Disseminated Intravascular Coagulation DIC n n An acquired


- Slides: 17

Disseminated Intravascular Coagulation.
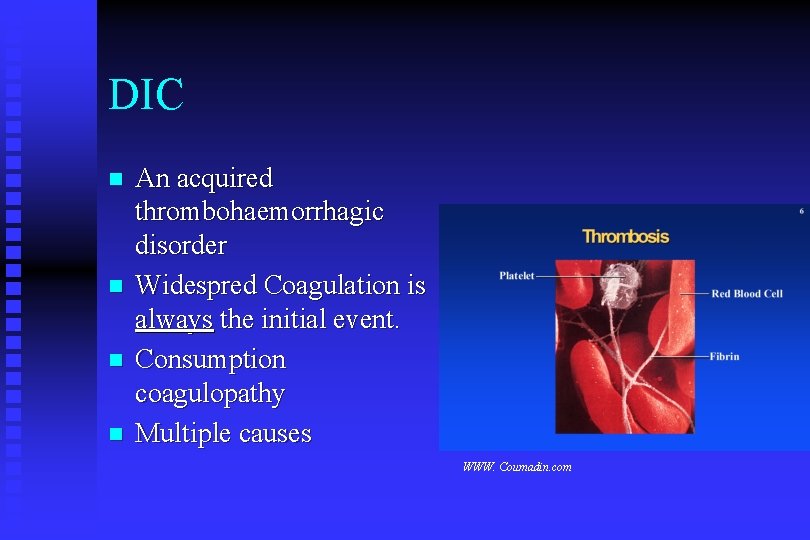
DIC n n An acquired thrombohaemorrhagic disorder Widespred Coagulation is always the initial event. Consumption coagulopathy Multiple causes WWW. Coumadin. com
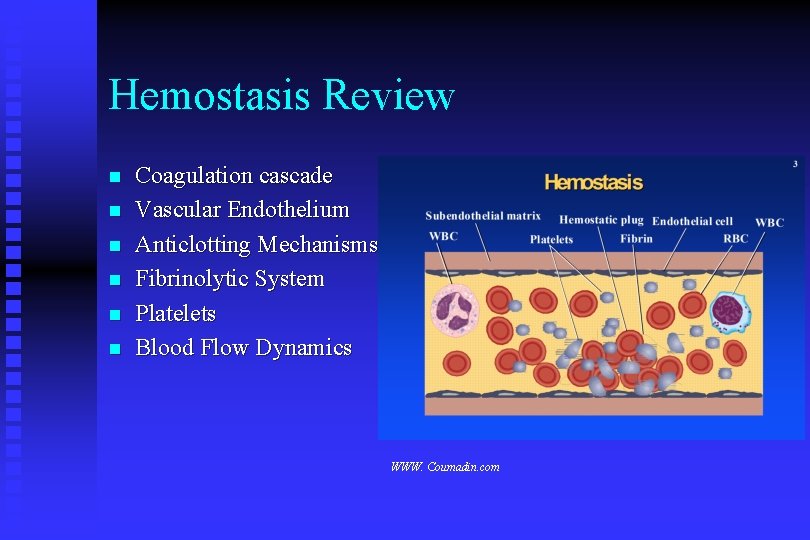
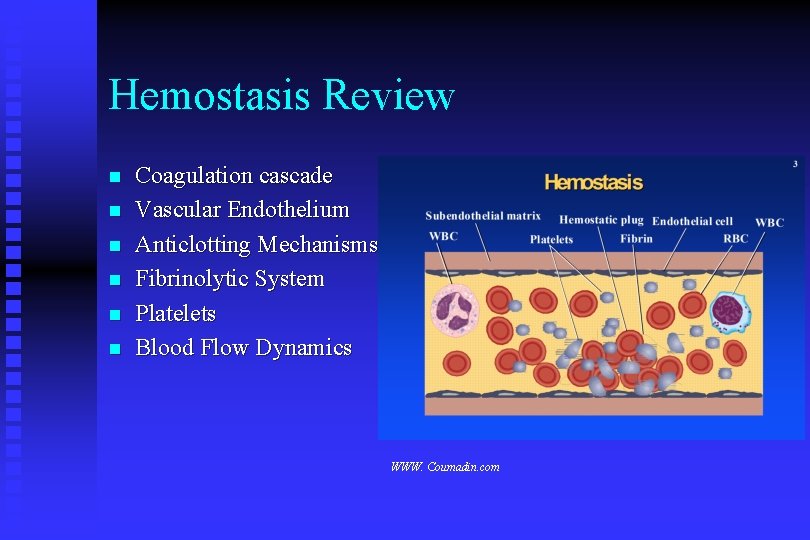
Hemostasis Review n n n Coagulation cascade Vascular Endothelium Anticlotting Mechanisms Fibrinolytic System Platelets Blood Flow Dynamics WWW. Coumadin. com
