UNIT VII Chapter 41 Regulation of Respiration Slides



- Slides: 55
UNIT VII Chapter 41: Regulation of Respiration Slides by Robert L. Hester, Ph. D Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
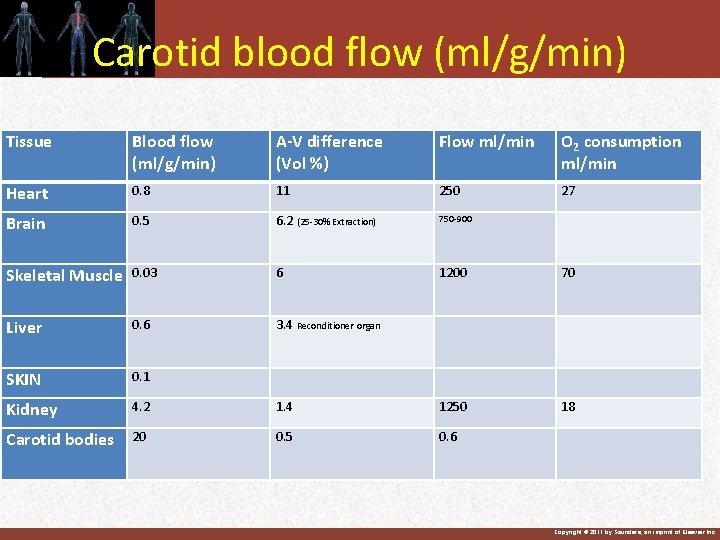
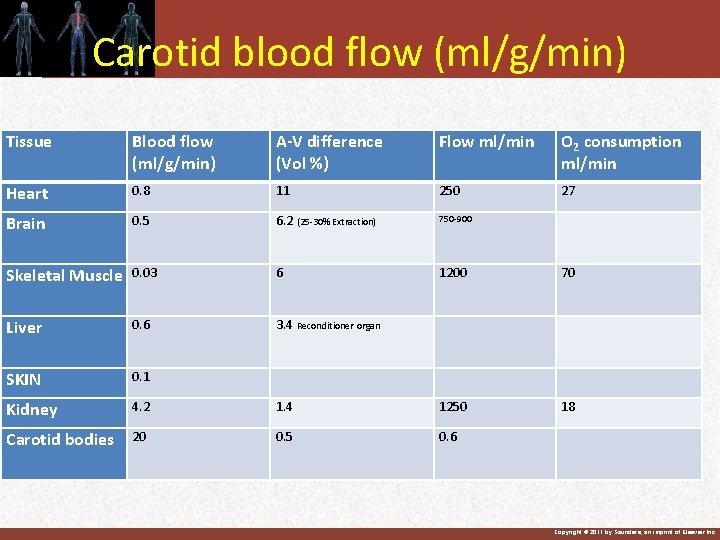
Carotid blood flow (ml/g/min) Tissue Blood flow (ml/g/min) A-V difference (Vol %) Flow ml/min O 2 consumption ml/min Heart 0. 8 11 250 27 Brain 0. 5 6. 2 (25 -30% Extraction) 750 -900 Skeletal Muscle 0. 03 6 1200 70 Liver 0. 6 3. 4 Reconditioner organ SKIN 0. 1 Kidney 4. 2 1. 4 1250 18 Carotid bodies 20 0. 5 0. 6 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
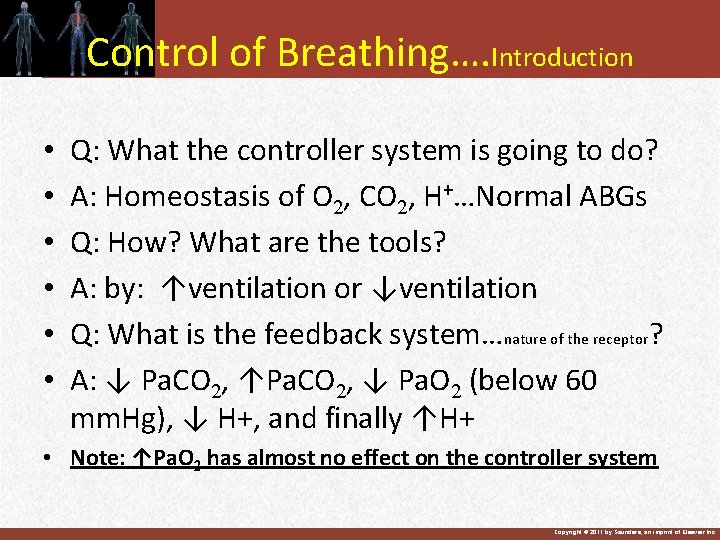
Control of Breathing…. Introduction • • • Q: What the controller system is going to do? A: Homeostasis of O 2, CO 2, H+…Normal ABGs Q: How? What are the tools? A: by: ↑ventilation or ↓ventilation Q: What is the feedback system…nature of the receptor? A: ↓ Pa. CO 2, ↑Pa. CO 2, ↓ Pa. O 2 (below 60 mm. Hg), ↓ H+, and finally ↑H+ • Note: ↑Pa. O 2 has almost no effect on the controller system Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Control Of Breathing …. Introduction • Again: The main goal of the respiratory system is to maintain normal ABGs: O 2, CO 2, and p. H • The controller center receives feedback response from O 2, CO 2, and p. H • What are the tools: Manipulating ventilation • Sensor and response: Peripheral and central nervous system Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
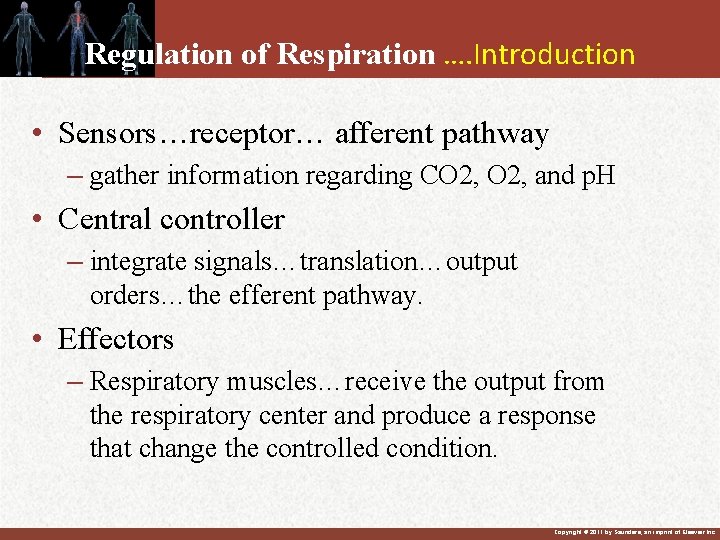
Regulation of Respiration …. Introduction • Sensors…receptor… afferent pathway – gather information regarding CO 2, and p. H • Central controller – integrate signals…translation…output orders…the efferent pathway. • Effectors – Respiratory muscles…receive the output from the respiratory center and produce a response that change the controlled condition. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
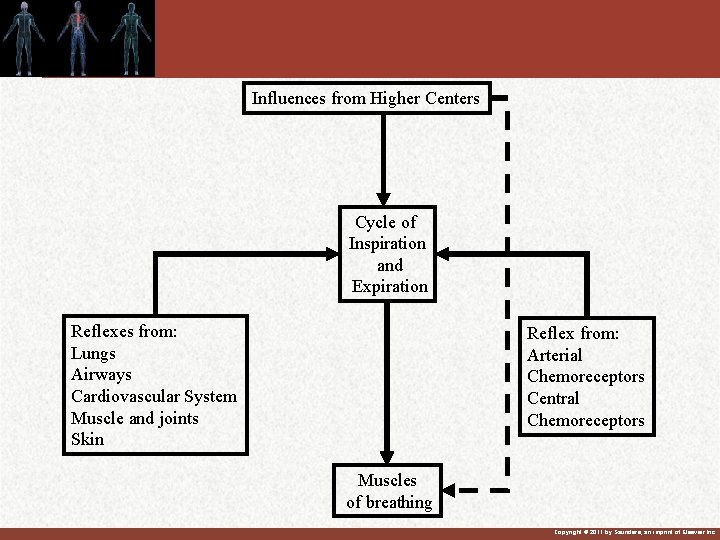
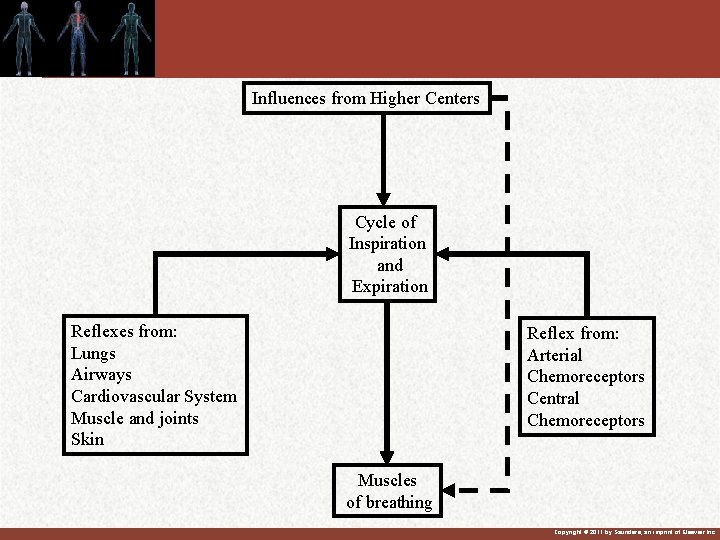
Influences from Higher Centers Cycle of Inspiration and Expiration Reflexes from: Lungs Airways Cardiovascular System Muscle and joints Skin Reflex from: Arterial Chemoreceptors Central Chemoreceptors Muscles of breathing Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
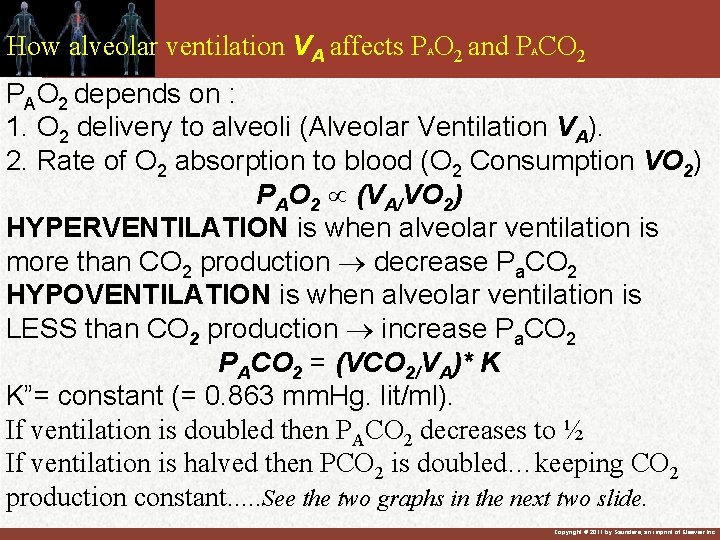
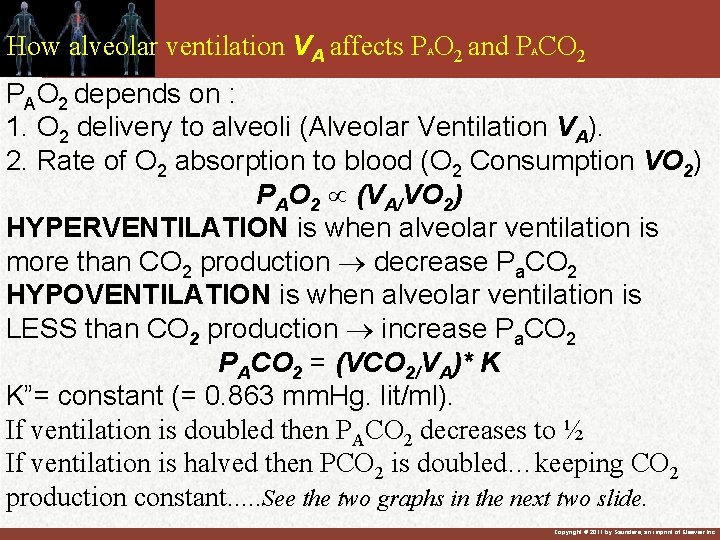
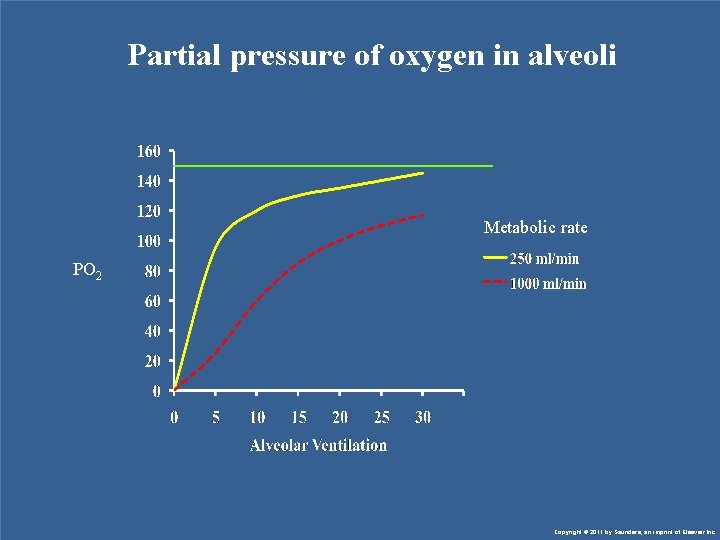
