Transplantation immunology Dr Adel Almogren Transfusion vs Transplantation

- Slides: 37
Transplantation immunology Dr Adel Almogren.
Transfusion vs. Transplantation Transfusion � transfer of blood � Ab-mediated reactions � Transplantation � transfer of any other tissue/organ � T cell mediated reactions �
Transplant Immunology Outline • • Introduction Graft compatibility Graft rejection Types of organ transplantation
Transplant Immunology Outline • Introduction
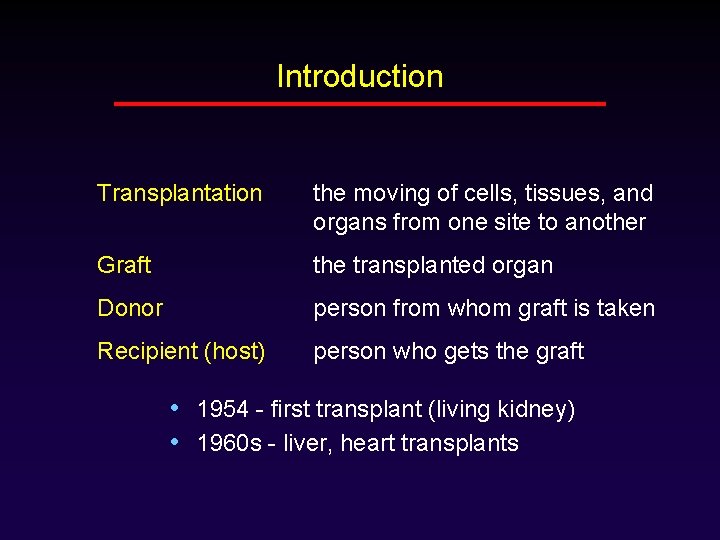
Introduction Transplantation the moving of cells, tissues, and organs from one site to another Graft the transplanted organ Donor person from whom graft is taken Recipient (host) person who gets the graft • 1954 - first transplant (living kidney) • 1960 s - liver, heart transplants
Introduction Transplantation problems • Surgical difficulties • Graft rejection • Organ shortage
Transplant Immunology Outline • Introduction • Graft compatibility
