TRANSFUSION REACTIONS IMMEDIATE HEMOLYTIC TRANSFUSION REACTION Intravascular lysis

- Slides: 11

TRANSFUSION REACTIONS
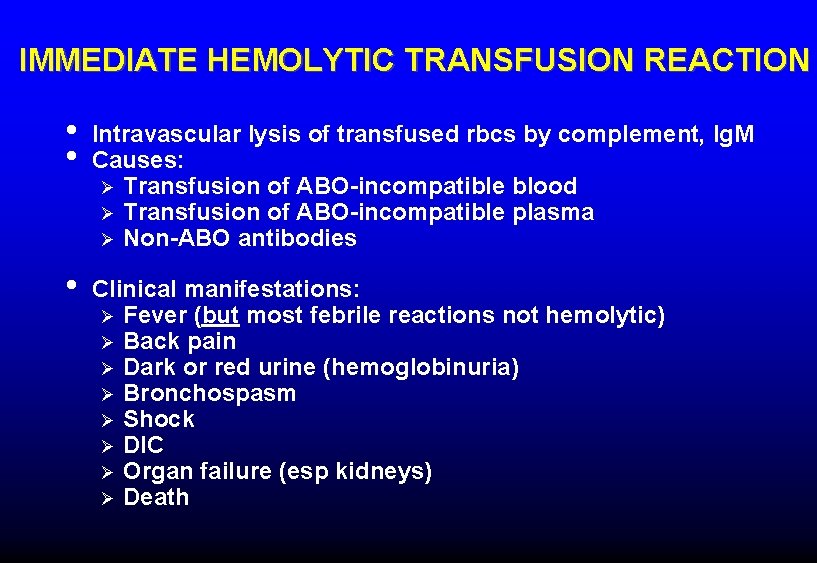
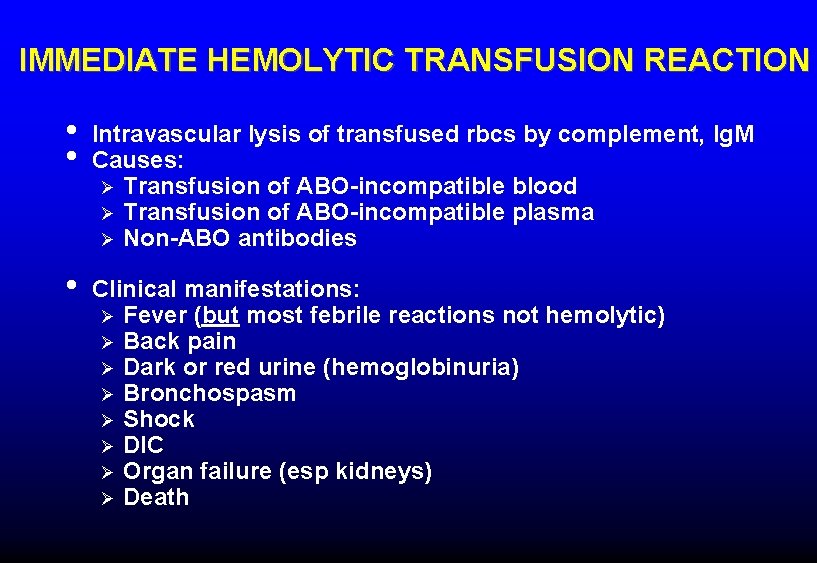
IMMEDIATE HEMOLYTIC TRANSFUSION REACTION • • Intravascular lysis of transfused rbcs by complement, Ig. M Causes: Ø Transfusion of ABO-incompatible blood Ø Transfusion of ABO-incompatible plasma Ø Non-ABO antibodies • Clinical manifestations: Ø Fever (but most febrile reactions not hemolytic) Ø Back pain Ø Dark or red urine (hemoglobinuria) Ø Bronchospasm Ø Shock Ø DIC Ø Organ failure (esp kidneys) Ø Death
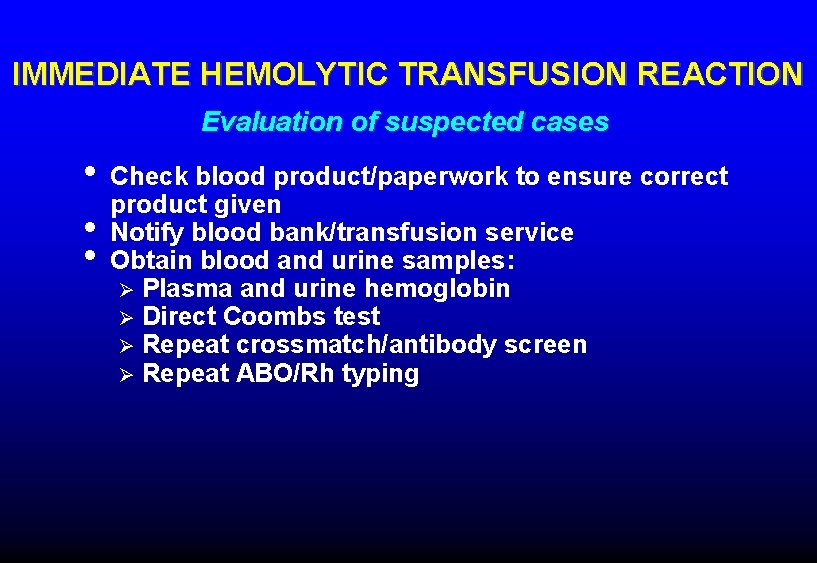
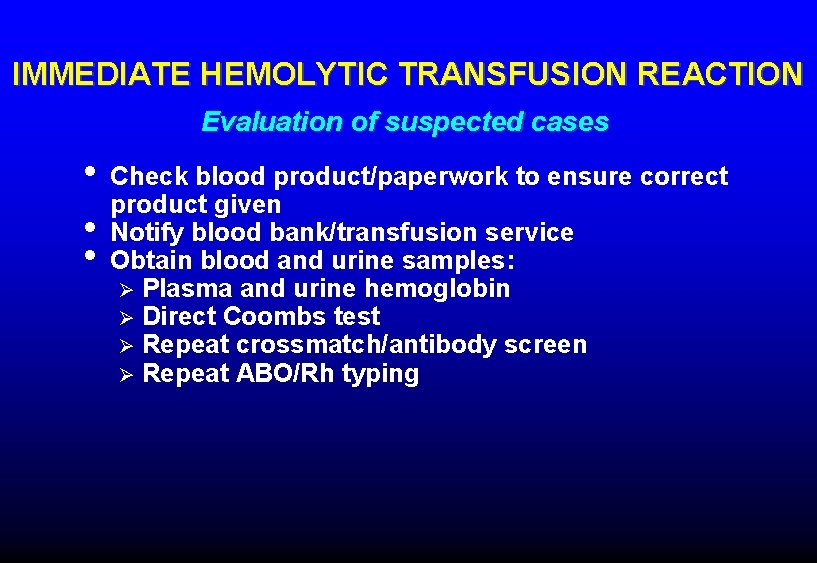