How alveolar ventilation VA affects P O 2 and P CO 2 A A PAO 2 depends on : 1. O 2 delivery to alveoli (Alveolar Ventilation VA). 2. Rate of O 2 absorption to blood (O 2 Consumption VO 2) PAO 2 (VA/VO 2) HYPERVENTILATION is when alveolar ventilation is more than CO 2 production decrease Pa. CO 2 HYPOVENTILATION is when alveolar ventilation is LESS than CO 2 production increase Pa. CO 2 PACO 2 = (VCO 2/VA)* K K”= constant (= 0. 863 mm. Hg. lit/ml). If ventilation is doubled then PACO 2 decreases to ½ If ventilation is halved then PCO 2 is doubled…keeping CO 2 production constant. . . See the two graphs in the next two slide. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
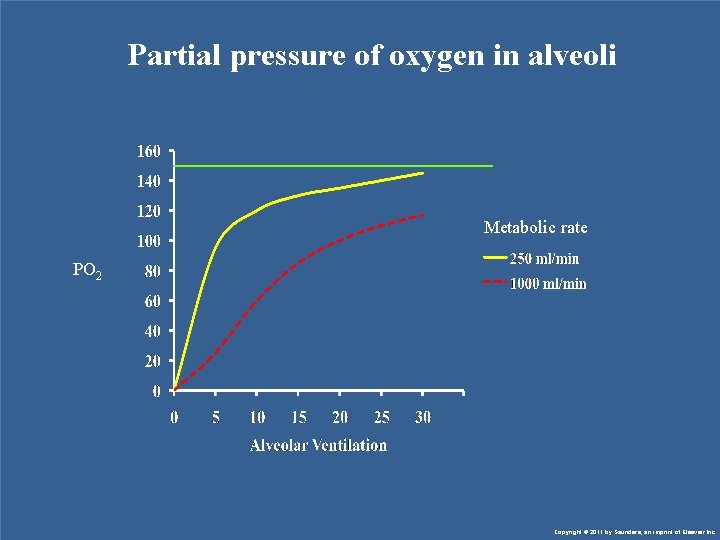
Partial pressure of oxygen in alveoli Metabolic rate PO 2 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.

Partial pressure of CO 2 in alveoli Metabolic rate PCO 2 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
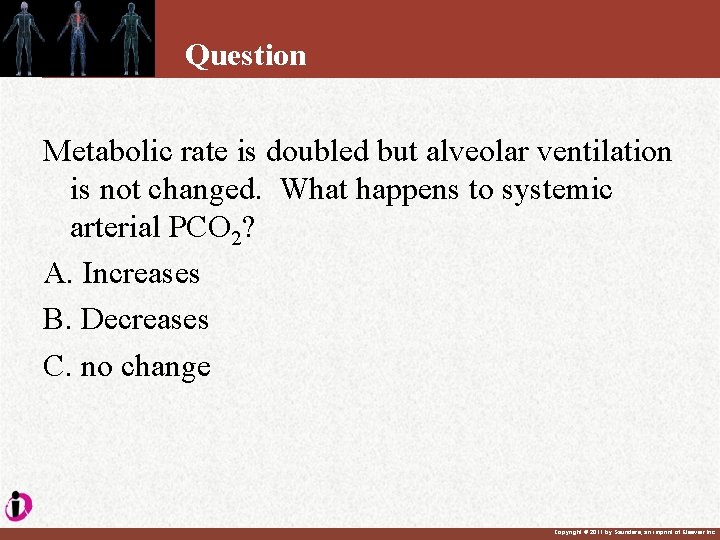
Question Metabolic rate is doubled but alveolar ventilation is not changed. What happens to systemic arterial PCO 2? A. Increases B. Decreases C. no change Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
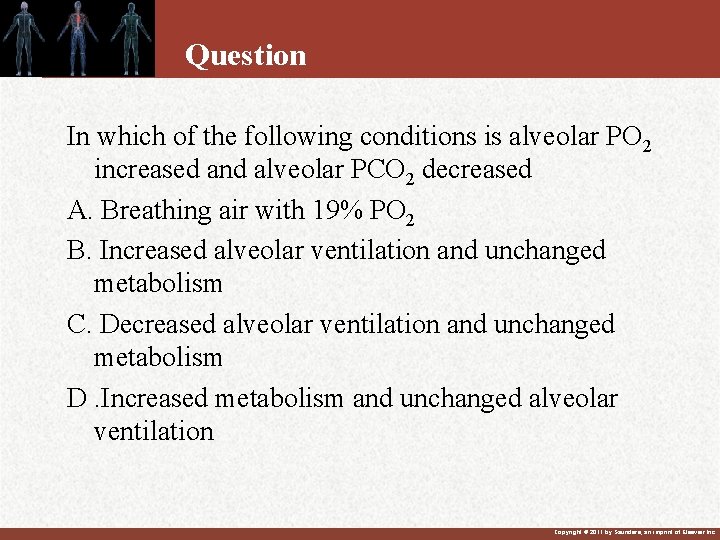
Question In which of the following conditions is alveolar PO 2 increased and alveolar PCO 2 decreased A. Breathing air with 19% PO 2 B. Increased alveolar ventilation and unchanged metabolism C. Decreased alveolar ventilation and unchanged metabolism D. Increased metabolism and unchanged alveolar ventilation Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Question What is the effect of anemia on ventilation? A. decrease ventilation B. increase ventilation C. no change in ventilation. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Question Breathing CO acutely will __? __ respiration? A. increase B. decrease C. not change Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Answer Breathing CO will not change respiration? Arterial PO 2 does not change, PCO 2 does not change Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
THE RESPIRATORY CENTER • It is a loose collection of inspiratory and expiratory neurons situated in the medulla oblongata of the brain stem. Is not a discrete identifiable center in the strict anatomical sense. When inspiratory neurons are active, expiratory neurons are inhibited and vise versa. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
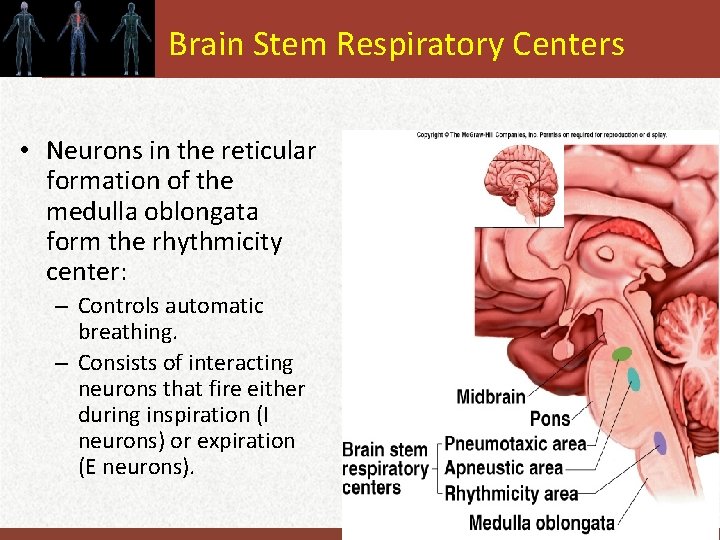
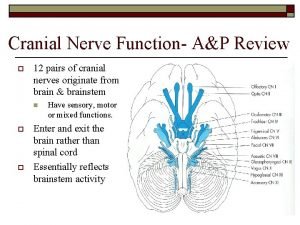
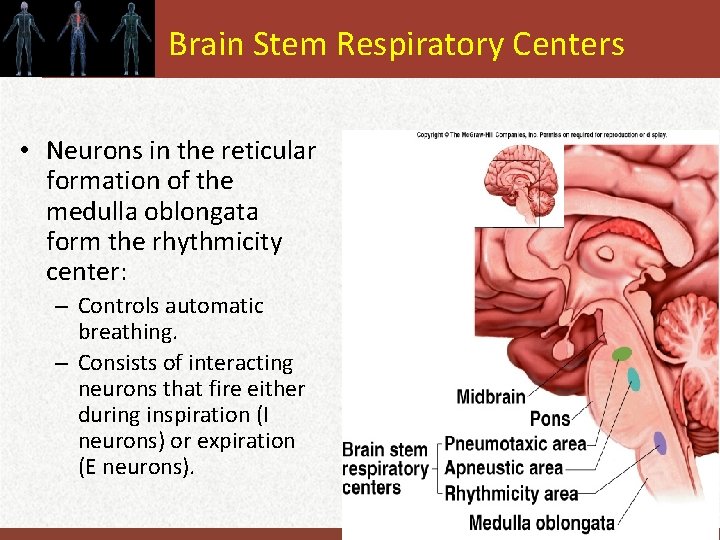
Brain Stem Respiratory Centers • Neurons in the reticular formation of the medulla oblongata form the rhythmicity center: Insert fig. 16. 25 – Controls automatic breathing. – Consists of interacting neurons that fire either during inspiration (I neurons) or expiration (E neurons). Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
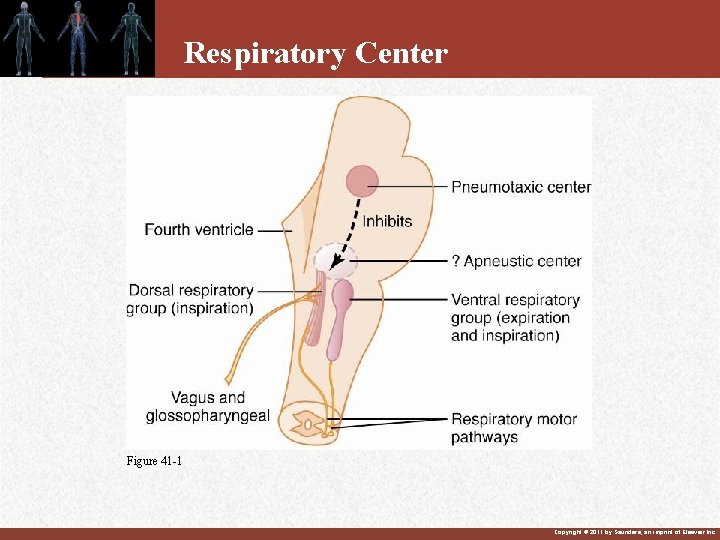
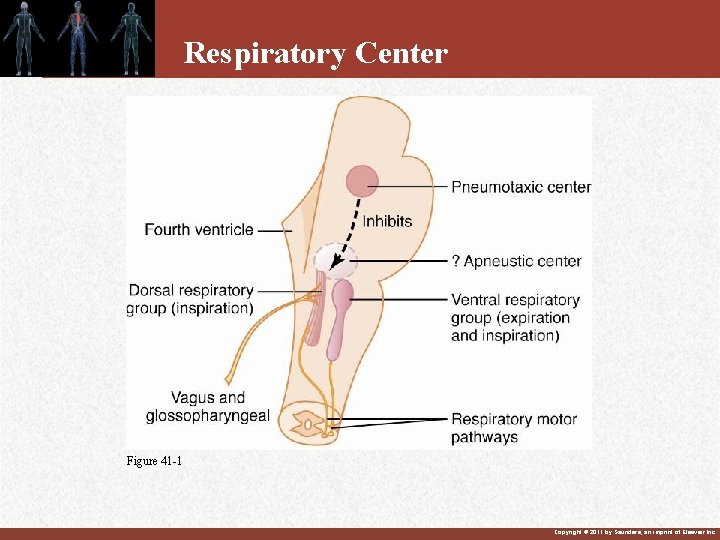
Respiratory Center Figure 41 -1 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
