Autoimmune Hepatitis Autore Dott ssa Claudia Coppo Tutor
- Slides: 33
Autoimmune Hepatitis Autore: Dott. ssa Claudia Coppo Tutor: Prof. ssa Patrizia Zentilin
Autoimmune Hepatitis Immune-mediated chronic hepatitis of unknown etiology that, if untreated, can evolve to cirrhosis and end stage liver disease. ü Incidence: from 0. 5 to 1. 9 x 105/year ü Prevalence: from 4 to 43 x 105 ü Serum autoantibodies ü Interface Hepatitis ü Hypergammaglobulinemia without cirrhosis
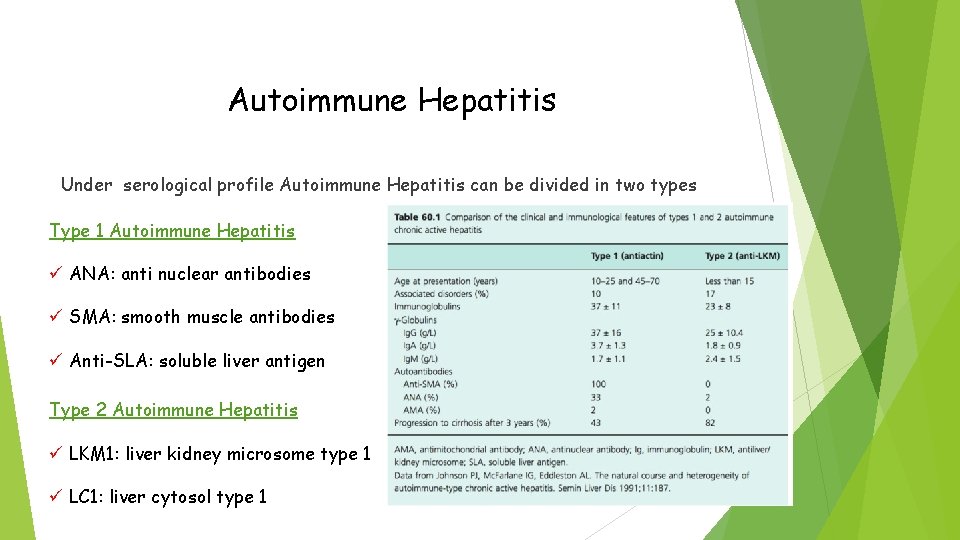
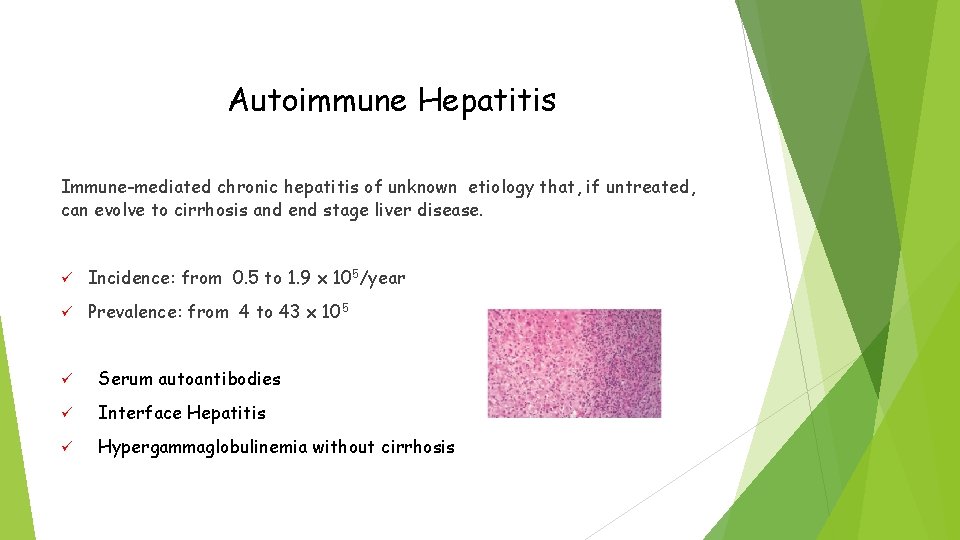
Autoimmune Hepatitis Under serological profile Autoimmune Hepatitis can be divided in two types Type 1 Autoimmune Hepatitis ü ANA: anti nuclear antibodies ü SMA: smooth muscle antibodies ü Anti-SLA: soluble liver antigen Type 2 Autoimmune Hepatitis ü LKM 1: liver kidney microsome type 1 ü LC 1: liver cytosol type 1
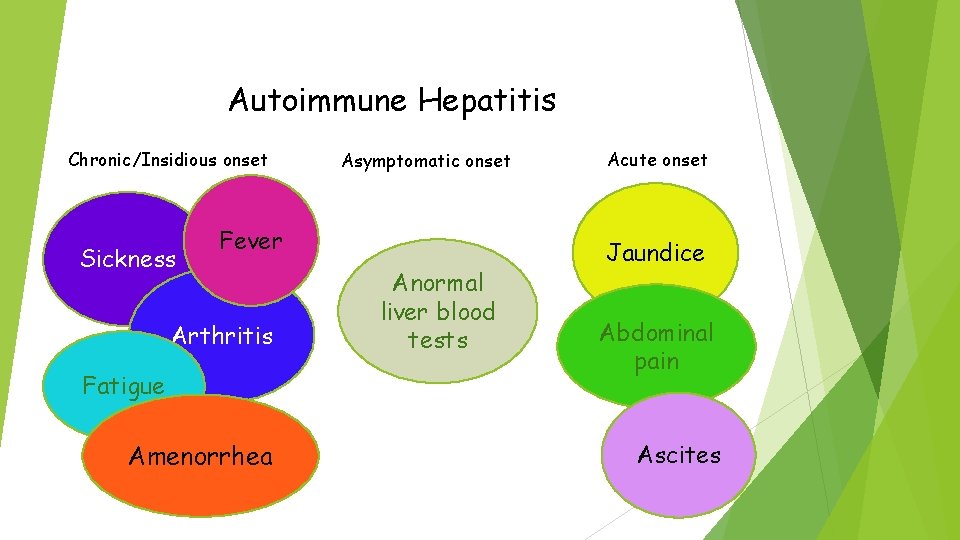
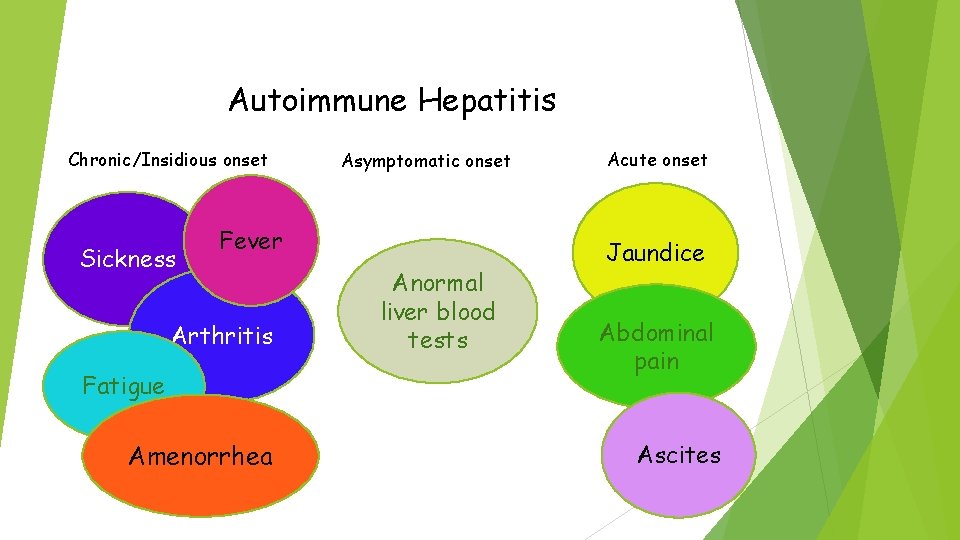
Autoimmune Hepatitis Chronic/Insidious onset Sickness Asymptomatic onset Fever Arthritis Fatigue Amenorrhea Anormal liver blood tests Acute onset Jaundice Abdominal pain Ascites
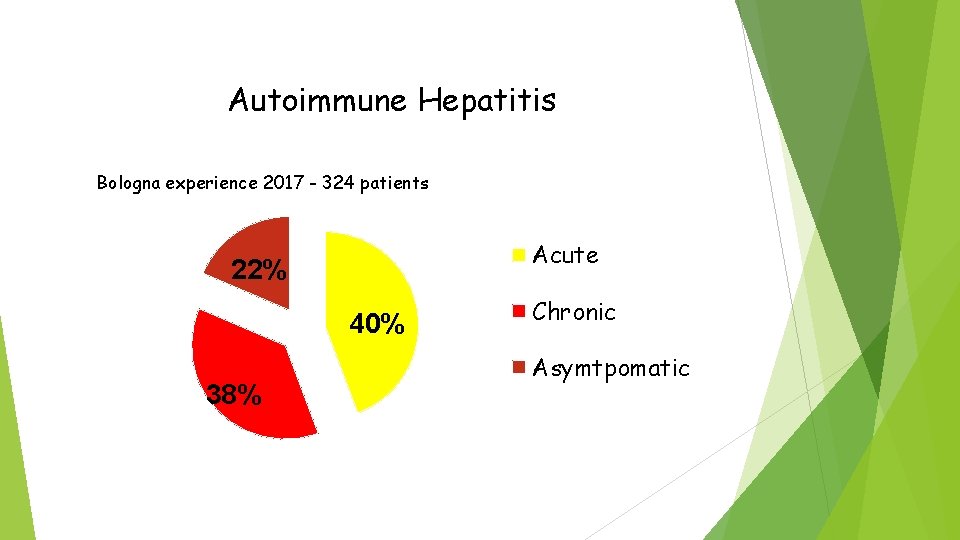
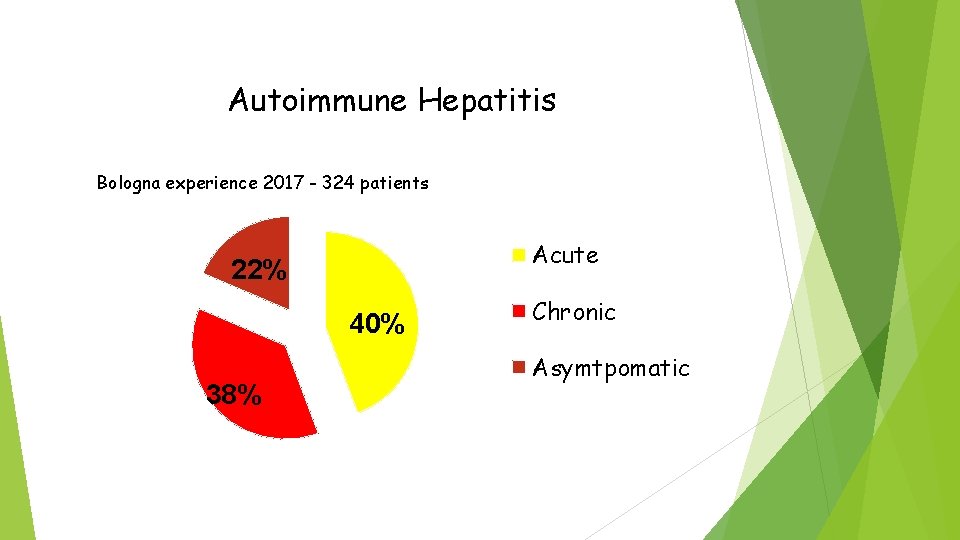
Autoimmune Hepatitis Bologna experience 2017 - 324 patients Acute 22% 40% 38% Chronic Asymtpomatic
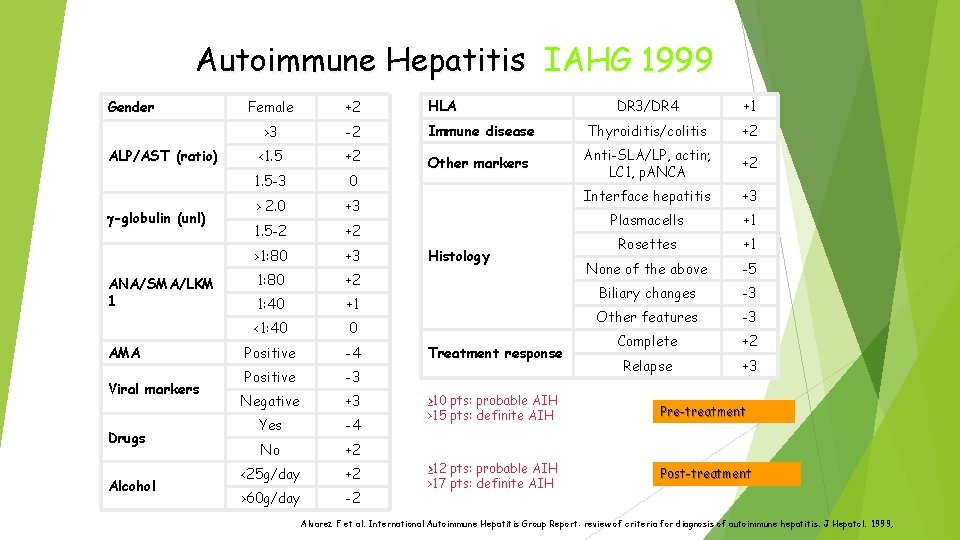
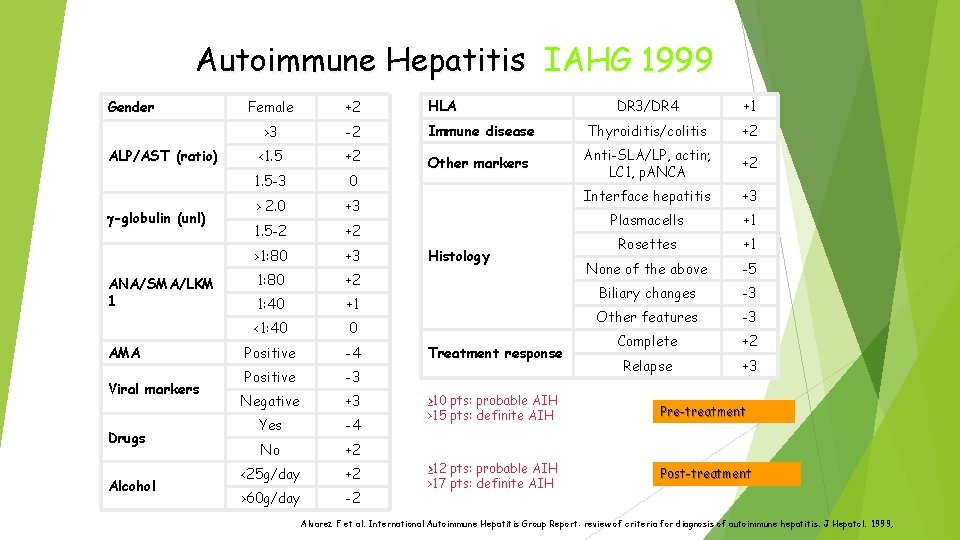
Autoimmune Hepatitis IAHG 1999 Gender ALP/AST (ratio) -globulin (unl) ANA/SMA/LKM 1 AMA Viral markers Drugs Alcohol Female +2 HLA DR 3/DR 4 +1 >3 -2 Immune disease Thyroiditis/colitis +2 <1. 5 +2 Other markers Anti-SLA/LP, actin; LC 1, p. ANCA +2 1. 5 -3 0 > 2. 0 +3 Interface hepatitis +3 1. 