39 Immunology Animal Defense Systems Chapter 39 Immunology

















- Slides: 104
39 Immunology: Animal Defense Systems
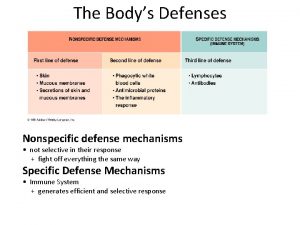
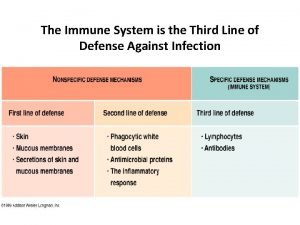
Chapter 39 Immunology: Animal Defense Systems Key Concepts 39. 1 Animals Use Innate and Adaptive Mechanisms to Defend Themselves against Pathogens 39. 2 Innate Defenses Are Nonspecific 39. 3 The Adaptive Immune Response Is Specific 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors
Chapter 39 Opening Question How can a person survive an infection and be resistant to further infection?
Concept 39. 1 Animals Use Innate and Adaptive Mechanisms to Defend Themselves against Pathogens Animals have various means of defense against pathogens—organisms or viruses that can cause disease. These defenses are based on the distinction between self—the animal’s own molecules— and nonself, or foreign, molecules.
Concept 39. 1 Animals Use Innate and Adaptive Mechanisms to Defend Themselves against Pathogens Response to invaders occurs in three phases: • Recognition phase: The animal must be able to discriminate between self and nonself. • Activation phase: Mobilization of cells and molecules to fight the invader. • Effector phase: Mobilized cells and molecules destroy the invader.
Concept 39. 1 Animals Use Innate and Adaptive Mechanisms to Defend Themselves against Pathogens Two categories of defenses: • Innate defenses—nonspecific, 1 st line of defense, rapid response § § Include physical barriers such as skin, molecules toxic to invaders, and phagocytic cells that ingest invaders Some are present all the time, others can be activated quickly
Concept 39. 1 Animals Use Innate and Adaptive Mechanisms to Defend Themselves against Pathogens • Adaptive defenses—aimed at specific pathogens; activated by innate systems § § Slower to develop and long lasting Example: Cells make antibodies— proteins that will recognize, bind to, and aid in the destruction of specific pathogens
Concept 39. 1 Animals Use Innate and Adaptive Mechanisms to Defend Themselves against Pathogens Immunity: when an organism has sufficient defenses to successfully avoid biological invasion by a pathogen
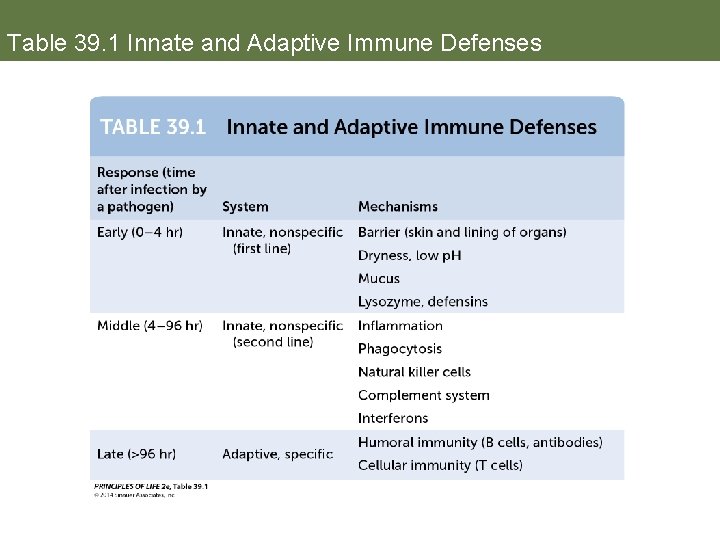
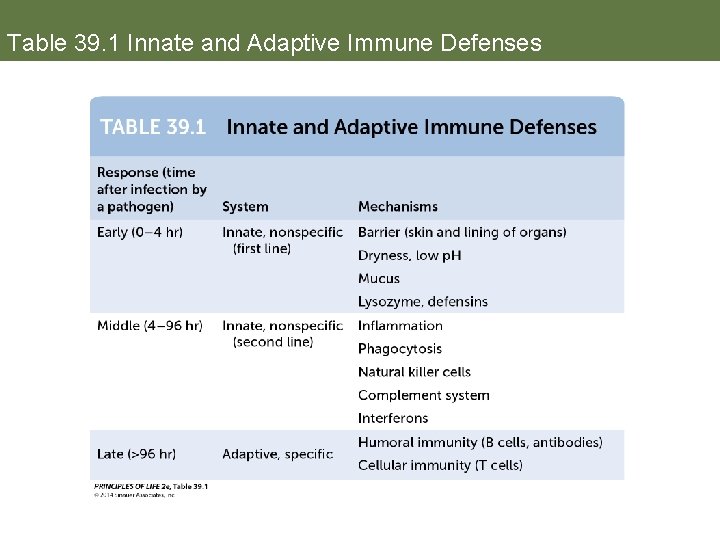
Table 39. 1 Innate and Adaptive Immune Defenses
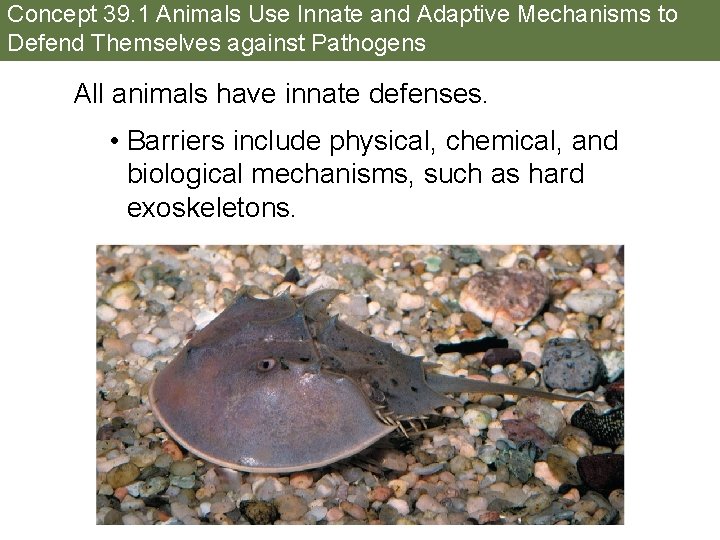
Concept 39. 1 Animals Use Innate and Adaptive Mechanisms to Defend Themselves against Pathogens All animals have innate defenses. • Barriers include physical, chemical, and biological mechanisms, such as hard exoskeletons.
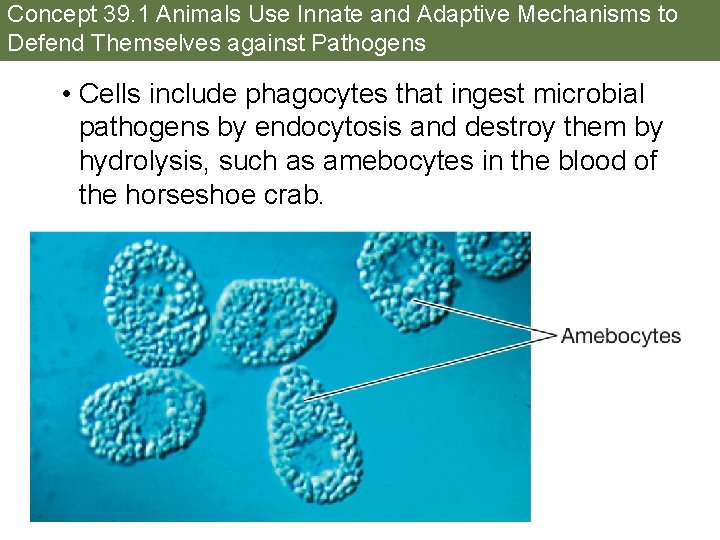
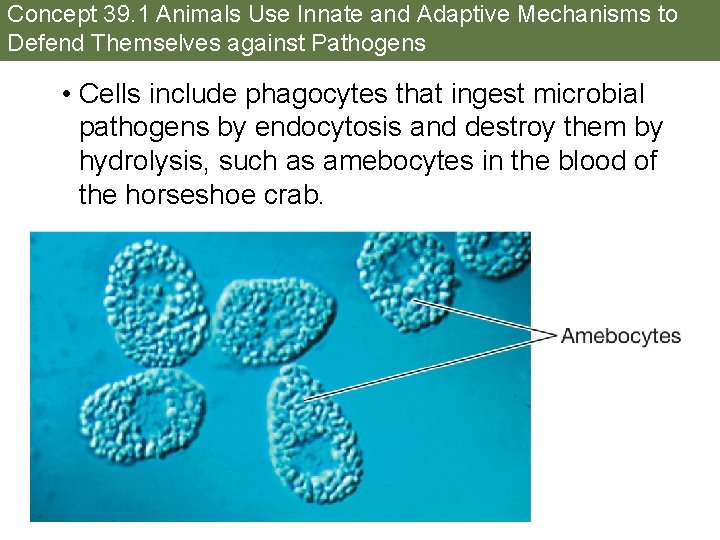
Concept 39. 1 Animals Use Innate and Adaptive Mechanisms to Defend Themselves against Pathogens • Cells include phagocytes that ingest microbial pathogens by endocytosis and destroy them by hydrolysis, such as amebocytes in the blood of the horseshoe crab.

Concept 39. 1 Animals Use Innate and Adaptive Mechanisms to Defend Themselves against Pathogens • Toxic molecules: horseshoe crab blood cells release molecules that can disrupt bacterial cell membranes or bind to bacterial surfaces and cross-link them.
Concept 39. 1 Animals Use Innate and Adaptive Mechanisms to Defend Themselves against Pathogens Vertebrates have both innate and adaptive defense systems—they work together as a coordinated system. The main factors in immunity are specific cells and proteins. • These cells are produced in the blood and lymphoid tissues and circulate throughout the body.
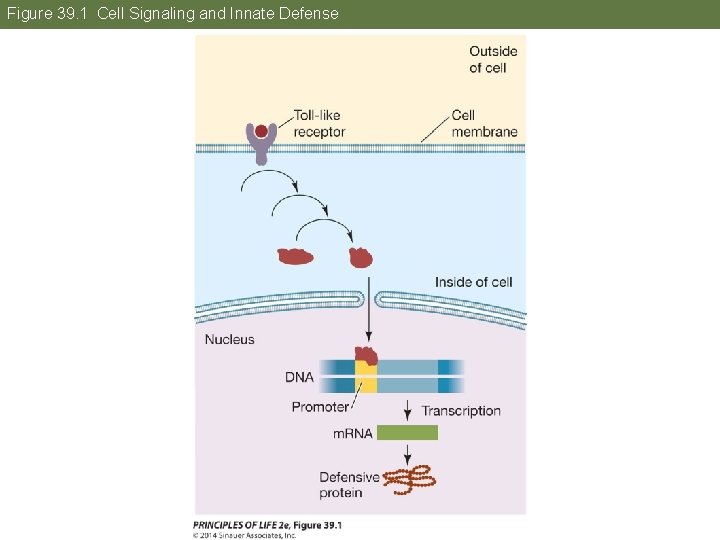
Concept 39. 1 Animals Use Innate and Adaptive Mechanisms to Defend Themselves against Pathogens The recognition and activation phases of innate immunity evolved very early in animals. Animals from humans to fruit flies have Toll-like receptors that recognize and bind to pathogen molecules, such as components of the bacterial cell wall. Binding sets off a signal transduction pathway that ends with expression of genes for antipathogen molecules.
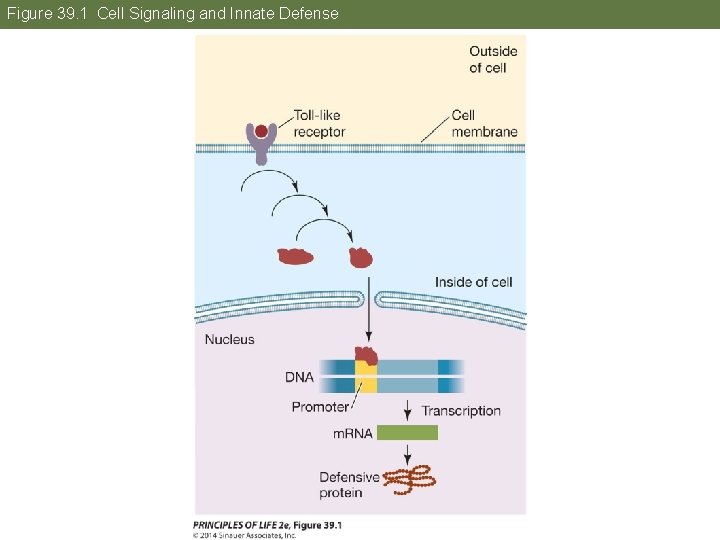
Figure 39. 1 Cell Signaling and Innate Defense

