Chapter 17 Transplantation Immunology v Transplantation is a


- Slides: 29

Chapter 17 Transplantation Immunology
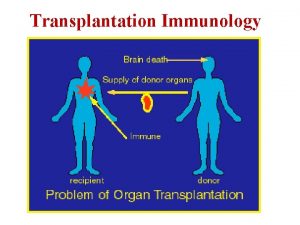
v Transplantation is a widely used treatment for replacement of nonfunctioning organs and tissues with healthy organs or tissues v Technically, transplantation is the process of taking cells, tissues, or organs, called a graft, from one individual and placing them into a (usually) different individual. v The individual who provides the graft is called the donor, and the individual who receives the graft is called either the recipient or the host. v Transfusion refers to the transfer of circulating blood cells or plasma from one individual to another.

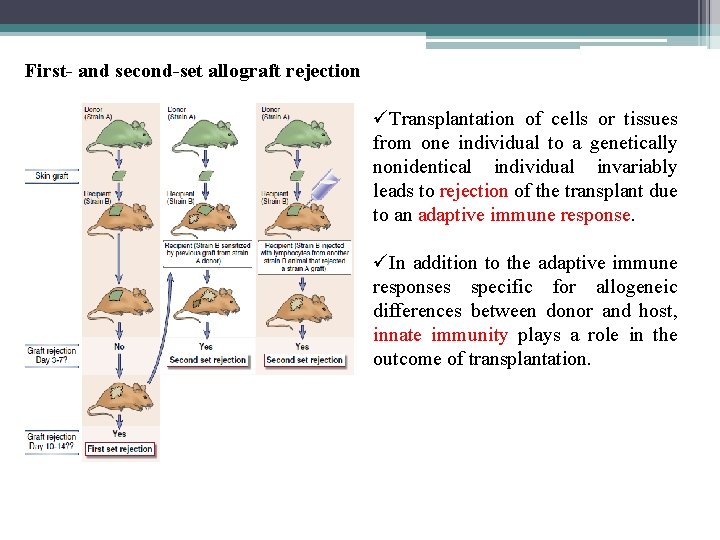
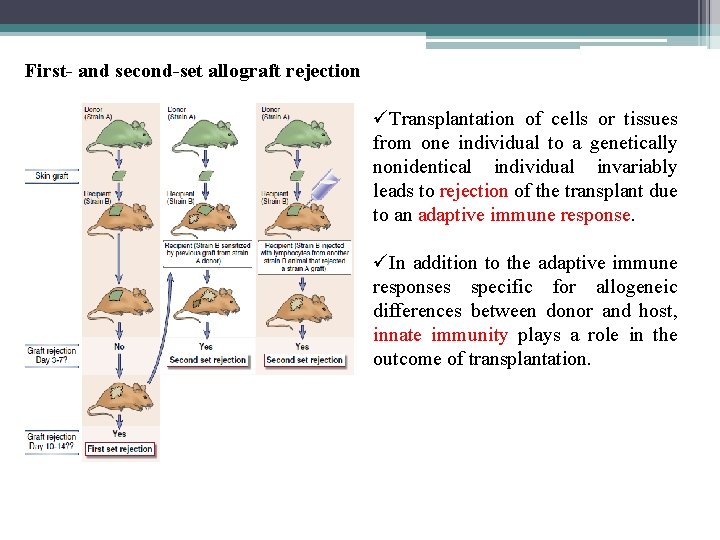
First- and second-set allograft rejection üTransplantation of cells or tissues from one individual to a genetically nonidentical individual invariably leads to rejection of the transplant due to an adaptive immune response. üIn addition to the adaptive immune responses specific for allogeneic differences between donor and host, innate immunity plays a role in the outcome of transplantation.
ü A graft transplanted from one individual to the same individual is called an autologous graft. ü A graft transplanted between two genetically identical individuals is called a syngeneic graft. ü A graft transplanted between two genetically different individuals of the same species is called an allogeneic graft (or allograft). ü A graft transplanted between individuals of different species is called a xenogeneic graft (or xenograft). ü The molecules that are recognized as foreign in allografts are called alloantigens, and those in xenografts are called xenoantigens. ü The lymphocytes and antibodies that react with alloantigens or xenoantigens are described as being alloreactive or xenoreactive, respectively.
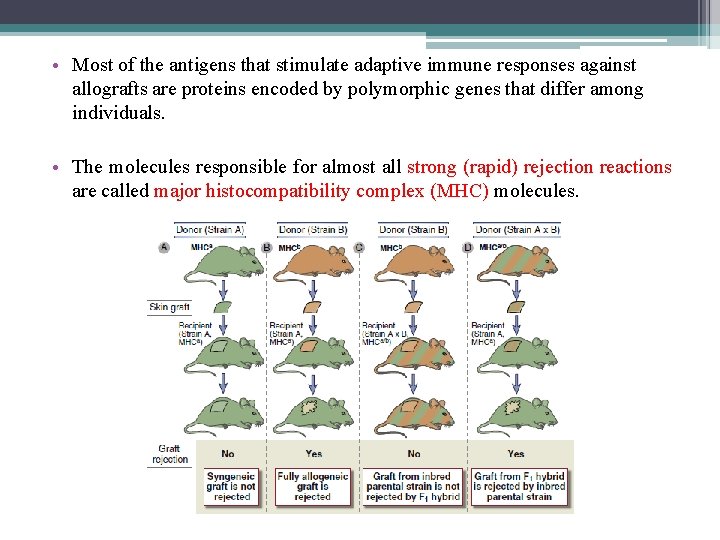
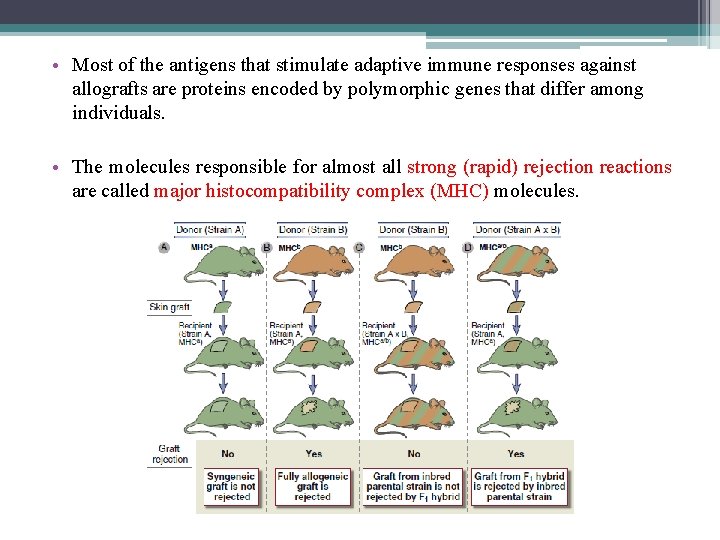
• Most of the antigens that stimulate adaptive immune responses against allografts are proteins encoded by polymorphic genes that differ among individuals. • The molecules responsible for almost all strong (rapid) rejection reactions are called major histocompatibility complex (MHC) molecules.