5 -2 +2 Plasmacells +1 >1: 80 +3 Rosettes +1 1: 80 +2 None of the above -5 1: 40 +1 Biliary changes -3 <1: 40 0 Other features -3 Positive -4 Complete +2 Positive -3 Relapse +3 Negative +3 Yes -4 No +2 <25 g/day +2 >60 g/day -2 Histology Treatment response ≥ 10 pts: probable AIH >15 pts: definite AIH Pre-treatment ≥ 12 pts: probable AIH >17 pts: definite AIH Post-treatment Alvarez F et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 1999;
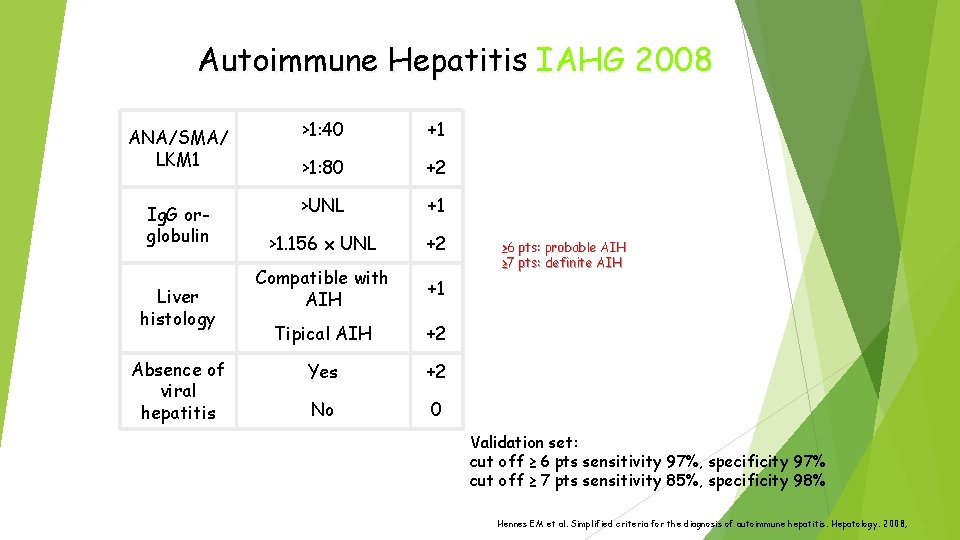
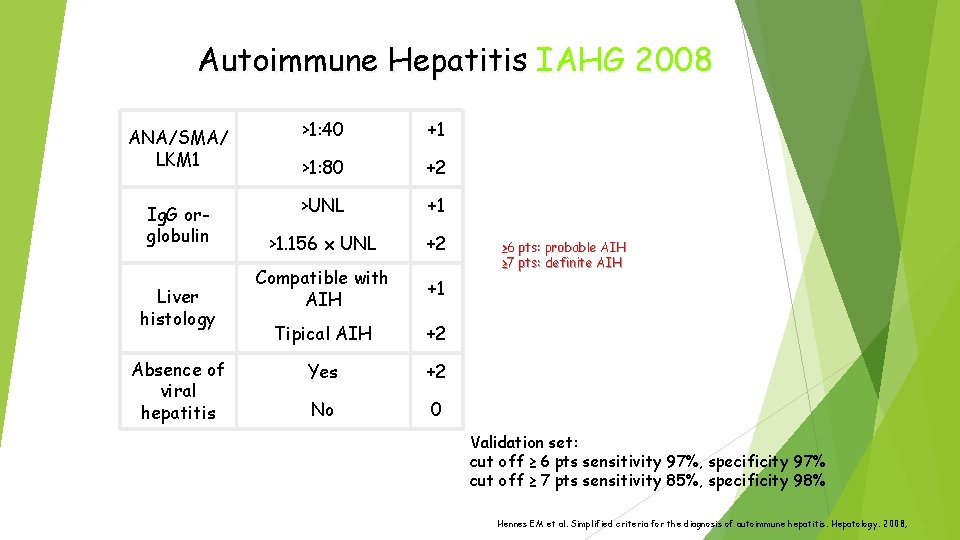
Autoimmune Hepatitis IAHG 2008 ANA/SMA/ LKM 1 >1: 40 +1 >1: 80 +2 Ig. G orglobulin >UNL +1 >1. 156 x UNL +2 Compatible with AIH +1 Tipical AIH +2 Yes +2 No 0 Liver histology Absence of viral hepatitis ≥ 6 pts: probable AIH ≥ 7 pts: definite AIH Validation set: cut off ≥ 6 pts sensitivity 97%, specificity 97% cut off ≥ 7 pts sensitivity 85%, specificity 98% Hennes EM et al. Simplified criteria for the diagnosis of autoimmune hepatitis. Hepatology. 2008;
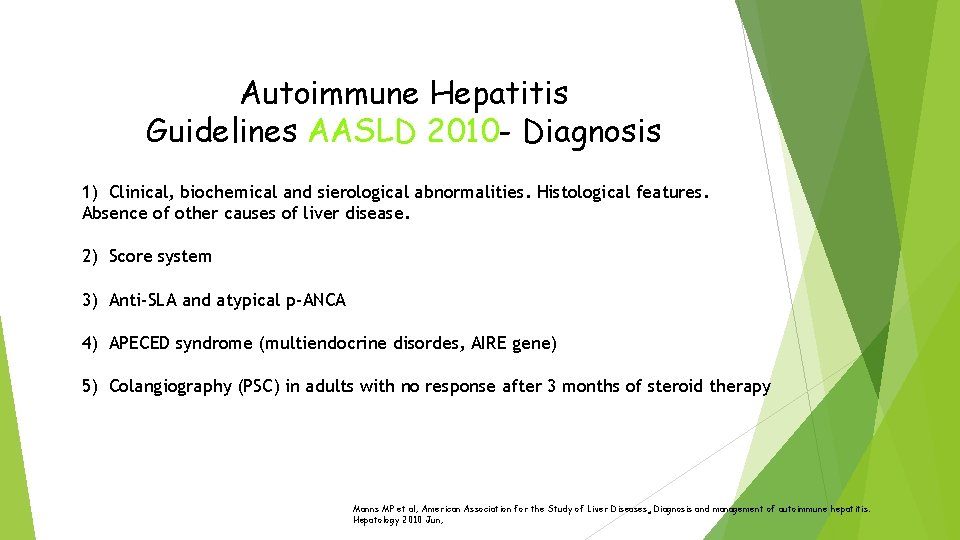
Autoimmune Hepatitis Guidelines AASLD 2010 - Diagnosis 1) Clinical, biochemical and sierological abnormalities. Histological features. Absence of other causes of liver disease. 2) Score system 3) Anti-SLA and atypical p-ANCA 4) APECED syndrome (multiendocrine disordes, AIRE gene) 5) Colangiography (PSC) in adults with no response after 3 months of steroid therapy Manns MP et al; American Association for the Study of Liver Diseases. Diagnosis and management of autoimmune hepatitis. Hepatology 2010 Jun;
Autoabs in AIH - diagnosis Autoabs anticipate autoimmune disorders for many years (even lifelong). This means: much more autoabs than diseases Diagnostic relevance of autoabs is age-dependent (immune senescence) Threshold of ANA IIF positivity: 1: 80 adults, 1: 20 -1: 10 children. AILD: a few well-defined disorders which can overlap each other. “overlap syndrome”: coexistenxe of features of two distinct AILD. Overlap can occurr also sequentially during time.