Compatibility Rejection = recipient recognizes graft as foreign, and destroys it Autograft within same person Isograft between identical twins Allograft between genetically different people Xenograft between different species
Compatibility Histocompatibility • Histocompatible: antigenically similar to the host • Histoincompatible: antigenically different from the host • MHC antigens are the most important • ABO antigens are also important • Minor histocompatiblity antigens are less important
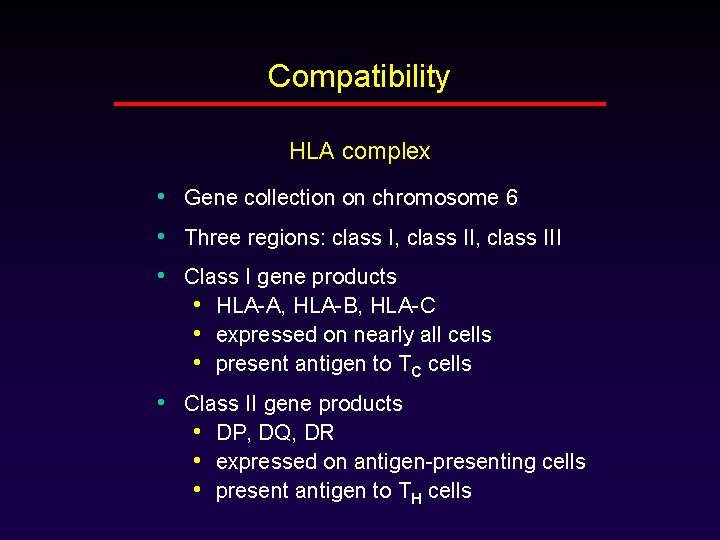
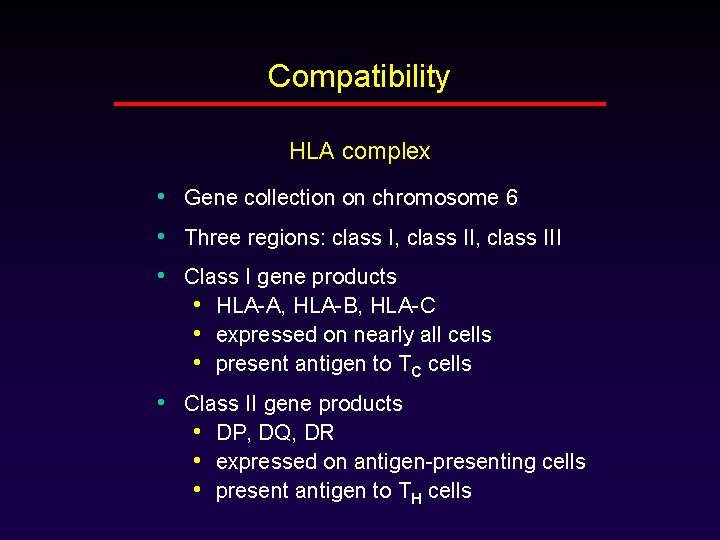
Compatibility HLA complex • Gene collection on chromosome 6 • Three regions: class I, class III • Class I gene products • HLA-A, HLA-B, HLA-C • expressed on nearly all cells • present antigen to TC cells • Class II gene products • DP, DQ, DR • expressed on antigen-presenting cells • present antigen to TH cells

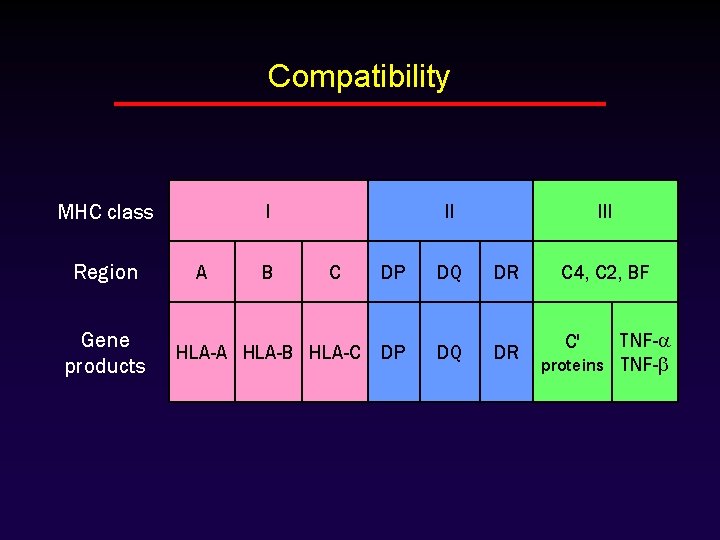
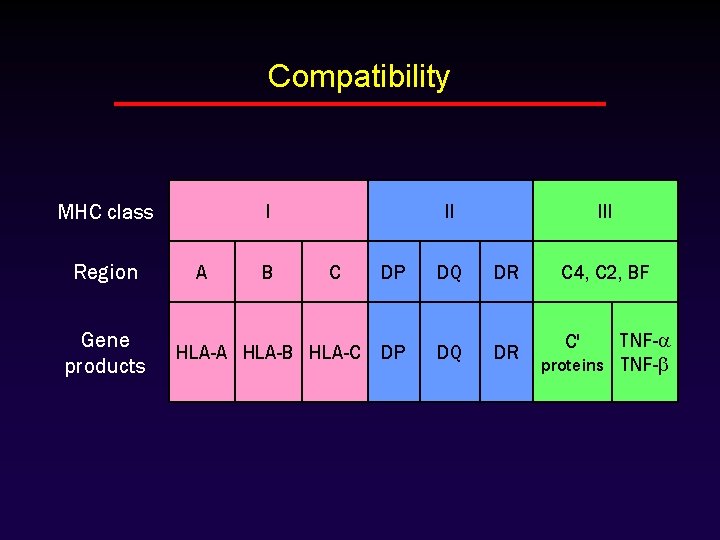