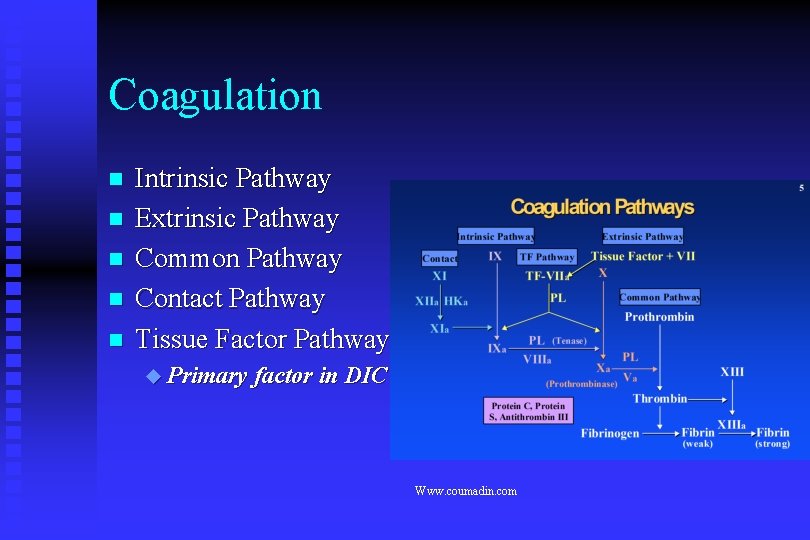
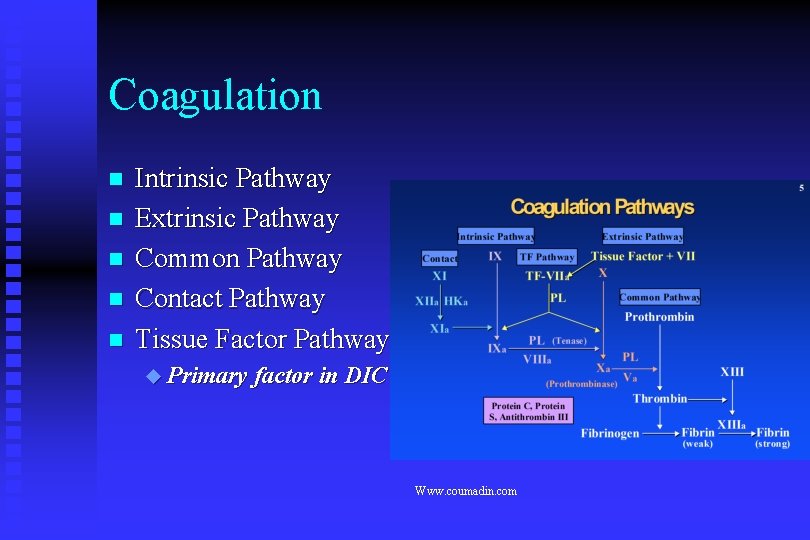
Coagulation n n Intrinsic Pathway Extrinsic Pathway Common Pathway Contact Pathway Tissue Factor Pathway Primary factor in DIC Www. coumadin. com
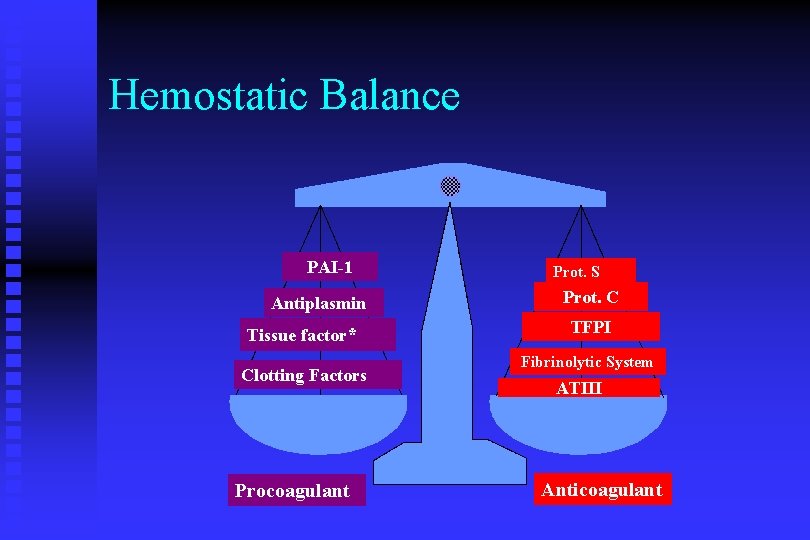
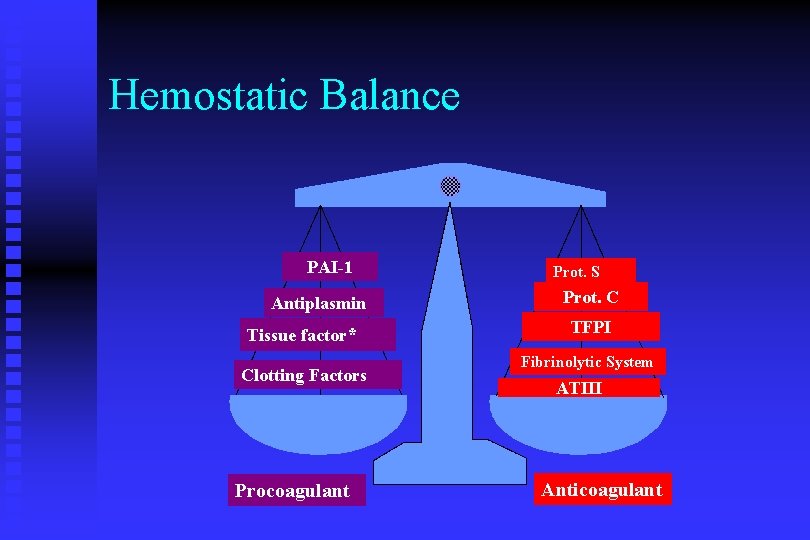
Hemostatic Balance PAI-1 Antiplasmin Tissue factor* Clotting Factors Procoagulant Prot. S Prot. C TFPI Fibrinolytic System ATIII Anticoagulant
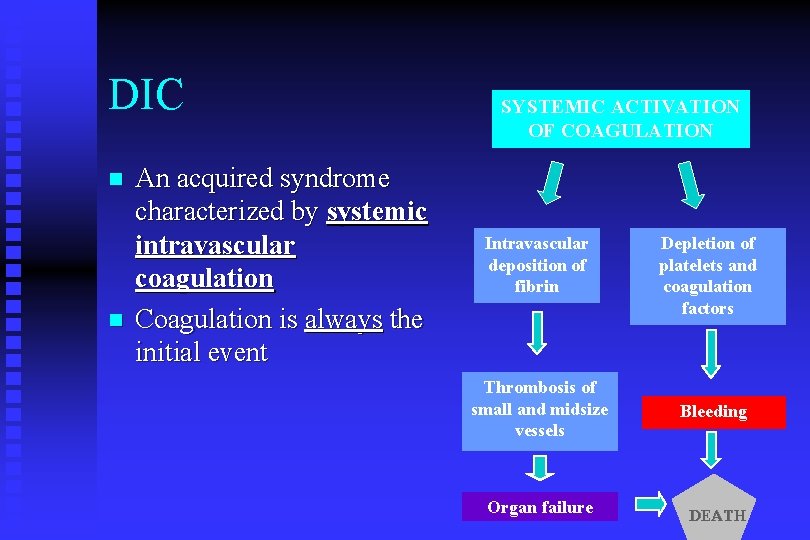
