Disseminated intravascular coagulation n Disseminated intravascular coagulation DIC
- Slides: 18
Disseminated intravascular coagulation n Disseminated intravascular coagulation (DIC) is a state/syndrome which is characterized by accelerated intravascular coagulation associated with increased consumption of platelets and plasma clotting factors.
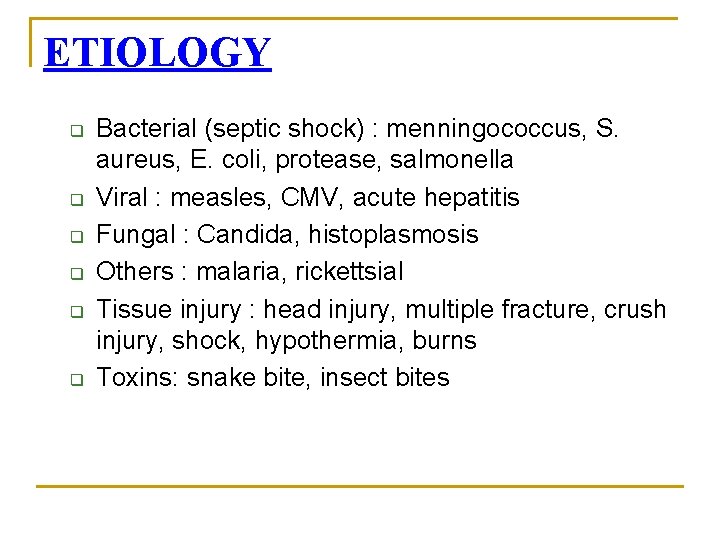
ETIOLOGY q q q Bacterial (septic shock) : menningococcus, S. aureus, E. coli, protease, salmonella Viral : measles, CMV, acute hepatitis Fungal : Candida, histoplasmosis Others : malaria, rickettsial Tissue injury : head injury, multiple fracture, crush injury, shock, hypothermia, burns Toxins: snake bite, insect bites
Cont. . q q q Hematological : incompatible blood transfusion, sickle cell anemia, acut iron toxicity Neonatal causes: septicemia, RDS, birth asphyxia, necrotising enterocolitis, hypothermia