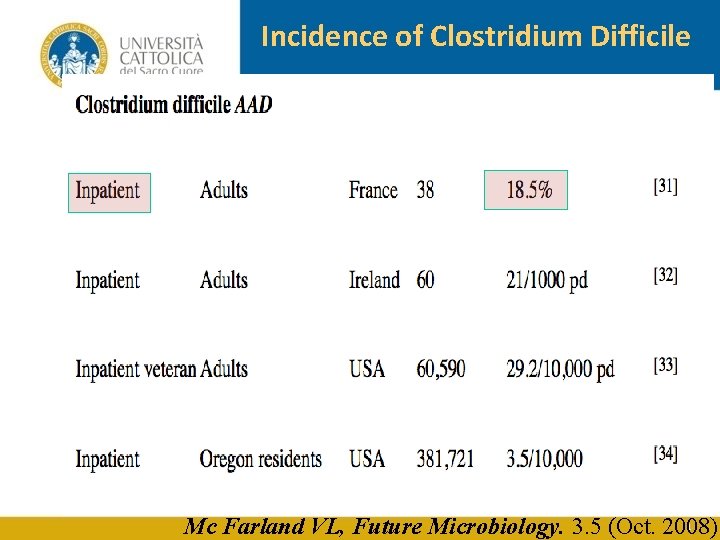
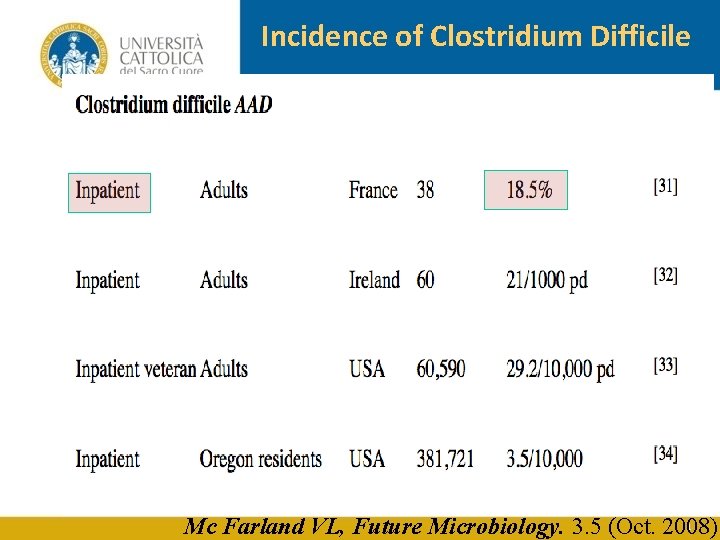
Incidence of Clostridium Difficile Mc Farland VL, Future Microbiology. 3. 5 (Oct. 2008)
Microbiota and antibiotics Ø Antibiotics act on single germ level Ø Antibiotics act on gut microbiota Ø Antibiotics impact on gut microbiota functions within the GI tract Ø Antibiotics impact on gut microbiota functions outside the GI tract
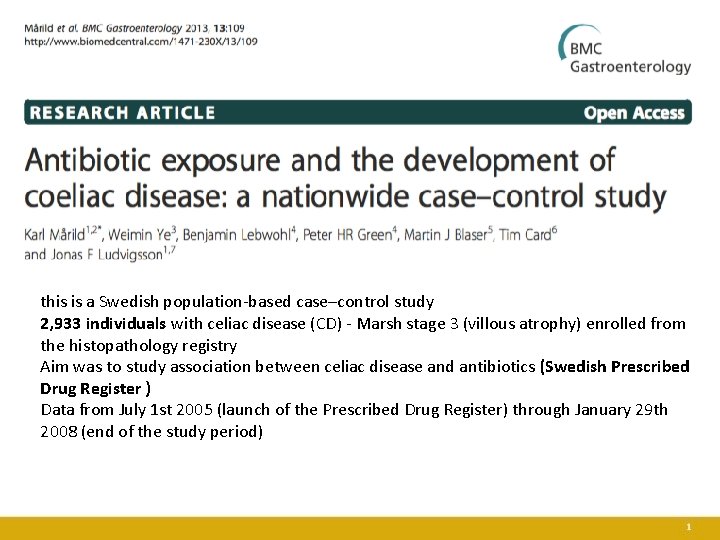
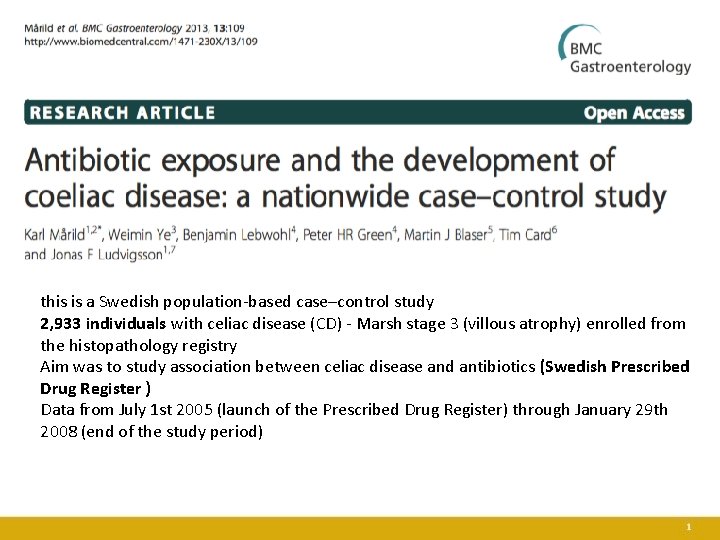
this is a Swedish population-based case–control study 2, 933 individuals with celiac disease (CD) - Marsh stage 3 (villous atrophy) enrolled from the histopathology registry Aim was to study association between celiac disease and antibiotics (Swedish Prescribed Drug Register ) Data from July 1 st 2005 (launch of the Prescribed Drug Register) through January 29 th 2008 (end of the study period)
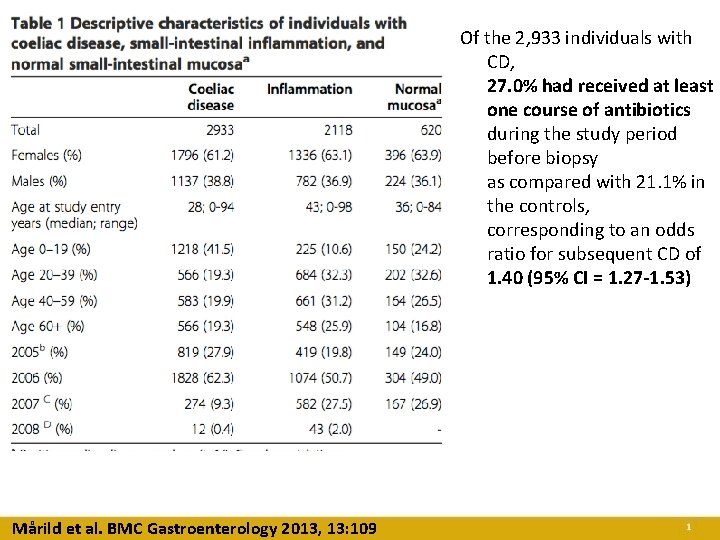
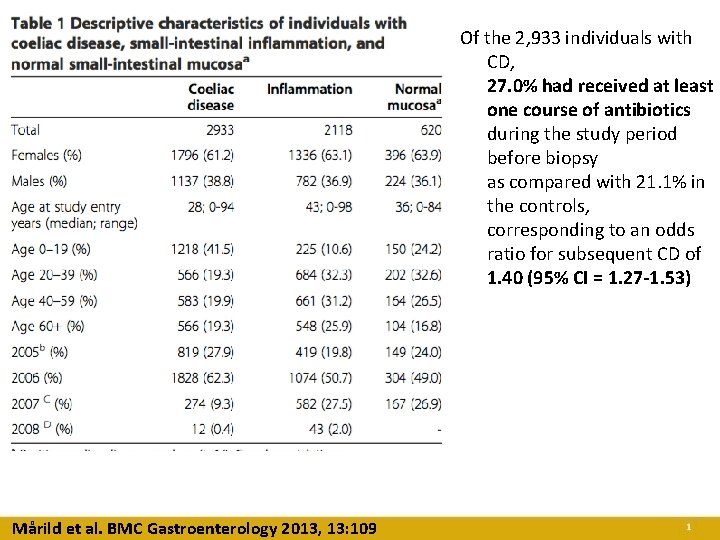
Of the 2, 933 individuals with CD, 27. 0% had received at least one course of antibiotics during the study period before biopsy as compared with 21. 1% in the controls, corresponding to an odds ratio for subsequent CD of 1. 40 (95% CI = 1. 27 -1. 53) Mårild et al. BMC Gastroenterology 2013, 13: 109
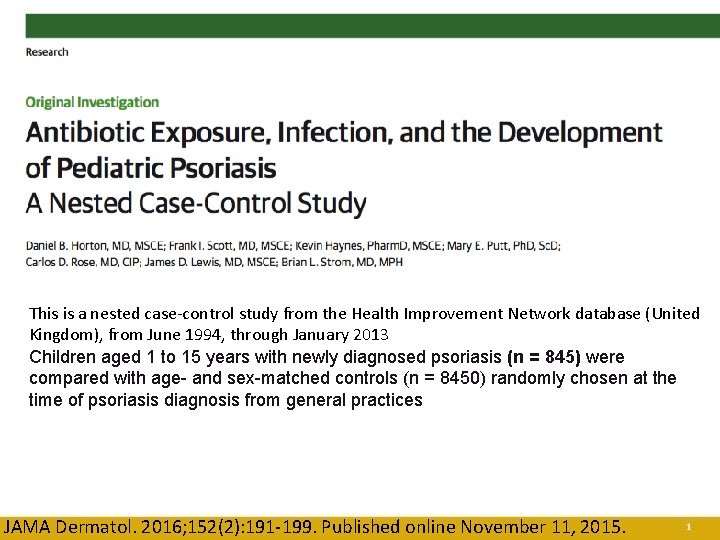
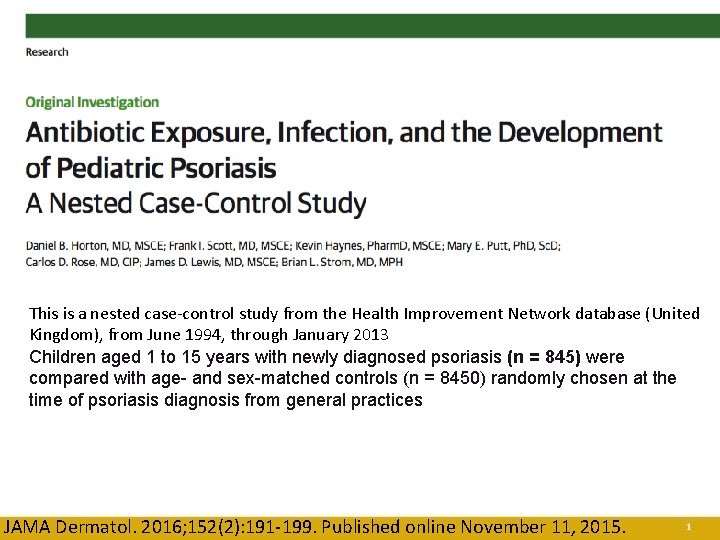
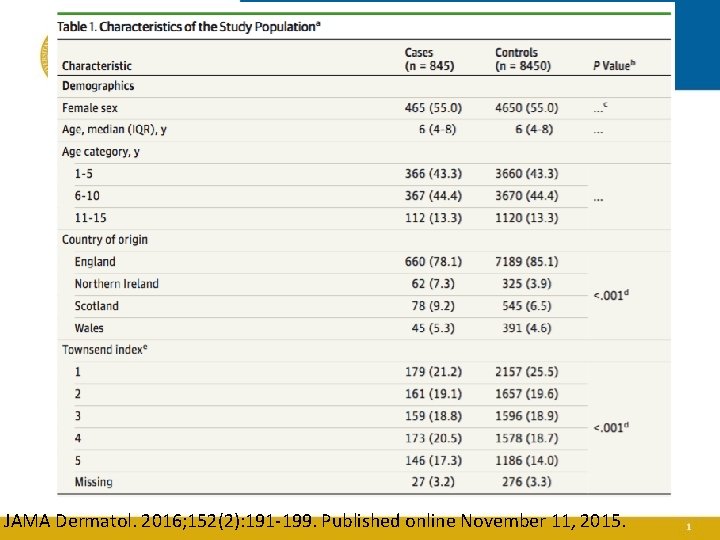
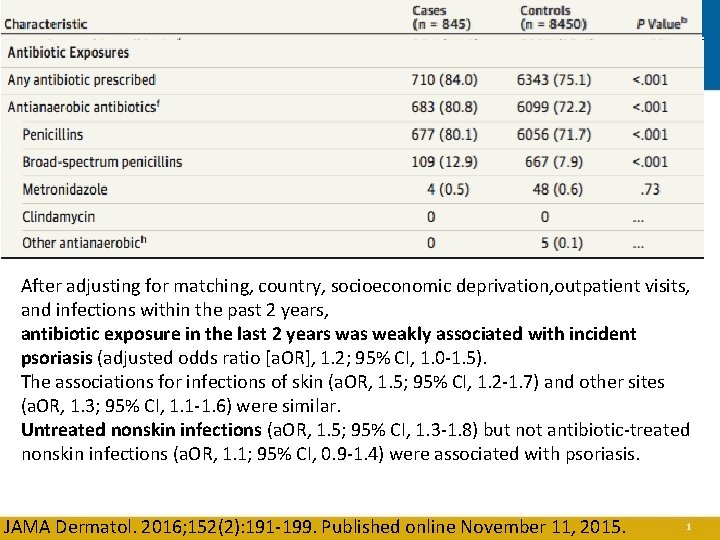
This is a nested case-control study from the Health Improvement Network database (United Kingdom), from June 1994, through January 2013 Children aged 1 to 15 years with newly diagnosed psoriasis (n = 845) were compared with age- and sex-matched controls (n = 8450) randomly chosen at the time of psoriasis diagnosis from general practices JAMA Dermatol. 2016; 152(2): 191 -199. Published online November 11, 2015.