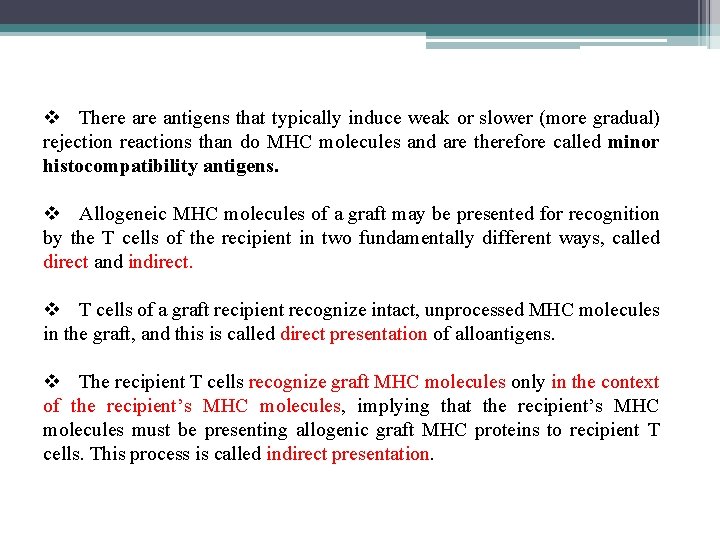
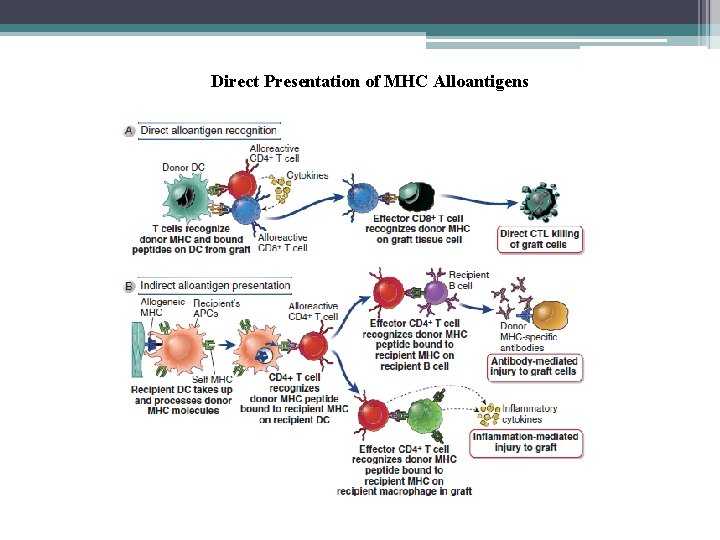
v There antigens that typically induce weak or slower (more gradual) rejection reactions than do MHC molecules and are therefore called minor histocompatibility antigens. v Allogeneic MHC molecules of a graft may be presented for recognition by the T cells of the recipient in two fundamentally different ways, called direct and indirect. v T cells of a graft recipient recognize intact, unprocessed MHC molecules in the graft, and this is called direct presentation of alloantigens. v The recipient T cells recognize graft MHC molecules only in the context of the recipient’s MHC molecules, implying that the recipient’s MHC molecules must be presenting allogenic graft MHC proteins to recipient T cells. This process is called indirect presentation.