Compatibility MHC class Region Gene products I A B II C HLA-A HLA-B HLA-C III DP DQ DR C 4, C 2, BF DP DQ DR TNF- proteins TNF- C'
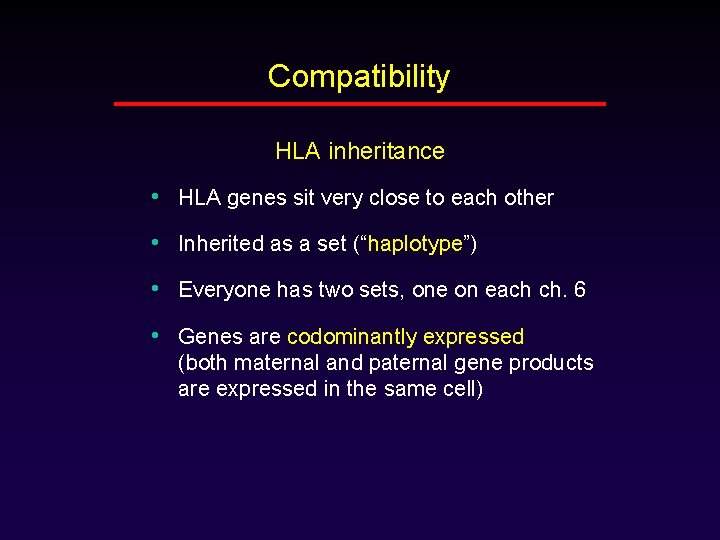
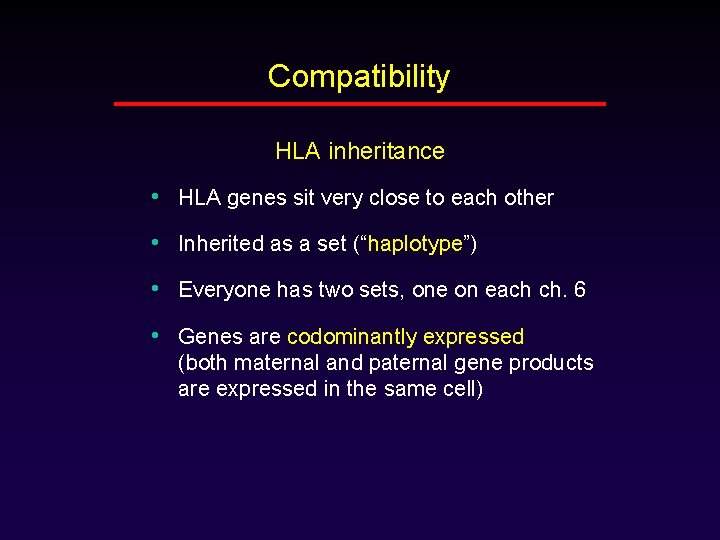
Compatibility HLA inheritance • HLA genes sit very close to each other • Inherited as a set (“haplotype”) • Everyone has two sets, one on each ch. 6 • Genes are codominantly expressed (both maternal and paternal gene products are expressed in the same cell)
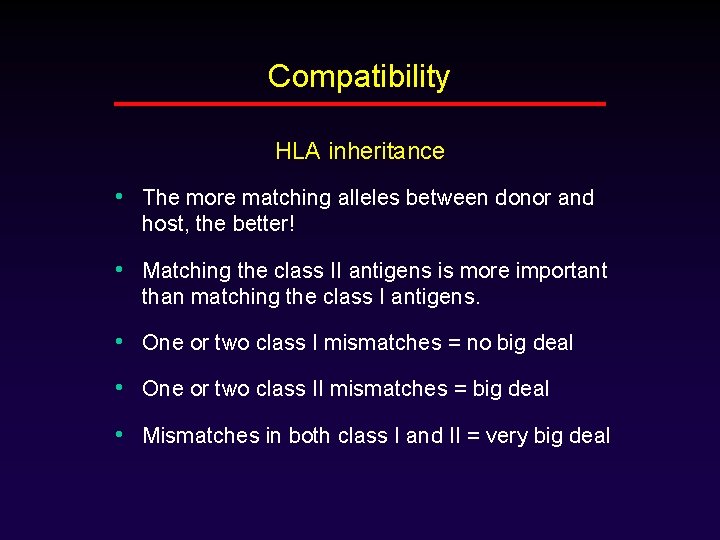
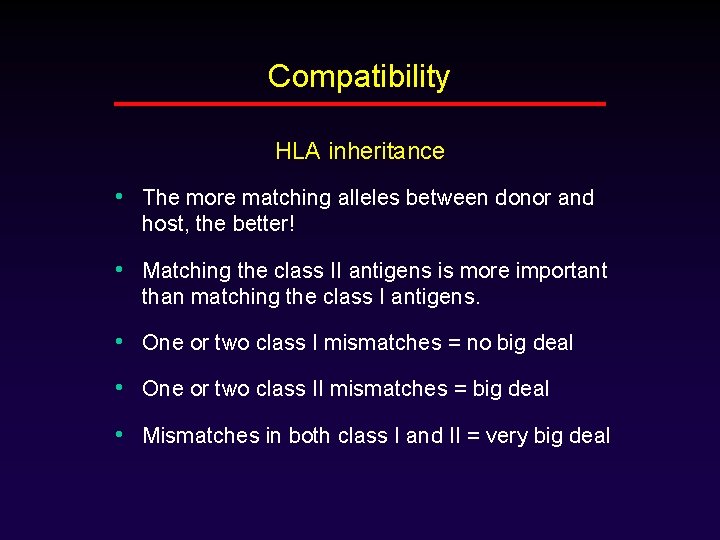
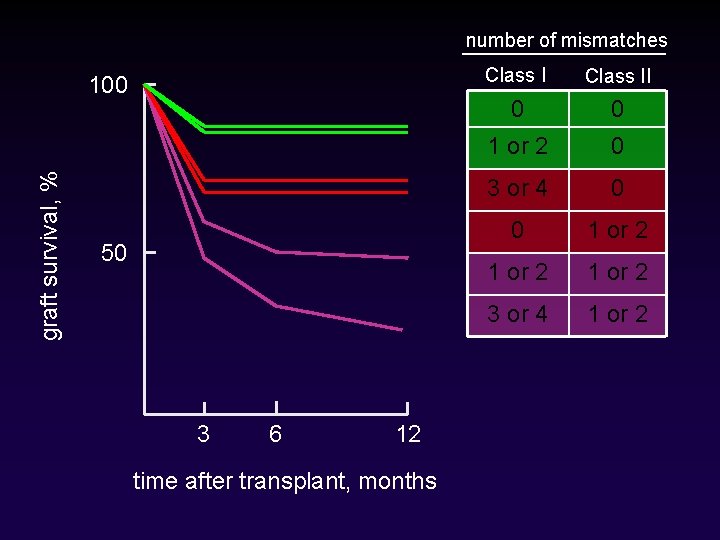
Compatibility HLA inheritance • The more matching alleles between donor and host, the better! • Matching the class II antigens is more important than matching the class I antigens. • One or two class I mismatches = no big deal • One or two class II mismatches = big deal • Mismatches in both class I and II = very big deal
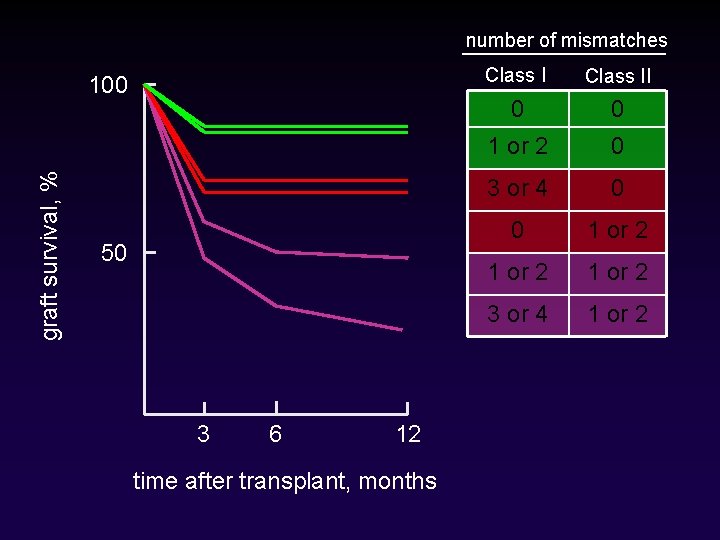