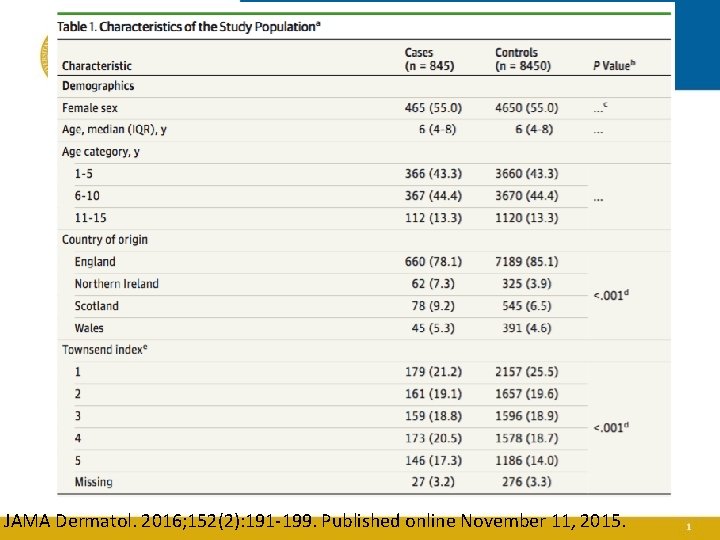
JAMA Dermatol. 2016; 152(2): 191 -199. Published online November 11, 2015.
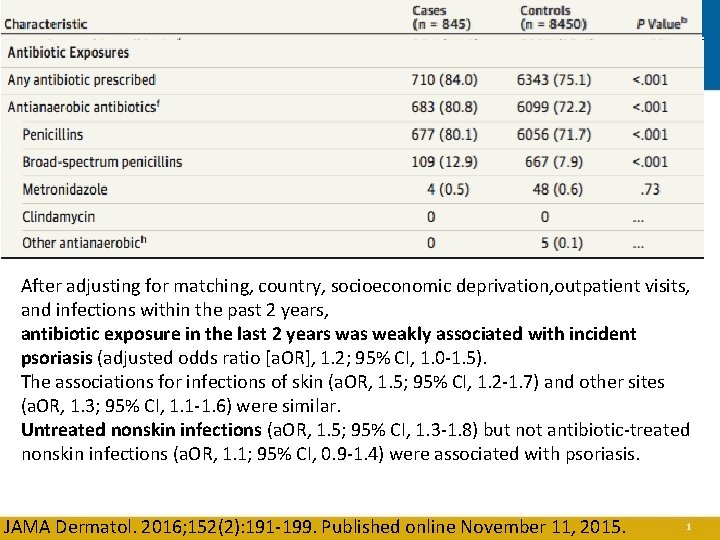
After adjusting for matching, country, socioeconomic deprivation, outpatient visits, and infections within the past 2 years, antibiotic exposure in the last 2 years was weakly associated with incident psoriasis (adjusted odds ratio [a. OR], 1. 2; 95% CI, 1. 0 -1. 5). The associations for infections of skin (a. OR, 1. 5; 95% CI, 1. 2 -1. 7) and other sites (a. OR, 1. 3; 95% CI, 1. 1 -1. 6) were similar. Untreated nonskin infections (a. OR, 1. 5; 95% CI, 1. 3 -1. 8) but not antibiotic-treated nonskin infections (a. OR, 1. 1; 95% CI, 0. 9 -1. 4) were associated with psoriasis. JAMA Dermatol. 2016; 152(2): 191 -199. Published online November 11, 2015.
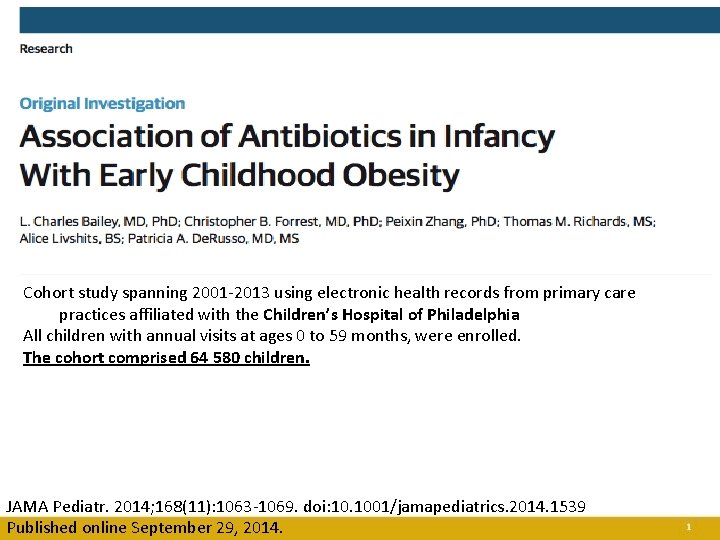
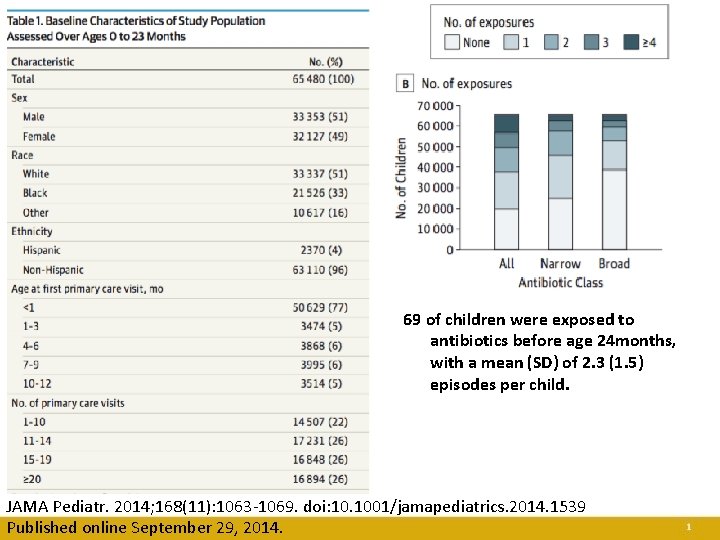
Cohort study spanning 2001 -2013 using electronic health records from primary care practices affiliated with the Children’s Hospital of Philadelphia All children with annual visits at ages 0 to 59 months, were enrolled. The cohort comprised 64 580 children. JAMA Pediatr. 2014; 168(11): 1063 -1069. doi: 10. 1001/jamapediatrics. 2014. 1539 Published online September 29, 2014.
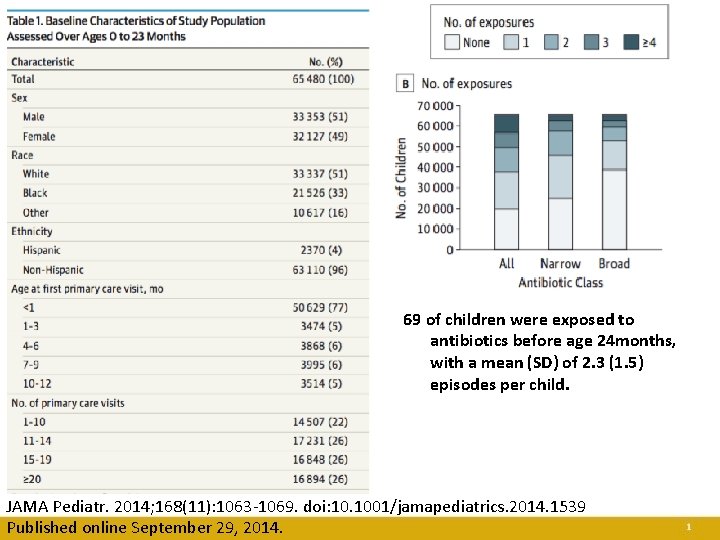
69 of children were exposed to antibiotics before age 24 months, with a mean (SD) of 2. 3 (1. 5) episodes per child. JAMA Pediatr. 2014; 168(11): 1063 -1069. doi: 10. 1001/jamapediatrics. 2014. 1539 Published online September 29, 2014.
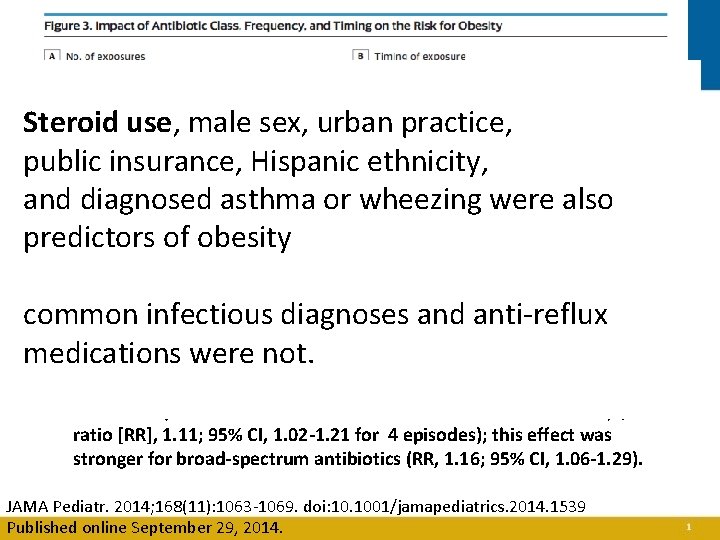
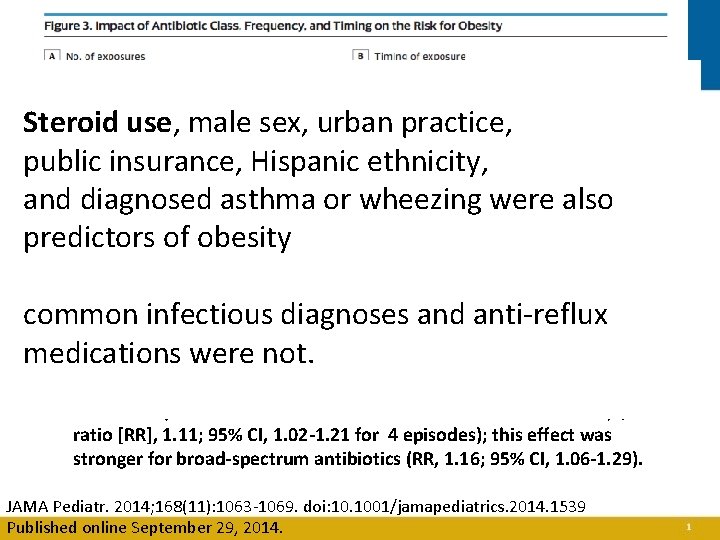
Steroid use, male sex, urban practice, public insurance, Hispanic ethnicity, and diagnosed asthma or wheezing were also predictors of obesity common infectious diagnoses and anti-reflux medications were not. Cumulative exposure to antibiotics was associated with later obesity (rate ratio [RR], 1. 11; 95% CI, 1. 02 -1. 21 for 4 episodes); this effect was stronger for broad-spectrum antibiotics (RR, 1. 16; 95% CI, 1. 06 -1. 29). JAMA Pediatr. 2014; 168(11): 1063 -1069. doi: 10. 1001/jamapediatrics. 2014. 1539 Published online September 29, 2014.