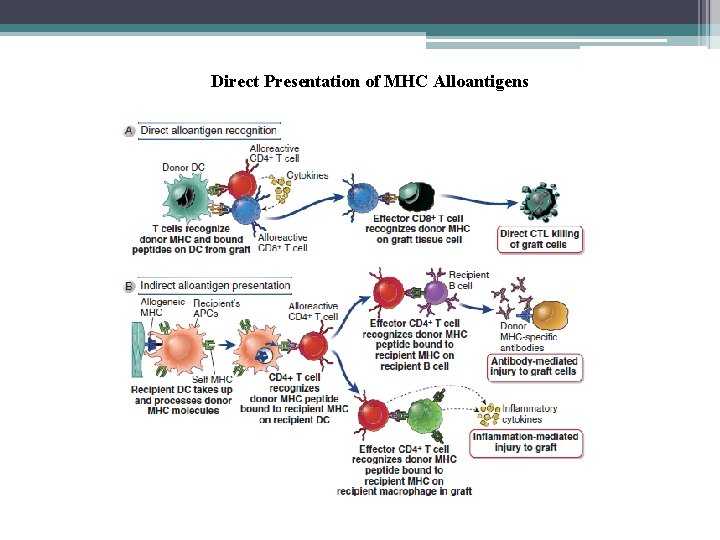
Direct Presentation of MHC Alloantigens
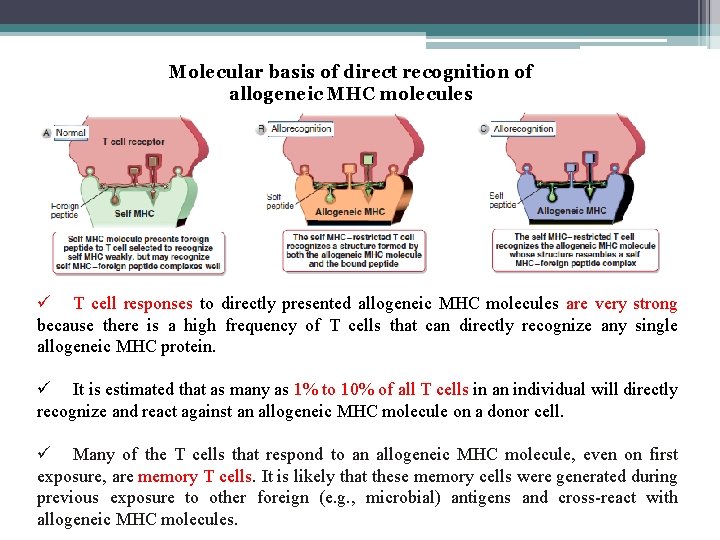
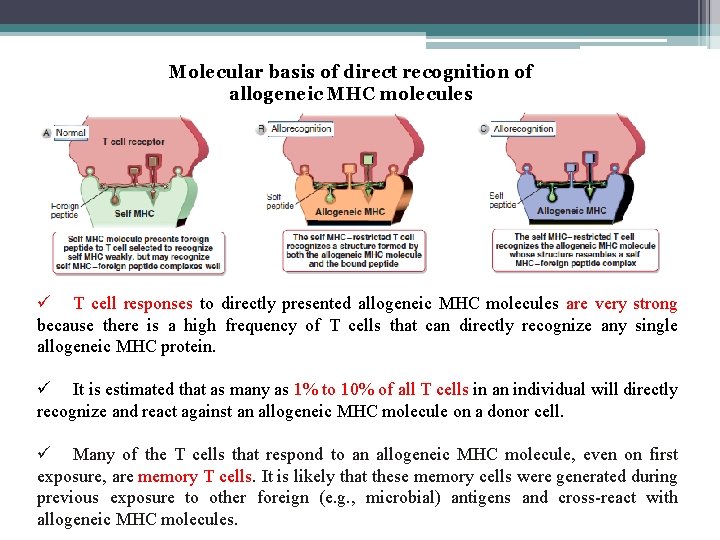
Molecular basis of direct recognition of allogeneic MHC molecules ü T cell responses to directly presented allogeneic MHC molecules are very strong because there is a high frequency of T cells that can directly recognize any single allogeneic MHC protein. ü It is estimated that as many as 1% to 10% of all T cells in an individual will directly recognize and react against an allogeneic MHC molecule on a donor cell. ü Many of the T cells that respond to an allogeneic MHC molecule, even on first exposure, are memory T cells. It is likely that these memory cells were generated during previous exposure to other foreign (e. g. , microbial) antigens and cross-react with allogeneic MHC molecules.
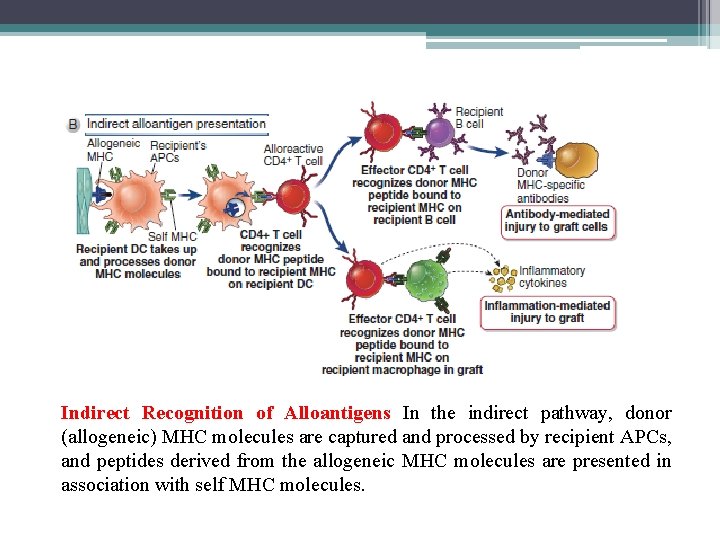
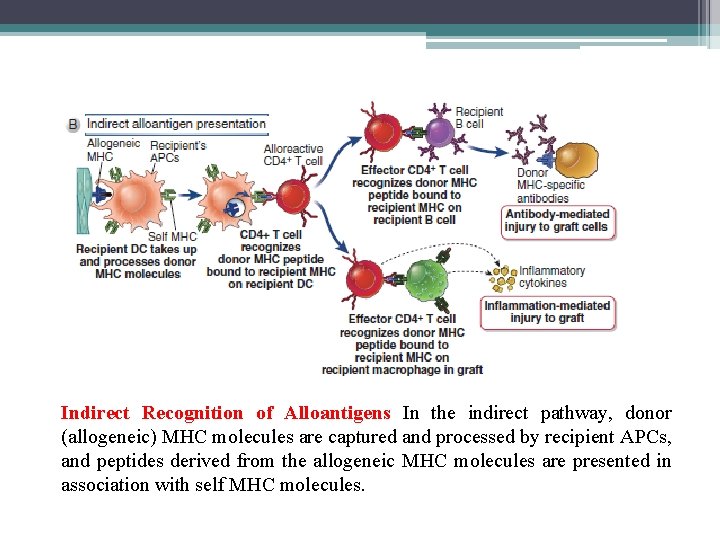
Indirect Recognition of Alloantigens In the indirect pathway, donor (allogeneic) MHC molecules are captured and processed by recipient APCs, and peptides derived from the allogeneic MHC molecules are presented in association with self MHC molecules.