number of mismatches graft survival, % 100 50 3 6 12 time after transplant, months Class II 0 0 1 or 2 0 3 or 4 0 0 1 or 2 3 or 4 1 or 2
Transplant Immunology Outline • Introduction • Graft compatibility • Graft rejection
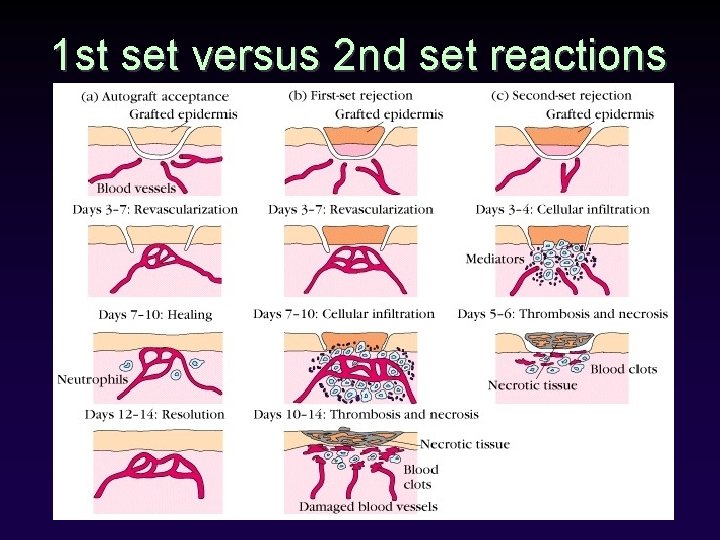
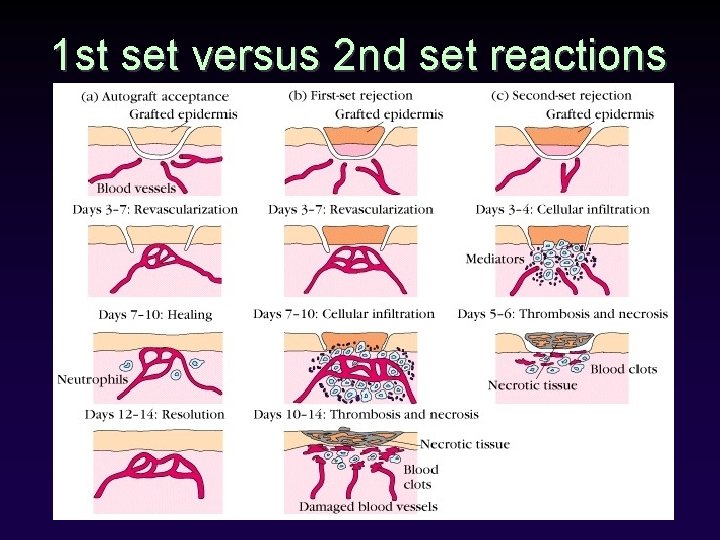
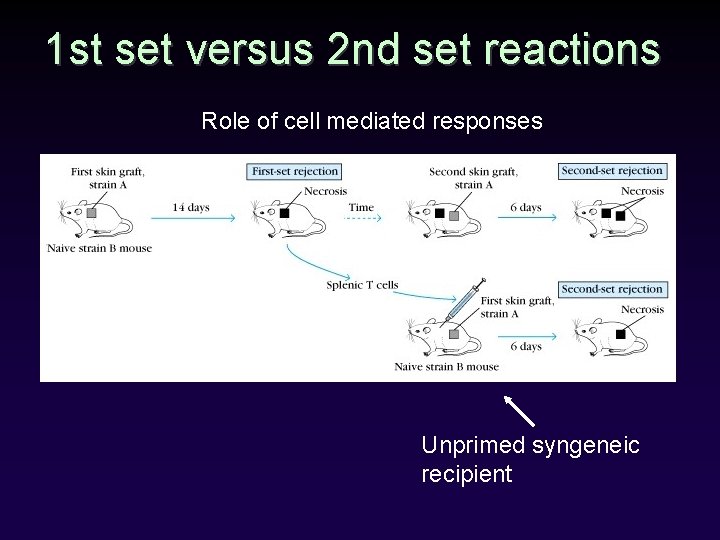
1 st set versus 2 nd set reactions
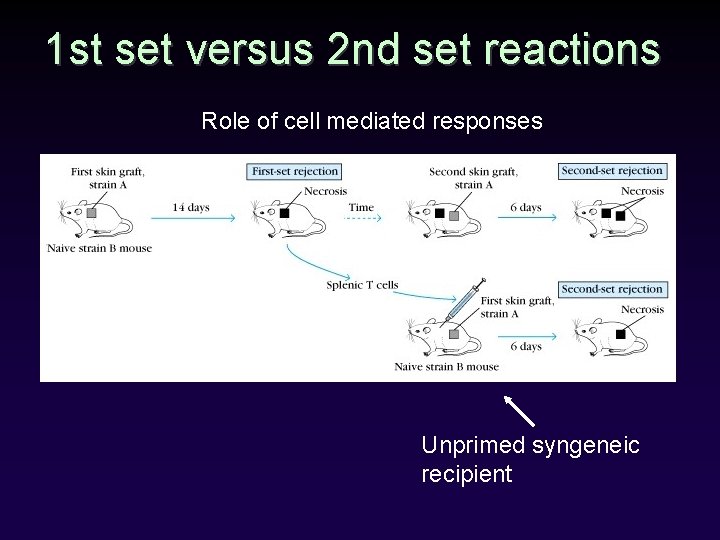
1 st set versus 2 nd set reactions Role of cell mediated responses Unprimed syngeneic recipient
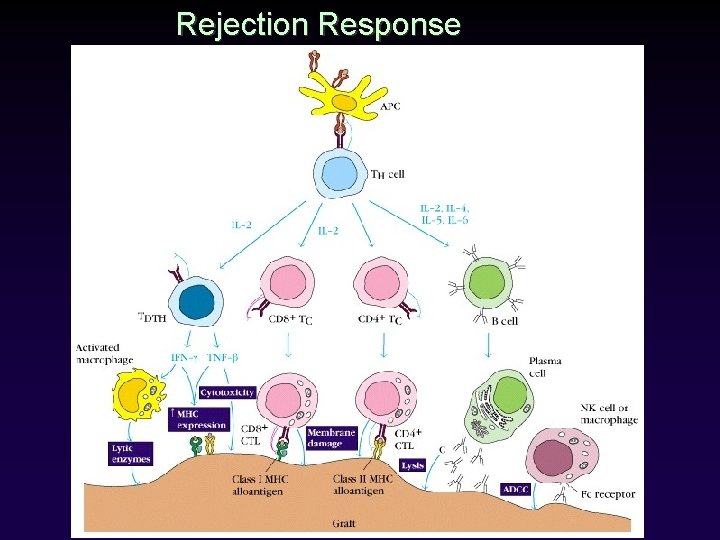
Rejection • Any two people (except identical twins) will express some HLA proteins that are different. • Every recipient will recognize, and react against, at least some foreign antigens in the graft • Rejection is complex, with lots of killing mechanisms.
Rejection How do recipient cells know which cells to kill? • Direct pathway of recognition • Indirect pathway of recognition
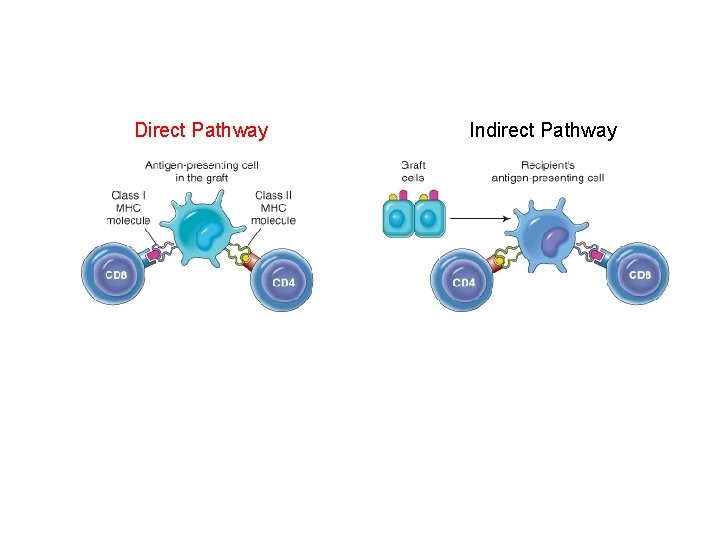
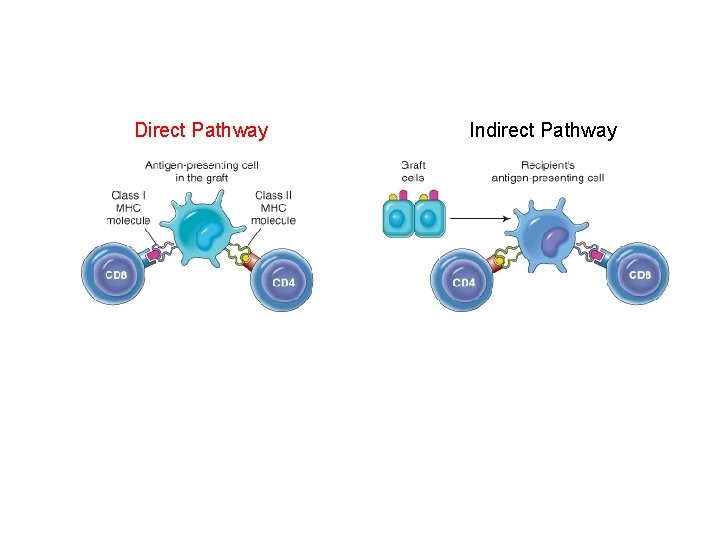