FMT “BLOOMING”
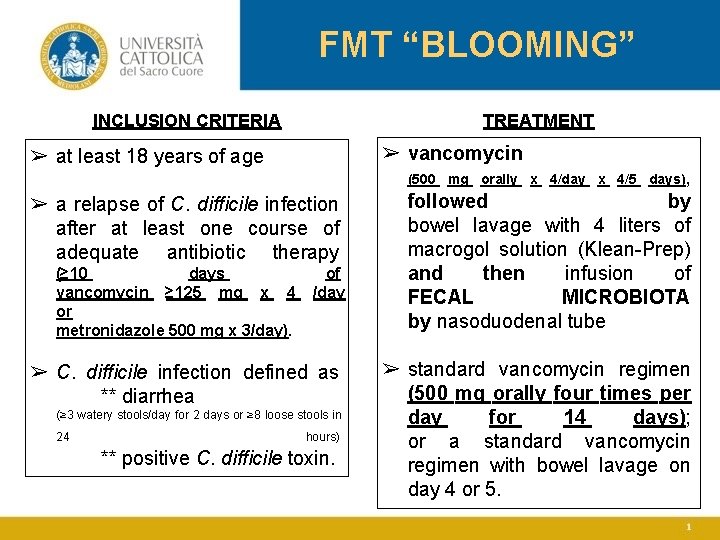
FMT “BLOOMING” INCLUSION CRITERIA TREATMENT ➢ vancomycin ➢ at least 18 years of age (500 mg orally x 4/day x 4/5 days), ➢ a relapse of C. difficile infection after at least one course of adequate antibiotic therapy (≥ 10 days vancomycin ≥ 125 mg x 4 or metronidazole 500 mg x 3/day). of /day ➢ C. difficile infection defined as ** diarrhea (≥ 3 watery stools/day for 2 days or ≥ 8 loose stools in 24 hours) ** positive C. difficile toxin. followed by bowel lavage with 4 liters of macrogol solution (Klean-Prep) and then infusion of FECAL MICROBIOTA by nasoduodenal tube ➢ standard vancomycin regimen (500 mg orally four times per day for 14 days); or a standard vancomycin regimen with bowel lavage on day 4 or 5.
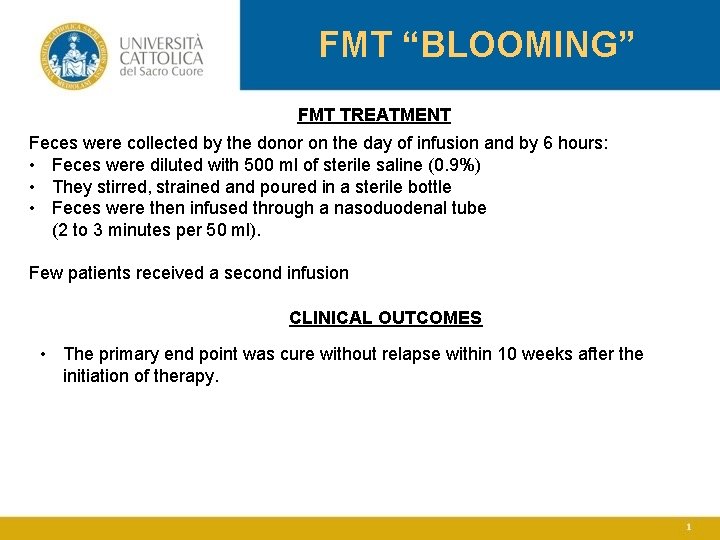
FMT “BLOOMING” FMT TREATMENT Feces were collected by the donor on the day of infusion and by 6 hours: • Feces were diluted with 500 ml of sterile saline (0. 9%) • They stirred, strained and poured in a sterile bottle • Feces were then infused through a nasoduodenal tube (2 to 3 minutes per 50 ml). Few patients received a second infusion CLINICAL OUTCOMES • The primary end point was cure without relapse within 10 weeks after the initiation of therapy.
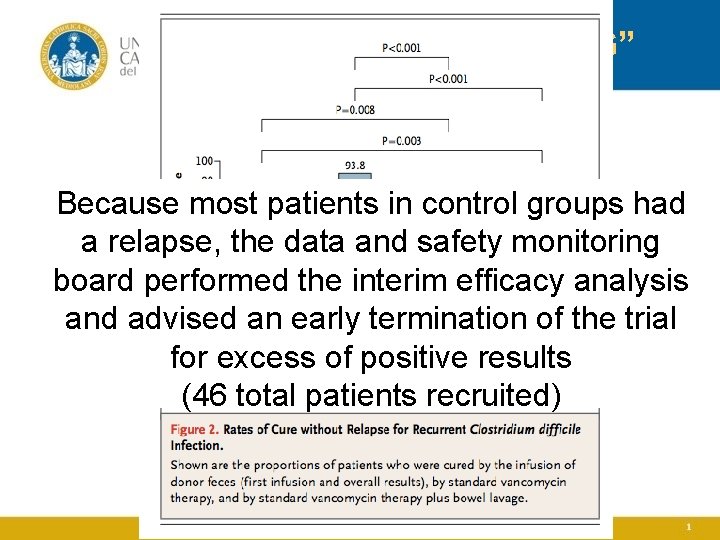
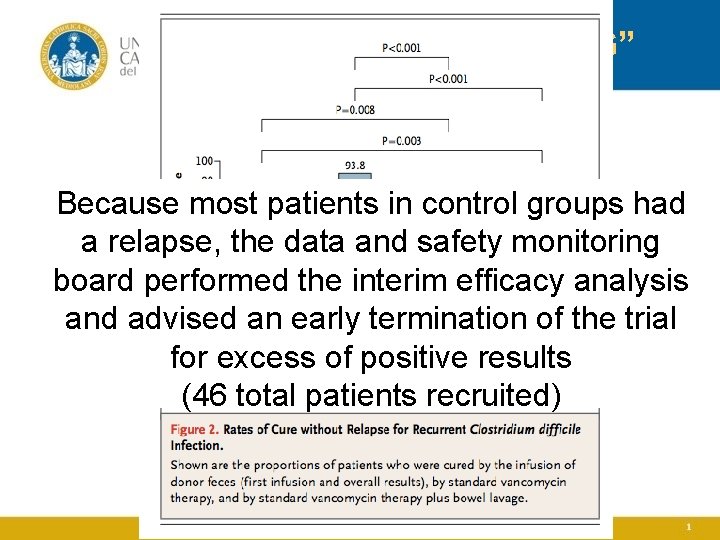
FMT “BLOOMING” Because most patients in control groups had a relapse, the data and safety monitoring board performed the interim efficacy analysis and advised an early termination of the trial for excess of positive results (46 total patients recruited)
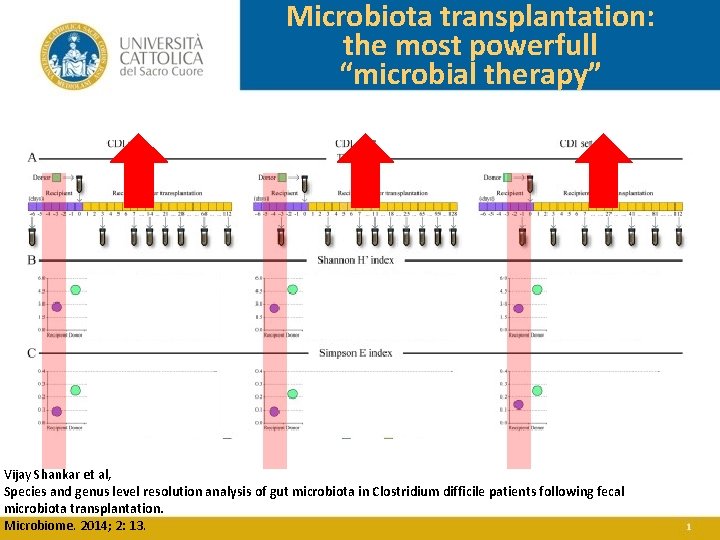
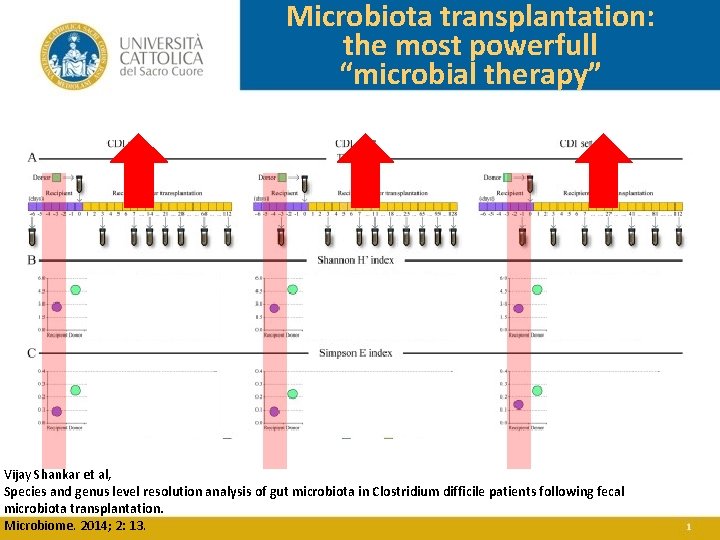
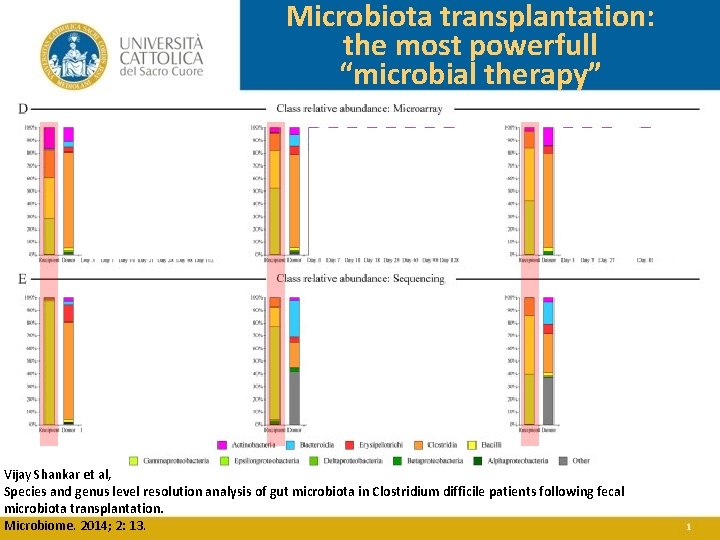
Microbiota transplantation: the most powerfull “microbial therapy” Vijay Shankar et al, Species and genus level resolution analysis of gut microbiota in Clostridium difficile patients following fecal microbiota transplantation. Microbiome. 2014; 2: 13.
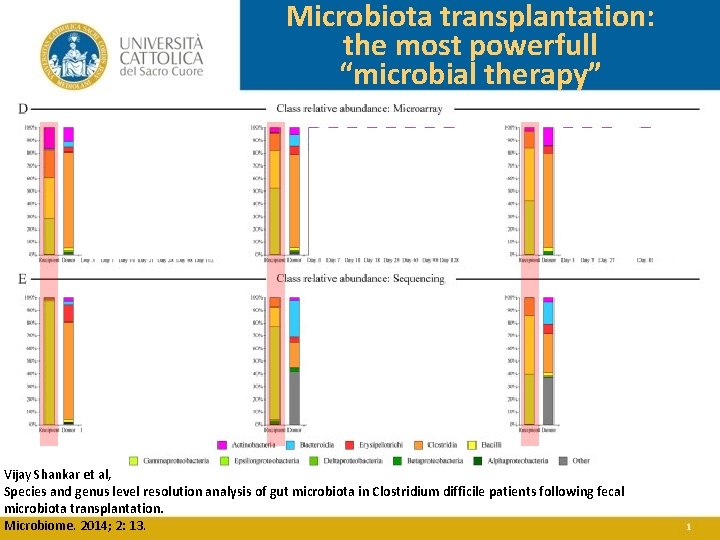
Microbiota transplantation: the most powerfull “microbial therapy” Vijay Shankar et al, Species and genus level resolution analysis of gut microbiota in Clostridium difficile patients following fecal microbiota transplantation. Microbiome. 2014; 2: 13.