Obstetric complication: pre – eclampsia, septic abortion, maternal toxemia, retained fetus Collagen vascular disease: JRA, SLE, acute vasculitis Miscellaneous: major surgery, heat stroke, graft reaction, acute pancreatitis
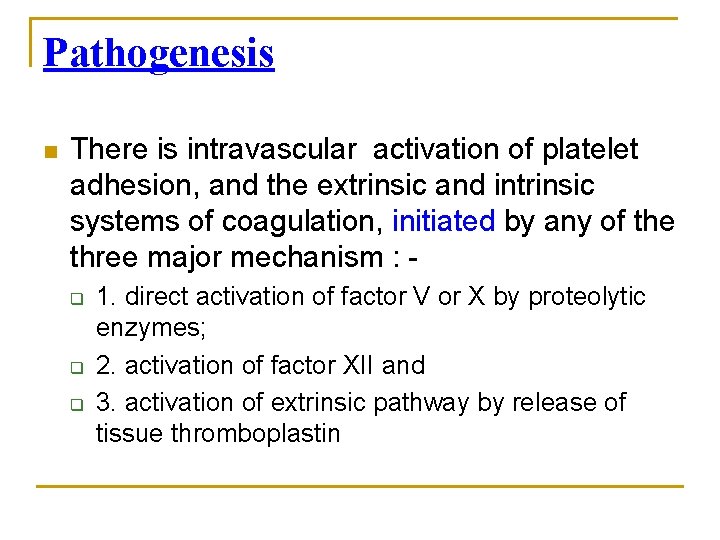
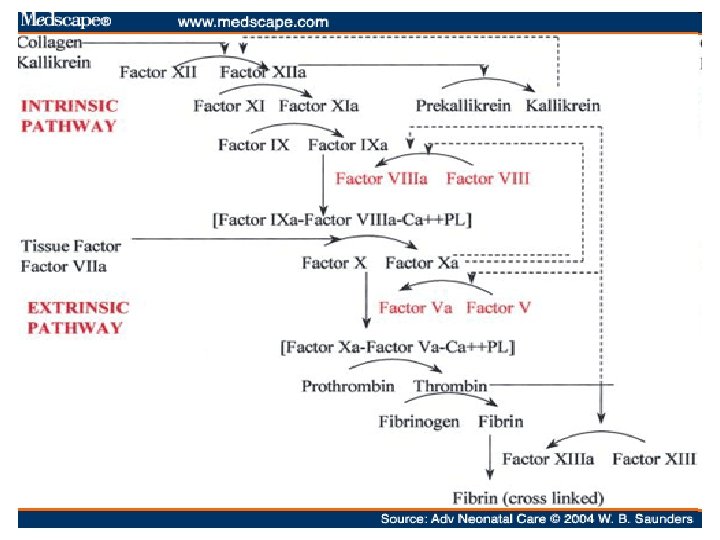
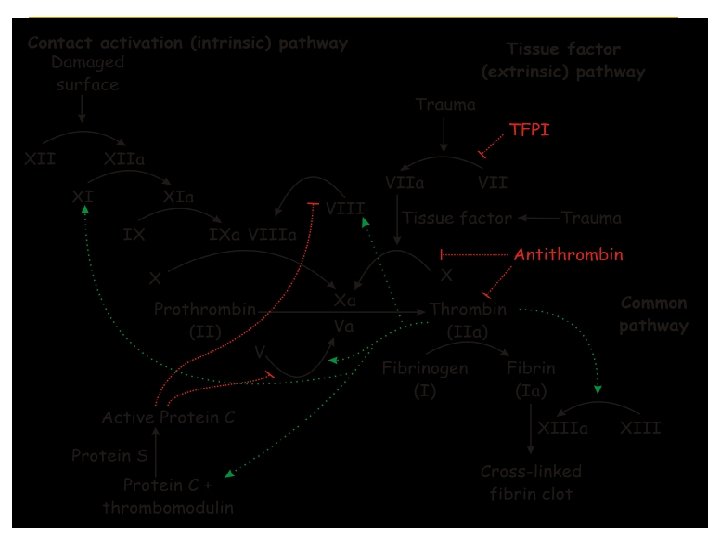
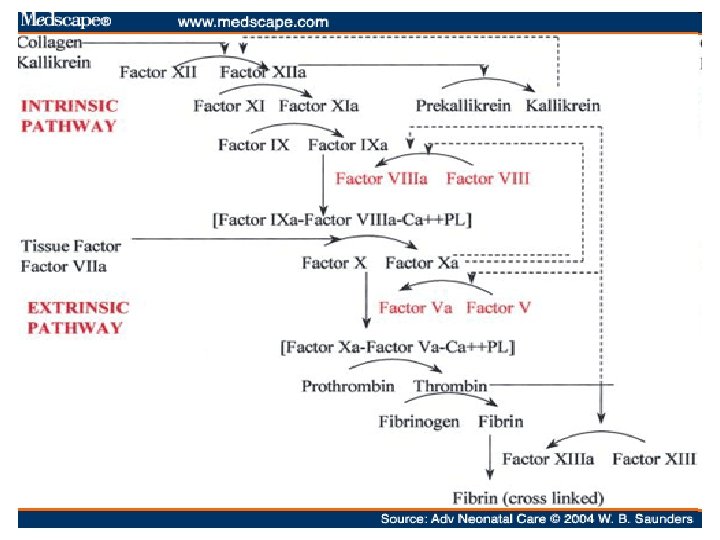
Pathogenesis n There is intravascular activation of platelet adhesion, and the extrinsic and intrinsic systems of coagulation, initiated by any of the three major mechanism : q q q 1. direct activation of factor V or X by proteolytic enzymes; 2. activation of factor XII and 3. activation of extrinsic pathway by release of tissue thromboplastin
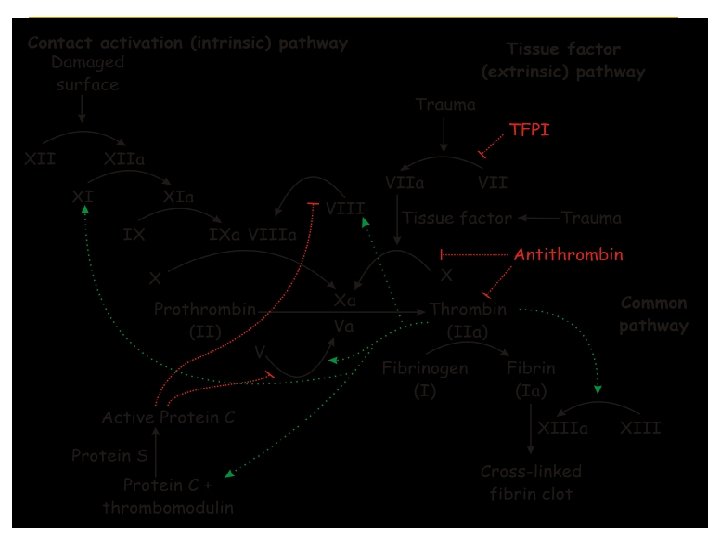
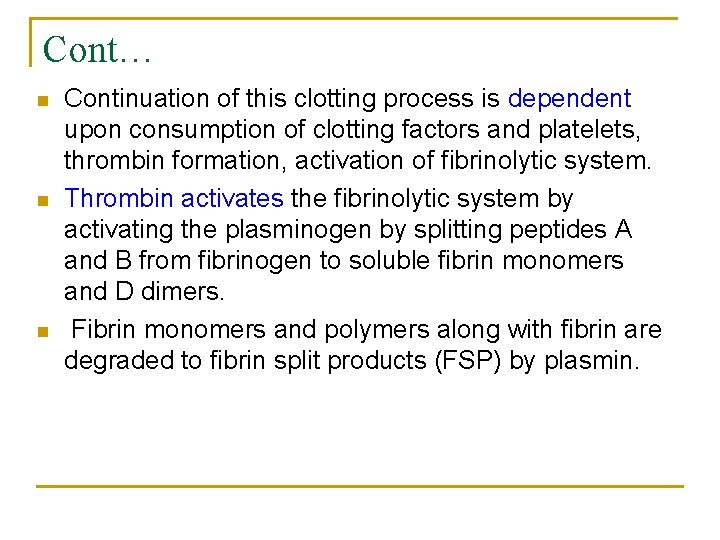