IMMEDIATE HEMOLYTIC TRANSFUSION REACTION Evaluation of suspected cases • • • Check blood product/paperwork to ensure correct product given Notify blood bank/transfusion service Obtain blood and urine samples: Ø Plasma and urine hemoglobin Ø Direct Coombs test Ø Repeat crossmatch/antibody screen Ø Repeat ABO/Rh typing
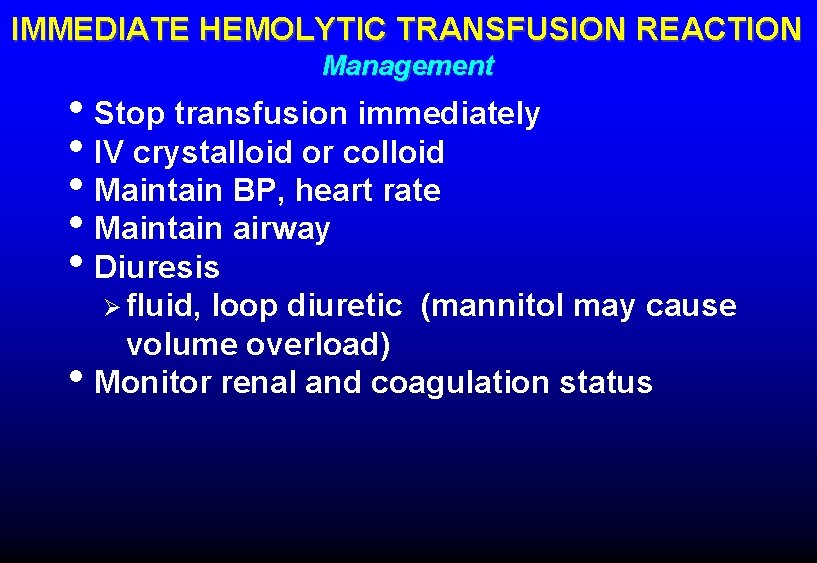
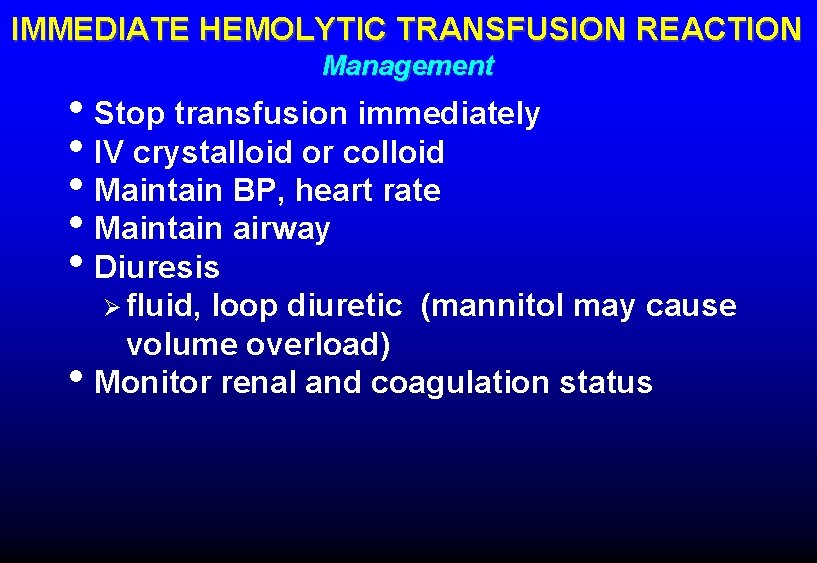
IMMEDIATE HEMOLYTIC TRANSFUSION REACTION Management • Stop transfusion immediately • IV crystalloid or colloid • Maintain BP, heart rate • Maintain airway • Diuresis Ø fluid, • loop diuretic (mannitol may cause volume overload) Monitor renal and coagulation status
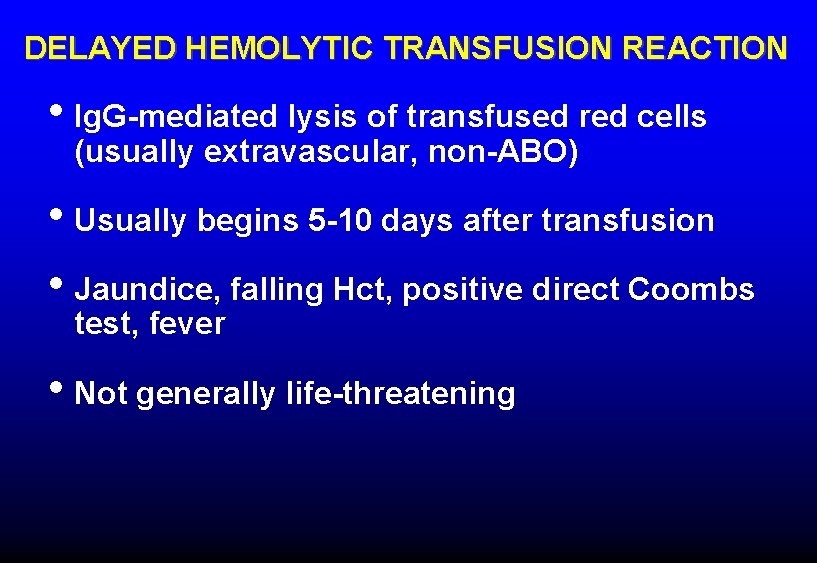