Autoabs in AIH - diagnosis - diagnostic, not pathogenic - reflect the abnormal immune regulation underlying the disease - probably result from a molecular mimicry between environmental agents and self antigens, in individuals genetically predisposed to autoimmunity
ANA – SMA IN AIH - frequently (~ 50% patients) associated (ANA and SMA), sometimes longitudinally; when associated, their diagnostic relevance for AIH is higher - disease profile substantially unaffected by type (ANA or SMA), number (either or both) and titer of ANA - SMA - titer can decline under therapy, but goal of therapy is disease remission, not ANA-SMA disappearence!
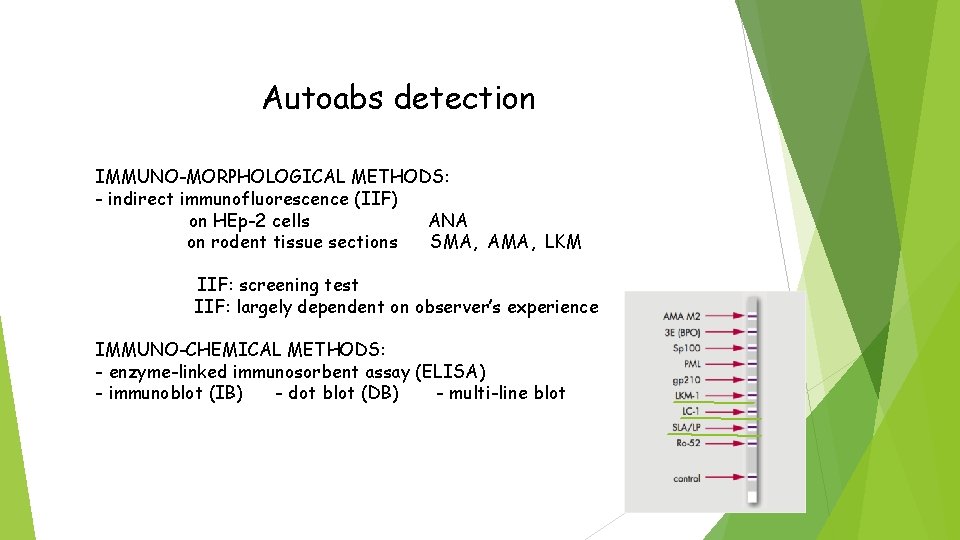
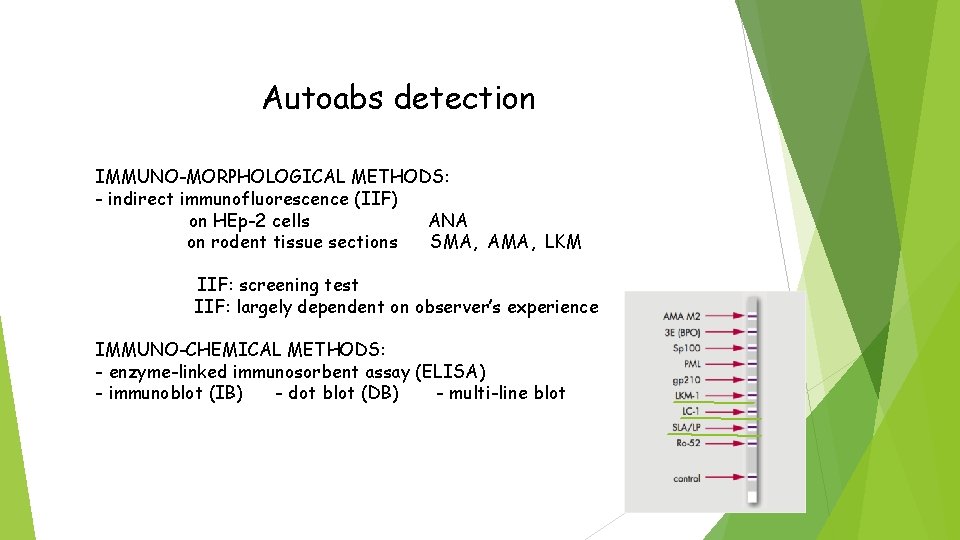
Autoabs detection IMMUNO-MORPHOLOGICAL METHODS: - indirect immunofluorescence (IIF) on HEp-2 cells ANA on rodent tissue sections SMA, AMA, LKM IIF: screening test IIF: largely dependent on observer’s experience IMMUNO-CHEMICAL METHODS: - enzyme-linked immunosorbent assay (ELISA) - immunoblot (IB) - dot blot (DB) - multi-line blot
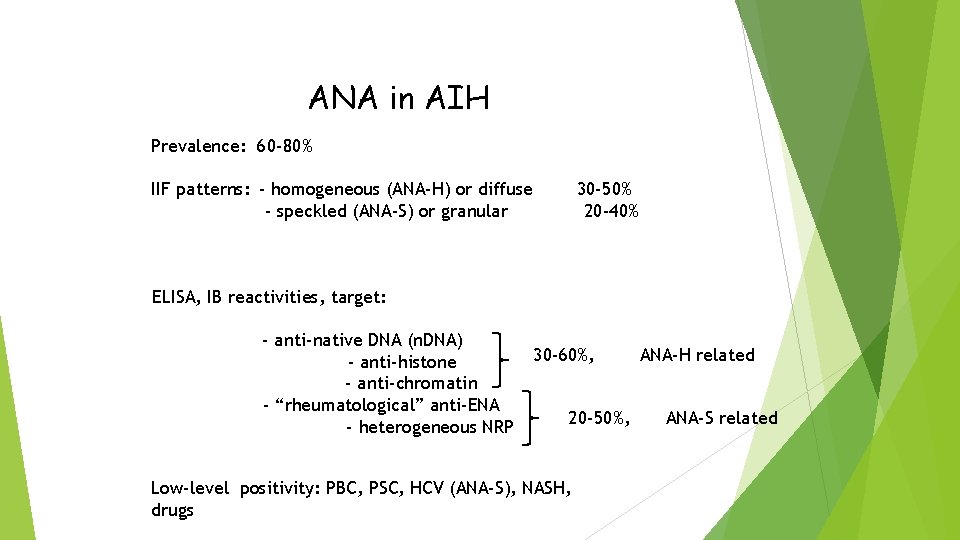
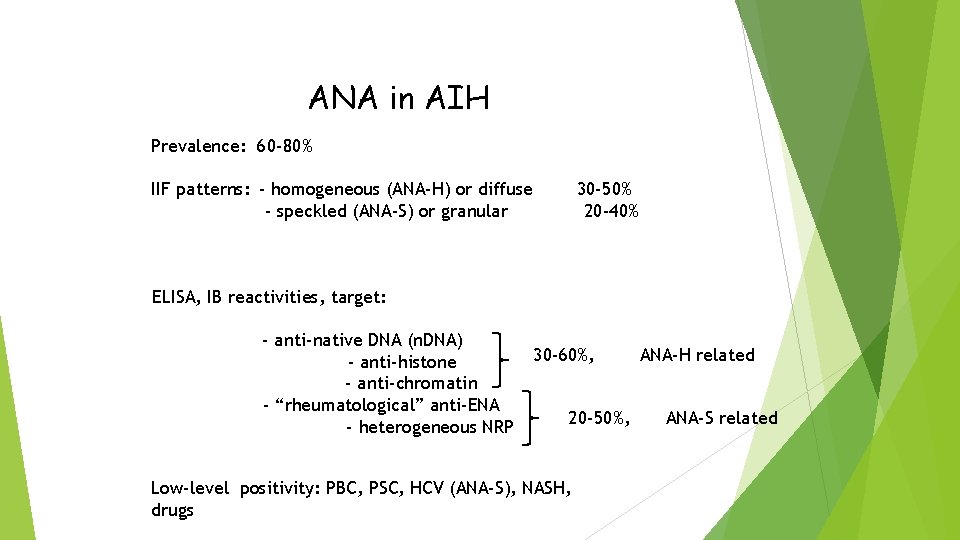
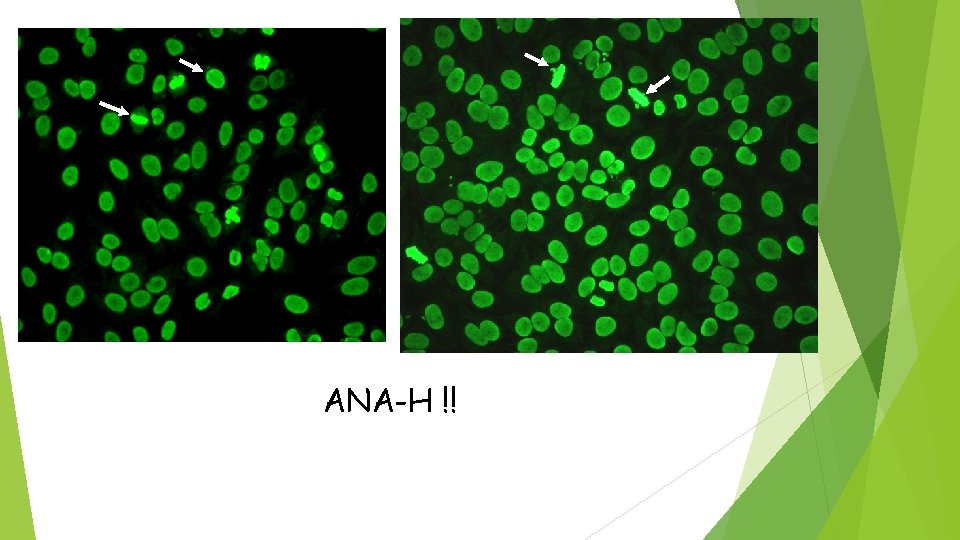
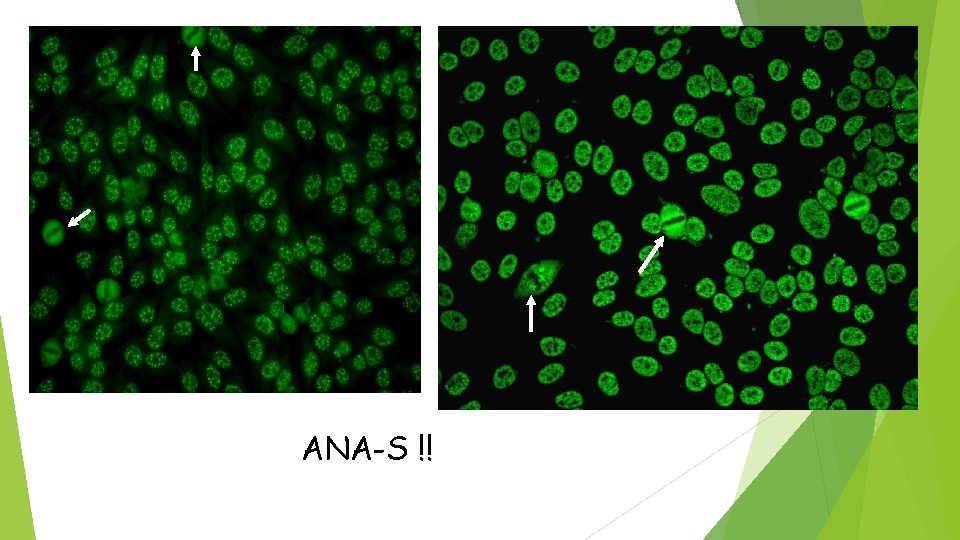