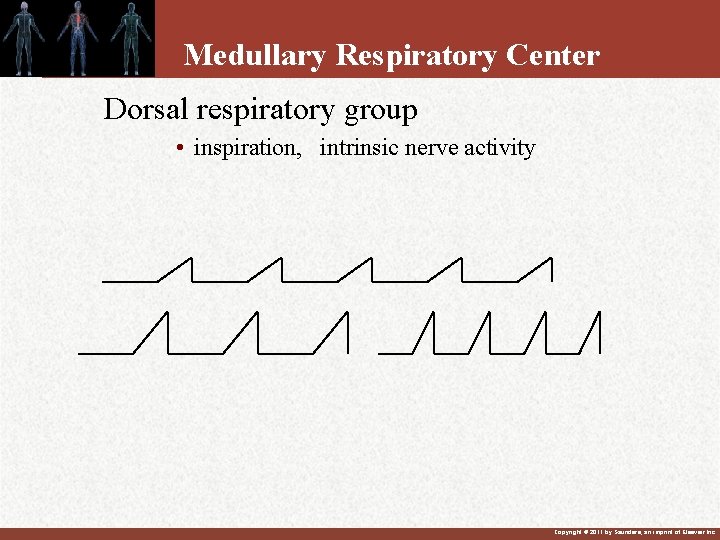
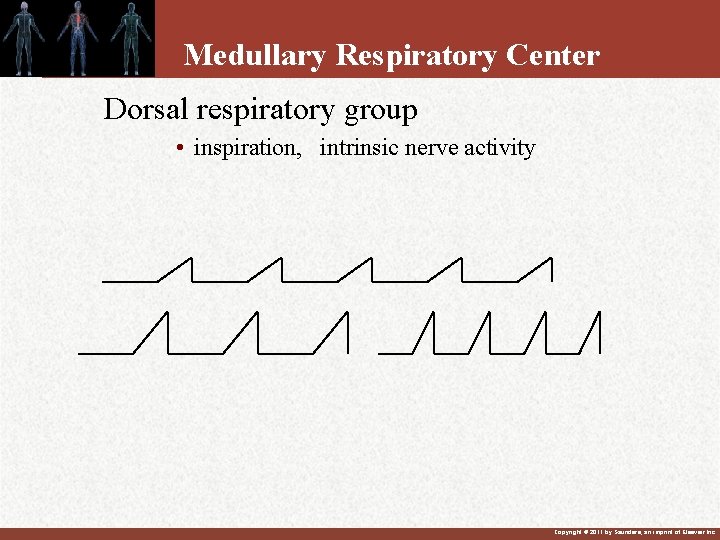
Medullary Respiratory Center Dorsal respiratory group • inspiration, intrinsic nerve activity Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Respiratory Center • Ventral Respiratory Group – Inactive during quiet respiration – Active respiration – Projections from the Dorsal Respiratory Group Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Brain Stem Respiratory Centers (continued) • “I” neurons project to, and stimulate spinal motor neurons that innervate respiratory muscles. • Expiration is a passive process that occurs when the I neurons are inhibited. • Activity varies in a reciprocal way. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Rhythmicity Center • “I” neurons located primarily in dorsal respiratory group (DRG): – Regulate activity of phrenic nerve. • Project to and stimulate spinal interneurons that innervate respiratory muscles. • “E” neurons located in ventral respiratory group (VRG): – Passive process. • Controls motor neurons to the internal intercostal muscles. • Activity of E neurons inhibit I neurons. – Rhythmicity of I and E neurons may be due to pacemaker neurons located in the upper part of the VRG. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Pons Respiratory Centers • Activities of medullary rhythmicity center is influenced by pons. • Apneustic center: – Promotes inspiration by stimulating the I neurons in the medulla. • Pneumotaxic center: – Antagonizes the apneustic center. – Inhibits inspiration and thus increase RR. – It is the Switch of inspiration and modulate respiratory system Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
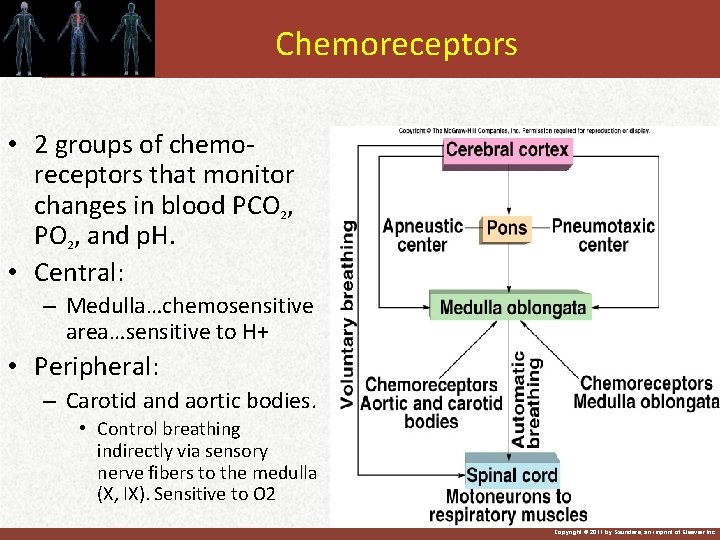
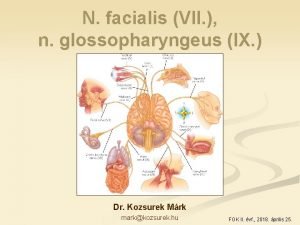
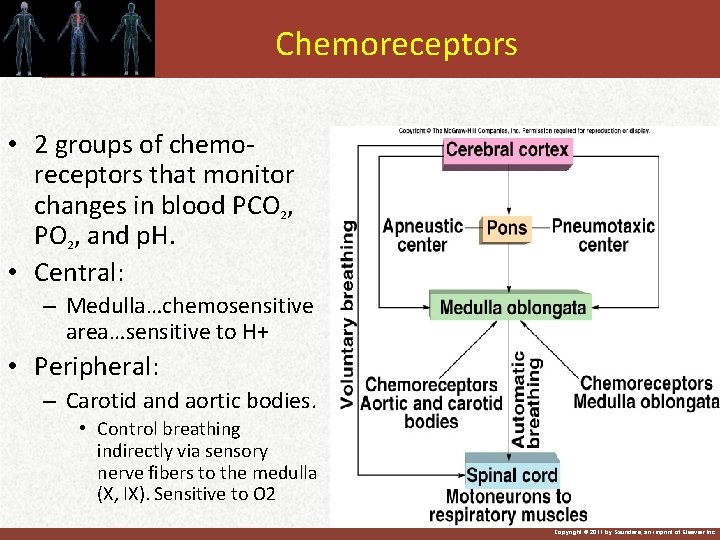
Chemoreceptors • 2 groups of chemoreceptors that monitor changes in blood PCO 2, PO 2, and p. H. • Central: Insert fig. 16. 27 – Medulla…chemosensitive area…sensitive to H+ • Peripheral: – Carotid and aortic bodies. • Control breathing indirectly via sensory nerve fibers to the medulla (X, IX). Sensitive to O 2 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
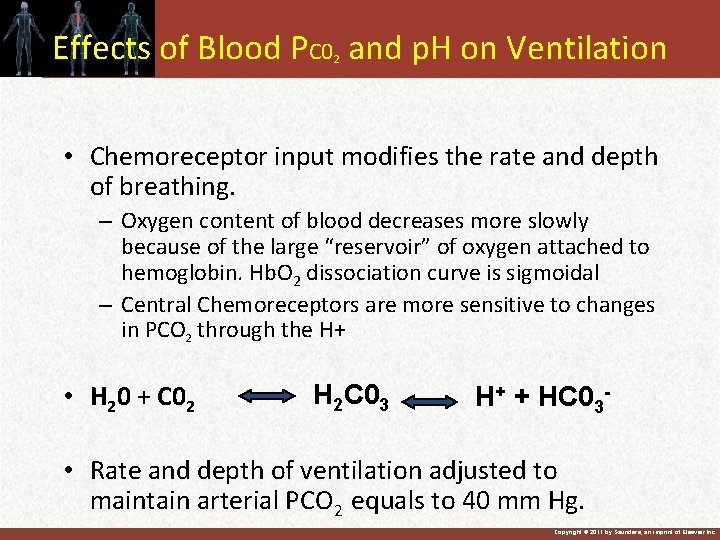
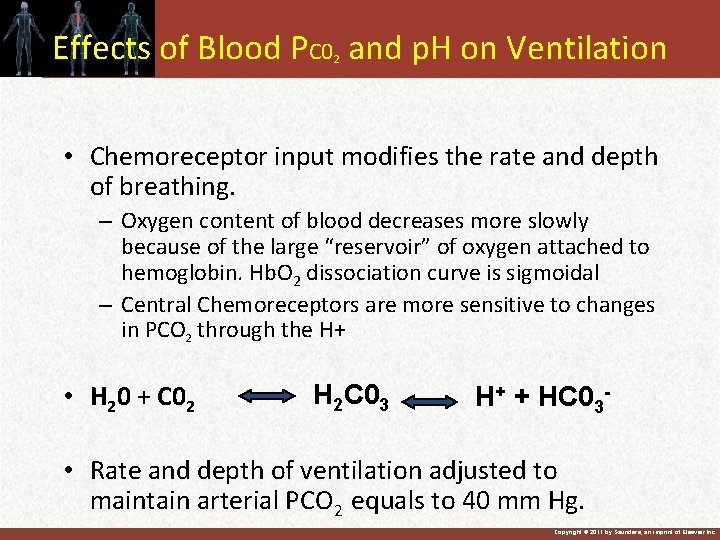
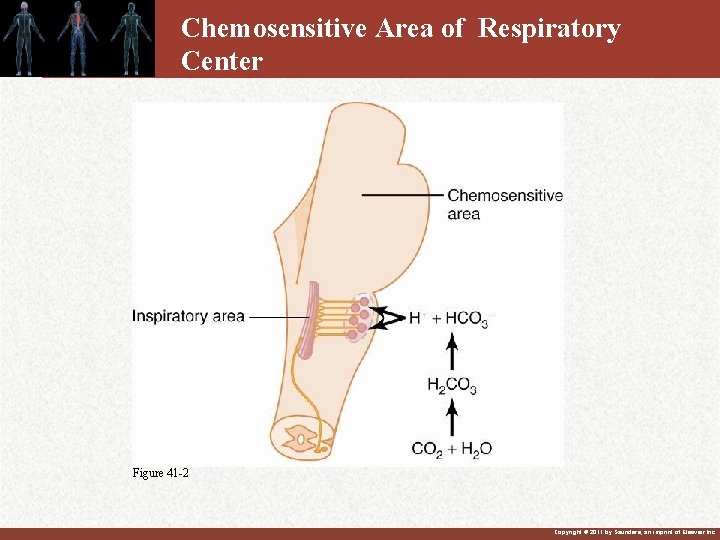
Effects of Blood PC 0 and p. H on Ventilation 2 • Chemoreceptor input modifies the rate and depth of breathing. – Oxygen content of blood decreases more slowly because of the large “reservoir” of oxygen attached to hemoglobin. Hb. O 2 dissociation curve is sigmoidal – Central Chemoreceptors are more sensitive to changes in PCO 2 through the H+ • H 20 + C 02 H 2 C 03 H+ + HC 03 - • Rate and depth of ventilation adjusted to maintain arterial PCO 2 equals to 40 mm Hg. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.