Cont… n n n Continuation of this clotting process is dependent upon consumption of clotting factors and platelets, thrombin formation, activation of fibrinolytic system. Thrombin activates the fibrinolytic system by activating the plasminogen by splitting peptides A and B from fibrinogen to soluble fibrin monomers and D dimers. Fibrin monomers and polymers along with fibrin are degraded to fibrin split products (FSP) by plasmin.
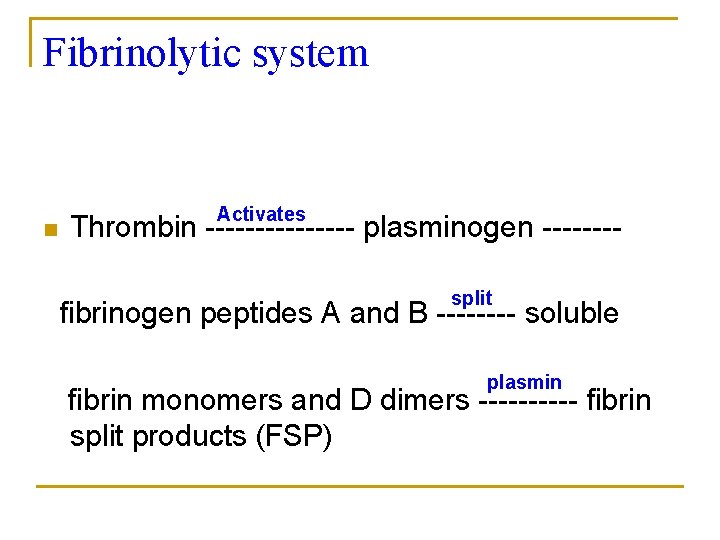
Fibrinolytic system n Activates Thrombin -------- plasminogen -------split fibrinogen peptides A and B ---- soluble plasmin fibrin monomers and D dimers ----- fibrin split products (FSP)
Cont. . n n Increased levels of D – dimers and FSP are the pathognomonic of DIC Thrombin functions : activates fibrinolytic system activates factor XIII which acts on the fibrin polymers to form fibrin split products. induces platelet adhesion and aggregation, leading to platelet consumption and thrombocytopenia.