ANA in AIH Prevalence: 60 -80% IIF patterns: - homogeneous (ANA-H) or diffuse - speckled (ANA-S) or granular 30 -50% 20 -40% ELISA, IB reactivities, target: - anti-native DNA (n. DNA) - anti-histone - anti-chromatin - “rheumatological” anti-ENA - heterogeneous NRP 30 -60%, 20 -50%, Low-level positivity: PBC, PSC, HCV (ANA-S), NASH, drugs ANA-H related ANA-S related
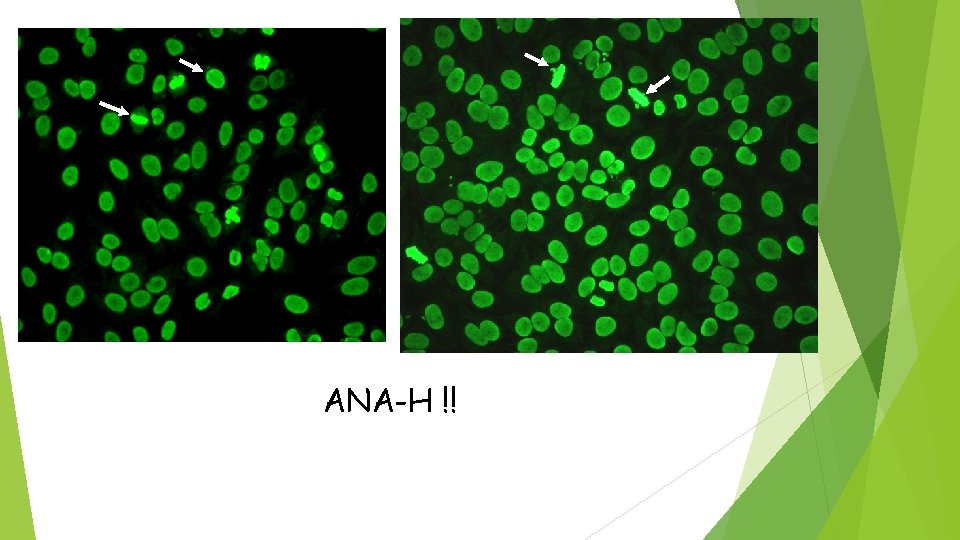
ANA-H !!
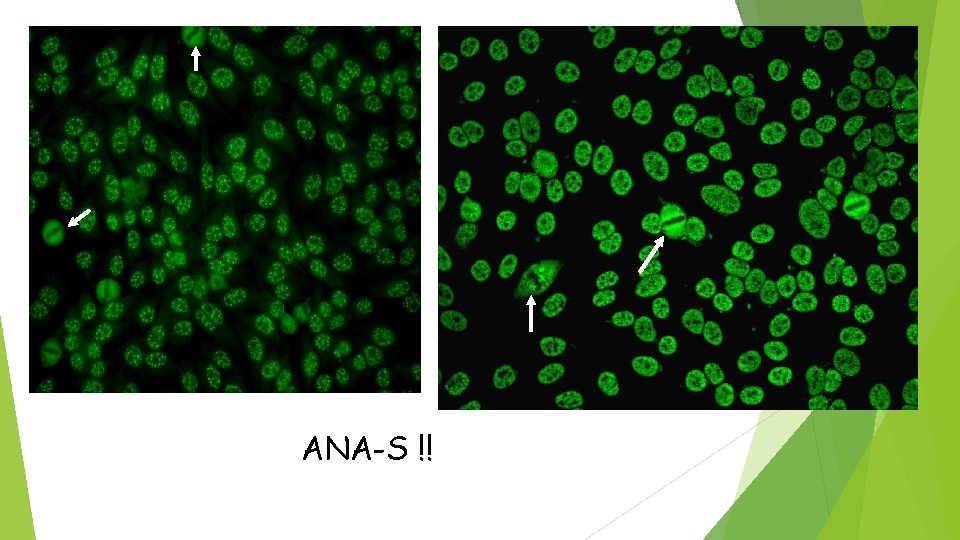
ANA-S !!
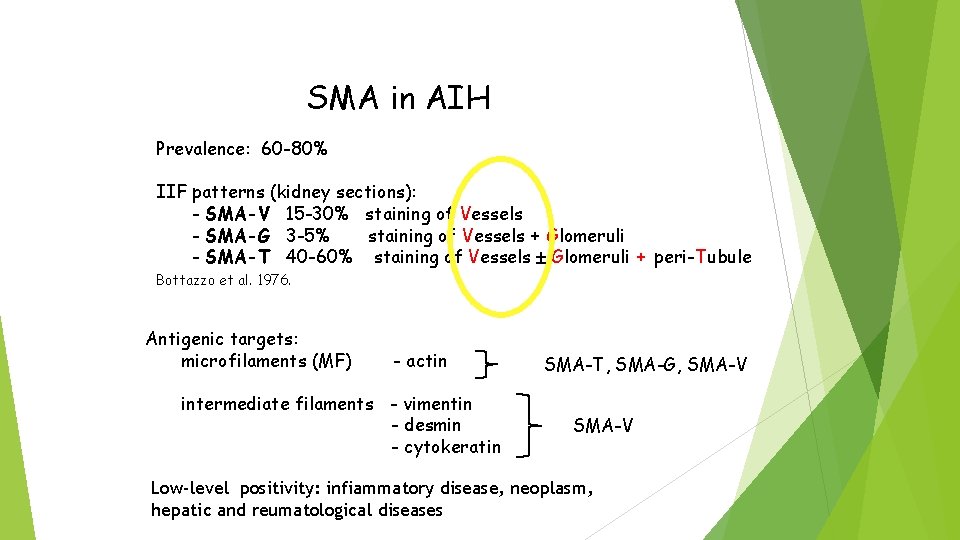
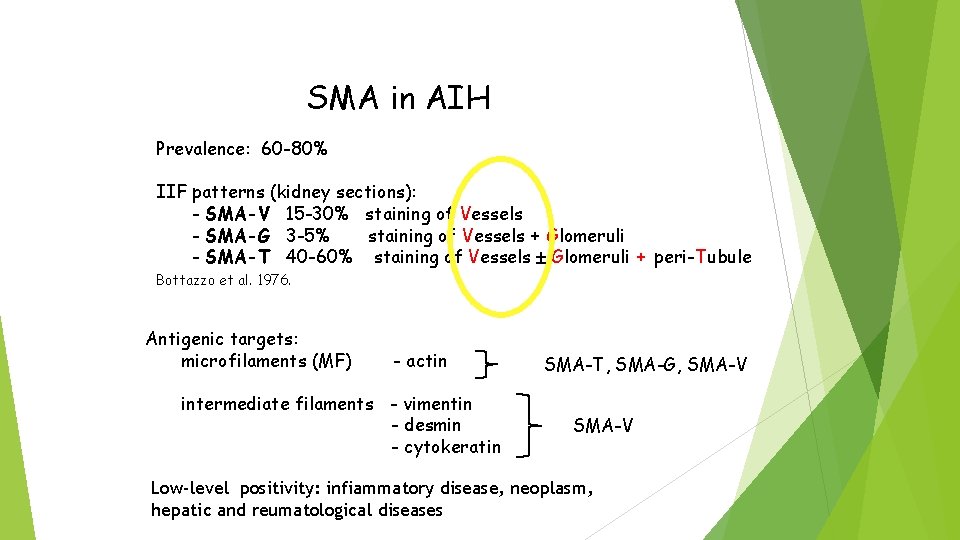
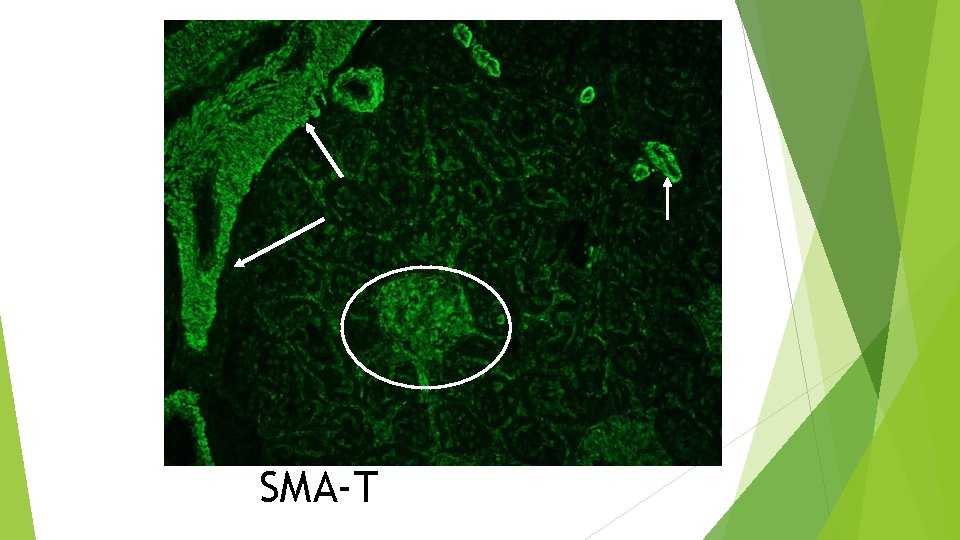
SMA in AIH Prevalence: 60 -80% IIF patterns (kidney sections): - SMA-V 15 -30% staining of Vessels - SMA-G 3 -5% staining of Vessels + Glomeruli - SMA-T 40 -60% staining of Vessels Glomeruli + peri-Tubule Bottazzo et al. 1976. Antigenic targets: microfilaments (MF) - actin intermediate filaments - vimentin - desmin - cytokeratin SMA-T, SMA-G, SMA-V Low-level positivity: infiammatory disease, neoplasm, hepatic and reumatological diseases
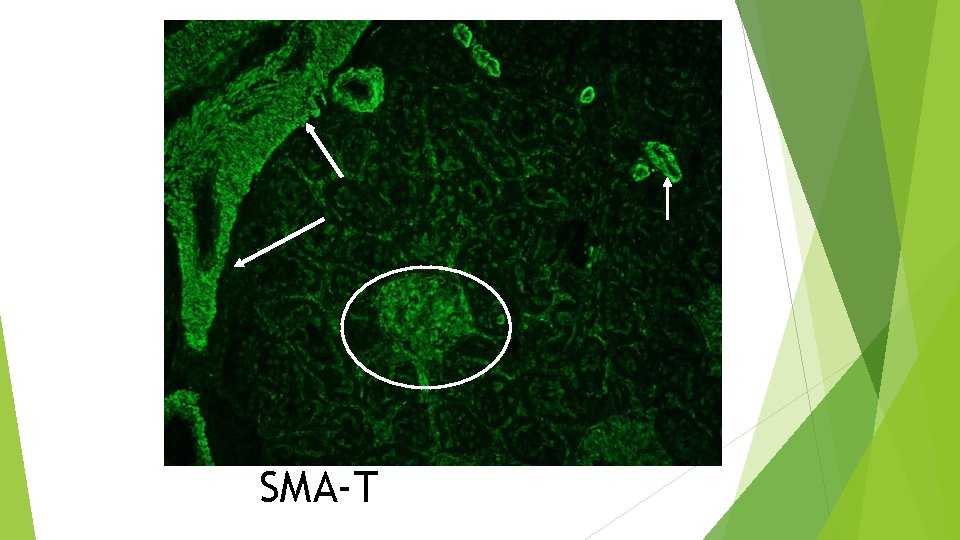
SMA-T
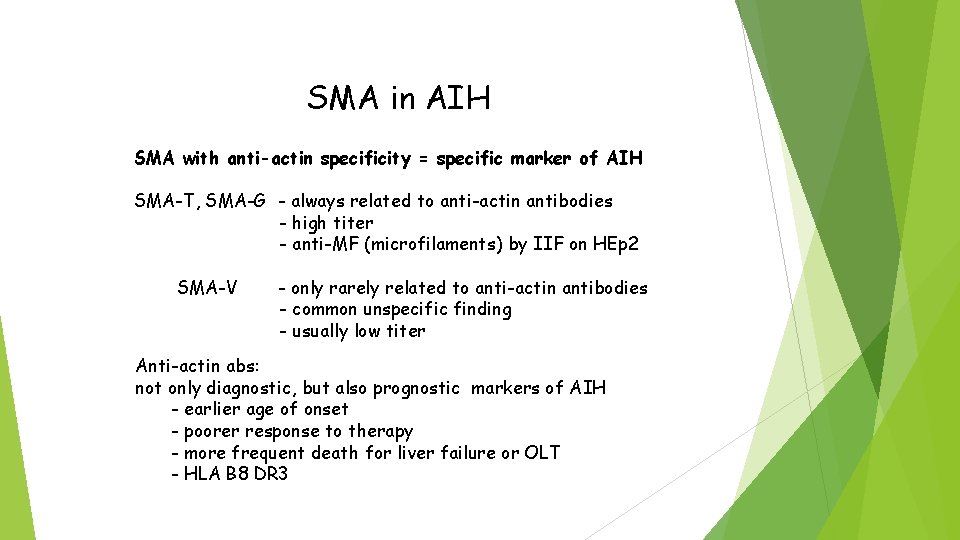
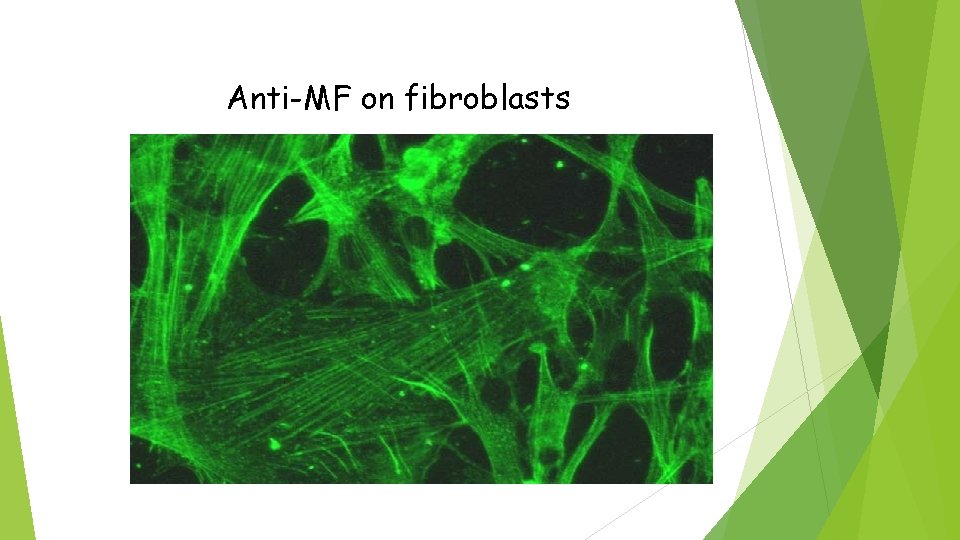
SMA in AIH SMA with anti-actin specificity = specific marker of AIH SMA-T, SMA-G - always related to anti-actin antibodies - high titer - anti-MF (microfilaments) by IIF on HEp 2 SMA-V - only rarely related to