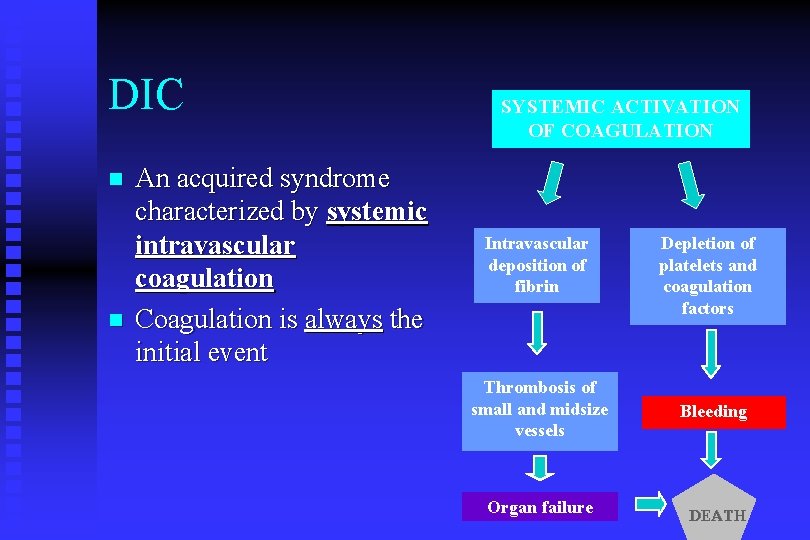
DIC n n An acquired syndrome characterized by systemic intravascular coagulation Coagulation is always the initial event SYSTEMIC ACTIVATION OF COAGULATION Intravascular deposition of fibrin Thrombosis of small and midsize vessels Organ failure Depletion of platelets and coagulation factors Bleeding DEATH
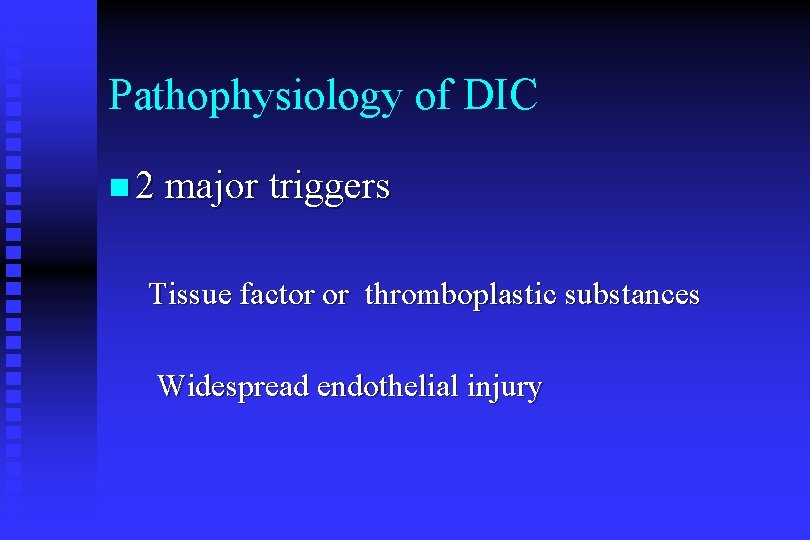
Pathophysiology of DIC n 2 major triggers Tissue factor or thromboplastic substances Widespread endothelial injury