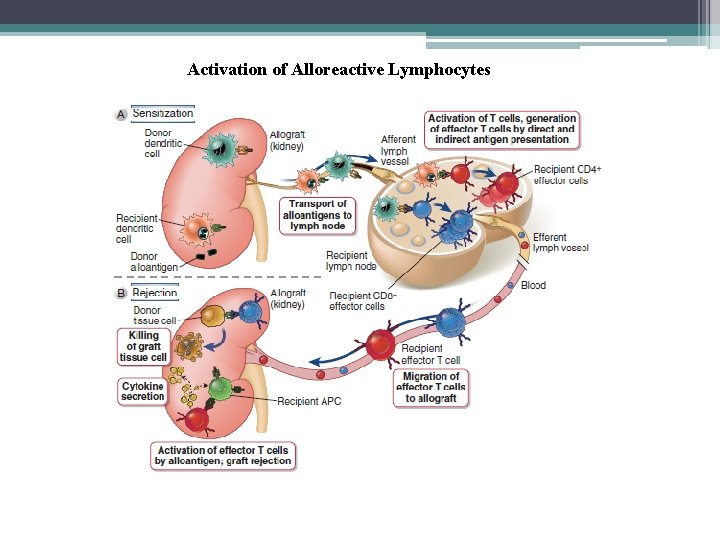
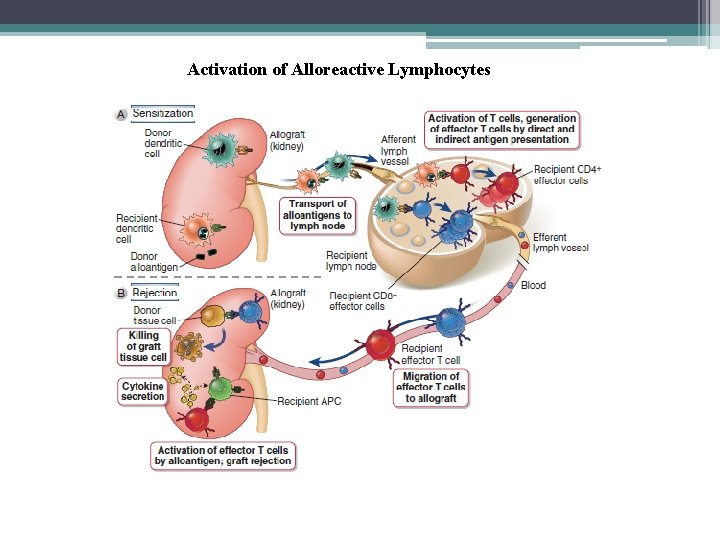
Activation of Alloreactive Lymphocytes
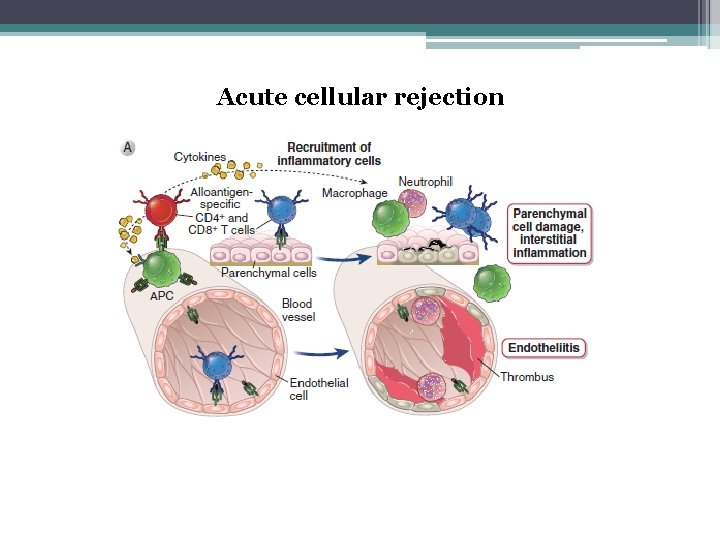
Effector Functions of Alloreactive T Cells ü CD 8+ CTLs that are generated by direct allorecognition of donor MHC molecules can recognize the same MHC molecules on parenchymal cells in the graft and kill those cells. These T cells can also secrete cytokines that cause damaging inflammation. ü In contrast, any CD 8+ CTLs that are generated in response to indirect recognition of allogeneic MHC will not be able to kill the foreign graft cells. ü When CD 4+ effector T cells are generated by direct or indirect recognition of allogeneic MHC, the principal mechanism of rejection is inflammation.
Activation of Alloreactive B Cells and Production and Functions of Alloantibodies ü Naive B lymphocytes recognize the allogenic MHC molecules, internalize and process these proteins, and present peptides derived from them to helper T cells that were previously activated by the same peptides presented by dendritic cells. ü In addition, donor-specific antibodies against non-HLA alloantigens also contribute to rejection. ü The alloreactive antibodies produced in graft recipients engage the same effector mechanisms that antibodies use to combat infections, including complement activation, and Fc receptor-mediated binding and activation of neutrophils, macrophages, and NK cells.