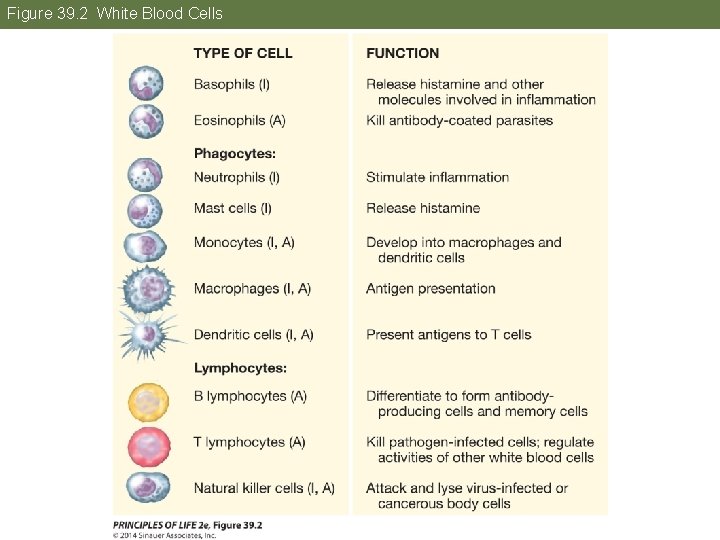
Concept 39. 1 Animals Use Innate and Adaptive Mechanisms to Defend Themselves against Pathogens White blood cells (leukocytes): • Phagocytes—large cells that engulf pathogens and other substances by phagocytosis • Lymphocytes—B cells and T cells are involved in adaptive immunity; natural killer cells are involved in both innate and adaptive immunity
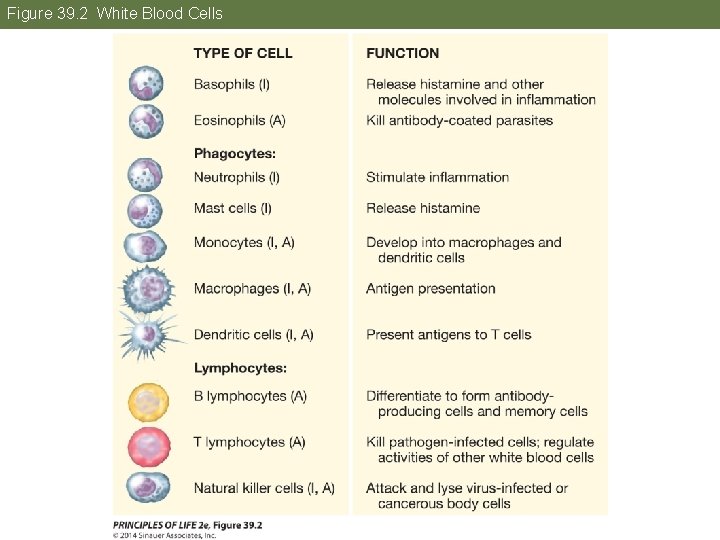
Figure 39. 2 White Blood Cells
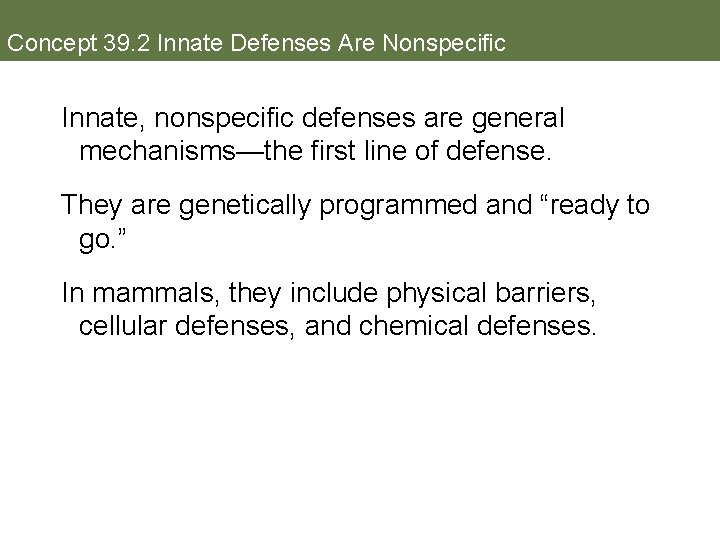
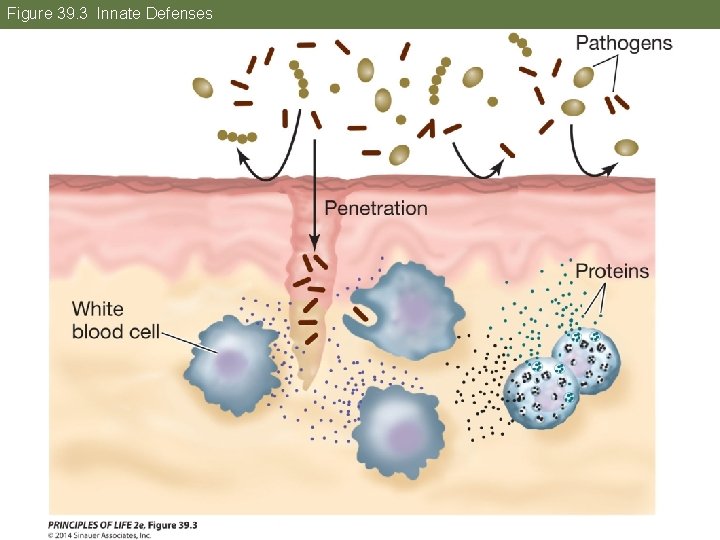
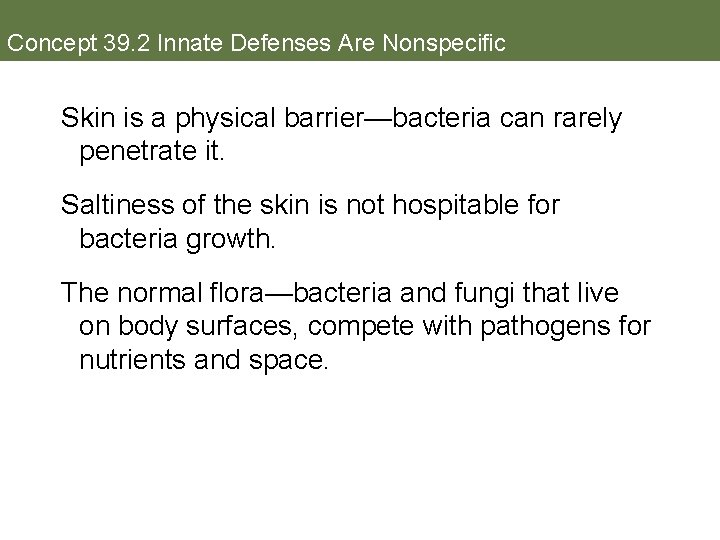
Concept 39. 2 Innate Defenses Are Nonspecific Innate, nonspecific defenses are general mechanisms—the first line of defense. They are genetically programmed and “ready to go. ” In mammals, they include physical barriers, cellular defenses, and chemical defenses.
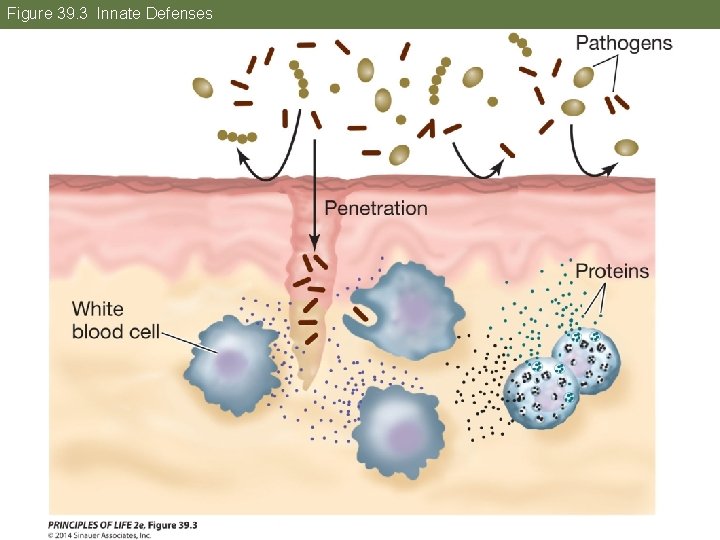
Figure 39. 3 Innate Defenses
Concept 39. 2 Innate Defenses Are Nonspecific Skin is a physical barrier—bacteria can rarely penetrate it. Saltiness of the skin is not hospitable for bacteria growth. The normal flora—bacteria and fungi that live on body surfaces, compete with pathogens for nutrients and space.