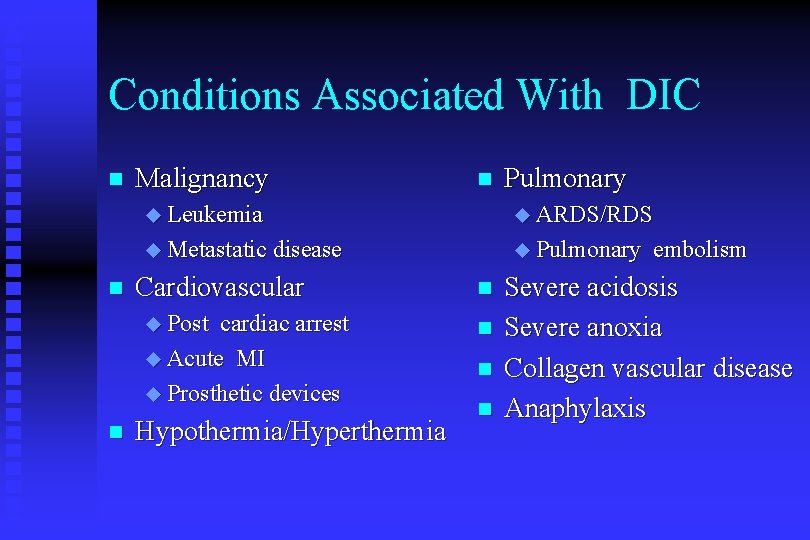
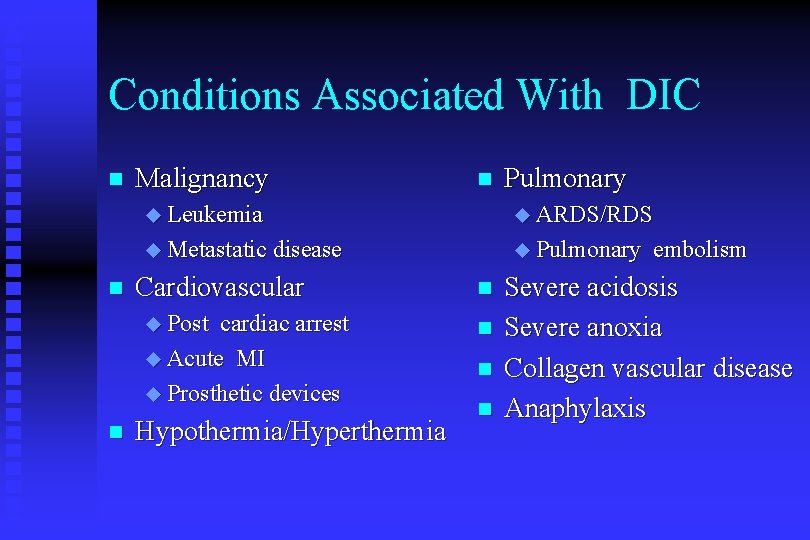
Conditions Associated With DIC n n Malignancy Pulmonary Leukemia ARDS/RDS Metastatic disease Pulmonary Cardiovascular Post cardiac arrest Acute MI Prosthetic devices n n Hypothermia/Hyperthermia n n embolism Severe acidosis Severe anoxia Collagen vascular disease Anaphylaxis
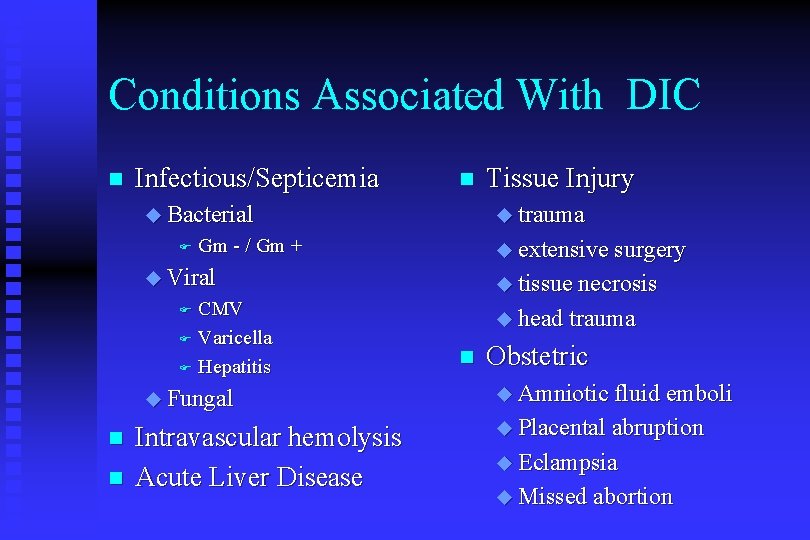
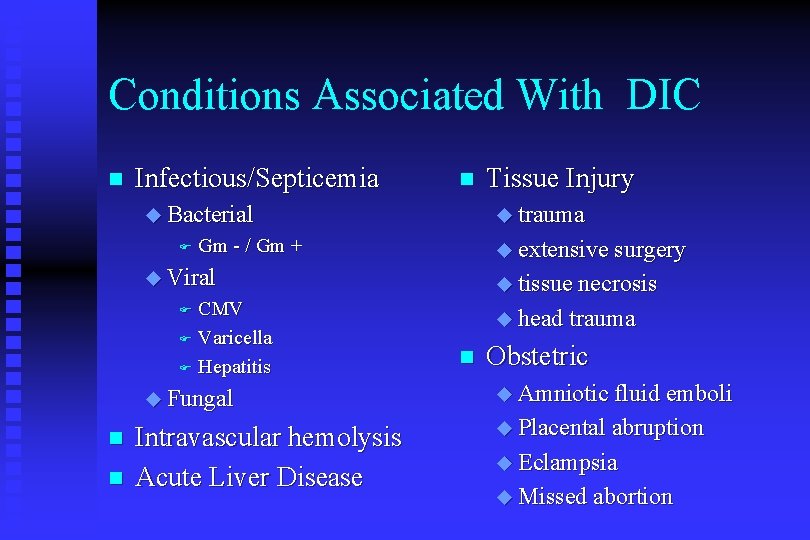