DELAYED HEMOLYTIC TRANSFUSION REACTION • Ig. G-mediated lysis of transfused red cells (usually extravascular, non-ABO) • Usually begins 5 -10 days after transfusion • Jaundice, falling Hct, positive direct Coombs test, fever • Not generally life-threatening
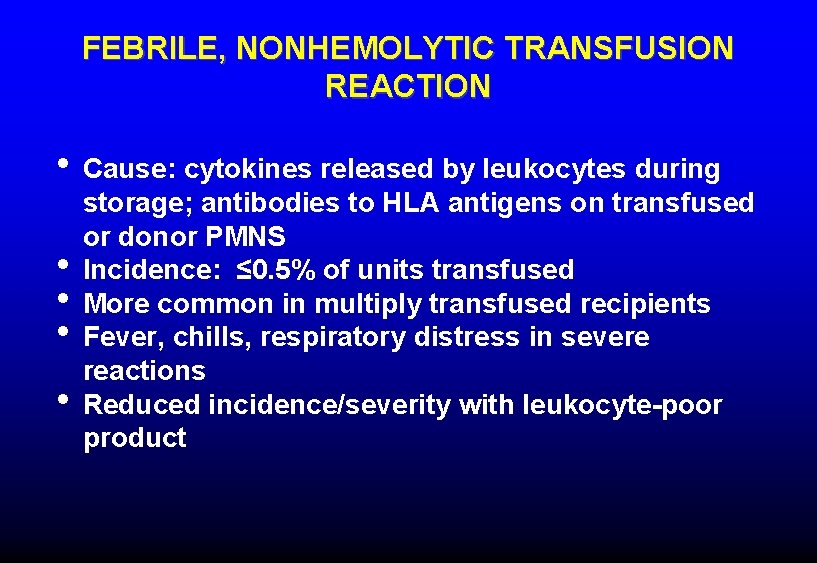
FEBRILE, NONHEMOLYTIC TRANSFUSION REACTION • Cause: cytokines released by leukocytes during • • storage; antibodies to HLA antigens on transfused or donor PMNS Incidence: ≤ 0. 5% of units transfused More common in multiply transfused recipients Fever, chills, respiratory distress in severe reactions Reduced incidence/severity with leukocyte-poor product
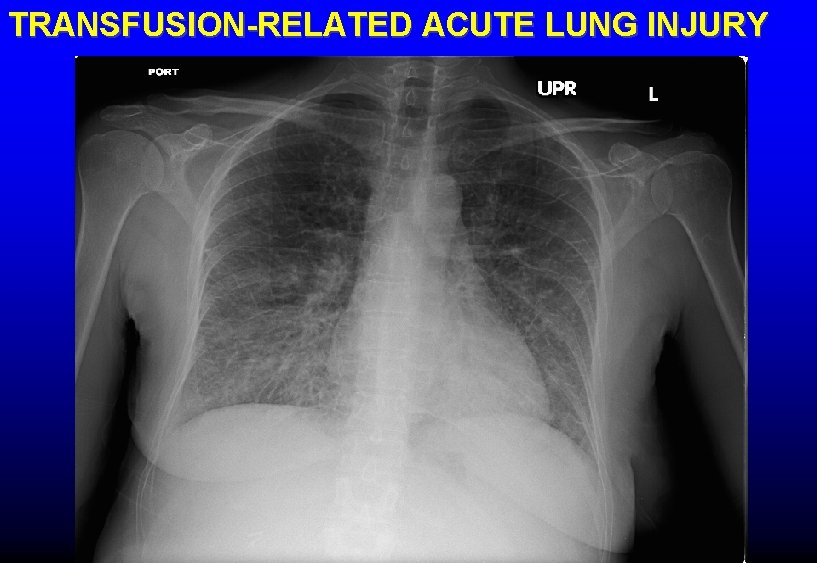
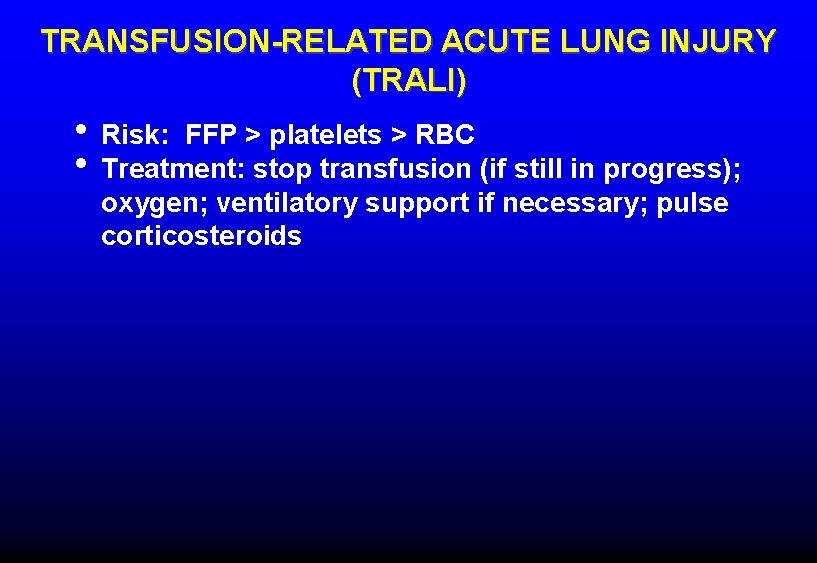
TRANSFUSION-RELATED ACUTE LUNG INJURY (TRALI) • Hypoxemia with bilateral pulmonary infiltrates • No increase in central venous