Concept 39. 2 Innate Defenses Are Nonspecific Mucus secreted by mucous membranes traps microorganisms. Beating of cilia continuously move the mucus and debris towards the outside of the body, such as in the respiratory tract. Lysozyme in mucus attacks bacterial cell walls and causes them to lyse.
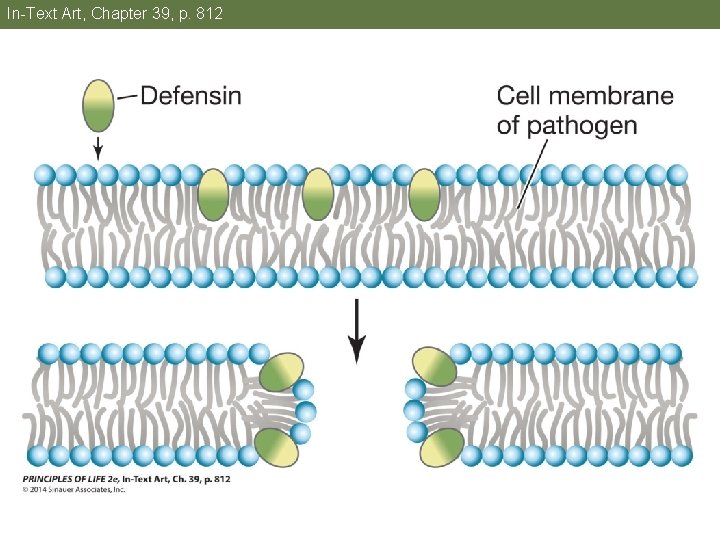
Concept 39. 2 Innate Defenses Are Nonspecific Mucous membranes also produce defensins, peptides with hydrophobic domains that are toxic to many pathogens. • Defensins insert themselves into the plasma membrane of the pathogen and make it permeable to water and solutes. • Defensins are also made in phagocytes, where they kill pathogens trapped by phagocytosis.
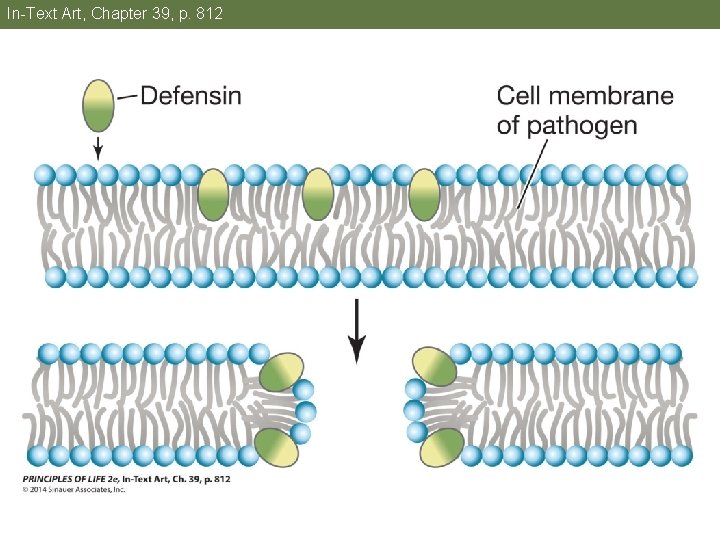
In-Text Art, Chapter 39, p. 812
Concept 39. 2 Innate Defenses Are Nonspecific Harsh conditions in the internal environment, can also kill pathogens; for example, the acids in the stomach.
Concept 39. 2 Innate Defenses Are Nonspecific Pathogens that do penetrate the body surfaces encounter more innate defenses. Activation of defensive cells; involves recognition of nonself molecules by pattern recognition receptors (PRRs) on phagocytes and natural killer cells. • Toll-like receptors are PRRs.
Concept 39. 2 Innate Defenses Are Nonspecific Molecules recognized by PRRs are pathogen associated molecular patterns (PAMPs)— molecules unique to classes of microbes, such as bacterial flagellin and fungal chitin. Binding of PAMPs to PRRs stimulates signal transduction pathways that lead to many responses: • Production of defensins and cytokines • Phagocytosis of invaders • Activation of natural killer cells and complement system
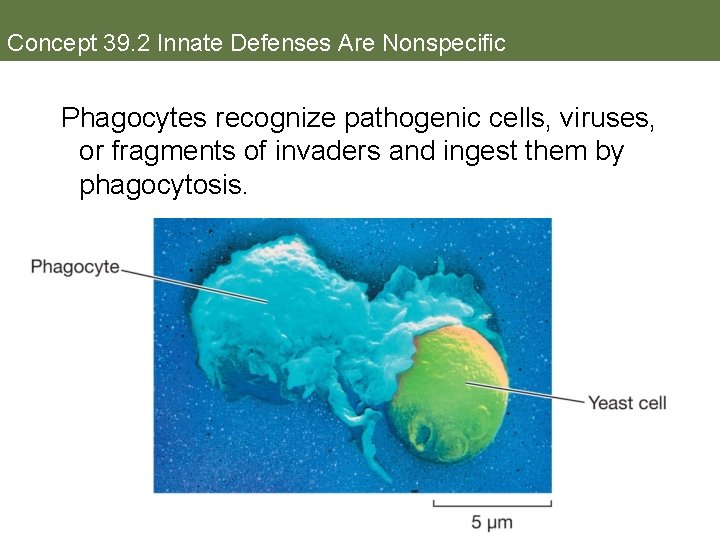
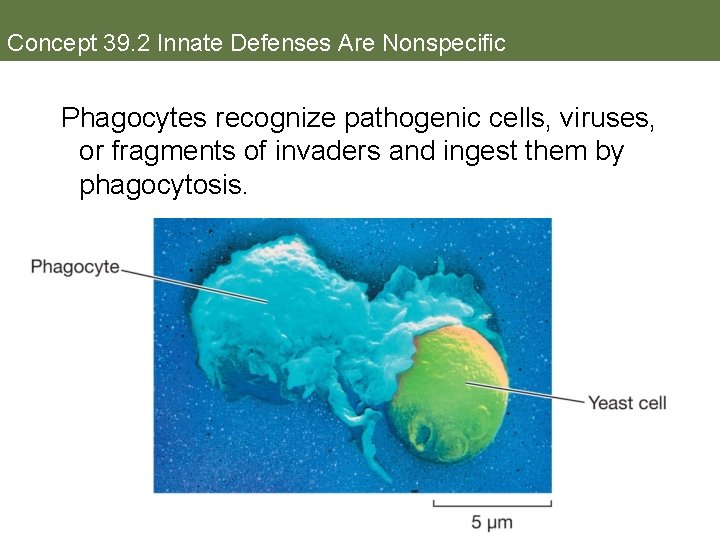
Concept 39. 2 Innate Defenses Are Nonspecific Phagocytes recognize pathogenic cells, viruses, or fragments of invaders and ingest them by phagocytosis.
Concept 39. 2 Innate Defenses Are Nonspecific Natural killer cells—lymphocytes that can distinguish between healthy cells and tumor cells or virus-infected cells • Initiate apoptosis in tumor cells • Can interact with adaptive defense mechanisms by lysing cells that have been tagged with antibodies
Concept 39. 2 Innate Defenses Are Nonspecific Complement system: antimicrobial proteins that act in a cascade—each protein activates the next • One complement protein binds to surface of invading cell, marking it for phagocytosis • Another protein activates the inflammation response and attracts phagocytes to site of infection • Still other proteins lyse the invading cells
Concept 39. 2 Innate Defenses Are Nonspecific The complement system can be activated by mechanisms in both the innate and adaptive immune systems. In the latter case, the complement cascade is initiated by binding of a complement protein to an antibody on the surface of the invading cell.
Concept 39. 2 Innate Defenses Are Nonspecific Cytokines: signaling proteins produced in response to PRR activation Includes interferons, which help increase resistance of neighboring cells to infection. They bind to uninfected cells and trigger pathways that prevent viral reproduction, and they stimulate breakdown of bacterial and viral proteins. Interferons can be induced by molecules such as double-stranded viral RNA.
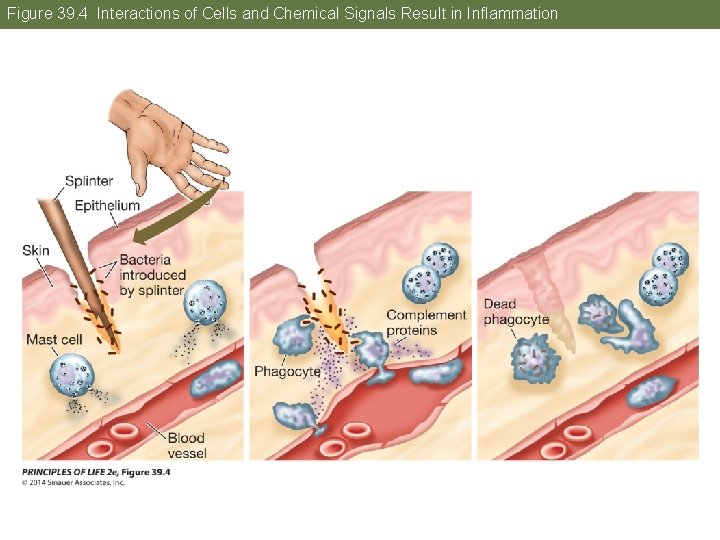
Concept 39. 2 Innate Defenses Are Nonspecific Inflammation is a coordinated response to infection or injury; it results in redness, swelling, heat, and pain at the damaged site. It isolates damage, recruits defense cells and molecules to the site, and promotes healing. Mast cells are the first responders, and they release chemical signals: • Tumor necrosis factor—cytokine that kills target cells and activates immune cells
Concept 39. 2 Innate Defenses Are Nonspecific • Prostaglandins—initiate inflammation in nearby tissues; many other roles • Histamine—amino acid derivative that increases permeability of blood vessels to white blood cells and proteins so they can act on nearby tissues

Concept 39. 2 Innate Defenses Are Nonspecific Redness and heat result from dilation of blood vessels in the area. Phagocytes enter the area and engulf pathogens and dead cells. Phagocytes produce cytokines—some can signal the brain to produce fever. Increased body temperature accelerates lymphocyte production and phagocytosis, thus speeding the immune response. Fever inhibits growth of some pathogens.
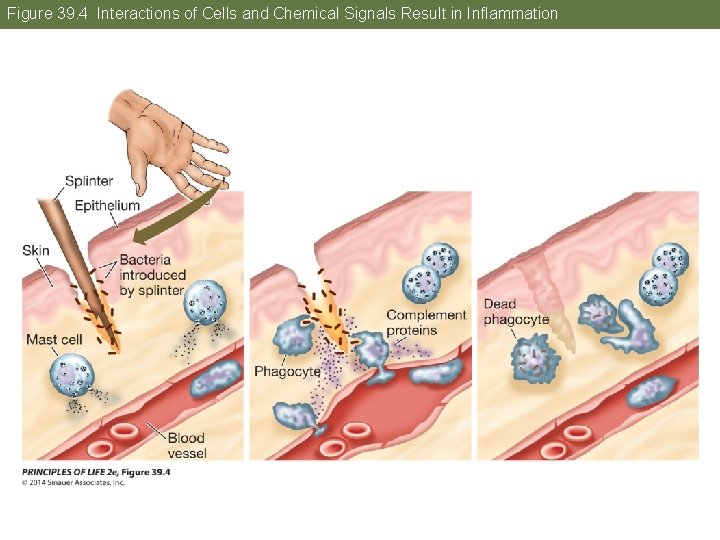
Figure 39. 4 Interactions of Cells and Chemical Signals Result in Inflammation
Concept 39. 2 Innate Defenses Are Nonspecific Pain of inflammation is from pressure due to swelling, action of leaked enzymes on nerve endings, and prostaglandins, which increase sensitivity of nerve endings to pain. Pus is a mixture of leaked fluid and dead cells. It gets consumed by macrophages. Platelets (blood cell fragments) appear near a wound to promote healing. They produce growth factors that stimulate skin cells to divide.
Concept 39. 2 Innate Defenses Are Nonspecific The inflammation response can be too strong: • Allergic reaction: a nonself molecule that is normally harmless binds to mast cells, causing the release of histamine and subsequent inflammation. • Autoimmune diseases: the immune system fails to distinguish between self and nonself and attacks tissues in the organism’s own body.

Concept 39. 2 Innate Defenses Are Nonspecific • Sepsis: inflammation due to a bacterial infection does not remain local. § Dilation of blood vessels throughout the body can result in a dangerous drop in blood pressure.
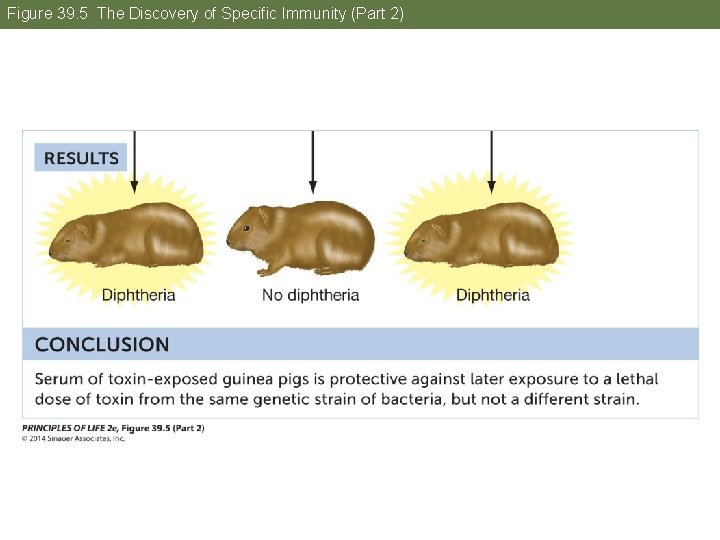
Concept 39. 3 The Adaptive Immune Response Is Specific Early experiments showed that factors in the blood were important in adaptive immunity. These factors were later identified as antibody proteins. Development of immunity from antibodies received from another individual is called passive immunity.