Conditions Associated With DIC n Infectious/Septicemia n Bacterial F trauma Gm - / Gm + extensive surgery Viral CMV F Varicella F Hepatitis tissue necrosis F Fungal n n Intravascular hemolysis Acute Liver Disease Tissue Injury head trauma n Obstetric Amniotic fluid emboli Placental abruption Eclampsia Missed abortion
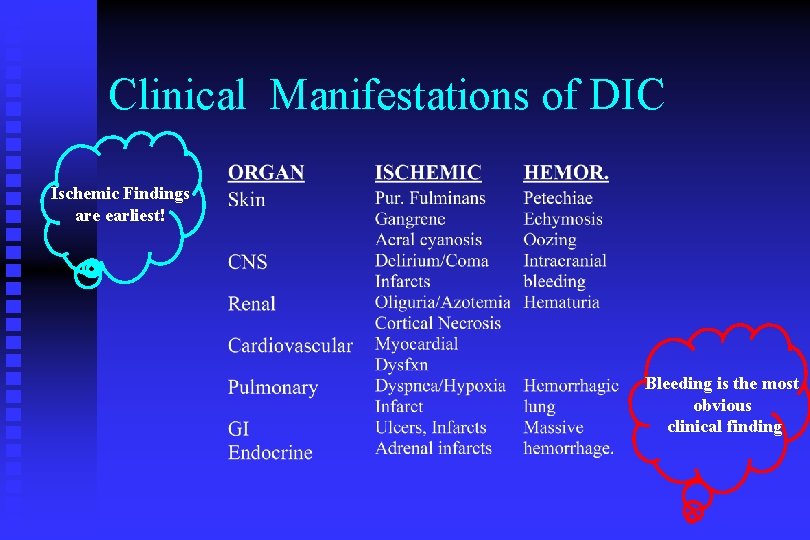
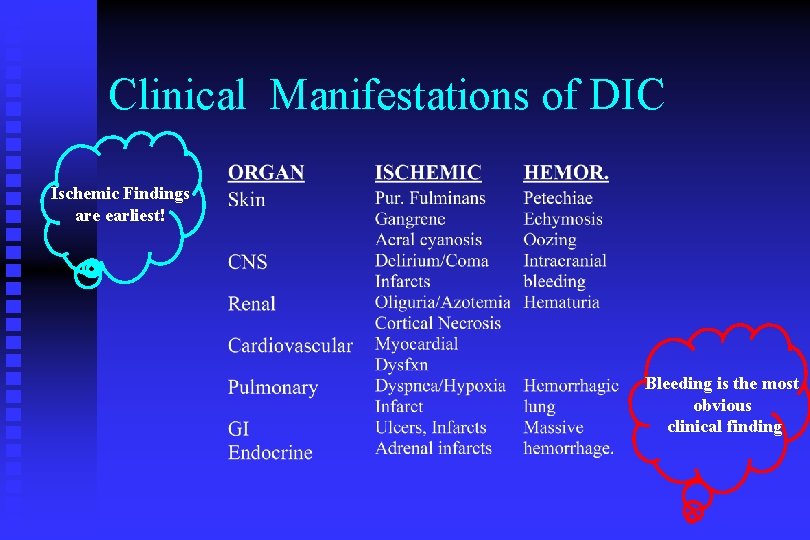
Clinical Manifestations of DIC Ischemic Findings are earliest! Bleeding is the most obvious clinical finding

Clinical Manifestations of DIC
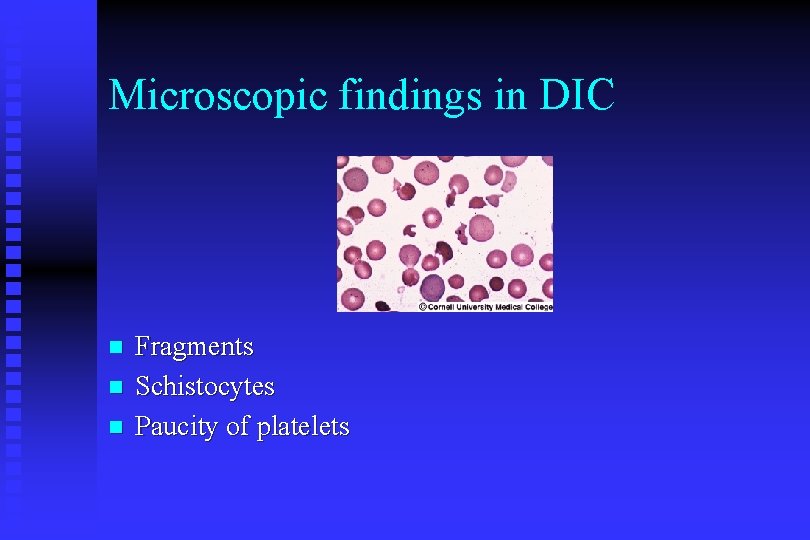