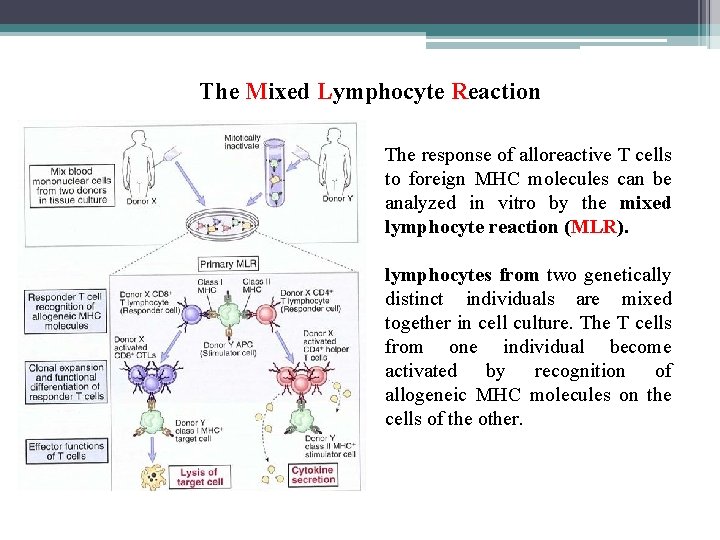
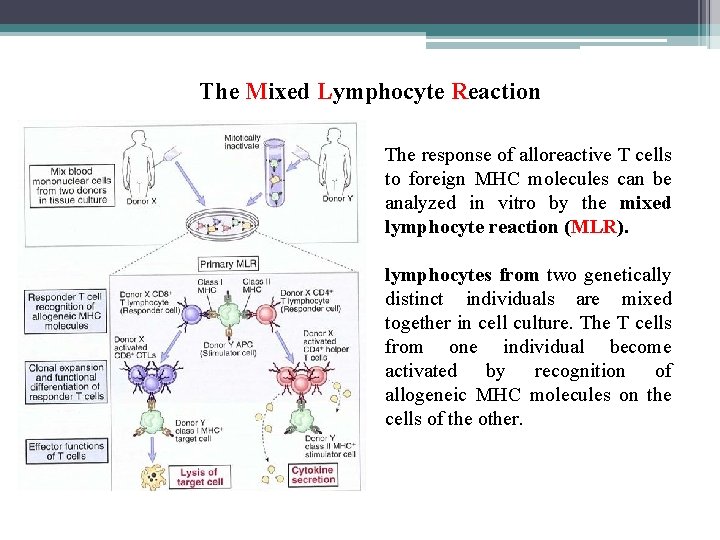
The Mixed Lymphocyte Reaction The response of alloreactive T cells to foreign MHC molecules can be analyzed in vitro by the mixed lymphocyte reaction (MLR). lymphocytes from two genetically distinct individuals are mixed together in cell culture. The T cells from one individual become activated by recognition of allogeneic MHC molecules on the cells of the other.
PATTERNS AND MECHANISMS OF ALLOGRAFT REJECTION v Graft rejection is classified on the basis of histopathologic features and the time course of rejection after transplantation rather than on the basis of immune effector mechanisms. v The histopathologic patterns are called hyperacute, and chronic.
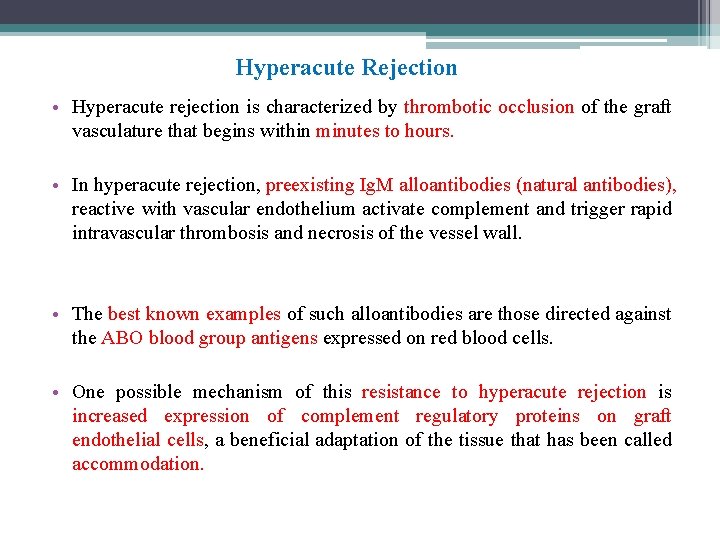
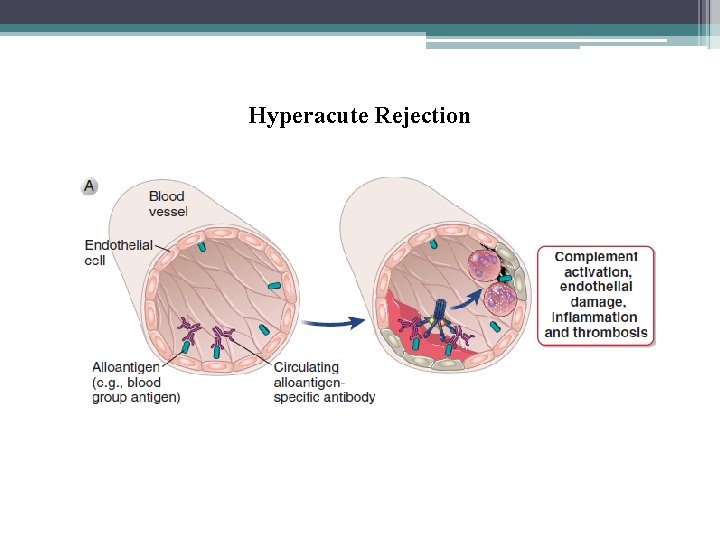
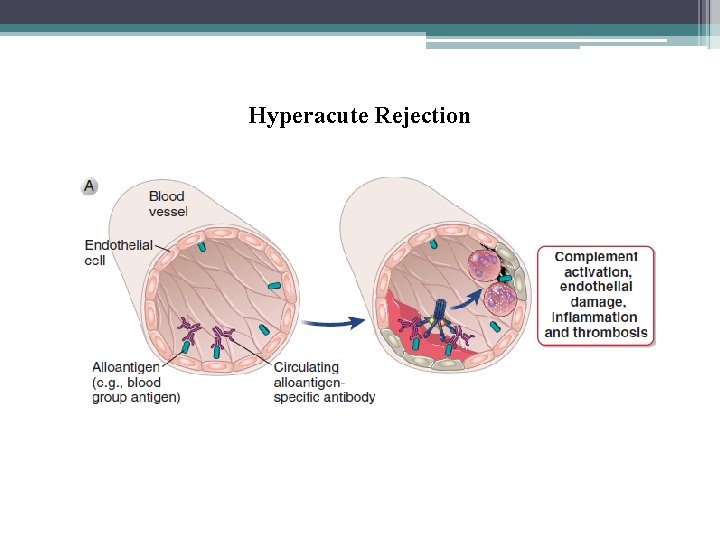
Hyperacute Rejection • Hyperacute rejection is characterized by thrombotic occlusion of the graft vasculature that begins within minutes to hours. • In hyperacute rejection, preexisting Ig. M alloantibodies (natural antibodies), reactive with vascular endothelium activate complement and trigger rapid intravascular thrombosis and necrosis of the vessel wall. • The best known examples of such alloantibodies are those directed against the ABO blood group antigens expressed on red blood cells. • One possible mechanism of this resistance to hyperacute rejection is increased expression of complement regulatory proteins on graft endothelial cells, a beneficial adaptation of the tissue that has been called accommodation.