anti-actin antibodies - common unspecific finding - usually low titer Anti-actin abs: not only diagnostic, but also prognostic markers of AIH - earlier age of onset - poorer response to therapy - more frequent death for liver failure or OLT - HLA B 8 DR 3
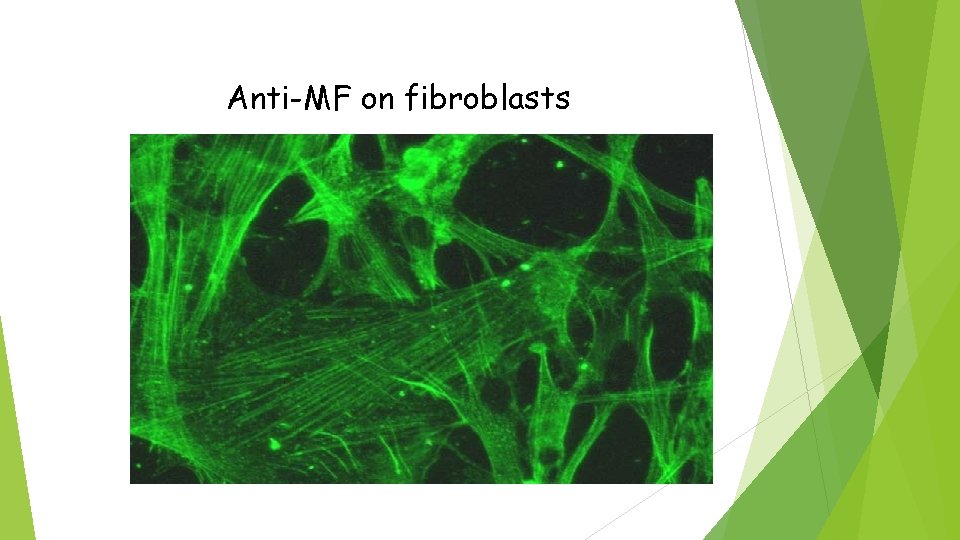
Anti-MF on fibroblasts
Others abs in AIH LC 1 (liver cytosol type 1) with LKM-1, disease activity, early onset of disease, concomitant autoimmune disease Target: formiminotransferase ciclodeaminase, liver metabolic enzime Anti-SLA: soluble liver antigen high specificity (99% of AIH), associated with HLA DRB 1*03 Target: ribonucleoprotein complex (RNP)
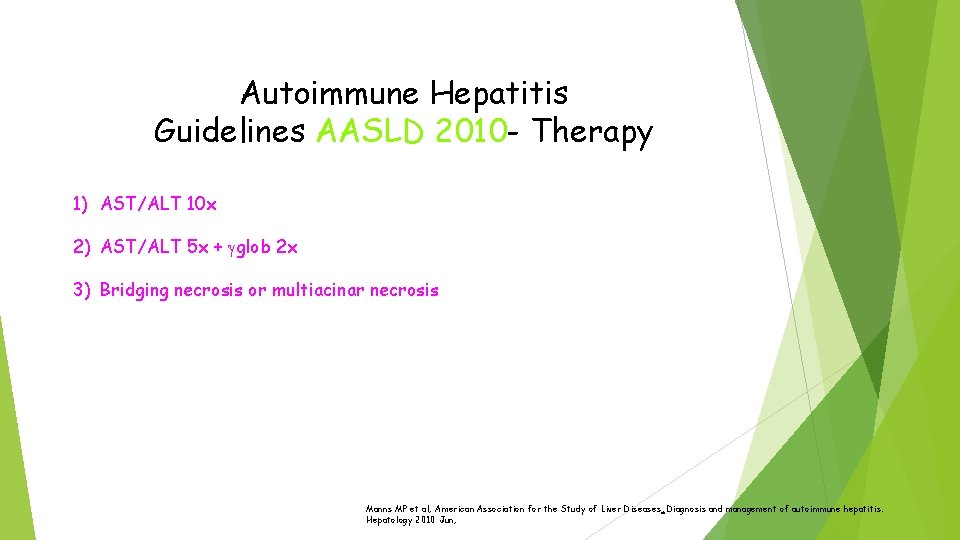
Autoimmune Hepatitis Guidelines AASLD 2010 - Therapy 1) AST/ALT 10 x 2) AST/ALT 5 x + gglob 2 x 3) Bridging necrosis or multiacinar necrosis Manns MP et al; American Association for the Study of Liver Diseases. Diagnosis and management of autoimmune hepatitis. Hepatology 2010 Jun;
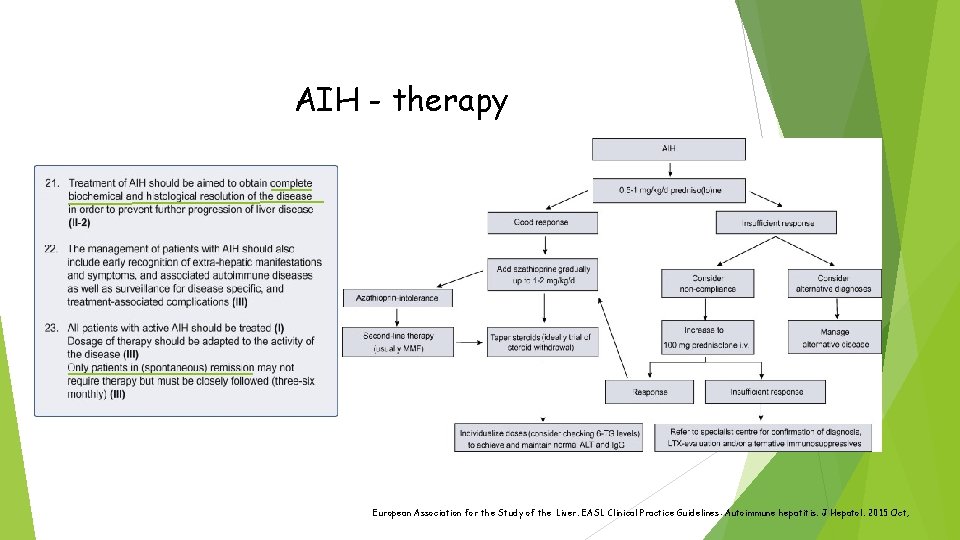
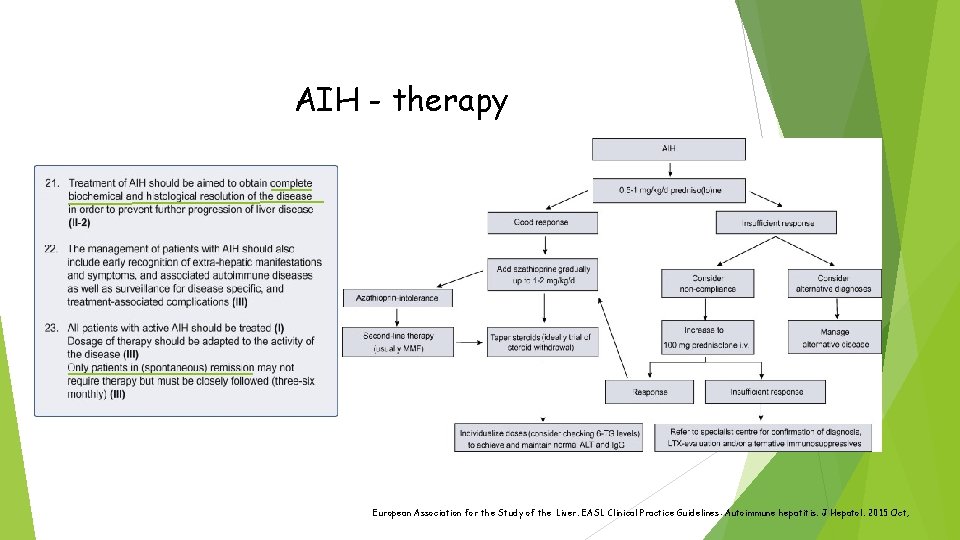
AIH - therapy European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Autoimmune hepatitis. J Hepatol. 2015 Oct;
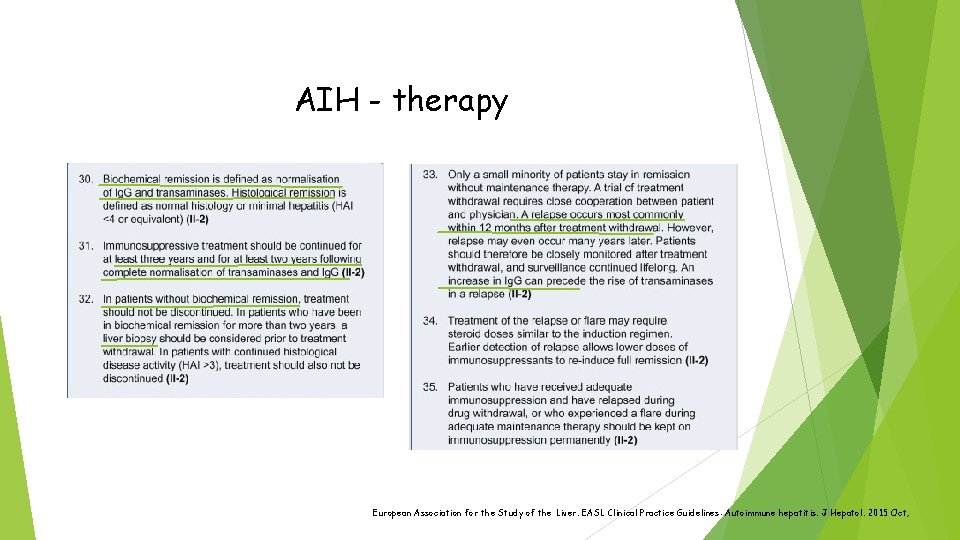
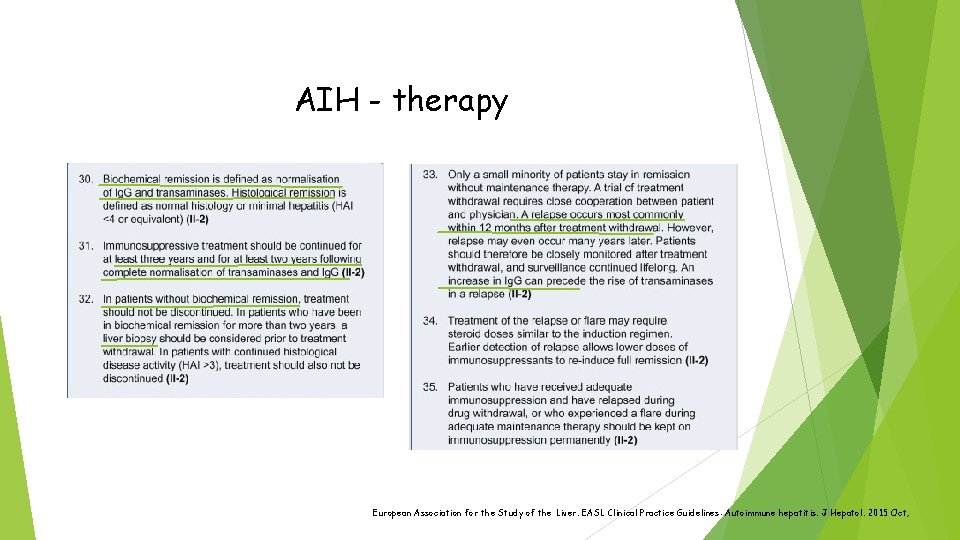