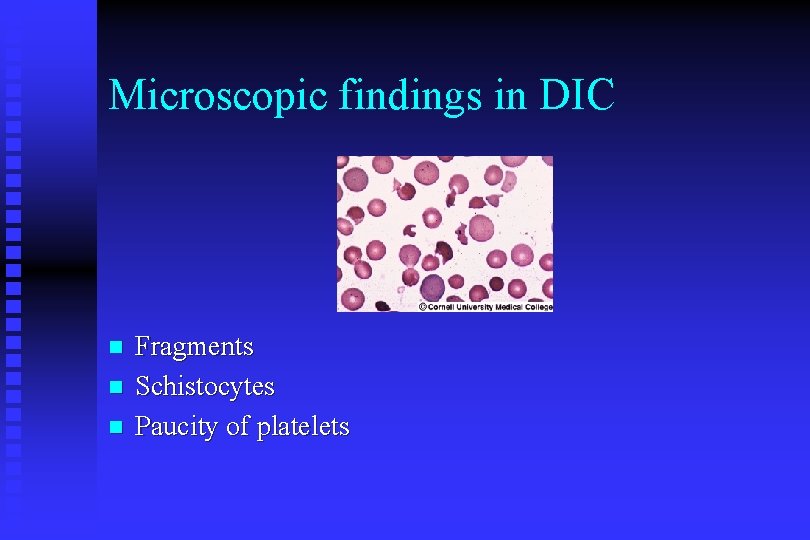
Microscopic findings in DIC n n n Fragments Schistocytes Paucity of platelets
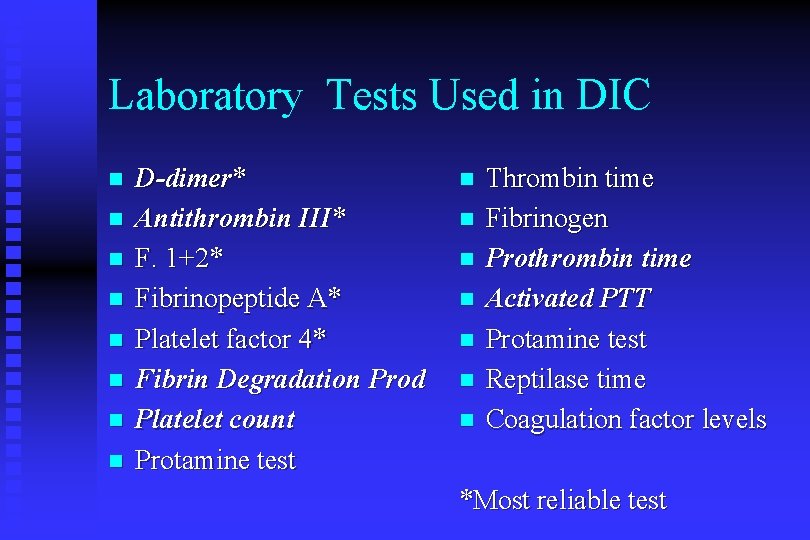
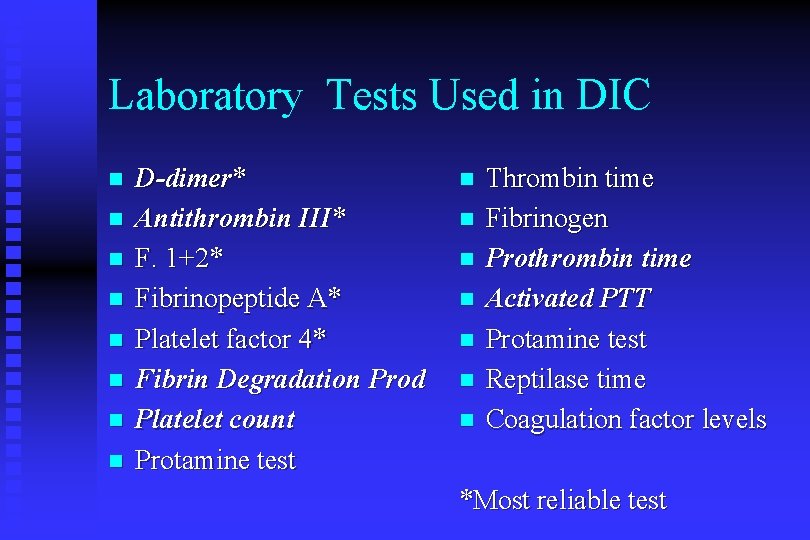
Laboratory Tests Used in DIC n n n n D-dimer* Antithrombin III* F. 1+2* Fibrinopeptide A* Platelet factor 4* Fibrin Degradation Prod Platelet count Protamine test n n n n Thrombin time Fibrinogen Prothrombin time Activated PTT Protamine test Reptilase time Coagulation factor levels *Most reliable test