Figure 39. 5 The Discovery of Specific Immunity (Part 1)
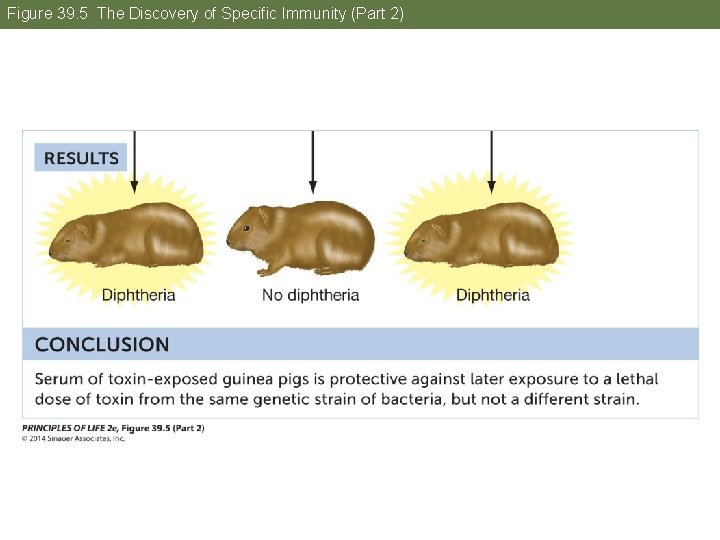
Figure 39. 5 The Discovery of Specific Immunity (Part 2)
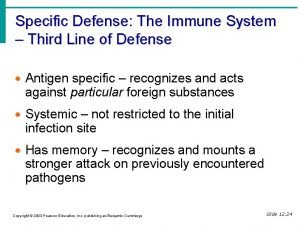
Concept 39. 3 The Adaptive Immune Response Is Specific Adaptive immunity has four key features: • Specificity • Distinguishing self from nonself • Diversity • Immunological memory
Concept 39. 3 The Adaptive Immune Response Is Specificity • Lymphocytes play the crucial role. • Nonself substances are called antigens. • T cell receptors and antibodies made by B cells bind to specific antigens. • Each T cell and each antibody-producing B cell is specific for a single antigen.
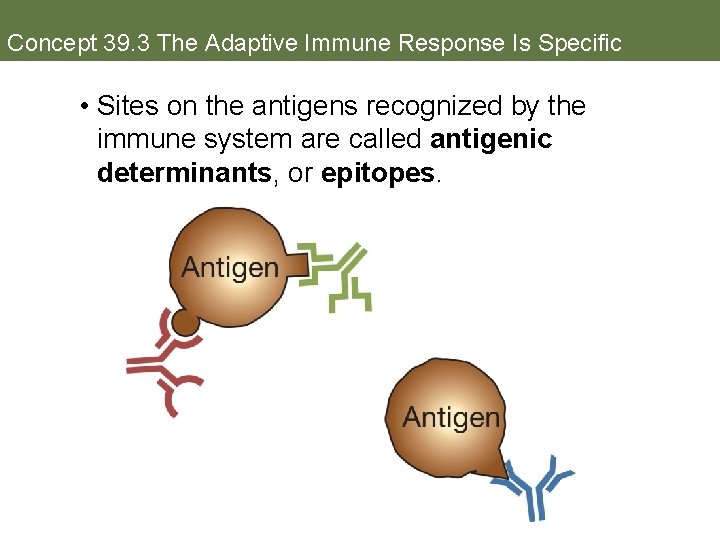
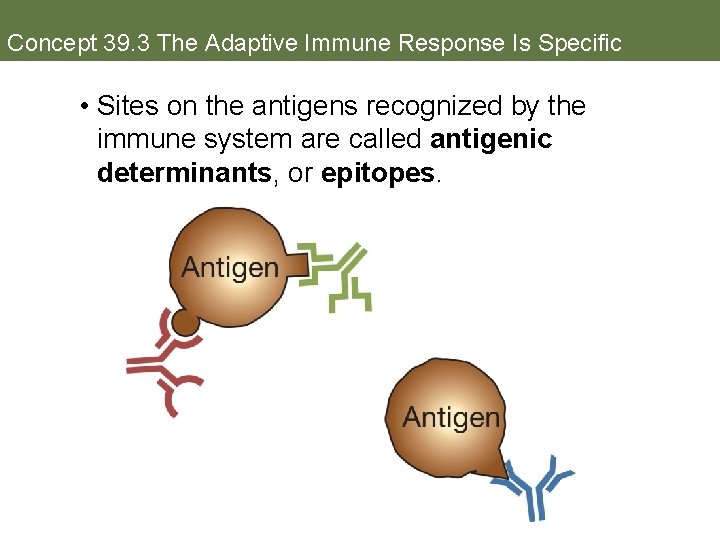
Concept 39. 3 The Adaptive Immune Response Is Specific • Sites on the antigens recognized by the immune system are called antigenic determinants, or epitopes.

Concept 39. 3 The Adaptive Immune Response Is Specific • Antigens are usually proteins or polysaccharides, and there can be multiple antigens on a single bacterium. • A single antigenic molecule can have multiple, different antigenic determinants. • Antigenic determinants are often referred to as antigens.
Concept 39. 3 The Adaptive Immune Response Is Specific Distinguishing self from nonself • An individual’s immune system must be able to recognize the body’s own antigens and not attack them. • When B and T cells encounter antigens during their early development, any cells that show potential to mount an immune response to self antigens undergo apoptosis (clonal deletion).
Concept 39. 3 The Adaptive Immune Response Is Specific • Failure of clonal deletion can lead to autoimmunity. • In diseases such as systemic lupus erythematosis (SLE) or Hashimoto’s thyroiditis, immune cells mount a response against normal tissues.
Concept 39. 3 The Adaptive Immune Response Is Specific Diversity • The immune system must respond to a wide variety of pathogens and a variety of genetic strains of those pathogens. • Humans can respond specifically to about 10 million different antigens. • The body generates a pool of lymphocytes from which specific cells are selected when needed.
Concept 39. 3 The Adaptive Immune Response Is Specific • Diversity is generated primarily by DNA changes that occur just after B and T cells are formed. • The adaptive immune system is “predeveloped”—all of the machinery available to respond to an immense diversity of antigens is already there, even before the antigens are encountered.
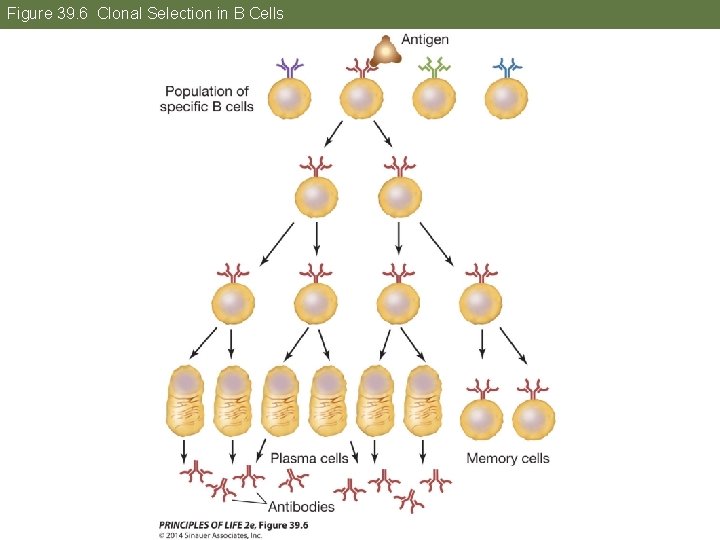
Concept 39. 3 The Adaptive Immune Response Is Specific • Antigen binding “selects” a particular B or T cell for proliferation. • Clonal selection: a particular lymphocyte is selected via binding and activation, and then it proliferates to generate a clone
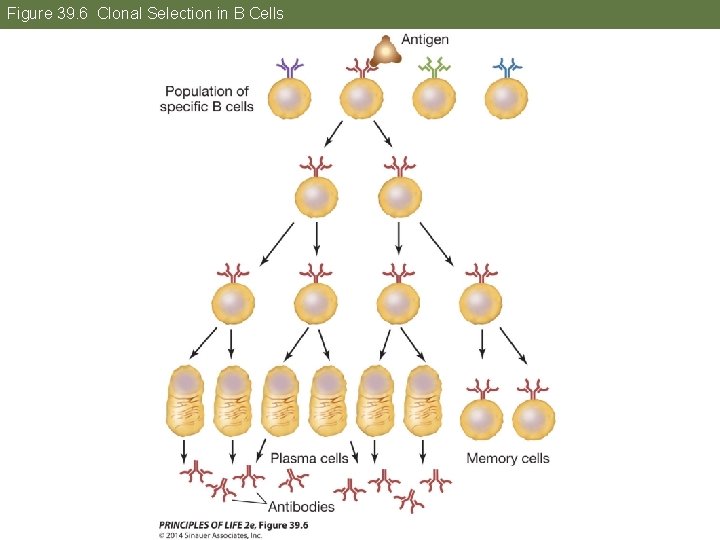
Figure 39. 6 Clonal Selection in B Cells
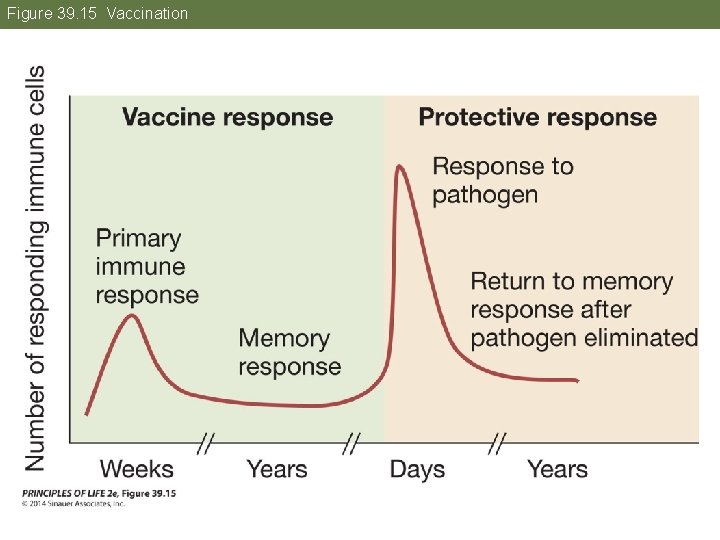
Concept 39. 3 The Adaptive Immune Response Is Specific Immunological memory • The immune system “remembers” a pathogen after the first encounter and can respond faster and more powerfully if the pathogen is encountered again. • Primary immune response—when antigen is first encountered, “naïve” lymphocytes proliferate to produce two types of cells—effector and memory cells.
Concept 39. 3 The Adaptive Immune Response Is Specific • Effector cells carry out the attack. Effector B cells (plasma cells) secrete antibodies. Effector T cells secrete cytokines and other molecules. • Memory cells are long-lived cells that can divide on short notice to produce effector cells and more memory cells. § Memory B and T cells may survive for decades.
Concept 39. 3 The Adaptive Immune Response Is Specific • Secondary immune response—when the antigen is encountered again, memory cells proliferate and launch an army of plasma cells and effector T cells. • Vaccinations trigger a primary immune response to prepare the body for a quicker, secondary response if it encounters the pathogen again.
Concept 39. 3 The Adaptive Immune Response Is Specific Phagocytosis is one mechanism for eliminating pathogens. After ingesting a pathogen or infected host cell, the phagocyte displays fragments of the pathogen on their surfaces, which function as antigens. This antigen presentation is one way the innate immune system communicates with the adaptive immune system.
Concept 39. 3 The Adaptive Immune Response Is Specific After engulfing pathogens or infected host cells, macrophages and dendritic cells migrate to lymph nodes, where they present the antigen to immature T cells. The antigen-presenting cells secrete cytokines and other signals that stimulate activation and differentiation of T cells. Developing B cells can also perform phagocytosis and function as antigenpresenting cells.
Concept 39. 3 The Adaptive Immune Response Is Specific The adaptive immune system has two types of responses that work simultaneously and cooperatively: • Humoral immune response—by B cells that make antibodies • Cellular immune response—by cytotoxic T (TC) cells
Concept 39. 3 The Adaptive Immune Response Is Specific Both types of responses have three phases: • Recognition phase—antigen is inserted into membrane of antigen presenting cell. § This antigen is recognized by a T-helper (TH) cell bearing a T cell receptor protein that is specific for the antigen. § In both humoral and cellular immunity, binding initiates the activation phase.