Hyperacute Rejection
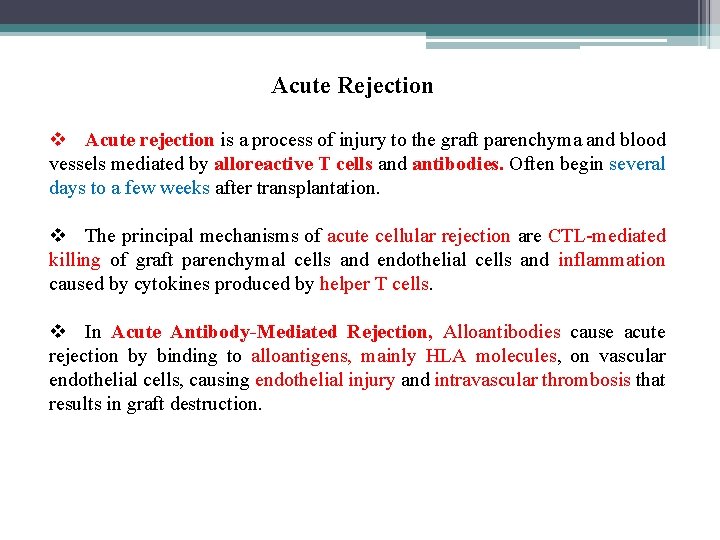
Acute Rejection v Acute rejection is a process of injury to the graft parenchyma and blood vessels mediated by alloreactive T cells and antibodies. Often begin several days to a few weeks after transplantation. v The principal mechanisms of acute cellular rejection are CTL-mediated killing of graft parenchymal cells and endothelial cells and inflammation caused by cytokines produced by helper T cells. v In Acute Antibody-Mediated Rejection, Alloantibodies cause acute rejection by binding to alloantigens, mainly HLA molecules, on vascular endothelial cells, causing endothelial injury and intravascular thrombosis that results in graft destruction.
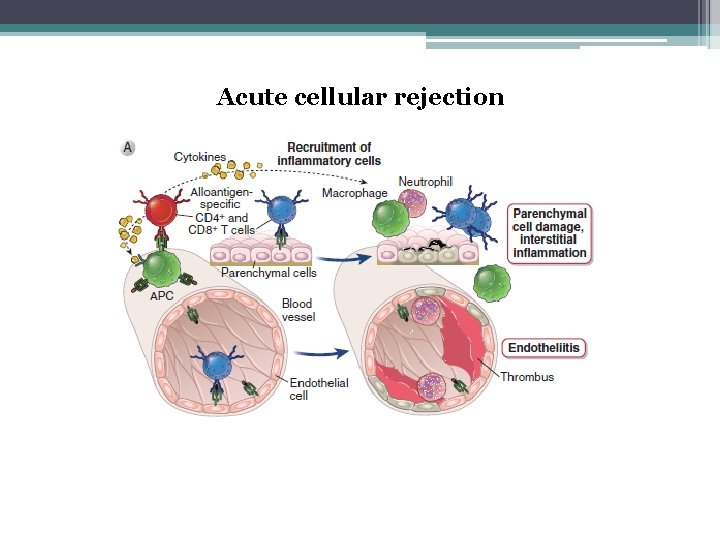
Acute cellular rejection
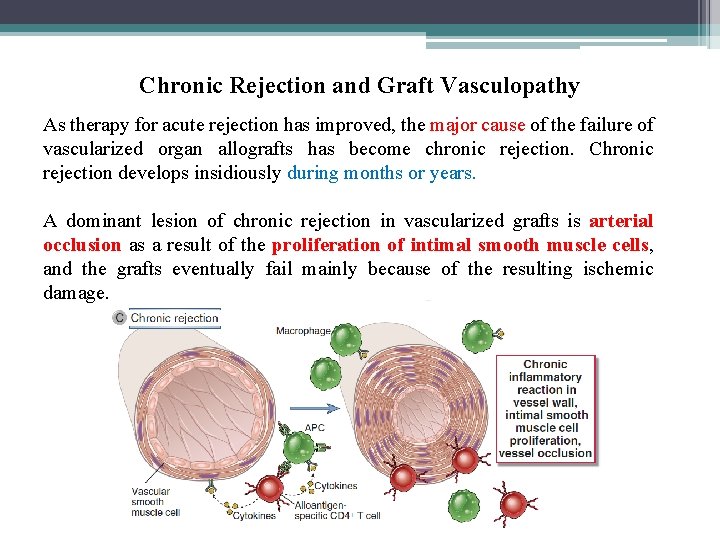
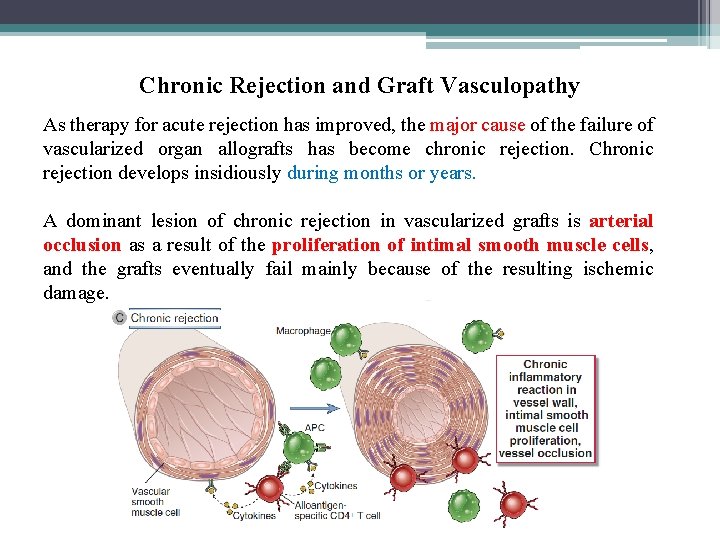
Chronic Rejection and Graft Vasculopathy As therapy for acute rejection has improved, the major cause of the failure of vascularized organ allografts has become chronic rejection. Chronic rejection develops insidiously during months or years. A dominant lesion of chronic rejection in vascularized grafts is arterial occlusion as a result of the proliferation of intimal smooth muscle cells, and the grafts eventually fail mainly because of the resulting ischemic damage.