Chemoreceptor Control • Central chemoreceptors: More sensitive to changes in arterial PC 02 through H+ • H 20 + CO 2 H 2 C 03 H+ • H+ cannot cross the blood brain barrier. • CO 2 can cross the blood brain barrier and will form H 2 CO 3. – H+ lowers p. H of CSF fasters than it lowers blood p. H…no enough buffers in CSF • Directly stimulates central chemoreceptors. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
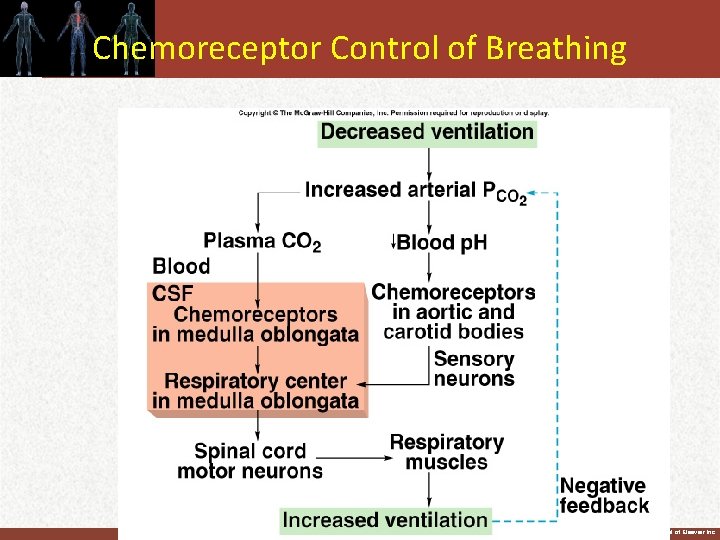
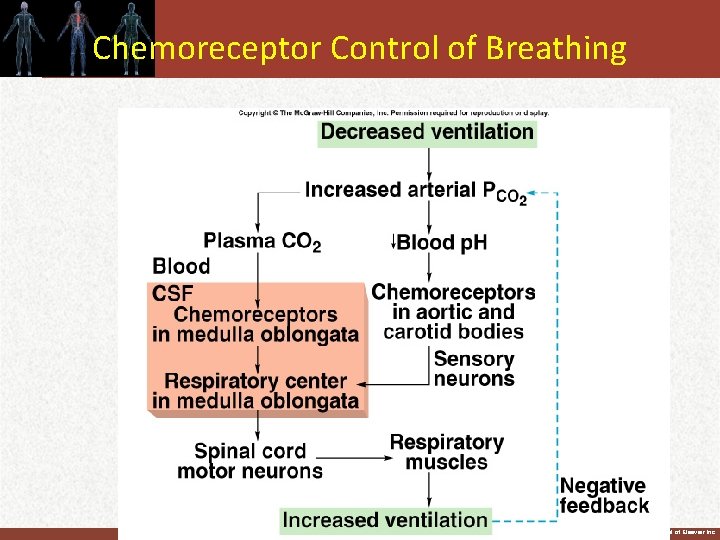
Chemoreceptor Control of Breathing Insert fig. 16. 29 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
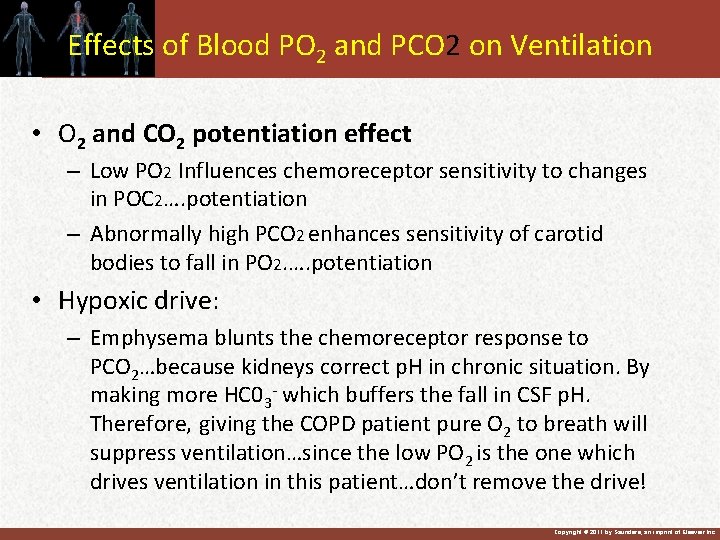
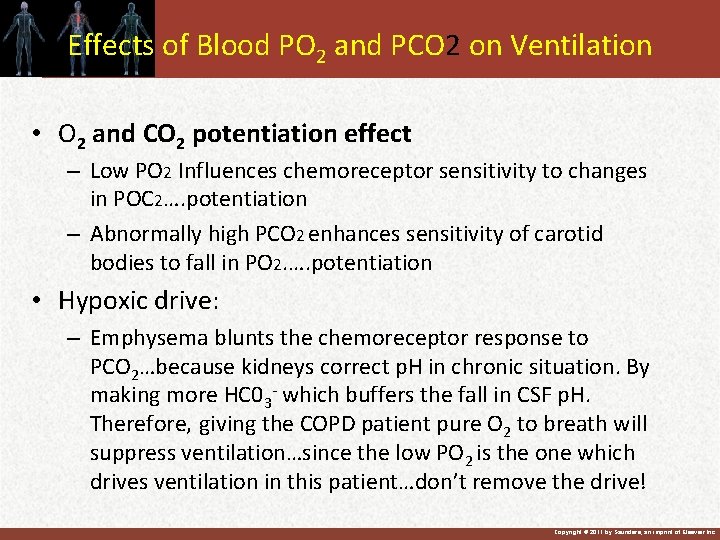
Effects of Blood PO 2 and PCO 2 on Ventilation • O 2 and CO 2 potentiation effect – Low PO 2 Influences chemoreceptor sensitivity to changes in POC 2…. potentiation – Abnormally high PCO 2 enhances sensitivity of carotid bodies to fall in PO 2. …. potentiation • Hypoxic drive: – Emphysema blunts the chemoreceptor response to PCO 2…because kidneys correct p. H in chronic situation. By making more HC 03 - which buffers the fall in CSF p. H. Therefore, giving the COPD patient pure O 2 to breath will suppress ventilation…since the low PO 2 is the one which drives ventilation in this patient…don’t remove the drive! Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Effects of Pulmonary Receptors on Ventilation • Lungs contain receptors that influence the brain stem respiratory control centers via sensory fibers in vagus. – Unmyelinated C fibers can be stimulated by: • Histamine and bradykinin: – Released in response to noxious agents. – Irritant receptors are rapidly adaptive receptors. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Lung receptors • Pulmonary Stretch Receptors - Located in smooth muscle of large and small airway and minimize work of breathing by inhibiting large tidal volumes - Hering-Breuer reflex” are Pulmonary stretch receptors activated during inspiration. - Inhibits respiratory centers to prevent undue tension on lungs. Hering Breuer inflation reflex can be easily manifested in dogs & cats but not in man (unless VT ≥ 1. 5 liters). So its function in man is uncertain. However, in newborn where VT is small, it may be important. • Irritant receptors – Nasal mucosa, upper airways, possibly alveoli – Bronchoconstriction which lead to cough and sneeze • J receptors – Located in the capillary wall, interstitium – Lung disease and edema (pulmonary congestion) – Rapid shallow breathing (tachypnea) Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Other Reflexes • Arterial Baroreceptors – Stimulation by elevated blood pressure results in brief apnea and bronchodilation • Muscles and Tendons – Muscles of respiration as well as skeletal muscles, joints and tendons – Adjust ventilation to elevated workloads Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Chemical Control of Respiration • Carbon Dioxide works centrally through H+ • Oxygen works peripherally at the carotid and aortic bodies. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
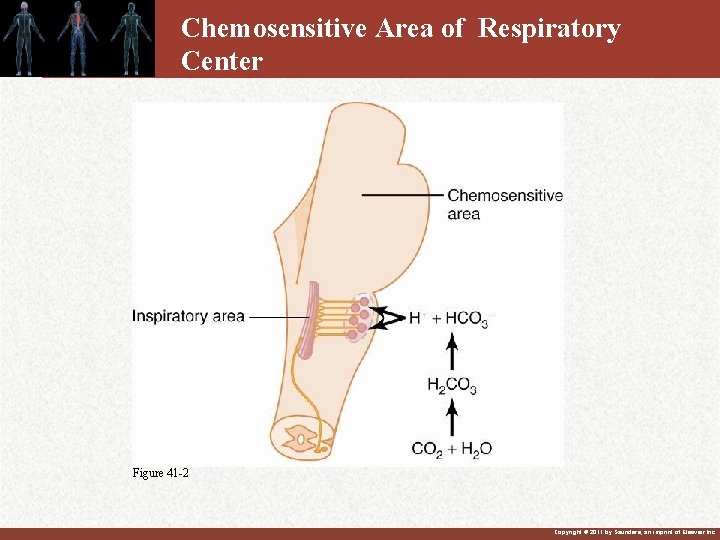
Chemosensitive Area of Respiratory Center Figure 41 -2 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.

Chemosensitive Area of Respiratory Center Brain Tissue H+ blood-brain barrier Blood low protein p. H=7. 32 PCO 2 =50 chemoreceptor CO 2 HCO 3 - CSF CO 2 slow H+ CO 2 HCO 3 - Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
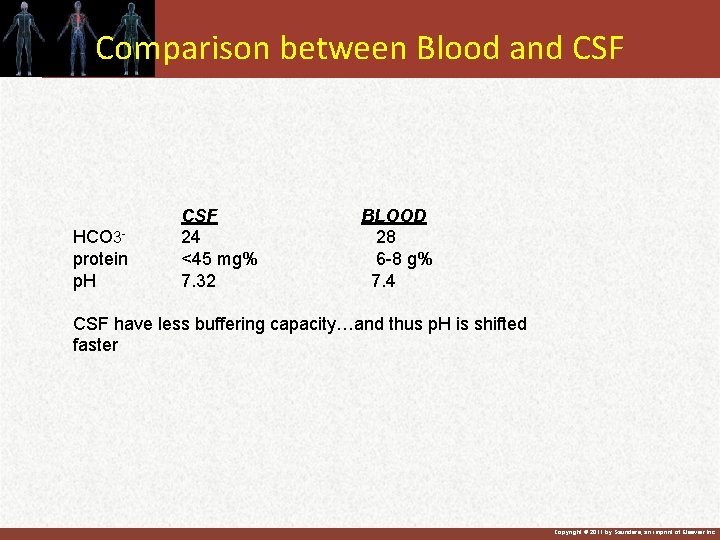
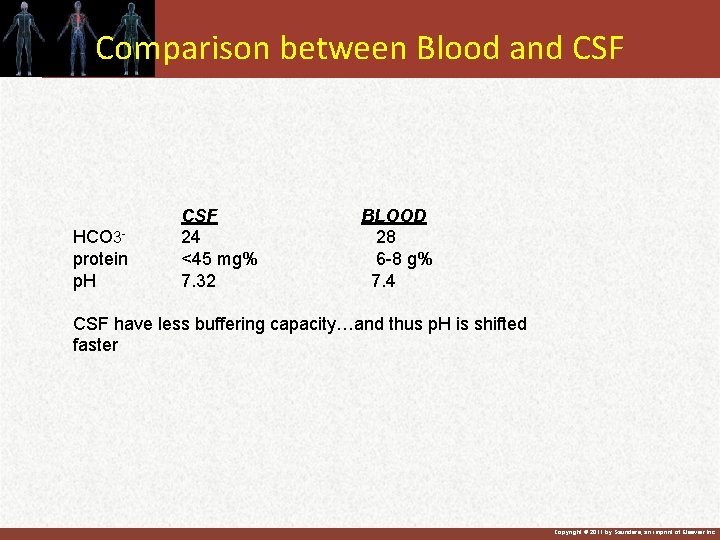
Comparison between Blood and CSF HCO 3 protein p. H CSF 24 <45 mg% 7. 32 BLOOD 28 6 -8 g% 7. 4 CSF have less buffering capacity…and thus p. H is shifted faster Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
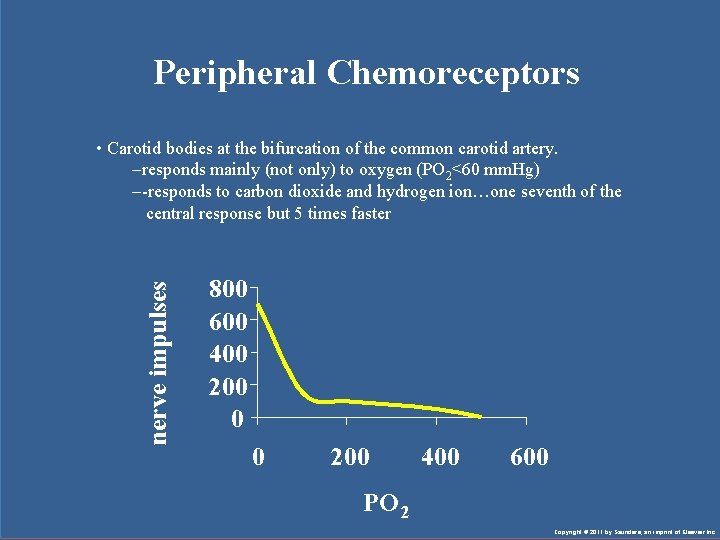
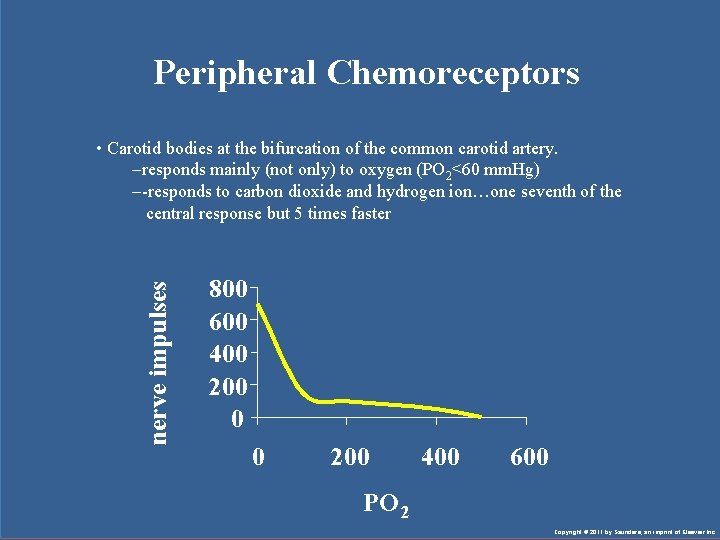
Peripheral Chemoreceptors nerve impulses • Carotid bodies at the bifurcation of the common carotid artery. –responds mainly (not only) to oxygen (PO 2<60 mm. Hg) –-responds to carbon dioxide and hydrogen ion…one seventh of the central response but 5 times faster 800 600 400 200 0 0 200 400 600 PO 2 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
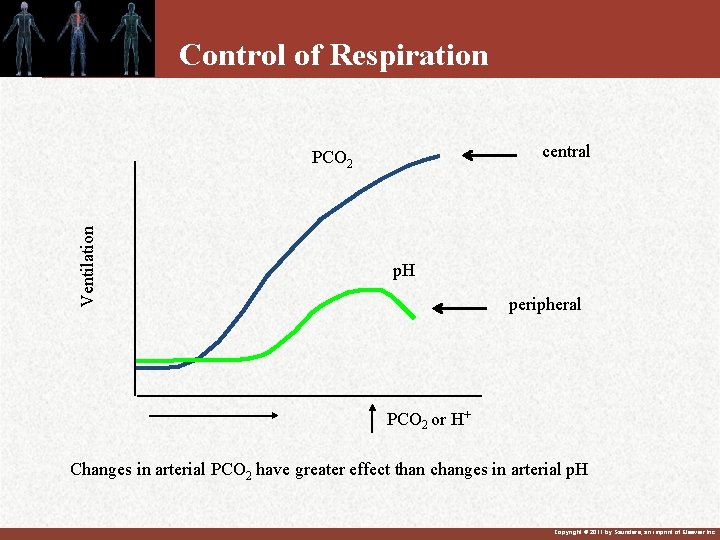
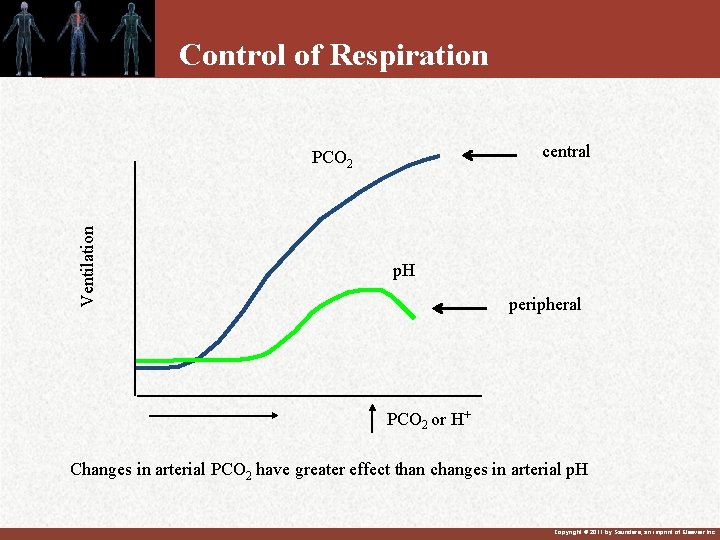
Control of Respiration central Ventilation PCO 2 p. H peripheral PCO 2 or H+ Changes in arterial PCO 2 have greater effect than changes in arterial p. H Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
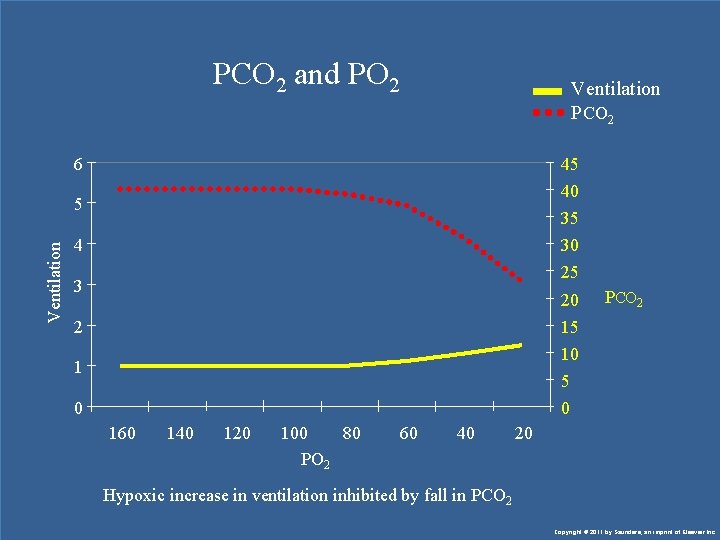
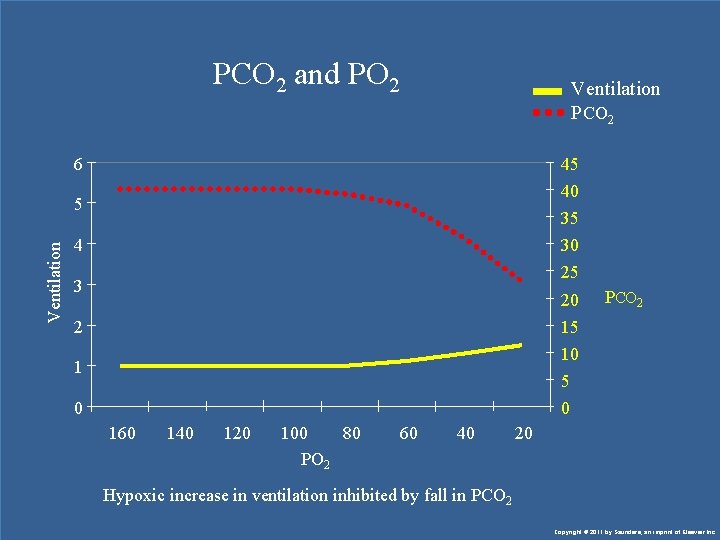
PCO 2 and PO 2 Ventilation PCO 2 6 45 40 Ventilation 5 35 30 4 25 3 20 2 PCO 2 15 10 5 0 160 140 120 100 80 PO 2 60 40 20 Hypoxic increase in ventilation inhibited by fall in PCO 2 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Chemoreceptor Control (continued) • Peripheral chemoreceptors mainly stimulated by ↓PO 2 • H 20 + C 02 H 2 C 03 H+ • Stimulated by rise in [H+] of arterial blood. – Increased [H+] stimulates peripheral chemoreceptors. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
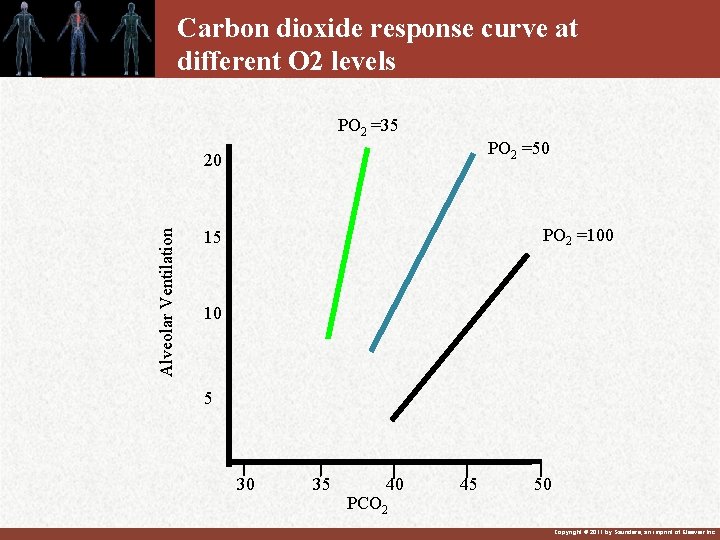
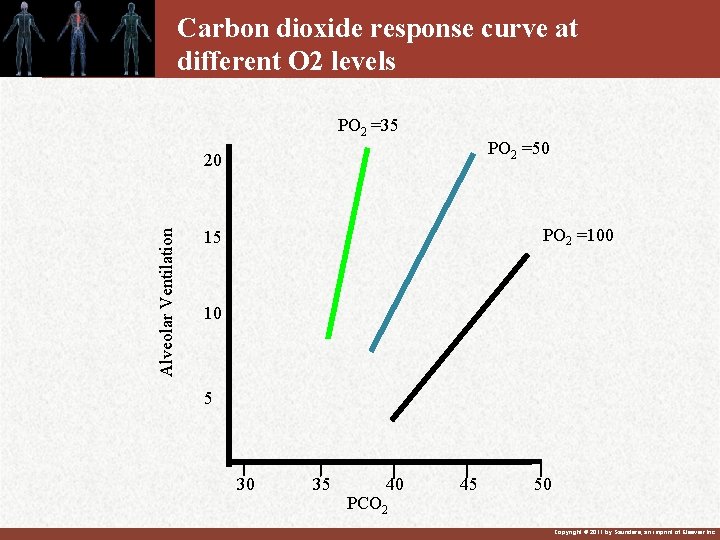
Carbon dioxide response curve at different O 2 levels PO 2 =35 PO 2 =50 Alveolar Ventilation 20 PO 2 =100 15 10 5 30 35 40 PCO 2 45 50 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