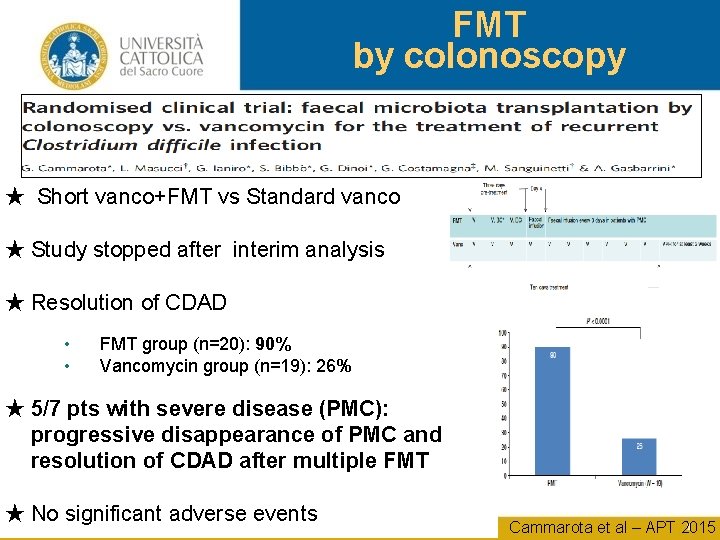
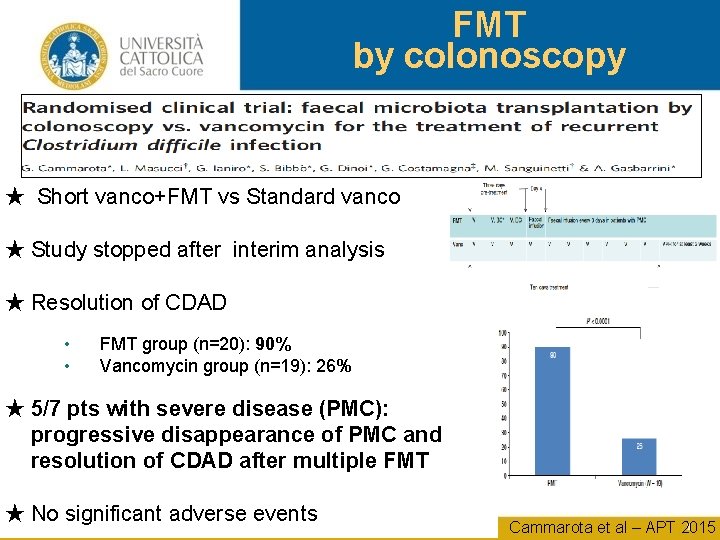
FMT by colonoscopy ★ Short vanco+FMT vs Standard vanco ★ Study stopped after interim analysis ★ Resolution of CDAD • • FMT group (n=20): 90% Vancomycin group (n=19): 26% ★ 5/7 pts with severe disease (PMC): progressive disappearance of PMC and resolution of CDAD after multiple FMT ★ No significant adverse events Cammarota et al – APT 2015
Fecal Microbiota Transplantation - FMT - In pediatrics? ?
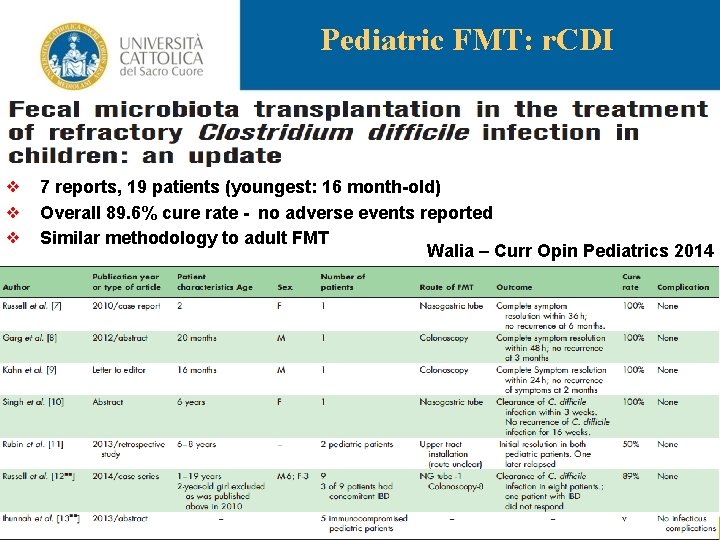
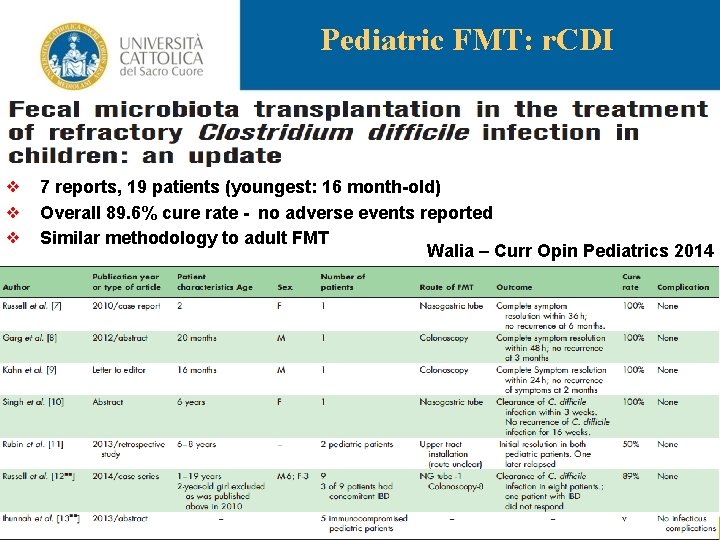
Pediatric FMT: r. CDI ❖ 7 reports, 19 patients (youngest: 16 month-old) ❖ Overall 89. 6% cure rate - no adverse events reported ❖ Similar methodology to adult FMT Walia – Curr Opin Pediatrics 2014
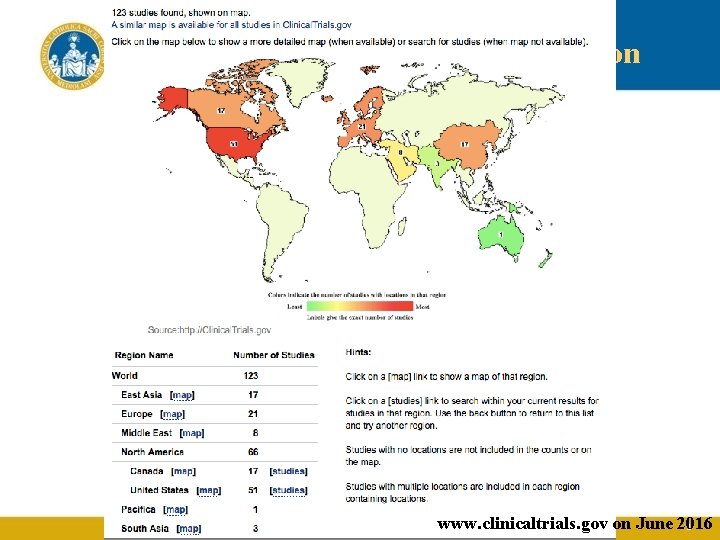
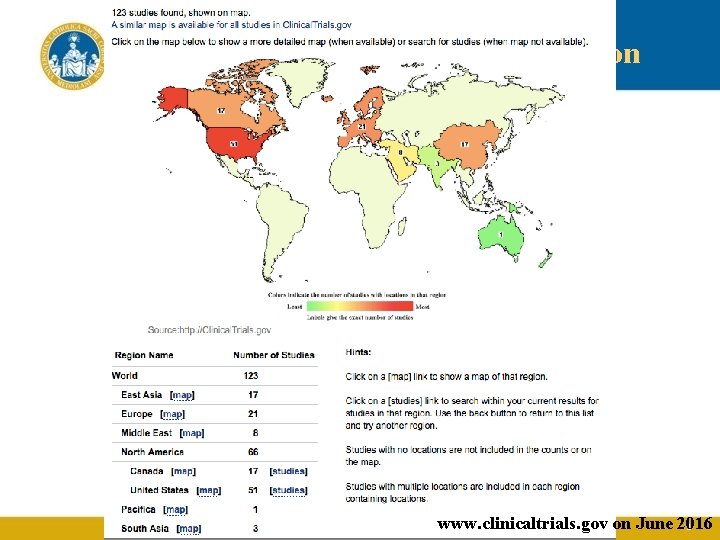
Clinical Trials for fecal-M transplantation www. clinicaltrials. gov on June 2016
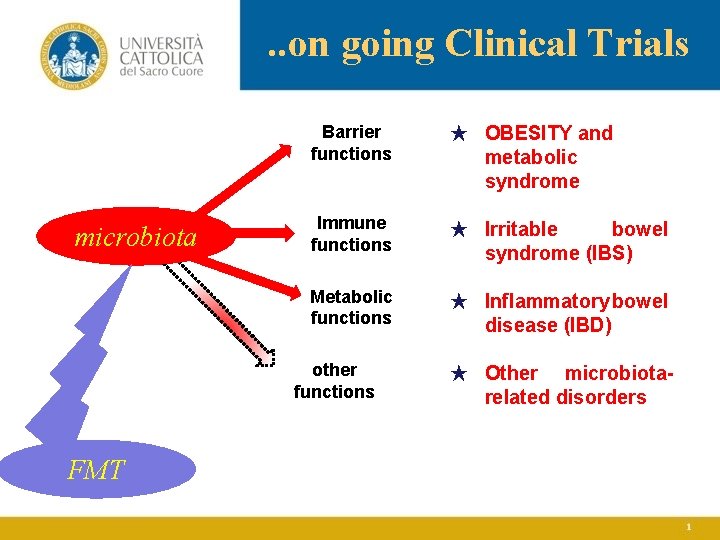
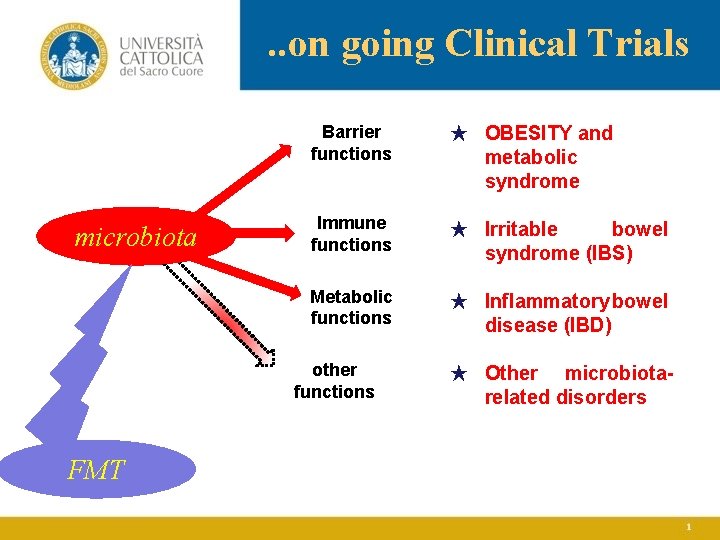
. . on going Clinical Trials microbiota Barrier functions ★ OBESITY and metabolic syndrome Immune functions ★ Irritable bowel syndrome (IBS) Metabolic functions ★ Inflammatory bowel disease (IBD) other functions FMT ★ Other microbiotarelated disorders
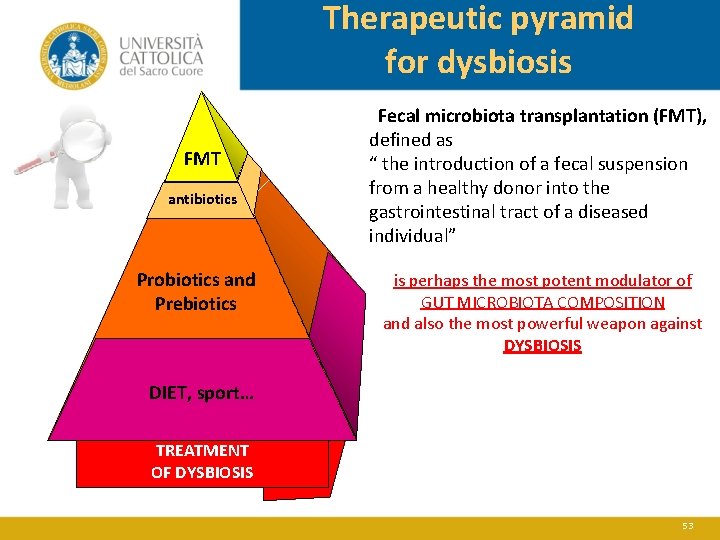
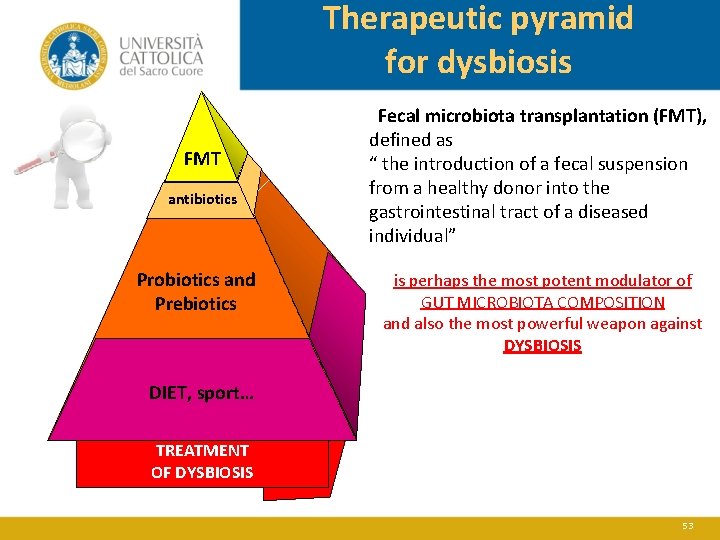
Therapeutic pyramid for dysbiosis FMT antibiotics Probiotics and Prebiotics Fecal microbiota transplantation (FMT), defined as “ the introduction of a fecal suspension from a healthy donor into the gastrointestinal tract of a diseased individual” is perhaps the most potent modulator of GUT MICROBIOTA COMPOSITION and also the most powerful weapon against DYSBIOSIS DIET, sport… TREATMENT OF DYSBIOSIS 53
Probiotics: definitions “Microorganisms that, when administrered in adequate amounts, confer health benefit to the host, expecially by improving intestinal microbial balance”. FAO/WHO. Joint FAO/WHO Working Group Report on Drafting Guidelines for the evaluation of Probiotics in Food (FAO/WHO, London, Canada, 2002). FAO/WHO. Probiotics in food. Health and nutritional properties and guidelines for evaluation. En “FAO Food and Nutrition Paper 85”, 2006, ISBN 92 -5 -105513 -0. Available at: ftp: //ftp. fao. org/docrep/fao/009/a 0512 e 00. pdf.