Figure 39. 7 The Adaptive Immune System

Figure 39. 7 The Adaptive Immune System
Concept 39. 3 The Adaptive Immune Response Is Specific • Activation phase—when the TH cell recognizes an antigen on an antigenpresenting cell, it releases cytokines that stimulate B cells and TC cells with receptors to the same antigen to divide. § The results are a clone of B cells that function in humoral immunity and a clone of TC cells that function in cellular immunity.
Concept 39. 3 The Adaptive Immune Response Is Specific • Effector phase—cells of the B clone produce antibodies that bind to viral particles and/or virus-infected cells. § § The bound antibodies attract phagocytes and complement proteins that engulf and destroy the virus and the virusinfected cells. In cellular immunity, cells of the TC clone bind to virus-infected cells and destroy them.
Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies B cells are the basis of the humoral immune response. A “naïve” B cell has a receptor protein specific for an antigen on its cell surface. Antigen binding activates the B cell. A TH cell that recognizes the anitgen secretes cytokines that stimulate the B cell to divide. The resulting clone of plasma cells produce antibodies specific for the antigen that originally bound to the parent B cell.
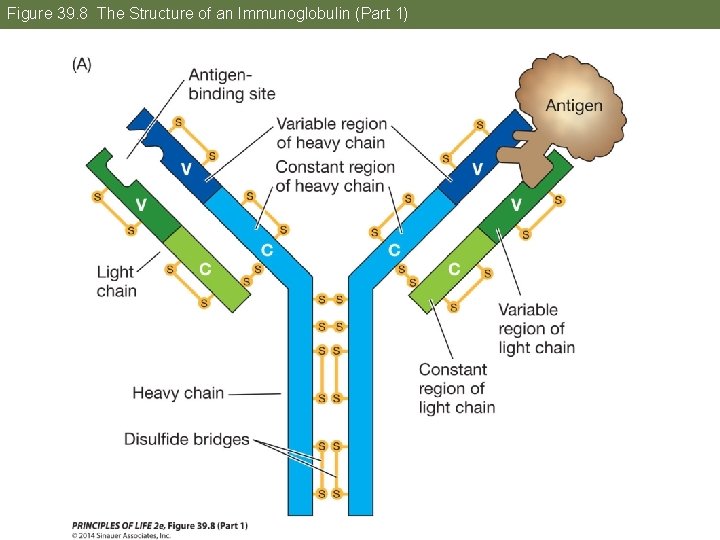
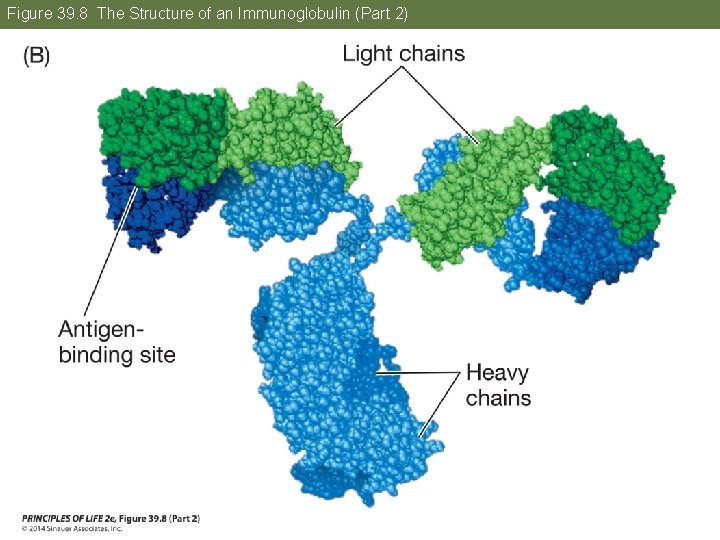
Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies, or immunoglobulins, are all tetramers of four polypeptides. Two light chains and two heavy chains are held together by disulfide bonds. Each chain has a constant region and a variable region.
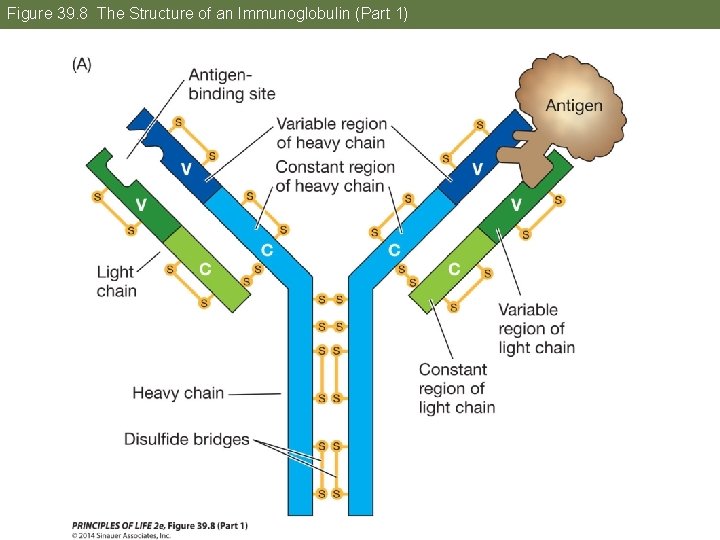
Figure 39. 8 The Structure of an Immunoglobulin (Part 1)
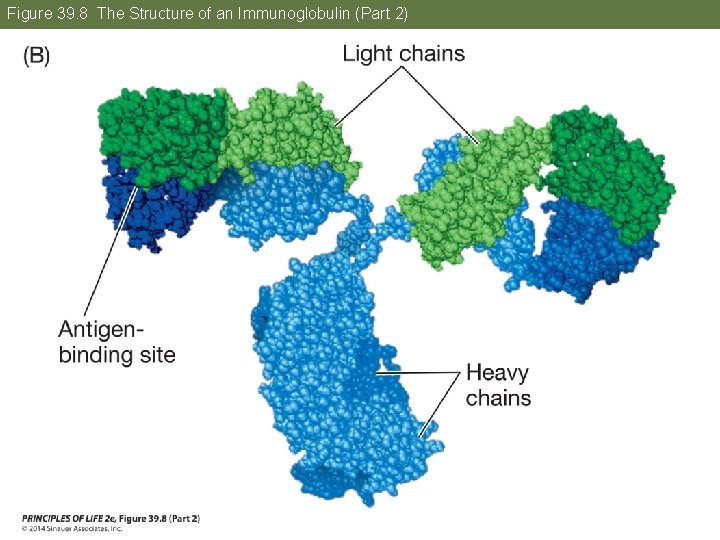
Figure 39. 8 The Structure of an Immunoglobulin (Part 2)
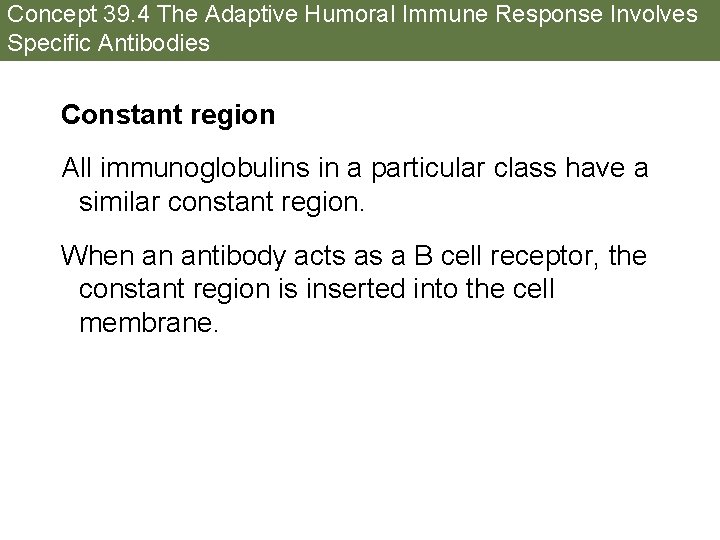
Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies Constant region All immunoglobulins in a particular class have a similar constant region. When an antibody acts as a B cell receptor, the constant region is inserted into the cell membrane.

Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies Variable region: where the amino acid sequence is different for each specific immunoglobulin The 3 -D shape of the variable region’s antigenbinding site is responsible for antibody specificity. The two antigen-binding sites are identical; the immunoglobulin is bivalent.
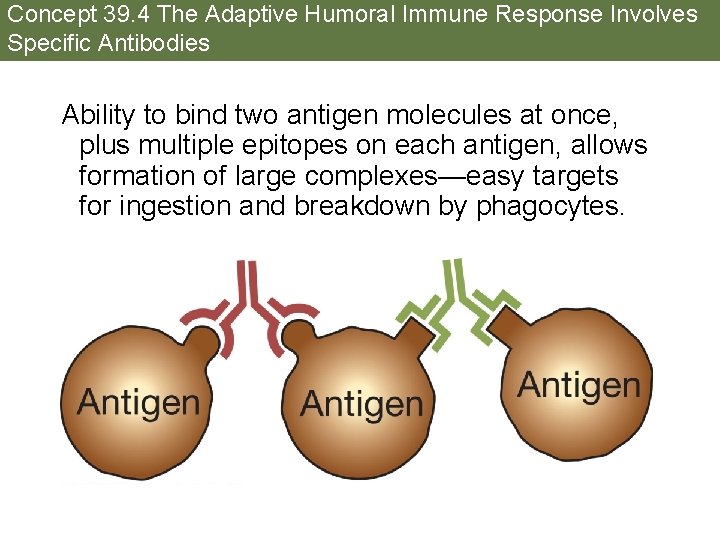
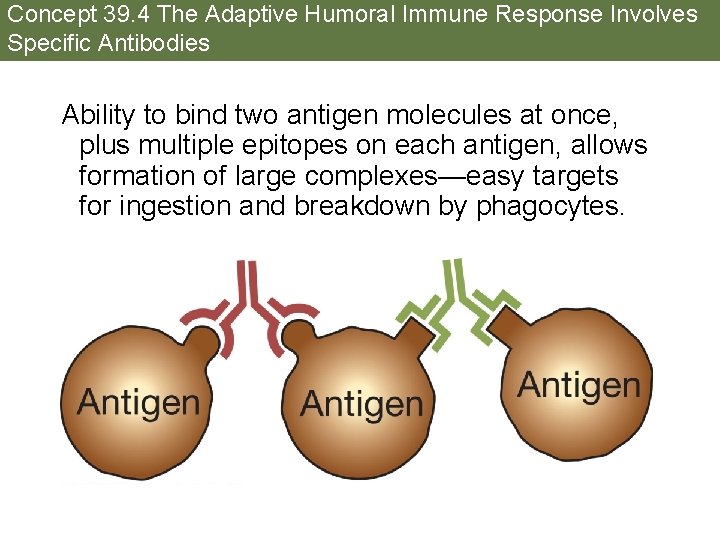
Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies Ability to bind two antigen molecules at once, plus multiple epitopes on each antigen, allows formation of large complexes—easy targets for ingestion and breakdown by phagocytes.

Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies Five classes of immunoglobulins (Ig): • Ig. G—about 80% of circulating antibodies • Ig. D—cell surface receptor on a B cell • Ig. M—initial surface and circulating antibody • Ig. A—protects mucus membranes exposed to the environment • Ig. E—binds to mast cells and is involved with inflammation
Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies The B cell genome has several different coding regions for each domain of an immunoglobulin. Diversity is generated by putting together different combinations of these regions. This generates the enormous immunological diversity in each individual.
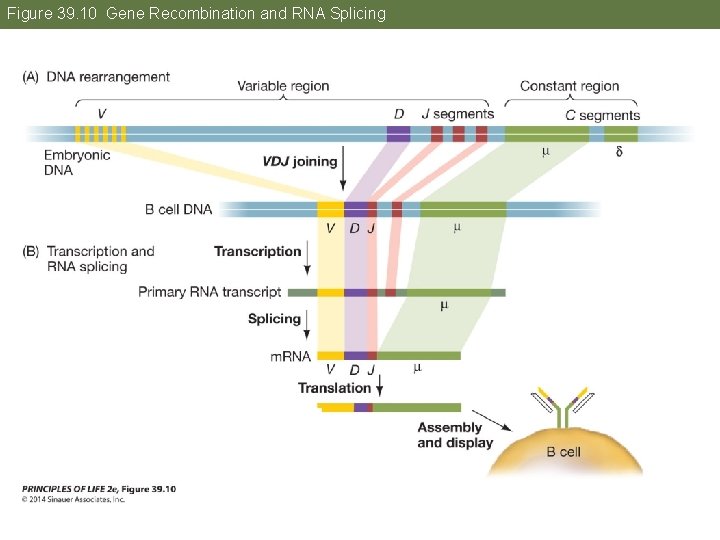
Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies Every cell in the body has hundreds of immunoglobulin genes located in separate clusters. During B cell development, these genes are cut out, rearranged, and joined together in DNA recombination events to form a “supergene. ”

Figure 39. 9 Super Genes
Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies One gene from each cluster is chosen randomly for joining, and others are deleted. For example, in one multigene set, the J genes, some of the extra sequences are removed by RNA splicing. Each B cell precursor assembles two unique supergenes, one for a specific heavy chain and one for a specific light chain.
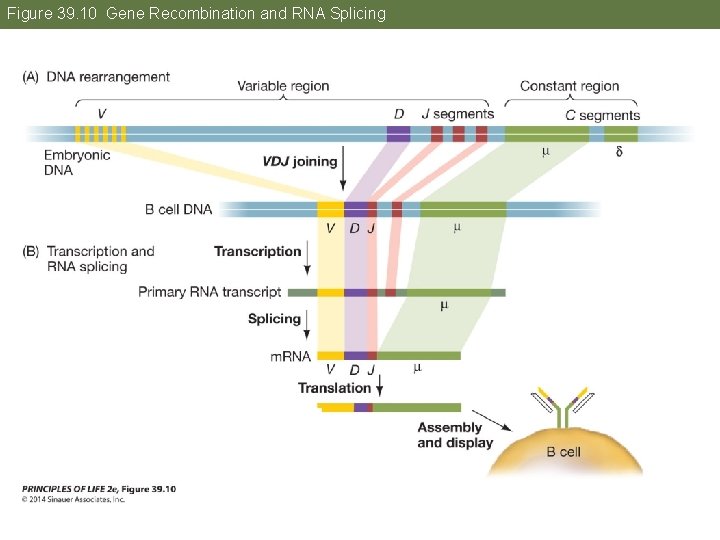
Figure 39. 10 Gene Recombination and RNA Splicing
Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies This remarkable example of irreversible cell differentiation generates an enormous diversity of immunoglobulins from the same genome. It is an exception to the generalization that all somatic cells of an individual have identical DNA.
Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies Other mechanisms that generate diversity: • When DNA is rearranged, errors can occur during recombination, creating new codons and thus amino acid changes. • Before DNA is rejoined, terminal transferase adds nucleotides, creating insertion mutations. • High spontaneous mutation rate creates new alleles.
Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies can act as receptors on B cell surfaces in the recognition phase of the humoral response. In the effector phase, antibodies are produced by the B cell clone and enter the blood stream. When antibodies bind to antigens on the surfaces of pathogens, they attract complement system proteins, which attack and lyse the pathogens.

Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies Binding of antibody and complement proteins stimulates phagocytes to ingest the pathogen.
Concept 39. 4 The Adaptive Humoral Immune Response Involves Specific Antibodies The large, insoluble antibody–pathogen or antibody–antigen complexes attract effector cells such as phagocytes and natural killer cells.
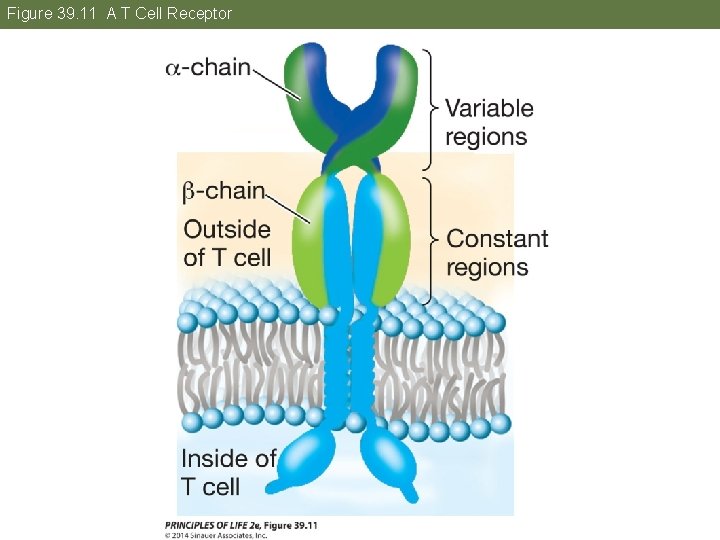
Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors T cells receptors are glycoproteins, with two polypeptide chains. Each chain is encoded by a different gene and has constant and variable regions. T cell receptors bind only to antigens displayed by an MHC (major histocompatibility complex) protein on the surface of an antigenpresenting cell.
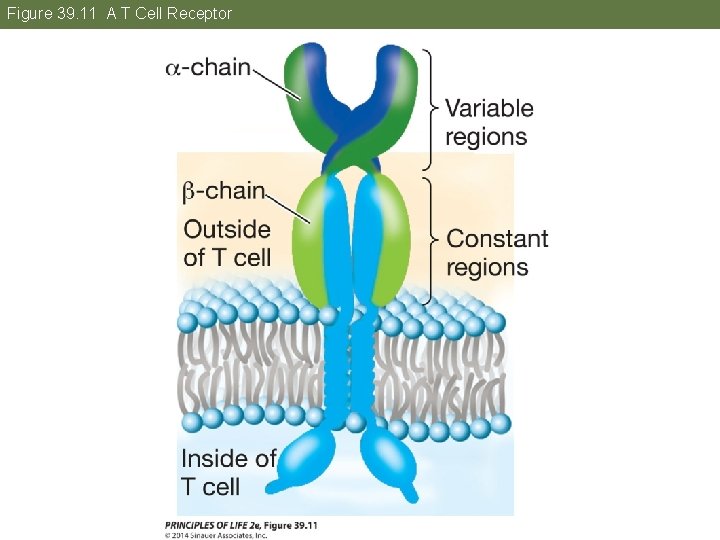
Figure 39. 11 A T Cell Receptor
Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors TH binding results in activation of the adaptive immune response. TC binding results in death of the cell carrying the antigen. MHC proteins form complexes with antigens on cell surfaces and assist with recognition by the T cells so that the appropriate type of T cell binds.
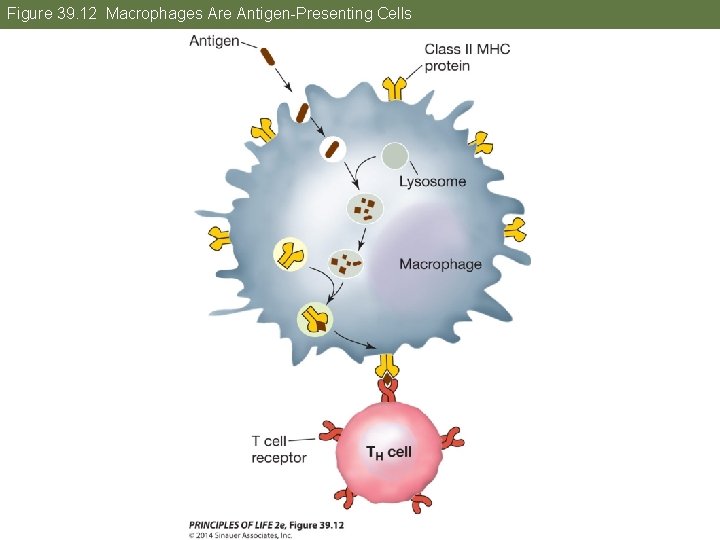
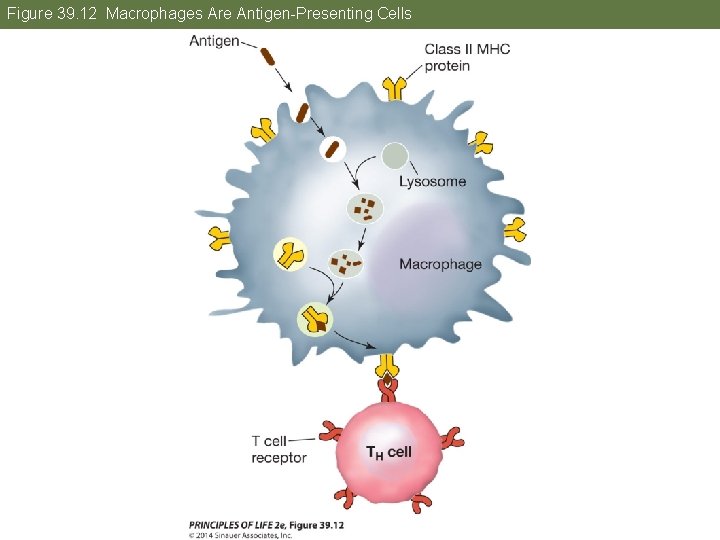
Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors Two types of T cells: • Class I MHC proteins are present on the surface of every nucleated cell. They present antigens to TC cells. • Class II MHC proteins are on macrophages, B cells, and dendritic cells. They present antigens to TH cells. § These cells ingest antigens and break them down; one of the fragments binds to MHC II for presentation.
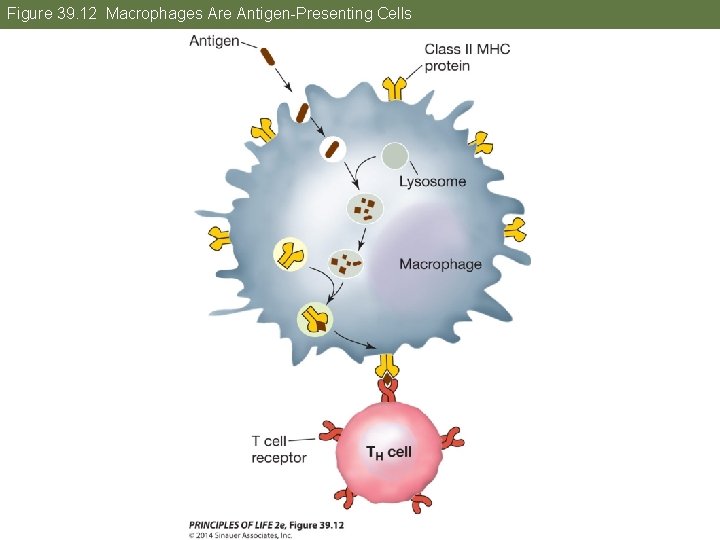
Figure 39. 12 Macrophages Are Antigen-Presenting Cells
Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors MHC proteins are “self” markers. People can have very different MHC genotypes due to many possible combinations of alleles. For antigen presentation, MHC I and MHC II proteins have an antigen binding site, which holds a polypeptide fragment. T cell receptors recognize the antigenic fragment and the I or II MHC bound to it.