AIH - therapy European Association for the Study of the Liver. EASL Clinical Practice Guidelines: Autoimmune hepatitis. J Hepatol. 2015 Oct;
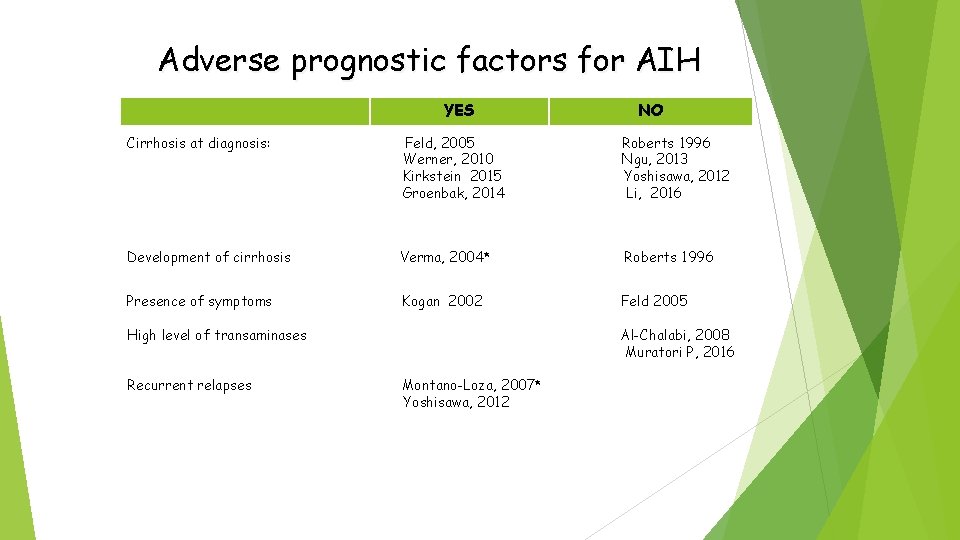
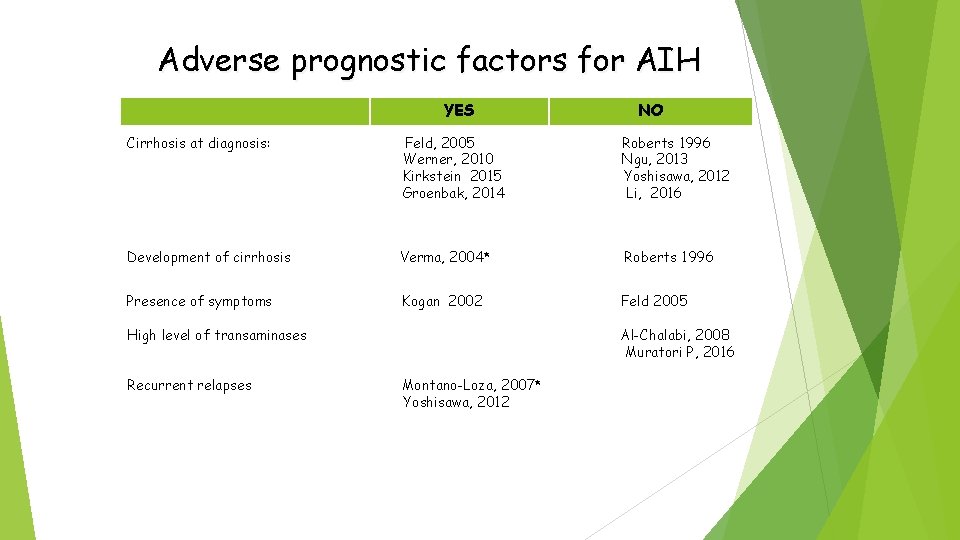
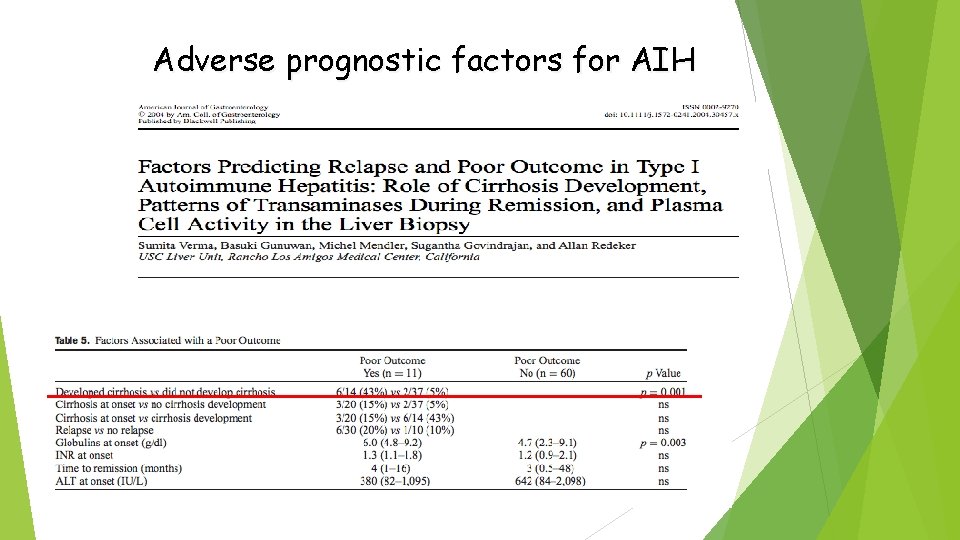
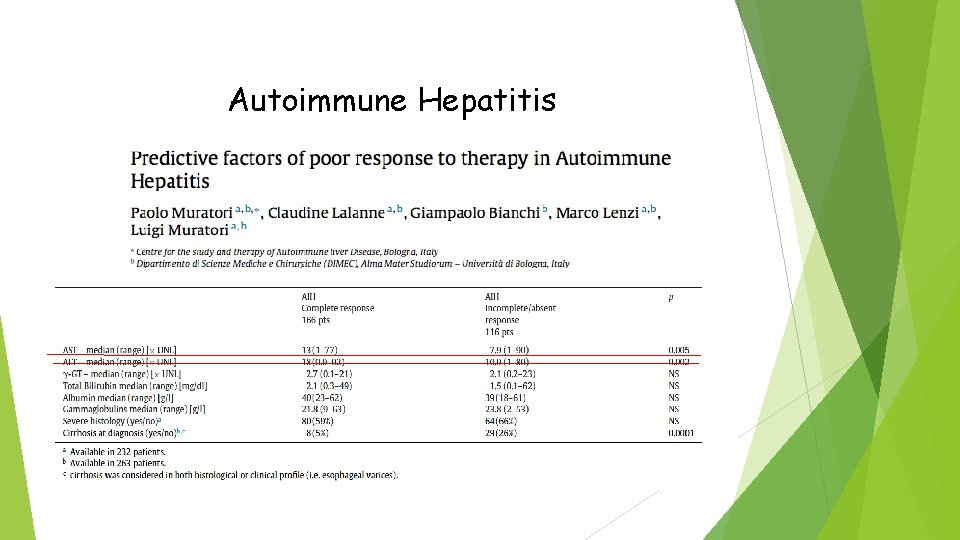
Adverse prognostic factors for AIH YES NO Cirrhosis at diagnosis: Feld, 2005 Werner, 2010 Kirkstein 2015 Groenbak, 2014 Roberts 1996 Ngu, 2013 Yoshisawa, 2012 Li, 2016 Development of cirrhosis Verma, 2004* Roberts 1996 Presence of symptoms Kogan 2002 Feld 2005 High level of transaminases Recurrent relapses Al-Chalabi, 2008 Muratori P, 2016 Montano-Loza, 2007* Yoshisawa, 2012
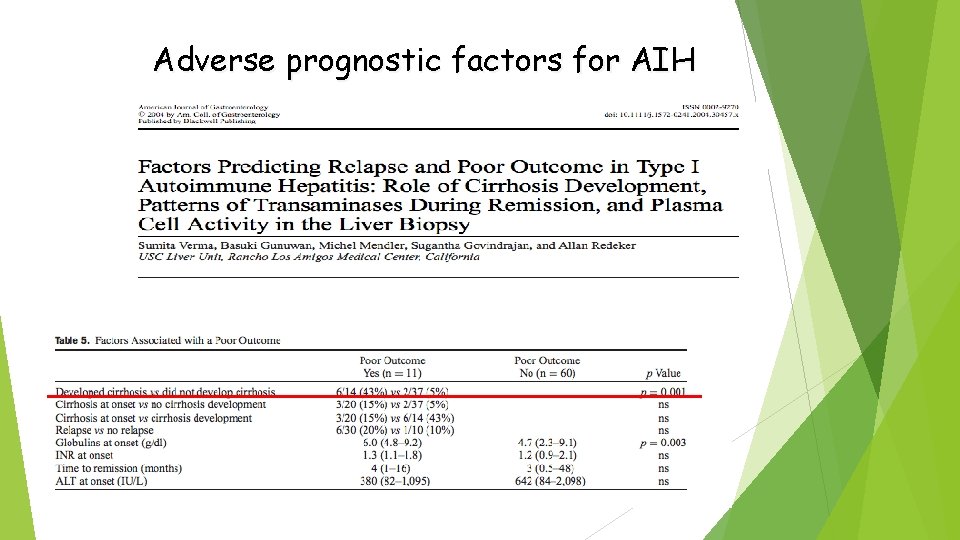
Adverse prognostic factors for AIH
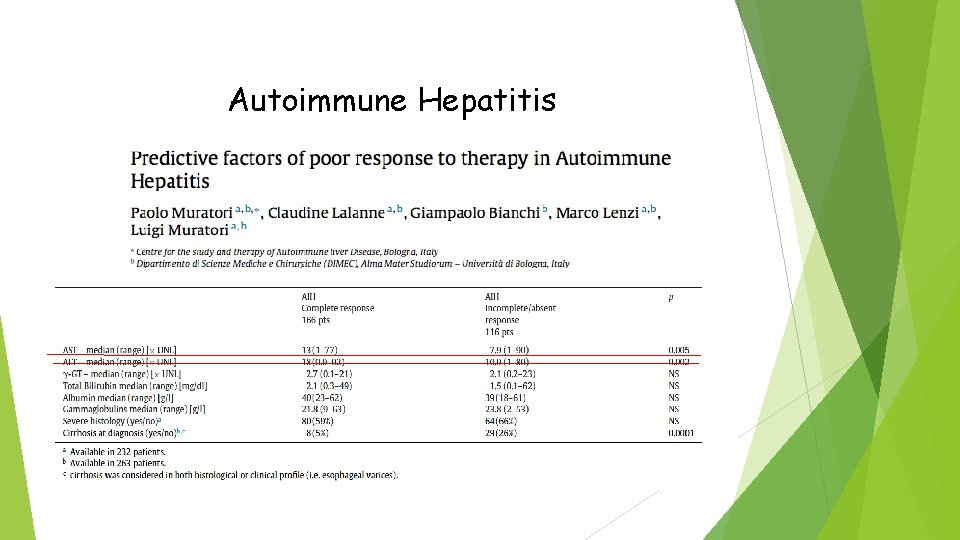
Autoimmune Hepatitis
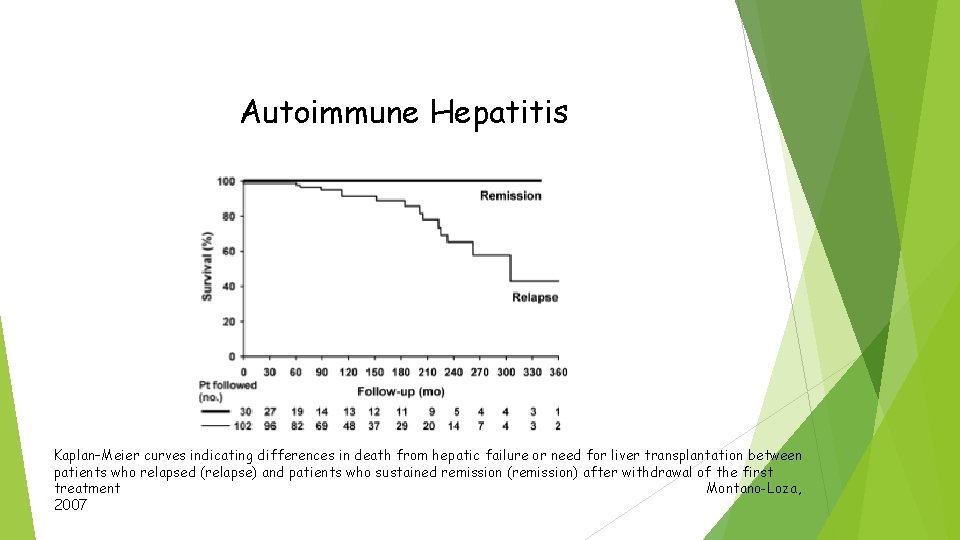
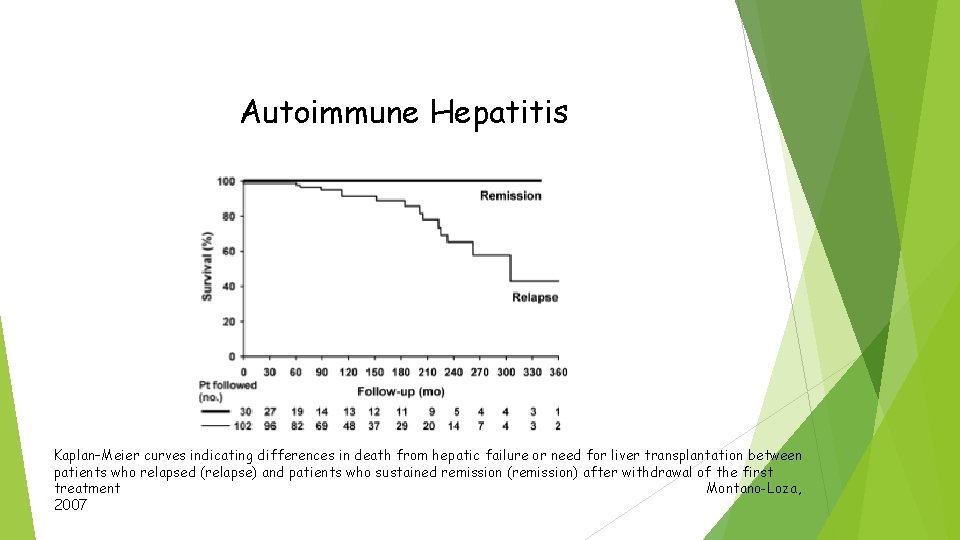
Autoimmune Hepatitis Kaplan–Meier curves indicating differences in death from hepatic failure or need for liver transplantation between patients who relapsed (relapse) and patients who sustained remission (remission) after withdrawal of the first treatment Montano-Loza, 2007
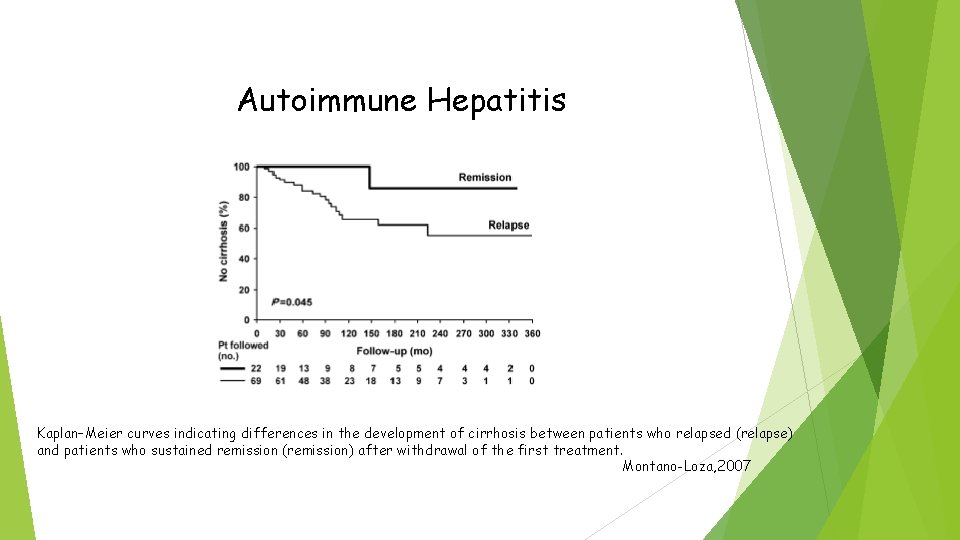
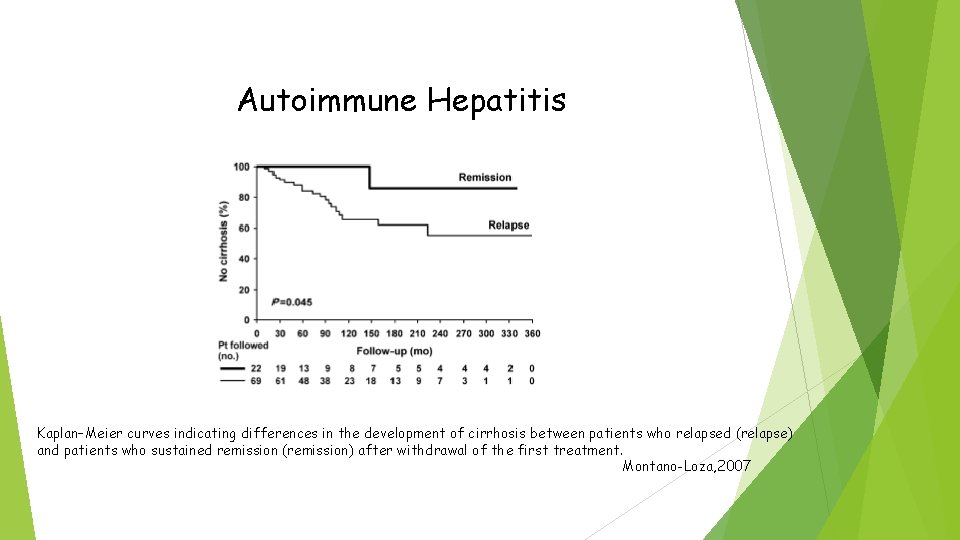