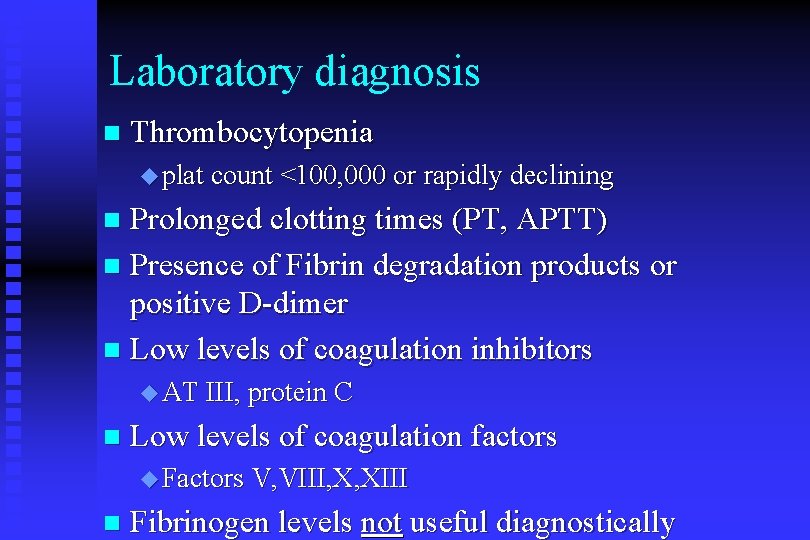
Laboratory diagnosis n Thrombocytopenia plat count <100, 000 or rapidly declining Prolonged clotting times (PT, APTT) n Presence of Fibrin degradation products or positive D-dimer n Low levels of coagulation inhibitors n AT III, protein C n Low levels of coagulation factors Factors V, VIII, X, XIII n Fibrinogen levels not useful diagnostically
Treatment of DIC n Stop the triggering process. The only proven treatment! Supportive therapy n No specific treatments n Plasma and platelet substitution therapy Anticoagulants Physiologic coagulation inhibitors