Table 39. 2
Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors Activation of a TH cell results in rapid clonal propagation. The TH cells release cytokines that stimulate other immune cells, including TC cells, to propagate. TH cells also interact with B cells that present antigens on class II MHC proteins.

Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors When a TH cell binds to the displayed antigen–MHC II complex, it stimulates the B cell to propagate and secrete antibodies.
Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors TC cells are activated when they bind to cells with an antigen–MHC I protein complex, such as a virus-infected cell. This results in a clone of TC cells with the same receptor. When bound, the TC cells release perforin, which lyses the bound target cell, or stimulates apoptosis in the target cell.
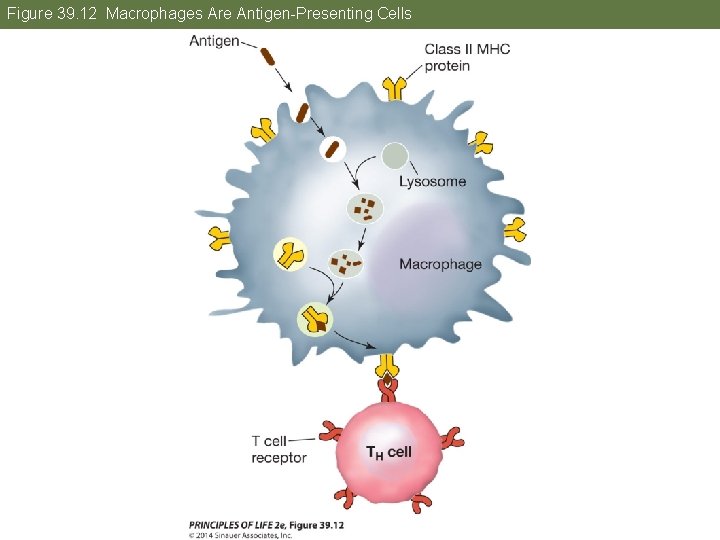
Figure 39. 12 Macrophages Are Antigen-Presenting Cells
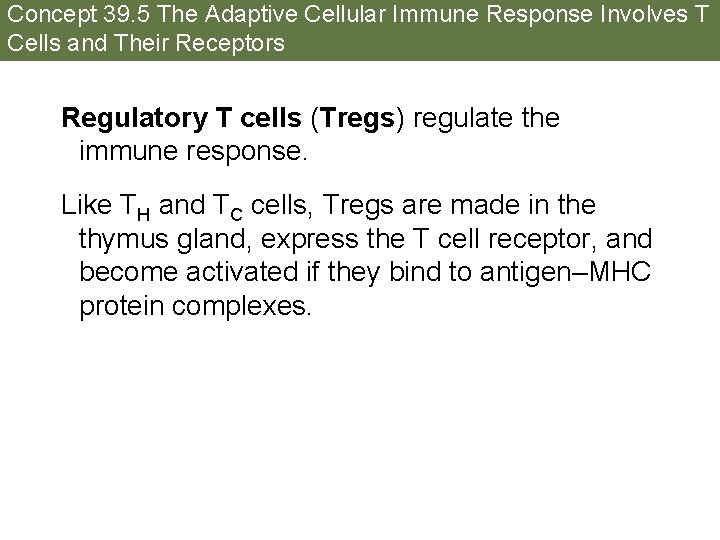
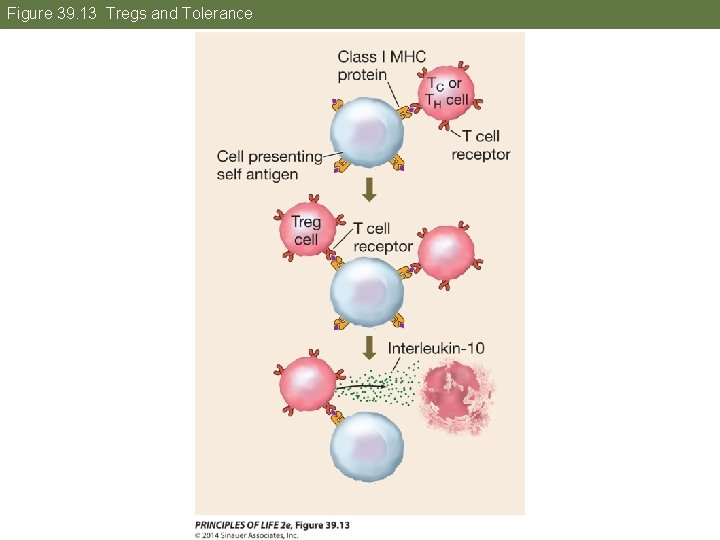
Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors Regulatory T cells (Tregs) regulate the immune response. Like TH and TC cells, Tregs are made in the thymus gland, express the T cell receptor, and become activated if they bind to antigen–MHC protein complexes.
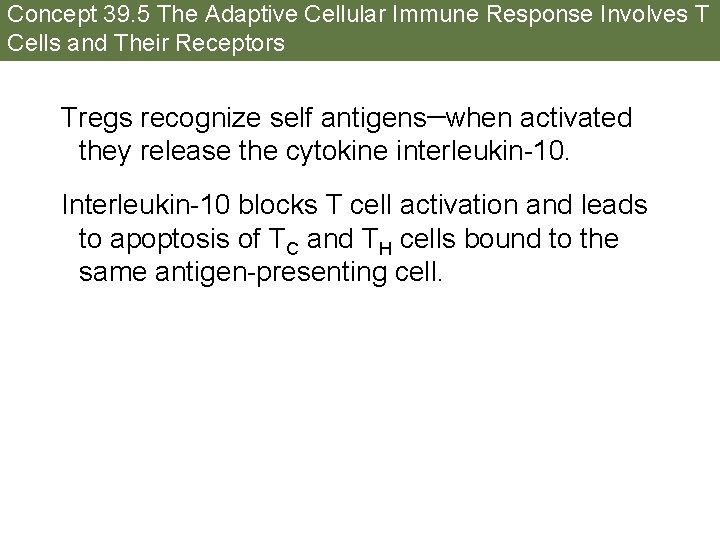
Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors Tregs recognize self antigens—when activated they release the cytokine interleukin-10. Interleukin-10 blocks T cell activation and leads to apoptosis of TC and TH cells bound to the same antigen-presenting cell.
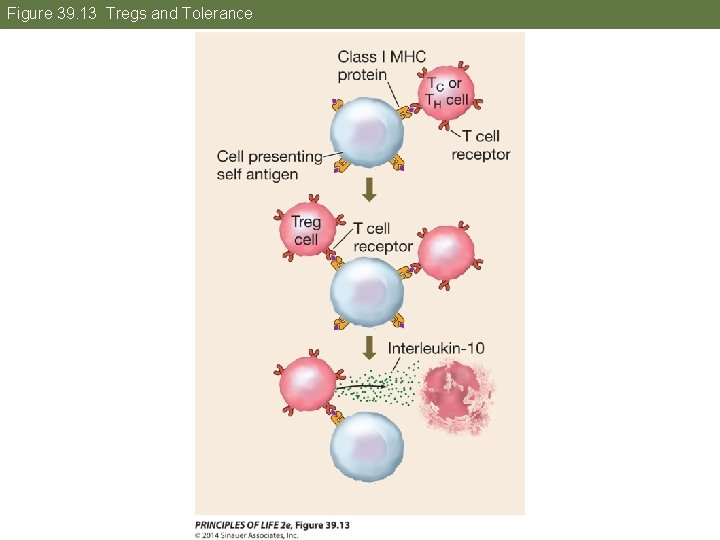
Figure 39. 13 Tregs and Tolerance
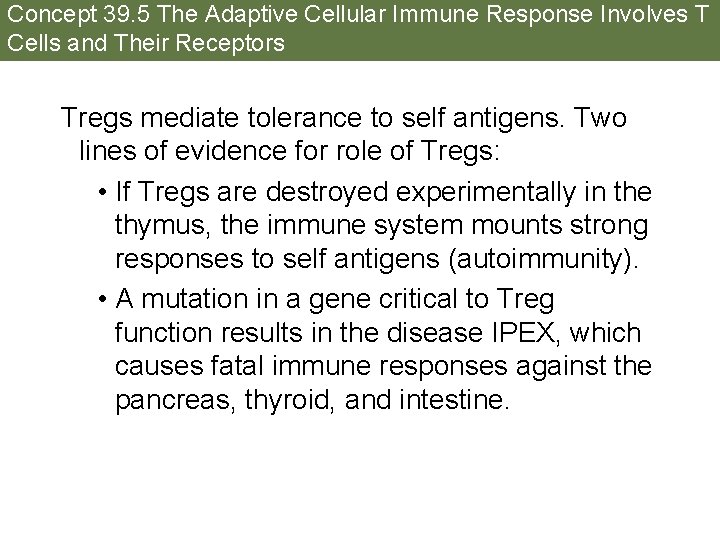
Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors Tregs mediate tolerance to self antigens. Two lines of evidence for role of Tregs: • If Tregs are destroyed experimentally in the thymus, the immune system mounts strong responses to self antigens (autoimmunity). • A mutation in a gene critical to Treg function results in the disease IPEX, which causes fatal immune responses against the pancreas, thyroid, and intestine.

Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors Immune deficiency disorders can be inherited or acquired. In some individuals, T or B cells never form, or B cells lose their ability to give rise to plasma cells—the affected individual lacks a major line of defense against pathogens.
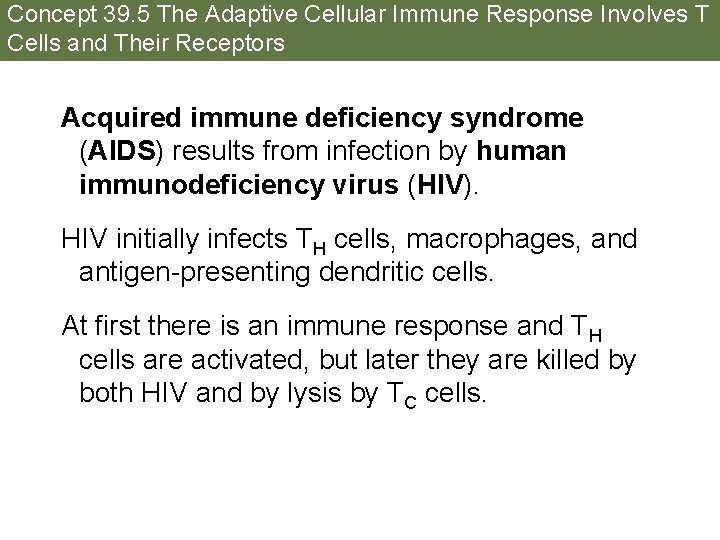
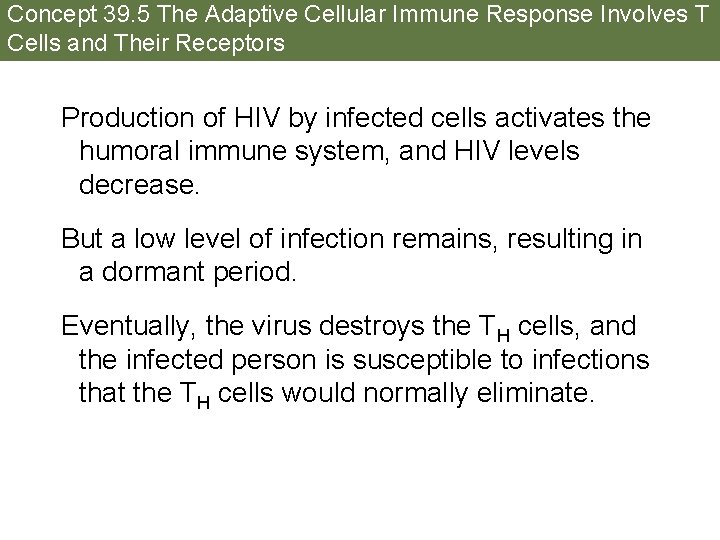
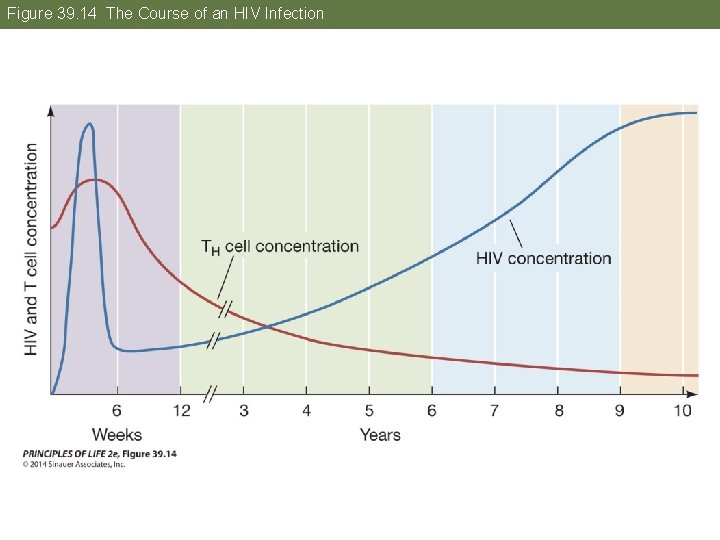
Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors Acquired immune deficiency syndrome (AIDS) results from infection by human immunodeficiency virus (HIV). HIV initially infects TH cells, macrophages, and antigen-presenting dendritic cells. At first there is an immune response and TH cells are activated, but later they are killed by both HIV and by lysis by TC cells.
Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors Production of HIV by infected cells activates the humoral immune system, and HIV levels decrease. But a low level of infection remains, resulting in a dormant period. Eventually, the virus destroys the TH cells, and the infected person is susceptible to infections that the TH cells would normally eliminate.
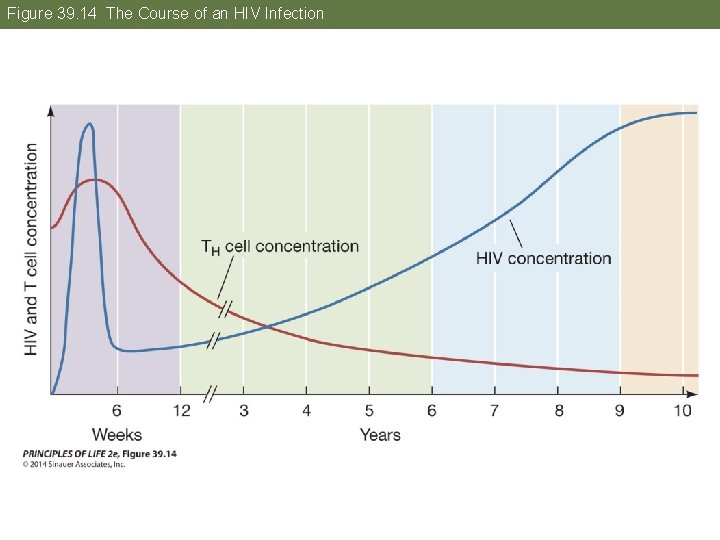
Figure 39. 14 The Course of an HIV Infection

Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors Opportunistic infections—pathogens take advantage of the crippled immune system: • Kaposi’s sarcoma, a rare skin cancer caused by a herpes virus • Pneumonia caused by fungus Pneumocystis jirovecii • Lymphoma tumors caused by Epstein-Barr virus
Concept 39. 5 The Adaptive Cellular Immune Response Involves T Cells and Their Receptors Drug treatments for HIV focus on inhibiting the processes of viral entry, assembly, and replication. Combinations of such drugs result in long-term survival. Unfortunately, like many medical treatments, HIV drugs are not available to all who need them, especially in poor regions of the world.
Answer to Opening Question Survivors of the Athenean plague had developed immunological memory. The T and B cells activated by adaptive immune responses formed clones of memory cells. Reentry of the pathogen provoked a rapid, massive T and B cell response, which prevented the pathogen from proliferating.
Answer to Opening Question Vaccines employ immunological memory. Exposure to an antigen in a form that does not cause disease can still initiate a primary immune response, generating memory cells without making the person ill. The antigens used for vaccines must be altered by chemical inactivation or mutation. Vaccines have nearly wiped out some diseases, including smallpox, diphtheria, and polio.
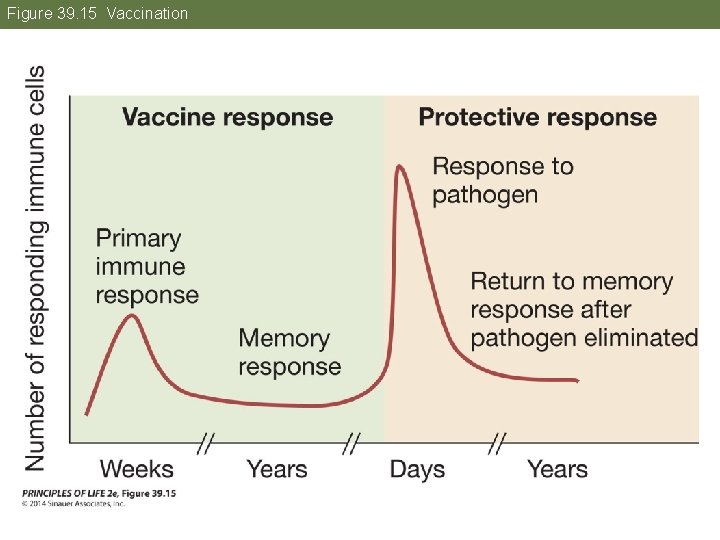
Figure 39. 15 Vaccination
 Specific defense vs nonspecific defense
Specific defense vs nonspecific defense Talley defense systems
Talley defense systems Forescout frontline
Forescout frontline What are the first line of defense
What are the first line of defense Defense systems management college
Defense systems management college Defense business systems
Defense business systems Phagocyte
Phagocyte Paraprotein
Paraprotein Central tolerance and peripheral tolerance
Central tolerance and peripheral tolerance Sle criteria
Sle criteria 17 tc
17 tc Cells
Cells Abbas basic immunology
Abbas basic immunology Immunology diploma
Immunology diploma Pcams immunology
Pcams immunology Assisting in microbiology and immunology
Assisting in microbiology and immunology Baltimore classification
Baltimore classification Ras
Ras Neutrophil extracellular traps
Neutrophil extracellular traps Molecular immunology ppt
Molecular immunology ppt Trends in immunology
Trends in immunology Nature reviews immunology
Nature reviews immunology Pals immunology
Pals immunology Kuby immunology
Kuby immunology Tumor immunology
Tumor immunology Nature reviews immunology
Nature reviews immunology Fraunhofer institute for cell therapy and immunology
Fraunhofer institute for cell therapy and immunology Avidity in immunology
Avidity in immunology Wiki
Wiki Ucsd immunology course
Ucsd immunology course Bmc immunology
Bmc immunology American academy of allergy asthma and immunology 2018
American academy of allergy asthma and immunology 2018 Servier medical art immunology
Servier medical art immunology Venn diagram plant and animal cell
Venn diagram plant and animal cell Plant vs animal cell venn diagram
Plant vs animal cell venn diagram Animal rights vs animal welfare
Animal rights vs animal welfare Chapter 17 section 1 mobilizing for defense answer key
Chapter 17 section 1 mobilizing for defense answer key Chapter 17 section 1 mobilizing for defense
Chapter 17 section 1 mobilizing for defense Chapter 17 section 1 mobilizing for defense
Chapter 17 section 1 mobilizing for defense Animal id systems - assessment v
Animal id systems - assessment v Animal systems agriscience project ideas
Animal systems agriscience project ideas Decision support systems and intelligent systems
Decision support systems and intelligent systems Principles of complex systems for systems engineering
Principles of complex systems for systems engineering Embedded systems vs cyber physical systems
Embedded systems vs cyber physical systems Engineering elegant systems: theory of systems engineering
Engineering elegant systems: theory of systems engineering Ddo sapphire
Ddo sapphire Usw strike and defense fund
Usw strike and defense fund Mom boy
Mom boy Army training information system
Army training information system Defense property system
Defense property system Gps thesis submission
Gps thesis submission Example of regression defense mechanism
Example of regression defense mechanism What is the third line of defense in the immune system
What is the third line of defense in the immune system The defense of poesy summary
The defense of poesy summary Defense logistics conference
Defense logistics conference Reciprocal determinism definition psychology
Reciprocal determinism definition psychology Stress versus burnout
Stress versus burnout How does a sponge defend itself
How does a sponge defend itself Third line of defense immune system
Third line of defense immune system An/psn-13 defense advanced gps receiver
An/psn-13 defense advanced gps receiver Zones de défense france
Zones de défense france Secretary of defense executive fellows program
Secretary of defense executive fellows program Defense requirements management training
Defense requirements management training Cisco ransomware
Cisco ransomware Mature defense mechanisms
Mature defense mechanisms Regression defense mechanism
Regression defense mechanism Attachment formulation
Attachment formulation Free will defense theodizee
Free will defense theodizee Rationalization defense mechanism examples
Rationalization defense mechanism examples Structure of personality development
Structure of personality development Is personality innate or learned
Is personality innate or learned Superego definition psychology
Superego definition psychology Undoing defense mechanism examples
Undoing defense mechanism examples Defense microelectronics activity
Defense microelectronics activity Ap psychology defense mechanisms worksheet answers
Ap psychology defense mechanisms worksheet answers Poison pill defense
Poison pill defense Autoplastic defense
Autoplastic defense What is a master's thesis defense
What is a master's thesis defense 3-5-3 defense
3-5-3 defense Defense mechanism of female genital tract
Defense mechanism of female genital tract Coso 3 lines of defense
Coso 3 lines of defense Cadet de la défense toulon
Cadet de la défense toulon The psychodynamic theory
The psychodynamic theory Next generation soc
Next generation soc Innate immunity first line of defense
Innate immunity first line of defense Categories of defense mechanisms
Categories of defense mechanisms Tiger box hacking tools
Tiger box hacking tools Guide to network defense and countermeasures
Guide to network defense and countermeasures Guide to network defense and countermeasures
Guide to network defense and countermeasures 3 lines of defense
3 lines of defense Freud projection
Freud projection Extremism in the defense of liberty is no vice
Extremism in the defense of liberty is no vice Displacement
Displacement 1 mef dts help desk
1 mef dts help desk Cba vs iba dts
Cba vs iba dts Defense readiness reporting system
Defense readiness reporting system Pctef
Pctef Executive order 12919
Executive order 12919 Defense office of hearings and appeals
Defense office of hearings and appeals Projective identification.
Projective identification. Types of defense mechanisms
Types of defense mechanisms Autistic fantasy defense mechanism example
Autistic fantasy defense mechanism example Displacement defense mechanism
Displacement defense mechanism Zones de défense france
Zones de défense france An/psn-13a
An/psn-13a