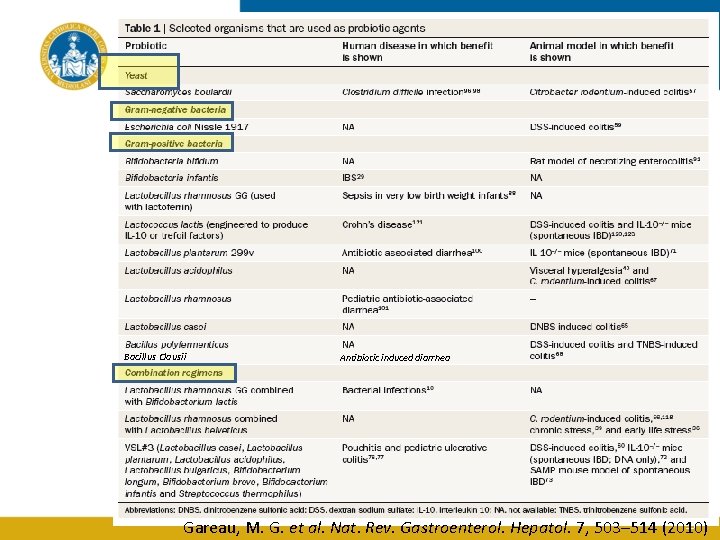
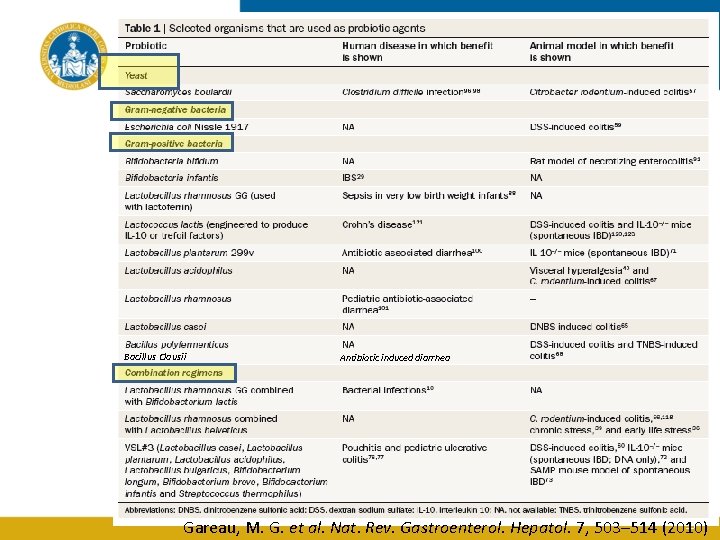
Bacillus Clausii Antibiotic induced diarrhea 55 Gareau, M. G. et al. Nat. Rev. Gastroenterol. Hepatol. 7, 503– 514 (2010)
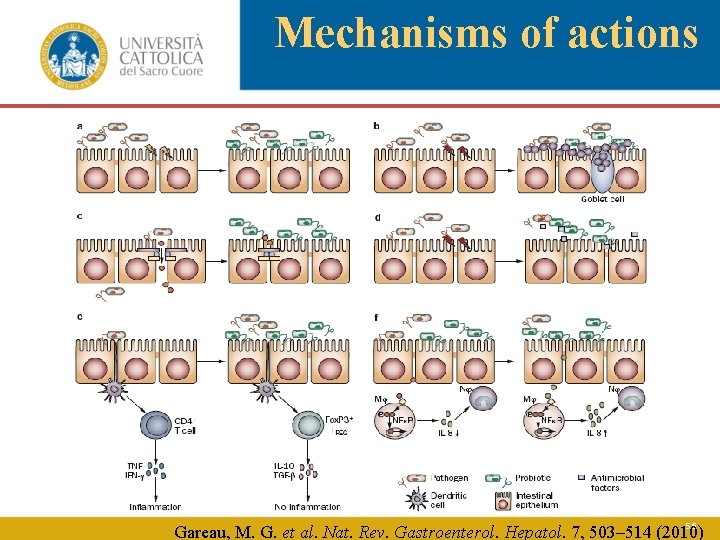
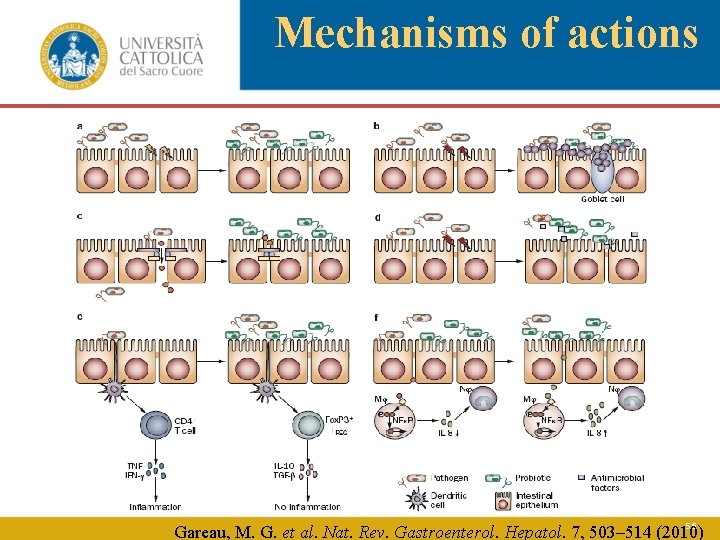
Mechanisms of actions 56 Gareau, M. G. et al. Nat. Rev. Gastroenterol. Hepatol. 7, 503– 514 (2010)
MODULATE GUT MICROBIOTA COMPOSITION? ? ? 57
Results from a preclinical study “Clausii in colitis: role and mechanisms of action of Bacillus clausii in experimental colitis” Franco Scaldaferri 1, Cristina Graziani 1, Valentina Petito 1 -3, Loris Riccardo Lopetuso 1, Gianluca Quaranta 2, Luca Masucci 2, Francesco Franceschi 1, Andrea Poscia 3, Vincenzo Arena 3, Domenico Scannone 3, Gianluca Ianiro 1, Giovanni Cammarota 1, Alessandro Sgambato 5 and Antonio Gasbarrini 1 1 ISTITUTO DI PATOLOGIA SPECIALE MEDICA, Università Cattolica del Sacro Cuore, L. go Gemelli 8, 00168 Rome, Italy 2 ISTITUTO DI MICROBIOLOGIA, Università Cattolica del Sacro Cuore, L. go Gemelli 8, 00168 Rome, Italy 3 ISTITUTO DI IGIENE, Università Cattolica del Sacro Cuore, L. go Gemelli 8, 00168 Rome, Italy 3 ISTITUTO ANATOMIA PATOLOGICA, Università Cattolica del Sacro Cuore, L. go Gemelli 8, 00168 Rome, Italy 4 ISTITUTO DI PATOLOGIA GENERALE, Università Cattolica del Sacro Cuore, L. go Gemelli 8, 00168 Rome, Italy SCALDAFERRI F ET AL, UEGW 2016, SIMI 2016, EHMSG 2016
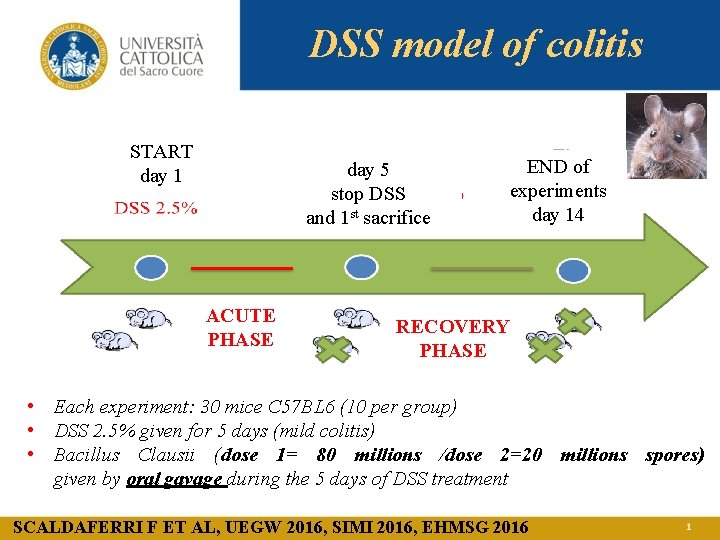
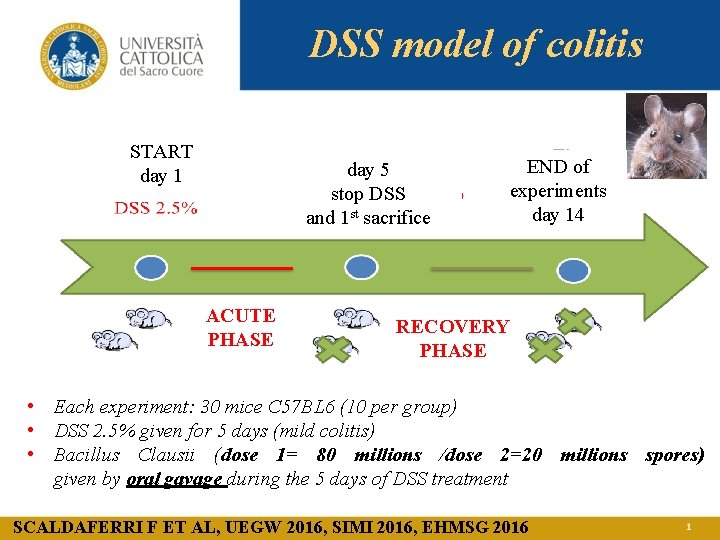
DSS model of colitis START day 1 day 5 stop DSS and 1 st sacrifice ACUTE PHASE END of experiments day 14 RECOVERY PHASE • Each experiment: 30 mice C 57 BL 6 (10 per group) • DSS 2. 5% given for 5 days (mild colitis) • Bacillus Clausii (dose 1= 80 millions /dose 2=20 millions spores) given by oral gavage during the 5 days of DSS treatment SCALDAFERRI F ET AL, UEGW 2016, SIMI 2016, EHMSG 2016
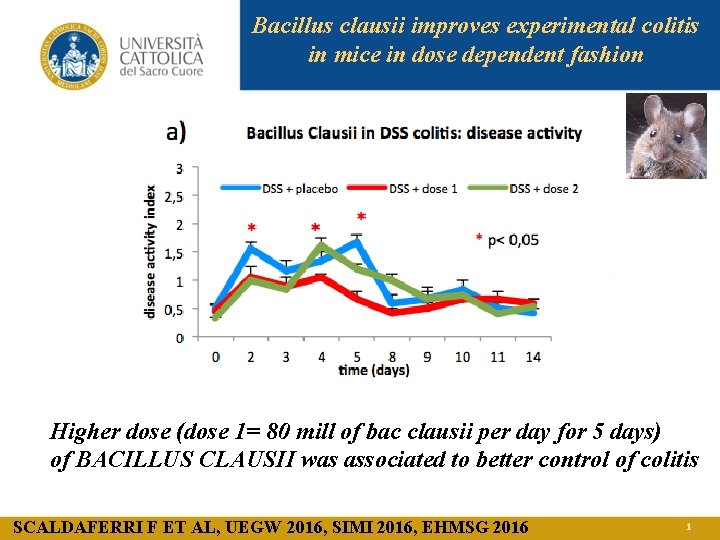
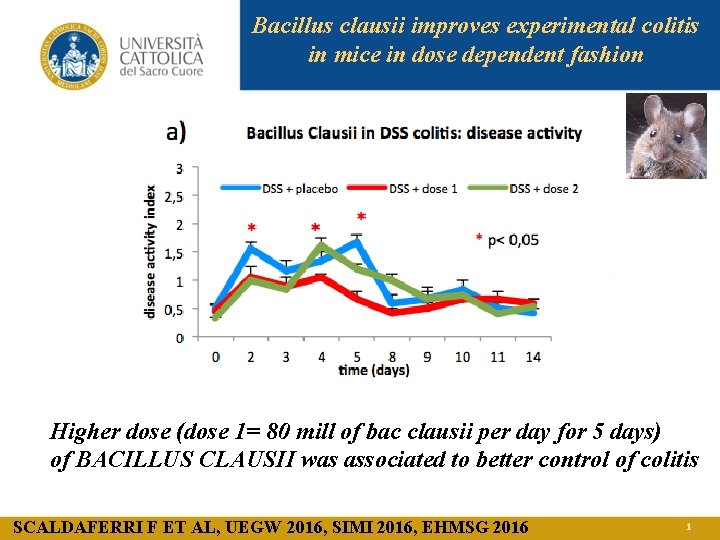