Direct Pathway Indirect Pathway
Rejection Two mechanisms of rejection • T-cell-mediated rejection • Antibody-mediated rejection
Rejection T-cell mediated rejection • CD 8+ CTLs kill graft cells directly • CD 4+ cells trigger a delayed hypersensitivity reaction
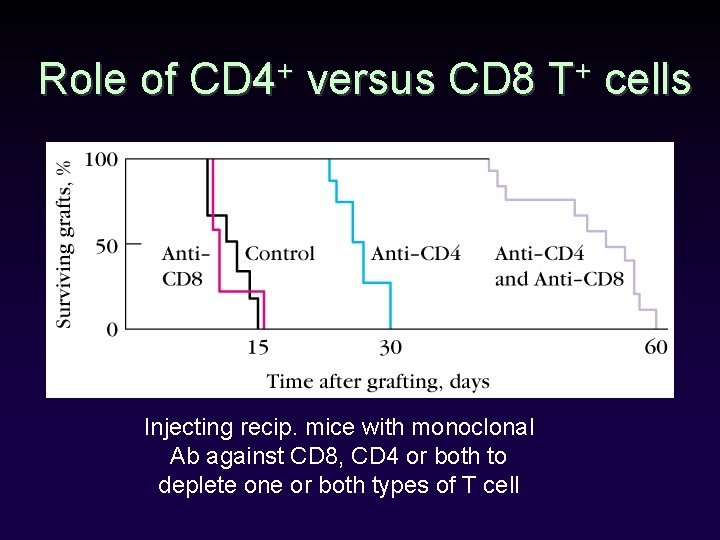
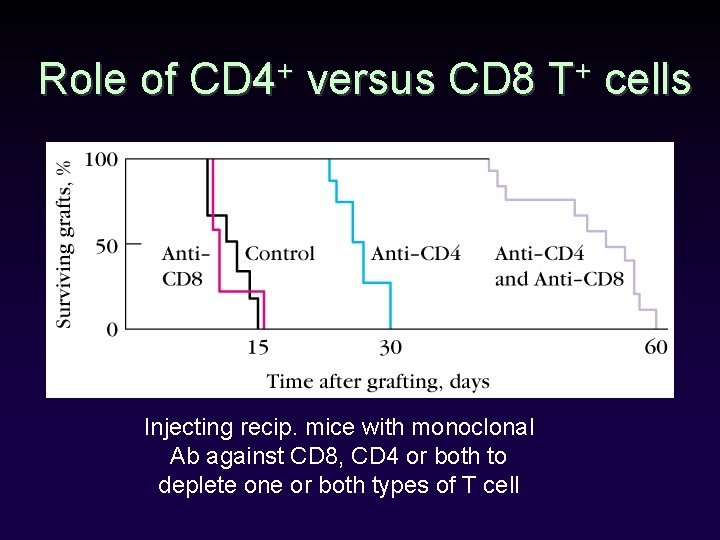
Role of CD 4+ versus CD 8 T+ cells Injecting recip. mice with monoclonal Ab against CD 8, CD 4 or both to deplete one or both types of T cell
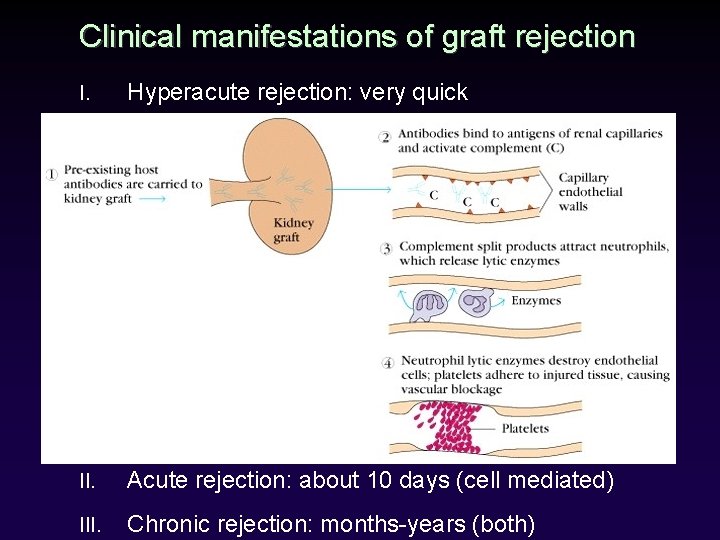
Rejection Clinical types of rejection • Hyperacute rejection • Acute rejection • Chronic rejection
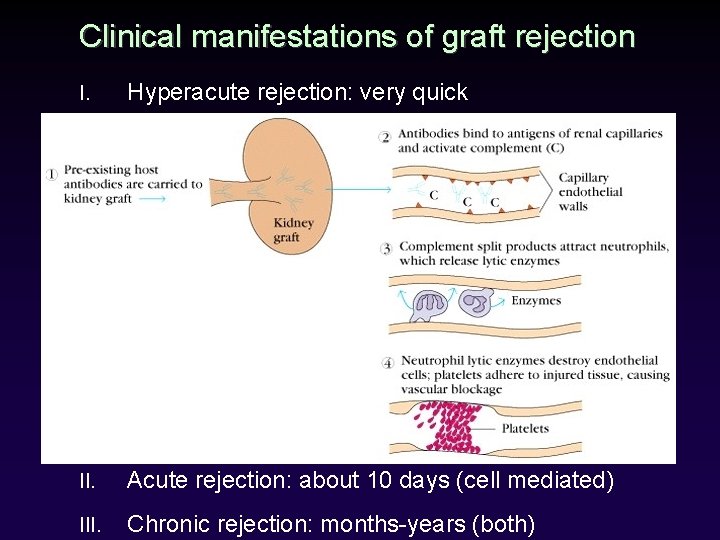
Clinical manifestations of graft rejection I. Hyperacute rejection: very quick II. Acute rejection: about 10 days (cell mediated) III. Chronic rejection: months-years (both)
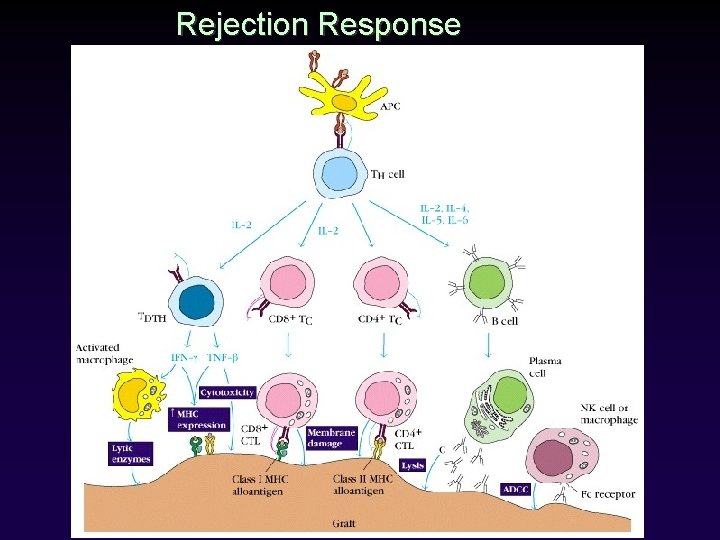
Rejection Response
Transplant Immunology Outline • • Introduction Graft compatibility Graft rejection Types of organ transplantation