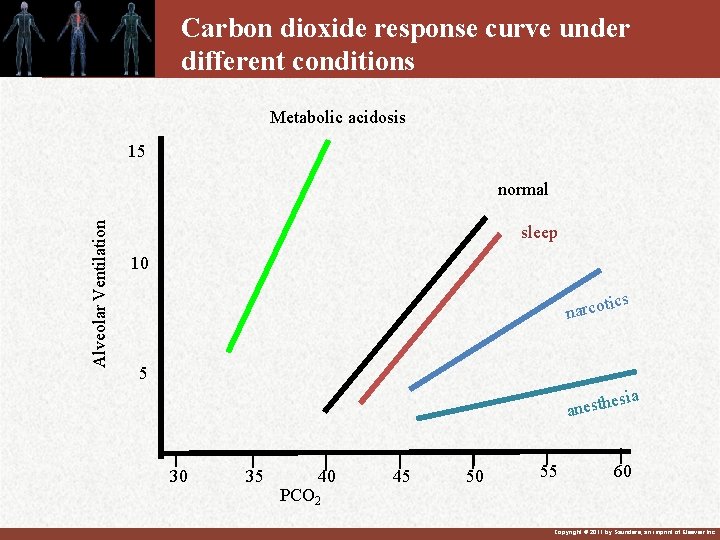
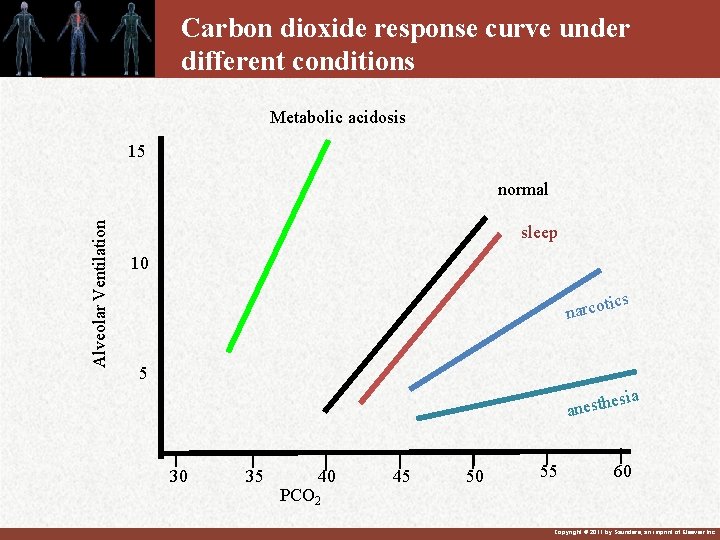
Carbon dioxide response curve under different conditions Metabolic acidosis 15 Alveolar Ventilation normal sleep 10 tics narco 5 sia e anesth 30 35 40 PCO 2 45 50 55 60 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Summary • Carbon dioxide is major stimulus for increased respiration • Acts on chemosensitive area through H+ • Peripheral chemoreceptors are mainly affected by low PO 2 • If PCO 2 is constant low oxygen can be important • Questions? – Why is oxygen’s effect on respiration blunted? – Explain ventilatory drive during severe lung disease…see next slide for answer. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
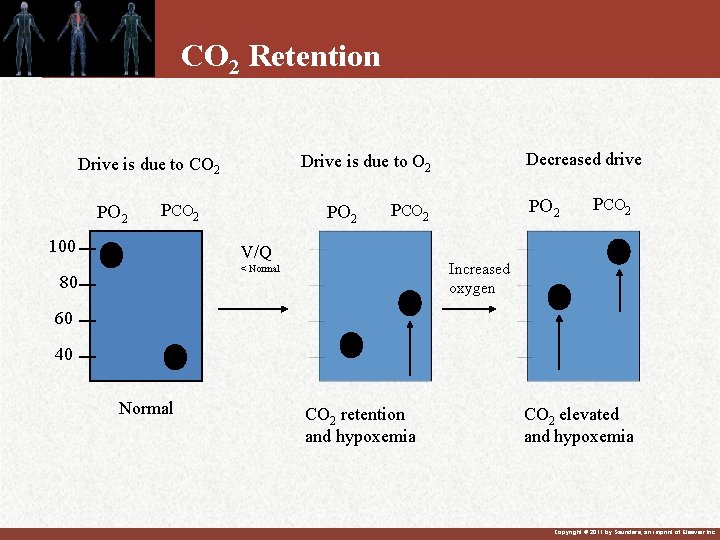
CO 2 Retention • • Severe lung disease, COPD Develop hypoxemia and hypercapnia Respiratory drive due to oxygen Renal control of acid-base balance Treat with oxygen inhibits respiratory drive High levels of PCO 2 Minimal levels of oxygen, monitor blood gases Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
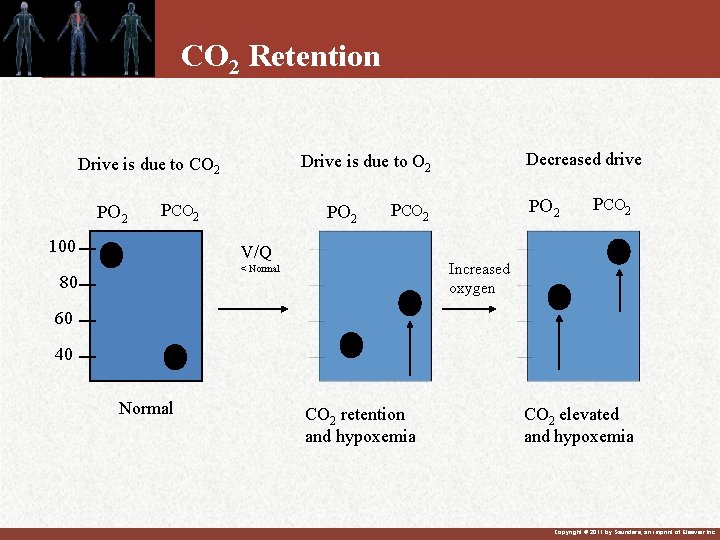
CO 2 Retention PO 2 PCO 2 100 PO 2 PCO 2 V/Q PCO 2 Increased oxygen < Normal 80 Decreased drive Drive is due to O 2 Drive is due to CO 2 60 40 Normal CO 2 retention and hypoxemia CO 2 elevated and hypoxemia Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
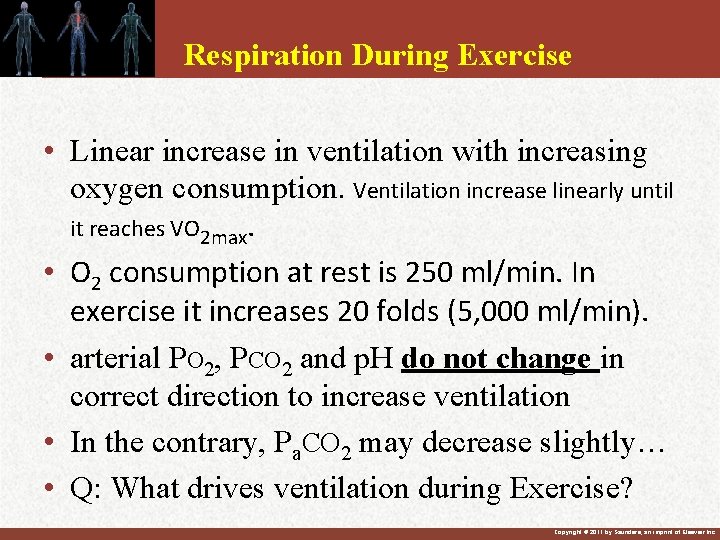
Respiration During Exercise • Linear increase in ventilation with increasing oxygen consumption. Ventilation increase linearly until it reaches VO 2 max. • O 2 consumption at rest is 250 ml/min. In exercise it increases 20 folds (5, 000 ml/min). • arterial PO 2, PCO 2 and p. H do not change in correct direction to increase ventilation • In the contrary, Pa. CO 2 may decrease slightly… • Q: What drives ventilation during Exercise? Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
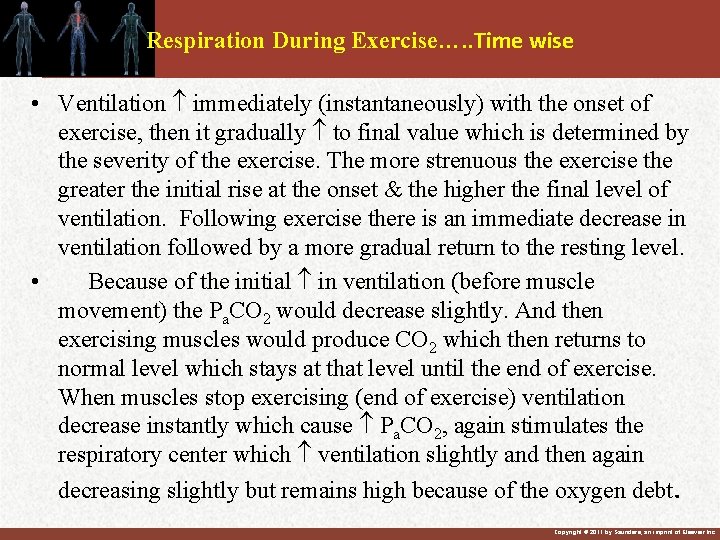
Respiration During Exercise…. . Time wise • Ventilation immediately (instantaneously) with the onset of exercise, then it gradually to final value which is determined by the severity of the exercise. The more strenuous the exercise the greater the initial rise at the onset & the higher the final level of ventilation. Following exercise there is an immediate decrease in ventilation followed by a more gradual return to the resting level. • Because of the initial in ventilation (before muscle movement) the Pa. CO 2 would decrease slightly. And then exercising muscles would produce CO 2 which then returns to normal level which stays at that level until the end of exercise. When muscles stop exercising (end of exercise) ventilation decrease instantly which cause Pa. CO 2, again stimulates the respiratory center which ventilation slightly and then again decreasing slightly but remains high because of the oxygen debt. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Respiration During Exercise…Drive • • • Overflow of signals from cortex Body movements Increased body temperature Designed to control PCO 2 Learned response Conclusion: we are not sure regarding the exact mechanism responsible for increased ventilation during exercise. Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Other Factors to Influence Respiration • Voluntary control • Activity from vasomotor center • Body temperature – increased production of carbon dioxide – direct effect on respiratory center • Irritants • Anesthesia Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
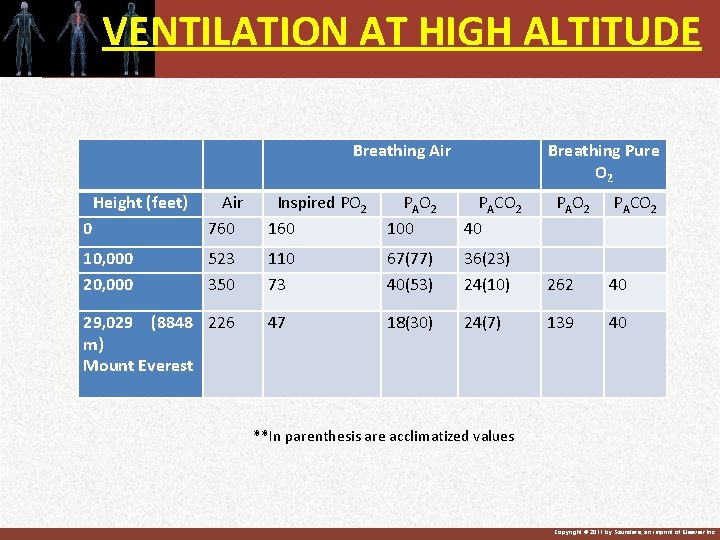
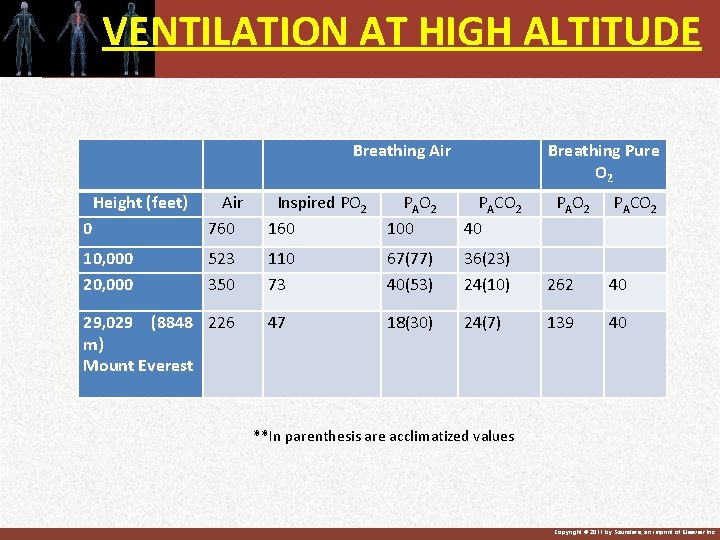
VENTILATION AT HIGH ALTITUDE Height (feet) Breathing Air Breathing Pure O 2 0 Air 760 Inspired PO 2 160 P A O 2 100 PACO 2 40 PACO 2 10, 000 20, 000 523 350 110 73 67(77) 40(53) 36(23) 24(10) 262 40 47 18(30) 24(7) 139 40 29, 029 (8848 226 m) Mount Everest P A O 2 **In parenthesis are acclimatized values Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
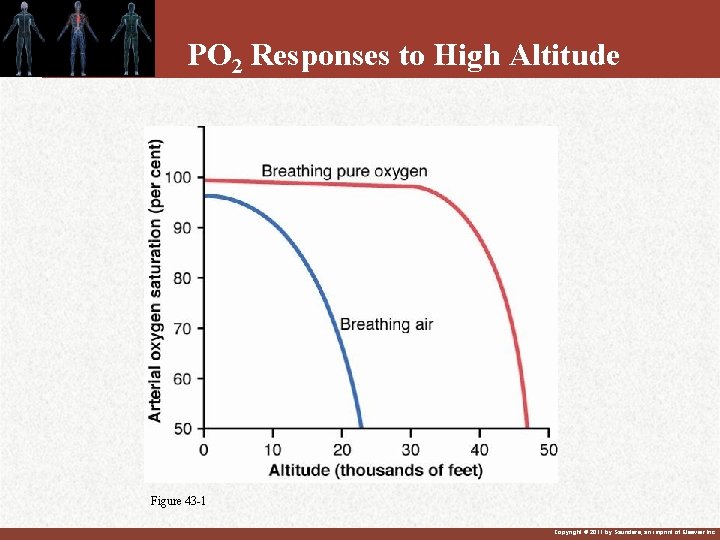
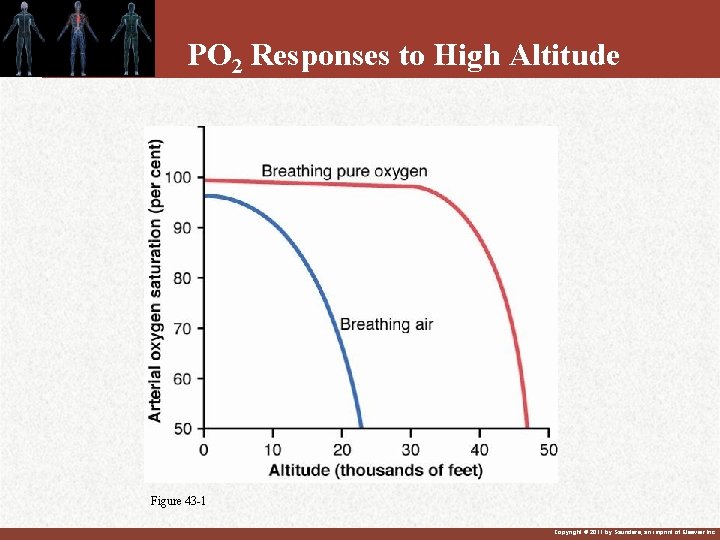
PO 2 Responses to High Altitude Figure 43 -1 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Acclimatization…. continue • Increased ventilation – due to decreased PO 2 – increase slowed by decreased Pc. O 2 – It increases 70% in the first day and 400 -500% in the coming few days. • Increased hematocrit (content) • Increased diffusing capacity • Increased capillarity Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
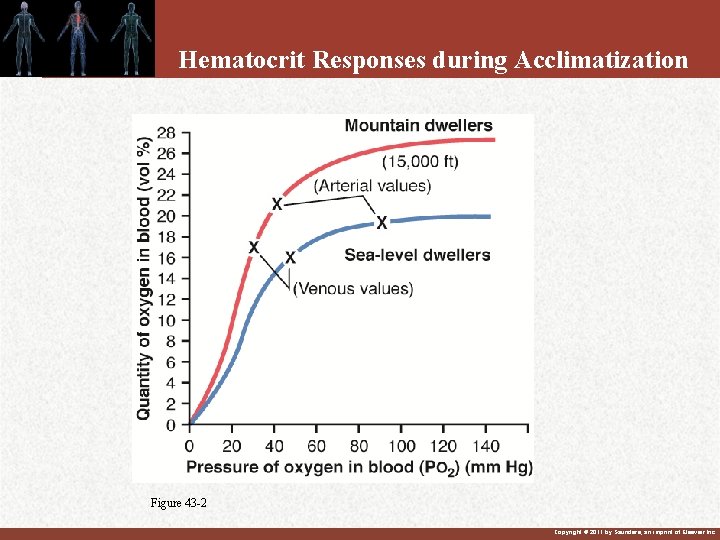
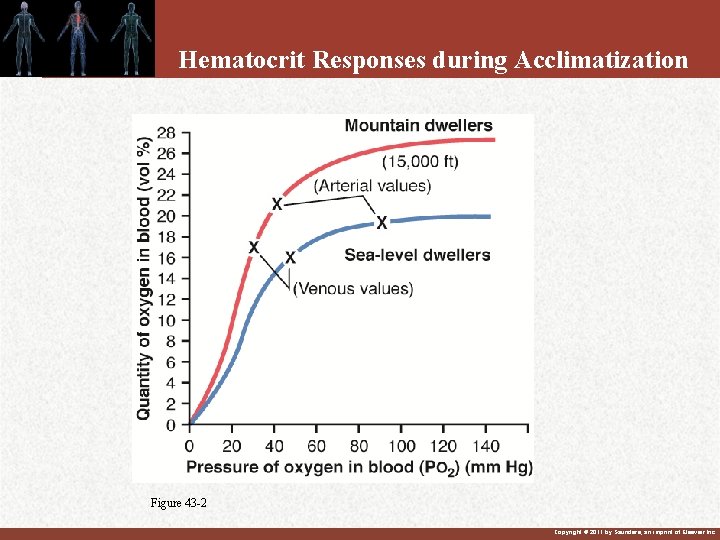
Hematocrit Responses during Acclimatization Figure 43 -2 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Mountain Sickness • Chronic mountain sickness – increase in red cell mass – increase in pulmonary arterial pressure – enlargement of right heart • Acute mountain sickness – acute cerebral edema – acute pulmonary edema Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Question What is atmospheric PO 2 at 10, 000 ft (barometric pressure = 508 mm. Hg)? Person has normal alveolar ventilation A. 95 mm. Hg B. 106 C. 149 D. 159 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
Answer 508*0. 21=106 Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
• See you again next semester in renal Physiology… • GOOD LUCK Copyright © 2011 by Saunders, an imprint of Elsevier Inc.
 Regulation of breathing
Regulation of breathing External respiration
External respiration External respiration vs internal respiration