Bacillus clausii improves experimental colitis in mice in dose dependent fashion Higher dose (dose 1= 80 mill of bac clausii per day for 5 days) of BACILLUS CLAUSII was associated to better control of colitis SCALDAFERRI F ET AL, UEGW 2016, SIMI 2016, EHMSG 2016
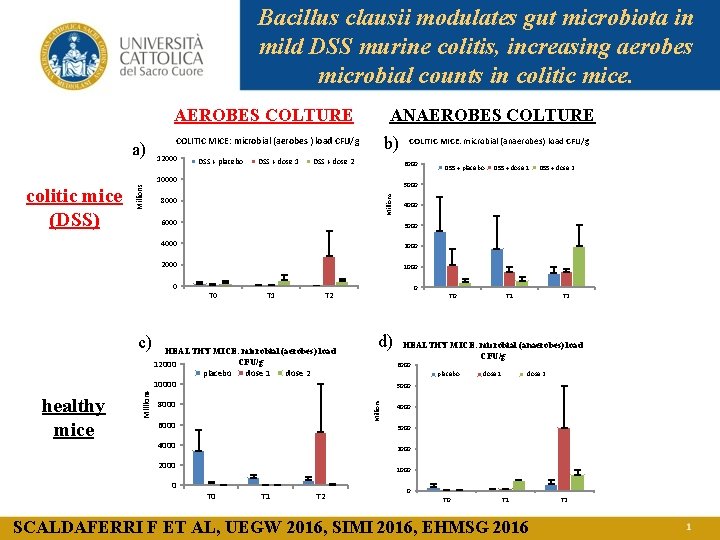
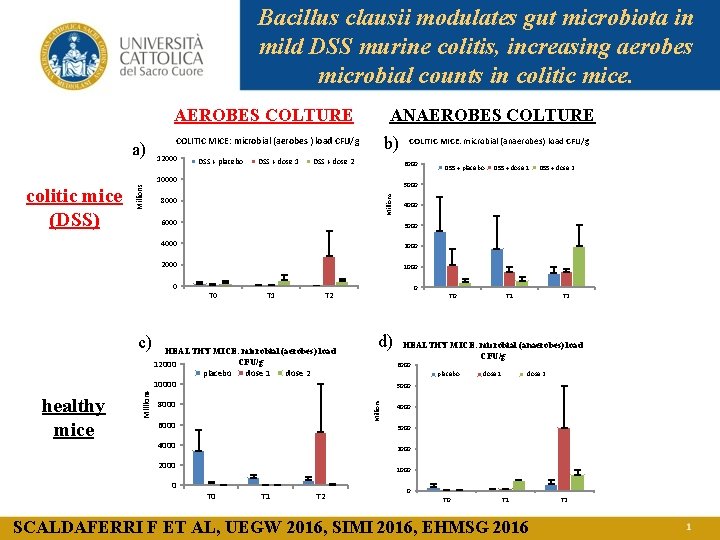
Bacillus clausii modulates gut microbiota in mild DSS murine colitis, increasing aerobes microbial counts in colitic mice. AEROBES COLTURE a) ANAEROBES COLTURE b) COLITIC MICE: microbial (aerobes ) load CFU/g 12000 DSS + placebo DSS + dose 1 DSS + dose 2 6000 8000 6000 3000 4000 2000 1000 T 1 HEALTHY MICE: microbial (aerobes) load CFU/g 12000 placebo dose 1 dose 2 10000 8000 6000 T 0 d) T 1 T 2 HEALTHY MICE: microbial (anaerobes) load CFU/g 6000 placebo dose 1 dose 2 5000 4000 3000 4000 2000 1000 0 DSS + dose 2 0 T 2 Millions healthy mice DSS + dose 1 4000 0 c) DSS + placebo 5000 Millions 10000 colitic mice (DSS) COLITIC MICE: microbial (anaerobes) load CFU/g T 0 T 1 T 2 0 T 1 SCALDAFERRI F ET AL, UEGW 2016, SIMI 2016, EHMSG 2016 T 2
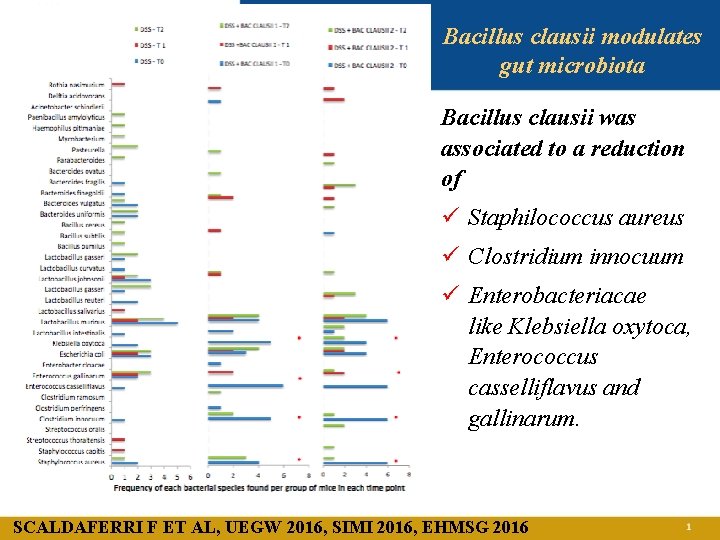
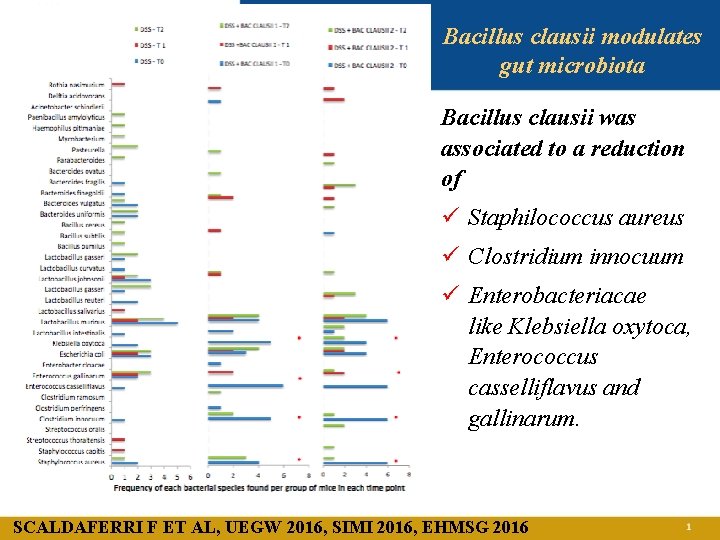
Bacillus clausii modulates gut microbiota Bacillus clausii was associated to a reduction of ü Staphilococcus aureus ü Clostridium innocuum ü Enterobacteriacae like Klebsiella oxytoca, Enterococcus casselliflavus and gallinarum. SCALDAFERRI F ET AL, UEGW 2016, SIMI 2016, EHMSG 2016

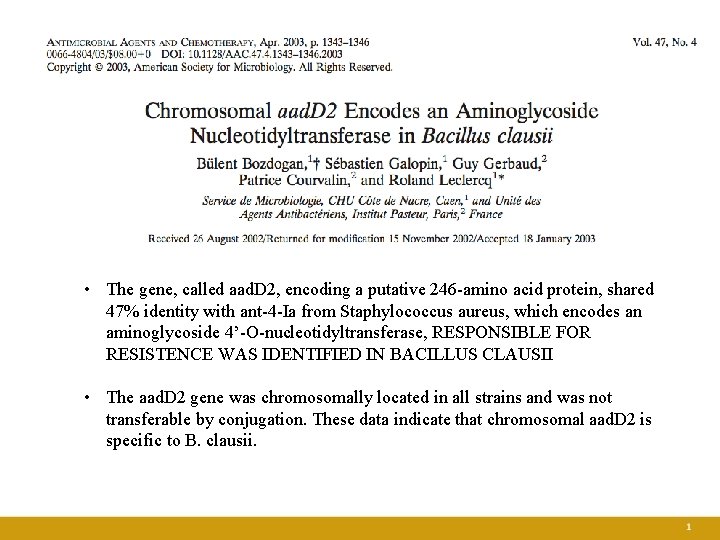
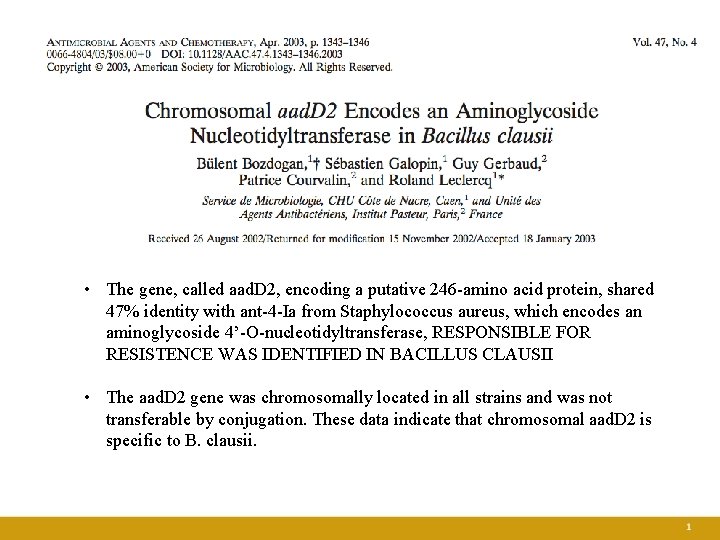
• The gene, called aad. D 2, encoding a putative 246 -amino acid protein, shared 47% identity with ant-4 -Ia from Staphylococcus aureus, which encodes an aminoglycoside 4’-O-nucleotidyltransferase, RESPONSIBLE FOR RESISTENCE WAS IDENTIFIED IN BACILLUS CLAUSII • The aad. D 2 gene was chromosomally located in all strains and was not transferable by conjugation. These data indicate that chromosomal aad. D 2 is specific to B. clausii.