PREVENTION AND TREATMENT OF ALLOGRAFT REJECTION v Several clinical laboratory tests are routinely performed to reduce the risk for immunologic rejection of allografts. v These include ABO blood typing; the determination of HLA alleles expressed on donor and recipient cells, called tissue typing. v Matching at HLA-A, HLA-B, and HLA-DR is most important for predicting survival of kidney allografts. v The detection of preformed antibodies in the recipient that recognize HLA and other antigens representative of the donor population. v The detection of preformed antibodies in the recipient that bind to antigens of an identified donor’s cells, called crossmatching.
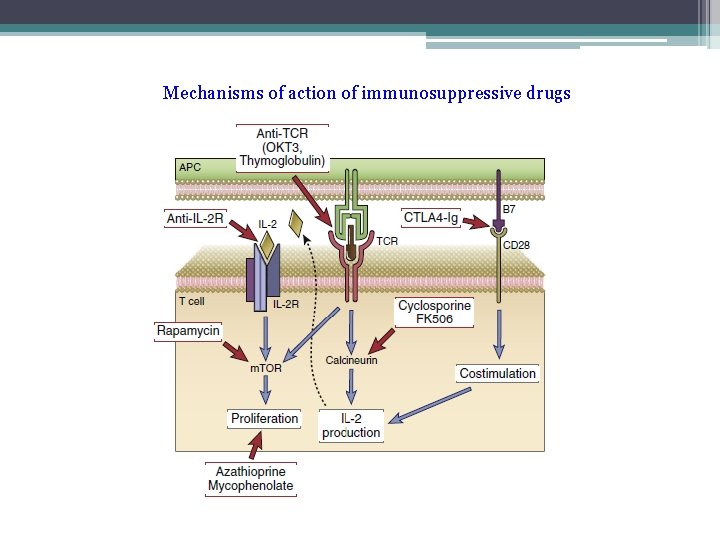
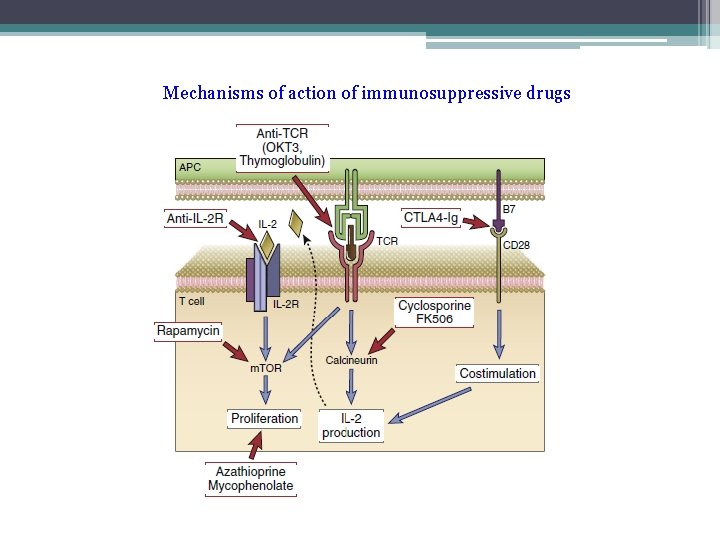
Mechanisms of action of immunosuppressive drugs
XENOGENEIC TRANSPLANTATION v A major immunologic barrier to xenogeneic transplantation is the presence of natural antibodies that cause hyperacute rejection. v Some of the complement regulatory proteins made by pig cells are not able to interact with human complement proteins and thus cannot limit the extent of injury induced by the human complement system. v Xenografts can also be rejected by T cell–mediated immune responses to xenoantigens.
BLOOD TRANSFUSION AND THE ABO AND Rh BLOOD GROUP ANTIGENS v The major barrier to successful blood transfusions is the immune response to cell surface molecules that differ between individuals. v The most important alloantigen system in blood transfusion is the ABO system. v Individuals who do not express a particular blood group antigen produce natural Ig. M antibodies against that antigen. v The preexisting antibodies bind to the transfused cells, activate complement, and cause transfusion reactions, which can be lifethreatening.