External respiration vs internal respiration A small child slides down the four frictionless slides
A small child slides down the four frictionless slides Starting from rest a marble first rolls down
Starting from rest a marble first rolls down Da form 3749 regulation
Da form 3749 regulation Unit 6 review questions
Unit 6 review questions Chapter 18 regulation of gene expression
Chapter 18 regulation of gene expression Chapter 18 regulation of gene expression
Chapter 18 regulation of gene expression Chapter 12 section 4 gene regulation and mutations
Chapter 12 section 4 gene regulation and mutations Chapter 18 regulation of gene expression
Chapter 18 regulation of gene expression Chapter 18
Chapter 18 Hexacarbon decahydride hexoxide
Hexacarbon decahydride hexoxide Fernando vii
Fernando vii Reach annex vii testing
Reach annex vii testing De ce numi vii
De ce numi vii Pedagogika fanining rivojlanish tarixi
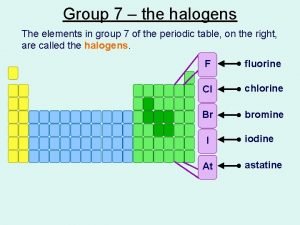
Pedagogika fanining rivojlanish tarixi What is halogen
What is halogen Unitatea fundamentala in clasificarea organismelor vii
Unitatea fundamentala in clasificarea organismelor vii Cn xi test
Cn xi test Cn viii test
Cn viii test Henryk vii tudor
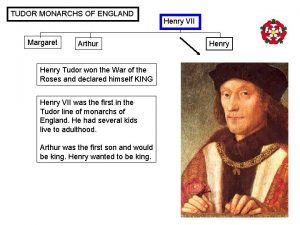
Henryk vii tudor Se inmultesc prin oua
Se inmultesc prin oua Henry vii
Henry vii King henry viii family tree
King henry viii family tree 100 people surveyed
100 people surveyed Lettera vii platone
Lettera vii platone Trou stylo mastoidien
Trou stylo mastoidien What is the theme of the poem song vii
What is the theme of the poem song vii 6/1996. (vii. 16.) müm rendelet
6/1996. (vii. 16.) müm rendelet Resolution 435 code of ethics
Resolution 435 code of ethics 10/2015 (vii. 30) hm
10/2015 (vii. 30) hm Fernando vii absolutismo
Fernando vii absolutismo Vii=i solucion
Vii=i solucion Lant trofic din parc
Lant trofic din parc Keputusan menteri kesehatan ri nomor 829/menkes/sk/vii/1999
Keputusan menteri kesehatan ri nomor 829/menkes/sk/vii/1999 Watak hang tuah
Watak hang tuah Rima vii becquer comentario
Rima vii becquer comentario Pearson vii
Pearson vii Canto 4 inferno parafrasi
Canto 4 inferno parafrasi Soarele de dupa vii isi arata fata
Soarele de dupa vii isi arata fata Handouts definition
Handouts definition Te har
Te har Rimaxxx
Rimaxxx Vestibulococlear
Vestibulococlear Title vii of the civil rights act
Title vii of the civil rights act Vestibulocochlear nerve.
Vestibulocochlear nerve. Title vii of the civil rights act
Title vii of the civil rights act Nerfs vii
Nerfs vii Nervus 7
Nervus 7 Reforma gregoriańska
Reforma gregoriańska Cq bw contest
Cq bw contest Superior salivatory nucleus
Superior salivatory nucleus Vii.a skupina
Vii.a skupina Vii. a skupina
Vii. a skupina Halogen group 7
Halogen group 7