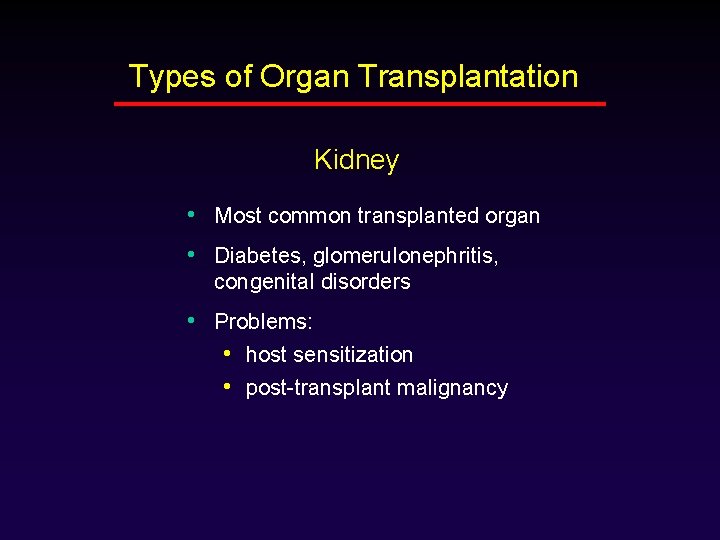
Types of Organ Transplantation Kidney • Most common transplanted organ • Diabetes, glomerulonephritis, congenital disorders • Problems: • host sensitization • post-transplant malignancy
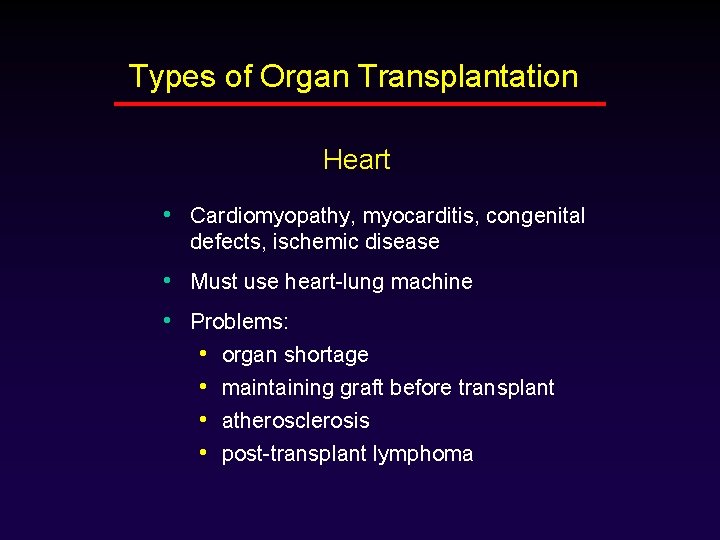
Types of Organ Transplantation Heart • Cardiomyopathy, myocarditis, congenital defects, ischemic disease • Must use heart-lung machine • Problems: • organ shortage • maintaining graft before transplant • atherosclerosis • post-transplant lymphoma
Types of Organ Transplantation Bone marrow • Leukemia, lymphoma • Find living donor (easy) that matches (hard) • Massive chemo/radiation first • Problem: GVHD
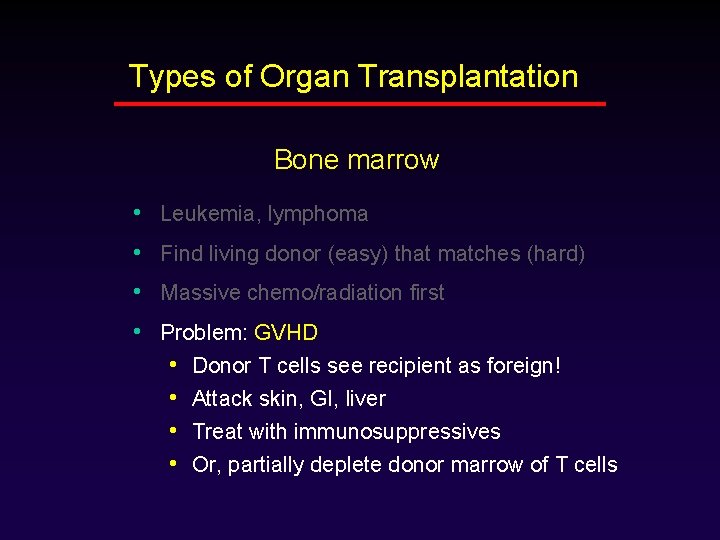
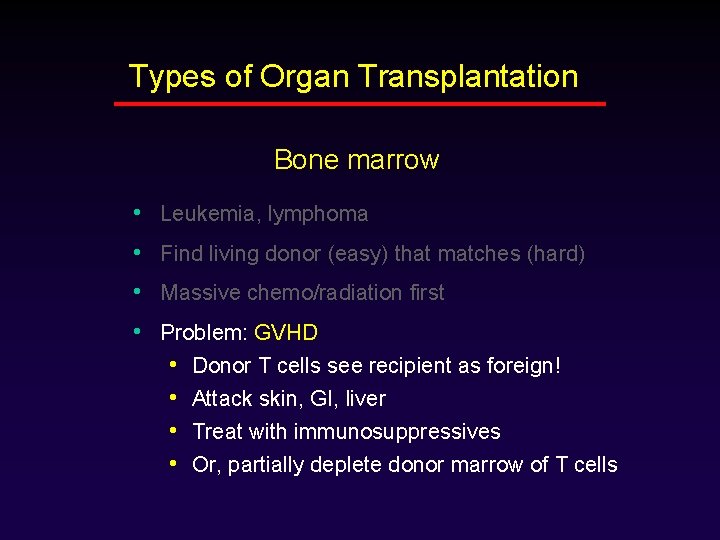
Types of Organ Transplantation Bone marrow • Leukemia, lymphoma • Find living donor (easy) that matches (hard) • Massive chemo/radiation first • Problem: GVHD • Donor T cells see recipient as foreign! • Attack skin, GI, liver • Treat with immunosuppressives • Or, partially deplete donor marrow of T cells