or pulmonary artery • • • pressures Usually begins acutely within 6 hours of transfusion Clinical: acute respiratory distress, fever, chills Pathophysiology: 1. Underlying lung injury (eg, sepsis, pneumonia) causes PMNs to adhere to pulmonary capillaries 2. Mediators in transfused blood product (neutrophil antibodies, cytokines) activate PMNs with resultant capillary injury
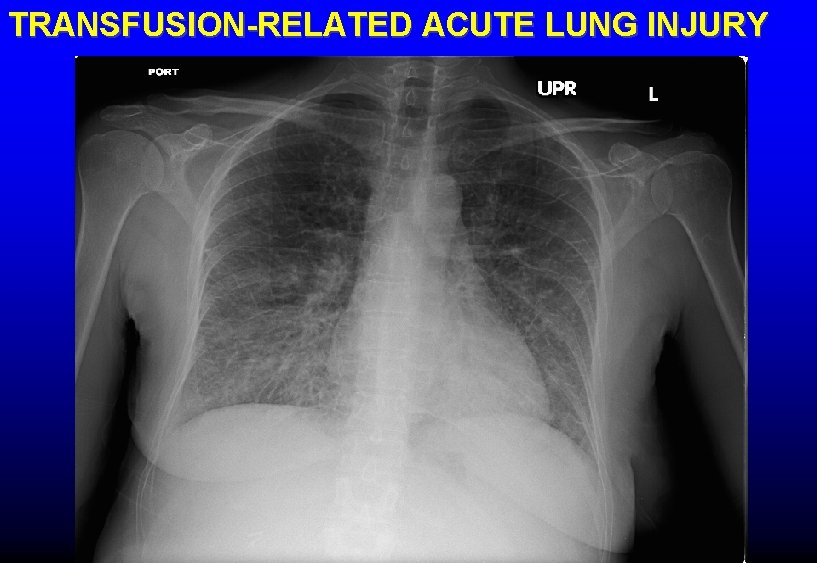
TRANSFUSION-RELATED ACUTE LUNG INJURY
TRANSFUSION-RELATED ACUTE LUNG INJURY (TRALI) • Risk: FFP > platelets > RBC • Treatment: stop transfusion (if still in progress); oxygen; ventilatory support if necessary; pulse corticosteroids
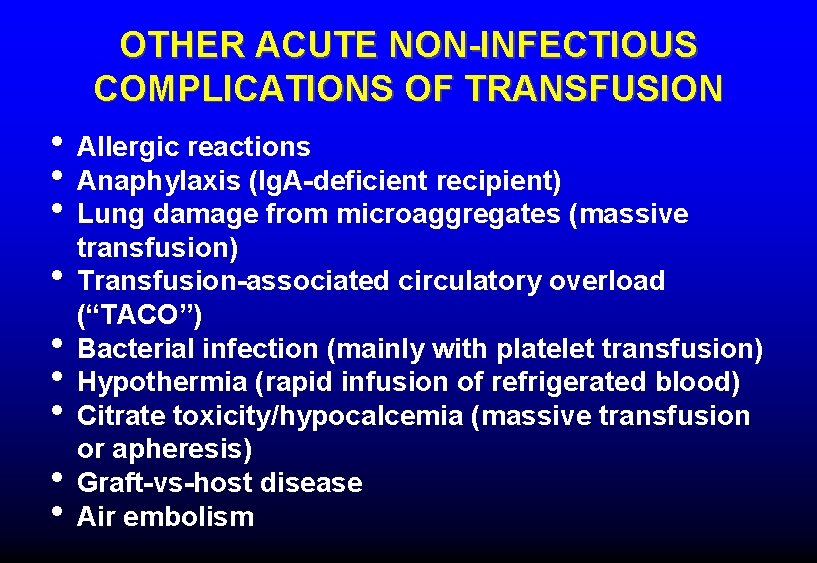