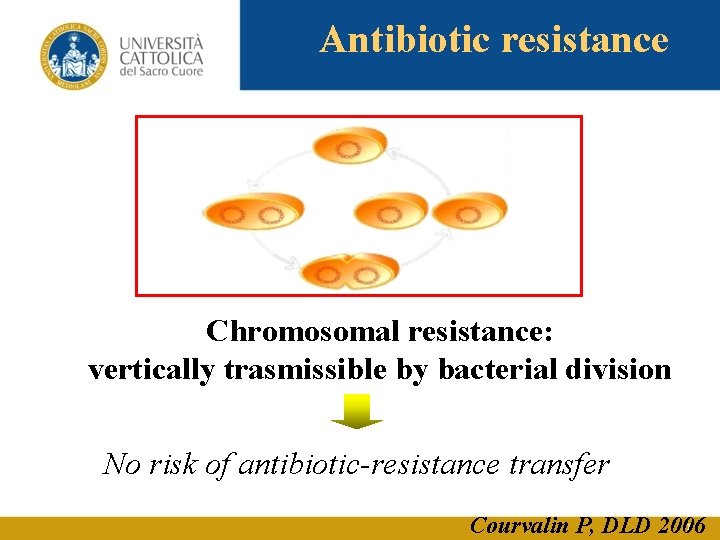
Antibiotic resistance Chromosomal resistance: vertically trasmissible by bacterial division No risk of antibiotic-resistance transfer Courvalin P, DLD 2006
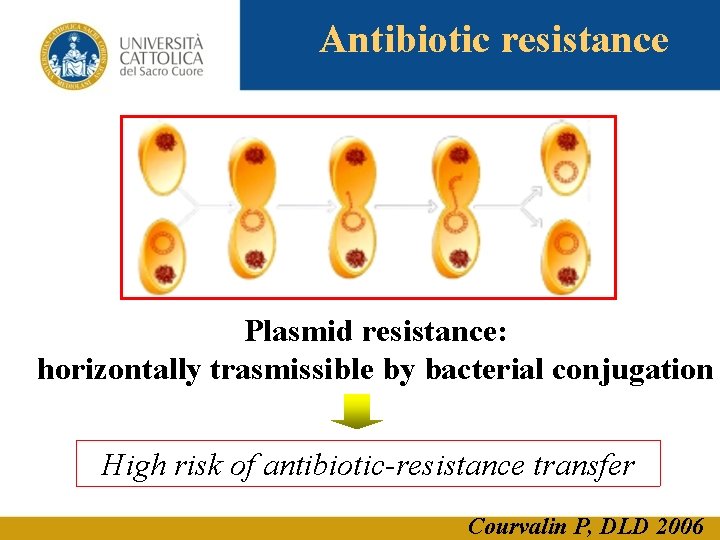
Antibiotic resistance Plasmid resistance: horizontally trasmissible by bacterial conjugation High risk of antibiotic-resistance transfer Courvalin P, DLD 2006
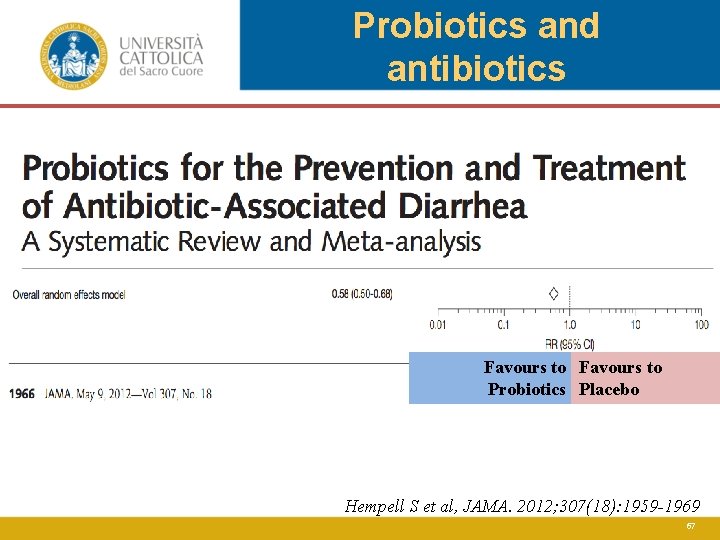
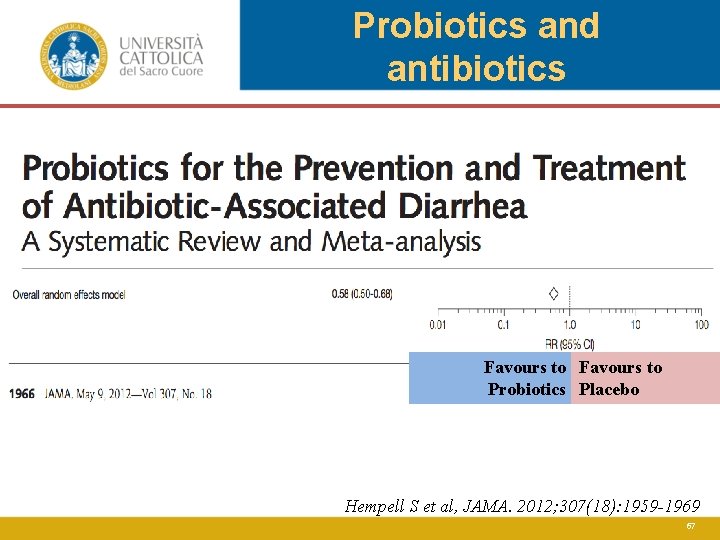
Probiotics and antibiotics Favours to Probiotics Placebo Hempell S et al, JAMA. 2012; 307(18): 1959 -1969 67
Review Team Francisco Guarner (Chair, Spain) Aamir G. Khan (Pakistan) James Garisch (South Africa) Rami Eliakim (Israel) Alfred Gangl (Austria) Alan Thomson (Canada) Justus Krabshuis (France) Ton Lemair (The Netherlands) Invited outside experts Pedro Kaufmann (Uruguay) Juan Andres de Paula (Argentina) Richard Fedorak (Canada) Fergus Shanahan (Ireland) Mary Ellen Sanders (USA) Hania Szajewska (Poland) B. S. Ramakrishna (India) Tarkan Karakan (Turkey) Nayoung Kim (South Korea) WGO: World Gastroenterology Organisation WGO, 2011 68
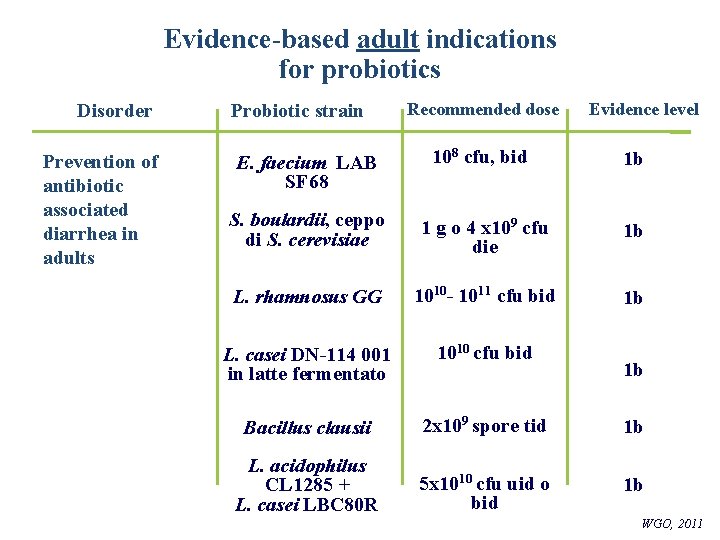
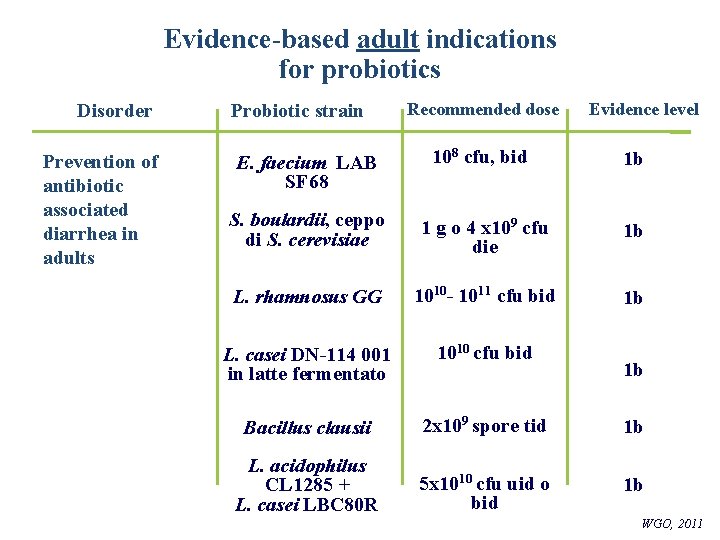
Evidence-based adult indications for probiotics Disorder Prevention of antibiotic associated diarrhea in adults Probiotic strain Evidence level E. faecium LAB SF 68 108 cfu, bid 1 b S. boulardii, ceppo di S. cerevisiae 1 g o 4 x 109 cfu die 1 b L. rhamnosus GG 1010 - 1011 cfu bid 1 b L. casei DN-114 001 in latte fermentato 1010 cfu bid Bacillus clausii 2 x 109 spore tid 1 b 5 x 1010 cfu uid o bid 1 b L. acidophilus CL 1285 + L. casei LBC 80 R WGO: Organizzazione Mondiale di Gastroenterologia Cfu: unità formanti colonie Recommended dose 1 b WGO, 2011
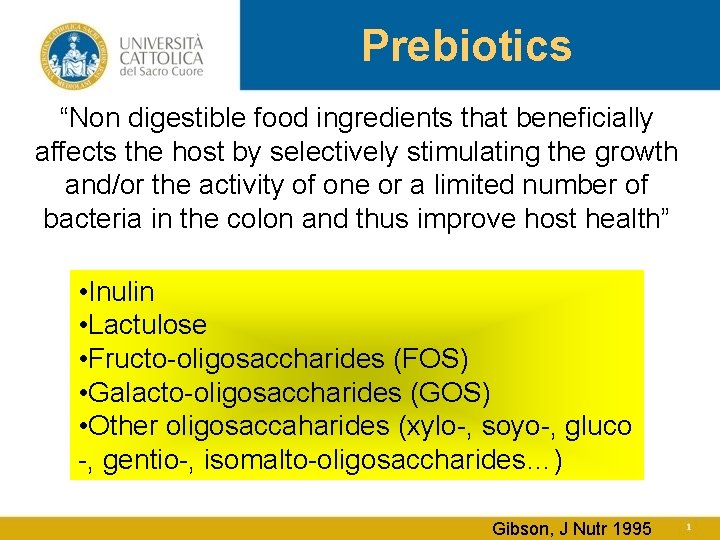
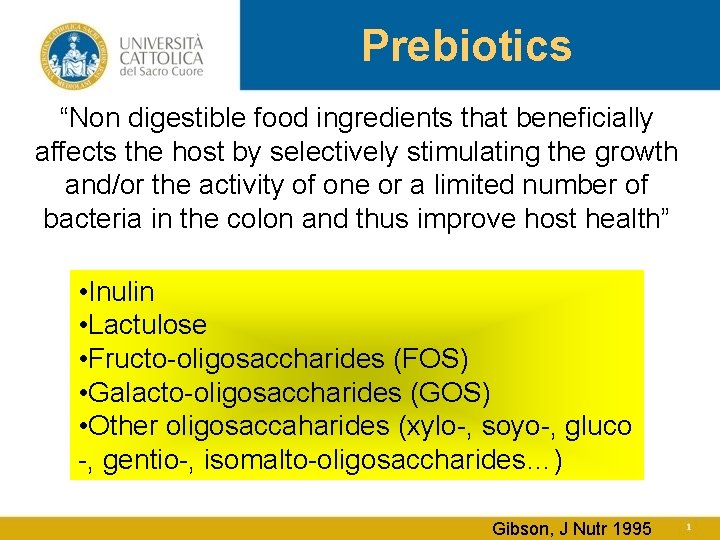
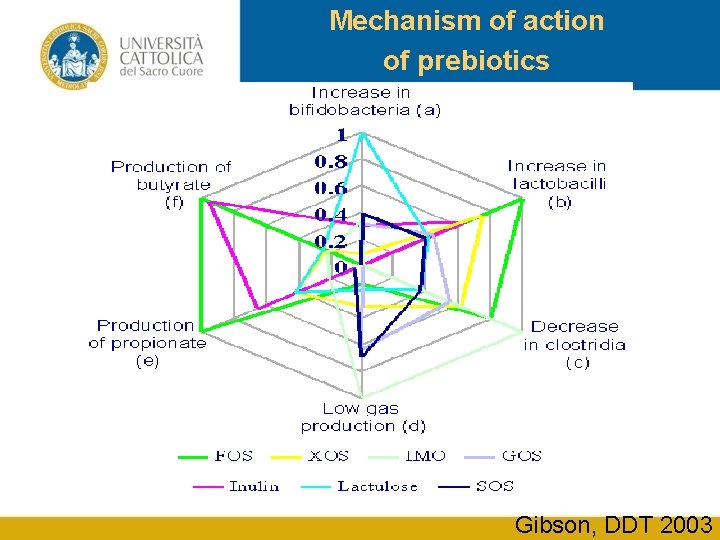
Prebiotics “Non digestible food ingredients that beneficially affects the host by selectively stimulating the growth and/or the activity of one or a limited number of bacteria in the colon and thus improve host health” • Inulin • Lactulose • Fructo-oligosaccharides (FOS) • Galacto-oligosaccharides (GOS) • Other oligosaccaharides (xylo-, soyo-, gluco -, gentio-, isomalto-oligosaccharides…) Gibson, J Nutr 1995
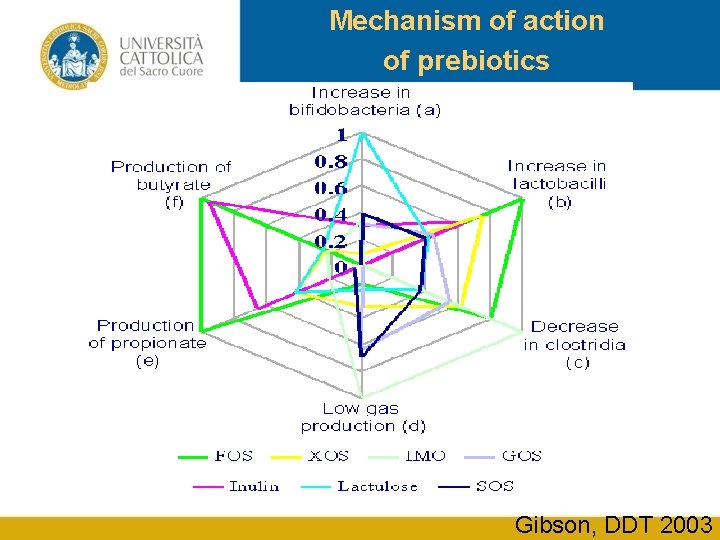
Mechanism of action of prebiotics Gibson, DDT 2003
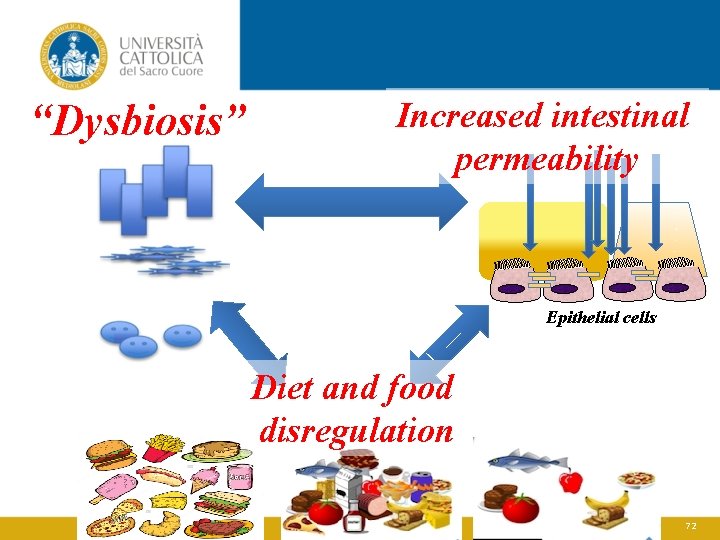
“Dysbiosis” Increased intestinal permeability Epithelial cells Diet and food disregulation 72
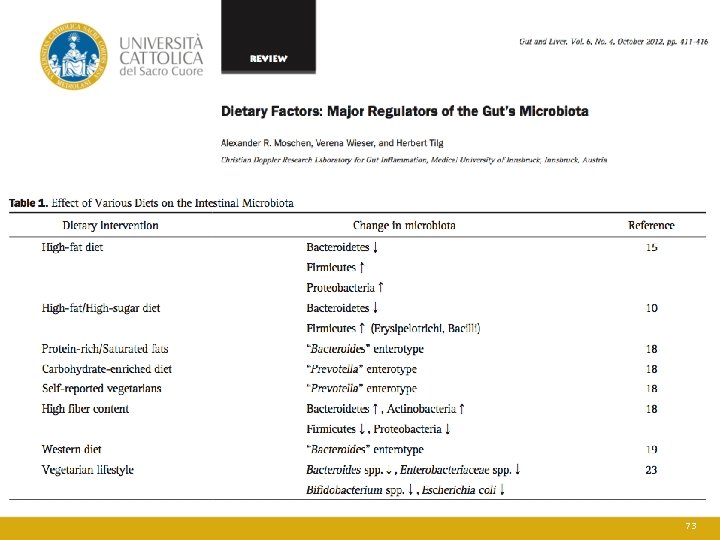
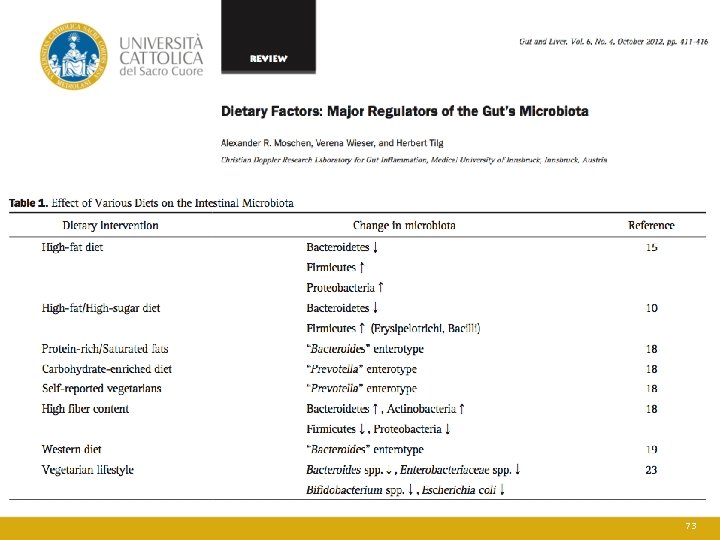
73
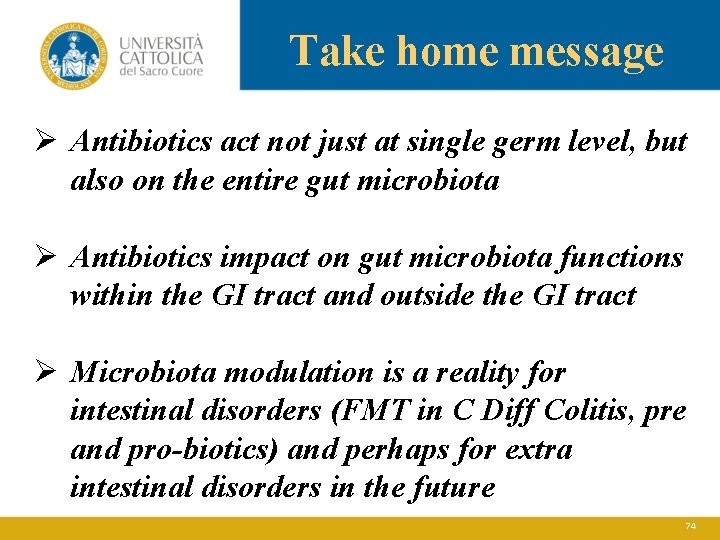
Take home message Ø Antibiotics act not just at single germ level, but also on the entire gut microbiota Ø Antibiotics impact on gut microbiota functions within the GI tract and outside the GI tract Ø Microbiota modulation is a reality for intestinal disorders (FMT in C Diff Colitis, pre and pro-biotics) and perhaps for extra intestinal disorders in the future 74

April 2017 75
 Oratorio sacro cuore cislago
Oratorio sacro cuore cislago Sacro cuore negrar
Sacro cuore negrar Coroncina al sacro cuore di gesù come si recita
Coroncina al sacro cuore di gesù come si recita Istituto salesiano sacro cuore napoli
Istituto salesiano sacro cuore napoli Sacro cuore don calabria
Sacro cuore don calabria Chiesa sacro cuore eboli
Chiesa sacro cuore eboli Facoltà di medicina cagliari
Facoltà di medicina cagliari Facolta di medicina messina
Facolta di medicina messina Il cuore parla al cuore significato
Il cuore parla al cuore significato Escotadura esternal
Escotadura esternal Quando si e stanchi si acuiscono