Autoimmune Hepatitis Kaplan–Meier curves indicating differences in the development of cirrhosis between patients who relapsed (relapse) and patients who sustained remission (remission) after withdrawal of the first treatment. Montano-Loza, 2007
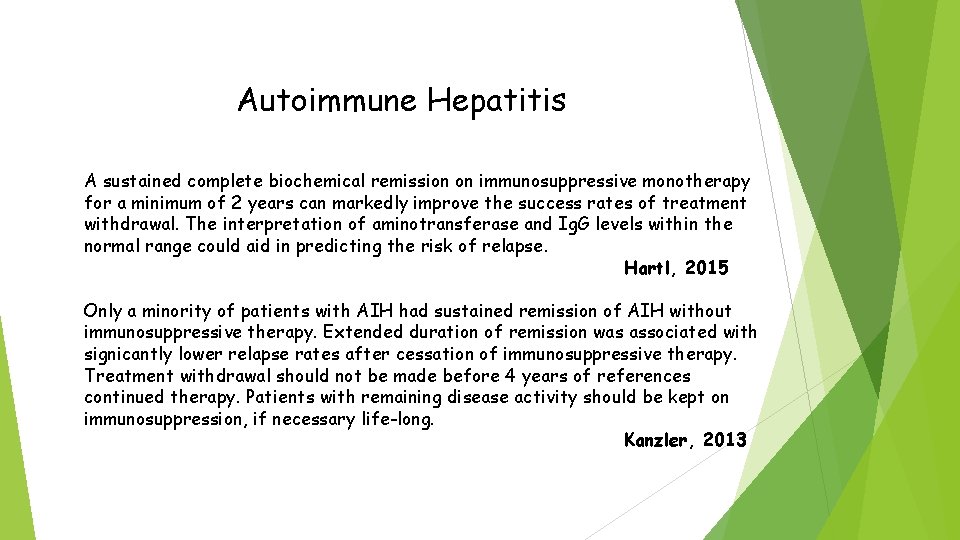
Autoimmune Hepatitis A sustained complete biochemical remission on immunosuppressive monotherapy for a minimum of 2 years can markedly improve the success rates of treatment withdrawal. The interpretation of aminotransferase and Ig. G levels within the normal range could aid in predicting the risk of relapse. Hartl, 2015 Only a minority of patients with AIH had sustained remission of AIH without immunosuppressive therapy. Extended duration of remission was associated with signicantly lower relapse rates after cessation of immunosuppressive therapy. Treatment withdrawal should not be made before 4 years of references continued therapy. Patients with remaining disease activity should be kept on immunosuppression, if necessary life-long. Kanzler, 2013
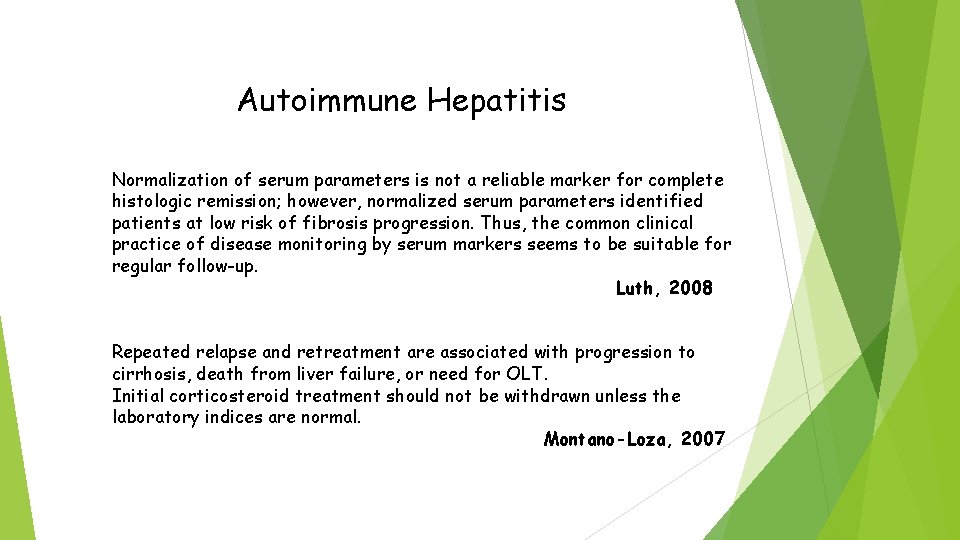
Autoimmune Hepatitis Normalization of serum parameters is not a reliable marker for complete histologic remission; however, normalized serum parameters identified patients at low risk of fibrosis progression. Thus, the common clinical practice of disease monitoring by serum markers seems to be