OTHER ACUTE NON-INFECTIOUS COMPLICATIONS OF TRANSFUSION • Allergic reactions • Anaphylaxis (Ig. A-deficient recipient) • Lung damage from microaggregates (massive • • • transfusion) Transfusion-associated circulatory overload (“TACO”) Bacterial infection (mainly with platelet transfusion) Hypothermia (rapid infusion of refrigerated blood) Citrate toxicity/hypocalcemia (massive transfusion or apheresis) Graft-vs-host disease Air embolism
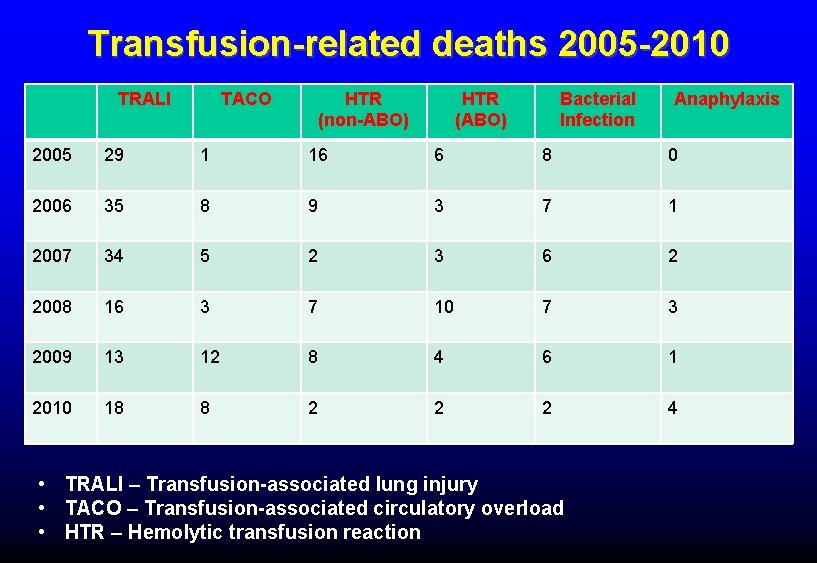
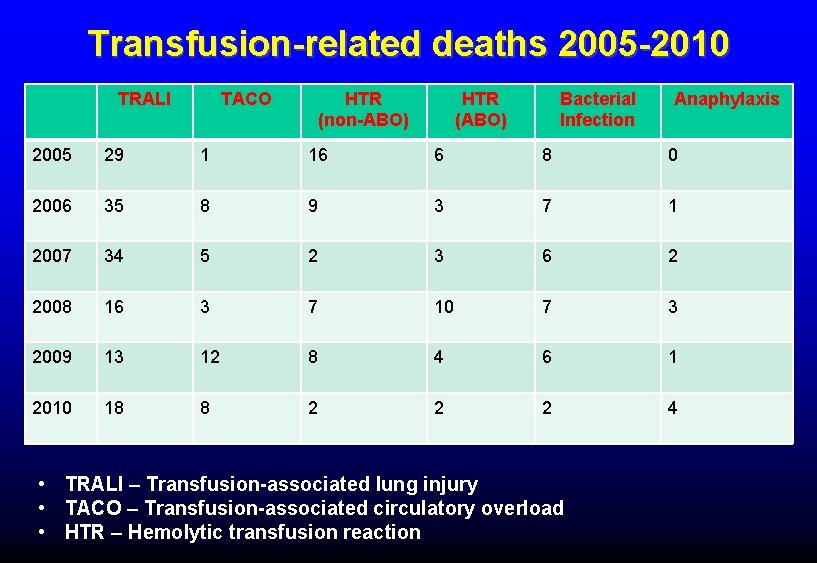
Transfusion-related deaths 2005 -2010 TRALI TACO HTR (non-ABO) HTR (ABO) Bacterial Infection Anaphylaxis 2005 29 1 16 6 8 0 2006 35 8 9 3 7 1 2007 34 5 2 3 6 2 2008 16 3 7 10 7 3 2009 13 12 8 4 6 1 2010 18 8 2 2 2 4 • TRALI – Transfusion-associated lung injury • TACO – Transfusion-associated circulatory overload • HTR – Hemolytic transfusion reaction
 Intravascular hemolytic anemia
Intravascular hemolytic anemia Blood loss
Blood loss Fresh frozen plasma contents
Fresh frozen plasma contents Febrile nonhemolytic transfusion reaction
Febrile nonhemolytic transfusion reaction Hemolytic transfusion reaction
Hemolytic transfusion reaction Transfusion en urgence vitale immédiate
Transfusion en urgence vitale immédiate Liquido intravascular
Liquido intravascular Hus dic
Hus dic Farmacodin
Farmacodin Disseminated intravascular coagulation pathophysiology
Disseminated intravascular coagulation pathophysiology Esquema de liquidos corporales
Esquema de liquidos corporales Generalidades de la mecanica corporal
Generalidades de la mecanica corporal