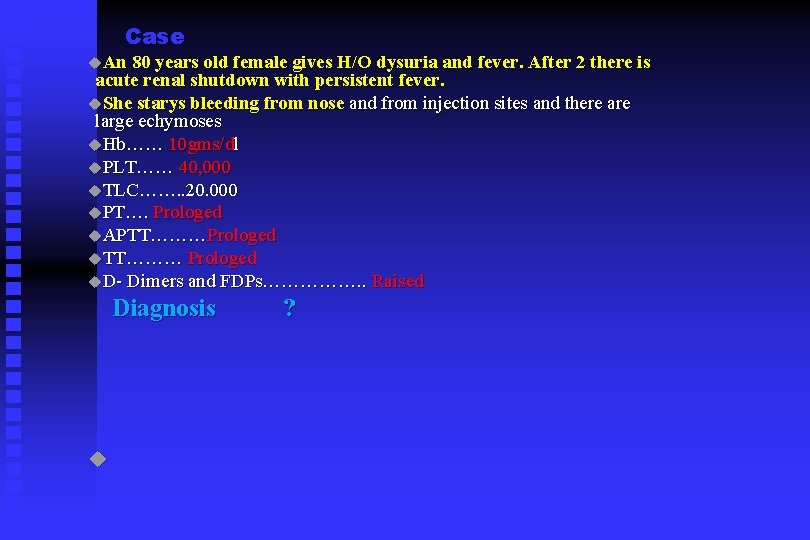
Case An 80 years old female gives H/O dysuria and fever. After 2 there is acute renal shutdown with persistent fever. She starys bleeding from nose and from injection sites and there are large echymoses Hb…… 10 gms/dl PLT…… 40, 000 TLC……. . 20. 000 PT…. Prologed APTT………Prologed TT……… Prologed D- Dimers and FDPs……………. . Raised Diagnosis ?
SEQ Q 10 page 25, Key to UHS n Q 27 page no. 35 Key to UHS n