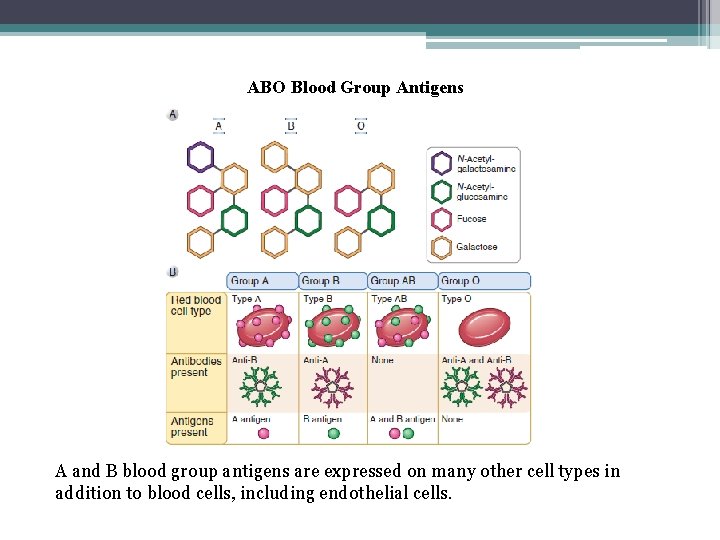
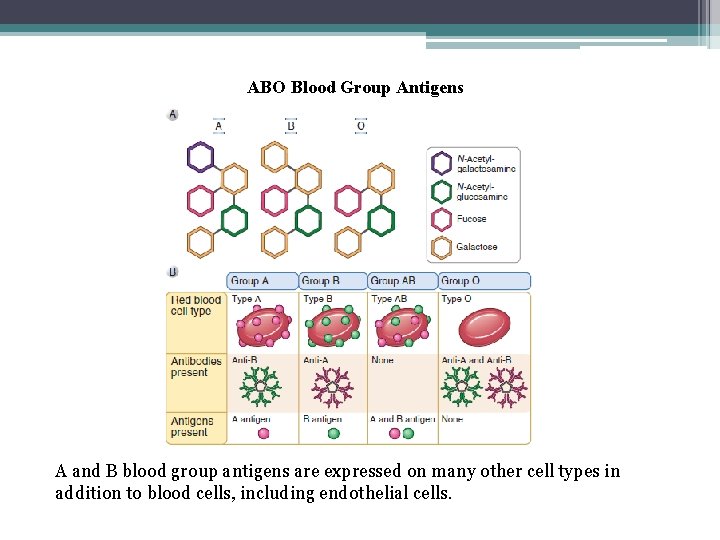
ABO Blood Group Antigens A and B blood group antigens are expressed on many other cell types in addition to blood cells, including endothelial cells.
Rhesus (Rh) Antigen • Rh antigens are nonglycosylated, hydrophobic cell surface proteins found in red blood cell membranes and are structurally related to other red cell membrane glycoproteins with transporter functions. • Rh proteins are encoded by two tightly linked and highly homologous genes, but only one of them, called Rh. D, is commonly considered in clinical blood typing. • The major clinical significance of anti-Rh antibodies is related to hemolytic reactions associated with pregnancy that are similar to transfusion reactions. • Subsequent pregnancies in which the fetus is Rh positive are at risk because the maternal anti-Rh antibodies can cross the placenta and mediate the destruction of the fetal red blood cells. This causes erythroblastosis fetalis (hemolytic disease of the newborn) and can be lethal for the fetus.
HEMATOPOIETIC STEM CELL TRANSPLANTATION • Examples of such diseases that can be cured by hematopoietic stem cell transfer are adenosine deaminase (ADA) deficiency, X-linked severe combined immunodeficiency disease, and hemoglobin mutations such as beta-thalassemia major and sickle cell disease. • Allogeneic hematopoietic stem cells are rejected by even a minimally immunocompetent host, and therefore the donor and recipient must be carefully matched at all MHC loci. • The mechanisms of rejection of bone marrow cells are not completely known, but in addition to adaptive immune mechanisms, hematopoietic stem cells may be rejected by NK cells
Graft-Versus-Host Disease (GVHD) • GVHD is caused by the reaction of grafted mature T cells in the marrow inoculum with alloantigens of the host. • Acute GVHD is characterized by epithelial cell death in the skin, liver and gastrointestinal tract. It is manifested clinically by rash, jaundice, diarrhea, and gastrointestinal hemorrhage. When the epithelial cell death is extensive, the skin or lining of the gut may slough off. In this circumstance, acute GVHD may be fatal. • Chronic GVHD is characterized by fibrosis and atrophy of one or more of the same organs, without evidence of acute cell death. Chronic GVHD may also involve the lungs and produce obliteration of small airways. When it is severe, chronic GVHD leads to complete dysfunction of the affected organ.
Immunodeficiency After Bone Marrow Transplantation • Radiation therapy and chemotherapy used to prepare recipients for transplantation are likely to deplete the patient’s memory cells and longlived plasma cells, • Recipients are susceptible to viral infections, especially cytomegalovirus infection, and to many bacterial and fungal infections • They are also susceptible to Epstein-Barr virus–provoked B cell lymphomas • Recipients commonly receive prophylactic antibiotics and anticytomegalovirus therapy and are often actively immunized against capsular bacteria such as pneumococcus before transplantation.
 Bone marrow transplantation sri lanka
Bone marrow transplantation sri lanka Law of transplantation
Law of transplantation Patrick evrard transplantation
Patrick evrard transplantation Cultural transposition
Cultural transposition How does a kidney transplant work
How does a kidney transplant work Stem cell or bone marrow transplantation thailand
Stem cell or bone marrow transplantation thailand History of immunology
History of immunology Antigen antibody
Antigen antibody Cellular and molecular immunology
Cellular and molecular immunology Lupus
Lupus Braverman reproductive immunology
Braverman reproductive immunology Cells
Cells Abbas basic immunology
Abbas basic immunology Immunology diploma
Immunology diploma Pcams immunology
Pcams immunology Assisting in microbiology and immunology
Assisting in microbiology and immunology Baltimore classification
Baltimore classification Ras
Ras Neutrophil extracellular traps
Neutrophil extracellular traps Immunology ppt template
Immunology ppt template Trends in education
Trends in education Nature reviews immunology
Nature reviews immunology Pals immunology
Pals immunology Kuby immunology
Kuby immunology Tumor immunology
Tumor immunology Nature reviews immunology
Nature reviews immunology Fraunhofer institute for cell therapy and immunology
Fraunhofer institute for cell therapy and immunology Avidity in immunology
Avidity in immunology Wiki
Wiki Ucsd immunology course
Ucsd immunology course