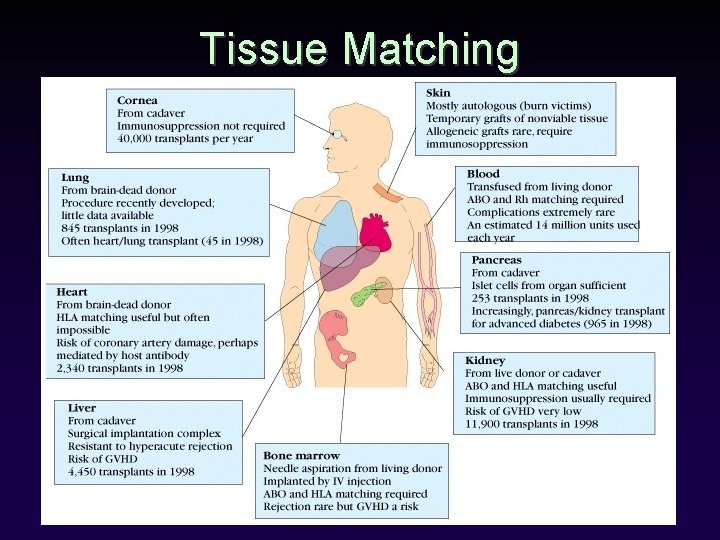
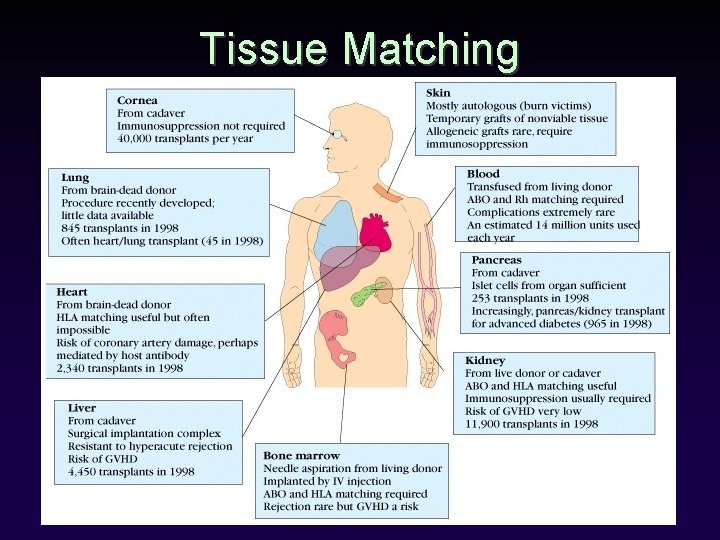
Tissue Matching
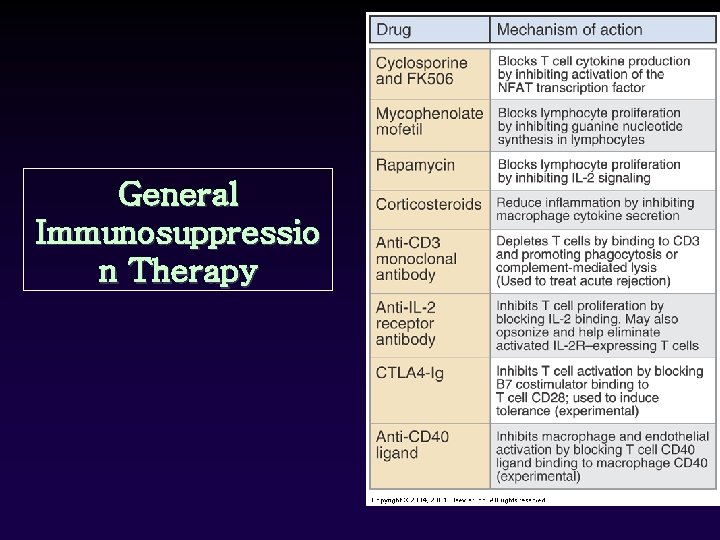
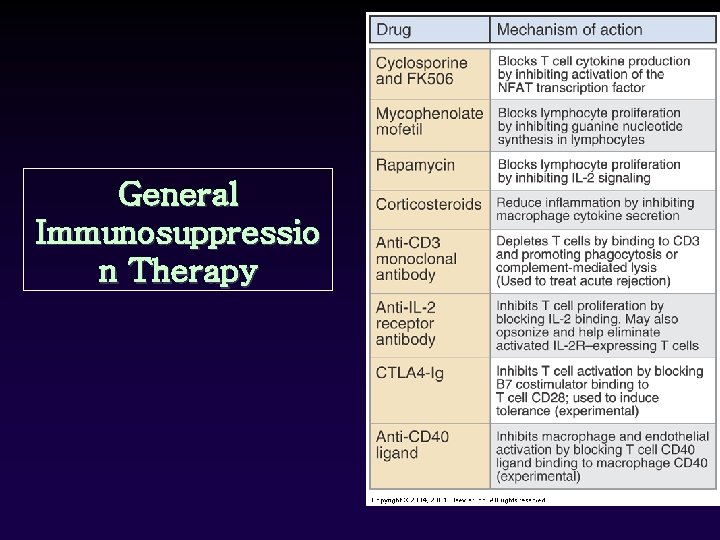
General Immunosuppressio n Therapy
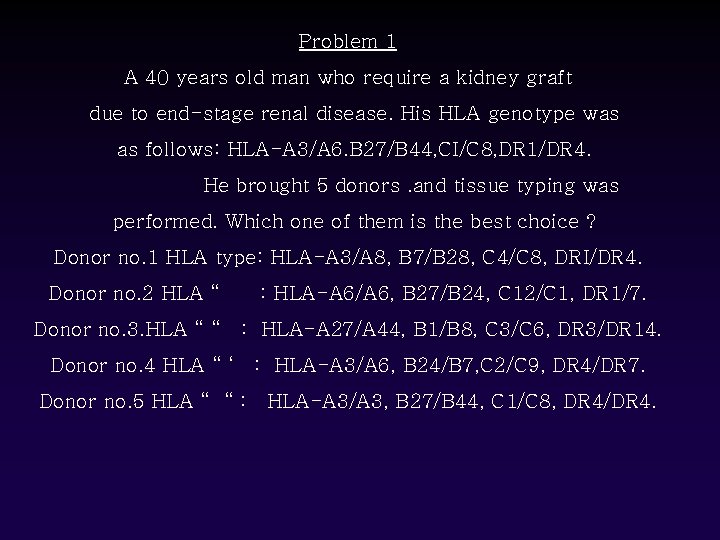
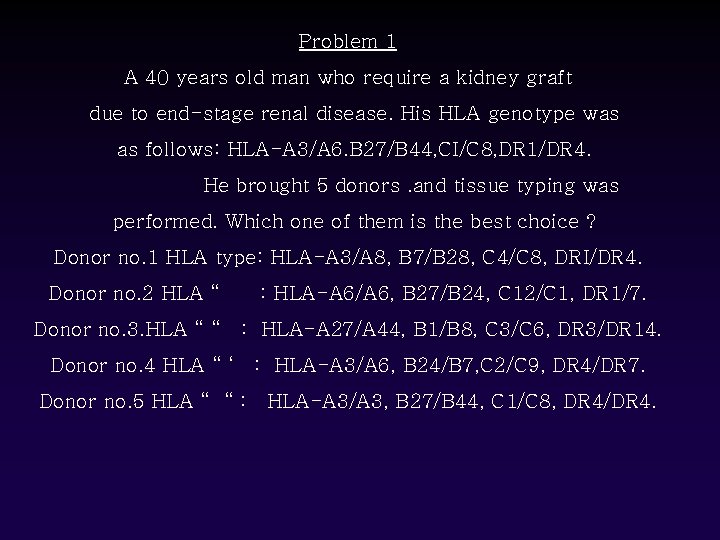
Problem 1 A 40 years old man who require a kidney graft due to end-stage renal disease. His HLA genotype was as follows: HLA-A 3/A 6. B 27/B 44, CI/C 8, DR 1/DR 4. He brought 5 donors. and tissue typing was performed. Which one of them is the best choice ? Donor no. 1 HLA type: HLA-A 3/A 8, B 7/B 28, C 4/C 8, DRI/DR 4. Donor no. 2 HLA “ : HLA-A 6/A 6, B 27/B 24, C 12/C 1, DR 1/7. Donor no. 3. HLA “ “ : HLA-A 27/A 44, B 1/B 8, C 3/C 6, DR 3/DR 14. Donor no. 4 HLA “ ‘ : HLA-A 3/A 6, B 24/B 7, C 2/C 9, DR 4/DR 7. Donor no. 5 HLA “ “ : HLA-A 3/A 3, B 27/B 44, C 1/C 8, DR 4/DR 4.