Cont. . Course of DIC is determined by : q q q 1. platelet production versus platelet destruction; 2. fibrin deposition versus fibrinolysis and 3. synthesis of coagulation factor versus their depletion
Cont. . Process of DIC results in : n n n 1. increased thromboembolic phenomenon causing tissue ischemia and necrosis of multiple organs; 2. depletion of clotting and antihemostatic effects of FSP resulting in bleeding and hemorrhages at multiple sites; 3. red cell fragments
Clinical features n n n Purpura, ecchymosis, easy bruising, and bleeding from gums and mucous membranes. Shock Hematuria, oliguria leading to acute renal failure, abdominal pain, vomiting and respiratory distress
Differential diagnosis n n n Acute fulminant liver failure Hemolytic uremia syndrome Renal failure
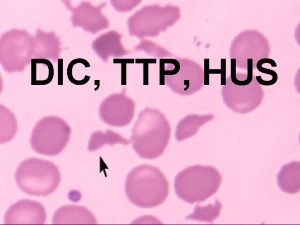
Lab investigation q q q Low platelet count Low levels of fibrinogen, factor II, V, X, VIII and XIII Prolonged PT, APTT and TT Low levels of antithrombin III, heparin cofactor II, protein C Increased level of fibrin split products and Microangiopathic hemolytic anemia as indicated by the presence of red cell fragmentation.
Treatment n n n Management of: Acidosis, electrolyte disturbances, hypoxia, shock Anemia (packed cells) Hydrocortisone Vitamin K
Cont… Replacement therapy : n Fresh frozen plasma (FFP) : q q q Fibrinogen level should be raised to over 150 mg/d. L 10 – 15 m. L/kg of FFP along with ½ to 1 unit of platele concentrates every 12 – 24 hours Platelat count should be maintained above 50, 000/micro. L while fibrinogen level should be maintained above 75 mg/d. L.
Cont…. Exchange transfusion : q q q Double volume exchange transfusion helps by providing the replacement factors and removing the A. circulating fibrin split products (FSP) B. activated procoagulant: and C. toxins Platelet concentrates should be administered after the exchange for the successful management of DIC.
Cont… Heparin : q q Inhibits number of proteolytic enzymes and factors such as thrombin, IXa and Xa Dose : 15 – 20 units/kg hour as continuous drip or 50 – 70 units/kg/6 hourly Mortality : q q Prolongation of PT (>1. 5 times) and APTT (>2, 5 times) indicates poor prognosis.
 Disseminated intravascular coagulation pathophysiology
Disseminated intravascular coagulation pathophysiology Dic labs
Dic labs Two node loop instability
Two node loop instability Distribucion agua corporal total
Distribucion agua corporal total Farmacodin
Farmacodin Liquido intravascular
Liquido intravascular Esquema de liquidos corporales
Esquema de liquidos corporales Intravascular hemolytic anemia
Intravascular hemolytic anemia Sergio atala dib
Sergio atala dib Intravascular ultrasound
Intravascular ultrasound Curva de titulação da glicina
Curva de titulação da glicina Ivus
Ivus Hus vs dic
Hus vs dic Differential interference microscopy
Differential interference microscopy Dic
Dic Monkey dic
Monkey dic Hola em dic
Hola em dic Dic phase contrast
Dic phase contrast Claudia coppo
Claudia coppo