Quando si e stanchi si acuiscono Facoltà ingegneria trento
Facoltà ingegneria trento Facoltà di farmacia siena
Facoltà di farmacia siena Kiro chimica unipv
Kiro chimica unipv Facoltà di architettura firenze
Facoltà di architettura firenze Religione costituzione italiana
Religione costituzione italiana Azione cattolica otranto
Azione cattolica otranto Cattolica scienze infermieristiche
Cattolica scienze infermieristiche Progetto alternativo alla religione cattolica
Progetto alternativo alla religione cattolica Missione cattolica italiana berna
Missione cattolica italiana berna Uscire dalla chiesa cattolica
Uscire dalla chiesa cattolica Azione cattolica vittorio veneto
Azione cattolica vittorio veneto Scienze motorie pisa
Scienze motorie pisa Università san cirillo e metodio skopje
Università san cirillo e metodio skopje Università infermieristica foligno
Università infermieristica foligno Lauree magistrali parthenope
Lauree magistrali parthenope Università degli studi di firenze psicologia
Università degli studi di firenze psicologia Mydesk unife docenti
Mydesk unife docenti Università della terza età fidenza
Università della terza età fidenza Scienze della formazione savigliano
Scienze della formazione savigliano Dipartimento economia genova
Dipartimento economia genova Agraria tolfa
Agraria tolfa Dario bressanini università
Dario bressanini università Università liuc costi
Università liuc costi Il nuovo sistema contabile e di bilancio delle università
Il nuovo sistema contabile e di bilancio delle università Università degli studi roma tre mascotte
Università degli studi roma tre mascotte Kit dello studente erasmus unige
Kit dello studente erasmus unige Mediazione linguistica ragusa piano di studi
Mediazione linguistica ragusa piano di studi Università ecampus fi
Università ecampus fi Università firenze
Università firenze Zoologia università napoli
Zoologia università napoli Dario bressanini università
Dario bressanini università Dario bressanini università
Dario bressanini università Legge del cuore di starling
Legge del cuore di starling 02112009 color
02112009 color Vie di conduzione del cuore
Vie di conduzione del cuore La guarigione del cuore
La guarigione del cuore Pestalozzi educazione del cuore
Pestalozzi educazione del cuore Soffio al cuore cos'è
Soffio al cuore cos'è Fascia pubocervical
Fascia pubocervical Miembro inferior
Miembro inferior Sacro cotyloid diameter
Sacro cotyloid diameter Diametre sacro tibial
Diametre sacro tibial Fossette sacro coccygienne quand s'inquiéter
Fossette sacro coccygienne quand s'inquiéter Tempo sacro
Tempo sacro Fondo vesicouterino
Fondo vesicouterino Diametre promonto sous pubien
Diametre promonto sous pubien Ischion barbu
Ischion barbu 3/4 alaire et 3/4 obturateur
3/4 alaire et 3/4 obturateur Bassin 3/4 alaire
Bassin 3/4 alaire Syndesmophytes
Syndesmophytes Sacro uteriene ligamenten
Sacro uteriene ligamenten Articulaciones de las costillas
Articulaciones de las costillas Mapa conceptual del imperio bizantino
Mapa conceptual del imperio bizantino Rx lombo sacro
Rx lombo sacro Sacro verticalizado
Sacro verticalizado Superior articular facet of axis
Superior articular facet of axis Crisi demografica del 600
Crisi demografica del 600 Biseau crural fauteuil roulant
Biseau crural fauteuil roulant Sacro cardinal vein
Sacro cardinal vein Shintoismo significato
Shintoismo significato Signo de puño percusion renal
Signo de puño percusion renal Sociedad vasca de medicina del trabajo
Sociedad vasca de medicina del trabajo Ti adoro, mio dio, e ti amo con tutto il cuore
Ti adoro, mio dio, e ti amo con tutto il cuore Ti adoro mio dio
Ti adoro mio dio Salmo 45
Salmo 45