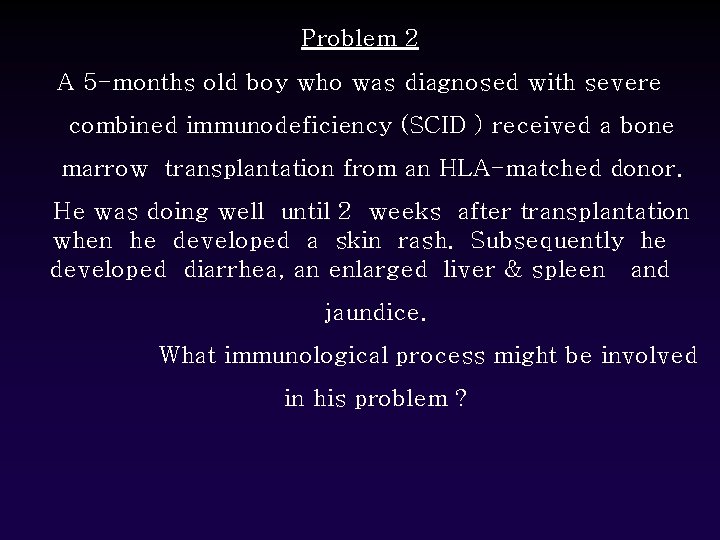
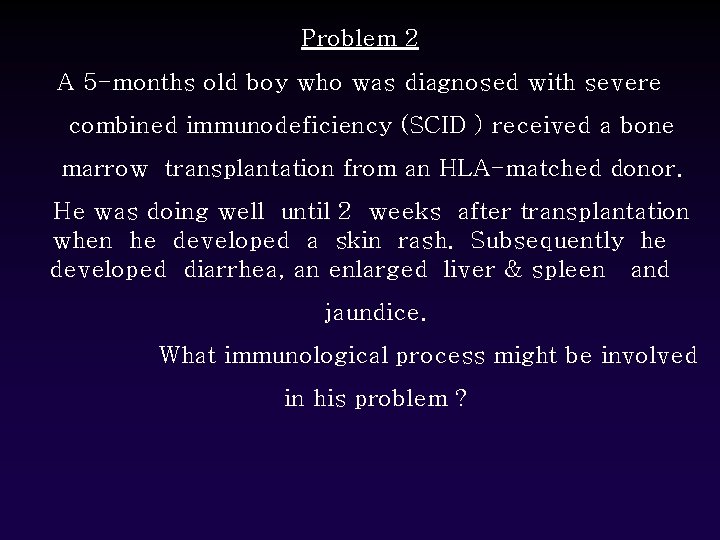
Problem 2 A 5 -months old boy who was diagnosed with severe combined immunodeficiency (SCID ) received a bone marrow transplantation from an HLA-matched donor. He was doing well until 2 weeks after transplantation when he developed a skin rash. Subsequently he developed diarrhea, an enlarged liver & spleen and jaundice. What immunological process might be involved in his problem ?
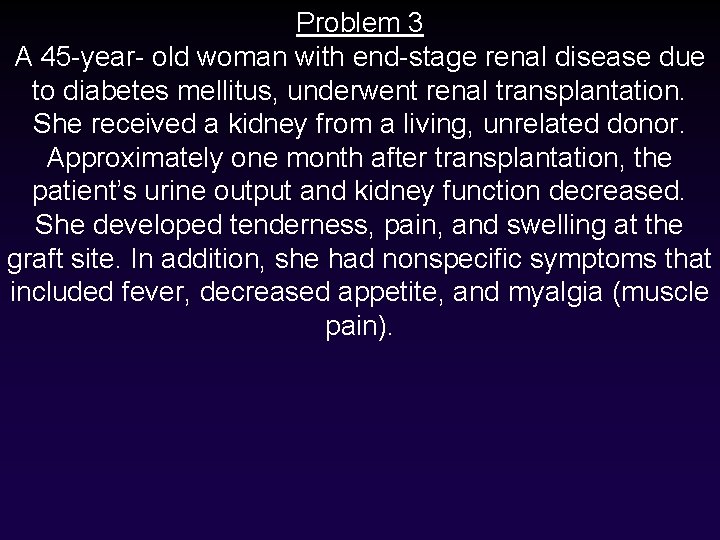
Problem 3 A 45 -year- old woman with end-stage renal disease due to diabetes mellitus, underwent renal transplantation. She received a kidney from a living, unrelated donor. Approximately one month after transplantation, the patient’s urine output and kidney function decreased. She developed tenderness, pain, and swelling at the graft site. In addition, she had nonspecific symptoms that included fever, decreased appetite, and myalgia (muscle pain).
 Patrick evrard transplantation
Patrick evrard transplantation Adel clerus derde stand
Adel clerus derde stand Bone marrow transplantation sri lanka
Bone marrow transplantation sri lanka Perczel adél
Perczel adél Adel nadjaran toosi
Adel nadjaran toosi Adel
Adel Unipolygrafia laite
Unipolygrafia laite Stem cell or bone marrow transplantation thailand
Stem cell or bone marrow transplantation thailand Seiltanz adel karasholi
Seiltanz adel karasholi Calque examples
Calque examples Law of transplantation
Law of transplantation Dr adel ibrahim
Dr adel ibrahim Adel ahmed alalla
Adel ahmed alalla Transplant
Transplant Abbas basic immunology
Abbas basic immunology Servier medical art immunology
Servier medical art immunology Nature reviews immunology
Nature reviews immunology Assisting in microbiology and immunology
Assisting in microbiology and immunology Central tolerance and peripheral tolerance
Central tolerance and peripheral tolerance Ucsd immunology course
Ucsd immunology course Pals immunology
Pals immunology Immunology ppt template
Immunology ppt template Abbas basic immunology
Abbas basic immunology Fraunhofer institute for cell therapy and immunology
Fraunhofer institute for cell therapy and immunology Nature reviews immunology
Nature reviews immunology Sle
Sle Bmc immunology
Bmc immunology Kuby immunology
Kuby immunology Trends in education
Trends in education Eshi diploma
Eshi diploma Avidity in immunology
Avidity in immunology Ras
Ras 17 tc
17 tc American academy of allergy asthma and immunology 2018
American academy of allergy asthma and immunology 2018 Nature reviews immunology
Nature reviews immunology Tumor immunology
Tumor immunology Phagocyte
Phagocyte Pcams immunology
Pcams immunology