suitable for regular follow-up. Luth, 2008 Repeated relapse and retreatment are associated with progression to cirrhosis, death from liver failure, or need for OLT. Initial corticosteroid treatment should not be withdrawn unless the laboratory indices are normal. Montano-Loza, 2007
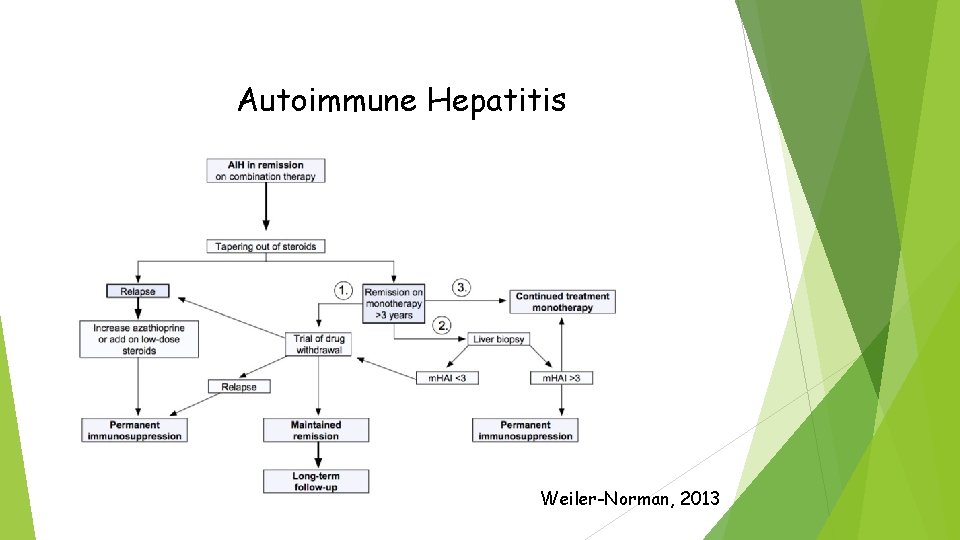
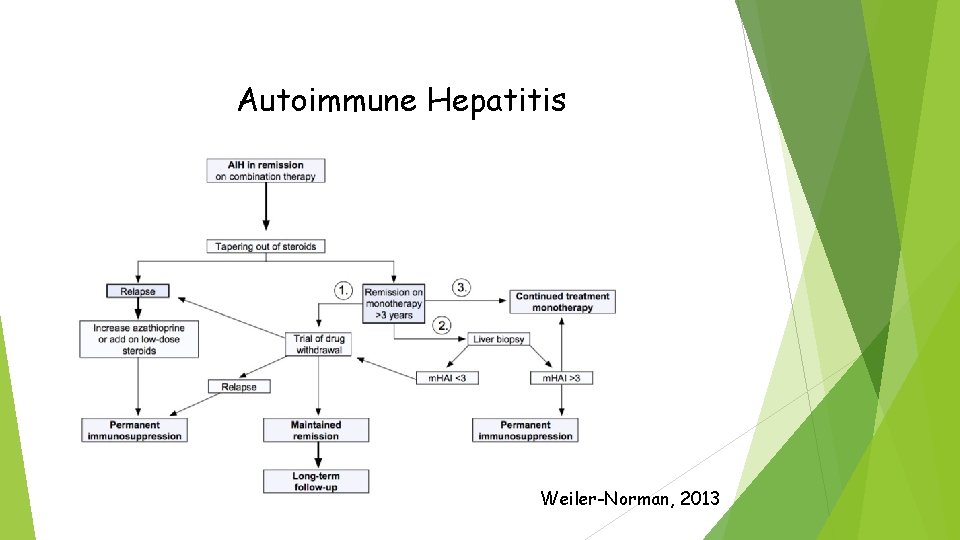
Autoimmune Hepatitis Weiler-Norman, 2013
Autoimmune Hepatitis in pediatric population Acute presentation (50 -60%), also fulminant AIH 2 LKM+ in 38% of cases Alteration biliary tree Therapy: - Treatment withdrawal more successful after at least 3 years of therapy rather than immediately before or during puberty. - Elevated Ig. G is a risk factor for relapse after withdrawal of immunosuppression in adults, but not in children. - Celiac disease guideline suggests screening all patients with AIH for celiac disease. Any formal recommendation to screen patients with AIH for autoimmune thyroid disease. Screening of all children with AIH for celiac disease and thyroid disease should be routine. Mark Deneau, 2014
Conclusions - AIH diagnosis remains a challenge for phisycians. - Multifactorial diagnosis (see AASLD 2010). - Importance of “time to diagnosis”!! - Further research are needed to more fully quantify therapeutic approach.